5
Occupational Risk of Tuberculosis
This chapter reviews what is known about the workplace risk of tuberculosis among employees covered by the proposed rule on occupational tuberculosis issued in 1997 by the Occupational Safety and Health Administration (OSHA). The specific questions addressed here include the following: Are health care and selected other categories of workers at a greater risk of infection, disease, and mortality due to tuberculosis than others in the community within which they reside? If so, what is the excess risk due to occupational exposure? Can the risk of occupational exposure be quantified for different work environments and different job classifications?
Most of the information relevant to these questions involves the occupational risk of tuberculosis in hospitals and, to a lesser extent, prisons. The committee found limited very information about the occupational risk of tuberculosis in other correctional settings, long-term-care facilities, home health and home care services, outpatient clinics of various kinds, and homeless shelters. The problem is not just that such information is unavailable to outsiders but that it may also be unavailable to support internal assessments of risk and then guide appropriate responses. This scarcity of surveillance information for settings such as homeless shelters and local jails is a concern because many of these facilities serve people at increased risk of active tuberculosis—including those who are unemployed, homeless, or poor; people with HIV infection or AIDS or substance abuse problems; and recent immigrants from countries with high rates of tuberculosis. Unlike hospitals, these organizations often lack strong institutional and professional traditions of in-
fection control, and the extent of external oversight by government agencies, accrediting bodies, or other entities varies. In addition, many of these facilities do not operate in an environment in which an outbreak of tuberculosis might threaten their reputations, although they may be vulnerable to civil law suits (e.g., by inmates citing deficient health and safety measures).
An assessment of the occupational risk of tuberculosis needs to take historical context into account. As described in Chapter 1, during the late 1980s and early 1990s, outbreaks of tuberculosis in several large, urban hospitals helped focus attention on the risk of tuberculosis in health care settings. They also raised concern about lapses in infection control measures. These outbreaks occurred against a backdrop of resurgent tuberculosis that has been linked to underfunded public health programs, incomplete treatment of the disease, and increasing numbers of people at risk because of human immunodeficiency virus (HIV) infection, homelessness, imprisonment, and immigration from countries where tuberculosis is common. Although these problems have not disappeared, they have been mitigated by increased funding for community tuberculosis control, intensive programs of directly observed therapy, more effective treatments for HIV infection and AIDS, and increased attention to tuberculosis control measures in the workplace. Since 1993, national tuberculosis case rates have dropped for seven successive years.
The discussion in this chapter draws extensively on the background paper by Thomas M.Daniel in Appendix C. That paper provides a more detailed review of the relevant literature and its limitations.
CONCEPTS AND DEFINITIONS
In its simplest sense, occupationally acquired disease means disease acquired during the course of a person’s work. The focus of those concerned about workplace transmission of tuberculosis is, however, on identifying workers whose duties could be reasonably anticipated to bring them into contact with (1) people who have infectious tuberculosis or (2) air that contains Mycobacterium tuberculosis. In OSHA’s terminology, this anticipated contact—not actual exposure—constitutes occupational exposure. Thus, a respiratory therapist in a facility that treats patients with tuberculosis would normally be categorized as having occupational exposure, whereas a financial analyst in the facility’s administrative offices normally would not.
Risk has a variety of technical and popular meanings, and the committee recognizes the technical, political, and ethical controversies and debates that surround the concept of risk, the characterization of risk, and public perceptions of risk (NRC, 1983, 1996). Used in a general sense, risk refers to the probability of adverse health effects of, for example, expo-
sure to infectious tuberculosis.1 The occupational risk of tuberculosis is the probability of acquiring tuberculosis infection or active tuberculosis as a result of workplace exposure. Occupational risk is usually described statistically. Depending on the purpose of an analysis and the available data, it can be described in absolute terms (for example, as the risk of acquiring active tuberculosis during a year or a working lifetime for a particular category of worker) or in comparative terms (for example, one group’s risk compared with another’s). Comparative data help in identifying possible causes of or contributors to a problem (e.g., by comparing skin test conversion rates in different areas of a facility). Comparisons also help in understanding or communicating the magnitude of a problem and in assessing priorities for spending public health funds or other resources.
CDC lists two options for defining a case of active tuberculosis (CDC, 2000b). The laboratory definition requires either the isolation of M. tuberculosis from a clinical specimen or the demonstration of acid-fast bacilli in a clinical specimen when a specimen for culture was not or could not be obtained. The clinical case definition requires all of the following: a positive tuberculin skin test result; other signs and symptoms compatible with tuberculosis (e.g., abnormal and unstable radiologic findings or persistent cough), treatment with two or more antituberculous medications, and a completed diagnostic evaluation. Physicians may begin treatment of suspected infectious tuberculosis based on symptoms and risk factors while awaiting test results.
The definition of infection with M. tuberculosis is based only on test results, specifically, the results of the tuberculin skin test. The foundation of workplace surveillance programs has been the finding and investigating of tuberculin skin test conversions. As discussed in Chapter 2 and Appendix B, the tuberculin skin test has serious limitations as a community or workplace surveillance tool, particularly in communities and workplaces where tuberculosis is uncommon. In very low-prevalence locales, most skin test conversions will be false positives.
In general, occupationally acquired tuberculosis infection or disease is easier to define than to document. Nationally reported data on the occupational status of reported tuberculosis cases do not distinguish between cases originating in the workplace and those originating in the
community. Direct evidence about the source of transmission typically comes from investigations of possible workplace outbreaks of tuberculosis. In this context, an “outbreak” may be defined as transmission of M. tuberculosis that results in infection or active disease among workers, patients, and others exposed in a health care facility, prison, or other setting in which people with tuberculosis are treated, served, or detained (Garrett et al., 1999).2 Investigations of possible outbreaks include the careful questioning of affected workers not only about possible workplace exposures but also about possible community-related exposures involving family members and other close contacts outside of work.
Some outbreak investigations are supported by molecular epidemiology (DNA fingerprinting), which compares isolates of M. tuberculosis recovered from different individuals. Molecular analyses can help establish a chain of transmission that links workplace cases of active tuberculosis (but not infection) to source cases in the workplace or the community. As discussed further below, inferences about the source of infection or disease for a worker are still most often based on comparisons of occupational and demographic information for workers with and without occupational exposure to tuberculosis. In some cases, no clear source of infection or transmission—either work related or community based—is identified.
In analyses of tuberculosis risk in workplaces and communities, the term “community” or “community of residence” has no precise definition.3 Although a facility’s location may be identified as a particular city, county, or metropolitan area, the residences of workers in that facility may be widely spread across areas with very different rates of tuberculosis. For example, someone living in central Harlem can be expected to have a higher risk of community exposure to tuberculosis than someone from the Connecticut suburbs.
Few studies have matched detailed information on worker place of residence against equally detailed community data on tuberculosis cases. Information on a worker’s home zip code may improve on city or county as an indicator of community of residence, but a single zip code may still encompass an area with quite variable resident characteristics (e.g., incidence of tuberculosis and income levels). Also, collection of zip code data
from workplace records can be very labor intensive, and address information may not be current or entered into computer databases. Because tuberculosis is negatively correlated with income, some studies have also investigated whether places of residence for workers with converted skin tests are clustered in low-income—and presumably higher-risk—areas. Others have simply used low income as a surrogate for higher risk of community exposure.
