CHAPTER 3
PATHWAYS TO A CHILD’S DEATH
. . . I ran downstairs . . . out into the pouring rain. . . . “For God’s sake, where is the ambulance?” . . . [At the hospital,] Dr. Stillman came back looking devastated, and utterly drained. . . . He said that Alexander had died of SIDS. . . . The whole thing was sick. I would know if Alexander was dead. Wasn’t I his mother?
Esmeralda Williamson-Noble, parent, no date
My twenty-year-old brother died 8 months ago from cancer. When he became ill, our whole family changed, and my parents didn’t have time to think of anything else. . . . It still seems as if Michael’s death is all my mother thinks about.
High school junior (Paulson, 2001)
Since birth [our son’s] medical needs have increased, and his health has deteriorated. . . . Our goal has been to try to provide him with the best quality of life he could have. . . . We live every day not knowing when will be our son’s last. . . . [For emergencies] we carry around a sheaf of papers—about 12 pages—that detail all of our wishes as we know them to this point, because we don’t know what every situation will bring.
Tina Heyl-Martineau, parent, 2001
Children who die follow many different pathways to death. Their families accompany them and then follow their own pathways of grief beyond the child’s death, even to the end of their own lives. Understanding the similarities and differences in pathways to a child’s death and in the experi-
ences of their families is a helpful foundation for considering the range of palliative, end-of-life, and bereavement services needed to assist children and families. In addition, it is important to keep in mind that for life-threatening conditions that are not invariably fatal, children who eventually die and children who survive often cannot be predictably distinguished at the time of diagnosis, during initial treatment, or sometimes even after initial treatments have failed. This unpredictability increases the challenges and the importance of understanding how to integrate aspects of palliative care from the time of diagnosis.
The first section of this chapter discusses prototypical trajectories of dying that depict in graphic form the different ways that death may come to children. The second section presents illustrative stories or vignettes that attempt to represent—in ways that epidemiologic data and charts cannot— the human dimensions of death in childhood. These stories, although they inevitably and greatly simplify real life, suggest how the varied circumstances that surround the deaths of children may affect the child, the family, and the health professionals who care for them.
The third section discusses prototypical patterns of care that illustrate traditional and newer perspectives on the relationship between curative or life-prolonging care and palliative and end-of-life care. The newer perspective, stressed in this report, encourages the integration of certain aspects of palliative care from the time a child is diagnosed with a fatal or potentially fatal medical condition. The section also discusses how the emphasis of care may vary depending on the medical circumstances and may, given similar medical “facts,” be affected by differences in family values and circumstances as well as differences in the resources available to them.
Documentation of the focus and adequacy of pediatric palliative and end-of-life care is very limited. The final section of the chapter reviews this small literature.
TRAJECTORIES OF DYING
To help illuminate differences in the paths that people follow to death, Glaser and Straus introduced the concept of a trajectory of dying. They proposed that “the dying trajectory of each patient has at least two outstanding [and variable] properties . . . duration and shape” (Glaser and Straus, 1965, p. 6). The shape of the trajectory depends on time and on the person’s level of functioning or health status. Figure 3.1 presents four simplified trajectories of death in childhood that depict time along the horizontal axis and health status along the vertical axis. These trajectories underscore the reality that no single model of care and support will apply to all dying children and their families. The trajectories do not, however, necessarily map in a straightforward fashion to specific models of palliative care.
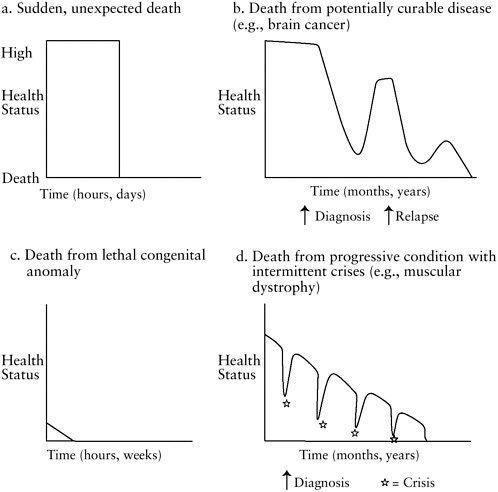
FIGURE 3.1 Prototypical trajectories of child death.
SOURCE: Adapted from IOM, 1997.
The most abrupt trajectory, Figure 3.1a, represents the unexpected, sudden death—for example, that of a child killed instantly in a car crash or discovered dead in his crib at home. Such events account for more than a third of childhood deaths. Although children who have died can themselves experience no medical or supportive care, first-response emergency medical personnel commonly follow protocols that require efforts at resuscitation. When a child is involved, only rarely is death actually declared “in the field” rather than in the hospital. If the declaration is based on criteria for brain death, protocols require a period of assessments and observation that may take from 12 to 48 hours or longer (see Chapter 1).
Figure 3.1b depicts the experience of children who respond positively to initial, sometimes difficult and possibly life-threatening treatment for a potentially fatal condition, for example, certain brain cancers, but who eventually die of their disease or its further treatment. At diagnosis and during the early stages of initial treatment, these children may not be uniformly distinguished either from children who will not respond or from children who will eventually be cured. (Overall, 70 percent of children with cancer are cured.) Even when an initial positive response to treatment is followed by a return of the disease, determining prognosis is not automatic. From a palliative care perspective, at least three tasks follow diagnosis— each adapted to the situation of the individual child and family. One task is to provide the family—and the child, as appropriate—with accurate and timely information on diagnosis, prognosis, and treatment options and to help them make informed decisions and prepare for a future that includes the hope of cure. A second task is to provide comfort to the child (in particular, by preventing or relieving symptoms of the disease or its treatment) and support to the family. If initial or subsequent treatment fails the child, families will need information about the benefits and burdens of remaining treatment options and about prognosis. When further curative or life-prolonging interventions fail, the additional task for the care team is to help the child and family through the dying phase of the child’s illness and then support the family at death and after.
Figure 3.1c depicts the brief trajectory of an infant born with problems incompatible with extended life. As described in Chapter 2, extreme prematurity, severe congenital anomalies, and other life-threatening conditions affecting infants account for a significant fraction of child deaths. With modern prenatal care, some families know in advance that their child will not survive, and some know that they are at significant risk of premature delivery. Extremely premature infants and infants with severe congenital anomalies have produced high-profile disagreements about appropriate care, but care to comfort the infant and the family is always appropriate. As illustrated later in this chapter and discussed further in Chapters 4 and 5, actual support for families may be very limited.
Figure 3.1d abstracts the experience of children who suffer from a fatal progressive illness—for example, muscular dystrophy—that is characterized by periods of slowly deteriorating health status that are interrupted by potentially fatal medical crises, which the child repeatedly survives until one crisis ends in death. In some situations, a child’s past favorable response to treatment may leave parents and even clinicians unprepared for and surprised by a subsequent failure of treatment. In other situations, clinicians and parents recognize that the child has reached the final stage of his or her illness and focus on physical and emotional comfort, accepting
that resuscitation and other life-sustaining interventions will be more burdensome than beneficial.
Various other trajectories for progressive conditions and for some chronic conditions could be mapped. For example, children with severe asthma and appropriate treatment may have mostly normal functioning without disease progression, but a sudden life-ending crisis may occur and be almost as unexpected as a death from injury.
The illustrative vignettes presented next describe experiences of a child’s death that approximate the four trajectories presented above. In addition to the two dimensions of health status and time, they depict other dimensions of a child’s death including the individuality of the child and family and the competence and compassion of health care professionals.
ILLUSTRATIVE STORIES OF CHILDREN AND THEIR FAMILIES
During the course of its work, the committee heard many compelling stories from parents whose child had died. In the details of their experiences and in their expectations, the families differed, but they made clear that parents long remember how health care professionals helped or hurt them.
Most parents reported a mix of good and bad experiences. Some told of exemplary care. Others reported insensitive and even cruel behavior from physicians, nurses, or others involved in their child’s care. Some found that insurers or health plans were supportive; some had no insurance; others had continuing and exhausting difficulties trying to get care approved—and then suffered with their child when coverage of hospice or other supportive services was denied. Often faced with uncertainty about their child’s prognosis and treatment options, some parents anguished over decisions about how far to pursue experimental treatments or whether and when mechanical ventilation or other life-support interventions should be withheld or withdrawn.
