2
TESTS OF VISUAL FUNCTIONS
Tests of visual functions are at the core of current disability determination practices for visually impaired claimants at the Social Security Administration (SSA), and the committee’s task required us to carefully review and evaluate these tests. This chapter presents the results of that review. Each fundamental function is discussed, beginning with acuity and visual fields, the functions currently tested by SSA for disability determination. Next we present the evidence on the testing of contrast sensitivity, followed by other visual functions that the committee judged worthy of consideration as candidates for testing by SSA—most of which were mentioned in the earlier NRC report (National Research Council, 1994). Some closely related functions are grouped in a single section.
For each function, we considered evidence on why the function is important in the evaluation of visual disability and reviewed and evaluated evidence of the relationships between that function and performance in the four daily living and work task domains selected (see Chapter 1). The committee established criteria for acceptable tests and then reviewed and evaluated currently available and emerging new tests of each function against these criteria. Each section describes the strengths and weaknesses of available and emerging tests
for a particular function. Finally, each section presents, with rationale, our recommendations for or against SSA’s testing that function for disability determination and describes further research required to improve testing or otherwise support better disability determination practices.
A separate section discusses ways in which scores on tests of visual function could be mathematically combined to yield a single index of visual impairment for a claimant. The committee’s recommendations for the testing of visual functions are summarized in the final section.
VISUAL ACUITY
Description
Visual acuity is a measure of the spatial resolving power of the visual system; it indicates the angular size of the smallest detail that can be resolved. Clinical tests of visual acuity determine a size threshold for a recognition task. The targets to be recognized are called “optotypes,” and typically they are letters, Landolt rings, or “tumbling E’s” designed so the width of the strokes and the gaps are one fifth of the height of the optotype character. An individual’s visual acuity is determined by measuring the angular size of the smallest optotypes whose identity (letters) or orientation (Landolt rings and tumbling E’s) can be recognized.
Visual acuity is typically measured under conditions of high contrast, using printed or projected charts with optotypes like those described above. The results of visual acuity testing are usually expressed in Snellen notation, which is the ratio of the test distance to the distance at which the critical detail of the smallest optotype resolved would subtend 1 minute of visual angle. Thus, a minimum angle of resolution (MAR) of 1 minute of visual angle (or arc, sometimes abbreviated as “min arc”) when tested at 20 feet (6 meters) is expressed as 20/20 (6/6), whereas an MAR of 10 minutes of arc if tested at 20 feet is expressed as 20/200 (6/60). Alternative means of expressing visual acuity are the decimal notation (the reciprocal of the MAR or the
Snellen fraction), logMAR notation (the common logarithm of the MAR), the visual acuity rating, VAR, where VAR = 100 − 50 (logMAR), and the Snell-Sterling visual efficiency (VE = 0.2(MAR-1)/9). Table 2-1 presents these alternative forms of measurement as a conversion table. The standard for normal acuity has traditionally been considered to be 20/20. However, individuals with normal, disease-free eyes often have acuity better than 20/20, provided that refractive error has been corrected (Elliott et al., 1995).
Evaluation
Why the Measurement Is Useful
Ophthalmologists and optometrists routinely measure visual acuity for various purposes. In the measurement of refractive error, the lens power that permits the best visual acuity is often an important criterion. In the diagnosis and monitoring of eye diseases that may affect vision, changes of visual acuity are often taken to indicate the presence and magnitude of change in the medical condition. Ocular diseases and disorders that affect the transparency and optical regularity of the cornea, lens, or vitreous will degrade the optical image, with adverse effects on visual acuity. Diseases affecting the central region of the retina or the associated optic nerve pathways are likely to cause reductions in visual acuity. Visual acuity measurements are also used by some licensing authorities and employers as eligibility criteria for some occupations (e.g., airline pilot, police officer) and activities (e.g., driving). Visual acuity has traditionally been used as the primary indicator of the magnitude of functional impairment due to vision loss.
Good spatial resolution is important for a variety of everyday tasks in the workplace, but probably most critically for reading text and interpreting symbols, key components of many jobs. Visual acuity also plays a central role in discriminating and recognizing small objects or the detailed features of objects. The visual acuity demand for a given task depends on the size of the critical detail in the task and the observation distance. For example, a person with good visual acuity might be expected to recognize faces at about 20 meters. To
TABLE 2-1 Conversion Table for Visual Acuity Notations
|
Distance Vision |
|||||
|
|
|||||
|
LogMAR notation |
MAR exact |
MAR notation* |
Decimal notation* |
VE% notation |
VAR notation |
|
−0.30 |
0.501 |
0.50 |
2.00 |
109.4% |
115 |
|
−0.20 |
0.631 |
0.63 |
1.60 |
106.8% |
110 |
|
−0.10 |
0.794 |
0.80 |
1.25 |
103.6% |
105 |
|
0.00 |
1.000 |
1.00 |
1.00 |
100.0% |
100 |
|
0.10 |
1.259 |
1.25 |
0.80 |
95.6% |
95 |
|
0.20 |
1.585 |
1.60 |
0.63 |
89.8% |
90 |
|
0.30 |
1.995 |
2.0 |
0.50 |
83.6% |
85 |
|
0.40 |
2.512 |
2.5 |
0.40 |
76.5% |
80 |
|
0.50 |
3.162 |
3.2 |
0.32 |
67.5% |
75 |
|
0.60 |
3.981 |
4.0 |
0.25 |
58.5% |
70 |
|
0.70 |
5.012 |
5.0 |
0.20 |
48.9% |
65 |
|
0.80 |
6.310 |
6.3 |
0.160 |
38.8% |
60 |
|
0.90 |
7.943 |
8.0 |
0.125 |
28.6% |
55 |
|
1.00 |
10.00 |
10.0 |
0.100 |
20.0% |
50 |
|
1.10 |
12.59 |
12.5 |
0.080 |
12.8% |
45 |
|
1.20 |
15.85 |
16 |
0.063 |
6.8% |
40 |
|
1.30 |
19.95 |
20 |
0.050 |
3.3% |
35 |
|
1.40 |
25.12 |
25 |
0.040 |
1.4% |
30 |
|
1.50 |
31.62 |
32 |
0.032 |
0.4% |
25 |
|
1.60 |
39.81 |
40 |
0.025 |
20 |
|
|
1.70 |
50.12 |
50 |
0.020 |
15 |
|
|
1.80 |
63.10 |
63 |
0.016 |
10 |
|
|
1.90 |
79.43 |
80 |
0.013 |
5 |
|
|
2.00 |
100.0 |
100 |
0.010 |
0 |
|
|
*Note: Numbers rounded to simplify sequences. Rounding errors do not exceed 1.2 percent. Source: Ian Bailey, personal communication. |
|||||
|
|
||||||
|
|
Near Vision |
|||||
|
Snellen Fractions |
At 40 centimeters |
|||||
|
Based on 20 ft.* |
Based on 6 m.* |
Based on 4 m.* |
Snellen notation 0.40 meters* |
M Units * |
Points * |
x-height (mm) |
|
20/10 |
6/3 |
4/2 |
0.40/0.20 |
0.20 |
1.6 |
0.29 |
|
20/12.5 |
6/3.8 |
4/2.5 |
0.40/0.25 |
0.25 |
2.0 |
0.36 |
|
20/16 |
6/4.8 |
4/3.2 |
0.40/0.32 |
0.32 |
2.5 |
0.47 |
|
20/20 |
6/6 |
4/4 |
0.40/0.40 |
0.40 |
3.2 |
0.58 |
|
20/25 |
6/7.5 |
4/5 |
0.40/0.50 |
0.50 |
4.0 |
0.73 |
|
20/32 |
6/9.5 |
4/6.3 |
0.40/0.63 |
0.63 |
5.0 |
0.92 |
|
20/40 |
6/12 |
4/8 |
0.40/0.80 |
0.80 |
6.3 |
1.16 |
|
20/50 |
6/15 |
4/10 |
0.40/1.00 |
1.00 |
8.0 |
1.45 |
|
20/63 |
6/19 |
4/12.5 |
0.40/1.25 |
1.25 |
10.0 |
1.82 |
|
20/80 |
6/24 |
4/16 |
0.40/1.60 |
1.60 |
12.5 |
2.33 |
|
20/100 |
6/30 |
4/20 |
0.40/2.0 |
2.0 |
16 |
2.91 |
|
20/125 |
6/38 |
4/25 |
0.40/2.5 |
2.5 |
20 |
3.64 |
|
20/160 |
6/48 |
4/32 |
0.40/3.2 |
3.2 |
25 |
4.65 |
|
20/200 |
6/60 |
4/40 |
0.40/4.0 |
4.0 |
32 |
5.82 |
|
20/250 |
6/75 |
4/50 |
0.40/5.0 |
5.0 |
40 |
7.27 |
|
20/320 |
6/95 |
4/63 |
0.40/6.3 |
6.3 |
50 |
9.16 |
|
20/400 |
6/120 |
4/80 |
0.40/8.0 |
8.0 |
63 |
11.6 |
|
20/500 |
6/150 |
4/100 |
0.40/10.0 |
10.0 |
80 |
14.5 |
|
20/630 |
6/190 |
4/125 |
0.40/12.5 |
12.5 |
100 |
18.2 |
|
20/800 |
6/240 |
4/160 |
0.40/16 |
16 |
125 |
23.3 |
|
20/1000 |
6/300 |
4/200 |
0.40/20 |
20 |
160 |
29.1 |
|
20/1250 |
6/380 |
4/250 |
0.40/25 |
25 |
200 |
36.4 |
|
20/1600 |
6/480 |
4/320 |
0.40/32 |
32 |
250 |
46.5 |
|
20/2000 |
6/600 |
4/400 |
0.40/40 |
40 |
320 |
58.2 |
recognize the same faces, a person with poor visual acuity would have to get significantly closer.
In the workplace, there is a multitude of tasks in which it is important to see fine details. Some examples are reading labels, gauges, and dials; inspecting products for cracks, scratches, and foreign material; and visually guided manipulation, as in needle-threading, surgery, and fine assembly tasks. In mobility, acuity is important for recognizing environmental landmarks, avoiding small obstacles, and reading highway signs during driving (Hofstetter, 1976). Acuity is also a strong predictor of self-reported vision-related quality of life.
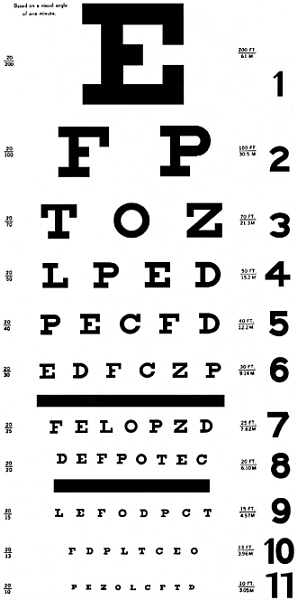
Value as a Practical Measure
In 1865, Hermann Snellen designed the first letter chart for the clinical measurement of visual acuity. It had a large letter at the top, and below it there were 6 rows of letters and numbers in progressively smaller sizes. The chart was viewed from a standard distance, and the size of the smallest letters that could be read provided the measure of visual acuity. Since then, numerous modifications have been made to Snellen’s original chart design, with changes being made to the selection and design of the letters or symbols, the range of sizes, the progression of sizes, the number of letters in the rows, and the spacing between letters and between rows (see Figure 2-1 for a sample chart). While the design has evolved to improve the validity and reliability of visual acuity measurement, Snellen’s letter chart approach has prevailed for more than a century. Letter charts are used almost universally for visual acuity testing of literate adults and school-age children in clinical and research settings. Alternative charts and other test procedures are sometimes necessary for testing infants and preschool children and other individuals who are unable to identify or respond appropriately to the letters or symbols on the chart. While there may be some further modifications to chart design or test procedures, it can be expected that letter chart testing will remain the standard means of measuring visual acuity.
Quantifying Performance
The current SSA standard defines Impairment of Central Visual Acuity as best-corrected Snellen acuity of 20/200 or worse in the better eye, measured with a distance visual acuity chart (Social Security Administration, 1999). Specific recommendations for visual acuity chart design and testing conditions have been made by several bodies (American National Standards Institute International Standards, 1986a, 1986b; Consilium Ophthalmologicum Universale Visual Functions Committee, 1988; National Research Council, 1980, 1994). On the basis of these recommendations, we identify four weaknesses in the current SSA standard:
-
In the SSA standard, the type of chart(s) to be used for testing visual acuity is specified only as “Snellen.” There is no standardized Snellen chart. The most commonly used projector charts and panel charts differ significantly from Snellen’s original chart design, but they are still referred to as Snellen charts. Commonly these charts have few letters at the larger sizes, the size progression varies from one chart to the next, and there is a pattern of having more letters and relatively closer spacings at the smaller sizes.
As emphasized by the 1980 report of the Committee on Vision (National Research Council, 1980), the design of the chart used (including optotype, the number and spacing of optotypes on a line, the range and progression of optotype sizes, the chart luminance, and the nominal contrast between the optotypes and their background) has an important influence on the results of visual acuity measurement. The present standard does not specify chart design requirements and permits the use of charts that may produce very different visual acuity scores. For example, the standard is met when someone fails to read any optotypes that are smaller than the 20/200 optotype. On the most commonly used Snellen charts, the next smallest size optotype is in a 20/100 row, but on others it may be 20/160 or even 20/180. Applying the SSA criterion of “20/200 or worse distance acuity” to such different charts has the functional effect of making the cutoff less than 20/100, less than 20/160, or less than 20/180, according to the chart being used.
-
The current SSA criterion cannot be applied consistently unless there are specific constraints on the design of the test charts. In particular, the optotype size that is next smallest to 20/200 should be specified. The recommended visual acuity chart design has two steps of size 20/125 and 20/160 between the 20/100 and 20/200 levels, and it is also recommend that credit be given for partial success in reading the sample of letters at each size. The SSA standard for Impairment of Central Visual Acuity is that the visual acuity should be 20/200 or worse. With charts of the recommended and more modern design, the literal application of the SSA criterion is that the standard is met when no letters at all can be read at the 20/160 level or smaller. However, the common practice has been and remains testing acuity with charts that have no intermediate sizes between 20/100 and 20/200. As it has been most commonly applied, this means that the SSA standard is met when no letters at all can be read at the 20/100 size or smaller. We are not recommending a change from the criterion for Impairment of Central Visual Acuity. We do, however, recommend standardization of chart design, which would raise policy issues for SSA.
