11
Findings, Policy Implications, and Recommendations
The nation needs new strategies to prevent cancer and, when cancer occurs, to catch it at its earliest stages. The failure to implement proven methods of cancer prevention and early detection results in more than 60,000 premature deaths each year. Behavioral interventions and cancer screening work; but they have not been fully adopted by individuals, physicians, health care systems, and society at large.
Much of the recent decline in U.S. cancer death rates is a result of cancer prevention and early detection, but more progress is possible by simply implementing known interventions. A 19 percent decline in the rate at which new cancer cases occur and a 29 percent decline in the rate of cancer deaths could potentially be achieved by 2015 if efforts to help people change their behaviors that put them at risk were stepped up and if behavioral change were sustained. Smoking, obesity, sedentary lifestyles, alcohol use, and failure to get screened for cancer all contribute to the excess burden of cancer. The possible reductions in cancer incidence are particularly striking for certain cancers: accelerated changes in risk behavior of a magnitude that is feasible by the application of current knowledge could reduce the number of colorectal cancer cases by up to 33 percent and halve the number of smoking-related cancer cases such as lung cancer. The health benefits of such behavioral change extend well beyond cancer, however. Significant reductions in the rates of cardiovascular disease and diabetes would also occur with the adoption of healthier lifestyles.
To save the most lives from cancer, health care providers, health plans, insurers, employers, policy makers, and researchers should be concentrating their resources on helping people to stop smoking, maintain a healthy
weight and diet, exercise regularly, keep alcohol consumption at low to moderate levels, and get screening tests for cancer that have proven effectiveness. Doing so could shift the balance away from the current devotion of attention and resources to the treatment of advanced disease to more effective prevention (Woolf, 1999).
In this chapter, the National Cancer Policy Board summarizes the evidence presented in the report to address four questions:
-
What lifestyle and health care behaviors contribute to the burden of cancer?
-
What share of new cases of cancer and cancer deaths could be prevented with changes in lifestyle and health care behavior?
-
What interventions work to bring about health-enhancing behavioral change?
-
What steps can be taken to overcome barriers to using effective interventions and to improve what we know about cancer prevention and early detection?
WHAT LIFESTYLE AND HEALTH CARE BEHAVIORS CONTRIBUTE TO THE BURDEN OF CANCER?
The Board recognized that a number of personal and health care behaviors are known to contribute to the burden of cancer but limited its review to tobacco use, obesity, physical activity, diet, alcohol use, and the use of screening tests. Examples of behaviors known to contribute to cancer risk but not considered in this report, include exposure to sun and exposure to cancer-causing viruses through sexual activity (e.g., human papillomavirus) and blood contact such as through intravenous drug use (e.g., hepatitis B virus).
Tobacco Use
Tobacco is responsible for approximately 30 percent of cancer deaths in the United States, an estimated 170,000 deaths in 2002 (ACS, 2002a). A causal link between smoking and lung and laryngeal cancer was first made public in the 1964 Surgeon General’s report, Smoking and Health (U.S. Department of Health Education and Welfare, 1964). Since then convincing evidence has accumulated to support smoking as a cause of several cancers including cancers of the oral cavity, esophagus, bladder, kidney, pancreas, cervix, colon, and stomach, and leukemia.
Smoking increases the risk of lung cancer 10- to 20-fold and the risk of other cancers up to 5-fold, depending on an individual’s smoking habits and history. Although the lung cancer risk in former smokers never quite returns to that for individuals who have never smoked, it is drastically
reduced. There are substantial health benefits for smokers who quit. A person who quits smoking before age 50, for example, has, on average, half the mortality risk of dying in the next 15 years compared with the risk for those who continue to smoke.
Obesity
Overweight, as indicated by a body mass index (BMI; weight [in kilograms] divided by height [in meters] squared) of 25.0 to 29.9, and obesity, as indicated by a BMI of =30.0, contribute an estimated 10 percent to the cancer mortality rate among men and 15 to 20 percent to the cancer mortality rate among women. There is convincing evidence that obesity contributes to a higher incidence of esophageal, breast, endometrial, colon, and kidney cancer. The high risk of esophageal cancer associated with obesity is likely due to its relationship with gastroesophageal reflux, a risk factor for esophageal adenocarcinomas. Obesity—or more precisely, excess body fat (adiposity)—affects levels of female hormones, which are known to affect the risk for breast and uterine cancers. Obesity may also modify insulin pathways, which, in turn, may affect colon cancer. The degree to which obesity elevates risk varies by cancer site. The elevation in risk is very large (a fivefold increase in risk) in the case of esophageal cancer, large (a two- to fourfold increase in risk) for cancers of the breast and uterus, and moderate (a 35 percent to twofold increase in risk) for colon cancer.
Physical Activity
Physical activity is associated with a 10 to 25 percent reduction in the risk for breast cancer and a potential 25 to 50 percent reduction in the risk for colon cancer. Although an association between cancer and physical activity is established, the mechanisms whereby physical activity reduce risk of cancer are not fully known.
Diet
There is clear and convincing evidence that a diet rich in plant foods and moderate in animal products lowers the risk of cardiovascular disease, diabetes, and other important outcomes, but evidence linking specific aspects of the diet to cancer risk is inconsistent. Recent evidence from large prospective studies, for example, has not consistently shown a reduced risk of cancer for those who consume large amounts of fruits and vegetables or small amounts of red meat, although a large number of case-control studies have shown those relationships. There is a growing body of evidence that certain nutritional components of foods affect cancer risk (e.g., calcium or
folate and colorectal cancer), but further research is needed to confirm these specific associations.
Alcohol
A downward shift in the population distribution of alcohol intake could lead to decreases in the incidence of cancer and injuries, but it could also lead to higher rates of cardiovascular disease because consumption of moderate amounts of alcohol confers some protection against cardiovascular disease. Public education campaigns must focus on reductions in hazardous drinking and encouraging those who choose to drink to do so moderately.
Use of Cancer Screening
A core consensus has emerged about the appropriateness of some methods of cancer screening. There is essentially universal agreement across organizations that all adults age 50 and older should be screened for colorectal cancer, that all women should receive mammograms every 1 to 2 years beginning at least by age 50, and that cervical cancer screening should occur regularly in all sexually active women with a cervix. Appropriate use of screening could reduce the rate of mortality from colorectal cancer by 30 to 80 percent (among adults age 50 and older), reduce the rate of mortality from breast cancer by 25 to 30 percent (among women age 50 and older), and reduce the rate of mortality from cervical cancer by 20 to 60 percent (among women age 18 and older).
WHAT SHARE OF NEW CASES OF CANCER AND CANCER DEATHS COULD BE PREVENTED WITH CHANGES IN LIFESTYLE AND HEALTH CARE BEHAVIORS?
Projections of the precise number of cancer cases and cancer deaths that could be averted with changes in individuals’ health behaviors are difficult to make, but recent estimates suggest that if current trends toward a decline in the prevalence of cancer risk factors continue over the next decade, by the year 2015 one could expect a 13 percent decline in cancer incidence rates and a 21 percent decline in cancer mortality rates below those in 1990. With redoubled efforts to reduce the prevalence of known cancer risk factors further, by the year 2015, cancer incidence rates could be reduced by 19 percent and cancer mortality rates could be reduced by 29 percent. Such redoubled efforts would equate to the prevention of approximately 100,000 cancer cases and 60,000 cancer deaths each year by the year 2015 (Byers et al., 1999).
More than half of the estimated future gains are attributable to projected reductions in tobacco use. Although it is difficult to predict the future
success of public health measures to reduce tobacco use, much progress has already been made. The rate of smoking among adult males has been nearly halved, to 26 percent in 1998 from 51 percent in 1965. Among adult females during this period, the prevalence of smoking has dropped to 22 percent in 1998 from 34 percent in 1965 (National Center for Health Statistics, 2000). It is these trends that are largely responsible for the recent declines in the numbers of deaths from all cancers—the first such decline ever recorded. Following years of steady decline, rates of smoking among adults appear to have leveled off in the 1990s, however.
Smoking cessation has major and immediate health benefits for men and women of all ages and for those who smoke at all levels. There is alarming evidence, however, that the rate of smoking is increasing among adolescents, giving rise to a new generation of adults whose health will be at risk. In 1999, as many as 35 percent of adolescents in grades 9 to 12 smoked (US DHHS and Office of Disease Prevention and Health Promotion, 2000) (Figure 11.1). Almost half of adolescents who continue smoking regularly will eventually die from a smoking-related illness.
