Page 200
6
The Health of Aging Populations
As the length of life and number and proportion of older persons increase in most industrialized and many developing nations, a central question is whether this population aging will be accompanied by sustained or improved health, an improving quality of life, and sufficient social and economic resources. The answer to this question lies partly in the ability of families and communities, as well as modern social, political, economic, and health service delivery systems, to provide optimal support to older persons. However, while all modern societies are committed to providing health and social services to their citizens, these systems are always in flux, guided by diverse and evolving national and regional policy formulations. Health, social, and economic policies for older persons vary substantially among industrialized nations. Analysis of these variations through appropriate cross-national research may assist greatly in the formulation of effective policies aimed at enhancing the health status, as well as the social and economic well-being, of elderly populations.
Among the most important policy concerns relevant to health and longevity are the future fiscal viability of pension, health, and social insurance systems, both public and private, and the implications of these systems for savings and investment rates (see Chapter 3). How long people continue working, paying taxes, and saving will feature prominently in the consequences of population aging. Many people already work less than half a lifetime because of extended periods of schooling and training in early life, earlier retirement, and enhanced longevity, pos
Page 201
ing a challenge to the sustainability of systems designed to support older persons. If the trend toward increased longevity continues without a parallel extension in working life, the stress on these systems could be even greater.
As discussed elsewhere in this volume, labor force participation, investment and saving behavior, and provision of health services are complex phenomena that are interrelated at both the individual and societal levels (Quinn and Burkhauser, 1994; Smith, 1999). For example, incentives provided by government and employers play important roles in determining labor force participation. Reducing the implicit tax on continuing work beyond the normal age of retirement and reducing the costs of hiring (and possibly retraining) older workers have the potential to encourage longer working lives (see Chapter 3). Yet in designing such incentives, policy makers need to know how long they can reasonably expect people to keep working. Just how physically and mentally capable are older people? What is the trajectory of health and function as people age? Can their productivity be maintained and enhanced at older ages, and at what cost? Does the type of productivity and engagement change with age? How can health care services be provided in such a manner as to maintain optimal health and function? Most basically, policy makers must make difficult decisions about the allocation of limited resources to preserving and improving health. How is good health achieved at a reasonable cost? Should more resources be directed toward behavioral change and other health promotion and disease prevention programs, including health enhancement in early life, or should more be dedicated to the treatment of patients with advanced diseases? How much should be invested in the development of new health care technologies, service delivery enhancements, and professional training?
A focus on national-level health status and its temporal trajectory is critical for several reasons. Health status is one of the most important indicators of well-being, and it predicts a large proportion of societal expenditures on health and social services for the elderly. Health status is also reciprocally affected by social and political policies and programs. Further, health status is malleable through high-quality health promotion and disease prevention programs, as well as effective medical services. National programs and policies that may appear to be devoted to health and health services for older persons often have important implications for and complex interactions with other economic sectors. Table 6-1 provides examples.
This chapter is devoted to the centrality of health status and change in informing health, social, and economic policy formulation. We first outline the key issues to be addressed by research on the health status of the elderly. We then present a conceptual model of the determinants of health
Page 202
|
Sector |
Relation to the Provision of Health Services for Older Persons |
|
Housing |
|
|
Public Health |
|
|
Education |
|
|
Manufacturing |
|
|
Urban Design |
|
|
Transportation |
|
status to provide a framework for the ensuing discussion. Next we review the basic measures of health status, presenting selected examples of basic international patterns and trends. This is followed by a brief look at the characteristics of national health systems. Data sources for cross-national research on the health status of the elderly are then considered, as well as the pitfalls and strengths of such research. Finally, we offer recommendations for strengthening research in this domain.
KEY ISSUES
National health policy decisions with respect to older persons are becoming increasingly complex for several reasons. As noted in Chapter 2, the numbers of the elderly and oldest old have increased dramatically in most industrialized nations. Countries that already have a substantial elderly population face increasing proportions in the coming decades, with all the accompanying social and economic demands. In addition, nations must prepare for the growing numbers of disabled younger persons who are now surviving to older ages because of improved health care. Policy decisions related to the provision of health services for the elderly have become complex from technological, fiscal, and ethical perspectives. Also, as noted above, health services are intimately tied to the
Page 203
provision of social services and economic support, including housing, nutrition, institutional care, and related activities. Preventive and rehabilitative services have added not only to the costs of care, but also to the potential for improved function, mobility, and social engagement. Health care for older persons is thus different from that provided to other age groups in several respects: greater resource demands; the intertwining of professional health services with social services; the frequent occurrence of important ethical conundrums; a higher prevalence of physical and mental disabilities; and, perhaps not as obvious in policy formulation, less scientific evidence for use in determining effective preventive and medical interventions. In this context, the following issues merit special emphasis.
- 1. What is the importance of health status for retirement preferences and patterns? How are health status and retirement age related? Have recent trends in reduced age-specific rates of disability translated into increased and longer labor force participation?
- 2. What impact does health have on families? How has the changing health status of older persons altered the productivity and economic status of families and households? How do families make economic provisions to care for unhealthy parents, and what are the effects on labor force participation? How does the changing health status of older persons, in particular the onset of infirmity, affect the capacity to be a caregiver for an ill or disabled spouse or other family member? What economic provisions do families make for long-term care of older persons, whether in the community or within chronic care institutions? How do these provisions dovetail with public and voluntary assistance and care programs?
- 3. How important is health to wealth and economic status? What evidence is there that health status directly affects individual wealth, assets, and economic productivity? What is the role of the health care system in the prevention, treatment, and rehabilitation of illnesses, and how does this work to maintain personal economic status? How do health shocks affect future economic status and personal and family wealth in accordance with underlying socioeconomic status?
- 4. How do economic status and educational levels affect the health of individuals across the life course? By what mechanisms and to what degree does economic status lead to better health status? At what ages do the effects of economic status have the greatest impact on health status? How does the distribution of wealth, income, and economic productivity within a nation serve to preserve, enhance, or depress health status independently of individual and family socioeconomic characteristics? How does the provision of health services affect long-term health outcomes?
Page 204
The formulation of health service delivery policies and systems for older persons requires a continuing flow of information, including quantitative data on the above and other issues related to population health status and directions, as well as the resources expended in the health care system. In particular, the ability to draw on international experiences in health and health care can greatly enhance the potential of such policies and systems. Moreover, cross-national research can enable the creation of evaluative mechanisms that would often not be feasible in any one country because of the homogeneity of medical practices and administrative cultures. Such research can also help address the above issues by providing a range of observations of change over time and, perhaps, early indications of emerging health trends. And comparative work can improve our understanding of how particular diseases and conditions are expressed as disability in a variety of work, social, policy, and living environments, thus providing insight into which adjustments in those environments may be most cost-effective.
CONCEPTUAL MODEL OF THE DETERMINANTS OF HEALTH STATUS
As noted above, the determinants of health are complex and comprise multiple policy domains. One basic but important conceptual model that can be used to illustrate the breadth of these determinants is shown in Figure 6-1. This construct represents the health of all demographic groups in a society, although the emphasis here is on the health of older persons. The determinants are presented in a set of concentric circles, with the community population at the center. Outermost, and often difficult to quantify, are the general social, economic, cultural, and environmental (physical-chemical) conditions that have important long-term health effects. The next circle contains society's basic social, health, and economic institutions, which sustain or impair a healthy existence. The next circle emphasizes the critical role of social and community interactions and exchanges, whereby individuals make their collective decisions. The circle next to the core highlights the importance of individual behavioral choices (e.g., cigarette smoking, risk-taking behaviors) in the determination of health status.
One drawback of a two-dimensional representation is the absence of time. Other models highlight more fully such issues as the role of infancy and childhood and the environment on health outcomes in later life. Nevertheless, the model in Figure 6-1 is useful in many respects. For example, it highlights the intimate interaction between the economic and employment environments and health discussed above (see Annex 6-1 for a specific policy example). As a corollary, the model places the role of
Page 205
FIGURE 6-1 A conceptual framework for determinants of health status. SOURCE: Dahlgren and Whitehead (1991). Reprinted with permission. 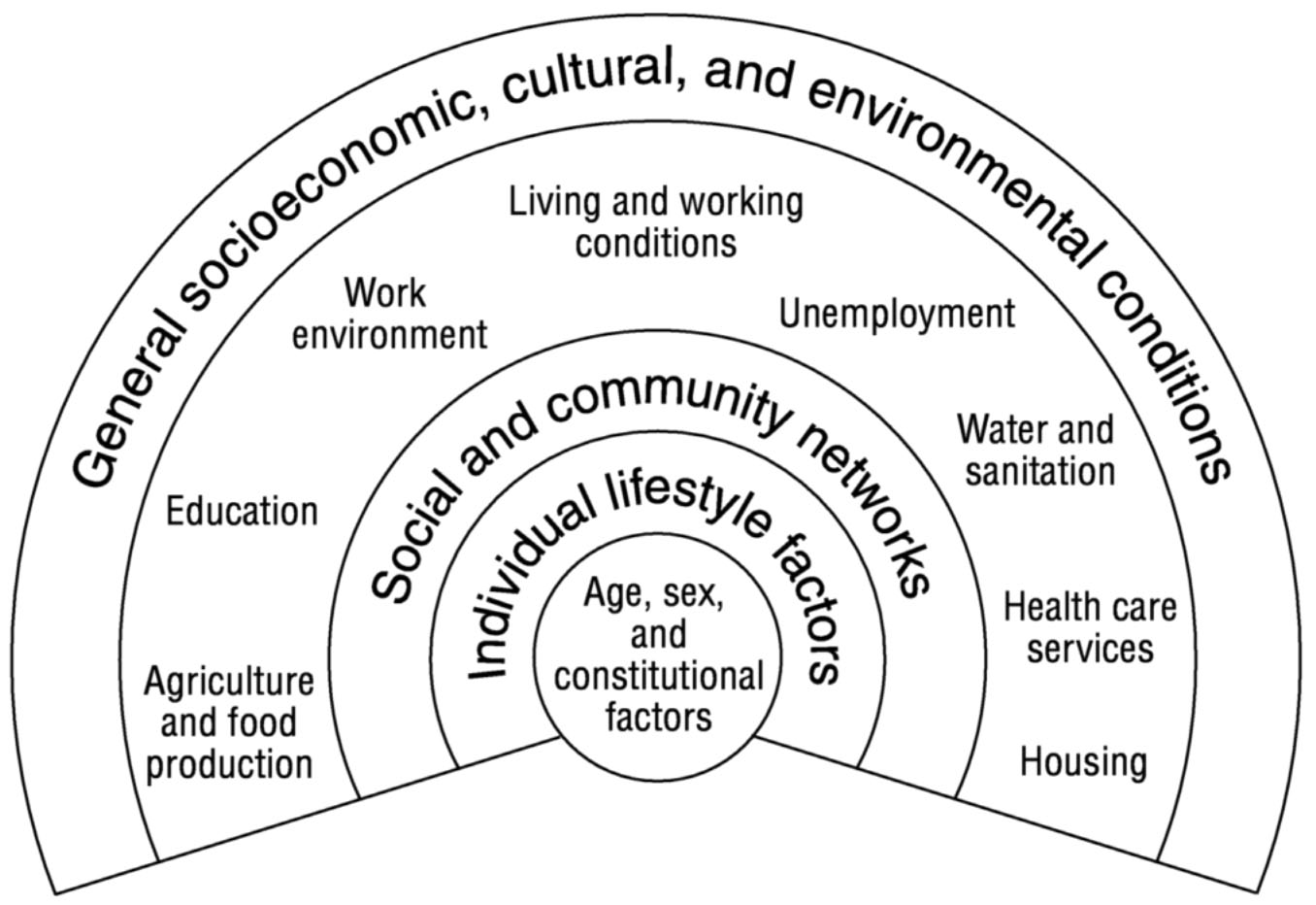
~ enlarge ~
professional health services in an important but not dominant role among the institutional forces that mediate health status. The model quite appropriately also emphasizes the role of basic public health determinants, such as the physiochemical environment and the provision of safe and adequate food and sanitary services. In addition, the model reflects an appreciation of individual responsibility for health status, both in the selection of behaviors and in the collective decisions made by individuals. Finally, the model shows that policy interventions in one institution or domain may or may not have the desired effect because of the multiple sectors involved. Thus, policy outcomes may be enhanced only through multiple intervention points; conversely, interventions in one sector may have unpredicted outcomes in others.
MEASURING HEALTH STATUS
During the 20th century there were great changes in patterns of population health status and survivorship in both the industrialized and developing worlds. Among industrialized nations, the early part of the century saw the greatest improvement in mortality among infants, children, and pregnant women. These improvements continue to the present time.
Page 206
Later in the century, however, substantial reductions in mortality among older adults occurred in nearly all developed countries as a result of declines in deaths primarily from heart disease, but also from other major causes. Moreover, there has been a shift among older persons to surviving, and even thriving, with prevalent chronic illnesses such as various heart conditions and arthritis. Population surveys have also indicated that the age-specific prevalence of physical disability has declined in some countries (Jacobzone et al., 1998). Developing countries have lagged behind their more industrialized counterparts in terms of mortality decline and the overall epidemiological transition from a preponderance of infectious and parasitic diseases to one of chronic and degenerative diseases. As noted in Chapter 2, however, the overall gap between more and less developed countries has narrowed considerably.
The last third of the 20th century also saw a significant expansion in the ways population health status can be characterized, particularly by supplementing mortality data with emerging measures of personal clinical signs and symptoms, diseases and conditions, and functional disabilities. The potential availability of more specific types of health data has greatly increased the set of quantitative tools for health policy and planning, particularly as regards older persons, whose rates of disease and disability are higher than those of other demographic groups.