The literal application of the 20/200 or worse criterion with a recommended chart would mean that a sizable group of people who currently qualify would be no longer classified as having Impairment of Central Visual Acuity. These are the people who would be able to read all or some of the letters at the 20/160 or 20/125 sizes while being unable to read any at the 20/100 level. Alternatively, SSA could choose to continue allowing the most commonly applied criterion: no letters can be read at the 20/100 size. This would lead to a sizable group of people’s meeting the criterion, even though their visual acuities could be anywhere in the range from 20/125 to one letter better than 20/200.
-
The standard does not specify the conditions under which visual acuity should be tested. The level of illumination and the testing environment are important factors affecting performance. Inadequate illumination leads to poor performance, as does glare from extraneous light sources. The standard does specify that visual acuity should be tested with best correction; thus, care should be taken to ensure that refractive error is properly corrected prior to visual acuity testing.
-
The standard does not specify the use of standardized testing procedures. There is no universal standard procedure for measuring performance on different lines of a chart, and there are no standard procedures for scoring performance; for example, what should be done when a subject is correct for some elements on each of two adjacent lines? It is common clinical practice to assign a score that indicates the smallest size at which a certain proportion of the optotypes can be read (often the required proportion is “greater than 50 percent”). Scores can depend on whether guessing is encouraged or is obligatory when letters are difficult to read. The absence of standard testing and scoring methods reduces the reliability of measurements.
-
The standard deals only with the performance of the better eye. Everyday vision, however, is based on simultaneous viewing of the world with both eyes. Monocular acuity of the better eye may sometimes underestimate binocular acuity, for example, under conditions in which binocular summation occurs (Cagenello et al., 1993; Home, 1978; Pardhan, 1993) or in subjects with latent nystagmus, a condition in which rhythmic eye movements occur in the unoccluded eye when the other eye is occluded (Helveston & Ellis, 1984). Alternatively, monocular acuity of the better eye may sometimes overestimate binocular acuity, for example, under conditions in which inhibition is produced by the worse eye (Pardhan, 1993; Taylor et al., 1991). Thus, monocular acuity of the better eye is not always an adequate predictor of binocular acuity and therefore of visual resolution in everyday life.
Standardizing Visual Acuity Measurement
Chart Design
There is general agreement that the design of a visual acuity chart should be such that the visual task is the same at each size level, so that size remains the only significant variable from one size level to the next (Bailey & Lovie, 1976). For this principle to be satisfied, the size progression should be logarithmic, there should be the same
number of optotypes at each size level, the spacings between optotypes within a row and between rows should be proportional to the size of the optotype, and the average recognition difficulty should be approximately the same for each row of optotypes.
The Committee on Vision (National Research Council, 1980) recommended the Landolt ring as the reference standard for optotypes, and it considered the Sloan family of 10 nonserif letters (CDHKNORSVZ) designed on a 5 × 5 grid (Sloan, 1959) to be acceptable. Another widely accepted family of optotypes is the British Standards family of 10 nonserif letters (DEFHNPRUVZ), which are designed on a 5 × 4 grid (British Standards Institution, 1968). Both of these charts use letters with a stroke width (critical detail) equal to 1/5 of the letter height. In clinical research today, there is almost universal use of the Early Treatment for Diabetic Retinopathy Study (ETDRS) chart (Figure 2-2) (Ferris et al., 1982), which uses Sloan letters, and the Bailey-Lovie (1976) chart, which uses the British family of letters. These two charts were found acceptable in the 1994 Committee on Vision report (National Research Council, 1994). Both charts have five letters per row, one letter width separating adjacent letters, with the spacing between adjacent rows equal to the height of the letters in the smaller row. Both charts have 14 rows covering a 20-fold range of letter sizes, and both follow a logarithmic (geometric) size progression with a ratio of 0.1 log unit (1.2589×) between each row and the next.
Observation Conditions
For assessment of distance visual acuity, test distance should be 3 meters (10 feet) or more, to minimize the need for the use of accommodation to bring the optotypes into focus. The traditional test distance is 6 meters (20 feet); however, the Committee on Vision (National Research Council, 1980) recommended that the standard test distance be changed to 4 meters because this distance presents an accommodation demand of exactly 0.25 D; it is also conveniently 10 times longer than 40 cm, which is a commonly used distance for testing near vision (Hofstetter, 1973). The ETDRS clinical research protocols use a 4-meter standard test distance, with a recommendation
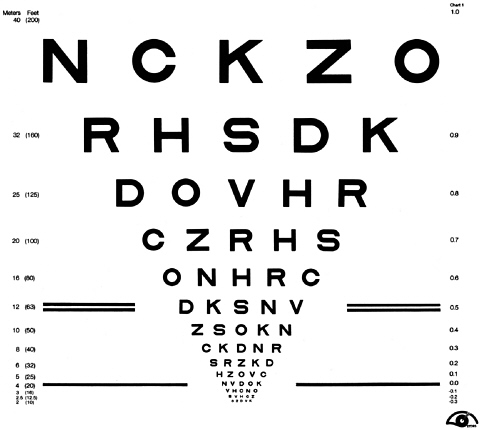
FIGURE 2-2. ETDRS “Chart 1” acuity chart. Source: National Eye Institute, National Institutes of Health.
for shortening of the viewing distance to 1 meter when a visual acuity of 4/40 (equivalent to 20/200) cannot be achieved.
On some charts, the print size is labeled in units of angular size that assume a certain presentation distance. If the testing is performed at some other distance, it is important to use care in scoring and in interpreting the score, to ensure that the nonstandard distance is correctly taken into account. For charts that carry labels in other units
that express angular size in logarithmic units (logMAR or VAR), using the chart at nonstandard distances requires a constant number to be added or subtracted from the score indicated by the size label on the chart.
The charts should be presented in high contrast at moderate photopic luminance. The Committee on Vision (National Research Council, 1980) recommended that the luminance of the chart background be 85+/−5 cd/m2, and that the general room illumination should be low enough that it does not reduce the contrast of the optotypes below 0.85. The 1994 Committee on Vision report recommended 160 cd/m2 background luminance, with a minimum of 80 cd/m2 (National Research Council, 1994). Most common clinical projectors are designed to produce a background luminance of 85 cd/m2, but higher luminances of about 300 cd/m2 are used in many modern projectors, particularly those from Europe. For normally sighted subjects, a twofold change in photopic luminance produces a change of about 5 percent (0.02 log unit) in the acuity score (Sheedy et al., 1984). Tighter tolerances for luminance (of about +/−10 percent or +/−0.04 log units) are recommended for clinical research or for clinical testing when it is important to standardize the luminance conditions (Ferris & Bailey, 1996). Many people with visual impairment can be extraordinarily sensitive to lighting levels (Lie, 1977; Lovie-Kitchin & Bowman, 1985; Sloan, 1969) and, if the goal is to assess functional disability, it may be appropriate to take additional measures of visual acuity at nonstandard luminance levels.
Glare conditions should be avoided. The luminance of the objects and surface surrounding the test chart should not exceed the luminance of the test chart. Care should be taken to avoid reflections from the surface of the chart. Any bright light source or bright reflection in the subject’s field of vision has the potential to be a source of disability glare, which can have the effect of reducing the contrast in the retinal image.
Testing Procedures
Normally, visual acuity is measured when the optimal optical correction (eyeglasses or contact lenses) is being worn. For disability determination, it is logically most appropriate to test binocular acuity. The older algorithm of the American Medical Association (AMA) (American Medical Association, 1993; American Medical Association & the Committee on Medical Rating of Physical Impairment, 1958) for calculating binocular visual efficiency took the monocular acuity of the better eye and added a negative weighting dependent on the visual acuity in the worse eye. The algorithm given in the 1993 AMA guide is
(American Medical Association, 1993). The 2001 AMA guide now recommends using a weighted combination of binocular, right eye, and left eye acuity scores to calculate an acuity-related impairment rating: “Visual impairment ratings are calculated using the formula (3OU + OD + OS)/5 instead of the prior formula (3 × better eye + 1 × lesser eye)/4. The new formula better accounts for situations where the binocular function is not identical to the function of the better eye” (American Medical Association, 2001, p.278).
Under section 12.2b.4, on monocular versus binocular acuity, the new AMA guide states: “Because binocular viewing represents the most common viewing condition in daily life, the impairment rating should consider the best-corrected binocular visual acuity as well as the best-corrected acuity for each eye separately” (American Medical Association, 2001, p.282).
In the committee’s view, measurement of binocular visual acuity is the most appropriate method for evaluating disability. The AMA’s recent inclusion of binocular acuity in their new formula for scoring visual acuity impairment provides similar recognition of the appropriateness of binocular visual acuity testing.
When being tested, the subject should be encouraged to guess at the letters in a row if 40 percent or more of the letters have been read correctly in the previous row. This procedure does not force the subject to guess, but encourages him or her to persist as the letters are becoming difficult to recognize with full confidence. It also does not oblige guessing when the subject feels that letter identification is impossible. If the subject cannot read all letters in the top (largest) row, then the chart should be moved to a closer distance. Should the subject be able to read the smallest letters, the chart should be moved farther from the subject.
Scoring Method
The Committee on Vision (National Research Council, 1980) recommended defining visual acuity as the smallest size at which at least 7 out of 10 optotypes are read correctly. The committee indicated that acuity could alternatively be specified as the last optotype size at which all letters were read, plus the number of optotypes read at the next smaller size (e.g., 20/30+3), or as the number of optotypes missed at the smallest line read (e.g., 20/30−2).
A number of studies have shown that, for logarithmically spaced charts with a constant number of letters per line, such as the Bailey-Lovie (1976) and ETDRS (Ferris et al., 1982) charts, there is greater accuracy in the acuity measurement (i.e., less deviation from the true acuity score) and less variation in test-retest scores when using letter-by-letter scoring rather than assigning a score on a row-by-row basis (Arditi & Cagenello, 1993; Bailey et al., 1991). The 1994 report of the Committee on Vision (National Research Council, 1994) recommended this scoring method. With the Bailey-Lovie and ETDRS charts, there are five letters per row and, given the size progression ratio of 0.1 log units, each letter read correctly can be assigned a value of 0.02 logMAR. Thus there is a total value of 0.1 logMAR per row. The VAR method of designating visual acuity operates similarly, with 1 point assigned for each letter read correctly, so there are 5 points per row. For any chart design, a logMAR value can be assigned to the letters in a given line by subtracting the logMAR value for that letter size from the logMAR
value of the next largest size and dividing that difference by the number of letters in that row.
Measurement reliability may be further increased by taking repeated measurements, but care must be taken to avoid subjects’ memorizing the letter sequences. Some letter charts are produced in multiple forms with different letter sequences that aid in preventing memorization.
Near Visual Acuity
Near visual acuity is measured with hand-held charts, typically at a distance of 40 cm. If the near vision test chart has the same or similar design features as the letter chart used for distance visual acuity, if other test conditions (luminance, contrast, etc.) are the same, and if the subject is wearing appropriate refractive error correction, then the distance and near visual acuity scores should be equivalent to each other. Lovie-Kitchin and Brown (2000) reported a difference of approximately one-half line (two letters) between distance and near visual acuity measured with Bailey-Lovie charts in 24 individuals between 25 and 77 years of age. Lovie-Kitchin attributed the slightly worse near acuity to variations in accommodation, pupil size, and/or depth of focus. In a more recent study of 78 individuals between 21 and 68 years of age, Lovie-Kitchin and Brown (2000) found a difference of one line between distance and near acuity, which they attributed largely to inadequate correction of near vision in older, presbyopic subjects who were tested with their habitual correction rather than the best correction.
Recommendations
Our recommendations concerning assessment of visual acuity are similar to those of the Committee on Vision in its 1980 and 1994 reports (National Research Council, 1980, 1994). We therefore recommend that visual acuity charts should contain the same number of optotypes in each row, the space between optotypes in a row
should be at least as wide as the optotypes in that row, and the size of the optotypes should decrease in 0.1 log unit steps from row to row. The recommended chart luminance is 160 cd/m2, and it should not be less than 80 cd/m2. Viewing should be free from glare, with a level of contrast between optotypes and background that is above 80 percent. The person being tested should be encouraged to read as many optotypes on the chart as possible and to guess at an optotype if he or she is unsure. Acuity results should be scored on an optotype-by-optotype basis, since this scoring procedure produces lower test-retest variability than does row-by-row scoring.
For disability determination, visual acuity should be tested under binocular conditions, since this provides the most representative measure of an individual’s everyday vision. The common clinical practice is to measure the two monocular visual acuities and not test acuity under binocular viewing. The AMA Guide to the Evaluation of Permanent Visual Impairment has used algorithms for combining the two monocular acuities using an averaging procedure that gives a weighting factor of 3:1 to the better eye, and more recently they have proposed an algorithm that combines the two monocular acuities and the binocular acuity. Rubin et al. (2000) found that neither of the AMA algorithms predicted binocular visual acuity as well as taking the visual acuity in the better of the two eyes. We recommend that if binocular vision is not tested, the acuity of the better eye should be used for disability determination.
SSA has need of a cutoff criterion for deciding whether or not an individual has a functional disability. We conclude that currently the scientific evidence does not support a particular visual acuity criterion as a determinant of visual disability. (Chapter 3 provides discussions of the evidence we considered.) Given the history and legislation behind the current SSA standard of “20/200 or worse distance acuity” as the principal criterion for visual disability, we recommend continued use of the 20/200 criterion. Since we recommend a visual acuity chart design that would include optotypes at the 20/160 level, applying the “20/200 or worse” criterion literally to scores obtained with such a chart would set the effective criterion to “worse than 20/160 distance acuity.” The scoring of the charts currently used in disability determination sets the effective criterion at “worse than 20/100.”
The recommended charts have a 20/100 line that would allow SSA to maintain the effective criterion at its current position, but SSA must make the decision on whether this should be done.
It is important to acknowledge the arbitrary nature of selecting a single criterion of visual acuity loss for automatically classifying an individual as having a disability. Visual loss, however it is measured, is associated with decreasing ability to carry out activities associated with employment or (in the case of children) age-appropriate activities. In choosing a visual acuity criterion for determining who is visually disabled, there are some complexities that must be recognized.
It is becoming increasingly clear that the relationships between deficits in visual acuity and deficits in functional status, whether involving mobility, face recognition, or performance of various motor tasks, are monotonic functions with considerable “noise.” This means that an individual’s disability level cannot be confidently predicted from his or her visual acuity alone. Smooth monotonic relationships between acuity and the various functional abilities mean that there will be no clear critical threshold point or sharp inflection above which there is a sharp increase in disability. For any arbitrary cutoff point, there will be substantial numbers of people with better vision who will have more difficulty than expected when performing the given task, and a similar number of people with poorer vision who will have less difficulty than expected when performing the task.
