6
Improving Participation in Cancer Screening Programs1
Screening programs can effectively reduce the burden ofcancer ifthey ensure that people get the tests that they need and that tests are performed accurately, are not conducted too often, and are followed up in a timely and appropriate manner. The principal challenges to optimizing the delivery of effective cancer screening services and reducing inappropriate testing lie in changing the behaviors of (1) systems of care, to make cancer screening services available to eligible populations; (2) health care providers, to perform cancer screening as recommended, on time, and with skill when they encounter patients eligible for screening; and (3) individuals, to obtain recommended screening tests and pursue follow-up tests. This chapter describes the major challenges to delivering cancer screening and reviews the literature to identify interventions that are successful in improving rates of participation in screening. Although there is a fairly extensive literature on barriers to access to screening, less is known about ways to optimize the delivery of screening to ensure quality and cost-effective testing. Resources can be wasted and harm can be done if screening is delivered badly, and more research is needed to assess ways to ensure quality in screening programs.
|
1 |
This chapter is based on a background paper prepared by Steven H. Woolf. Additional references were drawn from two other background papers commissioned for this report, the first by Edwin B. Fisher, Ross C. Brownson, Amy A. Eyler, Debra L. Haire-Joshu, and Mario Schootman, and the second by Judith Ockene, Jane Zapka, Lori Pbert, Suzanne Brodney, and Stephenie Lemon (www.iom.edu/ncpb). |
CHALLENGES FOR SYSTEMS OF CARE
One fundamental barrier to cancer screening imposed by the structure of the U.S. health care system is that a large proportion of the eligible population lacks access to health care. The policy issues surrounding the amelioration of the current situation in which some 39 million Americans (14 percent of the population) lack some type of health insurance are beyond the scope of this report, but the situation clearly constitutes a fundamental obstacle to optimizing the potential of cancer screening in the United States (http://www.census.gov/Press-Release/www/2001/cb01-162.html).
Even among persons with health insurance, the private payers and governmental programs that finance health care services face economic barriers to offering coverage for cancer screening. For payers and employer benefits managers, monetary costs pose an impediment to offering coverage for cancer screening, as they do for many other health care services, although the literature suggests that their cost-effectiveness ratios generally fall within affordable ranges. Managed care plans, whose members often remain enrolled for an average of just a few years, may be reluctant to extend coverage to screening tests with high up-front costs. Public insurance programs, such as Medicare and Medicaid, face similar concerns and statutory restrictions against covering prevention services, although the latter have been less of a concern in recent years. Between 1965 and 1990, the U.S. Congress introduced 453 bills proposing coverage for prevention services under Medicare, but the first prevention service was not covered until 1980 (Schauffler, 1993).
Developments in recent years have shifted payer policy toward more extensive coverage for cancer screening tests, making insurance coverage less of an impediment to screening than it was as recently as one decade ago. In addition, the competitive marketplace of private health insurance and the public’s interest in obtaining preventive care have made coverage of cancer screening a potent marketing tool, with coverage of cancer screening heavily promoted by the managed care industry, thereby providing an infrastructure for the delivery of cancer screening services. In fact, at least some studies suggest that patients who belong to health maintenance organizations are more likely to receive cancer screening tests than those covered by indemnity plans (Phillips et al., 2000; Gordon et al., 1998; Hsia et al., 2000).
Data from the Health Plan Employer Data and Information Set (HEDIS) reported to the National Committee for Quality Assurance reflect the successes of this infrastructure in the delivery of cancer screening at 273 organizations (health maintenance organizations, point-of-service plans, and other managed care plans) that collectively cover 63 million Americans. In 2000 these organizations reported that 76 percent of their female members
aged 52 to 69 had received a mammogram within the past 2 years and that 80 percent of women aged 21 to 64 had received at least one Pap test during the past 3 years (National Committee for Quality Assurance, 2001).
Coverage of prevention services has expanded under Medicaid and Medicare, with the latter now covering annual mammography beginning at age 40, Pap smears and pelvic examinations, prostate cancer screening (annual digital rectal examination and prostate-specific antigen [PSA] testing), and screening for colorectal cancer (annual fecal occult blood testing [FOBT] and flexible sigmoidoscopy every 4 years). This coverage has important policy implications for Medicare, whose 39 million beneficiaries make it the largest health insurance plan in the United States. Its coverage of colorectal cancer screening was recently expanded to include colonoscopy every 10 years, with barium enema covered as a substitute for either sigmoidoscopy or colonoscopy (see Chapter 9 for further discussion of the screening services covered by Medicare and Medicaid).
The coverage policies of the Medicare program appear to influence screening rates. When coverage for biennial mammography was offered beginning in 1991, it was followed by increased mammography use, at least among women with access to a usual source for primary care (Kelaher and Stellman, 2000). Similar influences are noted through initiatives at the state level. As of 2000, 43 states and the District of Columbia mandated coverage of cancer screening, even though the provisions of the mandates were not always in compliance with evidence-based guidelines (Rathore et al., 2000). Federal legislation establishing a national program for breast and cervical cancer screening services has had some salutary effects on screening rates (Lillquist, 2001).
Legislative and regulatory efforts by government and professional organizations have also focused on enhancing the quality with which screening tests are delivered to ensure that they are performed well and interpreted accurately and to ensure that patients receive appropriate follow-up. For example, the Mammography Quality Standards Act of 1992 (PL 102-539) seeks to improve the performance standards of mammographic facilities (Monsees, 2000). In 1999, the act was amended to require that mammographers send a written summary of findings directly to patients in terms easily understood by laypersons. The American College of Radiology maintains detailed standards for the performance of screening mammography (American College of Radiology, 2000) and has established the National Mammography Database, an effort to improve the quality of mammography through a reporting system for breast imaging facilities, regions, and states (www.acr.org/departments/stand_accred/nmd-intro.html).
Local and regional factors influence successes and failures in the delivery of cancer screening. For example, a major concern about making colonoscopy the preferred screening test for colorectal cancer is that some communities and regions lack an adequate supply of gastroenterologists to absorb the
volume; therefore, unqualified examiners may offer screening services and thereby increase the risk of complications. Communities struggling with the stresses of poverty, poor housing, inadequate jobs, domestic stresses, and crime have residents with urgent priorities that compete with cancer screening. The absence of public transportation, of social service agencies to support disadvantaged and non-English-speaking individuals, and of community health centers, free clinics, and public health departments impose added barriers to access to cancer screening. In attempting to correct the problem, communities face a variety of barriers, including state and local budget constraints and political dynamics.
Finally, the systems of care that deliver cancer screening within the community—primary care offices, clinics, emergency departments, urgent care centers, integrated health care delivery systems, hospitals, and institutions that provide long-term care—encounter a variety of operational barriers in delivering effective health care services that are too broad to review here. The systems that clinicians need to deliver effective cancer screening (see below) depend on supportive management structures; efficient patient-flow procedures; and information systems that support reminder systems, documentation of screening, timely follow-up and referrals, and coordinated communication with providers and institutions across the community. Some providers have succeeded in establishing such systems. Approximately 50 percent of capitated medical groups and independent practice associations in California mail patients reminders for mammography and Pap testing (Malin et al., 2000). The financial, organizational, and technological barriers that health systems face in making such reconfigurations are formidable and are the subject of a recent report by the Institute of Medicine (2001c).
CHALLENGES FOR INDIVIDUALS
Whether an individual is a physician or a patient, improvements in cancer screening practices (and most other changes in behavior) require a series of steps well known to psychologists. The four steps include knowledge, attitudes, ability, and reinforcement (Woolf, 2000a). The relevance of this framework is illustrated by considering how they result in changes in the behaviors of clinicians and patients.
Challenges for Clinicians
Knowledge
Clinicians do not promote or perform screening tests without the basic prerequisite of knowing that such screening is recommended and appropriate. Many studies have shown that simply disseminating a guideline is, for
a variety of reasons, an inadequate means to change practice behavior (Bero et al., 1998; Davis et al., 1992). For one, physicians may not see the guideline or retain its recommendations. Studies confirm that physicians tend to have limited familiarity with published practice guidelines, especially recent ones. A 1995 survey found that baseline mammograms, a practice no longer recommended, were still being ordered for women ages 30 to 39 (Reifel et al., 1998).
Physicians’ knowledge of practice guidelines tends to be uneven across organizations. The American Cancer Society guidelines on cancer screening, which were first issued in 1980 (ACS, 1980a), tend to be the most well known by physicians and the general public (Hamblin and Connor, 1998). When primary care physicians in Colorado were surveyed about the influence of guidelines on their screening practices for prostate cancer, 89 percent rated the American Cancer Society guidelines as moderately or highly influential, whereas fewer than one-third rated the guidelines of the U.S. Preventive Services Task Force as moderately or highly influential (Moran et al., 2000). A clear understanding of what is recommended is made more difficult by inconsistencies between the recommendations of different organizations and controversies over whether scientific evidence supports the practice.
Attitudes
Even if physicians are knowledgeable about recommendations, they may not agree that the proposed policy represents good care, is supported by valid evidence, meets accepted norms for their specialty or among local opinion leaders, or is applicable to their practice. Studies of family physicians in Ohio demonstrated disagreement with a substantial proportion of recommendations against cancer screening issued by the U.S. Preventive Services Task Force (Stange et al., 1992; Zyzanski et al., 1994). Finally, physicians may agree that it is appropriate for patients to obtain certain screening tests but disagree that it is their role to provide the service.
