2
Overview of the Government Health Care Programs
|
SUMMARY OF CHAPTER RECOMMENDATIONS The six major government health care programs—Medicare, Medicaid, the State Children’s Health Insurance Program (SCHIP), the Department of Defense TRICARE and TRICARE for Life programs (DOD TRICARE), the Veterans Health Administration (VHA) program, and the Indian Health Service (IHS) program—provide health care services to about one-third of Americans. The federal government has a responsibility to ensure that the more than $500 billion invested annually in these programs is used wisely to reduce the burden of illness, injury, and disability and to improve the health and functioning of the population. It is imperative that the federal government exercise strong leadership in addressing serious shortcomings in the safety and quality of health care in the United States. RECOMMENDATION 1: The federal government should assume a strong leadership position in driving the health care sector to improve the safety and quality of health care services provided to the approximately 100 million beneficiaries of the six major government health care programs. Given the leverage of the federal government, this leadership will result in improvements in the safety and quality of health care provided to all Americans. |
The six major government health care programs serve older persons, persons with disabilities, low-income mothers and children, veterans, active-duty military personnel and their dependents, and Native Americans. Three of these programs—Medicare, Medicaid, and the State Children’s Health Insurance Program (SCHIP)—were devised for groups for whom the health care market has historically failed to work because of their high health care needs and low socioeconomic status. The remaining three programs—DOD TRICARE, VHA, and IHS—serve particular populations with whom the federal government has a special relationship, respectively, military personnel and their dependents, veterans, and Native Americans.
Many millions of Americans receive services through multiple government programs simultaneously. Low-income Medicare beneficiaries who qualify for both Medicare and Medicaid account for 17 percent of the Medicare population and 19 percent of the Medicaid population (Gluck and Hanson, 2001; Health Care Financing Administration, 2000). These “dual eligibles” account for a total of 28 percent of Medicare expenditures and 35 percent of Medicaid expenditures. Native Americans eligible to receive services through IHS may also qualify for Medicaid if they satisfy income and other eligibility requirements, and those aged 65 and older may qualify for Medicare. Nearly 45 percent of veterans are 65 years and older and also qualify for Medicare (Van Diepen, 2001b). In addition, many Americans eligible for these programs have private supplemental insurance as well. Thus, patients and clinicians would surely benefit from greater consistency in quality enhancement requirements, measures, and processes across public and private insurance programs.
Table 2-1 provides a capsule summary of the six government health care programs. A more detailed description of the programs is provided in the following section. The broad trends affecting the needs and expectations of the programs’ beneficiaries are then reviewed. The final section examines some key features of the programs beyond their quality enhancement processes.
MEDICARE1
Medicare provides health insurance to all individuals eligible for social security who are aged 65 and over, those eligible for social security because of a disability, and those suffering from end-stage renal disease (ESRD)—a total of about 40 million beneficiaries and growing. While
TABLE 2-1 Government Health Care Programs and Populations at a Glance
|
Characteristic |
Medicare |
Medicaid |
|
Beneficiaries (2001)a |
40 million |
42.3 million |
|
Eligibility |
Eligibility for social security, (age 65 and over, end-stage-renal disease, or disabled) |
Percent of federal poverty level and eligibility category (e.g., children, pregnant women, disabled) |
|
Benefits |
Basic acute care coverage, some preventive; high cost sharing, no prescription drugs |
Comprehensive for both acute and chronic care plus institutional long-term care for the elderly, disabled, and mentally retarded; nominal cost sharing |
|
Structure |
Federal |
Federal/state |
|
Leading diagnoses |
Hypertension, osteoporosis, chronic obstructive pulmonary disease, asthma, diabetes, heart disease, and stroke |
Childbirth, asthma, hypertension, diabetes, congenital neurological and developmental disorders, mental health and substance abuse, tuberculosis, sexually transmitted diseases, and HIV/AIDS |
|
Expenditures (2001) |
$242.4 billion |
$227.9 billion |
|
aSome individuals are eligible for more than one government program. SOURCES: Centers for Medicare and Medicaid Services, 1998, 2000a, 2000c, 2002a; Department of Health and Human Services, 1997, 2002; Indian Health Service, 2002; Medical Expenditure Panel Survey, 1998; TRICARE, 2002; Veterans Administration, 2001b. |
||
Medicare is 100 percent federally financed and operated, health care services are delivered almost entirely through the private sector. In 2002, about 87 percent of Medicare beneficiaries were covered by the Medicare fee-for-service (FFS) program; 13 percent of beneficiaries were enrolled in Medicare+Choice and cost-based health maintenance organizations (HMOs) (Centers for Medicare and Medicaid Services, 2002b). The Medicare population carries a heavy burden of chronic illness (never resolved conditions with continuing impairments that reduce the functioning of individuals)—78 percent of Medicare beneficiaries have at least one
|
SCHIP |
VHA |
DOD TRICARE |
IHS |
|
4.6 million |
4 million |
8.4 million |
1.4 million |
|
Generally up to 200% of federal poverty level and under age 19 |
Veterans with priority based on service discharge status and income |
Active-duty military, their dependents, retirees |
American Indians and Alaska Natives who belong to federally recognized tribes |
|
Medicaid or actuarial equivalent of largest managed care plan in state; some cost sharing |
Comprehensive chronic and acute care, including long-term institutional care; minimal cost sharing |
Acute care coverage; no cost sharing for active duty personnel in military treatment facilities; some cost sharing for purchased care in civilian sector |
Acute care, public health services, dental services, nutrition, community health, and other services |
|
Federal/state |
Federal |
Federal |
Federal/tribal |
|
Not Available |
Psychosis, substance abuse, heart failure, chronic obstructive pulmonary disease, pneumonia, chest pain, neuroses, arteriosclerosis, and digestive disorders |
Childbirth, orthopedic injuries, chest pain, pneumonia, congestive heart failure, asthma, and depression |
Diabetes, unintentional injuries, alcoholism, and substance abuse |
|
$4.6 billion |
$20.9 billion |
$14.2 billion |
$2.6 billion |
chronic condition and 63 percent have two or more (Anderson, 2002). The over 30 percent of the Medicare population that has a physical and/or cognitive impairment accounts for about 60 percent of expenditures (see Figure 2-1). Medicare beneficiaries with three or more chronic conditions account for the bulk of program expenditures (see Figure 2-2). The most prevalent diagnoses in persons aged 65 and over—high blood pressure, osteoporosis, chronic obstructive pulmonary disease, asthma, diabetes, heart disease, and stroke—are all chronic illnesses requiring medical management over extended time periods and multiple settings (Medical Ex-
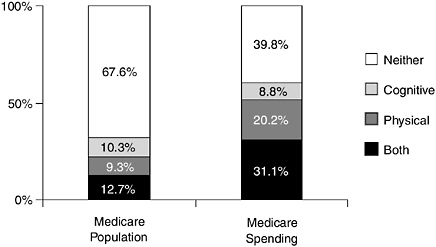
FIGURE 2-1 Medicare beneficiaries with cognitive and/or physical limitations as a percentage of beneficiary population and total Medicare expenditures, 1997. NOTE: A person with cognitive impairment has difficulty using the telephone or paying bills, or has Alzheimer’s disease, mental retardation, or various other mental disorders. A person with physical impairment is someone reporting difficulty performing three or more activities of daily living.
SOURCE: Reprinted with permission from Moon and Storeygard, 2001.
penditure Panel Survey, 1998). The fastest-growing sectors in Medicare in terms of spending (though not the largest proportion of total program spending) have been home health, skilled nursing facilities, and hospice care, reflecting a shift in demand toward more chronic care.
MEDICAID2
Medicaid serves about 42 million people who are poor and who require health care services to achieve healthy growth and development goals or meet special health care needs. The program covers low-income people who meet its eligibility criteria, such as children, pregnant women, certain low-income parents, disabled adults, federal Supplemental Security Income (SSI) recipients (low-income children and adults with severe disability), and the medically needy (non-poor individuals with extraordinary medical expenditures who meet spend-down requirements generally for long-term care). There is a good deal of variability across states in the maximum income for eligibility.