Beyond his or her medical condition, a child’s experience of dying will depend on many factors, including the family’s circumstances, values, and responses to the illness and the kind of medical and other services that are available to meet the child’s physical, psychological, spiritual, and other needs. The brief stories presented below suggest how the complex interplay of these factors may affect the level of distress experienced by children and their families.
None of the following stories depicts a specific child and family exactly, although each is based on real experiences. Some are fairly typical of childhood deaths, whereas others represent more unusual or particularly challenging situations. The stories are clearly simplified, but they highlight differences in the needs of children and families and differences in the
extent to which the care provided met these needs. Most depict deficits in some aspects of the care provided the child or family.
“Ana Rivera”
When death comes to children, it often is sudden and unexpected (Figure 3.1a). In this case, 3-month-old Ana’s father finds her lifeless body in her crib one morning. Her parents’ grief is complicated and intensified when they realize that a police officer’s questions are probing the possibility of homicide. This story also illustrates the special difficulties facing immigrant parents whose language abilities and resources are limited.
Jorge and Maria Rivera had emigrated from El Salvador two years prior to Ana’s birth, leaving their three children behind with Maria’s mother and promising to send money to support the family. Maria’s first husband and two older brothers had been killed during the war, but her cousin had escaped to the United States and urged Maria and her second husband Jorge to follow him. Jorge got a job at a fast-food restaurant and Maria cleaned houses, and they scrimped on everything so that they could send a little money back to their family in El Salvador. They felt isolated but were overjoyed when they learned that Maria was pregnant. A neighbor brought Maria to a clinic that provided prenatal care to poor women. The Riveras were proud to give this new baby—Ana—such a good start.
After an uneventful pregnancy, delivery, and first few months, Jorge found 3-month-old Ana cold, blue, and motionless in her crib one morning. The Riveras rushed Ana to the public hospital where she was immediately taken into a treatment room. In a short while, the Riveras were led into a small sitting room in the emergency department where a physician informed them, through a janitor who spoke both English and Spanish, that Ana had died. The janitor did not understand all of the words the physician said but assured the Riveras that everything had been done to help Ana. After the physician left, a police officer came into the room and began to ask Jorge questions about how he had found Ana, what he was doing prior to finding her, what her health had been like prior to that morning, and whether Jorge had ever hurt either Ana or Maria. Jorge remembered that he had been angry the night before and yelled at Ana when she wouldn’t stop crying, but he was afraid to tell the police officer this information. No charges were brought against Jorge and Maria, but they lived in fear that they would be arrested and sent back to El Salvador. Both had intense feelings of loss for Ana and for their three other children who were still in El Salvador. A hospital social worker told the Riveras about bereavement support groups, but none was nearby and none had groups for Spanish speakers. The social worker really helped in one way. She helped make sure that the Riveras qualified for free care under a community program for the
medically indigent, so at least they did not face medical bills that they could not possibly pay.
“Jimmy Marshall”
In this case, which involves another leading cause of child mortality, a car–bicycle collision set off a frantic effort to save an injured child’s life. To the parents, the emergency department and intensive care unit are frightening and strange. Despite the help of several social workers, there is much they do not understand and that is never explained. They are unwittingly misled by one clinician who is satisfied with the technical success of a procedure but not focused on what is still a very grim, likely fatal situation. One result is a father’s lifelong regret that he was not with his wife and son when the boy died.
While riding his bicycle with a friend, Jimmy Marshall, an 11-year-old boy, was struck by a car. Emergency personnel found him semiconscious with obvious head injuries and rushed him to the nearest trauma center, which treated but did not specialize in pediatric trauma. In the emergency department (ED), Jimmy was taken to a large, open resuscitation bay while the trauma team, including nurses, surgeons, neurosurgeons, emergency physicians, and pediatricians, cared for him. His condition was clearly very serious.
Friends rushed Jimmy’s mother to the hospital. In a small, windowless room, the social worker provided some brief information and comforting words. Then, the ED “attending” came in to explain that Jimmy had suffered a serious brain injury and they were doing everything they could to help him. Later, a “pediatric resident” said that Jimmy was being taken to x-ray for special scans of his brain and that the team was very worried. Fighting tears and hysteria, Mrs. Marshall asked, “But he is going to be all right isn’t he?” The resident appeared to almost shrug as she said, “I can’t tell you that.” The rest was a blur.
Just after Jimmy was taken to the intensive care unit, his father arrived. The attending physician gave a brief, grim update. Both Marshalls started to weep. The family would have welcomed the support of a hospital chaplain, but no one thought to see if someone was available. As they waited, the conversation around them sounded ominous, but the terminology was mysterious, and both parents were too bewildered or intimidated to ask many questions. Told that neurosurgeons needed to put a hole in their son’s skull in order to monitor dangerous swelling, Mr. Marshall protested that this might injure Jimmy’s brain. A doctor replied, “You have more important things to worry about right now.”
After the procedure, the neurosurgeon approached, smiling and commenting that things went “great.” For the first time, Jimmy’s parents felt
relieved and somewhat confident. The father, afraid that he would lose his job, then left to return to his construction work. However, when the doctor who appeared to be in charge returned, he told Mrs. Marshall that they needed to talk and that she should try to reach her husband.
In the interim, the doctor told Jimmy’s mother that there had been increasing brain injury and that the task was to prevent the brain from swelling and “crushing itself.” Her son might die. This seemed impossible given that only a few minutes earlier someone else had seemed so cheerfully pleased.
Suddenly, a nurse rushed in to say that the doctor was needed. Jimmy’s heart had stopped and CPR (cardiopulmonary resuscitation) had been initiated. The doctors knew that the likelihood of resuscitating Jimmy was negligible but were obligated to try. The doctors subsequently had to tell the Marshalls that they had done everything, but Jimmy had died. Later, Mr. Marshall agonized that he hadn’t been told enough to realize that he should stay with his wife and boy, and he sometimes felt angry at how the neurosurgeon misled them. He and his wife got a piece of paper with information about bereavement support, but it was laid aside and then lost in all the turmoil. There was no further contact from those who were with Jimmy when he died. At least, they had qualified for “free” hospital care.
“Melissa Devane”
As children mature, their intellectual and emotional understanding of serious illness and the prospect of death evolves. This story describes the complex relationships between a severely ill adolescent and her parents and physician and the different concerns she has as she moves from diagnosis and treatment, to recurrences and further treatment, to death (Figure 3.1b). The adolescent is in conflict with her parents and physician about undergoing burdensome experimental treatment but eventually persuades them to respect her wishes.
When Melissa was 13 years old, she was an excellent softball player who hoped some day to play on the Olympic softball team. Late one summer, her knee began to hurt severely and kept hurting. When Melissa’s primary care physician thought an x-ray suggested a tumor, she referred her to Dr. Garcia, a pediatric oncologist. After a biopsy, Dr. Garcia diagnosed osteogenic sarcoma, an invasive bone cancer. As Dr. Garcia recommended, Melissa had several weeks of chemotherapy followed by surgical removal of the tumor and then several months more of chemotherapy plus physical therapy. Although the hospitalizations for chemotherapy and episodes of fever were no fun, what bothered Melissa most was losing the ability to play her sport ever again. Also, her hair fell out just as school was starting. The social worker on her oncology team helped Melissa to get a wig and, as
part of the team’s attention to school reentry issues, explained Melissa’s situation to classmates and teachers.
The family celebrated the end of Melissa’s chemotherapy with a big party. Melissa was sad that only half of her former teammates made it to the party. She commented to the social worker that she had learned through the experience “who her real friends were.” The yearbook club and her younger sister’s softball games became new focal points.
At a follow-up appointment 13 months after the end of chemotherapy, Dr. Garcia found a spot on the CT (computed tomography) scan of Melissa’s right lung. He recommended surgical removal of the suspected tumor to confirm the diagnosis. The surgery was uneventful, and Melissa was pleased there would be no chemotherapy. Six months later, however, scans showed tumors in both lungs. This time, intensive chemotherapy followed surgery. Family and friends and an occasional tutor supported Melissa through the months of hospitalization.