HISTORICAL PERSPECTIVES ON THE OCCUPATIONAL RISK OF TUBERCULOSIS
A review article by Sepkowitz (1994) summarizes studies from the 1920s through the 1950s that showed that nurses, physicians, and others working with tuberculosis patients had high rates of positive skin tests or skin test conversions compared to the rates expected in the broader community. For nursing students who were initially tuberculin skin test negative, conversion rates reported in studies in the United States and Europe ran as high as 95 to 100 percent by the time the students graduated. The reported yearly incidence of active tuberculosis ranged from 2 to 12 percent in nursing schools.4 Comparative data on nonhealth care occupations or work settings is limited, but Sepkowitz cites studies in the 1930s that reported the incidence of active tuberculosis to be 1 percent for employees of a life insurance company and 2 percent for food handlers.
Other early studies reviewed by Sepkowitz focused on medical students. One survey of those who had been medical students between 1940 and 1950 reported a tuberculosis case rate of 334 per 100,000 medical students per year. In the general population during that period, the estimated tuberculosis case rates ranged between 32 and 100 per 100,000 population per year. Another study identified a particularly high risk to medical students of participation in autopsies on those who died with active tuberculosis.
Sepkowitz cites a 1953 study (Mikol et al., 1953) that found that hospital workers with direct patient contact had an 8- to 10-fold higher incidence of tuberculosis compared with that for workers without direct contact. A review by Menzies and colleagues of studies conducted in the 1960s reported that health care workers exposed to patients with known tuberculosis had a four to six times greater incidence of infection with M. tuberculosis than unexposed workers (Menzies et al., 1995). The quality of the studies that they reviewed varied considerably.
In sum, a number of studies indicate that health care workers, especially those who cared for patients, have historically been at higher risk of infection and disease than the general population. By the 1960s, effective treatment of tuberculosis was becoming widely available and public health programs were mobilizing to control if not eliminate the disease. In addition, health care facilities were beginning to adopt some tuberculosis control measures such as screening patients with chest radiographs and isolating those with known or suspected infectious disease.
MORE RECENT INFORMATION ON THE COMMUNITY AND OCCUPATIONAL RISK OF TUBERCULOSIS
U.S. Government Surveys and Databases
General Population
Active Tuberculosis and Mortality from Tuberculosis CDC reports annually on cases of active tuberculosis nationwide and by state and selected cities (see, e.g., CDC [2000b]). It reports national mortality data but does not break deaths down by state or other category.
Chapter 1 described the resurgence in tuberculosis cases and case rates beginning in 1985, an increase that followed uninterrupted declines since national data were first reported in 1953. After reaching a high of 10.5 per 100,000 population in 1992 (13 percent higher than in 1985), rates began to decline again in 1993. Case rates and case numbers reached their lowest levels yet in 1999, when CDC reported a case rate of 6.4 per 100,000 population and 17,528 cases of tuberculosis (CDC, 2000b). Rates of death from tuberculosis, which also rose in the 1980s and early 1990s, have also declined in recent years from 0.8 per 100,000 in 1989 to 0.4 per 100,000 in 1998, and numbers of deaths declined from 1,970 to 1,110.
CDC data make it clear that tuberculosis is not evenly distributed within the United States. For example, the increase in case rates from 1985 to 1992 was largely concentrated in a few states. During this period, the seven states with case rate increases of 4 percent or more (1984 to 1991) showed a collective increase from 11.2 to 16.8 cases per 100,000 popula-
tion (Comstock, 2000). In contrast, the overall case rate for the other states dropped from 8.5 to 7.4 cases per 100,000.
In 1999, case rates among states ranged from 0.5 per 100,000 population in Vermont to 15.5 per 100,000 population in Hawaii. Among metropolitan areas, rates varied from less than 1.3 per 100,000 population in Omaha to 17.7 per 100,000 population in New York City and 18.2 per 100,000 population in San Francisco. Data from government surveys and databases as well as other sources fairly consistently show that rates of active tuberculosis vary by race, ethnicity, age, and country of origin. Table 5-1 shows that such demographic variation persists despite the decline in case rates during recent years. As reported in Chapter 1, over 40 percent of tuberculosis cases reported in U.S. in 1999 involved people born in other countries with individuals from Mexico, the Philippines, and Vietnam accounting for nearly half of the cases among foreign-born persons.
TABLE 5-1. Tuberculosis Case Rates per 100,000 Population, United States, 1989–1999
|
Year |
1989 |
1992 |
1993 |
1999 |
|
Race/ethnicitya |
||||
|
White, non-Hispanic |
4.0 |
4.0 |
3.6 |
2.2 |
|
Black, non-Hispanic |
29.5 |
31.7 |
29.1 |
16.8 |
|
Hispanicb |
19.3 |
22.4 |
20.6 |
12.4 |
|
American Indian/Alaska Native |
19.8 |
16.2 |
14.6 |
11.8 |
|
Asian/Pacific Islander |
39.8 |
46.3 |
44.5 |
35.3 |
|
Unknown/missing |
0 |
0 |
1 |
0 |
|
Country of originc |
||||
|
U.S. born |
NAd |
8.2 |
7.4 |
4.0 |
|
Foreign borne |
NA |
34.2 |
33.6 |
29.2 |
|
Unknown |
2 |
1 |
2 |
1 |
|
Agea |
||||
|
0–14 years |
2.5 |
3.1 |
3.0 |
1.8 |
|
15–24 |
4.8 |
5.5 |
5.1 |
4.0 |
|
25–44 |
10.6 |
12.7 |
11.6 |
7.3 |
|
45–64 |
12.4 |
13.4 |
12.5 |
8.2 |
|
65+ |
19.7 |
18.7 |
17.8 |
11.7 |
|
Not stated |
0 |
0 |
0 |
0 |
|
aDenominators for computing these rates were based on official post-census estimates from the U.S. Census Bureau. bPersons of Hispanic origin may be of any race. cDenominators for computing these rates were obtained from Quarterly Estimates of the United States Foreign-born and Native Resident Populations: April 1, 1990 to July 1, 1999 (www.census.gov/population/estimates/nation/nativity/fbtab001.txt) dNA equals data not available. eIncludes persons born outside the United States, American Samoa, the Federated States of Micronesia, Guam, the Republic of the Marshall Islands, Midway Island, the Commonwealth of the Northern Mariana Islands, Puerto Rico, the Republic of Palau, U.S. Minor Outlying Islands, U.S. Miscellaneous Pacific Islands, and the U.S. Virgin Islands. SOURCE: CDC, 2000b (excerpted from Tables 2, 3, and 4). |
||||
Infection with M. tuberculosis In contrast to active tuberculosis, no routinely collected, national data document the prevalence or incidence of infection with M. tuberculosis in the U.S. population overall or in major population subgroups. The last effort to collect systematic information on the prevalence of tuberculosis infection nationwide dates back to the 1971– 1972 National Health Survey. For that survey, trained personnel administered and read tuberculin skin tests for a national sample of American adults. Based on the results, analysts estimated the prevalence of skin test reactivity among adults aged 25 to 74 years to be 21.5 percent during the survey period (Engel and Roberts, 1977).
