B
The Tuberculin Skin Test
John B.Bass, Jr., M.D.*
About 8 years after announcing the discovery of the tubercle bacillus, Robert Koch announced that he had discovered a cure for the disease.(1) He had prepared a concentrated filtrate from cultures of Mycobacterium tuberculosis which had been killed by heat, and he found that this material would protect guinea pigs from experimental tuberculosis. He called this material tuberculin and reported that a series of graduated injections starting with a dilute solution resulted in the cure of selected humans with tuberculosis. His work was hailed in the editorial pages of The Lancet(2) and the Journal of the American Medical Association,(3) but skeptics were plentiful and included such figures as Billroth, Virchow, and Sir Arthur Conan Doyle. The skepticism of the detractors was quickly confirmed, and Koch’s “cure” for tuberculosis was abandoned as a therapeutic maneuver. Despite its failure as a therapeutic substance, tuberculin rapidly became an important diagnostic test. Patients who received tuberculin in an attempt to cure them had generalized systemic reactions including fever, muscle aches, and abdominal discomfort with nausea and vomiting. People without tuberculosis did not develop this violent reaction and a number of investigators suggested the use of tuberculin as a diagnostic test. Local application of tuberculin avoided the serious systemic reactions and provided a local method of determining hypersensitivity to the substance. Methods of local application included a cutaneous scratch (Von Pirquet), a percutaneous patch (Moro), and conjunctival application (Calmette). Intracutaneous injection of tuberculin was described by Mantoux, and his method became widespread because of the reproducibility of the results.
TUBERCULINS
Koch’s original preparation of tuberculin was a relatively crude extraction from heat-killed cultures of M. tuberculosis.(4) His material contained a large number of carbohydrate and protein antigens as well as antigens from the beef broth used as a culture medium. Old tuberculin (O.T.) is still produced using methods similar to Koch’s original description, although antigens from the beef broth are no longer present. For many years tuberculins were manufactured without much attempt at standardization. Green described this situation:
It would surely simplify life for manufacture’s if O.T. were plainly described as “any witches” brew derived by evaporation of any unspecified fluid medium in which any unspecified strain of mammalian M. tuberculosis had been grown, provided its potency matched that of another witches’ brew kept in Copenhagen and called international standard, or any allegedly equivalent sub-standard thereof, when tested on an unspecified number of guinea-pigs without worrying too much about statistical analysis of results.(5)
In the 1930s Florence Seibert prepared trichloroacetic acid and ammonium sulfate precipitates of OT and called the material purified protein derivative (PPD).(6) PPD contains a number of antigenic components, most of which are low- and medium-weight proteins. PPD has less carbohydrate antigens than OT and results in fewer nonspecific immediate hypersensitivity reactions. In 1941, Seibert and Glenn(7) prepared a large batch of PPD (PPD-S) that has served as the standard reference material in the United States. The supply of PPD-S is currently becoming exhausted, and a replacement standard is being developed. Other improvements in tuberculin testing include the addition of Tween, a detergent that prevents adsorption of tuberculin to glass and plastic syringes(8,9) and a U.S. Food and Drug Administration requirement that all PPD lots in the United States demonstrate equal potency to PPD-S by bioassay.(10) Despite this demonstration of equal potency, there have been a number of reports suggesting an increase in false-positive reactions in skin testing programs that switched from Tubersol (Connaught, Swiftwater, PA) to Aplisol (Parke-Davis, Morris Plains, NJ).
“Tuberculins” and “PPDs” have been prepared from other mycobacterial species and have provided useful epidemiologic information,(11) but have not been demonstrated to have efficacy as diagnostic tests.
IMMUNE RESPONSE TO TUBERCULIN
Following infection with M. tuberculosis there is a sensitization and proliferation of T lymphocytes specific for antigens contained in tuberculin. In the Mantoux method of tuberculin testing, these T lymphocytes
accumulate at the site of injection and result in palpable induration. This response requires 24 to 48 hours and has been termed delayed-type hypersensitivity. Delayed hypersensitivity develops 2–10 weeks after initial infection and persists for many years, although reactivity may wane with advancing age.
