8
Programs for Suicide Prevention
Over the last 15–20 years, the first two generations of suicide prevention efforts have yielded valuable information on risk and protective factors, empirically based methods for preventing suicidal behavior, and improved research methods (Berman and Jobes, 1995; PHS, 2001). During this time, the following developments have been observed in the area of suicide prevention (1) a proliferation of curriculum-based suicide prevention programs in schools (cf., Garland et al., 1989) accompanied by increased attention and concerns voiced over format, goals, theoretic orientation, and safety issues (Hazell and King, 1996) that led to improved methods and prevention program designs (cf., Breton et al., 1998; Kalafat and Ryerson, 1999; Orbach and Bar-Joseph, 1993); (2) increased efforts to undertake empirical research on suicide prevention, prompted by a 1990 US Congressional mandate, and accompanied by the rapid development of suicidology as a multidisciplinary subspecialty with national and international professional organizations, new journals, and the establishment of centers for the study and prevention of suicide (PHS, 1999; 2001); (3) a new precisely defined prevention framework that places prevention programs on a continuum of universal, selective, and indicated interventions (Gordon, 1987; IOM, 1994); (4) the emergence of research on suicide prevention programs designed to target higher risk populations (e.g., Eggert et al., 1995b; Thompson et al., 2001); (5) improved screening tools and measures of suicide and suicidal behaviors (e.g., Eggert et al., 1994; Pfeffer et al., 2000; Reynolds, 1991; Reynolds, 1998; Shaffer and Craft, 1999; Thompson and Eggert, 1999), and (6) key advances in research methods,
including improved analytic tools and sophisticated models for measuring change over time in prevention trials (Brown and Liao, 1999).
In contrast to clinical approaches that explore the history and health conditions leading to suicide in the individual, the public health approach to suicide prevention focuses on identifying broader patterns of suicide and suicidal behavior throughout a group or population. The public health approach to suicide prevention is also reflected in an organized five-step process that has been developed for ensuring the effectiveness of preventive efforts (PHS, 2001:11). This chapter will describe the current public health preventive framework and then review some of the interventions for preventing suicide at each level. The focus will be primarily on school-based programs. As with all other behavioral interventions, the best effects are most likely to be achieved with multidimensional interventions (IOM, 2001), given the overlapping nature of risk and protective factors across domains of influence. The chapter then explores examples of programs targeting specific populations and concludes with an analysis of an integrated approach for reducing the incidence of suicide in the broad population.
FRAMEWORK FOR PREVENTION
The prevailing prevention model in the interdisciplinary field of prevention science is the Universal, Selective, and Indicated (USI) prevention model. This USI model focuses attention on defined populations—from everyone in the population, to specific at-risk groups, to specific high-risk individuals—i.e., three population groups for whom the designed interventions are deemed optimal for achieving the unique goals of each prevention type.
Universal strategies or initiatives address an entire population (the nation, state, local county or community, school or neighborhood). These prevention programs are designed to influence everyone, reducing suicide risk though removing barriers to care, enhancing knowledge of what to do and say to help suicidal individuals, increasing access to help, and strengthening protective processes like social support and coping skills. Universal interventions include programs such as public education campaigns, school-based “suicide awareness” programs, means restriction, education programs for the media on reporting practices related to suicide, and school-based crisis response plans and teams.
Selective strategies address subsets of the total population, focusing on at-risk groups that have a greater probability of becoming suicidal. Selective prevention strategies aim to prevent the onset of suicidal behaviors among specific subpopulations. This level of prevention includes screening programs, gatekeeper training for “frontline” adult caregivers
and peer “natural helpers,” support and skill building groups for at-risk groups in the population, and enhanced accessible crisis services and referral sources.
Indicated strategies address specific high-risk individuals within the population—those evidencing early signs of suicide potential. Programs are designed and delivered in groups or individually to reduce risk factors and increase protective factors. At this level, programs include skill-building support groups in high schools and colleges, parent support training programs, case management for individual high-risk youth at school, and referral sources for crisis intervention and treatment.
UNIVERSAL PREVENTIONS
Using health promotion strategies to combat symptoms of mental illness, including suicidality, represents a primary aspect of many universal suicide prevention programs. Although the field has traditionally separated health promotion from prevention (IOM, 1994), preventionists in the United States and abroad have increasingly turned to mental health promotion as a means of universal prevention (Beautrais, 1998; Cowen, 1994; Durlak, 2000; Waring et al., 2000). Reviews (Cowen, 1994; NRC, 2002) and at least one meta-analysis (Durlak, 2000) demonstrate that school-based programs employing such a health promotion approach can effectively prevent and/or reduce suicide risk factors and correlates like adolescent pregnancy, externalizing disorders (such as delinquency and substance abuse), and depression. These programs also promote protective factors against suicide including: self-efficacy, interpersonal problem solving, self esteem, and social support (see Chapters 3 and 6). Furthermore, throughout the 1990s, the World Health Organization developed evidence-based policies and recommendations for how schools can effectively engage in health promotion using a four-level model (see, WHO, 2002). The WHO model promotes universal prevention, targeting environmental conditions and mental health education for all students, as well as selective and indicated prevention, providing psychosocial interventions and professional treatment for those with mental illness or at significant risk (see also Waring et al., 2000; WHO, 1999; 2000a). As mentioned in Chapter 3, the U.S. Surgeon General (PHS, 2001), the United Nations (1996), and the World Health Organization (1999) have endorsed promoting mental health/resiliency as part of universal suicide reduction strategies.
Population-based prevention programs with a school or community focus have an important advantage over those aimed at individuals. There is usually a high participation rate in such programs because all students are exposed, for instance, to a teacher’s classroom management practices
and control of aggressive behavior (Kellam et al., 1998) or to a middle school drug prevention program (Botvin et al., 1995). These programs also have the advantage, because of inoculation, of having potential impact on not only those who are currently at risk, but also those whose risk status changes after the intervention takes place. Finally, many of these broad prevention programs target multiple outcomes, so overall risk for suicide may be reduced by diminishing developmental risk through multiple pathways.
Policy changes represent another universal strategy for reducing suicide. For example, Birckmayer and Hemenway (1999) conclude in their review of minimum drinking age policies in each state from 1970 to 1990 that increases in the legal drinking age reduce not only motor vehicle deaths but also suicides.
Media Campaigns
A traditional universal public health approach to behavior-related problems has been widespread education through mass-media campaigns. This technique has been used with varying levels of success for smoking, AIDS, and coronary heart disease (see IOM, 2002). A few countries, including the United Kingdom and Norway, have implemented such mass-media campaigns for suicide prevention as part of overall mental health promotion; evaluations of results are not yet available. Extensive media campaigns for suicide prevention are not common, largely due to fear of engendering suicide imitation. Media initiatives more often have focussed on modifying portrayals of suicide to reduce the likelihood of imitation. Since data are limited on use of media for education, this section discusses what is known about suicide imitation through the media, followed by a description of efforts to address this problem and the evidence for their effectiveness.
The Evidence for Imitation
Throughout history, people have expressed concern about suicide imitation, and have seen the opportunity for intervention in such matters, as evidenced by various anecdotal accounts in the literature of suicide imitation and clustering. For example, Goethe’s 1774 novel The Sorrows of Young Werther, in which the title character shoots himself after a failed love affair, was banned in Denmark, Saxony, and Milan in order to prevent further suicides that were thought to be a result of young men imitating the behavior of Werther (Phillips, 1974, 1985). These events led to the term the “Werther Effect” being used to describe imitation of this sort.
Today this effect is referred to as either suicide contagion or suicide imitation/modeling. Although they are often used interchangeably, each is based on a different theoretical framework. Each theoretical framework is useful, but Schmidtke and Schaller (2000) propose that the language of imitation and modeling is preferable to the language of a contagious process because it relies on active learning processes that do not imply the exclusion of individual volitional factors.
Imitation and modeling, which play a role in other harmful behaviors such as drug use and bullying, occur with suicide in several circumstances, such as in the case of temporal clusters of suicides in a particular community or culture (see Chapter 2), suicide among family members (see Chapter 5), and suicide following exposure to a media1 presentation of a real or fictional suicide.
Research shows that suicide contagion through the media is real (for review, see Gould, 2001a; 2001b). Recent meta-analyses report that studies conducted by clinically oriented investigators yield the strongest support for suicide imitation (cited in Schmidtke and Schaller, 2000). However, many of the studies of suicide imitation are beset with methodological problems; for example, many are based on aggregate-level data, which preclude the possibility of ruling out the influence of other factors.
Imitation can be linked to newspaper accounts of suicide (for review, see Gould, 2001b; Hassan, 1995; Phillips, 1974; Stack, 1996). Newspaper coverage of suicide is related to an increase in the rate of suicide, and the magnitude of the increase is proportional to the duration, prominence and amount of media coverage (Gould, 2001a). There has been less conclusive research on the consequences of television news programs on suicide imitation. Kessler et al. (1988; 1989) found no association over an 11 year period in the United States, but recent studies suggest imitation in specific groups (e.g., in the elderly, see Stack, 1990).
The influence of fictional presentations of suicide on imitation is less clear. Research into fictional portrayals has examined attempts or other suicidal behavior (such as ideation) rather than just rates of completed suicides, which allows for actual measurement of exposure. Some studies indicate that imitation occurs (e.g., Gould et al., 1988; Hawton et al., 1999); others do not (e.g., Phillips and Paight, 1987); still others are inconclusive (Berman, 1988).
Aspects of both the media presentation and the individual interact to produce imitation. The person who is likely to imitate a suicidal behavior
has underlying vulnerabilities. A healthy person is not likely to kill him-or herself as a result of seeing an example of suicide. Different media (e.g., book vs. television) are likely to exert differential effects on different populations. Both the form (headline, placement) and content (celebrity, mental illness, murder-suicide) of suicide coverage clearly impact the likelihood of imitation. Attractive models are more likely to cause imitation.
Similarities between a vulnerable person and the reported suicide victim increase the likelihood of contagion. This has been shown with age effects in both the young (Phillips and Carstensen, 1988) and the elderly (Stack, 1999, cited in Schmidtke and Schaller, 2000). Similarly, ethnicity is an important factor; Stack (1996) found that suicides of foreigners did not cause imitation among native populations.
Encouraging Responsible Coverage of Suicide
Many elements of media presentations influence the likelihood of imitation, and these all provide opportunities for prevention. In efforts to prevent contagion, several countries (including Australia, Austria, Canada, Germany, Japan, New Zealand, and Switzerland) and organizations, including the World Health Organization (United Nations, 1996; WHO, 2000b) have formulated guidelines for media coverage of suicide.
The National Strategy for Suicide Prevention in the United States includes as one of its major goals improving “the reporting and portrayals of suicidal behavior, mental illness, and substance abuse in the entertainment and news media” (PHS, 2001). To advance that goal, guidelines for media coverage of suicide were formulated by the Annenberg Public Policy Center of the University of Pennsylvania, the American Association of Suicidology (AAS) and the American Foundation for Suicide Prevention (AFSP) in collaboration with several government agencies (CDC, NIMH, Office of the Surgeon General, Substance Abuse and Mental Health Services Administration [SAMSHA]), the WHO, and other international suicide prevention groups. They were released in August 2001, and the full text of these guidelines can be found on the sites of the partner organizations that developed them, including www.appcpenn.org and www.afsp.org. These guidelines, “Reporting on Suicide: Recommendations for the Media” update those developed in 1989 at a national consensus conference on the topic.
The media guidelines include the stipulation that media accounts of suicide should neither romanticize nor normalize suicide; that is, individuals who kill themselves should not inadvertently be idealized as heroic or romantic. They also urge the inclusion of factual information on suicide contagion and mental illness, provide suggestions for questions to ask of relatives and friends of the victim, and suggest that information on
treatment resources be included. The guidelines also address issues of language such as the use of terms like “a successful suicide,” and speak to special situations that may arise such as a celebrity death by suicide. Finally, they suggest that media professionals address suicide as an issue in its own right, reporting on stigma, treatments, and trends in suicide rates, rather than only in response to a tragedy (AFSP, 2001). With shifts in focus and inclusion of educational material, the same articles that report on an unfortunate event can become part of universal preventive measures. This echoes other areas in the injury prevention field (Hemenway, 2001). The media now indicate the status of smoke detectors when a fire is reported, for example. Likewise, helmet use is indicated when reporting a bicycle accident.
Currently, many comprehensive suicide prevention programs include components to improve media response to suicide, including the Finland National Program, Maryland (see later in this chapter) and the Washington State Youth Suicide Prevention Program (Eggert et al., 1997), with the state programs often utilizing the nationally formulated guidelines. The Washington program included a media education component that was designed to impact reporting practices by (1) educating media personnel in ways to report youth suicide stories that prevent potential contagion effects and (2) educating select personnel such as crisis line workers, gatekeepers, and school personnel in how to respond to media requests for information and stories related to youth suicide and suicide prevention. It also focused on ensuring that the youth suicide prevention message was “in the news” by providing information to the media and encouraging ongoing and responsible coverage of suicide and suicide prevention.
Despite such efforts to shape discussion of suicide in the media, very little evidence exists to show that initiatives to promote responsible reporting in the media have a direct, significant effect on suicide rates. In Switzerland, implementation of media guidelines did increase responsible reporting of suicides; less sensational and higher quality stories resulted (Michel et al., 2000). But this has not yet been related to changes in suicide rates. An evaluation of media guidelines in Austria showed significant success in reducing suicides. The guidelines in that country were specifically formulated to address concerns that the increase in the number of suicides and suicide attempts on the subway in Vienna was related to the highly publicized and dramatic accounts of the deaths. Subsequent to the release of the guidelines, newspaper reporting of subway suicides decreased greatly and what was reported was much less prominent. The number of subway suicides significantly decreased in the second half of the year after release. In the 4 years following, the overall suicide rate decreased by 20 percent and the rate of subway suicides decreased by 75
percent with no substitution of method (Etzersdorfer and Sonneck, 1998; Etzersdorfer et al., 1992; Sonneck et al., 1994).
Reducing Access to Means
Universal measures can be used to reduce the availability of common tools for suicide. More restrictive legislation regarding firearms, barriers on bridges, or blister packs for medications are interventions that may be effective in reducing suicide or suicide attempts. This section focuses on the role of availability of methods of suicide, including the role that method availability and barrier restrictions may play in suicide by firearms, acetaminophen overdose, prescription drugs, jumping from buildings or bridges, domestic gas, automobile carbon monoxide, and railway suicides. Much of the research discussed has been done in Western societies, but suicide in rural Asian societies has been largely linked with availability of insecticides (Van der Hoek et al., 1998; Yip et al., 2000). Research is limited, but this underscores the need for implementing safe storage of agricultural poisons and using safety caps to reduce impulsive swallowing.
Firearms2
Epidemiological studies have consistently shown that firearms are most common method of suicide for all demographic groups in the United States (CDC, 1994). The association between suicide and firearms in the home is strong across all age groups, but is particularly high in the 24 and younger group (Odds Ratios3 [ORs] of 10.4 vs. 4.0–7.2 for those 25 and older) (Kellermann et al., 1992). The dramatic increase in the American youth suicide rate since 1960 is primarily attributable to an increase in suicide by firearms (see Figure 8-1a,b; Boyd, 1983; Boyd and Moscicki, 1986). In one study of youth suicide in Allegheny County from 1960–1983, the rate of suicide by firearms increased 330 percent, but the rate of suicide by other means increased only 150 percent (Brent et al., 1987b). The more recent increase in the suicide rate by African American males is also attributable primarily to an increase in suicide by firearms.
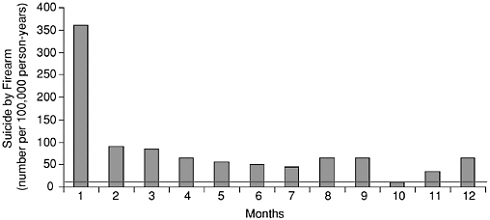
FIGURE 8-1a Rates of suicide by firearm in the first year after purchase among persons who purchased handguns in California in 1991. The horizontal line indicates the age- and sex-adjusted average annual rate of suicide by firearm in California in 1991 and 1992 (11.3 per 100,000 persons per year). SOURCE: Wintemute et al. 1999. Copyright © 1999 Massachusetts Medical Society. All rights reserved.
