2
Theory
This chapter synthesizes the main theories of communication and behavior change, including media advocacy and the diffusion of innovations, as they apply to health behavior change by diverse populations in the United States. Our perspective is restricted to those elements that appear to be most relevant to modifying a person’s health-directed activities through communication.
WHAT DOES THEORY DO?
Behavioral theories are defined by constructs, their relationships, and guidance for their implementation in applied settings. In health communication intervention programs, behavioral theories provide a framework for identifying the critical factors underlying the performance (or nonperformance) of specific health-related behaviors. The more one knows about the determinants of a given behavior, the more likely it is that one can develop an effective communication intervention to reinforce or change that behavior.
Perhaps the most critical determinant of whether a person does or does not perform a given behavior is the person’s beliefs about performing that behavior. Thus, behavioral theory, when properly applied, allows one to identify the beliefs that should be changed or reinforced to influence a given behavior change in a given population. Changing a person’s beliefs can be a precursor to changing a person’s behavior. Thus, behavior change can be said to be mediated by belief change. By recognizing that the critical beliefs in one population may be different from those in another population, behavioral theory helps in understanding the importance of diversity in developing effective health communications. However, knowing which beliefs to address does not tell us how to go about designing messages or interventions that can effectively reinforce or change those beliefs. Theories of communication and persuasion guide the selection of communication sources and channels and the preparation of the content of messages. For example, data about women’s beliefs regarding the value of mammography are important in creating interventions to enhance mammography use. However, finding out that many women in a given population do not believe that getting a mammogram will lead to early detection of breast cancer does not reveal how to design messages to convince them otherwise, or how to achieve social and environmental changes to influence this belief and therefore influence behavior change. By recognizing that different sources, channels, and message executions may be necessary for different populations, communication theories also point to the importance of considering diversity in developing effective health communication interventions.
We also recognize that communication interventions influence beliefs (and behavior) in different ways. Sometimes people exposed to a message learn the information that it contains, and this knowledge has a “direct” effect on their beliefs. But the context in which one receives the message also may influence how the message is received. For example, if a person is exposed to a message in the company of friends, their reactions to the message may strongly influence whether the person learns or accepts the mes-
sage content. If one’s friends respond to an antismoking or a dental hygiene message with anger or derision, the context may be converted into one of resistance rather than careful processing and possible acceptance of the message content. Theories of media effects provide a framework for understanding how mass communication messages ultimately influence beliefs and behavior.
In this chapter, we first consider behavioral theories and their implementation. We then consider theories of communication and persuasion, and theories of media effects. Rather than summarizing and describing the various theories in each of these areas, our focus is on identifying the critical concepts in these theories and on their theoretical integration. Many good reviews of theories have been conducted (e.g., Glanz, Lewis, and Rimer, 1997), but far fewer attempts have been made to synthesize constructs and achieve integration among behavioral theories or between behavioral and communication theories. Finally, we consider the implications of these theories for developing health messages for diverse audiences. “Good” theories not only recognize the role of diversity, but, when implemented properly, are specific to both the behavior of interest and to the population involved.
FACTORS INFLUENCING BEHAVIORAL PERFORMANCE: KEY CONSTRUCTS FROM BEHAVIORAL THEORIES
This volume shows that health disparities may reflect variations in biological risk factors, differences in access to diagnostic or treatment facilities, or behavioral differences. These latter differences (in health behaviors) are amenable to change via communication interventions. In order to develop health communication messages to eliminate or reduce the behavioral differences, it is essential to understand factors influencing the performance (or nonperformance) of a given health behavior. There are many theories of behavioral prediction, including:
-
Theory of Planned Behavior (e.g., Ajzen, 1985, 1991; Ajzen and Madden, 1986);
-
Theory of Subjective Culture and Interpersonal Relations (e.g., Triandis, 1972);
-
Transtheoretical Model of Behavior Change (Prochaska and DiClemente, 1983, 1986, 1992; Prochaska, DiClemente, and Norcross, 1992; Prochaska et al., 1994);
-
Information/Motivation/Behavioral-Skills Model (Fisher and Fisher, 1992);
-
Health Belief Model (Becker, 1974, 1988; Rosenstock, 1974; Rosenstock, Strecher, and Becker, 1994);
-
Social Cognitive Theory (Bandura, 1977, 1986, 1991, 1994);
-
Theory of Reasoned Action (Fishbein and Ajzen, 1975; Ajzen and Fishbein, 1980; Fishbein, Middlestadt, and Hitchcock, 1991).
However, there is a growing academic consensus that only a limited number of variables need to be considered in predicting and understanding any given behavior (see, e.g., Petraitis, Flay, and Miller, 1995; Fishbein, 2000). The variables come primarily from three theories that have been widely used in, and have a major influence on, current behavioral health research: the Health Belief Model, Social Cognitive Theory, and the Theory of Reasoned Action. (See Annex A at the end of this chapter for a brief description of each of these theories.)
One way to predict whether or not a given person will engage in a given health behavior is to ask. People are remarkably accurate predictors of their own behaviors, and appropriate measures of intention (one’s subjective probability that he or she will or will not engage in a given behavior) consistently have been shown to be the best single predictors of the likelihood that one will (or will not) perform the behavior in question (see, e.g., Sheppard, Hartwick, and Warshaw, 1988; Van den Putte, 1991). However, people do not always act on their intentions. One may intend to perform a given health behavior, but discover that he or she does not have the necessary skills and abilities to carry out the behavior. In addition, one may encounter unanticipated environmental con-
straints (or barriers) that impede or prevent behavioral performance. At the same time, it is important to recognize that environmental (or ecological) factors may also facilitate acting on one’s intentions as well as behavioral performance per se.
Nevertheless, if a person has made a strong commitment (or formed a strong intention) to perform a given behavior, and if he or she has the necessary skills and abilities required to perform that behavior, and if there are no environmental constraints or barriers to prevent performance of that behavior (i.e., if a context of opportunity exists for performing the behavior), the probability is very high that he or she will perform that behavior.
Thus, if one has formed a strong intention (or made a strong commitment) to perform a given behavior, but is unable to act on that intention, a communication intervention should be directed at “skills training,” or at removing or helping people to overcome barriers or environmental constraints. Such interventions often increase a person’s sense of personal agency or self-efficacy, a concept discussed later. On the other hand, if people are not engaging in a behavior because they have little or no intention to do so, the intervention should be directed at developing or strengthening intentions. Note that intention is viewed as a continuous, rather than as a dichotomous, variable. People do not simply “have” or “not have” an intention to perform a given behavior, but rather, people have stronger or weaker intentions to perform (or not perform) the health behavior in question. People may tell us that they “definitely will” versus “probably will” perform a given health behavior, such as obtaining a mammogram. Similarly, there is a difference between saying that it is “slightly probable,” “quite probable,” or “extremely probable” that one will engage (or not engage) in some health behavior. Although it could be argued that many health-related behaviors are performed automatically, without reflection on or awareness of intention, when asked, people can tell us whether they will or will not perform a given behavior, and these measures of intention (or self-prediction) are highly related to actual behavioral performance. Thus, from a communica-
tion perspective, it is important to know whether and why people do or do not hold a given intention.
Behavioral change theories suggest that only a limited number of variables directly influence the strength of intentions. Some theorists view these determinants of intention as also having a direct influence on behavior—an influence that goes beyond their indirect influence through intention.
Although different theories use different terminology, three major factors appear to influence intention (and thus behavior): (1) one’s attitude toward performing the behavior; (2) one’s perception of the norms governing performance or nonperformance of the behavior; and (3) one’s sense of personal agency or self-efficacy regarding personally performing the behavior.
Attitude
The attitude concept refers to the extent to which one “likes” or “dislikes” a given object, institution, event, or behavior, and is often defined as an overall feeling of favorableness or unfavorableness toward that object, institution, event, or behavior (Eagley and Chaiken, 1993). For the purpose of behavioral prediction, the critical attitude is the attitude toward one’s own performance of the behavior in question. The more favorable one is to personally performing a given behavior, the more likely it is that one will intend to perform that behavior. The attitude toward performing a given behavior is assumed to be based on a person’s beliefs about performing that behavior (Fishbein and Ajzen, 1975; Ajzen and Fishbein, 1980). The more a person believes that performing a given behavior will lead to positive consequences (e.g., “My performing this behavior will make me feel better”; “will show my partner that I care”; “is the responsible thing to do”) and/or prevent negative consequences (e.g., “will protect me from disease Y”; “will reduce the probability of an amputation”), the more favorable the person’s attitude is toward performing that behavior. Similarly, the more a person believes that performing the behavior will lead to negative consequences (e.g., “My performing this be-
havior will be painful”; “will be expensive”; “will make my partner angry”) or prevent positive consequences (e.g., “will not make me feel better”; “will not make me healthy”), the more unfavorable the attitude. Although many theories do not use the attitude construct, nearly all agree that intention (or behavior) is a function of one’s beliefs that performing the behavior will lead to various outcomes and the evaluation of those outcomes. It is assumed that a person will not form an intention (or perform a behavior) if the costs of performing that behavior outweigh the benefits. These underlying beliefs are called “outcome expectancies” or “behavioral beliefs.”