As America becomes increasingly diverse, lifestyle trends within some subpopulations are troubling. After years of declining rates of smoking
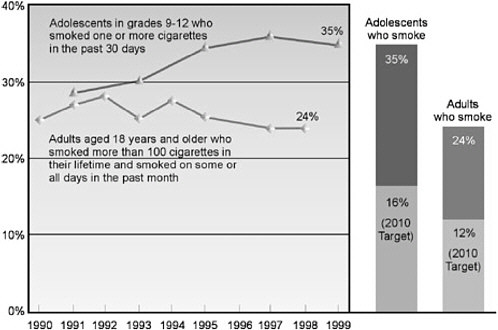
FIGURE 11.1 Cigarette smoking, United States, 1990–1999.
SOURCE: US DHHS and Office of Disease Prevention and Health Promotion, 2000.
among adolescents during the 1970s and 1980s, rates of cigarette smoking among white, African-American, and Hispanic high school students increased in the 1990s (US DHHS and Office of Disease Prevention and Health Promotion, 2000). In 1999, 39 percent of white high school students smoked cigarettes, whereas the rates were 33 percent for Hispanics and 20 percent for African Americans.
Among adults, American Indians and Alaska Natives, blue-collar workers, and military personnel have the highest rates of smoking (US DHHS and Office of Disease Prevention and Health Promotion, 2000). Lower incomes and lower levels of educational attainment are also linked to higher smoking rates among adults. Hispanic adults have relatively low rates of smoking, but analyses of smoking patterns by immigration status suggest that rates of smoking will likely increase among Hispanics because, over time, migrants tend to adopt the poorer health habits of the U.S. general population.
The levels of physical inactivity among Americans also pose a great threat to health. More than 60 percent of American adults are not regularly physically active (28 percent are not active at all), and physical activity levels continue to decline dramatically even in adolescents (US DHHS, 1996; CDC, 2001b). Groups with relatively low rates of physical activity include women, individuals with lower incomes and less education, African Americans, Hispanics, and elderly people. The major barriers that most people face when trying to increase physical activity are lack of time, lack of access to convenient facilities, and lack of safe environments in which to be active (US DHHS and Office of Disease Prevention and Health Promotion, 2000).
More than 1 in 10 children and more than half of adults in the United States are overweight or obese, representing sharp increases in rates of obesity over the last three decades (US DHHS and Office of Disease Prevention and Health Promotion, 2000). Trends are particularly alarming for children and adolescents (Figure 11.2).
Obesity is a result of a complex array of social, behavioral, cultural, environmental, physiological, and genetic factors and is especially prevalent among those with lower incomes. The prevalence of obesity is very high among African-American and Mexican-American women. The proportion of adolescents from poor households who are overweight or obese is twice that of adolescents from middle- and high-income households.
Many aspects of U.S. culture and society over the past few decades have discouraged youth physical activity, including the following (CDC, Division of Adolescent and School Health, 2000):
-
Community designs centered around the automobile have discouraged walking and bicycling and have made it more difficult for children to get together to play.
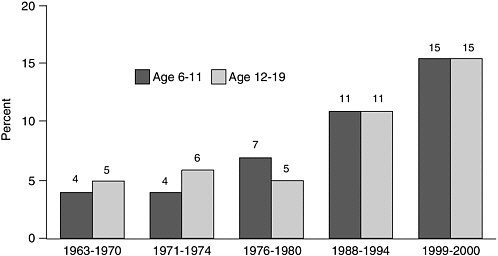
FIGURE 11.2 Prevalence of overweight among children and adolescents: United States, 1963–1970 to 1999–2000.
NOTE: Excludes pregnant women starting with 1971-1974. Pregnancy status not available for 1963-1965 and 1966-1970. Data for 1963-1965 are for children 6-11 years of age; data for 1966-1970 are for adolescents 12-17 years of age, not 12-19 years.
SOURCE: http://www.cdc.gov/nchs/products/pubs/pubd/hestats/overwght99.htm.
-
Increased concerns about safety have limited the times and places available to children to play outside.
-
New technology has conditioned young people to be less active, whereas new electronic media (e.g., video and computer games and cable and satellite television) have made sedentary activities more appealing.
-
States and school districts have reduced the amounts of time that students are required to spend in physical education classes.
-
Communities have failed to invest adequately in physical activity facilities (e.g., parks and recreation centers) close to places where children live.
The potential benefits of cancer screening in the United States fall far short of being achieved, costing health and lives. The lost opportunities take several forms: a substantial proportion of eligible people are never screened or are screened too infrequently to achieve early detection, those who are screened are not screened well, and the follow-up steps for abnormal results are often inadequate. Inadequate screening occurs more commonly among certain segments of the population. Insurance status, age, socioeconomic status, race, ethnicity, and education account for marked disparities in the access of Americans to cancer screening tests. Rates of screening of women for breast and cervical cancer are relatively high. Re-
cent estimates are that more than 60 percent of women age 50 and older have had a mammogram in the past year and that more than 80 percent of women age 18 and older have had a Pap test in the past 3 years. In contrast, only 40 percent of adults ages 50 and older report ever having had a screening test for colorectal cancer.
WHAT INTERVENTIONS WORK TO BRING ABOUT HEALTH-ENHANCING BEHAVIORAL CHANGE?
In its review of the literature on the effectiveness of interventions to change health behaviors, the Board encountered a recurring theme: programs are most successful if they intervene at multiple levels. To effectively make populationwide improvements in the major behavioral risk factors, changes must occur on many different social levels, and the policy recommendations in this report reflect this fact. They aim to create a prevention-oriented environment that makes risk reduction behaviors easier for individuals to choose. It is not enough, however, to assume that individuals who are educated about their cancer risk will modify their behavior to lower their risk (US DHHS, 1994).
Barriers to behavioral change exist not only at the individual level but also at the community level and within the broader social milieu. Broad social movements are needed if health behavioral changes are to be stimulated and sustained at the population level. Because U.S. society is heterogeneous, composed of persons of different racial, ethnic, and socioeconomic backgrounds, these social movements will of necessity be heterogeneous as well. It is only through such large-scale movements that barriers to healthy behavior (including economic, social, political, cultural, and psychological barriers) can be eliminated at the population level.
A comprehensive program to change a population’s cancer risk profile should engage individuals, health care providers, organizations, and whole communities. This finding reiterates a conclusion reached by the Institute of Medicine’s Committee on Capitalizing on Social Science and Behavioral Research to Improve the Public’s Health. In its 2000 report, Promoting Health: Intervention Strategies from Social and Behavioral Research (Institute of Medicine, 2000b), the committee concluded that “interventions on social and behavioral risk factors should link multiple levels of influence, individual, interpersonal, institutional, community, and policy levels” (Institute of Medicine, 2000b, p. 7).
Tobacco Use
Certain states such as California and Massachusetts have implemented comprehensive tobacco control programs and have achieved some important milestones: sharp reductions in smoking and declines in rates of chronic
illnesses associated with smoking such as cardiovascular disease and, more recently, lung cancer. Further reductions in the cancer burden are expected as the programs are in place for longer periods. The Board concluded in its 2000 report, State Programs Can Reduce Tobacco Use, that such programs are successful and should serve as models for other states (Institute of Medicine, 2000e).
A general consensus on what works in tobacco control has been reached by several organizations charged with reviewing the evidence of program effectiveness (e.g., the Task Force on Community Preventive Services, the Office of the Surgeon General, the U.S. Preventive Services Task Force, the Agency for Healthcare Research and Quality) (Hopkins et al., 2001a; Wasserman, 2001) (Box 11.1).
|
BOX 11.1 Interventions Recognized as Effective Against Smoking and Promoted by National Organizations To reduce youth initiation of smoking:
To decrease the effects of environmental tobacco smoke:
To assist with smoking cessation from a population orientation:
To assist with smoking cessation from a clinical perspective:
SOURCE: Wasserman (2001) and Hopkins et al. (2001a,b). |
Physical Activity and Healthy Weight and Diet
Relative to tobacco use, less is known about what interventions work to maintain a healthy diet, increase levels of activity, and reduce obesity, and there is less experience with such interventions. Efforts to maintain a healthy weight should start early in childhood and continue throughout adulthood, as this is likely to be more successful than efforts to lose substantial amounts of weight and maintain weight loss once obesity is established. It is also recognized that a healthy diet and regular physical activity are both important for the maintenance of a healthy weight. Over time, even a small decrease in the numbers of calories consumed and a small increase in physical activity can help prevent weight gain or facilitate weight loss.
