7
Medical and Psychotherapeutic Interventions
Almost half of the individuals who complete suicide in the United States are diagnosed with a mental disorder and are under treatment by a mental health professional (Conwell et al., 1996; Fawcett et al., 1991; Harris and Barraclough, 1997; Isometsa et al., 1994; Robins et al., 1959). To be able to prevent suicide through treatment and therapy, it is necessary to know when the individual is in immediate danger of dying by suicide. However, existing assessment instruments may help in identifying who is at risk, but do indicate when they will be at risk. Further, since certain life events can precipitate suicide in some but not all patients, their predictive value is poor. Many at-risk patients receive medication for mental disorders. But while these medications often reduce the symptoms of these disorders, the effectiveness of such medications to decrease the risk of suicide is unknown. Medications are best delivered in the context of a therapeutic relationship featuring an ongoing and appropriate psychotherapy or counseling, conscientious follow-up, and an overall flexible treatment plan that considers the socio-cultural context of the patient. This chapter addresses issues of assessment, reviews current knowledge about the effectiveness of medications for suicidality, and describes the impact of hospitalization and psychotherapy on suicidality.
ASSESSMENT
Suicide risk is difficult to assess. Individuals making serious suicide attempts may knowingly withhold their intentions (e.g., Apter et al., 2001;
Morrison and Downey, 2000; Negron et al., 1997). No psychological test, clinical technique, or biological marker is sufficiently sensitive and specific to accurately assess short-term prediction of suicide in an individual (Goldstein et al., 1991). A prospective study (Pokorny, 1983) of 4800 consecutive patients at a Veterans Administration hospital used 21 known suicide risk factors to identify 803 patients with increased risk of suicide. Thirty of these identified patients completed suicide during a 5-year follow-up period. But an additional 37 patients than had not been assessed as at-risk also completed suicide. Even an optimal measure with the unrealistically low rate of false-positives and false-negatives (1 percent) would only correctly assess 20 percent of those who complete suicide (MacKinnon and Farberow, 1976). Assessment instruments can be useful tools but are not a substitute for clinical judgement. Nevertheless, assessment is an important component of psychopharmacological and psychotherapeutic interventions.
Assessment Instruments
Whether using a standardized psychological test or interview only, it is important to assess for suicidal symptoms, symptoms of the known risk factors for suicide, and current abilities to cope with acute or chronic stress (Bech et al., 2001). Assessment instruments fall into four broad categories: (1) detection instruments, (2) risk assessment instruments, (3) assessment of clinical characteristics of suicidal behavior, and (4) a miscellaneous category (e.g., compilations, assessment of attitudes around suicide, projective psychological tests1). Assessment tools for adults and youths have been extensively reviewed by Brown (2000) and Goldston (2000), respectively.
One of the most widely used and best-evaluated measures is the Scale for Suicide Ideation (SSI) (Beck et al., 1979). It is a 19-item scale, available as interview, self-report, or computer-administered. Only if a person endorses an item indicating intent to complete suicide, is the rest of the scale administered. It has been standardized on both inpatient and outpatient clinical samples. It has also been used in emergency rooms, primary care settings, jails, and in college student samples. A prospective study with almost 7000 patients and an approximately 20-year follow-up with psychiatric outpatients used standardized, structured interviews and standardized assessment measures (Brown et al., 2000). These data were
matched to the National Death Index, and death certificates were obtained for those who had died. Through this process, 49 suicide cases were identified. The average length of follow-up was 10 years, and the average length of time to death was approximately 4.3 years from the baseline interview. Patients who scored above 3 on the SSI were about 6.5 times more likely to complete suicide than patients who scored below this cut-off.
Other scales that have been shown to have some predictive validity include the Beck Hopelessness Scale, Beck Depression Inventory, Beck Anxiety Scale, and the Hamilton Rating Scale for Depression. Measurements of personal contentment, such as Linehan’s (1983) Reasons for Living Inventory and Koivumaa-Honkanen and colleagues’ (2001) simple life satisfaction measure, also seem to have value in some populations. All of the instruments have their strengths as well as their weaknesses, but there may be no single “best” instrument for all purposes. The choice of instruments depends on the needs of the clinician or researcher, the intended use of the instruments, and an assessment of how an instrument compares to other similar instruments in meeting diagnostic needs. Furthermore, the age, gender, and culture of the suicidal individual must also be considered in choosing assessment scales. Some measures of psychopathology and suicide risk may not be as accurate or appropriate for specific populations, since risk and protective profiles differ across ethnicity, gender, and age. Cognitive measures of mental disorders, for example, may not be as sensitive for ethnic groups that experience psychopathology in more somatic than in cognitive terms (Marsella et al., 1975; Marsella and Yamada, 2000), and culture and developmental stage (e.g., single adolescent vs. adult parent) influence such things as reasons for living (see Chan, 1995; Linehan et al., 1983; Osman et al., 1998).
Confounding Factors
Variations in Purpose
Assessment tools differ; there are detection instruments, risk assessment instruments, and instruments for assessing clinical characteristics of suicidal behavior. Each of these groups of instruments is useful for answering certain types of questions, but the use of the wrong instrument may yield insufficient or even misleading information. A risk assessment instrument will not provide information about whether someone is currently suicidal (an issue of detection). A person may score “low” on a risk assessment instrument assessing a particular domain (e.g., hopelessness) while still experiencing suicidal ideation or even having made a recent attempt (Goldston, 2000).
Incomplete Use
Further confounding the use of assessment tools is their misuse. At times, researchers have used one or two items from an assessment scale, when the tools have only been validated in their full form. Studies frequently use just a single item from the Hamilton Depression Scale, a practice which results in a decreased sensitivity of the assessment tool. Complete, standardized suicide assessment measurements are most appropriate in clinical trials.
Population Specificity
Instruments may not have the same predictive utility when used in populations other than those in which they were developed (Meehl and Rosen, 1955). The base rate of risk factors may vary significantly across different populations, so that the same level of a risk factor may have significant predictive utility in some groups, but not others. In addition to base rate differences, risk factors may vary in meaning, salience, and/or presence across groups. The prevalence of risk factors for suicidal behaviors differs in different samples or population groups, just as the base rates of suicidal ideation and suicide attempts differ. Moreover, some instruments may be more appropriate than others for certain age groups, and some instruments may be more “culturally sensitive” than others. For these and other reasons, an instrument that has been demonstrated to be of use in one population may not be as useful with other groups.
Instruments developed with school-based or community samples may not have the same predictive utility in “high-risk” or clinically ascertained samples, and vice versa. Risk factors in a community may not be useful as a predictor of suicidal behavior in higher risk populations. First-time suicide attempters may differ from those who attempt more than once, and predicting first and later attempts may involve different risk factors. Goldston’s team (2001) found that hopelessness was a strong predictor of future suicide attempts following hospitalization among adolescents who previously had made at least a single suicide attempt, but hopelessness was not a significant predictor in those without a history of suicide attempt(s).
Distal vs. Proximal Factors
The relationship between vulnerability factors assessed with risk instruments (distal risk factors) and precipitating stresses (proximal risk factors) needs to be better understood. Using instruments focused on identifying groups based on various risk factors may tell us who is at risk,
but not when they are at risk. Specific life events may precipitate or provide the occasion for suicidal behavior, but they do not tell us who is likely to make those attempts. The course or persistence of vulnerability factors over time and an individual’s reactions to life events and stressors are important influences. To accurately predict suicidal behavior, a better understanding of the interplay between vulnerability factors and stresses is needed.
PSYCHOACTIVE MEDICATIONS
Since 90 percent of suicide occurs in people with mental disorders, it is thought that treating the underlying disorder could reduce suicide risk. For some medications there is evidence that the effects on suicidality may be independent from the effects on the mental disorder. This section reviews the evidence that medications used to treat mental disorders can influence the risk of suicide.
Mood Stabilizers
Mood stabilizers are used to treat bipolar illness. These drugs fall into two major classes. The first is lithium, a naturally occurring salt, which is effective in reducing the manic and depressive symptoms. Another group of medications proven effective for bipolar disorder is the anticonvulsants (e.g., carbamazepine and valproic acid).
Lithium
Evidence suggests that lithium treatment of bipolar disorder significantly reduces suicide rates (Baldessarini et al., 1999). In fact, lithium may have specific anti-suicide effects for people with this disorder since these effects may be separate from its antidepressant and antimanic effects. A prospective, randomized controlled clinical trial (Thies-Flechtner et al., 1996) in patients with bipolar illness found that lithium carbonate significantly reduced suicidal acts per patient, relative to patient years. A series of reviews and a meta-analysis of the effect of lithium on suicidality by Tondo and colleagues (Tondo et al., 1997; 1998; 2001) supported the finding that lithium reduced the rate of both suicides and suicide attempts in bipolar patients. The meta-analysis of 12 studies on lithium reported that the risk ratio in favor of a therapeutic lithium effect on suicide is 8.85 (confidence interval=4.14-19.1) (Tondo et al., 2001). This estimate, if correct, would make lithium the most potent therapeutic agent so far identified. However, the protective effects of lithium are not consistent across studies (see Bowden, 2000; Brodersen et al., 2000), and some method-
ological concerns have been raised (Bowden et al., 2000; Calabrese et al., 2001a; Goodwin, 1999). Some also caution that although the data is mostly positive, the anti-suicidal effect of lithium may not be as strong as originally thought (Bowden et al., 2000).
One of the confounding issues in these studies is the time course of psychopharmacological treatment. Decreased rates of suicide are most pronounced when lithium has been used for a minimum of 2 years (Baldessarini and Tondo, 1999). Rates were reduced only while the patients took lithium; following discontinuation of lithium, the rates began to rise to levels similar to those seen prior to the commencement of lithium. Rapid discontinuation of lithium may lead to a more dramatic increase in rates of suicidal behavior as compared to more gradual discontinuation. Early studies, because of their abrupt discontinuation of lithium, may have increased placebo relapse figures (Bowden et al., 2000). Tondo, Baldessarini and colleagues (Baldessarini and Tondo, 1999; Tondo and Baldessarini, 2000; Baldessarini et al., 1999; Tondo et al., 1997) noted that the latency from onset of bipolar disorder to lithium maintenance in their patients averaged 8.3 years, but that half of the suicidal acts had occurred in the first 7.5 years. Thus, it may be of crucial importance to commence lithium treatment as early as possible in the course of bipolar disorder for patients thought to be at risk for suicidal behavior. It is noteworthy that lithium and clozapine (see below) are both effective in reducing suicidal behavior and both require regular clinic visits and blood tests. This suggests a benefit from regular clinic monitoring.
Nonadherence with medication, particularly lithium, is a critical issue for individuals with bipolar disorder and one of the primary reasons for poor treatment response (Goodwin and Jamison, 1990). Since lithium treatment is associated with an almost 8-fold decreased suicide rate (Tondo and Baldessarini, 2000), this has a serious impact on suicide risk. Research has shown that almost one-half of patients with bipolar disorder are non-adherent to lithium treatment at some point in their lives, and one-third are non-adherent two or more times (Jamison and Akiskal, 1983; Jamison et al., 1979). Younger males within the first year of lithium treatment and those patients who have elevated moods and a history of euphoric manias, especially those who complain about missing the “highs” of their illness, are more likely to be nonadherent (Goodwin and Jamison, 1990). Many people stop taking their medication after being released from the hospital, one of the factors causing significantly increased risk of suicide during this period (see below). Furthermore, clinical research with bipolar populations is very difficult due to poor treatment adherence (Goodwin and Jamison, 1990; Goodwin, 1999; Jamison and Akiskal, 1983; Jamison et al., 1979), and the poor adherence rate makes interpreting results more difficult and the conclusions less powerful in many studies.
Important questions regarding lithium still remain. Greil and colleagues (1996; 1997a; 1997b), in a series of randomized controlled studies with treatment periods of 2.5 years, found that the prophylactic efficacy of lithium on suicidality varied according to the underlying mental disorder. Carbamazepine was more effective than lithium in reducing suicidal behavior in schizoaffective disorder, especially in subgroups with depressive or schizophrenia-like features; in bipolar types it was not superior (Greil et al., 1997a). For unipolar depressed patients, lithium was found to be superior to amitriptyline (Greil et al., 1996), and in bipolar disorder patients, lithium was judged to be superior to carbamazepine (Greil et al., 1997b). Several studies also suggest that bipolar patients with rapid cycling or mixed states are difficult to treat effectively and do not seem to respond as well to lithium (Bowden et al., 2000; Calabrese et al., 2001b; Montgomery et al., 2000). Comorbidities, especially with substance use disorder, also interfere with treatment outcome (Macqueen and Young, 2001; Vestergaard et al., 1998), though comorbidity appears to moderate outcomes via treatment adherence (Calabrese et al., 2001b).
The mechanism of action of lithium is unknown. It has been hypothesized that it exerts antisuicidal effects on aggressive impulsive traits via the serotonergic system or otherwise. Importantly, lithium appears to have a direct effect on suicidal behavior, not simply by reducing the suicidality caused by depressive relapses (Möller, 2001).