In the risk assessment section of its 1997 proposed rule on tuberculosis, OSHA presented an estimate of the prevalence of latent tuberculosis infection in the United States developed by Christopher Murray. Using a mathematical model of tuberculosis transmission, Murray estimated the prevalence of latent tuberculosis infection in 1994 to be about 6.5 percent for Americans over age 18 (62 FR 201 at 54199 [Table V-6] October 17, 1997).
Working from Murray’s prevalence estimates, OSHA estimated the weighted annual risk of infection for the U.S. population to be approximately 0.146 percent. For individual states, the estimates ranged from 0.02 percent in New Hampshire to 0.30 percent in New York and 0.35 percent in Hawaii. OSHA used these prevalence and incidence estimates as the bases for comparing the occupational risk of tuberculosis with the background risk of the disease in the general population (see Chapter 7).
In Appendix C, Daniel uses a technique for estimating the annual risk of tuberculosis infection based on the empiric ratio between this risk and the incidence of active disease (Daniel and Debanne, 1997). Using data derived from white male naval recruits between 1958 and 1965, he estimated this ratio to be approximately 150. When that ratio is applied to the 1998 tuberculosis case rate for the United States, it yields an annual risk of infection of approximately 0.05 percent per year, which is about one-third of the 0.146 percent per year figure used by OSHA in its risk assessment. The higher OSHA figure may reflect differences in the reference year used, their inclusion of racial and ethnic minorities, and possibly other factors such as the impact of HIV infection and AIDS since 1980.
Health Care and Other Workers
Active Tuberculosis and Mortality from Tuberculosis Since 1994 (for the year 1993), the CDC has reported occupational information for people diagnosed with active tuberculosis. The CDC data do not allow one to draw conclusions about the source—workplace versus community—of workers’ exposure to tuberculosis.
In 1999, those who had reported they were unemployed within the preceding 24 months accounted for nearly 60 percent of all cases of the disease (CDC, 2000b). Those who reported their occupation as health care workers within the preceding 24 months accounted for approximately 2.6 percent of the cases nationwide, down from 3.0 percent in 1998. In 1998, health care workers accounted for about 9 percent of employed persons and 8 percent of tuberculosis cases among employed persons (Amy Curtis, CDC, 2000, personal communication).5 During the period from 1994 to 1998, six states—California, Florida, Illinois, New Jersey, New York, and Texas—accounted for 57 percent of the cases of tuberculosis among health care workers and about the same percentage of all tuberculosis cases. (The six states account for just under 40 percent of the U.S. population.)
As shown in Figure 5-1, for the period 1994 to 1998, the overall incidence of active tuberculosis among health care workers was similar to that for other employed workers—about 5.1 per 100,000 population for the former and 5.0 per 100,000 population for the latter (Curtis et al., 1999). Between 1994 and 1998, the tuberculosis case rate for health care workers dropped from 5.6 to 4.6 per 100,000 population, whereas the rates for other employed workers stayed relatively steady at 5.2 per 100,000 population in both 1994 and 1998.
Looking only at cases of drug-resistant tuberculosis among U.S.-born workers from 1994 to 1998, CDC analysts found significantly higher rates of drug-resistant disease for health care workers (3.2 percent of cases) than for other workers (1.5 percent of cases) (Panlilio and Curtis, 2000). For the 2 most recent years, the difference in rates for the two groups was not statistically significant.
Among foreign-born health care workers, those born in the Philippines account for the largest percentage of cases of active tuberculosis (about 33 percent) (Curtis et al., 1999). Among all foreign-born employed workers (and for the U.S. population generally), those born in Mexico accounted for the highest percentage (about 25 percent) of tuberculosis cases.
In 1999, CDC reported that workers in correctional facilities accounted for about 0.1 percent of cases of active tuberculosis (CDC, 2000b). Most information on correctional facilities focuses on inmates, who have much
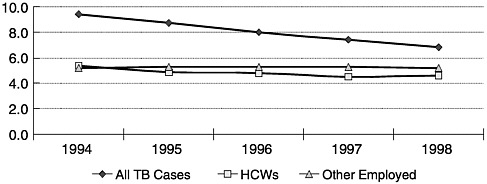
FIGURE 5-1. Tuberculosis incidence rates per 100,000 population by year and reported employment status within preceding 24 months. TB equals tuberculosis; HCW equals health care workers. SOURCE: Curtis et al. (1999).
higher rates of tuberculosis than the general population.6 A 1999 U.S. Department of Justice report could not report national data on tuberculosis case rates for inmates, but it cited New York State data for inmates showing a decrease in case rates from approximately 175 per 100,000 population in 1991 to 30 per 100,000 population in 1997 (NIJ, 1999). Factors identified by CDC as contributing to increased tuberculosis risk in correctional facilities included increasing numbers of HIV-infected inmates, crowding, and poor ventilation. Many workers in correctional facilities are also likely to be affected (although less intensely so) by these conditions.
Occupational information is not routinely reported for tuberculosis deaths. It is, however, recorded on death certificates. The committee found one analysis of data for 1979 to 1990 from the National Occupational Mortality Surveillance database (CDC, 1995a). In that analysis, CDC researchers identified occupational groups that had both four or more deaths from pulmonary tuberculosis and a high proportionate risk of mortality from the disease. In the 21 occupational groups that met their criteria, two race- and sex-specific subgroups had potential workplace exposure to tuberculosis. They were white male funeral directors
and white male health and nursing aides, orderlies, and attendants. Of the other occupational subgroups identified, six were classified as having the potential for substantial exposure to silica and two were associated with low socioeconomic status.
Infection with M. tuberculosis In 1992, concerned about a number of hospital outbreaks of tuberculosis, CDC sent questionnaires all 632 public hospitals and a 20 percent sample (444 institutions) of private hospitals with 100 beds or more that were listed in the American Hospital Association database (Manangan et al., 1998). About 70 percent for each group responded (726 institutions in total). Ninety-six of 716 hospitals (13 percent) reported transmission of M. tuberculosis to health care workers. In 1996, CDC randomly selected and resurveyed half of the 272 hospitals that had reported six or more admissions of tuberculosis patients in the 1992 survey (Manangan et al., 1998, 2000). Seventy-five percent (103 facilities) responded. In that survey of higher-risk facilities, 7 percent of 103 respondents reported transmission of M. tuberculosis to workers.
In 1995, CDC began a demonstration project to develop better estimates of workplace-related skin test conversions among health care workers and to test software to support more systematic collection and analysis of skin test data (McCray, 1999a,b). The project recruited 32 participating facilities from nine jurisdictions including both high-prevalence areas (New York City and San Francisco) and low prevalence areas (Oregon and Colorado). Using data collected prospectively from the demonstration project sites, CDC analysts reported an overall tuberculin skin test conversion rate of 5.9 per 1,000 health care workers. Rates differed little among the types of participating organizations (nine hospitals, seven correctional facilities, five health departments, two nursing homes, and seven other types of facilities). After adjusting for race, foreign birth, New York City residence, and household exposure, analysts found no statistically significant associations between skin test conversions and the occupational categories used (administrative/clerical, nurse, outreach worker, physician/physician’s assistant, and other). Data were not collected on the extent of workers’ contact with patients or on their work location within facilities (e.g., medical ward). More than 20 percent of those participating had either a positive skin test history or a positive test result at the baseline.