It is recommended that obese individuals who are trying to lose substantial amounts of weight seek the guidance of a health care provider (US DHHS and Office of Disease Prevention and Health Promotion, 2000). Worksite fitness programs have resulted in increased levels of physical activity among employees, and it is recognized that environmental policies related to zoning, land use, safety, and transportation greatly affect opportunities for exercise. Among youth, school policies regarding physical education requirements and the availability of after-school recreational programs and facilities affect rates of participation in exercise before and after school.
It is clear that efforts targeted only to individuals cannot be fully effective to prevent or manage obesity or increase physical activity. Governments, the food industry, international agencies, the media, communities, and individuals all need to work together to modify the environment so that it is less conducive to weight gain and more supportive of physical activity (World Health Organization, 1998).
Cancer Screening
To enhance the use of screening, multilevel approaches are also recommended. Optimizing the delivery of effective cancer screening services and reducing inappropriate testing lie in changing the behaviors of
-
systems of care, to make cancer screening services available to eligible populations;
-
health care providers, to perform cancer screening as recommended, on time, and with skill when they encounter patients eligible for screening; and
-
individuals, to obtain recommended screening tests and pursue follow-up.
The elimination of financial and access barriers to screening improves screening rates. These barriers can be reduced, for example, through health insurance coverage, reduced cost sharing, and the availability of free screening at public clinics. In addition, certain organizational innovations are tied to improved screening performance, such as the implementation of systems to prompt providers to recommend screening, facilitate referrals, and remind patients and providers of the need for rescreening. Other opportunities to improve screening rates, particularly among underserved populations, include outreach and education, case management, and facilitation of referrals.
WHAT STEPS CAN BE TAKEN TO OVERCOME BARRIERS TO USING EFFECTIVE INTERVENTIONS AND TO IMPROVE WHAT WE KNOW ABOUT CANCER PREVENTION AND EARLY DETECTION?
The Board recommends that the following steps be taken to increase the rate of adoption, the reach, and the impacts of evidence-based cancer prevention and early detection interventions.
Recommendation 1: The U.S. Congress and state legislatures should enact and provide funding for enforcement of laws to substantially reduce and ultimately eliminate the adverse public health consequences of tobacco use and exposure.
Tobacco is the greatest contributor to deaths from cancer, and reduction in tobacco use offers the greatest opportunity to reduce the incidence, morbidity, and mortality of cancer. Specific actions that would be effective include the following:
-
Taxation is the single most effective method of reducing the demand for tobacco (IOM 2000a). States should set sufficiently high levels of excise taxation on tobacco products to discourage tobacco use, but levels should not be so high that they encourage significant tax avoidance activities.
-
States should allocate sufficient funds from the Tobacco Master Settlement Agreement1 and tobacco excise taxes to support comprehensive, state-based tobacco control efforts consistent with guidelines of the Centers for Disease Control and Prevention (CDC).
The CDC’s Office on Smoking and Health has identified nine essential
elements of a state-level comprehensive tobacco control program (CDC, 1999d):
-
community programs to reduce tobacco use,
-
chronic disease programs to reduce the burden of tobacco-related diseases,
-
school programs,
-
enforcement,
-
statewide programs,
-
countermarketing,
-
cessation programs,
-
surveillance and evaluation, and
-
administration and management.
The estimated annual costs of implementing such a comprehensive program range from $7 to $20 per capita in smaller states (those with populations of less than 3 million), $6 to $12 per capita in medium-sized states (those with populations of 3 million to 7 million), and $5 to $16 per capita in larger states (those with populations of more than 7 million). California and Massachusetts, two states with large-scale and sustained tobacco control programs, fund the program using excise tax revenues and Tobacco Master Settlement Agreement funds. Only eight states (Arizona, Hawaii, Maine, Maryland, Massachusetts, Minnesota, Mississippi, and Ohio) meet these CDC guidelines on recommended levels of support for tobacco control (CDC, 1999d, 2002a). Recent estimates are that only 5 percent of the tobacco settlement monies have been invested in prevention (National Conference of State Legislatures, 2001).
Not all states are contributing money to tobacco control. In at least five states (Connecticut, North Carolina, North Dakota, Pennsylvania, and Tennessee) and the District of Columbia, federal and private funds are the only funds being invested in tobacco control. In at least 20 states, funding from the federal government and the private sector makes up 50 percent or more of the funds being invested. For the country as a whole, the combined resources available in fiscal year 2001 to fund tobacco use prevention and control programs in states total almost $1 billion, but this amount is less than one-sixth of the $8.2 billion that the tobacco industry spent annually in 1999 on promoting and advertising its products (National Conference of State Legislatures, 2001; CDC, 2002b).
Tobacco products cannot by law be sold to those under age 18, but local governments charged with imposing the law generally do not have adequate resources for monitoring and enforcement activities. (www.samhsa.gov/programs/content/brief2001/01csapsynar.htm).
-
States should improve compliance with the provisions of the 1992
-
Synar amendment, which requires that states have sales-to-minor rates of no greater than 20 percent in order to receive federal Substance Abuse Prevention and Treatment Block Grant awards. By 2000, only 25 states had achieved this level of compliance.
-
States should impose tobacco-licensing requirements for merchants selling tobacco products, as recommended in the 2000 report of the Surgeon General (U.S. Department of Health and Human Services and Office of Disease Prevention and Health Promotion, 2000). The threat of revocation of the license as a consequence of selling tobacco products to minors could provide a strong incentive for merchants to comply with existing laws. Further, requiring that merchants pay for a license to sell tobacco could provide needed funds for monitoring and enforcement.
-
Internet sales of tobacco products are not covered by the Synar amendment, which leaves a significant opening for minors to have access to tobacco. More than 90 websites sell cigarettes in the United States, and the number is expected to grow. Furthermore, tobacco products sold over the Internet are often not subject to state sales taxes, making them much less expensive than their counterparts sold in retail stores. Congress should therefore act to prohibit the promotion, sale, and distribution of tobacco products over the Internet to individuals under the age of 18.
-
Regulations at the state level vary greatly across the country. Until the passage of federal legislation, state and local legislatures should increase their regulatory efforts related to environmental tobacco smoke by establishing smoke-free indoor workplaces, public buildings, and restaurants. Eight states still have no restrictions on state government worksites, and 30 states have no restrictions on smoking in nongovernmental workplaces. For local jurisdictions, clean air legislation may be difficult to enact because of state preemption rules that make it unlawful for local governments to enact clean air restrictions that are more stringent than those imposed at the state level. If a state has no restrictions on worksite smoking, for example, it may be impossible for a local community to ban smoking in restaurants or other workplaces. Preemption laws need to be overturned to give local governments the right to protect their communities.
-
Further restrictions are needed to reduce tobacco promotion and advertising, which compromises youth tobacco prevention efforts. Restrictions now in place include a mix of voluntary agreements, restrictions resulting from settlements of law suits, and prohibitions defined by state or local ordinances, but some efforts have been hampered by protection of commercial speech (Bayer et al., 2002; Morrison, 2002). The Board urges renewed national consideration of how to address these issues.
The Board’s proposed recommendations are consistent with meeting the tobacco-related objectives outlined in Healthy People 2010 (US DHHS and Office of Disease Prevention and Health Promotion, 2000) (Box 11.2).
|
BOX 11.2 Summary of Objectives to Reduce Illness, Disability, and Death Related to Tobacco Use and Exposure to Secondhand Smoke Outlined in Healthy People 2010
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||
Recommendation 2: A national strategy should be developed and coordinated by the U.S. Department of Health and Human Services to address the epidemic of obesity, unhealthy diet, and physical inactivity in America, which are all significant risk factors for cancer and other diseases. Effective interventions need to be identified and broadly applied to reduce cancer risk among the general population and among populations at higher risk.
Dietary interventions to prevent cancer have, to date, focused primarily on particular components such as the consumption of fruits and vegetables, fiber, and fats. Obesity and physical inactivity have recently joined unhealthy diet as leading risk factors for cancer. Interventions aimed at maintaining a healthy weight and diet and increasing levels of physical activity can reduce the burden of cancer and other chronic illnesses such as cardiovascular disease and diabetes.
