7
Toward a New Definition of Diversity
DIMENSIONS OF DIVERSITY
One part of the committee’s charge was to review existing theory and research applications in health communication and behavior change, especially as they related to socioculturally and demographically diverse populations. Throughout this volume we have used traditional epidemiological categories to describe disparities in health risks and health outcomes for diverse populations and to characterize the research literature on communication interventions for those populations. However, there is a lack of clarity and consensus about the constructs commonly used for grouping individuals—specifically, race, ethnicity, and culture—as well as what is actually measured in studies that rely on these constructs. This makes the interpretation of the existing literature problematic.
This chapter has two purposes. The first is to comment on the broad demographic categories featured in most population-based descriptions of health status differences and most discussions of disparities. We show that even following such crude indicators, populations are more diverse—and vary more along multiple di-
mensions of demographic differences—than may be commonly assumed. The second purpose of this chapter is to offer an alternative concept of cultural processes that affords a more relevant base from which to understand sociocultural diversity and its implications for health communication. Our recommendations from this chapter stem from the perspective that understanding differences in health status or health behavior requires an examination of sociocultural processes and life experiences. Underlying this perspective is a radical reframing of cultural groupings because current categories are often misused in attempts to explain differences within and across groups. This new perspective suggests a fundamental reorientation in the research agenda.
In the discussion of culture and diversity in this chapter, a number of specific issues are raised, and suggestions are made to address those issues. The issues include:
-
Despite a lack of biological evidence for racial groupings, “race” as a social construct continues to be a reality that is reflected in discriminatory social relationships and actions (racism, discrimination, oppression). For this reason, the construct of “race” matters in our society.
-
Because these key social constructs of “race/ethnicity” (e.g. African-Americans and whites) are correlated, however imperfectly, with socioeconomic indicators, they are useful as rough indicators of health disparities. It is when we want to go beyond rough assessments of the health impacts of socially mediated macro forces that these constructs have little explanatory power, because of intragroup variation and other sociocultural and political factors that may have more important influences on behavior.
-
The identification of health disparities through the use of racial and ethnic categories has also led some to equate diversity with disparity and to contribute to a view that ethnic groups are homogeneous. Neither of these is necessarily the case. In fact, the use of racial/ethnic labels reifies the groups and conveys the sense that these group labels reflect some “cultural reality” in some meaningful way. This implies that the solution lies in dealing with
-
cultural differences even though positing a causal relationship is not warranted by the data.
-
There is also a tension resulting from the focus on “groups” and the tendency to reify culture as a static experience for members of so-called “ethnic groups” versus looking at cultural and social experiences or processes as they affect people’s lives and behavior. With regard to health communication efforts, the lack of a biological basis for grouping human beings means that the only avenue for the positing and creation of “groups” is in society (not in nature). Without race, experience-based constructs remain the main option for categorizing diversity. Highlighting experience does not move attention away from political-economic and structural impacts on health, but rather allows us to better grapple with disentangling and assessing the impact of the socially constructed world on the health of individuals. The sharing of socially mediated life experiences provides the basis for researchers to posit groupings that may be more meaningful for public health research in general.
-
Differences in health risks and health outcomes also may reflect environmental factors ranging from socioeconomic constraints and health care access barriers to poor air quality. Behavioral factors also may be affected by social and environmental parameters and by biological factors.
-
The risk of assuming that people have more power to alter their behavior or their environment than they may actually have can lead to “blaming the victim.”
Problems with Traditional Categories as Used in Federal Statistics
Federal categories focus primarily on so-called “race” and “ethnicity.” Diversity in the United States is culturally and socially constructed. Part of the complexity in talking about diversity is that the naming, grouping, and categorizing of perceived differences among human beings is done from a variety of perspectives, and to achieve a variety of ends.
Contradictions and inconsistencies exist in official use of terms for ethnic groups in the United States (Ahdieh and Hahn, 1996; Hahn, 1992, 1999; Hahn and Stroup, 1994). Pan-ethnic categories such as Asian American and Hispanic are largely arbitrary constructions created by demographers and social scientists for purposes of data development, analysis, and policy (Suárez-Orozco, 2000:14). For example, “Hispanic” was introduced by demographers working for the Bureau of the Census in the 1980s as a way to categorize people who are either historically or culturally connected to the Spanish language. Note that “Hispanic” has no precise meaning regarding racial or national origins, and is rejected by many individuals in favor of other terms, including Latino, Mexican American, or Puerto Rican. In addition, Latinos are white, Black, indigenous, Asian, and every possible combination thereof, and originate in more than 20 countries. They may have just arrived or been in this country for generations, speak Spanish but no English or English but no Spanish. An African-American may have been born in Nigeria, Panama, Barbados, or Britain; have lived in the rural south for generations; or be from the urban north. A Chinese Buddhist and a Filipino Catholic are both considered Asian American, though they may have little in common in terms of language, cultural identity, and sense of self (Suárez-Orozco, 2000:14).
This problem with current categories is recognized in the 1977 Office of Management and Budget (OMB, 1977a) directive, which states:
This directive provides standard classification for record keeping, collection, and preservation of data on race and ethnicity in Federal program administrative reporting and statistical activities. These classifications should not be interpreted as being scientific or anthropological in nature, nor should they be viewed as determinants of eligibility for participation in any Federal program. They have been developed in response to needs expressed by both the executive branch and the Congress to provide for the collection and use of compatible, nonduplicated, exchangeable racial and ethnic data by
Federal agencies [http://www.whitehouse.gov/omb/inforeg/stat97.html#classdata].