Perceived Norms
Perceived norms are the degree to which a person perceives that a given behavior is viewed as appropriate or inappropriate by members of the person’s social network or society at large. Norms reflect the amount of social pressure one feels about performing or not performing a specific behavior. Generally speaking, there are two types of normative pressure. On one hand, a person may believe that particular individuals or groups that are important to the person think that he or she should (or should not) perform the behavior in question. On the other hand, a person may believe these important others are, or are not, performing that behavior. Although it is likely that we have all been told to “do what I say, not what I do,” it is clear that both types of normative pressure ultimately influence behavior and intention. Although the notion of normative pressure seeks to capture an overall perception about what most “important” others are saying or doing concerning the behavior, this overall judgment must somehow incorporate and integrate the desires and/or actions of specific others. Indeed, these underlying normative beliefs (about the expectations or behaviors of specific others) are assumed to influence (or determine) a person’s overall perception of social pressure.
Personal Agency
Agency is a belief that one has the necessary skills and abilities to perform the behavior in question. Two types of considerations underlie a person’s sense of personal agency. First, there is the notion of self-efficacy, the belief that one can perform the behavior even under a number of difficult challenges. Second, there are beliefs that performance of the behavior is “up to me” and “under my control.” Both self-efficacy and perceived behavioral control are seen as a function of beliefs concerning specific barriers or impediments to behavioral performance.
Influence of Attitudes, Norms, and Personal Agency on Behavior
Although there seems to be general agreement among behavioral theorists that attitudes (or the outcome expectancies underlying attitude), perceived norms, and personal agency are critical to understanding why people do or do not engage in any given behavior, there is considerably less agreement concerning the ways in which these variables influence behavior. Some theorists view these variables as having only an indirect influence on behavior or behavior change through their influence on intentions, while others would argue that their influence is direct. This is particularly true with respect to personal agency, and considerable evidence shows that personal agency (or self-efficacy) directly influences the likelihood that one will or will not perform a given health behavior (for a comprehensive review, see Bandura, 2001). For example, the stronger one’s feeling of self-efficacy, the greater the probability that one will persist in attempts to perform a behavior, even after an initial failure (Bandura, 1997a).
Another disagreement among theoreticians concerns the role of social norms. Some theorists argue that perceived normative pressure directly influences intentions (and/or behavior) (e.g., Ajzen and Fishbein, 1980); others argue that normative pressure influences intentions (and/or behavior) only indirectly, by influencing outcome expectancies (Bandura, 1997). For example, from this
perspective, knowledge that another person “X” thinks one should not perform a given behavior will only influence performance of that behavior if this normative belief leads to an outcome expectancy, such as “My performing this behavior will make person X angry.”
Despite these differences, and regardless of the exact theoretical model one adopts, communication interventions to change health behavior should increase skills, remove or help individuals overcome environmental constraints, or change intention (by changing attitudes, norms, or a sense of personal agency; i.e., by changing the factors that directly or indirectly influence intention and behavior). The relative importance of these variables as determinants of behavior and behavior change will vary as a function of both the health behavior and the population being considered. Thus, a given health-protective behavior may not be performed because of a lack of skills, while another health-protective behavior may not be performed because people have no intention to do so. Similarly, the same behavior may not be performed in one population because of environmental constraints, while the failure of behavioral performance may be because of a lack of skills or abilities in another population.
The relative importance of attitudes, norms, and personal agency as determinants of intention (and behavior) also varies from behavior to behavior and from population to population. For example, intentions to perform one behavior (or the actual performance of that behavior) may be primarily under attitudinal control, while the intention to perform another behavior may be largely under normative control or be primarily influenced by beliefs about personal agency. Similarly, members of one population may intend to not perform a given behavior because they have negative attitudes toward performing that behavior, while members of another population may have decided not to perform the behavior because their important others think they should not perform the behavior or because they do not believe they have the necessary skills and abilities required to perform that behavior (i.e., they do
not have a sense of personal agency or self-efficacy with respect to performing that behavior).
One immediate implication is that health communication interventions should be directed at changing those variables that are important determinants of health behavior change in the population being considered. Communication interventions that address an “unimportant” variable are unlikely to be successful. Thus, prior to developing a communication intervention, it is important to determine whether people have or have not formed an appropriate intention, and, if not, to determine whether that intention is influenced primarily by attitudes, norms, and/or issues of personal agency.
Once the critical determinants of a specific behavior change in a particular population have been identified, one should be able to develop health communication interventions to change those determinants. Ultimately, this process involves changing a person’s underlying beliefs about the consequences of performing the health behavior, about the expectations or behaviors of others, or about one’s ability to perform the behavior under a variety of challenging circumstances. For example, in order to change an attitude, it is often necessary to change outcome expectancies, that is, beliefs that performing the behavior will lead to certain positively or negatively valued outcomes. Clearly, the more that one believes that performing the behavior in question will lead to “good” outcomes and prevent “bad” outcomes, the more favorable the person’s attitude will be toward performing that behavior. Similarly, the more one believes that specific relevant others think he or she should perform the behavior and the more one believes these others are performing the behaviors themselves, the more one will experience social pressure to perform the behavior change. Finally, the more one believes he or she can perform the health behavior, even when specific impediments are present, the stronger that person’s sense of self-efficacy or personal agency will be.
The substantive uniqueness of each behavior comes into play at this level of underlying beliefs. For example, the barriers to obtaining a mammogram and/or the outcomes (or consequences)
of getting a mammogram may be very different from those associated with taking a PSA test (a blood test for detecting prostate cancer), or getting genetic screening. These specific health beliefs must be addressed in a communication intervention if one wishes to change intentions and behavior. Although an investigator or a practitioner can sit in his or her office and develop measures of attitudes, perceived norms, and self-efficacy, he or she cannot know what a given population (or a given person) believes about performing a given behavior without interacting with that population. Thus, one must go to members of a target population to identify salient outcome, normative, and efficacy beliefs; one must understand the health behavior change from the population’s perspective. Although behavioral theory suggests that a common set of variables is relevant to all populations, it recognizes that the relative importance and substantive meaning of these variables depends on the specific population being considered. By appropriately implementing a theory, one can identify the behavioral, normative, and/or efficacy beliefs that discriminate between people, in any given population, who do and do not perform a specific behavior. Theories of communication and behavior change inherently recognize the role and importance of diversity. Program planners should act on this knowledge.
The above discussion focuses attention on a limited set of variables that have consistently been found to be among the strongest predictors of any given behavior (see, e.g., Petraitis, Flay, and Miller, 1995). Although focusing on behavior-specific variables may provide the best prediction of any given behavior, this approach does little to explain the genesis of the beliefs that underlie attitudes, norms, and self-efficacy. Clearly, the beliefs that one holds concerning his or her performance of a given behavior are likely to be influenced by a large number of other variables. For example, one’s life experience will influence what one believes about performing a given behavior, and thus one often finds relations among demographic variables such as gender, ethnicity, age, education, socioeconomic status, and behavioral performance. Similarly, women who perceive they are at high risk for, and/or are
afraid that they may have, breast cancer, may have beliefs about “My getting a mammogram” that are very different from women who do not believe they are at risk. Thus, factors that may influence one’s beliefs include perceived risk; moods and emotions as well as personality, culture, knowledge, and attitudes toward objects or institutions; and stigma. In addition, ecological and social factors such as availability of health services, types of interpersonal networks, and media exposure and/or exposure to various interventions may all serve to shape and influence one’s behavioral, normative, and efficacy beliefs.
Although these are all important variables, and although they may help us to understand why people hold a given belief, they are perhaps best seen as “distal” variables that exert their influence over specific behaviors by affecting the more “proximal” determinants of those behaviors. However, there is no necessary relationship between any of these variables and behavior-specific beliefs. That is, these distal variables may or may not affect people’s underlying behavioral, normative, or control beliefs about a given behavior. For example, rich and poor, old and young, those who do or do not perceive they are at risk for a given illness, those who do or do not have knowledge of a disease and how it is transmitted, and those who do or do not feel stigmatized may have different behavioral, normative, and control beliefs with respect to one behavior, but may have similar beliefs with respect to another.
When one or more of these distal variables leads to different beliefs, it is possible that the variable also will be related to behavior change. However, even though a given distal variable may influence outcome expectancies, that variable may still be unrelated to behavior if attitudinal considerations are not important determinants of that behavior change. Thus, rather than focusing on distal variables, to be most effective, health communication interventions should focus on the behavioral, normative, or control beliefs that underlie attitudes, perceived norms, and/or a person’s sense of personal agency.