Identifying the trajectories of important health measures is central to forecasting health care needs and generating policies for older persons. Yet, defining “health” and the health status of individuals is not an easy matter. Even under optimal circumstances and without resource constraints, it is challenging to fully assess the physiological state of individuals, to understand the nature and determinants of personal or social behavior, and to predict the range and intensity of the outcomes of environmental challenges (e.g., from the workplace or elsewhere in the community). Nor is it easy to predict what effects various medical services or interventions will have on individuals. With the newer and more precise measures of health status now available, however, much can be accomplished.
Health status can be characterized from varying perspectives depending on the goals and uses of the information. For example, personal health can be assessed by subjective self-report, more objective physiological and biochemical measurement, or standardized indicators of diseases and disabilities present. In fact, all of these perspectives are important and complementary. Further, health status may be characterized according to major domains such as physical health (e.g., the function of the heart and lungs), mental health (e.g., the presence of depressed mood), and physical and social functional health (e.g., the ability to climb stairs or work at a particular occupation). Health may also be thought of in its
Page 207
temporal, longitudinal dimensions. For example, how is health status changing, or did an individual live or die? Changes in health status may be reflected as well in the intensity of health care resource utilization, such as pharmaceutical, institutional, or rehabilitative care. This temporal perspective is critical and leads to an emphasis on longitudinal, cohort data sources.
While there are no wholly standardized approaches to characterizing health status, there are several meaningful ways in which individual health is assessed and described. These data may not be available from many areas in a computerized or otherwise readily retrievable format, but can usually be obtained by abstracting clinical records or surveying patients, health professionals, administrators, and/or populations within a geographic area. Annex 6-2 describes in detail the health status measures most commonly used for survey and administrative data collection in the categories of clinical signs, symptoms, and syndromes; morbidity (i.e., discretely defined medical conditions); self-rated health; functional status and disability; physiological and pathological measures; mortality data and derived measures; and aging and mental illness.
CHARACTERIZING HEALTH CARE SYSTEMS
As noted in the model of health determinants discussed above, both personal behaviors and many public health measures bear on health status. Health promotional activities aimed at older persons may or may not involve direct contact with the formal health care system; examples of the latter activities include education programs and provision of good preventive nutrition, safe transportation to enhance mobility, and assurance of adequate housing. Thus the efficacy and net impact of many basic public health programs, with their incumbent costs, can be assessed only by using population survey information in addition to the data derived from clinical sources. Moreover, decreased use of toxic substances and increased exercise and structured leisure activities, and even paid and unpaid work, are associated with enhanced function, decreased occurrence of physical and emotional illness, and higher quality of life among older adults. Effective national and regional policies for health promotion among older persons therefore require that important deficits in these areas be identified. Population surveys may be the only means of acquiring accurate information on such issues as cigarette and alcohol consumption, perceived elder abuse, the availability and use of exercise and other leisure and recreational programs, and levels of mobility and social interaction.
Also central to national health policy for older persons is the ability to provide community-based preventive services, generally delivered in the
Page 208
context of primary care. The presence of such services has been used in the United States and elsewhere as a benchmark of the general quality of care (Bloom et al., 2000). Included are such activities as provision of appropriate immunizations and screening for early and treatable conditions, such as colon and breast cancer, high blood cholesterol, high blood pressure, and depression. Explicit geriatric screening and management programs are recommended for falls, early cognitive impairment, physical disability, and inappropriate use of medication. Provision of these services leads to a higher quality of life and helps maintain or enhance function in the elderly. Even in the presence of overt illness, a systematic approach to the complex functional and medical problems of older persons, often referred to as geriatric assessment, can help maintain useful function. Some preventive activities may be recommended by health professionals but executed by others. An important example is environmental screening of residences to prevent falls and enhance mobility, such as by providing ramps rather than stairs and handrails at appropriate locations.
Coordination of public and clinical policies relevant to health promotion and disease prevention among the various sectors involved is essential if these policies are to have the desired positive effects on the health status of older persons. International comparisons of preventive service delivery programs may help identify those with the most desired outcomes and indicate which individual programs may be applied usefully in many nations. For example, standardized specific blood cholesterol levels predict very different heart disease rates in different countries (Kromhout, 1999), possibly leading to different priorities for prevention programs. Again, the most effective means of obtaining the information necessary for such cross-national research is representative household surveys of older persons.
All national health systems are extremely complex in structure, function, and administration. This complexity and diversity makes their classification difficult, a difficulty that is exacerbated by the fact that all health systems are constantly evolving in accordance with ongoing political and economic forces. This complexity also makes policy initiation and assessment, regardless of how broadly construed, extremely challenging. At the same time, however, most modern health care systems, particularly within developed countries, face common forces and challenges: rapid and costly technological innovation; the increasing infusion of business practices to contain the costs of delivering care; growing consumer demands for care that is uniformly distributed geographically and socioeconomically; the provision of effective quality assurance programs; the need to identify funding for the breadth of health services demanded by communities, to balance the needs of primary and specialty care programs,
Page 209
and to respond to complementary and alternative medical practices; and, in many cases, the decentralization of authority in previously monolithic systems.
A variety of classification systems have been proposed and applied in the comparative study of health systems, but no generally accepted taxonomy has emerged. A broad range of health system typologies is reviewed by Mechanic and Rochefort (1996); these typologies variously emphasize such dimensions as political organization and control, economics and fiscal management, population demands and utilization, the role of market forces, universality of coverage, cultural influences on professional practice, the degree of professional dominance, and adherence to various social movements and principles.
Because of the higher rates of morbidity and disability that occur with increasing age, older people make substantial use of formal health services. Such services consume an enormous amount of resources, and a central policy issue for all countries is how to expend available resources in a way that will yield the best health outcomes feasible by the most efficient means. Again, cross-national comparative research is one important avenue for addressing this issue by examining international variations in organization, financing, delivery, and evaluation of elder health services. To illustrate, Figure 6-2 highlights the international variation in per capita nursing home utilization across 20 countries, and Figure 6-3 shows variation in spending for health services across the G7 nations. One of the most important macroanalytical policy questions is the relationship of health system organization, administration, and financing to health status and outcomes. Little work has been done in this area, but cross-national analyses offer the best approach to understanding how major components, such as the level of investment in new technology, affect health outcomes.
There are many units of analysis for characterizing health systems, depending on the issues being addressed. Table 6-2 lists examples of analytic variables commonly used to describe health systems at either the national or regional level. These variables involve a substantial amount of conceptual complexity, and several issues should be considered when using them. As noted earlier, health status is determined only in part by the units of health service delivered. Health systems offer numerous preventive care and public health services in ways that are difficult to quantify. In all age groups, but particularly among older persons, there is a substantial amount of self-care, as well as varying levels of alternative and complementary health care practices, including self-medication with herbs and the use of alternative practitioners, that may have an impact on health outcomes. Further, both preventive and clinical care may impact health outcomes and quality of life only in future decades, and this latency
Page 210
FIGURE 6-2 Percent of elderly population in residential care: Circa 1991. SOURCE: Organization for Economic Co-Operation and Development (1996). 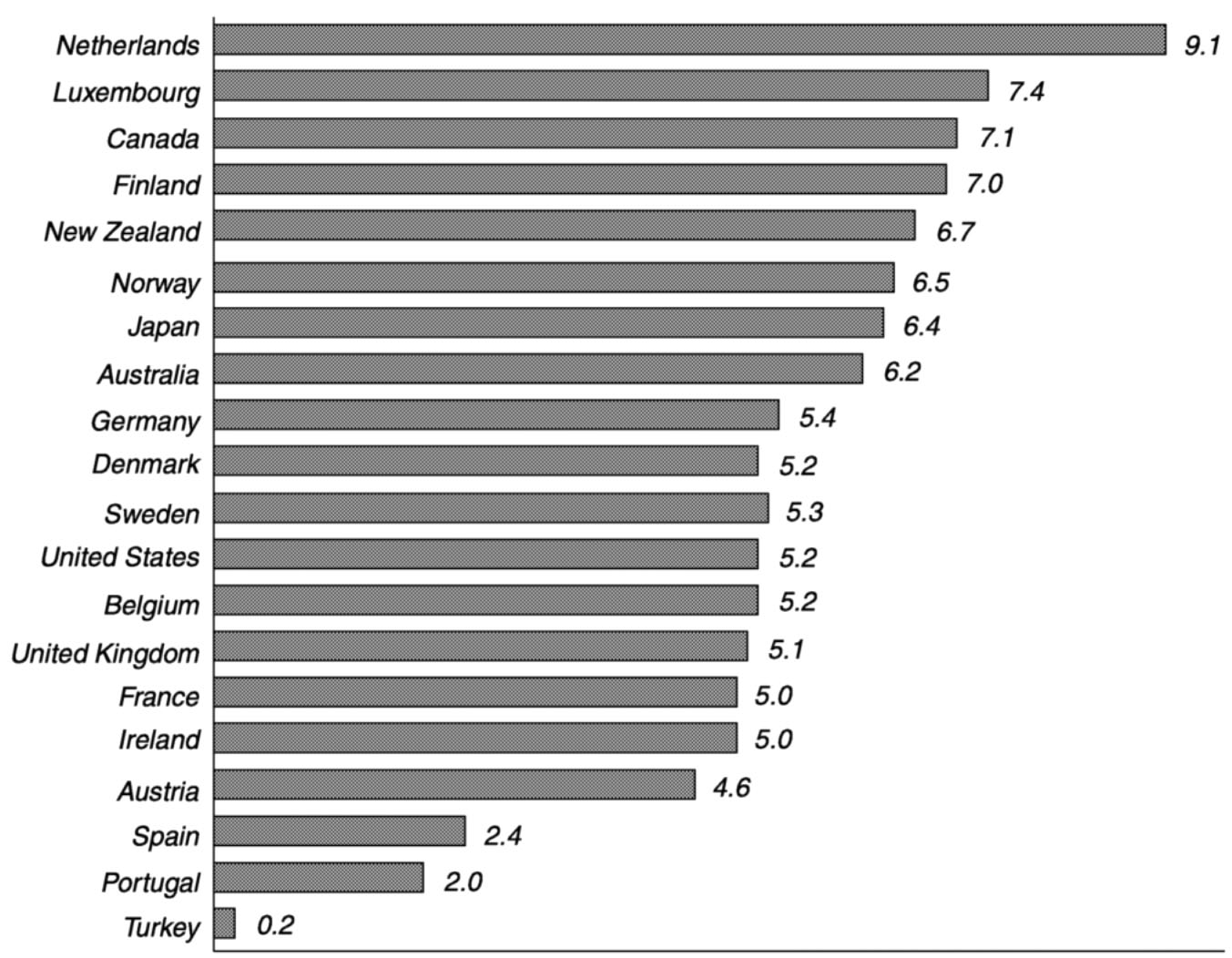
~ enlarge ~
FIGURE 6-3 Medical spending in the G7 countries: 1990. SOURCE: Cutler (1999). 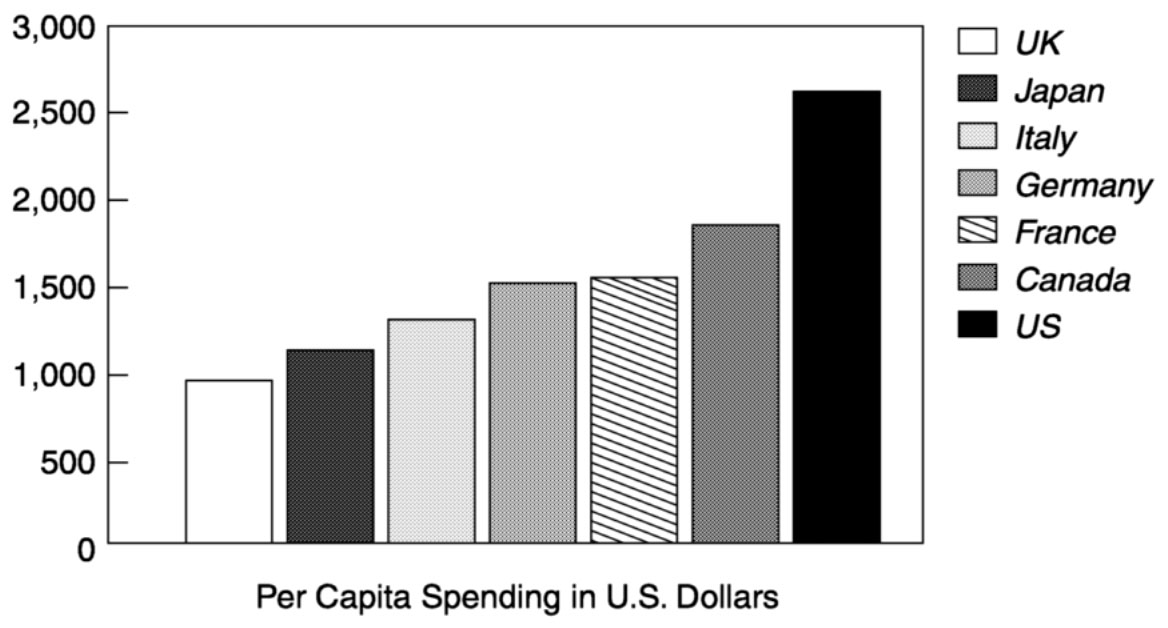
~ enlarge ~
Page 211
|
Category |
Variables |
|
Type of Formal Care: Location/Institutional Nature |
|
|
Basic Funding Mechanisms |
|
|
Community-Based Care Typologies |
|
|
Health Care Utilization Measures |
|
|
Patient-Centered Measures |
|
may be difficult to assess in analytical studies. In fact, many of the fundamental professional activities of health systems may be critically important to patients and their families, but would not be expected to result in objective, quantitative health outcomes; examples include ensuring that illness is not present, providing prognostic information, assisting with care administration issues, and delivering family-friendly hospice care. Despite these conceptual challenges, however, cross-national studies offer the best opportunity to determine how various health system structures and funding and management mechanisms affect health outcomes.
