Chapter 3
Priority Areas for Quality Improvement
The committee’s deliberations led to the selection of 20 priority areas for health care quality improvement:
-
Care coordination (cross-cutting)
-
Self-management/health literacy (cross-cutting)
-
Asthma—appropriate treatment for persons with mild/moderate persistent asthma
-
Cancer screening that is evidence-based—focus on colorectal and cervical cancer.
-
Children with special health care needs1
-
Diabetes—focus on appropriate management of early disease
-
End of life with advanced organ system failure—focus on congestive heart failure and chronic obstructive pulmonary disease
-
Frailty associated with old age—preventing falls and pressure ulcers, maximizing function, and developing advanced care plans
-
Hypertension—focus on appropriate management of early disease
-
Immunization—children and adults
-
Ischemic heart disease—prevention, reduction of recurring events, and optimization of functional capacity
-
Major depression—screening and treatment
-
Medication management—preventing medication errors and overuse of antibiotics
-
Nosocomial infections—prevention and surveillance
-
Pain control in advanced cancer
-
Pregnancy and childbirth—appropriate prenatal and intrapartum care
-
Severe and persistent mental illness—focus on treatment in the public sector
-
Stroke—early intervention and rehabilitation
-
Tobacco dependence treatment in adults
-
Obesity (emerging area)2
The committee made no attempt to rank order the priority areas selected. The first 2 listed above—care coordination and self-management/health literacy—are cross-cutting areas in which improvements would benefit a broad array of patients. The 17 that follow represent the continuum of care across the life span and are relevant to preventive care, inpatient/surgical care, chronic conditions, end-of-life care, and behavioral health, as well as to care for children and adolescents. Finally, obesity is included as an “emerging area” that does not at this point satisfy the selection criteria as fully as the other 19 priority areas.
This chapter first reviews the breadth of opportunities for health care improvement represented by the committee’s recommended list of priority areas. The three types of areas included on the list—cross-cutting areas, specific conditions, and emerging areas—are then described. The chapter next profiles each area in detail, including the aim of intervention in that area and the rationale for the area’s selection in light of the three criteria discussed in Chapter 2—impact, improvability and inclusiveness.
Breadth of Opportunities Represented by Priority Areas
The priority areas selected by the committee can be viewed through a variety of lenses. They represent a range of health care services and challenges, including:
-
The full spectrum of health care, from preventive and acute care, to chronic disease management, to long-term and palliative care at the end of life. Thus they encompass a wide variety of health care services, spanning both reactive acute, emergency, and surgical care and the proactive planned care required to prevent and manage chronic disease, pain, and disability.
-
Care provided for a variety of populations representing Americans of all ages and demographic groups, including care that is oriented to individuals and families, as well as populations.
-
Care delivered in a range of publicly and privately financed ambulatory and inpatient health care settings (outpatient and community health centers, home-based care, emergency departments, hospitals, and nursing homes) by a variety of health care practitioners (physicians, nurses, pharmacists, allied health professionals), including both generalists and specialists.
The Full Spectrum of Health Care
As noted, the priority areas recommended by the committee represent health care quality improvement challenges and opportunities across the full spectrum of health care. In fact, having relevance to multiple domains of care strengthened an area’s chances of being included on the final list. Boxes 3–1 to 3–6 show how the priority areas relate to a wide range of health care needs. For example, ischemic heart disease figures prominently in preventive care, inpatient/surgical care, chronic
care, and end-of-life care. Similarly, medication management cuts across inpatient/ surgical care, chronic care, end-of-life care, and child/adolescent care. Obesity—the emerging area—touches on preventive care, chronic care, behavioral health, and child/adolescent care.
The Entire Life Span
The committee made a concerted effort to ensure that the priority areas selected would represent issues pertinent to all age groups. Figure 3–1 shows how the priority areas cut across the stages of a typical life span. As demonstrated, only a few areas are unique to certain age groups, such as children with special health care needs and frailty prevention and management. Many areas, such as cancer screening and hypertension, cluster around adulthood and extend into end of life. Additionally, nine of the priority areas encompass the entire life span.
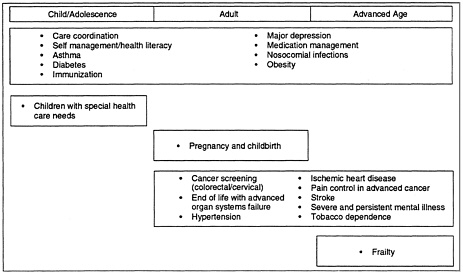
Figure 3–1: Priority areas across the life span.
Diverse Health Care Settings and Professions
The set of priority areas recommended by the committee involves care that is provided in multiple health care settings and organizations, care that is both privately and publicly funded, and care that is provided by a variety of health care professionals. For example, effective asthma management requires integration of care among primary care providers, pediatricians, schools, hospitals (particularly emergency rooms), and pharmacists. Adequate pain control in advanced cancer and stroke rehabilitation require a continuum of care that includes home, community, clinic, and hospital. Improving quality of care for severe and persistent mental illness, such as psychosis, provides an opportunity to focus on the effectiveness of mental health services provided by the public sector (Narrow et al., 2000; Wells, 2002a). To close the gaps between best practice and usual care for the full set of proposed areas will require the collective expertise of a vast array of doctors, nurses, pharmacists, allied health professionals, social workers, and vested laypersons. Virtually every conventional medical specialty will need to develop strategies for one or more of these priority areas.
|
Box 3–1 Priority Areas That Relate to Preventive Care
|
|
Box 3–2 Priority Areas That Relate to Behavioral Health
|
|
Box 3–3 Priority Areas That Relate to Chronic Conditions
|
|
Box 3–4 Priority Areas That Relate to End of Life
|
|
Box 3–5 Priority Areas That Relate to Children and Adolescents
|
|
Box 3–6 Priority Areas That Relate to Inpatient/Surgical Care
|
Three Types of Priority Areas
Cross-Cutting Areas
There was strong consensus among the committee members on the critical need to improve care coordination, support for self-management, and health literacy for all patients and their families. System and policy changes to achieve improvement in these cross-cutting priority areas would involve most health care organizations and practitioners, could impact all types of conditions, and could provide a means of dramatically improving health care for all Americans.
Improved care coordination would, if applied broadly, have an especially important impact on improving health care processes and outcomes for children and adults with serious chronic illness and multiple chronic conditions (Anderson and Knickman, 2001; Anderson, 2002b). Efforts to improve health literacy are in turn essential for effective self-management and collaborative care. For example, a recent study found that diabetics with poor health literacy, unable to read and/or comprehend directions on their pill bottles, had worse blood sugar control and higher rates of preventable vision impairment (Schillinger et al., 2002). Devising strategies to improve health literacy—both at the micro level, where patients and health care professionals interact, and at the macro level, where population health is the target—would not only improve diabetes outcomes, but also form part of a package of improvements for nearly all inadequate aspects of health care.
Specific Priority Conditions
Chronic Care
In keeping with the Quality Chasm report, which notes the critical need to close quality gaps for the growing numbers of Americans with chronic disease (Institute of Medicine, 2001a), the majority of the specific priority conditions recommended are chronic. For all of the recommended conditions, such as diabetes, hypertension, and ischemic heart disease, there are known, effective interventions that can be applied to improve health outcomes, reduce disease burden, and prevent more serious health problems later in life. Moreover, the enormous and rapid growth in the prevalence and burden of chronic disease over the past two decades has been a major force in clarifying the limitations of the current health care system—which evolved primarily to meet acute and emergency health care needs—thus motivating broad action for health care system redesign (Bodenheimer et al., 2002; Institute of Medicine, 2001a).
Acute Care
One priority area within the realm of acute care—effective medication management— focuses on preventing medication errors and the overprescribing of antibiotics, particularly for acute respiratory infections in children. This area provides an excellent opportunity for designing interventions that can enhance the use and capacity of management information systems. For example, lecturing to physicians about medical errors yields small gains, but technological advances, such as the electronic medical record tied to computerized medication orders with acceptable dosage ranges and interactions, can dramatically reduce errors arising from incorrect orders (Bates et al., 1999; Kaushal et al., 2001). Computerized alerts of potential drug interactions, prompts and reminders for required services, and electronic physician order entry for prescriptions could all be put in place to safeguard health and improve quality of care (Hunt et al., 1998). Corrective measures that redesign work so that errors are “engineered out” are repeatedly found to have high leverage.
Preventive Care
The committee explicitly included preventive services among the domains of health care that should be represented by the priority areas. Doing so reflected a growing body of evidence that early detection and timely
intervention for risk factors or diseases in their preclinical stages are effective in reducing both disease burden and costs. Selected priority areas represent a range of clinical preventive services involving immunization, screening, and counseling for lifestyle changes, which would singly and collectively reduce morbidity and mortality due to the nation’s leading chronic illnesses and infectious disease threats. Specifically, childhood/adult immunization, improved screening for colorectal and cervical cancers, and brief primary care interventions for adult tobacco dependence have been identified as major opportunities for cost-effective improvements in the nation’s health care system (Coffield et al., 2001).
For example, just 3–5 minutes of counseling and medication advice given to adult smokers by their physician could more than double the quitting success rates smokers achieve on their own (Fiore et al., 2000). Since there are over 430,000 tobacco-related deaths each year from heart disease, stroke, lung cancer, and chronic lung disease among U.S. adults, the impact of this simple intervention, combined with other effective modes of tobacco treatment, would be dramatic (Max, 2001; United States Department of Health and Human Services, 2000).
Unfortunately, only about 50 percent of patients who smoke receive such advice and assistance, largely because supports such as office-based reminder systems and insurance coverage for smoking cessation services are not widely in place (Goodwin et al., 2001; Thorndike et al., 1998). Treating tobacco dependence is critical to preventing disease in healthy populations of smokers, the progression of illnesses caused by tobacco use, poor pregnancy outcomes associated with smoking, and pediatric asthma in infants and adolescents whose parents smoke. Furthermore, there is growing evidence that the types of system and policy changes needed to spur broader use of evidence-based tobacco interventions are similar to those required to support the wider delivery of other proven interventions for changes in health behavior in primary care, such as counseling on physical activity and diet and on the importance of reducing risky consumption of alcohol (Glasgow et al., 2001).
Palliative Care
Between 2010 and 2030, America’s baby boomers will move beyond the age of 65 and swell the number of older persons to approximately 70 million, representing 20 percent of the population (Administration on Aging, 2002). Accordingly, the committee placed particular emphasis on addressing the complex care issues that surface after age 65 and particularly after age 80. One of the priority areas in the category of palliative care is frailty. Nearly everyone who survives past age 80 experiences a period of frailty involving decreased functional status as a result of multiple health problems, such as heart and lung disease, as well as cognitive deficits resulting from dementia or stroke. As more and more Americans face the physical and social challenges of frailty, systems of care must adapt in ways that allow them to live comfortably and safely at home. Advanced care plans should be put in place that are respectful of both the patient’s and family’s wishes. This priority area can serve as an exemplar for health care quality improvements that incorporate changes at various levels of the health care delivery system to provide integrated, dignified care for those of advanced age.
Emerging Areas
Obesity was intentionally placed last on the committee’s list and classified as an “emerging area.” The prevalence of overweight and obesity among Americans has reached epidemic proportions (Mokdad et al., 2001; Yanovski and Yanovski, 2002). Obesity represents an important medical condition in its own right and contributes to morbidity and mortality for other diseases, including heart disease, type II diabetes, osteoarthritis, hypertension, and cancer. Addressing growing rates of obesity and obesity-related disease in children and adults has been identified as an urgent national health care priority (Squires, 2001).
Obesity was selected as a priority area based on strong evidence for its impact and inclusiveness, but still emerging evidence for improvability. That is, there was relatively limited evidence for the efficacy of existing best-practice treatments for obesity in children and adults, such as behavioral counseling and drug and surgical interventions (Epstein et al., 2001). In addition, effective treatment for obesity will need to integrate many other aspects of society, such as housing, exercise opportunities, food supply, and work patterns, often considered outside the traditional realm of health care.
The committee’s aim in denoting obesity as “emerging” was to accelerate the rate at which research generates the evidence needed to identify effective interventions and to develop evidence-based treatment guidelines and valid performance measures. Since this area would serve as a model for potential future emerging priority areas, formal reviews of progress on obesity would be conducted more frequently than for other priority areas, perhaps as often as yearly, to determine future directions.
Priority Areas: Detailed Descriptions
The following brief descriptions are intended as illustrative rather than exhaustive profiles for each of the 20 recommended priority areas. The committee’s goal was to provide a starting point for experts in the field to undertake effective national health care quality improvement efforts over the next 3 to 5 years. Each priority area is discussed with reference to the committee’s three selection criteria—impact, improvability, and inclusiveness. A vignette is also provided for selected areas to illustrate how a transformed health care system would provide quality care in that area.
Care Coordination
Aim
To establish and support a continuous healing relationship, enabled by an integrated clinical environment and characterized by the proactive delivery of evidence-based care and follow-up. Clinical integration is further defined as “the extent to which patient care services are coordinated across people, functions, activities, and sites over time so as to maximize the value of services delivered to patients” (Shortell et al., 2000:129).
Rationale for Selection
Impact
Nearly half of the population—125 million Americans—lives with some type of chronic condition. About 60 million live with multiple such conditions. And more than 3 million—2.5 million women and 750,000 men—live with
SOURCE: Reprinted with permission from Gerard Anderson, Ph.D. (2002).
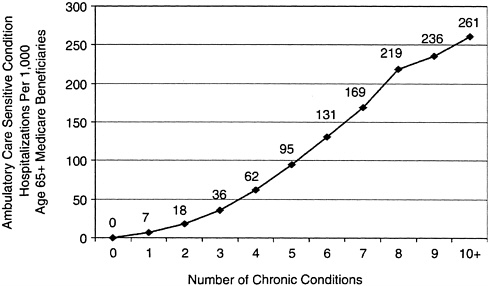
Figure 3–2. Hospitalizations among Medicare beneficiaries with multiple chronic conditions.
five such conditions (Partnership for Solutions, 2001). For those afflicted by one or more chronic conditions, coordination of care over time and across multiple health care providers and settings is crucial. Yet in a survey of over 1,200 physicians conducted in 2001, two-thirds of respondents reported that their training was not adequate to coordinate care or education for patients with chronic conditions (Partnership for Solutions, 2001).
More than 50 percent of patients with hypertension (Joint National Committee on Prevention, 1997), diabetes (Clark et al., 2000), tobacco addition (Perez-Stable and Fuentes-Afflick, 1998), hyperlipidemia (McBride et al., 1998), congestive heart failure (Ni et al., 1998), chronic atrial fibrillation (Samsa et al., 2000), asthma (Legorreta et al., 2000), and depression (Young et al., 2001) are currently managed inadequately. Among the Medicare-eligible population, the average beneficiary sees 6.4 different physicians in a year, 4.6 of those being in the outpatient setting (Anderson, 2002a).
Among this same population, as the number of chronic conditions a person has increases, so, too, does the number of hospitalizations that are inappropriate or avoidable because outpatient treatment would have been effective: from 7 per 1,000 for those with one chronic condition to 95 per 1,000 for those with five chronic conditions and 261 per 1,000 for those with ten or more such conditions (Anderson, 2002a). See Figure 3–2.
Improvability
In a randomized controlled trial of 970 patients with diabetes cared for by over 450 primary care providers, usual care was compared with a program utilizing regular follow-up, decision support, reminder systems, and modern self-management support. After 6 years, patients in the intervention group had significantly better outcomes, including lower HbAlc, blood pressure, and cholesterol levels (Olivarius et al., 2001). A recent review of ambulatory-care diabetic management programs found that patient education and an expanded role for a nurse in the intervention strategy also improved patient outcomes (Renders et al., 2001).