These categories are even more problematic. The Hispanic category is directly contrasted with the “race” classification that includes whites, Blacks, American Indians/Alaska Natives, Asians, and Pacific Islanders. Latinos are identified separately as an ethnicity; Latinos can be of any “race.” Thus, the census has racial group categories that include Latinos in the number of persons within each racial group (e.g., whites and Blacks) and racial group categories that exclude the portion of Latinos from the specific racial group (e.g., non-Hispanic whites).
The more recent U.S. census categories represent an attempt to better reflect the country’s increasing diversity. The 2000 census questionnaire is an improvement from the past in that it asks Americans whether they belong to one or more of some 14 “races” (though 4 are considered basic) or to some other race, and whether they are of Spanish/Hispanic/Latino ethnicity (of which there are 3 basic varieties and an additional fill-in-the-blank option).
Race
Discussions about race can be seen as grounded in perceived biological and physical differences. Problems with this view are discussed in several recent Institute of Medicine reports (1999c, 2000) and in the anthropological and public health literature, as we will describe.
The concept of biological race is inconsistent with scientific data to the extent that “race” is not a useful shorthand for human variation (Goodman, 2001:34). Goodman notes that:
The first leap [of illogic] is a form of geneticization, the belief that most biology and behavior are located “in the genes”. . . . Genes, of course, are often part of the complex web of disease causality, but almost always a minor, unstable and insufficient cause. The presence of GM allotype, for example, might correlate to increased rates
of diabetes in Native Americans, but the causal link is unknown. In other cases, the gene is not expressed without some environmental context, and it may interact with environments and other genes in nonadditive and unpredictable ways (Goodman 2000:700).
This concept has been confirmed recently by the results of the Human Genome Project, which, Collins and Mansoura noted (2001:221), “has helped to inform us about how remarkably similar all human beings are—99.9 percent at the DNA level. Those who wish to draw precise racial boundaries around certain groups will not be able to use science as a legitimate justification.” Goodman (2000:701) wrote more on the subject:
The attribution of racial differences in disease to genetic differences illustrates both geneticization and scientific racialism. For example, the rise in diabetes among some Native Americans is often thought to be caused by a genetic variation that separates Native Americans from European Americans. Type II diabetes, along with obesity, gallstones, and heart disease, is part of what has been called “New World Syndrome.” Contemporary variation in diabetes rates among Native North American groups is tremendous, however, and the rise in diabetes rates is a relatively recent phenomenon. Other groups experiencing shifts from complex carbohydrates to colas, from fast-moving foods to fast foods, and from exercise to underemployment have experienced very similar increases in diabetes rates. Rather than accept that diabetes is “in our blood” as articulated by the Pima [Indians], it might be more productive to locate diabetes in changeable lifestyles.
Sickle-cell anemia provides another good example of the problems inherent in racial reasoning. (Sickle cell anemia is not a “racial disease,” but a characteristic of some local populations.) Livingstone’s (1962) intervention four decades ago demonstrated that the frequency of this genetic trait is found among populations in tropical ecological niches in Africa as well as in certain environments in southern Europe and western Asia. He underscored the point that if sickle cell were “racial,” then the so-called “race” that
exhibits it “[consists] of some Greeks, Italians, Turks, Arabs, Africans, and Indians” (Livingstone, 1962:280).
“Race” may be biological and genetically meaningless, but racially defined concepts, based on presumptions of underlying biological differences, abound in the United States. The nation has the legacy of decisions like the 1896 Plessy versus Ferguson ruling, which declared a man Black on the basis of one Black ancestor among his eight grandparents (Davis, 1991). Another illustration is the debate over “blood quantum” within some Native American communities that has led to polarized positions and deep divisions over how much Native American blood is necessary for one to be considered a Native American and/or to hold tribal membership.
Racism, or the negative treatment of individuals based on perceptions of race, has been demonstrated to have negative effects on health. Krieger’s (2000) recent chapter presented a comprehensive summary of “discrimination and health.” James et al. (1984), Dressler (1990, 1991), and Krieger and Sidney (1996) demonstrated the relationship between self-reported experiences of discrimination and blood pressure. Many argue that epidemiological data may need to continue to be collected on the “social” categories of “race” in addition to the more logical categories of life experiences, cultural processes, and self-identity (discussed later in this chapter).
Race matters because the United States is not a colorblind society and the experience of race and racism (more than the genetics of race) has health consequences. Like other social constructs, races are often real cultural entities. For many people, membership in a racial group constitutes an important part of their social identity and self-image. “Because race and racism are sociopolitical realities, they affect individual biologies. Understanding this presents a new and radical biocultural agenda. The continuance of race and ethnic differences in health calls for an explication of the biology of inequality and racism” (Goodman, 2001:31).
Ironically, because of inequalities, groups often argue for increased political clout based on the numbers in the group—the bigger the group, the better. This is one reason Native Americans
find it acceptable to be grouped together under an umbrella term, even while advocating the need for tribe-specific data. Nobles (2000:1745) notes that “racial categories on censuses do not merely capture demographic realities, but rather reflect and help to create political realities and ways of thinking and seeing.” Furthermore, civil rights organizations have claimed racial categories (legal and census) have been bases of discrimination and thus bases of remedy. Racial categorization and racial data are now sometimes seen as having positive benefits, including providing a way to track the effects of racism.
A 1993 Centers for Disease Control and Prevention (CDC)/ Agency for Toxic Substances and Disease Registry (ATSDR) Workshop (Centers for Disease Control and Prevention, 1993: http://www.rice.edu/projects/HispanicHealth/mmwr.html) on the topic generated the following statements:
-
Emphasis on race and ethnicity in public health surveillance diverts attention from underlying risk factors.
-
Despite the potential limitations of the categories of race and ethnicity, such information can assist in public health efforts to recognize disparities between groups for a variety of health outcomes.
-
In all reports and other uses of surveillance data, the reason for analyzing race and/or ethnicity should be given, approaches to measurement of race and ethnicity should be specified, and findings should be interpreted.