Regardless of how sophisticated, modern, and comprehensive health services may be in a nation, utilization of those services is often uneven and may vary by socioeconomic status, ethnicity, geographic location,
Page 212
and many other factors. Equally important, there may be selective factors related to illness characteristics and personality among individuals that dictate special behaviors within the health system, confounding the study of health outcomes. Moreover, all health care systems have adverse effects, which can diminish the net positive effects of health outcomes. Common examples include hospital-acquired infections, misapplication of therapies, and the unintended adverse effects of medications and devices. It is important to identify these adverse effects, as many are remediable. Finally, there is variation within national health systems in the quality of care and quality assurance programs. For example, substantial small-area variation in medical/surgical procedure utilization rates and health outcomes has been demonstrated within many modern health systems. In addition, some services may be less sophisticated in rural or frontier areas or in other geographical locations. This variation highlights the need for comprehensive, large-area or national data with which to conduct suitable research.
EXISTING HEALTH DATA ON OLDER PERSONS: TYPES, AVAILABILITY, AND QUALITY
The data required to conduct cross-national research on the health status of the elderly may come from many sources, and it is not always possible to anticipate in advance what variables will be needed. Moreover, elderly populations have a number of special characteristics that make their health data needs different from those of other groups:
-
Health events on average occur at a more rapid rate among the elderly than in other age groups, increasing the need for longitudinal (panel) data on cohorts of elders.
-
Older persons have many clinical signs, symptoms, and functional impairments that need to be given special attention since they are not included within traditional administrative data systems that focus on morbidity.
-
Since older persons commonly have multiple medical conditions and functional impairments, there is a need to develop summary measures of comorbidity and health status in order to deal efficiently with the available health and administrative data. Considering the conditions and impairments of the elderly in isolation will, in some instances, impede global policy development.
-
Successful health service delivery for older persons benefits from data on their physical and social environments. Knowledge of the social environment is critical for the large number of elders who have limitations in mobility or self-care; it is also essential for ensuring that pre
Page 213
scribed medical regimens are delivered correctly in both home and community settings. Data on the physical environment are important as well for minimizing falls, injuries, and the progression of disability and, in some cases, for preventing deaths from climate-related causes.
-
Cognitive and mental impairments are common among the elderly, particularly among the oldest old. Such impairments can lead to a lack of social support and interchange, failure to follow medical treatment plans, inability to perform self-care, and increased need for structured supervision and institutionalization. Thus, acquisition of data on the population occurrence and correlates of mental impairments becomes critical for shaping elder health and health care policy. Because some of these impairments preclude direct interviewing of those involved, techniques for acquiring proxy data are necessary.
-
Compared with other age groups, older persons have much higher rates of institutional residence and use of long-term care services in the home and community. A comprehensive national population perspective on this large and growing group requires data on the health status of these persons and the nature of the long-term and institutional care being provided.
The remainder of this section reviews the various sources of health data on the elderly, along with ways in which these data could be made more useful for cross-national research and policy formulation.
Sources of National Health Data
A broad range of data on health and health status is available in most developed nations and increasingly in developing nations as well. These data must be approached cautiously and their limitations recognized. Table 6-3 (adapted from Andrews, 1999) summarizes health data sources and their potential limitations.
As Table 6-3 illustrates, a number of barriers may exist to the successful application of these potentially rich data sources. First, in many instances there may simply be insufficient or inappropriate data gathered or available, and the data collected may be of limited accuracy. There is also little standardization in the collection and representation of administrative data across nations, a limitation that may extend to computer software and formats. Information may not be available in a timely manner, often being delayed by several years. Policy and decision makers may misunderstand the relevance of information for research applications, and those conducting research studies and surveys may misunderstand the policy process, although the imposition of political perspectives on the conduct of research may be detrimental to all. Political, fiscal, and ethical
Page 214
|
Source |
Potential Limitations |
|
Census Data |
Infrequent collection; generally little health content |
|
National Household Surveys |
Target population, sample size, periodicity, comprehensiveness, survey design |
|
Mortality Vital Records |
Age accuracy among elders, analytical access |
|
Morbidity Information |
Accuracy, access, geographic coverage, variation in format and vocabulary/coding |
|
Health Administrative Data |
Timeliness, lack of analysis, format variation |
|
Special Research Studies |
Relevance, quality, presentation, national coverage, availability for analysis |
|
Health Care Evaluations |
Availability, timeliness, accuracy |
|
Outcomes Research |
Varying conceptual frameworks, availability, utility, legal implications |
|
Longitudinal Cohorts/Panels |
Design, costs, timeliness, relevance |
|
Qualitative Studies |
Design, coverage, relevance |
|
Market Research |
Target population, relevance, accuracy |
|
Institutional Sources |
National coverage, costs, data access, identification of all relevant populations, type of data |
considerations may not permit easy distribution of the data to appropriate analysts. Finally, there may be inadequate analytical methodology to summarize and interpret complex and large datasets. Thus concerted administrative and political effort is required to collect the data necessary to exploit the opportunities of cross-national research.
International Repositories of Health Data
Availability and access are key limitations for many of the health data sources listed in Table 6-3. While some datasets will inevitably have limited distribution, others would be usefully provided in repositories or catalogued for administrative and research analysts. No single central repository now exists for health information from population surveys or health system administrative data relevant to older persons. Important catalogues are being compiled, however, by such organizations as the United Nations (Agree and Myers, 1998), the Organization for Economic Cooperation and Development (OECD) (Gudex and Lafortune, 2000), the European Union (Hupkens, 1997), and the U.S. National Institute on Aging (2000). In addition, the Interuniversity Consortium for Political and Social Research at the University of Michigan operates a National Archive of Computerized Data on Aging HtmlResAnchor http://www.
Page 215
icpsr.umich.edu/NACDA/index.html) that is increasingly international in scope. The efforts of these organizations will continue to be important in identifying the data needed for cross-national research.
The Concept of the Graduated Minimum Dataset
The diverse practical needs of health care organizations and agencies that address aging issues, both within and among nations, pose a challenge to achieving the data comparability required to answer many fundamental questions that transcend local populations. Each unit builds administrative data systems and collects data consistent with its unique needs and perceptions of utility. A common problem that results is loss of the capacity to gain analytical power by comparing local experiences with those in other populations or regions.
National governments may deal with this issue by developing minimum and/or core datasets with precise definitions for each data element. Doing so enables common approaches to data reporting on vital and health statistics and to analysis across population groups, elements of service systems, and utilization and costs of care. In the United States, the National Center for Health Statistics, working with other agencies in the Department of Health and Human Services and with the advice of the National Committee on Vital and Health Statistics, establishes minimum datasets, data elements, and data definitions used uniformly throughout the Department of Health and Human Services. While these activities contribute importantly to common nomenclatures and data standards, special data repositories are needed for information thus collected in developed and, where possible, developing countries. The World Health Organization has worked and continues to work toward this end.
Most countries continue to standardize the vocabulary of health services administration. For example, the United States is moving toward a standard long-term care dataset with the following categories: demographic items, health status items, service items, and procedural items. Demographic items include sex, birth date, race, ethnicity, marital status, usual living arrangements (type and location), and court-ordered constraints if any. Such a list could be expanded substantially (for example, to include educational level attained, income from various sources, entitlements received, and religion and religious participation). The list can be altered in response to political, social, or economic forces, as well as agreed-upon international nomenclature where possible.
Variations in data collection across countries greatly compound the difficulties of obtaining comparable information. Even small variations in definition, question formulation, and mode of data collection may significantly alter responses and impair comparability. Moreover, under
Page 216
standing and interpretation of data elements may vary among cultural settings. It is essential to facilitate valid comparisons by easing the data collection burden on countries and regions that have many fewer information gathering resources than the richest Western countries, and by providing a basis for meaningful national comparisons across surveys, administrative data systems, and other sources of health and aging data.
The concept of the graduated minimum dataset could be applied to facilitate health research and policy analysis relevant to aging by providing basic descriptive data on individuals, disease and disability measures, long-term care programs and facilities, health service utilization, and related data elements. Since all nations cannot be expected to invest the same level of resources in data collection, a hierarchy of data collection modules, ranging from easily collected basic data elements to increasingly elaborate datasets, would be an appropriate universal approach. Such a hierarchy might have five to ten levels—from a bare minimum of descriptive statistics to rich and comprehensive data elements such as those found in the Health and Retirement Survey and the Medicare Current Beneficiary Survey. Each such level would have clear definitions of elements, precise wording, and defined response categories. The choice of data elements would be supported by reliability and validity studies justifying their inclusion. Any administrative authority could decide how extensive its data collection would be, but whatever the level selected, the data collected could be made comparable to those from other collection efforts. The value of such a system is that the administrative authority could add any data items needed to meet local purposes without undermining the comparability of the data collection efforts across geographic units. A feasibility study of a small number of aging-related measures, such as those related to disability, could be conducted to test this approach and assess the implementation issues that need to be resolved.
Linking of Health Data
Assessing the health of older persons requires the compilation of data from many sources, such as personal and family surveys, vital records, health care administrative records from various providers, and other health-relevant sectors of society. Moreover, since multiple conditions and impairments are common among older persons, they may seek medical and social services from a variety of providers. The value of data linkage for improved policy formulation has been well-documented (National Research Council, 1988). The use of primary institutional records increases the accuracy of the information available for analysis and complements information that can be gained only from interviews. At the same time, however, there are several potential impediments to record
Page 217
linkage, including costs, privacy concerns, and the logistics of assembling data from multiple sources.
OVERCOMING OBSTACLES TO CROSS-NATIONAL RESEARCH ON THE HEALTH STATUS OF THE ELDERLY
As noted earlier, cross-national comparisons can be useful in a number of ways in addressing issues related to the health status of elderly populations. A cross-national perspective encompasses a broad range of variations that can yield important qualitative insights into alternative institutional arrangements, policies, and programmatic interventions not available for study in one country. Cross-national comparisons can also provide some sense of the generalizability of observations made in specific national and cultural contexts. To the extent that similar patterns and trends are observed across nations that vary in social structure and culture, as well as in health and welfare approaches, one can have greater confidence that generalizations formulated have merit. Box 6-1 provides an example of how a key issue—deinstitutionalization of elders—could be illuminated by cross-national research.
At the same time, one must recognize the complexity involved in comparing national health systems with varying histories, organizational arrangements, cultural influences, and statistical systems. It is essential that when making such comparisons, the analyst understand thoroughly the contexts being compared and the special measurement, definitional, and linguistic features of each system to ensure that comparable units are being evaluated. Even apparently simple concepts can be difficult to compare across systems. As an example, physicians have varying functions in different national health care systems. General practitioners in the United Kingdom and other European nations, for instance, are exclusively community practitioners, while in the United States they typically provide some amount of in-patient and institutional care.
In addition to cultural variations, there are many factors that may limit or confound cross-national research and must be considered to maximize the credibility of the findings of such studies. For example, underlying population health status may vary across nations; this variation may lead to different outcomes of the same health policy or intervention. There may also be differences in the nature, selection, representativeness, or completeness of population samples and health administration databases, possibly leading to spurious analytic findings. Variation in the accuracy and completeness of clinical and vital records information can confound cross-national comparisons as well. Concepts of health states, individual diseases and conditions, and disability may likewise vary across nations and cultures, and such variations may not be fully captured using inter-
Page 218
BOX 6-1Deinstitutionalization of EldersWith continuing increases in longevity, many more people are surviving to advanced ages, when the prevalence of chronic illness and disability increases significantly. In the past, persons surviving with substantial disabilities typically were dependent on family members for their care or were institutionalized in mental hospitals, old-age homes, and other types of custodial institutions (Grob, 1991). Currently, national patterns of family care, the use of custodial institutions, and the mix of long-term care alternatives and services vary substantially (see, e.g., Ribbe et al., 1997; Mechanic and McAlpine, 2000). Thus it would be useful to have a better statistical description of cross-national variations in long-term care and how these services change over time. Future cohorts of elders with high levels of disability face two competing care approaches likely to affect their later years. One approach, which promotes increasing rates of institutionalization, responds to the limited capacities of family members as caregivers as a result of decreased family size, female labor force participation, high divorce rates, increased geographic mobility, and three- and four-generation families with growing care needs and care-giving burdens. A competing approach is focused on deinstitutionalizing dependent populations, including the elderly, those with mental illness, those with developmental disabilities, and others Vladeck, 1980; Mechanic and Rochefort, 1992), making institutional care less likely than demographic predictions would have suggested. In the United States, for example, nursing home rates per 1,000 population for the age groups 65-74, 75-84, and 85+ all declined between 1985 and 1995, resulting in less nursing home demand than was anticipated (Bishop, 1995). Decreasing disability by age may partly explain the decline, but other factors are likely to be salient as well. One important factor is the growth of home-based care. Much more medical and long-term care is provided in the home and homelike settings as a result of changes in technology and financial coverage, as well as the growth of organizational infrastructures needed to provide such care (Kane et al., 1998). These settings include life-care communities, assisted-living facilities, supervised housing, board-and-care and rooming-home residences, adult day care, foster care, and integrated community programs. There is increasing interest among public authorities who deal with the elderly, families, and elders themselves in maintaining as much independence as possible and providing needed care in the least restrictive setting. The extensive medicalization of long-term care characteristic of the American health care system has become less common in many western European countries, where old-age homes based on a social model and community care programs have been more fully developed. Cross-national comparative research is therefore needed to assess the relative costs and health outcomes of these alternative approaches. Such research is challenged, however, by the fact that health data systems are based largely on medical institutions, and few adequate data sources exist that can be used to quantify and characterize newly emerging institutional alternatives. We presently lack clear and consistent definitions of the relevant modalities or minimally adequate sampling frames for studying them. Some useful trend data are available from billing records for home health services, but even very large population sample surveys have too few individuals within each of these care alter |
Page 219
|
natives to provide any reliable information on developing trends. Such problems are compounded in cross-national efforts, in which the designations used may vary a great deal from one setting to another. To address this problem, better descriptive information is needed about the most prevalent long-term care programs in various nations, the range and mix of services they provide, the characteristics of the populations they serve, levels of disability, financing sources, and the intensity of the medical and social services provided (National Research Council, 1988; National Research Council, 1992). It is unlikely that truly comparable data will be acquired in the foreseeable future, but a database providing insight into long-term care alternatives and how they function in varying community and cultural settings could serve as important background for policy formulation on this issue in many nations. |
national disease coding systems. Differences in styles of clinical practice and healer-patient interaction and in the use of alternative practitioners may preclude full comparability of summary diagnostic information. And variations in health service organizational modes, financing, and budgeting may make it difficult to capture resource levels or allocations for comparable units of service delivery. Given these variations, the failure to find certain effects of national health systems on a particular health or programmatic outcome may be due to the noncomparability of the study units as well as to the possibility that no effect is actually present.