According to a meta-analysis of adult immunization and cancer screening programs, interventions that had the largest impact involved organizational changes, such as the use of a planned care visit for prevention, and designation of nonphysician staff to carry out specific prevention activities (Stone et al., 2002). There is also a growing body of evidence that planned (e.g., proactive, structured) care at set intervals makes a difference, and can be accomplished using nonstandard models, such as group visits (Beck et al., 1997; Sadur et al., 1999).
The Chronic Care Model, described in Chapter 1, provides a structure for planned, clinically integrated care. There are promising indications that a wide variety of health systems can reorganize themselves to deliver such care (The National Coalition on Health Care and the Institute for Healthcare Improvement, 2002; Wagner et al., 2001a).
Inclusiveness
The Institute of Medicine’s 2002 report Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care documents racial and ethnic disparities in several of the priority areas recommended in this report, all of which could benefit from a more integrated approach to care. These areas include children with special health care needs, diabetes, end of life with advanced organ system failure, frailty, pregnancy and childbirth, and severe and persistent mental illness (Institute of Medicine, 2002).
|
Box 3–7 Care Coordination One participating organization, Care Management Group of Greater NY, Inc. (CMGNY), in the Institute for Healthcare Improvement and The Robert Wood Johnson Foundation’s National Program on Improving Chronic Illness Care incorporated the elements of the Chronic Care Model to enhance recognition and treatment of depression in patients with congestive heart failure. This collaborative is an excellent example of how effective care coordination, or clinical integration of services, improved health outcomes for the chronically ill, particularly for patients with multiple chronic conditions. First, there was strong organizational support from key leaders at CMGNY, a subsidiary of the North Shore Long Island Jewish Health System. Second, clinical information systems were used to extract claims data and a disease registry was built to identify patients within the plan who had been diagnosed with congestive heart failure (CHF). Physicians participating in the program were given the names of their CHF patients for systematic screening for depression. Patients with recent hospitalizations, patients identified through care management, and patients whose annual costs exceeded $50,000 per year, were all targeted for depression assessment as well. Third, decision support was provided at many levels. Physicians within the plan were invited to attend “managed care college” where they were trained to recognize the classic signs of depression and coached to administer the Patient Health Questionnaire (PAQ), a screening tool for depression. Notably, clinicians were given financial incentives for incorporating the PAQ into their daily practice. Additionally, primary care physicians had access to a psychiatrist by telephone for consultation regarding medication dosage and depression management. Fourth, a nurse practitioner used telephone self-management support techniques to facilitate partnerships between patients and their providers. The hallmark of this relationship was active listening and empathy with the overarching goal to educate the patient about their condition and to monitor and encourage adherence to their treatment plan, including medications and appointments. In addition, goal-setting strategies were developed with the patient to encourage exercise and engagement in pleasant events as well as to resolve treatment-emergent problems such as side effects from antidepressant medications, attitudinal issues and social barriers. Fifth, the overall delivery of care was redesigned to incorporate elements of the chronic illness care model, including care management, decision support and development of community relationships. This included providing services outside the doctor’s office such as home health evaluations, home psychiatric evaluations, physical therapy and a home health aide. A nurse practitioner figured prominently in coordinating, monitoring and following-up of care. Lastly, patients were linked with community resources both on the local and national level. Outcomes from this study were dramatic. After 6 months a 50 percent or greater improvement in depression severity was observed among participants. In the words of one patient with CHF who was clinically depressed and on 20 medications “you have turned my life around” (Cole et al., 2002; Cole, 2002). |
Self-Management/Health Literacy
Aim
To ensure that the sharing of knowledge between clinicians and patients and their families is maximized, that the patient is recognized as the source of control, and that the tools and system supports that make self-management tenable are available.
Self-management support is defined as the systematic provision of education and supportive interventions to increase patients’ skills and confidence in managing their health problems, including regular assessment of progress and problems, goal setting, and problem-solving support. Health literacy is defined as the ability to read, understand, and act on health care information. Specifically, improvement in this area encompasses four features of successful programs: (1) providers communicate and reinforce patients’ active and central role in managing their illness; (2) practice teams make regular use of standardized patient assessments; (3) evidence-based programs are used to provide ongoing support; and (4) collaborative care planning and patient-centered problem solving result in an individualized care plan for each patient and support from the team when problems are encountered (Glasgow et al., 2002).
Rationale for Selection
Impact
According to the National Adult Literacy Survey, 40–44 million of the 191 million adults (21 percent) in the United States are functionally illiterate: they read at or below the fifth-grade level or cannot read at all (American Medical Association, 2002). Another 50 million adults (25 percent of adult Americans) are marginally literate: they are able to locate and assimilate information in a simple text, but are unable to perform tasks that require them to assimilate or synthesize information from complex or lengthy texts (American Medical Association, 2002). The Journal of the American Medical Association reported in 1999 that 46 percent of American adults are functionally illiterate in dealing with the health care system (American Medical Association, 2002). Patients with low literacy are frequently ashamed and hide it. A 1996 study of patients with reading difficulty confirmed that 67 percent had never told their spouse and 19 percent had never told anyone about their reading problem (American Medical Association, 2002).
People with low literacy skills have to rely on remembering what health professionals tell them. Recall of medical instructions is often poor; one study showed that people remembered only 14 percent of spoken instructions for managing fever or sore throat (Pfizer, 1998). A 1997 study of patients in two public hospitals found that those with inadequate literacy skills were five times more likely to misinterpret their prescriptions than patients with adequate reading skills, and averaged two more doctor visits per year than those with marginal or adequate literacy skills (American Medical Association, 2002). In one study, 23 percent of English-speaking and 34 percent of Spanish-speaking respondents were found to have an inadequate ability to read and comprehend medical information in their spoken language. Furthermore, of those with low ability to read medical information, only 55 percent reported having someone in their household who could read for them (Pfizer, 1998).
The estimated additional health care expenditures due to low health literacy skills total about $73 billion. Employers may be financing as much as 17 percent of these additional expenditures (American Medical Association, 2002).
Improvability
Self-management support is critical because patients and their families are the primary caregivers in chronic illness (Von Korff et al., 1997). There is evidence that in the current system, even minimal health education is inadequate for people with chronic illness: just 45 percent of persons with diabetes received
formal education on managing their condition in 1998; 42 percent of patients with a diagnosis of cardiovascular disease, diabetes, or hyperlipidemia received counseling or education on diet and nutrition in 1997; and 8.4 percent of patients with asthma received formal patient education in 1998 (United States Department of Health and Human Services, 2000). However, more than education is required for outcome change to occur. As noted by Norris (Norris et al., 2001) in a systematic review of diabetes self-management training: “It is apparent that factors other than knowledge are needed to achieve long-term behavioral change…and improved personal attitudes and motivations are more effective than knowledge in improving metabolic control in type II diabetes.”
There is strong evidence that support for self-management is a critical success factor for chronic disease programs. For example, a metaanalysis of primary care diabetes programs found that 19 of 20 interventions including a self-management component had improved a process or outcome of care (Renders et al., 2001). In addition, a study that investigated the effect of self-management education and regular practitioner review for adults with asthma demonstrated a statistically significant reduction in the proportion of subjects reporting hospitalizations and emergency room visits, unscheduled doctor visits, days lost from work, and episodes of nocturnal asthma (Gibson et al., 2000). A companion review analyzed trials that employed only limited education interventions and concluded that education did not have a significant effect unless it was coupled with an action plan, self-monitoring or regular review (Gibson et al., 2002).
With regard to health literacy, use of both written and verbal communication has been shown to be the most effective way of increasing patient understanding and compliance. (American Medical Association, 2002). Research with junior college students, for example, showed that recall of spoken medical instructions was enhanced by having pictographs representing those instructions present during learning and recall (Pfizer, 1998). The fact that the Hispanic subjects in the study did especially well in recalling pictograph meanings suggests that this approach may be helpful with groups for whom English is a second language.
Several measures of literacy have been found to correlate significantly with comprehension. The time spent reading sample leaflets and finding answers to questions about the documents was positively and significantly associated with comprehension measured by a true-false test. Two pronunciation measures and a literacy test based on correctly defining drug terminology also correlated significantly with true-false test comprehension (American Medical Association, 2002).
Inclusiveness
Poor health literacy is a widespread problem that affects people of all social classes and from all ethnic groups. Functional health literacy is worst among the elderly and low-income populations, impacting more than 66 percent of U.S. adults aged 60 and over and approximately 45 percent of all adults who live in poverty. Thus, the populations most in need of health care are least able to read and understand information needed to function as a patient (American Medical Association, 2002; United States Department of Health and Human Services, 2000).
Appropriate Treatment for Persons with Mild/Moderate Persistent Asthma
Aim
To ensure that all persons with mild/ moderate persistent asthma receive appropriate treatment with pharmacotherapy and suitable self-management support.
Rationale for Selection
Impact
It is estimated that in the United States, 14.6 million persons have active asthma (Centers for Disease Control and Prevention, 2001a). In 1999, an estimated 478,000 persons were hospitalized (Centers for Disease Control and Prevention, 1999b) and 2 million sought emergency care for acute asthma exacerbations (Centers for Disease Control and Prevention, 1999a). While death from asthma is almost always considered preventable, over 4,600 persons in the United States died from this condition in 1999 (United States Department of Health and Human Services, 2002).
In 1998, the economic burden associated with asthma was estimated at $12.7 billion annually. This figure includes nearly $7.4 billion in direct health care expenditures and an additional $5.3 billion in indirect costs. Loss of school days alone accounts for nearly $1.1 billion annually (Weiss and Sullivan, 2001). The inflation-adjusted costs of asthma have risen over the past decade (Weiss et al., 2000). Despite these increases in costs, however, there have been few clear signs that health care for those with asthma has substantively improved.
Numerous studies published throughout the 1990s and as recently as 2001 reveal that guidelines for asthma care are not being followed (Diette et al., 2001; Hartert et al., 2000; Legorreta et al., 1998). A number of national public and private agencies continue to recognize the suboptimal care and clinical outcomes for this disease. The United States Department of Health and Human Services (DHHS), through its Healthy People 2010 initiative, calls for reductions in asthma hospitalization rates (United States Department of Health and Human Services, 2000). The National Committee for Quality Assurance (NCQA) has added a performance measure to the Health Plan Employer Data and Information Set (HEDIS) that is aimed at improving the use of anti-inflammatory medications for persons with persistent asthma (National Committee for Quality Assurance, 1997). Most recently, the American Medical Association has focused on the importance of improving of asthma care through its physician-based measures (Antman, 2002).
The use of antiinflammatory medications and asthma education, including the provision of self-management support, are essential to improved asthma care. However, a number of studies suggest that health system redesign may also be required to optimally improve asthma care and thereby clinical outcomes (Evans et al., 1999; Greineder et al., 1999; Mayo et al., 1990; Zeiger et al., 1991). Studies such as the recently reported work of the Pediatric Asthma Care Patient Outcomes Research Team suggest that provider education alone will not significantly improve asthma outcomes without system redesign through a planned asthma care approach (Finkelstein et al., 2002).
Improvability
Since the late 1980s, there has been mounting evidence of substantial variations in asthma care and of the inadequate or suboptimal nature of much of the care provided (Diette et al., 2001; Hartert et al., 2000; Legorreta et al., 1998). In response to this problem, in 1987 the National Asthma Education and Prevention Program of the National Heart, Lung, and Blood Institute convened a national expert panel to develop guidelines for the treatment of the disease. These guidelines, first published in 1991 (National Asthma Education and Prevention Program, 1991) and updated in 1997 (NHLBIUSPHS, 1997) and 2002 (NAEPP Expert Panel Report, 2002), provide a benchmark by which to view the current
practice of asthma care.
One of the cornerstones of these guidelines is the use of anti-inflammatory medications for the treatment of persons with persistent asthma. A number of different medications make up this therapeutic group, and of these, inhaled corticosteroids have been recommended as the preferred therapy (NHLBIUSPHS, 1997). There are also a number of other key elements to the guidelines, few of which are as commonly agreed upon as the need to provide asthma education focused on support for self-management of the disease (NHLBIUSPHS, 1997).
Inclusiveness
Afflicting more than 14 million persons, asthma is a disease that affects all segments of the population—children and adults, males and females, urban and rural populations, and the wealthy and the poor (Centers for Disease Control and Prevention, 2001a). At the same time, perhaps the most important problem related to asthma care is the disproportionate impact of poor care on minority populations and persons of lower socioeconomic status (Centers for Disease Control and Prevention, 1998; Grant et al., 2000).
Asthma meets the inclusiveness criterion as it relates to the health care system. Care for persons with asthma extends across the primary care specialties of pediatrics, family medicine, and internal medicine. It also is an important health care concern for two subspecialty groups—allergists and pulmonolgists. Within asthma care, there are important lessons for outpatient, emergency department, and hospital-based care.
Cancer Screening That Is Evidence-Based
Aim
To enhance the effectiveness of screening programs designed to prevent colorectal and cervical cancer. More specifically, the aims are to increase the number of individuals who are offered appropriate screening for these cancers and to ensure that timely follow-up is provided.
In this report, colorectal and cervical cancer are used as examples, with the goal that effective systems-based interventions implemented for these two cancers could serve as models for other cancers where an evidence base is documented for screening or could be used once one has been established.
Rationale for Selection
Impact
Colorectal cancer is the third most common cancer among men and women in the United States, with an estimated incidence of 148,300 cases annually. In 2002, 56,600 Americans died from colorectal cancer, making it the nation’s second leading cause of cancer-related death. Lifetime risk for developing colorectal cancer is approximately 6 percent with over 90 percent of cases occurring after age 50 (American Cancer Society, 2002). The estimated long-term cost of treating stage II colon cancer is approximately $60,000 (Brown et al, 2002).
Cervical cancer is the ninth most common cancer among women in the United States, with an estimated incidence of 13,000 cases annually. Cervical cancer ranks thirteenth among all causes of cancer death, with about 4,100 women dying of the disease each year (American Cancer Society, 2002). The incidence of cervical cancer has steadily declined, dropping 46 percent between 1975 and 1999 from a rate of 14.8 per 100,000 women to 8.0 per 100,000 women (Ries et al., 2002). Despite these gains, cervical cancer continues to be a significant public health issue. It has been estimated that 60 percent of cases of cervical cancer are due to a lack of or deficiencies in screening (Sawaya and Grimes, 1999).
Improvability
Early diagnosis of colorectal cancer while it is still at a localized stage results in a 90 percent survival rate at 5 years (Ries et al., 2002). The American Cancer Society’s (ACS) guidelines recommend screening for colorectal cancer beginning at age 50 for adults at average risk using one of the following five screening regimens: fecal occult blood test (FOBT) annually; flexible sigmoidoscopy every 5 years; annual FOBT plus flexible sigmoidoscopy every 5 years; double contrast barium enema every 5 years; or colonoscopy every 10 years (American Cancer Society, 2001). The United States Preventive Services Task Force strongly recommends screening for men and women 50 years of age and or older for colorectal cancer. Screening has been found to be cost-effective in saving lives, with estimates ranging from $10,000 and $25,000 life-year saved. However, data were insufficient to determine whether one screening strategy is superior to another (Pignone et al., 2002; United States Preventive Services Task Force, 2002b).
In a nationally conducted survey assessing current rates of use of colorectal screening tests, 40.3 percent of respondents reported having had FOBT and 43.8 percent sigmoidoscopy or colonscopy at some point in time. With regard to screening being done within recommended ACS guidelines, 20.6 percent of respondents reported having FOBT within 1 year, and 33.6 percent reported having had sigmoidoscopy or colonoscopy within 5 years (Seeff et al., 2002). Another national survey found that between 1992–1998 only a slight increase was observed in screening for colorectal cancer, and in 1998, only 22.9 percent of respondents age 50 or older had been screened with a home administered FOBT in the past year or proctoscopy within 5 years (Nadel et al., 2002).
