Page 40
2
Defining the Contents of the Data Set: The National Health Care Quality Framework
This chapter lays out the framework for the National Health Care Quality Report (also referred to as the Quality Report). The framework largely determines the contents of the National Health Care Quality Data Set and categories of measures. The framework proposed by the committee includes two major dimensions: (1) an assessment of the components of health care quality—safety, effectiveness, “patient centeredness,” and timeliness—and (2) an assessment of how well the system responds to consumer perspectives on health care needs— staying healthy, getting better, living with illness or disability, and coping with the end of life. Some measures can be organized by specific condition (for example, diabetes), particularly for effectiveness. Equity can be assessed by analyzing quality of care across different groups of people.
RECOMMENDATION
RECOMMENDATION 1: The conceptual framework for the National Health Care Quality Report should address two dimensions: components of health care quality and consumer perspectives on health care needs. Components of health care quality—the first dimension—include safety, effectiveness, patient centeredness, and timeliness. Consumer perspectives on health care needs—the second dimension—reflect changing needs for care over the life cycle associated with staying healthy, getting better, living with illness or disability, and coping with the end of life. Quality can be examined
Page 41
along both dimensions for health care in general or for specific conditions. The conceptual framework should also provide for the analysis of equity as an issue that cuts across both dimensions and is reflected in differences in the quality of care received by different groups of the population.
The four system components of health care quality are defined as follows:
1. Safety refers to “avoiding injuries or harm to patients from care that is intended to help them” (Institute of Medicine, 2001).
2. Effectiveness refers to “providing services based on scientific knowledge to all who could benefit, and refraining from providing services to those not likely to benefit (avoiding overuse and underuse)” (Institute of Medicine, 2001). Overuse occurs when “a health care service is provided under circumstances in which its potential for harm exceeds its potential benefit.” Underuse “is the failure to provide a health care service when it would have produced a favorable outcome for a patient” (Chassin and Galvin, 1998:1002).
3. Patient centeredness refers to health care that establishes a partnership among practitioners, patients, and their families (when appropriate) to ensure that decisions respect patients' wants, needs, and preferences and that patients have the education and support they need to make decisions and participate in their own care.
4. Timeliness refers to obtaining needed care and minimizing unnecessary delays in getting that care.
The relative importance of the four components of health care quality may vary over time and for different providers and policy makers. These quality components apply across all health care settings—from institutionalized to inpatient and ambulatory care; from clinicians' offices to home health care and hospice care.
Consumers have several perspectives on health care. They want a system that will respond to their needs or reasons for seeking care, ranging from staying healthy to coping with the end of life. These needs vary over the life span and across groups of the population. Consumers would like to know about the overall quality of care, but they are particularly interested in care for specific conditions or situations that affect them or their families.
Equity in health care quality is considered an important cross-cutting issue. The framework allows for its consideration by comparing the quality of care for different groups of the population, across geographic areas and by condition, as appropriate.
Efficiency is not included in the committee's framework. Some aspects of efficiency are reflected in other components of quality. For example, errors in health care that result in additional procedures, hospitalizations, or other treat-
Page 42
ments are a form of waste or inefficiency. The provision of unnecessary services (that is, overuse or ineffectiveness) is another form of waste. Fragmentation of care and unnecessary waits and delays in service (that is, lack of timeliness) consume the patient's and the clinician's time and other resources that could be put to better use. One basic aspect of efficiency that is not reflected in the framework is the cost per unit of service (for example, cost per laboratory test), but this was viewed as falling outside the purview of a national report focusing on the quality of health care services.
IMPORTANCE OF THE FRAMEWORK
A framework serves several important purposes. The framework is a tool for organizing the way one thinks about health care quality. It provides a foundation for quality measurement, data collection, and subsequent reporting. A framework is a way of making explicit the aspects of health care that should be measured (Miles and Huberman, 1994) in order to assess quality and define policy accordingly. Given that quality is a multifaceted subject, the framework provides a way to organize the various elements of the National Health Care Quality Data Set and potential report contents.
A framework defines durable dimensions and categories of measurement that will outlast any specific measures used at particular times. In essence, it lays down an enduring way of specifying what should be measured while allowing for variation in how it is measured over time. For example, communication between clinicians and patients is an aspect of care that will always have to be measured. However, the ways that patients connect with their clinicians—ranging from office visits to electronic exchanges—will vary over time, and so will the corresponding measures (Balas et al., 1997). When a common framework is established internationally, it also allows for comparisons in the quality of care across countries. Although it will provide continuity for the Quality Report and the measures, the framework should be considered dynamic. In the long term, it may have to be adjusted in response to changes in the conceptualization of quality and/or significant changes in the nature of the U.S. health care system.
NATIONAL HEALTH CARE QUALITY FRAMEWORK
Overview
In order to develop a National Health Care Quality Framework, the committee examined many of the approaches available to analyze quality of care (see Appendix D). The framework proposed herein is based partially on elements from these other approaches. Its foundation ultimately derives from the purpose of the health care system, for which the committee endorses the following statement: “to continuously reduce the burden of illness, injury, and dis-
Page 43
ability, and to improve the health and functioning of the people of the United States” (Advisory Commission on Consumer Protection and Quality in the Health Care Industry, 1998:2).
To assess whether the health care delivery system is making progress in achieving this purpose, the committee developed a framework with two major dimensions. The first dimension consists of the components of health care quality. Building on the work of the Institute of Medicine (IOM) Committee on the Quality of Health Care in America (Institute of Medicine, 2001), these components of quality are defined as safety, effectiveness, patient centeredness, and timeliness. The second dimension addresses the consumer perspective on health care needs, which reflects the life cycle of people's involvement with the health care system or their reasons for seeking care at any particular time. Building on the work of the Foundation for Accountability (FACCT), consumer perspectives on health care needs are defined as staying healthy, getting better, living with illness or disability, and coping with the end of life (Foundation for Accountability, 1997).
As the committee refined the framework, it kept in mind the audiences for this report. The framework can be used to encourage measurement and reporting in specific areas to inform national and state policy makers, purchasers, providers, and other specialized audiences. It can also be used to encourage measurement and reporting in areas that consumers and the media will find meaningful and important, including condition-specific care. Equity can be assessed by analyzing the quality of care received by different groups of the population. Defined in this manner, the framework can be used to guide policy and to inform relevant audiences.
Components of Health Care Quality
For each of the four components of quality—safety, effectiveness, patient centeredness, and timeliness—the committee defined a set of subcategories ( Table 2.1) and specific examples of potential measures for the National Health Care Quality Report ( Box 2.1, Box 2.2, Box 2.3 to Box 2.4).1 The components of quality can be thought of as subsets of quality of care, but they are not completely independent of each other. There is some overlap at the boundaries.
1 These measures are offered as examples and are in no way intended to represent the ideal measures or a comprehensive measure set. They are based on a limited review and evaluation of existing measures, leaving gaps with reference to the proposed framework. They do provide an appreciation of the type and range of measures that will be required for the Quality Report.
Page 44
|
Safety |
Effectiveness |
Patient Centeredness |
Timeliness |
|
1. Diagnosis |
1. Preventive care |
1. Experience of care |
1. Access to the system of care |
|
2. Treatment a. Medication b. Follow-up |
2. Acute, chronic, and end-of-life care |
2. Effective partnership |
2. Timeliness in getting to care for a particular problem |
|
3. Health care environment |
3. Appropriateness of procedures |
3. Timeliness within and across episodes of care |
|
Safety refers to “avoiding injuries to patients from care that is intended to help them” (Institute of Medicine, 2001). |
Safety
In operational terms, improving safety means designing and implementing health care processes to avoid, prevent, and ameliorate adverse outcomes or injuries that stem from the processes of health care itself (National Patient Safety Foundation, 2000). Safety is best understood in terms of injuries that occur to patients and the errors or latent failures that lead to these injuries or harm. Although both perspectives are essential in building a safer health care system, the overriding priority in the short term is the reduction of injuries or harm to patients. Assessing errors that lead to patient injuries or harm is one method for organizing a framework of measures that will define the safety of the health care system.