Now almost 17 years old and hoping to plan for college, Melissa did her best to look to the future and regain her strength. By the winter of her senior year, she was back in school full time, working on the yearbook, and seeing a new boyfriend. Then, routine scans showed another recurrence in the lung, but this tumor was too big to remove surgically. Dr. Garcia proposed experimental chemotherapy that would require long hospitalization. Melissa reacted by saying, “I’d rather die than have more chemotherapy” and “you’re unreal—I’m going to die anyway.” This surprised everyone. Melissa had been “such a perfect patient.” Melissa’s dad felt the issue was settled. (“It’s our decision. She’s a child.”) Her mother felt that “since it is her body and her life,” Melissa should be part of the decision-making and that Dr. Garcia ought to be clearer about what could be expected. The subsequent discussions were emotional but less anger filled as they went along and Dr. Garcia acknowledged that it was unlikely that the experimental treatment would help meaningfully prolong her life and would be arduous.
Melissa explained that she wanted to live what time she had left by doing what she wanted to do: attend the prom, finish the yearbook, and coach her sister in softball a bit more. Melissa was able to do those things. She and her parents and Dr. Garcia ultimately agreed on palliative chemotherapy that was given by mouth. The Devanes’ health plan quickly approved referral to a local hospice. Because Melissa was likely to die within six months and because the family had opted for palliative care only, there was no issue of appealing the plan’s limits on hospice coverage. The hospice care team gave the family the help it needed to keep Melissa at home with minimal pain. Dr. Garcia continued to keep in regular touch with Melissa and her parents. Melissa died peacefully at home in July in her mother’s
arms, having lived longer than Dr. Garcia predicted and having seen her sister have a championship season with Melissa’s support and coaching.
“Sean Riley”
This story illustrates the increasingly common situation in which a fatal congenital anomaly is diagnosed prenatally and the families await a birth that likely will be followed by death within hours or days (Figure 3.1c). Although many mothers and fathers opt for abortion when faced with such a tragic diagnosis, others—for religious, philosophical, or emotional reasons—choose to continue the pregnancy. A few innovative programs have recently been developed to provide extensive clinical information and preparation and emotional, spiritual, and practical support (e.g., help with coordinating services) to these families following diagnosis and through and after the infant’s death (see, e.g., Sumner, 2001). Most parents, however, have limited access to such information, preparation, comfort, and assistance from health care professionals. They may be able to rely on families and friends, and some discover parent-to-parent support groups or other resources.
Catherine and Kevin Riley were delighted to learn that they were expecting a new baby to join their 4-year-old daughter, Caitlin. In Catherine’s sixteenth week of pregnancy, she had an ultrasound examination. From the reactions of the technicians, she knew immediately that something was wrong, but no one was willing to tell her anything except that she should contact her obstetrician.
Told initially that the ultrasound results would be reviewed at Catherine’s next regularly scheduled visit in four weeks, Kevin called the obstetrician’s office to explain the extreme stress they were under and their need to know the results. The obstetrician explained that the fetus had anencephaly (failure of the brain to develop), that he had little training in managing such pregnancies, and that they should consider termination of the pregnancy “because the baby would not live.” The Rileys were unwilling to consider termination and requested a referral to a new obstetrician who specialized in high-risk pregnancies. The second obstetrician said that there was nothing to be done for mother or fetus and that if they did not want to terminate the pregnancy, he would see Catherine again when she was ready to deliver (in about five months).
Without access to regular obstetrical visits for further information and preparation, the Rileys drifted in fear, uncertainty, and grief during the following weeks and months. They sought information from the Internet where they found stories from other families about anencephalic infants who had survived “for years” but learned little to answer their questions
about why this problem had happened and how they should prepare for what was to come.
Catherine went into labor at 38 weeks’ gestation. The Rileys found delivery room nurses who were unaware of her fetus’s diagnosis and an unfamiliar obstetrician who was covering for the obstetrician she had last seen. As Catherine’s contractions increased in intensity, the nursing staff on the delivery floor became concerned about the fetus’s heart rate. The obstetrician suggested delivery by cesarean section. Kevin questioned this recommendation, but the obstetrician and nursing staff both insisted it was needed and that if they refused both parents would have to sign a form stating their refusal. Confused by these demands given the diagnosis and prognosis, Kevin and Catherine requested a second opinion. Before the opinion could be obtained, the fetus’s heart rate dropped to dangerously low levels, and the baby was delivered by cesarean section with Catherine under general anesthesia. The obstetrician and anesthesiologist confirmed the diagnosis of anencephaly. Kevin was not allowed in the delivery room because Catherine was under general anesthesia. Neither saw their son, Sean, during his brief moments of life.
After delivery and her baby’s death, Catherine was placed on a floor in the hospital to recover where there were no babies or other postpartum women. She noticed that nursing staff avoided her, and she felt very isolated. Her obstetrician saw her once, inquired about her pain control, and said she could go home “when she was feeling better.” She was discharged three days later, after receiving an envelope with a lock of Sean’s hair, a handprint, and a Xeroxed paper about “grief.” Many of the Riley’s friends avoided any contact when news about Sean’s birth and death became known. Her employer refused postpartum leave or paid bereavement leave because “she had no baby.”
Kevin never spoke about Sean again, although he noticed that he became extremely sad unexpectedly for years afterward. Daughter Caitlin had stayed with relatives during the delivery. No one told her much about Sean’s birth and death. She began to think that her parents were angry with her. Expectations of both Kevin and Catherine for Caitlin increased significantly, which added more pressure for an already vulnerable child. Five years after Sean’s death, the Rileys remain a sad and troubled, though loving, family.
“Johnny Gabrielle”
Although caring for a child with a serious chronic condition is always demanding, the burden is significantly increased when the child is developmentally delayed and cannot communicate his or her needs directly. Most children and families can be helped to lead fairly normal lives for extended
periods, but they may face major financial, bureaucratic, and other problems in actually obtaining such assistance. When death approaches, systems focused on chronic medical conditions may not be prepared to help families face the end stage of illness. In some cases, a child’s medical problems severely test the ability of very experienced clinicians and others to identify effective therapies and relieve the suffering of the child and the family.
Shortly after Johnny Gabrielle was born, the doctors caring for him noted that his head was smaller than expected and that he had certain unusual facial features. A number of specialists examined him and eventually they diagnosed a rare genetic disorder. A pediatric neurologist informed Peter and Laura Gabrielle that Johnny would most likely be developmentally delayed and ultimately mentally retarded and probably would have a shortened life span. Although she tried to prepare the family for what lay ahead, the neurologist could only talk in general terms because so few children with his condition had been treated and their history documented. The neurologist became Johnny’s primary physician, assuring the Gabrielles that she would “be there” for them whatever the future brought, would bring other specialists in as needed, and would do everything she could to keep Johnny comfortable and free of pain and other distress.
As predicted, Johnny’s development was far behind that of his older brother. He never talked or achieved normal milestones, but his parents learned to recognize his cues. His sunny disposition brightened the lives of all who encountered him. Johnny’s main problem was that he never slept through the night but instead awakened repeatedly. Johnny’s physicians tried many drugs to induce sleep, but none were reliably successful. The Gabrielles developed a system of shared responsibility for his care at night but always felt tired. They felt fortunate to qualify for assistance under their state’s generous and well-managed programs for children with special health care needs. As time went by, they became acquainted with families from other states who had terrible financial problems and even had to sell their homes to pay medical bills.