Widespread use of the Papanicolaou (Pap) test over the past 50 years as a screening tool for cervical cancer has led to an estimated 70 percent decline in mortality from this disease
(Dewar et al., 1992; Saslow et al., 2002). Early detection of cervical cancer that is still localized results in a 5-year survival rate of 92 percent (American Cancer Society, 2002). The American Cancer Society’s guidelines recommend that cervical cancer screening should start 3 years after a woman begins having sexual intercourse, but not later than 21 years of age, given that cervical cancer risk has been associated with sexually transmitted infection with certain types of human papilloma virus (HPV). Subsequently, women should have a Pap test every 3 years (American Cancer Society, 2002; Saslow et al., 2002). A recently report controlled trial demonstrated that administration of a HPV vaccine reduced both the incidence of HPV infection as well as HPV related cervical cancer among study participants (Koutsky et al., 2002).
As of 2000, the median percentage of women who had had a Pap test within the past 3 years was 86.8 percent (Centers for Disease Control and Prevention, 2000a). Despite these high screening rates, more than 50 percent of women in the United States who develop cervical cancer have either never undergone screening or not done so within the 3 years prior to diagnosis (NIH Consensus Statement, 1996). These women are likely to be older, to live in rural communities, and to be of low socioeconomic status (Anderson and May, 1995). Immigrant women with limited English proficiency are at especially high risk of never undergoing screening (Harlan et al., 1991).
Outcomes of a 5-year demonstration project targeting low-income members of minority groups who received their health care through the Los Angles County Department of Health Services demonstrated that systems-level strategies increased cervical cancer screening rates among this traditionally high-risk group. Systems interventions included physician education to heighten awareness of screening guidelines; patient education regarding risk factors for cervical cancer; policy interventions, such as written protocols to ensure follow-up of abnormal results; and expanded capacity, for example, increased clinic hours and same-day appointments for referrals. During the intervention time period, patients were three times more likely to receive screening as compared with the base line year (Bastani et al., 2002).
Ambiguity among health plans regarding coverage for cancer screening is a systems-related barrier. A study in which insurance departments were queried nationally found that 28 states and Puerto Rico did not require coverage for cervical cancer screening. Lack of consensus pertaining to guideline use was also demonstrated. Fourteen states and the District of Columbia have adopted ACS guidelines for cervical cancer screening whereas seven states have elected to use nonconforming guidelines (Rathore et al., 2000).
Inclusiveness
African Americans have the highest incidence of and mortality from colorectal cancer among racial/ethnic groups. Their mortality rate from the disease is 22.8 per 100,000 in the U.S. population and is at least double that of Asians/Pacific Islanders (10.7 per 100,000), American Indians/Alaskan Natives (10.3 per 100,000), and Hispanics (10.2 per 100,000) (American Cancer Society, 2002).
Vietnamese women have the highest age-adjusted incidence rate for cervical cancer (43 per 100,000) as compared with Japanese women, who have the lowest rate (15 per 100,000). Three ethnic groups have incidence rates of 15 per 100,000 or higher—Alaska Natives, Koreans, and Hispanics. African American women have an incidence rate of 13.2 per 100,000 for cervical cancer as compared with Caucasian women with a rate of 8.7 per 100,000. Mortality rates are also higher among African Americans than Caucasians, at 6.7 per 100,000 and 2.5 per 100,000, respectively (National Cancer Institute, 1996). African Americans are less likely than Caucasians to have their cervical cancer diagnosed at an early stage, with 44 percent of invasive cancers being diagnosed at a localized stage for the former as compared with 56 percent for the latter (American Cancer Society, 2002).
Children with Special Health Care Needs
Aim
To maximize the quality of care for children with special health care needs by addressing key processes of care, including care planning; use of preventive services; access to specialists, ancillary services, mental health services, and dental services; and care coordination.
The Maternal and Child Health Bureau defines this population as “those (children) who have or are at increased risk for a chronic physical, developmental, behavioral or emotional condition and who also require health and related services of a type or amount beyond that required by children generally” (McPherson et al., 1998:138).
Rationale for Selection
Impact
Although children with special health care needs having substantial medical problems make up a relatively small proportion of the pediatric population, it is particularly important to focus on (1) maximizing the quality of their health care, because they are the most in need of services, and (2) increasing the cost-effectiveness of their health care, because it is the most expensive. In recent years, the prevalence of complex chronic conditions has dramatically increased even as medical, surgical, and technological advances have decreased the mortality rates for infants, children, and adolescents (Cadman et al., 1987; Gortmaker et al., 1990; Ireys, 1981; Newacheck et al., 1991; Newacheck et al., 1998; Newacheck and Taylor, 1992). Among the total pediatric population, it is estimated that 6.7 percent have significant activity limitations, 0.2 percent have a limitation in an essential activity, such as eating, bathing, or dressing; and 0.047 percent receive technology-assisted care.
While the proportion of severely afflicted children is relatively low, public and private health care costs for children with special needs are substantial (Ireys et al., 1997; Silber et al., 1999; United States General Accounting Office, 2000). For example, in fiscal year 1998, the 1 million disabled children on Medicaid constituted 7 percent of beneficiaries under the age of 21, but accounted for 27 percent of the $26 billion in payments for children (United States General Accounting Office, 2000).
Improbability and Inclusiveness
The process of developing, implementing, and monitoring a care plan that involves the active participation of the family and health professionals is the most effective vehicle for ensuring comprehensive, culturally sensitive, patient/family-centered care for this population. Developing a care plan using a collaborative, interactive process is important to help families gain an adequate understanding of their child’s chronic illness. Even when families play a central role in caring for their child, they often lack an adequate understanding of the condition (Carraccio et al., 1998). Increasing the parents’ (and patient’s) understanding through educational interventions has been shown to be beneficial (Bauman et al., 1997). Examples of successful interventions include programs for self-management of asthma (Clark et al., 1984), for children with cancer reentering school (Nolan et al., 1987), and for support for parents performing care coordination (Stein, 1983).
Care coordination should help the family obtain the necessary services and ensure that information is shared among all providers and agencies. The care plan should identify specific individuals responsible for coordinating services; all children with special needs benefit from such coordination. A parent, physician, nurse, social worker, school health professional, other medical home staff member, employee of a community-based service, or other support person (such as a family friend or clergy member) can potentially play a significant role in care coordination. School health providers should be included in developing the care plan because about half of children with special needs who require emergency admission to an intensive care unit (ICU) are of school age
(Dosa et al., 2001).
It is also important to note that special-needs patients and their family members often have or develop behavioral and mental health concerns (Breslau et al., 1982; Coupey and Cohen, 1984; Kronenberger and Thompson, 1992; Lavigne and Faier-Routman, 1993; Wallander et al., 1989). Children with special needs have higher rates of mental health problems compared with otherwise healthy children (Pless and Wadsworth, 1988; Wallander et al., 1988; Weiland et al., 1992), and these problems persist (Pless and Wadsworth, 1988). Unfortunately, these children and families too often do not receive needed mental health services (Ireys, 1981; Kanthor et al., 1974; Stein, 1983).
Children with special health care needs require access to a range of medical services, including primary care, medical subspecialty and surgical specialty services, other ancillary services, and dental care. Services are provided in the home, office, emergency room, and hospital. Home care, which continues to evolve, is a major component of health care delivery that must be integrated into the planning process (Guidelines for home care of infants, children, and adolescents with chronic disease. American Academy of Pediatrics Committee on Children with Disabilities, 1995; Ciota and Singer, 1992; Goldberg et al., 1994). In the office, routine pediatric health maintenance and condition-specific preventive care that addresses the prevention and early diagnosis of disease-related conditions or complications are often quite variable and difficult to track (Liptak et al., 1998). Urgent-care needs may supersede routine health care maintenance.
It is important to prepare families for unavoidable emergencies; this is especially so for families of children with special needs who require technology-assisted care (Emergency Medical Services for Children; Sacchetti et al., 1996). Dosa et al. (2001) report that children with special needs are more than three times more likely to have an unscheduled ICU hospital admission compared with previously healthy children. Among children with special needs, those who receive technology-assisted care are 373 times more likely to have an unscheduled ICU admission than other children with special needs. Almost one-third of ICU admissions of children with special needs are considered to be potentially preventable. Preventable admissions are more common for children with special needs who do not require technology-assisted care (38 percent) than for those who require such care (19 percent). Of preventable admissions, 56 percent are due to the physical or social environment and decisions made by the family.
There is a evidence that improved comprehensive medical care that integrates primary and specialty care has an impact on outcomes (Broyles et al., 2000; Reogowski J., 1998). Broyles et al. (2000) report that comprehensive care for infants of very low birth weight results in fewer life-threatening illnesses, intensive care admissions, and intensive care days without increasing the mean estimated cost per infant for all care.
Diabetes
Aim
To prevent the progression of diabetes through vigilant, systematic management of patients who are newly diagnosed or at a stage in their disease prior to the development of major complications.
Rationale for Inclusion
Impact
Diabetes ranks as the fifth leading cause of death in the United States, affecting 17 million people and a contributing factor to over 210,000 deaths in 1999. In 1997, the total annual economic costs attributed to diabetes-related illness was $98 billion. Of this total, $44 billion was direct costs, such as personal health care spending and hospital care, and $54 billion was indirect costs, including disability, premature mortality, and work-loss days (American Diabetes Association, 2002).
Diabetes predisposes individuals to many long-term, serious medical complications, including heart disease, stroke, hypertension, blindness, kidney disease, neurological disease, and increased risk of lower-limb amputation. For example, diabetics have at least twice the risk of heart disease and stroke of their nondiabetic counterparts (American Diabetes Association, 2002). Diabetes is the leading cause of kidney failure; 33,000 people with diabetes developed kidney failure in 1997. And 12,000–24,000 people go blind each year as a result of the disease (Centers for Disease Control and Prevention, 2000d).
The lifetime cost of complications from diabetes was recently estimated to be about $47,000 per patient over 30 years on average. Management of macro vascular disease is the highest-cost component at 52 percent, followed by nephropathy (21 percent), neuropathy (17 percent), and retinopathy (10 percent) (Caro et al., 2002).
Improvability
Tight glycemic control has been shown to lower health care costs, reduce primary and specialty care visits, and afford short-term gains in quality of life for individuals with diabetes (Testa and Simonson, 1998; Wagner et al., 2001b). In addition, professional and organizational interventions, including aggressive follow-up and patient education, have been shown to contribute to better health outcomes for diabetics (Renders et al., 2001).
The Diabetes Quality Improvement Project (DQIP), a collaborative public-private venture founded in 1997 by the Centers for Medicare and Medicaid Services (CMS), NCQA, and the American Diabetes Association, has developed standardized performance measures for accurately and reliably assessing the quality of diabetes care both within and across health care systems. DQIP measures include, for example, annual testing for HbAlc, annual foot exam and eye exam, biennial lipid testing, and control of blood pressure (Fleming et al., 2001). In a recently published study using DQIP measures to evaluate the quality of diabetes care in the United Sates from 1988 to 1995, it was found that 18.9 percent of participants had high HbAlc values, 58 percent had poor lipid control, 34.3 percent had poor blood pressure control, 36.7 percent did not receive an annual eye exam, and 45.2 percent failed to receive an annual foot exam (Saaddine et al., 2002).
Outcomes from the Diabetes Control and Complications Trial confirmed that lowering blood glucose levels slows or prevents complications arising from type I diabetes. Individuals in the intensive therapy group experienced a 60 percent reduction in risk for eye disease, kidney disease, and neurological disease as compared with the standard treatment group (Implications of the Diabetes Control and Complications Trial, 2002). The lifetime benefits of intensive therapy could translate to approximately 8 years of additional sight, 6 years free from end-stage renal disease, and 6 years’ deferral of lower-extremity amputation relative to conventional treatment (Lifetime benefits and costs of intensive therapy as
practiced in the diabetes control and complications trial. The Diabetes Control and Complications Trial Research Group, 1996).
The United Kingdom Prospective Diabetes Study analyzed the effect of improved glucose control on type II diabetes. Findings from this longitudinal 14-year study demonstrated a 25 percent decrease in the overall microvascular (retinopathy, nephropathy, and neuropathy) complication rate for patients who received intensive therapy and maintained HbAlc levels at <7 percent. Although no significant effect on cardiovascular complications was observed for lowering of blood glucose levels, an epidemiological analysis did demonstrate a continuous association between the risk of cardiovascular complications and elevated blood glucose levels. For example, a 1 percent point decrease in HbAlc resulted in a 25 percent reduction in diabetes-related deaths (Implications of the United Kingdom Prospective Diabetes Study, 2002; King et al., 1999).
Diabetes is a prime candidate as a priority area because convincing guidelines, a robust set of measures (for example, from DQIP) and known ways of improving delivery of care already exist. Diabetes could serve as a model for improving quality of care for other chronic diseases, particularly with regard to facilitating patient self-management and the active involvement of a multidisciplinary health care
|
Box 3–8 Diabetes The American Diabetes Association recognizes HealthPartners Medical Group of Minnesota as a model for diabetes care. Key components of the HealthPartners diabetes program include a diabetes registry that provides clinicians with automated reminders for needed services; use of interdisciplinary teams including physicians, diabetes nurse specialists, social workers, and mental health professionals; education programs, including counseling on diet and exercise; and implementation of a staged approach to diabetes management, with an action plan and timelines for stepping up care to meet therapy goals. As a result of these multifaceted interventions, improvements in both blood sugar and lipid control were observed over a 1-year period. For example, the proportion of patients with acceptable HbAlc levels (below 8 percent) rose from 60.5 to 68.3 percent, and the proportion of patients with acceptable control of their LDL (bad cholesterol) levels rose from 48.9 to 57.7 percent (HealthPartners, 2000; Sperl-Hillen et al., 2000). |
team. Improved care for this condition could also stimulate an approach that involves treating other risk factors (cardiovascular disease, hypertension, renal disease) through aggressive management of the disease as opposed to treatment of end-stage complications.
Inclusiveness
During the 1990s, the prevalence of diabetes increased by 33 percent. Most notably, this increase was seen in both males and females, across ethnic groups and educational levels, and among all age groups (Mokdad et al., 2000).
Racial and ethnic disparities have been documented with regard to the treatment of chronic diseases including diabetes (Chin et al., 1998; Institute of Medicine, 2002). For example, one study looking at racial disparities in quality of care for Medicare enrollees found that African Americans with diabetes were less likely than Caucasians to receive eye examinations (Schneider et al., 2002). African Americans are three times more likely than Caucasians to die of diabetes-related causes. And American Indians/Alaska Natives are 2.5 times more likely and Hispanics 1.5 times more likely to die of diabetes than Caucasians or Asians/Pacific Islanders (Centers for Disease Control and Prevention, 2000d).
End of Life with Advanced Organ System Failure
Aim
To arrange care so that people facing the end of life with heart, lung, or liver failure will have as few frightening exacerbations as possible, as few symptoms as possible, and as many opportunities for life closure and control of the circumstances of death as possible.