This tension between the lack of scientific validity for the current ways in which Americans are categorized by OMB and other government agencies and the reality of racism and its effects was debated extensively by our committee. We agree that “race” is an inaccurate concept biologically and that direct and indirect effects of racism on health need to be acknowledged and measured. Data continue to be collected, based on the rather arbitrary OMB, census, and other classifications, which means demographic and epidemiological data exist using only those classifications. These data
must be cited in order to make any statements about the distribution of populations across the country and about health disparities; however, it is important to work toward more sophisticated and accurate ways of understanding and describing the American people (Office of Management and Budget, 1997a, 1997b).
Reformulating Diversity as a Sociocultural Process
Culture
The concept of culture highlights the general potential for human beings to learn through social means, such as interaction with others and through the products of culture, such as books and television. Reliance on tools and symbolic resources, notably language, are hallmarks of culture. Language is central to social life and to acquiring cultural knowledge. Language “provides the most complex system of the classification of experience” and is “the most flexible and most powerful tool developed by humans” (Duranti, 1997:49 and 7). In addition, nonverbal-embodied ways of knowing and being take particular form in specific settings. Language also involves subtleties of meaning. For example, in one study the word “trauma” meant “injury” to a neurologist talking to the Mexican mother of a child with seizure disorders, but was often interpreted as “emotional shock” by the mother (Long, Scrimshaw, and Hernandez, 1992). Many words and phrases have no exact translation into another language because of subtleties of meaning.
It is important to note that culture is something we all have. “There is no such thing as a human nature independent of culture,” noted Geertz (1973:49). Culture is the “way of life and thought that we construct, negotiate, institutionalize, and finally . . . end up calling ‘reality’ to comfort ourselves” (Bruner, 1996:87), and culturally grounded taken-for-granted knowledge is “often transparent to those who use it. Once learned, it becomes what one sees with, but seldom what one sees” (Hutchins, 1980:12). Ways of physically being in the world, such as bodily experience
and the use of space, also assume cultural form without entering conscious apprehension. Culture has many definitions, but most include the following basic concepts:
-
Culture includes shared ideas, meanings, and values;
-
Culture is socially learned, not genetically transmitted;
-
Culture includes patterns of behavior that are guided by these shared ideas, meanings and values;
-
Culture is constantly being modified through “life experiences”; and
-
Culture often exists at an unconscious or implicit level.
Many people believe that specific culture can be recognized by culturally characteristic ways of being, but it is more complex than that. Although discussing culture in this way is often useful, it raises the risk of stereotyping. Intracultural variation—change and variation within a cultural group—occurs constantly. These variations occur among individuals in the same setting, across generations, between genders, across geographic and rural urban settings, and so on. As a counterpoint, much is shared across apparently diverse “cultures.” For example, many U.S. television shows can be viewed in local languages in many countries. Similarly, “McDonalds” is found in most countries today.
Ethnicity
The term “ethnic group” was rarely used in anthropology before the mid-1950s. It appeared, in part, as a substitute for “race” and “tribe” and as a synonym for “cultural group” (Zenner, 1996:393). Although social science discussions of this concept proliferated and no longer assume a one-to-one relationship between ethnic identity and culture, ethnic (or “racial”) groups are often talked about as bounded entities, with each one having a “culture.” This view of culture assumes that people’s behavior is locked in by their culture, an assumption that is incorrect and of-
ten resented as stereotyping. Imposed typologies that operationalize “ethnicity” in terms of checkboxes may, at times, be cast too broadly to relate to any meaningful discussion of cultural and social processes. As discussed earlier, examples include the conjunction of “Asian and Pacific Islander,” in which many diverse groups with distinct histories are placed together, and “Hispanic,” which includes people of many different origins and appearances. Ethnicity does imply some sharing of life experience and learned traditions, including meanings and values. These usually involve a shared group experience embedded in socially grounded processes, yet shared group experiences often are assumed to be a group’s culture.
Cultural and Social Processes
Anthropologists have become wary of talking about culture in ways that suggest bounded entities characterized by stability, internal coherence, and homogeneity, with members of a culture recognizable by a set of stereotypical characteristics that are generationally reproduced. Much less constancy across time and much more intracultural variation exists within any social group than a discrete notion of a “culture” admits. As Sapir noted (1985:515), “The true locus of culture is in the specific interactions of individuals and, on the subjective side, in the world of meanings which each one of these individuals may unconsciously abstract for himself from his participation in these interactions.”
The concept of cultural processes allows us to highlight the connections among life experiences, learning, and sharing. By learning about, belonging to, or participating in social groups, individuals become exposed to ways of thinking about the world (or specific aspects of the world) and ways of acting and responding. Culturally acquired knowledge also may reflect understandings gained through cultural products, such as books, television shows, and computer software (Garro, 2000).
Cultural processes are socially grounded ways of learning that contribute to the way an individual thinks, feels, and acts. Indi-
vidual lives are embedded in a variety of cultural processes that shape the individual, although not in a deterministic fashion. For example, children who grow up in different parts of the United States, but who watch the same television programs and play similar children’s games, come to share cultural understandings through their exposure to and participation in similar activities. To the extent that these life experiences differ from those of their parents, their parents will not be influenced by these same cultural processes and will differ from their children by not sharing in these same sources of experience. A strength of the concept of cultural processes is that it allows us to see individuals as unique and complex, but still exemplifying culture. It facilitates the understanding of the complexity of the multiple social and cultural influences that contribute to and shape who we are, what we do, and how we live (Garro, 2001, in press).