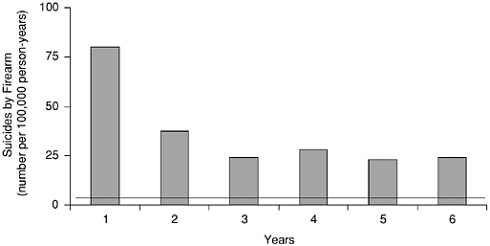
FIGURE 8-1b Rates of suicide by firearm during the six years after purchase among persons who purchased handguns in California in 1991. The horizontal line indicates the age- and sex-adjusted average annual rate of suicide by firearm in California in 1991 through 1996 (10.7 per 100,000 persons per year). SOURCE: Wintemute et al. 1999. Copyright © 1999 Massachusetts Medical Society. All rights reserved.
|
Ray, age 14, had made three suicide attempts prior to completing his suicide. Each time there had been someone there to stop him. He communicated often about his intent, remarking that “Life’s a bitch” and asking others about which way they thought it would be better to kill oneself. The day before his death, he asked his mother whether it would be better to stick a gun “in your mouth or in your temple?” He chose the latter, using a .357 Magnum that had been kept fully loaded, in his mother’s nightstand (Berman & Jobes, Adolescent Suicide: Assessment and Intervention, 1991:189). |
Alcohol and illicit drug abuse in the home greatly increase the risk of violent death, including suicide (Rivara et al., 1997). Youth who were drinking at the time of their suicide were much more likely to use a gun than were youth who were not drinking (Brent et al., 1987b; Brent et al., 1993; Hlady and Middaugh, 1988). The increase in youth alcohol abuse and in firearms availability over the past 3 decades may be related to the increase in youth suicide in general, and in youth firearms suicide in specific. However, it is important to note that youth suicide has also dramatically increased in geographic regions where firearms ownership and firearms suicides are relatively rare (e.g., New Zealand; Beautrais et al., 1996). Therefore, it would be an oversimplification to say that the increase in youth suicide, in the United States, or anywhere else in the world, is solely a function of increased firearms availability.
Several studies (Beautrais et al., 1996; Brent et al., 1991; Brent et al., 1988; Kellermann et al., 1992) have demonstrated that the presence of a gun in the home is highly predictive of its use for completed suicide (see Table 8-1). Firearms were between 31.1 and 107.9 times more likely to be used for the suicide if a gun was already in the home. This was even true in New Zealand, where firearms is a much less common method choice
TABLE 8-1 Case-Control Studies: Guns in the Home and the Method of Suicide
|
|
Brent 1993 |
Kellerman 1992 |
Beautrais 1996 |
|
Use of gun if kept in home |
87.8% |
88% |
33% |
|
Use of gun if not kept in home |
18.8% |
6% |
0.5% |
|
Guns in home and firearms as method (Odds Ratio [OR]) |
31.1 |
69.5 |
107.9 |
|
Firearms and alcohol use (OR [95%CI]) |
7.3 |
— |
— |
|
Bought gun within two weeks of suicide |
— |
3% |
— |
for suicide than in the United States (14 percent vs. 55–60 percent, Beautrais et al., 1996). Conversely, if a gun was not in the home, it was used as a method of suicide quite infrequently. Furthermore, in a study by Kellermann et al. (1992), only 3 percent of those who completed suicide had bought a gun within 2 weeks of the suicide. Wintemute et al. (1999) examined the standardized mortality rates (SMRs) of purchasers of handguns in California, who are registered by state law, and found an extremely high rate of suicide right after purchase. However, the rates remained elevated for the 6 years of analysis. This suggests that firearms are purchased for the purpose of completing suicide even though most of the suicides occurred some time after the purchase. Together, these data strongly suggest that it is the immediate gun availability that conveys the risk for firearms suicide, and supports method restriction as one means to prevent firearms suicide.
Method of storage and the type and number of guns modify suicide risk substantially. Higher risk is associated with handguns than with long guns, loaded guns than unloaded guns, and unlocked than locked guns (see Table 8-2, Brent et al., 1993; Kellermann et al., 1992). Long guns convey an increased risk to males, but not females, and handguns convey a particularly increased risk for females (Brent et al., 1993). Furthermore, in adolescents, long guns, but not handguns, convey an increased risk in rural areas (OR’s 4.5 vs. 1.0), while in urban areas, this situation is re-
TABLE 8-2 Risk of Suicide in the Home in Relation to Various Patterns of Gun Ownership
|
Variable |
Adjusted Odds Ratioa |
95% Confidence Interval |
|
Type of guns in the home |
||
|
One or more handguns |
5.8 |
3.1–4.7 |
|
Long guns only |
3.0 |
1.4–6.5 |
|
No guns in the home |
1.0 |
— |
|
Loaded guns |
||
|
Any gun kept loaded |
9.2 |
4.1–20.1 |
|
All guns kept unloaded |
3.3 |
1.7–6.1 |
|
No guns in the home |
1.0 |
— |
|
Locked guns |
||
|
Any guns kept unlocked |
5.6 |
3.1–10.4 |
|
All guns kept locked up |
2.4 |
1.0–5.7 |
|
No guns in the home |
1.0 |
— |
|
SOURCE: Kellermann et al., 1992. Copyright © 1992 Massachusetts Medical Society. All rights reserved. |
||
versed, with handguns conveying a much higher risk than long guns (OR’s 5.6 vs. 1.3) (Brent et al., 1993).
While firearms counseling has gained acceptance as an important component of health supervision, in reality this often fails to occur (Grossman et al., 1995). Depressed adolescent patients and their parents are often non-compliant with physician recommendations to secure or remove firearms (Weil and Hemenway, 1992). Only two studies have examined the impact of firearms counseling on the removal of firearms with the parents of youth at risk for suicide. In one study, eight parents of suicide attempters with firearms in the home were counseled about the danger conveyed by firearms in the home, and five either removed the gun, or stored the gun in a more secure manner (Kruesi et al., 1999). In a study of depressed adolescents who entered a randomized psychotherapy clinical trial, only 27 percent of parents who reported having guns in the home at intake removed the guns on follow-up after being urged by the clinician to do so (Brent et al., 2000). Therefore, it is unwise to assume that providing recommendations on removal of firearms from the home will automatically result in compliance. An alternative recommendation to improve the security of gun storage is often more favorably received (Webster et al., 1992).
The firearms suicide rate and the overall suicide rate are related to the strictness of gun control laws and the prevalence of gun ownership (Boor and Bair, 1990; Killias, 1993; Lester, 1988; Lester and Murrell, 1986). Quasi-experimental studies suggest that greater restrictiveness in gun control laws is associated with declines in firearms suicide, sometimes without compensatory method substitution (Loftin et al., 1991). In a particularly elegant cross-country comparison, the suicide rates were compared in two similar cities, Seattle and Vancouver. Because gun control is more restrictive in Canada, it was assumed suicide rates in Vancouver would be lower (Sloan et al., 1990). Instead, the overall suicide rates were similar in the two cities, albeit with a 10-fold higher rate of firearms suicides in Seattle. This was almost entirely reflected in 40 percent higher rate of suicide among 15–24 year olds in Seattle. These results suggest that the greater availability of firearms is particularly deleterious for younger people.
In a well-designed quasi-experimental study, Loftin et al. (1991) examined the relationship between legislation enacted in 1976 in the District of Columbia and subsequent time trends in suicide and homicide during the years 1968 through 1987. This legislation mandated the registration of all firearms, required that new purchasers meet “fitness” and knowledge of safety standards, and necessitated that owners store guns unloaded and disassembled, with certain occupational exceptions, such as law enforcement. The unusual aspect of this study was that changes in the rates
of suicide and homicide in the District of Columbia were compared to changes in rates of suicide and homicide in neighboring Maryland and Virginia counties, where no such change in firearms legislation had taken place. In the District of Columbia, subsequent to the enactment of this legislation, a 23 percent decline in firearms suicide and a 9 percent decline in non-firearms suicide were noted. Over the same period of time, in the adjoining Maryland and Virginia counties, a 12 percent increase in firearms suicide and a 2 percent decline in non-firearms suicide were observed. One weakness of all ecological studies is that it is impossible to monitor the extent to which these regulations were enforced or circumvented. However, one might have expected diffusion of unlawful firearms from neighboring counties into the District of Columbia, which would have diluted the potentially salutary impact of the legislation. The inference of a causal relationship between the change in legislation and the decline in suicide is bolstered by the greater effect on firearms vs. non-firearms suicide and the geographic specificity of this effect. Method substitution did not occur to any substantial degree, and an overall decline in the suicide rate prevailed. The impact of the Brady Act has been controversial. Although Ludwig and Cook (2000) found a significant reduction in suicide rates following enactment, their breakdown by age and their choice of duration of analysis may be problematic (Kleck and Marvell, 2000; Lott, 2000). Given the complexity of gun availability and fluctuations of these relatively infrequent events over time, a final judgement on the effectiveness of this legislation in reducing suicide is unlikely to happen soon.
The impact of firearms legislation on suicide was examined in Queensland, Australia (Cantor and Slater, 1995). The law required both current and prospective owners of long guns to obtain a license. A 28-day waiting period (“cooling off period”) was instituted prior to a new purchase, and owners were required to pass a safety test. The suicide rate by firearms declined among men in metropolitan areas and in provincial cities, but not in rural areas. This effect was most notable among individuals under the age of 30. However, method substitution occurred in all regions but the provincial cities, where overall suicide rates did decline. Two limitations of the study are the absence of a “control” community where no change in legislation had occurred and the brevity of the observation (only 1 year pre- and post-legislation).
Acetaminophen Overdose
The rate of acetaminophen (or paracetamol) self-poisoning from emergency room registries has been estimated 21.4/100,000 in one American emergency room, and as high as 70–90/100,0000 in one study based in
Scotland (Bond and Hite, 1999; McLoone and Crombie, 1996). In the Scottish study, the rates among male and female adolescents aged 15–19 were approximate 150 and 350/100,000, respectively (McLoone and Crombie, 1996). Hospitalizations due to acetaminophen rose rapidly from the 1970s through the early 1900s, especially in adolescents and young adults (McLoone and Crombie, 1996). This increase is explained in part by the increased availability of acetaminophen. High correlations have been noted between sales of acetaminophen and overdose rates in Oxford, England (r=.86) and in France (r=.99), with similar correlations between sales and completed suicide (Gunnell et al., 1997). In addition to availability, adolescents’ general ignorance about the risk for hepatotoxicity appears to contribute to the use of acetaminophen. Almost half of adolescents underestimate the potential lethality and toxicity of acetaminophen (Harris and Myers, 1997; Myers et al., 1992). Awareness is also limited that ingestion of acetaminophen in combination with alcohol greatly increases the likelihood of both hospitalization and of hepatotoxicity (Schiodt et al., 1997).
Restriction of drug content per purchase and the use of blister packs (requiring individual pill removal from a card with each pill in its own “bubble”) may reduce the morbidity and mortality due to acetaminophen overdose (Chan, 1996; Hawton et al., 1996). Restriction in the amount of drug available in a purchase resulted in a 4-fold lower fatality from overdose in France, compared to England (Gunnell et al., 1997). The introduction of blister packs as a method for dispensing acetaminophen was associated with a 21 percent reduction in overdoses and a 64 percent reduction in severe overdoses, whereas overdoses due to benzodiazepines, which were not subject to these restrictions, remained stable (Turvill et al., 2000).
Some have considered the benefit of labels warning of hepatotoxicity, but it is unclear if warnings would alter the behavior of impulsive adolescents (Harris and Myers, 1997). In one survey, only 25 percent thought that a warning would deter them (Hawton et al., 1996). The addition of methionine to prevent the hepatotoxic effects has been suggested but not yet evaluated.
Prescription Drugs
The rate of self-poisoning by prescription drugs in New York City is highest in Manhattan, which has the higher per-capita density of physicians of any of the boroughs of New York (Marzuk et al., 1992). The greater number of prescribed psychotropic agents is correlated with an increased risk of overdose, at an estimated rate of 3.8/1000 prescriptions (Forster and Frost, 1985). However, Moens and van Voorde (1989) found no relationship between availability of prescription drugs and completed
suicide. The prescription of a psychotropic agent is itself a marker for suicidal risk and it is important to consider its lethality in prescribing for patients with mental disorders. Furthermore, there is a marked gradient in toxicity among antidepressants (Cassidy and Henry, 1987; Kapur et al., 1992). In a study conducted in the United Kingdom, desipramine was reported to have over twice the death rate by overdose per 1,000,000 prescriptions compared to amitriptyline, imipramine, or nortriptyline, and 9 times the death rate by overdose of mianserin (Cassidy and Henry, 1987). In data from the United States, the toxicity of different antidepressants was examined using two different databases—the Association of Poison Control Centers (APCC) and the Drug Abuse and Early Warning Network (DAWN) (Kapur et al., 1992). In the APCC database the rate of overdose was adjusted for prescription volume based on the National Prescription Audit. Both APCC and DAWN databases revealed that desipramine had a higher risk for suicide attempt and greater fatality given an overdose than either amitriptyline or imipramine. The DAWN analysis also demonstrated that the three tricyclic antidepressants had between a 2.5 and 8.5 greater risk of death due to overdose than fluoxetine. Therefore, alteration in prescription practices to favor SSRIs over TCAs might result in a decline in deaths by overdose of antidepressants.
Suicide and suicide attempt are markedly increased in patients with epilepsy (Brent, 1986; Hawton et al., 1980; Mackay, 1979; Matthews and Barabas, 1981; Sillanpaa, 1973). While interictal psychopathology related to epilepsy seems to be an important risk factor for suicidal behavior (Mendez et al., 1989), phenobarbital may be an iatrogenic cause of depression and suicidal behavior in epilepsy (Brent, 1986; Brent et al., 1990; Brent et al., 1987a; Ferrari et al., 1983). One naturalistic study suggested that exposure to phenobarbital caused about a 4-fold risk for depression, which was most likely to occur if there was a family history of depression and very unlikely to occur in the absence of a family history of depression (Brent et al., 1987a). Phenobarbital is no longer a first-line anticonvulsant in the United States, but because of its overall safety and cost, it still is used quite commonly in developing countries. Screening for a family history of depression may help to avoid the iatrogenic difficulties associated with this medication.
Jumping from Buildings or Bridges
Availability of high buildings or bridges provides another means for suicide. In New York City, suicide by jumping was highest in Manhattan, and lowest in Staten Island, the two extremes for access to buildings of 7 stories or higher (Marzuk et al., 1992). In another study in New York, 81 percent of all suicides jumped from their own residences (Fischer et al.,
1993). One report suggested the efficacy of a crisis telephone line on a bridge. Its use in 30 cases resulted in only one completed suicide. Nine people jumped from the bridge and did not use the phone; 5 of the 9 completed the suicide. The availability of the phone line, staffed by mental health experts and with an automatic police alert, may have deterred some suicides (Glatt, 1987). As with injury control approaches, the creation of mechanical barriers on bridges could make jumping more difficult or impossible. Mechanical barriers in private residences would be more difficult to develop and enforce.
Domestic Gas Poisoning
Domestic gas poisoning was one of the leading causes of suicide in Great Britain; due to its high carbon monoxide (CO) content, domestic gas could be highly lethal. A decrease in CO content of domestic gas associated with decline in mortality in Great Britain, Austria, and Japan (Kreitman, 1976; Lester and Abe, 1989), but not in the Netherlands (Sainsbury, 1986). Method substitution eventually offset this decline in suicide by the mid 1980s in Great Britain (McClure, 1984), but not Japan (Lester and Abe, 1989). Therefore, in some locales, the detoxification of domestic gas has had a lasting effect, and even in Great Britain, where method substitution did eventually take place, this occurred after a reduction in the suicide rate which lasted for a 15-year period.
Suicide by Auto Exhaust
The rate of suicide by auto exhaust is, not surprisingly, related to the availability of automobiles (Marzuk et al., 1992; Ohberg et al., 1995; Ostrom et al., 1996). Suicide by auto exhaust is much more common in Queens and Staten Island (.46 and .40 per 100,000) than in Manhattan or the Bronx (0 and .08 per 100,000, Marzuk et al., 1992). A relationship between per-capita automobile ownership and suicide by carbon monoxide poisoning was also found in Finland (Ohberg et al., 1995).
Suicide by auto exhaust is often relatively impulsive and frequently occurs under influence of alcohol (Skopek and Perkins, 1998). Several suggestions for reducing the lethality of this method have been raised: a brief computer administered screen for sobriety as a condition for starting the car; decreasing the amount of CO in exhaust through a catalytic converter; having the engine cutoff if idling for too long; and modification of the end of the exhaust tail pipe to make it impossible to put a hose on the end (Ostrom et al., 1996). In the United States detoxification of car exhaust began in 1968 (8.5 percent CO content) and continued through 1980 (0.05 percent CO content). An examination of the suicide rate by this means
between 1950 and 1984 failed to show a straightforward relationship between detoxification and suicide rates. Suicide among men by this method began to decline along with detoxification until 1979, at which point it began to rise again. A decline in female suicides by this method began in 1975 (Clarke and Lester, 1986).
Railway Suicides
The rate of railway suicide (e.g., jumping in front of a train) also is related to access. In New York, the rate of railway or subway suicide is proportional to the amount of track in a given borough (Marzuk et al., 1992). However, among cities internationally, there are marked variations in the suicide rate per passenger. Rates are extremely low in Singapore, Tokyo, Budapest, and Hong Kong but much higher in London, Barcelona, Rio de Janeiro, and Paris (O’Donnell et al., 1994).