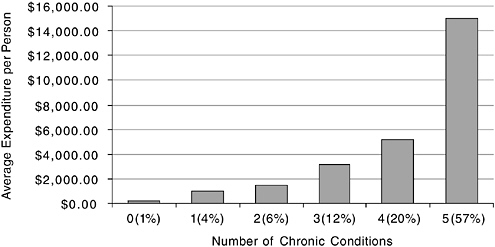
FIGURE 2-2 Medicare beneficiaries with five or more chronic conditions account for two-thirds of Medicare spending.
SOURCE: Centers for Medicare and Medicaid Services, 1999.
Medicaid is administered and financed jointly by the federal government and the states, although the federal government pays for over 50 percent of aggregate program expenditures (U.S. Government Printing Office, 2002). There is a good deal of variability in methods of health care delivery and financing across states. Medicaid programs rely extensively on private-sector health care providers, managed care plans, and community health centers to deliver services and, to a lesser degree, state, county, or other publicly owned facilities or programs. Nationwide, over half of the total Medicaid population is enrolled in Medicaid managed care arrangements. Institutionalized, disabled, dually eligible, and elderly beneficiaries are most likely to receive services through FFS payment arrangements.
The majority of Medicaid beneficiaries are children (54 percent), most under the age of 6 (see Figure 2-3). Each year, over one-third of all births in the United States are covered by Medicaid. While a minority of the program in terms of population (26 percent), the aged/blind/disabled account for 71 percent of program expenditures. Over half of Medicaid expenditures are for long-term care services, with the majority going to institutional long-term care providers (Centers for Medicare and Medicaid Services, 2000a).
While coordinated collection of Medicaid data from the states is lacking, other data sources indicate a substantial prevalence of chronic condi-
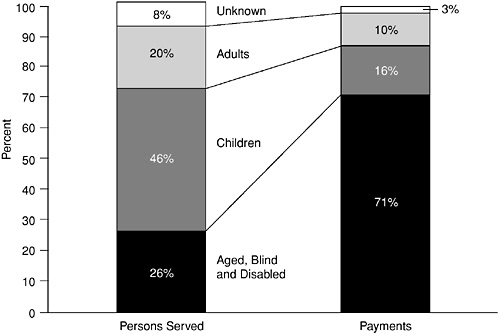
FIGURE 2-3 Distribution of persons served through Medicaid and payments by basis of eligibility, fiscal year 1998.
NOTE: Disabled children are included in the aged, blind and disabled category.
SOURCE: Centers for Medicare and Medicaid Services, 2000a.
tions in the program. These conditions include asthma, diabetes, neurological disorders, high blood pressure, mental illness, substance abuse, and HIV/AIDS (Centers for Medicare and Medicaid Services, 2001c; Medical Expenditure Panel Survey, 1996; Westmoreland, 1999).
STATE CHILDREN’S HEALTH INSURANCE PROGRAM3
Designed as a joint federal-state program, SCHIP was created in 1997 to provide health insurance to poor and near-poor children through age 18 without another source of insurance. Approximately 4.6 million children were enrolled in SCHIP as of fiscal year 2001 (Centers for Medicare and Medicaid Services, 2000b). SCHIP is targeted to children with incomes that exceed Medicaid eligibility requirements but remain under 200 percent of the federal poverty level (FPL) (Rosenbach et al., 2001). Some states
have expanded SCHIP to children with family incomes up to 300 percent of FPL (Rosenbaum and Smith, 2001).
SCHIP operates as a block grant program to the states. States have the option of creating SCHIP programs as Medicaid expansions, as separate programs, or as combined programs (i.e., Medicaid expansions for some income levels and separate programs for higher income levels).
The SCHIP program has been implemented slowly and variably across states. Most states rely on managed care arrangements as their primary mechanism of service delivery for both healthy children and those with special health care needs.
VETERANS HEALTH ADMINISTRATION
VHA was established in 1946 as a separate division within the Veterans Administration to meet the health care needs of U.S. veterans (Veterans Administration, 2001b).4 Veterans make up 10 percent of the nation’s population, but only a minority receive care through VHA (Kizer, 1999; Van Diepen, 2001a). Eligibility is triaged according to the available budget; those with compensable, service-connected disabilities are assigned the highest priority (Veterans Administration, 2001a). VHA serves as a payer of last resort for treatment not related to service-connected disabilities that is provided through VHA facilities.
Health care is delivered through 22 regional health care systems, referred to as Veterans Integrated Service Networks (VISNs). Each VISN contains 7 to 10 hospitals, 25 to 30 ambulatory care clinics, 4 to 7 nursing homes, and other care delivery units (Kizer, 1999). Most clinical and administrative staff are employees of VHA.
Generally, the VHA population is older, low-income, and characterized by high rates of chronic illness (see Table 2-1). Approximately 19 percent of the total VHA population sought inpatient and outpatient mental health services (including those related to substance abuse) in 2000 (Van Diepen, 2001a).
DOD TRICARE5
DOD TRICARE encompasses two health care programs operated by the Department of Defense. TRICARE provides services to active-duty military personnel, their dependents, retirees under the age of 65 and their
spouses, and survivors. TRICARE for Life, a recent addition to the military health program, provides supplemental coverage (e.g., for prescription drugs) to the population aged 65 and over who enroll in Medicare Part B.
TRICARE is administered by the Office of the Assistant Secretary of Defense (Health Affairs). At the core of the program is a direct care system of military treatment facilities (MTFs), which provide most of the care delivered to active-duty personnel and over half of that provided to TRICARE beneficiaries overall. There is an MTF located at most major military facilities in the United States and abroad, each operated by one of the military services. TRICARE also has regional contracts with private-sector health plans to provide active-duty personnel with certain services not available through MTFs and to serve other beneficiaries. Non–active-duty beneficiaries may choose from among three program options: (1) TRICARE Prime, the lowest-cost plan, which assigns beneficiaries to a primary case manager, emphasizes preventive care, and makes use of MTFs whenever possible for specialty care; (2) TRICARE Extra, a preferred provider–type FFS discounted cost option; and (3) TRICARE Standard, the highest-cost plan, which provides maximal flexibility in selection of providers.
TRICARE is intended to ensure “force health protection.” Active-duty personnel must be maintained at a level of health consistent with military demands according to a concept called “military readiness.” The TRICARE program must also be capable of providing urgent and emergency care to injured soldiers, sometimes stationed in remote areas. Lastly, since the Gulf War, a great deal of attention has been focused on early detection of risks associated with the activities and settings of deployment (e.g., exposure to biological, chemical, and nuclear hazards and combat stress) and the ongoing monitoring of health consequences and effects of treatment (Institute of Medicine, 2000).
The TRICARE beneficiary population tends to be young and healthy. In addition to force health protection, the service needs of other TRICARE beneficiaries, mostly active-duty dependents, are sometimes described as basically babies and bones (Jennings, 2001). With the implementation of TRICARE for Life, TRICARE’s elderly population can be expected to present health care needs similar to those of the Medicare population.
INDIAN HEALTH SERVICE6
IHS, an agency within the Department of Health and Human Services, is responsible for providing health services to members of federally
recognized American Indian and Alaska Native tribes. IHS currently provides health services to approximately 1.4 million American Indians and Alaska Natives belonging to more than 557 federally recognized tribes in 35 states.
The provision of these health services is based on treaties, judicial determinations, and acts of Congress that result in a unique government-to-government relationship between the tribes and the federal government. IHS, the principal health care provider, is organized as 12 area offices located throughout the United States. These 12 areas contain 550 health care delivery facilities operated by IHS and tribes, including: 49 hospitals; 214 health centers; and 280 health stations, satellite clinics, and Alaska village clinics. Almost 44 percent of the $2.6 billion IHS budget is transferred to the tribes to manage their own health care programs.