Paying attention to the broader community context is also important. The endorsement of the concept of cultural processes embedded in socially grounded processes that shape ways of learning and contribute to how an individual thinks, feels, and acts led the committee to adopt the concept of a “community of relevance” as fundamental to discussions on communication. Cultural processes unfold through many potential sources of shared learning, such as shared group experiences that are part of ethnic communities, training programs and professional behavior that is learned for a specific occupation, education, age, religion, language, gender, and generation. All of these sources may provide a basis for complex social groupings and contribute to intracultural variation because individuals participate in, or are exposed to, different cultural processes. Framing a message should be based on identifying the salient features for a recognized group, a subgroup, or a new composite collective based on other priorities such as region or language, which then form the community of relevance for a specific health issue, health condition, problem, or communication objective. Understanding the audience and the context it brings to the message is the first step in designing health communication interventions.
The concepts of life experiences and cultural processes need to be put into operation so that they can be used effectively in understanding and changing health behavior through communication. One way to describe these is the concept of experiential identity. Experiential identity represents the characteristics of an individual in terms of culture of origin, language, age, and gender combined with life experiences and cultural processes. Thus, someone whose parents come from different cultural and linguistic groups may have grown up in a multicultural city, lived in a rural area during college, and moved to another city with a different cultural mix from the city of origin. All of these experiences, including the learning of a profession, contribute to the individual’s experiential identity. Experiential identity may be important in assessment of individual response to behavior change strategies, but most communication for behavioral change strategies examined in this volume focuses on groups. The individual is at the intersection of life experiences that are shared by others. Individuals are impacted by intersecting strands of social and cultural processes, and the strands, alone or grouped, rather than the individuals, provide the basis for health communication efforts that go beyond the individual level. Common grouping variables—age, occupation, gender—indicate greater likelihood of shared experiences among individuals, but the markers only help direct attention; they are not the focus of interest in themselves.
Good and Good (1981) discuss a meaning-centered approach to clinical practice, including some principles that could be extrapolated from application to individuals to use in the development of measures for groups. As derived from their text, these include:
-
Groups vary in their style of medical complaints.
-
Groups vary in the nature of their anxiety about the meaning of symptoms;
-
Groups vary in their focus on organ systems; and
-
Groups vary in their response to therapeutic strategies.
Human illness is fundamentally semantic or meaningful. (It may have a biological base, but it is a human experience.) Clinical practice is inherently interpretive. Practitioners must elicit patients’ requests; elicit and decode patients’ semantic networks; distinguish disease and illness and develop plans for managing problems; elicit explanatory modes from patients and families; and analyze conflict among biomedical models and negotiate alternative treatment regimens.
Adapting these principles to communication strategies for groups should help to avoid stereotyping, while analyzing characteristics that may influence the acceptability and success of the strategies (Good and Good, 1981).
Both behavior change theories (discussed in Chapter 2) and social marketing strategies (discussed in Chapter 3) contain the tools to assess individual beliefs, knowledge, and attitudes without relying on rigid categories. It is essential to use these existing tools to assess populations, rather than to make assumptions based on superficial characteristics.
Social Discrimination and Health Outcomes
In the United States, whether framed as ethnicity (e.g., Mexican American) or socially constructed as race (e.g., American Indian by the U.S. census), people of color and/or those who speak a language other than English may be treated differently and in ways that lead to poorer health outcomes. Existing evidence on poor health outcomes for particular populations supports an interpretation that links poor health with factors such as poverty, discrimination, lack of access to adequate health care, and poor nutrition.
Frequently observed differences in behavior often are attributed to “culture” without careful analysis and/or consideration of alternative hypotheses, such as the impact of the broader social/ political/economic context on health behavior. For example, Young and Garro (1982, 1994) looked at treatment decision making in a rural Purépecha (Tarascan) community in Mexico, where “cultural beliefs” and “preferences” for local curanderos (curers)
previously had been suggested as reasons why community members consulted infrequently with physicians. However, it was found that community members generally believed that biomedical treatment was compatible with their own understanding about illness. They did, in fact, believe biomedical treatment would result in a cure compared to their other alternatives. The relative inaccessibility of physician services, including the high costs and transportation difficulties, accounted for the observed pattern of treatment actions. This finding suggests that behavior patterns in physician consultation will be impacted not by educational efforts directed at changing cultural beliefs, but rather by reducing the financial and structural limitations that keep community members from seeking a physician’s care.
Beliefs and behaviors regarding health and illness are influenced by culture and vary by “ethnicity” (Kleinman, 1980, 1986; Lindenbaum and Lock, 1993; Good and Good, 1981; Hunt et al., 1998; Rubel, O’Nell, and Collado-Ardon, 1984; Rubel and Garro, 1992; Nichter, 1981). The critique of cultural groups and the construct of “ethnicity” in this chapter applies to the terms as used in the past by anthropologists as well as demographers. Yet, as noted, people with common cultural processes and life experiences will be more likely to share health-related beliefs and behaviors. “Definitions of health are inherently subjective, influenced by the dialectic between the body and the self,” noted McElroy and Jezewski (2000:191), who diagrammed the analytic domains in the experience of health and illness to include individual (e.g., age, gender, genetics, health history), microcultural (e.g., ethnicity, socioeconomic status), and macrocultural (e.g., economy, environment, health care systems) factors (2000:192). The multitude of cultural, individual experience, ethnic, biological, social, economic, environmental, and other factors complicates analyses of influences on health and illness in general and on health disparities in particular. This complexity has led to the tendency to isolate one or two factors, rather than to consider the complex whole. This is necessary, but researchers need to be aware that they are selecting factors out of context. The key is to select the relevant factors.
Also, as noted earlier, there is a tendency for the onus for health problems to be put on the individual, to “blame the victim.”