Because the case fatality rate is high (estimated at 55 percent) and prediction is difficult, injury control methods have been suggested to reduce fatality. Suggestions include physical separation of passengers from the train bed, improved surveillance of passengers by station staff, liaison to hospital staff in stations with a high density of chronic mental patients, availability of emergency hotline telephones, redesign of bumper of train (including the addition of an airbag), increasing the distance between the train and the train bed, and a slower speed of approach to the station (Beskow et al., 1994; Clarke and Poyner, 1994). In addition to design issues, curbing media publicity about railway suicides may diminish the likelihood of imitation (Schmidtke and Hafner, 1988; Sonneck et al., 1994, see earlier section).
Hotlines and Crisis Centers
Research on the effectiveness of hotlines and crisis centers in reducing suicide is scarce, and what does exist is inconsistent. Yet the high prevalence of such services and their high usage warrants research so that the most effective services can be provided. There are over 350 Befrienders International Centers, associated with The Samaritans, in over 40 countries (see Scott, 2000), and there are over 1000 teen suicide hotlines alone in the United States as of 1992 (CDC, 1992). Hotlines and crisis intervention services include a broad scope of services including anonymous or non-anonymous phone counseling for suicidal individuals and/or their family and friends, face-to-face counseling, and referrals by professionals, paraprofessionals, and/or volunteers with various training. These services can intervene during an acute suicidal crisis and connect individuals to additional mental health services that they might not otherwise
seek. Certification is available through the American Association of Suicidology for North American phone help lines, and from the Samaritans for membership in Befrienders International, based in London, England. Yet accreditation or membership does not require formal evaluation of services, nor is monitoring of services provided (Mishara and Daigle, 2001).
Research on the effectiveness of hotlines and crisis intervention is hampered by at least two methodological problems. First, suicide is a low-base rate behavior and studies typically include those who both did and did not have contact with the services in the community. Second, suicide prevention accounts for only 5–20 percent of the services provided by many such organizations (Eastwood et al., 1976; France, 1982; Knickerbocker and McGee, 1973; Lester, 1972). Hence, the noted changes in mental health status of the community may be attributable to other aspects of the organizations’ work.
The research on hotline and crisis center effectiveness in reducing suicide shows three over-arching findings. First, the available data show either reductions (Bagley, 1968) or no change (Barraclough and Jennings, 1977; Lester, 1990) in suicide rates; no increased rates have been documented. Second, until recently young white females most frequently utilized these services (CDC, 1992; Stengel, 1964). Some studies examining suicide rates in white women 25 years and younger found significant decreases in counties with suicide prevention centers (Miller et al., 1984), but only for this demographic. Third, users of these services report high satisfaction with them and often use the services again. Numerous studies have found that about 80 percent of individuals report positive experiences with the hotlines (e.g., King, 1977; Motto, 1971; Stein and Lambert, 1984; Tekavcic-Grad and Zavasnik, 1987). These findings may be inflated due to reporting bias, since response rates to these inquiries range from 40–80 percent and may disproportionally include those who found the intervention helpful. Two researchers found that callers to hotlines may be more likely to attempt than complete suicide (Bagley, 1968), which may limit the potential usefulness of hotlines in reducing suicide rates.
Demographics of hotline use may be changing with an increase in usage by middle aged individuals (Scott, 2000). Baby-boomers are more likely than previous generations to use mental health services including hotlines, so that the demographics of highest usage may follow this cohort. Analogously, the majority of current teenagers look up health information on the Internet as their first resource (Borzekowski and Rickert, 2001a; Flowers-Coulson et al., 2000). Planning for interventions for this demographic will need to address the credibility of Internet health information (Borzekowski and Rickert, 2001).
No-Suicide Contracts
Suicide prevention contracts are widely used in all mental health settings as risk management tools, but they remain poorly evidenced. Also known as contracts for safety or no-suicide contracts, suicide prevention contracts ask the patient to make a commitment either verbally or in writing to avoid self-destructive behavior and to keep the clinician informed of any such suicidal impulses. However, there is no standardization in the form or content of the contract, nor in indications for use. Generally, no-suicide contracts are used in cases of acute suicidal thoughts, impulses, and behaviors, although chronic self-destructive behavior may also prompt the clinician to propose a contract.
There is scant evidence to support the efficacy of this widely used intervention, simply because so little evaluation has been done. One retrospective medical record study found that suicide prevention contracts did not prevent self-harm behaviors (Drew, 2001). Still, surveys of clinicians have found that suicide prevention contracts are commonly used, and that there is a general perception that they are helpful (Davidson et al., 1995; Green and Grindel, 1996).
A reason for the large variability in suicide prevention contracts as seen in practice is that they are not part of the formal, written tradition of suicide assessment. More often their use is perpetuated by word of mouth. A survey of psychiatrists and psychologists at Harvard Medical School points to the lack of formal training in the use of no-suicide contracts. Whereas 86 percent of the psychiatrists surveyed and 71 percent of the psychologists surveyed worked in places where contracts were regularly used, only 30–40 percent had received formal training or education during internship or residency concerning their use (Miller et al., 1998). This is just one element of the larger-scale problem in clinician training for treating suicidal patients, as discussed in Chapter 9. These data and other anecdotal accounts indicate that no-suicide contracts are a widely used intervention, but the precise prevalence rates of use are not known.
No-suicide contracts should never be used in place of appropriate suicide risk assessment and treatment (Miller, 1999; Simon, 1999). Refusal to sign a no-suicide contract does not necessarily indicate that the patient is in imminent danger of suicide, just as agreement to a contract does not mean that the risk of suicide and self-destructive behavior is lessened. The mental state of a patient is not static, and patients may have inconsistent and complex motivations for agreeing to or refusing a contract (Simon, 1999). A risk of using no-suicide contracts is that they may provide a false sense of security to the clinician and cause lessened diligence about the danger of suicide (Simon, 1999).
The usefulness of the suicide prevention contract may be dependent upon the strength of therapeutic relationship between the clinician and patient. In an emergency setting, for example, the patient has no investment in or commitment to the clinician, and thus, signing a contact would mean very little. In the context of a long-term therapeutic alliance, however, the commitment by the patient may carry more weight.
Additionally, the process of creating a contract can be either helpful or hurtful to the clinician–patient relationship. It may be beneficial if the process demonstrates to the patient a measure of caring and concern on the part of the clinician (Egan et al., 1997; Kroll, 2000) and may be harmful if the patient perceives that the clinician is attempting to reduce his or her own responsibility and involvement in the treatment (Miller et al., 1998). Other possible benefits of contracts include the opportunity to assess the nature of the therapeutic alliance, identify clear goals for treatment, and support coping mechanisms in some patients (Miller, 1999). Stanford and colleagues (1994) recommend that suicide prevention contracts be used as an assessment tool that can provide useful diagnostic information.
The legal implications of a no-suicide contract have been extensively explored by Simon (1999). He has concluded that the suicide prevention contract is not a legal contract and does not provide protection to the clinician in the event of a lawsuit. Alternate terminology is suggested, such as agreement, pact, or understanding (Simon, 1992). It should be recognized that suicide prevention contracts do not provide protection from lawsuits (and may have the opposite effect if it is determined that the contract took the place of a thorough assessment; Miller, 1999). As discussed in Chapter 10, suicide can be considered an expected outcome of some mental illnesses, and is very difficult to predict. Although the fear of lawsuits is understandable, the societal atmosphere that blames the clinician when a patient kills himself should not dictate clinical decisions.
In conclusion, suicide prevention contracts are likely overvalued and should never be used as the sole treatment for a patient with suicidal behavior. There is no convincing evidence to support the practice, and some evidence that points to its potential for harm with certain patients. The informed consent model proposed by Miller (1999) uses an agreement as one part of the collaboration between clinician and patient to create an ongoing treatment plan. This informed consent process involves exploring and fully explaining different treatment options and their various risks and benefits, including the risk of suicide, to the patient, and outlines the mutual commitment of the two parties to follow through with the plan. Of course, the patients’ ability to provide informed consent must be assessed (see Chapter 10).
Awareness and Skills Training
A number of studies have explored the impact on suicidality of universal prevention interventions at the middle and high school level. Suicide awareness training is the dominant strategy of these universal programs in the United States, although more schools are turning to broad-based competence-promoting programs as evidence mounts for their effectiveness in reducing the burden of behavioral and mental disorders (see introduction to universal approaches). As would be expected with a universal program assessed shortly after its completion, the changes in suicidal behaviors and related risk factors have generally been promising yet modest. Universal programming assumes a healthy population and is not necessarily designed to impact acute risk factors directly, but rather targets contextual variables, protective processes, and predisposing factors, including reducing barriers to care. It is delivered at a dose and in a format that is not generally appropriate for changing risk factors or suicidal behaviors in the short term, but rather long-term. The greatest and most sustainable changes in behavior appear to follow interventions employing the multi-dimensional approach typical of health-promoting prevention strategies, especially with skills training components embedded in an environment with trained, supportive adults.
Eleven universal suicide prevention strategies at the high school level were reviewed for this analysis of programming typical for the United States; 15 published papers were found that examine the efficacy of these programs (Ashworth et al., 1986; Ciffone, 1993; Eggert et al., 1999; Kalafat, 2000; Kalafat and Elias, 1994; Kalafat and Ryerson, 1999; Klingman and Hochdorf, 1993; Nelson, 1987; Orbach and Bar-Joseph, 1993; Overholser et al., 1989; Shaffer et al., 1991; Shaffer et al., 1990; Spirito et al., 1988; Vieland et al., 1991; Zenere and Lazarus, 1997). Typically, one individual delivered the majority of the programs to a classroom of students. The 11 programs reviewed varied from 1-to-12 sessions, and ranged in duration from 55 minutes to more than 16 hours. These programs primarily used didactic presentations that cover warning signs, provide information to dispel myths and promote healthy attitudes, and review strategies for accessing resources. Several of the programs showed gains in knowledge (Ciffone, 1993; Eggert et al., 1999; Kalafat and Elias, 1994; Klingman and Hochdorf, 1993; Nelson, 1987; Shaffer et al., 1991; Spirito et al., 1988) that seem to be enhanced when youth use this knowledge to teach others (Eggert et al., 1999).
In addition, programs that included the importance of telling adults and seeking help for self or friends (Ciffone, 1993; Eggert et al., 1999; Kalafat and Elias, 1994; Shaffer et al., 1991) did produce positive changes
in attitudes toward helping and behavioral intentions to help. Specifically, changes occurred in willingness to tell a friend or an adult, and in recommending resources, thus generally increasing the helping capacity among youth networks. A mixed response to seeking out a mental health professional was found that deserves attention. The finding at 18-months follow-up of various short-term curriculum-based programs that actual helping was not significantly different between participants and controls (Vieland et al., 1991) speaks to the importance of program length and need for skills training or practice, as differential effects were noted among youth who had participated in a more intensive, skill-based program (Eggert et al., 1999). Changes in helping behavior probably will not occur simply by fostering helping attitudes and increasing intentions to help; youth need skills training to act on these new attitudes and intentions. Behavioral intentions also improved for adults in the one skills-based program that reported on adult behaviors (Eggert et al., 1999). Although the program was delivered to youth, adults in the communities where the campaigns were delivered also showed benefits as opposed to comparison communities. For example, adults who had had contact with a youth showing signs of suicide risk were more likely to ask about suicide thoughts and give advice on where to get help.
Universal programs including skills-training components yield additional gains. Skills training as described was quite variable: a single session on active listening and other social skills for supporting a peer (Overholser et al., 1989); positive self-talk, situational analysis, empathy training, role playing, biblioguidance, interrupting automatic thoughts, rehearsal and skills strengthening (Klingman and Hochdorf, 1993); role-play with a suicidal peer emphasizing help-seeking (Kalafat and Elias, 1994); suicide-specific content included in the context of a 10th grade semester-long mental health course entitled “Life Management Skills” (Zenere and Lazarus, 1997); and a suicide intervention workshop, media training, and script writing and role-playing steps to helping a suicidal peer (Eggert et al., 1999).
Such programs increased adaptive coping skills (Klingman and Hochdorf, 1993; Overholser et al., 1989) and evidenced slight decreases in hopelessness (Ashworth et al., 1986; Orbach and Bar-Joseph, 1993; Overholser et al., 1989; Spirito et al., 1988). Furthermore, some studies have observed decreases in suicidal ideation (Klingman and Hochdorf, 1993; Orbach and Bar-Joseph, 1993) and suicide attempts (Zenere and Lazarus, 1997). Some evaluations have even noted decreases in rates of suicide completions among youth after program implementation (Kalafat, 2000; Kalafat and Ryerson, 1999; Zenere and Lazarus, 1997). For example, evaluation of the short behaviorally-oriented awareness program described by Kalafat and Elias (1994) has demonstrated long-term reduc-
tions in completed suicides compared to state and national rates (Kalafat and Ryerson, 1999). Evaluation of a comprehensive, skills-based, required mental health curriculum (Zenere and Lazarus, 1997) reported a decline in annual suicide rate from an average of 12.9 to 4.6 during the implementation of the district-wide pre-K–12 program as part of a suicide prevention strategy. Although this study employed no control data from comparable districts and the program was implemented following a year in which the district had experienced 19 suicides, Kalafat (2000) analyzed the county data in comparison to state and national suicide rates from 9 years before to 7 years after the initial program implementation and found a consistently lower post-program rate of completed suicide.
The current data support the importance of longer-term and skills-training prevention programs for schools that include accessible services. A broad review (Garland et al., 1989) of 115 school-based programs in the United States found that generally short-term interventions were not effective among past suicide attempters, specifically, and suggested that they might actually be harmful because they provided inadequate time to deal with the issues raised. Single-presentation interventions show limited effectiveness, and some studies found increased reporting of distress after the program (e.g., 2 of 14 youth suicide in Shaffer et al., 1990). Brief programs have also shown limited changes in attitude toward suicide (Ciffone, 1993; Nelson, 1987; Overholser et al., 1989; Shaffer et al., 1991). This may be due to the tendency to give socially desirable responses to attitude items, and the limited effectiveness of brief programs (Kalafat and Elias, 1994; Shaffer et al., 1991).
As with other issue-specific programs, the type of approach holds particular importance for outcomes. For example, film-based suicide awareness programs that depict suicidal acts may have negative effects because of potential imitation by suicidal adolescents (see earlier section, Gould and Shaffer, 1986; Shaffer et al., 1988). Given that prevention programs can exert differential effects on sub-groups, evaluation should examine how specific programs affect various sub-populations. Further, researchers have voiced concern about programs that do not use a solid scientific base, especially a tendency among some to ignore or even contradict research implicating mental illness in suicide (Shaffer et al., 1988).
In response to these issues about format of school-based suicide prevention programs, some United States researchers argue that universal interventions are inappropriate and recommend, instead, screening for those at risk (e.g., Shaffer and Craft, 1999). Others, such as the U.S. Task Force on Youth Suicide Prevention, have decided that suicide prevention should be integrated into “broader health promotion programs … directed at preventing other self-destructive behaviors, such as alcohol and substance abuse” (ADAMHA, 1989). The Surgeon General’s conference
report on children’s mental health (PHS, 2000) reiterates the necessity and efficacy of school-based universal mental health promotion programs to invest in children’s social and emotional development and thereby reduce numerous harmful outcomes. The World Health Organization has also endorsed school-based universal mental health promotion as a component of effective suicide prevention (WHO, 1999). In response to the mixed results of didactic suicide awareness programming in the United States and the World Health Organization’s school health promotion model (e.g., WHO, 2000a; WHO, 2002), New Zealand, Australia, and Sweden have developed mental health promotion curricula as components of their comprehensive suicide prevention strategies (Beautrais, 1998; Ramberg, 2000; Waring et al., 2000). Following WHO philosophy, their approach focuses on influencing health-related behaviors via knowledge, skills, attitudes, and support; creating conditions in the school and community that are conducive to health; and preventing leading causes of death, illness, and disability, including suicide.
Although these countries have only recently established their programs and results therefore represent only preliminary analyses, outcomes suggest important differences relative to typical short-term United States efforts. Sweden, for example, uses a film to depict teenagers who wrestled with suicidal thoughts and crises and emerged feeling that they had learned and grown from their adverse experiences (Ramberg, 2000). Teachers who want to show this film must first complete a 2-day training. The film’s objective involves helping students know about sources of help and understand that, when facing suicidal ideation, they are not alone. Unlike with many of the United States programs, high-risk students seem positive and interested in the film and indicate it helped them. Sweden’s full mental health curriculum includes suicidality and teaches about the medical aspects of mental illness and then the socio-environmental aspects of mental illness. Evaluation necessarily comprises a quasi-experimental design that limits outcome validity, but preliminary results indicate an as-yet nonsignificant trend in the intervention group toward fewer suicide attempts but no decrease in reports of suicidal ideation (Ramberg, 2000). This echoes results of the similar United States program reviewed by Zenere and Lazarus (1997), as described above. Current international suicide prevention strategies (described in a subsequent section) require evaluation of program elements, and will therefore provide much-needed information about which programs most effectively reduce suicide for various populations. Australia, for example, has started piloting its school programs and is publishing reports on common barriers to effective, sustained program implementation (e.g., Wyn et al., 2000).