A comprehensive set of recommendations, the Recommendations for Public Health Action on Weight Control and Physical Activity to Promote Cancer Prevention, has been proposed by the International Agency for Research on Cancer (IARC), an agency within the World Health Organization (2002) (Box 11.3). The National Cancer Policy Board endorses these recommendations for action.
|
BOX 11.3 Recommendations for Public Health Action on Weight Control and Physical Activity to Promote Cancer Prevention, IARC, WHO Governmental and Nongovernmental Organizations
|
|
Worksites and Schools
Health Professionals and Educators
Families and Individuals
|
Of special concern are the nation’s youth. Many children and adolescents are not engaged in recommended levels of physical activity and are increasingly overweight or obese. These trends, in addition to the prevalence of smoking among adolescents, threaten the recent gains made in reducing cancer deaths. Comprehensive school physical education and health programs have the potential to help students establish lifelong, healthy physical activity and eating patterns, thereby avoiding overweight and obesity.
The Board endorses the following 10 strategies designed to promote lifelong participation in enjoyable and safe physical activity and sports identified in Promoting Better Health for Young People Through Physical Activity and Sports, A Report to the President from the Secretary of Health and Human Services and the Secretary of Education (CDC, Division of Adolescent and School Health, 2000):
-
Include education for parents and guardians as part of youth physical activity promotion initiatives.
-
Help all children, from prekindergarten through grade 12, receive quality, daily physical education. Help all schools have certified physical education specialists; appropriate class sizes; and the facilities, equipment, and supplies needed to deliver quality, daily physical education.
-
Publicize and disseminate tools to help schools improve their physical education and other physical activity programs.
-
Enable state education and health departments to work together to help schools implement quality, daily physical education and other physical activity programs:
-
with a full-time state coordinator for school physical activity programs,
-
as part of a coordinated school health program, and
-
with support from relevant governmental and nongovernmental organizations.
-
-
Enable more after-school care programs to provide regular opportunities for active, physical play.
-
Help provide access to community sports and recreation programs for all young people.
-
Enable youth sports and recreation programs to provide coaches and recreation program staff with the training they need to offer developmentally appropriate, safe, and enjoyable physical activity experiences for young people.
-
Enable communities to develop and promote the use of safe, well-maintained, and close-to-home sidewalks, crosswalks, bicycle paths, trails, parks, and recreation facilities and community designs that feature mixed-use development and a connected grid of streets.
-
Implement an ongoing media campaign to promote physical education as an important component of a quality education and long-term health.
-
Monitor youth physical activity, physical fitness, and school and community physical activity programs in the nation and each state.
Most states do not adhere to these recommendations. As of 2001, for example, although 48 states had mandates for physical education, only Illinois required daily physical education for all students in kindergarten through grade 12 (Alabama required daily physical education for all students in kindergarten through grade 8). In states with mandatory physical education, many elementary and middle school students are spending relatively little time in physical education classes, and most high school students take physical education for only 1 of their 4 years (http://www.aahperd.org/naspe/pdf_files/shape_nation.pdf, assessed July 24, 2002).
Establishing healthy eating habits at a young age is critical because changing poor eating patterns in adulthood is difficult. Schools can help young people improve their eating habits by implementing effective policies and educational programs. CDC has issued guidelines for school health programs to promote lifelong healthy eating, including four attributes of effective school-based nutrition education programs (http://www.cdc.gov/nccdphp/dash/nutguide.htm):
-
help young people learn skills (not just facts);
-
give students repeated chances to practice healthy eating;
-
make nutrition education activities fun; and
-
involve teachers, administrators, families, community leaders, and students in delivering strong, consistent messages about healthy eating as part of a coordinated school health program.
The CDC guidelines provide schools with strategies to improve nutrition education programs through policies, curriculum, instruction, program coordination, staff training, family and community involvement, and program evaluation.
The 2001 Surgeon General’s Call to Action to Prevent and Decrease Overweight and Obesity proposed a framework, CARE: Communication, Action, Research, and Evaluation to address the problem (US DHHS, 2001b). Recognizing the need for interventions at multiple levels, the Surgeon General’s report outlines needed action within five settings: families and communities, schools, health care, media and communications, and worksites.
Recommendation 3: The U.S. Congress should provide sufficient appropriations to the Centers for Disease Control and Prevention to support innovative public and private partnerships to develop, implement, and evaluate comprehensive community-based programs in cancer prevention and early detection. Every state should have and implement a comprehensive cancer control plan.
No coordinated infrastructure involving public and private efforts to launch multilevel interventions known to be effective in bringing about behavioral change exists at the federal or state levels. CDC is the federal link to the nation’s public health infrastructure, principally through state and local health departments. It is most often at these levels that multilevel cancer prevention and early detection interventions are carried out. The network that makes up the public health infrastructure is vast and includes 59 state and territorial health departments, more than 3,000 county and city health departments, more than 3,000 local boards of health, tribal health departments, and other federal and private organizations. This network generally engages the support of partners including consumer and advocacy organizations, universities, and area health care providers. This network of systems and organizations is essential to the public health mission of health promotion and disease prevention, but it is fragile, under stress, and underfunded (Box 11.4) (Institute of Medicine, 2003).
CDC’s Center for Chronic Disease Prevention and Health Promotion is an important locus for activity to improve the nation’s and individual states’ capacities to provide comprehensive cancer control services. CDC’s Office of Smoking and Health, for example, provides technical assistance to states and monitors progress in reaching tobacco-related goals outlined in Healthy People 2010 (US DHHS and Office of Disease Prevention and Health Promotion, 2000). Other programs at CDC address other risk factors, for example, the Division of Nutrition and Physical Activity promotes healthy diet, weight control, and physical activity, and the Division of Cancer Prevention and Control oversees the National Breast and Cervical Cancer Early Detection Program that operates in all states to provide screening and follow-up services to underserved women.
CDC also supports states in the development and implementation of comprehensive cancer control plans. State efforts in cancer prevention and early detection are in many cases piecemeal and are organized around categorically funded programs. CDC needs to build the capacities of states—and in turn, their local partners—to both develop and implement comprehensive cancer control plans. As part of CDC’s National Comprehensive Cancer Control Program, cancer control plans have been defined as those with an integrated and coordinated approach to reduce the rates of incidence, morbidity, and mortality of cancer through prevention, early detec-
|
BOX 11.4 Public Health’s Mission and Services Public Health Mission
Essential Public Health Services
SOURCE: Public Health Functions Steering Committee, Public Health in America, July 1995 (www.health.gov/phfunctions/public.htm assessed July 24, 2002). |
tion, treatment, rehabilitation, and palliation (CDC, 2001a; www.cdc.gov/cancer/ncccp/index.htm) (see Chapter 9).
Roughly half of the states (27 states) report having a comprehensive cancer control plan, but the plans are in various stages of implementation. CDC is supporting states in developing and implementing such plans, but the available support has been modest (less than $37 million since 1998) (see Chapter 9). The CDC estimates that $30 million per year would be needed before states would have plans developed and implementation in progress by 2005 (Leslie Given, Division of Cancer Prevention and Control, CDC, personal communication to Maria Hewitt, IOM, September 9, 2002).
Many states have in place some of the essential elements of a comprehensive program. Approximately half of them, for example, have cancer registries that achieve the standards of completeness, timeliness, and coverage to provide accurate cancer incidence data for planning and evaluation. All states monitor the prevalence of cancer-related risk factors such as smoking, and all states have in place CDC-funded breast and cervical cancer screening programs targeted to low-income and underserved women.
State and local health departments can play important roles in institut-
ing and coordinating comprehensive cancer prevention programs. Health departments can, for example:
-
monitor and publicize state trends in cancer and cancer-related behaviors;
-
support media campaigns to promote healthy behaviors;
-
target interventions to low income and racial/ethnic groups at high risk for cancer, e.g., by providing breast, cervical, and colorectal cancer screening services to medically uninsured and medically underserved populations;
-
develop and distribute best-practice guidelines to major employer human resources departments to encourage smoking cessation programs, wellness programs, on-site healthy eating and exercise facilities, flexible time for employees to allow alternative means of commuting (e.g., by bicycle or foot), and use of preventive health services (e.g., screening and smoking cessation programs);
-
collaborate with school systems to develop cancer prevention-related educational curricula and programs;
-
collaborate with public and private organizations to provide incentives for physical activity, healthy eating, and participation in weight loss programs (e.g., reduced fees for fitness clubs, on-site weight control groups, employer nonautomotive commuting programs);
-
track state use of funds available through the 1998 Transportation Equity Act for the 21st Century (Public Law 105-178), which provides federal funds to construct sidewalks and bicycle trails and to integrate mass transit, roads, and pedestrian and bicycle facilities into a comprehensive transportation plan;
-
support free and reduced-fee health clinics organized through local health departments and other community-based programs; and
-
evaluate the effectiveness of services and programs.