For example, let us assume that a behavioral analysis indicated that whether or not one intended to (or actually did) get a flu
vaccination is determined primarily by the outcome expectancy (or behavioral belief) that “My getting a flu shot will protect me from getting the flu.” Assume that those who intended to get (or who actually got) a flu vaccination believed that getting the flu shot would protect them from the flu, while those who did not intend to get (or who did not get) the vaccination believed that “My getting a flu shot will not protect me from getting the flu.” If this scenario were the case, an appropriate communication to increase the likelihood that people will intend to and will actually get a flu vaccination would be one that tried to change this latter belief. The more we understand about why some people do or do not hold this belief, the more likely we are to be able to develop an effective communication intervention to change that belief.
However, there are many reasons why people may believe a flu vaccination will not protect them from getting the flu. Some may believe that they are not “at risk” for getting the flu, and, thus, they may not believe that “Getting a flu shot will protect me from getting the flu.” Others may believe that “Whether I get the flu or not is God’s will” and, therefore, they too might believe that getting a flu vaccination will not protect them. Still others may believe “There are too many different types of flu viruses out there and a vaccination can’t protect me from all of them” and thus, they also might not believe that “My getting a flu shot will protect me from getting the flu.” Although this type of information may be useful when one is dealing with a person via interpersonal communication, it is only helpful for developing health communication messages under certain circumstances.
More specifically, if within a given population a distal variable is consistently related to the “target belief,” and if it is possible to affect that distal variable through a communication intervention, then it may be reasonable to focus communication messages on that variable. For example, if the distal variable is “perceived risk” and if perceived risk is significantly related to the target belief (e.g., to the belief that “My getting a flu shot will protect me from getting the flu”), then a communication intervention directed at increasing one’s perception of personal risk may be appropriate.
However, one must ask whether one should try to increase perceived risk, or if one should use the information that perceived risk is related to the target belief to develop a message directed at changing the target belief per se. From a behavior theory perspective, if the distal variable cannot be shown to be causally related to the target belief, this latter strategy is more likely to increase the likelihood that members of the target audience will intend to get (and actually will get) a flu vaccination.
Even when a distal variable is not amenable to change through communication, it may provide important insights for designing health communication interventions. For example, we might find that women are more likely to believe that “Getting a flu shot will protect me from getting the flu” than are men, or that those with a college degree are more likely to hold this belief than are those with less education. Data such as these should influence the development of communication interventions under the following circumstances:
-
If the distal variable defines population segments that hold different beliefs, or that show different association of beliefs to intentions or behaviors, communication interventions may need to address different beliefs for different population segments. For example, if men and women hold different beliefs about the expected outcomes of “dieting,” the communication messages directed to each group should be correspondingly different.
-
If the distal variable defines population segments that are likely to be differentially exposed to a communication, different approaches may be necessary to reach different population segments. For example, assume that older and younger people differ on the target belief. Given that older and younger people use different media, a communication intervention should use different channels to reach these two population segments.
Figure 2-1 summarizes the preceding discussion. Intentions, skills and abilities, environmental constraints, and personal agency (or self-efficacy) are viewed as the immediate determinants of be-
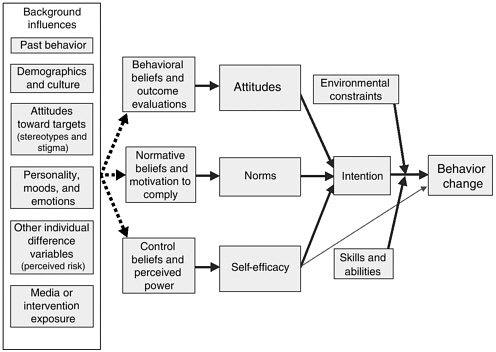
FIGURE 2-1 A general model of the determinants of behavior change.
havior, while attitudes, norms, and self-efficacy are viewed as the primary determinants of intention. These three determinants of intention are themselves determined by underlying behavioral, normative, and efficacy beliefs. Finally, Figure 2-1 shows that there are a large number of distal variables that may influence these underlying beliefs. Not all behavioral change theorists would agree with this general diagram. Some would delete certain variables; some scholars would treat what we called distal variables as more proximal determinants of intention (and/or behavior); others might rearrange the causal ordering of the variables. For ease of presentation, Figure 2-1 does not include feedback loops. Behavioral performance may lead to changes in a person’s behavioral, normative, or control beliefs, and these changes may, in turn, lead to changes in attitudes, perceived norms, or self-efficacy. We suggest that the variables connected by solid lines in Figure 2-1 are critical to an understanding of health behavior change and must be considered in developing health communication interventions. The
distal variables also may be important, but these variables have, at best, an indirect influence on behavior change, depending on whether they do or do not influence underlying beliefs. Figure 2-1 implies that changing health behavior ultimately will depend on changing behavioral, normative, or efficacy beliefs.
APPLYING BEHAVIOR CHANGE THEORY
The first step in applying any behavioral prediction or behavioral change model is to identify the specific behavior of interest. This task is not as straightforward as it seems. First, it is important to distinguish among behaviors, behavioral categories, and goals. The most effective health communication interventions are directed at changing specific behaviors (e.g., walking for 20 minutes three times a week) rather than behavioral categories (e.g., exercise) or goals (e.g., lose weight) (see, e.g., Fishbein, 1995, 2000).
The definition of a behavior involves several elements: the action (getting/using/buying/doing), the target (a mammogram/a condom), and the context (at the women’s clinic/for vaginal sex with spouse). A change in any one of the elements changes the behavior under consideration. For example, getting a mammogram is a different behavior than getting a PSA test (a change in target). Similarly, getting a mammogram at a women’s clinic is different from getting a mammogram at a university hospital (a change in context). Moreover, it is also important to include an additional element—time. This element is particularly important when one is developing a communication or other type of intervention. For example, getting a mammogram in the next 3 months or always using a condom are different behaviors than getting a mammogram in the next 2 weeks or occasionally using a condom. Clearly, a change in any one element in the behavioral definition usually will lead to very different beliefs about the consequences of performing that behavior, about the expectations and behaviors of relevant others, and about the barriers that may impede behavioral performance.
The selection of a target behavior depends on many factors. First and foremost, sound epidemiological evidence should link that behavior to a given health outcome. Second, the recommended behavior must be feasible; that is, it must be one that members of the target population can perform. For example, trying to get members of a given population to eat fruits and vegetables that are not available or are too expensive for most members of the population would be inappropriate. Thus, it is necessary to work with members of the target population to identify the behavior change that one wishes to influence. These considerations are addressed more fully in Chapter 3, which discusses mass media campaigns.
The second step in applying a behavior change theory is to identify the specific population. For any given behavior change, both the relative importance of attitudes, norms, and self-efficacy as determinants of intention (and/or behavior change) and the substantive content of the behavioral, normative, and control beliefs underlying these determinants may vary as a function of the population under consideration. Thus, it is imperative to define the population (or populations) to be considered. Because the “audience” is one of the critical constructs in theories of communication and behavior change, it will be considered in more detail in this chapter and in Chapter 3.
Once one or more behaviors and target populations have been identified, theory can be used to understand why some members of a target population are performing the behavior change and others are not. That is, by obtaining measures of each of the central variables in Figure 2-1 (i.e., beliefs, attitudes, norms, self-efficacy, intentions, and behavior), one can determine whether a given behavior or behavior change (e.g., getting a colonoscopy) is not being performed because people have not formed intentions to get a colonoscopy or because they are unable to act on their intentions. Similarly, one can determine, for the population under consideration, whether intention is influenced primarily by attitudes, norms, or self-efficacy. Finally, one can identify the specific beliefs (whether behavioral, normative, or control) that discriminate be-
tween those who do or do not (intend to) perform the behavior. It is important to recognize that behavioral theory focuses on the behavior of interest, and thus its primary focus is on beliefs about the performance of the behavior.
These discriminating beliefs need to be addressed in theory-based communication interventions. As discussed previously, although the ultimate goal of health communication should be to reinforce or change a given health behavior, communication creates, changes, or reinforces specific beliefs. When the beliefs are selected appropriately, these changes should, in turn, influence attitudes, perceived norms, or self-efficacy—the proximal determinants of one’s intentions to engage in (and often their actual performance of) that behavior change.
Identification of these beliefs requires understanding the behavior from the perspective of the population in question. Proper implementation of communication and behavior change theory requires that one goes to a sample of that population to identify the outcomes, referents, and barriers that are relevant for that population (see Middlestadt et al., 1996). Survey data can identify those beliefs that discriminate between those who do or do not (intend to) perform the behavior change in question (see, e.g., Hornik and Woolf, 1999). Once one has identified a set of “discriminating” beliefs, theories of communication and behavior change become important to develop messages and other interventions.