Given that many schools in the United States employ short-term school-based suicide awareness interventions that may be ineffective and even potentially harmful, evaluation of various models and dissemina-
tion of those found safe and effective emerges as a priority. The most effective United States and international programs integrate suicide prevention into a competence-promotion and stress-protection framework, suggesting closer examination of health promotion as a prevention strategy. The evidence reviewed here supports carefully designed, science-based programs, particularly longer-term approaches couched in a broader context of teaching skills and establishing appropriate follow-through and services, as part of an effective armamentarium against suicide. Brief, didactic suicide prevention programs with no connection to services should be avoided.
SELECTIVE PREVENTION
Prevention initiatives at the selective level include: (1) screening programs to identify and assess at-risk groups; (2) gatekeeper training, consultation, and education services; (3) support/skills training; and (4) crisis response and referral resources. This review focuses on the available empirical evidence regarding school-based suicide prevention efforts. For selective prevention, screening is a critical first step. Systematic identification can be accomplished when screening is routine. Tools such as the Suicide Ideations Questionnaire (Pinto et al., 1997; Reynolds, 1998) are available, and studies have suggested that screening combined with supportive intervention can work to decrease suicidal behaviors (Eggert et al., 1995b; Randell et al., 2001; Thompson et al., 2001). (The limitations of suicide assessment tools, however, are discussed in Chapter 7.) Because an adolescent’s suicidal feelings are often short-term in duration and episodic in nature, repeated screening of high-risk populations is required to identify youth at risk for suicide in order to intervene to prevent impulsive behavior. The use of screening to identify at-risk and high-risk youth creates a demand for trained gatekeepers and programs designed to increase personal competencies. Gatekeepers need to consider multiple risk factors that suggest greater risk of suicide in addition to suicide ideation, such as substance abuse, history of physical or sexual abuse, conduct disorder, aggression/impulsivity, and family discord. Systematic identification of these youth should not be undertaken until social network resources are in place to respond to the needs identified by these screening procedures.
Gatekeeper Training
School-based Programs
Two gatekeeper-training activities were identified that were part of an integrated school-based program: LivingWorks Suicide Intervention
Workshop (SIW) and Suicide, Options, Awareness and Relief (Project SOAR).
SIW delivered five modules over 2 full days (Ramsey et al., 1994). Upon completion of the 2-day SIW training participants acquired basic knowledge about how to assess and intervene with youth at risk of suicide. The program was evaluated by comparisons between the gatekeepers’ knowledge and helping intentions immediately post-training, and that of the general public who had been exposed to a public media campaign (Eggert et al., 1997). Trained gatekeepers were significantly more likely to know the suicide warning signs (Eggert et al., 1997).
Project SOAR was a mandatory 8-hour training course for school counselors in Dallas, Texas. School counselors who had completed SOAR as part of their district-wide training (48 percent in the last 3 years) were very knowledgeable about warning signs correctly identifying depression, previous attempts, low self-esteem and recent relationship breakups 87 percent of the time or better. They also were very knowledgeable about suicide intervention steps correctly responding (90 percent of the time or better) that they would call a parent, listen to the student, notify the principal, and ask for assistance from school resources. In the SOAR project, competencies were sustained for up to 3 years post-training and enhanced by actual assessment of suicidal youth. Knowledge of intervention steps was also significantly greater when counselors had 6 or more years of experience (King and Smith, 2000). Information provided by program participants suggested that participants in SOAR performed at a level above the national average based on a national survey (King and Smith, 2000).
The two programs demonstrated that motivated adult helpers/professionals have little difficulty learning critical facts regarding suicide and the associated warning signs/risk factors when delivered as part of a gatekeeper-training curriculum. Adults participating in skill-based, action-oriented programs endorse appropriate helper attitudes, have high behavioral intentions to help, demonstrate appropriate helping competencies in simulations, and report being comfortable when helping. Participation in gatekeeper training programs appears to produce significantly greater gains when compared to informational messages alone. “Booster” training every 2 to 3 years and mock assessment/intervention role-plays may be useful to maintain competence.
Primary Care Physicians: The Gotland Program
On the Swedish island of Gotland, Rutz and colleagues (Rutz et al., 1989) implemented a program of physician education. This effort included a structured educational program for general medicine physicians on rec-
ognition and treatment of depressive disorders. Training included interactive seminars. A primary goal of the program was to increase general practitioners’ responsibility for treating depressive disorders. Several variables were monitored, including psychiatric referrals, sick leave for depression, psychiatric inpatient hospitalization, suicides, and prescriptions for antidepressant and anti-anxiety (anxiolytic) medications. When compared to suicide rates of the preceding 4 years, Rutz and colleagues (Rutz et al., 1989) found a significant decrease after the physician training. Referrals to psychiatry for depression decreased by over 50 percent and inpatient care for depression decreased by approximately 75 percent. The number of prescriptions for antidepressants increased, whereas the number of prescriptions for anxiolytics decreased. It should be mentioned that the analysis of the results was subsequently debated (Macdonald, 1995; e.g., Williams and Goldney, 1994), and the suicide rate increased again over time, coinciding with about half of the trained physicians leaving their positions (Rutz et al., 1992; see also discussion in Chapter 7).
Primary care provides a critical opportunity for suicide reduction in the United States as well (Chapter 9). However, significant barriers need to be addressed before primary care can serve as an effective conduit to mental health treatment including the treatment of suicidality. These include fractionation of services, lack of motivation of consumers and providers for mental health services, as well as economic barriers (DHHS 2002; see Chapter 9).
Support/Skills Training
The personal competency training program for youth in five urban high schools, Reconnecting Youth (RY) (Eggert et al., 1995a), serves as a model program for this review. Because approximately 35–40 percent of youth at risk for school failure are also at risk for suicide (Thompson and Eggert, 1999), potential high school dropouts are the targeted audience. This program is delivered in high school classrooms to small groups of 10 youths per teacher/ facilitator. The class was offered as an elective as part of the student’s school schedule. It was offered usually on a daily basis for 55 minutes over a full semester (90 sessions), or following the schedule used for other classes in the school’s time table.
All students participated in a comprehensive suicide-risk assessment (using the Measure of Adolescent Potential for Suicide [MAPS], Eggert et al., 1994) and social connections intervention, called Counselors-CARE (C-CARE). They were sorted into three groups: Group I youth participated in one semester of RY; Group II youth completed two semesters of RY; and Group III, the “usual care” comparison group, had the comprehensive assessment only. When at-risk youth participated in support/
skills training activities, they experienced clinically significant declines in suicide-risk behaviors; significant decreasing trends in depression, hopelessness, anger, and stress; significant gains in self-esteem and personal control; and increases in social support (Eggert et al., 1995).
The C-CARE assessment and social connection protocol appeared to be essentially as effective as the RY class (either the 1-semester or the 2-semester version) in reducing suicide-risk behaviors and related risk factors (Eggert et al., 1994). Similarly, it worked equally well to increase self-esteem and support resources. Importantly, youth participating in RY, both the 1-semester as well as the 2-semester versions, demonstrated significant gains in personal control (self-efficacy) not evidenced by the usual care/C-CARE group. The observation that a brief assessment protocol reduced suicidal behaviors and emotional distress that are sustained over a 10-month period is noteworthy, as well. Gains in personal control are more likely to be associated with lasting changes and sustained reductions in risk factors over time; longitudinal follow-up is necessary to answer this critical question. Results also point to the critical nature of leader support in building a positive peer culture and creating a context in which effective skills training occurs.
INDICATED PREVENTION
Programs for Youth
Youth identified as being at risk, evidencing early warning signs of suicide risk, need indicated suicide prevention. Among the initiatives designated as indicated are: (1) family support training; (2) skill-building support groups for high-risk individuals; (3) case management/alternative programming; and (4) referral resources for crisis intervention/treatment. This section focuses on two school-based suicide prevention efforts (Counselors CARE [C-CARE] and Project CAST [Coping and Support Training]) primarily addressing skills training support groups and case management/alternative programming for high-risk youth.
Included in both interventions were strategies designed to enhance a youth’s sense of personal control. C-CARE is described as an in-depth motivational interview for assessing a comprehensive list of direct suicide-risk factors, related-risk factors, and protective factors. The interventions were designed for potential high school dropouts, all of whom had evidenced specific, early warning signs of suicide- and related-risk factors on the Suicide Risk Screen (Thompson and Eggert, 1999).
The two programs were tested with 150 youth in C-CARE, 155 youth in CAST, relative to 155 similar youth in a “usual care” control group. These “usual care” high-risk youth received a very brief assessment inter-
view (15–30 min), and standardized social connections procedures (as in C-CARE) with parents and designated school personnel.
Both CAST and C-CARE involved school support personnel, resources, and policies related to student suicidal behaviors. Delivery occurred with youth in grades 9–12 and at the students’ schools. C-CARE starts with a one-to-one, 2-hour assessment interview. An additional 1.5 to 2 hours counseling session and social “connections” intervention with parents and school personnel follows. A brief assessment/counseling “booster” session is held 6–8 weeks later. Project CAST adds a 12-session (12 hours) small-group skills training program combined with the C-CARE individual approach. It includes the initial and booster sessions of C-CARE. These 12 sessions focus on enhancing personal resources (self-esteem, personal control of moods, school performance, drug use, positive coping strategies, and monitoring/setting goals and staying on track) and support resources (giving and receiving group support; identifying support needs to ask for from school personnel, family, and friends). Key prevention strategies common to both interventions were assessment and feedback for empathy and motivation, access to help and support from school personnel and parents, control of lethal means as indicated, and school crisis-team support. Changes were assessed at four time points, including a 9-month follow-up (Thompson et al., 2001).
CAST was most effective in enhancing and sustaining increases in problem-solving coping and personal control (self-efficacy) (Thompson et al., 2001). Both CAST and C-CARE were effective in enhancing self-esteem over the short term to increase self-esteem. The greatest differences between youth in CAST vs. C-CARE and usual-care were in problem-solving coping at follow-up (Randell et al., 2001). C-CARE and CAST effectively reduced depression and hopelessness compared to “usual care.” Both programs reduced anxiety and anger control problems in females. All youth showed significant decreases in hard drug use (Eggert et al., in press) but CAST was better at reducing alcohol and marijuana use (Eggert et al., in press). Growth curve analyses showed significant rates of decline in suicidal behaviors including suicidal ideation in both programs. Rates of suicide communications and attempts were unaffected; however, their low base-rate limited their outcome measures.
Programs for Aging Populations
As discussed in Chapter 9, late-life suicide victims typically see their primary care physicians in the month prior to death and face many obstacles to receiving appropriate care. A recent study on treatment outcome in suicidal versus non-suicidal depressed elderly patients showed that the two groups had identical remission rates (77 percent versus 78
percent) when treated with combined pharmacotherapy and interpersonal psychotherapy, but that the relapse rate was higher among suicidal elderly (26% versus 13%, Szanto et al., 2001). These data suggest that elderly suicidal depressed patients have an overall favorable treatment outcome, but that treatment response may be more brittle and may require the continuing use of adjunctive medication to prevent early relapse.
A recent “indicated” preventive intervention in the elderly looks promising. An NIMH-supported study on Prevention of Suicide in Primary Care Elderly: Collaborative Trial (PROSPECT; Bruce and Pearson, 1999) is testing the effectiveness of placing depression care managers in primary care practices in preventing and reducing suicidal ideation and behavior, hopelessness, and depressive symptomatology. The study is obtaining a sample representative of practice populations and is over-sampling patients with depression and the very old, i.e., those aged 75 and above. The essential tasks of the depression care manager are to convey clinical information to the primary care physician, to monitor the patient’s treatment compliance with treatment that is informed by Agency for Health Care Policy and Research guidelines, to assess the patient’s clinical status, to provide psychotherapy when requested, and to arrange specialist referrals. Preliminary data suggest that PROSPECT’s intervention is more effective than treatment as usual. Although both patient populations had similar base rates, after 12 months, 10 percent of the patients in the intervention group had suicidal ideation compared to 17 percent of those in usual care; and only 5 percent expressed hopelessness compared to 17 percent in usual care (Reynolds et al., 2001). These data suggest that a depression care manager can be an effective intervention.
INTEGRATED APPROACHES TO PREVENTION
The World Health Organization (WHO) began espousing national responses to the problem of suicide by 1989, and in 1996 the United Nations formulated official guidelines for national suicide prevention strategies that urged governments to adopt comprehensive approaches to reducing suicidality and increasing personal resilience and community connectedness (United Nations, 1996). Currently, Asian countries generally experience significant lack of basic mental health services, and often only have either the volunteer “Befrienders” services (see hotlines section) for those contemplating suicide or a few crisis centers staffed by volunteers. Furthermore, some countries still consider suicide a crime, thus limiting health care services available to attempters (for review, see Murthy, 2000).
A number of European national and United States state governments,
however, have responded to the complex nature of suicide by developing comprehensive suicide prevention strategies that incorporate all levels of prevention methods. In accordance with UN/WHO recommendations, such programs typically target both the reduction of mental illness and the promotion of mental health, employing everything from macro-level changes in social policy and the media to gatekeeper training and coordinated services for high-risk individuals. Many of these programs also establish improved data-gathering and surveillance systems. Although some comprehensive suicide prevention programs appear to reduce rates of suicide, evaluation of such programs remains challenging given the multitude of variables on the individual and aggregate level that interact to affect suicide rates. Omission of data collection from non-medical paradigms and lack of adequate planning and funding for evaluation have seriously hampered prevention efforts. Recent prevention strategies in Norway and Australia, for example, have therefore designated evaluation of all aspects of their programs as requirements for funding. As evaluation of comprehensive prevention models continues, nations and states will have more concrete information about what specific strategies effectively reduce suicide, how much funding such efforts require, and how best to coordinate efforts within and between levels of intervention.
Maryland Youth Suicide Prevention Strategy
The State of Maryland implemented a comprehensive suicide prevention model in the mid-1980s, but decided to focus on reducing youth, not general, suicide. According to a study by the Big Horn Center for Public Policy using data from the Centers for Disease Control and Prevention, Maryland has seen a reduction in suicide rates across age groups after program implementation. The greatest reduction has occurred in the 15– 24 year old range targeted by the prevention strategy, with a drop of 21.4 percent in Maryland, while youth suicide increased 11 percent nationally over the same decade (Westray, 2001a). This evaluation has not, however, ruled out other causal explanations for this lower suicide rate in Maryland. Nonetheless encouraged by the apparent success of the Maryland strategy, the program’s coordinators have trained 20 other United States states in how to implement its model and accepted an invitation from Australia to provide consultation to its national youth suicide prevention team.
As a means of organizing and administering the various components of the prevention strategy, Maryland created the “Governor’s Inter-Agency Workgroup on Suicide Prevention.” The Workgroup builds on existing agencies already targeting suicide risk factors such as substance abuse, child abuse, and mental disorders, and includes the involvement
of the Maryland Department of Juvenile Justice, Education, and the Office of Chief Medical Examiners, as well. Various subcommittees then focus on particular levels of intervention, such as media education, the Maryland youth crisis hotline, and gun control efforts.
Maryland represents the first state to institute a statewide, toll-free youth crisis telephone hotline. Six centers comprise the hotline network, with several of them offering walk-in counseling, emergency shelter, and community education. Trained local crisis intervention counselors staff the hotline, and, in addition to making general mental health referrals, counselors make appointments at local mental health centers for those adolescents willing to disclose their identity. In the 10 years since its inception, Maryland has seen a 47 percent increase in calls to the hotline, with the modal age group increasing from 12–17 to 18–24 (Westray, 2001b).
A significant aspect of Maryland’s youth suicide prevention plan involves funds for schools to develop prevention programs. Every district chooses a particular focus: some have implemented general mental health curriculum, others have established school gatekeeper training and crisis response teams, and others employ peer helper programs, suicide awareness education, and mental health referral systems. If properly evaluated, such program diversity could perhaps give insight into which approaches most effectively reduce youth suicide.
The Maryland youth suicide prevention plan, in contrast to Finland’s program, for example, targets reduction of access to means by working to change policy regarding gun use and by educating the public on the relationship between handguns and suicide. The program also initiated an AIDS hotline in English and Spanish to reach traditionally underserved populations at risk for suicide. The Maryland model also includes educating the media on appropriate reporting practices concerning suicide, and uses public service announcements to influence community awareness of youth suicide and available services. Finally, the program collaborates with the University of Maryland to obtain research expertise for evaluation of program elements and for data surveillance.