From the published relationships between acuity and functional abilities, it might be predicted that an individual with reduced visual acuity would have certain deficits in functional abilities in several different functional tasks. However, the individual is likely to function better than expected at some tasks and worse at others. Overall disability depends not only on the extent of functional deficits at specific tasks, but also on the relative importance that each of those tasks has in the individual’s regular day-to-day activities.
In conclusion, because available scientific evidence does not justify any criterion for disability, further research is warranted that relates scores on tests of visual impairment to self-report, performance of tasks of everyday life, and performance in the workplace. Such
research would provide urgently needed information on possible disability criteria.
VISUAL FIELDS
Description
The visual field refers to the spatial extent over which the visual system is sensitive to light. The size of the visual field is expressed in terms of visual angle, which is simply the angle subtended at the eye. Visual field eccentricity is the angular distance from the point of fixation, known as the fovea, out to peripheral visual field locations. In normal eyes, the total monocular visual field extent is approximately 160° horizontally and 100° vertically. The visual fields of the two eyes overlap, except for the far temporal visual field of each eye. The binocular visual field thus extends slightly farther horizontally to approximately 180-200°. By convention in clinical perimetry, the macular region extends out to 5° radius (10° diameter) from fixation, the central visual field refers to peripheral eccentricities out to 30° radius (60° diameter), and the peripheral visual field refers to eccentricities that are beyond 30° radius (60° diameter). Throughout this section on visual fields, these definitions of macular, central, and peripheral visual fields are employed.1
For normal illumination in the work environment, visual function and visual sensitivity are not uniform over the entire visual field. Under typical illumination conditions for the workplace, the point of fixation has the best visual function and highest sensitivity. Visual sensitivity and other visual functions systematically decline with increasing peripheral eccentricity.
The visual field is typically measured by one of several methods of perimetry, which in its most conventional form involves the detection of a small spot of light projected onto a uniform background. The 1994 report of the Committee on Vision (National Research Council, 1994) provides an overview of visual field measurement techniques and important factors relevant to visual field testing. Currently, the most common form of visual field testing is automated static perimetry. For the most commonly used test procedure, the sensitivity for detecting a small spot of light projected onto a uniform white background (the minimum amount of light needed to detect the spot of light) is measured for 76 locations on an evenly spaced grid (6° spacing) throughout the central 30° radius of the visual field.
Evaluation
Why the Measure Is Useful
Perimetry and visual field testing are methods commonly used in clinical ophthalmic settings to provide a quantitative assessment of the integrity of the field of view. Visual field testing is important because it is the only clinical test that evaluates vision outside the macula. All other tests of visual function that are performed in a clinical ophthalmic setting evaluate foveal vision (vision at the point of fixation). Thus, measurement of the visual field provides information that does not overlap with other procedures. Peripheral and central vision have been found to be important for performing many daily activities, and people with significantly restricted visual fields experience many difficulties with occupational demands and other activities (Gutierrez et al., 1997; Johnson & Keltner, 1983; Lovie-Kitchin, Mainstone, et al., 1990; Lovie-Kitchin, Woods, et al., 2001; Marron & Bailey, 1982). As mentioned earlier, visual field measurements are currently used by SSA as part of their visual disability determination procedures. This section provides a summary of the relationship between visual fields and four tasks that are important with respect to the work environment: reading, orientation/mobility, social participation, and tool use.
Reading. Most of the research on reading has been concerned with factors related to foveal vision capabilities. The relationship between reading and nonfoveal visual fields has mainly been centered on two areas: (1) the residual reading capabilities of the remaining visual field in people with central visual loss and (2) reading problems in people with homonymous hemianopsia, which is complete loss of either the right or left side of the visual field, usually due to stroke. When foveal vision is degraded, reading speed and comprehension are reduced (Chung et al., 1998; Rayner & Bertera, 1979; Rubin & Turano, 1994). Some of this loss is due to inaccurate eye movements, and some is due to the limited rate at which the remaining visual field can perform the pattern decoding required for reading (Rubin & Turano, 1994). In subjects with simulated central scotomas (blind spots or areas of nonseeing surrounded by areas of seeing), reading rates are faster when the material is presented to the inferior visual field than for other visual field locations (Petre et al., 2000).
During reading, people with right homonymous hemianopsias make a greater number of refixation saccades that are smaller in amplitude than for normally sighted individuals (DeLuca et al., 1996; Trauzettel-Klosinski & Brendler, 1998). People with left homonymous hemianopsias make a greater number of refixations on the return sweep to begin reading a new line (Trauzettel-Klosinski & Brendler, 1998). Although both types of hemianopsias reduce reading speed, right homonymous hemianopsias have been reported to produce greater deficits than left homonymous hemianopsias (Trauzettel-Klosinski & Brendler, 1998).
Orientation/Mobility. Much is known about the relationship between visual field status and mobility, particularly for driving. Marron and Bailey (1982) found that the visual field was an important predictor of success in mobility training for people with low vision. Turano and colleagues have reported that people with either central or peripheral visual field loss exhibit a deficit in the visual stabilization of body sway (Turano, Dagnelie, & Herdman, 1996; Turano, Herdman, & Dagnelie, 1993). In addition, they have reported deficits in mobility performance in people with restricted visual fields due to glaucoma or retinitis pigmentosa (Geruschat et al., 1998; Turano et al., 1999).
Lovie-Kitchen et al. (1990) evaluated the relationship between visual field size and orientation and mobility performance in nine people with low vision and nine age-matched normal controls, using an indoor obstacle course. They found that mobility performance (time taken to traverse the course and number of errors) was significantly influenced by total visual field extent. Individuals with smaller visual field extents had poorer mobility performance. Although both time to traverse the course and errors were affected by visual field size, errors were more highly correlated with visual field extent. The central 37° radius and the right, left, and inferior zones in the midperiphery were the most important visual field locations for mobility performance. Horizontal objects at head height and large objects on or suspended just above the floor were the most difficult for people with low vision to distinguish. A recent follow-up study of 79 people with low vision and 20 age-matched controls (Lovie-Kitchin et al., 2001) confirmed these findings. In addition, they reported that mobility performance became impaired when the visual field extent was smaller than 85°, and that mobility training would be required at some point when an individual’s visual field was between 20° and 85°.
The visual field requirements for a driver’s license vary considerably from one country to another (Charman, 1985) and from one state to another in this country (Keltner & Johnson, 1987). For those entities that have a visual field requirement for driving, the horizontal extent varies from about 20° to about 140°. A number of investigators have found statistically significant relationships between visual field size and driving accident and conviction records (Burg, 1967, 1968; North, 1985; Shinar, 1977; Shinar et al., 1975). However, although these relationships are statistically significant, the correlations are quite low, and visual field extent typically accounts for only about 5 percent of the variance for accident and conviction records.
Council and Allen (1974) found no relationship between the visual field size and accident and conviction records, although their peripheral vision test procedure was not validated and was likely to have rather high false positive and false negative rates. Johnson and Keltner (1983) found that accidents and convictions were more than twice as high in drivers with visual field loss in both eyes, compared with age- and sex-matched controls with normal peripheral vision.
There was no difference in accident and conviction records of drivers with visual field loss in only one eye compared with age- and sex-matched controls with normal peripheral vision.
Evaluation of the driving performance of people with various ocular and neurological disorders has been performed with the use of driving simulators (Hedin & Lovsund, 1986; Szlyk & Brigell, 1992). Although people with visual field loss tended to demonstrate deficits in driving performance, there were large individual differences. Some individuals appeared to be able to compensate for their visual field loss while others did not, even though they may have had equivalent visual field damage.
Wood and Troutbeck (1992) evaluated the influence of restricting the binocular visual field of drivers using a closed road track. They found that restricted visual fields impaired several driving tasks, including identification of road signs, efficiency in traversing the course, obstacle avoidance, and maneuvering through limited spaces. However, these deficits were not significant until the binocular visual field had been reduced to 40° or less.
Ball, Owsley, and colleagues have developed an alternative method of evaluating the central visual field (Owsley et al., 1991). Their test procedure evaluates visual search, localization, and divided attention tasks and is known as the useful field of view. Deficits in the useful field of view are more prevalent in older drivers than is traditionally measured visual field loss. Their findings suggest that the useful field of view may be a better predictor of accidents than visual fields or any other vision test. Chapter 3 presents a more detailed discussion of this research in the section on driving mobility.
Social Participation. There is only sparse information in the literature concerning the relationship between visual fields and social participation. Gutierrez et al. (1997) reported a statistically significant relationship (p < .001) between the visual field status of the better eye and the VF-14 social function scale (r = −0.29) and the emotion/well-being scale (r = −0.28) for people with glaucoma. From a practical standpoint, extensive visual field loss can impair an individual’s ability to be aware of the presence and location of others, which can affect social interactions.
Tool Use/Manipulation. There is little or no formal literature on the role of the peripheral visual field and tool use/manipulation. Most tasks involving the use of tools are primarily dependent on central vision. However, any activity concerned with tool use/manipulation that incorporates a visual search task (e.g., detection of warning lights on a panel display, localization of objects to reach) may be affected by visual field loss, particularly if it is severe loss in both eyes.
Value as a Practical Measure
For nearly 200 years, perimetry and visual field testing procedures have been used clinically to assess the status of the peripheral visual field. Although there are a small number of individuals who are unable to perform perimetry because of significant physical or mental limitations, most adults can be tested with some form of perimetry. Automated static perimetry is currently a standard clinical ophthalmic diagnostic procedure that is used by the majority of eye care practitioners.
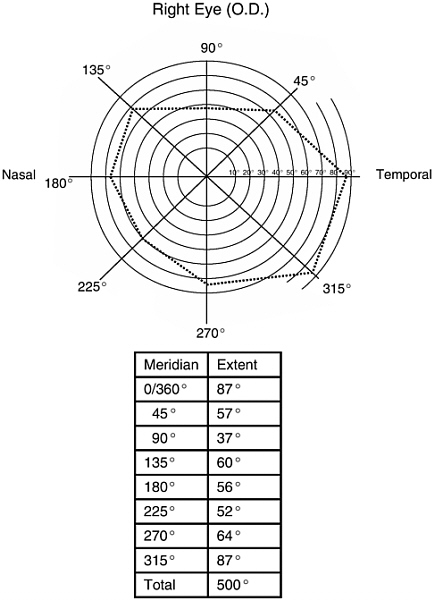
Quantifying Performance
The current visual field requirement for legal blindness is defined in terms of the size of the isopter generated by a Goldmann III/4e stimulus along eight principal meridians (0, 45, 90, 135, 180, 225, 270 and 315°). Figure 2-3 illustrates the plotting of an isopter. The chart represents the visual field of a normal right eye, with the greatest measured extent of vision, in degrees from the point of fixation (center of the diagram), marked on each of the eight meridians. The heavy dotted line connecting these points is the isopter. The Goldmann III/4e stimulus consists of a 0.43° target of 318 cd/m2 luminance (1,000 apostilbs) projected onto a 10 cd/m2 background luminance (31.5 apostilbs). A visual field is considered to be normal if the sum of the radii of the eight principal meridians is equal to or greater than 500°. Total visual disability (0 percent efficiency) is defined as a contraction of the visual field of the better eye to less than or
equal to 10° from fixation, or less than or equal to 20° maximum diameter. For less than total disability, the percentage of visual efficiency is calculated as the sum of the radii of the eight principal meridians divided by 500° multiplied by 100.
There are several problems associated with the current method of making disability determinations for visual field loss. First, there is the very practical issue that Goldmann perimeters are becoming increasingly scarce, and fewer individuals have the proper training for performing kinetic testing on the Goldmann perimeter (Anderson & Patella, 1999). It is estimated that more than 95 percent of all eye care practitioners in the United States use an automated device to perform visual field testing. Second, with Goldmann perimetry a single isopter is used to define the outer limit of peripheral vision. This ignores scotomas, which could represent a large portion of the visual field.
For example, an individual with retinitis pigmentosa could have an extensive “ring” scotoma extending from approximately 3° from fixation out to more than 50°. However, with a rim of seeing beyond the ring scotoma, it is possible that the individual could show a normal or nearly normal Goldmann III/4e isopter despite having a scotoma encompassing a major portion of the visual field. Third, kinetic testing on the Goldmann perimeter can vary considerably from one examiner to another, whereas automated perimetric test strategies are conducted in the same manner every time. Fourth, Goldmann perimetric testing does not provide a standard means of assessing the reliability of the individual being tested or the accuracy and reliability of fixation, whereas automated perimetry does. Fifth, the Goldmann testing protocol evaluates the visual field extent along only eight meridians; intermediate areas between these meridians are not evaluated. Finally, the current standards are based on monocular visual field characteristics, whereas performance in real life is dependent on the binocular visual field. Because areas of nonseeing in the two eyes do not always overlap, the visual field of the better eye does not necessarily provide the best indication of the functional binocular visual field. However, there is currently no simple procedure available commercially for determining the binocular visual field from monocular data. Until such procedures become available, the visual field of the better eye should be used for disability
determination. Many of these issues were pointed out previously by the Committee on Vision (National Research Council, 1994).
We conclude from our study of available perimetry methods that automated threshold static perimetry procedures should be employed as the method of performing visual field disability determinations. To ensure that accurate, reliable and valid results are obtained, we also recommend that an automated static perimeter meet the following criteria to be considered as an approved visual field device for SSA disability determinations:
-
The automated static perimeter should be capable of performing threshold testing using a white size III Goldmann target and a 31.5 apostilb (10 cd/m2) white background.
-
The perimeter should be capable of measuring sensitivity for the central 30° radius of the visual field with equal numbers of target locations in each quadrant of the field, and target locations no more than 6° apart.
-
The perimeter should be a projection perimeter or should produce measures that are equal to those obtained on a projection perimeter.
-
The perimeter should have an internal normative database for automatically comparing an individual’s performance with that of the general population.
-
The perimeter should have a statistical analysis package that is able to calculate visual field indices, particularly mean deviation or mean defect (MD), which is the average deviation of visual field sensitivity in comparison to normal values for the central 30° radius of the visual field.
-
The perimeter should demonstrate high sensitivity (ability to correctly detect visual field loss) and specificity (ability to correctly identify normal visual fields).