THEORIES OF COMMUNICATION AND BEHAVIOR CHANGE: KEY CONSTRUCTS
Because of our central concern about health communication for diverse audiences, the remainder of this chapter focuses primarily on factors that should be considered in order to develop effective communication campaigns and other interventions. Although messages and campaigns comprise only one type of behavior change intervention, most of these factors are also relevant for the development of other types of interventions. Theories of commu-
nication, directly or indirectly, address the question of “Who says what to whom, through what channel, with what effect?” This single framework, suggested by Harold Lasswell in 1939, often has been criticized because it has been interpreted as focusing all attention on the efforts of the communicator. In recognition of this concern, effects in the current view of much communication theory also are defined by how audiences process the messages. It is important to consider how prior beliefs and social and institutional affiliations affect how people make sense of, and respond to, messages. Thus, in attempting to develop effective health communication interventions, one must consider the communicator, the audience, the message, and the medium.
The Audience
To effectively implement behavioral theory and to develop effective health communication interventions, a precise description of the intended audience is needed first. The intended audience is the segment of the population whose behavior a health communication intervention attempts to change.
Communication campaigns select and define their intended audiences in very different ways. Some campaigns divide the prospective audience into segments according to characteristics of social diversity such as age, income, gender, or education. Even a single segment characterized by one demographic variable may comprise multiple diverse audiences. For example, the intended audience for a mammography campaign for older women will include women varying in ethnicity, income, education, age, family history, sexual orientation, and beliefs.
Information about intended audiences can be obtained through existing national or local survey data or by conducting formative research. These procedures involve data collection on an audience’s sociodemographic characteristics (e.g., age, education, gender, employment, ethnicity, marital status, sexual orientation), behavioral predictors or antecedents (e.g., audience beliefs, values, skills, attitudes), and current behaviors.
For example, a nutrition campaign intended for Hispanics and non-Hispanic whites from the Southwestern United States may choose to further segment by age, but select the age groupings differently for the two ethnic groups, based on differences in lifestyle factors. Young, single whites not living with their parents may be a separate segment requiring specific health communication messages, while young Hispanics, who are more likely to live with their parents, may receive a nutrition message that is similar to the one developed for their parents. In this case, it may be more useful to segment based on variables such as living conditions, social values, or language in the development of a culturally specific campaign.
Campaigns may have single or multiple intended audiences; campaign planners should first know as much as possible about the audience in order to develop appropriate and effective campaign goals and strategies. This need is amplified when the intended audience represents diverse population segments with which the campaign implementers are initially unfamiliar. For a more complete discussion of segmentation, see Chapter 3. Once an audience segment(s) is identified, the campaign intervention is designed and altered to communicate effectively with the target segment and change their health behavior.
The Message
A message is a specific statement of limited scope that usually contains only one main idea and relates to the communication objectives specified by a given health communication intervention (Ferguson, 1999). Ideally, message content is developed based on carefully planned communication strategies, which are derived from a knowledge of behavior change and communication theories as well as data collected through formative audience research (Weinreich, 1999). Although messages may be designed for different purposes (e.g., to increase awareness or knowledge, to increase self-efficacy, or to change attitudes and perceived norms), we will focus on communication messages designed to change health be-
havior. As indicated earlier, the most effective messages are those designed to change one or more well-defined behaviors.
Health campaigns are refined for diverse audiences by adapting behavior change goals so that they are relevant, appropriate, and appealing to the audience being addressed. Health campaigns must specify, as precisely as possible, the health behavior change that is desired from a specific audience when its members are exposed to the messages. The action behaviors promoted by the message should be within a range of what realistically can be accomplished by the target audience (Weinreich, 1999). This strategy may involve promoting adoption of a new health-enhancing behavior or the cessation of a risk behavior. The desired action ideally is determined from a thorough analysis of the audience’s current behavior. Appropriate implementation of behavioral theories then can serve to identify factors that can influence the desired behavior change in relation to the current behavior.
As already indicated, proper use of theory should help one to identify whether a given health behavior change is determined primarily by attitudinal, normative, and/or efficacy considerations, and should lead to the identification of a number of behavioral, normative, and/or control beliefs that clearly discriminate between members of any given population who do, or do not, engage in the behavior in question (i.e., that are highly correlated with the intention or behavior change). In addition, proper application of theory also should help to identify beliefs that are supportive of the behavior change and that are already held by most members of the population, but that have only moderate correlations with the intention or behavior. Which of these beliefs should a communication intervention address?
Beliefs
Belief Change
Hornik and Woolf (1999) described three factors to consider in identifying beliefs to target (i.e., try to change) in a communica-
tion (or other type of intervention). First, in the population under consideration, the belief should be strongly related to the intention or health behavior to be changed. Second, there should be enough people who do not already hold the targeted belief to warrant trying to change it. An example would be the belief that “My smoking is harmful to my health.” Because this belief is widely held by smokers as well as nonsmokers, little will be accomplished by trying to change it. Thus one must consider whether a communication intervention designed to change a given belief has the potential of moving enough people to make the intervention worthwhile. Finally, one must consider whether changing the belief is even possible. That is, can one support the targeted belief with a plausible argument based on strong evidence?
Relationship with Intentions and Behaviors
Clearly, with respect to the first criterion, theory-based survey data can identify beliefs that discriminate between intenders and nonintenders or that are highly related to the intention or behavior one wishes to change.
How Many People Already Hold the Targeted Belief?
Even though a belief may be highly related to the intention and behavior one wishes to change, little will be accomplished if most people already strongly hold the belief in question. It is important to recognize, however, that beliefs are not “held” versus “not held,” but vary in degree of strength. For example, people may “strongly agree” (think it is “extremely likely”) or “agree” (think it is “quite likely”) that a given behavior will lead to a given outcome. Clearly, if 80 percent of those who “strongly agree” but only 20 percent of those who “agree” have strong intentions to perform the behavior in question, then strengthening this belief is an appropriate target for an intervention. Thus, it is important to consider “belief strength” and to determine whether strengthening existing beliefs (i.e., moving people from “quite likely” to “ex-
tremely likely”) could influence their intentions (and behavior). Messages that can move people from “quite” to “extremely” likely can significantly affect the likelihood that these people will form strong intentions to perform the behavior in question.
Can the Belief Be Changed?
In stark contrast to the first two criteria, which are empirically based, the third criterion suggested by Hornik and Woolf (1999) is largely a subjective judgment. Clearly, not all beliefs are equally amenable to change, and relatively little will be accomplished by attacking a belief that is very difficult, if not impossible, to change. For example, if a woman’s regular partner tells her that “I hate condoms and will not use them,” it is extremely unlikely that one will be able to develop a message that would increase her belief that “My regular partner thinks we should always use condoms for vaginal sex.” Similarly, if a man has used a condom and, as a result, strongly believes that “using a condom decreases my sexual sensation,” it may not be possible to change this belief with a communication message. Beliefs based on direct experience are more difficult to change than are those based on information provided by others. Similarly, it seems reasonable to assume that people will find it more difficult to accept beliefs that may produce dissonance (i.e., that are inconsistent with their beliefs, attitudes, intentions, and behaviors) than to accept beliefs that are consonant with one or more of these psychosocial variables (Festinger, 1957).
Priming
In addition to changing behavior by changing beliefs, it is also assumed that behavior can be changed by changing the strength of the association between proximal variables. For example, by raising the accessibility or “salience” of certain beliefs, one may strengthen the association between those beliefs and attitudes, perceived norms, or personal agency. Similarly, by increasing the salience or accessibility of attitudes, norms, or self-efficacy, one may
strengthen the association between these variables and intentions (or behavior). When such increases in the association between variables occur, it is often referred to as “priming.” Thus, rather than focusing exclusively on beliefs that clearly discriminate between intenders and nonintenders (or actors and nonactors), it often may be useful to identify beliefs that support a given behavior, that are held (at least to some extent) by most of the population, and that have only a low or moderate relationship to the intention or behavior in question. Targeting these beliefs could strengthen their association with attitudes, perceived norms, or self-efficacy. It is important to recognize that priming (i.e., the strengthening of the association between two variables) may also involve some belief change, although not necessarily a change in mean belief strength. That is, the size of a correlation is a function of the covariance between two variables, as well as the total variance of each of the two variables, and changes in variance are due to changes in belief.
Message Content and Delivery
Although appropriate application of a theory of behavioral prediction can identify the critical determinants of a given intention (or behavior) as well as the critical beliefs underlying these determinants, the theory does not tell one how to best change these beliefs or whether these beliefs are amenable to change. Consistent with this view, Hornik and Woolf (1999) distinguished between message strategy and the message per se. According to these authors, message strategy is “the essential belief(s) that a message will be designed to impart,” while the message per se is “the product of a creative process that will turn the strategy into a specific realization.”
Although there are no empirically supported theories to guide the convergence of a given strategy into a specific realization, communication research identified a number of message factors that can influence the likelihood that a given message will be accepted. For example, two-sided messages (i.e., those that recognize and
refute counterarguments) are usually more effective than one-sided messages (Hovland, Janis, and Kelley, 1953; Hovland, Lumsdaine, and Sheffield, 1949; Allen, 1998), and messages that explicitly state a conclusion are often more effective than those that leave the conclusion implicit (McGuire, 1969; Cruz, 1998). By contrast, there is considerably less agreement concerning the role of fear or humor in developing effective messages (Mongeau, 1998). For example, considerable debate continues about the use and misuse of fear appeals (or threat), with some scholars and health professionals regarding “fear” as a central factor in motivating behavioral change (Rogers, 1983; Leventhal, Singer, and Jones, 1965; Leventhal, 1970),1 and others viewing it as a source of defensiveness and resistance to change (Janis, 1967; Rippletoe and Rogers, 1987).