At the same time, there clearly is increased comparability among nations in the clinical/administrative and survey data being collected. In the future, cross-national research is likely to be facilitated by increased international exchange of scientific information, as well as by advances in survey instruments and measurement techniques; health care evaluation methodology; clinical training and achievement norms; database computerization and management; and regulatory standards for drugs, devices, and other medical interventions. These advances will be enhanced by the growth of international companies and industries that address the provision of clinical services in many parts of the world.
RECOMMENDATIONS
6-1. Designers of government-sponsored nationwide surveys should enhance basic health information on older persons and strengthen the foundation for standardized measures that can be applied to cross-national comparisons. Health status information on older persons should, at a minimum, include the frequency and rates for (1) deaths and their major causes; (2) important acute and chronic medical conditions and their major manifestations; (3) measures of important self-reported health status; (4) popula-
Page 220
tion levels of physical, social, and mental function; (5) preventive and health promotional behaviors; and (6) important disabilities. In addition, minimum health care information for older persons should include (1) utilization rates for important types of health services, including institutional and home-based care; (2) personal and family expenses for formal health services; (3) rates of use of medications and devices; (4) major cultural influences on the concept of health and the use of health services (such as gender, ethnicity, geographic residence, and socioeconomic status); and (5) the use of informal and alternative and complementary health care services, including self-care practices and assistance from families and other nonprofessional sources.
6-2. The concept of a graduated minimum dataset should be implemented as a means of facilitating health research and policy analysis relevant to aging populations. To provide basic descriptive data on individuals, disease and disability measures, long-term care programs and facilities, and health service utilization, countries should adopt systematic data collection procedures. All nations cannot invest the same level of resources in data collection; thus a hierarchy of data collection modules ranging from easily collected basic data elements to increasingly elaborate datasets would be an appropriate universal approach. Such a hierarchy might have five to ten levels—from a bare minimum of descriptive statistics to rich and comprehensive data elements such as those found in certain OECD countries.
6-3. All countries should facilitate the linkage of population-based and administrative health information with other important economic, social, and health service data. Despite logistical and other challenges, linking population survey data to medical, vital, and administrative records, as well as other social and economic data sources, can expand the value of the data for determining population health status and conducting programmatic and policy planning and evaluation (e.g., for assessing levels and changes in disability rates, estimating the effects of insurance coverage on health system expenditures, and providing supplementary information on medical program functions).
6-4. Longitudinal data on the health of older persons should be collected to enable identification of the risk factors, causes, and preventive interventions for disease and disability. Panel (cohort) studies should also include economic, behavioral, and social domains to make it possible to identify those groups and individuals at special risk for illness and their respective consumption of health care resources, and to determine whether health outcomes differ according to variations in health care interventions, programs, and policies.
6-5. Cross-national panel studies should be used to clarify the relationship between health system organization, administration, and financing on the one hand, and health status and outcomes on the other. Data from longitudinal, population-based surveys, linked to administrative records and with com
Page 221
parable questions across countries, are essential in comparing health across countries and attributing changes in health to particular factors. Moreover, comparative work can improve our understanding of how particular diseases and conditions are expressed as disability in a variety of family, social, and residential environments, thus providing insight into which policies and interventions are most efficacious.
ANNEX 6-1
THE ROLE OF SOCIAL INEQUALITY IN THE HEALTH OF ELDERS
In all societies, health and functioning vary according to socioeconomic position. The magnitude of these differences and their causes vary over time both within and among societies. To develop policies that can effectively ameliorate these differences requires an understanding of their causes. Policy responses to socioeconomic differentials in health and functioning will ideally cover a wide range of determinants, including medical care and social services. There are likely to be socioeconomic differences in the provision of, access to, and response to these services.
Social inequalities in health affect older as well as younger people. Annex Figure 6-1 shows mortality by employment grade among British civil servants who were part of the first Whitehall study (Marmot and Shipley, 1996). The figure shows clearly that mortality rates follow a social gradient. The implication for monitoring and for policy is that this is not a clear case of poor health among those who are materially deprived and better health for everyone else; the social gradient in health runs the social gamut from top to bottom. While Annex Figure 6-1 is confined to mortality, social inequalities in morbidity loom large among the elderly, and the implications for policy are perhaps even more challenging here. A particular problem in many industrialized countries is the large numbers of elderly women living alone and hampered by disability. Their situation is worsened by factors related to social position, with implications discussed below.
Annex Figure 6-1 also shows that the relative difference in mortality from top to bottom is less at older than at younger ages. This raises two further issues: the appropriate measure of disease burden and the appropriate measure of social classification. Although the relative difference in mortality may be less at older ages, the absolute difference is greater because overall mortality rates are higher. Although relative differences are usually taken as a guide to the strength of causal factors, absolute differences are a better indicator of the social importance of the total burden of disease and suffering.
Page 222
ANNEX FIGURE 6-1 Relative mortality (all causes) by grade of employment, Whitehall men, 25-year follow-up. SOURCE: Marmot and Shipley (1996). 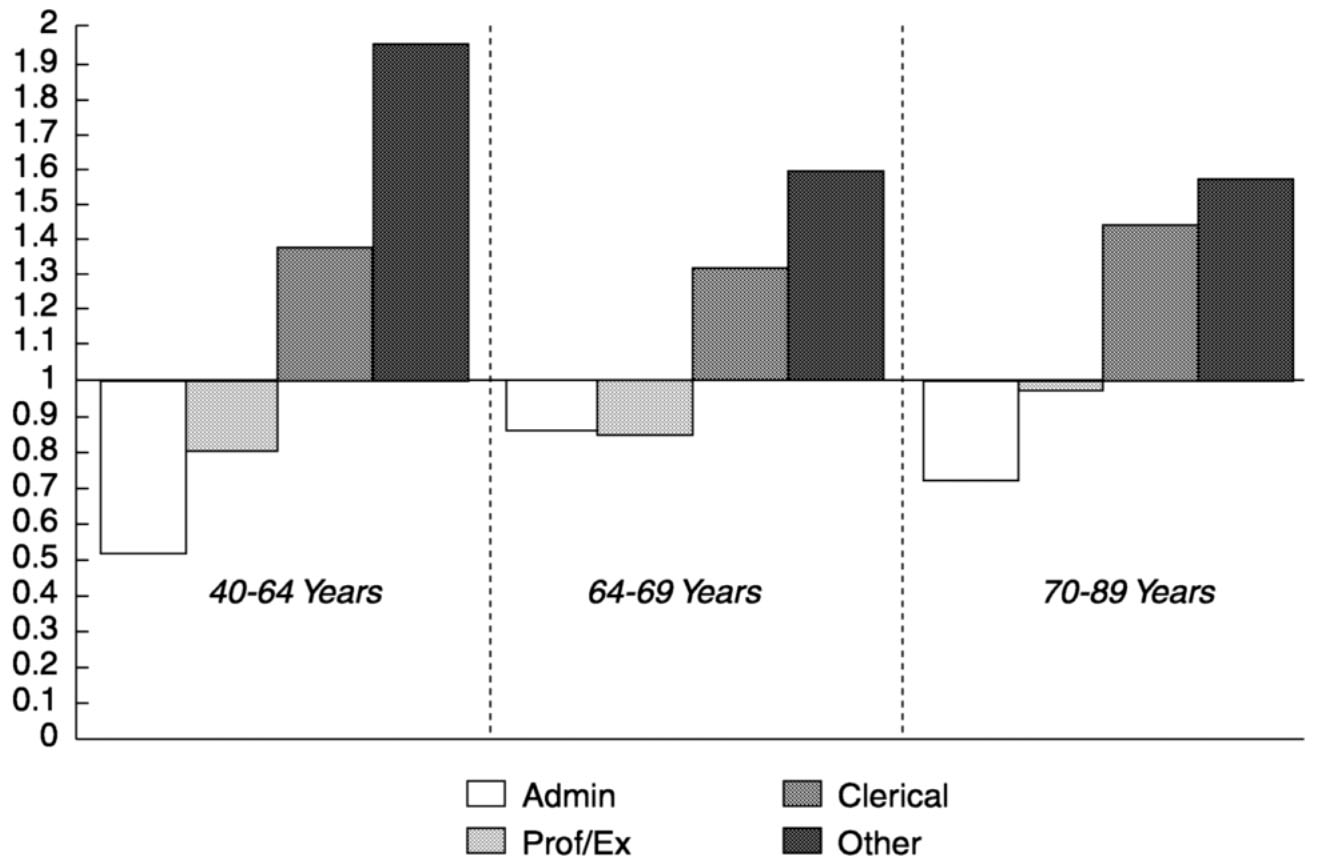
~ enlarge ~
Classification of Socioeconomic Position
Some countries have had a long tradition of measuring socioeconomic position. The theoretical basis for the various measures that have been used is sometimes explicit, more often implicit, and sometimes nonexistent. Measures based on education, income, occupation, or some combination of these are commonplace and often atheoretical. It has been argued that a sounder theoretical basis for socioeconomic classification would yield better understanding of the determinants involved. One approach to this end is to conceive of three different modes of social stratification: one based on degree of material deprivation, one based on social power relations, and one based on general social standing (Bartley and Marmot, 2000).
Measures of material deprivation are appropriate for assessing health differences among those living under conditions of absolute poverty. Such measures are less appropriate where health follows a social gradient, such as in the Whitehall studies (Marmot and Shipley, 1996; Marmot et al., 1991). In such cases there are clear social inequalities in health among people who are not materially deprived. Other concepts must therefore come into play. A second approach that does potentially relate
Page 223
to the whole social gradient is based on power relations in the workplace. Occupations are defined in terms of power and autonomy, a perspective that has its origins in the Marxist concept of class. This approach is the basis for the Eriksson-Goldthorpe scheme, which in turn provided the framework for the new British socioeconomic classification that will be used nationally for the 2001 census. A third approach, that of general social standing, has features in common with Weber's concept of status, based on patterns of consumption and lifestyle. The status group shares the same level of prestige or esteem and, in addition to common forms of consumption and lifestyle, limits its interactions with members of other groups.
It is impossible to give a blanket prescription for the most appropriate measures of socioeconomic position in different cultures. As measures are developed and applied, it would be valuable to attempt to relate them to theoretical concepts such as the three sketched above.
A measure that is appropriate for social classification among people of working age may be less appropriate for those beyond working age. In many countries, occupation is used as a basis for social classification. There is ample justification for this approach in that work is central to peoples' lives (Marmot and Feeney, 1996). Occupation is a major determinant of income, which in turn affects life chances. Also, the work career is an important part of socialization and achievement of social identity outside the family. It offers opportunities for both fulfillment and frustration of life's goals. Self-esteem, social approval, personal attitudes, and behavioral patterns are all influenced by occupational level. Finally, occupation itself and conditions in the workplace may be important determinants of social inequalities in health.
The degree to which occupation continues to provide a reliable indicator of these four elements in people beyond working age will vary. Additional methods of social classification will be needed. This will especially be the case for older women, particularly those single, widowed, or divorced. Other socioeconomic measures that have been used include education; income; housing tenure; characteristics of area of residence; and, in Britain, household access to a car. The issue of appropriate classification bears on the question of why social inequalities in health may be of lesser magnitude in women than in men. In the past, the social status of married women was better defined by their husband's occupation than by their own. While this situation may still obtain in some circumstances and populations, it is being challenged by dramatic social changes (Bartley et al., 1999). Close attention must be paid to the most appropriate measures that will allow comparison of social inequalities in health within and between genders.
Page 224
Data Needs for Understanding Determinants of Social Inequalities in Health and Well-Being
Any feature of social or personal life, of biology, and of services may influence social inequalities in health. At the request of the World Health Organization, the International Center for Health and Society at University College London organized research findings on the social determinants of health under 10 headings (Wilkinson and Marmot, 1998).
-
Social gradient through the life course
-
Stress
-
Early life
-
Social exclusion
-
Work
-
Unemployment
-
Social support
-
Addiction
-
Food
-
Transport
While these categories were intended as a guide to policy makers, they may also serve as a template for research (Marmot and Wilkinson, 1999). One area that does not appear obvious from this list is the quality of housing and the physical and social environment of neighborhoods. These may be thought of as falling under social exclusion, but, as with health itself, their quality is likely to follow a social gradient. A fuller understanding of the appropriate determinants of socioeconomic differences in health and functioning generally requires longitudinal, representative population surveys. Such surveys are essential for establishing causal associations and assessing the magnitude of causes operating in all directions. In other words, longitudinal data are important for determining the degree to which levels of health and functioning determine social and economic position, as well as for assessing the magnitude and nature of the social determinants of health.
A Policy Response: The British Independent Inquiry into Inequalities in Health
In the late 1970s, Britain took the lead internationally in marshalling the evidence on inequalities in health with a government-sponsored inquiry that became known as the Black Report (Black et al., 1988). The Black Report stimulated research on this subject in Britain and internationally, but had little detectable effect on policy. In 1997, the new Labor
Page 225
government in Britain set up an independent inquiry into inequalities in health under the chairmanship of a former chief medical officer, Sir Donald Acheson (Acheson, 1998). The Acheson Inquiry summarized the evidence on the determinants of social inequalities in health and made 39 recommendations. Importantly, these recommendations were organized by stages of the life course to focus on elders as well as other age groups. The government is currently in the process of acting on these recommendations.