At about age 5, Johnny became increasingly irritable and was diagnosed with gastroesophageal reflux. Medication and position did not seem to help nor did surgery. Physicians eventually placed a tube directly into Johnny’s stomach so he could be fed. Shortly thereafter, Johnny’s personality began to change. He became inconsolable at times and would scream out and tighten his body throughout the day. His sleeping became even more disrupted, lasting only an hour at a time before he screamed again. He was hospitalized frequently, but physicians could find no specific explanation for his problems. Morphine slightly reduced his crying and irritability, which led his care providers to believe that he might be experiencing pain at times. Even with pain medications, he was still inconsolable much of the time. His physicians, who now included a specialist in pediatric pain, man-
aged a fine line between relief and excessive sedation and were alert to other potential complications of his treatments. Although the Gabrielles had written documents that listed Johnny’s medications and described their preferences for the use of certain life support technologies should Johnny’s condition suddenly deteriorate, it was hard for either Johnny’s parents or physicians to know what to expect in the near term (days, weeks, or months).
Up every night for weeks, the Gabrielles’ relationship with their older son began to deteriorate. None of their large, supportive family could provide real respite because Johnny was so medically fragile and required so much nursing care. Even during hospitalizations, the Gabrielles were always present and responding to nurses’ questions about strategies that seemed to help Johnny. The same was true for visiting nurses at home; even when they didn’t ask for help, Laura could still hear Johnny crying in his room. Recognizing the Gabrielles’ exhaustion, the health care team looked for formal respite care for Johnny, but they never identified an appropriate setting. He was not sick enough for an acute care setting but was too medically complex for the available medical foster care homes.
All involved felt helpless and frustrated. This pattern persisted for approximately four months. One night, when Johnny didn’t awaken at the expected one to two hours after going to sleep, his mother went to check. Johnny was dead. The cause was later determined to be aspiration. At the wake, while being consoled by a huge cadre of friends and family, the Gabrielles told themselves that at least now, “Johnny was finally sleeping” and no longer in pain. They appreciated the presence of some of Johnny’s main doctors and nurses. They did not seek outside bereavement support but felt ready to face the future.
Summary
Consistent with the experiences of real children and families, these vignettes include examples of good care as well as examples of care that falls considerably short of meeting child and family needs. Bereavement care is particularly limited. Measured against the criteria for a “good or decent” death as defined in Chapter 1, some of the care described is insensitive and some leads to avoidable physical or emotional suffering for the child, the family, or both. No vignette describes a real “horror” story of care that violates norms of decency, although such cases do exist.
The vignettes also suggest that some of the dilemmas facing parents, children, and clinicians may not have a clear or successful answer—even with everyone trying his or her best. This is a particular dilemma when a child suffers from a rare condition that has few cases documented in the
literature and no condition-specific research to guide physician’s decisions about curative, life-prolonging, or palliative care.
No small collection of stories can adequately portray the struggles that families with a seriously ill child often experience in trying to coordinate care that may involve multiple sites (e.g., specialized referral center, outpatient clinic, community hospital, home), a large and frequently changing array of health care professionals (e.g., generalist and specialist pediatricians, nurses, social workers, child-life specialists, case managers), and differing criteria for insurance coverage of different services (e.g., inpatient care, home health services, hospice, psychosocial services, respite care, outpatient drugs and equipment).
PATHWAYS OF CARE
The vignettes suggest that just as pathways to death will vary for children, the pathways of care—that is, the mix of curative or life-prolonging care and palliative care—will vary depending on the child’s condition and other factors, including family circumstances and values. Even for some conditions that are invariably fatal, the timing of death may vary considerably. For different children, the same diagnosis and initial prognosis can be followed by quite different pathways that end in death for some and, depending on the condition, extended survival or cure for others.
The unpredictability of many life-threatening medical problems can make it difficult for families to decide when further efforts to save their child will only prolong the child’s suffering and dying. Faced with similar facts and uncertainties, families will differ in their responses, and their values and personalities will influence their decisions about the goals of care for their child. Some families will emphasize prolonging life until death removes the choice whereas others will, as death approaches, choose care that is focused entirely on their child’s comfort and quality of life. Both may be doing their best for their child, and both may live in peace—or with regrets—about their choices.
The emphasis of care may also reflect the resources—or lack of resources—available to the child and family. For example, as discussed in Chapter 6, few children’s hospitals have specialized palliative care services or consulting teams, although all hospitals should be able to provide the fundamentals of such care, for example, effective assessment and management of pain. They may not, however, have clinicians who are trained to explain the child’s situation fully and compassionately, to make clear the likelihood of harms as well as benefits from different treatments, and to assure the family that it will be supported in its choices.
Traditional views of patient management have often referred to a “switch” from curative (or life-prolonging) care to palliative care. This
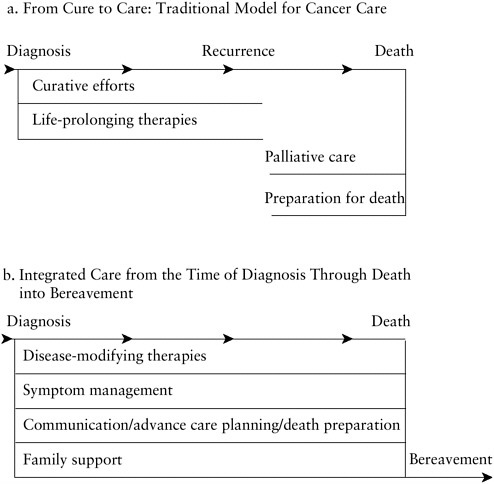
FIGURE 3.2 Sequential versus integrated models of care for advanced illness.
SOURCE: Adapted from IOM, 1997.
phrasing suggests that the two are separate worlds—even mutually exclusive—with an abrupt transition in patient care from one to the other. Figure 3.2a presents this perspective.
An alternative perspective proposes that providing some elements of palliative care closer to the time of diagnosis than happens traditionally may benefit patients and families and may coexist with and support active curative or life-prolonging treatment. For example, not only may meticulous efforts to prevent or relieve the pain and other distress that accompany certain treatments improve a child’s comfort and quality of life, it may improve the child’s ability to tolerate or cooperate with treatment. Just as hospice providers work with patients and families to reevaluate the goals of
cure as the end stage of an illness approaches, “upstream palliative care” involves the periodic discussion of prognosis and care options and, as appropriate, the reconsideration of the goals of care during the early stages of complex chronic illnesses, for example, during “routine” visits and check ups.
Figure 3.2b illustrates the concept of integrated care in which multiple objectives are pursued concurrently after the diagnosis of life-threatening condition. The emphasis and specific elements of care may vary depending on the situation. Thus, some aspects of advance care planning (e.g., discussion of preferences for cardiopulmonary resuscitation, weighing of hospital versus home care as death approaches) are less urgent when a child’s condition is possibly curable, treatments are not themselves life-threatening, and early crises such as cardiac arrest are uncommon. Likewise, if early symptoms are minimal, the emphasis may be on reassuring parents that the child’s care team will do everything possible to anticipate and prevent problems and to make their child comfortable if treatments or worsening of the condition brings pain or other symptoms.
Although this report emphasizes the model of integrated care following diagnosis, situations exist in which care may indeed switch abruptly from a near total emphasis on cure or life prolongation to a total commitment to palliation, preparation for death, and support for grieving family members. For example, with some seriously injured children, physicians may initially assume—pending further evaluation—that survival is possible and work intensively and virtually exclusively toward that goal. Test results or poor response to treatment may then demonstrate irreversible damage that will lead inevitably and fairly soon to death. At that point, the emphasis of care may shift quickly to relieving any distress that the patient might be experiencing and preparing the patient (if conscious) and family members for death. When this happens, the message is never that “there is nothing we can do” but that “we must refocus on efforts” on comfort and peace and making the most of the family’s remaining time together.
Similarly, for some children, the emphasis of care may always be palliative. For example, in the vignette earlier in this chapter, Sean Riley’s medical condition was incompatible with extended life, but the family could have been provided active emotional support before, during, and after the birth. Physicians and nurses could have planned and prepared to manage the delivery in accord with the family’s goal of having time with the baby after birth. Care would have been intensively palliative from the time of prenatal diagnosis, supporting the parents as parents before and after the baby’s death and reducing their sense of powerlessness.