-
The perimeter should demonstrate good test-retest reliability.
-
The perimeter should have undergone clinical validation studies by three or more independent laboratories with results published in peer-reviewed ophthalmic journals.
At the present time, two perimeters are known to meet these criteria: the Humphrey Field Analyzer and the Octopus. Several studies have shown that the results obtained by the Humphrey Field Analyzer and the Octopus are highly correlated (Funkhouser & Funkhouser, 1991; Johnson et al., 1987b; Papp et al., 2001).
Mean deviation (MD) on the Humphrey Field Analyzer and mean defect (MD) on the Octopus perimeter represent the average overall deviation of visual field sensitivity from normal for the central 30° radius of the visual field. MD is a suitable marker of visual field status that takes into account both the size and depth (severity) of sensitivity losses. MD is automatically calculated by a statistical analysis program provided in the perimeter software that compares individual results to a database, and is printed out in hard copy. The normative databases include people of different ages, gender, and ethnicity. For each visual field location, the subject’s sensitivity is compared with the average sensitivity for people of the same age, using the values in the database. For each visual field location, a “deviation from average normal” value in decibels (dB), a logarithmic scale, is determined. If the subject’s sensitivity is better than the average normal individual of the same age, then the deviation value is positive. If the subject’s sensitivity is lower, then the deviation is negative. Mean deviation or mean defect is thus the average sensitivity deviation from the normal values for all measured visual field locations.
There are several advantages to using these values as a means of determining visual field loss. First, MD represents a direct comparison of the subject’s sensitivity with that of the normal population. Second, it automatically takes normal aging changes of the visual field into account, comparing the subject’s results to normal individuals of the same age. Third, it is a quantitative measurement. Fourth, it not only takes into account the extent of the visual field, but it also evaluates the density of sensitivity loss. It therefore represents a better indicator of the individual’s overall visual field capabilities. Finally, it
serves as the best overall quantitative indicator of the amount of visual field damage.
There are two minor disadvantages. MD does not provide an indication of the spatial extent of visual field loss, and it is derived from evaluations of only the central visual field (60° diameter or 30° radius). The advantages greatly outweigh the disadvantages for disability determinations, however. If an individual had complete peripheral visual field loss and normal vision within the central 10° radius (the current SSA visual field standard), this would correspond to an MD of approximately −22 dB, which is considered to represent extensive visual field loss.
Relation to Other Measures
Visual field measures can be somewhat independent of visual acuity, contrast sensitivity, color vision, stereopsis, and other central visual function measures. For some disorders, visual field loss can be present when visual acuity and contrast sensitivity are normal. In other cases, visual field loss can occur in conjunction with visual acuity or contrast sensitivity deficits. Thus, it is important that the visual field and visual acuity be considered together for disability determinations. A method of combining visual field and visual acuity values to derive an aggregate disability score is presented later in this chapter.
Quality of Information Available
Automated threshold static perimetry using a projection perimeter is the current gold standard for ophthalmic visual field testing. The threshold procedures for those perimeters meeting our proposed criteria have been shown to produce accurate and reliable information concerning visual field sensitivity. Recently, new threshold test strategies for the Humphrey Field Analyzer, SITA-standard and SITA-fast, have been able to reduce testing time by 35 to 50 percent (Bengtsson & Heijl, 1998a, 1998b, 1999a, 1999b; Bengtsson, Heijl, et
al., 1998; Bengtsson, Olsson, et al., 1997; Wild et al., 1999), while maintaining the same accuracy and reliability as previous staircase threshold procedures. A similar efficient test strategy, Tendency Oriented Perimetry (TOP), has been introduced for the Octopus perimeter (Morales et al., 2000). Automated threshold testing of the central 30° radius seems to be the most appropriate means of obtaining the best visual field information for disability determinations.
Recently, there was an investigation of an experimental automated kinetic perimetry procedure implemented on the Humphrey Field Analyzer (Odom et al., 1998). Based on their findings, those authors recommend that this new custom automated kinetic perimetry procedure be used for disability determinations. The committee disagrees with these recommendations for several reasons. First, kinetic perimetry is more variable than static perimetry, even when the procedure is automated (Lynn et al., 1991; Keltner et al., 1999). Second, there have been numerous attempts over the past 25 years to develop and validate an automated procedure for performing kinetic perimetry (Johnson et al., 1987a; Lynn et al., 1991; Miller et al., 1989; Schiefer et al., 2001; Zingirian et al., 1991). To date, all of these attempts have failed to produce a valid kinetic visual field test, in spite of the fact that some of these utilized much more sophisticated algorithms than those described in the Odom et al. (1998) report. Examples of the many problems encountered for automated kinetic perimetry can be found in Lynn et al. (1991). In the committee’s view, automated kinetic perimetry affords no clear advantages over automated static perimetry and has a number of drawbacks. It should be noted that Humphrey Systems has recently released an automated kinetic perimetry program that it is promoting for disability determinations. However, no clinical validation studies of this procedure have been performed to date, and therefore its performance characteristics are unknown at the present time. In our judgment, automated threshold static perimetry should be used as the basis for establishing visual field status for disability determinations.
Recommendations
The committee recommends that the current SSA standard should be revised so that disability determinations are based on the results of automated static projection perimetry rather than Goldmann (kinetic, nonautomated) visual fields. At present, the Humphrey Field Analyzer and the Octopus perimeters are known to meet the criteria that we propose for automated perimeters that are to be used for disability determination. (Previous recommended methodology and scoring procedures for manual kinetic perimetry using the Goldmann perimetry were not based on empirical data. No validation study of the Goldmann disability determination procedure was performed.)
For both devices, we recommend that a threshold procedure should be employed for visual field determinations (for example, Full Threshold, Fastpac, SITA, and SITA Fast are all suitable alternatives for the Humphrey; Threshold, TOPS, and TOPS Plus are suitable alternatives for the Octopus). We recommend using a target presentation pattern that can measure sensitivity for the central 30° radius of the visual field with equal numbers of target locations in each quadrant of the field, and target locations no more than 6° apart.
We recommend that suprathreshold screening procedures should not be used because the techniques have not been validated, the results from them are not quantitative, and they generally do not provide a good indication of the amount of visual field damage that is present. We also recommend not using the visual field scoring procedures recently published by the American Medical Association (1993). The AMA guidelines are not based on empirical data, the procedures have not been validated, and their properties are largely unknown.
To account for scotomas and normal visual field locations between major meridians, we recommend that an index of the overall visual field status be used for disability determinations. MD provides the best overall indication of visual field status, taking into account both the spatial extent and the localized sensitivity variations that are present in the visual field. An MD of −22 dB approximately corresponds to a visual field extent of less than 10° radius (the current SSA standard). Mean deviation and Advanced Glaucoma Intervention
Study (AGIS) scores (which are highly correlated with mean deviation because both are derived from individual total deviation values) have been shown to be related to quality of life indicators and mobility skills (Gutierrez et al., 1997; Sumi et al., 2000). For this reason, MD represents an excellent measure on which to base disability determinations.
Ideally, one would have a measure of the binocular visual field serve as the basis for disability determinations because the binocular visual field is what people use for daily activities. However, simple procedures for determining the binocular visual field empirically, or deriving it from monocular visual field results, are not currently available. Current automated perimeters are not designed to perform binocular testing. Neither is an easy procedure for calculating the binocular visual field currently available. We recommend further research to be directed toward developing such procedures. Until such procedures can be implemented, we recommend that the visual field results for the better eye should be used for disability determinations. Thus, the recommended visual field criterion for SSA disability determinations would be an MD in the better eye of −22 dB or worse.
Issues Needing Further Study
Aside from studies of driving and a few investigations of mobility performance in people with low vision, there is currently very little information on the relationship between the status of the visual field and performance of daily activities, occupational demands, and task performance. Several validation studies have been performed for occupational vision requirements of correctional officers, youth counselors, and a group of California supervisors, parole agents, game wardens, park rangers, driver’s license examiners, and youth authority academic teachers (Johnson, 1993; Johnson & Brintz, 1994, 1996, 1997; Johnson & Day, 1994a, 1994b; Johnson et al., 1992). The specific tasks that were performed in these studies were different for each occupation and were designed to simulate activities that were an essential part of the job. However, in each instance, performance deficits were found for visual field sizes below 60° in diameter. This is
similar to the findings by Lovie-Kitchen and colleagues (2001) that mobility performance became impaired for those with visual field sizes less than 85° in diameter. For some demanding surveillance and search tasks, a visual field of 120° or more in diameter was necessary for maintaining adequate task performance. However, very little is known about the impact of reduced visual fields on activities of daily living and occupational requirements. Another area in need of future research is the development of techniques for providing valid and reliable measures of binocular visual field sensitivity.
CONTRAST SENSITIVITY
Description
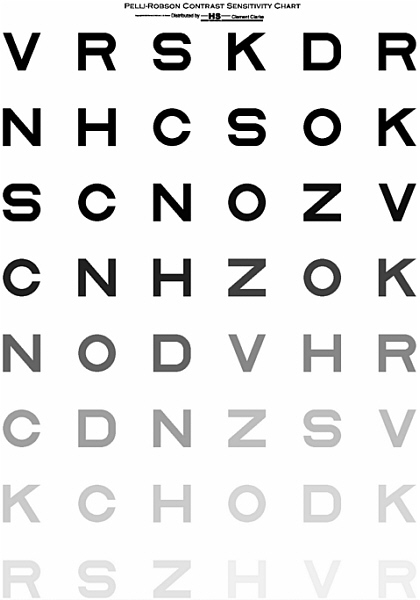
Contrast is a measure of the differences in luminance (brightness) across borders. For example, typical text, consisting of black print on a white background, has very high contrast. Figure 2-4 (Pelli et al., 1988) illustrates letters with high contrast (about 100 percent) at the top left, becoming lower contrast as one reads down the chart. Contrast sensitivity is a measure of the lowest contrast that an observer can detect. A subject’s contrast sensitivity on such a chart is expressed as a measure of the lowest contrast letters he or she can read correctly.
Evaluation
Why the Measure Might Be Useful
Contrast provides critical information about edges, borders, and variations in luminance. Thus, the normal visual system has high contrast sensitivity. While it has long been realized that measurements of contrast sensitivity might be particularly informative about visual disability, it is only in the past decade or so that it has become possible to measure contrast sensitivity simply and accurately in clinical practice or to use measures of contrast sensitivity in screening conducted by lay people.
Current disability assessment for vision involves primarily high-contrast letters; however, the world is not always seen in high contrast. The standard high-contrast visual acuity chart measures the ability to see black letters (about 1 or 2 percent reflectance) on a white background (close to 100 percent reflectance) giving close to 100 percent contrast.2 Furthermore, the measurement is conducted in excellent lighting. The real world, however, is very far from this ideal. It consists of objects with an average reflectance of 18 percent, and the contrast between objects of interest and their backgrounds is usually much less than 100 percent. For example, the contrast between the pavement and the sidewalk, which is the main cue that defines the edge of a curb, may typically be just a few percent.
Contrast sensitivity tests can pick up losses that are not evident from measuring visual acuity. For example, contrast sensitivity tests may be sensitive to visual loss caused by cataracts, glaucoma, and multiple sclerosis (diseases in which impairment in contrast sensitivity is common), in subjects with little or no loss in visual acuity (Regan, 1991b). These people may fail to see large, low-contrast objects under conditions of poor visibility (such as fog) despite normal or near normal visual acuity. Elliott (1998) lists additional situations in which contrast sensitivity testing may be useful. In addition, several chapters in the Spatial Vision volume of Cronly-Dillon (Cronly-Dillon, 1991; Regan, 1991a) discuss contrast sensitivity in normal vision and in disease.
As Regan (1991b) points out, these losses are “hidden to the Snellen test.” Moreover, as documented below, contrast sensitivity may predict performance for both reading and mobility in persons with low vision and makes strong predictions related to driving. Similarly, contrast sensitivity may be an important predictor of performance in individuals with cerebral lesions (Regan, 1991b). Although contrast sensitivity may not be very helpful in diagnosis, it is very useful in predicting disability.
Reading. Reading is remarkably robust to contrast variations in normally sighted readers (Legge, Rubin, & Luebker, 1987; Legge, Rubin, Pelli, & Schleske, 1985). However, in one small-sample study it was estimated that the “critical contrast” (i.e., the contrast at which the reading rate drops to half of its maximum value) is, on average, four times higher in persons with low vision than in normally sighted persons, and this critical contrast is strongly correlated with the person’s contrast sensitivity (Rubin & Legge, 1989). Indeed, Rubin and Legge suggest that there is a subset of individuals with low vision (with cataract and cloudy media) who are essentially normal readers, except for an early stage of reduction in retinal image contrast. Based on this and other evidence, Leat et al. (1999) suggest that a Pelli-Robson contrast sensitivity score of less than 1.5 would result in visual impairment and a score of less than 1.05 would result in disability. (The Pelli-Robson test is described in detail below. It measures contrast sensitivity using a single large letter size, with contrast varying across groups of letters.) In a recent large-scale study, West et al. (in press) found that more than 50 percent of people with a Pelli-Robson score of lower than 1.4 read fewer than 90 words per minute (wpm) (defined as disabling).
The Pelli-Robson score represents the logarithm of the subject’s contrast sensitivity. Thus a score of 2, indicating a contrast sensitivity of 100 percent, means that the lowest contrast letters the observer can read correctly have a contrast of 1 percent (i.e., 1/100).
Whittaker and Lovie-Kitchin (1993) surveyed the literature on the effects of various parameters, including contrast, on reading speed. They defined the “contrast reserve” as the ratio of print contrast to threshold contrast. From their survey of the published data on low and normal reading rates versus text contrast, they concluded that the contrast reserve had to be at least 10:1 for reading at a low normal speed of 174 wpm; a 4:1 reserve to read at 88 wpm, and a 3:1 reserve for “spot reading,” i.e., 44 wpm. These were upper-bound values, and many subjects who had contrast reserves of, say, 10:1 did not reach 174 wpm.
For text contrast of 100 percent, a person would require a contrast threshold of 10 percent or lower in order to achieve the 10:1 contrast
reserve necessary for the low normal rate of 174 wpm. If the text itself is lower contrast, for example, newsprint with a contrast of 70 percent, then the reader’s contrast threshold would have to be lower than 7 percent to achieve the desired 10:1 reserve. A contrast threshold of 10 percent corresponds to a Pelli-Robson score of 1.0. Based on the analysis of Whittaker and Lovie-Kitchin, we can conclude that a contrast sensitivity of 1.0 or better is required to read high-contrast print at a low normal speed. Although the details of the Whittaker and Lovie-Kitchin and the Leat et al. (1999) studies differ, their conclusions are rather close.