Some ethnic groups or cultural groups are more likely to be impoverished, which affects their health status. The committee concluded that none of the current terms, including “race,” ethnicity, and culture (interpreted as cultural group), successfully captures the complexity of people’s experiences and contexts, which may explain the disparate health risks and outcomes found in American society. Thus, in order to understand and, ultimately, to contribute to the elimination of health disparities, we should think in terms of cultural processes and examine how the life experiences of people may be impacted by social forces, such as discrimination, that are based on perceptions of difference. For this reason, breaking out of ethnic and cultural boundaries to embrace the concept of experiential identity is important.
It is not within the scope of this volume to operationalize the concepts of cultural group identity proposed here. It is important for future committees or task forces to work toward ways of operationalizing “cultural group identity” that would serve as markers of increased likelihood of shared experiences among those identifying with a cultural group.
CULTURAL COMPETENCE AND HEALTH COMMUNICATION
Cultural competence has been investigated largely in the context of the delivery of health services in clinical contexts. The field of cultural competency is based on an underlying belief that disparities in health outcomes are the result of a range of social factors, including race/ethnicity, education, socioeconomic position, gender, age, and sexual orientation. A wide range of models has been offered; many of the models use cases to illustrate key points. Systematic research rarely has been applied to develop or test existing models.
Models of cultural competency and tools to assess the capacity of organizations to serve cross-cultural populations, and those de-
signed to help practitioners provide cross-cultural services and care, point to the importance of attending to the social context of health behaviors when providing health services and when designing health communications. Models of cultural competency offer a variety of definitions that attempt to capture or expand on five elements considered essential to providing culturally competent health care across cultures. These elements are as follows:
-
Valuing diversity;
-
Developing the capacity for self-assessment;
-
Raising awareness of dynamics inherent when cultures interact;
-
Using organizational processes to institutionalize cultural knowledge; and
-
Striving to develop individual and organizational adaptations to diversity.
Cultural competency models incorporate how individuals, organizations, and society at large interface with, influence, and are influenced by cultural artifacts, such as language, beliefs, and practices (Cross et al., 1989; Leininger, 1978; Tirado, 1996; Campinha-Bacote, 1994). Attitudes and beliefs and the behaviors they produce are the basis of interactions at all levels. The interpersonal dimension includes the attitudes and consciousness of individuals. Organizational contexts created by policies and procedures, leadership attitudes, and other factors also influence and reinforce individual responses that contribute to a health care organization’s ability to competently serve diverse populations. In addition, cultural competency models suggest that the way society influences individuals, their communities, and health care organizations needs to be considered.
The concept of cultural competency only recently has begun to enter the health service literature. Because of its origins outside of academia and its recent appearance in the research literature, the discussion of cultural competence tends to be largely conceptual in nature.
Cultural competency implies more than beliefs, attitudes, and tolerance. It includes the ability to act appropriately in the context of daily interactions with individuals who are culturally unlike the health care providers. The providers and provider organizations need to honor and respect beliefs, interpersonal styles, and attitudes and behaviors of recipients. Cultural awareness is the deliberative and cognitive process through which an individual learns to appreciate and become sensitive to the values, lifestyles, practices, and problem-solving strategies of an individual with a different cultural background (Campinha-Bacote, 1994). Such cultural awareness includes refraining from forming stereotypes and judgments based on one’s own cultural framework.
Cultural knowledge is the process of actively seeking information about different cultural and ethnic groups, such as their world views, health conditions, and practices, including their concepts of health and illness; use of home remedies and self-medication; dietary habits; pregnancy and childbearing practices; perceptions of Western medical care, health care providers, and barriers; risk-taking and health-seeking behavior; biological variations and drug metabolism tendencies; and reasons for migration and occupational hazards.
Cultural skill is the ability to discern values, beliefs, and practices in individual encounters and the ability to extract cultural or group variations in health statistics and program data. This skill is a type of cultural assessment. It is the ability to maintain an open and objective attitude about individuals and their culture and to remain open to the possibility of differences. Health providers should be nonjudgmental regarding cultural differences.
Communication is the means by which culture is transmitted and preserved (Delgado, 1983). Cultural patterns of communication affect the expression of ideas and feelings, as well as decision-making and communication strategies (Hedlund, 1988; Kretch, Crutchfield, and Ballachey, 1962). Many factors influence communication, both messages sent and those received, such as per-
sonal needs and interests; cultural, social, and philosophical values; personal tendencies; the environment in which communication takes place or the medium through which it is communicated; past experiences as they relate to message content; knowledge of the subject and basic beliefs or understandings; and how the message is understood. For example, a Vietnamese individual may smile in response to a message to avoid confrontation or to show respect for the speaker. Nodding may not be an indication that the message was understood or accepted (Rocereto, 1981).
Increased diversity and changing demographics in the United States have driven the demand for culturally sensitive public health messages. Rensnicow et al. (1999) defined cultural sensitivity as the extent to which ethnic and cultural characteristics, experiences, norms, values, behavioral patterns, and beliefs—including the relevant historical, environmental, and social forces of a target population—are incorporated into the design, delivery, and evaluation of communication messages and programs. A model for developing health promotion and disease prevention interventions should look at cultural sensitivity in terms of “surface and deep structures.” Surface structures involve matching intervention materials and messages to characteristics of a target population, such as using people, places, language, music, food, locations, and clothing that are familiar to the target population. Deep structures involve incorporating the cultural, social, historical, environmental, and psychological forces of the target population in messages to influence health behavior change. The Navajo, for example, value living in harmony with nature and with other people. Illness is perceived as falling out of harmony with others and the individual’s environment, and curing is believed by the Navajo to restore such harmony. Alcohol treatments and diabetes interventions designed and evaluated by scholars at the University of New Mexico suggest that the concept of harmony can be considered in ways to make these interventions more effective in health behavior change.
