Background
In the United States, the purchase of vaccines and the delivery of immunization services depend on a complex mix of public and private funding and health care services. Although immunization coverage rates have reached high levels during the past few decades, a measles epidemic from 1989 to 1991 drew attention to the continuing health threat from vaccine-preventable diseases, especially when immunization rates are low. Since 1963, the federal government has provided states with immunization assistance, primarily for vaccine purchase, through a CDC-administered program known as the Section 317 program. After the measles epidemic, the federal government substantially increased Section 317 program grant funds to states for immunization program infrastructure. The Vaccines for Children program (VFC), implemented in 1994, provided a source of new federal funding to purchase vaccines for qualifying children, primarily those who are uninsured or who are enrolled in Medicaid. States continued to receive federal funds through the Section 317 program for the purchase of vaccines.
With the sudden and significant increases in federal support in the early 1990s, many states found it difficult to expend their awards for immunization program infrastructure during the 1-year grant period. Large amounts of state grants were carried over to subsequent years. By 1996, the U.S. Congress cut back funding for Section 317 program grants for immunization program infrastructure, indicating its uncertainty that the states needed, or could manage, federal assistance in this area.
Other developments in the 1990s also affected the immunization sys-
tem. New and more expensive vaccines were added to the recommended schedule of immunizations. Health care reforms resulted in an increasing reliance on health care providers in the private sector for the delivery of immunization services to disadvantaged populations, accompanied by fundamental changes as a result of the growth of managed care in the larger health care delivery system.
In the wake of these changes, the roles of state and local health departments became more ambiguous and more complex. Their need to provide direct services diminished as private providers and health plans acquired the capacity and resources to deliver primary care services— including immunizations—to disadvantaged groups. However, a new role for public health departments emerged, one that places greater emphasis on performance monitoring and the development of community-level health indicators (IOM, 1996, 1997). This role requires collaboration among multiple sectors to enhance the ability of public agencies to assess immunization coverage rates in samples within small areas and to respond to specific health care needs when the private sector is not able—or not willing—to absorb the costs involved in sustaining high immunization coverage rates among hard-to-reach populations.
EXAMINING IMMUNIZATION FINANCE POLICIES AND PRACTICES
In 1998, the U.S. Congress asked IOM to conduct a study of the Section 317 program and of broader questions regarding appropriate levels of effort to achieve national immunization goals. The IOM study committee met during 1999 and 2000 to collect relevant information and to develop a framework to guide its deliberations. As part of this effort, a research team directed by Gary Freed at the University of Michigan conducted a series of structured telephone interviews with immunization program officials in all 50 states regarding the ways in which federal policies and funding patterns during the 1990s influenced the goals, priorities, and activities of state immunization programs (Freed et al., 2000). IOM staff and consultants developed eight case studies of public-sector immunization efforts in the states of Alabama, Maine, Michigan, New Jersey, North Carolina, Texas, and Washington and in San Diego and Los Angeles Counties in California (Fairbrother et al., 2000a).1 Four site visits to Detroit, Newark, Houston, and Los Angeles supplemented the case study materials with discussions with local providers and immunization
|
1 |
Each case study is available electronically via the website of the National Academy Press: www.nap.edu/html/case_studies. |
program representatives. IOM convened a workshop in Washington, D.C., in September 1999 to examine issues related to “pockets of need.” To supplement material available in the research literature, the committee also commissioned background papers on topics such as adult immunization, registries, measuring immunization coverage (Fairbrother et al., 2000b), and federal immunization policy (Johnson et al., 2000). Selected materials from the case study reports and commissioned papers were published in a supplemental issue of the American Journal of Preventive Medicine in October 2000.
IOM FINDINGS AND RECOMMENDATIONS
In opening remarks at the Austin workshop, David R. Smith, president of Texas Tech University Health Sciences Center and chair of the IOM committee organizing the workshop, highlighted key findings and recommendations from the Calling the Shots report (IOM, 2000).2 The study found that the nation’s immunization system faces serious challenges that could undermine past achievements and hinder the effort still needed to reach targeted levels of immunization coverage. Some of these demands include sustaining current rates of coverage with the addition of new and more expensive vaccines to the immunization schedule, responding to concerns about the safety of vaccines, serving an increased number of people as a result of recommendations for expanded vaccination of adolescents and adults, and adapting to changes in the health care delivery system that can affect the availability and affordability of vaccines in the private sector. The report recommends a renewal and strengthening of the federal-state partnership that is a fundamental element of the national immunization system. The report also recommends strategic investments in immunization efforts and closer collaboration between public and private health care systems to coordinate immunization roles and responsibilities in the wake of health care reforms.