Anticonvulsants
The other class of mood stabilizers found to reduce symptoms of bipolar disorder are the anti-convulsants, such as carbamazepine, divalproex, and valproic acid. These medications are recommended for bipolar patients when lithium is not an option, whether due to lithium intolerance or resistance to lithium treatment (Möller, 2001). Valproate is the most commonly prescribed mood stabilizer in the United States, overtaking lithium. However the data are very limited on the efficacy of anticonvulsants to reduce suicidal behavior; only one randomized controlled study was identified in a recent review (Goodwin and Ghaemi, 2000). Thies-Flechtner et al. (1996) conducted a 2.5 year prospective study on 175 inpatients with bipolar disorder. These patients were treated either with carbamazine or with lithium. Of the 6 patients who committed suicide, 4 were taking carbamazine. None were taking lithium at time of death, but one had discontinued lithium. All of the suicide attempts occurred in patients who were taking carbamazine. These data demonstrated a statistically significant benefit of lithium over carbamazine in the prevention of suicide. Because of the frequency with which anticonvulsants are prescribed for bipolar disorder, it is exceptionally
important to evaluate their effectiveness compared to lithium for prevention of suicide.
Anti-Psychotic Medications
Anti-psychotic medications, including neuroleptics, may also be effective in the reduction of both suicidal behavior and the overall suicide rate when suicidality is seen as a feature of psychosis in schizophrenia. Particularly compelling evidence exists for the atypical anti-psychotic, clozapine.
Meltzer (1999) found that the mortality rate from suicide was reduced by 80 to 85 percent of the expected rate for schizophrenic patients in a population of treatment-resistant schizophrenic patients treated with clozapine after adjusting for the duration of treatment.
Recently, Meltzer and colleagues (2001) reported that in a multi-centered, randomized clinical trial of 980 patients with schizophrenia or schizoaffective disorder, treatment with clozapine when compared to treatment with olanzapine resulted in significantly fewer suicide attempts and a reduced need for additional medications to control suicidality.
Meltzer and Okayli (1995) reported that clozapine in neuroleptic-resistant psychotic patients, when given as continuation or maintenance pharmacotherapy, was associated with markedly less suicidality. They reported that the number of serious suicide attempts decreased significantly and that this decrease was associated with a reduction in depression and hopelessness. Interestingly, they stated that the beneficial effect occurred independently of the response to the psychosis, so it appears to be more attributable to the effect on depression and hopelessness. Both treatment-responsive and treatment-resistant patients were included, but similar results were obtained in the two groups for both prior suicidal behavior and suicidal behavior on treatment. The suicide attempt rate fell from 25 percent prior to treatment to 3.4 percent after clozapine treatment. The lethality of the suicide attempts was also significantly reduced after clozapine treatment.
Walker and colleagues (1997) reported on data from a national registry of clozapine recipients involving 67,072 current and former clozapine users, linking the data to the National Death Index and the Social Security Administration Death Master Files. They identified 396 deaths in 85,399 person-years for patients ages 10–54 years. Mortality was lower during current clozapine use than during periods of nonuse. The mortality from suicide decreased in current clozapine users by comparison with past users. The investigators confirmed that the principal reason for the reduction in deaths was a decrease in the suicide rate. Using the Texas Department of Mental Health and Mental Retardation database, Reid’s research
team (1998) found that the annual suicide rate for 30,000 patients with schizophrenia and schizoaffective disorders was 63.1 per 100,000 patients (between 1993 and 1995), approximately five times higher than in the general population. In contrast, only one suicide occurred in 6 years among patients treated with clozapine who were of similar diagnosis, age, and sex (a yearly rate of about 12.7 per 100,000 patients). Similarly, the suicide rate was found to be 15.7 per 100,000 patients per year in all United States patients treated with clozapine based on the clozapine national registry system maintained by Novartis Pharmaceutical Corporation, the United States manufacturer of clozapine. Similar analyses with other novel antipsychotic medications have been initiated, and preliminary results suggest that they may also have some beneficial effect in reducing suicide rates.
Antidepressant Medications
A number of investigators worldwide have recently reviewed outcomes across large populations showing that a decrease in suicides correlates with the increase of antidepressant use in various European countries (Isacsson et al., 1996; Markowitz, 2001; Ohberg et al., 1998; Rich, 1999; Rihmer et al., 1998) and that suicidal behavior correlates with the inadequate prescription of antidepressants (Henriksson et al., 2001; Oquendo et al., 1999). Such population-based changes in the suicide rate may be due to numerous causes in addition to the increase in antidepressant prescriptions, but these findings suggest a benefit from receiving antidepressants which may be related to appropriate treatment of the underlying depression.
Psychological autopsy studies suggest that the rate of adequate treatment with antidepressants of depressed suicide victims is about 6–14 percent, and toxicological analyses indicate the presence of antidepressants and other prescription psychotropics in about 8–17 percent of suicides, with the frequency in men being about half that of women, and in Blacks and Hispanics being half that of Caucasians (Blazer et al., 2000; Isacsson et al., 1999; Marzuk et al., 1995; Rich and Isacsson, 1997). In general, surveys of university teaching hospitals indicate that most depressed outpatients, even in such academic centers, are either not treated or are under-treated with antidepressant medications (Keller et al., 1986; Oquendo et al., 1999). Oquendo and colleagues (1999) showed that this was just as frequent a problem for those depressed patients with a history of suicidal behavior as for those without.
A variation on the epidemiological studies is the examination of the benefits of an educational intervention. Gotland, an island province of Sweden with a population of 58,000, is a single epidemiological catch-
ment area and most treatment is provided by general practitioners (GPs). In a series of papers since 1989, Rutz, Rihmer, and colleagues (Rihmer et al., 1995; Rutz, 2001; Rutz et al., 1989a; Rutz et al., 1989b) reported that educating the Gotland GPs about depression recognition increased the use of antidepressants and lowered suicide rates by 60 percent (see also Chapter 8).
SSRIs
Serotonin reuptake inhibitors (SSRIs) are used to treat depressive symptoms in the affective disorders as well as for symptom relief for those who have other diagnoses, or do not meet the criteria for the major affective disorders. SSRIs have gained great popularity in recent years, with the number of prescriptions increasing both in the United States and in other western nations (Isacsson, 2000; Lawrenson et al., 2000; Sclar et al., 1998). Although the SSRIs reduce depressive symptoms, their potency in reducing suicide is uncertain.
Verkes et al. (1998) found that patients with personality disorders and brief depression, but not major depression, had fewer suicide attempts when treated with paroxetine as compared with placebo. On the other hand, most studies failed to find statistically significant differences in suicide or suicidal behavior with SSRI treatments. Leon et al. (1999) followed 185 patients treated with fluoxetine (from among 643 patients as part of the NIMH Collaborative Depression Study). Using a mixed effects survival analysis, they found a decreased risk of suicide attempts and completions in the fluoxetine group, but this decrease did not achieve statistical significance, perhaps because the patients given fluoxetine were more severely ill than the comparison group before treatment. On the other hand, three meta-analyses failed to show effects of the SSRIs on suicide. Two (Khan et al., 2001; Khan et al., 2000) assessed FDA trials for efficacy and found that the major SSRI antidepressants were not significantly different than placebo with respect to suicides. Another meta-analysis of 17 clinical trials (Beasley et al., 1991) indicated that fluoxetine may reduce suicidal ideation but was not significantly different from either placebo or the tricyclic antidepressants in reducing suicides or attempts.
Several factors may enter into the interpretation of these results. Hirschfeld (2000) pointed out that these studies were time-limited. In addition, they mostly attempted to screen out those at risk for suicide. In most of the clinical studies, the base rate of suicide attempts was too low to determine effectively whether the antidepressant medications reduced the number of suicide attempts or suicides in comparison with placebo (Khan et al., 2001; Khan et al., 2000; Letizia et al., 1996; Montgomery et al., 1994; Tollefson et al., 1993). To a large extent, the low base rate of suicidal
acts in most studies was a consequence of the exclusion of suicidal patients for safety reasons (see Chapter 10). Some investigators (Khan et al., 2001; Khan et al., 2000) also note that the increased contact with mental health professionals for both treatment and placebo groups confounds the observed relationships, and could possibly represent a kind of treatment in itself.
As mentioned earlier, however, increasing prescription rates for antidepressants, in particular SSRIs, has correlated with declines in suicide rates observed in a number of countries including Sweden, Finland, Hungary, and the United States (Isacsson, 2000; Ohberg et al., 1998; Rich and Isacsson, 1997; Rihmer et al., 2001). With access to national health data, it was found that with a doubling of the number of SSRI prescriptions, the suicide rate was reduced by 25 percent in Sweden (Isacsson et al., 1992). A similar result was reported in Italy, but the effect was confined almost entirely to females (Barbui et al., 1999). Though these correlations do not determine causality, they suggest the potential for antidepressants, particularly SSRIs, to reduce suicide rates. This is further supported by the findings of psychological autopsies and toxicological analyses that frequently have found that suicide victims with a mood disorder were taking inadequate therapeutic amounts of antidepressants (Blazer et al., 2000; Isacsson et al., 1994; Isacsson et al., 1992; 1997; Marzuk et al., 1995; Ohberg et al., 1996; Rich and Isacsson, 1997).
Tricyclic Antidepressants
The tricyclic antidepressants are effective for the treatment of depressive symptoms. A tricyclic such as amitriptyline may be chosen in cases of suicidality due to its sedative effects, but the high risk of fatal outcome in overdose of tricyclics is a particular concern with regard to suicidal patients. Soloff et al. (1986) found that amitriptyline non-responders made more suicidal communications than placebo non-responders in a group of 29 borderline personality disorder patients.
Other Classes of Antidepressants
In terms of actual suicidal behavior, a prospective long-term, placebocontrolled treatment study of 1141 patients found more suicide attempts, including suicides in the group treated with the norepinephrine reuptake inhibitor maprotiline compared with placebo (Rouillon et al., 1989). While maprotiline was an effective antidepressant, it was associated with increased suicide attempts.
Comparison Studies
Four of 11 randomized controlled clinical studies demonstrated that an SSRI reduced suicidal ideation compared to another antidepressant (usually a tricyclic antidepressant) and to placebo (Eberhard et al., 1988; Gonella et al., 1990; Kasper et al., 1995; Montgomery et al., 1978). Venlafaxine, given in a dose that predominantly inhibits the serotonin transporter, showed greater efficacy compared with a tricyclic after up to six weeks of treatment (Mahapatra and Hackett, 1997). Four of the remaining studies found comparable improvement in suicidal ideation with SSRIs and the reference compound (Judd et al., 1993; Lapierre, 1991; Möller and Steinmeyer, 1994; Tollefson et al., 1993). In a comparison of moclobemide, a reversible monoamine oxidase inhibitor, with the SSRI clomipramine, increased suicidality was seen among the moclobemide group but not among the clomipramine group (Danish University Antidepressant Group, 1993).
Possible Adverse Effects of Antidepressants
Mental illness can be incapacitating, and the possibility exists that as the symptoms lift (because of treatment) individuals become more capable of carrying out plans of violence toward self or others. This has been of great concern in the use of antidepressants. Müller-Oerlinghausen and Berghofer (1999) have described situations where antidepressants increase the risk of suicide in some patients by “energizing patients with preexisting suicidal thoughts or inducing akathisa (increased movement with associated anxiety/agitation).” It has long been known that affective disorders can carry a significant risk of suicide, and that some small number of patients will deteriorate rather than improve after being treated with any antidepressant or will become at an increased risk for suicide associated with abrupt improvement.
Case reports have led some investigators to suggest that there may be a risk of emergent suicidality on SSRIs, in particular, fluoxetine. For example, Teicher and colleagues (1990) observed eight patients with major depression and personality disorders who developed suicidal thoughts and in some cases made attempts as their clinical condition deteriorated and fluoxetine was being increased to the 80 mg dosing range. There were several criticisms of these conclusions, including atypical EEG findings in these patients and the persistent increase in dosage as the patients deteriorated.
Healy and colleagues (1999) have outlined several possible mechanisms by which antidepressant medication may lead to suicide in some depressed patients. These proposed mechanisms include antidepressants
simply ameliorating the lethargy and immobility of depression more rapidly than the depressed mood, suicide by overdose of medication, specific actions of antidepressant medication(s), or through side-effects of the antidepressants. Lastly, antidepressants may not be effective, or have yet to exert their therapeutic effects during the first weeks of the regime, hence the risk of suicide has not yet changed. However, the frequency of emergent suicidality has been evaluated in controlled treatment studies in mood disorders and non-mood disorders treated with SSRIs (see Montgomery et al., 1995 for paroxetine in depression; see Tollefson et al., 1993 for fluoxetine in depression). Emergent suicidality is more frequent on placebo than with SSRIs. Wheadon et al. (1992) examined fluoxetine in bulimia and found more emergent suicidality with placebo than with fluoxetine.
Marchesi et al. (1998) compared drugs in two different chemical classes of anti-depressant medication, fluoxetine (a serotonin re-uptake inhibitor) versus amitriptyline (a noradrenergic receptor blocker) treatment in 142 patients with major depression. They found no significant differences in measures for “psychic anxiety,” “somatic anxiety,” “agitation,” and “insomnia” and no increase in these measures with fluoxetine treatment. Similar claims of causing a worsening of these symptoms have been made in the course of a number of lawsuits blaming medications and the companies who develop and market them for suicides.
However, a review of emergent suicidality (see Mann et al., 1993; Mann and Kapur, 1991) has found that such reports exist for almost all classes of psychotropics (with no evidence of pharmacological specificity) and there is no consistent temporal or dose relationship. Thus, the case reports are not convincing. It has been hypothesized that this alleged effect is due to the development of akathisia. Although akathisia reports with SSRIs have occurred with or without suicidal behavior, the akathisia-like features are generally less frequent than reported with antipsychotic medications and also milder. Thus, it is not clear that this kind of akathisia-like effect can actually lead to suicidal behavior or, for that matter, violent behavior, in patients receiving SSRIs.