ETHICS OF HEALTH COMMUNICATION INTERVENTIONS FOR DIVERSE POPULATIONS
Principles of ethics are important in developing and implementing health communication interventions. Although there are competing ways to consider ethical principles, we focus our attention on four core values that are central to effective ethical analysis for health care: respecting an individual’s autonomy, providing benefit (beneficence), avoidance of harm, and treating groups and individuals justly and equitably (Beauchamp, 1994). The application of these principles to the design and implementation of health communication recognizes that the goal of improving health behavior is important, but it is not the only important goal in an individual’s life. Therefore, it must be balanced against other interests, particularly in a world of divergent views, diverse cultures, and differences in understanding of health. The principles have been defined as follows:
-
Respecting an individual’s autonomy is based on the premise that a fundamental dignity of human beings resides in their capacity for rational choice and their right to make their own choices.
-
Beneficence concerns the balance between benefits and risks; the guideline is that the benefits must outweigh or at least be equivalent to the risks the individual is being asked to take.
-
Avoidance of harm involves ensuring that such actions as stereotyping, blaming the victim, and presenting conflicting messages are avoided.
-
Treating groups and individuals justly and equitably suggests that all people should be treated similarly and fairly regarding the distribution of benefits and harms.
Table 7-1 provides some examples of questions guided by these principles that might be asked at different points in the design and implementation of a health communication intervention.
Implementing ethical principles can be complicated by a number of factors. First, the developers’ consideration of tradeoffs
TABLE 7-1 Ethical Aspects of the Design and Conduct of Health Promotions
|
Facets |
Examples of guiding questions and ethical issues |
|
|
The right and obligation to sponsor the intervention |
• Who has the moral right to intervene on this health issue? (respect for autonomy; utility/public good) • Who has the obligation to intervene? (obligation to do good) |
|
|
Framing, problem definition, and choice of strategies |
• How are the causes for the problem defined? (respect for autonomy) • Are factors related to different levels of the health issue represented in the framing of the problem, beyond the individual level? (e.g., family relations, cultural norms, economic factors, enforcement of protective laws and regulations) (justice) • Are the diverse perspectives of population members or of the individual client represented in the way the problem is framed? (respect for autonomy) • Does the client/patient or do the intervention’s populations have issues that need to be addressed that may have a higher priority than the intervention’s behavior-change objectives? (avoidance of harm) • Does the intervention run counter to other important behaviors related to maintaining/enhancing the individual, family, or community? (beneficence) • Are there opportunities for the client or the population members to participate in decisions regarding problem definition and choice of strategies? (respect for autonomy) |
|
|
Evaluation |
• Are evaluation findings and conclusions made available to the population members? (respect for autonomy) • Are the evaluation findings and recommendations formulated in a way that they can be used for improving future activities? (utility) |
|
|
Segmentation, targeting and tailoring |
• Which segments should be targeted and on the basis of which ethical justifications (e.g., particular needs or vulnerabilities, ability to reach, relationship with sponsoring organization)? (equity) |
|
|
Facets |
Examples of guiding questions and ethical issues |
|
|
|
• To what extent should messages and strategies be tailored? To whom should they be tailored? (equity) • Who may tailored messages offend? How would individuals who are not their intended audience respond when they are exposed to the tailored messages? (avoidance of harm; equity) |
|
|
Persuasive and dialogical approaches |
• How to attract the attention, interest, and make the health message salient without using appeals that can be considered manipulative? (respect for autonomy) • How to provide accurate and complete information to support the health claim without overloading the client or the intervention population with messages that may be too cumbersome or confusing? (avoidance of harm, comprehensibility) • Can the persuasive strategies be compatible with the culture of the population? When is it justifiable to adopt strategies that are not compatible? (avoidance of harm, providing benefit) |
|
|
Cultural symbols and themes |
• Is there a possibility that the use of cultural themes may serve to stereotype the population? (avoidance of harm) • Are there any individuals or groups that may be excluded and even stigmatized when certain cultural themes are made a dominant part of the intervention? (avoidance of harm) |
|
|
Information |
• Is the information presented in a way that all members of the population, regardless of language skills or cultural background, are able to relate to it and understand the messages for health behavior change? (equity, comprehensibility) |
|
|
Deprivation |
• Do certain practices that the health interventions aim to eliminate have important sociocultural or personal gratification functions? Would people, particularly members of vulnerable populations, be deprived in any way? (avoidance of harm, equity) |
|
|
Facets |
Examples of guiding questions and ethical issues |
|
|
|
• Does the intervention proffer alternatives for practices that fulfill an important function for the population? (avoidance of harm, equity) |
|
|
Responsibility |
• How are responsibility and irresponsibility defined? (avoidance of harm, respect for autonomy) • Is culpability implied in messages related to responsibility? (avoidance of harm) • Are messages that appeal to responsibility using high emotional appeals? (respect for autonomy, justice) • What is the ethical base of appeals that relate to obligations to significant others and the community? (respect for autonomy, justice) |
|
among efficiency, cost, and improving the health of the most in need versus a broader range of persons can lead to conflicting goals. Second, the design of a communication strategy guided by ethical principles for one segment of the population may not be appropriate for another segment. Third, there is always the opportunity for unintended consequences, even with the most well-intentioned and well-executed health communication interventions. Possible outcomes for diverse populations include confusion about the meaning of the message, manipulation of individuals or groups without their understanding or consent, unwarranted anxiety resulting from implying individual culpability, and the stigmatizing of certain cultural practices.
In the interest of providing benefit and supporting the individual’s autonomy to choose, it is important for the message to be truthful and clear. This may require providing risk probabilities of specified health-related behaviors. The format in which probabilities of risk and benefit are presented can significantly affect the way people estimate the probability of their own risk (Singer and Endreny, 1993; Slovic, 1987; Slovic et al., 1987; Tversky and Kahneman, 1981).