Air Force Suicide Prevention Strategy
In response to an increased awareness of suicide as the second leading cause of death among active duty United States Air Force personnel (CDC, 1999), the Air Force formed a committee of civilian and military multidisciplinary experts to design a service-wide comprehensive suicide prevention strategy in 1996–1997. Drawing from the experiences of previous models, the Air Force prevention approach, dubbed “LINK,” emphasizes the social and community aspects of suicide alongside individual,
psychiatric elements. The Air Force suicide prevention program therefore targets both suicide risk reduction and mental and behavioral health promotion, goals that concur with those of the United Nations and the World Health Organization recommendations (United Nations, 1996). Primary aspects of the LINK strategy include encouraging early mental health intervention and offering coordinated services among agencies, normalizing help-seeking behavior, and increasing protective factors such as social connectedness, support, and effective coping skills (USAFMS, 2000). Further, the Air Force has implemented suicide awareness training for staff, changed certain Air Force policies in response to epidemiological research, and developed a database for collecting a broad array of information regarding suicide attempts and completions throughout Air Force personnel and their families.
The Air Force has aggressively pursued increasing community awareness of suicide risks and available services and decreasing the stigma surrounding accessing mental health services. Senior Air Force staff reinforce the perspective that suicide prevention is a community effort and regularly distribute notices to personnel regarding the problem of suicide within the Air Force (USAFMS, 2000). Regular staff development courses have also now incorporated suicide prevention education for all officers. Such training describes the risk and protective factors for suicide, including contexts and symptoms of acute suicide risk, and when and to whom to refer individuals at risk of suicide. Further, LINK espouses establishing “buddy care,” in which everyone is encouraged to look out for others within the community. Enhancing the mental well-being of the entire unit is therefore conveyed as each staff member’s responsibility. Supervisors and unit members alike are encouraged to persuade those facing mental health issues (including substance abuse and domestic violence) to self-refer to services. The Air Force presents such actions as a means of increasing unit productivity and helping the individual reach his or her fullest potential, and explicitly states these goals as motivation for commander-directed mental health evaluations when individuals do not self-refer (USAFMS, 2000). After reviewing personnel surveys regarding behavioral health concerns, the Air Force has recently expanded its education program to include violence and homicide risk (Staal, 2001).
Given the research on overlapping risk factors for suicidality, the Air Force recognized a need to coordinate its mental health and social services. The suicide prevention program established a collaboration among six agencies: chaplains, child and youth programs, family advocacy, family support, health promotion/health and wellness centers, and mental health clinics. This Integrated Delivery System oversees and organizes overlapping suicide prevention efforts while maintaining individual agencies’ unique missions. The Delivery System therefore offers its services at
schools, work sites, and community facilities in addition to usual care at the member agency facilities. Representatives from member agencies and senior military installation commanders form the Community Action Information Boards that manage collaborative efforts among Delivery System agencies and between the Delivery System and their respective communities (USAFMS, 2000).
After epidemiological research regarding suicide among Air Force personnel demonstrated that situations such as legal investigations increased suicide risk, the Air Force suicide prevention program spear-headed policy changes to encourage help-seeking in these contexts. Specifically, the Air Force initiated a “hand-off” policy requiring that anyone facing legal issues be released to a supervisor or, minimally, only after notification of the supervisor, to ensure that an authority figure would be ready to refer the individual to helping agencies if deemed necessary (USAFMS, 2000). The Air Force implemented an additional measure that departs from military tradition by extending limited patient privilege to those under legal investigation. Thus, Air Force personnel receiving mental health treatment know that what they share with their mental health provider will not be used against them in military court or to characterize their service at the time of their separation from the military.
After implementing its comprehensive suicide prevention program, the Air Force saw a significant decrease in suicide rates among its active-duty personal, from 16.4 per 100,000 to 9.4 per 100,000 (p< 0.002) between 1994 and 1998 (Litts et al., 2000). By 1999, the rate dropped to 5.6 per 100,000. These rates represent a 78 percent decline in the suicide rate among active duty Air Force personnel over the last 5 years (Staal, 2001). In contrast, over the same period, suicide rates in other branches of the United States military (Navy, Army, and Marines) have not shown the same sustained decline (Litts et al., 2000). As with the other programs reviewed here, despite apparent success, the Air Force has not established that this reduction in suicide follows directly from LINK’s implementation (Litts et al., 2000; USAFMS, 2000).
An external evaluation of the program is currently under way at the University of Rochester School of Medicine’s Center for the Study and Prevention of Suicide. The Air Force also plans to continue analyzing its data to determine the effects of its suicide prevention efforts (Staal, 2001; USAFMS, 2000), and has established an epidemiological database and surveillance system. This system collects psychological, social, behavioral, economic, and relationship factors surrounding suicide attempts and completions among active and non-active duty cases. This database operates independently from other Air Force databases to enhance the confi-
dentiality of mental health provider reports and to include data from Reservists, National Guard, and Department of Defense members.
If analysis of the Air Force LINK model finds it effective in reducing suicide, exporting it to other communities could prove valuable. However, difficulties are anticipated. For example, the Air Force is a controlled environment in which commanding officers can forcibly refer individuals deemed at high risk for suicide to mental health services. Moreover, given personnel assignments to units, military service membership creates a salient community. Program elements establishing social support, sense of belonging, and social responsibility therefore take root much more easily in such a setting than in the broader society. Furthermore, the Air Force can routinely include suicide/mental health education into staff development and can form system-wide policies aimed at specific suicide-reduction efforts more quickly and with greater power to enforce such policies than the United States government as a whole. The Centers for Disease Control thus recommends first using the Air Force’s LINK model in occupation-related communities such as law enforcement and investigative agencies (CDC, 1999). The Department of Defense is currently implementing the LINK model, which should yield more information about its effectiveness in reducing suicide.
Suicide Prevention Programs for Rural American Indian Communities
Integrated approaches to suicide prevention have been used effectively in several American Indian reservation communities in the United States and Canada for at least three decades. These efforts were in response to either high suicide rates or apparent suicide clusters. They utilized universal, selected, and indicated intervention/prevention methods through community and public service agencies.
In the 1960s, the Shoshone-Bannock Tribal Council worked to reduce the high rate of suicide of 98 per 100,000 (mostly involving adolescents and young adults) in their community (Dizmang, 1969; Dizmang et al., 1974; Shore et al., 1972), but the rate continued to rise into the early 1970s. A partnership was formed among the tribe, NIMH, and the Indian Health Service (IHS) in 1968 in response to this crisis. Epidemiological research during the early part of this program identified acute alcohol intoxication, arrest for minor infraction, and high family disruption as risk factors for suicide, and services were designed to reduce these risks (Dizmang et al., 1974; Levy, 1988; May, 1987; Shore et al., 1972). This program included social and economic improvements, traditional Indian cultural enhancement programs, and increasing mental health services (Dizmang, 1969).
One of the hallmarks of this program was the active and enthusiastic participation of the local tribal members. Community awareness and organizing was used, and a tribal holding facility was established for youths “at risk” for suicide, or who had made low lethality suicide attempts. Here they received informal counseling, help, and support from volunteers from the Shoshone-Bannock tribal members who were on call around the clock. These volunteers had been trained by local mental health professionals and had ongoing support from health, mental health, and law enforcement officials. The suicide rate fell from a high of 173.1 per 100,000 in 1972–1976 to 21.5 in 1977–1980, but then rose again to 45.4 in 1981–1984 (May, 1987).
The suicide rate had also been very high in another Native American community, the Jicarilla Apache Tribe of northern New Mexico; 41 to 61 per 100,000 for a 10 year period (1969–1979) (VanWinkle and May, 1986; 1993). The rate was extraordinarily high among adolescents and young adults, exceeding 160 per 100,000 among those aged 15–24 during this same time-span (VanWinkle and May, 1986; 1993). Again, as with the Shoshone-Bannock, a partnership was formed between the Jicarilla Apache Tribal Council and Tribal Health Programs, with the Indian Health Service, and later the CDC. The program utilizes multiple agencies in the community including the IHS clinic, tribal mental health and substance abuse programs, the high school, and law enforcement. As a result of this partnership, this Jicarilla Apache community has had a comprehensive youth suicide prevention program since 1989 targeting 15–18 year olds in school and in the community with a variety of measures including public education, risk assessment, counseling, and alcohol abuse prevention initiatives (Serna et al., 1998).
Like the Shoshone-Bannock community program, the Jicarilla Apache program emphasized the use of “Natural Helpers” (local, indigenous persons trained to recognize symptoms of self-destruction and perform lay counseling) as key vehicles for prevention. The Natural Helpers work with the support and utilization of mental health professionals who serve as therapists for the highest risk and most serious cases. Professionals also provide training, advice, and support to community and staff alike. The program has drastically lowered the rate of suicide gestures, attempts, and completions combined (Serna et al., 1998). One of the consistent effects is not only a significant lowering of the rate of attempted and completed suicide in the targeted ages of 15–18, but a gradual lowering of the rates in older age brackets (e.g., 19–24), as the target population ages (P. May, University of New Mexico, personal communication, December 2001; VanWinkle and Williams, 2001).
Since the majority of suicides among American Indians occur among the young, schools have been a primary focus of some American Indian
suicide prevention programs. An effective school-based suicide prevention program was developed and implemented among the people of the Zuni Pueblo Tribe in western New Mexico (LaFramboise, 1996). This approach arose from the concern of the indigenous administrators of the Zuni Tribal School District over a 20-year pattern of 2 suicides per year in their high school. American Indian psychology and counseling researchers were brought into the community from Stanford University, the University of Oklahoma, and the University of Wisconsin to examine and define the situation among the youth and to develop strategies for the prevention of suicide. A number of risk factors and possible solutions were identified from survey research among the students, teachers, tribal leaders, and others within the community. The research at Zuni pin-pointed correlates of suicide specific to this community that identified high risk youths as having experience similar to that of other populations (e.g., suicide ideation, depression, poor social support, and hopelessness, among others), but also identified variables of help-seeking behavior, communication, and cultural resources that were specific to this particular tribal community and clearly differentiated those Zuni youths that were high risk and those that were not (Bee-Gates et al., 1996; Howard-Pitney et al., 1992). The research and the school collaboration led to the development of a comprehensive school curriculum that covered everything from building self-esteem, dealing with emotions and stress, and communication, to recognizing self-destructive behavior and helping those who may be suicidal (LaFramboise, 1996). The program was integrated into the language arts classes of the school rather than presented as a stand-alone course. Detailed research analysis indicated that students who were exposed to the program scored better than a no-intervention group at post test in hopelessness, problem-solving ability, and suicide intervention skills, with nonsignificant yet encouraging declines in suicide probability, as well (LaFramboise and Howard-Pitney, 1995). Though no formal evaluation of post-program suicide completions has been conducted, the school has experienced a reversal of its 20-year suicide rate, with zero completions noted since the program was taught in the late 1980s (P. May, University of New Mexico, and H. Lewis, past superintendent of the Zuni Public School District, personal communication, February 2002).
The fourth and final program discussed in this section on rural American Indian communities was implemented in Canada. After a suicide cluster of eight young adults in 1974–1975 on an Ottawa reserve in northern Canada, risk factors were identified by case control research within the community (Ward and Fox, 1977). Social isolation, family disruption, and poor coping skills were identified, in addition to acute and chronic misuse of alcohol (Ward and Fox, 1977). Because of the link of suicide
with alcohol problems, suicide awareness, prevention strategies, and a counseling program were all placed into service in the community via the counselors of the alcohol treatment program and with support from other mental health professionals and educators. Five years later the suicide rate in this community had fallen 10-fold, from 267 per 100,000 to 26.7. In addition, the overall violent death rate dropped from 253 per 100,000 to 109 (Fox et al., 1984; Ward, 1984). For a critical review of these and other suicide prevention programs among American Indians and Alaska Native communities, see Middlebrook et al., 2001.
International Programs
Lessons from Finland
Finland countered its unusually high rate of suicide (see La Vecchia et al., 1994) by establishing the world’s first nationally implemented, research-based comprehensive suicide prevention program. Organized into a research (1986–1991), implementation (1992–1996), and evaluation (1997–1998) phase, Finland’s National Suicide Prevention Project has offered itself as a learning opportunity for the world’s suicidologists. Both internal and external international teams have evaluated the project, and the United Nations/World Health Organization guidelines (1996) have included the model as a prime example for others to follow. Finland saw a peak in suicide rates in 1990 before project implementation, and then a 20 percent reduction between 1991 and 1996. The suicide rate has since stabilized at 9 percent below pre-project levels (Beskow et al., 1999).
The Suicide Prevention Project seeks to combine reducing suicide and promoting mental health, and therefore includes selective and indicated strategies, such as improving responsibility and cooperation between health services agencies, and universal measures such as enhancing individuals’ inner resources and living conditions. A foundational strategy involved building a national network of contact persons, primarily in health care, but also in the social services, churches, and police and rescue departments. Many prevention components arose from this network as schools and churches developed prevention projects specific to their settings, for example. National policy created better care for suicide attempters, increased knowledge among members of the media about suicide and mental illness, and promulgated media guidelines for reporting on suicide. Furthermore, the national players created an organizational frame for increased mental health research. An acclaimed national depression program targeting the general population that features coordinated basic and specialized services for all ages has also arisen from the Suicide Prevention Project.
Noted shortcomings of Finland’s project include, however, no selected or indicated focus on the elderly. The project also fails to include policies on reducing access to means. From a research perspective, Finland’s prevention project falls short in planning for sound evaluation; program developers did not collect data that could enable researchers to control for possible confounding variables. An international evaluation team further noted a lack of data collected from social psychological, sociological, and cultural perspectives that could enhance the science of suicide prevention (Beskow et al., 1999).
Finland did not implement its prevention program in a traditional fact-oriented, didactic fashion, but rather in a collaborative manner of guiding and supporting practitioners and service providers through joint reflections on prevention methods based on their expertise and existing activities. Evaluators note that participants found this approach and its attendant emphasis on “learning by doing” rewarding and psychologically effective, with key players/gatekeepers embracing the model. However, a general lack of studies on effective program implementation processes currently hampers prevention efforts. The Finland project, for example, still experiences tensions between the public and private sectors regarding hierarchy and organization (Beskow et al., 1999).
In summarizing the primary lessons from Finland’s experience with comprehensive suicide prevention programming, Beskow and colleagues (1999) mention the need for prevention strategies to carefully plan economic resources and evaluation. They also stress that a strong anchoring of the prevention strategy with city administrators and politicians and within professional organizations ensures its continuation.
Of paramount importance stands the need to understand and bridge differences between medical and other paradigms. Beskow’s evaluation team laments the presence of such conflicts in Finland that remain even after 11 years. The prestige of medical research can lend authority to a prevention strategy based on psychiatric-epidemiological research. Published results of a national psychological autopsy study alone brought suicide to the national consciousness in Finland and evoked willingness among professionals to tackle the problem. Ignoring other research paradigms, however, hampered evaluation efforts, for example, and made determining whether the prevention program accounts for the reduction in suicide rates virtually impossible. The program evaluators cite the encouraging trend within biopsychosocial research to use cross-disciplinary approaches as reason to believe that divisions between paradigms will be diminishing.
Other Recent International Programs
Certain other countries have designed comprehensive suicide prevention programs that will be evaluated continuously, yielding invaluable information about best practices for other governments. Australia, for example, used UN/WHO guidelines, the Finland experience, and consultation with the State of Maryland to design a national youth suicide prevention strategy that has now expanded to the general population. The Australia program uses evidenced-based practices to deliver and enhance cross-sectoral services; has developed and started implementing national university suicide prevention curriculum for doctors, nurses, teachers, and journalists; is re-orienting health services to focus on mental health promotion; and has started piloting a mental health curriculum for schools. The program also includes social change strategies such as media education, reducing access to lethal means, and investing in parenting programs (Commonwealth Department of Health and Family Services, 1997; Waring et al., 2000; Wyn et al., 2000). New Zealand’s youth suicide prevention program incorporates virtually the same elements, including the parenting interventions (Beautrais, 1998). Sweden’s program is very similar (Ramberg, 2000; The National Council for Suicide Prevention, 1996).
Norway, however, departs from these models by considering universal prevention and promotion factors as valuable social resources, but not part of a national strategy. Norway’s program therefore focuses on selected and indicated prevention, particularly increasing services to attempters after hospital release, though it does also support training for health providers and media education to reduce the stigma surrounding suicide (Norwegian Board of Health, 1995).
Finally, England represents a different approach by couching mental health issues within a truly comprehensive health strategy (Great Britain Department of Health, 1999). England’s prevention and health promotion efforts encompass physical and mental health, with suicide reduction a key element of their mental health program (see also Thornicroft, 1999). Concerning suicide, England engages in very similar cross-cutting activities as the previously mentioned programs, with policies to reduce access to lethal means, public education campaigns, improved mental health services, and mental health promotion components for youth and adults.
Summary of Integrated Approaches
Suicidologists and preventionists have monitored a number of comprehensive suicide prevention models implemented in sundry settings and cultures. These programs demonstrate that government workgroups
can, through cooperative efforts, mobilize health professionals and change service delivery, access to means, and public awareness regarding suicide. The Maryland and Air Force models, in particular, offer insight into how to establish effective inter-agency cooperation of services, and Finland has produced suicide prevention guidebooks for many specific settings (e.g., churches, police force). The programs of various American Indian communities provide models of culture-specific approaches to suicide reduction, especially for marginalized/ minority populations. Research from Finland and Australia provides valuable information regarding barriers to program implementation and the importance of pilot projects.