An error of execution is the failure of a planned action to be completed as intended, while an error of planning is the use of a wrong plan to achieve an aim (Reason, 1990). Errors have also been classified into errors of commission (doing unnecessary things or doing them wrongly) and errors of omission (failing to do necessary things) (Iezzoni, 1997; Leape et al., 1991). As a component of quality health care, safety problems or patient injuries have been found to occur along the continuum of clinical care functions and in the general environment of care (see examples of safety measures in Box 2.1). Errors in diagnosis, including misdiagnosis (wrong diagnosis) and missed diagnosis (failure to diagnose), are relatively
Page 45
BOX 2.1 Examples of Areas in Which Measures of Safety May Be Applied and Selected Measures
Diagnosis
Treatment
Medication
Follow-Up
|
Page 46
|
Safety of the Environment
|
common (Leape et al., 1991). Their prevalence is estimated at 10 percent among hospital populations based on autopsy studies (Bordage, 1999) and even higher for patients in intensive care units (Mort and Teston, 1999). Treatment errors are problems related to planning, technical proficiency, or prescription practices. Lack of technical proficiency or competence in procedures such as colonoscopy (Miller, 1997) can lead to complications or nosocomial infections.
Medication-related adverse events are a subset of treatment errors that has been studied extensively (Institute of Medicine, 2000). It has been estimated that medication-related adverse drug events occur In nearly 10 percent of all hospital admissions (Leape et al., 1995). Errors can also occur in follow-up care (Christakis and Lamont, 2000). Finally, the safety of the overall health care environment (Gershon et al., 2000) is essential to avoid gross errors such as wrong-site surgery, patient suicide, homicide, and other sentinel events (Joint Commission on Accreditation of Healthcare Organizations, 2000a).
The site of care is one of several characteristics that can be used to further subclassify safety problems. This is an increasingly important aspect to document, given that much of health care, including surgery, is gradually moving away from the hospital to the ambulatory sector (Phillips et al., 1998; Quattrone, 2000). In order to ultimately improve patient safety in health care (as has occurred in high-reliability industries such as aerospace and nuclear power) safety has to be designed or built into the care system at all levels. The Quality Inter-agency Coordination Task Force (QuIC) has issued a report to the President defining needed actions to improve patient safety, which begins to address many of these issues (Quality Interagency Coordination Task Force, 2000). The Quality Report should include measures to assess the effects of some of these actions as they are implemented.
Page 47
|
Effectiveness refers to “providing services based on scientific knowledge to all who could benefit, and refraining from providing services to those not likely to benefit (avoiding overuse and underuse)” (Institute of Medicine, 2001). |
Effectiveness
Overuse occurs when “a health care service is provided under circumstances in which its potential for harm exceeds its potential benefit”. Underuse “is the failure to provide a health care service when it would have produced a favorable outcome for a patient” (Chassin and Galvin, 1998:1002). Effectiveness is probably the component of health care quality most readily identified because ultimately it represents the “bottom line,” that is, whether care leads to improved outcomes in terms of health status and quality of life for patients (Greenfield et al., 1994). People assume that care will be safe, but they want it to be effective as well. A growing body of evidence has documented problems of effectiveness with respect to the overuse of services that cannot help and may harm the patient, as well as problems arising from the underuse of care where benefit is likely to exceed harm (Chassin and Galvin, 1998). A number of studies have also documented the inappropriateness of specific procedures (McGlynn and Brook, 1996). These problems of effectiveness occur in all types of care and across sites.
Effectiveness should be distinguished from efficacy. The latter refers to the benefits achievable from a therapy or intervention under ideal conditions (such as a randomized controlled trial) while the former refers to the results of care in everyday clinical practice settings (Brook and Lohr, 1985). In evaluating the quality of the health care delivery system under actual operating conditions, it is effectiveness rather than efficacy that should be assessed. Effectiveness can be assessed according to the type of care (for example, preventive care, acute, chronic, and end-of-life care) or for specific conditions. The appropriateness of selected procedures is another subcategory of effectiveness (see examples of effectiveness measures in Box 2.2 and Appendix B).
The effectiveness of preventive care can be assessed comprehensively by examining the full spectrum of needs for a defined population or age group such as children or the elderly (see Appendix B). In this case, the services actually received by a specific group as reflected in medical records or a similar data source are compared to the services they should receive according to prevailing guidelines (U.S. Preventive Services Task Force, 1996). The effectiveness of preventive care can also be assessed selectively by examining screening and interventions for specific conditions or problems such as childhood immunizations (Centers for Disease Control and Prevention, 1999), prenatal care (Expert Panel on Prenatal Care, 1989; Genest, 1981; Grad and Hill, 1992), or cervical cancer screening (National Institutes of Health, 1996).
Page 48
BOX 2.2 Examples of Areas in Which Measures of Effectiveness May Be Applied and Selected Measures
Preventive Care
Active, Chronic, and End-of-Life Care Asthma
Heart Disease
Cancer (breast, prostate, colon) Breast Cancer
Prostate Cancer
Colon Cancer
HIV/AIDS
|
Page 49
|
Diabetes Diabetes Quality Improvement (DQuIP) measure set including
Depression
Hypertension
General
Appropriateness of Procedures
|
Page 50
Effectiveness can also be assessed by examining care for particular chronic or acute conditions as well as end-of-life care. For example, effective care for diabetes includes the reduction of potential complications through preventive retinal eye exams, monitoring of hemoglobin A1c, and regular lipid profiles (American Diabetes Association, 1998; Health Care Financing Administration, 2000; National Committee for Quality Assurance, 2000). Care for selected types of cancer and terminal conditions includes appropriate pain management near the end of life (American Pain Society, 1995; Cherny and Catane, 1995; Wagner et al., 1996).
Much of the work on measures of quality of care has concentrated on effectiveness, usually based on practice guidelines for specific conditions (Medscape, 2000). Practice guidelines and well-tested quality measures are available for a variety of conditions including diabetes, acute myocardial infarction, heart failure, asthma, breast cancer, pneumonia, and stroke (Health Care Financing Administration, 2000; Jans et al., 2000; National Committee for Quality Assurance, 2000; Rolnick et al., 2000; Shiffman et al., 2000; Soumerai et al., 1998). However, well-defined measure sets that include both process and outcome measures and cover the entire spectrum of care are available for only a few conditions such as diabetes (American Diabetes Association, 1998; Health Care Financing Administration, 2000; Loeb, 2000; Tuckson, 2000).
In addition, effectiveness is reflected in the appropriateness with which selected surgical and diagnostic procedures are performed. One of the largest studies of overuse ever conducted found that 17 percent of coronary angiographies, 32 percent of carotid endarterectomies, and 17 percent of upper gastrointestinal tract endoscopies performed on Medicare beneficiaries were for inappropriate indications (Chassin et al., 1987). Overall, it is estimated that about one-third of the procedures performed in the United States are of questionable health benefit relative to their risks (McGlynn and Brook, 1996).
Patient Centeredness2
Patient centeredness is a characteristic of the relationship between clinician and patient (Charles et al., 1999a; Roter, 2000) and can be contrasted to disease-
Patient centeredness refers to health care that establishes a partnership among practitioners, patients, and their families (when appropriate) to ensure that decisions respect patients' wants, needs, and preferences and that patients have the education and support they need to make decisions and participate in their own care.
2 This topic is treated in depth in a paper commissioned by the committee from Christina Bethell on measures of patient centeredness for the National Health Care Quality Report (2000).
Page 51
centered (Stewart et al., 1999b) and clinician-centered care (Byrne and Long, 1976). Patients of different races, cultures, genders, and ages have different preferences and beliefs that providers must take into account in order to achieve patient-centered care (Cooper-Patrick et al., 1997, 1999; Gostin, 1999; Ngo-Metzger et al., 2000; Stewart et al., 1999a). Patients vary in the degree of autonomy and involvement they want in health care decision making. Some prefer active self-management, while others prefer to rely completely on the clinician's recommendations (Arora and McHorney, 2000; Beisecker and Beisecker, 1990; Benbassat et al., 1998; Blackhall et al., 1995; Deber et al., 1996; Degner and Russell, 1988; Guadagnoli and Ward, 1998; Mazur et al., 1999; Wagner et al., 1995).