Messages should be appropriate for, and relevant to, the population being considered. Very different messages will be needed if, for example, one is trying to increase the condom use of a person who says “I hate condoms and I’m never going to use them” or “I’ve thought about using condoms, but I don’t know how to introduce their use to my partner.” This simple illustration has two important implications. First, it suggests that behavior is not an “all or none” event, but that people may go through a number of steps or stages in adopting a behavior. One attempt to formalize this process has been proposed by Prochaska and associates (Prochaska, DiClemente, and Norcross, 1992). They proposed a stages of change or transtheoretical model that suggests that people move through the following stages:
-
Precontemplation, where the individual has no intention to perform the health behavior change and may not have even considered it.
|
1 |
Annex B provides a description of self-regulation models in which fear is considered as a central factor. |
-
Contemplation, where the individual has formed an intention to perform the new behavior sometime in the future, but has not yet done so.
-
Preparation, where the individual has a positive intention and makes some initial or occasional attempts to perform the behavior change.
-
Action, where the behavior is being performed consistently.
-
Maintenance, where the individual persists in performing the behavior change consistently for a long enough time period (usually defined as 6 months) that it becomes a regular part of one’s routine and where the probability of relapse is greatly reduced.
Stage models do not assume that the process of change is necessarily linear. That is, people may skip certain stages and/or go back to previous stages. For example, if in the preparation stage the individual is negatively reinforced for trying to perform the behavior change, the individual may go back to either the contemplation or precontemplation stage. Similarly, circumstances or events may lead to a “relapse,” sending those in the action or maintenance stage back to the preparation or contemplation stage. Perhaps the most important feature of stage-related models is that they suggest that attempts to evaluate the effectiveness of health communication interventions by looking solely at whether or not the target audience is consistently performing the recommended behavior change may be missing important campaign effects. For example, a campaign that moves people from precontemplation to contemplation may be an important first step in a behavior change process, especially for complex behaviors that are difficult to adopt.
A second implication of stage-based models is that a message that may be effective in moving people from preparation to action, for example, may be completely ineffective in moving people from the precontemplation to the contemplation stage. Communication interventions that may help people act on their intentions may have little or no effect on those individuals who have yet to form strong
intentions. Thus, it becomes important to design messages that take into account what stage people are in during the process of change. Very different communication interventions are required for audiences that have formed an intention to engage in some recommended behavior change, compared with interventions for audiences that have not formed an intention. (Chapter 6 discusses how new communication technologies may facilitate this process.)
Finally, it is important to recognize that message production values (e.g., black and white printing versus color printing; multiple versus few scene changes; hard rock versus rap music) also can influence the likelihood that people will accept a given health behavior change. For example, Palmgreen and associates (Palmgreen et al., 1991; Stephenson, 1999) showed that changes in these types of production values substantially affect the extent to which “high-sensation seekers” attend to, and learn the contents of, a given drug abuse prevention message. Thus, many of the variables that are viewed as “external” to theories of behavior change (e.g., personality, demographics, and culture) may directly influence the likelihood that a given message will lead to health behavior change. However, other important variables also may influence the outcome of behavior change.
The Communicator or Source
The source of health communication messages may be someone whom the intended audience relates to or knows, someone who represents the target audience, someone who is a recognizable celebrity or public figure, someone whom the intended audience regards as an influential role model, or someone who is friendly and anonymous, such as a fictional/animated character (Weinreich, 1999).
The source that delivers health communication campaign messages can have an important impact on whether messages are perceived as meaningful, credible, and/or relevant to target audiences. The selection of a source may be particularly important for health communication messages to diverse populations. Different popu-
lations will relate to, and be more or less influenced by, different messengers. The appropriate messenger may vary with the health issue of focus, the characteristics of the intended audience, and the purpose and style of the message. Furthermore, different subgroups within an audience may find different types of information supportive of the desired action. For example, scientific findings from an expert source may be the most important and credible basis for health behavior change for one audience segment, while information about social norms from a peer may be most important to another audience segment.
In the selection of appropriate, effective sources of communication messages, it is important to understand various characteristics of the intended audience, such as: Who influences the relevant behaviors of the target audience? Who are the most important role models? Who does the audience trust for credible information? What kind of person does the audience turn to for information related to the health topic at hand (i.e., authority figures, health professionals, peers, parents, celebrity role models) (Weinreich, 1999)? This information can be obtained through formative research. The most influential sources of communication may vary with the specific health behavior change and with the characteristics of the intended audience; formative research is necessary to identify the most relevant, appropriate sources of social influence for specific groups.
For example, formative research revealed that health providers are commonly identified as an important source of health communication messages relevant to health behavior change (Snell and Buck, 1996; Rimer, 1994). Promotion of health behaviors that are largely mediated by social influences and norms may be communicated more effectively through peer groups or by family or community members, celebrity role models, or religious leaders (Cruz and Mickalide, 2000; National Safe Kids Campaign, 2000). Messages that attempt to achieve health behavior change in environmental issues or politically mediated public health problems, such as traffic safety or the sale of alcohol and cigarettes to minors, may
be communicated most effectively by authority figures or representatives of law enforcement agencies.
Generally speaking, the most effective communication sources are those that are viewed as trustworthy and as having expertise in the relevant behavioral domain (Eagley and Chaiken, 1993). In some cases, however, the similarity of the source with the audience is critical. For example, Bandura (1997) identified four sources for the development of self-efficacy beliefs: enactive mastery experiences, vicarious learning, persuasion, and one’s own physiological and affective states. Particularly in the case of vicarious learning (i.e., learning through seeing others perform or attempt to perform the behavior in question), the selection of the other (or “model”) is critical. The more one can “identify” with the model (i.e., see the model as similar to one’s self), the more one is likely to view the model’s attainments as diagnostic of one’s own capabilities.
Although a complete discussion of vicarious learning and modeling is beyond the scope of this chapter, our previous discussion shows that, in order to maximize the potential impact of a given message, the selection of a communication source is a complex process involving knowledge of the audience and of the health behavior change message. However, the influence of a source depends, in part, on the nature of the message per se. The “stronger” the message, the less important the source. Credible sources can increase the likelihood that a “weak” message will be accepted, but the credibility of the source has relatively little influence on the likelihood that an audience will accept a “strong” message (McCroskey, 1970).
The Channel of Communication
The wide range of channels through which health communication messages are disseminated includes the mass media (television, radio, magazines, newspapers, and advertising); outdoor advertising; brochures, posters, and newsletters; comic books and fotonovellas; direct mail; interpersonal communications (such as in-person and telephone counseling); music and other videos;
songs; dramatic presentations; community events; point-of-purchase materials; and the Internet (Weinreich, 1999). Different age, gender, ethnic, and socioeconomic categories tend to favor different media, so it is prudent when targeting by these individual characteristics to investigate which media are best for each group. For example, a health communication campaign may use billboards and store displays to reach lower-income, inner-city dwellers, and newspapers to reach suburban households. Efforts to reach gay, lesbian, and bisexual populations often supplement mainstream media with specialized publications geared toward these groups, such as gay newspapers.
Generally speaking, in considering choice of channels, three questions should be addressed: (1) What messages can be sent through a particular channel? (2) How is each channel perceived by the audience? (3) When multiple channels are present, how do they interact in their effects?
What messages can be sent through a particular channel? The answer can be divided into two parts: First, the choice of a channel may impose limitations on what message content can be communicated. Radio provides no visuals, but may encourage the imagination; television provides information through sight and sound dynamically, but can only simulate interaction; online media provide opportunities for structured interaction, but may not be able to control individual paths of such interaction; outreach workers may be able to respond to the concerns and questions raised by individuals, but the health messages they transmit may lack consistency or fidelity. The effects of modes (e.g., visual and audio) incorporated in a channel, the effects of static versus continuing motion, and the effects of lesser and greater opportunities for interaction with audience individuals are all important exemplars.
The choice of channel may affect the fidelity of a health communication. For example, health communication that depends on interpersonal networks or on the voluntary involvement of institutions may provide less control over the exact content of a health message. A campaign may target the audience of a daytime talk
show program for a message about domestic violence, but the nature of the talk show, which may be sympathetic to the message but whose primary purpose is attracting audiences, will affect the final shape of the message. A health communication campaign that depends on “free” exposure is forced to use channels over which it has less control.