Rationale for selection
Impact
Heart, lung, or liver failure is one of the more common conditions experienced at the end of life (Standards for the diagnosis and care of patients with chronic obstructive pulmonary disease. American Thoracic Society, 1995; Gillum, 1993; Higgins, 1989; Levenson et al., 2000; Lynn et al., 2000; McAlister et al., 2001; Rich, 1997; Rich, 1999; Roth et al, 2000; United States Department of Health and Human Services, 1998). People live with these conditions for long periods of time that have become longer now that better treatments slow the progression of illness. However, the conditions still cause death eventually, and living for a long time in perilous circumstances poses its own challenges. Heart failure is one of the most common hospitalization diagnoses in Medicare, and lung failure is close behind (Standards for the diagnosis and care of patients with chronic obstructive pulmonary disease. American Thoracic Society, 1995; Rich, 1999). As many more people survive their first few heart attacks, their first episodes of lung infection with emphysema, and their first bleeds with cirrhosis, many more live with advanced organ system failure.
The normal course of such conditions is one of stability and comfort on a “usual” day, with a string of those usual days being interrupted by a rather sudden exacerbation in response to some stress (Levenson et al, 2000; Lynn et al, 2000; Roth et al, 2000). A fever, a small new heart attack, or a bowel problem is enough to disturb the fragile balance being enjoyed by the patient (Burns et al., 1997; Chin and Goldman, 1996). Often, one of these exacerbations is the cause of death, but the timing of that eventuality generally remains unclear to within a week of the patient’s dying. Good care for this population requires reducing the rate of exacerbations, diminishing their effects, and planning for the eventuality of an unsurvivable episode.
Improvability
Many studies have shown that the rate of exacerbations can usually be cut in half, and sometimes much more (McAlister et al., 2001; Rich, 1997; Rich, 1999). Doing so requires self-care education, reliable availability of medications, early intervention at the least sign of trouble, and mobilizing of services to the home setting. Most important, good care requires continuity in the care plan and in caregivers across time and settings. Some hospice programs support nearly all patients at home at the end of life (Lynn et al., 2000).
Most health care is loosely organized by referral patterns, and patients from the same neighborhood may go to disparate providers. In end-of-life care for persons facing organ system failure, services are probably best organized so that the same provider of services takes care of all persons in one area, or at least so that only a very small number of providers are working in one area. The number of persons affected by advanced heart, lung, and liver disease is not large, so even urban areas cannot efficiently support more than a few services for around-the-clock availability.
Improving care for this population also requires close monitoring and rapid responses. When a patient becomes quite ill, mobilizing of services-including both urgent and end-of-life services-to the home is essential. Thus, implementing good care for this population requires learning how to work in communities, how to plan ahead, and how to provide good care for very sick people in their homes and nursing homes.
Inclusiveness
Heart, lung, and liver failures account for about one-fifth of all fatal illness in the United States (Lunney et al., 2002), and they strike rather equitably across all genders, ethnic groups, and geographic areas. Cirrhosis tends to kill somewhat earlier than the other
|
Box 3–9 End of Life with Advanced Organ System Failure: A Current and Future Scenario In the current system, an elderly man lives with his wife in a small duplex, and their son lives nearby. As the man has become more disabled with heart attacks and progressive heart failure, his living arrangements have become more constrained. The family moved his bed to the living room, they arranged a long ramp to the door, and they changed the family diet to avoid salt. Nevertheless, he goes into an episode of “failure” every few months and is rushed to the hospital by the emergency ambulance, struggling to breathe. His wife lives in terror of these episodes, and shakes and trembles for days afterwards. She has lived through breast cancer and a stroke herself, and she worries all the time about what would happen to her husband if she died first, and what would happen to her if he died first. Their assets have been spent, and they routinely skimp on their prescription medications, since otherwise they could not meet their rent and food bills. Their son helps out by keeping the place repaired, but he works as a clerk in a convenience store and does not really have funds to assist his parents. Every time the man is hospitalized, he has a different set of doctors, who never seem even to have his medical record. Between hospitalizations, he is scheduled for a follow-up visit in “resident’s clinic,” but he does not usually go since it costs so much and seems to do very little good. He does not understand his medications, does not weigh himself, does not know what to do if he starts to become short of breath, and has had no conversations with any physicians in which it was implied that this condition will eventually take his life. In a transformed health care system, the same elderly man and his wife are enrolled in a complex care management program that ensures that they receive good medical services and helps with financial planning, family support, and advance care planning. Both have come to understand how to manage medicines and weight, and know what extra medications to take at the earliest signs of trouble. The man has had only two more hospitalizations–one for prostate trouble and one for heart failure brought on by a bad cold with a fever. As his condition has worsened, nurses have become available at home. As planned, he eventually dies at home, and the same care team continues to support his wife with the health and living challenges she faces. |
conditions, with many deaths occurring before Medicare eligibility (Roth et al., 2000). Heart and lung failures tend to reach life-threatening levels in the 65–80 age group (Lunney et al., 2002).
Frailty Associated with Old Age
Aim
To arrange care so that people in frail health can count on living in optimally safe environments, free of unnecessary threats to their physical safety, assisted as necessary with the tasks of daily living, encouraged to maintain functioning whenever possible, treated early for complications, and with care shaped by advance care plans that reflect patient and family preferences.
Rationale for Selection
Impact
As Americans routinely no longer die from infections, childbirth, early heart attacks, and the various threats to longevity that were commonplace just a few score years ago, they increasingly live out the end of life in advanced old age, afflicted by multiple medical problems, significant disability, and limiting social challenges, ultimately spiraling into a condition tht can be characterized as frailty (Fried and Walston, 1998; Walston and Fried, 1999). This condition is marked by having multiple chronic ailments and a lack of reserve capacity to endure health setbacks in most body parts and systems (Buchner and Wagner, 1992; Fretwell, 1993; Fried et al., 2001). About half of the people affected past the age of 85 have cognitive deficits from dementia, stroke, or other causes. Many have problems with falls or develop other impediments to mobility. Many have heart or lung problems, but even more have problems with vision, hearing, foot pain, and bowel discomfort (Fried and Guralnik, 1997). Approximately two-fifths of Americans now live with frailty for a few years before dying (Lunney et al., 2002).
The average person living with frailty at the end of life probably faces more than 2 years of self-care disability (Manton, 1989). Unfortunately, the current American health care system was never designed to support large numbers of people with cognitive and other self-care disabilities. Services for frail older adults are often poorly coordinated, entail differing and mismatched sets of eligibility criteria and coverage, and are inadequate to meet important care needs (Moon, 1996; Wagner et al., 1996). The shortcomings have been documented most extensively with regard to nursing facility care, but undoubtedly affect family care at home, paid help at home, hospice care, assisted living settings, and other strategies for services to this population (Bodenheimer, 1999).
The challenge of providing for the large numbers of elderly anticipated over the next quarter century is widely regarded as a major crisis for health care and for society generally (American Medical Association white paper on elderly health. Report of the Council on Scientific Affairs, 1990). Not only will the numbers of dependent elderly nearly double, but also the availability of family caregivers will actually decline.
Improvability
Achieving excellence in care for this vulnerable population will take some time, but some of the needed changes are well documented, highly visible, and strategically important, and it is these changes that the committee recommends making a priority. For example, good care systems have exceedingly low rates of skin breakdown from pressure and poor hygiene. Until the last few weeks of life, when some patients do not want to be turned, the rates can be kept to only a few percent. However, doing so requires assiduous nursing care around the clock (Prevention Program Reduces Incidences of Pressure Ulcers by Up to 87%, 2002; Bates-Jensen, 2001).
As another example, the death of frail patients is no surprise to anyone when it occurs. Advance care planning averts the inappropriate implementation of rescue efforts not desired by patient and family and offering little benefit. In some parts of the country, virtually all persons living in nursing homes or receiving regular home care for frailty have advance care plans that address what is to be done about
hospitalization, resuscitation, and other aggressive means to sustain life. In most parts of the country, however, advance care planning is the exception (Fried et al., 2002; Kolarik et al., 2002; Schwartz et al., 2002).
As a final example, many frail people sustain completely preventable injuries due to unsafe home environments. Surveillance of the risks at home, together with the use of improved lighting, warning systems, floor coverings, grip bars, and other environmental modificationsm, has been shown to greatly reduce the incidence of falls and injuries. Yet these measures are not routinely provided or even available to most frail patients (Guideline for the prevention of falls in older persons. American Geriatrics Society, British Geriatrics Society, and American Academy of Orthopaedic Surgeons Panel on Falls Prevention, 2001; Fleming and Pendergast, 1993; Tinetti and Williams, 1998).
In addition, reliable care for the elderly should include interventions such as increased physical activity and strengthening, to prevent further declines in function. For example, in a program designed to prevent functional decline for frail elderly persons, participants were assessed on eight activities of daily living3 at 3,7, and 12 months, and the results were compared against baseline scores on a disability scale. Moderately frail persons who received the home-based interventions, which consisted of physical therapy targeting improved balance, muscle strength, ability to transfer from one position to another, and mobility, demonstrated less functional decline over time as compared with the control group (Gill et al., 2002).
Improving care for the frail elderly and the provision of support for their family caregivers will require transforming much of health care for this population to a chronic illness model. Continuity and reliability are priorities. Given the large numbers of people involved and the scarcity of caregivers, efficiency needs to be built in from the start. As noted, for example, reducing rates of skin breakdown to the extent possible will require adequate round-the-clock nursing care, thus pressuring the care system to attend to personal care and not overemphasize procedures. The development of advance care plans for most frail persons will require that professionals learn to counsel patients and families about their future prospects and to maintain effective continuity of the care plan over time. And preventing falls and injuries will necessitate mobilizing services to the places where the frail live, again requiring caregivers to adapt to the needs of this population.
Inclusiveness
Frailty awaits those who survive long enough simply to have diminished reserves, as well as those who encounter mental decline in old age. The condition is now so dominant at the end of life that all ethnic groups, both genders, and all parts of the country are affected roughly equally.
Hypertension
Aim
To reduce the incidence of complications resulting from inadequately treated hypertension (i.e., coronary artery disease, congestive heart failure, renal insufficiency, peripheral vascular disease, and stroke) through early detection, effective treatment, and appropriate follow-up.
Rationale for Selection
Impact
Hypertension (high blood pressure) affects approximately 43 million Americans aged 18 or older, representing 1 in 4 adults.
Approximately 20 million of these individuals are not receiving necessary blood pressure medication, and for another 12 million who are being treated, the condition is inadequately
Table 3–1. Estimated Number of Americans Age 25 and Older by Category of High Blood Pressure
|
|
Population in Million |
|||
|
Age group |
Treated, Controlled |
Treated, Uncontrolled |
Aware, Untreated HBP |
With HBP, Unaware |
|
25–34 |
1.7 |
0.9 |
1.9 |
2.9 |
|
45–64 |
4.5 |
4.2 |
2.8 |
4.4 |
|
65+ |
3.5 |
6.9 |
2.3 |
5.8 |
|
SOURCES: (Burt et al., 1995; Hyman and Pavlik, 2001) |
||||
Table 3–2. Extent of Awareness, Treatment, and Control of High Blood Pressure Race/Ethnicity 1988–1994
|
|
Percent of Population with High Blood Pressure |
|||
|
Race/ Ethnicity |
Treated, Controlled |
Treated, Uncontrolled |
Aware, Untreated HBP |
With HBP, Unaware |
|
Caucasians |
24 |
29 |
17 |
31 |
|
African Americans |
24 |
32 |
17 |
27 |
|
Mexican Americans |
15 |
25 |
19 |
41 |
|
SOURCES: (Burt et al., 1995; Hyman and Pavlik, 2001) |
||||
controlled (Burt et al., 1995). In 1999, high blood pressure was the primary cause of death for 42,997 Americans and was a contributing cause of death in 227,000 cases. In 2002, the economic costs of hypertension totaled $47.2 billion (American Heart Association, 2001). Table 3–1 presents the estimated number of Americans with high blood pressure by age group.
Overall, 32 percent of people with high blood pressure are unaware they have the disease. If left untreated hypertension can lead to several life-threatening complications, such as stroke, heart attack, heart failure, and kidney failure (American Heart Association, 2002). Table 3–2 shows the extent of awareness of high blood pressure among different racial/ethnic groups.
According to a recent study, the lifetime risk of developing hypertension for middle-aged and elderly individuals is 90 percent.
Notably, while women’s risk for hypertension remained constant over the two time frames evaluated in this study (1952–1975 and 1976– 1998), men’s risk increased by 60 percent (Vasan et al., 2002).
Improvability
Data from the Framingham Heart Study and the National Health and Nutrition Examination Survey II indicate that lowering of diastolic blood pressure by a slight percentage–2 millimeters of mercury (mm/Hg) could result in a 17 percent decrease in the prevalence of hypertension, a 6 percent decrease in coronary heart disease, and a 15 percent reduction in stroke (Cook et al., 1995). However, statistics released by the NCQA in its 2002 State of Health Care Quality report indicate that of those being treated for hypertension only 55.4 percent maintain their blood pressure at an adequate level. Although this current rate is unacceptable, gains have been made, as the rate was 39 percent in 1999 (National Committee for Quality Assurance, 2002).
A systematic review of 18 long-term randomized controlled trials revealed that the use of low-dose diuretic therapy was effective in reducing stroke, coronary artery disease, congestive heart failure, and total mortality. Additionally, beta blockers were demonstrated to decrease the incidence of congestive heart failure and stoke (Psaty et al., 1997). These findings are consistent with the guidelines of the Sixth Report of the National Committee on Prevention, Detection, Evaluation and Treatment of High Blood Pressure (JNC-VI), which recommends the use of diuretics and/or beta blockers for initial drug therapy for patients with hypertension (The sixth report of the Joint National Committee on prevention, detection, evaluation, and treatment of high blood pressure, 1997). Despite these evidence-based guidelines, a recent study revealed that in 62 percent of visits, physicians failed to introduce proper pharmacologic therapy to patients with a systolic blood pressure of 140 mm/Hg or higher, the JNC-VI recommended cut-off point. On average, physicians were willing to accept a higher cut-off point of 150 mm Hg before believing it necessary to initiate or change drug therapy (Oliveria et al., 2002).
The most recent recommendations of the National High Blood Pressure Education Program Coordinating Committee for primary prevention of hypertension include a two-pronged approach employing population-based strategies and an intensive strategy targeting individuals known to be at high risk, such as African Americans. The recommendations focus on six lifestyle modifications that have not only been proven to be effective in preventing an increase in high blood pressure at the population level, but also can be readily applied to individuals with hypertension or with high normal blood pressure: weight loss; dietary sodium reduction; increased physical activity; moderation of alcohol consumption; potassium supplementation; and modification of diet to include foods rich in fruits, vegetables, and low-fat dairy products and to reduce the intake of saturated and total fat (Whelton et al., 2002).
Inclusiveness
Hypertension affects all races and ethnic groups; however, certain groups are more heavily burdened. For example, compared with Caucasians, African Americans develop high blood pressure earlier in life and have a 1.3 times greater rate of nonfatal stroke, 1.5 times greater rate of heart disease, and 4.2 times greater rate of end-stage renal disease (American Heart Association, 2001). Table 3–3 presents death rates per 100,000 population from high blood pressure by race and sex for African Americans and Caucasians.
Immunization (Children)
Aim
To sustain the momentum to ensure high levels of immunization coverage for children and to decrease disparities in levels of childhood immunization coverage in metropolitan areas with large populations of low-income residents.
Rationale for Selection
Impact
Vaccines are biological substances that interact with a person’s immune system to produce an immune response identical to that caused by the natural infection (United States Department of Health and Human Services, 2000). As a result, they prevent the illness and disability associated with infectious diseases. They also protect society. When vaccination levels are high in communities, the few who are not vaccinated are often indirectly protected because of group immunity. Vaccination is cost-effective as well. Savings range from $2 to $24 for every dollar spent (United States Department of Health and Human Services, 2000). Vaccines in the combined series include diphtheria-tetanus-pertussis or diphtheriatetanus, poliovirus, a measles-containing vaccine, Haemophilus influenzae type b, and hepatitis B (The Commonwealth Fund, 2002).