Despite the evidence of success of tobacco control efforts, the effort to support comprehensive plans to further a wide range of cancer prevention activities remains a promising but untested approach. Rigorous assessments of this approach, with an eye to defining essential components, innovative delivery systems, and model programs, need to be integrated into the plans themselves. Key to success is also the incorporation at the outset of broad community input into the plans, especially from important constituencies such as minority groups, elderly people, parents, and the advocacy community. Successful implementation of plans will depend on collaborative public-private partnerships because in many areas, state and local health departments lack the infrastructure needed to fully carry out a comprehensive plan. With these components in place, the Board
recommends further support to allow states to develop and implement comprehensive state plans.
The National Dialogue on Cancer (NDC), an initiative spearheaded by the American Cancer Society, has since 1999 provided a forum for leaders in both the public and private sectors to foster and support efforts to overcome cancer. In the area of prevention and early detection, NDC has convened an issue team to address primary cancer prevention and a team to formulate a strategy for ensuring the development and implementation of cancer prevention and early detection plans in every state (www.ndoc.org). NDC has recently recommended that all states have a comprehensive plan in place by 2003 and that implementation of the plan be in progress by 2005.
Recommendation 4: Public and private insurers and providers should consider evidence-based cancer prevention and early detection services to be essential benefits and should provide coverage for them. These services at a minimum should include interventions recommended in the 2000 U.S. Public Health Service’s clinical practice guideline on treating tobacco use and dependence, screening for breast cancer among women age 50 and older, screening for cervical cancer among all sexually active women with an intact cervix, and screening for colorectal cancer among adults age 50 and older.
Public and private health insurers and providers who want to improve the health of their beneficiaries should include in their benefit packages coverage for evidence-based interventions for cancer prevention and early detection. Nicotine replacement therapy, treatment with certain antidepressants (i.e., Bupropion SR), and counseling, for example, are effective in helping individuals quit smoking. Very few insurers or health maintenance organizations cover the cost of pharmaceutical treatment for smoking cessation and health education and preventive counseling are usually not defined benefits. In one innovative program funded by the Robert Wood Johnson Foundation, health plans are collaborating to examine ways to provide coverage for smoking cessation services.
States have mandated coverage for some cancer prevention and early detection interventions. As of 1998, for example, 43 states and the District of Columbia mandated coverage of cancer screening tests. Such mandates, however, do not always apply broadly to all insured individuals. Employers that are self-insured, for example, are usually exempt from such mandates (Rathore et al., 2000).
For insurers that offer coverage for preventive services, the reduction or elimination of cost sharing (e.g., coinsurance and copayments) can address a financial deterrent to seeking services and can improve the rate of service
use (Solanki et al., 1999, 2000). The specifics of an insurer’s coverage policy may be dictated broadly by the insurer or plan, or they may be negotiated with employers or other group purchasers. In the latter case, employer benefits managers informed of the effectiveness of cancer prevention services might be motivated to obtain more comprehensive coverage for their employees.
Just as preventive services of proven effectiveness should be covered under insurance plans, services for which evidence of benefit is lacking should be excluded from coverage. Population-based or routine screening of smokers for lung cancer using spiral or helical computed tomography (CT) scans, for example, does not yet meet standards of evidence to support their coverage under health insurance plans. Evidence was not sufficient to include a recommendation regarding mandated reimbursement for interventions to increase physical activity, improve diet, and reduce obesity as a general cancer prevention strategy, though optional offerings by insurers should be encouraged.
There are many opportunities for employers, business coalitions, and other large purchasers of health insurance to exert influence to encourage the use of cancer prevention and early detection services. Employers can provide coverage for preventive services as part of their insurance benefit packages, give discounts to employees who choose plans with more extensive prevention services, and can create financial incentives for health plans to meet performance goals. The Pacific Business Group on Health (PBGH), for example, is a nonprofit coalition of 45 large health care purchasers in California and Arizona representing 3 million insured individuals who account for $3 billion in annual health care expenditures (www.pbgh.org). PBGH also oversees a small business purchasing group that includes more than 9,500 small businesses. PBGH collects and analyzes health plan and provider performance data to produce report cards for consumers, promotes shared treatment decision making between providers and consumers, and promotes value-based buying decisions among its purchasers (Castles et al., 1999; Schauffler and Rodriguez, 1996; President’s Advisory Commission, 1998; www.pbgh.org).
Working with health plans in California, an agreement was reached to follow a uniform set of minimum preventive care guidelines based on the US Preventive Services Task Force recommendations (Partnership for Prevention, 1997). In 2000, PBGH approved new benefits for treatment to aid smoking cessation, including behavioral interventions and over-the-counter pharmacotherapy (Harris et al., 2001). PBGH was the first purchasing coalition to impose a condition on contracting plans whereby it would withhold 2 percent of the premium until the plans achieved specific goals for improving customer satisfaction and quality of care, including adherence to cancer screening guidelines. The Alliance, a health insurance purchasing cooperative in Denver, Colorado, subsequently adopted a similar
approach (Darby, 1998). General Motors, the nation’s largest private employer, has recently collaborated with CDC to examine barriers to the use of prevention services and to devise strategies to improve the rate of use of such services by its employees. Partnership for Prevention, a national nonprofit organization, provides guides for employers and health plans regarding highest value preventive health services (http://www.prevent.org/publications.htm).
Actions taken on behalf of federal employees in some areas of cancer control provide models that private-sector employers can emulate. In 1997, an executive order established smoke-free environments for the more than 1.8 million civilian federal employees and members of the public visiting or using federal facilities. In 2001, federal departments and agencies were directed to establish a policy that provides up to 4 hours of excused absence each year, without a loss of pay or a charge to leave, for participation in preventive health screenings. Agencies were also directed to develop or expand programs offered at the worksite to help employees understand their risks for disease, obtain preventive health services, and make healthy lifestyle choices. The Office of Personnel Management has issued guidance for a model smoking cessation program and is compiling a list of best practices to be shared with agencies. Agencies can pay the costs incurred by employees participating in agency-authorized smoking cessation programs, including payment for nicotine replacement therapy when purchased as part of an agency’s smoking cessation program (www.opm.gov/ehs).
Other opportunities to encourage prevention include employer-sponsored wellness and physical fitness programs, either through on-site facilities or through discounts to local gymnasiums or fitness programs. Relatively few employers offer such benefits, and employees with the least access to them are blue-collar or service workers and those working for small firms.
Recommendation 5: The U.S. Congress should increase support for programs that provide primary care to uninsured and low-income people (e.g., Community and Migrant Health Centers and family planning programs of Title X of the Public Health Service Act). These programs increase the use of cancer prevention and early detection services among medically underserved populations.
A pervasive problem in the United States is poor access to health care because of a lack of health insurance. Persons with health insurance are more likely to have a primary care provider and to have received appropriate preventive care such as recent cancer screening tests. Adults with health insurance are twice as likely as adults without health insurance to receive a routine checkup. In 2001, an estimated 15 percent of the U.S. population (41.2 million individuals) was uninsured during the entire year (U.S. Census
Bureau, 2002). Many others are underinsured, with poor coverage for interventions that have been proven to be effective, such as smoking cessation counseling and products. In fact, smokers are more likely than nonsmokers to be uninsured, making them less able to gain access to effective programs.
Individuals who are uninsured (or underinsured) rely on a patchwork of public and private programs for primary care (IOM, 2000d). Community and Migrant Health Centers and Title X family planning clinics are vital sources of primary health care and are important providers of cancer prevention and early detection services (see Chapter 9). Full support for these programs enhances the nation’s health care safety net and at the same time extends the availability of cancer prevention and early detection services to vulnerable populations. Even with increased program support, however, many people would likely remain underserved, given the fragmented and limited nature of the nation’s health care safety net (Norton and Lipson, 1998).
Recommendation 6: Support for the Centers for Disease Control and Prevention’s National Breast and Cervical Cancer Early Detection Program should be increased so that the program can reach all uninsured women using innovative delivery strategies. Support is also needed for a similar program at the CDC to provide screening for colorectal cancer for uninsured and low-income men and women.