How is each channel perceived by the audience? A continuing issue in the literature compares mass media versus interpersonal channels with regard to their role at various stages in the diffusion of a new idea (Rogers, 1995). People often rely more heavily on mass media channels when they are first learning about an idea, but use interpersonal channels as they move toward making a decision (Rogers, 1995). Depending on the nature of the health behavior change and its context, either mass media or interpersonal communication channels can play an important role at either stage (Chaffee, 1982; Hornik, 1989; Schooler et al., 1998; Hornik, 1997). Audience individuals may not view messages from various channels as equally credible. Some communication channels and sources may be perceived by certain individuals as credible when they address health behavior change, while other channels (such as salespeople or Web sites on the Internet) may engender skepticism. These perceptions of communication channels may vary at different stages in the diffusion process.
When multiple channels are present, how do they interact in their effects? There are three possibilities. Channels may be additive—an exposure achieved through one channel is the same as exposure through any other channel. Alternatively, channels may positively interact or reinforce one another, such that the effects of exposure through any one channel increase when other channels are present. For example, the effect of an antismoking television message may be greater when a complementary school-based antismoking program reaches some audience individuals. Finally, channels may interact negatively, if additional exposures through one channel add nothing to the already available message exposures provided by another channel. Here, channels may substitute for one another. In addition, messages coming from different chan-
nels (and sources) may also be in conflict. For example, messages about antismoking conveyed by a school-based intervention may disagree with tobacco company advertising.
Media Effects
Assuming that behavior change theory was used to identify the critical beliefs to target in a given population, to develop an appropriate message, and to select an appropriate source and channel, two additional questions must be addressed. First is the question of audience exposure. Will enough members of the target audience be exposed to the message, either directly or indirectly? Second, given sufficient exposure, how does the message influence beliefs (and behavior change)?
No matter how well designed a health communication message may be, it is unlikely to produce belief (or behavior) change if people are not exposed to the message. Considerations of exposure address two complementary issues: (1) What influences the likelihood that a person will be exposed to a given message? (2) How do effects vary with the degree of exposure achieved?
People cannot be exposed to a message if that message is not made available to them; perhaps the primary factor influencing whether or not a message will be available is funding. Money can buy media time and space, and unfortunately for the great majority of health communication intervention messages, little money is often available for purchasing media time/space or for paying outreach agents. Thus, the practical question for most health communication interventions is what gets a message free distribution. Free distribution may involve time or space in the mass media, whether in the form of public service announcements, health messages embedded in entertainment programs, or coverage of a health topic on news programs, in newspapers or magazines, or on talk shows. Free distribution outside the mass media may involve adoption of a message by community institutions. For example, youth organizations may offer to distribute antidrug messages to their members, or schools may add antidrug components to their after-school
sports programs. Some messages are distributed through social networks, generating “buzz,” while other messages do not attract such social multiplication. Whether or not an individual is exposed to a message is influenced by message content, formal features of the message, or the context in which the messages are embedded.
How many exposures to a message, and what density of exposures in a given period of time, are needed before health behavior change occurs? How many exposures are needed before there are decreasing returns, such that additional exposure has little effect, or even a rejection of the message? The relationship between exposure and a given outcome effect (e.g., a change in belief) is determined by many factors, including: (1) the way humans attend to, and process, information (Zajonc, 1998; Petty and Cacioppo, 1979a; Peachmann and Stewart, 1990); (2) other characteristics of target audiences; (3) the complexities of the health problem addressed; (4) the presence of competing messages; and (5) the intrinsic character of the health message.
Repeated exposure by an individual provides more opportunities for learning the health message: Ten exposures to a message that marijuana initiation will damage parent-child relations may produce more awareness and more belief change than five exposures. Repeated exposure to a given message also may have an agenda-setting or priming effect (Dearing and Rogers, 1994; Cappella et al., 2001). Youth may already know that parents would be upset if they initiated marijuana use, but they may consider it more closely in deciding whether or not to initiate use after exposure to repeated messages on this topic. Repetition carries with it a message that the issue is important for consideration in making a decision about drug use.
Repeated exposure, particularly when a message is carried by a variety of communication channels, may carry an implicit message about what is socially expected. Repeated messages about marijuana use may address specific beliefs about the consequences of use, but they will also carry a message about the nature of societal norms for the health behavior change. Repetition through
diverse channels may convey the meta-message that society cares about this health issue. Similarly, repeated exposure to a message in multiple channels may increase the probability of interpersonal discussion of the message, further multiplying exposure and diffusion of a communication message. Finally, repeated message exposure carries with it an implicit legitimization of the subject of the health message. It also may increase the likelihood of policy attention to the problem. Issues given high exposure often interest politicians.
The previous discussion sets the stage for considering media effects. It is often assumed that a portion of the target audience will be exposed to a given message, and that a portion of those exposed to the message will learn its contents and change their health behavior. For example, consider again adolescent initiation of marijuana use. A health communication message might focus on the belief that beginning marijuana use will damage relationships with parents. We might hypothesize that youth watching the marijuana use ad immediately form (or strengthen) their belief, and as a result of this belief change, some youth may reduce their intention to use or their actual use of marijuana. Communication also can affect one’s beliefs (and behaviors) in other ways. For example, rather than having an immediate direct effect on beliefs, there may be a time lag between exposure to the message and belief (and/or behavior) change. In addition, rather than being directly exposed to a message, one may be indirectly exposed to the contents of the message through interpersonal interaction. Equally important, messages directed toward a specific belief or behavior may generalize to other beliefs or health behavior changes.
Five different paths through which a health communication message may have an effect on target beliefs (and behaviors) are: (1) immediate learning, (2) delayed learning, (3) generalized learning, (4) social diffusion, and (5) institutional diffusion.
-
Immediate learning. People can learn directly from health communication messages that enable them to make different decisions. For example, youth learn that trying marijuana has negative
-
consequences, so they form more negative attitudes and intentions and therefore are less likely to try marijuana. This new knowledge is assumed to have immediate consequences on their beliefs and behaviors. In this way, young people may learn about the negative and positive consequences of using a particular drug, about social expectations regarding drug use, and about skills and self-efficacy in avoiding drug use.
-
Delayed learning. Even though a communication message is conveyed today, its impact may not be appreciated until some time in the near future. For example, antidrug messages for 12-and 13-year-old youth (who rarely use marijuana) might be expected to influence future behavior only when opportunities to engage in drug use occur.
-
Generalized learning. Communication interventions provide direct exposure to specific messages, but people may be persuaded about related concepts as well. Thus, an anticocaine campaign might produce messages saying that cocaine has a particular negative consequence and that medical authorities are opposed to cocaine use. People exposed to these messages may generalize these cognitions to a broad negative view of other types of drug use. Thus, although the message focused on cocaine use, beliefs about marijuana use also change. This generalized learning means that exposure effects are not message specific and will not necessarily operate through an intervening path of acceptance of the specific consequences emphasized.
-
Social diffusion. Messages can stimulate discussion among peers and between youth and their parents, and these discussions can affect what people believe. Such discussions may provide new information about consequences or social expectations as well as new skills or increased self-efficacy. Discussions may link individuals who have been exposed to the communication message with those who have not. Thus, the effects of a health communication intervention would not be limited only to those individuals who have been directly exposed to the health communication messages. If the messages are about drugs, discussions may produce or reinforce antidrug ideas, or they may produce prodrug ideas.
-
Institutional diffusion. The presence of advertisements (or other intervention messages) can produce a broad response among public institutions (such as school boards, state legislatures, and the media). In turn, these institutions may initiate health policies or programs that affect cognitions and social expectations of the targeted audience. Thus, an antidrug communication intervention may stimulate concern among school board members about drug use and lead them to allocate more school time to drug education. Religious, athletic, and other private youth organizations may increase their antidrug activities. News organizations may cover drug issues more actively, and the nature of their messages may change. Movies, music, or entertainment television may change their level of attention to, and the content of, drug-related messages. Like the social diffusion route, institutional diffusion does not require an individual-level association between message exposure and beliefs or behavior change. This path of influence can be seen at the level of community analysis. Also, institutional diffusion can be a slow process, and there might be a relatively long lag between exposure to aspects of the communication intervention and institutional response and an even longer lag until the effects on audience beliefs or behavior become apparent.
Each of the five models of communication effects described represents a complementary process through which a health communication intervention might influence underlying beliefs and behavior. Any one of these models may describe the actual path of effect, or all of them may describe paths of effect that occurred. One important implication of these models is that they suggest that very different strategies may be necessary for evaluating the effectiveness of a given health communication intervention. Models of immediate, delayed, or generalized learning suggest that evaluating message (or campaign) effectiveness by comparing individuals who have or have not been exposed is appropriate. These models differ, however, in that they suggest that the evaluation of campaign effects should focus on different outcomes or on different time frames.
The diffusion model focuses attention on the social process surrounding health communication interventions. Messages may not only persuade individuals directly, but also stimulate interpersonal discussion about health behavior change. Evaluations under this model could not rely on comparing individuals who varied in exposure to the health messages, but would need to compare social networks that were more and less likely to have diffused messages. The institutional diffusion path carries with it a different implication. The audience for the communication interventions may be decision makers who determine institutional policies, rather than individuals whose behavior(s) are of concern. Indeed, if individuals are the audience, this audience may be seen primarily as a constituency who can influence policy makers, rather than as individuals whose risk behavior is to be changed. Evaluations of health communication interventions whose major path to influence is through institutional action cannot be conducted by comparing individuals with more and less exposure to messages. The appropriate unit of analysis is the institutional catchment area, often a geographically or politically defined unit, such as a city or state.