Poverty and low education levels strongly affect the health status of the Indian people. Approximately 26 percent of American Indians and Alaska Natives live below the poverty level, and more than one-third of Indians over age 25 who reside in reservation areas have not graduated from high school. Common inpatient diagnoses include diabetes, unintentional injuries, alcoholism, and substance abuse.
BROAD TRENDS AFFECTING THE NEEDS AND EXPECTATIONS OF BENEFICIARIES
In identifying ways to improve the quality enhancement processes of government health care programs, it is important to understand both the needs and expectations of today’s beneficiaries and the trends likely to affect these needs and expectations in the future. As beneficiaries’ needs and expectations evolve over time, so, too, must the government health care programs. This section highlights two important trends: the increase in chronic care needs and expectations for patient-centered care.
Chronic Care Needs
Trends in the epidemiology of health and disease and in medical science and technology have profound implications for health care delivery. Chronic conditions (defined as never resolved conditions, with continuing impairments that reduce the functioning of individuals) are now the leading cause of illness, disability, and death in the United States and affect almost half the U.S. population (Hoffman et al., 1996). Most older people have at least one chronic condition, and many have more than one (Administration on Aging, 2001). Fully 30 percent of those aged 65–74, and over 50 percent of those aged 75 and older report a limitation caused by a chronic condition (Administration on Aging, 2001). The proportion
of children and adolescents with limitation of activity due to a chronic health condition more than tripled from 2 percent in 1960 to over 7 percent in the late 1990s (Newacheck and Halfon, 1998).
Thus, the majority of U.S. health care resources is now devoted to the treatment of chronic disease (Anderson and Knickman, 2001). This trend is strongly reflected in the government health care programs. In the Medicare and VHA programs, most of the beneficiaries have multiple chronic conditions. Diseases such as asthma, diabetes, hypertension, cancer, congestive heart failure, and mental health and cognitive disorders are important clinical concerns for all or nearly all of the programs.
The increasing prevalence of chronic illness challenges systems of care designed for episodic contact on an acute basis (Wagner et al., 1996). Hospitals and ambulatory settings are generally designed to provide acute care services, with limited communication among providers, and communication between providers and patients is often limited to periodic visits or hospitalizations for acute episodes. Serious chronic conditions, however, require ongoing and active medical management, with emphasis on secondary and tertiary prevention. The same patient may receive care in multiple settings, so that there is frequently a need to coordinate services across a variety of venues, including home, outpatient office or clinic setting, hospital, skilled nursing facility, and when appropriate, hospice.
There is mounting evidence that care for chronic conditions is seriously deficient. Fewer than half of U.S. patients with hypertension, depression, diabetes, and asthma are receiving appropriate preventive, acute, and chronic disease management services (Clark, 2000; Joint National Committee on Prevention, 1997; Legorreta et al., 2000; Wagner et al., 2001; Young et al., 2001). Health care is typically delivered by a mix of providers having separate, unrelated management systems, information systems, payment structures, financial incentives, and quality oversight for each segment of care, with disincentives for proactive, continuous care interventions (Bringewatt, 2001). For individuals with multiple chronic conditions, coordination of care and communication among providers are major problems that require immediate attention.
There are many efforts under way to develop new models of care capable of meeting the needs of the chronically ill. For example, Healthy Future Partnership for Quality, an initiative in Maine now in its fifth year, enrolls insured individuals (from leading health plans and the state Medicaid program) and uninsured individuals (covered by a 10 percent surcharge on the fee for each insured participant and paid by insurance companies) with chronic illness in an intensive care management program that provides patient education, improved access to primary care and preventive services, and disease management (Healthy Futures Partnership
for Quality Project, 2002). The diabetes telemedicine collaborative in New York State (IDEATel, 2002) is a randomized controlled trial supported by CMS and others. It involves 1,500 patients, half of whom participate in home monitoring (using devices that read blood sugar, take pictures of skin and feet, and check blood pressure), intensive education on diabetes, and reminders and instructions on how to manage their disease.
The changing clinical needs of patients have important implications for government quality enhancement processes. These processes and the health care providers they monitor should be capable of assessing how well patients with chronic conditions are being managed across settings and time. This capability necessitates consolidation of all clinical and service use information for a patient across providers and sites, a most challenging task in a health care system that is highly decentralized and relies largely on paper medical records.
Patient-Centered Care
Patient-centered care is respectful of and responsive to individual patient preferences, needs, and values and ensures that patient values and circumstances guide all clinical decisions (Institute of Medicine, 2001). Informed patients participating actively in decisions about their own care appear to have better outcomes, lower costs, and higher functional status than those who take more passive roles (Gifford et al., 1998; Lorig et al., 1993, 1999; Stewert, 1995; Superio-Cabuslay et al., 1996; Van Korff et al., 1998). Most patients want to be involved in treatment decisions and to know about available alternatives (Guadagnoli and Ward, 1998); (Deber et al., 1996; Degner and Russell, 1988; Mazur and Hickam, 1997). Yet many physicians underestimate the extent to which patients want information about their care (Strull et al., 1984), and patients rarely receive adequate information for informed decision making (Braddock et al., 1999).
Patient-centered care is not a new concept, rather one that has been shaping the clinician and patient relationship for several decades. Authoritarian models of care have gradually been replaced by approaches that encourage greater patient access to information and input into decision making (Emanuel and Emanuel, 1992), though only to the extent that the patient desires such a role. Some patients may choose to delegate decision making to clinicians, while patients with cognitive impairments may not be capable of participating in decision making and may be without a close family member to serve as a proxy. Patients may also confront serious constraints in terms of covered benefits, copayments, and ability to pay (discussed below under benefits and copayments)
The recently released physician charter by the American Board of Internal Medicine (ABIM) Foundation, the American College of Physicians-
American Society of Internal Medicine (ACP-ASIM) Foundation, and the European Federation of Internal Medicine embodies three fundamental principles to guide the medical profession, including:
Principle of Patient Autonomy. Physicians must have respect for patient autonomy. Physicians must be honest with their patients and empower them to make informed decisions about their treatment. Patients’ decisions about their care must be paramount, as long as those decisions are in keeping with ethical practice and do not lead to demand for inappropriate care (American Board of Internal Medicine et al., 2002, p. 244).
The current focus on making the health care system more patient-centered stems at least in part from the growth in chronic care needs discussed above. Effective care of a person with a chronic condition is a collaborative process, involving extensive communication between the patient and the multidisciplinary team (Wagner et al., 2001). Patients and their families or other lay caregivers deliver much if not most of the care. Patients must have the confidence and skills to manage their condition, and they must understand their care plan (e.g., drug regimens and test schedules) to ensure proper and safe implementation. For many chronic diseases, such as asthma, diabetes, obesity, heart disease, and arthritis, effective ongoing management involves changes in diet, increased exercise, stress reduction, smoking cessation, and other aspects of lifestyle (Fox and Gruman, 1999; Lorig et al., 1999; Von Korff et al., 1997).
Pressures to make the care system more respectful of and responsive to the needs, preferences, and values of individual patients also stem from the increasing ethnic and cultural diversity that characterizes much of the United States. Although minority populations constitute less than 30 percent of the national population, in some states, such as California, they already constitute about 50 percent of the population (Institute for the Future, 2000). A culturally diverse population poses challenges that go beyond simple language competency and include the need to understand the effects of lifestyle and cultural differences on health status and health-related behaviors; the need to adapt treatment plans and modes of delivery to different lifestyles and familial patterns; the implications of a diverse genetic endowment among the population; and the prominence of nontraditional providers as well as family caregivers.