In yet other circumstances, the emphasis or balance of care may fluctuate over time, for example, when a child has with a progressive, fatal condition such as muscular dystrophy or certain heart conditions. In the
Gabrielle vignette in Chapter 3, the parents and other caregivers spent an increasing amount of time trying to relieve Johnny’s distress. Periodically, however, Johnny was hospitalized—sometimes in attempt to relieve his apparent pain, sometimes in an intensive effort to save his life following an acute problem (e.g., an infection). The Gabrielles’ physicians attempted to extend Johnny’s life while doing their best to relieve his intractable distress; they explained their best understanding of Johnny’s diagnosis and prognosis but did not take away his parent’s hopes. To depict this as a modification of Figure 3.2b, the horizontal lines under the elements of care could increase and decrease in thickness to represent the varying emphasis on life-prolonging care or palliative care.
In sum, the ratio of palliative care compared to curative or life-prolonging care and the ratio of palliative care compared to true end-of-life care will vary for different medical conditions and at different points during the course of a fatal illness. Depending on a child’s diagnosis and stage of illness as well as available resources, some palliative or end-of-life care may be delivered by specialized inpatient or home hospice teams, some by palliative care teams, and some by the primary team (e.g., oncology, cardiology, neurology) caring for the child. All will need appropriate education and training, funding, and institutional structures and processes that support the timely, coordinated provision of the right mix of care for the child and family.
The next section of this chapter reviews evidence about the adequacy of palliative, end-of-life, and bereavement care provided to children and families. Additional studies are cited in the discussions in Chapter 4 and 5 of the elements of palliative, end-of-life, and bereavement care.
WHAT DO WE KNOW ABOUT THE FOCUS AND ADEQUACY OF CARE FOR CHILDREN WHO DIE?
I had to fight with the doctors to get him on morphine. They tried fentanyl patches and other things. They did not want to send him home on morphine. I screamed and cried and got them to understand that the short time he had left must be without pain, or at a minimum of pain. He had morphine in the hospital, but didn’t want it for home use. Finally, they agreed.1
Becky Wooten, parent, 2001
The pathway followed by a dying child and his or her family can be marked by competent, consistent, and compassionate care, by care that fails on these dimensions, or by care that falls somewhere in between these poles. In recent years, several studies and reports have attempted to document and understand more systemically the strengths and weaknesses of palliative, end-of-life care for adults (see, e.g., SUPPORT, 1995; IOM, 1997; Webb, 1997; Lynn et al., 2000; Meier et al., 2000; IOM, 2001a). They have described inadequate assessment, documentation, and management of pain and other symptoms, sometimes in combination with overtreatment, including unwanted or ineffective resuscitation and other life-support interventions. Referrals to specialists in palliative and end-of-life care have been late or altogether absent. Poor communication includes insensitive delivery of bad news, inattention to patient and family preferences, and failure to provide accurate, timely information needed by patients and families to guide decisions.
Efforts to remedy these shortfalls in palliative and end-of-life care and to increase public understanding and expectations are growing and becoming more sophisticated (see, e.g., Higginson, 1993; Doyle et al., 1998; Emanuel et al., 1999; Lynn et al., 2000; Ferrell and Coyle, 2001; AAP, 2000g).2 The goal—still to be achieved—is to create systems that people can trust to provide competent, consistent, and compassionate care to seriously ill and dying patients and that families can count on for support and solace as they experience a loved one’s grave illness or death.
What is the picture for children who die and their families? Research on palliative and end-of-life care for children and their surviving families is very sparse. Some of it focuses rather narrowly on decisions involving cardiopulmonary resuscitation, mechanical ventilation, and other life-sustaining technologies—with little investigation of the adequacy of physical, emotional, spiritual, and practical support (e.g., help in coordinating services from multiple different providers) for the children and their families. Such research as the committee did locate generally follows the pattern found for adults, reporting inadequate assessment, documentation, and management of pain and other symptoms; late consideration of the benefits of palliative or hospice care; and problems in communication.
|
2 |
Useful information and links to other resources are also available on a number of Web sites, for example, those of the Center to Advance Palliative Care, Mt. Sinai School of Medicine (http://www.capcmssm.org); Project on Death in America, Open Society Institute (http://www.soros.org/death); and Last Acts, a coalition initiated by the Robert Wood Johnson Foundation (http://www.lastacts.org). |
Assessment, Documentation, and Management of Pain and Other Distress
Pain management practices and problems have been more often discussed and better documented than problems in other aspects of pediatric palliative and end-of-life care. In the past, physicians often discounted pain in children. For example, a 1960s survey of postoperative pain in children argued that they “seldom need medication for relief of pain [and] . . . tolerate pain well” (Swafford and Allan, 1967, cited in McGrath, 1998, p. 1020). Neonates were thought to lack sufficient neurophysiologic and other development to suffer pain and thus not to need pain relief during surgical procedures such as circumcision.
Both behavioral and physiological research have repudiated these arguments and clarified the existence and seriousness of pain in children (see, e.g., McGrath, 1987; Bush and Harkins, 1991; Barr, 1994; Walco et al., 1994; APS, 1995; Duke, 1997; Schechter et al., 1997, 2002; Anand et al., 1999). Nonetheless, misunderstandings and ignorance have continued. As a 1998 editorial in the British Journal of Medicine stated, “Current practice still falls short of the ideal of safe and effective pain relief for all children” (Zacharias, 1998, p. 1552).
Groups including the World Health Organization (WHO) and the American Academy of Pediatrics (AAP) still find it necessary to issue policy statements that remind pediatricians of their obligations to recognize and prevent or relieve children’s pain and to keep abreast of research on the tools available to do so (see, e.g., WHO, 1998; AAP, 2000a, 2001a). A 1998 WHO statement on pediatric cancer pain reported that 70 percent of children with cancer suffered severe pain at some point and that such pain was often not recognized or, if recognized, not treated adequately. More recently, the AAP specifically stressed that systemic pain medications are essential to manage predictable pain associated with bone marrow aspiration and other procedures (AAP, 2001a). It likewise emphasized that reliance on sedatives or antianxiety agents alone will not only allow children to experience pain but leave them less able to communicate their distress. The AAP identified the following barriers to the appropriate recognition and treatment of pain in children including
-
myths that children, especially infants, do not feel pain the way adults do or that, if they do, there is no untoward consequence;
-
failures of physicians to assess and reassess for the presence of pain;
-
inadequate understanding of children’s subjective experience of pain;
-
insufficient knowledge of strategies for assessing, preventing, and relieving pain;
-
concerns that pain management in children is too time-consuming and difficult; and
-
disproportionate fears of adverse treatment effects such as respiratory depression and addiction.
Although most pain now can be relieved (in principle if not in practice), some pain is intractable without sedation (Swarm and Cousins, 1998). Some therapies produce side effects such as nausea, itching, confusion, or sleepiness that can cause considerable distress and require shifts in pharmcologic or other interventions (McGrath, 1998). Pain may also be necessary in pursuit of certain therapeutic benefits, for example, evaluating certain injuries or judging the success of orthopedic surgery during rehabilitation. In the latter case, Walco and colleagues (1994) suggest that clinicians should ask themselves whether a less hurtful approach is possible and whether the pain inflicted on the child is the least possible needed to achieve the benefit.
Research on the adequacy of pain assessment and management in children is scarcer than that for adults, but the findings raise concern. For example, although the majority of pediatric oncologists consider themselves competent in managing pain and other symptoms (Hilden et al., 2001a), a recent study at a leading pediatric cancer center and children’s hospital found that 89 percent of children dying of cancer were reported by parents in after-death interviews to have suffered substantially at the end of their lives (Wolfe et al., 2000a).3 The most common symptoms were fatigue, pain, and shortness of breath. Half of the children suffered from three or more symptoms. The most commonly treated symptoms were pain (76 percent of cases) and shortness of breath (65 percent). Treatment was, however, reported to be successful less than 27 percent of the time for pain and 16 percent of the time for shortness of breath. Fatigue was little treated, and the study authors suggested that physicians may be unaware that some apparently effective treatments are available for this common symptom of advanced illness (or its treatments). Children with cancer who died of treatment-related complications suffered more symptoms than children who died of progressive disease.