The IOM study committee identified six fundamental roles for the nation’s immunization system (see also Figure 1):
-
Control and prevent infectious disease;
-
Assure the purchase of recommended vaccines for the total population of U.S. children and adults, with particular emphasis on the protection of vulnerable groups;
|
2 |
An audiocast of each presentation and the speaker’s visual aids are available in electronic form at the workshop website: www.iom.edu/iom/iomhome.nsf/pages/hcs+immunization+finance+dissemination. |
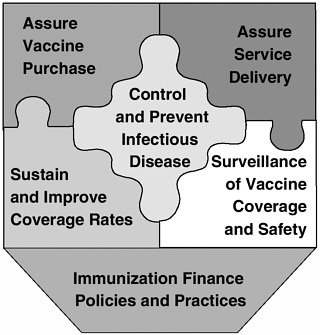
FIGURE 1 Six roles of the national immunization system.
-
Assure access to such vaccines within the public sector when private health care services are not adequate to meet local needs;
-
Conduct populationwide surveillance of immunization coverage levels, including the identification of significant disparities, gaps, and vaccine safety concerns;
-
Sustain and improve immunization coverage levels within child and adult populations, especially in vulnerable communities; and
-
Use primary care and public health resources efficiently in achieving national immunization goals.
The committee used this framework to guide its finance recommendations. The report concluded that adequate, stable, and predictable funding is necessary for the development of effective state immunization programs and that the fluctuations in funding for the Section 317 program infrastructure during the 1990s made it difficult for states to achieve program goals. With only a 1-year grant period, many state immunization programs could not invest in multiyear programs to support long-term strategic planning or data collection efforts.
The committee also concluded that immunization policy should be national in scope but flexible enough to accommodate important political, socioeconomic, and structural differences among states and communities.
Furthermore, federal and state governments share responsibility for supporting vaccine purchase and the infrastructure essential for achieving and sustaining national immunization goals. Data reviewed for the study showed that some states appeared to provide little or no state funding for immunization, whereas others invested substantially more than they received from federal sources. Finally, the IOM committee observed that the private sector, through health plans and individual health care providers, has the capacity to do more to ensure the delivery of appropriate immunization services to health plan members and providers’ patients. Yet such efforts do not replace the need for a public health infrastructure capable of ensuring that the immunization needs of the whole population are addressed.
The IOM study recommendations addressed federal and state funding levels, grant mechanisms for immunization programs, and the need for better measurement of immunization coverage levels. The committee concluded that annual budgets for the purchase of vaccines for children have been adequate. However, this finding was made before the addition of the pneumococcal conjugate vaccine to the recommended schedule for children, and this vaccine is more expensive than all other vaccines routinely administered to children combined. The committee recommended that increases in both federal and state budgets be made to provide for the purchase of additional vaccines for those high-risk adolescents and adults under age 65 who do not qualify for other federal assistance. The committee also recommended increases in financial and administrative support from federal and state governments for immunization program infrastructure.
In addition to budgetary increases, Dr. Smith noted that the IOM report proposed new operational and reporting requirements for the federal grants linked to the six fundamental roles for the national immunization system. The committee recommended that CDC distribute Section 317 program awards to states through a formula grant mechanism, with the formula reflecting base funding levels and additional amounts that reflect state need, capacity, and performance. In addition, a state matching requirement should be added, and the federal grants should have a 2-year budget cycle to give states greater flexibility to plan and implement multiyear efforts. Finally, the IOM report recommended that federal and state agencies develop a set of consistent and comparable measures for use in monitoring the immunization status of children and adults enrolled in private and public health plans as well as those of populations in defined geographic areas.
CDC RESPONSES TO IOM RECOMMENDATIONS
Lance Rodewald of the National Immunization Program at CDC reported on CDC’s responses to the IOM recommendations. He noted that the report’s articulation of the six broad roles of the national immunization system offered a valuable conceptual framework that CDC now uses to guide the development and assessment of immunization program activities. CDC has, for example, revised the Section 317 program grant guidance and program operations manual to give states greater flexibility to tailor programs to local needs within the immunization system framework outlined by the IOM study. CDC is also placing greater emphasis on opportunities to use Section 317 program funds to purchase vaccines for high-risk adolescents and adults. Through the Association of State and Territorial Health Officials, CDC has begun a dialogue with the states to develop a formula for the distribution of Section 317 program grant funds. Efforts are also being made to improve the harmonization of the immunization measures in the Health Plan Employer Data and Information Set (HEDIS) and the National Immunization Survey (NIS) and to expand the use of tools to assess coverage rates in individual clinics and physician practices.