Although there has been a virtual explosion in Web-based health and health care information that might help patients and clinicians make more informed decisions, the information provided is of highly variable quality (Berland et al., 2001; Biermann et al., 1999; Landro, 2001). Some sites provide valid and reliable information. These include the National Library of Medicine’s Medline Plus sites (Lindberg and Humphreys, 1999); the National Diabetes Education Program, launched by the Centers for Disease Control and Prevention and the National Institutes of Health (U.S. Gov-
ernment Printing Office, 2001); and the National Health Council’s public education campaign. There are also notable efforts to provide consumers with comparative quality information on providers and health plans. Examples are the health plan report cards produced by the National Committee for Quality Assurance and by the Consumers Union/California HealthCare Foundation Partnership and nursing home quality reports produced by CMS (Centers for Medicare and Medicaid Services, 2001a; Consumers Union/California Healthcare Foundation Partnership, 2002; National Committee for Quality Assurance, 2002). These efforts are discussed further in Chapter 5. There is little doubt, however, that we are embarking on a long journey to determine how best to make valid and reliable information available to diverse audiences with different cultural and linguistic capabilities (Foote and Etheredge, 2002).
In general, communication with consumers is enhanced through the use of common terminology, standardized performance measures, and reporting formats that follow common conventions. At the program level, the predilection of each government program to design and operate its health care quality enhancement processes independently is a serious problem.
KEY PROGRAM FEATURES
Although the focus of this report is on quality enhancement processes, the committee believes it important to acknowledge other important program features—such as benefits, payment approaches, and program design and administration—that influence quality. Just as the quality enhancement processes of the government programs are being assessed in this report, these other aspects of program design must be evaluated in the future for alignment with the objectives of those processes.
Benefits and Copayments
Health insurance was established in the United States in the 1930s and 1940s as a way to help the average person cope with the high costs of hospital care (Stevens, 1989). Today hospital care, although still very expensive, consumes about one-third of the health care dollar, and other facets of health care, such as prescription medications (9 percent with a growth rate of 13.8 percent) have grown in importance (Centers for Medicare and Medicaid Services, 2002c; Strunk et al., 2002). Increased demand for these other facets of care reflects the growth in chronic care needs discussed earlier as well as new treatment options stemming from the extraordinary advances made in medical knowledge and technology, including minimally invasive surgery.
TABLE 2-2 Insurance Plans Covering Benefits Important to Chronically Ill Persons, 2000
|
Benefitsa |
% of Fortune 100b |
Medicare |
Medicaid Floridac |
|
Prescription drugs |
100 |
no |
yes |
|
Mental health outpatient services |
100 |
yes |
yes |
|
Mental health inpatient services |
100 |
yes |
yes |
|
Home health care |
100 |
yes |
yes |
|
Physical therapy |
100 |
yes |
yes |
|
Durable medical equipment |
100 |
yes |
yes |
|
Occupational therapy |
99 |
yes |
yes |
|
Speech therapy |
99 |
yes |
yes |
|
Skilled nursing facilities |
99 |
yes |
yes |
|
Chiropractor |
97 |
yes |
yes |
|
Family counseling |
50 |
yes |
yes* |
|
Dietitian–nutritionist |
45 |
yes |
yes* |
|
Medical social worker |
37 |
yes |
yes* |
|
Respite care |
0 |
yes |
yes |
|
Personal care |
0 |
no |
yes* |
|
Non-emergency transportation |
0 |
no |
yes |
|
Home (environmental) modifications |
0 |
no |
yes* |
|
*These services are provided to a limited subset of the state’s Medicaid population. aList of important benefits identified through focus group discussions and interviews with experts (Montenegro-Torres et al., 2001). bPercentage of leading Fortune 100 companies providing this benefit to their employees in 2000 (Montenegro-Torres et al., 2001). |
|||
The benefit package of an insurance program has a direct effect on the likelihood of patients receiving needed health care services (Federman et al., 2001). Although there are frequent changes in the benefit packages of the various government health care programs, these modifications have not always kept pace with the needs, especially the chronic care needs, of the populations being served (Bringewatt, 2001).
When one assesses the extent to which the government health care programs provide coverage for benefits important to persons with chronic conditions, the results are mixed (see Table 2-2). The basic Medicare package, for example, generally does not cover outpatient prescription drugs or personal care, and coverage is very limited for preventive services, nursing home services, family counseling, and dietitian–nutritionist services. Medicare payment mechanisms are designed for acute care, often by a single provider; there is no Medicare payment mechanism that recognizes care delivered by a team of providers to an individual with mul-
|
Medicaid Arizonac |
Medicaid Connecticutc |
VHA |
TRICARE |
|
yes |
yes |
yes |
yes |
|
yes |
yes |
yes |
yes |
|
yes |
yes |
yes |
yes |
|
yes |
yes |
yes |
yes |
|
yes |
yes |
yes |
yes |
|
yes |
yes |
yes |
yes |
|
yes |
yes |
yes |
yes |
|
yes |
yes |
yes |
yes |
|
yes |
yes |
yes |
yes |
|
no |
yes |
yes |
no |
|
yes |
yes |
yes |
yes |
|
yes |
yes |
yes |
outpatient |
|
no |
yes* |
yes |
yes |
|
yes |
yes |
yes |
some cases under hospice |
|
yes |
no |
yes |
no |
|
yes |
yes |
yes |
no |
|
yes |
yes* |
yes |
no |
|
cThere is a good deal of variability across states in covered benefits. These three states were selected at random, and may or may not be representative of Medicaid plans in general. SOURCES: Agency for Health Care Administration, 2002; Anderson, 2002; Arizona Health Care Cost Containment System, 2002; Centers for Medicare and Medicaid Services, 2001b; and Connecticut Department of Social Services, 2002. |
|||
tiple chronic conditions or that rewards prevention efforts such as extensive patient education for self-care.
Other government programs offer important benefits in specific areas. VHA provides extensive mental health outpatient and inpatient services, especially for veterans with service-related disabilities. Medicaid provides residential care to the disabled and mentally retarded and long-term care for the elderly as a major part of program spending. Its benefit package is very comprehensive, including complex therapies for chronic conditions and congenital neurological disorders, such as cerebral palsy and Down syndrome, although states vary substantially in the scope of such benefits. Both Medicaid and SCHIP programs cover outpatient prescription medications. Note that IHS is not included in Table 2-2 because it is not an entitlement program or an insurance plan; therefore, it has no established benefit package (Indian Health Service, 2001). It is estimated
that funds appropriated to IHS by Congress cover approximately 60 percent of the health care needs of beneficiaries (Indian Health Service, 2001)
Cost-sharing provisions are also important. Persons with chronic conditions are the heaviest users of health care services. Deductibles and especially copayments can be sizable for these individuals. Some government health care programs, such as VHA, have minimal cost-sharing provisions, while others, especially Medicare, make more extensive use of such provisions.
Also important is how the different programs interpret “medical necessity.” Even when a service is covered, payment for that service to a particular patient can be denied because of failure to meet a medical necessity criterion. In some instances, the quantity and duration of certain repetitive services may be limited unless the person shows functional improvement, not just stability or a slowing of decline (Anderson et al., 1998).
The committee believes that each of the six government health care programs should review its benefit package and medical necessity criteria to identify enhancements in coverage or cost sharing that would facilitate the provision of more appropriate care to today’s beneficiaries. Such analyses should be conducted under alternative financial scenarios, including budget neutrality and varying levels of growth in expenditures. Efforts should also be made to understand how well the benefit packages of various government health care programs meet the needs of vulnerable populations and how well these packages fit together for those who are dual- or triple-eligible.
Payment Approaches
Efforts to improve quality of care will be far more effective if implemented in an environment that encourages and rewards excellence. Unfortunately, current methods of payment to health plans and providers have the unintended consequence of working against quality objectives. This is true for both capitated and FFS payment methods.
Capitation is a payment arrangement in which health plans are paid a fixed amount for each enrollee under their care, regardless of the level of services needed by and actually provided to the person. Some health plans also pay physicians on a capitated basis for certain outpatient care, putting them at some degree of financial risk.