To summarize, it seems reasonable to conclude that a person with a contrast sensitivity of 1.0 might sometimes be able to achieve a low normal reading speed (174 wpm), but most will read more slowly. If text contrast is lower or contrast sensitivity is poorer, reading will be slower. Thus, setting a Pelli-Robson boundary of about 1.0 almost certainly guarantees that everyone below this line will have functionally significant contrast limitation in reading.
Although standard letter chart acuity and contrast sensitivity are highly correlated in the overall population, it is not possible on an individual (clinical) basis to predict contrast sensitivity accurately from acuity (Haegerstrom-Portnoy, et al., 2000). It is therefore necessary to measure both, because measuring contrast sensitivity provides new information related to visual disability.
Mobility. For normally sighted people, mobility is remarkably robust to contrast, at least under controlled conditions. Pelli (1987) found that in normally sighted subjects mobility is only slightly impaired when the contrast is reduced to 2 to 4 percent of the normal level. However, these studies were performed in a relatively safe shopping mall environment, with few of the typical low-contrast hazards, such as step-ups. Poor contrast sensitivity (a Pelli-Robson score of 0.9 or lower) is disabling with regard to walking speed (West et al., in press).
In contrast, for those with visual impairments, a number of studies have shown an association between contrast sensitivity and mobility (Geruschat et al., 1998; Kuyk & Elliott, 1999; Kuyk, et al., 1998; Marron & Bailey, 1982; Rubin, et al., 1994; Turano et al., 1999). As noted in the section on ambulatory mobility (in Chapter 3), in nearly
all cases, contrast sensitivity was a far better predictor of mobility performance than acuity (and often the only predictor). For example, Marron and Bailey (1982) reported a strong correlation between mobility and contrast sensitivity in a group of people with low vision. Contrast sensitivity was a better predictor of mobility performance than visual acuity. Combining visual field measures with contrast sensitivity provided the best predictor of mobility performance.
Contrast sensitivity is a better predictor of driving performance than visual acuity. Reduced contrast sensitivity is associated with older persons’ reports of difficulty in mobility and driving (Rubin et al., 1994). Closed road driving with simulated cataracts produces decrements in driving performance, and the overall driving score is correlated with Pelli-Robson contrast sensitivity (Wood & Troutbeck, 1995; Wood, et al., 1993). There have also been several reports that suggest a relationship between contrast sensitivity and number of (at-fault) crashes (Ball et al., 1993; Owsley, Ball, et al., 1998). As noted in Chapter 3, contrast sensitivity impairment in older drivers, especially those with cataracts, is associated with crash involvement, when visual acuity shows no association (Owsley, McGwin, et al., 2001).
Social Participation and Tool Use/Manipulation. Not much is known about the relationship between contrast sensitivity and social participation or tool use. Contrast sensitivity has been related to face recognition (Owsley & Sloane, 1987). West et al. (in press) showed that subjects with 1.3 log contrast would be unable to recognize more than 50 percent of faces in a face recognition test. Contrast sensitivity loss has been associated with difficulty with everyday tasks, both self-reported difficulty (Rubin et al., 2001) and difficulty based on performance measures (Rubin et al., 1994; West et al., in press); however, these areas require additional study. It is clear from observations of typical manual tasks (e.g., sewing with a dark thread on dark cloth, doing woodwork and joinery) that the contrasts between different crucial parts of the task materials can be very low, as can the luminances of the materials. It is likely that if one’s ability to see under such reduced contrast (and luminance) is impaired, task performance will be adversely affected.
Potential Value as a Practical Measure
The importance of measuring contrast sensitivity is that it can provide information that cannot be obtained from visual acuity measures, and it is often a better predictor of performance than visual acuity, as discussed above.
Quantifying Performance
In the laboratory, contrast sensitivity is usually measured psychophysically, using patches of grating (bars) that vary over a wide range of sizes (spatial frequencies). Typically, the gratings are computer generated and displayed on a computer screen or cathode ray tube. This allows the experimenter to construct a contrast sensitivity function. However, for clinical, screening, or disability determination purposes the contrast sensitivity function is inefficient and difficult to interpret. Moreover, the typical laboratory test for it requires sophisticated and specialized equipment.
Ideally, a contrast sensitivity test for disability determination should satisfy several criteria. It should be simple to administer, requiring no sophisticated electronic or computer equipment, well standardized, reliable, valid, sensitive to visual loss, and relatively insensitive to changes in focus, viewing distance, and illumination. It should provide a single score that is meaningful and can easily be compared with extensive normative data and should provide information about visual function not captured by other tests (such as high contrast acuity).
Several clinical tests of contrast sensitivity have been developed over the last two decades. One of the first was the Vistech charts, which measure contrast sensitivity for gratings of several spatial frequencies. One difficulty with these charts is that the result is a contrast sensitivity function rather than a single number. Another difficulty is that test-retest reliability for the Vistech charts has been shown to be lower than for some other contrast sensitivity tests (Rubin, 1988). Reliability is a critical requirement for disability determination. The
Vistech test is not suitable for individuals with significant degrees of astigmatism, because the gratings are oriented. Finally, there is only a single target at each contrast level, so there is effectively one trial per level. In addition to the Vistech, there are also several low (fixed) contrast letter charts available, as well as CRT-based contrast sensitivity tests.
The currently available test that best meets the requirements laid out above is the recently developed Pelli-Robson chart (Pelli et al., 1988). This test measures contrast sensitivity for a single (large) letter size. Specifically, the chart uses Sloan letters (6 per line), arranged in groups whose contrast varies from high to low. The chart is simple to use, because the subject simply reads the letters, starting with the highest contrast, until she or he misses two or three letters in a single group. Each group has three letters of the same contrast level, so there are three trials per contrast level. The subject is assigned a score based on the contrast of the last group in which two or three letters were correctly read. The score, a single number, is a measure of the subject’s log contrast sensitivity. Thus a score of 2 means that the subject was able to read at least two of the three letters with a contrast of 1 percent (contrast sensitivity = 100 percent or log 2). The single score facilitates combining scores across visual functions to obtain an aggregate visual impairment score for use in determining disability.
The Pelli-Robson chart is quick and easy to administer. Because it is based on reading letters, it can be easily administered to anyone who is literate; however, it is not useful with nonverbal individuals or those who are unfamiliar with the alphabet. It is robust to changes in viewing distance, defocus, and to some degree illumination level. Also, since letters contain many orientations, it is not strongly dependent on a particular orientation, as the Vistech chart is. It is simple, efficient, and provides user-friendly information by providing a single number to describe the observer’s contrast sensitivity. The chart has been extensively normed and validated, and there is now an extensive literature on the reliability and validity of the test.
The Pelli-Robson chart reflects contrast sensitivity near the peak of the contrast sensitivity function (Rohaly & Owsley, 1993). It is actually a measure of the height of the contrast sensitivity function, similar to
measuring contrast sensitivity for a luminance edge. Thus, it should be sensitive to losses that affect low and medium spatial frequencies, losses that might not be evident for high-contrast acuity, thus providing information not captured by acuity testing. The Pelli-Robson chart is now widely used in clinical trials and is being considered for use by some state departments of motor vehicles as part of their driving test battery.
The Pelli-Robson chart provides a graded index of performance (log contrast sensitivity), and the score appears to reasonably reflect degree of ability or disability. As noted above, Leat et al. (1999) argue that a score of less than about 1.5 reflects visual impairment, and they estimated that a score of less than 1.05 would result in disability. This score represents an approximately 10-fold loss of contrast sensitivity. That is, the person requires 10 times as much contrast to see the target letters as a person with normal vision (e.g., 10 percent contrast versus the normal 1 percent). A loss of this magnitude would have a huge impact on one’s ability to drive or read. In short, a 10-fold loss of letter contrast sensitivity would be quite disabling.
Relation to Other Measures
Contrast sensitivity measures provide information that is related to, but is also distinct from, high-contrast visual acuity measures. For example, a number of studies have reported that the correlation between high-contrast acuity and contrast sensitivity is on the order of 0.5 to 0.6 (Rubin, Bandeen-Roche, et al., 1994; Rubin, West, et al., 1997). It is widely believed that letter contrast sensitivity (as assessed by Pelli-Robson) reflects the contrast sensitivity near the peak of the contrast sensitivity function, while high-contrast letter acuity probably reflects sensitivity at high spatial frequencies.
Does contrast sensitivity provide a unique measure of disability? It subsumes visual acuity. Thus an individual with visual acuity poorer than 20/200 is likely to have reduced contrast sensitivity, and one with a visual acuity of 20/40 or better is unlikely to have significantly reduced contrast sensitivity. However, between those limits (acuity
between about 20/50 and 20/100), contrast sensitivity may distinguish individuals with visual impairment from those with no impairment; in other words, some individuals whose visual acuity is better than the current SSA disability standard have genuine visual impairment that is evident in their contrast sensitivity scores. For example, people with multiple sclerosis (Regan, 1991b) or visual pathway disorders (Elliott, 1998) may show significant contrast sensitivity loss with little visual acuity loss and, as discussed in Chapter 3, contrast sensitivity is a better predictor of mobility and reading performance than visual acuity.
Quality of Information Available
A number of different contrast sensitivity tests are available. As noted above, contrast sensitivity is the standard laboratory measure of spatial vision. There are now a number of commercially available charts for testing contrast sensitivity, the most widely used of which are the Vistech charts and the Pelli-Robson card. The latter is very well standardized, and both have been widely used and tested in clinical populations. In a group of 66 normally sighted subjects and 64 patients ranging from 16 to 83 years of age, the Pelli-Robson chart had higher test-retest reliability (0.98 for normal subjects and 0.86 for patients) than either the Vistech charts or lab-based measurements (Rubin, 1988). The coefficient of repeatability (95 percent confidence interval) of Pelli-Robson contrast sensitivity scores is ±0.15 log units (Elliott, Hurst, & Weatherill, 1990). The Elliott et al. study suggests that a score of 1.65 log units for young subjects and 1.5 log units for older subjects corresponds to the lower limit for normal performance (based on the 95 percent confidence limits). For older adults, a contrast sensitivity score less than about 1.3 is associated with an increased risk of driving accidents relative to those with normal contrast sensitivity (Owsley & McGwin, 1999).
Recommendations
Currently SSA does not test contrast sensitivity to determine a person’s visual disability. It is possible for individuals to have relatively good visual acuity and/or fields and have reduced contrast sensitivity that is disabling. Therefore, we recommend adding contrast sensitivity as an additional basis for disability determination for individuals with visual acuity between a lower limit of 20/50 and an upper limit of 20/200. It is not necessary to measure contrast sensitivity in individuals who meet the SSA medical listings criteria for visual acuity or visual fields, but it is recommended for those with visual acuity between 20/50 and 20/200 and other indications or self-report of serious visual impairment. This idea is illustrated in Figure 2-5.
The test used should be simple to administer, require no sophisticated equipment, and be well-standardized, reliable, valid, sensitive to visual loss, and relatively insensitive to changes in focus, viewing distance, and illumination. It should provide a single score that can be compared with normative data. One currently available test, the Pelli-Robson, is known to meet these criteria, and other tests now available or to be developed in the future may do so as well. We recommend that if the Pelli Robson test is used, testing should be done at 160 cd/m2, the same luminance used for acuity testing. A score of less than 1.05 on the Pelli-Robson test would be a reasonably conservative boundary for disability.
Issues Needing Further Study
The relationships of contrast sensitivity to performance on tests of mobility, social participation, and tool use/manipulation are areas clearly in need of further study. Glare is an exacerbating factor for seeing low-contrast objects. There is no standard, widely available test for glare; however, it should be noted that people who perform poorly under low-contrast conditions usually perform even more poorly under glare, due to light scatter. Thus glare testing is an area requiring further study.
It is also well known that low light levels are a serious exacerbating factor in one’s ability to see low-contrast objects, particularly for older and visually impaired persons. New tests such as the SKILL Card (Haegerstrom-Portnoy et al., 1997) exist for this condition, but they have not been extensively used with working-age visually impaired subjects and therefore require further study. Another area requiring further study is the contrast sensitivity testing of young children (see Chapter 4).
COLOR VISION
Description
The color of a surface is determined by how it reflects light and is generally a stable property of the surface. This makes color a reliable cue for distinguishing and identifying objects, and normal color vision permits us to distinguish a rich range of naturally occurring surfaces. Inability to distinguish colors may make objects less distinguishable. Impaired capacity to distinguish colors can be congenital or acquired.
Congenital deficits occur in approximately 8 percent of Northern European men, perhaps less in other ethnic groups, and less than 0.5 percent of women (Hsia & Graham, 1965). Mild deficit results when an individual has the usual three kinds of cone photoreceptors but with one or more of these being most sensitive in an unusual part of the visible spectrum. This happens in about 5 percent of men. Severe deficit results from the absence of one of the normal three classes of cone photoreceptor; about 2 percent of men lack either the long-wavelength (L) or middle-wavelength (M) cone receptor. This leads to very poor color discrimination in the red-green part of the spectrum. Loss of the short-wavelength (S) cone, which affects men and women equally and leads to a severe impairment of discrimination in the blue region of the spectrum, is very rare. Even in cases of severe color vision deficiency, color confusion occurs for only some portions of the color spectrum, and many colors can still be distinguished.
Acquired color vision deficiencies are produced by pathological changes to the visual system. Yellowing of the lens and cataract development produce blue (tritan) deficiencies. Most diseases of the retina tend to produce color vision deficits in the short-wavelength (blue) part of the spectrum, whereas optic nerve diseases tend to produce red-green deficits. In some cases, nonspecific color deficits are found for certain eye diseases, in which color discrimination is poor throughout the color spectrum. Pokorny et al. (1979) and Adams et al. (1998) provide comprehensive discussions of congenital and acquired color vision deficiencies.