U.S. federal and state governments created an immunization system during the 1990s that has demonstrated the capacity to deliver vaccines to children in a variety of health care settings. As a result, record levels of immunization have been achieved across the United States (Institute of Medicine, 2000a). Nonetheless, in 2000 over one-quarter of young children aged 19 to 35 months were not up to date on all recommended doses of vaccines in the combined series (The Commonwealth Fund, 2002). The resurgence of measles in 1989– 1991 in the United States was unexpected. Many believe it was fueled by complacency and an absence of data that fostered the mistaken idea that immunizations were up to date (Institute of Medicine, 2000a). The United States lags behind other nations in achieving widespread vaccination of children (The Commonwealth Fund, 2002). In a study produced by the Partnership for Prevention (2002), vaccinating children is cited as the number one priority among recommended clinical preventive services (Partnership for Prevention, 2002).
Each day sees nearly 11,000 new births, and a strong immunization system is required to ensure the delivery of routine immunizations to these children. In addition to the limited coverage noted above, it is expected that the current system will soon be strained by the addition of new vaccines to the recommended schedule. For example, the American Academy of Pediatrics has recently released a policy statement encouraging that healthy children aged 6–23 months to be immunized for influenza. Recent data has indicated that healthy children younger than 24 months have a high risk of hospitalization due to influenza, and this risk was demonstrated to be greater than healthy adults older than 50 who are routinely recommend to be immunized (American Academy of Pediatrics, 2002; Rennels and Meissner, 2002). Further, state and local budget cuts due to the downturn in the economy are expected to impact the vitality and flexibility of the immunization system. Moreover, studies have noted a strong relationship between low socioeconomic status and vaccine coverage rates (Rodewald et al., 1999). Specifically, children who are poor and live in urban areas may have immunization rates below those in other parts of the United States (Institute of Medicine, 2000a; Rodewald et al., 1999). New strategies need to be developed for reaching out to inner-city populations and raising immunization rates.
Improvability
National objectives include increasing the proportion vaccinated to 80 percent of young children aged 19–35 months (United States Department of Health and Human Services,
2000). Many parents cannot remember the recommended immunization schedule for childhood vaccination, and both parents and providers tend to overestimate the immunization status of their children or patients (Rodewald et al., 1999). Client reminder/recall interventions are strongly recommended by the Centers for Disease Control and Prevention (2000) to remind members of a target population when vaccinations are due. A synthesis of controlled studies revealed that patients who received reminders (such as postcards, letters, or phone calls) about upcoming or overdue immunizations were more likely to be vaccinated or up to date on their vaccinations than those who did not receive such reminders (Centers for Disease Control and Prevention, 2000b; The Commonwealth Fund, 2002).
Multicomponent interventions (including education) are strongly recommended by the Centers for Disease Control and Prevention (2000). For example, vaccination requirements for child care and school attendance can improve coverage and immunity and reduce rates of disease. A decrease in out-of-pocket costs to families for vaccinations and administration of vaccinations has the potential to increase rates of coverage as well; a series of studies showed that this measure led to an improvement in vaccine coverage of 15 percentage points (Centers for Disease Control and Prevention, 2000b).
Inclusiveness
As noted, coverage levels for children less than 3 years of age remain significantly lower among urban and low-income populations (Rodewald et al., 1999). In 1998, 70 percent of children aged 19–35 months from the lowest-income households received the combined series of recommended immunizations, compared with 77 percent of those from higher-income households (United States Department of Health and Human Services, 2000). In California, results of the 1999 California Kindergarten Retrospective Survey indicate that African American and Hispanic children continue to be immunized at lower rates than Caucasians and Asians (Center for Health Improvement, 2001).
Immunization (Adult)
Aim
To increase the proportion of adults who are vaccinated annually against influenza and ever vaccinated against pneumococcal disease through changes in clinical procedures, such as the use of standing orders. Special efforts should be made to improve immunization rates among African American and Hispanic adults and nursing home residents.
Rationale for Selection
Impact
Pneumonia and influenza are the seventh leading cause of death in the United States (The Commonwealth Fund, 2002). Pneumococcal disease causes 10,000 to 14,000 deaths annually; influenza causes an average of 110,000 hospitalizations and 20,000 deaths annually (United States Department of Health and Human Services, 2000). Approximately 30–43 percent of elderly people who have invasive pneumonia will die from the disease (United States Preventive Services Task Force, 1996). The elderly are also at increased risk for complications associated with influenza, and approximately 90 percent of the deaths attributed to the disease are among those aged 65 and older (Vishnu-Priya et al., 2000).
To decrease the burden of these diseases, including incapacitating malaise, doctor visits, hospitalizations, and premature deaths, experts recommend vaccination. Yet one-third to one-half of older adults (aged 65 and over) do not receive these vaccinations (The Commonwealth Fund, 2002). Coverage rates for high-risk adults who suffer from chronic disease are especially poor, with only 26 percent receiving an influenza vaccination and 13 percent a pneumococcal vaccination (Institute of Medicine, 2000). Adults report that they do not
get these vaccinations because they are not aware of the need to do so, lack a doctor’s recommendation, or forget (United States Department of Health and Human Services, 2000).
Improvability
Adults living in nursing homes are especially susceptible to contagious illness because of close living quarters (Vishnu-Priya et al., 2000). Use of standing orders for immunizations for nursing home residents can improve coverage for this population. Standing orders involve programs in which nonphysician medical personnel prescribe or deliver vaccinations to clients without direct physician involvement at the time of the visit (Centers for Disease Control and Prevention, 2000b). Use of standing orders in settings other than nursing homes has also been shown to improve vaccination coverage among adults. Research has shown standing order programs to result in a median percentage point increase in vaccination coverage of 28 percent (Centers for Disease Control and Prevention, 2000b).
A meta-analysis found organizational change interventions, such as prevention clinics and planned prevention visits, to be highly effective in increasing immunization rates for adults. Specifically, the research focused on strategies that involve searching for system-based problems and solutions and depending on input from teams of involved health care providers to design appropriate interventions (American College of Physicians, 2002).
To increase influenza immunization rates and decrease the possibility of serious illness or death among the elderly, at least 11 states have laws related to immunization in long-term care facilities. For example, New York requires that all long-term care facility residents and employees receive influenza and pneumococcal immunizations (National Conference of State Legislatures).
As noted, the most effective strategies for increasing immunization rates for adults include organizational changes that make the identification and delivery of immunization a routine part of patient care. Only recently has research been available to identify which such changes work best to improve coverage rates (American College of Physicians, 2002).
Inclusiveness
Both influenza and pneumococcal immunization rates are significantly lower for African American and Hispanic adults than for Caucasian adults (United States Department of Health and Human Services, 2000). The percentage immunized among adults aged 55– 64 is lower than that among adults 65 and older, with a median of 38.2 percent nationwide (Institute of Medicine, 2000a). The highest incidence rates of pneumonia are among people over age 65, nursing home residents, and certain ethnic groups, including Native Americans and Alaskan Natives (United States Preventive Services Task Force, 1996).
Ischemic Heart Disease
Aim
To achieve improvements in the prevention of artherosclerotic disease, reduction of reoccurring events, and optimization of functional capacity.
Rationale for Selection
Impact
Ischemic (coronary) heart disease caused 513,758 deaths in 2000, representing 1 of every 5 deaths (Minino and Smith, 2001). The lifetime risk of developing heart disease at age 40 is one in two for men and one in three for women (Lloyd-Jones et al., 1999). Ischemic heart disease plays a major role in physical disability among the U.S. labor force, accounting for 19 percent of allowances by the Social Security Administration (American Heart Association, 2001). Total expenditures for heart disease were approximately $112 billion in 2002, with direct costs, such as hospitals/ nursing homes and prescription drugs, totaling $58 billion and indirect costs, including lost productivity/morbidity, totaling $54 billion (American Heart Association, 2001).
A 50-year retrospective study found that the incidence of heart failure has declined by one-third for women but has remained unchanged for men. However, overall survival rates after the initial onset of heart failure have increased approximately 12 percent per decade since 1950. Despite these gains, heart disease continues to be the leading cause of death among both men and women, with half of patients diagnosed with heart failure in the 1990s dying within 5 years (Levy et al., 2002).
Improvability
A meta-analysis of the effect of lipid-lowering drugs on the incidence of coronary heart disease indicated that drug treatment reduced the risk of nonfatal heart attack and death from coronary artery disease by 30 percent (Pignone et al., 2000). In a study of seven countries, it was shown that an increase in total serum cholesterol was accompanied by an increased risk of coronary heart disease. These findings were consistent across cultures. Notably, however, the absolute level of risk for coronary heart disease was markedly different among cultures, a finding that points to other factors, such as diet, in preventing heart disease (Verschuren et al., 1995). In a randomized controlled study investigating the effect of physical activity on risk factors for cardiovascular disease, it was demonstrated that regular exercise, even with minimal weight change, had a positive impact on lipoprotein levels (Kraus et al., 2002).
Evidence from a retrospective meta-analysis comparing coronary angioplasty and intravenous thrombolytic therapy for acute myocardial infarction (heat attack) indicated that angioplasty significantly reduced the risk of death, repeat heart attack, and stroke. However, it should be noted that lack of access to fully equipped and staffed catheterization laboratories can be an impediment to expeditious receipt of this treatment (Weaver et al., 1997). A recent study examined the cost-effectiveness of early invasive interventions, such as catheterization, for treating acute myocardial infarction as compared with more conservative strategies favoring medical stabilization followed by catheterization for high-risk patients. It was discovered that invasive strategies were more costly by $1600 per patient, but this figure was later reduced to $586 per patient as a result of lower hospitalization rates after 6-month follow-up. Projected estimates of cost of life year gained (between $8,000 and $ 15,000) supported the use of more invasive strategies, with the exception of low-risk patients (Cohen, 2002; Mahoney et al., 2002).
The use of beta blockers has long been demonstrated as an effective drug therapy for preventing cardiac death following myocardial infarction (Viskin and Barron, 1996; Yusuf et al., 1985). A recent systematic review of randomized controlled trials investigating the use of beta blockers confirmed that these drugs
are still successful in reducing mortality and morbidity in patients (Freemantle et al., 1999). However, short-term use of beta blockers after acute myocardial infarction is of questionable benefit unless long-term therapy is sustained.
The Minnesota Heart Survey showed a decline in both out-of-hospital death rates and recurrence of acute myocardial infarction from 1985 to 1997. Marked increases in survival of acute myocardial infarction were also observed. Deaths related to cardiac disease fell 47 percent for men and 51 percent for women. These positive outcomes were attributed to increased use of thrombolytic therapy, emergency angioplasty, angiotensin-converting enzyme (ACE) inhibitors, beta blockers, heparin, and aspirin during this period (McGovern et al., 2001). Over a 20-year period, the Veterans Health Administration in California saw nearly a 10 percent reduction in mortality associated with acute myocardial infarction; 71 percent of this decease was attributed to increased use of aspirin, beta blockers, ACE inhibitors, and reperfusion (Heidenreich and McClellan, 2001).
The Intensive Lifestyle Heart Trial demonstrated that lifestyle changes could slow the progression of coronary artherosclerosis. The intervention group of this study underwent intensive lifestyle changes, including a vegetarian diet emphasizing whole foods with no more than 10 percent fat, aerobic exercise, stress management training, smoking cessation, and group psychological support. In 1 year, a 37 percent reduction in LDL (bad cholesterol) levels and a 91 percent reduction in the frequency of angina attacks were observed. After 5 years, the intervention group showed additional regression of artherosclerosis, whereas the control group showed progression of artherosclerosis and twice as many cardiac events(Ornish et al., 1998). In addition, cardiac rehabilitation, including exercise training, nutritional counseling, and drug therapy, has been shown to reduce morbidity and mortality. However, only 10–20 percent of ideal candidates participate in formal programs (Ades, 2001).
Inclusiveness
Marked regional variations across the United States in the clinical management of acute myocardial infarction have been documented. The Global Utilization of Streptokinase and Tissue Plasminogen Activator for Occluded Coronary Arteries trial (GUSTO-1) found substantial regional variation in the use of both cardiac medications and cardiac procedures. For example, administration of beta blockers ranged from 55 to 81 percent across the country, and angiography from 52 to 81 percent (Pilote et al., 1995). The National Cooperative Cardiovascular Project found that use of beta blockers among patients aged 65 or older varied significantly by state, ranging from 30 to 77 percent (Krumholz et al., 1998; O’Connor et al., 1999). A study examining the treatment of Medicare patients with acute myocardial infarction revealed that a significantly higher proportion of patients received aspirin, IV nitroglycerin, and heparin in urban as compared with rural hospitals. Once again, older patients were less likely to receive recommended therapy (Sheikh and Bullock, 2001).
An evaluation of 81 Veterans Administration acute care hospitals revealed that African Americans were less likely to receive thrombolytic therapy and undergo bypass surgery, even when identified as being at high risk (Petersen et al., 2002). Another study designed to evaluate how race and sex influence physicians’ management of chest pain found that women and African Americans were less likely to be referred for cardiac catheterization than men and Caucasians, respectively. In addition, African American women were significantly less likely to be referred for catheterization than Caucasian men (Schulman et al., 1999).
Major Depression
Aim
To improve national rates of diagnosis and appropriate treatment of major depression.
Rationale for Selection
Impact
Major depression is a disorder characterized by depressed mood, loss of interest or pleasure, and other symptoms that may include changes in sleep and appetite and thoughts of suicide. The disorder differs both quantitatively and qualitatively from normal sadness and bereavement (American Psychiatric Association, 1994). Approximately one in seven men and one in four women will have an episode of major depression at some point during their lives (Blazer et al., 1994).
Major depression is associated with an enormous clinical and societal burden in the United States. Depressed patients suffer from levels of disability similar to or greater than those associated with a host of other chronic medical conditions (Wells et al., 1989). The 2000 Global Burden of Disease Study estimates that major depression contributes to more disability in the United States than any other single medical condition (World Health Organization, 2000). Despite this high burden, fewer than half of individuals with depression in the community and in primary care medical settings are correctly diagnosed (Hirschfeld et al., 1997; Simon et al., 1999), and fewer than one-third receive care that is concordant with clinical treatment guidelines (Wang et al., 2000; Young et al., 2001). Rates of treatment for depression are substantially lower than for many other chronic conditions (Druss et al., 2001a), and national health expenditures for depression, while substantial, are low relative to the disorder’s associated disability (Druss et al., 2002).
Improvability
A variety of highly efficacious clinical treatments exist for depression, most of which involve psychotherapy, psychopharmacology, or a combination of the two (United States Public Health Service, 1999). Guidelines have been developed for the treatment of depression in primary care (Depression Guideline Panel, 1993; Schulberg et al., 1998), and algorithms are being formulated to guide depression care in specialty mental health settings (Crismon et al., 1999; STAR*D Program, 2002).
Systems of care can be improved to provide better care for depression. A number of interventions have shown that collaborative models designed to improve coordination and follow-up by a multidisciplinary team can improve the process and clinical outcomes of care (Katon et al., 1995; Simon et al., 2000). These models are grounded in principles drawn from Wagner’s Chronic Care Model for improving the care of individuals with serious mental illnesses (Wagner et al., 2001c). See Chapter 1 for a discussion of the Chronic Care Model.
Treatment for major depression is increasingly occurring in two settings-primary care medical settings and specialty organizations, which provide services for mental health separately from those for general health care (Frank et al., 1996). Because depression commonly occurs in conjunction with other mental disorders, primary care clinicians are often the first-line providers for the condition’s diagnosis and treatment. This practice has become more widespread, with the growing expectation that primary care providers will manage rather than refer common mental disorders, as newer antidepressants are developed that are easier and safer to prescribe (Pincus et al., 1998). With regard to the use of specialty organizations, it has been estimated that approximately 160 million Americans are enrolled in such plans. However, little is known about the impact of these plans on patients’ mental health care, and even less is known about their impact on the quality and costs of general medical care for patients enrolled in the
programs (Sturm, 1999).