Dose of Tuberculin
In the early 1900s, tuberculin testing consisted of a series of graduated doses of tuberculin. Any reaction to any dose was considered a positive test, and testing was used largely to eliminate tuberculosis as a diagnostic possibility in sick patients. In the 1920s and 1930s, the decreasing prevalence of tuberculosis resulted in decreased transmission of the infection to younger age groups and tuberculin was suggested as a method of diagnosing the infected state rather than the disease. The use of a series of skin tests with graduated doses of tuberculin was impractical, and in 1941, Furcolow and colleagues(12) reported a dose of 0.0001 mg discriminated patients with tuberculosis from others with the greatest accuracy. This amount of tuberculin was five times the usual starting dose with the graduated regimen and was said to contain 5 tuberculin units (TUs). This 5-TU dose has become the standard for tuberculin testing in the United States. Newly manufactured batches of tuberculin are currently bioassayed, and the 5-TU standard is the amount of material which produces results equal to those produced by 0.0001 mg of PPD-S. Other doses of tuberculin, such as “first strength” (1 TU) and “second strength” (250 TU) represent the smallest and largest doses of tuberculin that were administered in the abandoned graduated tuberculin testing method. These doses have been commercially available in the past, but they are not standardized by bioassay and have no use in diagnostic tuberculin testing programs.
Reading the Tuberculin Test
Although induration is generally accompanied by erythema, results using erythema are less precise and repeatable than those measuring induration, and measurement of induration is the standard. The injection is usually administered on the volar surface of the forearm, and induration is measured 48 to 72 hours following administration. Variation in tests administered simultaneously to both forearms averages about 15 percent and variability in measuring induration among experienced observers is similar. Although interobserver variability may be decreased by using the ballpoint pen method of Sokal,(13) most studies are based on palpation by experienced observers. Even with experienced observers, there is a tendency for clustering around predetermined cut-points and this can be
avoided by reading the tests using unmarked calipers. Interpretation of results using methods other than the Mantoux method is problematic, and multiple puncture devices appear to be less sensitive and specific than the Mantoux method. Specificity becomes increasingly important as the prior probability of infection becomes low and the Mantoux method is suggested as the standard.
OPERATING CHARACTERISTICS OF THE TUBERCULIN TEST
Despite the fact that PPD is a relatively crude material and results are dependent on the variability in immunologic reactivity in recipients of the test, the operating characteristics of the tuberculin test appear to be superior to those of many other tests which are commonly used in clinical medicine. Despite the superior operating characteristics, the positive predictive value of the test is probably poor whenever the prior probability of infection is less than 1 percent.(14,15) Unfortunately for the test, but fortunately for the individuals involved, this situation applies to almost all medical occupations currently. This difficulty was recognized as early as 1960: “There may be nostalgia for the days when all tuberculin reactions meant tuberculous infection, and no nonsense”(16)
Sensitivity
In the absence of an independent means of determining whether or not a person is infected with M. tuberculosis, the sensitivity of the tuberculin test in detecting latent infection cannot be determined with absolute accuracy. Most estimates of sensitivity have been derived from testing in patients with known tuberculosis. The sensitivity of tuberculin testing in patients presenting with newly diagnosed pulmonary tuberculosis is approximately 80 percent.(17,18) The 20 percent false-negative rate is due to a combination of specific immunosuppression of delayed hypersensitivity from cytokines plus overwhelming acute illness and poor nutrition. After such patients have received several weeks of therapy and nutrition, the sensitivity of tuberculin testing is approximately 95 percent. This correlates well with older studies in the prechemotherapeutic area which showed a 96 percent sensitivity in relatively stable patients in tuberculosis hospitals. Patients who are critically ill with tuberculosis (especially those with disseminated tuberculosis and tuberculous meningitis) may have false-negative rates exceeding 50 percent. T-cell depletion from infection with human immunodeficiency virus also commonly causes false-negative tuberculin reactions. Anergy testing with several other delayed hypersensitivity antigens will not detect all of these false-negative reactions,(18) and the recommendation to use anergy testing clinically in such
circumstances has been deleted from the latest American Thoracic Society/Centers for Disease Control and Prevention recommendations.(19)
Although the sensitivity of tuberculin testing cannot be accurately determined in subjects without tuberculosis, a reasonable assumption is that the sensitivity is approximately that seen in patients with tuberculosis who have received adequate treatment and is approximately 95 percent. There are hypothetical reasons that the test might be more or less sensitive in people without disease. It is possible that people infected with M. tuberculosis without disease have better immunity to the infection and might be more likely to react to tuberculin. It is also possible that people who are infected without disease have a smaller antigenic burden and might be less reactive to tuberculin. The likelihood that either of these hypotheses is of major importance is small, and the sensitivity of the tuberculin test in latent tuberculosis infection is assumed to be approximately 95 percent.