All of the controlled clinical data do not provide evidence of emergent suicidality, even among patients without mood disorders who are receiving SSRIs (Montgomery et al., 1995; Tollefson et al., 1993). There have been no double-blind controlled challenge and re-challenge studies done to confirm the hypothesized emergence of suicidal behavior or ideation in patients receiving SSRIs. There is a case report of individuals re-challenged with a SSRI, but that was not done in a double-blind controlled fashion (Rothschild and Locke, 1991). Thus, the anecdotal evidence at this stage is unsupported by any controlled clinical trial data. A related hypothesized mechanism for explaining the alleged relationship between
SSRIs and suicidality is the induction of anxiety and agitation by SSRIs. Again, controlled studies do not support this suggestion; in fact, they suggest the converse. Controlled studies such as those reported by Sheehan et al. (1992) demonstrate that SSRIs result in an earlier onset of therapeutic effect on somatic anxiety compared with other antidepressants or placebo. Paroxetine is superior to placebo in the treatment of agitation after 4 and 6 weeks of treatment, and superior to the active control after 4 weeks of treatment. Both paroxetine and the active control are more protective against newly emergent agitation compared with placebo. So, there appears to be little evidence of an aggravating effect on anxiety. Controlled studies indicate that drugs like paroxetine seem to have a therapeutic effect and not an aggravating effect on agitation.
Postmarketing surveillance studies have been carried out that bear on this question of emergent suicidality (Inman et al., 1993; Zaninelli and Meister, 1999). Such postmarketing surveys of thousands of patients who received paroxetine found the incidence of reported suicidal behavior attributed to the medication to be so infrequent as to be negligible. Thus, both controlled clinical trials, including large meta-analyses of large groups of patients as well as these postmarketing surveys, provide no support for the concerns of emergent suicidality.
Anxiolytic Medications
Anxiety is a common symptom in many mental illnesses, including depression, bipolar disorder, and schizophrenia, and acute anxiety and agitation are associated with an increased risk of both suicide and suicide attempts. Additionally, anxiety is a prominent feature in suicidality that is related to psychosocial stressors. Benzodiazepines are the most commonly used medications to relieve anxiety in such cases. The data relating benzodiazepines to suicide are limited. There are, in fact, some reports (Melander et al., 1991; Neutel and Patten, 1997; Taiminen, 1993) that suggest that the use of benzodiazpines is associated with an increased risk of suicide. Causality is unknown and difficult to assess. The interpretation of this observation is confounded by the fact that benzodiazepines are often used as a means to complete suicide.
ELECTROCONVULSIVE THERAPY
Electroconvulsive therapy (ECT) is a safe and effective medical treatment for affective disorders (Avery and Winokur, 1977), particularly in severe refractory depression. It is most often used in the treatment of depression with or without psychotic features, acute mania, and schizophrenia (APA, 1990; Fink and Sackeim, 1996; Mukherjee et al., 1994),
though rates of use are low, and in decline. Many texts and official recommendations indicate that when suicidal ideation and behavior is seen as a symptom of these mental disorders, ECT should be considered. It is clinically indicated in these cases of acute suicidality because of the rapid onset of its ameliorating effects (AHCPR, 1993; Goodwin and Jamison, 1990); the swift onset of action can provide time to decide on and implement appropriate long-term treatments such as anti-depressants and psychotherapy (APA, 1990). ECT is also recommended for people who have psychotic depression, for whom medications pose a medical risk, who have previously responded well to ECT, who have mixed manic episodes, and who are unresponsive to medications with catatonia, major depressive disorder, schizoaffective disorder, or melancholic symptoms.
Success rates for ECT have been found as high as 80–90 percent for unipolar and bipolar major depressive episodes and mania (Metzger, 1999), which is higher than most estimates of pharmacological treatment effectiveness, and is particularly notable given that ECT is often reserved for patients with medication resistant illnesses. In general, these studies did not differentiate by severity of illness and medication resistance status, and in studies that looked at this it was found that medication resistant patients show a 50–70 percent response rate (Prudic et al., 1990). Due to various methodological constraints, ECT has not been directly compared to drug therapy in terms of speed of onset. Thus, the commonly accepted belief that ECT is the fastest available treatment for depression (and thus indicated for acute suicidality) has not been subject to clinical studies (Roose and Nobler, 2001).
There is no evidence that ECT has a long-term effect on the suicide rate and suicidal behavior (Prudic and Sackeim, 1999). It is notable that the majority of studies have found a lower mortality rate for ECT treated psychiatric patients versus psychiatric patients with other treatment modalities, but these mortality risk studies are plagued by methodological problems. Interestingly, it has been found that the reduced mortality rate holds even after excluding suicides. Some of these studies have not noted the cause of death, so the conclusions to be drawn are limited. Even so, these studies may underestimate the positive effect of ECT on mortality since ECT is often used specifically for patients with suicidality, where a higher mortality rate would be expected. One naturalistic study of elderly patients with long-term follow-up found that the patients receiving ECT had lower mortality rates compared to patients receiving pharmacotherapy, but non-random assignment to treatment modality confounds these results; it appears that these patients may have been healthier at the outset (Philibert et al., 1995). Clinicians may be reluctant to recommend ECT in medically ill patients; however, medical illness, which may limit
the tolerability of drug treatment, is a specific indication for the consideration of ECT.
There is evidence for a short-term effect of ECT on the reduction of suicidality. Given that suicidal ideation and behavior is a key symptom of the affective disorders, it would follow that an effective treatment for the disorder would also alleviate one of its symptoms. Additionally, Prudic and Sackeim (1999) found that both the ECT responders and the non-responders showed a large decrease in scores on the suicide item of the Hamilton Rating Scale for Depression, and this decrease was greater than the average improvement on the other items.
There has been much debate about the efficacy of ECT. Results have been fairly inconclusive due to methodological problems such as lack of controlled trials, and many variations in study protocol, which makes cross-study comparison extraordinarily difficult. Also the treated patients are often extremely diverse demographically, and in terms of their diagnoses. The case of suicide is particularly problematic because even when studies on ECT have been done, either they have not looked at suicide as an outcome, or the fact of suicide being such a low base rate behavior has thwarted any strong conclusions from being drawn. Knowledge about the effectiveness and mode of action of ECT has not grown as quickly as that for the psychotherapeutic drugs, which may in part be due to its controversial reputation among clinicians, the public, and mental health consumers.
PSYCHOTHERAPIES
Data show that medicine alone is not sufficient for treatment of mental disorders or suicidality. Individuals need to be supported while they pursue adequate care for the mental disorders that put them at increased risk for suicide. Psychiatric drugs can take over a month to take effect, and finding the right combination and doses to best treat an individual can take some months. During this time people experience often unpleasant side-effects, the stigma of mental disorders, and changes in life-circumstances secondary to the disorders in some cases. Furthermore, psychotherapeutic interventions target very different variables than do psychotropic drugs.
There are several different types of psychotherapies,2 including behavioral therapy, psychodynamic (or insight-oriented) therapy, and supportive therapy. Behavioral therapies include cognitive behavioral therapy (discussed further below) and focus on directly altering current behavior. Psychodynamic therapy, on the other hand, concentrates on increasing self-understanding (see also footnote 3). Supportive therapy provides patients with a non-judgmental environment in which to offer advice, attention, and sympathy. Psychotherapy often focuses on:
-
changing long-term social-cognitive suicide risk factors such as hopelessness, low self-esteem and self-efficacy (see Chapter 3)
-
interpersonal problem-solving deficits (see Chapter 3)
-
socio-environmental risks such as family violence and parenting style (see Chapter 5)
Although certain psychotherapeutic interventions appear more effective in reducing suicide risk than others (see below), in the last 40 years mental health research has suggested that the most critical component of therapeutic treatment is the quality of the therapeutic relationship rather than the type of psychotherapy (e.g., Sexton and Whiston, 1991, see Chapter 6 for protective effects of social support).
|
The debt I owe my psychiatrist is beyond description. I remember sitting in his office a hundred times during those grim months and each time thinking, What on earth can he say that will make me feel better or keep me alive? Well, there never was anything he could say, that’s the funny thing. It was all the stupid, desperately optimistic, condescending things he didn’t say that kept me alive; all the compassion and warmth I felt from him that could not have been said; all the intelligence, competence, and time he put into it; and his granite belief that mine was a life worth living. He was terribly direct, which was terribly important, and he was willing to admit the limits of his understanding and treatments and when he was wrong. Most difficult to put into words, but in many ways the essence of everything: He taught me that the road from suicide to life is cold and colder and colder still, but—with steely effort, the grace of God, and an inevitable break in the weather—that I could make it. (Jamison, An Unquiet Mind: A Memoir of Moods and Madness, 1995:118). |
Given logistical constraints, evaluations of long-term therapeutic interventions are rare. Although numerous studies document the efficacy
of therapeutic interventions, especially cognitive behavioral therapy (CBT),3 in treating mental disorders such as depression and post-traumatic stress disorder that increase suicide risk (see Foa et al., 2000 and Chapter 3), far fewer studies document the direct effects of therapy on suicidal behavior and intent. As with pharmacotherapeutic interventions, many methodological problems currently plague studies of psychotherapeutic treatment efficacy for suicidality. Reviews of efficacy trials have noted a lack of operational definitions for the suicidal behavior studied (see Chapter 10) and paucity of standardized, reliable assessment tools to measure the suicidal outcome (see Chapter 7, above) (Hawton et al., 1998; Linehan, 1997). Many studies also fail to use blind assessment and true randomization procedures. These reviews further caution that therapist quality and adherence to treatment protocol are difficult to control and assess. Lastly, a critical limitation involves inadequate power as a risk in most of these studies, given that the infrequency of suicidal behavior makes most clinical trials too small to uncover treatment effects. Hawton and colleagues (1998), for example, estimated necessary sample sizes needed given expected effect sizes and concluded that even the pooled data from meta-analyses were probably of inadequate size (see also Chapter 10). This chapter reviews the relatively few studies utilizing adequate methodology and design.
Most studies on the efficacy of short-term treatment assessed the therapeutic potential of developing problem-solving skills, given suicidal individuals’ serious skill deficits (see Chapter 3). In general, these studies have produced positive results for both adolescent and adult samples. Four studies of suicidal adolescents and young adults suggest that CBT with problem-solving components and general problem-solving therapy4 reduces suicidal ideation and associated symptomatology such as depressive symptoms, hopelessness, and loneliness for at least 2 years (Harrington et al., 1998; Joiner et al., 2001; Lerner and Clum, 1990; Rudd et al., 1996). Three of these studies utilized group therapies; two used CBT
with a problem-solving component (Joiner et al., 2001; Rudd et al., 1996) and the other used social problem-solving therapy (Lerner and Clum, 1990). Harrington et al. (1998) used a brief, home-based intervention targeting family-based problem solving. The positive effects of these interventions held even among high-risk, multiple-attempt patients and patients with comorbid mood and anxiety disorders (Joiner et al., 2001; Rudd et al., 1996). In addition, treatment adherence in such interventions appears to be greater for high-risk, multiple-attempt patients. However, these interventions do not appear to have a significant impact on the long-term rate of suicide attempts. Harrington and colleagues’ (1998) study also found that their short-term family-based therapy specifically reduced suicidal ideation for those youth without major depression, pointing to a need for more research on the differential effects of interventions on suicidal subtypes.
Similar positive outcomes have been reported among adults receiving short-term, problem-solving and/or CBT treatments. In general, CBT and problem-solving treatment led to increased treatment adherence, reduced levels of suicidal ideation and attempts, and reductions in related symptomatology (Evans et al., 1999; Hawton et al., 1981; Hawton et al., 1987; Liberman and Eckman, 1981; McLeavey et al., 1994; Patsiokas and Clum, 1985; Salkovskis et al., 1990; van der Sande et al., 1997b). Reductions in suicide attempt rates, however, did not remain significant in long-term evaluations. Such short-term treatment approaches may prove cost effective, as indicated by Evans et al.’s (1999) pilot study.
These brief therapies in adults, as with youths, were effective even among high-risk, repeat suicide attempters, but with limitations. Liberman and Eckman (1981) compared brief (10-day) behavioral therapy including a problem-solving component versus insight-oriented therapy. The behavioral therapy group showed greater reductions in depression and suicidal ideation, but no between-group differences emerged with respect to suicide attempts over a 9-month follow-up. Patsiokas and Clum (1985) found similar results for cognitive therapy, problem-solving therapy, and supportive therapy over the course of 10 individual sessions, as all three groups showed reductions in hopelessness and suicide intent. Notably, patients who received problem-solving therapy demonstrated significantly greater reductions in hopelessness than patients who received supportive therapy. Other between-groups differences may have emerged if a larger sample had been used. Salkovskis et al. (1990) compared the relative efficacy of five sessions of CBT with a problem-solving component versus a referral to a general practitioner. Despite using a small sample (n=20), they found significantly reduced rates of suicidal ideation, depression, and hopelessness over a 12-month follow-up for the CBT group. The CBT group also showed a greater reduction in the rates of
suicide attempt over a 6-month follow-up, but not over a 12-month follow-up. Finally, Evans et al. (1999) found that bibliotherapy5 with cognitive therapy and aspects of dialectical behavior therapy (DBT)6 led to decreased depressive symptoms, but no statistically significant decreases in suicide attempts, compared to treatment as usual.7
One of the only trials of long-term therapeutic interventions for suicidality involves DBT. In a randomized, controlled trial, Linehan and colleagues (1991) found that DBT consisting of weekly individual therapy, group skills training, and as-needed phone calls led to a greater reduction in the rate of suicide attempts and the number of hospitalized days for suicidal behaviors over a 12-month follow-up, as compared to a group who received a referral to other outpatient treatment. The DBT group also displayed greater treatment adherence. The groups did not differ with regard to depression, hopelessness, suicidal ideation, and reasons for living, however. A very small randomized, controlled trial recently found that a shortened version of DBT (all the components in half the dose) did reduce suicidal ideation, hopelessness, and depression compared to treatment as usual (Koons et al., 2001). Similarly, pilot results from a quasi-experimental trial of a 12-week DBT program for adolescents (DBT-A) suggest that DBT-A may be more effective than twice-weekly individual and family therapy at increasing treatment adherence and reducing suicide ideation, depression, impulsivity, and psychiatric hospitalizations (Miller et al., 1997).