Most studies of end-of-life care for children focus on physical symptoms rather than emotional symptoms or quality of life. In their study, Wolfe and colleagues (2000a) reported that parents of children with cancer stated that, in the last month of life, their child had little or no fun (53
percent), was more than a little sad (61 percent), was not calm and peaceful most of the time (63 percent), and was often afraid (21 percent). Despite the suffering experienced by their children at the end of life, 70 percent of parents described their child’s death itself as “peaceful.”
In the United Kingdom, several studies of children cared for by Helen House (the first pediatric hospice) documented the serious symptoms experienced by many children. One study reported that more than a third of the children who died of neurodegenerative disorders suffered from pain, most often due to muscle spasms (Hunt and Burne, 1995). More than four-fifths of all patients experienced pain in the last month of their lives (Hunt, 1990). Of 30 children with various conditions who died between 1983 and 1987, 80 percent required strong analgesics during the last month of their lives for pain, shortness of breath, or both. Children with cancer were the most likely to receive analgesics for pain, whereas children with other conditions were the most likely to receive opiates for shortness of breath (Hunt, 1990). The Helen House researchers also reported that one-third of the children who died experienced seizures, and a quarter of them suffered from excessive oral secretions (often accompanied by swallowing difficulties). In addition, they reported that the dying children were commonly described as “frightened,” “grumpy,” “disoriented,” or “anxious and irritable” (Hunt, 1990). Even those children who could not communicate (due to age or disease progression) were described as “distressed, crying frequently” or looking “frightened.”
A Canadian study of 77 children who died anticipated deaths in intensive care relied on narrative progress notes to identify how the children died (McCallum et al., 2000). Although 84 percent of the children (who had conditions such as cancer, heart disease, AIDS, organ failure, and cystic fibrosis) received opioid analgesics, only 6 percent had specific pain assessment and treatment notes recorded in their charts, and such recording was sporadic. Systematic assessment and monitoring are essential to effective, reliable pain prevention and management and to quality assurance. The study also reported that the majority of children were intubated prior to their death and that most were “comatose, sedated, or medically paralyzed,” which the authors said could be interpreted as indicating “excessively invasive treatment” (McCallum et al., 2000, p. 421). Four-fifths of the patients had do-not-resuscitate (DNR) orders documented during the final hospital admission, but only 8 percent had such orders prior to that admission. The median time from recording of the DNR order to death was less than a day. In only one case did progress notes indicate that the prospect of death was specifically discussed with the child.
One study of 100 deaths in three pediatric intensive care units (PICUs) reported that nearly 90 percent of children who died had received sedatives, pain medications, or both (Burns et al., 2000). Physicians substantially
increased the use of sedatives and pain medications before the withdrawal of mechanical ventilation (which was usually one of the first therapies stopped for these children). Relief of suffering (e.g., air hunger, pain) was the justification for this increase, and the only patients not receiving such care were comatose and thought not to be suffering. The researchers reported no use of paralyzing agents, the use of which they considered indefensible.
Parental and clinical assessments of children’s pain and other distress may differ. For example, as shown in Table 3.1, Wolfe and colleagues (2000a) found “considerable discordance” for certain symptoms including fatigue, poor appetite, constipation, and diarrhea.
Although some observational tools have been developed to assess certain symptoms in children, clinicians or researchers often depend on parental assessments of children’s pain not only in retrospective studies following a child’s death but also for very young children, children with cognitive
TABLE 3.1 Discordance Between the Reports of Parents and Physicians Regarding Children’s Symptoms in the Last Month of Life
|
|
Reported by Parent but Not by Physician (N = 92) |
Reported by Physician but Not by Parent (N = 92) |
|
|||
|
Symptom |
No. |
(%) |
No. |
(%) |
Kappa Statistic (95% CI)a |
P Valueb |
|
Fatigue |
44 |
(48) |
1 |
(1) |
–0.02(–0.07 to 0.02) |
<0.001 |
|
Pain |
15 |
(16) |
11 |
(12) |
0.10(–0.12 to 0.32) |
0.56 |
|
Dyspnea |
19 |
(21) |
10 |
(11) |
0.10(–0.11 to 0.31) |
0.14 |
|
Poor appetite |
33 |
(36) |
1 |
(1) |
0.29(0.15 to 0.43) |
<0.001 |
|
Constipation |
31 |
(34) |
7 |
(8) |
0.16(–0.02 to 0.33) |
<0.001 |
|
Nausea/vomiting |
25 |
(27) |
18 |
(20) |
0.06(–0.14 to 0.26) |
0.36 |
|
Diarrhea |
20 |
(22) |
8 |
(9) |
0.31(0.12 to 0.51) |
0.04 |
|
aData were missing for 10 children for whom there was no documentation of clinic or hospital visits in the last month of life and for 1 child whose records were not available for review. CI denotes confidence interval. bMcNemar’s test was used. SOURCE: Wolfe et al., 2000a. Used with permission. |
||||||
impairments, and children with very advanced disease. One review of studies comparing parental and child assessments concluded that the evidence is mixed but parents tend to underestimate their child’s pain (Chambers and Craig, 1999).
A Swedish study of children being treated for cancer interviewed children and parents (Ljungman et al., 1999). It reported that “treatment-related pain was constant and dominant,” that treatment- and procedure-related pain was more severe than pain due to malignancy, and that pain evaluations were unsystematic. An older study by McGrath and colleagues (1990) also reported that treatment- and procedure-related pain was common, with more than a third of the children reporting moderate to severe pain from chemotherapy and 61 and 78 percent reporting such pain from lumbar puncture and bone marrow aspiration, respectively. The study did not report on treatment strategies. A 1995 article reporting on severe pain in children dying of cancer concluded that following WHO pain guidelines was adequate for most children but that a subgroup required extraordinary measures (Collins et al., 1995). Individualized management and careful assessment of pain were essential.
Studies by Ferrell and colleagues also suggest the inadequate management of cancer pain in children (Ferrell et al., 1994; Rhiner et al., 1994). The studies assessed the impact on families of living with and trying to manage a child’s pain and identified parents’ feelings of helplessness and stress.
Additional studies have examined pain assessment and management for broader groups of children. A 1994 article reported on pain management practices in three Canadian neonatal intensive care units (NICUs). It concluded that procedural and disease-related pain is frequently untreated or undertreated (Fernandez and Rees, 1994).
A study by Kazak and colleagues (1996) compared distress during invasive procedures for childhood leukemia as rated by mothers and nurses. Children receiving a pharmacological-only intervention were rated as having more distress than children receiving a combined pharmacological and psychological intervention. Younger children were rated as having more distress than older children. A 1999 review of the literature on psychological interventions for disease-related pain in children identified relatively few studies, most of which had methodological problems (e.g., small sample size, no control group) (Walco et al., 1999). Taken together, the studies suggested benefits of some interventions but they were not definitive.
Unexplained variation in pain management and other practices is also a concern. One study of narcotics use for very low birth weight babies in NICUs reported a 29-fold variation in the use of opioids (Kahn et al, 1998). This kind of variation demands further investigation. Differences may re-
late, in part, to differences in the degree to which physicians feel legally vulnerable in administering pain medications or have misconceptions about addiction from long-term use of narcotics. Variation in methods used to assess the contribution of pain in prematurely born infants may also play a role. Pain assessment tools that have been validated in premature babies at different gestational ages and at different chronological ages should prove useful in evaluating the adequacy of neonatal intensive care, reduce unexplained variations in treatment, and reduce infants’ distress (see, e.g., Krechel and Bildner, 1995).
Palliative Care Consultations and Discussions
The extent of explicit palliative care consultations is little documented for children and families. A recently published study examined all 196 deaths in an NICU between 1994 and 1997 (Pierucci et al., 2001; see also Leuthner and Pierucci, 2001). The authors reported that palliative care consultations were associated with significantly more supportive services (e.g., referrals to chaplains or social workers) for infants and families, fewer medical procedures (e.g., blood draws, radiographs, endotracheal tubes but not intravenous fluids, nutritional support, narcotics), and documentation of family emotional needs and support. Consultations prior to the child’s death increased during the period studied from 5 to 38 percent. The authors could not assess whether lack of consultation reflected lack of physician or family readiness for palliative care or other factors. They did not attempt to measure the effectiveness of the supportive services provided in relieving child or family distress.