ANNEX 6-2
COMMONLY USED MEASURES OF HEALTH STATUS
The measures of health status commonly used for survey questionnaires and administrative data collection can be grouped into seven categories: clinical symptoms, signs, and syndromes; morbidity, or discretely defined medical conditions; self-rated health; functional status and disability; physiological and pathological measures; mortality data and derived measures; and aging and mental illness. The measures used in each of these categories are reviewed in turn below.
Symptoms, Signs, and Syndromes
Illness-related observations and perceptions are by clinical definition called symptoms, signs, or syndromes.
Symptoms are bodily perceptions that people interpret as being abnormal. Many types of symptoms exist, such as knee pain, headache, fatigue, itching skin, decreasing movement of a joint, sleeplessness, or a depressed mood. These are by nature subjective and may result in differing individual interpretations and subsequent behaviors. For example, one person may seek medical attention for a given symptom, while another may not. Symptoms are particularly common among older persons, and because of this and the frequent lack of objective confirmatory evidence, they make medical diagnosis among elders complex and challenging. Knowing the prevalence rates for important symptoms may assist in understanding the demand for medical care. Symptoms may or may not be harbingers of important underlying medical problems, but substantial resources are often spent in further diagnosis and treatment. Cross-cultural studies of symptoms have been conducted to evaluate differences and similarities in implications for health care provision in such areas as jaw arthritis (Suvinen et al., 1997) and tooth pain (Moore et al., 1998).
Signs are objectively detectable evidence of an abnormality that may be seen both by the individual and the health care professional. Examples include skin rashes, warmth or redness of a body part to the touch, au-
Page 226
dible wheezing sounds, and inappropriate behaviors in a particular social setting. Signs are also very common among older persons. As with symptoms, they may or may not be indicative of a serious underlying medical problem and may or may not lead to seeking medical care.
When characteristic patterns or clusters or signs and symptoms occur in an individual, they may be called a syndrome. An example is a cold or influenza, with which there is a characteristic pattern of cough and running nose, headache, fever, muscle aches, and weakness. In general, syndromes are common but do not always imply a particular underlying disease; for example, in a few instances, the “flu syndrome” might actually reflect tuberculosis or an immune deficiency. Most important, syndromes, like signs and symptoms, represent a significant factor in medical care. Most “flu syndromes” are caused by viral infections and lead to high utilization of medical services. Thus providing data on the frequency of these syndromes in both geographic and patient populations becomes essential for the formulation of health care policies. Knowing their occurrence rates and demands on health care resources across cultures and nations can assist in understanding approaches to their efficient management.
Morbidity, or Discretely Defined Medical Conditions
The term “morbidity” in the present context refers to the named medical conditions that health professionals, administrators, and patients and their families use to define and communicate health information. Most morbid conditions, such as diabetes mellitus, stroke, lung cancer, and myocardial infarction (heart attack), have consensual definitions that apply in most instances. However, there can be important variations in disease vocabulary and usage within a language group or country, in addition to important international variations. The result is less precision and accuracy of information obtained from medical records, and the attendant need to perform standardized relabeling (coding) of diagnostic designations for clinical and administrative purposes. While there can be variation in the extent and severity of any clinical condition, disease names provide considerable information on the biological and clinical effects of a particular condition within both individuals and populations, including the average extent of bodily pathology, usual treatment patterns, and prognosis. Clinical care resource consumption can be inferred from a disease name within a given country and health care system. Despite the current limitations of morbidity designations and their classification, then, familiarity with disease names and taxonomy is critical for deriving and quantifying information for policy, research, and administrative purposes.
Page 227
In addition, accurate, consensually defined disease names frequently form the basis for assessment of clinical evidence, development of practice guidelines, and quality assurance activities (Grimshaw and Russell, 1993; Muir Gray, 1997) for both national and international applications.
The policy relevance of morbidity data for older persons is clear. The development, maintenance, and evaluation of programs that provide resources for the prevention, treatment, or rehabilitation of various diseases require detailed knowledge of the occurrence, severity, and functional impact of those conditions. Such information can often be acquired from health care data, and its acquisition is becoming easier as a result of computerization of clinical encounter records in both ambulatory and institutional settings. However, obtaining a population view of morbidity occurrence may require population sample surveys, since health system coverage may not coincide with geographic regions and applies only to actual users. Population surveys can add this critical perspective, but information obtained from older lay persons in this manner may be incomplete or only partially valid. Some persons may not fully understand or be able to name their own conditions, and some conditions may not have been clinically evaluated. For example, adult-onset, non-insulindependent diabetes remains undetected in at least a third of older Americans. As a result, morbidity rates should be acquired from combined population and institutional sources for maximum validity and policy value.
Older persons often have multiple medical conditions, any of which may alter the nature of the others. Thus comparing the diagnosis, treatment, or outcomes of a particular condition, either within a country or region or cross-nationally, often requires adjustment for other diseases and conditions, or “comorbidity.” For example, the presence of comorbid conditions in addition to the disease under consideration can affect quality-of-life scale scores (Xuan et al., 1999), promote the progression of disability (Fried et al., 1999), enhance prediction of hospital lengths of stay (Roe et al., 1998), and generally alter health outcomes after hospitalization (Elixhauser et al., 1998). Comorbidity scales can be applied both to population survey data and to health care administrative datasets (Katz et al., 1996).
The universal approach to organizing morbidity and clinical diagnoses into an internationally acceptable taxonomy is the International Classification of Diseases and Conditions (ICD). The ICD, currently in its 10th edition, is promulgated by the World Health Organization (WHO). It contains several thousand medical conditions and rubrics and is intended to reflect both the complexity of and progress in understanding health and disease. The ICD has enjoyed application in all Western-style health systems, having been adapted and translated for many general
Page 228
applications. However, while the ICD is critical for analyzing community disease information, some limitations should be noted:
-
The ICD is a mix of anatomy, physiology, disease behavior, and causation that can only reflect the existing state of disease understanding.
-
Some types of clinical information are not available in disease names, such as individual functional status (see below) or the physiological severity of a condition.
-
As noted above, there is little ability to deal with the multiple conditions that frequently occur among older persons (comorbidity) and how these conditions affect the disease of interest.
-
Rubrics often do not map easily onto other taxonomic systems.
-
Because of scientific uncertainty, partial understanding of the nature of many diseases, and the growing relationship between diagnostic rubrics and health system reimbursement, the ICD often reflects political, economic, and intellectual controversy.
-
The ICD does not deal easily with the preventive, legal, and administrative aspects of clinical practice.
Because of these and other limitations, alternative and ancillary disease nomenclature and taxonomic systems have been developed. One example is the Systematized Nomenclature of Medicine (SNOMED) system (Lussier et al., 1998), which uses a multiaxial approach to the designation of a given condition. Separate information is provided for different domains, such as anatomical locale, physiological impact, and putative causes of the condition. Several other taxonomies have been developed as well, such as the ICD-O, a detailed catalogue of cancer types, severity, and disease extent; E-Codes, an exhaustive coding system for environmental exposures associated with human disease; and N-Coding, a detailed taxonomy of bodily injuries.
Collaborative international studies of morbidity occurrence have been conducted to assist program planning for health services. An important example is the WHO program on Multinational Monitoring of Trends and Determinants in Cardiovascular Disease (MONICA). Coronary disease is the most common cause of death among elders in most countries. Through MONICA, coronary disease events have been monitored regionally in 16 European countries and Australia, Canada, China, New Zealand, and the United States since 1981. In a recent large-scale cross-national analysis (Tunstall-Pedoe et al., 2000), incremental enhancements to the quality of coronary care in various geographic areas were correlated with short-term heart attack survival (the “case-fatality ratio”). This ecological analysis, done separately for men and women, produced evidence that greater improvement in coronary care (a higher “treatment score”) is associated with a larger decline in the case-fatality ratio, indicating im-
Page 229
proved survivorship. While further assessment is needed, this type of cross-national study supports the value of investing in improved coronary care facilities across a broad range of approaches to such care.
Self-Rated Health
Items measuring self-rated health are frequently found in surveys of many kinds. An example is a question asking respondents to characterize their overall state of health using categories such as excellent, good, fair, or poor. Such evaluations may or may not correspond to that which would be provided by a physician.
The person-centeredness of such questions make them extremely useful for a number of purposes in health research. First, self-related health is used in measures of health, psychological well-being, and health-related quality of life, concepts that are usually ill-defined but nearly always include some element of physical well-being and functioning. These are matters for which the individual is certainly the best source of information. Second, self-rated health can be used as a screening tool to identify high-risk groups and risk factors; poor self-rated health is consistently associated with low socioeconomic status and high levels of other illness risk factors in both national and international studies. Third, self-rated health can be used as an outcome in the evaluation of medical interventions as an important addition to the usual mortality and morbidity outcomes; treatments with similar effects on length of life may have different implications with respect to the quality of those years. Fourth, self-rated health can be used as a predictor of illness behavior, retirement, or the long-term use of medication and other health care services; studies of retirement decision making have often included this measure as the only indicator of health status (Bjorner et al., 1996). Finally, the most compelling reason for including self-rated health on surveys is its apparent predictive power with respect to mortality. In 1982, a Canadian study showed that self-ratings of health given by a representative sample of elderly residents of Manitoba in 1971 were better predictors of mortality by 1977 than either their medical records or self-reported conditions. A 1997 review found 27 published studies of representative samples from 13 countries reporting analyses of self-rated health and mortality; in 23 of these studies, self-rated health was a significant predictor of mortality for males and/or females even after other measures of health status had been taken into account (Idler and Benyamini, 1997). Another review conducted 2 years later found 19 studies that included an additional 4 countries; only 2 of these studies reporting no significant association between self-rated health and mortality risk (Benyamini and Idler, 1999).
The number of such studies and the consistency of their findings is
Page 230
impressive for several reasons. The very appearance of so many studies in such a short time (a span of 17 years, with most appearing after 1990) is noteworthy in itself, especially considering that the data reported are from longitudinal studies, many of which had been planned and were begun years earlier. The implication is that some question eliciting a global evaluation of health was used in the interviews for these studies because it had been deemed useful for some other purpose and subsequently was found to be related to mortality risk in secondary analyses. This large body of findings also presents two paradoxes. One is that the interviews on which the analyses were based were conducted in the language of the respondents, and few if any attempts were made to standardize the questions or the response categories. A second is that the countries involved vary a great deal in the proportion of respondents that evaluate their health in the poorest category (“poor,” “bad,” “extremely bad,” “very sick,” “worse health compared with others,” or “not healthy”). This variation renders the near uniformity of the findings all the more surprising, since cultural as well as linguistic meanings of health differ greatly from one country to another, as do the more objective morbidity and mortality rates. Indeed in many of the studies, poor self-related health predicts mortality with effect sizes and significance levels similar to those associated with smoking. These findings underscore, as few others could, the validity of lay perspectives on health and the usefulness of a holistic approach to defining health. Respondents to surveys are supplying their own meanings of health, which may include some or all of WHO's broad definition of human health (a “complete state of physical, mental, and social well-being”). Self-ratings of health thus provide a simple, direct, and economical way of capturing perceptions of health using criteria that are as broad and inclusive as the responding individual wants to make them.
Functional Status and Disability
The functional characterization of older persons along physical, cognitive, and social dimensions is extremely important in directing health policy. Functional disability is uniquely common among older persons, and there is substantial potential for its prevention. Age-related increases in physical and cognitive disability are often a direct result of chronic medical conditions such as heart disease, stroke, vascular disease, arthritis, Parkinson's disease, cancers, and dementia. Yet they are also related to social and environmental factors. Decreases in social interaction and engagement can be a result of both physical and cognitive changes, as well as a loss of friends and family to mortality and migration and a decline in social roles, including productive work. Decreases in social
Page 231
engagement can in turn worsen the outcomes of physical disability and cognitive impairment.
Physical Disability
Physical disability results in a decreased ability to perform roles essential to remaining independent and productive and maintaining a home. It is estimated that in the United States, more than 20 percent of older adults have limitations in their ability to perform major daily activities as a result of underlying disease (Manton et al., 1997). The aspects of physical disability most frequently considered are the ability to perform tasks essential to living independently in the home (e.g., meal preparation or bill paying) or to self-care (e.g., bathing and dressing). However, a broad spectrum of more demanding activities, such as paid work, voluntary activities, and recreation, are also affected.
Disability and dependency rates among older adults, as well as use of long-term care, vary substantially among regions and cultures and by socioeconomic status and social structure. Understanding rates of disability within and among countries and regions, as well as the health, health care, social, and economic factors that may affect these rates, helps provide a basis for planning for future chronic care needs. Moreover, disabled older adults require the most intensive and costly general health care and community services. The size of the disabled population, therefore, has a tremendous impact on current and overall future health care needs.
As noted, there is increasing evidence of the potential for preventing disability. Such measures include the primary prevention of disabling diseases and tertiary prevention to minimize their progression and impact. It may also be possible to decrease disability through social approaches (e.g., altering the social factors that affect function) and through environmental modifications. Moreover, newly developed methods can be used to screen for individuals at risk of disability or its progression, so that appropriate interventions can be undertaken. It may be noted that the potential for all of these various approaches to reduce disability argues for continuous national tracking of disability levels through representative surveys and related methods.
Cognitive Impairment
The loss of cognitive function increases with age in all populations studied. This cognitive loss, in turn, leads to important clinical and functional consequences termed dementia. In the majority of industrialized countries, the most important dementing illness is Alzheimer's disease.
Page 232
As with physical function, rates of dementia prevalence vary among communities, cultures, and nations (Jorm and Jolley, 1998). Rates among those aged 85 and older in industrialized countries may be as high as 50 percent. A key factor associated with dementia is a loss of independence in one or more aspects of everyday function. This association between functional impairment and subsequent dementia suggests that cognitive impairment mediates selected age-related transitions in physical function (Carlson et al., 1999).