An issue cutting across both types of settings is the fact that mental health benefits are subject to restrictions, such as caps and copayments, not imposed for other medical conditions. A major focus of mental health policy at both the federal and state levels over the past decade has been on seeking to pass legislation mandating parity with general medical benefits. However, the same factors that drive these disparities-economic forces and stigma-may mean that such legislation alone may not be enough to ensure equal access to mental health care (Frank et al., 2001). To truly transform care for depression in the United States, it will be important to monitor not only benefit packages, but also access to and quality of care for depressed individuals receiving those benefits.
|
Box 3–10 Major Depression Partners in Care was a multisite quality improvement project designed to examine whether and how system change could improve care for depression in real-world settings (Wells, 2002b; Wells et al., 2000). The study team worked with leading depression researchers to develop a “toolkit” of services for local primary care providers and patients. This package included an institutional commitment to quality improvement, training in how to provide clinician and patient education, and access to local expertise in psychotherapy or medication follow-up. The study randomly assigned 46 clinics treating 1,356 patients to either this quality improvement program or usual care. The study found that patients treated under the enhanced systems of care received higher-quality depression treatment, had a better chance of recovering from the disorder, and were more likely to stay in their jobs than those treated in the usual manner. The enhanced care was cost-effective compared with other interventions-an approximately $500 expenditure per patient led to the equivalent of a full month of feeling completely well (over the 2-year follow-up period) and an additional month of employment (Schoenbaum et al., 2001). The Partners in Care study demonstrates that changing systems of care can have a real and profound impact on the clinical care and lives of people with depression, and can do so at a modest cost. |
Inclusiveness
A number of subgroups may be vulnerable to undertreatment and poor quality of care for depression. Ethnic minorities, older patients, and less-educated patients are less likely to receive antidepressant treatment and more likely to receive lower quality of care than are other depressed patients (Melfi et al., 2000; Young et al., 2001). Minority groups may derive particular benefit from quality improvement in care for depression that can help reduce these treatment disparities (Miranda et al., 2002).
Medication Management
Aim
To prevent and provide ongoing surveillance of adverse drug events (ADEs), and to reduce inappropriate antibiotic use in particular for acute respiratory infections.
Rationale for Selection
Impact
A recent report of the Institute of Medicine placed patient safety issues on the national radar screen by reporting that an estimated 44,000 to 98,000 Americans die each year as a result of medical errors (Institute of Medicine, 2000b). Most common are medication-related errors, which have been estimated to account for over 7,000 deaths annually (Leape et al., 1991; Phillips et al., 1998). ADEs have been associated with longer hospital stays, higher costs, and almost twice the risk of death (Classen et al., 1997). The Adverse Drug Event Prevention Study Group found that ADEs occur in 6.5 of every 100 hospital admissions, with 42 percent of these events being either serious or life threatening (Bates et al., 1995). In another study by the same group, it was determined that the estimated cost for an ADE was approximately $2,600, translating to $5.6 million in annual costs for an average-sized teaching hospital (Bates et al., 1997). Overall, the cost of drug-related deaths and complications exceeds $136 billion a year in the United States (Johnson and Bootman, 1995).
With regard to inappropriate antibiotic use, treatment of acute respiratory infections accounts for 75 percent of all antibiotics prescribed in ambulatory settings. Although the majority of these illnesses are viral in nature and do not benefit from antimicrobial drug therapy, antibiotics are prescribed during over 50 percent of visits for colds and upper respiratory tract infections in the United States annually (Gonzales et al., 1999; Gonzales et al., 1997; McCaig and Hughes, 1995; Schappert, 1997). Such overuse of antibiotics has contributed to the emergence and spread of antibiotic-resistant bacteria (Kunin, 1993). For example, during the past 5 years, the rate of penicillin-resistant S. pneumoniea, the causative agent of pneumonia, has increased by more than 300 percent (Centers for Disease Control and Prevention, 2002a). In a recent study that examined the impact of patient pressure on physicians’ prescribing behavior, it was found that in 68 percent cases of acute respiratory infection, antibiotics were prescribed even though 80 percent of those prescriptions were deemed unnecessary according to the guidelines of the Center for Disease Control and Prevention (CDC) (Scott et al., 2001).
The emergence of antibiotic-resistant bacterial strains capable of causing infection alters the initial selection of antibiotics for patients suspected of having a serious bacterial infection. For example, meningitis must be treated with multiple antibiotics that will cover possible resistant bacteria. Not only is this approach expensive, but it also promotes the emergence of bacterial strains resistant to currently effective antibiotics.
Improbability
After assessing ADEs for their root cause, Classen et. al (1998) found that half of the events were potentially preventable. These events included excessive dosage (42 percent), drug interactions (4.6 percent), cases of known drug allergies (1.5 percent), and patient identification errors (3.5 percent) (Classen, 1998; Evans et al., 1992). From 1993 to 1998, the Food and Drug Administration’s Adverse Event Reporting System showed that the most common types of fatal errors included improper dose (41 percent), use of the wrong drug (16 percent), and use of the wrong route of administration (10 percent). These errors were attributed mainly to preventable performance and knowledge deficits (44 percent) and communication errors (16 percent) (Phillips et al., 2001).
Computerized physician order entry is a tool that has been shown to reduce medication errors. In one study, use of computer systems
equipped with only basic decision support led to a 64 percent reduction in medication errors, and use of systems equipped with advanced decision support resulted in an 83 percent decrease (Bates et al., 1999). Employing a multidisciplinary team approach, the medical intensive care unit at Massachusetts General Hospital in Boston included a pharmacist on its patient care team, which resulted in a 77 percent reduction in medication errors (Cullen, 1998). Barnes-Jewish Hospital in St. Louis has implemented two automated safety net computer systems that detect potentially dangerous drug combinations (PharmADE) and identify inappropriate dosages (DoseChecker). PharmADE has reduced the number of patients receiving dangerous drug combinations at discharge from 36 to 7 percent. In addition, physicians adjusted their original dosage on medications 71 percent of the time after having been notified by pharmacists using DoseChecker (McMullin et al., 1998).
With regard to antibiotic overuse, several studies have demonstrated the positive impact of educational interventions targeted at both physicians and parents to curb inappropriate prescribing of antibiotics. A randomized controlled trial of 12 practices in Massachusetts and Washington State showed that educational outreach to providers and parents resulted in a 16 percent decrease in antibiotic dispensing for children under 3 years of age and a 12 percent decrease for children aged 3 to 6 years. The physician/practice group interventions included two meetings of the group with a physician peer leader who promoted CDC guidelines and feedback on prescribing rates. Parental interventions included mailings of CDC brochures and literature made available in the physician’s office (Finkelstein et al., 2001). A community-based intervention trial in Wisconsin designed to enhance awareness of antibiotic resistance and appropriate antibiotic prescribing revealed an increase of 15 percent in parent’s awareness after educational interventions and declining expectations for antibiotics for their children (Trepka et al., 2001). In a community-wide campaign based in Tennessee, educational efforts directed at health care professionals, parents, and the general public reduced prescription rates by 11 percent (Perz et al, 2002).
Antimicrobial prescribing rates for children and adolescents have begun to show significant improvement. For example, from 1980 to 1992, a 48 percent increase in antibiotic prescriptions for children was observed as compared with recent data showing a 40 percent decrease from 1989–1990 through 1999–2000 (McCaig et al, 2002; McCaig and Hughes, 1995). Despite these encouraging outcomes, efforts to sustain this downward trend are still essential, as resistant strains of bacteria have continued to emerge during this period. Efforts to reduce inappropriate antibiotic use for acute respiratory infections should continue to be directed at both the clinician and patient/family. Systems should be set up to track antibiotic use for various acute respiratory diagnoses, as well as resistance patterns of common respiratory pathogens isolated in local hospitals. This information should be provided to clinicians on a regular basis, and clinicians should as a community set goals for reducing inappropriate antibiotic use.
Inclusiveness
Although medication errors impact all ages, races, and ethnic groups, certain groups are particularly susceptible. These include patients with chronic illness who are being treated with multiple medications. For example, several studies have shown that 14–24 percent of the elderly were inappropriately prescribed drugs that could have been harmful or of questionable value (General Accounting Office, 1995; Leatherman and McCarthy, 2002; Meredith et al, 2001; Spore et al, 1997; Stuck et al, 1994; Willcox et al, 1994; Zhan et al, 2001). Children also have a higher risk of an ADE related to dosing errors because their medications must be adjusted to their weight (Kaushal et al., 2001).
Although the bulk of research on medication errors has been conducted in hospitals, the problem clearly is not isolated to this type of setting. In one study that examined
drug complications in 11 ambulatory clinics in Boston, 18 percent of patients reported such a complication, while a chart review revealed only a 3 percent ADE rate. In 13 percent of the cases, the patient had already had a documented reaction to the drug (Gandhi et al., 2000).
With regard to antibiotic overuse, since children and adolescents have the highest rates of antibiotic use and infection with antibioticresistant microorganisms, they are a subgroup warranting particular attention (McCaig and Hughes, 1995; Nyquist et al., 1998; Perz et al., 2002; Whitney et al., 2000). The increased distribution of antimicrobial-resistant bacteria also poses a threat to the elderly, who are more vulnerable to nosocomial infections as they are more likely to be hospitalized or in a nursing home (Norman, 2002). Adults, too, are at risk, as they are often treated with antibiotics for viral-related illnesses. In a study comparing antibiotics with placebos for treatment of acute cough in adults, it was found that resolution of the cough was not affected by antibiotic treatment and that the risk of potential antibiotic side effects outweighed any marginal benefit of the drug therapy (Fahey et al., 1998).
Nosocomial Infections
Aim
To significantly reduce the number of preventable nosocomial infections in the nation’s hospitals and care centers through the implementation of CDC guidelines (Centers for Disease Control and Prevention, 2000c) and other evidenced-based protocols, coupled with a surveillance system for voluntary monitoring. CDC defines a nosocomial infection as a localized or systemic condition that resulted from an adverse reaction to the presence of an infectious agent(s) or toxin(s) and was not present or incubating at the time of admission to the hospital (Garner et al., 1996).
Rationale for Selection
Impact
Nosocomial infections account for 50 percent of all major hospital complications (Becker et al., 1987). Up to 2 million Americans every year-1 in 20 of all those admitted to hospitals-contract such infections (MMWR Weekly, 2000). In 1995, nosocomial infections cost $4.5 billion and contributed to more than 88,000 deaths, translating to 1 death every 6 minutes (Weinstein, 1998). Nosocomial bloodstream infections are a leading cause of death in the United States, with 57 being the median age of those who die from these infections. It has been estimated that the total number of years of life lost annually in the United States as a result of nosocomial infections is 350,000 (Wenzel and Edmond, 2001).
Improvability
CDC has developed seven guidelines for the prevention of health care-associated infections. These guidelines cover the following: prevention of catheter-associated urinary tract infections, hand washing and hospital environmental control, infection control among hospital personnel, prevention of intravascular infections, isolation precautions in hospitals, prevention of nosocomial pneumonia, and prevention of surgical site infection (Centers for Disease Control and Prevention, 2000c).
In addition to the implementation of evidence-based guidelines, it has been shown that surveillance is an effective tool for curtailing nosocomial infections. The Study on the Efficacy of Nosocomial Infection Control (SENIC), which analyzed over 338,000 patient records across the United States, found that hospitals with the lowest rates of nosocomial infection had implemented rigorous surveillance programs (Gaynes, 1997; Haley et al., 1985).
For example, the National Nosocomial Infections Surveillance System (NNISS), overseen by CDC, was established in 1970 to collect data on hospital-acquired infections. The goal of this initiative was to establish a national database to better understand the epidemiology of nosocomial infections, to track antimicrobial resistance trends, and to provide nosocomial infection rates for use by hospitals as benchmarks for quality improvement efforts. Hospitals voluntarily participate in the NNISS program with the understanding that their identity will be kept confidential (Centers for Disease Control and Prevention, 2001b; 2001d; Gaynes and Solomon, 1996b; Richards et al., 2001). Over 75 percent of hospitals across the United States are now voluntarily submitting their nosocomial infection outcome measures. Currently, the database is being expanded to collect information from nursing homes for the next submission cycle. Many hospitals are electing to forego their anonymity and are releasing their results to the public. Participants in the program have experienced dramatic reductions in rates of infection of the bloodstream and other body sites, including the respiratory and the urinary tracts. From 1990 to 1999, bloodstream infection rates decreased by 44 percent, 31 percent, and 32 percent in medical, surgical, and pediatric intensive care units, respectively (Gaynes et al., 2001).
Despite encouraging outcomes demonstrated by the NNISS, the value of surveillance of nosocomial infections as a quality improvement tool is often overlooked
because of both time and cost constraints (Gaynes, 1997). Presently there are no state or federal mandates that require hospitals to publicly report their nosocomial infection rates. As of 2000, 315 hospitals were participating in the NNISS, representing only a small fraction of the 5,810 hospitals in the United States (American Hospital Association, 2001).
Although the importance of actions of individuals, such as hand washing, should not be understated, prevention of nosocomial infections through the implementation of evidence-based guidelines and a surveillance program demonstrates how effective systems interventions can lead to more widespread improvements in quality of care. Collection of national data on nosocomial infections provides a benchmark by which individual hospitals can gauge their performance, thus enabling them to design targeted interventions for problem areas (Gaynes and Solomon, 1996a).
Inclusiveness
Nosocomial infections affect both genders and all ethnic/racial groups. They occur in all American hospitals, but they are not limited to hospitals; they are of equal importance in nursing homes, outpatient facilities, and doctors’ offices. Reducing the incidence of these infections will involve the concerted efforts of all health care workers.
Pain Control in Advanced Cancer
Aim
To ensure that patients facing incurable and progressive cancer can count on living without serious pain through to the end of life.
Rationale for Selection
Impact
Cancer is the second leading cause of death in the United States, responsible for one out of every four deaths. Approximately 550,000 Americans will die of cancer in 2002, greater than 1,500 people per day (American Cancer Society, 2002). Many with cancer experience substantial pain throughout the course of their illness and that pain is widely dreaded (Cleeland et al., 1994; Sloan et al., 1999). Cancer related pain affects 20 percent to 50 percent of patients at the time of their diagnosis and during subsequent treatment and 55 percent to 95 percent of those in the advanced stages of their disease (Allard et al., 2001). Living with overwhelming pain is demoralizing, removes dignity and interferes with daily life activities (Cassell, 1992; Ferrell et al., 1991).
Improvability
Various programs have shown that the pain associated with advanced cancer can almost always be controlled to a level that the patient finds tolerable and with acceptable side effects, and that more overwhelming pain can be overcome with sedating levels of relief (Fitzgibbon, 2001). Fewer than 10 percent of cancer patients near death have pain that requires sedation to overcome; through most of the illness, at least 90 percent of patients can be comfortable (e.g., a level of less than 5 on a scale of 0–10) with medications and special procedures (Levy, 1996; Zech et al., 1995). Despite proven guidelines for pain relief, such as the World Health Organization’s three-step analgesic ladder, which gradually adjusts the potency of medication as the patient’s level of pain increases, pain continues to be undertreated (Mercadante, 1999; World Health Organization, 1996). The National Cancer Policy Board (Institute of Medicine, 1999; Institute of Medicine, 2001b) and others, including the National Institutes of Health (National Institutes of Health, 2002) and the Joint Commission on Accreditation of Healthcare Organizations (Phillips, 2000), have stated that the major cause of serious pain in cancer is failure to use methods already proven effective.