As shown in Table 2.1, the committee has defined two subcategories of patient centeredness that should be assessed in the National Health Care Quality Framework. They are the patient's experience of care and the presence of an effective partnership (for examples of measures of patient centeredness, see Box 2.3). The patient's experience of care refers to the caring (Scott et al., 1995), communication (Ong et al., 1995; Roter et al., 1997), and understanding that should characterize the clinician–patient relationship. The emphasis here is on the patient's report of her or his experience with specific aspects of care and goes beyond her or his general satisfaction or opinion regarding the adequacy of care.
An effective partnership should be the result of a clinical encounter shaped around the patient's needs and the context in which he or she lives (for example, his or her family relationships, job situation, and home life). It should increase understanding by both the clinician and the patient to enable the patient to act on the information provided (Bopp, 2000; Braddock et al., 1999; Maly et al., 1999; Mazur et al., 1999; Parrott, 1994). Creating effective partnerships means encouraging the kind of shared decision making and patient skills and knowledge needed for self-management of health conditions (Charles et al., 1999b). The degree of shared decision making is partly dependent on the clinician's participatory decision-making style (Brock, 1991; Emanuel and Emanuel, 1992; Kaplan et al., 1995; Kaplan et al., 1996; Szasz, 1956), the degree of trust established (Safran et al., 1998), the patient's desire to have a role in decisions (Mechanic and Meyer, 2000; Mechanic, 1998; Meehan et al., 1997; Pearson and Racke, 2000), and patient–clinician characteristics such as race (Cooper-Patrick et al., 1999), as has already been discussed.
An effective partnership also involves the opportunity for patient self-management or patient involvement in care for specific conditions (generally chronic problems), including self-monitoring and shared goal setting, so that a true partnership between the clinician and the patient and his or her family can be established (Center for the Advancement of Health and Milbank Memorial Fund, 1999). Through an effective partnership with their clinician, patients and their families obtain the skills and knowledge necessary for self-management and a sense of efficacy for managing their own conditions (Anderson et al.,
Page 52
1995). Patient self-management, particularly for chronic diseases, has been found to be associated with improved health status (Lorig et al., 1999).
Finally, an effective partnership is facilitated by culturally competent health care. For example, patient centeredness can be furthered when patients receive information in their own language, when the clinicians have greater awareness of potential communication difficulties, and most importantly, when care is provided taking into account the context of the patient's cultural beliefs and practices (Chin, 2000; Langer, 1999; Rivadeneyra et al., 2000; Robins et al., 2001).
Patient centeredness, like other components of health care quality, can be measured. Research suggests that the trust established through the patient–provider relationship, the information exchanged between patient and provider, and the problem solving that occurs in the context of the patient-centered model of
Patient's Experience of Care Time spent with provider Patient's perception of the clinician's skills Patient's perception of being treated with respect and dignity Patient's perception of being listened to or having attention given to what he or she says Patient's perception of how much he or she was helped by the care he or she received Patient's ability to understand the clinician's explanations Effective Provider–Patient Partnership Patient involvement in care in general Patient involvement in care for specific conditions (e.g., asthma, cancer, diabetes, depression) Patient offered choice of treatment Clinician's participatory decision-making style Frequency of self-monitoring by patient Patient involvement in decisionmaking Degree of patient self-management efficacy (patient's confidence in his/her ability to manage a specific condition) Cultural competence (e.g., clinician's sensitivity to cultural differences, patient reports that information was provided in his or her own language)
BOX 2.3 Examples of Areas in Which Measures of Patient Centeredness May Be Applied and Selected Measures
Page 53
care are the chief mechanisms that link patient-centered care to improved outcomes (Brody, 1989; DiMatteo et al., 1994; Prochaska, 1996; Seeman and Seeman, 1983; Von Korff et al., 1997).
|
Timeliness refers to obtaining needed care and minimizing unnecessary delays in getting that care. |
Timeliness
Timeliness combines being able to obtain care and getting it promptly. It includes both access to care (people can get care when needed) (Aday and Anderson, 1975) and coordination of care (once under care, the system facilitates moving people across providers and through the stages of care) (Shortell, 1976).
As shown in Table 2.1, the committee has operationalized the concept of timeliness into three subcategories relative to the time elapsed until care is obtained. Timeliness requires access to the system of care, timeliness in getting to care for a particular problem, and timeliness within and across episodes of care (for examples of timeliness measures, see Box 2.4). Access to care is viewed as an aspect of timeliness and, ultimately, an antecedent to securing high-quality health care (Lave et al., 1979). It can be assessed from the patient's perspective or against absolute standards based on the clinical effects of delays in care.
Timeliness, as applied to general access to the health care system, is defined by the ability to obtain primary (Lambrew et al., 1996; Starfield, 1992; Starfield et al., 1998) and specialty care (Grumbach et al., 1999; Kassirer, 1994) when needed. Timeliness may also require access to special services, such as being able to obtain physical therapy for a disability or chronic condition and being able to obtain home health care when needed (Cheh and Phillips, 1993; Thomas and Payne, 1998). For example, access to home health care can affect the quality of end-of-life care since it influences the place of death and access to palliative home care (Grande et al., 1998).
The second subcategory of timeliness includes measures of whether people are actually able to obtain care for a specific problem once they have entered the system and how long it takes them to do so. It includes aspects such as delays and difficulties in getting a checkup, obtaining routine care, or obtaining urgent care (Bindman et al., 1991; Derlet and Hamilton, 1996). Delays in obtaining care can directly affect the effectiveness of care and health outcomes. In some cases, delays in care can endanger the life of the patient—for example, delays in receiving antibiotics for pneumonia (Centers for Disease Control and Prevention, 1995; Health Care Financing Administration, 2000; Meehan et al., 1997) or delays in reperfusion therapy after a heart attack (Brodie et al., 1998; Health
Page 54
BOX 2.4 Examples of Areas in Which Measures of Timeliness May Be Applied and Selected Measures
Access to Care
Timeliness in Getting Care Once Having Accessed the System
Timeliness for an Episode of Care
|
Care Financing Administration, 2000; Marciniak et al., 1998; Ryan et al., 1999). Timeliness in getting to care can also be measured by the absence of administrative-based delays in care for specific conditions (for example, time from diagnosis to treatment for breast cancer).
The third subcategory of timeliness refers to timeliness within an episode of care and across multiple episodes of care for a single condition. It is characterized by smooth and continuous flow through the stages of care (Murray, 1998; Nolan et al, 1996) and by coordination across services and providers for a spe-
Page 55
cific problem or for diverse problems (Starfield, 1998) It includes timeliness in starting care once a patient is at the provider site (for example, time in the waiting room); timeliness in moving through care for a specific problem (for example, time between evaluation, diagnosis, and treatment; between parts of the treatment; between different services at one visit or across separate visits) (Caplan and Helzlsouer, 1992; Mechanic et al., 2001; Meehan et al., 1997); and coordination of care across providers, for example, for children with special needs (Appleton et al., 1997).3
Consumer Perspectives on Health Care Needs
Systems of care and clinicians should provide high-quality health care for the different types of care sought by consumers. At one time or another, consumers may need such care to stay healthy, get better (or recover from a specific illness), live with an illness or disability, or cope with the end of life ( Figure 2.1). Together, these consumer perspectives on health care needs represent the most important reasons why people seek care. They also reflect the life cycle of their involvement with the health care system.
~ enlarge ~
FIGURE 2.1 Consumer perspectives on health care needs
3 As mentioned earlier, the components of quality may overlap Although coordination of care around the ensemble of needs for care of a particular person can also be regarded as an aspect of patient centeredness, the committee opted for including it in the framework as a subcategory of timeliness to emphasize the work flow aspects of coordination, that fit better with other system-related aspects affecting timeliness of care. Lack of coordination can also affect safety when there are problems with the flow of information.
Page 56
The relative importance of each of these health care needs changes over the life span of each individual from conception to death. For instance, “staying healthy” characterizes most of children's needs for care since they are generally healthy. At the other end of the spectrum, as an individual reaches an advanced age, the likelihood of dying increases and “coping with the end of life” becomes more of a concern. Furthermore, an individual may experience several health care needs simultaneously. For example, an elderly woman may seek care to get advice on managing her diabetes (“living with illness”) and at the same time seek care to get a flu shot (“staying healthy”).