Social Function
Social function denotes the extent of individual engagement with family, friends, and society. Individual social networks vary in the type, quality, and frequency of interactions with others. Engagement with society takes many forms, including participation in social, religious and political institutions and paid and volunteer work. Such engagement frequently provides a sense of productivity and of making a contribution to society. Ongoing participation in structured activity, such as paid or volunteer work or managing a household (Glass et al., 1999; Musick et al., 1999), has been shown to decrease the risk of mortality. Positive social networks have also been associated with decreased risk of disability with regard to basic self-care activities (activities of daily living), as well as other health outcomes. Conversely, social disengagement has been shown to predict cognitive decline and disability (Bassuk et al., 1998). However, it should be acknowledged that a better health status may also allow more active and productive social function.
Assessment of Functional Status
An individual's ability or limitation in performing the tasks of daily life is commonly assessed through self-reports or through functional performance testing in the home or clinic. Functional measures can be used to describe specific limitations in discrete areas, such as using a spoon or remembering numbers. Other measures can be used to describe the cumulative impact on an individual of one or more chronic conditions, cognitive impairments, and physiological changes associated with aging, as well as social, environmental, and psychological modifiers of these conditions. Thus, functional status and disability measures serve both to assess the net impact of disease and aging on the individual and to express the ability of the individual to care for him- or herself and to manage a household.
Disability measures essentially describe a syndrome rather than one or more specific diseases; for example, someone may have difficulty walk
Page 233
ing across a room because of arthritis, a neurological condition, cardiopulmonary disease, or many other factors. While chronic diseases have an important impact on functional levels, not all persons with a particular disease have measurable functional decrements, and not all will become disabled from their disease.
Physical function typically is assessed with reference to activities in which physical movement predominates, such as basic self-care activities (including bathing, dressing, and toileting); more complex, instrumental activities (including cooking, shopping, and recreational exercise); and mobility (moving from one place to another) and other basic physical movements (including reaching, kneeling, and fine hand movements). It should be noted here that in some instances, these measures may be heavily influenced by living environments and social role expectations.
Cognitive function is usually assessed through special cognitive-psychological testing of basic cognitive processes performed by the human brain, such as memory, calculation, visuo-spatial abilities, and reasoning, although impairment may sometimes be inferred from declines in the performance of instrumental activities. Measurement of a decline in particular cognitive functions generally cannot be used to diagnose a specific disease and must be accompanied by thorough clinical evaluation. Formal psychological testing also is used to assist in determining mental illness.
Finally, assessment of social function is usually performed by querying individuals, families, and others to determine the nature of social networks—type; quality, positive or negative; and frequency of interaction. Types of social engagement (frequency of participating in social or productive activities) are also determined.
Functional status measures are increasingly collected in clinical practice. In contrast with information on morbidity (diseases) encountered in the health care system, however, the information on such measures is often not coded or easily retrieved from administrative datasets or clinical records. Sometimes, functional status can be inferred from various diagnostic rubrics (e.g., dementia) or from clinical interventions (e.g., physical rehabilitation), but drawing such inferences is challenging. An increasing number of population surveys with health and economic goals contain functional status measures, often in longitudinal perspective, and offer considerable analytical potential for policy applications. Some recent examples from various countries are shown in Annex Box 6-1.
There are numerous measures of functional status, and while they can be used in cross-national research for understanding the causes of various levels and changes among the elders of many nations, the number of comparisons could be large. One way to deal with this problem is to apply summary measures of several individual functional attributes, us-
Page 234
ANNEX BOX6-1Examples of National and Regional Surveys of Older Populations Using Functional Status MeasuresAustralia: Australian Longitudinal Study of Ageing Bangladesh: Matlab Health and Socioeconomic Survey Europe: European Longitudinal Study on Aging (11-county study) Indonesia: Health and Aging Dynamics in a Low-Income Population Israel: Cross-Sectional and Longitudinal Aging Study United States: Survey of Asset and Health Dynamics Among the Oldest Old, Established Populations for Epidemiologic Studies of the Elderly, Longitudinal Study of Aging and Supplement on Aging II, National Long-Term Care Survey, Women's Health and Aging Study, Cardiovascular Health Study International Comparisons: Luxembourg Income Study (data from more than 25 countries for 1 or more years, including disability status of head of household and spouse) |
ing survivorship methods or “health expectancy measures” (Robine et al., 1999) to create a disability profile employing the time to onset of disability among the population of each age in the context of general survivorship. An example of the application of this approach is shown in schematic form in Annex Figure 6-2. Age-specific prevalence rates provide important information and have been determined for representative population samples in many countries. Annex Figure 6-3 shows gender- and age-specific prevalence rates for severe disability in four countries. Interestingly, there are clear differences among countries in trends by age that require further exploration. 1 Such cross-national differences offer special opportunities to explore environmental, cultural, and biological explanations. Given that analyses of declines in age-specific levels of physical disability (Freedman and Martin, 1998; Manton et al., 1993; Crimmins et al., 1997) do not go far in explaining such trends, there is a clear need for international contrasts to provide and test causal hypotheses. Also of interest is the extent to which the more recent epidemiological transition
1Documenting and exploring these differences has been the goal of REVES (International Network on Health Expectancy and the Disability Process), a group of international researchers that has been meeting regularly since 1989. Estimates of healthy life expectancy are now available for at least 49 countries worldwide, and time series exist for 15 of these nations (Robine, 1999). To date, however, harmonization of concepts among countries has proven elusive, and differences in definitions and methodologies among countries preclude strict cross-national comparison.
Page 235
SOURCE: World Health Organization (1984). Reprinted with permission. 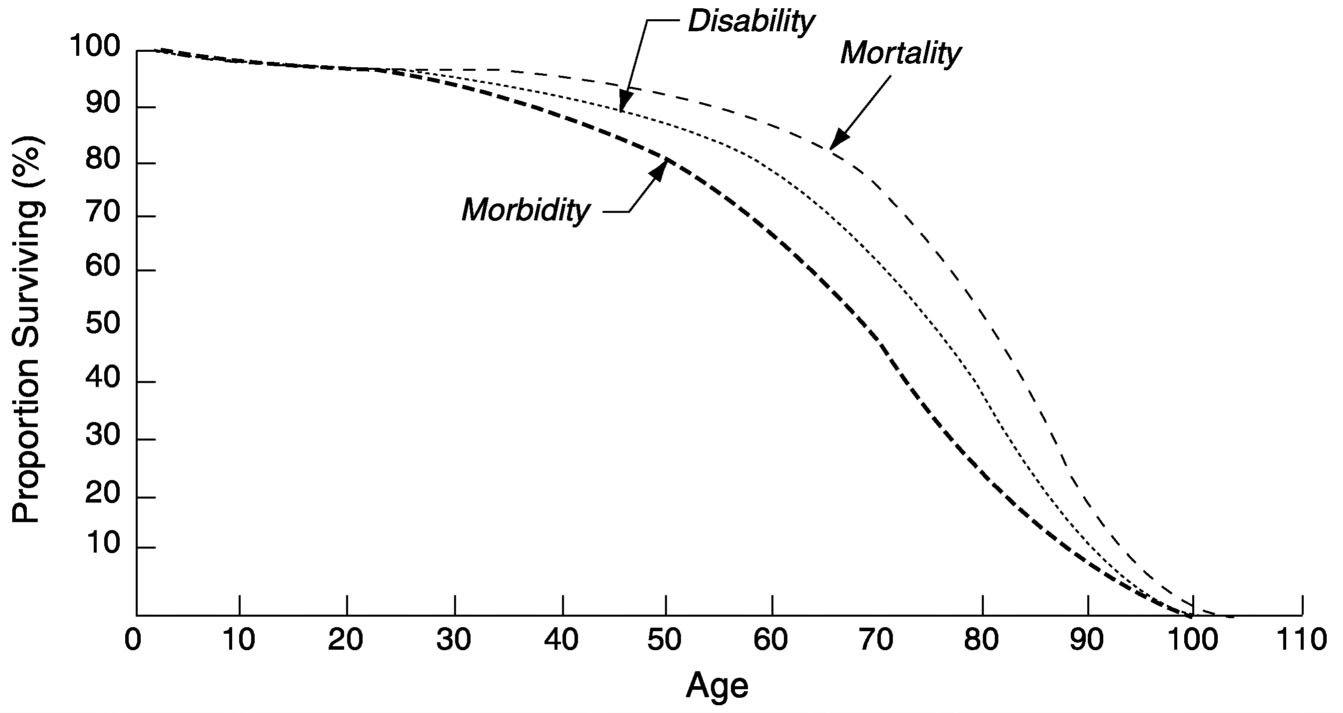
~ enlarge ~
ANNEX FIGURE 6-2 A general model of health status and change (observed mortality and hypothetical morbidity and disability survival curves for U.S. females in 1980).
in poorer countries will lead to different patterns of disability change as mortality decline proceeds.
Physiological and Pathological Measures
For at least 150 years, the acquisition of bodily materials and the measurement of human physiological functions have been part of medical practice for purposes of diagnosis and assessment of the efficacy of treatment. Rapid advances in such measures in clinical practice have been limited only by the availability of the necessary resources and the ability of patients to accept the diagnostic burden. In the Western tertiary care setting, many technologically complex determinations are being performed, including complex metabolic investigations, noninvasive imaging of body organs, and assessment of complex organ functions (e.g., of the brain and heart). Genetic determinations are also becoming an increasingly important part of clinical practice. More traditional and routine blood and urine evaluations are extremely common as well, and literally hundreds of specific determinations are available for evaluating disease processes.
Several important policy questions relevant to older persons stem from these laboratory assessments. Does the increasing availability of
Page 236
ANNEX FIGURE 6-3 Trends in the prevalence of severe disability among the elderly in four countries. NOTES: Australia: severe handicap, households and institutions; Canada: HALS survey, households and institutions, severe disability; France: households, confined to bed; Germany: households, microcensus, severe disability. SOURCE: Jacobzone et al. (1998). 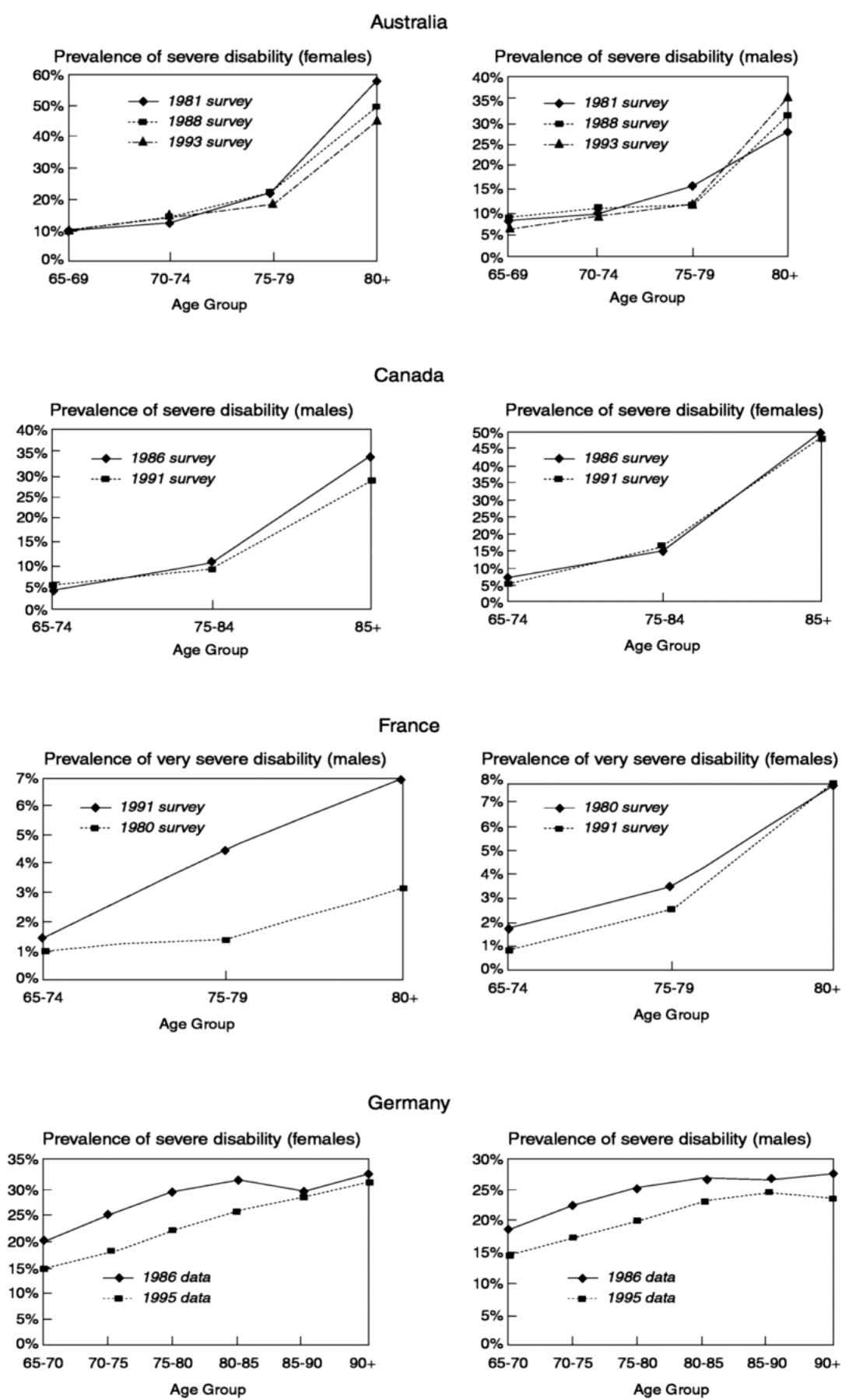
~ enlarge ~
Page 237
these sophisticated measures contribute to improved health outcomes among older persons? How should these complex and expensive tests be applied more efficiently both geographically and to individual patients? Does their use lead to secondary medical care activities that improve health status? Do long-term adverse health effects occur because of improper medical decision making based on these tests? Several of these questions can be addressed in cross-national investigations since there is considerable regional and national variation in access to and funding and application of such procedures, enabling useful and important outcome studies. However, cross-national evaluation of the outcomes of various medical tests and procedures requires assurance that these tests and procedures have similar properties and interpretation to allow comparative studies.