Specificity
Just as with the sensitivity, the lack of an independent method of determining infection means that the specificity cannot be determined with complete accuracy. The major reasons for false-positive tests in uninfected persons are thought to be cross-reactions in persons who have been vaccinated with bacille Calmette-Guérin (BCG)(20) or persons who have environmental exposure to other mycobacteria.(21) Prior BCG vaccination is generally known, but environmental exposure to other mycobacteria varies widely geographically and is difficult to estimate.
The large scale skin-testing surveys in the past have shown a great deal of geographic variability in skin testing results.(11) In areas of the country where environmental mycobacteria are uncommon, the distribution of skin-test reactions approximates that shown in Figure B-1. This distribution is similar to results obtained in skin testing of patients with active tuberculosis, and the presumption is that there are few false-positive tests in such a population. At the other end of the spectrum, areas of the country with likely exposures to environmental mycobacteria more closely resemble the distributions seen in Figure B-2. In such a population there is no clear-cut unimodal distribution of positive results and many more false-positive tests are present. In such a population, false-positive results can be minimized and the specificity of the test can be improved by progressively increasing the cutoff point for determination of positivity. In the United States there is a tendency for results to resemble those shown in Figure B-2 in the eastern and southern parts of the country. However, considerable variability occurs even within a single state, and the U.S. population is much more diverse and mobile than it was when these results were obtained.
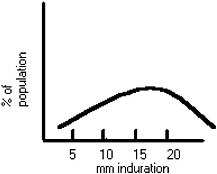
FIGURE B-1. Distribution of skin test reactions in a population with little cross sections.
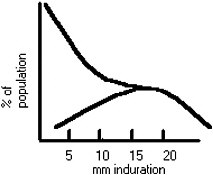
FIGURE B-2. Distribution of skin test reactions in a population with many cross sections. A hypothetical population of true positives is superimposed.
A large number of recent studies of serial skin testing programs in hospitals and other medical facilities have shown a clustering of yearly conversion rates around 0.5–1 percent in institutions without obvious exposure to undiagnosed and untreated cases of tuberculosis.(22,23) Although it is unproveable, it seems a reasonable assumption that these rates of conversion represent the false-positive rate of serial tuberculin testing and that the specificity of the test is 99 to 99.5 percent. The specificity is likely to be somewhat less than this in areas of the country where exposure to other mycobacteria is common.