Other forms of therapeutic intervention may also be effective. Guthrie (2001) investigated the efficacy of four weekly home-based sessions of brief psychodynamic interpersonal therapy. At a 6-month follow-up, the brief psychodynamic group showed a significantly greater reduction in the rate of suicide attempts and suicidal ideation. They also reported greater satisfaction with treatment than the control group in this study, which received treatment as usual (usually referral to their general practitioner).
Yet, some treatments are not definitively effective. Three months of task-centered casework with a social worker (Gibbons et al., 1978) was
not more effective than referral to outpatient treatment in reducing suicide attempts or reducing depression and social problems. Inpatient crisis intervention followed by either short-term outpatient psychotherapy with the same clinician during and after hospitalization or a referral to outpatient suicide prevention services did not offer an advantage for rates of suicide or suicide attempts (Möller, 1989). Both of these studies excluded high-risk patients, however.
Certain psychotherapeutic interventions, therefore, hold promise to reduce suicidality, even for (high-risk) individuals identified by at least one prior attempt. Comparing across all CBT trials, two meta-analyses reached different conclusions about behavioral interventions. Hawton and colleagues (1998) included psychosocial crisis intervention and not DBT in problem-solving therapy and did not find these interventions effective. By contrast, van der Sande and colleagues (1997a) separated psychosocial crisis interventions from CBT and included DBT and the CBT condition of the Liberman and Eckman (1981) inpatient study in the CBT category. Their meta-analysis found psychosocial crisis intervention ineffective, but CBT effective. The studies reviewed in this section therefore indicate that psychotherapy can more effectively reduce depression, hopelessness, suicidal ideation, and suicide attempts compared to treatment as usual. Short-term psychotherapy with CBT and/or problem-solving training components may also positively influence a wider range of suicide risk factors than does solely supportive or insight-oriented therapy.
A critical finding from several studies of patients at higher risk involves the apparently separate treatment responses of depression and suicidal behavior. Brent and colleagues (1997) compared CBT, systematic behavior family therapy, and non-directive supportive treatment for 107 adolescents with major depressive disorder. They did not exclude participants based on suicide risk and at intake 36 percent reported current suicidality and 24 percent had a history of at least one suicide attempt. Results indicated comparable decreases in suicidality in all three treatment conditions, but significantly more rapid response in depression symptoms with CBT. Lerner and Clum (1990) found comparable results in comparison of problem-solving therapy and supportive therapy for college students with suicidal ideation. All subjects showed reduced suicidal ideation following the treatment, but depressive symptoms were significantly more reduced in the problem-solving condition. The opposite result was found by Linehan and colleagues (1991) in their comparison of DBT versus usual care for suicidal women with borderline personality disorder. In their study, there was a comparable decrease in depression symptoms between treatment conditions, but significantly fewer suicidal behaviors in the DBT condition. This highlights the gap in
the literature between what is known about general risk factors versus knowledge of specific etiological pathways to suicide.
Several points should be noted that might explain the differing results in the efficacy literature. Linehan (1997) evaluated trials in her review based on the inclusion or exclusion of “high risk” patients (operationalized as needing immediate psychiatric treatment, at high risk of suicide or having characteristics known to increase suicide risk). Forty-five percent of the efficacy trials for treatment of suicidal behavior excluded high-risk individuals. (For comparison, this is fewer than the 88 percent exclusion for high-risk individuals in pharmacotherapy trials for depression [Beasley et al., 1991] but greater than one might think in studies on suicidal behavior.) Linehan then examined the 13 outpatient studies, of which six excluded high-risk individuals. None of the 6 studies excluding high-risk individuals showed beneficial effects, but six of the seven including high-risk did show significant effects. This effect may be one of power (i.e., the frequency of suicide attempts during follow-up is likely to be greater in high-risk individuals, thus creating a larger possible effect size), which suggests the need for larger trials. This also highlights, however, that high-risk individuals are able to benefit from outpatient interventions and, therefore, exclusion from such treatments is unwarranted (see Chapter 10 for further discussion of research issues).
INPATIENT AND FOLLOW-UP CARE FOR SUICIDALITY
Inpatient Care
Although suicidality is the most common precipitant for psychiatric inpatient admission (Friedman, 1989), no randomized clinical trials have been done to determine whether hospitalizing high-risk suicide attempters saves lives (AACAP, 2001). Between 60 and 75 percent of child, adolescent, and adult patients and 40 to 55 percent of geriatric patients are admitted to inpatient units with concerns of self-harm (Jacobson, 1999). Hospitalization may be voluntary or involuntary. Involuntary hospitalization is legally permitted when an individual meets criteria for mental illness and dangerousness to self or others, per each jurisdictions’ laws.
Involuntary hospitalization is correlated with many of the common risk factors for suicide, including serious suicide attempts and completed suicide on the unit, a diagnosis of schizophrenia; history of prior attempts of high lethality; and history of living alone or living in a household without younger children (Roy and Draper, 1995).
The immediate priority upon hospitalization is to reduce the suicidal thoughts, anxiety, and other symptoms associated with the suicide attempt. Various pharmacological approaches are generally used. Patients
are sometimes more responsive to medications during hospitalization than as outpatients (Kotin et al., 1973), perhaps because of increased adherence. ECT or sedation may be indicated (Möller, 2001). However, some patients may remain actively suicidal even if symptoms improve when life stresses are not resolved.
The effectiveness of brief hospitalizations is questionable, especially when they entail no psychiatric services or post-discharge services. One randomized controlled trial compared the efficacy of general hospital admission versus discharge in reducing the repetition of suicidal symptoms and suicide attempts over 4 months and found that short-term hospitalization (i.e., a mean of less than 24 hours) without psychiatric care produced no beneficial effect (Waterhouse and Platt, 1990). However, the follow-up period was short and only low-risk attempters could be included in the study, so this may have been a problem of insufficient power (see Hawton et al., 1998).
|
On the morning of August 7th, Tom, 23, visited a former middle school teacher and confided that he was contemplating suicide and had been very close to killing himself the day before. Tom also said that he had thought about hurting his former girlfriend, sold his car, bought a gun and ammunition, and planned to buy two more guns. The teacher and the school’s principal called the police after obtaining Tom’s consent. After speaking to the officer, Tom consented to being handcuffed and taken to the hospital. The police emergency petition only required the hospital to evaluate him. Tom was kept overnight for psychiatric evaluation and released the next day. No medications were prescribed but a follow-up visit was scheduled. Tom shot himself two days later in an apartment next door to his girlfriend’s home. His mother believes her son was released too soon (O’Hagan, 2001). Name has been changed to maintain privacy. |
Five to 6 percent of suicides in United States and Great Britain occurred during psychiatric hospitalization. Robins and coworkers (1959) reported that 7 percent of their patient population completed suicide while in a psychiatric hospital. Among different populations, the rate of suicides occurring during inpatient care is higher; for example, one study of manic-depressive patients found that of those who completed suicide, 27 percent did so while under hospital care (Weeke, 1979), although half of these had left the hospital either on a pass or unapproved absence. Most frequently, inpatient suicides occur early in the hospitalization. One study found that 43 percent of the suicides during hospitalization occurred dur-
ing the first week (Crammer, 1984). However, longer stays do not prevent suicide in the hospital (Jacobson, 1999).
After Discharge Risk
The period directly following discharge from a psychiatric hospitalization is a period of significantly increased risk. There appear to be multiple reasons for this. Patients who are hospitalized are some of the most severely affected individuals. While in the hospital, they are under surveillance and do not have the opportunity or means to commit suicide. When these patients are released from the hospital, they frequently lose their support system and they again have the opportunity and the means to commit suicide. A study in Great Britain reported that within the first 28 days after discharge, suicide was more likely (7 times in men and 3 times in women) than during the remaining 48 weeks of the year (Goldacre et al., 1993). Another study similarly found that 24 percent of the suicides among discharged patients occurred within the first 3 months of discharge, primarily in the first week (see Figure 7-1) (Appleby et al., 1999b).
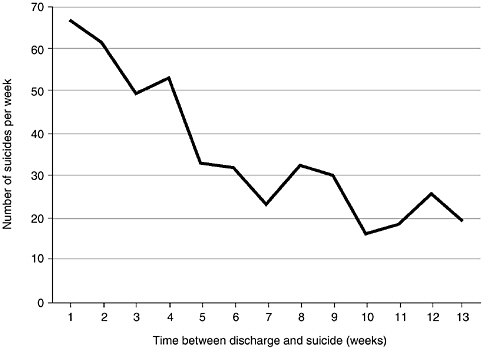
FIGURE 7-1. Number of suicides each week after discharge. SOURCE: Appleby et al., 1999b. Reprinted with permission from the BMJ Publishing Group.
Most of those who completed suicide were considered to be low risk. Discharged patients who completed suicide were 3.7 times more likely to have had their care reduced at their most recent outpatient appointment (Appleby et al., 1999a). A higher suicide rate was found to be associated with the loss of contact with the primary mental health professional (King et al., 2001). Other risk factors for suicide in recently discharged patients include living alone, hopelessness, relationship difficulties, loss of a job, a history of self harm, and a diagnosis of depression (King et al., 2001; McKenzie and Wurr, 2001). Patients who maintained care in the community (King et al., 2001) or maintained pharmacotherapy (Modestin et al., 1992) had lower suicide rates. These results suggest that discharged psychiatric patients are at higher risk of suicide for many reasons, but by maintaining some continuity of care and increasing adherence to treatment plans, some of the deaths may be prevented.
Although the risk of death by suicide appears low in medically hospitalized patients, estimated at 1.8 per 100,000 (Hung et al., 2000), the period immediately following hospitalization may be one of increased risk for these patients, as well. Dhossche and colleagues (2001) found that 73 percent (8 of 11) recently discharged medical patients who suicided were diagnosed with depression and/or substance abuse, whereas only 33 percent (11 of 33) of those who had not suicided had these diagnoses.
|
Angela, age 14, was treated in the emergency room after ingesting a “handful” of prescription pills in front of her mother and younger sister. This she did in retribution for being reprimanded and hit by her mother for staying out late. In the intake interview, she denied current suicidal ideation and stated that she was “glad” that her mother was worried. Once medically cleared, she was given an appointment with the outpatient psychiatry clinic for 9 days later, an appointment that was never kept. The nurse who attempted to contact the family by phone to follow up learned that the phone number given at intake had been disconnected for over 2 months (Berman & Jobes, Adolescent Suicide: Assessment and Intervention, 1991:164). |
Treatment Adherence
Individuals who do not adhere to their treatment regimens, including medication and therapy, are at greater risk for suicide. The period following hospitalization is a time of increased likelihood that individuals will stop taking their medications (Appleby, 2000). As described in a recent
IOM report (2001) and by Goodwin and Jamison (1990), the reasons for non-adherence can range from failure to understand the regimen or to appreciate the consequences of not following it, to adverse side effects. Lithium, for example, can cause cognitive impairment, weight gain, tremor, thirst, or lethargy (Goodwin and Jamison, 1990). It may also be that those who do not maintain their medication regimen had been reaping no benefit from it. This in turn is related to two possibilities. First, the individual may not have been on the medication for a long enough period of time to experience symptom relief; most psychiatric medications exert the desired beneficial effects only after taking them for multiple weeks. Meanwhile, unpleasant side-effects often occur during this initial period. Second, there are some people for whom the medications do not bring significant symptom relief; these “treatment resistant” individuals range upwards of 25 percent of those treated for some disorders. However, true non-response to medication is difficult to study because of the high incidence of non-adherence to dosing regimes for psychiatric drugs.
Non-adherence to treatment is a critical issue in suicide prevention since a large percentage of those taking psychiatric medications who complete suicide have been shown to have insufficient blood levels of the drugs to have reaped any benefits. Adherence to psychiatric treatment is lower than for treatment of somatic disorders, likely due to the societal stigma and unpleasant drug side effects, which typically start before the therapeutic benefit. In addition, for bipolar disorder and schizophrenia, suicide is most likely during the first years after diagnosis, often before consistent drug and therapy treatments have been established. These two disorders are most frequently diagnosed in early adulthood, a period when people may not yet have the maturity and/or financial resources to overcome the high stigma, tolerate the unpleasant side effects, and mount the barriers to accessing treatment and establishing a successful treatment regimen.