Additional, older data analyzed in Appendix C by Daniel are mixed. He concludes that health care workers are at risk in the workplace of being infected with tuberculosis but that the risk has been declining in recent years and now approaches community levels. Where modern infection control measures have been implemented, occupational risk approaches the level of risk in the communities in which workers reside.
Overall, data for the mid-1990s do not show that health care workers as a group are at higher risk of active tuberculosis than other employed
workers, but for some of the period they may have been at higher risk of multidrug-resistant disease. No national data report on the rate of tuberculosis infection among workers, but a small CDC demonstration project has suggested no association between job category and risk after demographic factors were taken into account. No recent occupation-specific mortality rates are available, but an analysis of older data suggests that some subgroups of health care workers may have been at higher risk of death than other workers.
Other Surveys and Reports Not Involving Outbreaks
Literature Reviews
In a 1995 review of data on tuberculosis among health care workers, Menzies and colleagues reviewed studies based on disease registries in several other countries. The studies reported “estimated risk ratios of 0.6 to 2.0, indicating at most only modest increased risk” of disease for health care workers compared with that for others in the community (Menzies et al., 1995, p. 92). Menzies and colleagues noted that such studies may underestimate risk because they do not standardize for age. This is important because the working population is younger and healthier than the general population. The authors also noted that cohort nor disease registry analyses are limited by “the inability to distinguish occupational from nonoccupational exposure” (Menzies et al., 1995, p. 92). The review also covered questionnaire studies from the 1950s through the 1980s that reported higher rates of disease for pathologists, certain laboratory technicians, and physicians. It noted concerns about modest response rates and possible recall biases for these studies. The authors identified no “recent” cohort studies comparing the risk of infection with M. tuberculosis among U.S. health care workers with the risk among individuals in the general community. Although they reviewed several studies reporting rates of tuberculosis infection among health care workers, the authors cited the limitations of the studies and did not present an overall assessment of infection risk in the postantibiotic era. They did not present mortality data.
Garrett and colleagues also reviewed U.S. surveys and surveillance reports for a variety of health care workers (e.g., physicians and house staff) and locales dating back to the 1960s (Garrett et al., 1999). They concluded that “available data suggest that the [annual] risk of [tuberculin skin test] conversions among hospital employees in general [i.e., for all categories of workers in nonoutbreak situations] is approximately 1 percent or less” (Garrett et al., 1999, p. 484). They did not present corresponding disease or mortality estimates. The authors noted that the data, which were sometimes inconsistent and subject to many methodologic limita-
tions, also suggested that the risk of conversions varied considerably by type of hospital, geographic location, job category, and likelihood of contact with high-risk patients. (This review’s discussion of outbreak reports is summarized later in this chapter.)
Another review by Dooley and Tapper (1997) similarly concluded that overall skin test conversion rates for facilities are typically 1 percent or less in nonoutbreak environments, but they emphasized that “overall rates in a facility can mask very high rates in some areas or occupational groups” (p. 368). In studies not specific to outbreak situations, the review authors found mixed results for comparisons of skin test conversion rates for different job categories and different assumed levels of patient contact. Some studies found higher skin test conversion rates for those in jobs with more patient contact (e.g., nursing and respiratory therapy); others did not. The work categorization and other methods and the detail reported in these studies varied considerably (e.g., whether categorizations by patient contact differentiated between contact with patients at high risk of tuberculosis and contact with other patients). The review authors noted that skin test conversion rates in health care workers probably represent a combination of community- and workplace-related transmission of M. tuberculosis. (This review’s discussion of outbreak reports is summarized later in this chapter.)
Individual Studies and Reports
During the 1980s and 1990s, a number of published articles reported skin test conversion information from state databases, surveys, or studies in one or a few organizations. Most are limited to hospitals.
In a 1987 article entitled “Is the Tuberculosis Screening Program of Hospital Employees Still Required?,” researchers at the University of Washington analyzed skin test conversion data for 1982 to 1984 for 114 hospitals in Washington (Aitken et al., 1987). They put the estimated overall conversion rate for these hospitals at 0.09 percent over the 3-year period (0.03 percent per year), with slightly higher rates for hospitals that admitted tuberculosis patients and slightly lower rates for those that did not. They concluded that the conversion rates in hospitals did not differ significantly from the estimated rate for the state population overall.
A study in a nonoutbreak environment found correlations between positive skin test conversions and the worker’s age, the worker’s race, and the poverty level in the worker’s zip code of residence (Bailey et al., 1995). (Data on tuberculosis case rates were not reported by zip code.) For the period January 1989 through July 1991, the overall rate of skin test conversions was 0.93 percent (0.37 percent annually). After controlling for other variables, the analysts found an association between higher poverty levels and higher rates of positive skin tests and test conversions. Risk
was not associated with patient contact or occupational category, so analysts concluded that community rather than occupational exposure was more likely.
In a national survey that focused on infection control measures, responding hospitals showed overall annual skin test conversion rates of 0.6 to 0.7 percent for 1989 through 1992 (Sinkowitz et al., 1996). Higher conversion rates were found among those involved in bronchoscopy (3.7 percent) and respiratory therapy (1.0 percent). No information was collected on employee demographic characteristics or on the details of the testing procedures used by the facilities.
Another study reporting higher rates of skin test conversions for respiratory therapists involved a military medical center in Maryland (Ball and Van Wey, 1997). Annual skin test conversion rates, which ranged between 0.4 and 2.6 percent across the occupational categories identified, did not differ significantly for patient-contact and non-patient-contact categories. Respiratory therapists, however, had an annual conversion rate of 15.6 percent.
In a study of 56 of 167 North Carolina hospitals reporting data on tuberculin skin test conversions, researchers reported a 5-year mean annual conversion rate for all employees of 1.14 percent (Price et al., 1987). Mean annual conversion rates varied by region of the state (1.80 percent in the east, 0.70 percent in the center, and 0.61 percent in the west). This was consistent with variations in rates for the general population in these sections of the state. The researchers concluded that this association pointed to community rather than workplace origins for new employee infections with M. tuberculosis. In its initial risk assessment for the proposed rule on tuberculosis, OSHA analysts also used these North Carolina data. After critics noted the high prevalence of atypical mycobacteria in the eastern part of North Carolina, the analysts used only the figures for hospitals in the western part of the state to estimate the risk of infection for workers in areas with a moderate prevalence of active tuberculosis. (Other criticisms of the data noted the high nonresponse rate, the limited use of two-step initial testing, and inconsistencies in testing practices. See Chapter 7 for further discussion.)