Currently evaluated comprehensive programs offer the striking lesson that lack of evaluation planning has seriously handicapped the field of suicide prevention. Although each of these programs based their strategy on the scientific literature regarding suicide, they lack the means to determine accurately whether their methods have specifically affected suicide rates. Suicide prevention researchers therefore have voiced concern about how funders and scientists have poured the bulk of their resources into more well-developed fields while communities continue to establish prevention efforts whose true effects remain largely unknown. Recently launched programs have responded to this by requiring evaluation, and will therefore fill much of the gap in knowledge concerning implementation and effectiveness of comprehensive national approaches to suicide prevention.
ASSESSING THE EFFECTIVENESS OF PREVENTION APPROACHES
To effectively reduce the incidence of suicide in the population, both the relative risk associated with a particular risk factor and its rate of occurrence within the population must be taken into consideration. It is very difficult to have broad population impact by focusing on a risk factor (as predictive of suicide as it might be) if it is itself a rare event. An analysis by Brown (2001) demonstrates that high-risk, and therefore also low-prevalence conditions, are always linked with low population-atttributable risk4 (PAR) and population preventive effects5 (PPE) (see Table 8-3a,b). Those who are hospitalized for unipolar depression, for example, have an extremely high relative risk, but the low prevalence of
TABLE 8-3 High-Risk Strategies for Reducing Attempted and Completed Suicide
|
High-Risk Group |
p(X)a |
RRb |
PARc |
IE(X)d |
IE(Xc) |
PPEe |
|
a. Reducing Completed Suicide |
|
|||||
|
Serious Suicide Attempt |
0.30% |
25.9 |
7% |
50% |
0% |
4% |
|
Psychiatric Hospitalization 1st Month |
0.09% |
129 |
10% |
50% |
0% |
6% |
|
Psychiatric Hospitalization 1st Year |
0.09% |
34 |
3% |
50% |
0% |
2% |
|
Unipolar Depression Hospitalization |
0.03% |
100 |
3% |
50% |
0% |
2% |
|
Unemployed |
6.00% |
2.5 |
8% |
50% |
0% |
8% |
|
Psychotic Like Symptoms |
0.50% |
15 |
7% |
50% |
0% |
4% |
|
b. Reducing Attempted Suicide |
|
|||||
|
Teen Suicide Attempt |
3.00% |
10 |
21% |
50% |
0% |
15% |
|
Psychiatric Diagnoses |
10.00% |
4 |
23% |
50% |
0% |
20% |
|
Major Depressive Disorder |
9.00% |
4 |
21% |
50% |
0% |
18% |
|
3 or More Symptoms |
12.00% |
3.5 |
23% |
50% |
0% |
21% |
|
2 or More Symptoms |
23.00% |
3.6 |
37% |
50% |
0% |
41% |
|
1 or More Symptoms |
38.00% |
2.7 |
39% |
50% |
0% |
51% |
|
a P(x) is the percentage of population with the trait or risk factor X. b Relative risk (RR) is defined as the proportion of people with a disorder among those exposed to a particular risk factor divided by the proportion of people with the disorder among those not exposed to the risk factor. c The population attributable risk, PAR , is the relative decrease in the disorder that we would expect if we were able to reduce the risk associated with X in a population at risk to that of the rest of the population not at risk. d Intervention effectiveness, IE , is the relative reduction indisorder that would occur if the intervention were implemented for the full population. IE(X) and IE(Xc) represent the intervention’s effectiveness on the subgroup sharing risk factor X and the subroup without risk factor X. IE takes into account factors such as level of program implementation and participation. Thus IE can be no larger than the participation rate. e Population preventive effect, PPE , is the relative reduction in the disorder within a population, if the intervention were applied to the full population. SOURCE: Brown, 2001. |
||||||
this population implies that targetting this group alone will not make a large impact on suicide in the general population. Note also that the last three rows, indicating number of psychiatric symptoms, have a decreasing relationship with both PAR and PPE. This indicates that broadening the target group can lead to a higher population effect than a strategy relying on a very high risk group.
When population-based strategies are considered, a larger impact can be effected. This can be illustrated with an example for early risk interventions such as prevention of aggression and conduct disorder, and substance abuse. In this illustration, it is estimated that the early risk factor (whichever example might be chosen) has 15 percent prevalence in the population (similar to early aggressive behavior). Because the risk factor has relatively high prevalence, its relative risk is rather modest (a value of 2 is selected for analysis). Two situations are considered for early risk interventions (see Table 8-4). The first is based on the highly optimistic assumption that a broad-based prevention program has completely successful impact on the high-risk group but produces only a 5 percent decrease in risk among the low-risk group. In this case, the overall reduction in risk is 34 percent. A second alternative is to assume 50 percent impact in the high-risk group and no impact in the low-risk group. This still produces a respectable 15 percent reduction in overall risk for suicide.
These strategies compare quite favorably with the impact of strategies involving crisis telephone lines. Crisis lines are now being used by about 2 percent of the population. Various technologies currently exist to improve participation in prevention programs and through higher utilization increase hotline effectiveness; the analysis here uses 5 percent. Even with the assumption of a very liberal relative risk of 2.5–10 for
TABLE 8-4 PAR and PPE for Alternative Population-Based Prevention Programs
|
|
p(X) |
RR |
PAR |
IE(X) |
IE(Xc) |
PPE |
|
Early Risk |
15.00% |
2 |
13% |
100% |
5% |
34% |
|
|
15.00% |
2 |
13% |
50% |
0% |
15% |
|
Crisis Line |
2.00% |
2.5 |
3% |
10% |
0% |
1% |
|
|
5.00% |
2.5 |
7% |
10% |
0% |
1% |
|
|
2.00% |
10 |
15% |
10% |
0% |
2% |
|
|
5.00% |
10 |
31% |
10% |
0% |
5% |
|
Gatekeeper |
10.00% |
2.5 |
13% |
10% |
0% |
3% |
|
|
20.00% |
2.5 |
23% |
20% |
0% |
10% |
|
SOURCE: Brown, 2001. |
||||||
suicide among would-be crisis line callers, the PAR and PPE are still quite small (Table 8-4). Their value in making a dramatic reduction in suicide is limited because of two factors—they are not used by a high percentage of those at risk, and successful treatment referral is also modest (Gould and Kramer, 2001).
For gatekeeper training, there is some opportunity for significant benefit, provided sufficient numbers of gatekeepers can reach out to those at risk. Two situations are compared to give a range of potential benefit (Table 8-4). In the first situation, the assumption is that gatekeepers are effective in reaching the upper 10 percent who are at risk, and they are only 10 percent effective in reducing their risk. Under these conditions, PAR and PPE are quite modest. On the other hand, if gatekeepers can work more effectively with the top 20 percent at risk, this could lead to sizable reductions in suicide.
In summary, high-risk strategies alone cannot suffice to significantly reduce the incidence of suicide. Our current knowledge forces us to examine universal and selective strategies that can reach individuals early on, when developmental patterns leading to youth problem behavior and psychiatric symptoms can potentially be changed.
FINDINGS
-
Imitation of suicides depicted in the media occurs. Education of media professionals can change reporting practices and such changes seem to reduce suicide in certain contexts but the data are limited.
Long-term public education campaigns and media training should be evaluated for their effectiveness both to change the public’s knowledge and attitudes and to reduce suicide and suicidal behaviors.
-
Reduction in access to a means of suicide can result in a decline in the use of that method. This decline sometimes occurs without substitution of means, thereby reducing suicide. Access to firearms is a particular risk factor for youth. Families often do not comply with counseling about the removal of guns from the home or securing the firearms. Evidence suggests that legislation can be effective.
Measures should be taken to reduce the fatality of all methods. Access to guns should be reduced, especially for those at high risk of suicide. Health care providers should involve families in working to reduce access to means. Education of health care providers about these issues would increase their knowledge regarding concerns and options and should be implemented.
-
Universal, selective, and indicated prevention programs that provide skills training show promise in increasing coping skills and to reducing hopelessness. School-based programs have been shown to enhance social support, self-efficacy, and self-esteem and may reduce depression, substance abuse, and suicidality. Training gatekeepers including responsible school staff or primary care physicians may be effective for identifying individuals at risk and obtaining assistance. Placing depression care managers in primary care practices may prove to be of benefit in reducing suicidal behaviors. The value of intervention programs, however, is frequently difficult to assess because of their short duration, often inadequate control populations, and limited long-term follow-up.
School-based intervention programs at the universal, selective, and indicated levels can help to limit suicide among youths and should be pursued. Efforts should provide skills training, gatekeeper training, a crisis response plan, and screening for youth at risk. Evidence-based programs, especially longer-term approaches couched in a broader context of teaching skills and establishing appropriate follow-through and services appear the most effective against suicide. Brief, didactic suicide prevention programs with no connection to services should be avoided.
-
Some suicide prevention programs targeting special populations have shown promise. Such models can inform national efforts regarding specific strategies for implementing effective programs in high-risk or special populations, such as policemen, indigenous peoples, and the elderly.
-
Comprehensive, integrated state and national suicide prevention strategies that target suicide risk and barriers to treatment across levels and domains appear to reduce suicide. Evaluation of such programs remains challenging given the multitude of variables on the individual and aggregate level that interact to affect suicide rates. Lack of adequate planning and funding for evaluation have seriously hampered prevention efforts.
Prevention and intervention trials must be carefully designed with appropriate controls and rigorously evaluated with long-term follow-up in order to know what works. Furthermore, it is critical that these interventions be assessed to determine if they can be applied to populations other than those in the original test and to define the characteristics that make a program generally effective.
REFERENCES
ADAMHA (Alcohol, Drug Abuse, and Mental Health Administration). 1989. Report of the Secretary’s Task Force on Youth Suicide. Washington, DC: U.S. Government Printing Office.
AFSP (American Foundation for Suicide Prevention). 2001. Reporting on Suicide: Recommendations for the Media. [Online]. Available: http://www.afsp.org/index-1.htm [accessed December 5, 2001].
Ashworth S, Spirito A, Colella A, Drew CB. 1986. A pilot suicidal awareness, identification, and prevention program. Rhode Island Medical Journal, 69(10): 457-461.
Bagley C. 1968. The evaluation of a suicide prevention scheme by an ecological method. Social Science and Medicine, 2(1): 1-14.
Barraclough BM, Jennings C. 1977. Suicide prevention by the Samaritans. A controlled study of effectiveness. Lancet, 2(8031): 237-239.
Beautrais A. 1998. A Review of Evidence: In Our Hands—The New Zealand Youth Suicide Prevention Strategy. Wellington, New Zealand: Ministry of Health, New Zealand.
Beautrais AL, Joyce PR, Mulder RT. 1996. Access to firearms and the risk of suicide: A case control study. Australian and New Zealand Journal of Psychiatry, 30(6): 741-748.
Bee-Gates D, Howard-Pitney B, LaFromboise T, Rowe W. 1996. Help-seeking behavior of Native American Indian high school students. Professional Psychology—Research and Practice, 27(5): 495-499.
Berman AL. 1988. Fictional depiction of suicide in television films and imitation effects. American Journal of Psychiatry, 145(8): 982-986.
Berman AL, Jobes DA. 1991. Adolescent Suicide: Assessment and Intervention. Washington, DC: American Psychological Association.
Berman AL, Jobes DA. 1995. Suicide prevention in adolescents (age 12-18). Suicide and Life-Threatening Behavior, 25(1): 143-154.
Beskow J, Kerkhof A, Kokkola A, Uutela A. 1999. Suicide Prevention in Finland 1986–1996: External Evaluation by an International Peer Group. Helsinki: Ministry of Social Affairs and Health.
Beskow J, Thorson J, Ostrom M. 1994. National suicide prevention programme and railway suicide . Social Science and Medicine, 38(3): 447-451.
Birckmayer J, Hemenway D. 1999. Minimum-age drinking laws and youth suicide, 1970– 1990. American Journal of Public Health, 89(9): 1365-1368.
Bond GR, Hite LK. 1999. Population-based incidence and outcome of acetaminophen poisoning by type of ingestion. Academic Emergency Medicine, 6(11): 1115-1120.
Boor M, Bair JH. 1990. Suicide rates, handgun control laws, and sociodemographic variables. Psychological Reports, 66: 923-930.
Borzekowski DL, Rickert VI. 2001a. Adolescent cybersurfing for health information: A new resource that crosses barriers. Archives of Pediatrics and Adolescent Medicine, 155(7): 813-817.
Borzekowski DL, Rickert VI. 2001b. Adolescents, the internet, and health: Issues of access and content. Journal of Applied Developmental Psychology, 22(1): 49-59.
Botvin GJ, Baker E, Dusenbury L, Botvin EM, Diaz T. 1995. Long-term follow-up results of a randomized drug abuse prevention trial in a white middle-class population. Journal of the American Medical Association , 273(14): 1106-1112.
Boyd JH. 1983. The increasing rate of suicide by firearms. New England Journal of Medicine, 308(15): 872-874.
Boyd JH, Moscicki EK. 1986. Firearms and youth suicide. American Journal of Public Health, 76(10): 1240-1242.
Brent DA. 1986. Overrepresentation of epileptics in a consecutive series of suicide attempters seen at a children’s hospital, 1978–1983. Journal of the American Academy of Child Psychiatry, 25(2): 242-246.
Brent DA, Baugher M, Birmaher B, Kolko DJ, Bridge J. 2000. Compliance with recommendations to remove firearms in families participating in a clinical trial for adolescent depression. Journal of the American Academy of Child and Adolescent Psychiatry, 39(10): 1220-1226.
Brent DA, Crumrine PK, Varma R, Brown RV, Allan MJ. 1990. Phenobarbital treatment and major depressive disorder in children with epilepsy: A naturalistic follow-up. Pediatrics, 85(6): 1086-1091.
Brent DA, Crumrine PK, Varma RR, Allan M, Allman C. 1987a. Phenobarbital treatment and major depressive disorder in children with epilepsy. Pediatrics, 80(6): 909-917.
Brent DA, Perper JA, Allman CJ. 1987b. Alcohol, firearms, and suicide among youth: Temporal trends in Allegheny County, Pennsylvania, 1960 to 1983. Journal of the American Medical Association, 257(24): 3369-3372.
Brent DA, Perper JA, Allman CJ, Moritz GM, Wartella ME, Zelenak JP. 1991. The presence and accessibility of firearms in the homes of adolescent suicides: A case-control study. Journal of the American Medical Association, 266(21): 2989-2995.
Brent DA, Perper JA, Goldstein CE, Kolko DJ, Allan MJ, Allman CJ, Zelenak JP. 1988. Risk factors for adolescent suicide. A comparison of adolescent suicide victims with suicidal inpatients. Archives of General Psychiatry, 45(6): 581-588.
Brent DA, Perper JA, Moritz G, Baugher M, Schweers J, Roth C. 1993. Firearms and adolescent suicide. A community case-control study. American Journal of Diseases of Children, 147(10): 1066-1071.
Breton JJ, Boyer R, Bilodeau H, Raymond S, Joubert N, Nantel MA. 1998. Review of Evaluative Research on Suicide Intervention and Prevention Programs for Young People in Canada: Theoretical Context and Results. Montreal, Quebec, Canada: Université de Montréal.
Brown CH. 2001. Designs to Evaluate High-Risk and Population-Based Suicide Prevention Programs: Maximizing Our Potential for Reducing Completed Suicide: Paper commissioned for the Institute of Medicine.
Brown CH, Liao J. 1999. Principles for designing randomized preventive trials in mental health: An emerging developmental epidemiology paradigm. American Journal of Community Psychology, 27(5): 673-710.
Bruce ML, Pearson JL. 1999. Designing and intervention to prevent suicide: PROSPECT (Prevention of Suicide in Primary Care Elderly: Collaborative Trial). Dialogues in Clinical Neuroscience, 1(2): 100-112.
Cantor CH, Slater PJ. 1995. The impact of firearm control legislation on suicide in Queensland: Preliminary findings. Medical Journal of Australia, 162(11): 583-585.
Cassidy S, Henry J. 1987. Fatal toxicity of antidepressant drugs in overdose. British Medical Journal (Clinical Research Edition), 295(6605): 1021-1024.
CDC (Centers for Disease Control and Prevention). 1992. Youth Suicide Prevention Programs: A Resource Guide. Atlanta: Centers for Disease Control.
CDC (Centers for Disease Control and Prevention). 1994. Deaths resulting from firearm-and motor-vehicle-related injuries—United States, 1968–1991. Journal of the American Medical Association, 271(7): 495-496.
CDC (Centers for Disease Control and Prevention). 1999. Suicide prevention among active duty Air Force personnel—United States, 1990–1999. Morbidity and Mortality Weekly Report, 48(46): 1053-1057.