Follow-Up Care
Because of the high post-discharge suicide risk, many hospitals have implemented various forms of follow-up care for suicidal patients. Intensive follow-up, case management, telephone contacts, letters, or home visits sometimes improves treatment adherence (e.g., Termansen and Bywater, 1975; van Heeringen et al., 1995; Welu, 1977). Such interventions have produced mixed results with regard to suicidal behaviors: some have demonstrated decreased suicide attempts (Aoun, 1999; Termansen and Bywater, 1975; van Heeringen et al., 1995; Welu, 1977) and even completions (Motto and Bostrom, 2001), while others have found no effect on suicide attempts (Chowdhury et al., 1973; Litman and Wold, 1975).
Intervention efficacy may sometimes depend on the diagnosis of the suicidal individual (e.g., Byford et al., 1999).
Termansen and Bywater (1975) investigated the relative efficacies of no intervention, emergency room assessment alone, emergency room assessment plus as-needed follow-up care at a volunteer crisis center, and emergency room assessment plus a 3-month follow-up by the same mental health worker who conducted the assessment. Over the 3-month follow-up period, they found that the group who received follow-up by the same mental health worker demonstrated lower rates of suicide attempts and higher treatment adherence. Motto and Bostrum (2001) examined the impact of regular follow-up letters to suicidal individuals who refused ongoing treatment after discharge from a hospital. The study randomly assigned those refusing follow-up care or dropping out of follow-up care after hospitalization for severe depression or suicidality to either usual care or to receive regular letters from staff. Results of a survival analysis showed that for the first 2 years, the difference in the survival curves was significant, with the time to suicide longer in the contact vs. no contact group. When evaluated over the full five years the curves were not significantly different. It is important, however, that differences were greatest during the first 2 years, which is when suicides are most likely to occur. This was also when contact with the subjects was most frequent (in year 1). This is the only study to show a significant difference between experimental and usual care conditions for completed suicide.
In a comprehensive intervention, Aoun (1999) (1) instituted a standardized hospital protocol for dealing with cases of deliberate self-harm, (2) employed a suicide intervention counselor who worked with patients from within 48 hours of admission until 6 weeks post-discharge, and (3) provided professional and community education about intervention, risk assessment, and access to service. The experimental group received treatment from the suicide intervention counselor, and the control group received treatment as usual. Patients who received treatment from the suicide intervention counselor had significantly lower rates of hospital readmission for suicide attempts over a 22-month follow-up, as compared to readmission rates among patients who received treatment as usual and patients who were admitted prior to the start date of the intervention. Unfortunately, the findings of this study are limited by non-randomized groups and a variable length of follow-up depending on when the patient entered the study.
Rotheram-Borus, Piacentini, Cantwell, Belin, and Song (2000) provided specialized emergency room care to adolescent females with the goal of enhancing adherence to outpatient therapy. The intervention included a soap opera video regarding suicidality, a family therapy session, and staff training. The control group received standard emergency room
care. At an 18-month follow-up, no significant between-group differences emerged in suicidal ideation or the rate of suicide attempts, although lack of power may have obscured treatment effects. Nevertheless, the experimental group showed significantly lower depressive symptoms and higher family cohesion, and these effects were greatest among those with higher suicidal symptomatology at admittance to the emergency department. This intervention also appears to improve treatment adherence among high-risk Latina adolescents (Rotheram-Borus et al., 1996; 1999).
CULTURAL CONSIDERATIONS AND FAITH-BASED INTERVENTIONS
When assessing risk and creating a treatment plan for suicidal individuals, as for any patient with mental illness (US DHHS, 2001), taking their cultural and spiritual views and needs into account emerges as a critical component of effective interventions. Language barriers prevent thousands of immigrants in the United States from receiving proper mental health care (US DHHS, 2001, see also Chapter 9 for discussion of barriers to treatment). Furthermore, racial and ethnic factors may affect how individuals respond metabolically to some common psychoactive medications (US DHHS, 2001). Individuals from ethnic and racial minority populations are far less likely to turn to professional mental health providers than are European Americans; some prefer traditional and/or spiritual methods of healing to mainstream medical and mental health strategies (see US DHHS, 2001, and Chapter 2, section on African Americans). Cultural and spiritual beliefs concerning self, psychobiological functioning (mind-body interactions), and disease causation influence the expression of mental disorders and response to treatment, including treatment adherence (Hsu, 1999; Marsella, 1988; Marsella and Yamada, 2000).
Clergy/spiritual ministers represent key gatekeepers for suicide prevention. In the United States, older adults, African Americans, and Hispanic Americans, in particular, more often turn to clergy than to professional mental health services when facing mental health issues, including suicide (Husaini and Moore, 1994; Starrett et al., 1992; Weaver and Koenig, 1996). Data from a large nationally representative study indicate that clergy see individuals with the same severity of mental disorders as do mental health professionals (Larson et al., 1988). Another study suggests that those who first go to clergy with mental health complaints are least likely to seek professional mental health services (Neighbors et al., 1998). A high percentage of clergy in Australia reported that they had been approached by suicidal adolescents (Leane and Shute, 1998). Studies in the United States document that older adults often seek help from clergy for suicidal crises, as well (Domino, 1985; Weaver and Koenig, 1996).
The few studies conducted on clergy knowledge and attitudes regarding suicide suggest that many clergy members need and desire training in assessing suicide risk (Domino, 1985; Leane and Shute, 1998). Although many congregations forge formal collaborations with professional mental health services (e.g., Thomas et al., 1994), Mannon and Crawford (1996) found that clergy from small congregations or from more conservative backgrounds are less likely to refer individuals to professional mental health services. They also reported that many clergy feel less confident about providing support and advice about severe mental disorders than about other matters. However, the African American ministers in their sample reported high levels of confidence even about handling serious mental disorders among their parishioners. Given the positive effects on mental health and suicidality of religious involvement and complementary faith-based treatment (e.g., Donahue, 1995; including seeking help from clergy, Koenig et al., 1998; Propst et al., 1992, see Chapter 6) and the widespread use of clergy, many comprehensive suicide prevention programs incorporate faith-based interventions into their strategies (see Chapter 8). Some researchers have also authored articles and handbooks delineating appropriate responses to suicidal and distressed elderly and youths for clergy (e.g., Koenig and Weaver, 1997; Weaver, 1993; Weaver et al., 1999).
To maximize treatment effectiveness and to reach under-served groups, collaborations of mental health professionals with culturally relevant providers, including spiritual ministers could be effective (Marsella and Yamada, 2000; Weaver, 1993). In recognition of the importance of cultural context, the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) (APA, 1994) provides guidelines for a culturological assessment of individuals presenting with mental disorders and includes mention of cultural variations in the expression of psychopathology. Nursing diagnoses have included spiritual distress and spiritual well-being for years (Johnson et al., 2001). The framework for culturally and spiritually sensitive approaches to treating and reducing mental disorders and suicidality is emerging.
FINDINGS
-
Assessment tools are inadequate to determine acute suicide risk or to predict when a person will attempt or complete suicide. Assessment tools must be validated for various populations since they may not be generally applicable. Despite the limitations, tools for detection or risk assessment can be an important component of treatment when used appropriately.
The development of accurate measures for assessing acute suicide risk would likely enhance prevention efforts. Given the accuracy of certain measures in predicting lifetime risk for suicide, identified individuals should be referred for support and/or treatment.
-
Large epidemiological studies demonstrate reductions in suicide rates with increased antidepressant use. Randomized, controlled trials of the effects of these anti-depressants on suicide have largely failed to reveal significant differences versus placebo, perhaps due to methodological limitations.
-
Compelling evidence suggests that lithium maintenance treatment reduces suicide in certain populations. Evidence is mounting that clozapine treatment reduces suicide in specific populations, as well.
Important questions regarding lithium still remain. Controlled studies are needed to confirm the effectiveness of lithium and to define the factors (e.g., timing, dose, diagnosis) that influence it.
-
Despite manifest anxiety and agitation often marking acute suicide risk, the effects of anti-anxiety drugs on suicidality remains largely unknown. Likewise, the literature contains virtually no new and only non-randomized, uncontrolled studies regarding the potentially effective treatment modality of electroconvulsive therapy.
Carefully designed trials are necessary to understand the potential of pharmacotherapies to reduce suicidal behavior. Studies should include the antidepressants, lithium, clozapine, anti-anxiety drugs, as well as electroconvulsive therapy. The lack of long-term assessment of therapeutic strategies and the exclusion of high-risk patients from clinical trials represent critical gaps in the field.
-
Medicine alone is not sufficient for treatment of suicidality, nor are treatments equally effective across individuals and diagnoses. Psychotherapy provides a necessary therapeutic relationship that reduces the risk of suicide. Cognitive-behavioral approaches that include problem-solving training seem to reduce suicidal ideation and attempts more effectively than treatment as usual or supportive therapy. As with drug therapy, research on the long-term effectiveness of these interventions is lacking.
Controlled clinical trials are necessary to determine the types and aspects of psychotherapy that are effective in reducing suicide for diverse individuals. Current evidence suggests that continued contact with a psychotherapist is critical. This needs to be rigorously evaluated.
-
Suicide is far more likely to occur in the first month after discharge from a psychiatric hospital than subsequently; low treatment adherence poses a major risk for suicidal individuals. Long-term follow-up care of discharged suicidal individuals holds promise for reducing suicide. For example, a psychosocial intervention that effectively reduced completed suicides entailed regularly mailing letters to those patients who refused or dropped out of follow-up care.
Further research on the peri-hospital period to assess the risk and protective effects of hospitalization, the relationships between length of stay and outcomes, and the factors post-hospital that account for the increased risk for suicide would provide critical information for suicide reduction strategies. The efficacy of different approaches to follow-up care in reducing suicide across populations must also be established, and successful interventions should be replicated and widely disseminated.
-
Efficacy studies of both psychopharmacological and psychosocial interventions demonstrate that suicidality often either fails to remit or returns even when symptoms of a mental disorder decrease due to treatment. The most effective psychopharmacological and psychosocial treatment strategies generally involve long-term and/or maintenance treatment. Maintenance treatment with lithium, clozapine, and electroconvulsive therapy, during which patients must regularly see health care professionals, appears more effective in reducing suicidality than only prophylactic treatments; regular contact with health care staff via mail and weeks or months of psychotherapy also appear to reduce suicide.
Longitudinal research is needed to assess outcomes of prophylactic/short-term versus maintenance/long-term treatment for suicidality. The course of suicidality across the life span suggests it may at times represent a life-long condition requiring sustained treatment; further life-course research is required to verify this.
REFERENCES
AACAP (American Academy of Child and Adolescent Psychiatry). 2001. Summary of the practice parameters for the assessment and treatment of children and adolescents with suicidal behavior. Journal of the American Academy of Child and Adolescent Psychiatry, 40(4): 495-499.
AHCPR (Agency for Health Care Policy and Research). 1993. Clinical Practice Guideline 5. Depression in Primary Care: Volume 2. Treatment of Major Depression. AHCPR publication 93-0551. Rockville, MD: United States Department of Health and Human Services, Agency for Health Care Policy and Research.
Aoun S. 1999. Deliberate self-harm in rural Western Australia: Results of an intervention study. Australian and New Zealand Journal of Mental Health Nursing, 8(2): 65-73.
APA (American Psychiatric Association Task Force on ECT). 1990. The Practice of ECT: Recommendations for Treatment, Training and Privileging. Washington, DC: American Psychiatric Association.
APA (American Psychiatric Association). 1994. The Diagnostic and Statistical Manual of Mental Disorders. 4th ed. Washington, DC.
Appleby L. 2000. Prevention of suicide in psychiatric patients. In: Hawton K, van Heeringen K, Editors. The International Handbook of Suicide and Attempted Suicide. (pp. 617-630). Chichester, UK: John Wiley and Sons.
Appleby L, Dennehy JA, Thomas CS, Faragher EB, Lewis G. 1999a. Aftercare and clinical characteristics of people with mental illness who commit suicide: A case-control study. Lancet, 353(9162): 1397-1400.
Appleby L, Shaw J, Amos T, McDonnell R, Harris C, McCann K, Kiernan K, Davies S, Bickley H, Parsons R. 1999b. Suicide within 12 months of contact with mental health services: National clinical survey. British Medical Journal, 318(7193): 1235-1239.
Apter A, Horesh N, Gothelf D, Graffi H, Lepkifker E. 2001. Relationship between self-disclosure and serious suicidal behavior. Comprehensive Psychiatry, 42(1): 70-75.
Avery D, Winokur G. 1977. The efficacy of electroconvulsive therapy and antidepressants in depression. Biological Psychiatry, 12(4): 507-523.
Baldessarini RJ, Tondo L. 1999. Antisuicidal effect of lithium treatment in major mood disorders. In: Jacobs DG, Editor. The Harvard Medical School Guide to Suicide Assessment and Intervention. (pp. 355-371). San Francisco: Jossey-Bass Publishers.
Baldessarini RJ, Tondo L, Hennen J. 1999. Effects of lithium treatment and its discontinuation on suicidal behavior in bipolar manic-depressive disorders. Journal of Clinical Psychiatry, 60(Suppl 2): 77-84.
Barbui C, Campomori A, D’Avanzo B, Negri E, Garattini S. 1999. Antidepressant drug use in Italy since the introduction of SSRIs: National trends, regional differences and impact on suicide rates. Social Psychiatry and Psychiatric Epidemiology, 34(3): 152-156.