For its risk assessment, OSHA staff used 1994 Washington State data as a basis for estimating worker risk in low-prevalence areas (62 FR 201). Based on comparisons between hospitals “in zero-TB counties and with no known TB patients” and other hospitals, they estimated that the occupational risk of transmission of M. tuberculosis in Washington State hospitals was 1.5 times higher than the background rate of transmission. For other ways of comparing hospitals, the estimated risk was less. For employees of long-term-care facilities (including nursing homes) and home health care workers, OSAH estimated the risk to be 11 and 2 times the background rate respectively. As noted earlier, OSHA estimated the latter
risk to be about 0.15 percent per year. (OSHA’s risk assessment is reviewed in Chapter 7.)
A few reports focus on correctional facilities. A 1994–1995 survey of correctional facilities noted that many responding facilities could not report skin test conversions because skin testing for employees was done by private physicians and the results were not communicated and entered into employee records (NIJ, 1996). A later survey found that more than half of state and federal prison systems and more than a third of the jail systems failed to report conversion data (NIJ, 1999).
At the Cook County Jail in Chicago, the facility began offering tuberculin skin testing to health care workers (mandatory) and correctional officers (voluntary) in 1994 (McAuley, 2000). Health care staff at the jail have documented 24 known exposure episodes involving workers and have concluded that these were associated with 10 documented and 30 possible skin test conversions, none of which involved health care workers. The test results for correction officers did not differ by the area of the facility in which they worked.
Outbreak Reports
This section reviews information from published reports of workplace outbreaks of tuberculosis. Most reports of outbreaks have involved units of hospitals including inpatient medical wards (general medical, HIV, infectious disease, and renal transplant units), surgical suites, emergency departments, laboratories, intensive care units, an autopsy room, radiology suites, an inpatient hospice, outpatient clinics, and bronchoscopy rooms (see Dooley and Tapper [1997], Garrett et al. [1999], and Appendix D).
Probable cases of workplace transmission of tuberculosis have also been reported in prisons and jails (Campbell et al., 1993; Pelletier et al., 1993; Prendergast et al., 1999; Bergmire-Sweat et al., 1996; Jones et al., 1999), a freestanding primary care clinic (Howell et al., 1989), long-term-care facilities (Stead, 1981; Munger et al., 1983; Stead et al., 1985; Brennen et al., 1988 [and possibly Steimke et al., 1994]), a residential HIV infection treatment facility (Hoch and Wilcox, 1991), homeless shelters (Nolan et al., 1991; Curtis et al., 2000; Moss et al., 2000), public health laboratories (Kao et al., 1997), a medical examiner’s office (Ussery et al., 1995), and a funeral home (Sterling et al., 2000a). In addition, outbreaks have been reported in settings where occupational exposure is not anticipated, including naval vessels and airplanes (DiStasio and Trump, 1990; Aguado et al., 1996).
Low-prevalence communities are not immune from outbreaks. For example, CDC investigators recently reported an outbreak in North Dakota. It involved a child from the Marshall Islands who transmitted M.
tuberculosis to 3 of 4 household members, 16 of 24 classmates, 10 of 32 school-bus riders, and 9 of 61 day-care contacts (Curtis et al., 1999). This case was also unusual because tuberculosis in children is not usually transmitted to others.
Although national CDC data show approximately 400 to 600 cases of tuberculosis in health care workers per year in recent years, case investigations of hospital or other outbreaks indicate that outbreaks reports account for only a small number of all cases of tuberculosis (Dooley and Tapper, 1997; Garrett et al., 1999, CDC, 2000b). For example, the 19 outbreak reports (1965 to 1995) summarized by Dooley and Tapper (1997) covering the period 1965 to 1995 account for fewer than 50 cases of active disease among health care workers. The 28 outbreak reports (one covering more than one institution) (1962 to 1996) reviewed by Garrett and colleagues (1999) account for fewer than 90 cases, of which 27 were associated with one 1962 to 1964 outbreak. The outbreak investigations have linked some cases of active disease to workplace exposure, but other cases were not explicitly linked to either a workplace or a community source. The reviews by Dooley and Tapper and Garrett and colleagues did not report on deaths associated with the outbreak studies they summarized, although Garrett and colleagues noted 9 deaths among at least 20 workers known to have contracted multidrug-resistant disease. Chapter 6 discusses what these investigations suggest about the association between outbreaks and the implementation of tuberculosis control measures.
Cautions
As a source of information on the occupational risk of tuberculosis, outbreak reports have a number of limitations. Most are retrospective or observational. Skin testing procedures are often poorly described, as are data about test skin conversions and cases of tuberculosis. Important information about the facilities and their employees is often missing, inadequately described, or inconsistently measured across outbreak studies. For example, many reports do not include information about variables such as employee age, length of employment, job category, work location within a facility, country of origin, race, and past vaccination with bacille Calmette-Guérin (BCG).
In addition to the limitations of individual reports, no comprehensive, systematic national system exists for the reporting and publishing of information on workplace outbreaks of tuberculosis. Published reports do not represent the universe of outbreaks (even those investigated by CDC staff), and they may appear years after the first investigation of an outbreak. Moreover, published reports on outbreaks probably over represent unusual circumstances (e.g., an unusual location). Indeed, as the very
label suggests, outbreaks represent atypical rather than normal circumstances, at least in relatively low-prevalence regions such as the United States.
Thus, reports of outbreaks do not provide a solid basis for estimating the occupational risk of latent tuberculosis infection or active disease. Nonetheless, careful analyses of outbreaks can provide suggestive information about the potential risk of infection or disease among different types of workers. Particularly useful are studies that have compared workers with and without potential risk factors such as contact with patients at increased risk of tuberculosis (e.g., those on medical wards, HIV/AIDS units), work involving aerosol-generating procedures, and various demographic characteristics (e.g., income, race, place of birth, and place of residence). Although statistical analyses may find similar levels of risk in workplaces and workers’ community of residence, workplace investigations, including DNA analyses, make clear that workers do face a real risk of acquiring tuberculosis from patients, inmates, or others who they encounter on the job.
Review Articles
Garrett and colleagues searched the literature for published reports of tuberculosis outbreaks in health care settings (Garrett et al., 1999). They located reports on 28 outbreaks occurring between 1960 and 1996, mostly in hospitals. The more recent outbreaks (late 1980s and 1990s) differed from earlier outbreaks in that they more often involved serious cases of multidrug-resistant disease, affected relatively large numbers of patients and workers, and spread rapidly enough to be picked up by hospital and public health surveillance systems. A high percentage of the cases involved patients or workers who were seriously immunocompromised due to HIV infection or AIDS and who were thus at high risk of progressing quickly from tuberculosis infection to active disease. This made it easier for clinicians and others to recognize possible links to earlier hospital stays. In these more recent outbreaks, at least 20 health care workers developed multidrug-resistant tuberculosis, and 9 of them died. Skin test information for workers was often incomplete but pointed to additional workers who had become infected with M. tuberculosis without developing active disease. Garrett and colleagues described the epidemiological evidence for transmission of tuberculosis in the health care setting as “compelling” (Garrett et al., 1999, p. 489).