In the study by Wolfe and colleagues (2000a) cited above, earlier discussion of hospice care was associated with parental reports that their child was peaceful and calm during the last month of life. For about two-thirds of the children who died of progressive disease (rather than treatment complications), charts noted a discussion of hospice care, which occurred, on average, about 58 days before death. Further, suffering was greater in children whose parents reported that the child’s physician was not involved in his or her end-of-life care. This pattern held after adjusting the analysis for cause of death, child’s age at death, place of death, interval between the child’s death and the parental interview, and physician clustering (Wolfe et al., 2000a).4
Limitations of Life-Support and Disease-Modifying Interventions
A recent examination of the limitation of aggressive life support concluded that much attention had been paid to the question of whether and when to limit these interventions and argued that more research should focus on how to assess and improve the quality of care for patients once the decision has been made (Rubenfeld and Curtis, 2000). Studies of pediatric deaths in intensive care have found that deaths are often preceded by limitations of life support interventions—more than half of the deaths in one recent study (Keenan et al., 2000), more than one-third to one-half in an earlier study (Vernon et al., 1993;5 Levetown et al., 1994), and more than 70 percent in a neonatal intensive care unit (Wall and Partridge, 1997). The accompanying assessment and management of pain, air hunger, or other distress has been less documented as has the timing of decisions to limit life support.
Even though death is often preceded by limitations of life-support interventions, studies also suggest that during their last month of life, the majority of children who die from chronic conditions receive some form of medical treatment that is regarded as curative or life prolonging. The earlier-cited study by Wolfe and colleagues (2000a) reported that 56 percent of children with cancer received some sort of cancer-directed therapy in the last month of their lives. More than one-third (36 percent) had undergone a bone marrow transplant, and for 60 percent of these children, the transplant was their last cancer-directed treatment. Two-thirds of children in the study had DNR orders. These orders were entered, on average, 33 days before death for children who died of their disease and 1.7 days before death for children who died of treatment-related complications. An earlier study of DNR orders in one children’s hospital also reported that most of these orders were written for children who were receiving “aggressive” medical therapy in intensive care units (Lantos et al., 1993, p. 52). Orders were more common for older children than for infants. Wolfe and colleagues suggest that when life-prolonging treatment is pursued to the last, more attention to concurrent palliative therapies might reduce children’s suffering.
Possibly reflecting the difficulty of changing a long-term pattern of treatment, one small study suggests that children with chronic illness hospitalized in PICUs were less likely to have life-sustaining treatment withheld or withdrawn than were acutely ill patients (Keenan et al., 2000). Levetown’s 1994 study, however, reported no difference between the two
groups on this aspect of care. Additional research on treatment patterns for acute versus chronic conditions could inform understanding of the factors influencing treatment choices. For children with serious, chronic conditions, repeated hospitalizations may be an almost routine part of life. Families may become used to seeing the ill child “bounce back” after numerous life-threatening acute events. Then, as Ann Goldman suggests, “After a lifetime of intensive treatment, it can be difficult to abandon past patterns of care” (Goldman, 1999, p. 30).
With advances in organ transplantation, patients with conditions such as cystic fibrosis (often now young adults) and their families may regard what was previously seen as the end stage of their disease as an opportunity to be listed for a transplant, thus maintaining a hope for survival rather than preparing for death. Long-term survival, while improving, varies for different kinds of conditions (see Kurland and Orenstein, 2001), and a shortage of donated organs limits the number of transplants. Of the 45 patients who died of cystic fibrosis in Canada in 1996, an analysis found that 93 percent had been considered for transplant, 7 (17 percent) had been listed, and 2 (4 percent) had received the transplant (Mitchell et al., 2000). The analysis did not report how many received a transplant and did not die.6 Palliative care was never discussed for one-quarter of the patients and was discussed a month before death for 40 percent.
Another study, this one in the United States, evaluated records for 44 patients more than 5 years of age who died of cystic fibrosis at one institution between 1984 and 1993. The majority of these patients were over age 20. Four died after lung transplants, and four died on mechanical ventilators in the PICU awaiting transplant (Robinson et al., 1997). Three-quarters of the patients were receiving therapeutic (e.g., intravenous antibiotics, chest physical therapy) or preventive (e.g., oral vitamins) interventions in the last 12 hours of life. Compared to surgical interventions, most cancer chemotherapy, and some other drug regimens, these therapies are less invasive and produce limited side effects. All patients had do-not-resuscitate orders, and nearly all received some opiates for pain (two of six patients who did not refused for religious reasons). Of the 44 patients, one died at
home under hospice care; the remainder died in the hospital with “many of the important psychological and emotional aspects of hospice” (Robinson et al., 1997, p. 208). The authors of this study noted that while the final outcome of the disease is certain, uncertainty about short-term prognosis and the waxing and waning nature of respiratory failure in cystic fibrosis make it difficult to abandon antibiotics, physical therapy, mechanical ventilation, and similar measures. Again, some of these interventions impose relatively little burden on patients.
Despite prognostic complexities, improvements in the care of patients with unpredictable life-shortening conditions are possible. The strategy of “hoping for the best while preparing for the worst” allows clinicians and families to pursue life-prolonging interventions such as transplants with conviction and, at the same time, to be attentive to symptom management, personal goals (e.g., a family vacation), and other steps to help families make the most of the time they have.
One study of the withdrawal of life support in adults reported that “forms of life support that were perceived as more artificial, scarce, or expensive were withdrawn earlier” and that “once the decision has been made to forgo life-sustaining treatment, the process remains complex and appears to target many different goals simultaneously” (Asch et al., 1999, p. 153). If anything, the complexity of the process and the existence of multiple goals of care are likely to be even more evident when decisions involve children.
Inconsistency in clinical decisions about life-support and disease-modifying interventions is a concern. One survey study of pediatricians’ decisionmaking found considerable variation in management strategies about withholding or withdrawing life-support interventions for chronically ill children as described in eight clinical scenarios (Randolph et al., 1999). For six of the eight scenarios, less than half the respondents chose the same intensity of care (e.g., mechanical ventilation, dialysis, antibiotics). For three of the scenarios, at least 10 percent chose the most intensive level of management while at least 10 percent chose comfort measures only. The most important influences on choices were the probability of acute (short-term) survival and parental wishes. Those who rated parental wishes highly were more likely to choose aggressive care when parents wanted it, even when the long-term prognosis was poor. Also, those who rated themselves as more likely than their colleagues to withdraw life support were indeed more likely to make that choice. Although the authors note that decisions in actual practice needed investigation, they observed that “variability in decision-making may lead to unnecessary suffering, lack of fairness when making decisions about neurologically handicapped infants, and inappropriate use of scarce resources in futile cases” (Randolph et al.,
1999, p. e46). They recommended clearer guidelines for decisions about limitation of life support for children.
A recent study of European neonatologists also found considerable variability in how quality-of-life was weighed in decisions in the NICU (Rebagliato et al. 2000). The authors concluded that the country in which a physician practices was the most powerful predictor of choices. The researchers also found that physician attitude, seniority of position, length of experience, and working in larger NICUs were significantly correlated with a greater likelihood of a physician’s choosing to limit life-sustaining medical interventions based on predicted quality of life.
In the United States, studies examining the attitudes of neonatologists report that neonatologists frequently are willing to limit treatment in severely malformed, premature, or ill babies. One study examined the actual practices of neonatologists at a university medical center as documented in medical records. It found that 73 percent of all neonatal deaths at a tertiary NICU followed the withdrawal or withholding of life-sustaining treatment (Wall and Partridge, 1997). In contrast, a similar study in 1973 reported that only 14 percent of neonatal deaths were attributed to withdrawing or withholding treatment (Duff and Campbell, 1973). In the 1997 study, death attributable to withdrawing or withholding life-sustaining treatment was more common in severely neurologically damaged babies (more than 85 percent) than in babies with major congenital anomalies (67 percent). Neonatologists most commonly noted futility of treatment as the reason for limiting or withdrawing treatment (74 percent). They noted quality-of-life issues in 51 percent of cases (more often mentioning severe disability than unnecessary suffering as the issue). Quality of life, exclusive of any reference to the futility of treatment, was mentioned as the reason for withdrawing or withholding treatment in 23 percent of the deaths. The authors of the study observe that medical records might underdocument the importance of quality-of-life considerations based on concerns about federal “Baby Doe” regulations on treatment of infants with life-threatening conditions (see Chapter 8).