Ability
Clinicians who agree that screening is appropriate may be unable to offer testing and follow-up for a variety of operational reasons. These include lack of time, skills, personnel, equipment, adequate reimbursement, information systems, freedom from bureaucratic obstacles and medicolegal liability, and patient cooperation (see below). As noted earlier, the practice systems in which clinicians care for patients must be configured in an efficient design to facilitate the recognition of when patients are in need of screening (e.g., through the use of prompts or flow sheets); ease in administering tests or expediting referrals for testing elsewhere; and tracking sys-
tems to ensure receipt, interpretation, reporting, and appropriate follow-up of test results. An integrated, multifaceted approach to the reconfiguration of clinical operations and personnel duties is often necessary to make this happen. Studies have shown that such changes can improve cancer screening rates, although some randomized trials have shown modest incremental benefit (Dietrich et al., 1994b, 1998; Solberg et al., 1998).
Reinforcement
Even when providers are able to deliver screening tests well, reminder systems and feedback are important to identify when the need for rescreening has arisen. Tracking systems are necessary to indicate when the results of screening tests have not returned and to ensure that prompt and appropriate action is taken for patients with abnormal results. In an era when patients change providers and relocate geographically on a frequent basis, providers have limited ability to determine retrospectively from medical records when screening was last performed, and patients’ memories are an imprecise substitute.
Measures to address these behaviors are not uniformly effective. The Cochrane Collaboration, an international effort to systematically review randomized clinical trials of health care, analyzed 18 systematic reviews of methods for the dissemination and implementation of evidence in practice. Although some interventions were consistently effective (e.g., educational outreach, reminders, multifaceted interventions, and interactive education), others were rarely or never effective (e.g., educational materials and didactic teaching) or were inconsistently effective (e.g., audits, feedback, local opinion leaders, local adaptation, and patient-mediated interventions) (Bero et al., 1998). Similarly, a review of 58 studies of strategies for the improvement of preventive care found that most were effective in some studies but not others (Hulscher et al., 1999).
A review of 187 studies by the RAND Corporation on behalf of the Health Care Financing Administration (now the Centers for Medicare and Medicaid Services) evaluated interventions that can be used to increase the rates of delivery of mammography, Pap smears, and FOBT (HCFA, 2001). Organizational changes and financial incentives most consistently produced the largest improvements in screening services. Examples of successful organizational changes include the use of a prevention team that includes standing orders for mammography by nurses (i.e., nurses may routinely refer eligible patients for mammograms), the use of nurses to distribute kits and instruct patients in the completion of FOBT, and the use of a health educator to contact patients via telephone to offer counseling or to assist in the scheduling of an appointment for cervical cancer screening. Patient reminders were somewhat less effective than organizational changes or financial incentives. Patient reminders that are personalized or signed by
the provider appear to be modestly more effective than generic reminders. Provider education is moderately effective at increasing cancer screening, but patient education and provider feedback were least effective. Multiple interventions were more effective than single measures. Computer-assisted provider reminders are more cost-effective than patient reminders in the few studies that have addressed the issue.
What these reviews indicate is that there is no “magic bullet” that can be used to improve rates of cancer screening. A more rational strategy is to take a diagnostic approach, to identify which barriers account for the unsatisfactory screening practices, and to tailor strategies accordingly (Grol, 1997; Woolf, 2000b). Depending on which barrier(s) is(are) pertinent, a menu of options for improvement of the quality of interventions is available.
Challenges for Patients
Patients face the same four-part spectrum of challenges faced by clinicians (knowledge-attitudes-ability-reinforcement), although patients face these challenges from a different perspective.
Knowledge
The first impediment that patients face in pursuing cancer screening is inadequate knowledge of a variety of issues related to cancer: simple awareness of the existence of the cancer, knowledge of the fact that they face a risk of acquiring cancer, the cancer-associated morbidity and mortality, the availability of screening tests that can reduce these risks, and recommendations regarding when and how often they should be screened. People are unlikely to consider, let alone pursue or obtain, screening without this information. Not surprisingly, people with limited education and limited exposure to health information are less likely to have this knowledge. Knowledge about breast and cervical cancer among Hispanic women, for example, is related to age, education, income, language preference, and recent screening history (Ramirez et al., 2000a).
Inaccurate knowledge can influence screening behavior, leading to overutilization and underutilization of cancer screening. As noted earlier, research has documented that many patients have inaccurate perceptions about the magnitude of their risk from cancer (Clarke et al., 2000) and the likely benefits that they will obtain from screening.
Attitudes
Even if people have the facts about cancer screening right, they may lack motivation to obtain screening for a variety of attitudinal reasons.
Personal and cultural beliefs may influence attitudes about the importance of cancer, the acceptability of the tests that they must undergo, and the mores of trying to alter the natural history of disease rather than allowing nature to take its course (Mandelblatt et al., 1999; Paskett et al., 1997; Bowen et al., 1997; Tortolero-Luna et al., 1995). Fears of cancer and fears of knowing whether it is present also influence the motivation to get tested. Finally, attitudes about cancer prevention exist in the context of the competing priorities patients face in their daily lives. Concerns related to one’s livelihood, income, family, or safety are often too substantial to make cancer screening a priority.
These attitudinal factors vary across ethnic and cultural traditions. Hispanic or Latino population groups are often treated as a monolithic entity on this (and many other) topics without consideration of heterogeneous cultural diversities. For example, Mexican Americans and Puerto Ricans may have more negative or fatalistic views about breast and cervical cancer than Cubans or Central Americans do (Ramirez et al., 2000a). Understanding of these cultural contexts and, more importantly, the involvement of individuals from within the particular culture who are sensitive to these concerns help craft interventions that are effective in shifting attitudes. For example, one randomized controlled trial found that the intervention that was effective in improving rates of screening for breast and cervical cancer among Latinas was organization of educational group sessions led by consejeras, lay Latino community volunteers (Navarro et al., 1998). Other research suggests that lay health advisers are effective among low-income women (Margolis et al., 1998; Skinner et al., 2000). Self-reported Pap smear utilization rates doubled in 6 months when lay health advisers assisted American Indian women (Dignan et al., 1996).
Ability
Even if people are knowledgeable about cancer and want to be screened, they may not be able to. A fundamental impediment is a lack of access to screening services. People who lack health insurance are less likely to receive cancer screening tests (Breen et al., 2001; Gordon et al., 1998; Hsia et al., 2000; Potosky et al., 1998), and this applies to a large proportion of U.S. citizens. In 1997, 22 percent of adults ages 18 to 44 and 12 percent of adults ages 45 to 64, respectively, were uninsured; among individuals under age 65 classified as poor or near poor, 34 and 36 percent, respectively, were uninsured. The proportion of older persons (age 65 and older) who are uninsured, however, is 1 percent because of Medicare coverage (National Center for Health Statistics, 2000). As noted earlier, people with health insurance typically find that most cancer screening tests are covered under their plans, although there are notable exceptions and an increasing requirement for copayments, a factor known to reduce the rate of adherence to screening tests
(Solanki et al., 2000; Solanki and Schauffler, 1999; Partnership for Prevention, 1997). Studies from the early 1990s suggested that individuals with Medicaid coverage were screened at lower rates than those with private insurance (Makuc et al., 1994); however, more recent studies suggest comparable screening rates for the two groups (Potosky et al., 1998).
A related but separate part of access to health care is having a provider, in particular, a regular source of primary care. Adults who receive regular care from a family physician are more likely to receive mammography and Pap smears (McIsaac et al., 2001). Low-income individuals and families are less likely to enjoy this degree of access. In 1997, 9 to 16 percent of adults reported that they needed to see a doctor but could not because of the cost, irrespective of insurance status (CDC, 2000a). Even among individuals with a health problem, however, 12 percent had no physician contact within the past year (the rates were 21 and 12 percent for poor or near-poor men and women, respectively) (National Center for Health Statistics, 1998).
Patients with insurance and access to providers face other barriers that impede their ability to be screened. Work, school, or family responsibilities may make the tasks of scheduling and traveling to appointments, undergoing tests, and arranging and attending follow-up procedures too time-consuming or inconvenient. Women who report that they must take time off from work to see a physician are less likely to be screened (Lantz et al., 1995). Inconvenience of appointments, long waits for appointments, and scheduling difficulties may also discourage screening and follow-up (Glasgow et al., 2000; Marcus and Crane, 1998; McCarthy et al., 1996). On-site technology, such as a mammography unit (Potter et al., 1996) or a sigmoidoscope (Schroy et al., 1999), and extended and convenient hours (Potter et al., 1996) can increase screening use in primary care settings.
Physical limitations, such as those imposed by frail health in elderly individuals, may interfere with the ability to perform or undergo screening tests (e.g., handling of stool for FOBT or suitability for colonoscopy). Illiteracy, cognitive deficits, or language barriers may make it difficult to understand or follow instructions from medical staff. Patients referred to specialists to obtain screening tests or follow-up procedures may be unable to understand or navigate the increasingly onerous administrative tasks of dealing with health plans to obtain referrals to the recommended provider or facility, scheduling appointments, and being adequately prepared on arrival.