Often, pain is especially bad around the time patients are transferred from one setting to another (e.g., hospital to nursing home) or in cases of poorly supported home care (Bernabei et al., 1998). Hospice programs have earned a good reputation with regard to pain management, and anesthesiologists have developed a number of special approaches that limit side effects and optimize pain relief (Lynn, 2001). Achieving improvement in this area requires a number of elements that would be useful models for other reforms:
-
Skillful use of pain-relieving medications
-
Cooperation in protocols across settings of care (Cringles, 2002)
-
Advance planning for changes in setting and increases in pain
-
Public education to foster a balanced view of the merits of opioid medications (Allard et al., 2001; Dahl et al., 2002)
-
Epidemiological surveillance of the population affected to monitor changes over time and to compare the experience of populations defined by geography, delivery system, age, type of cancer, and other factors
Overall, it would be a triumph for the nation to be able to count on competent and reliable pain prevention and relief throughout the course of fatal cancer.
Inclusiveness
While there are small differences in rates of fatal cancer across populations, the disease is commonplace among the rich and the poor, in all parts of the country, and among every ethnic
and religious group. African Americans have higher rates of cancer, and die of it both more often and earlier, than Caucasians, Asians, or Hispanics (American Cancer Society, 2002; Hodgson et al., 2001). Some evidence indicates that minorities are less likely to be treated effectively for pain (Anderson et al., 2002).
|
Box 3–11 Pain Control in Advanced Cancer: A Current and Future Scenario In the current system, the Main Street Church support group for advanced cancer patients meets every week/and at this meeting, as at many others, the conversation turns to the reality and the fear of pain. One participant has a doctor who will not give anything very strong yet “because you’ll need those strong drugs later.” Only when she got her granddaughter, a nurse, to help her change doctors did she become comfortable enough even to come to the support group meetings. Another participant had a problem getting a pharmacy to fill his prescription, and none would deliver it to his part of town, “which was considered too dangerous.” A third participant had just come home from the hospital, where he had been in terrible pain for days while the house staff and attending physician made adjustments to his medications on morning rounds each day. It took a week before he became comfortable enough to sleep or eat. Still another participant is not at the meeting, being “too exhausted from not sleeping” since she moved into a nursing home and cannot take her medications when she wants them. The social worker coordinating the support group helps participants deal with their anger and frustration. In a transformed system, the Main Street Church support group for advanced cancer patients meets every week, and usually the participants discuss family concerns and spiritual issues. One participant mentions that her mother was afraid her daughter would be miserable when she went to the local university hospital for special treatment because her aunt had had that experience 10 years ago. The participant’s mother was delighted to find that things had changed and the care was excellent, including asking about and ensuring comfort. Another participant reflects on a conversation with his doctor about his fears that pain might “get out of hand” as his cancer got worse, but his doctor was able to reassure him that this would not occur, citing data from the regional cancer alliance’s interviews with patients and family members about their experiences. Two other participants move the conversation along to other topics because there is just not much to say about pain when everyone is confident that it will never be allowed to become overwhelming. |
Pregnancy and Childbirth
Aim
To improve the quality of care provided during pregnancy and childbirth by appropriately using proven health-care interventions at key times during pregnancy and delivery, and successfully applying these interventions to populations known to be at risk.
Rationale for selection
Impact
Pregnancy and childbirth may be associated with several complications and adverse outcomes, such as preterm delivery (11 percent), preeclampia (4 percent), gestational diabetes (2–3 percent), and multiple gestations (1 percent), with each of these factors contributing to greater perinatal morbidity and mortality (Martin et al., 2001). In 2000, there were approximately 4 million births in the United States. Of these births, 23 percent were delivered by cesarean section, making this the most common major surgical procedure in the United States (Hoyert et al., 2001).
The annual maternal mortality rate during 1982–1996 remained essentially unchanged at 7.5 maternal deaths per 100,000 live births (Maternal mortality—United States, 1982–1996, 1998), and the infant mortality rate in 2000 was 6.9 per 1000 live births (Hoyert et al., 2001). Many women still miss the opportunity for health promotion and disease prevention early in pregnancy, with approximately 17 percent of mothers not starting prenatal care in the first trimester (Hoyert et al., 2001).
Effective management of pregnancy, including prenatal and intrapartum care, offers opportunities and challenges for quality improvement given the diverse group of conditions and interventions involved, such as infectious diseases (particularly sexually transmitted diseases and HIV/ADDS); chronic diseases (particularly diabetes and hypertension); tobacco cessation counseling; and management of surgical complications. Moreover, quality improvements in this area could simultaneously enhance health outcomes for two distinct but inextricably interrelated populations-mothers and newborns. Finally, since pregnancy represents a pivotal leverage point for promoting healthy behavior, and since neonatal morbidity will affect a child for many years, health care interventions at this critical juncture can have a lasting impact (Huntington and Cornell, 1994; Kogan et al., 1998; Rogowski, 1998).
Improbability
There are multiple opportunities for quality improvement related to prenatal care and intrapartum (labor and delivery) management. A recent study demonstrated that both Caucasian and African American women who received prenatal care experienced fewer neonatal deaths. Lack of prenatal care was associated with higher infant death rates, particularly if complications presented, such as preterm premature rupture of membranes, placenta previa, fetal growth restriction, and post-term pregnancy (Vintzileos et al., 2002).
A recent national survey indicated that only 30–32 percent of physicians screened pregnant women for sexually transmitted diseases. Screening rates were higher among obstetricians/gynecologists and ranged from 75 to 85 percent, however, these rates were still below nationally recommended guidelines (St Lawrence et al., 2002).
Tobacco cessation counseling can serve as the exemplar for this priority area. Smoking during pregnancy has been estimated to cause about 7–10 percent of preterm deliveries, 17–26 percent of low-birth-weight births, and 5–6 percent of perinatal deaths (United States Preventive Services Task Force, 1996). Fortunately, tobacco cessation interventions during early pregnancy have been demonstrated to improve perinatal outcomes, as well as to increase abstinence rates. Data from randomized controlled clinical trials have shown that smoking cessation counseling can reduce the incidence of intrauterine growth
retardation and decrease the risk of low-birth-weight births (Law and Tang, 1995; Lumley et al., 2000; United States Preventive Services Task Force, 1996). In addition, tobacco cessation programs have been shown to be cost-effective (Shipp et al., 1992). Despite this evidence supporting their effectiveness, such programs do not appear to have been universally developed and incorporated into prenatal care.
During labor and delivery, specific opportunities for quality improvement include continuing to increase the appropriate use of antenatal corticosteroids (Leviton et al., 1999), decreasing the inappropriate use of tocolytics in threatened preterm labor (Jones et al., 2000), ensuring appropriate antibiotic treatment for preterm premature rupture of membranes (Egarter et al., 1996), reducing rates of inappropriate elective induction of labor (Kozak and Weeks, 2002), and promoting appropriate use of cesarean delivery (Bailit et al., 2002).
Inclusiveness
Pregnancy and childbirth is a priority area that is clearly relevant for a broad range of populations. Women and their families of all demographic profiles are affected by the quality of care provided during the prenatal period and delivery.
Substantial racial/ethnic disparities have been documented for both maternal and infant mortality. Maternal mortality rates are higher for African American women (25 per 100,000 births) and for Hispanic women (10 per 100,000 births) than for Caucasian women (6 per 100,000 births) (Centers for Disease Control and Prevention, 2002c). The infant mortality rate is 2.5 greater for African American than for Caucasian newborns (Beck et al., 2002). The percent of women receiving prenatal care in the first trimester varies by race, with African Americans and Hispanics being 14 percent less likely to receive prenatal care than Caucasians (Hoyert et al., 2001).
Marked geographic variations in prenatal care also exist. In 1999, 16.1–29.9 percent of women who responded to the CDC’s Pregnancy Risk Assessment Monitoring System reported having received prenatal care late or not at all. The prevalence of late or no prenatal care was lowest in Maine and highest in Oklahoma (Beck et al., 2002). Variations in the rates of infant mortality have been demonstrated in U.S. metropolitan areas, with postneonatal mortality among American Indians and Alaskan natives being twice that of Caucasians (Grossman et al., 2002).
Severe and Persistent Mental Illness
Aim
To improve care for patients with severe and persistent mental illness treated in the public mental health sector.
Rationale for Selection
Impact
Clinically and legally, severe and persistent mental illness is defined through “diagnosis, disability, and duration” (Senate report number 102–397,). The term encompasses disorders with psychotic symptoms, such as schizophrenia, bipolar disorder, and autism, as well as severe forms of other conditions, such as major depression. From a systems perspective, patients with these conditions are commonly treated in the public mental health sector (Narrow et al., 2000). This sector, which includes state hospitals, community mental health centers, the Veterans Administration, and other state and federal government programs, provides a safety net for individuals who do not have or have exhausted private health insurance benefits.
About 3 percent of the adult population in the United States experiences severe mental disorders in a 1-year period. During 1990, these patients accounted for an estimated $74 billion in national expenditures (Health care reform for Americans with severe mental illnesses: Report of the National Advisory Mental Health Council, 1993). Despite this clinical and financial burden, care for these patients remains inadequate. As many as half of all individuals with severe mental illness receive no care at all (Narrow et al., 2000; Von Korff et al., 1985), most commonly because they do not regard themselves as having a problem that requires treatment (Kessler et al., 2001). Once in treatment, only about a third of individuals with serious mental illness (a somewhat broader group than those with severe mental illness) receive treatment that is concordant with treatment guidelines (Wang et al., 2002).
Improvability
As with other disabling chronic illnesses, the focus of treatment for severe and persistent mental illness is less on curing the condition and more on minimizing symptoms, maximizing function, and preventing relapse. Highly efficacious pharmacological treatments are available to achieve the latter objectives for schizophrenia and other severe mental disorders (Burgess et al., 2001; Thornley et al., 2000; Wahlbeck et al., 2000). Indeed, many of the most important barriers to care for those afflicted with these disorders lie not in an absence of effective treatments, but in the fact that the symptoms and stigma associated with severe mental illness may make it difficult for patients to obtain and follow through with appropriate care. Both case management (Jinnett et al., 2001) and more intensive Program of Assertive Community Treatment programs (described in greater detail below) have been found to be useful means of overcoming these barriers.
Many of the greatest challenges faced by these patients lie at the interface between the public mental health system and other clinical and social service sectors. Much of the best evidence on systems improvability comes from studies of programs seeking to better integrate care across these boundaries. For example, patients with severe mental disorders have been shown to derive substantial benefit from interventions designed to improve the integration of mental health services with substance use treatment (Drake and Mueser, 2000), work rehabilitation (Drake et al., 1999; Lehman et al., 2002), and primary medical health care (Druss et al., 2001b).
The existence of a separate public mental health sector poses a unique set of challenges to efforts to transform the care of patients with severe and persistent mental disorders. First, the presence of this safety net system has made it relatively easy for private insurers to cap lifetime limits on mental health benefits, with the knowledge that patients exceeding those caps will likely be eligible for treatment in the public sector. Similarly, the public system
provides a mechanism for private hospitals to engage in “dumping” —the economically motivated transfer of patients into public-sector settings (Schlesinger et al., 1997). The fact that the states bear ultimate responsibility for these sickest of patients has made care inconsistent across states and vulnerable to shortfalls in state budgets. Indeed, state programs face increasing fiscal strain as they seek to care for these patients with limited, and often shrinking, financial resources (Lamb and Bachrach, 2000). Finally, it has been argued that the “two-tiered” (private-public) mental health system perpetuates both the stigma and the social disadvantages experienced by patients treated in the public mental health sector (Hogan, 1998).
One of the best-validated models for improving care for patients with severe mental illness is the Program of Assertive Community Treatment model, or PACT. This service-delivery model provides intensive, community-based services to patients at high risk of psychiatric hospitalization. It was developed during the early 1970s as a response to the deinstiutionalization movement to allow the most severely ill patients to live and function successfully in the community (Marx et al., 1973). In the years since it was developed, it has proved successful in engaging and maintaining these high-risk patients in mental health care, reducing hospital costs, and improving patients’ clinical and housing outcomes (Lehman et al., 1997; Marshall and Lockwood, 2000; Rosenheck and Dennis, 2001). Despite these potential benefits, however, only six states have statewide PACT programs, and fewer than half of all states even have pilot programs in place (National Alliance for the Mentally Ill, 2002).
Transforming care for the severely mentally ill will ultimately require transforming the public mental health sector. That transformation will in turn require a federal effort to ensure better standards of care and funding across states, along with a particular focus on interfaces between the public mental health sector, other social service sectors, and the general medical system.
Inclusiveness
The onset of serious mental illness most commonly occurs in early adulthood, and because of their chronic nature, these disorders generally persist throughout the life span. Moreover, they are seen across social classes, ethnic groups, and genders (Tamminga, 1997). Because African Americans with these disorders tend to be overdiagnosed (Baker and Bell, 1999) and undertreated (Dixon et al., 2001; Kuno and Rothbard, 2002), they should be considered a potentially vulnerable subpopulation in treatment studies and quality improvement efforts.
Stroke
Aim
To maximize the stroke patient’s abilities and likelihood of returning to a full and independent life.
Rationale for Selection
Impact
Approximately 600,000 Americans suffer from a new or recurrent stroke each year. Stroke is the third leading cause of death in the United States, accounting for 1 of every 14 deaths; in 1999 it was responsible for 167,366 deaths. Stroke is also the leading cause of long-term disability in the United States, resulting in functional limitations and/or trouble with activities of daily living among 1,100,000 American adults. Analyses of the 1994–1995 National Health Interview Survey Disability supplement (NHIS-D) found that among persons aged 70 and older, cerebrovascular disease was the third leading cause of major mobility problems, after arthritismusculoskeletal conditions and ischemic heart disease (lezzoni et al., 2001). In 1998, $3.6 billion was paid to Medicare beneficiaries who had short-term hospital visits for stroke (American Heart Association, 2001).
Improvability
A recently published scientific review documents the effectiveness of the following strategies for primary prevention of stroke: adequate blood pressure reduction, treatment of hyperlipidemia, use of antithrombotic therapy in patients with atrial fibrillation, and antiplatelet therapy in patients with heart attack. Additionally, for secondary prevention of stroke, the evidence base supports treatment of hypertension and hyperlipidemia, antithrombotic therapy for patients with atrial fibrillation, antiplatelet therapy, and carotid endarterectomy in patients with coronary artery stenosis (Strauss and Pollack, 2001).
Even the best preventive treatment of stroke does not correct for the inevitable chronic loss of function experience by many patients. Often, this is the area in which the medical system is least effective in dealing with the long-term complications of stroke. In the first few weeks following a stroke, patients may begin to recover spontaneously some of the functional ability lost because of the stroke; this spontaneous recovery may progress for months. Nevertheless, beginning rehabilitation as soon as possible after a stroke can help patients learn better how to accommodate any remaining debility so they can perform daily activities and return home.
Rehabilitation following stroke has been studied extensively, with most researchers agreeing that “a comprehensive, intense rehabilitation program is key to a successful convalescence” for stroke patients (Rosenberg and Popelka, 2000). Therapeutic benefits include better functional abilities, decreased disability, greater likelihood of returning home, and superior quality of life (Cifu and Stewart, 1999; Freburger, 1999; Halar, 1999; Kwakkel et al., 1997; Kwakkel et al., 1999; Rosenberg and Popelka, 2000; van der Lee et al., 1999). To benefit patients maximally, however, rehabilitation must be timely, preferably beginning during acute hospitalization for the stroke, although there is some disagreement about whether more intense treatment improves outcomes (Cifu and Stewart, 1999; Rosenberg and Popelka, 2000). A critical review of 79 studies published from 1950 to 1998 found improved outcomes with better baseline functioning, early intervention, and an interdisciplinary team approach, but no benefit from specialized therapies or greater service intensity (Cifu and Stewart, 1999). One study of over 400 patients revealed that even those without substantial impairment from their stroke benefited from rehabilitation (Roth et al., 1998). The Agency for Health Care Policy and Research (now the Agency for Healthcare Research and Quality) published guidelines for post stroke rehabilitation in 1995 (Post-stroke Rehabilitation Panel, 1995). One medical record review study found that these guidelines
are not followed consistently in routine practice (Forbes et al., 1997).