The four categories of consumer perspectives on health care needs were adapted from FACCT's Consumer Information Framework (Foundation for Accountability, 1997) and correspond roughly to the clinical designations for different types of care.
|
Staying healthy refers to getting help to avoid illness and remain well. |
To stay healthy, consumers need care that recognizes the importance of preventing conditions they may be at special risk of developing. To avoid illness, the health care system should encourage the development of healthy behaviors, facilitate early detection of illness, and educate consumers about how they can reduce health risks. From the point of view of clinicians, this category includes measures of preventive care.
|
Getting better refers to getting help to recover from an illness or injury. |
If people develop an illness or injury, they need proper medical attention and follow-up care. In these situations, people seek care to help them recover and reestablish their daily activities as soon as possible. From the point of view of clinicians, this category includes measures of acute care.
Page 57
|
Living with illness or disability refers to getting help with managing an ongoing, chronic condition or dealing with a disability that affects function. |
If people develop an illness or disability that they must live with, they seek care to receive treatment based on the best evidence available. They also seek a health practitioner who will work with them to help them remain as healthy and active as possible. They want someone who will show them what they can do to take care of themselves, how to recognize warning signs, and how to avoid any related problems. From the point of view of clinicians, this category includes measures of chronic care and care for people with disabilities.
|
Coping with the end of life refers to getting help to deal with a terminal illness. |
People and their families also seek care when needs change dramatically because of a terminal illness. A person facing death needs access to a wide range of services. She or he also needs a practitioner who will recommend and coordinate these services, including palliative treatment and caregiver support. From the point of view of clinicians, this category of care includes terminal and end-of-life care.
The committee chose to use modifications of the FACCT terminology rather than the more traditional, clinically focused terminology for three reasons. First, the FACCT terms have been shown to make more sense to consumers and policy makers (Foundation for Accountability, 1997). Second, they are worded in terms of the point of view of the consumer or patient rather than the clinician. Third, unlike clinical terminology, they are not directly linked to particular sites of care, encouraging a broader range of measures.
Consumer Perspectives on Health Care Needs as Reflected in Care for Specific Health Conditions
In addition to examining the quality of health care overall, presenting consumer perspectives on health care needs according to specific conditions will increase the usefulness of the National Health Care Quality Report and its policy relevance. In particular, it will increase understanding of the quality of care for
Page 58
BOX 2.5 Sample Measures of Quality of Breast Cancer Care by Consumer Health Care Needs
Staying Healthy
Getting Better
Living with Illness or Disability
Coping with the End of Life
|
particular health problems on the part of consumers and policy makers. Box 2.5 presents an example of how measures regarding care for breast cancer could be classified using the categories of consumer perspectives on health care needs.
Page 59
A focus on selected conditions is in line with both consumer and policy-maker perspectives on care and consumers’ interest in specific conditions that affect them and their families (Hibbard et al., 1996). Media coverage of health care issues also tends to focus on specific conditions, such as breast cancer, rather than generic aspects of health and health care.
In addition, a condition focus facilitates the study of the linkages between specific processes and outcomes of care for particular conditions. It would also allow an examination of care for specific conditions across health care settings (which may change over time), populations, and, in certain cases, stages of disease. For example, just as one might compare the quality of care received by low- and high-income people to examine equity, subanalyses of quality of care for people with heart disease versus those with diabetes might be used to compare achieved levels of quality of care by condition and corresponding clinical specialties. However, when comparing quality of care for different conditions it will be important to take into account possible confounding of the results by differences in the specific quality indicators used for each condition rather than true differences in the underlying quality of care.
The specific conditions or clinical areas that are the focus of the Quality Report can change from year to year, but they should be limited in number. Several methods are available for the prioritization of conditions (Siu et al., 1992). Two important national efforts have produced lists of priority conditions: Healthy People 2010 (U.S. Department of Health and Human Services, 2000) and the Medical Expenditure Panel Survey (MEPS) (Agency for Healthcare Research and Quality, 2000a). Both used the importance of the problem, as defined by morbidity and mortality, as an essential criterion for defining disease priorities.
The 28 focus areas in Healthy People 2010 represent the country’s public health priorities and underwent extensive review and public comment (U.S. Department of Health and Human Services, 2000). Among these, 11 focus areas refer to conditions or health problems that may also be relevant to the National Health Care Quality Report ( Table 2.2).4 The Agency for Healthcare Research and Quality (AHRQ) has also produced a list of 15 priority conditions for the MEPS. Initially, the MEPS sample will be expanded to produce reliable estimates for seven of these conditions ( Table 2.2 ) (Agency for Healthcare Research and Quality, 2000c; Cohen, 2000). Conditions can be used to examine quality across the two main dimensions of the framework (components of quality and health care needs) and, in certain cases, to prioritize measures. Although the conditions set forth in Table 2.2 would be a good starting point, a formal process
4 Given the hoped-for policy focus on Healthy People 2010 targets, it will also be important to assess whether quality improves more in focus or target areas than in non-target areas and to ensure that quality does not worsen in the latter due to a redirection of leadership and resources.
Page 60
would be necessary to define the conditions for the National Health Care Quality Report, which could change periodically. Ideally, and in the long term, the Quality Report should expand to examine care comprehensively, and for the population as a whole, by selecting enough clinical areas to represent the majority of health care delivery, as discussed in Chapter 3.
|
MEPSa |
Healthy People 2010 b |
|
Long Term, Life Threatening |
Arthritis, osteoporosis, and chronic back conditions |
|
Cancer (any body part) | |
|
Diabetes |
Cancer (lung, pharynx, breast, cervical, colon, prostate, melanoma) |
|
Emphysema |
|
|
HIV/AIDS |
Diabetes |
|
Hypertension |
Respiratory diseases (includes asthma, chronic obstructive pulmonary disease, and sleep apnea) |
|
High cholesterol |
|
|
Ischemic heart disease |
|
|
Stroke |
HIV |
|
Heart disease and stroke (includes blood pressure and cholesterol) |
|
|
Chronic, Manageable Diseases |
|
|
Arthritis |
Immunizations and infectious diseases |
|
Asthma |
Chronic kidney disease |
|
Back problems |
Mental health |
|
Gall bladder disease |
Overweight and obesity |
|
Stomach ulcers |
Sexually transmitted diseases |
|
Mental Health Issues |
|
|
Alzheimer’s and other dementias |
|
|
Depression and anxiety disorders |
a These are the conditions designated as "priority conditions" for MEPS sample expansion.
b This list includes only those Healthy People 2010 focus areas that refer to health conditions.