Reinforcement
Finally, even if patients are willing and able to be screened, remembering that screening is due or remembering to perform self-examination is often difficult simply because of forgetfulness. This is especially problematic for screening tests with long recommended intervals between testing. Patients who are advised to return for sigmoidoscopy in 5 years or colonoscopy in 10
years may have difficulty remembering when the test must be done and relating to new providers which test they underwent previously.
Intermingling of Challenges
The disentangling of health systems, providers, and patients as separate sources of challenges to screening is a somewhat artificial construct given their complex interrelationships. The example of the barriers to optimizing colorectal cancer screening, seen from the provider’s perspective, illustrates the intermingling of the three groups (Box 6.1).
CLOSER EXAMINATION OF SPECIFIC CANCER SCREENING TESTS
Using the four-part model of behavioral change (knowledge-attitudes-ability-reinforcement) as an organizational framework for understanding the patient’s perspective on reasons for inadequate screening, this section reviews in greater detail the evidence regarding the factors associated with cancer screening and the effectiveness of interventions that can enhance the appropriateness of screening practices. Evidence is examined for screening for cancer of the colon-rectum, breast, prostate, and cervix. (Lung and skin cancer are not considered in this discussion because of the lack of an organized interest in promoting screening for lung cancer and the lack of current evidence regarding efforts to improve skin cancer screening. The history of attempts to screen for lung cancer is described in Chapter 7). Evidence regarding predictors of cancer screening is understandably derived largely from observational studies, but, where possible, evidence regarding the effectiveness of interventions to improve screening rates emphasizes evidence from randomized controlled trials. The review considers the evidence available as of February 2001 but not more recently published evidence.
Colorectal Cancer Screening
Size of the Gap
Many of the lives claimed each year by colorectal cancer are attributable to the small proportion of the population that undergoes screening. As of 1999, approximately 60 percent of U.S. adults age 50 and older reported that they had never been screened for colorectal cancer (by FOBT, sigmoidoscopy, or colonoscopy). Others had been screened, but not recently. Only 19 percent had undergone home FOBT within the past year, 32 percent had undergone sigmoidoscopy or colonoscopy within the past 5 years, and 44 percent had received at least one of the tests within the preceding 5 years (CDC, Behavioral Risk Factor Surveillance System, 2000; CDC, 2001c).
|
BOX 6.1 Challenges to Providers in Improving Rates of Screening for Colorectal Cancer Knowledge Many physicians are unaware of the evidence that screening for colon cancer reduces the rate of mortality from that disease. Until recent trials demonstrated otherwise, the conventional wisdom was that colorectal cancer screening had no proven benefit. Furthermore, clinicians may not know current protocols for screening. Many assume that guaiac testing in the office, performed with the glove used in a rectal examination, constitutes FOBT screening (the procedure that lowered the rates of mortality in clinical trials was the collection of six specimens, two specimens from three consecutive stools, at home). Physicians know little about the effects of rehydrating FOBT cards (which results in a better sensitivity but a decreased specificity, increasing the probability of obtaining false-positive results and the need for workups). They do not know which types of polyps are premalignant and, having detected them by endoscopy or barium enema, the sizes of polyps that require biopsy. Attitudes Clinicians can know the facts but remain uneager. For many years, colorectal cancer screening was the focus of conflicting guidelines and controversy. Not until 1996 did the U.S. Preventive Services Task Force abandon the position that there was insufficient evidence to make a recommendation. That this group—and most others—now enthusiastically recommends colorectal cancer screening is not well known. The ambiguity and the dismal compliance rates of patients are fresh in mind, and many clinicians give priority to other prevention services (e.g., counseling against tobacco use and control of blood pressure, and lipid levels). Some physicians who know the data are not impressed by the magnitude of benefit; by one calculation, 1,374 patients must undergo screening by FOBT for 5 years to prevent one death from colorectal cancer. Ability Even enthusiastic physicians cannot screen patients if they lack time, patient cooperation, office help, ease of referral to gastroenterologists, and insurance coverage. They cannot perform endoscopy skillfully without training and without conducting a large volume of procedures. Changes in the practice environment, for example, implementing an office system to generate reminders for screening and follow-up, can enhance practice. Reinforcement Screening cannot occur if clinicians do not remember when patients are due for screening or forget to act on abnormal results. |
The probability of having done FOBT at home was 18.2 percent for whites, 20.3 percent for African Americans, 14.2 percent for Hispanics, and 12.3 percent for American Indians (CDC, Behavioral Risk Factor Surveillance System, 2000). The probability of having had a flexible sigmoidoscopy or colonoscopic examination within the past 5 years was 30.4 percent for whites, 28.2 percent for African Americans, 22.4 percent for Hispanics, and 27.6 percent for American Indians (CDC, Behavioral Risk Factor Surveillance System, 2000).
An additional problem beyond access to screening is the quality of testing. Patients with positive FOBT results often receive incomplete follow-up investigation (Shields et al., 2001).
Predictors of Screening
Knowledge A likely reason for the failure of many Americans to obtain screening for colorectal cancer is unfamiliarity with the disease (Newman, 2001). In contrast to breast cancer, most people have never heard of colorectal cancer. Although breast cancer claims 11,000 fewer lives each year, it is perceived as a more deadly threat to health. Many women misperceive colorectal cancer as a man’s disease (Burke et al., 2000). Most women know about breast and cervical cancer screening, and an increasing number of men know about screening for prostate cancer, but both women and men are generally unaware that all adults should be screened for colorectal cancer beginning at age 50. Some evidence suggests that physicians are not providing patients with the information that they need to facilitate screening. Individuals not screened by sigmoidoscopy report that their physician did not recommend it (Beeker et al., 2000; Vernon, 1995; Weitzman et al., 2001). A recent study of Massachusetts residents found that only 34 percent of people aged 50 to 64 and 43 percent of people aged 65 and older reported that a physician had ever recommended sigmoidoscopy (Erban et al., 2001). Among a sample of family physicians in Washington state, 30 percent of age-appropriate patients had received recommendations for screening sigmoidoscopy within the previous 5 years (Montano et al., 2000). In another study, only 58 percent of older women in a large health maintenance organization reported that they had been encouraged by their physician to receive screening for colorectal cancer, but this factor was strongly related to screening participation (Mandelson et al., 2000).
Attitudes Among people who are aware of colorectal cancer and the recommendation to be screened, attitudes about the disease, the anatomic part of the body involved, and the nature of the tests pose barriers to screening. Some find distasteful or inconvenient the notion of handling stool specimens for FOBT at home (Myers et al., 1991). The inconvenience of having to avoid certain foods in the days preceding the test may dissuade patients from completing the test (Robinson et al., 1994). Others anticipate discomfort and embarrassment from screening by endoscopy or barium enema or the bowel preparation procedure that precedes those tests. Their attitudes may be amplified if their prior screening examinations were unpleasant.
As with other screening tests, however, patients’ attitudes are more likely to shift in favor of screening if a physician recommends the test. If a physician recommends the test, approximately 50 to 70 percent of patients complete the FOBT and 25 to 50 percent undergo sigmoidoscopy (Vernon, 1997).
Ability Patients who want to be screened for colorectal cancer may be unable to do so. They may lack insurance coverage or access to care. In certain communities and regions of the country, gastroenterologists who can perform screening colonoscopic examinations, radiology facilities where high-quality double-contrast barium enemas can be performed, or openings on schedules for timely appointments may not be available to patients. Patients may be unable to understand, perform, or tolerate bowel preparation procedures. Reading and language barriers can make instructions useless. Older patients with poor vision or manual dexterity may have difficulty collecting stool specimens for FOBT.
Reinforcement For patients who want to undergo annual FOBT, few may remember when 1 year has passed. Even fewer remember, 5 years hence, that it is time for another sigmoidoscopy. Reminders from the physician who performed the test help little if the patient has moved out of the area or, as occurs frequently in the current environment of managed care, has acquired a new physician.
Interventions to Enhance Colorectal Cancer Screening
Knowledge Interventions In recent years, considerable effort has gone into heightening public awareness of colorectal cancer. Much of this has been accomplished by celebrities, a noteworthy example being Katie Couric, a television personality, who has spearheaded an effort to promote screening for colorectal cancer (Gorman, 2000; Newman, 2001). A live television broadcast of her colonoscopy screening examination was associated with a subsequent increase in requests for screenings and referrals to gastroenterologists.
In 1997 the CDC and the American Cancer Society established the National Colorectal Cancer Roundtable, a coalition of medical professional, consumer advocacy, and volunteer organizations committed to raising awareness about colorectal cancer. The U.S. Congress designated March of each year the National Colorectal Cancer Awareness Month. The annual program Screen for Life, A National Colorectal Cancer Action Campaign, is a collaboration among the CDC, the National Cancer Institute, and the Centers for Medicare and Medicaid Services (formerly the Health Care Financing Administration) and promotes the distribution of television and radio public service announcements, brochures, posters, and fact sheets for the public and providers (http://www.cdc.gov/cancer/colorctl/calltoaction).
Attitude Interventions The review of the literature for this chapter found little current evidence of whether the efforts described above have been effective in shifting attitudes about the acceptability of screening tests for colorectal cancer.