Underfunding of CDC’s National Breast and Cervical Cancer Early Detection Program (NBCCEDP) contributes to lost opportunities for prevention. This program provides screening services to uninsured and underinsured women, but the program reaches only 15 percent of eligible women because of limited financial support. This is especially unfortunate insofar as racial, ethnic, and socioeconomic disparities in cancer mortality can often be traced to poor use of screening services. Racial and ethnic disparities in cancer incidence could in fact widen if this gap in access to effective prevention services is not addressed. Despite its lack of coverage because of limited funding, NBCCEDP has succeeded in improving screening rates among medically underserved populations.
Because screening for colorectal cancer is also a proven strategy for reducing cancer mortality in people over 50 years of age, a similar program is needed to provide colorectal cancer screening to people who are uninsured and underinsured. The majority of individuals eligible for colorectal screening have not been screened, and screening rates are particularly low among minority and low-income populations.
Recommendation 7: The U.S. Department of Health and Human Services
should complete a comprehensive review to assess whether evidence-based prevention services are being offered and successfully delivered in federal health programs.
The federal government administers or funds Medicare; Medicaid; the Health Resources and Services Administration’s Community and Migrant Health Centers; Title X family planning clinics; the U.S. Department of Agriculture’s programs such as the Special Supplemental Nutrition Program for Women, Infants, and Children; the Indian Health Service; U.S. Department of Defense health programs; and Federal Employees Health Benefits Program. These programs do not always reflect best practices in cancer prevention and early detection.
The Medicare program, for example, does not cover any costs for smoking cessation treatment, and two-thirds of state Medicaid programs cover such treatments (Schauffler et al., 2001a). The lack of coverage for effective prevention services in public programs introduces a significant barrier to those most burdened by cancer: the uninsured population and members of racial and ethnic minority groups who often depend on federal programs for care. The availability of evidence-based prevention services should be ensured in these and other public programs. The Centers for Medicare and Medicaid Services (CMS, formerly the Health Care Financing Administration) is examining how a smoking cessation benefit might best be structured through a demonstration program.
Evidence-based prevention services should be available in these and other public programs. Therefore, a comprehensive review of the benefits being offered and the effectiveness of delivery systems is needed to identify opportunities to improve access to cancer prevention and early detection services in federal programs.
Recommendation 8: Programs are needed for health care providers to improve their education and training, monitor their adherence to evidence-based guidelines, and enhance their practice environments to support their provision of cancer prevention and early detection services.
Primary care providers in health care settings are effective agents of behavioral change. When counseled about smoking in clinical settings, 5 to 10 percent of individuals are able to quit. Evidence suggests, however, that physicians and other practitioners are not providing effective clinical interventions such as counseling and screening tests as often as would be beneficial. Fewer than half of adults who smoke cigarettes, for example, report that at their last visit the physician inquired whether they smoked.
Shortcomings in providers’ delivery of clinical preventive services can, in part, be traced to a lack of education and training. There is evidence of programmatic deficits in medical, dental, and nursing schools, despite nu-
merous calls to improve the education and training of health care professionals in health promotion and disease prevention. A problem of greater magnitude is upgrading the knowledge and skills of practicing clinicians whose performance reflects their lack of training. Health care providers who completed their training 10 or more years ago are unlikely to have been trained in cancer prevention and control. In the early 1990s, for example, relatively few medical schools offered any training in smoking cessation. Ensuring the inclusion of comprehensive prevention curricula in health professional schools is necessary, but the larger task is reaching providers who have completed their training. Continuing medical education programs can be made more accessible by applying new learning technologies (e.g., distance learning and online continuing medical education). Innovative alternative teaching methods are among the interventions being targeted as part of translational research in multimedia technology funded by the National Cancer Institute (2000a).
To address the deficits observed in medical schools, the Association of American Medical Colleges (AAMC) has developed population health guidelines to help ensure that medical students are able to “incorporate principles of disease prevention and behavioral change appropriate for specific populations of patients within a community” (Association of American Medical Colleges, 1999, p. 139). The AAMC Population Health Perspective Panel recommended that medical schools develop an action plan, identify teaching faculty, form liaisons with groups that can help (e.g., Teachers of Preventive Medicine), and show evidence of success. The panel also recommended that population health competencies be tested in the examinations of the National Board of Medical Examiners. Similar actions could be taken by dental, nursing, and other health professional schools to improve their inclusion of course work in cancer prevention and early detection in their curricula.
The Board recommends the following strategies for improving education and training:
-
Professional education and training programs should adequately cover cancer prevention and early detection in their curricula.
-
Training institutions and professional organizations should provide continuing education in cancer prevention and early detection. Continuing medical education programs can be made more accessible by applying new learning technologies (e.g., distance learning and online continuing medical education).
-
Professional organizations representing primary care providers should promote their members’ adherence to evidence-based cancer prevention and early detection guidelines.
Systems of care encounter a variety of infrastructure and operational
barriers in the delivery of prevention services. The systems that health care providers need depend on supportive management structures; efficient patient-flow procedures; and information systems that support reminder systems, documentation of services, timely follow-up and referrals, and coordinated communication with providers and institutions across the community. Evidence consistently shows that such support systems improve physician and patient compliance with recommended preventive practices.
-
Health systems should support the infrastructure needed to identify patients in need of intervention (e.g., smokers or those who are due for screening), remind providers to intervene, and track progress toward clinical goals.
Efforts to improve the quality of health care delivery have increasingly relied on monitoring the performance of health care providers and systems of care. Clinicians want to provide good care and need to know the effects of their actions and be in a position to respond to incentives (Center for the Advancement of Health, 2001). There are many opportunities to monitor performance and assist providers in improving their practices:
-
CMS could examine provider performance regarding adherence to recommended cancer prevention and early detection recommendations. CMS has specified in the most recent scope of work for peer review organizations that the quality of breast cancer services is a priority area. Assessments of provider adherence to mammography guidelines could be undertaken.
-
State health departments could use data from cancer registries to examine regions and population subgroups characterized by high rates of late-stage diagnoses of breast, cervical, and colorectal cancer, for which screening programs are available, to identify where to target outreach efforts.
-
The National Committee for Quality Assurance could expand efforts to monitor preventive practices of managed care plans through its Health Plan Employer Data and Information Set system.
-
Employers and other group benefit managers could define performance targets for health education and preventive counseling to hold health plans accountable for the provision of these services (Schauffler et al., 1999; Schauffler et al. 1996).
-
The Joint Commission on the Accreditation of Healthcare Organizations could evaluate the availability of services to promote risk behavior change as part of its accreditation process.
Quality assurance systems must not only track the appropriate provision of services, but they must also assess the quality of the services provided. Clinicians, for example, need to collect samples properly, laborato-
ries must adhere to standards in processing specimens and interpreting results, and rigorous follow-up must be carried out for patients with positive screening test results. Adherence to quality standards maximizes the benefits of prevention services.
The aging of the nation’s population will sharply increase the demand for certain cancer prevention services such as screening. There may be an inadequate supply of personnel to meet these demands. There are uncertainties, for example, about the supply of gastroenterologists to perform colonoscopy for colorectal cancer screening programs and the adequacy of the numbers of mammography personnel (Institute of Medicine, 2001c). If such shortages are anticipated, policies to address them will need to be identified.
-
The Health Resources and Services Administration should assess the adequacy of the future supply of providers of cancer prevention and early detection services.
Models of successful delivery of services are as essential as an adequate supply of trained providers. There is convincing evidence that nonphysician providers are just as effective as physician providers in delivering certain smoking cessation and screening services, but research is needed on how to integrate provision of prevention services by such providers into routine primary care.
-
The Agency for Healthcare Research and Quality and other research sponsors should support demonstration programs to evaluate innovative models of prevention service delivery.
Recommendation 9: The U.S. Congress should provide sufficient support to the U.S. Department of Health and Human Services for the U.S. Preventive Services Task Force and the U.S. Task Force on Community Preventive Services to conduct timely assessments of the benefits, harms, and costs associated with screening tests and other preventive interventions. Summaries of recommendations should be made widely available to the public, health care providers, and state and local public health officials and policy makers.
Evidence-based guidelines for clinical and community practice provide maps for action. Rigorous assessments of the effectiveness of clinical prevention services are conducted periodically by the U.S. Preventive Services Task Force,2 and the effectiveness of interventions aimed at communities
are being assessed by the U.S. Task Force on Community Preventive Services.3 These task forces are overseen by the Agency for Healthcare Research and Quality and CDC, respectively, federal agencies that have been at the forefront in identifying effective prevention intervention strategies. Widely accepted public health goals and objectives have been established through the Healthy People 2010 initiative (US DHHS and Office of Disease Prevention and Health Promotion, 2000), and efforts are under way to chart the nation’s progress toward those goals (see Chapter 9, Box 9.1).