Beasley CM Jr, Dornseif BE, Bosomworth JC, Sayler ME, Rampey AH Jr, Heiligenstein JH, Thompson VL, Murphy DJ, Masica DN. 1991. Fluoxetine and suicide: A meta-analysis of controlled trials of treatment for depression. British Medical Journal, 303(6804): 685-692.
Bech P, Olsen LR, Niméus A. 2001. Psychometric scales in suicide assessment. In: Wasserman D, Editor. Suicide: An Unnecessary Death. (pp. 147-157). London: Martin Dunitz.
Beck AT, Kovacs M, Weissman A. 1979. Assessment of suicidal intention: The Scale for Suicide Ideation. Journal of Consulting and Clinical Psychology, 47(2): 343-352.
Berman AL, Jobes DA. 1991. Adolescent Suicide: Assessment and Intervention. Washington, DC: American Psychological Association.
Blazer DG, Hybels CF, Simonsick EM, Hanlon JT. 2000. Marked differences in antidepressant use by race in an elderly community sample: 1986–1996. American Journal of Psychiatry, 157(7): 1089-1094.
Bowden CL. 2000. Efficacy of lithium in mania and maintenance therapy of bipolar disorder. Journal of Clinical Psychiatry, 61: 35-40.
Bowden CL, Lecrubier Y, Bauer M, Goodwin G, Greil W, Sachs G, Von Knorring L. 2000. Maintenance therapies for classic and other forms of bipolar disorder. Journal of Affective Disorders, 59: S57-S67.
Brent DA, Holder D, Kolko D, Birmaher B, Baugher M, Roth C, Iyengar S, Johnson BA. 1997. A clinical psychotherapy trial for adolescent depression comparing cognitive, family, and supportive therapy. Archives of General Psychiatry, 54(9): 877-885.
Brodersen A, Licht RW, Vestergaard P, Olesen AV, Mortensen PB. 2000. Sixteen-year mortality in patients with affective disorder commenced on lithium. British Journal of Psychiatry, 176: 429-433.
Brown GK. 2000. A Review of Suicide Assessment Measures for Intervention Research With Adults and Older Adults. Technical report submitted to NIMH under Contract No. 263-MH914950. Bethesda, MD: National Institute of Mental Health.
Brown GK, Beck AT, Steer RA, Grisham JR. 2000. Risk factors for suicide in psychiatric outpatients: A 20-year prospective study. Journal of Consulting and Clinical Psychology, 68(3): 371-377.
Byford S, Harrington R, Torgerson D, Kerfoot M, Dyer E, Harrington V, Woodham A, Gill J, McNiven F. 1999. Cost-effectiveness analysis of a home-based social work intervention for children and adolescents who have deliberately poisoned themselves. Results of a randomised controlled trial. British Journal of Psychiatry, 174: 56-62.
Calabrese JR, Rapport DJ, Shelton MD, Kimmel SE. 2001a. Evolving methodologies in bipolar disorder maintenance research. British Journal of Psychiatry. Supplement, 41: S157-S163.
Calabrese JR, Shelton MD, Bowden CL, Rapport DJ, Suppes T, Shirley ER, Kimmel SE, Caban SJ. 2001b. Bipolar rapid cycling: Focus on depression as its hallmark. Journal of Clinical Psychiatry, 62 (Suppl 14): 34-41.
Chan DW. 1995. Reasons for living among Chinese adolescents in Hong Kong. Suicide and Life-Threatening Behavior, 25(3): 347-357.
Chowdhury N, Hicks RC, Kreitman N. 1973. Evaluation of an after-care service for parasuicide (attempted suicide) patients. Social Psychiatry, 8(2): 67-81.
Conwell Y, Duberstein PR, Cox C, Herrmann JH, Forbes NT, Caine ED. 1996. Relationships of age and axis I diagnoses in victims of completed suicide: A psychological autopsy study. American Journal of Psychiatry, 153(8): 1001-1008.
Crammer JL. 1984. The special characteristics of suicide in hospital in-patients. British Journal of Psychiatry, 145: 460-463.
Danish University Antidepressant Group. 1993. Moclobemide: A reversible MAO-A-inhibitor showing weaker antidepressant effect than clomipramine in a controlled multicenter study. Journal of Affective Disorders, 28(2): 105-116.
Dhossche DM, Ulusarac A, Syed W. 2001. A retrospective study of general hospital patients who commit suicide shortly after being discharged from the hospital. Archives of Internal Medicine, 161(7): 991-994.
Domino G. 1985. Clergy’s attitudes toward suicide and recognition of suicide lethality. Death Studies, 9(3-4): 187-199.
Donahue MJ. 1995. Religion and the well-being of adolescents. Journal of Social Issues, 51(2): 145-160.
Eberhard G, von Knorring L, Nilsson HL, Sundequist U, Bjorling G, Linder H, Svard KO, Tysk L. 1988. A double-blind randomized study of clomipramine versus maprotiline in patients with idiopathic pain syndromes. Neuropsychobiology, 19(1): 25-34.
Evans K, Tyrer P, Catalan J, Schmidt U, Davidson K, Dent J, Tata P, Thornton S, Barber J, Thompson S. 1999. Manual-assisted cognitive-behavior therapy (MACT): A randomized controlled trial of a brief intervention with bibliotherapy in the treatment of recurrent deliberate self-harm. Psychological Medicine, 29: 19-25.
Fawcett J, Clark DC, Scheftner WA. 1991. The assessment and management of the suicidal patient. Psychiatric Medicine, 9(2): 299-311.
Fink M, Sackeim HA. 1996. Convulsive therapy in schizophrenia? Schizophrenia Bulletin, 22(1): 27-39.
Foa EB, Keane TM, Friedman MJ, Editors. 2000. Effective Treatments for PTSD: Practice Guidelines From the International Society for Traumatic Stress Studies. New York: The Guilford Press.
Friedman RS. 1989. Hospital treatment of the suicidal patient. In: Jacobs DG, Brown HP, Editors. Suicide: Understanding and Responding. (pp. 379-402). Madison, CT: International Universities Press.
Gibbons JS, Butler J, Urwin P, Gibbons JL. 1978. Evaluation of a social work service for self-poisoning patients. British Journal of Psychiatry, 133: 111-118.
Goldacre M, Seagroatt V, Hawton K. 1993. Suicide after discharge from psychiatric inpatient care. Lancet, 342(8866): 283-286.
Goldstein RB, Black DW, Nasrallah A, Winokur G. 1991. The prediction of suicide. Sensitivity, specificity, and predictive value of a multivariate model applied to suicide among 1906 patients with affective disorders. Archives of General Psychiatry, 48(5): 418-422.
Goldston DB. 2000. Assessment of Suicidal Behaviors and Risk Among Children and Adolescents. Technical report submitted to NIMH under Contract No. 263-MD-909995. Bethesda, MD: National Institute of Mental Health.
Goldston DB, Daniel SS, Reboussin BA, Reboussin DM, Frazier PH, Harris AE. 2001. Cognitive risk factors and suicide attempts among formerly hospitalized adolescents: A prospective naturalistic study. Journal of the American Academy of Child and Adolescent Psychiatry, 40(1): 91-99.
Gonella G, Baignoli G, Ecari U. 1990. Fluvoxamine and imipramine in the treatment of depressive patients: A double-blind controlled study. Current Medical Research and Opinion, 12(3): 177-184.
Goodwin FK, Ghaemi SN. 2000. The impact of mood stabilizers on suicide in bipolar disorder: A comparative study. CNS Spectrum 5 , 2(Supplement 1): 12-18.
Goodwin FK, Jamison KR. 1990. Manic-Depressive Illness. New York: Oxford University Press.
Goodwin GM. 1999. Prophylaxis of bipolar disorder: How and who should we treat in the long term? European Neuropsychopharmacology, 9: S125-S129.
Greil W, Ludwig-Mayerhofer W, Erazo N, Engel RR, Czernik A, Giedke H, Muller-Oerlinghausen B, Osterheider M, Rudolf GA, Sauer H, Tegeler J, Wetterling T. 1996. Comparative efficacy of lithium and amitriptyline in the maintenance treatment of recurrent unipolar depression: A randomised study. Journal of Affective Disorders, 40(3): 179-190.
Greil W, Ludwig-Mayerhofer W, Erazo N, Engel RR, Czernik A, Giedke H, Muller-Oerlinghausen B, Osterheider M, Rudolf GA, Sauer H, Tegeler J, Wetterling T. 1997a. Lithium vs carbamazepine in the maintenance treatment of schizoaffective disorder: A randomised study . European Archives of Psychiatry and Clinical Neuroscience, 247(1): 42-50.
Greil W, Ludwig-Mayerhofer W, Erazo N, Schochlin C, Schmidt S, Engel RR, Czernik A, Giedke H, Muller-Oerlinghausen B, Osterheider M, Rudolf GA, Sauer H, Tegeler J, Wetterling T. 1997b. Lithium versus carbamazepine in the maintenance treatment of bipolar disorders—A randomised study. Journal of Affective Disorders, 43(2): 151-161.
Guthrie E, Kapur N, Mackway-Jones K, Chew-Graham C, Moorey J, Mendel E, Marino-Francis F, Sanderson S, Turpin C, Boddy G, Tomenson B. 2001. Randomised controlled trial of brief psychological intervention after deliberate self poisoning. British Medical Journal, 323(7305): 135-138.
Harrington R, Kerfoot M, Dyer E, McNiven F, Gill J, Harrington V, Woodham A, Byford S. 1998. Randomized trial of a home-based family intervention for children who have deliberately poisoned themselves . Journal of the American Academy of Child and Adolescent Psychiatry, 37(5): 512-518.
Harris EC, Barraclough B. 1997. Suicide as an outcome for mental disorders. A meta-analysis. British Journal of Psychiatry, 170: 205-228.
Hawton K, Arensman E, Townsend E, Bremner S, Feldman E, Goldney R, Gunnell D, Hazell P, van Heeringen K, House A, Owens D, Sakinofsky I, Träskman-Bendz L. 1998. Deliberate self harm: Systematic review of efficacy of psychosocial and pharmacological treatments in preventing repetition. British Medical Journal, 317(7156): 441-447.
Hawton K, Bancroft J, Catalan J, Kingston B, Stedeford A, Welch N. 1981. Domiciliary and out-patient treatment of self-poisoning patients by medical and non-medical staff. Psychological Medicine, 11(1): 169-177.
Hawton K, McKeown S, Day A, Martin P, O’Connor M, Yule J. 1987. Evaluation of outpatient counselling compared with general practitioner care following overdoses. Psychological Medicine, 17(3): 751-761.
Healy D, Langmaak C, Savage M. 1999. Suicide in the course of the treatment of depression. Journal of Psychopharmacology, 13(1): 94-99.
Henriksson S, Boethius G, Isacsson G. 2001. Suicides are seldom prescribed antidepressants: Findings from a prospective prescription database in Jamtland county, Sweden, 1985-95. Acta Psychiatrica Scandinavica, 103(4): 301-306.
Hirschfeld RM. 2000. Suicide and antidepressant treatment. Archives of General Psychiatry, 57(4): 325-326.
Hsu SI. 1999. Somatisation among Asian refugees and immigrants as a culturally-shaped illness behaviour. Annals of the Academy of Medicine, Singapore, 28(6): 841-845.
Hung CI, Liu CY, Liao MN, Chang YH, Yang YY, Yeh EK. 2000. Self-destructive acts occurring during medical general hospitalization. General Hospital Psychiatry, 22(2): 115-121.
Husaini BA, Moore ST. 1994. Psychiatric symptoms and help-seeking behavior among the elderly: An analysis of racial and gender differences. Journal of Gerontological Social Work, 21(3): 177-195.
Inman W, Kubota K, Pearce G, Wilton L. 1993. PEM report number 6: Paroxetine. Pharmacoepidemiology and Drug Safety, 2: 393-422.
IOM (Institute of Medicine). 2001. Health and Behavior: The Interplay of Biological, Behavioral, and Societal Influences. Washington, DC: National Academy Press.
Isacsson G. 2000. Suicide prevention—a medical breakthrough? Acta Psychiatrica Scandinavica, 102(2): 113-117.
Isacsson G, Bergman U, Rich CL. 1994. Antidepressants, depression and suicide: An analysis of the San Diego study. Journal of Affective Disorders, 32(4): 277-286.
Isacsson G, Bergman U, Rich CL. 1996. Epidemiological data suggest antidepressants reduce suicide risk among depressives. Journal of Affective Disorders, 41: 1-8.
Isacsson G, Boethius G, Bergman U. 1992. Low level of antidepressant prescription for people who later commit suicide: 15 years of experience from a population-based drug database in Sweden. Acta Psychiatrica Scandinavica, 85(6): 444-448.
Isacsson G, Holmgren P, Druid H, Bergman U. 1997. The utilization of antidepressants—a key issue in the prevention of suicide: An analysis of 5281 suicides in Sweden during the period 1992-1994. Acta Psychiatrica Scandinavica, 96(2): 94-100.
Isacsson G, Holmgren P, Druid H, Bergman U. 1999. Psychotropics and suicide prevention. Implications from toxicological screening of 5281 suicides in Sweden 1992-1994. British Journal of Psychiatry, 174: 259-265.
Isacsson G, Holmgren P, Wasserman D, Bergman U. 1994. Use of antidepressants among people committing suicide in Sweden. British Medical Journal, 308(6927): 506-509.
Isometsa ET, Henriksson MM, Aro HM, Heikkinen ME, Kuoppasalmi KI, Lönnqvist JK. 1994. Suicide in major depression. American Journal of Psychiatry, 151(4): 530-536.