Ability Interventions It is difficult for the large proportion of the U.S. population that lacks health insurance or access to health care providers to obtain colorectal cancer screening. Interventions to correct this formidable defect in the U.S. health care system are beyond the scope of this review. For insured populations, however, major steps have been taken to expand coverage for colorectal cancer screening. Most private health plans offer coverage for screening by FOBT and flexible sigmoidoscopy, a growing number offer coverage for colonoscopy, and congressional legislation may mandate such coverage. As already noted, the Medicare program began offering coverage for colorectal cancer screening tests in 1998 and now includes coverage for colonoscopy.
The review of the literature for this chapter found little current published evidence of organized efforts to address the potential shortage of physicians available to screen the millions of Americans for whom it is recommended by current guidelines. Low reimbursement rates for screening work against efforts to expand the workforce for this task (Lewis and Asch, 1999). Studies have demonstrated that nurses can be trained to perform sigmoidoscopy and even colonoscopy and thereby expand the number of health professionals available to perform screening (see Chapter 8).
The lack of a requirement for dietary restrictions before home FOBT was shown in one randomized trial to improve adherence rates (Robinson et al., 1994). The present review otherwise found few published studies about efforts to enhance the patient’s ability to schedule, prepare, and undergo colorectal cancer screening tests, although manufacturers, public health departments, and community health centers have undertaken efforts with these aims, with a particular focus on patients with limited education and limited English-language proficiency.
Reinforcement Interventions Some work has gone into developing reminder systems to alert physicians and patients when screening for colorectal cancer is due. Computerized reminder systems have been shown to improve compliance with screening by FOBT (Litzelman et al., 1993). In a review of the effectiveness of interventions aimed at increasing rates of screening by FOBT, Vernon (1997) showed that studies that deliver minimal or relatively impersonal interventions were generally not effective (King et al., 1992; Myers et al., 1991, 1994). In general, the rate of adherence was lowest when persons were asked to pick up a test kit or to mail in a reply card to receive a kit (Lallemand et al., 1984; Nichols et al., 1986). More intensive interventions appeared to be more effective (Vernon, 1997), such as combining reminder telephone calls with self-help screening booklets (Myers et al., 1991).
As discussed below with regard to breast cancer screening, the ability of physicians’ offices and clinics to establish reminder systems and institute appropriate follow-up for colorectal cancer screening appears to be facili-
tated by the adoption of comprehensive office system changes (e.g., through the use of office chart reminders, patient health maintenance cards, on-site training and start-up assistance visits, continuing education seminars, and quality assurance feedback). Such programs have proved effective in increasing the rates of performance of FOBT (Manfredi et al., 1998). In one randomized trial, the intervention consisted of an 11-minute video about colon cancer screening, the selection of a color-coded educational brochure reflecting degree of interest in screening, and a marker of the same color attached to the chart. The numbers of requisitions for FOBT and flexible sigmoidoscopy and the rates of completion of these tests increased signifi cantly under this program (Pignone et al., 2000).
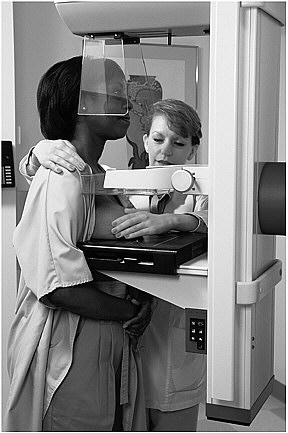
SOURCE: PhotoDisc, Inc.
Breast Cancer Screening
Size of the Gap
In contrast to colorectal cancer screening, a relatively large proportion of women have availed themselves of screening mammography. Approxi
mately 64 percent of women age 50 and older report that they have had a mammogram in the past year (CDC, Behavioral Risk Factor Surveillance System, 2000), and 74 percent report that they have had one within the past 2 years (CDC, 2000a). Approximately 57 percent of women in this age group have also reported that they have had a clinical breast examination in the past year (CDC, Behavioral Risk Factor Surveillance System, 2000), and 66 percent have reported that they have had both a mammogram and a clinical breast examination within the past 2 years (CDC, 2000a). Fully 59 percent of women age 40 and older reported that they have had a mammogram within the preceding year (CDC, Behavioral Risk Factor Surveillance System, 2000). In fact, breast imaging accounts for 10 percent of all examinations performed by radiologists (Sickles, 2000a).
These numbers, however, leave a substantial proportion of women who have not been screened recently and a disturbing minority of women who have never been screened, a more common occurrence among poor women. Whereas 72 percent of women age 50 and older with family incomes at or above the poverty level have had a mammogram in the past 2 years, the same is true for only 53 percent of women of the same age who have family incomes below the poverty level. (National Center for Health Statistics, 2000). Among women age 40 and older, the probability of having had a mammogram within the past 2 years was 73 percent for women with at least some college education but 55 percent for those with less than a high school education (National Center for Health Statistics, 2000). Screening rates are lower in urban inner-city America (Ekeh et al., 2000; Taylor et al., 1998). In community-based screening in Albuquerque, New Mexico, only 50 percent of women aged 50 to 74 were screened each year in the study period from 1994 to 1997 (Gilliland et al., 2000).
There are important racial and ethnic disparities in breast cancer screening rates, but in contrast to other areas of health care, African Americans do not appear to be disadvantaged in terms of screening for breast cancer. After controlling for income, African-American women are just as likely (if not more so) to have had a recent mammogram as white women. The probability of having had a mammogram within the past 2 years is 73.7 percent for whites, 76.1 percent for African Americans, and 63.5 percent for Hispanics (CDC, Behavioral Risk Factor Surveillance System, 2000). In fact, among poor women, African-American women were about 60 percent more likely than white women to have had a recent mammogram (National Center for Health Statistics, 1998). Also, in contrast to other areas of health care, African-American women do not appear to be more likely to receive substandard mammographic services (Jones et al., 2001).
Other minority groups, particularly Hispanic and Asian women, are more likely to receive substandard screening. In one study in Albuquerque, New Mexico, only 20 percent of Hispanic women ages 50 to 74 had re-
ceived routine annual mammograms (Gilliland et al., 2000). Breast cancer screening rates are significantly reduced among Asian Americans and Pacific Islanders (Kagawa-Singer and Pourat, 2000). Only 47 percent of Korean Americans have had a mammogram in the past 2 years (Juon et al., 2000). Among Cambodian Americans, approximately 40 percent are up to date on their clinical breast and mammography examinations (Tu et al., 2000). Screening rates are also low among American Indians. A 1995 audit of diabetes care at Indian Health Service centers found that at some centers as few as 35 percent of women had ever had a mammogram, and at one center only 28 percent had received a clinical breast examination in the past year (Giroux et al., 2000).
Access to mammography is also affected by age, with older women less likely to have kept up to date with screening mammography. An audit of 110,000 mammograms in New Hampshire confirmed that the rate of screening was higher for younger women (40 to 48 percent for those ages 44 to 64) than for older women (34 to 39 percent for those ages 65 to 84) (Carney et al., 2000). Overuse and exposure to unnecessary false-positive results are potential risks for elderly women. A chart review of women age 75 and older in a skilled nursing facility revealed that an average of 1.9 mammograms were performed per patient, with 45 percent producing abnormal results requiring investigation (Kerins et al., 2000).
Gaps exist not only in breast cancer screening rates but also in what happens next if the findings are abnormal. In one health maintenance organization, in 34 percent of patients, follow-up for an abnormal mass or a suspicious calcification detected on mammography was not completed within 1 month, and it was delayed beyond 2 months in an additional 35 percent of patients (Burack et al., 2000b). Another analysis estimated that 14 percent of patients with abnormal findings on breast cancer screening received inadequate follow-up (Schootman et al., 2000). In a setting where most physicians advise annual mammograms, the median time to subsequent screening was 18 months (Ulcickas Yood et al., 1999).
Predictors
Knowledge Studies of women who receive inadequate screening mammographies reveal women’s misperceptions of their perceived and actual risks of breast cancer (Clemow et al., 2000). There are misconceptions that mammography is unnecessary unless a mass is palpable. In one study of low-income African-American women, those who lacked breast symptoms were more likely to miss appointments (Crump et al., 2000).
Misperceptions about whether one is supposed to have a mammogram is an obvious and proven correlate of whether screening occurs (MacDowell et al., 2000), and confusion on this topic is more prevalent in certain
groups. Older women (i.e., those over age 65), for example, are more likely to express doubts about whether they need to have a mammogram (King et al., 1993a; Taplin and Montano, 1993). Only 53 percent of women attending an urban emergency department knew the correct age to begin screening mammography or the recommended frequency of breast self-examination, and knowledge tended to be poorer among African Americans, Asians, and Hispanics (Takakuwa et al., 2000). In a telephone survey of Hispanic women, accurate knowledge of the screening guidelines ranged from 58 percent for Mexican Americans to 72 percent for Cubans (Ramirez et al., 2000a). A study of urban Chinese-American women age 60 and older revealed that a low level of perceived need affected whether they had had a mammogram in the past year (Tang et al., 2000).
Knowledge in the form of misperceptions also contributes to over-demand for screening mammographies that may not be recommended. Although experts debate whether mammography has significant benefit for women ages 40 to 49 (see Chapter 5), a survey of American women (Woloshin et al., 2000) revealed that 83 percent believed that it did. In fact, 38 percent believed that benefit was proven for women younger than 40 years. Most women suggested that women should begin screening mammography before age 40, whereas only 5 percent believed that it should not begin until age 50. When asked why mammography was controversial, the lead answer (49 percent of respondents) was cost.