A review by Dooley and Tapper (1997) of 21 outbreaks in adult inpatient settings (many also reviewed by Garrett and colleagues [1999]) reported that a single source of transmission was identified for 10 settings, whereas the others involved multiple sources. Some sources were discovered as a result of formal investigations, whereas others were discovered
incidentally. The source cases often had HIV infection or AIDS and had atypical radiographs and negative sputum smears that made it easier for them to go undetected and untreated. A majority of the health care workers who developed active multidrug-resistant tuberculosis had HIV infection or AIDS, as did most of those who died. The estimated duration and consequences of reported exposures varied widely. In one outbreak involving an autopsy on a person with unsuspected tuberculosis, all five of those present for the 3-hour procedure—including one person present for only 10 minutes—subsequently had skin test conversions and two developed active tuberculosis (Templeton et al., 1995). Two developed active tuberculosis. Other reports also indicate that transmission of M. tuberculosis can occur during relatively short periods of exposure (e.g., 2 to 4 hours).
Individual Reports: Hospitals
Some studies of hospital outbreaks of tuberculosis have reported information useful in assessing the likelihood of occupational versus community transmission of tuberculosis. Most of these studies have also attempted to assess the effects of implementing tuberculosis control measures consistent with the 1990 or 1994 CDC guidelines. The discussion below focuses on evidence of workplace transmission of M. tuberculosis. Chapter 6 reviews evidence on the effects of tuberculosis control measures.
After an outbreak of multidrug-resistant tuberculosis at St. Clare’s Hospital and Health Center (New York City) in the early 1990s, researchers compared tuberculin skin test conversion rates for different occupational categories (nurse, physician, laboratory, housekeeping, social service, and finance) (Louther et al., 1997). They found the highest rate of skin test conversions among housekeeping employees. A multivariate analysis showed that significant differences in conversion rates by job category remained after adjustment for differences in age, BCG vaccination status, country of birth, gender, and the tuberculosis incidence in the zip code area of residence. In the multivariate analysis, residence was not associated with risk of conversion. As discussed in Chapter 6 and Appendix D, that study also reported decreases in conversion rates following the implementation of tuberculosis control measures.
Following an outbreak at the Cabrini Medical Center (New York City), researchers compared rates of skin test conversion for workers on wards admitting patients with tuberculosis with rates for workers on wards that did not admit such patients (Maloney et al., 1995). For the 18-month period before tuberculosis control measures were implemented, conversion rates were 16.7 percent for the former group and 2.8 percent for the latter group, a statistically significant difference. Following the introduction of infection control measures from June through October 1991, rates fell on wards that admitted patients with tuberculosis but not on other wards.
For the 13-month period from June 1991 through August 1992, the difference in conversion rates for the more exposed and the less exposed groups of workers had narrowed to a nonsignificant 5.1 versus 4.0 percent respectively. The researchers did not find that conversion rates correlated with zip code of residence, race, or other demographic characteristics. Again, the investigators documented lapses in infection control measures.
At Grady Memorial Hospital in Atlanta, hospital staff tracked skin test conversion rates after an outbreak of tuberculosis and the implementation of infection control measures (Blumberg et al., 1995; Sotir et al., 1997).7 In the first period studied, January through June 1992, 3.3 percent (annual rate, 6.49 percent) of workers with previous negative skin tests converted. For January through June 1994, the conversion rate had dropped to 0.4 percent (annual rate, 0.89 percent).
A later report focused on house staff, who served in hospitals affiliated with Emory University and typically spent about half their training at Grady Memorial Hospital (Blumberg et al., 1998). Over the study period, skin test conversion rates dropped from approximately 6.0 per 100 person-years to 1.1 after implementation of expanded tuberculosis control measures. Over the entire period studied, house officers in the medicine and obstetrics/gynecology departments had significantly higher skin test conversion rates than house officers in other departments, but the rates for the groups were not significantly different by the end of the study period. Graduates of foreign medical schools had much higher conversion rates than graduates of U.S. medical schools. Throughout the study period the house staff continued to care for large numbers of patients with active tuberculosis.
Some workplace investigations have used DNA fingerprinting in an effort to assess the likelihood of a workplace rather than community source of transmission. Some have concluded that transmission of M. tuberculosis to health care workers resulted from workplace sources.
Individual Reports: Prisons and Jails
Of the outbreak reports that the committee found on organizations other than hospitals, most involve correctional facilities. The reports, however, often focus on inmates rather than correctional facility workers.
Prisons Three studies have reported on outbreaks in California prisons that involved the transmission of M. tuberculosis from inmates to correctional facility personnel. For one 1990–1991 outbreak, the skin test
results for 2 of 11 previously skin test-negative physicians and nurses in a prison infirmary converted to positive during the period November 1990 through March 1991 after exposure to a prisoner with active multidrugresistant tuberculosis (annual rate of infection, 6.4 percent) (Campbell et al., 1993). A report on two other outbreaks in 1995 and 1996 cited annual skin test conversion rates for previously negative employees of 2.8 percent for those exposed in one prison and 4.9 percent for those exposed in a second prison (Prendergast et al., 1999). No employees developed active tuberculosis.
A 1991 outbreak of tuberculosis among New York state prison inmates resulted in the transmission of M. tuberculosis to prison workers. The state then instituted a program of mandatory tuberculin skin testing for employees beginning in November 1991 (Steenland et al., 1997). For 1992, investigators concluded that approximately one-third of new tuberculosis infections among workers were due to occupational exposure, with higher rates for workers in prisons that reported cases of active disease among inmates. They suggested that 1992 was probably the peak year for transmission because the incidence of tuberculosis among prisoners dropped by about 40 percent during the next 3 years.
A report on a 1994 outbreak in a Texas prison found a clustering of cases of active tuberculosis including 15 cases in inmates and one case in a prison worker (an instructor in educational program) (Bergmire-Sweat et al., 1996). The report did not include skin test information for workers but found higher conversion rates for inmates in the wing on which the source case resided and for those having classes in the same classroom as the source case.
A recent outbreak in a South Carolina state prison is still being investigated, but investigators have indicated that a medical student exposed to infectious inmates developed active tuberculosis. A brief abstract describes the setting for this outbreak as a segregated dormitory for HIV-infected inmates (Spradling et al., 2000). Twenty-nine inmates in the population investigated developed active tuberculosis, and 26 of these inmates were housed in the same area of the segregated dormitory as the index case.
Prisons differ from hospitals in that they more often draw inmates from distant communities. For example, New York City residents convicted of violating state laws may be incarcerated in upstate prisons, whereas those convicted of violating federal laws may go to an out-of-state prison. Some prison systems actively seek to import prisoners from other states. For example, a private prison in Oklahoma, a state with a low prevalence of tuberculosis, has contracted to house prisoners from Hawaii, a high-prevalence state (Kakesako, 1998). Other inmates from Hawaii have gone to Minnesota and Tennessee prisons.
Although facilities that import prisoners may seek relatively low-risk offenders and screen them for tuberculosis and other medical problems,
protocols and tests for the identification of individuals with infectious tuberculosis are not perfect and may also be imperfectly implemented. Recently, a Pennsylvania prison that contracts to house detainees of the U.S. Immigration and Naturalization Service (INS) received a detainee with infectious, multidrug-resistant tuberculosis following a “paperwork error” (Lang, 2000; Lebo and Scolforo, 2000). News stories have cited county officials as planning to improve the “sieve-like” system of transferring medical records. As noted in Chapter 1, INS was recently cited by OSHA for failing to protect workers from known hazardous conditions that put workers at risk of exposure to tuberculosis (OSHA Region 6, 2000).