Table B-1 shows the influence of prior probability or prevalence of infection on the positive predictive value of a tuberculin test for varying levels of specificity. The two columns on the right give the range of the positive predictive value for any given prevalence of infection for a specificity of 99 to 99.5 percent. The column with a specificity of 95 percent may represent a “worse-case” scenario in areas where cross-reactions to other mycobacteria are very common. To put these prevalences in perspective, 100 years ago about 90 percent of all adults were infected with M. tuberculosis. This was when the tuberculin test was introduced, and at that time it had a very high positive predictive value. Many nations around the globe continue to have infection rates of 25 to 50 percent and people from these countries commonly immigrate to the United States. Close contacts to active cases of tuberculosis may also have a 25 to 50 percent likelihood of being infected. Tuberculin testing targeted toward such populations is warranted.(19) The general adult population of the United States at this time has an infection rate approximately 5 to 10 percent and in this group the predictive value of a positive test begins to fall. Baseline transmission of tuberculosis infection in the United States has been estimated to be 0.05 percent per person a year. Testing of the
TABLE B-1. Predictive Value of a Positive Tuberculin Test
|
Predictive Value (%) at Indicated Specificity |
Prevalence of Infection (%) |
||
|
|
0.95 |
0.99 |
0.995 |
|
90 |
99 |
99 |
99 |
|
50 |
95 |
99 |
99 |
|
20 |
86 |
97 |
98 |
|
10 |
67 |
91 |
95 |
|
5 |
50 |
83 |
90 |
|
2 |
29 |
67 |
80 |
|
1 |
16 |
49 |
67 |
|
.1 |
3 |
10 |
17 |
|
.05 |
.9 |
4.8 |
9 |
general population of the country on a yearly basis to detect this transmission would have a positive predictive value of less than 10 percent (see Table B-1).
THE BOOSTER PHENOMENON
Although skin testing with tuberculin does not induce enough immunologic challenge to induce a positive reaction on subsequent tests, waned delayed hypersensitivity reactions from remote infections with M. tuberculosis and cross-reactions to antigens from other mycobacteria can be boosted or enhanced.(24) Such boosting generally occurs within 1 week and may persist for a year or more. Boosted reactions are particularly common in people who have received BCG vaccination,(20) people with environmental exposure to other mycobacteria, and people from countries with a high prevalence of tuberculosis. False conversions due to boosting are particularly common in these populations when the second skin test is placed in a serial skin testing program.(25) In order to detect this phenomenon, it is recommended that serial skin testing programs use an initial two-step test in which a second skin test is placed approximately 1-week after the first if there is no reaction to the first and that significant reactions to the second test are considered boosted reactions rather than conversions. There is a suggestion that boosted reactions may continue to occur subsequent to the second test in persons who have been vaccinated with BCG and persons from high-prevalence countries, but no practical method of detecting these late boosters is available.
Implications of Operating Characteristics of Tuberculin Test for Serial Skin Testing in Medical Populations
In considering serial tuberculin testing, the values in Table B-1 will represent incidence rather than prevalence, and this incidence is the like-
lihood of true transmission of M. tuberculosis infection in the interval between skin tests. The influence of serial skin testing on the specificity of the test is unknown. To the extent that false-positive results are random biologic events, the false-positive rate will remain relatively constant regardless of the interval between tests, and the number of people in a given population with false-positive test results will gradually grow over time in inverse proportion to the testing interval. Thus, frequent testing will gradually result in the accumulation of a large proportion of the population with false-positive results regardless of the incidence of true transmission of infection.
If false-positive results are not true random biologic events but, rather, reflect individual immunologic responsiveness to tuberculin, persons predisposed to such false-positive results may be removed from a serially tested population and the specificity of the test may improve with time. Most authors have concluded that serial skin testing programs tend to overestimate the incidence of new tuberculosis infection in the populations being tested,(26,27) and it seems likely that false-positive results are random biologic events which will be magnified as the interval between serial tests is decreased.
In the absence of documented nosocomial epidemics of tuberculosis, almost all estimates of hospital transmission of tuberculosis infection are less than 1 percent yearly. If the previous estimates of specificity are accepted, the predictive value of positive tuberculin test done at yearly intervals in such populations will be less than 50 percent. If the assumption that the false-positive rate is a random biologic event is correct, this positive predictive value would be further reduced by testing at 6- or 3-month intervals.