Whether a woman acquires accurate knowledge about breast cancer screening is obviously affected by language barriers, an important problem in certain ethnic minority groups. For example, proficiency with the English language is a correlate of recent mammography among Korean-American women (Juon et al., 2000).
Attitudes Personal emotions and values and beliefs about breast cancer and mammography affect the motivation to be screened (King et al., 1995b). An important attitude through which women filter their knowledge of breast cancer screening is fear, including both worry about breast cancer and fear of learning that one has breast cancer (Clemow et al., 2000). Women’s attitudes are influenced by the experiences of family and friends who have had breast cancer (King et al., 1995b).
Women may be reticent to be screened because of fatalistic beliefs. This is especially true for older, African-American, and less educated women (Mayo et al., 2001). In one study, older women (ages 65 to 74) who had never had a mammogram expressed anxieties about the consequences, stating that having a mammogram means “looking for trouble” and that it “makes me nervous” (King et al., 1993a). Other considerations that dampen attitudes about screening include fear of embarrassment (Crump et al., 2000) or discomfort and being in poor health (Taplin et al., 1994). External influences also affect attitudes about screening. A woman is less likely to
have a mammography if a family member or friend discourages it or if her social network lacks someone with whom to discuss health concerns (Pearlman et al., 1997).
An important external influence on women’s attitudes about mammography, both in general and in ethnic and racial groups, is the advice of their health care provider to have the test (Gnanadesigan et al., 2000; Halabi et al., 2000; Juon et al., 2000; MacDowell et al., 2000; Pearlman et al., 1997; Simon et al., 1998; Tang et al., 2000). Such advice may come irregularly, however. Most physicians regularly recommend screening mammography for asymptomatic women ages 50 and older, with estimates ranging from 53 to 81 percent of physicians in recent studies (Lane et al., 2000; May et al., 1999; O’Malley et al., 2001). Uninsured and underinsured women are, however, less likely to receive a recommendation from their doctors to be screened (Lane et al., 2000; May et al., 1999). Studies have not consistently linked age, income, or race or ethnicity to the likelihood of a physician recommendation (Lane et al., 2000; O’Malley et al., 2001; Solberg et al., 1997a). With respect to physician characteristics, asymptomatic women seeing female physicians or younger physicians (i.e., physicians age <40) report receipt of mammography recommendations most often (Lane et al., 2000; Levy et al., 1992).
Having the clinical encounters that provide the opportunity to get screening advice depends on access to health care and health insurance, barriers (O’Malley et al., 2001) discussed below under “Ability,” but the propensity of clinicians to give the advice appears to be influenced by some of the patient’s other socioeconomic conditions, independent of access. Women age 65 and older are less likely to receive a physician recommendation with increasing age and decreased income and education (Lane et al., 2000). Rural women in a study conducted in North Carolina were significantly less likely to be advised to have a mammogram if they were older, less educated, or had a lower family income (O’Malley et al., 2001).
Women may also be influenced by the type of provider who gives the advice. One study found that low-income African-American women were less likely to miss their appointment if they were referred by a physician’s assistant or a nurse practitioner than if they were referred by a physician (Crump et al., 2000).
Aside from what they hear from their personal physician, women’s attitudes are affected by the messages conveyed in practice guidelines and the controversies that they engender. One survey conducted following the controversial 1997 NIH Consensus Development Conference on breast cancer screening for women ages 40 to 49 found 28 percent confused about the schedule on which women should have mammograms. Confusion was a significant predictor of being off schedule (Rimer et al., 1999). Studies of women who have had a mammogram but who have not returned for timely repeat screening find that they are more likely to be confused about screen-
ing guidelines and to express ambivalence than those who have kept current with their screening mammographies (Halabi et al., 2000). A survey of American women revealed that 95 percent were aware of the debate over screening mammography guidelines. Half reported being upset by the public disagreement among experts, and only 24 percent said the discussion had improved their understanding (Woloshin et al., 2000). Another survey of women conducted in western Washington state suggests that conflicting recommendations do not necessarily depress use of mammography. More important than controversy surrounding guidelines was physician recommendation and women’s self-reported likeliness to follow physician advice (Taplin et al, 1997b).
Values about the importance of breast cancer screening vary by race and ethnicity, but it is difficult to disentangle the extent to which these relate to socioeconomic variables. This interrelationship illustrates the overlaps between knowledge, attitudes, ability, and reinforcement as determinants of cancer screening. For example, researchers have used “willingness to pay” for mammography as an indicator of the relative importance that women assign to screening. One study of low-income, ethnically diverse women found that this willingness, which varied by ethnic group, was statistically associated with elements that this report classifies under knowledge (perceived risk of cancer or the knowledge that one needs a mammogram even after a clinical breast examination) and elements related to ability (household income) (Wagner et al., 2000).
Attitudes that are unmistakably cultural and ethnic also influence interest in breast cancer screening. Acculturation and the proportion of a woman’s life spent in the United States are important factors among some immigrant and ethnic populations, such as Korean women (Juon et al., 2000). A study of urban Chinese-American women age 60 and older revealed that acculturation and issues surrounding modesty affected ever having had a screening mammography or a clinical breast examination, and the lack of a physician recommendation affected having it in the past year. Cambodian women, even those with Asian-American physicians, are less likely to be screened if the physician is a man (Tu et al., 2000). Within Hispanic populations, attitudes differ among ethnoregional subgroups (Ramirez et al., 2000b).
Ability Access to health care and insurance coverage are closely correlated with whether women obtain screening mammography. As noted earlier with regard to HEDIS indicators, health maintenance organizations report that large proportions of their female enrollees have received regular screening mammographies. By 1992, 75 percent of women who had been members of the Kaiser Permanente, Northwest Region, health maintenance organization for at least 2 years had undergone a screening mammography (Glass et al., 1996).
The potential for confounding variables in this association is strong, given the linkages between income and private insurance and the tendency of such women to have greater knowledge about breast cancer screening (Takakuwa et al., 2000). Many of the seemingly cultural differences in obtaining screening mammography are functions of poverty and educational status (Facione and Katapodi, 2000). Nonetheless, even after multivariate logistic regression analysis for other preventive health behaviors, education, and socioeconomic status, access to health care and insurance coverage remain independent predictors of screening (Qureshi et al., 2000). Along with low income, they tend to have a disproportionate role as barriers to breast cancer screening among Asian Americans and Pacific Islanders (Coughlin and Uhler, 2000; Kagawa-Singer and Pourat, 2000; Tang et al., 2000).
In an era when screening mammography is increasingly covered by health insurance, it is important to recognize that insurance status is not the only factor limiting the ability of women who want mammograms to obtain them. Other barriers include not knowing the name of their primary care physician (Simon et al., 1998), difficulty with access (King et al., 1995b), and geographic distance from the provider (Hyndman et al., 2000; Taplin et al., 1994).
Reinforcement As with other cancer screening tests, the maintenance of schedules for breast cancer screening is influenced by forgetfulness (Crump et al., 2000). For similar reasons, women forget to perform breast self-examination (Tang et al., 2000).
Interventions to Enhance Breast Cancer Screening
By far, the most extensive research on interventions that improve the effectiveness of cancer screening is in the area of promoting mammography and clinical breast examinations. A 1999 meta-analysis attempted to summarize this evidence by reviewing 43 studies of 63 interventions. It concluded that behavioral interventions increased the rate of breast cancer screening by 13.2 percent (95 percent confidence interval [CI], 4.7 to 21.2 percent). Cognitive interventions that used generic education strategies had little impact, but those that used theory-based education (e.g., health belief model) increased rates of screening by 23.6 percent (95 percent CI, 16.4 to 30.1 percent). Sociological interventions also increased screening rates (Yabroff and Mandelblatt, 1999).
This literature is examined in more detail below by using the four-part knowledge-attitude-ability-reinforcement model as an organizational framework. The interventions are reviewed in terms of their effectiveness in improving screening rates, focusing primarily on evidence from randomized
controlled trials. The incremental benefit of these interventions in improving rates of screening mammography is often marginal in comparison with their costs, yielding various estimates of their cost-effectiveness (Lantz et al., 1996; Saywell et al., 1999; Wagner, 1998). These monetary factors must be considered by health care systems in determining whether the costs per additional mammogram are worth the benefit, but such considerations are not the focus of this review.
Knowledge Interventions Some efforts to promote breast cancer screening rely on dissemination of information about the disease and the importance of screening. Much of this comes through press reports, television and radio broadcasts, articles about breast cancer in women’s magazines, and advertisements. Research by the Annenberg School of Communication has documented the influence of media coverage, independent of physician’s advice, on women’s decisions to have mammograms, especially women without regular access to or contact with a physician (Yanovitzky and Blitz, 2000). One study in Washington state has confirmed the expected correlation between community newspaper advertisements and mammography use (Urban et al., 1995). Others have concluded that messages in the media can heighten awareness and increase behavioral intention but are unlikely to assert their influence beyond awareness of breast cancer screening (Rimer, 1997).
Attitude Interventions The sources of information and promotional messages have important influences on attitudes, and considerable research and programmatic activity have gone into the effort to deliver messages through venues and individuals who have greater credibility with women. Much of this work has targeted the populations that are least adequately screened, including inner-city low-income women, rural women, and women in certain ethnic and minority groups.