Media Advocacy
One possible way to speed up the likelihood of an institutional response is through media advocacy, the strategic use of mass media in combination with community organizing to advance healthy public policies. The primary focus is on the role of news media, with secondary attention to the use of paid advertising (U.S. Department of Health and Human Services, 1988; Wallack et al., 1993; Wallack, 1994; Wallack and Dorfman, 1996; Wallack and Sciandra, 1990-91; Winett and Wallack, 1996; Wallack et al., 1999). Media advocacy seeks to raise the volume of voices for social change, and to shape the sound so that it resonates with social justice values that are the presumed basis of public health (Beauchamp, 1976; Mann, 1997). Media advocacy has been used by a wide range of grassroots community groups, public health
leadership groups, public health and social advocates, and public health researchers (Wallack et al., 1993; Wallack et al., 1999).
From a theoretical perspective, media advocacy borrows from mass communication research, political science, sociology, and political psychology to develop strategy. Central to media advocacy are the concepts of agenda setting (McCoombs and Shaw, 1972; Dearing and Rogers, 1994) and framing (Iyengar, 1991; Gamson, 1989; Ryan, 1991). From a practical perspective, media advocacy borrows from community organizing, key elements of formative research (i.e., focus groups and polling), and political campaign strategy (e.g., application of selective pressure on key groups or individuals) (Wallack et al., 1993).
Media advocacy differs from traditional public health campaigns. It is most marked by an emphasis on:
-
Linking public health and social problems to inequities in social arrangements rather than to flaws in the individual.
-
Changing public policy rather than personal health behavior.
-
Focusing primarily on reaching opinion leaders and policy makers, rather than on those individuals who are directly affected (the traditional audience of public health communication campaigns).
-
Working with groups to increase participation and amplify their voices rather than providing health behavior change messages.
-
Having a primary goal of reducing the power gap, rather than filling the information gap.
Media advocacy is generally seen as part of a broader strategy, rather than as a strategy per se. It focuses on four primary activities in support of community organizing, policy development, and advancing policy:
-
Developing overall strategy. Media advocacy uses critical thinking to understand and respond to problems as social issues, rather than as personal problems. Following problem definition,
-
the focus is on elaborating policy options; identifying the person, group, or organization with the power to create the necessary change; and identifying organizations that can apply pressure to advance the policy and create change. (For example, in Oakland, California, various elements of the community were organized to apply pressure on the zoning commission, mayor’s office, city council, and state legislature, which were all targets at various points in the campaign.) Finally, various messages for the different targets of the campaign are developed.
-
Setting the agenda. Getting an issue in the media can help set the agenda and provide legitimacy and credibility to the health issue. Media advocacy involves understanding how journalism works in order to increase access to the news media. This approach includes maintaining a media list, monitoring the news media, understanding the elements of newsworthiness, pitching stories, and holding news events and developing editorial page strategies for reaching key opinion leaders about a given health issue.
-
Shaping the debate. The news media generally focus on the plight of the victim, while policy advocates emphasize social conditions that create victims. Media advocates frame policy issues using public health values that resonate with broad audiences. Some of the steps include “translate[ing] personal problems into public issues” (Mills, 1959); emphasizing social accountability as well as personal responsibility; identifying individuals and organizations who must assume a greater burden for addressing the problem; presenting a clear and concise policy solution; and packaging the story by combining key elements such as visuals, expert voices, authentic voices (those who have experience with the problem), media bites, social math (creating a context for large numbers that is interesting to the press and understandable to the public), research summaries, fact sheets, and policy papers.
-
Advancing the policy. Policy battles are often long and contentious, and it is important to use the media effectively to keep the issue on the media agenda. The Oakland, California, effort took 4 years and now must focus media attention to ensure that the policy
-
is properly implemented. Thus, it is important to develop strategies to maintain the media spotlight on the policy issue on a continuing basis. This effort means identifying opportunities to reintroduce the issue to the media—informing them of key anniversaries of relevant dates, publication of new reports, and significant meetings or hearings—and linking the policy solution to breaking news.
Diffusion of Innovations
When a new idea or innovation is introduced, diffusion theory (see, e.g., Rogers, 1995) suggests that the innovation has five characteristics, as perceived by members of a social system, that determine its rate of adoption: (1) relative advantage—the degree to which an innovation is perceived as being better than the idea it supersedes; (2) compatibility—the degree to which an innovation is perceived as being consistent with the existing values, past experiences, and needs of potential adopters; (3) complexity—the degree to which an innovation is perceived as being difficult to understand and use; (4) trialability—the degree to which an innovation may be experimented with on a limited basis; and (5) observability—the degree to which the results of an innovation are visible to others. In summary, innovations that are perceived by individuals as having greater relative advantage, compatibility, trialability, and observability and less complexity will be adopted more rapidly than other innovations.
In addition to the perceived characteristics of the innovation, people (or organizations and other units of adoption) vary in their innovativeness, the degree to which they are relatively earlier in adopting new ideas than other members of a social system. According to diffusion theory, there are five adopter categories: (1) innovators—the first 2.5 percent of the individuals in a system to adopt an innovation; (2) early adopters—the next 13.5 percent of the individuals in a system to adopt the innovation; (3) early majority—the next 34 percent to adopt; (4) late majority—the next
34 percent; and (5) laggards—the last 16 percent of the individuals in a system to adopt an innovation.
Generally speaking, the early adopter category, more than any other, has the greatest degree of opinion leadership in most systems, and potential adopters often look to early adopters for advice and information about the innovation. Several health communication interventions identified opinion leaders in a given community (e.g., among medical practitioners or members of the public), and then introduced innovations through these opinion leaders, in order to speed up the rate of diffusion of a health innovation (Kelly et al., 1992; Kelly, 1994).
IMPLICATIONS OF THEORY FOR HEALTH COMMUNICATION WITH DIVERSE POPULATIONS
It should be clear that theories of communication and behavior change, and theories of media effects, all recognize the importance of considering diversity in developing effective health communication interventions to produce behavior change. More specifically, behavior change theories recognize that the relative importance of the theoretical determinants of any given behavior may vary across populations. For example, a given health behavior change may be attitudinally driven in one population, normatively driven in another, and primarily under the influence of personal agency in a third population. Moreover, even if the same determinant is of primary importance for two diverse populations, the substantive content of the beliefs underlying that determinant may differ. For example, although attitude may be the most important determinant of a given health behavior in both Asian-American and African-American communities, members of one community may hold very different beliefs from members of the other community about the consequences of performing that health behavior.
Similarly, theories of communication and behavior change recognize that sources and channels that are perceived as credible by one population (i.e., for one audience) may be distrusted or not
utilized by another. Moreover, production values and formats in communication messages that positively appeal to one population may be viewed as unpleasant or boring by another. Finally, a message may lead directly to immediate or delayed health behavior change in one population, but will only affect beliefs if it leads to institutional diffusion in another. Although these considerations make it clear that one should develop health communication interventions with a specific target audience in mind, it is important to recognize that in many cases, the same belief or set of beliefs may be identified as a critical target for a number of diverse populations. The same message may be equally effective for diverse audiences. Moreover, when there is a “strong” message, the source may be less important than the message per se. Indeed, there is growing evidence that the source of a message is most important with a “weak” message, but has little or no effect with a “strong” message.
Does theory matter? Theory can increase the potential effectiveness of communication interventions by identifying critical beliefs to target, by structuring the communication message, and by guiding the selection of sources and channels of communication.
Does diversity matter in developing health communication interventions? To maximize communication effectiveness, one should adapt message formats, sources, channels, and frequency of exposure for different audiences. Factors such as age, gender, race/ ethnicity, and sexual orientation all draw on different interactions with the world and lead to different understandings regarding what is important and what is appropriate. Theory provides us with a roadmap to incorporate cultural differences into health communication interventions.
Do we need new behavior change theories? Existing behavioral theories need to be more fully applied in implementing health communication interventions. The main need is not for new theory, but for better application of the communication and behavior change theories that we already have. Individuals developing communication interventions need to fully understand the behavior they are trying to change or to reinforce from the per-
spective of the particular population with whom they are dealing. That is, they need to know whether, in that population, a given health behavior is controlled by attitudes, perceived norms, or issues of personal agency. More important, they need to identify these behavioral, normative, and/or control beliefs that most strongly discriminate between those who do and do not perform a given health behavior. Once target beliefs have been identified, one must identify the communicator, medium, and type of message that will have the greatest chance of influencing the beliefs either directly or indirectly.