SOURCES: Agency for Healthcare Research and Quality, 2000c; U.S. Department of Health and Human Services, 2000.Using a Matrix to Portray the Framework
The framework provides a way of classifying possible measures for the National Health Care Quality Report. Measures included in the report should reflect the components of health care quality for one or more consumer perspec-
Page 61
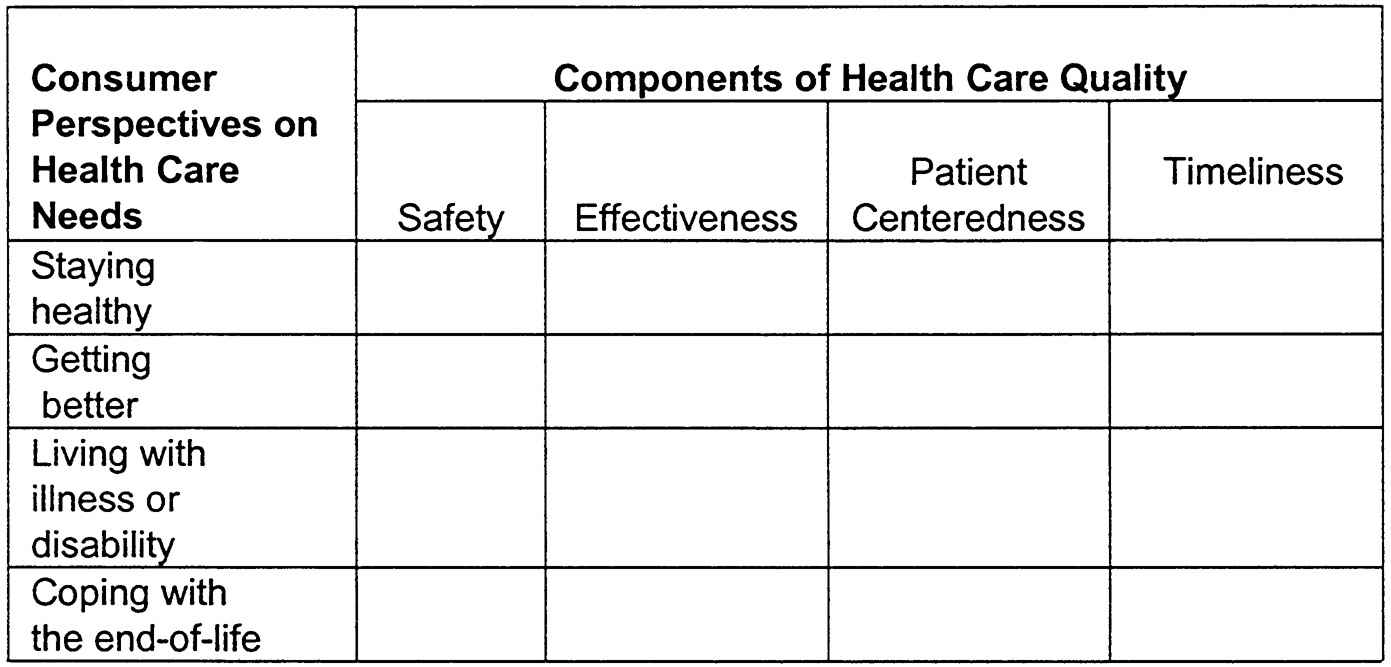
tives on health care needs. Figure 2.2 shows the framework illustrated as a four-by-four matrix. The four consumer perspectives on health care needs—staying healthy, getting better, living with illness or disability, and coping with the end of life—are shown as rows, while the components of health care quality—safety, effectiveness, patient centeredness, and timeliness—are shown as columns.
Potential quality measures can be placed in one of the cells corresponding to the particular component of quality and the specific health care need it most reflects. For example, a measure of surgical errors would belong in the safety– getting better cell, whereas having an indication of egg sensitivity clearly noted in the medical record would be found in the safety–staying healthy cell. Likewise, waiting time for a well-baby visit would belong under timeliness–staying healthy, and waiting time for placement in a hospice would belong under timeliness–coping with the end of life. Some measures may appear in multiple rows, such as being able to understand your clinician (an aspect of patient centeredness), but the relative importance or salience given such measures may vary with the specific consumer perspective.
~ enlarge ~
FIGURE 2.2 Classification matrix for measures for the National Health Care Quality Report.
The matrix can be used to help define the type of measures that should go into the report, to categorize the measures, and to examine how various aspects of the framework may relate to each other. Every cell will not necessarily be of equal importance to policy makers and consumers, nor will all combinations of rows and columns be equally rich in data. When necessary and useful, the relative importance of each cell can be denoted by weights; however, the method used to arrive at these weights needs to be clearly explained and scientifically based. Ultimately, the matrix is intended only as a heuristic tool, rather than as a
Page 62
formulaic and inflexible template. It can be used when considering approaches to quality measurement to help visualize possible combinations of the two dimensions of the framework that could be used to evaluate quality.
The matrix should not be used as a template or checklist of measures for several reasons. First, it does not indicate the subcategories of measures for each core competency. For example, patient centeredness should be assessed using measures of both the patient's experience of care and the presence of an effective partnership, but this is not evident from the matrix. Second, measures may fit into more than one cell in the matrix. For example, measures for timeliness as the receipt of care when needed are relevant for all four consumer perspectives on health care needs. Third, the matrix format does not reflect the fact that some cells will provide more information than others. For example, although safety is important in all situations, instances in which safety is problematic or can be improved are more common when getting better or recuperating from acute illnesses that require hospitalization than in other situations. Finally, some cells in the matrix will not contain measures because the measures have not been developed yet. For example, very few measures exist for end-of-life care for any of the four components of quality. In this case, the matrix can serve to evaluate the extent to which indicators that are currently available through existing data sources provide some depth and breadth in capturing respective dimensions. Rather than being a drawback, the matrix can serve to point out areas of quality measurement that require further research.
|
Equity refers to providing care that does not vary in quality because of personal characteristics such as gender, ethnicity, geographic location, and socioeconomic status (Institute of Medicine, 2001). |
Equity in Quality of Care as a Cross-Cutting Issue in the Framework
The committee recommends that equity be examined as an essential cross-cutting issue that may influence system performance and the quality of health care. Equity has to be assessed across all components of health care quality: safety, effectiveness, patient centeredness, and timeliness. Equity can also be assessed across consumer perspectives on health care needs and for specific conditions. Variations in the quality of care for any quality component may be analyzed by examining disparities among groups by race, ethnicity, gender, age, income, geographic location, or insurance status and other socioeconomic conditions. These are the factors that have to be considered within each cell of the classification matrix in order to examine equity or variations in quality of care for various subgroups ( Figure 2.2). For example, to assess equity in the timeliness of care when patients seek to stay healthy, the waiting time for a well-baby
Page 63
visit for those living in rural areas can be compared to the waiting time for those living in urban areas. Such analyses would focus on the nonclinical sources of variations in quality and potential disparities in quality of care.5
The National Health Care Quality Report and Data Set should provide policy makers with the capability of examining issues of equity. Two aspects of quality are of particular interest: (1) differences in access to health care services by various subpopulations, and (2) differences in treatment received based on unrelated personal characteristics. The committee proposes that both of these aspects of equity be examined by conducting cross-cutting analyses.
A growing body of literature points to variations in access to health care services by several population characteristics (Ayanian et al., 2000; Fiscella et al., 2000). A recent article cited more than 100 studies indicating inequalities in access to care, utilization of services, treatment, and outcomes of care by race, ethnicity, age, insurance, and socioeconomic status, with a large number of these documenting differences between blacks and whites (Fiscella et al., 2000). The twenty-second report on the health status of the nation—Health United States 1998—documented inequalities in access to care and health status by income, education, gender, race, and Hispanic origin (National Center for Health Statistics, 1998). Other studies have shown that access to providers, use of services, and health outcomes are better for those with health insurance than for those without it, even after taking into account race and income (American College of Physicians–American Society of Internal Medicine, 1999). The National Health Care Quality Data Set and the Quality Report should permit identification of areas in which disparities are the greatest. They should also provide information on whether such disparities are getting larger or smaller over time in response to policy initiatives and/or general social and economic conditions.
A second aspect of equity has to do with the delivery of health care services to individuals. Recent studies, including the literature review by Fiscella and colleagues (2000) previously cited, raise concerns about whether treatment options identified, and the nature and quality of health care services provided, may vary by factors such as race, ethnicity, gender, age, income, or insurance status (Ayanian and Epstein, 1991; Ayanian et al., 1999; Bennett et al., 1991; Dedier et al., 1999; Gatsonis et al., 1995; Parham et al., 1997; Schulman et al., 1999). For example, studies have shown that African-American Medicare beneficiaries are less likely
5 Nonclinical sources are those determined by social factors of both patients and providers and by geographical factors, rather than by the capabilities of the health care system in various clinical areas. Variations in quality may also be clinically driven, as is the case for variations in the quality of care across different chronic conditions, determined largely by the state of the science. Clinically driven variations are not the focus of this discussion because they are not indicators of equity; rather they are indicators of technological advances and of the extent of the evidence base regarding care for specific conditions.
Page 64
than whites to receive many kinds of medical procedures, including cardiovascular procedures, orthopedic and back procedures, and several surgical procedures, and are more likely to die as a consequence of these procedures (McBean and Gornick, 1994). Others have shown that Hispanics are less likely than non-Hispanic whites to receive major inpatient therapeutic procedures for 24 of 63 conditions examined including coronary artery disease, several types of cancer (breast, colon, lung), most traumas, and several gastrointestinal conditions (Andrews and Elixhauser, 2000). Hispanics were more likely to receive major therapeutic procedures for four of the conditions examined including renal failure.