Interventions aimed at reminding physicians and health care systems to advise women about the need for screening mammography, an important motivator that shapes women’s attitudes about the importance of screening, also serve as reminder systems when screening is overdue and are therefore reviewed below under “Reinforcement Interventions.” Other studies have engaged other health care professionals in the community in this role. For example, a before-and-after study reported that a program that was conducted by pharmacists and that incorporated risk assessment software and education and training about breast self-examination, clinical breast examination, and mammography was associated with a substantial increase in the rate of adherence to guidelines (Giles et al., 2001).
Some interventions focus on enlisting the aid of individuals familiar to women. A randomized trial sponsored by the American Cancer Society
demonstrated that screening mammography rates increased among women who received a telephone call from a friend offering encouragement to have a mammogram (Calle et al., 1994). Other strategies focus on empowering women to become involved in screening choices. In one study, older women in an urban setting were more likely to have current mammograms because they took an active role and had recurrent participation in screening (Gnanadesigan et al., 2000).
Other interventions tend to be multifaceted and highly coordinated group or community-based efforts that often rely on volunteers and community outreach. Rural communities have used volunteers for individual counseling or community activities (Andersen et al., 2000). In Minneapolis, Minnesota, a randomized trial targeting low-income women in public housing high-rise buildings found that screening rates increased for women living in buildings where health professionals spoke about screening and where community volunteers held small group discussions and the women had an opportunity to request assistance with obtaining mammograms or mammogram reminders (Slater et al., 1998). In Hawaii, Kokua Groups, which provide culturally tailored education to native Hawaiian women in a group setting, have observed some improvements in screening activities (Gotay et al., 2000).
Researchers have worked toward understanding how to more effectively shift attitudes about breast cancer screening by crafting messages with an understanding of different ethnic, racial, and cultural traditions. Research suggests, for example, that African-American women’s intentions to get mammograms following receipt of such messages are influenced by both the message’s arguments and the degree of favorable “peripheral cues” (Kirby et al., 1998). A randomized trial involving inner-city Spanish-speaking Hispanic women found success with a culturally sensitive, linguistically appropriate computerized education program with an interactive soap opera format, the viewers of which demonstrated increased knowledge and altered beliefs about breast cancer compared with controls (Jibaja et al., 2000).
Ability Interventions The same interventions that would eliminate a lack of access to health care and inadequate health insurance as barriers to breast cancer screening are those that would solve these problems for the U.S. health care system in general and are beyond the scope of this review. It is the case that some women—because they misunderstand their insurance coverage status, their covered benefits, or the affordability of obtaining screening without insurance—are under the misconception that these barriers make them unable to be screened. Simply mailing a notice to Medicare beneficiaries indicating that mammography was subsidized under the program was associated with increased rates of utilization (Fox et al., 2001).
Other problems that affect the ability to be screened, such as ease of access and geographical proximity to mammography services, have been eased in some communities by offering screening at nontraditional sites such as workplaces and churches, operating mobile mammography vans, and establishing geographically dispersed imaging facilities (see Box 6.2). The more organized health care systems and managed care plans have developed systems that streamline the process of obtaining referrals and arranging mammography to remove operational impediments that frustrate, delay, or sabotage the efforts of women who want to obtain a mammogram (Taplin et al., 1997a).
Reinforcement Interventions Although some women who know they are due for screening proactively visit their physician or radiology facility to obtain a breast examination and mammogram, it is important that women who are unaware of this need receive timely reminders so that their screening is not delayed. One strategy is for physicians or mammography facilities to mail reminder letters or postcards to patients when their mammogram is due. Studies of the effectiveness of this intervention
|
BOX 6.2 Cancer Screening at Worksites and Places of Worship Worksites Relatively few worksites provide cancer screening services, but screening at worksites represents an opportunity to increase access to screening. As of 1995 an estimated 7 percent of worksites offered cancer screening; and of these, 59 percent offered breast cancer screening, 25 percent offered colorectal screening, and 17 percent offered cervical cancer screening (CDC, 1997b). Occupational health nurses often manage the screening programs, and key organizational factors associated with success in at least some worksites include the endorsement of upper management and the employee’s immediate supervisor (Caplan and Coughlin, 1998). Most worksites that offer breast cancer screening use mobile mammography units (Caplan and Coughlin, 1998; Dershaw et al., 1992; Kessler et al., 1991), which appear to be cost-effective (Schrammel et al., 1998). Few studies, however, have assessed the effectiveness of cancer screening programs at worksites (Hart et al., 1998; Lee, 1983, 1991; Marcus and Crane, 1998; Tilley et al., 1999b; Vernon, 1997), but some evidence suggests that workplace settings could offer a complementary location for the delivery of screening services. Places of Worship Although places of worship are often noted to be key channels for reaching African Americans and Hispanic groups (e.g., Davis et al., 1994; Fisher et al., 1992; Ransdell, 1995), few studies that have evaluated interventions aimed at improving cancer screening at places of worship are available. Results from some church-based efforts appear to be promising (Bailey et al., 2000; Marcus and Crane, 1998), whereas the results of other efforts have been disappointing (Mitchell-Beren et al., 1989). |
have yielded mixed results. Some randomized trials and community studies report a significant improvement in the rate at which women return for mammography (King et al., 1994; Mayer et al., 2000; Urban et al., 1995). A randomized trial in a Philadelphia health maintenance organization found that a birthday card reminder was more effective than a personalized letter from the medical director accompanied by materials promoting mammography (Davis et al., 1997b). A 1998 meta-analysis of 16 articles concluded that women who received reminders were 50 percent more likely to get a mammogram and that tailored letters were more effective than generic reminders (Wagner, 1998). Women with family histories of breast cancer are more likely to obtain mammograms if reminders are tailored to emphasize that history and the consequent increased importance of testing (Curry, 1993).
Other studies have reported more pessimistic results. Randomized trials have reported no benefit when a radiology department (Bodiya et al., 1999) or a health maintenance organization serving urban, predominantly African-American women (Burack et al., 1996) sent reminder letters. A subsequent article from the same research team noted that although 48 percent of the recipients of the reminder letter completed a mammogram within the following year and 72 percent remembered that they had received it, only 5 percent responded to its recommendations (Simon et al., 1998). Having the letter come from the primary care physician rather than the program director had no incremental benefit in one randomized trial, but sending a subsequent reminder postcard doubled screening mammography rates (Taplin et al., 1994).
Some work has focused on the incremental benefit of following reminder letters with telephone contacts that offer reminders or encouragement to obtain a mammogram. These calls are generally made to women who are overdue for a mammogram, have not responded to previous reminders, are older, or are in low-income groups. The results are generally positive; but the magnitude of benefit varies depending on the content of the conversation, motivational techniques, the stage of readiness to change of the women, the number of repeat calls, whether the opportunity to schedule a screening appointment is included, and whether past mammography experiences are discussed (Bodiya et al., 1999; Crane et al., 2000; Davis et al., 1997a; Janz et al., 1997; King et al., 1994, 1995b; Lantz et al., 1995; Ludman et al., 1999; Taplin et al., 2000).
Telephone calls may be more effective than mailed reminders, at least in some trials (Lipkus et al., 2000b). Calls placed by church-based volunteers delivering culturally specific information about mammograms and where to obtain them at low cost appear to attract women who were previously not adherent to screening recommendations (Duan et al., 2000). One randomized trial found that calls by trained counselors focusing on barriers to screening were no more effective than annual mailed reminders but did produce
some modest benefit in the subset of women who had previously undergone mammography (Costanza et al., 2000). Another trial found no difference between a simple reminder telephone call and a motivational call addressing barriers (Taplin et al., 2000). Calls placed by medical assistants from a primary care office appear to be more effective than those placed by physicians and are considerably more cost-effective (Mohler, 1995).
It is important that women who do not receive reminders by mail or telephone or who forget to act on them be reminded to get an examination or mammogram when they visit their primary care physician for other reasons and that they receive assistance in expediting the process. For this to occur efficiently, practices and providers must have in place systems that identify women who are overdue for screening and that remind or prompt providers to notify women who are overdue for screening. In addition, it is important to have in place a streamlined process for obtaining examinations and mammograms that removes impediments that account for failures or delays in screening.
A number of randomized trials have examined different strategies for reconfiguring office and clinic operations and modifying manual or computerized information systems to provide these services in a comprehensive and efficient format. The components of such interventions have included various combinations of on-site training and start-up assistance, patient-administered computer reminder software in the waiting room, office chart reminders (notices placed in the medical record), computerized reminder systems, physician and office staff training to enhance counseling skills, patient health maintenance cards, continuing education seminars, and quality assurance feedback.
These trials have generally reported promising results from such efforts, including improved rates of clinical breast examinations (Manfredi et al., 1998; Williams et al., 1998) and mammograms (Burack and Gimotty, 1997; Litzelman et al., 1993; Williams et al., 1998), although successes were not uniform across practices (Burack et al., 1996). One trial reported an increase in the mention of mammography but not of mammography rates among women who have been the targets of such efforts (Kinsinger et al., 1998). Another trial found the effort no more effective than mailing annual reminders to patients, although it did offer modest incremental benefit among women who had previously had a mammogram (Costanza et al., 2000). One study found that screening rates improved by coupling mammography with completion of a clinical breast examination or a Pap smear (Cummings et al., 2000).