Although there is a general consensus among public health scientists regarding interventions that work, many areas of controversy remain and evidence is inconsistently applied across federal, state, and private programs. There are examples of screening and other prevention interventions that were quickly adopted before adequate research had been completed to fully understand their potential benefits and harms. Screening for prostate cancer by prostate-specific antigen testing, for example, for which there is comparatively little evidence of effectiveness, is more commonly used than colorectal cancer screening, for which there is strong evidence of effectiveness. More recently, low-dose computed tomography scanning has been promoted as a screening test for lung cancer among high-risk individuals, with the scientific community divided on the merits of its effectiveness. The history of the rapid dissemination into practice of X-ray screening for lung cancer in the 1960s and 1970s and its later withdrawal after evidence from clinical trials showed that it did not reduce the rate of mortality from lung cancer provides a cautionary precedent for the use of computed tomography scanning as a routine screening test for lung cancer. It will be years before the results of clinical trials are available to answer questions about the test’s effectiveness. Until definitive evidence is available to resolve the controversies, clear information should be available to the public on the potential benefits, harms, and costs of new technologies so that consumers and health care providers can make informed judgments.
The U.S. Preventive Services Task Force has provided comprehensive assessments of clinical prevention services, but the task force has, until recently, been convened only periodically. In 2001 it published selected updates of recommendations made in 1996 (U.S. Preventive Services Task Force 2001a,b, 2002). Assessments of prevention services are needed on a
|
|
Currently, the third USPSTF, convened in 1998, is issuing recommendations updated from its 1996 Guide to Clinical Preventive Services (U.S. Preventive Services Task Force, 1996) (www.ahcpr.gov/clinic/uspstfaab.htm). |
|
3 |
The 15-member independent, nonfederal U.S. Task Force on Community Preventive Services first met in 1996 and has issued reports on improving vaccination coverage, reducing exposure to environmental tobacco smoke, and increasing physical activity (www.thecommunityguide.org). |
continual basis to ensure that public health recommendations are current and incorporate the latest scientific evidence. The task force’s main responsibility is making clinical recommendations, but its role should be expanded to also recommend priority areas for research on clinical preventive services.
The U.S. Community Services Task Force is relatively new and has the responsibility to identify interventions that work for communities. As state efforts to implement comprehensive cancer control plans gain momentum, guidance on the effectiveness of public health interventions will be critically needed.
The Board recommends that support for both task forces be sufficient for systematic syntheses and meta-analyses of data from the literature and to keep abreast of developments in both clinical and community disease prevention and health promotion. Greater investments in dissemination activities are also needed to reach health providers and the general public, both about areas of consensus among public health scientists regarding interventions that work, and about the areas of controversy that remain. Some evidence suggests that health care providers and the public are not very familiar with the recommendations of the U.S. Preventive Services Task Force. Likewise, individuals who make insurance coverage decisions for employers are unfamiliar with these recommendations (Partnership for Prevention, 1997).
A promising complementary development aimed at improving dissemination of evidence-based cancer control interventions has been initiated at the National Cancer Institute (NCI), Closing the Discovery to Delivery Gap: Translating Research into Improved Outcomes (TRIO). The effort aims to (National Cancer Institute, 2001):
-
model and monitor the impacts of diffusion and dissemination efforts on the health promotion and cancer control objectives of Healthy People 2010 (US DHHS and Office of Disease Prevention and Health Promotion, 2000);
-
collaboratively promote adoption of evidence-based cancer control interventions by local, state, and national service organizations; and
-
focus on eliminating cancer-related health disparities among medically underserved populations with cancer.
Recommendation 10: Public and private organizations (e.g., the National Cancer Institute, the American Cancer Society) should take steps to improve the public’s understanding of cancer prevention and early detection with a focus on promoting healthy lifestyles and informed decision making about health behaviors and cancer screening.
Raising public awareness of the benefits of cancer prevention and early detection is central to reducing the cancer burden. Despite the public’s keen interest in the potential hazards and benefits of various lifestyle factors, several barriers to effective communication exist. The first is the difficulty of dealing with media coverage that is often contradictory and based on questionable research. In some cases the results of a single study or preliminary laboratory findings are well publicized and their implications are over-stated in the press. In other cases, lifestyle recommendations based on years of descriptive epidemiology are countered by new evidence from more robust studies, for example, clinical trials. The recommendation to consume fiber to prevent cancer, for example, was grounded in good evidence from descriptive population studies (e.g., studies of the health of migrants), but the recommendation was undermined by new scientific findings from clinical trials that showed that no clear benefit was associated with fiber consumption. The public is generally not equipped to interpret the seemingly conflicting advice, and confusion, skepticism, and cynicism may result.
The public’s thirst for quick medical “miracles” and simple impatience also pose significant barriers to progress in cancer prevention and early detection. It can take many years to reap the benefits of behavioral change like smoking cessation and the rewards of many other interventions can take time to be realized. Significant reductions in breast cancer mortality rates as a result of screening programs have only recently been observed in the general population. The fascination of the American public with advanced technology and “getting tested,” the commercial and marketing interests in servicing this demand, and the sense of urgency to take action in combating cancer set the stage for the premature adoption of interventions that are potentially ineffective or harmful. That screening can be harmful is itself an unfamiliar concept to the general public and many health care professionals. Cultivating a deeper awareness of the health risks of screening might promote more responsible choices about screening at both the individual and the population levels and undo the popular misconception that the only arguments against screening are economic (Woolf, 2001).
Increasingly, cancer screening guidelines incorporate the tenets of informed decision making. Rather than issuing prescriptive recommendations regarding prostate-specific antigen testing, for example, most organizations are suggesting that individuals discuss the relative benefits and harms of screening, weigh these factors according to their individual values and preferences, and decide whether or not to proceed with screening. Although this shared decision-making approach tends to be embraced by the well-educated health consumer, little is known regarding its acceptance among the general public and how best to incorporate it into the delivery of preventive services.
Improved understanding of cancer prevention by the general public is also critical to support for research in this area. Although the public is
generally supportive of clinical medical innovations, it has less of an appreciation of the potential of public health interventions. Clinical interventions play an essential role in prevention, but public health programs can more effectively reach a broader audience and bring about shifts in behavior within a population. There is generally a failure to appreciate the significance of the levels of change achieved with current interventions. A program that helps 10 to 15 percent of individuals stop smoking has tremendous rewards in terms of reductions in morbidity and mortality rates. Likewise, support for cancer prevention may lag behind that for other interventions because many people do not acknowledge the difficulty of initiating behavioral change and the need for supportive systems to help individuals maintain healthy behavioral change.
Recognizing that society is in the midst of a communications revolution, NCI (2001) has found that an extraordinary opportunity to invest in communications about cancer exists at present. Effective communication can move people to engage in behaviors that will improve their health, can give people the information that they need to make informed cancer-related decisions, and may empower people by raising their awareness of health problems and recommended actions. The goals of the NCI initiative are to
-
accelerate reductions in the U.S. cancer burden through the use of communications about cancer;
-
integrate communications about cancer into the cancer care continuum so that it is an accepted and practiced component of quality care; and
-
increase the demand for, access to, and use of communications about cancer by diverse populations including the public, high-risk persons, underserved and disabled populations, children, patients, survivors, and health care professionals.
Among the activities to be sponsored as part of this initiative are national surveys to assess public perceptions; monitoring of emerging information needs; creation of cancer-related communications centers of excellence; development of tool kits for the public, patients, underserved populations, advocacy groups, and others; and training of health communications scientists, researchers, and practitioners (National Cancer Institute, 2001).
The lessons learned from the research supported by this initiative will inform the educational programs of both public and private organizations. Knowledge of how to frame educational messages that will lead to both increased knowledge and health-promoting behaviors could, for example, be applied by the American Cancer Society in its community-based programs and by CMS in its beneficiary education campaigns.
Recommendation 11: Public and private initiatives to reduce disparities in the cancer burden (e.g., initiatives of the National Cancer Institute and the American Cancer Society) should be supported.