Jacobson G. 1999. The inpatient management of suicidality. In: Jacobs DG, Editor. The Harvard Medical School Guide to Suicide Assessment and Intervention. (pp. 383-405). San Francisco, CA: Jossey-Bass Publishers.
Jamison KR. 1995. An Unquiet Mind: A Memoir of Moods and Madness. New York: A.A. Knopf.
Jamison KR, Akiskal HS. 1983. Medication compliance in patients with bipolar disorder. Psychiatric Clinics of North America, 6(1): 175-192.
Jamison KR, Gerner RH, Goodwin FK. 1979. Patient and physician attitudes toward lithium: Relationship to compliance. Archives of General Psychiatry, 36: 866-869.
Johnson M, Bulecheck G, McCloskey Dochterman J, Maas M, Moorhead S, Editors. 2001. Nursing Diagnoses, Outcomes, and Interventions: NANDA, NOC, and NIC Linkages. St. Louis, MO: Mosby.
Joiner TEJr, Voelz ZR, Rudd MD. 2001. For suicidal young adults with comorbid depressive and anxiety disorders, probem-solving treatment may be better than treatment as usual. Professional Psychology—Research & Practice, 32(3): 278-282.
Judd FK, Moore K, Norman TR, Burrows GD, Gupta RK, Parker G. 1993. A multicentre double blind trial of fluoxetine versus amitriptyline in the treatment of depressive illness . Australian and New Zealand Journal of Psychiatry, 27(1): 49-55.
Kasper S, Moller HJ, Montgomery SA, Zondag E. 1995. Antidepressant efficacy in relation to item analysis and severity of depression: A placebo-controlled trial of fluvoxamine versus imipramine. International Clinical Psychopharmacology, 9 (Suppl 4): 3-12.
Keller MB, Lavori PW, Klerman GL, Andreasen NC, Endicott J, Coryell W, Fawcett J, Rice JP, Hirschfeld RM. 1986. Low levels and lack of predictors of somatotherapy and psychotherapy received by depressed patients. Archives of General Psychiatry, 43(5): 458-466.
Khan A, Khan SR, Leventhal RM, Brown WA. 2001. Symptom reduction and suicide risk in patients treated with placebo in antidepressant clinical trials: A replication analysis of the Food and Drug Administration Database. International Journal of Neuropsychopharmacology, 4(2): 113-118.
Khan A, Warner HA, Brown WA. 2000. Symptom reduction and suicide risk in patients treated with placebo in antidepressant clinical trials: An analysis of the Food and Drug Administration database. Archives of General Psychiatry, 57(4): 311-317.
King EA, Baldwin DS, Sinclair JM, Baker NG, Campbell MJ, Thompson C. 2001. The Wessex Recent In-Patient Suicide Study, 1. Case-control study of 234 recently discharged psychiatric patient suicides. British Journal of Psychiatry, 178: 531-536.
Koenig HG, Pargament KI, Nielsen J. 1998. Religious coping and health status in medically ill hospitalized older adults. Journal of Nervous and Mental Disease, 186(9): 513-521.
Koenig HG, Weaver AJ. 1997. Counseling Troubled Older Adults: A Handbook for Pastors and Religious Caregivers. Nashville, TN: Abingdon Press.
Koivumaa-Honkanen H, Honkanen R, Viinamaki H, Heikkila K, Kaprio J, Koskenvuo M. 2001. Life satisfaction and suicide: A 20-year follow-up study. American Journal of Psychiatry, 158(3): 433-439.
Koons CR, Robins CJ, Tweed JL, Lynch TR, Gonzalez AM, Morse JQ, Bishop GK, Butterfield MI, Bastian LA. 2001. Efficacy of dialectical behavior therapy in women veterans with borderline personality disorder. Behavior Therapy, 32(2): 371-390.
Kotin J, Post RM, Goodwin FK. 1973. Drug treatment of depressed patients referred for hospitalization. American Journal of Psychiatry, 130(10): 1139-1141.
Lapierre YD. 1991. Controlling acute episodes of depression. International Clinical Psychopharmacology, 6 (Suppl 2): 23-35.
Larson DB, Hohmann AA, Kessler LG, Meador KG, Boyd JH, McSherry E. 1988. The couch and the cloth: The need for linkage. Hospital and Community Psychiatry, 39(10): 1064-1069.
Lawrenson RA, Tyrer F, Newson RB, Farmer RD. 2000. The treatment of depression in UK general practice: Selective serotonin reuptake inhibitors and tricyclic antidepressants compared. Journal of Affective Disorders, 59(2): 149-157.
Leane W, Shute R. 1998. Youth suicide: The knowledge and attitudes of Australian teachers and clergy. Suicide and Life-Threatening Behavior, 28(2): 165-173.
Leon AC, Keller MB, Warshaw MG, Mueller TI, Solomon DA, Coryell W, Endicott J. 1999. Prospective study of fluoxetine treatment and suicidal behavior in affectively ill subjects. American Journal of Psychiatry, 156(2): 195-201.
Lerner MS, Clum GA. 1990. Treatment of suicide ideators: A problem-solving approach. Behavior Therapy, 21(4): 403-411.
Letizia C, Kapik B, Flanders WD. 1996. Suicidal risk during controlled clinical investigations of fluvoxamine. Journal of Clinical Psychiatry, 57(9): 415-421.
Liberman RP, Eckman T. 1981. Behavior therapy vs insight-oriented therapy for repeated suicide attempters. Archives of General Psychiatry, 38(10): 1126-1130.
Linehan MM. 1997. Behavioral treatments of suicidal behaviors. Definitional obfuscation and treatment outcomes. Annals of the New York Academy of Sciences, 836: 302-328.
Linehan MM, Armstrong HE, Suarez A, Allmon D, Heard HL. 1991. Cognitive-behavioral treatment of chronically parasuicidal borderline patients. Archives of General Psychiatry, 48(12): 1060-1064.
Linehan MM, Goodstein JL, Nielsen SL, Chiles JA. 1983. Reasons for staying alive when you are thinking of killing yourself: The reasons for living inventory. Journal of Consulting and Clinical Psychology, 51(2): 276-286.
Litman RE, Wold C. 1975. Beyond crisis intervention. In: Shneidman E, Editor. Suicidology: Contemporary Developments. (pp. 528-546). New York: Grune & Stratton.
MacKinnon DR, Farberow NL. 1976. An assessment of the utility of suicide prediction. Suicide and Life-Threatening Behavior, 6(2): 86-91.
Macqueen GM, Young LT. 2001. Bipolar II disorder: Symptoms, course, and response to treatment. Psychiatric Services, 52(3): 358-361.
Mahapatra SN, Hackett D. 1997. A randomised, double-blind, parallel-group comparison of venlafaxine and dothiepin in geriatric patients with major depression. International Journal of Clinical Practice, 51(4): 209-213.
Mann JJ, Goodwin FK, O’Brien CP, Robinson DS. 1993. Suicidal behavior and psychotropic medication. Accepted as a consensus statement by the ACNP Council, March 2, 1992. Neuropsychopharmacology, 8(2): 177-183.
Mann JJ, Kapur S. 1991. The emergence of suicidal ideation and behavior during antidepressant pharmacotherapy. Archives of General Psychiatry, 48(11): 1027-1033.
Mannon JD, Crawford RL. 1996. Clergy confidence to counsel and their willingness to refer to mental health professionals. Family Therapy, 23(3): 213-231.
Marchesi C, Ceccherininelli A, Rossi A, Maggini C. 1998. Is anxious-agitated major depression responsive to fluoxetine? A double-blind comparison with amitriptyline. Pharmacopsychiatry, 31(6): 216-221.
Markowitz JC. 2001. Antidepressants and suicide risk. British Journal of Psychiatry, 178: 477.
Marsella AJ. 1988. Cross-cultural research on severe mental disorders: Issues and findings. Acta Psychiatrica Scandinavica. Supplement, 344: 7-22.
Marsella AJ, Sanborn KO, Kameoka V, Shizuru L, Brennan J. 1975. Cross-validation of self-report measures of depression among normal populations of Japanese, Chinese, and Caucasian ancestry. Journal of Clinical Psychology, 31(2): 281-287.
Marsella AJ, Yamada A. 2000. Culture and mental health: An introduction and overview of foundations, concepts, and issues. In: Cuellar I, Paniagua FA, Editors. Handbook of Multicultural Mental Health: Assessment and Treatment of Diverse Populations. (pp. 3-24). San Diego, CA: Academic Press.
Marzuk PM, Tardiff K, Leon AC, Hirsch CS, Stajic M, Hartwell N, Portera L. 1995. Use of prescription psychotropic drugs among suicide victims in New York City. American Journal of Psychiatry, 152(10): 1520-1522.
McKenzie W, Wurr C. 2001. Early suicide following discharge from a psychiatric hospital. Suicide and Life-Threatening Behavior, 31(3): 358-363.
McLeavey BC, Daly RJ, Ludgate JW, Murray CM. 1994. Interpersonal problem-solving skills training in the treatment of self-poisoning patients. Suicide and Life-Threatening Behavior, 24(4): 382-394.
Meehl PE, Rosen A. 1955. Antecedent probability and the efficiency of psychometric signs, patterns, or cutting scores. Psychological Bulletin, 52: 194-216.
Melander A, Henricson K, Stenberg P, Lowenhielm P, Malmvik J, Sternebring B, Kaij L, Bergdahl U. 1991. Anxiolytic-hypnotic drugs: Relationships between prescribing, abuse and suicide. European Journal of Clinical Pharmacology, 41(6): 525-529.
Meltzer HY. 1999. Suicide and schizophrenia: Clozapine and the InterSePT study. International Clozaril/Leponex Suicide Prevention Trial. Journal of Clinical Psychiatry, 60 (Suppl 12): 47-50.
Meltzer HY, Alphs L, Altamura C, Kerwin R, Chouinard G, Green A, Lindenmayer JP, Potkin S, Islam Z, Kane J, Krishnan R, Anand R. 2001. Effect of Clozapine on the Reduction of Suicidality in Schizophrenia and Schizoaffetive Disorder. Abstract # 175 at the annual meeting of the American College of Neuropsychopharmacology in Kona, Hawaii, December 2001.
Meltzer HY, Okayli G. 1995. Reduction of suicidality during clozapine treatment of neuroleptic-resistant schizophrenia: Impact on risk-benefit assessment. American Journal of Psychiatry, 152(2): 183-190.
Metzger ED. 1999. ECT and suicide. In: Jacobs DG, Editor. The Harvard Medical School Guide to Suicide Assessment and Intervention. (pp. 406-413). San Francisco, CA: Jossey-Bass Publishers.
Miller AL, Rathus JH, Linehan MM, Wetzler S, Leigh E. 1997. Dialectical behavior therapy adapted for suicidal adolescents. Journal of Practical Psychiatry and Behavioral Health, 3(2): 78-86.
Modestin J, Schwarzenbach FA, Wurmle O. 1992. Therapy factors in treating severely ill psychiatric patients. British Journal of Medical Psychology, 65 (Pt 2): 147-156.
Möller HJ. 1989. Efficacy of different strategies of aftercare for patients who have attempted suicide. Journal of the Royal Society of Medicine 82: 643-647.
Möller HJ. 2001. Pharmacological treatment of underlying psychiatric disorders in suicidal patients. In: Wasserman D, Editor. Suicide: An Unnecessary Death. (pp. 173-178). London: Martin Dunitz.
Möller HJ, Steinmeyer EM. 1994. Are serotonergic reuptake inhibitors more potent in reducing suicidality? An empirical study on paroxetine. European Neuropsychopharmacology, 4(1): 55-59.
Montgomery DB, Roberts A, Green M, Bullock T, Baldwin D, Montgomery SA. 1994. Lack of efficacy of fluoxetine in recurrent brief depression and suicidal attempts. European Archives of Psychiatry and Clinical Neuroscience, 244(4): 211-215.
Montgomery S, Cronholm B, Asberg M, Montgomery DB. 1978. Differential effects on suicidal ideation of mianserin, maprotiline and amitriptyline. British Journal of Clinical Pharmacology, 5 (Suppl 1): S77-S80.
Montgomery SA, Dunner DL, Dunbar GC. 1995. Reduction of suicidal thoughts with paroxetine in comparison with reference antidepressants and placebo. European Neuropsychopharmacology, 5(1): 5-13.
Montgomery SA, Schatzberg AF, Guelfi JD, Kasper S, Nemeroff C, Swann A, Zajecka J. 2000. Pharmacotherapy of depression and mixed states in bipolar disorder. Journal of Affective Disorders, 59: S39-S56.
Morrison LL, Downey DL. 2000. Racial differences in self-disclosure of suicidal ideation and reasons for living: Implications for training. Cultural Diversity and Ethnic Minority Psychology, 6(4): 374-386.
Motto JA, Bostrom AG. 2001. A randomized controlled trial of postcrisis suicide prevention. Psychiatric Services, 52(6): 828-833.
Mukherjee S, Sackeim HA, Schnur DB. 1994. Electroconvulsive therapy of acute manic episodes: A review of 50 years’ experience. American Journal of Psychiatry, 151(2): 169-176.
Müller-Oerlinghausen B, Berghofer A. 1999. Antidepressants and suicidal risk. Journal of Clinical Psychiatry, 60(Suppl 2): 94-99.