A variety of tests is available for evaluating color discrimination. Rapid screening procedures include pseudoisochromatic plate tests, such as the Ishihara, Dvorine, H-R-R, and others (which are able to distinguish between persons with normal color vision and those with any type of color vision deficiency) and the Farnsworth panel D-15 test (which distinguishes individuals with severe color vision deficiencies from those with normal color vision or only mild color vision losses). These tests are good for screening and classifying color vision abnormalities, but they do not accurately quantify the extent of color vision deficiency. More sophisticated test procedures, such as the Farnsworth-Munsell 100 Hues test and the Nagel and Pickford-Nicholson anomaloscopes, are able to classify both the type of color vision deficiency and its severity. All of these test procedures, with the exception of the anomaloscope, are available in most eye clinics, as well as for testing general populations. Specialized color vision testing can be undertaken in the laboratory, but this requires the construction of custom equipment that is not generally available to others. A description of the commonly used color vision tests is available in Pokorny et al. (1979).
Evaluation
Why the Measure Might Be Useful
Impairments of color vision make objects harder to distinguish and identify. In some instances, a difference in color may be the
predominant or only cue available to distinguish objects. People who suffer from one form of congenital color vision loss (protanopia) may also find it hard to see lights of long wavelength. Well-established tests are available to characterize impaired color vision, and some of these are relatively easily administered.
Potential Value as a Practical Measure
Most of the work on predicting real-world performance from color vision tests has been concerned with tasks involving transportation (vehicle driving, aviation, etc.) and tasks of specific occupations in which color discrimination is crucial (appraisers of precious stones, quality control specialists for paint and dye samples, etc.). For example, Lakowski and Oliver (1978) found that color-defective individuals could not identify different grades of fuel oil, which are instilled with a dye to provide unique tints for different fuel oil grades. Similarly, they also reported that normal color vision was essential for the accurate grading of diamonds. An excellent comprehensive review of the importance of color vision for the transportation industry is found in Vingrys and Cole (1988). Pokorny et al. (1979) also provide a review of the implications of color vision deficiencies for various occupations. North (1993) includes an appendix table by Voke that lists occupations in which defective color vision may impair performance. This list represents a very small subset of the total number of occupations in the general workforce.
Quantifying Performance
Several varieties of color vision tests are used for clinical and occupational purposes. An excellent review of these can be found in Pokorny et al. (1979). The simplest tests are those used for screening purposes; various forms of pseudoisochromatic plate tests (Ishihara, Dvorine, H-R-R, etc.) have been developed and validated for rapid screening. They consist of a series of plates containing dots of various sizes and colors. Persons with normal (trichromatic) color vision are
able to distinguish from its background an object or number defined by similarly colored dots, whereas a person with impaired color vision will not be able to distinguish the object from the background. In some versions, a larger series of plates is used to determine the type (red/green/blue) and severity (mild/moderate/severe) of color deficiency. In general, properly designed and administered pseudoisochromatic plates have been found to do an excellent job of distinguishing persons with normal color vision from those with color deficiencies. However, their ability to accurately determine the type and severity of color vision deficit is quite limited.
The Farnsworth panel D-15 is another screening test. It consists of a series of 15 color chips that are to be arranged in order of their color similarity. The D-15 test clearly distinguishes persons with severe color vision deficiencies and those with normal color vision or only mild to moderate deficit. It also is able to accurately determine the type of color vision deficiency (red/green/blue). The D-15 was designed as an occupational color vision test procedure because it is a good predictor of whether a person will have difficulties for those occupations in which color discrimination is routinely performed as part of the job. The Farnsworth-Munsell 100 Hues test is an extended form of the D-15 test. It consists of 85 color chips in 4 boxes that must be arranged in order of their color similarity. Arrangement errors are recorded on a polar coordinate chart that has the color spectrum arranged in a circle. The spectral locations at which color arrangement errors occur define the type of color deficiency, and the magnitude of the arrangement errors measures the severity of the deficit. For occupational purposes, it provides the best quantitative information about the severity of color vision deficiency, and it has often been used as the color vision measure to correlate with task performance.
Finally, anomaloscopes provide an accurate and precise measurement of color vision deficiency, although they are not commonly used for occupational purposes.
Relation to Other Measures
Unlike visual function measures that demonstrate some degree of correlation with each other, such as visual acuity and contrast sensitivity, which to some extent tap the same underlying capabilities, color vision is a relatively independent dimension of vision.
Quality of Information Available
A number of investigations have examined the relationship between color vision deficits and task performance in controlled studies, many of which are reviewed in Vingrys and Cole (1988) and Pokorny et al. (1979).
Recommendations
To the extent that normal color discrimination is a critical factor for specific jobs, color deficient individuals may be unable to perform them or may require a longer time to perform them. Only a limited number of tasks (e.g., quality control of paint and dye samples, grading of precious gems, identification of plant and animal species) depend significantly on normal color vision. In some others (e.g., law enforcement, firefighting, civil aviation, the military) color-blind people may have restrictions placed on them or be excluded from certain positions. Color vision has a minor or negligible role for most jobs, and we recommend that it not be considered further with regard to visual disability determination.
BINOCULAR FUNCTION
Description
Binocular vision (seeing with two eyes) is normal and confers three benefits: it makes hard-to-see objects easier to detect, it enlarges the total field of view, and it improves a person’s capacity to distinguish small differences in depth.
Visual performance is normally slightly but reliably better when people undertake tasks using two eyes rather than one. In studies of binocular summation tasks that have examined this explicitly, the contrast required to detect a grating pattern binocularly is lower by a factor of about 1.4 than the contrast required to detect it monocularly (Campbell & Green, 1965; Legge, 1984a; Pardhan, 1993). The benefits of binocular vision are smaller when the task is to discriminate small differences in the contrast of clearly visible patterns (Legge, 1984b). Binocular acuity is slightly better than monocular acuity (Blake & Fox, 1973; Cagenello et al., 1993; Rubin et al., 2000). For this reason, we recommend that, for the purposes of determining disability, acuity be tested binocularly. A similar small advantage of binocular vision has been shown in more complex perceptual-motor tasks, such as finding objects in camouflage, controlling posture, pointing, and reading (Jones & Lee, 1981; Sheedy et al., 1986).
The normal field of view is comprised of regions contributed by the two eyes. Because the eyes face forward, these regions overlap substantially, although not completely. With the eyes looking ahead, each eye’s field extends about 95° toward the temple and about 55° toward the nose in Caucasians (Fischer & Wagenaar, 1954). The overlapping region is known as the binocular visual field and normally spans horizontally the central 110°. To either side of it is a region, about 40° wide at its maximum, seen by one or the other eye alone. Thus using two eyes extends the width of the field that can be seen at any one time. When one eye has an impaired visual field in the region of binocular overlap, the other eye may provide normal vision.
The most distinctive benefit of using two eyes derives from the fact that, because they are horizontally separated, they do not have exactly the same view of the visual world. The small differences between the images in the two eyes are systematically related to the arrangement of objects in depth, providing information from which the visual system is able to distinguish small differences in the distances at which objects lie. This capability, known as stereopsis, is most beneficial for making fine depth judgments, especially when objects are nearby (i.e., within arm’s reach) (Howard & Rogers, 1995).
For all three of these capabilities, enhanced acuity, field of view, and stereopsis, the brain must properly combine information from the two eyes. If vision in the two eyes differs substantially, the brain may be unable to combine the information into a unified view (binocular single vision) or may be unable to use the differences between the images to distinguish small differences in depth. Binocular vision can also be disturbed even though each eye alone is functioning normally. Abnormalities in the brain, or improperly coordinated movements of the eyes, or misalignment of them, can disrupt normal binocular vision. When the brain is unable to combine information from the two eyes, a person may experience double vision (diplopia) or binocular rivalry, a sometimes haphazard switching of vision from one eye to the other.
Binocular function is unusually sensitive to visual experience during development. If early in life the eyes are misaligned (strabismus) or the images in the two eyes differ substantially (as might occur when one is well focused but the other not), one eye tends to become dominant, stereopsis often does not develop, and the weaker eye may never become capable of seeing well, even after appropriate refraction. About 3 percent of the population lacks stereopsis (Richards, 1970), and 2-5 percent of the population has some visual abnormality that leaves them with uncorrectable poor vision in one eye but not the other (Cross, 1985; Ehrlich et al., 1983; Flom & Neumaier, 1966; Thompson et al., 1991). Richards (1970) reports that up to 30 percent of the adult population has some deficiency of stereopsis.
Evaluation
Why the Measure Might Be Useful
Failure to combine information from the two eyes can lead to a reduced ability to see small differences in depth. Moreover, under some circumstances, the vision of the two eyes might conflict, making vision poorer than if one eye alone was used.
Potential Value as a Practical Measure
Binocular vision has very little effect on reading (Jones & Lee, 1981; Legge, Pelli, et al., 1985; Sheedy et al., 1986), but at least one study (Ivers et al., 2000) showed that impaired stereopsis is associated with hip fractures among older people. Ivers et al. reported a significant trend toward elevated odds ratios for hip fracture as stereopsis impairment increased, compared with those whose stereopsis was in the normal range.
Loss of vision in one eye does not appear to affect the performance of drivers in test maneuvers (McKnight et al., 1991; Wood & Troutbeck, 1992; Wood et al., 1993), but it has been found in some studies to elevate crash risk (Laberge-Nadeau et al., 1996; Maag et al., 1997; Rogers, Ratz, & Janke, 1987). Depth perception, for which stereopsis is helpful under some circumstances, is frequently considered moderately important, although seldom essential, in using tools. In the workplace overall, depth perception is rated as being of moderate or high importance in only 15 percent of jobs, as discussed in the occupational analysis section of Chapter 3 (see Table 3-1 for PAQ ratings).
Quantifying Performance
Several simple tests exist to characterize stereopsis. This is usually done through the measurement of stereoacuity, the smallest discernible separation in depth that a person can detect, based on the geometry of the images in the two eyes. These include the Randot stereo test, the TNO stereo test, the Lang stereo test, and others. The Randot stereo
test uses images produced on polarization film. The viewer wears a pair of polarizing glasses so that one image is viewed by one eye and the other image is viewed by the other eye. A slight difference in the position of the image between the two eyes creates a small retinal disparity, which serves as the stereopsis cue and causes the image to “stand out” from the page. The test contains some images that do not stand out, and the subject’s task is to select the ones that do stand out. The test has a graded series of images to determine the minimal retinal disparity at which stereoacuity is present. The TNO stereo test is similar, except that it uses a series of red and green dots to create images, and the subject views the test through a pair of glasses with a red filter over one eye and a green filter over the other. The Lang stereo test is also similar, except that it uses a Fresnel lens above the test plate to produce slightly different images to the two eyes, while avoiding the need for special glasses.
Recommendations
Our recommendations here concern impairments of binocular function and are distinct from our recommendations in other sections that other visual functions should be tested binocularly. Abnormalities of binocular function are relatively common, and for most people intrude little on everyday life. Few, if any, tasks depend on the visual capability that requires the two eyes to work in partnership (stereopsis), and people with only monocular vision are seldom circumscribed in what they can do. When disrupted binocular function interferes with binocular single vision (via diplopia or rivalry) this can generally be circumvented by patching one eye. We therefore recommend that abnormalities of binocular function not be considered in the determination of disability.
VISUAL SEARCH
Visual search is a crucial ability in everyday life and consists of localizing or finding an object of interest among other objects or
“distractors.” We live in a visually cluttered world with a myriad of objects and ongoing events. Thus, visual search is essential to the performance of tasks typical of the workplace, such as reading, mobility, social participation, and the manipulation of objects. Although visual search is not a basic visual sensory function, it is a function of the visual system and can therefore be considered a visual function as defined in Chapter 1.
Previous research on normally sighted persons has demonstrated that it is possible to predict visual search performance in laboratory tasks on the basis of visual sensory factors, such as visual acuity, contrast sensitivity, and visual field sensitivity (Carrasco & Chang, 1995; Carrasco & Frieder, 1997; Geisler & Chou, 1995; Verghese & Nakayama, 1994). However, there is little research on whether visual sensory factors correctly predict the visual search abilities of people with low vision, either in laboratory tasks or, more relevant to our discussion here, tasks performed in the real world. Given that visual search is a fundamental part of seeing, future research should consider whether a visual search screening test would be useful in disability determination screening batteries in order to validly capture task performance problems experienced by visually impaired persons, or whether visual sensory tests (e.g., visual acuity, visual field) are alone sufficient.
Evaluation
Driving is a task for which it is already clear that visual sensory tests by themselves are inadequate for predicting performance problems (see Chapter 3). As mentioned earlier, a visual search task called the useful field of view test (Ball et al., 1990) has been used extensively to study driving. It consists of a radial localization task performed under divided attention conditions, wherein targets are presented briefly (<250 msec) among distracting stimuli. Those persons who have slow visual processing speed and divided and selective attention problems perform poorly on the test. Research has shown that poor scores on the useful field of view test are better predictors of crash involvement and driving performance problems among older drivers than are visual sensory tests like visual acuity (Ball et al., 1993; Cushman, 1996;
Duchek et al., 1998; Hunt et al., 1993; Owsley, Ball, et al., 1998; Rizzo et al., 1997; Rubin et al., 1999; Wood et al., 1993). Research using other tests of visual search further confirms the critical nature of visual search in safe driving (Barrett et al., 1977; Duchek et al., 1998; Goode et al., 1998; Kahneman et al., 1973; Mihal & Barrett, 1976). Test features that appear to be most critical in identifying crash-prone drivers are those that embody divided attention components and place high demands on rapid visual processing (Owsley, Ball, et al., 1998). The critical nature of visual search abilities in driving is not surprising since controlling a vehicle is a complex visual task not only involving the sensory registration of events, but also requiring the simultaneous monitoring of central and peripheral vision and the filtering out of irrelevant stimuli, all performed under time-limited conditions. Research has demonstrated that the vast majority of crash-involved older drivers have excellent visual sensory ability (Ball et al., 1993; Owsley, Ball, et al., 1998), so crash-prone drivers would remain largely undetected by a visual sensory screening test.
There is some evidence that visual search ability is also independently related to the performance of other types of tasks, such as locating objects of interest in the environment, reading text on objects, and using tools (Owsley, McGwin, et al., 2001; Owsley, Sloane, et al., 2001). However, research in this area is relatively sparse.
Recommendations
Given the available evidence to date, the committee recommends at this time that a test of visual search ability not be used in the visual disability determination process. Since visual search is a fundamental aspect of seeing, further work is needed to clarify the relationship between visual search impairments and the performance of work-related tasks. However, it is already clear that deficits in visual search ability are associated with an increased risk for motor vehicle collision and impaired driving performance. Thus, for jobs involving driving, a useful addition to a driving fitness evaluation would be a test of visual search ability. The most effective design of this test needs to be determined by further research.