The committee views the lack of equity in access to care and medical treatment as a quality problem. Other things being equal, the presence of disparities may be an indication that quality is below the maximum obtainable level for some groups of the population given that others have attained higher levels. Current data collection and reporting systems are inadequate to examine disparities in quality of care (Eisenberg and Power, 2000; Fiscella et al., 2000). Given the U.S. Department of Health and Human Services' goal of eliminating disparities in health and health care within the next 10 years (U.S. Department of Health and Human Services, 2000), the importance of examining issues of equity in quality of care should not be underestimated. As mentioned in Chapter 1, the Quality Report, together with a planned report on disparities in health care delivery mandated by the same legislation, should help to remedy this situation (Healthcare Research and Quality Act, 1999:Sec. 902). One of the uses of the National Health Care Quality Report and Data Set should be to document and disseminate information on the equity of health care delivery for all the people of the United States. The Quality Report should be articulated with the planned “disparities report,” which—according to the committee's understanding— would feature in-depth analyses of disparities in health care delivery by race and socioeconomic status.
What About Efficiency?6
As mentioned at the beginning of this chapter, the committee is aware of the economic size and importance of the health care industry and of the fact that quality is only one of several system goals. Efficiency, defined as “avoiding waste, including waste of equipment, supplies, ideas, and energy” by the IOM Committee on Quality of Health Care in America, is one of six health care system aims for quality improvement proposed by that same committee (Institute of Medicine, 2001). Health care systems and processes of care, in particular, can be
6 This topic is treated in depth in a paper commissioned by the committee from Mark McClellan on measures of efficiency for the National Health Care Quality Report (2000).
Page 65
BOX 2.6 Questions Addressed by the National Health Care Quality Report
Overall
Components of Health Care Quality
Consumer Perspectives on Health Care Needs
Equity
|
Page 66
wasteful due to deficiencies in any of the four components of quality as defined in the framework. Quality measures related to safety, effectiveness, patient centeredness, or timeliness can indicate potential problems in the efficiency of production and/or the allocation of services. For example, lack of safety indicated by errors in health care that lead to avoidable complications can result in greater resource use. Efficiency is clearly related to the quality of care. For example, quality measures of specific aspects of effectiveness—particularly overuse and inappropriateness—may indicate potential problems of efficiency in service allocation. Ineffectiveness stemming from overuse or inappropriateness can result in wasted resources, as well as problems that include poor health associated with readmissions (Oddone et al., 1996) and lengthened hospital stays (Broderick et al., 1990). Ultimately, inefficiency is characterized by the use of resources that do not provide the best value in meeting people's health care needs.
Efficiency is clearly related to the quality of care. Many of the quality issues that will be presented in the Quality Report will require potential trade-offs. However, efficiency, particularly with regard to cost per unit of service, falls outside the scope of the Quality Report and will be better addressed by specific efforts designed to face the considerable methodological and measurement challenges involved (McClellan, 2000). Doing so will allow for examination of the value of health care as reflected in the relationship between quality and costs. It will also make possible the definition of appropriate policies to address each of these aspects of value separately.
SUMMARY
The National Health Care Quality Framework described in this chapter responds to a set of basic questions that together provide a picture of the quality of health care being delivered in this country over time. These questions refer to the components of health care quality and consumer perspectives on health care needs, including care for specific conditions. The measures included in the framework can be used to examine equity, or how certain groups of people fare compared to others, and to describe the evolution in the quality of care being delivered in the United States over time. Box 2.6 presents the list of basic questions that should be addressed by the Quality Report.
REFERENCES
, , and . 1975. Development of Indices of Access to Medical Care. Ann Arbor, Mich.: Health Administration Press.
. 1998. Quality First: Better Health Care for All Americans. Washington, D.C. : U.S. Government Printing Office.
. 1998. CAHPS 2.0 Questionnaires . [on-line] http://www.ahrq.gov/qual/cahps/cahpques/htm [Feb. 18,. 2001].
Page 67
2000a. Overview of MEPS [on-line]. Available at: http://www.meps.ahrq.gov/WhatIsMEPS/Overview.htm [Jan. 3, 2001].
. 2000b. What Is MEPS? [on-line]. Available at: http://www.meps.ahrq.gov/whatis/htm [Jan. 3, 2001].
2000c. MEPS HC-006R: 1996 Medical Conditions [on-line]. Available at: http://www.meps.ahcpr.gov/pubdoc/hc6rdoc.pdf [Feb.26, 2001].
2001. Survey Instruments and Associated Documentation [on-line]. Available at: http://www.meps.ahrq.gov/survey.htm [Feb. 18, 2001].
. 1999. No Health Insurance? It's Enough to Make You Sick. Philadelphia. Available at: http://www.acponline.org/uninsured/lack-contents.htm .
. 1998. The Diabetes Quality Improvement Project [on-line]. Available at: http://www.diabetes.org/dqip.asp [Jan. 12, 2001].
, . 1995. Quality improvement guidelines for the treatment of acute pain and cancer pain. Journal of the American Medical Association 274: 1874–1880.
, , , , , , and . 1995. Patient empowerment: Results of a randomized control trial. Diabetes Care 18(7): 943–949.
, , and . 2000. Use of major therapeutic procedures: Are Hispanics treated differently than non-Hispanic whites? Ethnicity and Disease 10: 384–394.
, , and . 1997. Beyond child development centres: Care coordination for children with disabilities. Child: Care, Health and Development 23: 29–40.
, , and . 2000. Patient preferences for medical decision making: Who really wants to participate? Medical Care 38(3): 335–341.
, , and . 1991. Differences in the use of procedures between women and men hospitalized for coronary heart disease. New England Journal of Medicine 325(4): 221–225.
, , , , and . 1999. Quality of care by race and gender for congestive heart failure and pneumonia. Medical Care 37(12): 1260–1269.
, , , , , and . 2000. Unmet health needs of uninsured adults in the United States. Journal of the American Medical Association 284(16): 2061–2069.
, , , , , , Francesco Pinciroli , and . 1997. Electronic communication with patients: Evaluation of distance medicine technology. Journal of the American Medical Association 278(2): 152–159.
, , and . 1990. Patient information-seeking behaviors when communicating with doctors. Medical Care 28(1): 19–28.
, , , and . 1998. Patients' preferences for participation in clinical decision making: A review of published surveys. Behavioral Medicine 24(2): 81–88.
, , , , , , and and . 1991. Patterns of care related to age of men with prostate cancer. Cancer 67(10): 2633–2641.
Page 68
, . 2000. Measuring Patient Centered Care Across Consumer Relevant Domains of Quality. Commissioned paper for the Institute of Medicine Committee on the National Quality Report on Health Care Delivery.
, , , , , and . 1991. Consequences of queing for care at a public hospital emergency department. Journal of the American Medical Association 266(8): 1091–1096.
, , , , , and . 1995. Ethnicity and attitudes toward patient autonomy. Journal of the American Medical Association 274(10): 820–825.
, 2000. Information services that make patients co-producers of quality health care. Studies in Health Technology and Information 76: 93–106.
, . 1999. Why did I miss the diagnosis? Some cognitive explanations and educational implications. Academic Medicine 74(10 (Supplement)): S138–S143.
, , , , , and . 1999. Informed decision making in outpatient practice: Nicole M. Hasenberg Time to get back to basics. Journal of the American Medical Association 282(4): 2313–2320.
, 1991. The ideal of shared decision making between physicians and patients. Kennedy Institute of Ethics Journal 1(1): 28–47.
, , , , , and . 1990. Nosocomial infections: Validation of surveillance and computer modeling to identify patients at risk. American Journal of Epidemiology 131(4): 734–742.
, , , and . 1998. Media coverage of managed care: Is there a negative bias? Health Affairs 17(1): 9–25.
, . 1989. Transparency. Informed consent in primary care. Hastings Center Report 19: 5–9.
, , and . 1985. Efficacy, effectiveness, variations, and quality—Boundary-crossing research. Medical Care 23(5): 710–722.