Chan TY. 1996. Safety packaging of acetaminophen combination preparations and severity of adult poisoning. Journal of Toxicology. Clinical Toxicology, 34(6): 747-749.
Ciffone J. 1993. Suicide prevention: A classroom presentation to adolescents. Social Work, 38(2): 197-203.
Clarke RV, Lester D. 1986. Detoxification of motor vehicle exhaust and suicide. Psychological Reports, 59(3): 1034.
Clarke RV, Poyner B. 1994. Preventing suicide on the London Underground. Social Science and Medicine, 38(3): 443-446.
Commonwealth Department of Health and Family Services, Mental Health Branch. 1997. Youth Suicide in Australia: the National Youth Suicide Prevention Strategy. Canberra, Australia: Australian Government Publishing Service.
Cowen EL. 1994. The enhancement of psychological wellness: Challenges and opportunities. American Journal of Community Psychology, 22(2): 149-179.
Davidson MW, Wagner WG, Range LM. 1995. Clinicians’ attitudes toward no-suicide agreements. Suicide and Life-Threatening Behavior, 25(3): 410-414.
Dizmang LH. 1969. Observations on suicidal behavior among the Shoshone-Bannock Indians. U.S. Senate Committee on Labor and Public Welfare, Part 5. Special Subcommittee on Indian Education. (pp. 2351-2355). Washington, DC: U.S. Governement Printing Office.
Dizmang LH, Watson J, May PA, Bopp J. 1974. Adolescent suicide at an Indian reservation. American Journal of Orthopsychiatry, 44(1): 43-49.
Drew BL. 2001. Self-harm behavior and no-suicide contracting in psychiatric inpatient settings. Archives of Psychiatric Nursing, 15(3): 99-106.
Durlak JA. 2000. Health promotion as a strategy in primary prevention. In: Cicchetti D, Rappaport J, Sandler I, Weissberg RP, Editors. The Promotion of Wellness in Children and Adolescents. (pp. 221-241). Washington, DC: CWLA Press.
Eastwood MR, Brill L, Brown JH. 1976. Suicide and prevention centres. Canadian Psychiatric Association Journal, 21(8): 571-575.
Egan MP, Rivera SG, Robillard RR, Hanson A. 1997. The ‘no suicide contract’: Helpful or harmful? Journal of Psychosocial Nursing and Mental Health Services, 35(3): 31-33.
Eggert LL, Karovsky PP, Pike KC. 1999. School-Based Public Education Campaign. Washington State Youth Suicide Prevention Program: Pathways to Enhancing Community Capacity in Preventing Youth Suicidal Behaviors. Final Report. Seattle: University of Washington.
Eggert LL, Nicholas LJ, Owen LM. 1995a. Reconnecting Youth: A Peer Group Approach to Building Life Skills. Bloomington, IN: National Educational Service.
Eggert LL, Randell BR, Thompson EA, Johnson CL. 1997. Washington State Youth Suicide Prevention Program: Report of Activities. Seattle, WA: University of Washington.
Eggert LL, Thompson EA, Herting JR. 1994. A measure of adolescent potential for suicide (MAPS): Development and preliminary findings. Suicide and Life-Threatening Behavior, 24(4): 359-381.
Eggert LL, Thompson EA, Herting JR, Nicholas LJ. 1995b. Reducing suicide potential among high-risk youth: Tests of a school-based prevention program. Suicide and Life-Threatening Behavior, 25(2): 276-296.
Eggert L, Thompson E, Pike K, Randell B. in press. Preliminary effects of two brief school-based approaches for reducing youth suicide-risk behaviors, depression and drug involvement. Journal of Child and Adolescent Psychiatric Nursing.
Etzersdorfer E, Sonneck G. 1998. Preventing suicide by influencing mass-media reporting: The Viennese experience 1980–1996. Archives of Suicide Research, 4: 67-74.
Etzersdorfer E, Sonneck G, Nagel-Kuess S. 1992. Newspaper reports and suicide. New England Journal of Medicine, 327(7): 502-503.
Ferrari M, Barabas G, Matthews WS. 1983. Psychologic and behavioral disturbance among epileptic children treated with barbiturate anticonvulsants. American Journal of Psychiatry, 140(1): 112-113.
Fischer EP, Comstock GW, Monk MA, Sencer DJ. 1993. Characteristics of completed suicides: Implications of differences among methods. Suicide and Life-Threatening Behavior, 23(2): 91-100.
Flowers-Coulson PA, Kushner MA, Bankowski S. 2000. The information is out there, but is anyone getting it? Adolescent misconceptions about sexuality education and reproductive health and the use of the Internet to get answers. Journal of Sex Education and Therapy, 25(2-3): 178-188.
Forster DP, Frost CE. 1985. Medicinal self-poisoning and prescription frequency. Acta Psychiatrica Scandinavica, 71(6): 567-574.
Fox J, Manitowabi D, Ward JA. 1984. An Indian community with a high suicide rate—5 years after. Canadian Journal of Psychiatry, 29(5): 425-427.
France MH. 1982. Seniors helping seniors: A model of peer counseling for the aged. Canada’s Mental Health, 30(3): 13-15.
Garland A, Shaffer D, Whittle B. 1989. A national survey of school-based, adolescent suicide prevention programs. Journal of the American Academy of Child and Adolescent Psychiatry, 28(6): 931-934.
Glatt KM. 1987. Helpline: Suicide prevention at a suicide site. Suicide and Life-Threatening Behavior, 17(4): 299-309.
Gordon R. 1987. An operational classification of disease prevention. In: Steinberg JA, Silverman MM, Editors. Preventing Mental Disorders. (pp. 20-26). Rockville, MD: Department of Health and Human Services.
Gould MS. 2001a. Suicide contagion. Workshop presentation at the Institute of Medicine’s Workshop on Suicide Prevention and Intervention, May 14, 2001. Summary available in: Institute of Medicine. Suicide Prevention and Intervention: Summary of a Workshop. (pp. 8-10). Washington, DC: National Academy Press.
Gould MS. 2001b. Suicide and the media. Annals of the New York Academy of Sciences, 932: 200-221; discussion 221-224.
Gould MS, Kramer RA. 2001. Youth suicide prevention. Suicide and Life-Threatening Behavior, 31 (Suppl): 6-31.
Gould MS, Shaffer D. 1986. The impact of suicide in television movies. Evidence of imitation. New England Journal of Medicine, 315(11): 690-694.
Gould MS, Shaffer D, Kleinman M. 1988. The impact of suicide in television movies: Replication and commentary. Suicide and Life-Threatening Behavior, 18(1): 90-99.
Great Britain Department of Health. 1999. Saving Lives: Our Healthier Nation. London: The Stationery Office. [Online]. Available: http://www.archive.official-documents.co.uk/document/cm43/4386/4386.htm [accessed April 8, 2002].
Green JS, Grindel CG. 1996. Supervision of suicidal patients in adult inpatient psychiatric units in general hospitals. Psychiatric Services, 47(8): 859-863.
Grossman DC, Mang K, Rivara FP. 1995. Firearm injury prevention counseling by pediatricians and family physicians. Practices and beliefs. Archives of Pediatrics and Adolescent Medicine, 149(9): 973-977.
Gunnell D, Hawton K, Murray V, Garnier R, Bismuth C, Fagg J, Simkin S. 1997. Use of paracetamol for suicide and non-fatal poisoning in the UK and France: Are restrictions on availability justified? Journal of Epidemiology and Community Health, 51(2): 175-179.
Harris HE, Myers WC. 1997. Adolescents’ misperceptions of the dangerousness of acetaminophen in overdose. Suicide and Life-Threatening Behavior, 27(3): 274-277.
Hassan R. 1995. Effects of newspaper stories on the incidence of suicide in Australia: A research note. Australian and New Zealand Journal of Psychiatry, 29(3): 480-483.
Hawton K, Fagg J, Marsack P. 1980. Association between epilepsy and attempted suicide. Journal of Neurology, Neurosurgery, and Psychiatry, 43(2): 168-170.
Hawton K, Simkin S, Deeks JJ, O’Connor S, Keen A, Altman DG, Philo G, Bulstrode C. 1999. Effects of a drug overdose in a television drama on presentations to hospital for self poisoning: Time series and questionnaire study. British Medical Journal, 318(7189): 972-977.
Hawton K, Ware C, Mistry H, Hewitt J, Kingsbury S, Roberts D, Weitzel H. 1996. Paracetamol self-poisoning. Characteristics, prevention and harm reduction. British Journal of Psychiatry, 168(1): 43-48.
Hazell P, King R. 1996. Arguments for and against teaching suicide prevention in schools. Australian and New Zealand Journal of Psychiatry, 30(5): 633-642.
Hemenway D. 2001. Firearm availability and suicide. Workshop presentation at the Institute of Medicine’s Workshop on Suicide Prevention and Intervention, May 14, 2001. Summary available in: Institute of Medicine. Suicide Prevention and Intervention: Summary of a Workshop. (pp. 17-20). Washington, DC: National Academy Press.
Hlady WG, Middaugh JP. 1988. Suicides in Alaska: Firearms and alcohol. American Journal of Public Health, 78(2): 179-180.
Howard-Pitney B, LaFromboise TD, Basil M, September B, Johnson M. 1992. Psychological and social indicators of suicide ideation and suicide attempts in Zuni adolescents. Journal of Consulting and Clinical Psychology, 60(3): 473-476.
IOM (Institute of Medicine). 1994. Mrazek PJ, Haggerty RJ, Editors. Reducing Risks for Mental Disorders: Frontiers for Preventive Intervention Research. Washington, DC: National Academy Press.
IOM (Institute of Medicine). 2001. Health and Behavior: The Interplay of Biological, Behavioral, and Societal Influences. Washington, DC: National Academy Press.
IOM (Institute of Medicine). 2002. Speaking of Health: Assessing Health Communication Strategies for Diverse Populations. Washington, DC: National Academy Press.
Kalafat J. 2000. Issues in the evaluation of youth suicide prevention initiatives. In: Joiner T, Rudd MD, Editors. Suicide Science: Expanding the Boundaries. (pp. 241-249). Boston: Kluwer Academic Publishers.
Kalafat J, Elias M. 1994. An evaluation of a school-based suicide awareness intervention. Suicide and Life-Threatening Behavior, 24(3): 224-233.
Kalafat J, Ryerson DM. 1999. The implementation and institutionalization of a school-based youth suicide prevention program. Journal of Primary Prevention, 19: 157-175.
Kapur S, Mieczkowski T, Mann JJ. 1992. Antidepressant medications and the relative risk of suicide attempt and suicide. Journal of the American Medical Association, 268(24): 3441-3445.
Kellam SG, Ling X, Merisca R, Brown CH, Ialongo N. 1998. The effect of the level of aggression in the first grade classroom on the course and malleability of aggressive behavior into middle school. Development and Psychopathology, 10(2): 165-185.
Kellermann AL, Rivara FP, Somes G, Reay DT, Francisco J, Banton JG, Prodzinski J, Fligner C, Hackman BB. 1992. Suicide in the home in relation to gun ownership. New England Journal of Medicine, 327(7): 467-472.
Kessler RC, Downey G, Milavsky JR, Stipp H. 1988. Clustering of teenage suicides after television news stories about suicides: A reconsideration. American Journal of Psychiatry, 145(11): 1379-1383.
Kessler RC, Downey G, Stipp H, Milavsky JR. 1989. Network television news stories about suicide and short-term changes in total U.S. suicides. Journal of Nervous and Mental Disease, 177(9): 551-555.
Killias M. 1993. International correlations between gun ownership and rates of homicide and suicide. Canadian Medical Association Journal, 148(10): 1721-1725.
King GD. 1977. An evaluation of the effectiveness of a telephone counseling center. American Journal of Community Psychology, 5(1): 75-83.
King KA, Smith J. 2000. Project SOAR: A training program to increase school counselors’ knowledge and confidence regarding suicide prevention and intervention. Journal of School Health, 70(10): 402-407.
Kleck G, Marvell T. 2000. Impact of the Brady Act on homicide and suicide rates. Journal of the American Medical Association, 284(21): 2718-2719; discussion 2720-2721.
Klingman A, Hochdorf Z. 1993. Coping with distress and self harm: The impact of a primary prevention program among adolescents. Journal of Adolescence, 16(2): 121-140.
Knickerbocker DA, McGee RK. 1973. Clinical effectiveness of nonprofessional and professional telephone workers in a crisis intervention center. In: Lester D, Brockopp GW, Editors. Crisis Intervention and Counseling by Telephone. (pp. 298-309). Springfield, IL: Charles C. Thomas.
Kreitman N. 1976. The coal gas story. United Kingdom suicide rates, 1960–71. British Journal of Preventive and Social Medicine, 30(2): 86-93.
Kroll J. 2000. Use of no-suicide contracts by psychiatrists in Minnesota. American Journal of Psychiatry, 157(10): 1684-1686.
Kruesi MJ, Grossman J, Pennington JM, Woodward PJ, Duda D, Hirsch JG. 1999. Suicide and violence prevention: Parent education in the emergency department. Journal of the American Academy of Child and Adolescent Psychiatry, 38(3): 250-255.
La Vecchia C, Lucchini F, Levi F. 1994. Worldwide trends in suicide mortality, 1955–1989. Acta Psychiatrica Scandinavica, 90(1): 53-64.
LaFramboise TD. 1996. American Indian Life Skills Development Curriculum. Madison, WI: University of Wisconisn Press.
LaFramboise TD, Howard-Pitney B. 1995. The Zuni Life Skills Development Program: Description and evaluation of a suicide prevention program. Journal of Counseling Psychology, 42: 479-486.
Lester D. 1972. The myth of suicide prevention. Comprehensive Psychiatry, 13(6): 555-560.
Lester D. 1988. Gun control, gun ownership, and suicide prevention. Suicide and Life-Threatening Behavior, 18(2): 176-180.
Lester D. 1990. Was gas detoxification or establishment of suicide prevention centers responsible for the decline in the British suicide rate? Psychological Reports, 66(1): 286.
Lester D, Abe K. 1989. The effect of restricting access to lethal methods for suicide: A study of suicide by domestic gas in Japan. Acta Psychiatrica Scandinavica, 80(2): 180-182.
Lester D, Murrell ME. 1986. The influence of gun control laws on personal violence. Journal of Community Psychology, 14: 315-318.
Levy JE. 1988. The effects of labeling on health behavior and treatment programs among North American Indians. American Indian and Alaska Native Mental Health Research, 1 (Mono 1): 211-231; discussion 232-243.
Litts DA, Moe K, Roadman CH, Janke R, Miller J. 2000. From the Centers for Disease Control and Prevention. Suicide prevention among active duty Air Force personnel— United States, 1990–1999. Journal of the American Medical Association, 283(2): 193-194.
Loftin C, McDowall D, Wiersema B, Cottey TJ. 1991. Effects of restrictive licensing of handguns on homicide and suicide in the District of Columbia. New England Journal of Medicine, 325(23): 1615-1620.
Lott JR Jr. 2000. Impact of the Brady Act on homicide and suicide rates. Journal of the American Medical Association, 284(21): 2718; discussion 2720-2721.
Ludwig J, Cook PJ. 2000. Homicide and suicide rates associated with implementation of the Brady Handgun Violence Prevention Act. Journal of the American Medical Association, 284(5): 585-591.
Macdonald AJ. 1995. Suicide prevention in Gotland. British Journal of Psychiatry, 166(3): 402.
Mackay A. 1979. Self-poisoning—a complication of epilepsy. British Journal of Psychiatry, 134: 277-282.
Marzuk PM, Leon AC, Tardiff K, Morgan EB, Stajic M, Mann JJ. 1992. The effect of access to lethal methods of injury on suicide rates. Archives of General Psychiatry, 49(6): 451-458.
Matthews WS, Barabas G. 1981. Suicide and epilepsy: A review of the literature. Psychosomatics, 22(6): 515-524.
May PA. 1987. Suicide and self-destruction among American Indian youths. American Indian and Alaska Native Mental Health Research, 1(1): 52-69.
McClure GM. 1984. Recent trends in suicide amongst the young. British Journal of Psychiatry, 144: 134-138.
McLoone P, Crombie IK. 1996. Hospitalisation for deliberate self-poisoning in Scotland from 1981 to 1993: Trends in rates and types of drugs used. British Journal of Psychiatry, 169(1): 81-85.
Mendez MF, Lanska DJ, Manon-Espaillat R, Burnstine TH. 1989. Causative factors for suicide attempts by overdose in epileptics. Archives of Neurology, 46(10): 1065-1068.
Michel K, Frey C, Wyss K, Valach L. 2000. An exercise in improving suicide reporting in print media. Crisis, 21(2): 71-79.
Middlebrook DL, LeMaster PL, Beals J, Novins DK, Manson SM. 2001. Suicide prevention in American Indian and Alaska Native communities: A critical review of programs. Suicide and Life-Threatening Behavior, 31 (Suppl): 132-149.
Miller HL, Coombs DW, Leeper JD, Barton SN. 1984. An analysis of the effects of suicide prevention facilities on suicide rates in the United States. American Journal of Public Health, 74(4): 340-343.