Although theory is quite clear about the need to consider population differences in developing effective communication interventions, is there evidence that the appropriate use of theory helps to change health behaviors in diverse audiences? In the following chapters we examine the existing evidence and determine whether there are research gaps that need to be addressed.
In sum, communication and behavior change theories provide a powerful tool for organizing our thoughts, the existing evidence, and cultural realities so that health communication interventions can be more comprehensive, more sophisticated, and more likely to have desired effects on health behavior change. The following annex (Annex A) describes three of the behavioral theories that have had the strongest impact on health behavior interventions. Annex B describes self-regulation models.
ANNEX A: OVERVIEW OF KEY CONCEPTS IN THREE BEHAVIOR CHANGE THEORIES
The Health Belief Model
According to the original Health Belief Model, two major factors influence the likelihood that a person will adopt a recommended health-protective behavior change. First, the person must feel susceptible to a disease with serious or severe consequences. Second, the person must believe that the benefits of taking the rec-
ommended action outweigh the perceived barriers to (and/or costs of) performing the preventive action. In addition, the model recognized that a number of events (e.g., knowing someone who is ill, exposure to media campaigns, or other information) can serve as “cues to action.” These cues sometimes have been viewed as influencing “threat” (Janz and Becker, 1984) and sometimes as influencing behavior directly (Rosenstock, Strecher, and Becker, 1994). Most recently, the concept of self-efficacy has been added to the Health Belief Model (Rosenstock, Strecher, and Becker, 1994). Finally, the Health Belief Model also recognized that a number of demographic and individual difference variables could influence health beliefs (i.e., susceptibility, severity, costs, benefits, and self-efficacy).
Social Cognitive Theory
According to Social Cognitive Theory (Bandura, 1977b, 1986, 1997a), three primary factors determine the likelihood that someone will adopt a health behavior change: (1) self-efficacy, (2) goals, and (3) outcome expectancies. To adopt a given behavior change, individuals must have a sense of personal agency or self-efficacy that they can perform the desired behavior change, even in the face of various circumstances or barriers that make the change difficult to adopt and implement. Unless people believe they can exercise some control over their health behavior, they have little incentive to act or to persevere in the face of difficulties.
Health behavior also is affected by the outcomes that people expect their actions to produce. These expected outcomes include physical effects, social costs and benefits, and positive and negative self-evaluative reactions to one’s health behavior. Personal goals, rooted in a value system, provide further self-incentives and guides for health habits. Personal health behavior change would be easy if there were no impediments to surmount. The facilitators and obstacles that people perceive in changing their behavior is another determinant of health behavior change.
In effecting large-scale change, communication systems operate through two pathways (Bandura, 2002a). In the direct pathway, communication media promote change by informing, modeling, motivating, and guiding people. In the socially mediated pathway, media influences are used to link people in social networks and community settings. These places provide continued personalized guidance, as well as natural incentives and social supports for desired changes.
The Theory of Reasoned Action
According to the Theory of Reasoned Action (Fishbein and Ajzen, 1975; Ajzen and Fishbein, 1980), performance of a given behavior change is determined primarily by the strength of a person’s intention to perform that behavior. The intention to perform a given behavior is, in turn, viewed as a function of two factors, namely the person’s attitude toward performing the behavior (i.e., one’s overall positive or negative feeling about personally performing the behavior) and/or the person’s subjective norm concerning the behavior (i.e., the person’s perception that his or her important others think he or she should or should not perform the behavior). Attitudes are a function of behavioral beliefs (i.e., beliefs that performing the behavior will lead to certain outcomes) and their evaluative aspects (i.e., the evaluation of these outcomes); subjective norms are viewed as a function of normative beliefs (i.e., beliefs that a specific individual or population thinks one should or should not perform the behavior in question) and motivations to comply (i.e., the degree to which, in general, one wants to do what the referent thinks one should do).
It is worth noting that an extension of the Theory of Reasoned Action, the Theory of Planned Behavior (Ajzen, 1988, 1991), includes the concept of personal agency or perceived behavioral control. More specifically, according to the Theory of Planned Behavior, perceived behavioral control is viewed as a factor that directly influences both intention and behavior.
*****
Taken together, these three theories identify a limited number of variables that serve as determinants of any given health behavior change. All or some of these variables are found in nearly all other behavioral theories (e.g., the Information, Motivation, Behavioral Skills Model, Prochaska’s Stages of Change Model). Although there is considerable empirical evidence for the role of attitude, perceived norms, and self-efficacy as proximal determinants of intention and behavior (e.g., Shepphard, Hartwick, and Warshaw, 1988; Sheeran, Abraham, and Orbell, 1999), there is only limited support for the role of perceived risk (e.g., Gerrard, Gibbons, and Bushman, 1996). Thus, most behavior change theories suggest three critical determinants of a person’s intentions and behaviors: (1) the person’s attitude toward performing the behavior, which is based on one’s beliefs about the positive and negative consequences (i.e., costs and benefits) of performing that behavior; (2) perceived norms, which include the perception that those with whom the individual interacts most closely support the person’s adoption of the behavior and that others in the community are performing the behavior; and (3) self-efficacy, which involves the person’s perception that he or she can perform the behavior under a variety of challenging circumstances.
ANNEX B: SELF-REGULATION MODELS
The Common Sense Model (Skelton and Croyle, 1991; Leventhal, Meyer, and Nerenz, 1980; Petrie and Weinman, 1997; Cameron and Leventhal, 2002), is a specific example of a self-regulation that adds a detailed set of constructs specific to health behaviors presented in cognitive behavioral models. The model is based on findings from studies of health communication (Leventhal, 1970), showing that health actions are a product of a cognitive system representing the individual’s subjective or perceptual experience of health threats, and a system representing emotional reactions to these threats. The cognitive system is composed of 4 components: (1) the representation of the threat (e.g., the
name of the disease and the symptoms identifying its presence, likely duration and time of onset, cause, consequences (physical, social, economic), and controllability); (2) procedures for avoiding and/or controlling it and how these procedures are represented (medication is necessary; medication is addictive and dangerous; see Horne, 1997); (3) action plans (Leventhal, 1970) or implementation intentions (Gollwitzer and Oettingen, 1998), which specify time and place to perform specific procedures; and (4) the appraisal of action outcomes. Appraisal or efficacy assessments are made in relation to the goals set by the representation of both the threat and the procedure. For example, an analgesic medication will be appraised for its efficacy in eliminating pain and the time it takes to do so. The temporal expectations will be longer for more severe injuries and shorter for strong than for mild analgesics, e.g., ibuprofen versus aspirin. A key proposition of the Common Sense Model is that representations of both health dangers and procedures are abstract (e.g., labels such as diabetes, coronary disease) and concrete and/or experiential (symptoms of diabetes, effects of insulin, etc.).
Fear of a disease threat, i.e., the emotional response, can stimulate avoidance responses (minimization of the threat, avoidance of information), though these interfering effects are usually short lived and visible among individuals lacking a sense of self-efficacy. Evidence from multiple studies suggests that fear focuses attention on the danger (Lieberman and Chaiken, 1992) and encourages protective action among message recipients with high self-efficacy (Leventhal, 1970; Witte and Allen, 2000). Even individuals inclined to avoid exposure to threat information return to learn about and confront threats once their fear subsides (Wiebe, in press). Unlike planned behavior where social influences are conceptualized as norms (Ajzen and Fishbein, 1980), social influence takes multiple forms in the Common Sense Model. Observation of others, including observation of strangers, can provide information on cause, proximity and symptoms of health threats, efficacy and side effects of treatment, modeling of skills, assistance and barriers for both changing and maintaining health behaviors, and
amplify or reduce fear associated with health threats and treatment procedures (Leventhal, Robitaille and Hudson, 1997).
Most of the studies guided by the “self-regulation” framework have focused on actions for primary, secondary, and/or tertiary prevention that occur repeatedly over relatively long time frames for chronic illnesses such as diabetes, cardiovascular disease and cancer (the majority of the 1,800 plus items using the keyword “self-regulation” that were entered in the PsychINFO data base since 1990 are focused on health issues (see Leventhal, Brissette, and Leventhal, in press; Petrie and Weinman, 1997). The focus on chronic illness is consistent with hypothesis and data showing that representations of health threats and the procedures for control evolve over time as a function of changes in the individual’s concrete experience with illness and its symptoms and information from other persons and various media messages. Data supporting the Common Sense Model indicate that the great majority of behaviors initiated for health reasons are motivated by symptoms or functional deficits in the self or by observations of such changes in other persons. Symptoms and functional change are indicators of the state of the system, whether one is ill, stressed, or simply feeling the effects of aging, and changes in these perceptions over experienced (rather than clock) time are typically used as criteria for evaluating the efficacy of self selected and medically recommended interventions for avoiding and controlling illness threats. Although the Common Sense Model and the Social Learning Models (e.g., Bandura, 1977) were developed in parallel, they hold common assumptions about the determinants of health action.
















