, , and . 1976. Doctors Talking to Patients. A Study of the Verbal Behavior of General Practitioners Consulting in Their Surgeries. London: H.M.S.O.
, , and . 1992. Delay in breast cancer: A review of the literature. Public Health Review 93(20): 187–214.
. 1999. Patients as Effective Collaborators in Managing Chronic Conditions, New York.
. 1995. Pneumonia and influenza death rates—United States, 1979–1994. Morbidity and Mortality Weekly Report 44: 535–537.
. 1999. National vaccination coverage levels among children ages 19–35 months—United States , 1998. Morbidity and Mortality Weekly Report 48: 829–830.
, , , and . 1999a. Decision-making in the physician–patient encounter: Revisiting the shared treatment decision-making model. Social Science and Medicine 49(5): 651–661.
, , , and . 1999b. What do we mean by partnership in making decisions about treatment? British Medical Journal 319: 780–782.
Page 69
, , and . 1998. The urgent need to improve health care quality: Institute of Medicine National Roundtable on Health Care Quality. Journal of the American Medical Association 280(11): 1000–1005.
, , , , , , , , , , and . 1987. Does inappropriate use explain geographic variations in the use of health services? A study of three procedures. Journal of the American Medical Association 258(18): 2533–2537.
, , and . 1993. Adequate access to posthospital home health services: Differences between urban and rural areas. Journal of Rural Health 9(4): 262–269.
, , and . 1995. Professional negligence in the management of cancer pain: A case for urgent reforms. Cancer 76(11): 2181–2185.
, . 2000. Culturally competent health care. Public Health Reports 115(1): 25–33.
, , and . 2000. Extent and determinants of error in doctors' prognoses in terminally ill patients: Prospective cohort study. British Medical Journal 320(7233): 469–473.
, , 2000. Personal communication, October 5. Agency for Healthcare Research and Quality.
, , , , , , , and . 1999. Race, Gender, and Partnership in the Patient-Physician Relationship. Journal of the American Medical Association 282(6): 583–589.
, , , , , , and . 1997. Identification of patient attitudes and preferences regarding treatment of depression. Journal of General Internal Medicine 12(7): 431–438.
, , , and . 1996. What role do patients wish to play in treatment decision making? Archives of Internal Medicine 156: 1414–1420.
, , , , and 1999. Race, ethnicity, and the patient–caregiver relationship. Oncologist 4(4): 325–331.
, and . 1988. Preferences for treatment control among adults with cancer. Research in Nursing and Health 11: 367–374.
, , and . 1996. The impact of health maintenance organization care authorization policy on an emergency department before California's new managed care law. Academic Emergency Medicine 3(4): 338–344.
, , , and . 1994. Enhancing medication adherence through communication and informed collaborative choice. Health Communication 6(4): 253–265.
, , and . 2000. Transforming insurance coverage into quality health care. Journal of the American Medical Association 284(16): 2100–2107 .
, , and . 1992. Four models of the physician–patient relationship. Journal of the American Medical Association 267(16): 2221–2226.
. 1989. Caring for Our Future: The Content of Prenatal Care. Washington, D.C.: U.S. Public Health Service.
Page 70
, , , , and . 2000. Inequality in quality: Addressing socioeconomic, racial, and ethic disparities in health care. Journal of the American Medical Association 283(19): 2579–2584.
. 1996. Measuring Quality [on-line]. Available at: http://www.facct.org/measures.html.
. . Reporting Quality Information to Consumers , Portland, Ore.: FACCT.
, , , , , and . 1995. Variations in the utilization of coronary angiography for elderly patients with an acute myocardial infarction. Medical Care 33(6): 625–642
. 1981. Preparation for childbirth—Evidence for efficacy. A review. Journal of Obstetric, Gynecologic, and Neonatal Nursing 10(2): 82–85.
, , , , , , , , , and . 2000. Hospital safety climate and its relationship with safe work practices and workplace exposure incidents. American Journal of Infection Control 28(3): 211–221.
, 1999. Informed consent, cultural sensitivity, and respect for persons. Journal of the American Medical Association 274(10): 844–845.
, , and . 1992. Financing maternal and child health care in the United States. Pp. 173–185 in A Pound of Prevention: The Case for Universal Maternity Care in the U.S. eds. Jonathan B. Kotch, Craig H. Blakely, Sarah S. Brown, and Frank Y. Wong. Washington, D.C.: American Public Health Association.
, , , and . 1998. Place of death and access to home care services: Are certain patient groups at a disadvantage? Social Science and Medicine 47(5): 565–579. ,
, , , , , , , and . 1994. The use of outcomes research for medical effectiveness, quality of care, and reimbursement in type II diabetes. Diabetes Care 17(Supplement 1): 32–39.
, , , , , , , and . 1999. Resolving the gatekeeper conundrum: What patients value in primary care and referral to specialists. Journal of the American Medical Association 282(3): 261–266.
, , and . 1998. Patient participation in decision making. Social Science and Medicine 47(3): 329–339.
. 2000. Medicare Priorities. Baltimore, Md.: U.S. Department of Health and Human Services.
, , , and . 1996. Conditionspecific performance information: Assessing salience, comprehension, and approaches for communicating quality. Health Care Financing Review 18(1): 95–109.
, 1997. Assessing quality using administrative data. Annals of Internal Medicine 127(8): 666–674. . 2000. To Err Is Human: Building a Safer Health System. eds. Linda T. Kohn, Janet M. Corrigan, and Molla S. Donaldson. Washington, D.C.: National Academy Press.
Page 71
. 2001. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, D.C.: National Academy Press.
, , , and . 2000. Improving general practice care of patients with asthma or chronic obstructive pulmonary disease: Evaluation of a quality system. Effective Clinical Practice 3(1): 16–24.
. 2000a. Sentinel Event Statistics [on-line]. Available at: http://www.jcaho.org/sentinel/se_stats.html [Aug. 7, 2000].
. 2000b. Joint Commission and Health Care Financing Administration Core Measure Crosswalks for Acute Myocardial Infarction, Heart Failure and Community Acquired Pneumonia [on-line]. Available at: http://www.jcaho.org/perfmeas/coremeas/letter.html [Feb. 19, 2001].
, , and . 1998. Guidelines for the clinical use of electronic mail with patients. Journal of the American Medical Informatics Association 5(1): 104–111.
, , , , and . 1995. Patient and visit characteristics related to physicians' participatory decision-making style: Results from the Medical Outcomes Study. Medical Care 33(12): 1176–1187.
, , , , , and . 1996. Characteristics of physicians with participatory decision-making styles. Annals of Internal Medicine 124(5): 497–504.
, 1994. Access to specialty care. New England Journal of Medicine 331(17): 1151–1153.
, , , , ; , and . 1996. The effects of having a regular doctor on access to primary care. Medical Care 34(2): 138–151.
1999. Culturally competent professional in therapeutic alliances enhance patient compliance. Journal of Health Care for the Poor and Underserved 10(1): 19–26.
, , , , and . 1979. Characteristics of individuals who identify a regular source of medical care. American Journal of Public Health 69(3): 261–267.
, , , , , , , , , , and . 1991. The nature of adverse events in hospitalized patients: results of the Harvard Medical Practice Study II. New England Journal of Medicine 324(6): 377–384.
, , , , , , , , , , , , , , , , , , , and . 1995. Systems analysis of adverse drug events. Journal of the American Medical Association 274(1): 35–43.
, , 2000. Letter to Margarita Hurtado, July 13. Joint Commission on Accreditation of Healthcare Organizations
, , , , , , , , , and .
Page 72
1999. Evidence suggesting that a chronic disease self-management program can improve health status while reducing hospitalization. Medical Care 37(1): 5–14.
, , , , and . 1999. Evaluating the quality of cancer care: Development of cancer quality indicators for a global quality assessment tool. Cancer 88(3): 701–707.
, , , and . 1999. A randomized controlled trial of facilitating information given to patients with chronic medical conditions. Journal of Family Practice 48(5): 356–363.
, , , and . 1999. Proposed agenda for the measurement of quality-of-care outcomes in oncology practice. Journal of Clinical Oncology 17(8): 2614–2622.