GLARE AND LIGHT/DARK ADAPTATION
Measurement of visual function in the clinic or the laboratory is usually performed under ideal conditions of daytime (“photopic”) lighting and the absence of extraneous light sources. Recommended lighting for acuity testing is on the order of 160 cd/m2 (National Research Council, 1994). In the real world, however, levels encountered in bright sunlight can be up to 400 times greater than this, and in night driving typically 500 times dimmer (Pitts, 1993). Strong extraneous light sources such as oncoming headlights or a bright sky often surround a visual target, creating glare problems. Also, a person may have to adapt to rapidly changing lighting conditions (as when coming into a dimly lit room from bright sunlight).
Conditions of glare and low lighting arise in the course of many workplace tasks (e.g., driving, construction work, computer use). They are only a minor annoyance to most people, who can quickly compensate, but they can be disabling for those with certain eye conditions. Conversely, individuals with rod monochromacy or cone dystrophies may experience substantially impaired vision at high light intensities (Elliott et al., 1989; National Research Council, 1994; Zadnik et al., 2000).
The committee examined the impacts of low and changing light levels and glare on vision impairment to determine whether special tests should be included for identification and assessment of individuals unduly affected by these conditions.
Vision at Low Light Levels
The normal visual system can adapt to a wide range of light levels, although acuity and contrast sensitivity are reduced as light level is reduced. However, ability to function in low light is dramatically disrupted in aging (Adams et al., 1988; Sloane et al., 1988), macular disease (Jacobson et al., 1986; Owsley, Jackson, et al., 2001), congenital stationary night blindness, retinitis pigmentosa (Brown et al., 1984),
diabetes (Wolfe & Sadun, 1991), optic neuritis (Schneck et al., 1993), fundus albi punctatis, and glaucoma (Glovinsky et al., 1992). Large changes in visual acuity can occur with relatively modest changes in illumination in many people with impaired vision (Lie, 1977; Lovie-Kitchin & Bowman, 1985; Sloan, 1969).
In studies of vision in macular degeneration, Bullimore and colleagues have found that changes in illumination could produce substantial decrements in reading acuity, maximum reading speed, and reading eye movement patterns, as well as in face recognition ability (Bullimore et al., 1991). The measured size of scotomas and field constrictions can often be dependent on luminance levels in macular degeneration and retinitis pigmentosa (Bullimore & Bailey, 1995).
Studies demonstrate that mobility problems in visually impaired people are exacerbated under low illumination (Kuyk et al., 1996; Turano et al., 1999), particularly in those with age-related maculopathy (Brown et al., 1986). Surveys indicate that the most frequent complaint of older people about their vision is the inability to read fine print under poor lighting conditions (Brabyn et al., 1995; Kosnik et al., 1988). Inability to see well in low light conditions would clearly be disabling for many employees, such as movie theater personnel and darkroom technicians, who perform their work in a dimly lit environment.
Low luminance testing in the clinic is not often performed due to problems in producing calibrated light levels. An alternative method, the SKILL card (Haegerstrom-Portnoy et al., 1997) uses a dark gray acuity card with black letters to measure acuity under low-contrast, low-luminance conditions without turning down the lights. Although norms and an increasing body of data on this test exist, to date it is used mainly in research settings. Light sensitivity under scotopic (low luminance) conditions has also been tested using specially modified automated perimeters in studies designed to improve understanding of retinal degenerations (e.g., Jacobson et al., 1986). However, these devices are not commercially available.
Adaptation to Rapidly Changing Light Conditions
Retinal diseases can cause a slowing in the rate of adaptation to low or medium light after exposure to bright light, a process referred to as dark adaptation, which depends mainly on the dynamics of the retina’s response to light (Barlow, 1972). The magnitude and duration of the temporary vision impairment depends on such test conditions as the intensity and duration of the initial “bleaching” light and the wavelength of the test target. The return to normal visual function is a gradual process; it may take many seconds but sometimes extends to over 30 minutes.
Difficulty adapting to poor or changing light levels is widely acknowledged to have a serious impact on the mobility of many visually impaired persons (Geruschat & Smith, 1997; Szlyk et al., 1990). Even if vision returns to normal after a period of adaptation, an extended period of adaptation may expose such an individual to such dangers as tripping and falling when going from bright sun to indoors or being temporarily blinded by oncoming headlights. Problems with visual adaptation in older adults have been linked to involvement in motor vehicle collisions and falls that result in injuries (Massie et al., 1995; McMurdo & Gaskell, 1991; Mortimer & Fell, 1989). Severe deficits in adaptation could have disabling effects on any task performed under changing lighting conditions.
Although dark adaptometry is an accepted clinical tool, especially in the diagnosis of retinal disorders, there are few instruments designed to carry out this assessment. The Goldmann-Weekers Adaptometer is the most common instrument; however, its test protocol is vulnerable to examiner and subject biases, similar to those discussed in the context of Goldmann visual fields. Custom-made dark adaptometers have been used to measure dark adaptation in research (Jackson et al., 1998; Jacobson et al., 1986; Steinmetz et al., 1993) but these devices are not commercially available.
Recovery of vision after a drastic change in luminance is often referred to as “glare recovery.” In the macular photostress test (Glaser et al., 1977), the subject is presented with a bright light (e.g., an ordinary penlight held an inch from the eye) for a short time (e.g., 10 seconds).
The time taken for vision to recover to some predetermined endpoint is measured. There is no agreed-on standardization of glare recovery testing in terms of such factors as glare intensity, time, and type and size of target used.
Glare Disability
Glare disability is a reduction of the contrast of the retinal image caused by extraneous bright light sources present in the visual field. People with conditions that increase light scatter within the eye experience exaggerated impairments under conditions of glare (Rubin et al., 1993). Glare resulting from light scatter may be due to optical irregularities in the ocular media, such as cataract, corneal opacification, and keratoconus, or it might have origins external to the eye, such as scatter from airborne particles or irregularities on otherwise transparent surfaces, such as windows and spectacle lenses. The intensity of the scattered light depends on the area and luminance of the glare source and its angular proximity to the line of sight. Disability glare can also be of retinal origin, when strong stimulation of one large region of the retina affects the sensitivity of other regions of the retina.
The impact of veiling glare depends on the contrast and acuity demands of the visual task. For example, when looking at a person silhouetted against a window or a very bright sky, contrast reduction can make it difficult to discern features in the face. In driving, detecting pedestrians, the edge of the roadway, or reading signs against a bright sky, sun, or headlights is likely to be difficult if ability to see in the presence of glare is impaired. Disability glare has been associated with the occurrence of motor vehicle collisions (Brabyn et al., 1994), although not all studies agree (Owsley, Jackson, et al., 2001), and with self-reported difficulty in performing night driving and near vision tasks (Rubin et al., 2001). People with retinitis pigmentosa have particularly severe problems with glare in mobility tasks (Turano et al., 1998). Severe glare disability is likely to affect aspects of mobility, such as reading street signs against a bright sky, detecting low-contrast curbs, or seeing objects on white pavement when walking into the sun, although research has not comprehensively addressed these issues.
In tests of disability glare, the subject is usually required to perform a visual task (visual acuity, low-contrast visual acuity, and contrast sensitivity tests) in the presence of the glare source. Some tests use small, bright glare sources at a fixed location relative to the test task, while others use a more extensive glare source surrounding the task. The intensity of the scattered light depends on the angle from the glare source. Glare testers have been commercially available since the predecessors of the Miller Nadler test (1990), which used a slide projector viewer that provided the surround glare for Landolt ring targets of various contrasts. The Brightness Acuity Tester (BAT) (Holladay et al., 1987) is a hemispherical bowl with a controlled glare source held close to the eye, with a 12 mm aperture that allows the viewing of test targets. The clinician chooses the specific test task (e.g., ETDRS chart, Pelli-Robson chart, Bailey-Lovie low-contrast visual acuity chart) (Elliott & Bullimore, 1993). The Berkeley Glare Test (Bailey & Bullimore, 1991) uses low-contrast acuity charts against a large, bright background and can assess disability glare under binocular viewing conditions. Van den Berg and colleagues (de Waard et al., 1992) describe a test to measure intraocular light scatter in which an annulus (or ring) of flickering light is the glare source, and a small spot inside the annulus, flickering in counterphase to the glare source, is the test target whose modulation is adjusted until it appears that there is no flicker.
Today, none of these glare tests is widely used apart from research applications, except for the BAT, which is somewhat popular clinically in cataract surgery evaluation. Other disability glare tests that have not been widely discussed or studied in the literature are the InnoMed true vision analyzer (TVA), the VisTech VCT 8000, the EyeCon 5 (Neumann et al., 1988), the Humphrey Automatic Refractor Model 570 (Beckman et al., 1992), and the Opthimus glare test (Martin, 1999). Each is different in its visual stimulus parameters, and no standardized method of measurement has been widely agreed on. A phenomenon known as “glare discomfort” has also been described in the clinical literature, referring to a subjective feeling of unpleasantness from exposure to bright light. Its functional impact is poorly understood, and there are no standard and accepted tests.
Recommendations
There is a growing body of evidence that low luminance and conditions of glare can significantly accentuate visual disability and even elicit impaired function in a person whose vision may be normal under ideal conditions. Because of the relative lack of standardization in test procedures, the committee recommends not adopting low luminance, glare, dark adaptation, or glare recovery tests as part of the disability determination procedure at this time, but further research should be encouraged on the impact of these exacerbating factors on task performance and on methods for documenting these problems. Meanwhile, the inclusion of contrast sensitivity testing should at least partly address the need for testing under less than ideal viewing conditions that are closer to those encountered in the real world.
VISUAL EFFICIENCY
SSA recognizes that impaired central acuity and impaired visual fields, neither of which alone would meet the disability standard in the listings, can in combination result in an overall impairment that is disabling. Impairment is characterized by a composite measure of the visual efficiency of the better eye, derived from component measures of central visual efficiency (from measured acuity) and visual field efficiency (from measured fields).
We examined the computation of central visual efficiency and visual field efficiency, considering how well each index characterizes impairments and how an appropriate composite index of performance might best be calculated in the context of our recommended methods for measuring visual function. This composite measure would also need to accommodate measurements of contrast sensitivity, when these had been made as part of the disability assessment.
In addition to examining the measure of efficiency, we examined the criterion for disability, to establish whether the relationships between performance on tests of visual function and performance on everyday tasks suggest any natural criterion. Given our recommended changes
to the procedures for measuring visual acuity and fields and changes to the ways in which performance is scored, we also considered what level of efficiency would correspond to the current criterion for disability.
Central Visual Efficiency
Following an investigation of how glasses that diffused light to varying degrees impaired visual acuity and considering perceptual scaling issues generally, Snell and Sterling (1925) proposed that as the minimum angle of resolution increased linearly (from a standard 1 minute of arc) a person’s visual efficiency (E) decreased geometrically:
E = k(1-MAR)
where k is a constant of proportionality. Snell and Sterling found experimentally that to reduce normal (20/20) acuity to “qualitative vision” (no useful resolving power) required six times the diffusing strength needed to reduce 20/20 acuity to 20/40, so they proposed that 20/40 vision represented a one-sixth (16.7 percent) loss of visual efficiency. An acuity of 20/200 would represent an 83 percent loss of efficiency; Snell and Sterling defined 20/200 to represent 80 percent loss of efficiency and thereby established k to be 0.83625. The resulting visual efficiency scale is that still used by SSA. The current standard offers alternative efficiency scales for use when one or both eyes lack a lens (aphakia). Table 1-3 illustrates these scales.
The available evidence on the real-world consequences of different degrees of impaired acuity (Rubin et al., 2001; West et al., in press) endorses the principle embodied in the current standard that (as with many visual functions) there is a logarithmic relationship between visual acuity and overall performance. Thus, for example, an acuity of 20/80 is as much worse than 20/40 as an acuity of 20/200 is worse than 20/100. Nevertheless, the efficiency scale has weaknesses. First, it provides little room to distinguish individuals whose impairments range from severe low vision (represented by the current 20/200 criterion for statutory blindness) through complete blindness. The difference between 20/200 and 20/277 represents a decrease in
efficiency of 0.1 (0.2 − 0.1), and the difference between 20/277 and no useful vision represents an efficiency change of the same magnitude. Second, the prescribed adjustment for aphakia is no longer appropriate. An allowance for aphakia might have been reasonable when a person whose lens had been removed in cataract surgery had to wear powerful glasses, which magnified the image and created a significant reduction in visual field. Nowadays, correction is almost always provided by a surgically implanted intraocular lens, usually supplemented by spectacles and less often by contact lenses. Acuity should always be tested with the best tolerable correction.
The procedure and measure we have recommended for characterizing acuity gives rise to a logarithmic measure (logMAR, see the acuity section) that provides a simple proportional indicator of visual performance. This measure directly expresses visual impairment (as performance declines, the score rises): a score of 1.0 corresponds to the current acuity criterion of 20/200. Because of this, the committee recommends that the logMAR score be used directly in the computation of an overall measure of visual performance for disability determination, as described in the section on combining measures, below. There is no need to compute any index of central visual efficiency.
Visual Field Efficiency
The SSA standard computes visual field efficiency as the sum of the field extents measured along eight directions from the line of sight (up, down, left, right, and the intermediate diagonals), divided by 500, the sum considered to represent the normal field. This ratio is expressed as a percentage. The standard for severe impairment is a visual field efficiency of 20 percent or less. The standard for statutory blindness is a visual field extent of 10° or less from the fixation point, or a greatest diameter of 20° or less.
The prescribed method of estimating visual field efficiency ignores scotomas within the outer bound of the measured visual field, and it provides no means to estimate the visual field available by using both
eyes. A better measure of efficiency would make use of the richer and more reliable characterization of the visual field now possible with modern instruments, and it would be based on the effective binocular visual field rather than the monocular field of the better eye.
Our recommended method for expressing impairment is the mean deviation (MD, see the visual fields section). It characterizes the aggregate loss of sensitivity within the central 60° of visual field on a logarithmic scale. The MD score captures performance over a range that extends to 30 dB mean loss of sensitivity, which is essentially complete blindness. Like the proposed measure of acuity, the MD score is a logarithmic measure that provides a direct proportional indicator of impairment that can be used in disability determination. The current disability criterion (a field restricted to the central 20° or less) would correspond to an MD of −22 dB, assuming an intact field in the central 20° and complete loss beyond. Given the directness and simplicity of MD as measure of performance, it can be used without modification in the computation of an overall measure of visual impairment for disability determination, as described in the section on combining measures below. There is no need to compute an index of percentage remaining visual field efficiency.