An additional and important issue is the application of laboratory testing procedures to surveys of geographically defined older populations. Such application has generally lagged behind clinical use because of difficulties in test portability for community studies, lesser acceptance of such testing among those without overt clinical conditions, and impeded access to persons having substantial functional impairment or residing within an institutional setting. Several approaches to this problem have been devised, including inviting survey participants to regional clinical testing centers; creating more acceptable portable testing and specimen-collection devices; and limiting the testing in various ways, for example, to tests for risk factors for important chronic conditions of older persons (e.g., blood pressure or blood cholesterol or sugar levels), use of simple physical testing devices (e.g., those for respiratory function or muscle strength), physical performance tests that reflect common functions (e.g., self-care activities of daily living), and tests for blood determinants that reflect more complex constructs (e.g., levels of environmental contaminants or genetic determinations). 2 It may be noted that new testing procedures for population health assessments are continually being evaluated and should always be considered.
Mortality Data andDerived Measures
Mortality data, despite certain weaknesses in accuracy and as measures of population health, have been widely applied to guide health policy, in part because of their universal availability from industrialized countries. As noted in Chapter 2, recent advances in both the socioeco
2For two recent discussions of new testing procedures and their relevance to populationbased studies, see United States Agency for International Development (2000) and National Research Council (2001).
Page 238
nomic and health spheres, along with changes in individual and group lifestyles, have ensured a notable increase in life expectancy among the elderly. A 60-year old European, North American, or Japanese woman may expect to live another 20-25 years and her male peer another 18-20 years. As recently as 20 years ago, men and women of the same age lived 2 to 4 years less. Much of this recent gain in survivorship has been due to declines in mortality from heart disease. It is expected that survivorship among older persons, particularly the oldest old, will continue to increase, and this increase may trigger higher health and welfare costs. Costs could increase in particular for the prevention and care of chronic degenerative diseases, for assistance for the disabled, and for care associated with other disabling diseases that afflict the oldest old. These potential changes argue for the collection of data needed to estimate trends in future total mortality and specific diseases.
Despite generally decreasing mortality rates, there are disparities among various groups within industrialized countries; mortality rates are lower among women, married persons, and those of higher social class. There are also substantial regional and national variations, necessitating the collection of region-specific health data and the formulation of health and social policies that allow flexibility in managing this variation. To study elderly mortality and survival patterns, data are needed for total mortality (deaths from all causes) and for particular causes, classified according to specific features; data are also needed for characterizing the population at risk of dying.
Mortality data typically come from death certificates of national vital record systems. Currently, however, there is substantial variation in the quality of the data, and information may be missing for certain geographic jurisdictions, impeding understanding of mortality trends for policy purposes. Just how this variation in quality affects analytical studies depends on the goals and policy questions involved. Annex Table 6-1 summarizes options for comparing mortality rates among various older populations, either cross-sectionally or longitudinally. Options are shown for both group or collective mortality findings and individually followed mortality as part of the lifetime history of health and disease.
Availability of General Mortality Information
Mortality data by gender and age have been available for 48 European and non-European countries since World War II. Only a few countries possess longer time series. Some central statistical offices supply data that are also classified according to year of birth, thus facilitating the study of mortality for different cohorts. Usually, deaths and the relative population exposed to the risk of dying are classified for individual ages
Page 239
|
Type of Data |
Approaches |
Data Needs |
Measures and Methods |
|
Collective |
Cross-sectional |
Deaths by age, gender, and calendar year; population at risk Deaths by cause and year, population at risk, and competing events |
Rates by age, age-standardized cancer ratio, proportional mortality ratio, standardized mortality rates, probability, life table, life table by cause |
|
Longitudinal (by cohort) |
Deaths by age and year of birth, population at risk |
Rates by age and cohort, probability and life tables by cohort |
|
|
Individual |
Longitudinal biographies |
Death records, data on individual survival, linkage data |
Survival analyses, Kaplan-Meier models, Cox models, etc. |
|
Follow-up data |
Analysis of life histories, biographies (hazard models) |
through age 99 and as a single group for those aged 100 and over, although most countries have recently made efforts to publish data for individual ages for the latter segment of the population as well.
Kannisto (1994) has constructed a database that comprises a mortality series for persons aged 80 and over for a set of industrialized countries that publish such data annually. The data have been subjected to a number of tests of their plausibility and internal consistency. On the basis of these tests, countries have been classified into four quality categories: those with good-quality data (Czechoslovakia, Denmark, England and Wales, Finland, France, Germany, Hungary, Iceland, Italy, Japan, Luxembourg, the Netherlands, Norway, Scotland, Sweden, and Switzerland); those with acceptable-quality data (Australia, New Zealand-non Maori, and Portugal); those with acceptable data under certain conditions (Estonia, Ireland, Latvia, Poland, and Spain); and those whose data should be used with caution (Canada, New Zealand-Maori, and the United States).
Page 240
The database was constructed from data on deaths arranged into cohort survival histories. Once mortality measures by age are available, life tables can be constructed and analyses of elderly survival performed. Amalgamation of data on life expectancy, diseases, and disabilities will make it possible to derive measures that incorporate healthy and disabled life expectancy.
Quality of Vital Records
It is well known that mortality estimates at old ages may be hampered by various problems (Coale and Kisker, 1986, 1990; Kannisto, 1994, 1996; Thatcher et al., 1998). For example, age misreporting is usually found both in death registration and in censuses and other surveys. The most common manifestations of the data quality problem are implausible age-specific mortality fluctuations and abnormally low mortality estimates at older ages (Preston et al., 1997). Two common problems are the tendency to report age in round numbers (the nearest 5 or 0) and age exaggeration among the oldest old. Other problems in the quality of data on occupation, education, and surviving kin have been described.
Causes of Death
While causes of death have been registered throughout the industrialized world dating back to the beginning of the 20th century, it is only recently that certain quality changes have been introduced in standardized registration procedures. Death certificates are the responsibility of medical doctors, according to WHO guidelines. The certificate is divided into two sections. The first lists the diseases leading to death, and the second details other conditions, so-called associated causes, which may have contributed to the death event. In the first section, the doctor must list the direct cause of death, known as the immediate cause; followed by the pathology immediately preceding this, or the intermediate cause; and lastly the originating or initial or main cause. A death certificate may contain indications regarding more than one cause, thus making it possible to trace back the whole process leading to death, at least in theory. Death is taken to be the end result of a chain of diseases, whose advent and development may be linked to other preexisting diseases. Published mortality analyses tend to emphasize the main cause, which, particularly when dealing with the elderly, is often difficult to identify. To shape policies targeted at the prevention and treatment of selected diseases, it would be highly useful to have available all the information contained in the death certificate. Having these data is crucial to identifying certain diseases, such as diabetes, that may not appear among the principal causes
Page 241
on the certificate but play a leading role in mortality levels. Indicators of mortality by multiple causes (Nam, 1990) may also be defined if the necessary data are available.
It should be noted that there are several sources of error in certification of the causes of death. Physician certifiers may make errors in diagnosis, or there may be inadequate clinical information available. Sometimes, ill-defined descriptors of older persons, such as “senility” or “heart attack,” are entered when no specific clinical information is available. There may also be errors in coding of reported death events by vital registrars. However, quality control in this area is increasing, and this source of error is diminishing.
Individual Data and Mortality Differentials
The study of mortality differentials has provided a number of explanatory hypotheses and offered the possibility of moving from description of the differences observed to identification of their root causes. Many studies have involved analyzing mortality differences according to socioeconomic status, usually encompassing cross-sectional analyses of older populations (e.g., Mare, 1990; Martelin, 1995). However, the impact of social status may be cumulative throughout the life course. Mortality at old age can depend on living conditions during childhood, adolescence, and adulthood, and thus a longitudinal approach may be valuable. Such an approach involves a more complete overview of the entire process as it occurred during the individual's lifetime (Sahli et al., 1995). Death is considered the final event in a life history composed of a succession of various passages spanning a variety of situations and experiences, gradually culminating in an illness (or accident) and then death (Caselli et al., 1987). Data from health, census, and other sources are linked to derive a lifetime picture of social, economic, medical, and other influences.
Cross-National Mortality Contrasts
Cross-national comparisons of the mortality of older persons can be instructive. Annex Figure 6-4 shows the probabilities of death for men and women aged 80-99 (the oldest old) in five countries—Sweden, Japan, France, Italy, and Australia—during the last half of the 20th century. In addition to the clear decline over the study interval and the almost universal finding of higher mortality probabilities in men than in women, three observations stand out. One is that gains in survivorship are happening even among the oldest segments of the world's elders. Another is that the relative survivorship gains among women have been greater than those among men. Finally, the dispersion of the gains is greater among
Page 242
SOURCE: Prepared by the panel based on data from the Max Planck Institute for Demographic Research, Rostock, Germany. 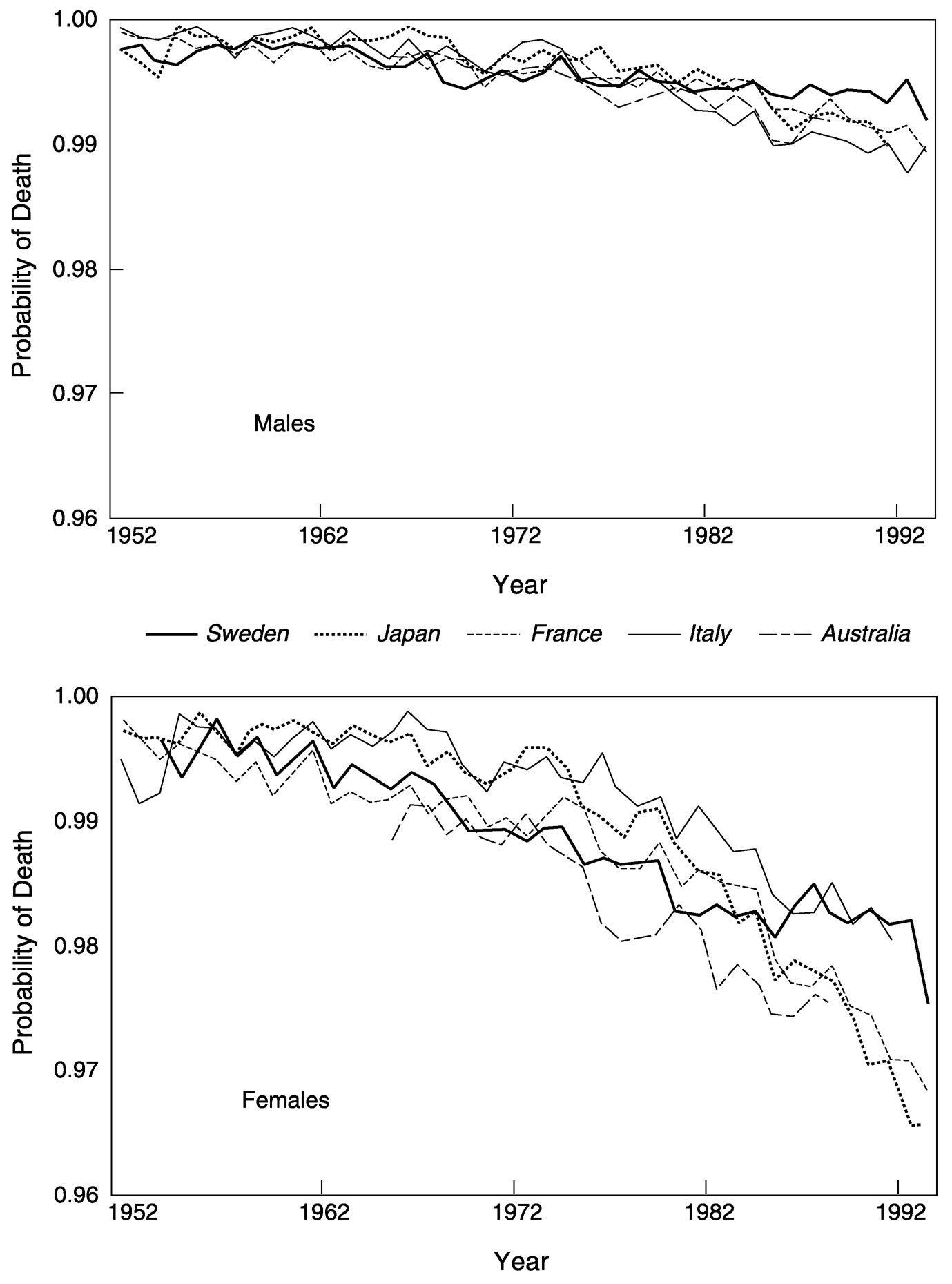
~ enlarge ~
ANNEX FIGURE 6-4 Probability of death at ages 80-99 in five countries: 1952 to 1994.
Page 243
women than among men. The latter two findings should prompt cross-national research into national differences in changing survivorship.
Aging and Mental Illness
Psychiatric disorders are significant contributors to physical, social, and emotional dysfunction and disability among the elderly, but it is only recently that such problems have drawn significant attention (Wells et al., 1989). All of the important mental conditions of young adulthood and middle age, including depression, mania, schizophrenia, personality disorders, addictions (including alcoholism), phobias, anxiety, and panic disorders, occur in older persons. Moreover, with increased survivorship and longevity among older persons, dementia and Alzheimer's disease have become quite common. The dementing illnesses themselves are often accompanied by additional psychiatric symptoms that require medical treatment. These symptoms are among the most important reasons for institutionalization or community-based long-term care. Various approaches to institutionalization of elders with mental and physical disability were discussed earlier in Box 6-1.