Negron R, Piacentini J, Graae F, Davies M, Shaffer D. 1997. Microanalysis of adolescent suicide attempters and ideators during the acute suicidal episode. Journal of the American Academy of Child and Adolescent Psychiatry, 36(11): 1512-1519.
Neighbors HW, Musick MA, Williams DR. 1998. The African American minister as a source of help for serious personal crises: Bridge or barrier to mental health care? Health Education and Behavior, 25(6): 759-777.
Neutel CI, Patten SB. 1997. Risk of suicide attempts after benzodiazepine and/or antidepressant use. Annals of Epidemiology, 7(8): 568-574.
O’Hagan M. 2001, August 23. Man sought help, then killed self. The Washington Post. H3
Ohberg A, Vuori E, Klaukka T, Lonnqvist J. 1998. Antidepressants and suicide mortality. Journal of Affective Disorders, 50(2-3): 225-233.
Ohberg A, Vuori E, Ojanpera I, Lonnqvist J. 1996. Alcohol and drugs in suicides. British Journal of Psychiatry, 169(1): 75-80.
Oquendo MA, Malone KM, Ellis SP, Sackeim HA, Mann JJ. 1999. Inadequacy of antidepressant treatment for patients with major depression who are at risk for suicidal behavior. American Journal of Psychiatry, 156(2): 190-194.
Osman A, Downs WR, Kopper BA, Barrios FX, Baker MT, Osman JR, Besett TM, Linehan MM. 1998. The Reasons for Living Inventory for Adolescents (RFL-A): Development and psychometric properties. Journal of Clinical Psychology, 54(8): 1063-1078.
Patsiokas AT, Clum GA. 1985. Effects of psychotherapeutic strategies in the treatment of suicide attempters. Psychotherapy, 22(2): 281-290.
Philibert RA, Richards L, Lynch CF, Winokur G. 1995. Effect of ECT on mortality and clinical outcome in geriatric unipolar depression. Journal of Clinical Psychiatry, 56(9): 390-394.
Pokorny AD. 1983. Prediction of suicide in psychiatric patients. Report of a prospective study. Archives of General Psychiatry, 40(3): 249-257.
Propst LR, Ostrom R, Watkins P, Dean T, Mashburn D. 1992. Comparative efficacy of religious and nonreligious cognitive-behavioral therapy for the treatment of clinical depression in religious individuals. Journal of Consulting and Clinical Psychology, 60(1): 94-103.
Prudic J, Sackeim HA. 1999. Electroconvulsive therapy and suicide risk. Journal of Clinical Psychiatry, 60(Suppl 2): 104-110.
Prudic J, Sackeim HA, Devanand DP. 1990. Medication resistance and clinical response to electroconvulsive therapy. Psychiatry Research, 31(3): 287-296.
Reid WH, Mason M, Hogan T. 1998. Suicide prevention effects associated with clozapine therapy in schizophrenia and schizoaffective disorder. Psychiatric Services, 49(8): 1029-1033.
Rich CL. 1999. Relationship between antidepressant treatment and suicide. Journal of Clinical Psychiatry, 60(5): 340.
Rich CL, Isacsson G. 1997. Suicide and antidepressants in south Alabama: Evidence for improved treatment of depression. Journal of Affective Disorders, 45(3): 135-142.
Rihmer Z, Belso N, Kalmar S. 2001. Antidepressants and suicide prevention in Hungary. Acta Psychiatrica Scandinavica, 103(3): 238-239.
Rihmer Z, Rutz W, Pihlgren. 1995. Depression and suicide on Gotland: An intensive study of all suicides before and after a depression-training programme for general practitioners. Journal of Affective Disorders, 35: 147-152.
Rihmer Z, Rutz W, Pihlgren H, Pestality P. 1998. Decreasing tendency of seasonality in suicide may indicate lowering rate of depressive suicides in the population. Psychiatry Research, 81(2): 233-240.
Robins E, Murphy GE, Wilkinson RHJr, Gassner S, Kayes J. 1959. Some clinical considerations in the prevention of suicide based on a study of 134 successful suicides. American Journal of Public Health, 49: 888-899.
Roose SP, Nobler M. 2001. ECT and onset of action. Journal of Clinical Psychiatry, 62 (Suppl 4): 24-26; discussion 37-40.
Rotheram-Borus MJ, Piacentini J, Cantwell C, Belin TR, Song J. 2000. The 18-month impact of an emergency room intervention for adolescent female suicide attempters. Journal of Consulting and Clinical Psychology, 68(6): 1081-1093.
Rotheram-Borus MJ, Piacentini J, Van Rossem R, Graae F, Cantwell C, Castro-Blanco D, Feldman J. 1999. Treatment adherence among Latina female adolescent suicide attempters. Suicide and Life-Threatening Behavior, 29(4): 319-331.
Rotheram-Borus MJ, Piacentini J, Van Rossem R, Graae F, Cantwell C, Castro-Blanco D, Miller S, Feldman J. 1996. Enhancing treatment adherence with a specialized emergency room program for adolescent suicide attempters. Journal of the American Academy of Child and Adolescent Psychiatry, 35(5): 654-663.
Rothschild AJ, Locke CA. 1991. Reexposure to fluoxetine after serious suicide attempts by three patients: The role of akathisia. Journal of Clinical Psychiatry, 52(12): 491-493.
Rouillon F, Phillips R, Serrurier D, Ansart E, Gerard MJ. 1989. Recurrence of unipolar depression and efficacy of maprotiline. L’Encephale, 15(6): 527-534.
Roy A, Draper R. 1995. Suicide among psychiatric hospital in-patients. Psychological Medicine, 25(1): 199-202.
Rudd MD, Rajab MH, Orman DT, Joiner T, Stulman DA, Dixon W. 1996. Effectiveness of an outpatient problem-solving intervention targeting suicidal young adults: Preliminary results. Journal of Consulting and Clinical Psychology, 64(1): 179-190.
Rutz W. 2001. Preventing suicide and premature death by education and treatment. Journal of Affective Disorders, 62(1-2): 123-129.
Rutz W, von Knorring L, Walinder J. 1989a. Frequency of suicide on Gotland after systematic postgraduate education of general practitioners. Acta Psychiatrica Scandinavica, 80(2): 151-154.
Rutz W, Walinder J, Eberhard G, Holmberg G, von Knorring AL, von Knorring L, Wistedt B, Aberg-Wistedt A. 1989b. An educational program on depressive disorders for general practitioners on Gotland: Background and evaluation. Acta Psychiatrica Scandinavica, 79(1): 19-26.
Salkovskis PM, Atha C, Storer D. 1990. Cognitive-behavioural problem solving in the treatment of patients who repeatedly attempt suicide. A controlled trial. British Journal of Psychiatry, 157: 871-876.
Sclar DA, Robinson LM, Skaer TL, Galin RS. 1998. Trends in the prescribing of antidepressant pharmacotherapy: Office-based visits, 1990–1995. Clinical Therapeutics, 20(4): 871-884; 870.
Sexton TL, Whiston SC. 1991. A review of the empirical basis for counseling: Implications for practice and training. Counselor Education and Supervision, 30(4): 330-354.
Sheehan D, Dunbar GC, Fuell DL. 1992. The effect of paroxetine on anxiety and agitation associated with depression. Psychopharmacology Bulletin, 28(2): 139-143.
Soloff PH, George A, Nathan RS, Schulz PM, Perel JM. 1986. Paradoxical effects of amitriptyline on borderline patients. American Journal of Psychiatry, 143(12): 1603-1605.
Starrett RA, Rogers D, Decker JT. 1992. The self-reliance behavior of the Hispanic elderly in comparison to their use of formal mental health helping networks. Clinical Gerontologist, 11(3-4): 157-169.
Taiminen TJ. 1993. Effect of psychopharmacotherapy on suicide risk in psychiatric inpatients. Acta Psychiatrica Scandinavica, 87(1): 45-47.
Teicher MH, Glod C, Cole JO. 1990. Emergence of intense suicidal preoccupation during fluoxetine treatment. American Journal of Psychiatry, 147(2): 207-210.
Termansen PE, Bywater C. 1975. S.A.F.E.R.: A follow-up service for attempted suicide in Vancouver. Canadian Psychiatric Association Journal, 20(1): 29-34.
Thies-Flechtner K, Muller-Oerlinghausen B, Seibert W, Walther A, Greil W. 1996. Effect of prophylactic treatment on suicide risk in patients with major affective disorders. Data from a randomized prospective trial. Pharmacopsychiatry, 29(3): 103-107.
Thomas SB, Quinn SC, Billingsley A, Caldwell C. 1994. The characteristics of northern black churches with community health outreach programs. American Journal of Public Health, 84(4): 575-579.
Tollefson GD, Fawcett J, Winokur G, Beasley CM, Potvin JH, Faries DE, Rampey AH, Sayler ME. 1993. Evaluation of suicidality during pharmacologic treatment of mood and nonmood disorders. Annals of Clinical Psychiatry, 5(4): 209-224.
Tondo L, Baldessarini RJ. 2000. Reduced suicide risk during lithium maintenance treatment. Journal of Clinical Psychiatry, 61 (Suppl 9): 97-104.
Tondo L, Baldessarini RJ, Hennen J, Floris G, Silvetti F, Tohen M. 1998. Lithium treatment and risk of suicidal behavior in bipolar disorder patients. Journal of Clinical Psychiatry, 59(8): 405-414.
Tondo L, Hennen J, Baldessarini RJ. 2001. Lower suicide risk with long-term lithium treatment in major affective illness: A meta-analysis. Acta Psychiatrica Scandinavica, 104(3): 163-172.
Tondo L, Jamison KR, Baldessarini RJ. 1997. Effect of lithium maintenance on suicidal behavior in major mood disorders. Annals of the New York Academy of Sciences, 836: 339-351.
US DHHS (U.S. Department of Health and Human Services). 2001. Mental Health: Culture, Race and Ethnicity—A Supplement to Mental Health: A Report of the Surgeon General. Rockville, MD: U.S. Department of Health and Human Services, Substance Abuse and Mental Health Services Administration, Center for Mental Health Services, National Institutes of Health, National Institute of Mental Health.
van der Sande R, Buskens E, Allart E, van der Graaf Y, van Engeland H. 1997a. Psychosocial intervention following suicide attempt: A systematic review of treatment interventions. Acta Psychiatrica Scandinavica, 96(1): 43-50.
van der Sande R, van Rooijen L, Buskens E, Allart E, Hawton K, van der Graaf Y, van Engeland H. 1997b. Intensive in-patient and community intervention versus routine care after attempted suicide. A randomised controlled intervention study. British Journal of Psychiatry, 171: 35-41.
van Heeringen C, Jannes S, Buylaert W, Henderick H, De Bacquer D, Van Remoortel J. 1995. The management of non-compliance with referral to out-patient after-care among attempted suicide patient: A controlled intervention study. Psychological Medicine, 25(5): 963-970.
Verkes RJ, Van der Mast RC, Hengeveld MW, Tuyl JP, Zwinderman AH, Van Kempen GM. 1998. Reduction by paroxetine of suicidal behavior in patients with repeated suicide attempts but not major depression. American Journal of Psychiatry, 155(4): 543-547.
Vestergaard P, Licht RW, Brodersen A, Rasmussen N-A, Christensen H, Arngrim T, Gronvall B, Kristensen E, Poulstrup I. 1998. Outcome of lithium prophylaxis: A prospective follow-up of affective disorder patients assigned to high and low serum lithium levels. Acta Psychiatrica Scandinavica, 98(4): 310-315.
Walker AM, Lanza LL, Arellano F, Rothman KJ. 1997. Mortality in current and former users of clozapine . Epidemiology, 8(6): 671-677.
Waterhouse J, Platt S. 1990. General hospital admission in the management of parasuicide. A randomised controlled trial. British Journal of Psychiatry, 156: 236-242.
Weaver AJ. 1993. Suicide prevention: What clergy need to know. Journal of Psychology and Christianity, 12(1): 70-79.
Weaver AJ, Koenig HG. 1996. Elderly suicide, mental health professionals, and the clergy: A need for clinical collaboration, training, and research. Death Studies, 20(5): 495-508.
Weaver AJ, Preston JD, Jerome LW. 1999. Counseling Troubled Teens and Their Familes: A Handbook for Pastors and Youth Workers. Nashville, TN: Abingdon Press.
Weeke A. 1979. Causes of death in manic-depressives. In: Schou M, Strömgren E, Editors. Origin, Prevention and Treatment of Affective Disorders. (pp. 289-299). London: Academic Press.
Welu TC. 1977. A follow-up program for suicide attempters: Evaluation of effectiveness. Suicide and Life-Threatening Behavior, 7(1): 17-20.
Wheadon DE, Rampey AH Jr, Thompson VL, Potvin JH, Masica DN, Beasley CM Jr. 1992. Lack of association between fluoxetine and suicidality in bulimia nervosa. Journal of Clinical Psychiatry, 53(7): 235-241.
Zaninelli R, Meister W. 1999. The treatment of depression with paroxetine in psychiatric practice in Germany: The possibilities and current limitations of drug monitoring. Pharmacopsychiatry, 30: 9-20.
And Levin, a happy father and a man in perfect health, was several times so near suicide that he hid the cord, lest he be tempted to hang himself, and was afraid to go out with his gun, for fear of shooting himself. But Levin did not shoot himself, and did not hang himself; he went on living.
—LEO TOLSTOY
Anna Karenina












