, , , , , , , , , , and . 1998. Improving the quality of care for Medicare patients with acute myocardial infarction. Journal of the American Medical Association 279(17): 1351–1357.
, , , and . 1999. How patients' preferences for risk information influence treatment choice in a case of high risk and high therapeutic uncertainty: Asymptomatic localized prostate cancer. Medical Decision Making 19(4): 394–398.
, and . 1994. Differences by race in the rates of procedures performed in hospitals for Medicare beneficiaries. Health Care Financing Review 15(4): 77–90.
, . 2000. Potential Efficiency Measures for the National Quality Report on Health Care. Commissioned paper for the Institute of Medicine Committee on the National Quality Report on Health Care Delivery.
, , and . . Ensuring Quality of Care. Beyond Health Care Reform: Key Issues in Policy and Management. eds. R.J. Anderson, T.H. Rice, and G.F. Kominski. San Francisco, Calif.: Jossey-Bass.
, . 1998. The functions and limitations of trust in the provision of medical care. Journal of Health Politics, Policy and Law 23(4): 661–686.
, , , and . 2001. Are patients' office visits with physicians getting shorter? New England Journal of Medicine 344(2): 190–204.
, , and . 2000. Concepts of trust among patients with serious illness. Social Science and Medicine 51 (5): 657–658.
. 2000. Medscape Multispecialty Practice Guidelines [on-line]. Available at: http://www.medscape.com/Home/Topics/multispecialty/directories/dir-MULT.PracticeGuide.html [Oct. 15, 2000].
, , , , , , , , , , and . 1997. Quality of care, process, and outcomes in elderly patients with pneumonia. Journal of the American Medical Association 278(23): 2080–2084.
, , and . 1994. Qualitative Data Analysis. Thousand Oaks, Calif.: Sage.
1997. Office procedures. Education, training, and proficiency of procedural skills. Primary Care 24(2): 231–240.
Page 73
, and . 1999. The relationship of pre-mortem diagnoses and postmortem findings in a surgical intensive care unit. Critical Care Medicine 27(2): 299–303.
, , and . 1998. Must patients wait? Joint Commission Journal on Quality Improvement 24(80): 423–425.
. 1998. Health, United States, 1998: Socioeconomic Status and Health Chartbook, Hyattsville, Md.: U.S. Government Printing Office.
. 2000. HEDIS 2001, Vol. 1. Washington, D.C.: NCQA.
. 1996. Cervical Cancer. NIH Consensus Statement. 14(1): 1– 38.
. 2000. Agenda for Research and Development in Patient Safety [on-line]. Available at: www.npsf.org.
, , , , , , and . 2000. Patient-centered quality measures for Asian Americans: Research in progress. American Journal of Medical Quality 15(4): 167–173.
, , and . 1996. Reducing Delays and Waiting Times Throughout the Healthcare System. Boston, Mass.: Institute for Healthcare Improvement.
, , , , , , , , , , , , , , , and . 1996. Classifying general medicine readmissions. Are they preventable? Veterans Affairs Cooperative Studies in Health Services Group on Primary Care and Hospital Readmissions. Journal of General Internal Medicine 11(10): 597–607.
, , , and . 1995. Doctor–patient communication: A review of the literature. Social Science and Medicine 40(7): 903–918.
, , and . 1997. The National Cancer Data Base report on malignant epithelial ovarian carcinoma in African-American women. Cancer 80: 816–826.
, . 1994. Exploring family practitioners' and patients' information exchange about prescribed medications: Implications for practitioners' interviewing and patients' understanding. Health Communication 6(4): 267–280.
, , and . 2000. Patients' trust in physicians: many theories, few measures, and little data. Journal of General Internal Medicine 15(7): 509–513.
, , , and . 1998. Increase in U.S. medication-error deaths between 1983 and 1993. Lancet 351: 643–644.
, 1996. A revolution in health promotion: Smoking less as a case study. Health Psychology Through the Lifespan: Practice and Research. eds. Robert J. Resnick and Ronald H. Rozensky. Washington, D.C.: American Psychological Association.
. 2000. Doing What Counts for Patient Safety: Federal Actions to Reduce Medical Errors and Their Impact. Report of the Quality Interagency Coordination Task Force to the President , Rockville, Md.
2000. Is the physician office the wild, wild west of health care? Journal of Ambulatory Care Management 23(2): 64–73.
, 1990. Human Error. New York: Cambridge University Press.
, , , and . 2000. Patient centeredness in medical encounters requiring an interpreter. American Journal of Medicine 108(6): 470–474.
Page 74
, , , , and . 2001. Assessing medical students' awareness of a sensitivity to diverse health beliefs using a standardized patient station. Academic Medicine 76(1): 76–80.
, , , and . 2000. The implementation of clinical guidelines in a managed care setting: Implications for children with special health care needs. Managed Care Quarterly 8(2): 29–38.
, 2000. The enduring and evolving nature of the patient–physician relationship. Patient Education and Counseling 39(1): 5–15.
, , , , , , and . 1997. Communication patterns of primary care physicians. Journal of the American Medical Association 277(4): 350–356.
, , , , , , , , , , , and . 1999. ACC/AHA Guidelines for the Management of Patients with Acute Myocardial Infarction: 1999 Update: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Management of Acute Myocardial Infarction) [on-line]. Available: http://www. acc.org/ clinical/guidelines/nov96/1999/amipdf99.pdf [Jan. 17, 2001].
, , , , , , and . . Linking primary care performance to outcomes of care. Journal of Family Practice 47(3): 213–220.
, , , , , , , , , , , , and . 1999. The effect of race and sex on physicians' recommendations for cardiac catheterization. New England Journal of Medicine 340(8): 618–626.
, , , , and . 1995. Organizational aspects of caring. Milbank Quarterly 73(1): 77–95.
, , and . 1983, Health behavior and personal autonomy: A longitudinal study of the sense of control in illness. Journal of Health and Social Behavior 24: 144–160.
, , , , , and . 2000. A guideline implementation system using handheld computers for office management of asthma: Effects on adherence and patient outcome. Pediatrics 105(4 Pt. 1): 767–773.
, . 1976. Continuity of medical care: Conceptualization and measurement. Medical Care 14: 377–391.
, , , , , , , , , , , , , and . 1992. Choosing quality of care measures based on the expected impact of improved care on health. Health Services Research 27(5): 619–650.
, , , , , , , , , , , , and . 1998. Effect of local medical opinion leaders on quality of care for acute myocardial infarction: a randomized controlled trial. Journal of the American Medical Association 279(17): 1358–1363.
Page 75
, . 1992. Primary Care: Concept, Evaluation, and Policy. NewYork: Oxford University Press.
, . 1998. Primary Care: Balancing Health Needs, Services, and Technology. New York: Oxford University Press.
, , , , , and 1998. Consumer experiences and provider perceptions of the quality of primary care: Implications for managed care. Journal of Family Practice 46(3): 216–226.
, , , and . 1999a. Interpersonal processes of care in diverse populations. Milbank Quarterly 77(3): 305–339.
, , , , , and . 1999b. Evidence on patient-doctor communication. Cancer Prevention and Control 3(1): 25–30.
, . 1956. The basic models of the doctor–patient relationship. Archives of Internal Medicine 97: 585–592.
, and . 1998. Home alone: Unmet need for formal support services among home health clients. Home Health Care Services Quarterly 17(2): 1–20.
, , 2000. Letter to Margarita Hurtado, July 25. American Medical Association.
. 2000. Healthy People 2010, Washington, D.C.: U.S. Government Printing Office.
. 1996. Guide to Clinical Preventive Services, 2nd Baltimore, Md.: ed. Williams and Wilkins.
, , , , , and . 1997. Collaborative management of chronic illness: Essential elements. Annals of Internal Medicine 127(12): 1097–1102.
, , and . 1996. Pain Prevalence and Pain Treatments for Residents in Oregon's Long-Term Care Facilities. State of Oregon Senior and Disabled Services Division, Client Care Monitoring Unit.
, , , and . 1995. The effect of a shared decisionmaking program on rates of surgery for benign prostatic hyperplasia. Pilot results. Medical Care 33: 765–770.




