Some interventions focus on easing the difficulties that women face in obtaining referrals to mammographic facilities and arranging their appointments. The barriers are modest (e.g., the inconvenience) for many women but are overwhelming for women who are elderly, have limited
education, or have language barriers or other difficulties that make it difficult to navigate the health care system. One strategy to reduce the inconvenience is to arrange same-day mammography services for women who are advised to have a mammogram. Such programs have improved screening rates in urban academic general medicine practices (Dolan et al., 1999). A British study suggests that fixed appointments are more effective than inviting women to telephone to make their own arrangements (Stead et al., 1998).
More intensive assistance (case management) in obtaining mammograms has been evaluated in settings where obtaining mammograms is especially difficult. For example, a primary care referral project operating within an urban emergency department improved screening rates by offering older minority women a brief motivational interview and a mammography referral and scheduling a next-day, no-cost appointment (Bernstein et al., 2000). A randomized trial reported a tripling of mammography rates among inner-city women by offering case management by culturally sensitive community health educators (Weber and Reilly, 1997). Case management at senior citizens’ housing facilities encouraged mammography through the distribution of a Medicare mammography benefit flier, community education, and arrangements for mammography appointments and transportation, but primarily among women who were already predisposed to having the test. The investigators suggested that individual targeted interventions may be needed for women who have not had or who do not wish to have a mammogram (King et al., 1998).
Multiple interventions directed at patients, physicians, the health care system, and the community may provide the best approach to improving rates of screening for breast cancer (Rimer, 1997). In one review, 33 percent of studies that used single interventions and 85 percent of multicomponent trials were associated with increased rates of screening (Rimer, 1994). Diverse strategies, such as patient and community education, enabling legislation, and efficacious screening technology, can play independent yet synergistic roles (Zapka, 1994; Montano et al., 1997). According to one meta-analysis, all types of provider-targeted strategies to increase use of mammography were found to be effective, but those targeting both patients and providers were not significantly better at increasing screening than those targeting providers alone (Mandelblatt and Yabroff, 1999). The behavior involved in obtaining mammograms is complex, and it is usually not sufficient to solely target women. Without a physician recommendation, the behavior might not be enabled. Without access-enhancing and cost-reducing strategies, even a physician recommendation might not be enough (Rimer, 1994).

SOURCE: Centers for Disease Control and Prevention.
Prostate Cancer Screening
Awareness of prostate cancer in the United States has increased significantly in association with public education campaigns, media attention, and advocacy spearheaded by celebrities and prominent national figures. Screening for prostate cancer by testing for PSA is increasingly common in the United States. According to one survey, 87 percent of family physicians and 98 percent of urologists reported using the test for screening (McKnight et al., 1996). Studies conducted by the New York State Department of Health suggest that 60 to 64 percent of men age 50 and older have heard of the PSA test and have had it done (Smith et al., 2001). A 1997 survey in Texas revealed that 37 percent of men age 40 or older had received the PSA test (CDC, 2000b).
Given the controversy surrounding the appropriateness of PSA screening, it is unclear whether failure to be screened is properly viewed as a “gap” in care or carries the same public health significance as gaps in receiving tests with proven benefits in terms of reducing rates of mortality (e.g., colorectal, breast, and cervical cancer screening).
In fact, recent data support concerns about excessive PSA screening in the United States. Men for whom most professional organizations do not recommend PSA screening are receiving this test. Examples of such categories include men older than age 75, asymptomatic men with a life expectancy of less than 10 years, asymptomatic men with no risk factors who are younger than age 50, and men with risk factors before age 40. Studies report that 17 to 21 percent of PSA tests are ordered for such men (McNaughton Collins et al., 2000; Poteat et al., 2000). Although some of this testing probably represents a response to high patient demands or efforts by physicians to minimize medicolegal liability, to some extent it represents physicians’ misconceptions about appropriate indications. In one survey, 16 percent of urologists and 43 percent of radiation oncologists recommended routine PSA testing in men with a life expectancy of less than 10 years (Fowler et al., 2000). This tendency is not limited to specialists. In one survey, 65 percent of primary care physicians reported “almost always” ordering a PSA test for men aged 70 to 74; 53 percent reported doing so for men aged 80 and older (Barry et al., 1996).
Even for men for whom current guidelines consider screening appropriate (for a description of current guidelines, see Box 5.4 in Chapter 5), what is advised is shared decision making rather than routine testing. Yet patients often undergo PSA screening without receiving any information about the consequences and sometimes without even being told that they received the test. In one study, more than 50 percent of men who had undergone PSA screening 2 weeks earlier said that they had not heard of the test and were unaware that they had received it (Diefenbach et al., 1996). As long ago as 1995, when PSA screening was less entrenched, 55 percent of primary care physicians reported ordering the PSA test “often” or “always” as part of the periodic health examination (Austin et al., 1997). In a study discussed in Chapter 5, a recent survey of internists found that only 17 percent consider patient preferences before ordering a PSA test (Dunn et al., 2001).
Randomized trials involving videotapes and pamphlet aids on the decision to undergo PSA screening have consistently demonstrated their effectiveness in improving patients’ knowledge about the test (Flood et al., 1996; Schapira and VanRuiswyk, 2000; Volk et al., 1999). In most cases the intervention resulted in a statistically significant reduction in the rates of PSA testing (Flood et al., 1996; Schapira and VanRuiswyk, 2000; Volk et al., 1999; Wilkins et al., 1999), on average reducing interest in undergoing PSA screening by 65 percent (Volk and Spann, 2000).
Cervical Cancer Screening
Size of the Gap
The proven efficacy of cervical cancer screening and its remarkable success in reducing the disease to being an uncommon cause of cancer death in the United States have focused attention on screening failures as the primary cause of continued deaths from this disease. It has been estimated that 60 percent of cases of cervical cancer are associated with absent or deficient screening (Sawaya and Grimes, 1999). As of 1999, 88 percent of women ages 18 to 44 and 81 percent of women ages 45 or older have received a Pap smear within the past 3 years (CDC, Behavioral Risk Factor Surveillance System, 2000). The fact that more than 80 percent of women have had a Pap smear within the past 3 years is encouraging, but considerable progress needs to be made to achieve the goal set forth in Healthy People 2010 (US DHHS and Office of Disease Prevention and Health Promotion, 2000), that is, for 90 percent of all women ages 18 and over to have had a Pap smear screen within the past 3 years.
The proportions of women who have had a Pap smear within the previous 3 years decline with age: among women ages 55 to 64, 65 to 74, and 75 and older, the median proportions across states are 83, 77, and 58 percent, respectively (CDC, 1999c). Other analyses show that higher income levels and higher levels of educational attainment are associated with an increased likelihood that eligible women have had a Pap test within the past 3 years (Blackman et al., 1999).
The probability of having had a Pap test within the past 3 years is 85 percent for whites, 91 percent for African Americans, 81 percent for Hispanics, and 95 percent for American Indians (CDC, Behavioral Risk Factor Surveillance System, 2000). Cervical cancer screening rates are significantly reduced among Asian Americans and Pacific Islanders (Kagawa-Singer and Pourat, 2000). For the period from 1994 to 1997, approximately 74 percent of women in these groups who were age 18 or older (and who had not undergone a hysterectomy) had received a Pap smear within the past 3 years (Coughlin and Uhler, 2000). Only 50 percent of Korean-American women have had a Pap smear in the past 2 years (Juon et al., 2000). American Indian women are more likely than others to report never having had a Pap test and to have a higher proportion of abnormal results (Benar et al., 2001). In a study of American Indians with diabetes, some Indian Health Service centers reported that as few as 26 percent of women had received a Pap smear test in the last year (Giroux et al., 2000).
Follow-up for an abnormal screening test result is an extremely important step in the cancer control process, yet many women fail to receive timely or any resolution of an abnormal screening test result. In one study, rates of nonresolution varied considerably across settings and populations, ranging between 7 and 49 percent (Yabroff et al., 2000). Factors associated
with incomplete or delayed follow-up included younger patient age, financial barriers, lower education and income levels, non-white race, and certain psychosocial characteristics.
Predictors of Screening
Knowledge Most American women are familiar with cervical cancer screening and consider the Pap smear and pelvic examination a standard component of the well-woman examination. It is less likely that they have an accurate understanding of screening guidelines, in particular, the lack of necessity for annual or more frequent screening. The level of knowledge about cervical cancer screening is lower among certain socioeconomic and ethnic groups. A telephone survey of Hispanic women demonstrated that the proportions of individuals who had knowledge of guidelines ranged from 41 percent for Puerto Ricans to 56 percent for Cubans (Ramirez et al., 2000a). Follow-up for an abnormal Pap smear is associated with a memory of being informed of the test results (McKee et al., 1999) and understanding the purpose of colposcopy (Lerman et al., 1992).
Attitudes Several studies have demonstrated that poor adherence to cervical cancer screening is associated with attitudinal factors, such as fear of cancer and treatment (Khanna and Phillips, 2001; Lerman et al., 1992), but some have suggested that poor adherence is not associated with such factors (McKee et al., 1999). In Hispanic and Latino cultures, especially among Mexican Americans, Central Americans, and Cubans, social integration networks have a significant influence on cervical cancer screening rates (Suarez et al., 2000).