Capitated payment rates are usually based on the average cost per enrollee of the enrolled group, often with adjustments for demographic characteristics (e.g., age and sex). Capitation rates are usually not adjusted for the health status of the enrolled population. Therefore, health plans and providers receive the same payment for someone who is less healthy and more likely to use a large number of services, such as a person with a
chronic condition, as they do for someone who is healthier and likely to use no or fewer services during the year.
Health plans or clinicians that develop exemplary care programs for persons with chronic conditions may, as a result, attract a disproportionate share of these individuals. Under capitated payment systems, this situation has a highly negative financial impact on the health plan and providers (Luft, 1995; Maguire et al., 1998). Persons with chronic conditions are more likely both to use services and to use a greater number of services during the year than those without chronic conditions. In 1996, for example, mean health care expenditures for a person with one or more chronic conditions were nearly 4 times the overall average ($3,546 versus $821) (Partnerships for Solutions, forthcoming). The average number of inpatient days per year is 0.2 for persons with no chronic conditions compared to 4.6 for those with five or more such conditions.
Risk adjustment is a mechanism designed to ensure that payments to health plans and other capitated providers more accurately reflect the expected cost of providing health care services to the population enrolled. Capitated plans and providers caring for a population that includes less healthy, higher-cost enrollees should receive higher payments. As more states require their entire Medicaid populations, including those who are disabled and have high health care needs, to enroll in managed care, adjustment of payments becomes even more necessary to ensure quality of care for enrollees (Maguire et al., 1998). Some states have addressed this issue. Michigan, for example, has created a separately funded capitated option for children with special health care needs (Department of Health and Human Services, 2000).
Numerous options exist for risk-adjusting payments, but their application in government health care programs has been limited (Ellis et al., 1996; Hornbrook and Goodman, 1996; Newhouse et al., 1997; Starfield et al., 1991). The Medicare+Choice program has initiated demonstration projects to pilot the application of capitated payments adjusted for health status (Centers for Medicare and Medicaid Services, 2000d).
Regardless of whether the beneficiary is enrolled in an indemnity or capitated plan, the physicians on the front line of care delivery in the private sector are generally compensated under FFS payment methods (Center for Studying Health System Change, 2001; Institute of Medicine, 2001). FFS is the most common method of payment to physicians under Medicare, Medicaid, and SCHIP.
Under FFS payment, physicians have strong financial incentives to increase their volume of billable services (e.g., visits and office-based procedures and tests). Sometimes the incentives of FFS or other physician payment methods are attenuated by incentives (e.g., bonuses) tied to performance (e.g., measures of safety, clinical quality, service), but this is not
the norm. In a 1998–1999 survey of a nationally representative sample of physicians, fewer than 30 percent indicated that their compensation was affected by performance-based incentives, a result similar to findings from a survey conducted in 1996–1997 (Stoddard et al., 2002). When they are used, performance-based incentives are more likely to be tied to patient satisfaction (24 percent) and quality measures (19 percent) than to measures that may restrain care, such as profiling (14 percent).
The principal “reimbursable event” under FFS is a face-to-face encounter between a physician and patient, which may or may not trigger other reimbursable events, such as diagnostic tests and minor office procedures. Services such as e-mail communications, telephone consultations, patient education classes, and care coordination are important for the ongoing management of chronic conditions, but they are not reimbursable events. Moreover, physicians who communicate with patients through e-mail or telephone to emphasize patient education, self-management of chronic conditions, and to coordinate care may experience a reduction in overall revenues if these uncompensated services have the effect of reducing patient demand for or time available to devote to reimbursable face-to-face encounters.
There is no perfect payment method; all methods have advantages and disadvantages. FFS contributes to overuse of billable services (e.g., face-to-face encounters, ancillary tests, procedures) and underuse of preventive services, counseling, medications, and other services often not covered under indemnity insurance programs. Overuse, especially the provision of services that expose patients to more potential harm than good, is a serious quality-of-care and cost concern. On the other hand, capitated payments may contribute to underuse—the failure to provide services from which patients would likely benefit. This is especially true when there is a good deal of turnover among plan enrollees so that the long-term cost consequences of underuse tend to be borne by another insurer. Although particular payment methods may contain a bias towards underuse or overuse, it is important to note that the quality-of-care literature contains ample evidence of both phenomena occurring in both FFS and capitated payment systems, reinforcing the notion that payment is but one, albeit an important, factor influencing care (Chassin and Galvin, 1998).
The committee believes enhancements can be made in both capitated and FFS payment approaches to encourage the provision of quality health care. It should also be noted that there are some promising efforts under way to design alternative payment approaches and evaluate their impact on quality. The National Health Care Purchasing Institute, a nonprofit research institute supported by The Robert Wood Johnson Foundation, has identified various incentive models that might be effective in motivat-
|
BOX 2-1 Quality bonuses—An additional annual payment is made to a provider (usually 5 to 10 percent of annual compensation) based on the achievement of certain performance goals. Compensation at risk—A portion of a provider’s compensation is placed “at risk” based on the provider’s performance on quality measures. Performance fee schedule—A provider’s fee schedule is linked to performance on a set of quality measures (e.g., providers achieving exemplary levels of performance might receive 115 percent of the base fee schedule, while poor performers might receive 85 percent). Variable cost sharing for patients—A patient’s deductible and copayments are linked to the provider’s performance on a set of quality measures (e.g., patients who see providers with high performance scores have lower cost sharing than those who see the poorer performing providers). SOURCE: Adapted from Bailit Health Purchasing, 2002b. |
ing providers to improve their performance; some of these models are highlighted in Box 2-1. Numerous efforts are under way to test some of these approaches. Examples include the following:
-
The Buyers Health Care Action Group, an employer coalition in Minnesota, provides gold ($100,000) and silver ($50,000) awards to care systems for performance on quality improvement projects (Bailit Health Purchasing, 2002a)
-
PacifiCare in California has developed a quality index that profiles providers on the basis of measures of clinical quality, patient safety, service quality, and efficiency. This information is used to reward providers on the basis of their performance, as well as to construct a tiered system of premiums, copayments, and coinsurance rates for enrollees that vary inversely with provider performance in terms of quality and efficiency (Ho, 2002)
-
The Employers’ Coalition on Health in Rockford, Illinois, makes incentive payments to provider groups based on whether the group completes care flowsheets on 95 percent of its diabetic encounters and maintains hemoglobin A1c levels below 7.5 for the majority of patients. Incentive payments to medical groups have been approximately $28,000 per year ($3.60 per member per year) (Bailit Health Purchasing, 2002a)
-
Blue Shield of California has introduced a variable cost-sharing model under which patients pay either an additional $200 copayment or 10 percent of the hospital’s fee each time they are admitted to a hospital that is not on Blue Shield’s preferred list. Blue Shield rates hospitals on the basis of measures of quality, safety, patient satisfaction, and efficiency (Freudenheim, 2002)
-
General Motors’ value-based purchasing approach rates health plans according to their performance on various clinical quality measures, patient satisfaction measures, NCQA accreditation results, and cost-effectiveness measures, and adjusts employee out-of-pocket contributions so that those choosing the best-ranked plans have the lowest contributions (Salber and Bradley, 2001).
It may be hoped that much more will be known about the impact of various financial and non-financial incentive models in the near future. The Robert Wood Johnson Foundation (National Health Care Purchasing Institute, 2002) has recently announced an initiative entitled “Rewarding Results,” which will provide support for payment demonstrations that reward improvements in quality. This initiative is being evaluated under an Agency for Healthcare Research and Quality contract.
Program Design and Administration
Benefits coverage and payment methods are among the most important design features of the six government health care programs reviewed in this report, but they are not the only ones that influence the likelihood of patients receiving high-quality care. Other important features include delivery system and provider choices, fluctuations in eligibility and delivery system options, and administrative efficiency.