Jails A study of tuberculosis cases associated with a Nassau County (New York) jail found that 24 percent of the cases in the county were associated with the jail (Pelletier et al., 1993). Most of the cases involved prisoners, but one case involved a correctional officer. DNA analysis of M. tuberculosis isolates suggested that transmission of the disease was occurring within the jail. The jail did not screen detainees or workers for tuberculosis infection or active tuberculosis.
Jones and colleagues (1999) reported on an outbreak in the Memphis city jail that involved 38 inmates and five guards who were diagnosed with active tuberculosis between January 1995 and December 1998. Among the 24 inmates with positive cultures, DNA fingerprinting matched the isolates from 19 inmates to isolates found among 2 or more other inmates. For the two culture-positive guards, isolates from both individuals matched the dominant inmate strain. Among a randomly selected sample of 43 isolates from patients with tuberculosis identified in the community, 6 percent matched the dominant inmate strain and 4 of these came from individuals who had been incarcerated in the jail. Of 686 jailers evaluated in October 1997, 1.2 percent had a skin test conversion following a negative test the previous year.
In addition, the article of Jones and colleagues (1999) cited 14 published reports of outbreaks of tuberculosis in U.S. prisons since 1985 but identified only 2 published reports of outbreaks in U.S. jails, with one report dating back to 1977. It also noted that nearly 10 million individuals were admitted to local jails and that 6 percent of the nation’s jails housed 50 percent of jail inmates.
Individual Reports: Long-Term-Care Settings
Nursing homes, chronic care units of hospitals for veterans, long-term psychiatric facilities, and other similar settings often serve elderly people and others at increased risk of tuberculosis. They also typically offer the opportunity for the sustained close contact that facilitates the transmission of tuberculosis.
Most reports on nursing homes have examined the transmission of M. tuberculosis in nursing home residents. Data from the mid-1980s suggest that the incidence of active tuberculosis may be almost twice as high among elderly nursing home residents as among elderly people living in the community (CDC, 1990b). In 1998, residents (all ages) of nursing homes and long-term-care facilities accounted for 3.5 percent of tuberculosis cases nationwide (CDC, 1999b).
In the early 1980s, two reports of tuberculosis outbreaks in nursing homes pointed to workplace transmission of tuberculosis infection and disease to workers (Stead, 1981; Munger et al., 1983). Another report on a skin testing program for workers on a chronic care ward in a Veterans Administration Medical Center found evidence of “occult” transmission of endemic tuberculosis (Brennen et al., 1988).
Since 1995, New York State has required acute-care hospitals and long-term-care facilities to report clusters of tuberculin skin test conversion and evidence of nosocomial tuberculosis transmission as well as cases of active tuberculosis (Rachel L.Stricof, Bureau of Tuberculosis Control, New York State Department of Health, personal communication, October 3, 2000). The number of reports and the seriousness of the events reported have declined over that period. Between 1995 and 1997, covered facilities reported 15 clusters of possible or confirmed tuberculin skin test conversion among health care workers. One of the 15 clusters involved a hospitalized patient who was considered no longer infectious and was transferred to a long-term-care facility that subsequently failed to maintain appropriate therapy for the person. The other clusters were associated with exposure to unsuspected or unconfirmed index cases. During this same period, eight pseudo-outbreaks were reported involving clusters of skin test conversions linked, for example, to atypical mycobacteria or deficiencies in the tuberculin skin test procedure. Since 1998, the state has undertaken numerous contact investigations but has not documented any further outbreaks involving patients or health care workers in recent years.
Recently, investigators at the Arkansas Department of Health reported on probable transmission of tuberculosis to two health care workers from a resident of a nursing home who died in a hospital with undiagnosed tuberculosis. Investigators later located a radiograph for the individual showing a cavitary lesion (Ijaz et al., 1999). The investigation started when the nursing home’s surveillance program detected skin test conversions in four previously negative employees. The secondary cases of active tuberculosis included an employee in the nursing home where the source patient was a resident, a nurse in the hospital that treated the source patient, and a nursing home resident who moved from the nursing home that housed the source patient to a second jointly operated facility in the community. DNA fingerprinting found the same strain of M. tuberculosis in all three individuals. On-site investigation determined that the source resident was very
mobile and had a persistent, spraying cough. Investigators also found that laboratory tests for possible tuberculosis were ordered but not performed during one of the resident’s several hospital stays (Kevin Ijaz, Arkansas Department of Health, personal communication, August 23, 2000). In addition, investigators determined that an air intake for the air-conditioning system was located outside the resident’s nursing home room.
The committee located one report of a skin test conversion in an employee of a residential substance abuse facility in Michigan following diagnosis of multidrug-resistant tuberculosis in a resident of the facility (Hoch and Wilcox, 1991). The facility had no health screening program for patients and a high attrition rate.
Individual Reports: Other Settings
Homeless Shelters The committee located only one published report on transmission of tuberculosis to workers in a homeless shelter. That report involved a 1987–1988 outbreak in a Syracuse, New York, shelter for men (Curtis et al., 2000). Investigators found that 70 percent of 257 clients and staff had positive tuberculin skin test results. Although skin test conversions were documented in 2 of 8 previously tuberculin skin test negative staff members, 52 other staff members who might have been exposed were not available for skin testing. Shelter workers are often previous shelter clients. They tend to be more transient and less available for follow-up than workers in many of the other settings reviewed in this chapter.
Hospice and Home Care Although the advent of effective treatment for people with HIV infection or AIDS has reduced their need for hospice care, hospice workers still care for many people at higher than average risk of tuberculosis. One outbreak of tuberculosis in a hospital-based hospice has been reported (Pierce et al., 1992). Eleven of 65 workers converted their skin tests after exposure to an AIDS patient with a delayed diagnosis of tuberculosis.
Ambulatory Care Setting The committee located one report of an outbreak in an ambulatory care setting. It occurred in 1988 among workers in a Florida clinic that reported skin test conversions for 17 of 30 (57 percent) workers with previously negative test results (Howell et al., 1989). Investigators identified four possible sources of transmission including 1 nurse with noncavitary pulmonary tuberculosis, 39 clinic patients with pulmonary tuberculosis (14 with at least one positive smear), sputum inductions for 13 culture-positive patients, and aerosolized pentamidine treatments for 2 culture-positive patients. The investigation identified ventilation problems in the facility that could have contributed to transmission.
Funeral Homes Two cases of tuberculosis transmission from cadavers to embalmers have recently been documented (Lauzardo et al., 2000; Sterling et al., 2000a). Before death, one individual had been under treatment for AIDS and active tuberculosis. The employee who embalmed the body was diagnosed with active tuberculosis, and DNA fingerprinting showed that the strain matched that from the cadaver (Sterling et al., 2000a). Investigators suggested aerosolization from the airway during the embalming process as a possible means of transmission. In the other case of transmission related to embalming, DNA fingerprinting again linked the disease in the embalmer to a deceased person under treatment for AIDS and rifampin-resistant tuberculosis (Lauzardo et al., 2000).