Contrast Sensitivity
We have recommended that contrast sensitivity be measured when a claimant has a best corrected acuity of 20/50 (logMAR 0.4) or worse but does not meet the SSA listing criterion of 20/200 or worse. Our recommended instrument for measuring contrast sensitivity is scored in a way that provides a direct expression of log contrast sensitivity (based on the Weber contrast ratio, Lmax − Lmin/Lmax). Taking normal log contrast sensitivity as 2.0, an expression of impairment that is commensurate with those obtained from the recommended measurements of visual acuity and visual fields would be 2 − CS. As discussed earlier, there is considerable evidence that a threefold loss of sensitivity (impairment score 1.5) represents consequentially impaired vision, and a tenfold loss (impairment score 1.0) represents severely impaired vision.
Combining Measures
SSA regulations prescribe a method for computing the overall loss of visual function that might result from impairments of both acuity and visual fields. Overall efficiency (visual efficiency) is calculated as
Visual efficiency = central visual efficiency × visual field efficiency.
This measure gives equal weight to the component scores. The standard for severe impairment is an overall efficiency in the better eye of 20 percent or less. Two important issues arise: Is the equal weighting of component scores reasonable, and do the impairments act multiplicatively?
Because impairments of acuity and fields limit performance in quite different ways and generally in different domains of activity, their relative importance is likely to be task-dependent. One approach to understanding their relative importance would be to establish what levels of impairment on each have equivalent effects on higher-level performance indicators, such as quality of life measures. At present there is insufficient evidence on what might be the appropriate weightings of acuity and fields in any composite measure to be used for disability determination. We recommend that research be done on this question. In the meantime, we recommend that SSA continue its current practice of giving equal weight to the measures of visual acuity and visual fields.
Recommendations
Beyond establishing commensurate scales for characterizing acuity, visual fields, and contrast sensitivity, we need to be able to compute an aggregate indicator of impairment. We know too little about the interactions between multiple visual impairments to recommend a change in SSA’s current practice of deriving an overall measure by multiplicative combination of component measures. Some recent evidence (Rubin et al., 2001) suggests that impairments act independently in affecting overall visual performance. We
recommend that further research be undertaken to examine directly how different kinds of impairments interact in determining overall visual performance.
In the meantime, the committee recommends that, with the modification noted below, SSA continue its current practice of computing an overall measure of performance as the product of the component measures. This principle implies that different tests measure independent aspects of visual function, which cannot be completely true. For example, a central scotoma will be reflected in both an acuity score and a visual field score, but its weight in the visual field score will be slight. The problem is consequential for acuity scores and contrast sensitivity scores, which are generally well correlated. For this reason, we recommend that when contrast sensitivity has been measured (which would be done only when a loss is suspected beyond that captured by an acuity score), the contrast sensitivity score should supplant the acuity score in the calculation.
Because our recommended measures of acuity, visual fields, and contrast sensitivity are already logarithmic measures of impairment, we need only add the scores to compute an overall measure in order to achieve a combined multiplicative score. Recognizing that we must give equal weight to visual fields and to visual acuity (or contrast sensitivity), but that we use either a measure of acuity or a measure of contrast sensitivity, we recommend that the overall measure of impairment should be computed as:
aggregate impairment = logMAR + |MD|/22
when the scores to be combined are visual acuity and visual field and
aggregate impairment = (2 − CS) + |MD|/22
when the scores to be combined are contrast sensitivity and visual field. The current standard for disability would be met when the aggregate impairment equals or exceeds 1.0.
Disability Criteria
The acuity standard for statutory blindness (central acuity of 20/200 or worse) appears to have resulted from an examination (Snell, 1925) of the fitness for work of individuals with varying degrees of visual impairment. Snell found that the “threshold for incapacity” lay between 20/200 and 20/400. There is little evidence that this criterion reflects current employment rates of people with visual impairments or that it provides a reliable characterization of their visual capabilities in the workplace.
The studies we have reviewed and also clinical consensus (American Medical Association, 1993, 2001) suggest that the current acuity standard and the current visual field standard represent severely impaired vision. Nevertheless, the evidence also shows that overall visual performance varies continuously, and roughly linearly, with the measures of visual acuity, visual fields, and contrast sensitivity that we have recommended. Evidence about visual function therefore provides no guidance on where it might be appropriate to place a criterion for eligibility for disability benefits. While recognizing that a criterion is required, we make no recommendation about where it should be placed.
A decision about where to place the criterion involves many policy factors, including considerations of overall cost. At present, it is not possible to estimate the cost increases or savings that would result from changing the disability criteria now in place, for we do not know how the measures of acuity, fields, and contrast sensitivity are distributed among the population of working age. We therefore recommend that research be undertaken to establish the distributions of our recommended measures of acuity, fields, and contrast sensitivity in the working-age population.
Should SSA implement our recommendations for testing and scoring acuity, fields, and contrast sensitivity and at the same time retain a disability standard equivalent to the current one, we make these observations:
-
From measurement of visual acuity, a logMAR score of 1.0 or greater meets the current standard.
-
From measurement of visual fields, an MD score of −22db or worse meets the current standard.
-
It is not necessary to recommend a criterion for contrast sensitivity alone, because such a score will be used only in combination with a visual field score when visual acuity is 20/50 or worse.
-
An aggregate impairment score of 1.0 or more corresponds to the current standard of 20 percent visual efficiency.
Children
An aggregate impairment score may be calculated for children who are old enough to be tested using the instruments designed for adults.
RECOMMENDATIONS FOR TESTS OF VISUAL FUNCTIONS
The committee’s recommendations for the testing of visual functions for determination of disability focus on strengthening the testing of visual acuity and visual fields and adding one additional test, of contrast sensitivity, under certain circumstances. Another important recommendation is to consider establishing formal methods to ensure the quality of test administration and to evaluate new tests as they are proposed for use. In addition, the committee recommends that SSA support specific research efforts that will provide a firm scientific basis for future decisions about disability determination for people with visual impairments.
Acuity Testing
Our recommendations concerning assessment of visual acuity are similar to those of the Committee on Vision in its 1980 and 1994 reports (National Research Council, 1980, 1994). We therefore recommend that visual acuity charts should contain the same number of optotypes in each row; the space between optotypes in a row should be at least as wide as the optotypes in that row; and the size of the optotypes should decrease in 0.1 log unit steps from row to row. Chart luminance should be at least 80 cd/m2, with 160 cd/m2 optimal, free from glare, with a level of contrast between optotypes and background that is above 80 percent. The person being tested should be encouraged to read as many optotypes on the chart as possible and to guess at an optotype if he or she is unsure. Acuity results should be scored on an optotype-by-optotype basis, since this scoring procedure produces lower test-retest variability than does row-by-row scoring.
For disability determination, visual acuity should be tested under binocular conditions, since this provides the most representative measure of an individual’s everyday vision. However, if monocular acuity is tested rather than binocular acuity, the acuity of the better eye should be used for disability determination. Testing should be performed with the subject wearing the best tolerable refractive correction.
Given the history and legislation behind the current SSA standard of “20/200 or worse distance acuity” as the principal criterion for visual disability, the committee recommends continuation of the 20/200 cutoff criterion. Since we recommend a visual acuity chart design that would include optotypes at the 20/160 level, applying the “20/200 or worse” criterion literally to scores obtained with such a chart would set the effective criterion to “worse than 20/160 distance acuity.” The scoring of the charts currently used in disability determination sets the effective criterion at “worse than 20/100.” The recommended charts have a 20/100 line that would allow SSA to maintain the criterion at the current effective acuity level, but SSA must make the decision on whether this should be done.
Visual Field Testing
The committee recommends that the current SSA standard should be revised so that disability determinations are based on the results of automated static projection perimetry rather than Goldmann (kinetic, nonautomated) visual fields.
We propose the following criteria for any perimeter to be used by SSA for disability determination:
-
The automated static perimeter should be capable of performing threshold testing using a white size III Goldmann target and a 31.5 apostilb (10 cd/m2) white background.
-
The perimeter should be capable of measuring sensitivity for the central 30° radius of the visual field with equal numbers of target locations in each quadrant of the field, and target locations no more than 6° apart.
-
The perimeter should be a projection perimeter or should produce measures that are equal to those obtained on a projection perimeter.
-
The perimeter should have an internal normative database for automatically comparing an individual’s performance with that of the general population.
-
The perimeter should have a statistical analysis package that is able to calculate visual field indices, particularly mean deviation or mean defect (MD), which is the average deviation of visual field sensitivity in comparison to normal values for the central 30° radius of the visual field.
-
The perimeter should demonstrate high sensitivity (ability to correctly detect visual field loss) and specificity (ability to correctly identify normal visual fields).
-
The perimeter should demonstrate good test-retest reliability.
-
The perimeter should have undergone clinical validation studies by three or more independent laboratories with results published in peer-reviewed ophthalmic journals.
At present, the Humphrey Field Analyzer and the Octopus perimeters are known to meet these criteria.
For qualified devices, we recommend that a threshold procedure should be employed for visual field determinations (for example, Full Threshold, Fastpac, SITA, and SITA Fast are all suitable alternatives for the Humphrey; Threshold, TOPS, and TOPS Plus are suitable alternatives for the Octopus).
Ideally, one would have a measure of the binocular visual field serve as the basis for disability determinations because the binocular visual field is what people use for daily activities. However, simple procedures for determining the binocular visual field empirically, or deriving it from monocular visual field results, are not currently available. Until such procedures can be implemented, we recommend that the visual field results for the better eye should be used for disability determinations.
To account for scotomas and normal visual field locations between major meridians, we recommend that an index of the overall visual field status, such as mean deviation or mean defect, should be used for disability determinations. MD provides the best overall indication of visual field status, taking into account both the spatial extent and the localized sensitivity variations that are present in the visual field. An MD of −22 dB approximately corresponds to a visual field extent of less than 10° radius (the current SSA standard) and would serve as a reasonable criterion for disability determination.
Contrast Sensitivity Testing
The committee recommends that contrast sensitivity be assessed as an additional basis for disability determination for claimants who do not meet the current medical listing criteria for disability, but who have acuity between 20/50 and 20/200 and show other evidence or self-
report of serious visual impairment. Contrast sensitivity testing of this subset of claimants can provide useful information not captured by high-contrast acuity testing.
A contrast sensitivity test should be simple to administer, requiring no sophisticated electronic or computer equipment, well-standardized, reliable, valid, sensitive to visual loss, and relatively insensitive to changes in focus, viewing distance, and illumination. It should provide a single score that is meaningful and can easily be compared with extensive normative data, and it should provide information about visual function not captured by other tests (such as high contrast acuity).
One available test, the Pelli-Robson, is known to meet these criteria for a satisfactory test, as may others now available or emerging in the future.
Testing of Other Visual Functions
The committee recommends not testing visual functions other than acuity, fields, and contrast sensitivity at this time. Our review of the evidence has not shown that testing of color vision is justified by the additional information it would provide. Testing of binocularity, visual search, and adaptation to glare and luminance change, although worthy of further study because of their potential importance to visual task performance, are not recommended with the tests now available. Well-documented severe impairments of visual functions other than acuity, fields, or contrast sensitivity could be taken into account as “adjustments” in the disability determination process.
Combining Scores to Derive a Measure of Impairment
We know too little about the interactions between multiple visual impairments to recommend a change in SSA’s current practice of deriving an overall measure by multiplicative combination of
component measures. We recommend that research be undertaken to examine directly how different kinds of impairments interact in determining overall visual performance, so that the appropriate rule may be developed for combining component measures.
In the meantime, the committee recommends that, with the modification noted below, SSA continue its current practice of computing an overall measure of performance as the product of the component measures. For reasons fully explained in the chapter, we recommend that when contrast sensitivity has been measured (which would be done only when a loss is suspected beyond that captured by an acuity score), the contrast sensitivity score should supplant the acuity score in the calculation.
Because our recommended measures of acuity, visual fields, and contrast sensitivity are already logarithmic measures of impairment, it is not necessary to calculate central visual efficiency and visual field efficiency. We need only add the scores to compute an overall measure. Recognizing that we must give equal weight to visual fields and to visual acuity (or contrast sensitivity), but that we use either a measure of acuity or a measure of contrast sensitivity, we recommend that the overall measure of impairment should be computed as:
aggregate impairment = logMAR + |MD|/22
when the scores to be combined are visual acuity and visual field and
aggregate impairment = (2 − CS) + |MD|/22
when the scores to be combined are contrast sensitivity and visual field. The current standard for disability would be met when this aggregate impairment equals or exceeds 1.0.
Assurance of Test Quality
The committee recommends that SSA should develop standards for the selection of tests to be used in disability determination and consider establishing a formal body of experts on vision testing to
implement these standards. This could take the form of a standing advisory board or a panel of consultants with both clinical and scientific expertise; it would review proposed new tests and changes to tests now used, approving those that meet the standards.
The committee also recommends that SSA consider developing standards for test administration, in consultation with the ophthalmological and optometric communities, exploring ways to ensure that such standards are met by professionals testing SSA claimants, while respecting the value of practitioners’ clinical judgment. This could greatly improve the reliability of testing. Implementation possibilities range from initiating an accreditation or certification system for providers and their test facilities to establishing dedicated test centers that would operate under SSA supervision.
These quality assurance recommendations apply to tests of visual task performance (discussed in Chapter 3) as well as to tests of basic visual functions.
Research Recommendations
Research is needed relating the outcome of visual assessment using such tools as visual acuity charts to an individual’s ability to function in the workplace and in society. The results of such studies would allow future evaluation of the adequacy of the traditional cutoff of 20/200.
There is currently very little information available on the relationship between the status of the peripheral visual field and the performance of daily activities, occupational demands, and task performance. This area merits further research to support the validity of using visual field measurements as predictors of functional capabilities. Another important area is the development of techniques for providing valid and reliable measures of binocular visual field sensitivity.
The relationships of contrast sensitivity to performance on tests of mobility, social participation, and tool use/manipulation are areas
clearly in need of further study, as is the contrast sensitivity testing of young children (see Chapter 4).
Glare and vision in poor and changing lighting are exacerbating factors for seeing low-contrast objects. There is no standard, widely available test for glare. Thus research is needed on glare testing and on the impact of exacerbating factors, including glare, on task performance, and methods for documenting these problems. New tests are available to test low luminance, low-contrast acuity, but they have not been extensively used among working-age visually impaired people and therefore require further study, which would also be useful for tests of binocularity and of visual search and related functions.