In some government health care programs, consumers have multiple options in terms of delivery system and choice of providers, while in others the options are more limited. Under Medicare, 87 percent of beneficiaries have chosen to enroll in FFS arrangements, which provide extensive choice of clinicians and hospitals. Most Medicare beneficiaries who live in metropolitan areas also have the option of enrolling in Medicare+Choice plans, enrollment that historically has been associated with enhanced benefits for little or no additional out-of-pocket expense. Enrollment in managed care is mandatory for the majority of the Medicaid population in most states, and in some instances, there is little or no choice of plan. DOD TRICARE, the VHA, and IHS programs are all structured to encourage, and in some cases require, use of their own health care delivery systems, which are similar to group or staff-model health plans.
Studies of the clinical quality (in terms of both medical care processes and patient outcomes) in managed care and indemnity settings consis-
tently find little or no difference between the two (Chassin and Galvin, 1998; Miller and Luft, 1993; Schuster et al., 1998). But it is clear that some consumers have strong preferences for one delivery system over another, and that most prefer to have choice (Gawande et al., 1998; Ullman et al., 1997). Limited choice of health plans may or may not seriously constrain the choice of clinicians and hospitals, since plan networks vary greatly in size and structure (Lake and Gold, 1999). In the private sector, there has been a pronounced trend in recent years toward larger networks of providers in response to consumer demand for more extensive choice (Draper et al., 2002; Lesser and Ginsburg, 2000). In the absence of comparative quality information on providers, consumers apparently equate choice with quality.
The design and financing of some government health care programs result in frequent changes in eligibility and delivery system options that disrupt patterns of care delivery. Since the implementation of changes in Medicare payment policies stemming from enactment of the Balanced Budget Act of 1997, there has been a steady erosion of health plans participating in the Medicare+Choice program. Since 1998, 2.2 million Medicare beneficiaries have been involuntarily disenrolled from Medicare+Choice plans, affecting approximately 5 percent of beneficiaries in 2002. Of the health plans that remain, the proportion offering prescription drug coverage during the period 1999 through 2002 dropped from 73 to 66 percent, and the proportion charging zero premiums to beneficiaries from 62 to 39 percent (Gold and McCoy, 2002). Under Medicaid, beneficiaries move in and out of the program as their eligibility changes in accordance with minor fluctuations in income, causing beneficiaries to lose contact with providers and further complicating the tracking of care. For many eligible children and women, the re-enrollment process is initiated only when they present themselves at a hospital or physician’s office seeking service for an illness; this process results in adverse selection in capitated plans.
Lastly, efforts must be made to reduce administrative burden. In recent years, there has been a steady growth in regulatory requirements in most if not all of the government health care programs. The Secretary’s Advisory Committee on Regulatory Reform estimates that about two regulations are published each week, resulting in the promulgation of more than 120 regulations in each of the last two years (Wood, 2002). The American Hospital Association (2002) has identified 100 new or revised regulations pertaining to hospitals that have been issued by federal agencies since 1997, of which 57 are significant. Some of these regulations relate to quality enhancement processes and data requirements, while others relate to such areas as payment, patient confidentiality and privacy, and fraud and abuse.
Regulatory oversight is necessary, but it must be balanced and effi-
cient. The current practice of promulgating separate regulations for each type of provider (e.g., hospital, home health agency, nursing home, ambulatory care provider) has produced excessive burdens and barriers to the provision of coordinated care. Unnecessary regulations frustrate clinicians and reduce the time available to devote to patient care. They can also interfere with the movement of individuals across settings, thus hampering the transition from hospital to nursing home to home health agency, for example.
Regulatory burden must also be fair. For example, the quality measurement and reporting requirements applied to Medicare+Choice plans should be applied to FFS Medicare institutional and individual providers. These issues are addressed further in Chapters 3 and 4.
In summary, while technically comprising separate areas of analysis, the issues of benefits, payment, program design, and administration are inextricably linked to achieving consistent levels of high-quality care.
REFERENCES
Administration on Aging. 2001. “Profile of Older Americans: 2000.” Online. Available at http://www.aoa.dhhs.gov/aoa/STATS/profile/default.htm. [accessed Aug. 3, 2001].
Agency for Health Care Administration. 2002. “Florida Medicaid Program: Summary of Services.” Online. Available at http://www.fdhc.state.fl.us/Medicaid/sos.pdf [accessed Apr. 8, 2002].
American Board of Internal Medicine, ACP-ASIM Foundation, and European Federation of Internal Medicine. 2002. Medical professionalism in the new millennium: a physician charter. Ann Intern Med 136 (3).
American Hospital Association. 2002. Patients or Paperwork? The Regulatory Burden Facing America’s Hospitals. Washington DC: PricewaterhouseCoopers for American Hospital Association.
Anderson, G. 2002. “Testimony Before the Subcommittee on Health of the House Committee on Ways and Means Hearing on Promoting Disease Management in Medicare.” Online. Available at http://waysandmeans.house.gov/health/107cong/4-16-02/4-16ande.htm [accessed May 3, 2002].
Anderson, G., M. A. Hall, and T. R. Smith. 1998. When courts review medical appropriateness. Med Care 36 (8):1295-302.
Anderson, G., and J. R. Knickman. 2001. Changing the chronic care system to meet people’s needs. Health Aff 20 (6):146-60.
Arizona Health Care Cost Containment System. 2002. “2001 AHCCCS Overview: Table of Contents.” Online. Available at http://www.ahcccs.state.az.us/Publications/Overview/2001/contents.asp [accessed Apr. 8, 2002].
Bailit Health Purchasing. 2002a. Ensuring Quality Health Plans: A Purchaser’s Toolkit for Using Incentives. Washington DC: National Health Care Purchasing Institute.
———. 2002b. Provider Incentive Models for Improving Quality of Care. Washington DC: National Health Care Purchasing Institute.
Berland, G. K., M. N. Elliott, L. S. Morales, J. I. Algazy, R. L. Kravitz, M. S. Broder, D. E. Kanouse, J. A. Munoz, J. A. Puyol, M. Lara, K. E. Watkins, H. Yang, and E. A. McGlynn. 2001. Health information on the Internet: accessibility, quality, and readability in English and Spanish. JAMA 285 (20):2612-21.
Biermann, S., G. Golladay, M. Greenfield, and L. Baker. 1999. Evaluation of Cancer Information on the Internet. Cancer 86 (3): 381-90.
Braddock III, C., K. Edwards, N. Hasenberg, T. Laidley, and W. Levinson. 1999. Informed decision making in outpatient practice: time to get back to basics. JAMA 282 (24):2313-20.
Bringewatt, R. 2001. Making a business case for high-quality chronic illness care. Health Aff (Millwood) 6 (20):59-60.
Center for Studying Health System Change. 2001. Community Tracking Study Physician Survey 1998-1999 [United States]. Washington DC: ICPSR.
Centers for Medicare and Medicaid Services. 1998. “A Profile of Medicare.” Online. Available at http://www.hcfa.gov/pubforms/chartbk.pdf [accessed Aug. 22, 2001].
Centers for Medicare and Medicaid Services. 1999. Medicare Standard Analytic File. Washington DC: U.S. Department of Health and Human Services.
Centers for Medicare and Medicaid Services. 2000a. “A Profile of Medicaid: Chartbook 2000.” Online. Available at http://www.hcfa.gov/stats/stats.htm [accessed Oct. 16, 2001a].
———. 2000b. “State Children’s Health Insurance Program (SCHIP) Aggregate Enrollment Statistics for the 50 States and the District of Columbia for Federal Fiscal Year (FFY) 2000.” Online. Available at http://www.hcfa.gov/init/fy2000.pdf [accessed Oct. 16, 2001b].
———. 2000c. “Medicare Profile Chart Book from the 35th Anniversary Event.” Online. Available at http://www.hcfa.gov/stats/stats.htm [accessed Oct. 16, 2001c].
———. 2000d. “Operational Policy Letter #126 re: Reconciliation of Calendar Year (CY) 2000 Payments Based on Changes in Risk Adjuster Factors/Enhanced Monthly Membership Reporting.” Online. Available at http://www.hcfa.gov/medicare/opl126.htm [accessed Apr. 10, 2002d].