COMMITTEE CONCLUSIONS
Context
Are health care, correctional, and selected other categories of workers at greater risk of infection, disease, or mortality due to tuberculosis than others in the community in which they reside? This question has no simple yes-or-no answer. Instead, conclusions must be qualified to reflect the
-
changing epidemiology of tuberculosis,
-
continuing geographic variation in tuberculosis case rates,
-
evolving institutional and public responses to tuberculosis in the community and the workplace, and
-
ongoing risk from people with undiagnosed infectious tuberculosis.
The changing epidemiology of tuberculosis encompasses both the decline in the number of tuberculosis cases and case rates since 1993 and the decline in the proportion of cases accounted for by multidrug-resistant disease, as described in Chapter 1. Overall, fewer cases of tuberculosis and less multidrug-resistant disease means less risk for nurses, doctors, correctional officers, and others who work for organizations that serve people who have tuberculosis or who are at increased risk of the disease.
Despite the general decline in rates of tuberculosis in recent years, marked geographic variation in tuberculosis case rates persists. Today, as in the past, a few states and cities account for a disproportionate share of cases of active tuberculosis. Nonetheless, even within areas with relatively high rates of tuberculosis, risks to health care and other workers are not equal. Some hospitals have policies to transfer rather than treat patients with suspected or confirmed tuberculosis. Many nursing homes, jails, and other facilities will not accept persons known to have active tuberculosis. Although these policies should reduce risk, workers may still be exposed to individuals with undetected disease. In contrast to these “transfer rather than treat” institutions are the so-called safety net hospitals whose workers
care for a high proportion of people who are at increased risk of tuberculosis (e.g., those who are unemployed or homeless, recent immigrants from developing countries, and individuals with HIV infection or AIDS).
Workers’ risk of tuberculosis is also affected by employer and community efforts to prevent the spread of tuberculosis. Investigations of workplace outbreaks of tuberculosis have typically identified lapses in infection control measures as probable contributors to transmission. As discussed in Chapter 6, much of the support for the effectiveness of tuberculosis control measures comes from outbreak investigations and subsequent studies of the implementation of administrative controls and other measures. In workplaces that have many workers in direct contact with infectious individuals, employers’ policies and procedures affect the likelihood that employees will acquire tuberculosis infection or disease on the job.
Although Chapter 6 points to the importance of careful and alert application of protocols for identifying those likely to have infectious tuberculosis, application of such protocols does not guarantee that all cases will be promptly identified. Unsuspected and undiagnosed tuberculosis is the primary threat to workers.
The committee’s conclusions about the workplace risk of tuberculosis must be understood against this backdrop. If the conclusions highlighted below are taken out of context, the occupational risk of tuberculosis may be misunderstood. Although the committee judged that the following conclusions were reasonably supported by the available literature, it notes that most of the studies that it consulted involved hospitals and were inconsistent in methods, reporting, and results.
Conclusions
Through at least the 1950s, health care workers were at higher risk from tuberculosis than others in the community. Before the development of effective treatments for the disease, several studies documented very high rates of infection for nurses and physicians. The available data do not allow conclusions about the historical risk to other categories of workers covered by the 1997 proposed OSHA rule.
Despite the availability of effective treatments, the last decade and a half has shown that tuberculosis remains a threat to health care and other workers, especially when workplaces neglect basic infection control measures and when multidrug-resistant disease is present. The primary risk today comes from patients, inmates, and others with unsuspected and undiagnosed infectious tuberculosis. Even with good tuberculosis control measures, some workers will still be exposed to people with unsuspected infectious disease, particularly in communities where the disease is common.
Available data suggest that where tuberculosis is uncommon or where basic infection control measures are in place, the occupational risk to health care work-
ers of tuberculosis infection now approaches the level in their community of residence. Tuberculosis risk in communities has been declining since 1993. Overall, rates of active tuberculosis among health care workers are similar overall to those reported for other employed workers. Comparable data are not available to compare mortality risk. Whatever the origins of their disease, health care workers and others with compromised immune systems are at high risk of death if they contract multidrug-resistant tuberculosis. The limited information available to the committee and the changing epidemiology of tuberculosis did not allow the committee to make quantitative estimates or comparisons.
The potential for exposure to tuberculosis in health care and other facilities varies within and across communities. In general, where the disease is more common, health care and others workers are at higher risk of coming into contact with people who have infectious tuberculosis. The U.S. population is, however, mobile, and visitors and new residents can bring tuberculosis with them into communities where the disease is rare. Should a hospital or other worker encounter such an unexpected person, she or he may be at higher risk than colleagues in high-prevalence inner cities, who are more likely to be familiar with and alert to the signs and symptoms of tuberculosis.
The occupational risk of exposure to tuberculosis varies with job category and work environment. Only some health care, correctional, and other workers are reasonably anticipated to have contact with people with tuberculosis, even in facilities that treat or admit such individuals. For example, many administrative and other personnel in hospitals have little contact with patients of any sort and little chance of exposure to contaminated air. For those with direct patient contact, the risk of tuberculosis infection and disease is also not uniform. Although data are not completely consistent, the risk tends to be higher for those who work on wards where patients with suspected or confirmed tuberculosis are admitted and for those whose jobs involve aerosol-generating procedures such as bronchoscopies. For these workers, in particular, the effectiveness of workplace tuberculosis control measures matters.
Workers at particular risk from occupationally acquired tuberculosis infection include those with HIV infection or AIDS or other conditions associated with suppression of normal functioning of the immune system. Data about cases of tuberculosis among health care and other workers are limited, but those with HIV infection or AIDS (or other conditions affecting the immune system) are disproportionately represented in reports of tuberculosis cases and deaths during hospital and prison outbreaks of multidrug-resistant disease. CDC guidelines recommend that health care workers with HIV infection be counseled about the risk of contact with patients who have tuberculosis and be offered assignments that minimize such contact (CDC, 1994b).
Many health care, correctional facility, and other workers are at increased risk of tuberculosis for reasons unrelated to their work. Most people spend more time in the community than at work. In general, low-income individuals, members of racial and ethnic minorities, immigrants from developing countries, and people living in low-income neighborhoods are at higher risk of community-acquired tuberculosis infection and active tuberculosis. This does not mean that the risk of workplace transmission of tuberculosis can be disregarded for workers with these demographic risk factors. It does mean, however, that workplace surveillance programs need to consider the likelihood of community exposure in assessing the results of tuberculin skin tests.
SUMMARY
Historically, health care workers were at higher risk from tuberculosis than others in the community. Since then, effective treatment has drastically cut tuberculosis case rates and consequently reduced health care workers’ occupational risk of tuberculosis. Lower community case rates also mean that prison, jail, homeless shelter, and other workers are less likely to be exposed to tuberculosis than in the past.
Still, tuberculosis remains a threat, particularly when the disease is unsuspected and undiagnosed and when infection control measures are neglected. Other risk factors for health care, correctional, and other workers include work that involves direct contact with people who have infectious tuberculosis and work in communities with high prevalence of the disease.



