Because health communication initiatives often encourage individuals to take responsibility for their own well-being (Kirkwood and Brown, 1995; Knowles, 1977; Guttman, 2000), it is important for developers to assess environmental constraints, access to health care resources and facilities, and the values and beliefs of the group. In some health communication interventions, people may be urged to make prudent and responsible choices about food consumption, leisure activities, intimate relations, and other lifestyle options. In response, those who are economically or otherwise disadvantaged might be compromised in their ability to follow the recommendations and may, as a result, be viewed as lacking motivation to change, being “difficult to reach,” and deserving of negative health outcomes (Daniels, 1985). Although health messages do not usually blame individuals for being responsible for their illnesses, they may frame disease prevention as if it were primarily a matter of individual control (Wallack, 1989). In doing so, they deemphasize structural factors related to employment and housing, access to health care, access to healthy and inexpensive food stuffs, pollution, and other factors that can precipitate or exacerbate serious health risks. Such messages also may deemphasize the importance of institutional changes that may supersede changes by individuals alone (e.g., Ellison et al., 1989; Coreil and Levin, 1984; Glanz and Mullis, 1988; Glanz et al., 1995; Green and Raiburn, 1990; Milio, 1981; Wallack, 1989; Williams, 1990).
Appeals to personal responsibility also may be viewed as manipulative (Bayer, 1996; Niebuhr, 1978; Veatch, 1982). Persuasive messages using personal responsibility as an emotional appeal may warn people that failure to adopt a responsible lifestyle may lead to illness or disability, which could turn them into a burden on their family or society as a whole. Health behavior change messages may imply that people have an obligation to help promote or protect the health of significant others. For example, people may be told that they should help their spouses maintain a healthy diet, insist that their adolescent children use seatbelts, and support the efforts of siblings and friends to quit smoking. Such messages can reinforce moral commitments such as service, re-
sponsiveness to others with special needs, fidelity, compassion, kindness, and keeping promises (Baier, 1993; Pellegrino, 1993). These ethical imperatives also can be associated with the ethic of care and other principles that emphasize the importance of being connected to others (Hallstein, 1999; Nodding, 1990; Pellegrino, 1985). These kinds of messages can cause dissonance when, for example, family members become antagonistic toward one another in the name of promoting their health (Kleinman, 1988).
The principle of avoiding harm is particularly important when applied to health communication interventions conducted in a community or large-scale national setting because the effects of the communication on different segments of the audience can be difficult to gauge. Special care should be taken to ensure that information and messages do not confuse and/or offend populations. For example, information that is presented in a tentative way or with caveats may be perceived as confusing, culturally inappropriate, and even culturally irrelevant. Words, concepts, and terms that are meaningful to one audience may have entirely different connotations for another. Moreover, because health messages disseminated through mass media must deal with complex social or medical topics in an extremely short time frame, they must provide a simplified distillation that can lead to incomplete or inaccurate understanding.
In developing health messages for specific populations, care should be taken to avoid stereotyping and underscoring disadvantages. For example, developers of communication interventions intended for populations with limited literacy skills should be aware of the potential to embarrass their intended audience with text messages (Davis et al., 1998). In another example, the positive application of a belief through cultural message themes can contribute to a positive feeling of self-determination and cultural pride as well as being effective in achieving behavior change. Also, positive themes can promote notions of responsibility and benefit. However, using these beliefs in a way that detaches them from their original meaning may be perceived as demeaning. This ap-
propriation may offend groups that may not want their cultural symbols used in a particular way, even in health communication efforts, out of concern that such use will have a stereotyping effect (López, 1997).
Audience selection can raise concerns about equity of benefits. One approach is to focus on relatively large segments of the population. The rationale for this approach is that even modest health-related changes (for example, modifying diet to lead to reductions in blood cholesterol levels or systolic blood pressure) in large populations will produce substantial changes in overall morbidity and mortality (Rose, 1985). These efforts can have a positive effect on those with easy-to-modify behavior—but those whose behaviors are most difficult to change may be shortchanged. The population approach is valuable because it represents an efficient use of resources, it avoids stigmatizing effects, and it may do some degree of good in reaching those with hard-to-modify behaviors (Beauchamp, 1988). However, health communication initiatives should not overlook harder to reach groups, and sponsors may wish to dedicate at least a portion of their resources to these individuals.
In terms of gauging social equality, all health promotion campaigns can be guided by a consideration of the following questions. How is the relationship between the behavior and the adverse health outcome framed? Is the behavior portrayed as a sufficient cause (or preventive measure) for the health effect? Do people, particularly members of socially or culturally disadvantaged populations, have a choice of whether to engage or not engage in the recommended health practice? Do they fully understand the relationship between the behavior and potential adverse health outcomes? Do people engage in the potentially hazardous behavior only for their own personal gratification? Finally, to what extent should health promotion messages be framed in a way that reinforces a perception of responsibility for the behaviors and outcomes of others?
THE SOCIOCULTURAL ENVIRONMENT
The fields of social epidemiology, psychology, anthropology, sociology, and economics are converging in the development of theories and methodologies, helping us to understand factors underlying health disparities. Levine and his colleagues set the stage for this convergence, especially with the Handbook of Medical Sociology (Freeman and Levine, 1989). Recent reviews by Yen and Syme (1999) and Social Studies in Health and Medicine (Albrecht, Fitzpatrick, and Scrimshaw, 2000) are among many recent analyses dealing with these complex issues. The recent Institute of Medicine report, Promoting Health (2000), advances our understanding of health behavior and health disparities. Some common themes from these sources give directions to the underlying factors contributing to health disparities, as follows:
-
Disparate access to prevention and treatment services;
-
Differences in patterns of use of services;
-
Differences in behaviors in response to illness;
-
Differences in environmental and occupational risks;
-
Differences in health promotion and disease prevention behaviors;
-
Differences in community factors such as stress, societal support, and community cohesion; and
-
Genetic factors that come into play for individuals, but seldom for groups.