———. 2001a. “Nursing Home Compare - Home.” Online. Available at http://www.medicare.gov/NHCompare/home.asp [accessed May 6, 2002a].
———. 2001b. “Your Medicare Benefits.” Online. Available at http://www.medicare.gov/Publications/Pubs/pdf/yourmb.pdf [accessed Apr. 8, 2002b].
———. 2001c. “Fact Sheet: Center for Medicaid and State Operations; Medicaid and Acquired Immunodeficiency Syndrome (AIDS) and Human Immunodeficiency Virus (HIV) Infection.” Online. Available at http://www.hcfa.gov/medicaid/obs11.htm [accessed Aug. 15, 2001c].
———. 2002a. “State Children’s Health Insurance Program: Fiscal year 2001 annual enrollment report.” Online. Available at http://www.cms.hhs.gov/schip/schip01.pdf [accessed June 28, 2002a].
———. 2002b. “Program Information on Medicare, Medicaid, SCHIP, and other programs of the Centers for Medicare & Medicaid Services.” Online. Available at http://cms.hhs.gov/charts/series/sec3-b1.pdf [accessed Aug. 14, 2002b].
———. 2002c. “Where the Nations’s Health Dollar Came From and Where it Went.” Online. Available at http://cms.hhs.gov/statistics/nhe/historical/chart.asp [accessed Sept. 26, 2002c].
Chassin, M., and R. Galvin. 1998. The urgent need to improve health care quality: Institute of Medicine National Roundtable on Quality. JAMA 280 (11):1000-05.
Clark, C. 2000. Promoting early diagnosis and treatment of type 2 diabetes. Journal of the American Medical Association 284 (3):363-65.
Connecticut Department of Social Services. 2002. “State of Connecticut Department of Social Services.” Online. Available at http://www.dss.state.ct.us [accessed Apr. 8, 2002].
Consumers Union/California Healthcare Foundation Partnership. 2002. “Guide to California Medicare HMOs: All Medicare HMOs are NOT alike.” Online. Available at http://admin.chcf.org/documents/hmoguide/GuideToCaliforniaMedicareHMOs.pdf [accessed May 6, 2002].
Deber, R., N. Kraetschmer, and J. Irvine. 1996. What role do patients wish to play in treatment decision making? Arch Int Med 156 (1414-20).
Degner, L., and C. Russell. 1988. Preferences for treatment control among adults with cancer. Res Nurs Health 11:367-74.
Department of Health and Human Services. 1997. “State Children’s Health Insurance Program homepage.” Online. Available at http://www.hcfa.gov/init/children.htm [accessed Apr. 5, 2002].
———. 2000. Secretary of the Department of Health and Human Services, Report to Congress: Safeguards for Individuals with Special Health Care Needs Enrolled in Medicaid Managed Care. Washington DC: U.S. Department of Health and Human Services.
———. 2002. 2002 CMS Statistics. CMS Publication No. 03437. Baltimore MD: U.S. Department of Health and Human Services.
Draper, D. A., R. E. Hurley, C. S. Lesser, and B. C. Strunk. 2002. The changing face of managed care. Health Aff (Millwood) 21 (1):11-23.
Ellis, R., G. Pope, L. Iezzoni, et al. 1996. Diagnosis-based risk adjustment for Medicare capitation payments. Health Care Financ Rev 17 (3):101-28.
Emanuel, E., and L. Emanuel. 1992. Four models of the physician-patient relationship. JAMA 267 (16):2221-6.
Federman, A. D., A. S. Adams, D. Ross-Degnan, S. B. Soumerai, and J. Z. Ayanian. 2001. Supplemental insurance and use of effective cardiovascular drugs among elderly Medicare beneficiaries with coronary heart disease. JAMA 286 (14):1732-39.
Foote, S., and L. Etheredge. 2002. Strategies to Improve Consumer Health Information Services. Health Insurance Reform Project. Washington DC: The George Washington University.
Fox, D., and J. Gruman, Milbank Memorial Fund and Center for the Advancement of Health. 1999. “ Patients as Effective Collaborators in Managing Chronic Conditions.” Online. Available at http://www.milbank.org/990811chronic.html [accessed 2001].
Freudenheim, M. June 26, 2002. Quality goals in incentives for hospitals. New York Times. Sect. Late Edition: Final, Section C, Page 1, Column 5.
Gawande, A. A., R. Blendon, M. Brodie, J. M. Benson, L. Levitt, and L. Hugick. 1998. Does dissatisfaction with health plans stem from having no choices? Health Aff (Millwood) 17 (5):184-94.
Gifford, A. L., D. D. Laurent, V. M. Gonzales, M. A. Chesney, and K. R. Lorig. 1998. Pilot randomized trial of education to improve self-management skills of men with symptomatic HIV/AIDS. J Acquir Immune Defic Syndr Hum Retrovirol 18 (2):136-44.
Gluck, M., and K. W. Hanson. 2001. Medicare Chart Book. Menlo Park CA: Henry J. Kaiser Family Foundation.
Gold, M., and J. McCoy. 2002. Monitoring Medicare and choice: fast facts. Choice continues to erode in 2002. Mathematica Policy Research 7:1-2.
Guadagnoli, E., and P. Ward. 1998. Patient participation in decision-making. Soc Sci Med 47 (3):329-39.
Health Care Financing Administration. 2000. A Profile of Medicaid: Chart Book. Baltimore MD : U.S. Department of Health and Human Services.
Healthy Futures Partnership for Quality Project. 2002. Healthy Futures and the Maine Center for Public Health, unpublished paper.
Ho, S. (Pacificare). 13 May 2002. Provider quality index. Personal communication to Janet Corrigan.
Hoffman, C., D. Rice, and H. Sung. 1996. Persons with chronic conditions. Their prevalence and costs. JAMA 276 (18):1473-79.
Hornbrook, M., and M. Goodman. 1996. Chronic disease, functional health status, and demographics: a multi-dimensional approach to risk adjustment. Health Serv Res 31 (3):283-307.
IDEATel. 2002. “Informatics for Diabetes Education and Telemedicine.” Online. Available at http://www.ideatel.org/info.html [accessed July 30, 2002].
Indian Health Service. 2001. “Indian Health Service: Customer Services.” Online. Available at http://www.ihs.gov/GeneralWeb/HelpCenter/CustomerServices/approp.asp [accessed Aug. 14, 2002].
———. 2002. “Indian Health Service Homepage.” Online. Available at http://www.ihs.gov [accessed Feb. 14, 2002].
Institute for the Future. 2000. Health and Health Care, 2010: The Forecast, the Challenge. Based on 1998 data provided by the Department of Finance, State of California. San Francisco CA: Institute for the Future.
Institute of Medicine. 2000. Protecting Those Who Serve: Strategies to Protect the Health of Deployed U.S. Forces. Washington DC: National Academy Press.
———. 2001. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington DC: National Academy Press.
Jennings, B. (TMA). September 2001. TRICARE. Personal communication to Barbara Smith.
Joint National Committee on Prevention. 1997. Detection, evaluation, and treatment of high blood pressure, Sixth Report. Arch Intern Med 157 (21):2413-46.
Kizer, K. 1999. The new VA: a national laboratory for health care quality management. Am J Med Qual 14 (1):3-20.
Lake, T., and M. Gold. 1999. Health plan selection and payment of health care providers. Washington DC: MedPAC.
Landro, L. Nov. 12, 2001. Getting reliable health information. Wall Street Journal.
Legorreta, A. P., X. Zaher, C. A. Liu, and D. E. Jatulis. 2000. Variation in managing asthma: experience at the medical group level in California. Am J Manag Care 6 (4):445-53.
Lesser, C. S., and P. B. Ginsburg. 2000. Update on the nation’s health care system: 1997-1999. Health Aff (Millwood) 19 (6):206-16.
Lindberg, D., and B. Humphreys. 1999. A time for change for medical informatics in the USA. Yearbook of Medical Informatics 53 (7).