Ability As with the other screening tests evaluated in this chapter, insurance coverage, access to care, time, money, and transportation are important determinants of Pap smear use and adequate follow-up (Lerman et al., 1992). A lack of insurance, a low level of income, and a lack of a usual source of health care appear to play disproportionate roles as barriers to cervical cancer screening among Asian Americans and Pacific Islanders (Coughlin and Uhler, 2000; Kagawa-Singer and Pourat, 2000).
Reinforcement Many women have difficulty remembering how much time has elapsed since their last Pap smear and become overdue for screening. A lack of follow-up for abnormal smears has been linked to forgetting the appointment (Lerman et al., 1992).
Interventions to Enhance Cervical Cancer Screening
The review conducted for this chapter found little current evidence regarding the effectiveness of interventions to influence the knowledge or attitudes of women about cervical cancer screening or their ability to obtain
the tests. Studies have examined reinforcement interventions. Randomized trials have not found physician or patient reminders to be particularly effective in improving cervical cancer screening rates (Buehler and Parsons, 1997; Burack et al., 1998; Ward and Proude, 1999), but the statistical powers of some studies may have been limited. A meta-analysis of randomized controlled trials assessing the value of patient letter reminders concluded that they increase the rate of cervical cancer screening, but are less effective among lower socioeconomic groups (Tseng et al, 2001). At least one randomized trial indicated that the combination of a physician reminder letter and a telephone contact increased the rate of Pap smear testing (Lantz et al., 1995). Another randomized trial involving low-income minority women who had received an abnormal Pap smear result reported higher rates of follow-up from telephone calls about the need for follow-up colposcopy (Miller et al., 1997).
Comprehensive office system changes such as those described above for breast cancer screening have proved effective in increasing Pap smear testing rates (Manfredi et al., 1998). One randomized trial reported higher Pap smear testing rates among Vietnamese women by use of such a program that also included Vietnamese-language educational materials, newsletters, and oncology data-query programs (Nguyen et al., 2000).
Some evidence suggests that lay health advisers can effectively promote cervical cancer screening (Dignan et al., 1996; Marcus and Crane, 1998). The use of such outreach staff may be enhanced when their work is coordinated with existing resources in the community, such as residents of low-income housing, and door-to-door recruitment (Davis et al., 1994; Dignan et al., 1996; Dunn and Sprunt, 1955; Evans et al., 1980; Hulka, 1966, 1967). The use of outreach clinics or mobile examination rooms also appears to increase rates of screening (Satariano et al., 1982; White et al., 1990). Educational campaigns to promote these clinics are required to ensure increases in rates of screening (Hirst et al., 1990; Holland et al., 1993).
PRIORITIZING CANCER SCREENING
Limited resources, both personal and economic, make it necessary for providers, health care systems, payers, and patients to set priorities in cancer screening. Ideally, this would be determined by knowing which approaches to cancer screening are most likely to improve health. From the patient’s perspective, it would be useful to know whether one screening test may reduce the risk of premature death more substantially than another. Policy makers would benefit from knowing whether more gain in health is purchased by intensifying delivery of a particular screening test (e.g., introducing more frequent or more accurate testing or expanding coverage of screening to populations with limited access) or by directing resources to other screening maneuvers.
Given the larger goal of preventing premature death from cancer, consideration might also be given to the relative benefits of focusing on primary prevention over screening. Resources directed at smoking cessation and the consumption of a healthy diet might offer greater incremental benefits than the intensification of screening campaigns. The even larger aim of preventing premature morbidity and mortality might be achieved by directing resources to the prevention of coronary artery disease, stroke, or diabetes rather than optimizing the delivery of cancer screening tests. Studies indicate that as many disability-adjusted life years are claimed by road traffic collisions as by lung cancer (Michaud et al., 2001). Directing public resources toward effective injury prevention strategies might ultimately save more lives.
The modeling tools needed to make definitive comparisons of the relative health benefits of preventive maneuvers are not fully developed, offering patients, providers, and policy makers limited data with which to set priorities. Progress in this area has been inhibited by the paucity of firm data and methodological difficulties in arriving at valid projections. Even the crude modeling efforts undertaken thus far, however, hint at the relative importance of competing priorities in terms of preventive maneuvers. By one analysis, for example, closing the gap in the proportion of Americans who receive annual FOBT and screening mammography would prevent 9,632 and 4,475 deaths per year, respectively, whereas eliminating cigarette smoking would prevent 328,044 deaths (Woolf, 1999). By application of the same model to a hypothetical 45-year-old woman who smokes, the probability that stopping smoking would prevent her death before age 75 is 10.9 percent, whereas the probability that mammography every 1 to 2 years would do so would be 0.5 percent.
A modeling effort undertaken by the Partnership for Prevention in collaboration with the CDC and the Health Care Financing Administration (now called the Centers for Medicare and Medicaid Services) compared prevention services on the basis of preventable burden, the burden of disease that could be reduced if the service was delivered to 100 percent of the target population. The numbers of quality-adjusted life years (QALYs) that could be added by optimizing screening according to this model were 357,554 for cervical cancer, 293,092 for colorectal cancer, and 268,780 for breast cancer. By comparison, screening for high cholesterol levels would add 585,000 QALYs (Coffield et al., 2001).
The broadest approach to priority setting would take account of the other determinants of health, such as income disparities and inadequate education. Given the documented disadvantage that certain populations face in overcoming the burden of cancer and other chronic diseases, it is conceivable that efforts directed at improving access to health care and correcting social impediments to self-care and productivity (e.g., improving education and job security) might accomplish more in reducing rates
of morbidity and mortality than investing further in refining screening technologies.
SUMMARY AND CONCLUSIONS
The possible benefit of cancer screening in the United States falls far short of its potential, costing health and lives. The lost opportunities take several forms: a substantial proportion of eligible persons are never screened or are screened too infrequently to achieve early detection, those who are screened may not be screened well, and the follow-up steps for abnormal results are often inadequate.
Inadequate screening occurs more commonly among certain segments of the population. Age, socioeconomic status, race or ethnicity, education, and health status account for marked disparities in the access of Americans to cancer screening tests. Older women, for example, are less likely than younger women to be screened for breast and cervical cancer (Mandelblatt and Yabroff, 2000). Women who do not receive breast cancer screening are also less likely to undergo cervical cancer screening (Cummings et al., 2000; Glasgow et al., 2000). Screening is also less common among low-income households and those with limited education or limited or no health insurance.
Members of certain ethnic and racial groups are significantly more likely to develop cancer and suffer higher mortality rates than whites. The reasons for this are not entirely clear but are certainly multifactorial. One important contributor may be the disproportionate difficulties that these individuals face in obtaining cancer screening. For virtually every cancer reviewed in this report, certain ethnic and racial minorities are less likely to be screened, making early detection less likely.
The complex interrelationships among the demographic variables mentioned above—income, education, and race and ethnicity—make it difficult to know the extent to which the reasons for inadequate screening are racial or ethnic status itself rather than the socioeconomic characteristics with which racial or ethnic status is often associated. An extensive body of social epidemiological research has examined this issue (Berkman and Kawachi, 2000), and data support the concern that race and ethnicity influence cancer screening even after adjustment for these cofactors (Smith, 1998; Institute of Medicine, 1999b).
Underuse of cancer screening is not the only problem in the United States. Overuse of screening tests (the widespread performance of screening tests that are not recommended or the performance of testing too frequently) potentially exposes patients to net harm and consumes resources needed for more effective health care, including cancer screening services for high-risk groups. Examples of overuse include the use of routine chest radiographs to screen for lung cancer or the rising use of whole-body
computed tomography scanning to screen for various cancers and other health conditions (Smith, 2001) (see Chapter 7). Excessive levels of resource consumption and rates of false-positive test results are also amplified when screening is performed too frequently, such as when Pap smears are performed every 6 months.
To enhance the use of effective screening tests, multilevel approaches are recommended. Optimization of the delivery of effective cancer screening services and reductions in the numbers of inappropriate tests that are performed lie in changing the behaviors of the following:
-
systems of care, to make cancer screening services available to eligible populations;
-
health care providers, to perform cancer screening as recommended, on time, and with skill when they encounter patients eligible for screening; and
-
individuals, to obtain recommended screening tests and to pursue follow-up.
Elimination of financial and access barriers to screening improves screening rates, for example, through the use of health insurance coverage, reduced cost sharing, and the availability of free screening at public clinics. In addition, certain organizational innovations are tied to improved rates of screening, such as the implementation of office systems to prompt health care providers to recommend screening, facilitate referrals, and remind patients and providers of the need for rescreening. Other opportunities to improve screening rates, particularly among underserved populations, include the use of nurses to provide outreach and education, case management, and facilitation. Increased opportunities for the provision of screening in health care settings (e.g., screening in emergency departments and screening during acute care visits) and the encouragement and provision of screening in nontraditional settings such as worksites and places of worship also hold some promise, although evidence of their effectiveness is limited.
Evidence suggests that multistrategy interventions are more effective than any one intervention alone (Sin and Leger, 1999). Examples include programs that integrate case management by culturally sensitive community health educators and the print or other media to communicate the benefits of mammography, general education of the community regarding screening, and the handling of logistic barriers by arranging appointments for mammography and transportation to those appointments (King et al., 1998; Weber and Reilly, 1997). Systematic and integrated approaches such as these offer great promise in the effort to optimize the quality and timeliness of cancer screening available to Americans.



