A particularly important and common condition of older persons is depression, a disorder that illustrates the difficulties of determining the population burden and health service needs associated with psychiatric illness. Early epidemiological studies of mental illness indicated lower rates of depression among the elderly than among younger population subgroups, but there is much reason to doubt the validity of such estimates. Older people are more reluctant to admit to depressive symptoms than younger persons and are more likely to express their symptoms in somatic terms. Most of the instruments measuring depression in community settings, however, depend substantially on psychological items that elderly persons are less likely to endorse. Prevalence estimates of depression among the elderly can vary as much as 15-fold depending on the definitions used, populations studied, and research approaches (Gurland et al., 1996). An important difficulty in assessing and treating depression among older persons involves their different life circumstances as compared with younger persons. Elders have more physical illness and take more medications, making it more difficult to differentiate depression from other health states. In addition, older persons who suffer decrements in function and who lose spouses and friends experience depressive symptoms that they and health professionals commonly view as part of the aging process itself. Researchers often have difficulty differentiating reactions to the losses of normal aging from depression per se. Depression among the elderly is common in primary care practice, and doctors caring for this population tend to be skeptical of the psychologically
Page 244
oriented epidemiological instruments. New efforts are being made to derive valid measures of depression in elderly populations and to provide more appropriate treatment (Unutzer et al., 1999).
Depression exemplifies the problems of determining the care burden of mental illness among older persons. Among elders, mental conditions are often associated with important medical illnesses, but receive lower priority in clinical diagnosis and treatment. In addition, as noted, many mental problems are mistakenly considered to be part of normal aging and not given appropriate attention, particularly in the primary care setting. Also, administrative and clinical records related to treating mental illness, while sometimes in the mainstream of medical systems, are often kept in separate locations with separate access restrictions. Thus, population rates of mental illness may not be attainable from clinical or administrative records, and the use of population surveys for this purpose should be considered. It is ironic that surveying for mental illness requires a substantial participant burden, as the instruments are often long and detailed. This constraint has limited the number of community- and population-based assessments available for planning and evaluation. Thus it is not surprising that even among industrialized countries, clinical services for the prevention and treatment of mental illness are often lacking because of their costs and competing clinical priorities. There are also substantial differences among cultures in the behavioral manifestations and lay and professional interpretations of mental symptoms and conditions. This variation makes international comparisons particularly hazardous, and necessitates extreme care and documentation of clinical events when conducting such research studies.
REFERENCES
1998 Independent Inquiry into Inequalities in Health Report . London : The Stationery Office .
, and 1998 Aging Research in Europe: Demographic, Social and Behavioral Aspects . Geneva : United Nations Economic Commission for Europe .
1999 A Research Agenda on Ageing for the Twenty-first Century. Draft report of an Expert Consultative Meeting, 1-3 February, Vienna .
, and 2000 Social class and power relations at the workplace. In The Workplace and Cardiovascular Disease, Occupational Medicine: State of the Art Reviews 15(1), P.L. Schnall, K. Belkic, P. Landsbergis, and D. Baker, eds. Philadelphia : Hanley and Belfus .
, , , and 1999 Understanding social variation in cardiovascular risk factors in women and men: The advantage of theoretically based measures. Social Science and Medicine 49: 831-845 .
Page 245
, , and 1998 Depressive symptomatology and incident cognitive decline in an elderly community sample. Archives of Geriatric Psychiatry 55: 1073-1081 .
, and 1999 Community studies reporting association between self-rated health and mortality: Additional studies, 1995 to 1998. Research on Aging 21: 392-401 .
1995 Where are the missing elders? The decline in nursing home use, 1985 and 1995. Health Affairs 18: 146-155 .
, , , , , and 1996 Self-Rated Health: A Useful Concept in Research, Prevention, and Clinical Medicine . Stockholm : Swedish Council for Planning and Coordination of Research .
, , , , and 1988 Inequalities in Health . The Black Report: The Health Divide . London : Penguin Books .
, , , , and 2000 Tracking clinical preventive service use: A comparison of the health plan employer data and information set with the behavioral risk factor surveillance system. Medical Care 38: 187-94 .
, , , , , and 1999 Association between executive attention and physical functional performance in community-dwelling older women. Journals of Gerontology, Series B, Psychological Sciences and Social Sciences 54(5): S262-270 .
, , and 1987 L'apport de la démographie à l'explication de la mortalité différentielle. In L'explication en Sciences Sociales. La Recherche des Causes en Démographie . Chaire Quetelet '87, Institut de Démographie, Louvain-la-Neuve: Université Catholique de Louvain .
, and 1986 Mortality crossover: Reality or bad data? Population Studies 40: 389-401 .
1990 Defects in data on old-age mortality in the United States. Asian and Pacific Population Forum , Spring .
, , and 1997 Further evidence on recent trends in the prevalence and incidence of disability among older Americans from two sources: The LSOA and the NHIS. Journals of Gerontology 52: S59-S71 .
1999 Data Needs for Studying the Health Care System. Paper prepared for the Panel on a Research Agenda and New Data for an Aging World, Committee on Population, National Research Council .
, and 1991 Policies and Strategies to Promote Social Equity in Health . Stockholm : Institute for Futures Studies .
, , , and 1998 Comorbidity measures for use with adminstrative data sets. Medical Care 36: 8-27 .
, and 1998 Understanding trends in functioning among older Americans. American Journal of Public Health 88: 1457-1462 .
, , , and 1999 Association of comorbidity with disability in older women. Journal of Clinical Epidemiology 52: 27-37 .
Page 246
, , , and 1999 Population based study of social and productive activities as predictors of survival among elderly Americans. British Medical Journal 319(7208): 478-483 .
, and 1993 Effect of clinical guidelines on medical practice: A systematic review of rigourous evaluations. Lancet 342(8883): 1317-1321 .
1991 From Asylum to Community . Princeton : Princeton University Press .
, and 2000 An Inventory of Health and Disability-related Surveys in OECD Countries. Paper prepared for the Organization for Economic Co-operation and Development, Paris .
, , and 1996 Epidemiological perspectives on opportunities for treatment of depression. American Journal of Geriatric Psychiatry 4: 7-14 .
1997 Coverage of Health Topics by Surveys in the European Union . EUROSTAT Working Papers, Population and Social Conditions 3/1998/E/No. 10. Luxembourg : Statistical Office of the European Communities .
, and 1997 Self-rated health and mortality: A review of twenty-seven community studies. Journal of Health and Social Behavior 38: 21-27 .
, , , and 1998 The Health of Older Persons in OECD Countries: Is It Improving Fast Enough to Compensate for Population Ageing? Labour Market and Social Policy Occasional Papers 37. Paris : Organization for Economic Co-operation and Development .
, and 1998 The incidence of dementia: A meta-analysis. Neurology 51(3): 728-733 .
, , and 1998 The Heart of Longterm Care . New York : Oxford University Press .
1994 Development of Oldest-Old Mortality, 1950-1990: Evidence from 28 Developed Countries . Monographs on Population Aging 1. Odense, Denmark : Odense University Press .
1996 The Advancing Frontier of Survival: Life Tables for Old Age . Monographs on Population Aging 3. Odense, Denmark : Odense University Press .
, , , , and 1996 Can comorbidity be measured by questionnaire rather than by medical record review? Medical Care 34: 73-94 .
1999 Serum cholesterol in cross-cultural perspective. The Seven Countries Study. Acta Cardiologica 54: 155-158 .
, , and 1998 The SNOMED model: A knowledge source for the controlled terminology of the computerized patient record. Methods of Information in Medicine 37: 161-164 .
, , and 1993 Estimates in the change in chronic disability and institutional incidence and prevalence rates in the U.S. elderly population from the 1982, 1984 and 1989 National Long Term Care Survey. Journal of Gerontology 48: S153-S166 .
1997 Chronic disability trends in elderly United States populations. Proceedings of the National Academy of Sciences, Medical Sciences 94: 2593-2598 .
Page 247
1990 Socio-economic careers and differential mortality among older men in the United States. In Measurement and Analysis of Mortality , J. Vallin, S. D'Souza, and A. Palloni, eds. Oxford : Clarendon Press .
, , , , , , , , and 1991 Health inequalities among British civil servants: The Whitehall II study. Lancet 337: 1387-1393 .
, and 1996 Work and health: Implications for individuals and society. In Health and Social Organisation , D. Blane, E. Brunner, and R.G. Wilkinson, eds. London : Routledge .
, and 1996 Do socioeconomic differences in mortality persist after retirement? 25 year follow-up of civil servants from the first Whitehall study. British Medical Journal 313: 1177-1180 .
Marmot, M., and R.G. Wilkinson, eds. 1999 Social Determinants of Health . Oxford : Oxford University Press .
1995 Sociodemographic differential in mortality at older ages in Finland. In Health and Mortality among Elderly Populations , G. Caselli and A. Lopez, eds. Oxford : Clarendon Press .
, and 2000 Use of nursing homes in the care of persons with severe mental illness: 1985 to 1995. Psychiatric Services 51(3): 354-358 .
, and 1992 A policy of inclusion for the mentally ill. Health Affairs 11: 128-150 .
1996 Comparative medical systems. Annual Review of Sociology 22: 39-70 .
, , , , and 1998 Perceived need for local anesthesia in tooth drilling among Anglo-Americans, Chinese and Scandinavians. Anesthesia Progress 45: 22-28 .
1997 Evidence-based Healthcare: How to Make Health Policy and Management Decisions . London : Churchill Livingstone .
, , and 1999 Volunteering and mortality among older adults: Findings from a national sample. Journals of Gerontology. Series B, Psychological Sciences and Social Sciences 54(3): S173-180 .
1990 Mortality differentials from a multiple-cause of death perspective. In Measurement and Analysis of Mortality , J. Vallin, S. D'Souza, and A. Palloni, eds. Oxford : Clarendon Press .
2000 Databases on Aging. Survey Summaries . Bethesda, MD : National Institute on Aging .
1988 The Aging Population in the Twenty-First Century. Statistics for Health Policy . Committee on National Statistics. P.M. Gilford, ed. Commission on Behavioral and Social Sciences and Education. Washington, DC : National Academy Press .
1992 Toward a National Health Care Survey: A Data System for the 21 st Century . Panel on the National Health Care Survey. G.S. Wunderlich, ed. Commission on Behavioral and Social Sciences and Education. Washington, DC : National Academy Press .
Page 248
2001 Cells and Surveys. Should Biological Measures Be Included in Social Science Research? Committee on Population. C.E. Finch, J.W. Vaupel, and K. Kinsella, eds. Commission on Behavioral and Social Sciences and Education. Washington, DC : National Academy Press .
1996 Caring for Frail Elderly People . Social Policy Studies 19. Paris : Organization for Economic Co-Operation and Development .
, , and 1997 Effect of Age Misreporting on Mortality Estimates at Older Ages . Working Paper 98-01. Philadelphia : Population Aging Research Center, University of Pennsylvania .
, and 1994 Retirement and labor force behavior of the elderly. In Demography of Aging . Committee on Population. L.G. Martin and S.H. Preston, eds, pp. 50-101 . Commission on Behavioral and Social Sciences and Education. Washington DC : National Academy Press .
, , , , , , , and 1997 Nursing homes in 10 countries: A comparison between countries and settings. Age and Ageing 26(S2): 3-12 .
1999 Can We Hope for Both Long Life and Good Health? Paper prepared for the Panel on a Research Agenda and New Data for an Aging World, London , September, Committee on Population, National Research Council .
, , and 1999 Health expectancy indicators. Bulletin of the World Health Organization 77: 181-185 .
, , , and 1998 Comorbidities and prediction of length of hospital stay. Australian and New Zealand Journal of Medicine 28: 811-815 .
, , , , , , and 1995 Assessing mortality differentials using life histories: a method and applications. In Adult Mortality in Developed Countries: From Description to Explanation , A. Lopez, G. Caselli, and T. Valkonen, eds., pp. 57-79 . Oxford : Clarendon Press .
1999 Healthy bodies and thick wallets: The dual relationship between health and economic status. Journal of Economic Perspectives 13: 145-166 .
, , , , and 1997 Temporomandibular disorders. Part I: A comparison of symptom profiles in Australian and Finnish patients. Journal of Orofacial Pain 11: 58-66 .
, , and 1998 The Force of Mortality at Ages 80 to 120 . Monographs on Population Aging 5. Odense, Denmark : Odense University Press .
, , , , , , and 2000 Estimation of the contribution of changes in coronary care to improving survival, event rates, and coronary heart disease mortality across the WHO MONICA Project Populations. Lancet 355: 688-700 .
2000 Biological and Clinical Data Collection in Population Surveys in Less Developed Countries. Summary of a Meeting held January 24-25 by MEASURE Evaluation, Washington, DC .
Page 249
, , , and 1999 Treating depressed older adults in primary care: Narrowing the gap between efficacy and effectiveness. Milbank Quarterly 77(2): 225-256 .
1980 Unloving Care: The Nursing Home Tragedy . New York : Basic Books .
, , , , , , , and 1989 The functioning and well-being of depressed patients: Results from the Medical Outcomes Study. Journal of the American Medical Association 262: 914-919 .
Wilkinson, R., and M. Marmot, eds. 1998 Social Determinants of Health: The Solid Facts . Geneva : World Health Organization .
1984 The Uses of Epidemiology in the Study of the Elderly: Report of a WHO Scientific Group on the Epidemiology of Aging . Technical Report Series 706. Geneva : World Health Organization .
, , , and 1999 Effects of co-morbidity on health-related quality-of-life scores: An analysis of clinical trial data. Clinical Therapeutics 21: 383-403 .


















