Lorig, K., P. Mazonson, and H. Holman. 1993. Evidence suggesting that health education for self management in chronic arthritis has sustained health benefits while reducing health care costs. Arthritis Rheumatism 36 (4):439-46.
Lorig, K. R., D. S. Sobel, A. L. Stewart, B. W. Brown Jr, A. Bandura, P. Ritter, V. M. Gonzalez, D. D. Laurent, and H. R. Holman. 1999. Evidence Suggesting that a Chronic Disease Self-Management Program Can Improve Health Status While Reducing Hospitalization: A Randomized Trial. Med Care 37 (1):5-14.
Luft, H. 1995. Potential methods to reduce risk selection and its effects. Inquiry 32:23-32.
Maguire, A. M., N. R. Powe, B. Starfield, J. Andrews, J. P. Weiner, and G. F. Anderson. 1998. “Carving out” conditions from global capitation rates: protecting high-cost patients, physicians, and health plans in a managed care environment. Am J Manag Care 4 (6):797-806.
Mazur, D. J., and D. H. Hickam. 1997. Patients’ preferences for risk disclosure and role in decision making for invasive medical procedures. J Gen Intern Med 12 (2):114-17.
Medical Expenditure Panel Survey. 1996. CCS clinical conditions from MEPS, 1996; for persons with primary medicaid coverage during year, all ages; estimated number of persons with medicaid coverage: sorted by total cost of chronic condition.
———. 1998. Counts and expenditures for specific conditions; MEPS 1998 data.
Miller, R., and H. Luft. 1993. Managed care: past evidence and potential trends. Front Health Serv Manage 9 (3):3-37.
Montenegro-Torres, B., T. Engelhardt, M. Thamer, and G. Anderson. 2001. Are Fortune 100 companies responsive to chronically ill workers? Health Aff 20 (4):209-19.
Moon, M., and M. Storeygard. 2001. One-Third at Risk: The Special Circumstances of Medicare Beneficiaries with Health Problems. New York NY: The Commonwealth Fund.
National Committee for Quality Assurance. 2002. “NCQA Report Cards.” Online. Available at http://hprc.ncqa.org/menu.asp [accessed May 6, 2002].
National Health Care Purchasing Institute. 2002. “Rewarding Results.” Online. Available at http://www.nhcpi.net/rewardingresults/index.cfm [accessed Apr. 22, 2002].
Newacheck, P. W., and N. Halfon. 1998. Prevalence and impact of disabling chronic conditions in childhood. Am J Public Health 88 (4):610-7.
Newhouse, J., M. Buntin, and J. Chapman. 1997. Risk adjustment and Medicare: taking a closer look. Health Aff (Millwood) 16 (5):26-43.
Partnerships for Solutions. forthcoming. Medicare Expenditures Increase with the Number of Chronic Conditions; 1996 MEPS data. Baltimore MD: John Hopkins University.
Rosenbach, M., M. Ellwood, J. Czajka, C. Irvin, W. Coupe, and B. Quinn. 2001. Implementation of the State Children’s Health Insurance Program: Momentum is Increasing After a Modest Start. Princeton, NJ: Mathematica Policy Research, Inc.
Rosenbaum, S., and B. M. Smith. 2001. Policy Brief #1: State SCHIP Design and The Right to Coverage. Washington, D.C.: Center for Health Services Research and Policy, George Washington University School of Public Health.
Salber, P., and B. Bradley. 2001. “Perspective: Salber and Bradley Web Exclusive.” Online. Available at http://www.healthaffairs.org/WebExclusives/Salber_Bradley_Perspective_Web_Excl_112801.htm [accessed Aug. 14, 2002].
Schuster, M. A., E. A. McGlynn, and R. H. Brook. 1998. How good is the quality of health care in the United States? Milbank Q 76 (4):517-63.
Starfield, B., J. Weiner, L. Mumford, and D. Steinwachs. 1991. Ambulatory care groups: a categorization of diagnoses for research and management. Health Serv Res 26 (1):53-74.
Stevens, R. 1989. In Sickness and Wealth: American Hospitals in the 20th Century. New York: Basic Books, Inc.
Stewert, M. 1995. Effective physician-patient communication and health outcomes: a review. Can Med Assoc J 152 (9):1423-33.
Stoddard, J., J. Grossman, and L. Rudell. 2002. Physicians More Likely to Face Quality Incentives Than Incentives That May Restrain Care. Washington DC: Center for Studying Health System Change.
Strull, W., B. Lo, and G. Charles. 1984. Do patients want to participate in medical decision-making? JAMA 252 (21):2990-2994.
Strunk, B., P. Ginsburg, and J. Gabel. 2002. “Data Bulletin No. 22: tracking health care cost. Hospital spending spurs double-digit increase in 2001.” Online. Available at http://www.hschange.com/CONTENT/472/ [accessed Sept. 26, 2002].
Superio-Cabuslay, E., M. Ward, and K. Lorig. 1996. Patient education interventions in osteoarthritis and rheumatoid arthritis: a meta-analytic comparison with non-steroidal antiinflammatory drug treatment. Arthritis Care Res 9 (4):292-301.
TRICARE. 2002. “TRICARE Homepage.” Online. Available at http://www.tricare.osd.mil/ [accessed Apr. 3, 2002].
U.S. Government Printing Office. 2001. National Diabetes Education Program. “Changing the Way Diabetes is Treated.” Washington DC: U.S. Government Printing Office.
———. 2002. “Chapter 4 Promoting Health Care Quality and Access.” Economic Report of the President.
Ullman, R., J. W. Hill, E. C. Scheye, and R. K. Spoeri. 1997. Satisfaction and choice: a view from the plans. Health Aff (Millwood) 16 (3):209-17.
Van Diepen, L. (VA). 19 July 2001a. VA Stats. Personal communication to Barbara Smith.
Van Diepen, L. (VA). 14 August 2001b. RE: # VA hospitals. Personal communication to Elaine Swift.
Van Korff, M., E. Moore, K. Lorig, D. C. Cherkin, K. Saunders, V. M. Gonzalez, D. Laurent, C. Rutter, and F. Comite. 1998. A randomized trial of a lay person-led self-management group intervention for back pain patients in primary care. Spine 23 (23):2608-51.
Veterans Administration. 2001a. “Enrollment in VA’s Health Care System: Eligibility.” Online. Available at http://www.va.gov/health/elig/eligibility.html [accessed May 3, 2001a].
———. 2001b. “Facts about the Department of Veterans Affairs.” Online. Available at http://www.va.gov/pressrel/vafact01.htm [accessed Apr. 3, 2002b].
Von Korff, M., J. Gruman, J. Schaefer, S. Curry, and E. Wagner. 1997. Collaborative management of chronic illness. Ann Intern Med 127 (1097-1102).
Wagner, E., B. Austin, and M. Von Korff. 1996. Organizing care for patients with chronic illness. Milbank Q 74 (4):511-42.
Wagner, E. H., B. T. Austin, C. Davis, M. Hindmarsh, J. Schaefer, and A. Bonomi. 2001. Improving chronic illness care: translating evidence into action. Health Aff (Millwood) 20 (6):64-78.
Westmoreland, T., Federal Legislation Clinic of Georgetown University Law Center, Prepared for The Henry J. Kaiser Family Foundation. 1999. “KFF: Medicaid and HIV/ AIDS Policy: A Basic Primer (pdf).” Online. Available at http://www.kff.org/content/1999/2136/1891-KFF.pdf [accessed Apr. 1, 2002].
Wood, D. L. (Chair, Secretary’s Advisory Committee on Regulatory Reform). 10 August 2002. Final Report, to be issued in October 2002. Personal communication to Janet Corrigan.
Young, A. S., R. Klap, C. D. Sherbourne, and K. B. Wells. 2001. The quality of care for depressive and anxiety disorders in the United States. Arch Gen Psychiatry 58 (1):55-61.




