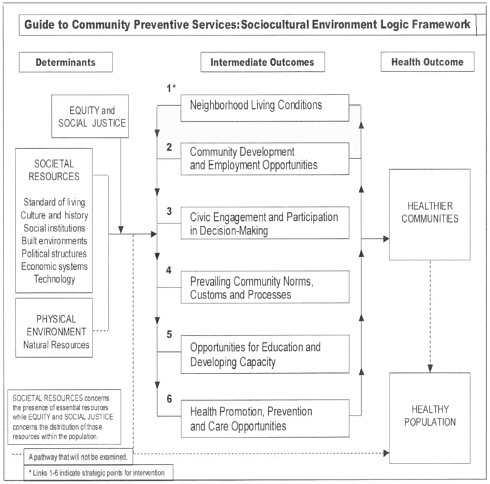
The Centers for Disease Control and Prevention Task Force on the Guide to Community Preventative Services developed an organizing logic framework for looking at many of these themes (see Figure 7-1). The Task Force was charged with developing evidence-based guidelines for community public health practice (Truman et al., 2000; Centers for Disease Control and Prevention, 2000b). Other topics in the guide include major risk behaviors such as smoking, sex, drugs, injury, nutrition, and exercise, and some diseases, such as cancer and diabetes. The discussion of the
sociocultural environment looks at underlying contextual issues related to health status. The framework includes six areas of potential interventions, with the outcomes being healthier communities and a healthier population. The six areas are:
-
Neighborhood living conditions;
-
Community development and employment opportunities;
-
Civic engagement and participation in decision making;
-
Prevailing community norms, customs, and processes;
-
Opportunities for education and developing capacity; and
-
Health promotion, prevention, and care opportunities.
Any communication efforts to change health behavior should understand these contextual factors and their influences on both reception of communication efforts and the ability of individuals to change behaviors.
SUMMARY AND CONCLUSIONS
All bases for categorizing humans are socially derived, change over time, and have bounded situational relevance. Powerful social forces, such as the desires to advance political agendas or to obtain resources, lead to an emphasis on differences among groups. Health communication efforts must recognize these social realities, but not be driven by them without careful consideration on the part of the communicators of their impact on a given message.
For health communication purposes, the way we divide this real-world complexity should reflect an understanding of relevant dynamic social and cultural processes. Diversity has been conceptualized in terms of broad “ethnic” and/or “racial” categories. These categories, which reflect shared group and life experiences, have been useful in identifying disparities in health status and may be useful in developing effective health communication strategies.
A focus on ethnoracial groups tends to confuse culture with ethnicity, risks, and stereotyping, and creates a view of culture as static and of groups as more homogeneous than they really are.
This view of culture deflects attention from a richer understanding of the diverse social and cultural processes that are meaningful for the development of effective health communication strategies. Cultural processes are dynamic, embedded in social context, and therefore influenced by social factors such as immigration or discrimination as well as by interactive social processes and cultural products like music, food, and language.
The consideration of the proximal social and cultural processes, as opposed to group categories, facilitates the translation of theory-based strategies to reflect the life experiences of targeted communities. For example, to develop a health communication strategy for the population age 80 and up requires the identification of factors in their daily lives that are related to the message and specific health behavior under consideration. Their lives may be impacted by a lack of economic resources, limited accessibility of health care services, deaths of significant others, or decreasing physical and cognitive capabilities.
The concept of self-identity allows us to look at individuals in the context of their life experiences and realities. Knowledge of the relevant experiences that individuals are likely to share allows health communicators to package the theoretical constructs of attitudes, norms, and efficacy beliefs in ways that are meaningful to the targeted group—and therefore will result in more effective health communication.
RECOMMENDATIONS
Based on its consideration of the various issues related to diversity, the committee offers the following recommendations:
-
Demographic factors are useful in epidemiological studies to understand whether health benefits are distributed equally and to identify intergroup differences. Policy makers and program planners should continue to use demographic factors to understand whether health benefits are equally distributed and to identify intergroup differences. Where there are existing disparities, it will
-
be important to monitor trends in gap opening and closing according to these categories.
-
However, because demographic groupings are limited and crude categories with relatively little explanatory power, they should be avoided as markers for designing health communication strategies or developing health messages. Instead, researchers and practitioners should identify and operationalize the particulars associated with a group’s life experiences, attitudes, and behaviors in designing and assessing health communication strategies.
-
Health communication strategies focusing on demographically diverse populations must be based on a recognition that demographic groupings represent a constellation of individuals with shared and unique life experiences, social processes, and cultural artifacts, and that the examination of these particulars as they impact individuals is important to understanding the context for health communication.
-
Health communication strategies and health messages must be informed by an understanding of the sociocultural environment of individuals within populations to be reached. Economic contexts, discrimination, and community resources such as access to health services are some of the important aspects of the sociocultural environment. These contextual factors have implications for the commonly held attitudes, norms, efficacy beliefs, and practices pertinent to the health issue in question.
-
We recommend that greater support be provided for qualitative research that examines the historical, social, and cultural contexts of communities’ health behavior. Such research should be designed to result in greater understanding of the implications of cultural factors and processes on effective health communications, and lead to more efficient ways of assessing relevant cultural processes in health communication interventions. A focus on qualitative ethnographic studies is likely to be required to identify cultural processes relevant to health communication, but it is also important to develop strategies that permit those processes to be reflected in large-scale health communication interventions.