The major value of a serial skin testing program is to alert the system that an abnormally high rate of tuberculosis transmission is occurring.(28,29,30,31,32)Table B-2 shows the range of actual transmission of infection based on the observed rate of skin test conversion assuming a 99 to 99.5 percent specificity. Skin test conversion rates below 1 percent probably reflect very low actual transmission and the majority of skin test conversions are probably false-positive reactions. Conversion rates above 2 percent probably represent actual transmission of infection.
Implications of Decreased Positive-Predictive Value for Tuberculin Test on a Tuberculosis Program
Almost all information concerning interventions in tuberculosis infection without disease are based on studies in populations with a high prevalence of tuberculosis infection and thus a high positive predictive value of the tuberculin skin test. A good example is preventive therapy. Estimates of efficacy and efficiency of preventive therapy are based on
TABLE B-2. Range of Actual Transmission Rates for Observed Skin Test Conversion Rate
|
Conversion Rate |
Actual Transmission Rate (%) |
|
0.5 |
~0 |
|
1 |
0–0.5 |
|
2 |
0.5–1 |
|
5 |
4–4.5 |
data from populations where a positive tuberculin reaction had a very high likelihood of indicating true infection.
If we apply these interventions to populations with a lesser likelihood of being truly infected, two phenomena will occur. The first is that the effectiveness of the intervention will appear to be increased. As the number of persons with false-positive reactions increases, the likelihood of true infection in the population decreases, and the likelihood of disease developing subsequent to the intervention decreases in like proportion. Second, the true effectiveness of the intervention actually decreases. As the proportion of people with the condition to be prevented decreases, there is less to prevent and the number of cases actually prevented falls. This actual decrease in true benefit results in a rise in the cost-benefit and risk-benefit ratios.
REFERENCES
1. Koch R.Über bacteriologische Forschung. Deutsche Medizinische Wochnschrift 1890; 16:756 (translated in Lancet 1890; 2:673).
2. Editorial. The nature of Dr. Koch’s liquid. Lancet 1890; 2:1233.
3. Editorial. Koch and his critics. Journal of the American Medical Association 1890; 15:902.
4. Koch R.Fortsetzung der Mittheilungen über ein Heilmittel gegen Tuberculose. Deutsche Medizinische Wochnschrift 1891; 17:101 (translated in Lancet 1891; 1:168).
5. Green H.H. Discussion on tuberculins in human and veterinary medicine. Proceedings of the Royal Society of Medicine 1951; 44:1045.
6. Seibert F.B. The isolation and properties of the purified protein derivative of tuberculin. American Review of Tuberculosis 1934; 30:713.
7. Seibert F.B. and Glenn J.T. Tuberculin purified protein derivative: preparation and analyses of a large quantity for standard. American Review of Tuberculosis 1941; 44:9.
8. Landi S., Held H.R., Houschild A.H.W., et al. Adsorption of tuberculin PPD to glass and plastic surfaces. Bulletin of the World Health Organization 1966; 35:593–602.
9. Zack M.B. and Fulkerson L.L. Clinical reliability of stabilized and nonstabilized tuberculin PPD. American Review of Respiratory Diseases 1970; 102:91–93.
10. Sbarbaro J.A. Skin test antigens: an evaluation whose time has come. American Review of Respiratory Diseases 1978; 118:1–5.
11. Edwards L.B., Acquaviva F.A., Livesay V.T., Cross F.W., and Palmer C.E. An atlas of sensitivity to tuberculin, PPD-B, and histoplasmin in the United States. American Review of Respiratory Diseases 1969; 99:1–132.
12. Furcolow M.L., Hewell B., Nelson W.E., and Palmer C.E. Quantitative studies of the tuberculin reaction. I. Titration of tuberculin sensitivity and its relation to tuberculous infection. Public Health Reports 1941; 56:1082.
13. Sokal J.E. Measurement of delayed skin-test responses. New England Journal of Medicine 1975; 293:501–502.
14. Bass J.B. The tuberculin test. IN: Reichman L.B., Hershfield E.S. (eds.). Tuberculosis: A Comprehensive International Approach. Marcel Dekker, New York, 1993.