Problems in Communication
Hilden and colleagues observe that physicians report anxiety about discussing an impending death with children and their parents (Hilden et al., 2001a). Anxiety and dread may interfere with a thorough assessment of a child’s emotional and spiritual well being and careful evaluation of child and family circumstances (e.g., cultural values, religious beliefs). Inadequate assessment may, in turn, compromise timely efforts to identify and relieve physical and emotional distress.
Clinicians’ anxiety may also contribute to poor communication about the child’s situation and prognosis, which may deprive children and families of information they need to plan for the future and weigh the pain or other suffering expected from an intervention against its probability of meaningfully extending a child’s life. Certainly, most pediatric specialists have less experience than similar adult specialists in communicating a grim prognosis, although both groups have little or no training in this task (see Chapters 5 and 9).
A survey of 122 experienced emergency room physicians published in 1997 reported that few of the respondents reported any training in telling parents about a child’s death or any familiarity with guidelines for such notifications (Ahrens and Hart, 1997; Maruyama, 1997). Two-thirds of the respondents described communicating with parents after a child’s death as the most difficult part of emergency medicine. A similar percentage said communicating with parents about a child’s death was more difficult than communicating with a family about an adult’s death. Even more striking in this small survey, more than two-thirds of the respondents said that they had prolonged resuscitation efforts solely to delay telling parents that their child had died.
Khaneja and colleagues (1998) surveyed residents, fellows, and attending pediatricians at one institution to describe their general attitudes toward pediatric death and dying. Of those responding, 61 percent of all attending physicians and 73 percent of attending physicians in specialties with a higher predicted patient mortality rate reported that they sometimes consider a patient’s death to be a personal failure. Conversely, residents and fellows rarely felt this sense of personal failure when a patient died. Despite feelings of failure, when a patient died, older physicians not surprisingly felt more prepared to deal with issues of death and dying than younger physicians: 13 percent of residents, 56 percent of fellows, and 71 percent of attending physicians felt adequately trained to deal with end-of-life issues, but the study did not independently assess skills. However, almost all of the physicians agreed that there was a need for further support of health care workers in dealing with death and dying (100 percent of residents, 83 percent of fellows, and 90 percent of attending physicians wanted more support). Most also agreed that the existing support systems in the pediatric department of their hospital were inadequate. Many physicians expressed a desire to attend funerals of patients, for instance, but very few had actually done so. Most cited conflicting clinical duties as a reason they were unable to attend funerals.
Other researchers as well as personal stories also point to physician anxiety and confusion about communicating bad news and discussing death and dying (see, e.g., Solomon, 1993; Nuland, 1994; ABIM, 1996a,b; IOM, 1997; Christakis and Iwashyna, 1998; Bruera et al., 2000; for pediatricians
specifically, see Ahrens and Hart, 1997; Vazirani et al., 2000). Although most of these studies involve adult patients and families, it seems reasonable that some of the problems they identify will apply to communication involving children with life-threatening conditions. For example, a study by Lamont and Christakis (2001) reported that clinicians may consciously withhold information or provide cancer patients and families with misleadingly optimistic assessments and that younger adult patients were more likely to receive such misleading assessments than older patients.
A recent project to improve communication about organ donation in adult neurologic and pediatric intensive care units reported on training sessions that involved conversations between health care teams and standardized patient families. As reported in a conference poster session (Williams et al., 2001b), the researchers found that physicians were reluctant to use the “d” words (death, dying), that euphemisms confused family members, and that teamwork among team members (physicians, nurses, transplant coordinators, and clergy) contributed to effective communication. (Following training, organ donation rates increased on the study units.)
One small study of residents’ competence in delivering bad news (a diagnosis of lung cancer) to adults concluded that they were not very good at it (Eggly et al., 1997). Using a 16-item instrument, the authors rated residents’ skills as displayed during taped interviews with simulated patients. Residents were rated weakest in eliciting the patient’s perspective. The authors concluded that the residency program was not doing an adequate job of teaching residents to use a patient-centered approach to discussions with patients. Another small study also used simulated parents as part of the process of assessing the parent counseling and information-giving skills of pediatric residents and emergency department fellows, providing feedback, and assessing improvement in subsequent discussions (Greenberg et al., 1999). The investigators reported improvements in two areas: reducing parents’ feelings of dependence and improving feelings of trust. A third small study of pediatric critical care fellows using a somewhat different methodology also showed improvements following feedback by the simulated parents (Vaidya et al., 1999). Other studies have concluded (through self-reports and clinician assessments) that communications training for medical students and residents can improve their self-confidence, comfort, or skills in breaking bad news (Cushing and Jones, 1995: Garg et al., 1997; Vetto et al., 1999).
If physicians cannot face fully a child’s poor prognosis and then appropriately communicate their assessment to families, timely reexamination of the goals of care and corresponding adjustments in care plans may be delayed. One retrospective study of parent and physician perceptions of the end-of-life care of 103 child cancer patients found a significant disparity between the time the physician first documented that the child was entering
the end-of-life phase of his or her illness and the time the parents reported recognizing that there was no realistic chance for cure (mean difference of 101 days) (Wolfe et al., 2000b). The differences in physician and parent understanding of prognosis were not statistically significantly associated with differences in the care outcomes studied. However, when the physician’s and parents’ understanding of prognosis correlated more closely early on, the goals of care were more likely to be directed at lessening the child’s suffering. Hospice was introduced earlier. Parents also were more satisfied with home care during the end-of-life period. When a psychologist or social worker was involved in the child’s care, agreement between physician and parent assessments was more likely.
IMPLICATIONS
Children who die vary in the paths they follow, and some children with grave medical problems survive. Thus, pediatric palliative care—and if death occurs, end-of-life and bereavement care—must be flexible to meet the highly variable, changing, and sometimes difficult-to-predict needs and circumstances of children and families.
Evidence about the adequacy of current care for children with fatal or potentially fatal medical problems is limited but generally consistent with that found for adults in pointing to shortfalls in many dimensions of care. Specifically, pain and other symptoms are inadequately and variably assessed and treated, despite the availability of treatments that are effective, especially for pain. Palliative care consultations appear to increase the use of supportive services, but late or absent consideration of the benefits of palliative or hospice care is a problem. This puts children at risk of needless suffering from invasive and uncomfortable procedures that promise little or no benefit. Routine discussion and re-evaluation of the goals of care, which assists parents in making medical and other decisions, does not appear to be a part of “normal” health care for children with complex medical conditions.
More children with fatal conditions are dying after the limitation of life-support interventions, but the adequacy of care to manage any distress associated with stopping or not starting such interventions is little studied. Little research is likewise available on the prevalence, intensity, and management of symptoms other than pain and of psychological distress in children with fatal or potentially fatal conditions. Different studies point to problems in the communication of information to help families understand what may lie ahead and to make decisions about different courses of care. Barriers to these “just in case” conversations include physicians’ discomfort in discussing bad news, fragmentation of care, and financial disincentives.
The literature reviewed in this chapter as well as illustrative vignettes suggest several directions for improving the effectiveness and consistency of pediatric palliative and end-of-life care. These directions include better understanding of the dimensions of pediatric palliative and end-of-life care and better understanding and application of existing knowledge and resources. Other directions include changes in the organization of care that may increase the effectiveness and reliability of such care, better training of health professionals in the principles and techniques of palliative and end-of-life care (including accurate but sensitive communication), and more research on almost every dimension of such care and the medical and other criteria for identifying children and families who might benefit from it. The next several chapters expand on these topics and also review the financing, legal, and ethical context of care for children with fatal or potentially fatal medical conditions.
