There are glaring disparities in rates of morbidity and mortality from cancer between socioeconomic groups, insured and uninsured populations, and certain racial and ethnic groups (IOM, 1999b). The differences among these various groups present both a challenge in terms of understanding the reasons and an opportunity in terms of reducing the burden of cancer (US DHHS and Office of Disease Prevention and Health Promotion, 2000). Lack of health insurance coverage is a key predictor of lower rates of use of cancer screening tests. Other psychological and sociocultural factors may also be at play. Personal barriers can include cultural differences, language barriers, not knowing what to do or when to seek care, or concerns about confidentiality or discrimination (US DHHS and Office of Disease Prevention and Health Promotion, 2000). In a nation of increasing diversity, interventions to improve cancer prevention and early detection must accommodate different languages, cultural values, and beliefs.
The elimination of racial and ethnic disparities in health is an over-arching goal of Healthy People 2010 (US DHHS and Office of Disease Prevention and Health Promotion, 2000), and an ongoing initiative involving agencies of the U.S. Department of Health and Human Services is in place. Cancer screening and management is one of six focus areas of the initiative (http://raceandhealth.hhs.gov/sidebars/sbinitOver.htm). The National Institutes of Health (NIH) has drafted a trans-NIH, 5-year Strategic Research Plan to Reduce and Ultimately Eliminate Health Disparities (www.nih.gov/about/hd/strategicplan.pdf), and in December 2000 NCI established the Center to Reduce Cancer Health Disparities (http://crchd.nci.nih.gov) to implement the NCI Strategic Plan to Reduce Health Disparities. Through this initiative, NCI aims to understand the causes of health disparities as they relate to cancer and develop effective interventions to eliminate these disparities. Specific initiatives and an action plan have been developed for each of the five objectives outlined in the strategic plan (http://www.cancer.gov/announcements/healthdisp.html):
-
expand the capacity to conduct fundamental cancer control and population research to elucidate the determinants of cancer-related health disparities;
-
expand the ability to define and monitor cancer-related health disparities;
-
support intervention research in prevention, early detection, treatment, and communications that may reduce cancer-related health disparities;
-
expand the channels for research dissemination and diffusion and
-
foster collaborations with allied agencies and organizations to facilitate the translation of evidence into practice; and
-
strengthen training and education in health disparities research and increase the number of minority scientists working in cancer control science.
The Board fully supports this NCI initiative and encourages NCI to collaborate with other private and public efforts to achieve success. Also needed are effective methods to evaluate and track the success of this and other initiatives.
Recommendation 12: Public and private sponsors of research including the National Institutes of Health, the Agency for Healthcare Research and Quality, the Centers for Medicare and Medicaid Services, the Centers for Disease Control and Prevention, the U.S. Department of Defense, and the American Cancer Society should expand their support of applied behavioral research and how best to disseminate evidence-based prevention interventions. Effective strategies are especially needed to encourage healthy behaviors among children and their families, medically underserved populations, and the public at large through multicomponent interventions.
The United States is at a crossroads in cancer prevention research. Basic science and epidemiology are advancing knowledge in a variety of areas, from the relationship between cancer and modifiable behavioral risk factors all the way down to the molecular pathways that mediate the actions of those risk factors. At the same time applied research is illustrating how the already vast amount of available evidence can be better used to more rapidly reduce cancer rates. To effectively reduce the cancer burden in the United States, however, there needs to be greater emphasis on action-oriented research (Colditz, 1997, 2001; Wegman, 1992). Knowledge about health problems and their causes does not automatically guarantee that appropriate actions are taken. Only when etiological knowledge is linked to evidence on the effectiveness of behavioral change strategies, and in turn to public awareness and policy support can the potential to reduce the burden of cancer be realized.
IDENTIFYING RESEARCH PRIORITIES
The Board has prioritized research to encourage healthy behaviors among children and their families, underserved populations, and the public at large through multicomponent interventions. In its review of the evidence regarding the effectiveness of cancer prevention and early detection, the Board identified specific research priorities in the major areas covered in
this report: tobacco use, physical activity, obesity and diet-nutrition, and cancer screening. The research priorities in each of these areas are described in the following sections.
Tobacco Use
-
Evaluate tobacco control programs, especially those that attempt to promote change through multiple channels including schools, community-based organizations, and the media. States need to know what works when allocating limited resources.
-
Assess the Tobacco Master Settlement Agreement, in particular, industry adherence to its provisions and the success of these provisions in reducing youth smoking rates.
-
Evaluate the effectiveness of channels for the delivery of smoking cessation services (e.g., workplaces, the Internet, families, health care providers, and peers) and other approaches to smoking cessation (e.g., restrictive smoking policies in schools and workplaces).
-
Identify effective cessation strategies for youth and young adults. Although many programs are designed to prevent smoking in adolescents and young adults, few evidence-based programs are aimed at smoking cessation in this age group. Research is needed to identify effective strategies for smoking cessation in young people.
-
Identify factors that increase demand for smoking cessation services. Researchers need to identify barriers to participation, factors that foster participation, and factors that promote sustained program participation.
-
Identify factors related to disparities in tobacco use and success in quitting by gender, race-ethnicity, occupation, educational level, and socioeconomic status. Understanding the social contextual factors such as social support, social networks, social norms, cultural beliefs, language, and psychological stressors could further understanding of how underserved groups can be helped to quit smoking.
-
Identify ways to help low-income smokers quit smoking. Applied research is needed into ways to make pharmacotherapy (e.g., nicotine replacement therapy) available and affordable for low-income groups.
Physical Activity
-
Identify strategies to build community support for environmental changes to promote activity. The Centers for Disease Control and Prevention has established a blueprint for promoting physical activity in communities, but support for the implementation of the recommendations presented in that blueprint has not been forthcoming. Research is needed to identify strategies that promote physical activity at the local level and that are tailored to the needs of individual communities.
-
Identify the optimal approaches to comprehensive health education programs for children and young adults to promote lifelong activity. Research is needed that provides a better understanding of the tracking of activity into the early adult years, the types of programs that foster lifelong activity, and the components of programs that foster adequate levels of physical activity to maintain a healthy weight through the adult years.
-
Identify strategies to make the work environment and social environments conducive to increased activity.
-
Identify how best to implement counseling for physical activity and weight management into routine, ongoing medical care.
Obesity and Diet-Nutrition
-
Translate the health benefits of weight maintenance through the adult years into health messages that motivate population-based strategies for the maintenance of healthy weight.
-
Identify strategies that can be used to reinforce behavioral changes that will promote and sustain a healthy weight.
-
Conduct long-term clinical intervention studies to alter behavioral patterns that may influence weight gain.
-
Identify the underlying causes of racial-ethnic and socioeconomic differences in obesity, and evaluate methods that deliver effective interventions to reduce disparities.
-
Conduct community-based intervention studies involving public and private partners (e.g., employers, food and fitness industry) to prevent weight gain and promote healthy diet and physical activity.
Cancer Screening
-
Develop useful methods for implementing shared decision making as applied to cancer screening. Given the growing number of cancer screening tests for which shared decision making is recommended, there is a growing need to answer questions surrounding the appropriateness, feasibility, and proper methods of this form of counseling.
-
Identify the underlying causes of racial-ethnic and socioeconomic disparities in the use of screening tests, and evaluate methods for the delivery of screening tests to reduce such disparities.
-
Encourage research to ensure that screening is performed well—with proper timing, technique, follow-up, and repeat screening—and that all eligible persons are screened.
-
Examine opportunities to increase rates of access to cancer screening in non-clinical venues such as worksites.
-
Evaluate the success of state and local health departments in using state and local estimates of screening use to target areas (and providers)
-
for improvement. Likewise, for Medicare beneficiaries, evaluate the success of peer review organizations in targeting areas (and providers) for improvement.
-
Clarify the effectiveness of screening tests relative to the effectiveness of primary prevention and other clinical or public health interventions in lowering rates of morbidity and mortality. The findings from such research can guide decisions about resource allocation.
The Board aims, with this summary of research priorities, to motivate research sponsors to invest in research that will lead to the identification of interventions that work and dissemination strategies that effect behavioral changes in the population. Essential too are investments in basic research in both cancer biology and behavioral health that can lead to the development of improved methods for cancer prevention and control (IOM, 2001a). The Board concurs with IOM’s Committee on Health and Behavior: Research, Practice and Policy when they concluded in their report, Health and Behavior: The Interplay of Biological, Behavioral, and Societal Influences, that “Most studies, though demonstrating the ability to alter behavior, either do not test, or when tested do not demonstrate, sustained behavior change. These factors present major challenges for the research and application of behavioral interventions and point to the need for long-term studies” (IOM, 2001a, page 334).






