15. Huebner R.E., Schein M.F., and Bass J.B. The tuberculin skin test. Clinical Infectious Diseases 1993; 17:968–975.
16. Edwards P.Q. and Edwards L.B. Story of the tuberculin test. American Review of Respiratory Diseases 1960; 81:1–49.
17. Holden M., Dubin M.R., and Diamond P.H. Frequency of negative intermediate-strength tuberculin sensitivity in patients with active tuberculosis. New England Journal of Medicine 1971; 285:1506–1509.
18. Nash D.R. and Douglass J.E. A comparison between positive and negative reactors and an evaluation of 5 TU and 250 TU skin test doses. Chest 1980; 77:32–37.
19. ATS/CDCP (American Thoracic Society/Centers for Disease Control and Prevention). Targeted tuberculin testing and treatment of latent tuberculosis infection. American Journal of Respiratory and Critical Care Medicine 2000; 161:S221–S247.
20. Sepulveda R.L., Ferrer X, Latrach C, and Sorensen R.U. The influence of Calmette-Guérin bacillus immunization on the booster effect of tuberculin testing in healthy young adults. American Review of Respiratory Diseases 1990; 142:24–28.
21. Daniel T.M. and Janicki B.W. Mycobacterial antigens: a review of their isolation, chemistry, and immunological properties. Microbiological Review 1978; 42:84–113.
22. Bowden K.M. and McDiarmid M.A. Occupationally acquired tuberculosis: what’s known. Journal of Occupational Medicine 1994; 36:320–325.
23. Aitken M.L., Anderson K.M., and Albert R.K. Is the tuberculosis screening program of hospital employees still required? American Review of Respiratory Diseases 1987; 136:805– 807.
24. Thompson N.J., Glassroth J.L., Snider D.E., Jr., and Farer L.S. The booster phenomenon in serial tuberculin testing. American Review of Respiratory Diseases 1979; 119:587–597.
25. Bass J.B., Jr., and Serio R.A. The use of repeat skin tests to eliminate the booster phenomenon in serial tuberculin testing. American Review of Respiratory Diseases 1981; 123:394–396.
26. Bass J.B., Sanders R.V., and Kirkpatrick M.B. Choosing an appropriate cutting point for conversion in annual tuberculin skin testing. American Review of Respiratory Diseases 1985; 132:379–381.
27. De March-Ayuela P. Choosing an appropriate criteria for true or false conversion in serial tuberculin testing. American Review of Respiratory Diseases 1990; 141:815–820.
28. Louther J., Rivera P., Feldman J., Villa N., DeHovitz J., and Sepkowitz K.A. Risk of tuberculin conversion according to occupation among health care workers at a New York City hospital. American Journal of Respiratory and Critical Care Medicine 1997; 156:201–205.
29. Fella P., Rivera P., Hale M., Squires K., and Sepkowitz K. Dramatic decrase in tuberculin skin test conversion rate among employees at a hospital in New York City. American Journal of Infection Control 1995; 23:352–356.
30. Sotir M.J., Khan A., Bock N.N., and Blumberg H.M. Risk factors for tuberculin skin test (TST) positivity and conversion among employees at a public inner-city hospital in a high incidence area. Journal of Investigative Medicine 1997; 45:64 A.
31. Blumberg H.M., Sotir M., Erwin M., Bachman R., and Shulman J.A. Risk of house staff tuberculin skin test conversion in an area with a high incidence of tuberculosis. Clinical and Infectious Diseases 1998; 27:826–833.
32. Boudreau A.Y., Baron S.L., Steenland N.K., Van Gilder T.J., Decker J.A., Galson S.K., Seitz T. Occupational risk of Mycobacterium tuberculosis infection in hospital workers. American Journal of Industrial Medicine. 1997; 32:528–534.