Miller MC. 1999. Suicide-prevention contracts: Advantages, disadvantages, and an alternative approach. In: Jacobs DG, Editor. The Harvard Medical School Guide to Suicide Assessment and Intervention. (pp. 463-481). San Francisco: Jossey-Bass Publishers.
Miller MC, Jacobs DG, Gutheil TG. 1998. Talisman or taboo: The controversy of the suicide-prevention contract. Harvard Review of Psychiatry, 6(2): 78-87.
Mishara B, Daigle M. 2001. Helplines and crisis intervention services: Challenges for the future. In: Lester D, Editor. Suicide Prevention: Resources for the Millennium. (pp. 153-171). Philadelphia, PA: Brunner-Routledge.
Moens GF, van de Voorde H. 1989. Availability of psychotropic drugs and suicidal self-poisoning mortality in Belgium from 1971–1984. Acta Psychiatrica Scandinavica, 79(5): 444-449.
Motto JA. 1971. Evaluation of a suicide prevention center by sampling the population at risk. Suicide and Life-Threatening Behavior, 1(1): 18-22.
Murthy RS. 2000. Approaches to suicide prevention in Asia and the Far East. In: Hawton K, van Heeringen K, Editors. The International Handbook of Suicide and Attempted Suicide. Chichester, UK: John Wiley and Sons.
Myers WC, Otto TA, Harris E, Diaco D, Moreno A. 1992. Acetaminophen overdose as a suicidal gesture: A survey of adolescents’ knowledge of its potential for toxicity. Journal of the American Academy of Child and Adolescent Psychiatry, 31(4): 686-690.
Nelson FL. 1987. Evaluation of a youth suicide prevention school program. Adolescence, 22(88): 813-825.
Norwegian Board of Health. 1995. The National Plan for Suicide Prevention 1994–1998. [Online]. Available: http://www.helsetilsynet.no/english.htm [accessed December 22, 2001].
NRC (National Research Council). 2002. Eccles J, Gootman JA, Editors. Community Programs to Promote Youth Development. Washington, DC: National Academy Press.
O’Donnell I, Arthur AJ, Farmer RD. 1994. A follow-up study of attempted railway suicides. Social Science and Medicine, 38(3): 437-442.
Ohberg A, Lonnqvist J, Sarna S, Vuori E, Penttila A. 1995. Trends and availability of suicide methods in Finland. Proposals for restrictive measures. British Journal of Psychiatry, 166(1): 35-43.
Orbach I, Bar-Joseph H. 1993. The impact of a suicide prevention program for adolescents on suicidal tendencies, hopelessness, ego identity, and coping. Suicide and Life-Threatening Behavior, 23(2): 120-129.
Ostrom M, Thorson J, Eriksson A. 1996. Carbon monoxide suicide from car exhausts. Social Science and Medicine, 42(3): 447-451.
Overholser JC, Hemstreet AH, Spirito A, Vyse S. 1989. Suicide awareness programs in the schools: Effects of gender and personal experience. Journal of the American Academy of Child and Adolescent Psychiatry, 28(6): 925-930.
Pfeffer CR, Jiang H, Kakuma T. 2000. Child-Adolescent Suicidal Potential Index (CASPI): A screen for risk for early onset suicidal behavior. Psychological Assessment, 12(3): 304-318.
Phillips DP. 1974. The influence of suggestion on suicide: Substantive and theroretical implications of the Werther effect. American Sociological Review, 39(3): 340-354.
Phillips DP. 1985. The Werther effect. Suicide, and other forms of violence, are contagious. Sciences, 25: 32-39.
Phillips DP, Carstensen LL. 1988. The effect of suicide stories on various demographic groups, 1968–1985. Suicide and Life-Threatening Behavior, 18(1): 100-114.
Phillips DP, Paight DJ. 1987. The impact of televised movies about suicide. A replicative study. New England Journal of Medicine, 317(13): 809-811.
PHS (Public Health Service). 1999. The Surgeon General’s Call to Action to Prevent Suicide. Rockville, MD: U.S. Department of Health and Human Services.
PHS (Public Health Service). 2000. Report of the Surgeon General’s Conference on Children’s Mental Health: A National Action Agenda. Rockville, MD: U.S. Department of Health and Human Services.
PHS (Public Health Service). 2001. National Strategy for Suicide Prevention: Goals and Objectives for Action. Rockville, MD: U.S. Department of Health and Human Services.
Pinto A, Whisman MA, McCoy KJM. 1997. Suicidal ideation in adolescents: Psychometric properties of the Suicideal Ideation Questionnaire in a clinical sample. Psychological Assessment, 9(1): 63-66.
Ramberg IL. 2000. Presentation of a Youth Suicide Prevention Programme. Presentation at Youth Suicide Prevention: European Conference, September 19-20, 2000 in Nantes, France.
Ramsey RF, Tanney BL, Tierney RJ, Lang WA. 1994. Suicide Intervention Handbook. Calgary, Alberta, Canada: Living Works Education.
Randell BP, Eggert LL, Pike KC. 2001. Immediate post intervention effects of two brief youth suicide prevention interventions. Suicide and Life-Threatening Behavior, 31(1): 41-61.
Reynolds CF, Schulberg HC, Bruce M, Alexopoulos GS, Katz IR, Mulsant BH. 2001. Depression Treatment in Primary Care Elderly: Preliminary Outcomes of the NIMH PROSPECT Collaborative. Abstract presented at the annual meeting of the American College of Neuropsychopharmacology in Kona, Hawaii, December 10, 2001.
Reynolds WM. 1991. A school-based procedure for the identification of adolescents at risk for suicidal behaviors. Family and Community Health, 14: 64-75.
Reynolds WM. 1998. Suicide Ideation Questionnaire: A Professional Manual. Odessa, FL: Psychological Assessment Resources.
Rivara FP, Mueller BA, Somes G, Mendoza CT, Rushforth NB, Kellermann AL. 1997. Alcohol and illicit drug abuse and the risk of violent death in the home. Journal of the American Medical Association, 278(7): 569-575.
Rutz W, von Knorring L, Walinder J. 1989. Frequency of suicide on Gotland after systematic postgraduate education of general practitioners. Acta Psychiatrica Scandinavica, 80(2): 151-154.
Rutz W, von Knorring L, Walinder J. 1992. Long-term effects of an educational program for general practitioners given by the Swedish Committee for the Prevention and Treatment of Depression. Acta Psychiatrica Scandinavica, 85(1): 83-88.
Sainsbury P. 1986. The epidemiology of suicide. In: Roy A, Editor. Suicide. (pp. 17-40). Baltimore: Williams and Wilkins.
Schiodt FV, Rochling FA, Casey DL, Lee WM. 1997. Acetaminophen toxicity in an urban county hospital. New England Journal of Medicine, 337(16): 1112-1117.
Schmidtke A, Hafner H. 1988. The Werther effect after television films: New evidence for an old hypothesis. Psychological Medicine, 18(3): 665-676.
Schmidtke A, Schaller S. 2000. The role of mass media in suicide prevention. In: Hawton K, Van Heeringen K, Editors. The International Handbook of Suicide and Attempted Suicide. (pp. 675-697). Chichester, UK: John Wiley and Sons.
Scott V. 2000. Crisis services: Befrienders International: Volunteer action in preventing suicide. In: Lester D, Editor. Suicide Prevention: Resources for the Millenium. (pp. 265-273). Ann Arbor, MI: Sheridan Books.
Serna P, May P, Sitaker M. 1998. Suicide prevention evaluation in a Western Athabaskan American Indian Tribe—New Mexico, 1988–1997. Morbidity and Mortality Weekly Report, 47(13): 257-261.
Shaffer D, Craft L. 1999. Methods of adolescent suicide prevention. Journal of Clinical Psychiatry, 60(Suppl 2): 70-74.
Shaffer D, Garland A, Gould M, Fisher P, Trautman P. 1988. Preventing teenage suicide: A critical review. Journal of American Academy of Child and Adolescent Psychiatry, 27(6): 675-687.
Shaffer D, Garland A, Vieland V, Underwood M, Busner C. 1991. The impact of curriculum-based suicide prevention programs for teenagers. Journal of the American Academy of Child and Adolescent Psychiatry, 30(4): 588-596.
Shaffer D, Vieland V, Garland A, Rojas M, Underwood M, Busner C. 1990. Adolescent suicide attempters: Response to suicide-prevention programs. Journal of the American Medical Association, 264(24): 3151-3155.
Shore JH, Bopp JF, Waller TR, Dawes JW. 1972. A suicide prevention center on an Indian reservation . American Journal of Psychiatry, 128(9): 1086-1091.
Sillanpaa M. 1973. Medico-social prognosis of children with epilepsy. Epidemiological study and analysis of 245 patients. Acta Paediatrica Scandinavica. Supplement, 237: 3-104.
Simon RI. 1992. Clinical risk management of suicidal patients: Assessing the unpredictable. In: Simon RI, Editor. Review of Clinical Psychiatry and the Law, Volume 3. (pp. 3-63). Washington, DC: American Psychiatric Press.
Simon RI. 1999. The suicide prevention contract: Clinical, legal, and risk management issues. Journal of the American Academy of Psychiatry and Law, 27(3): 445-450.
Skopek MA, Perkins R. 1998. Deliberate exposure to motor vehicle exhaust gas: The psychosocial profile of attempted suicide. Australian and New Zealand Journal of Psychiatry, 32(6): 830-838.
Sloan JH, Rivara FP, Reay DT, Ferris JAJ, Path MRC, Kellermann AL. 1990. Firearms regulations and rates of suicide: A comparison of two metropolitan areas. New England Journal of Medicine, 322(6): 369-373.
Sonneck G, Etzersdorfer E, Nagel-Kuess S. 1994. Imitative suicide on the Viennese subway. Social Science and Medicine, 38(3): 453-457.
Spirito A, Overholser J, Ashworth S, Morgan J, Benedict-Drew C. 1988. Evaluation of a suicide awareness curriculum for high school students. Journal of the American Academy of Child and Adolescent Psychiatry, 27(6): 705-711.
Staal MA. 2001. The assessment and prevention of suicide for the 21st century: The Air Force’s community awareness training model. Military Medicine, 166(3): 195-198.
Stack S. 1990. Audience receptiveness, the media, and aged suicide. Journal of Aging Studies, 4: 195-209.
Stack S. 1996. The effect of the media on suicide: Evidence from Japan, 1955–1985. Suicide and Life-Threatening Behavior, 26(2): 132-142.
Stanford EJ, Goetz RR, Bloom JD. 1994. The no-harm contract in the emergency assessment of suicidal risk. Journal of Clinical Psychiatry, 55(8): 344-348.
Stein DM, Lambert MJ. 1984. Telephone counseling and crisis intervention: A review. American Journal of Community Psychology, 12(1): 101-126.
Stengel E. 1964. Suicide and Attempted Suicide. Harmondsworth, England: Penguin Books.
Szanto K, Mulsant BH, Houck PR, Miller MD, Mazumdar S, Reynolds CF 3rd. 2001. Treatment outcome in suicidal vs. non-suicidal elderly patients. American Journal of Geriatric Psychiatry, 9(3): 261-268.
Tekavcic-Grad O, Zavasnik A. 1987. Comparison between counselor’s and caller’s expectations and their realization on the telephone crisis line. Crisis, 8(2): 162-177.
The National Council for Suicide Prevention. 1996. Support in Suicidal Crises. Stockholm, Sweden: The National Council for Suicide Prevention.
Thompson EA, Eggert LL. 1999. Using the Suicide Risk Screen to identify suicidal adolescents among potential high school dropouts. Journal of the American Academy of Child and Adolescent Psychiatry, 38(12): 1506-1514.
Thompson EA, Eggert LL, Randell BP, Pike KC. 2001. Evaluation of indicated suicide risk prevention approaches for potential high school dropouts. American Journal of Public Health, 91(5): 742-752.
Thornicroft G, Chairman, Expert Reference Group. 1999. National Service Framework for Mental Health. London: Great Britain Department of Health.
Turvill JL, Burroughs AK, Moore KP. 2000. Change in occurrence of paracetamol overdose in UK after introduction of blister packs. Lancet, 355(9220): 2048-2049.
United Nations. 1996. Prevention of Suicide: Guidelines for the Formulation and Implementation of National Strategies. New York: United Nations.
USAFMS (U.S. Air Force Medical Service). 2000. The Air Force Suicide Prevention Program: A Description on Program Intiatives and Outcomes. AFPAM 44-160. Washington, DC: United States Air Force.
Van der Hoek W, Konradsen F, Athukorala K, Wanigadewa T. 1998. Pesticide poisoning: A major health problem in Sri Lanka. Social Science and Med, 46(4-5): 495-504.
VanWinkle NW, May PA. 1986. Native American suicide in New Mexico, 1957–1979: A comparative study. Human Organization, 45(4): 296-309.
VanWinkle NW, May PA. 1993. An update on American Indian suicide in New Mexico, 1980–1987. Human Organization, 52(3): 304-315.
VanWinkle NW, Williams M. 2001. Evaluation of the National Model Adolescent Suicide Prevention Project: A Comparison of Suicide Rates Among New Mexico American Indian Tribes, 1980–1998. Tulsa, Oklahoma: Oklahoma State University, College of Osteopathic Medicine.
Vieland V, Whittle B, Garland A, Hicks R, Shaffer D. 1991. The impact of curriculum-based suicide prevention programs for teenagers: An 18-month follow-up. Journal of the American Academy of Child and Adolescent Psychiatry, 30(5): 811-815.
Ward JA. 1984. Preventive implications of a Native Indian mental health program: Focus on suicide and violent death. Journal of Preventive Psychiatry, 2(4): 371-385.
Ward JA, Fox J. 1977. A suicide epidemic on an Indian reserve. Canadian Psychiatric Association Journal, 22(8): 423-426.
Waring T, Hazell T, Hazell P, Adams J. 2000. Youth mental health promotion in the Hunter region. Australian and New Zealand Journal of Psychiatry, 34(4): 579-585.
Webster DW, Wilson ME, Duggan AK, Pakula LC. 1992. Parents’ beliefs about preventing gun injuries to children. Pediatrics, 89(5 (Pt 1)): 908-914.
Weil DS, Hemenway D. 1992. Loaded guns in the home. Analysis of a national random survey of gun owners. Journal of the American Medical Association, 267(22): 3033-3037.
Westray H Jr. 2001a. The Maryland Suicide Prevention Model: A Caring Community Saves Lives. Baltimore, MD: Presented at the 13th Annual Maryland Youth Suicide Prevention Conference, October 11, 2001.
Westray H Jr. 2001b. Maryland Youth Crisis Hotline. Baltimore, MD: Presented at the 13th Annual Maryland Youth Suicide Prevention Conference, October 11, 2001.
WHO (World Health Organization). 1999. Violence Prevention: An Important Element of a Health-Promoting School. WHO/SCHOOLS/98.3, WHO/HPR/HEP/98.2. Geneva: World Health Organization WHO Information Series on School Health.
WHO (World Health Organization). 2000a. Local Action: Creating Health Promoting Schools. WHO/NMH/HPS/00.3, WHO/SCHOOL/00.2. Geneva: World Health Organization WHO Information Series on School Health.
WHO (World Health Organization). 2000b. Preventing Suicide: A Resource for Media Professionals. Geneva.
WHO (World Health Organization). 2002. Global School Health Initiative. [Online]. Available: http://www.who.int/hpr/archive/gshi/index.html [accessed January 9, 2002].
Williams JM, Goldney RD. 1994. Suicide prevention in Gotland. British Journal of Psychiatry, 165(5): 692.
Wintemute GJ, Parham CA, Beaumont JJ, Wright M, Drake C. 1999. Mortality among recent purchasers of handguns. New England Journal of Medicine, 341(21): 1583-1589.
Wyn J, Cahill H, Holdsworth R, Rowling L, Carson S. 2000. MindMatters, a whole-school approach promoting mental health and wellbeing. Australian and New Zealand Journal of Psychiatry, 34(4): 594-601.
Yip PS, Callana C, Yuen HP. 2000. Urban/rural and gender differentials in suicide rates: East and west. Journal of Affective Disorders, 57(1-3): 99-106.
Zenere FJ 3rd, Lazarus PJ. 1997. The decline of youth suicidal behavior in an urban, multicultural public school system following the introduction of a suicide prevention and intervention program. Suicide and Life-Threatening Behavior, 27(4): 387-402.
Encompass’d with a thousand dangers,
Weary, faint, trembling with a thousand terrors…
I … in a fleshy tomb, am
Buried above ground.
—WILLIAM COWPER (1731-1800)
From the poem “Lines Written During a Period of Insanity”.
Cowper on several occasions tried to hang, poison, or stab himself. The lines above were composed after one of his suicide attempts.


























