Improvements in this area derive from the seamless integration of care across various settings and clinical disciplines (e.g., medical specialties and/or neurology, physical and occupational therapy, speech-language pathology services). Quality problems are especially likely to occur as patients shift from one care site to another; after a stroke, patients may move several times, ideally to increasingly independent locations. Rehabilitation can occur in a variety of settings, starting with inpatient acute care hospitals and including inpatient rehabilitation hospitals, nursing homes, outpatient offices, and homes. Sometimes Medicare payment policy dictates the location (e.g., restricting payment for nursing homes). Nevertheless, it is critical to ensure that clinicians are monitoring patients’ progress over time, tracking functional milestones, and working with patients and their families to make appropriate treatment decisions. Once care moves into the home, oversight of rehabilitation becomes especially challenging. Although physicians must approve therapists’ services for the therapists to be reimbursed, many physicians are poorly trained for evaluating and treating functional impairments. The decision about when to stop rehabilitation services is often complex, frequently dictated by reimbursement policies: Medicare generally pays for rehabilitation only when patients are making documented progress toward some prespecified goal.
Inclusiveness
The greatest proportion of stoke-related deaths occurs among those over age 85 (40 percent), followed by those aged 75–84 (34 percent), 65–74 (14 percent), and younger than 65 (11.2 percent). The chance of stroke more than doubles for those above age 55. Stroke is more prevalent overall in men than women; at older ages, however, the incidence in women is higher. Age-adjusted death rates for stroke are 62.4 for men and 60.5 for women (American Heart Association, 2001; Centers for Disease Control and Prevention, 2002b).
African Americans have higher age-adjusted death rates due to stroke than Caucasians–225.2 and 166.7, respectively. Younger African Americans have two to three times the risk of stroke of Caucasians, and African Americans of both genders are more likely to die of a stroke (American Heart Association, 2001; Centers for Disease Control and Prevention, 2002b).
Tobacco Dependence Treatment in Adults
Aim
To improve national rates of screening and appropriate treatment for tobacco use and dependence among adults.
Rationale for Selection
Impact
Tobacco use and dependence represent the nation’s single most preventable cause of disease and death. Over 25 percent of adults and over 30 percent of high school seniors-almost 50 million Americans-report regular tobacco use. Tobacco-related deaths number more than 430,000 per year among U.S. adults, including deaths due to heart disease, stroke, lung cancer, and chronic lung disease, accounting for approximately 1 in 5 deaths overall (United States Department of Health and Human Services, 2000). Maternal smoking in pregnancy is the single most important preventable cause of poor pregnancy outcomes, resulting in low birth weight, perinatal mortality, and sudden infant death syndrome (United States Department of Health and Human Services, 2001b). Currently, 27 percent of U.S. children aged 6 and under are exposed to tobacco smoke at home, increasing their risks of respiratory illnesses, middle-ear infections, and decreased lung function (DiFranza and Lew, 1996; Wisborg et al., 1999).
Annual direct medical costs attributable to smoking are estimated at $80 billion-an estimated 6–12 percent of all health care expenditures-not including societal costs due to absenteeism and lost productivity (Max, 2001; The Robert Wood Johnson Foundation, 2001). The direct medical costs of complicated birth are 66 percent higher for pregnant smokers than for pregnant nonsmokers, and the direct medical costs of the effects of parental smoking on children aged 6 and under are estimated at $4.6 billion (Aligne and Stoddard, 1997).
Smoking cessation is extremely cost-effective compared with other preventive interventions (Cromwell et al., 1997). Treating tobacco dependence in pregnancy generates $3– 6 in savings for every dollar invested (Marks et al., 1990). On the basis of estimates of both the magnitude of disease and injury prevented and cost-effectiveness (net cost of per quality-adjusted life years saved), assessment and counseling of adults for tobacco use has been ranked the second-highest priority among all 30 clinical preventive services recommended by the U.S. Preventive Services Task Force, and is the single highest-ranked service now in use with less than 50 percent of its target audience (Coffield et al., 2001).
Improvability
Closing the gap between what is known and what is done about treating tobacco use and dependence has been identified as one of the nation’s leading opportunities for health care quality improvement (Coffield et al., 2001). Most smokers want to quit, but only about 50 percent of patients report having received smoking cessation advice from their doctor in the past year, and even fewer (25 percent) report any further counseling or pharmacotherapy (Coffield et al., 2001; Thorndike et al., 1998; Tomar et al., 1996). Almost all OB-GYNs report that they ask about tobacco use in pregnancy, but fewer than half go on to discuss cessation strategies and offer self-help materials (The Robert Wood Johnson Foundation, 2002). Healthy smokers are less likely to receive evidence-based smoking treatment than those already suffering from tobacco-related disease (Jaen et al., 1998).
Providers have long reported a lack of training, reimbursement, and supportive office systems as barriers to the delivery of best-practice care for tobacco use and dependence (Glynn et al., 1993). Numerous surveys and reviews have documented limited system supports, insurance coverage, and reimbursement for smoking cessation services (e.g., (Goodwin et al., 2001; Harris et al., 2001; McPhillips-Tangum, 1998; McPhillips-Tangum C, 2001; Partnership for Prevention, 1999;
Solberg et al., 1997). Medicare, for example, provides no coverage for such services (Ossip-Klein et al., 1999). In 2000, only 33 states provided Medicaid coverage for any of the proven treatments recommended by the guideline, and only 21 states covered the no-medication counseling services appropriate for pregnant smokers (Ibrahim et al., 2002).
On the other hand, growing evidence and emerging evidence-based guidelines point to the types of system changes and reimbursement policies that can improve treatment delivery and use. CDC’s Guide to Community Preventive Services cites strong scientific evidence for recommending multicomponent health care system interventions that include at a minimum a provider reminder system and a provider education program. Such interventions have been found effective in increasing providers’ delivery of advice to quit and patients’ cessation of tobacco (Centers for Disease Control and Prevention, 2001c). The clinical practice guideline of the U.S. Public Health Service (Fiore et al., 2000) recommends creating clinic screening systems (e.g., expanding the vital signs to include tobacco-use status) or manual or computerized reminder systems as essential to assessment and intervention for routine tobacco use. Both the guideline and the CDC Guide to Community Preventive Services recommend reducing patient out-of-pocket costs for effective cessation therapies in light of evidence for increased use of effective therapy and cessation of tobacco use as a result of such measures. These findings fit well with growing evidence that multicomponent system changes (e.g., combining education, performance feedback, reminders, local consensus processes, and incentives) are often needed to promote guideline-based care (Bero et al., 1998) and prevention (Hulscher et al., 1999). The findings are also consistent with a recent review proposing that the organizational and system changes recommended to improve the delivery of preventive care, including treatment for smoking dependence in particular, are fundamentally the same as those recommended by the Chronic Care Model (Wagner et al., 1996) for improving the management of chronic disease (Glasgow et al., 2001).
Inclusiveness
Americans with the fewest educational and economic resources are most likely to smoke; there are also important variations in tobacco use based on race, ethnicity, and gender (Centers for Disease Control and Prevention, 2001c; United States Department of Health and Human Services, 2000). The percentage of those aged 25 and older with less than 12 years of education who are current smokers is nearly three times that of persons with 16 or more years of education. Overall, American Indians and Alaska Natives and blue-collar workers have the highest rates of adult smoking. Rates of smoking among men (25.7 percent) are slightly higher than among women (21.5 percent). Among Asians and Pacific Islanders, however, rates of smoking are more than four times higher among men than women. Smoking prevalence in pregnancy is at least 12 times higher among women with 9–11 years of education (25 percent) than among women who hold a college degree (2 percent) (Martin et al., 2001), and is particularly common among Caucasian, American Indian, and Hawaiian women. Low-income and minority smokers continue to be the least likely to receive appropriate treatment for their tobacco use and dependence (Fiore et al., 1990; Gilpin et al., 2001).
The harm caused by smoking and the benefits of cessation are apparent across the life span-from maternal smoking and cessation in pregnancy, to the effects of parental smoking/ cessation on young children (DiFranza and Lew, 1996; Wisborg et al., 1999), to smoking and cessation among adults 65 and older (Ossip-Klein et al., 1999; Rimer et al., 1990; Taylor et al., 2002). The harm and benefits are also important across the spectrum of health care, from staying healthy, to improving outcomes from acute care (e.g., medication efficacy, wound healing), to improving the management and slowing the progression of chronic disease (United States Department of Health and Human Services, 1990). Besides being declared
a chronic disease in its own right (Fiore et al., 2000), smoking is an essential factor in many chronic disease management protocols (e.g., asthma, cancer, diabetes, heart disease).
|
Box 3–12 Tobacco Dependence Treatment in Adults Group Health Cooperative (GHC) of Puget Sound undertook a well-documented organizational effort to integrate screening and treatment for tobacco use and dependence into routine health care for all its members. This effort has recently been described with reference to the elements of the Chronic Care Model (Glasgow et al., 2001). Organizational leadership and incentives were substantial. Senior leaders made reducing tobacco use their top prevention priority. They worked to systematically improve key clinical processes and realign incentives as necessary to achieve this goal; the changes made included supporting dedicated clinic staff, offering incentive to providers, and eliminating patient copayments for smoking cessation counseling (e.g., (Curry et al., 1998; McAfee et al.,1995).Clinical information systems were used to create a population-based registry of tobacco users, identified at the time of enrollment and patient visits, to track utilization of cessation treatment resources and to generate patient Quitline calls and provider feedback reports. Decision support was provided through extensive provider training, ongoing consultation, and feedback from the automated patient assessment and treatment tracking system. Practice redesign and self-management support involved the use of a formal treatment program that minimized provider burden by relying on pre-tested self-help materials and telephone counseling to supply essential counseling and pharmacotherapy prescriptions. Finally, linkages to community resources included referral to local quit-smoking clinics and related health improvement programs (e.g., weight loss, physical activity, stress management), as well as support for workplace promotional campaigns, smoking restrictions, and other beneficial local policy changes (Thompson, 1996). Fully implemented in 1993, this initiative has produced a variety of impressive behavioral, clinical, and economic outcomes. For instance, by 1994 the prevalence of tobacco use at GHC had dropped to 15.5 percent from 25 percent in 1985, with comparable data for Washington State showing a much slower rate of decline (McAfee et al., 1995). Rates of tobacco use documentation rose from 40 percent in 1994 to 98 percent in 1999 (Dacey, 2000; McAfee et al., 1995). The proportions of patients enrolled in GHC’s formal quitting programs and GHC’s overall population quit rate rose substantially with the elimination of copayments (Curry et al., 1998). And compared with continued smokers, quitters who took part in GHC’s self-help program used significantly fewer inpatient and outpatient health care services 3 to 5 years after quitting (Wagner et al., 1995). |
Obesity
Aim
To improve national rates of screening and appropriate treatment for obesity among children and adults.
Rationale for Selection
Impact
The prevalence of overweight and obesity among Americans has reached epidemic proportions (Mokdad et al., 2001; Yanovski and Yanovski, 2002). The prevalence of obesity has doubled among adults and tripled among children in recent decades, and current trends suggest that prevalence rates will continue to rise (United States Department of Health and Human Services, 2001a). In 1999, an estimated 61 percent of adults (131 million individuals) were classified as either overweight or obese. The prevalence of overweight among children aged 6–11 increased from 4 percent in 1963 to 13 percent in 1999 (the latter figure representing almost 14 million children) (United States Department of Health and Human Services, 2001a).
Over 300,000 deaths are attributed to obesity each year, and experts suggest that the combined effects of sedentary lifestyles and unhealthy food choices that contribute to the development of obesity will eventually make this condition the number one cause of preventable premature death and disability. Obesity is a major risk factor for the leading causes of death and disability: heart disease, including high blood pressure; stroke; some forms of cancer; and diabetes, including insulin resistance and metabolic syndrome (which encompasses some combination of insulin resistance, hypertension, and abdominal obesity and affects an estimated 42 million adults) (Must et al., 1999; United States Department of Health and Human Services, 2001a). Approximately 60 percent of overweight children aged 5–10 already have one associated biochemical or clinical cardiovascular risk factor, such as hyperlipedemia, elevated blood pressure, or increased insulin levels, and 25 percent have two or more (Freedman et al., 1999). In fact, the obesity epidemic has caused a related epidemic of type II diabetes, including unprecedented rates of type II juvenile diabetes (McGinnis, 2002). In part as a result, obesity now outranks both smoking and drinking in its deleterious effects on health and health care costs, including spending on inpatient and ambulatory care and medication use: adult obesity increases health care costs by 36 percent and medication costs by 77 percent as compared with care for adults of normal weight (Sturm, 2002). Obesity’s total costs to the nation are now estimated at $117 billion annually, including $61 billion in direct health care costs and $56 billion in indirect costs (United States Department of Health and Human Services, 2001a).
Improvability
Nearly half of U.S. women and more than a third of U.S. men report having attempted to lose weight, most unsuccessfully (Serdula et al., 1999). Several pharmacological agents, many over-the-counter products, and various diets and dietary weight loss aids and programs are widely promoted but essentially unproven to help Americans combat obesity (Fontanarosa, 1999). However, growing research evidence and emerging evidence-based guidelines indicate the effectiveness of three major forms of treatment for obesity that can be offered through the health care system: counseling and behavioral interventions aimed at lifestyle modification, pharmacotherapy, and surgery (Epstein et al., 2001; National Heart Lung and Blood Institute (NHLBI), 1998; Wadden and Foster, 2000; Yanovski and Yanovski, 2002).
In 1998, the National Institutes of Health published Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults, outlining effective behavioral and medical approaches to the assessment, treatment, and management of overweight and obese patients in primary care settings (National Heart Lung and Blood
Institute (NHLBI), 1998). Behavioral treatments focused on helping people to restrict caloric intake through dietary change and to increase caloric expenditure through greater physical activity can help them lose 5–10 percent of pretreatment weight over a period of 4–12 months, though these weight losses typically are not maintained in the absence of follow-up treatment or environmental changes (Wadden and Foster, 2000; Yanovski and Yanovski, 2002).
Higher-intensity treatments and those that include maintenance components are more successful in promoting sustained weight loss. Current research is exploring innovative maintenance strategies (Jeffery et al., 2000), including those based on the use of information technologies (e.g, telephone, Internet) that can deliver individually tailored interventions in ways that dramatically reduce the counseling burden on busy primary care providers (Boucher et al., 1999). Likewise, there is growing evidence for the effectiveness, health benefit, and cost-effectiveness of individual and family-oriented behavioral treatment for pediatric obesity (Epstein, 1996; Epstein et al., 2001; Goldfield et al., 2001). Pharmacological approaches for treating adult obesity, including recently approved sibutramine and orlistat, used alone and in concert with behavioral treatments, show new promise, as do surgical bariatric treatments, including gastric bypass, for selected morbidly and medically high-risk obese adults (Yanovski and Yanovski, 2002).
Newly released guidelines of the U.S. Preventive Services Task Force recommend intensive dietary behavioral counseling for at-risk adult patients with known risk factors, including obesity, for diet-related disease. The guidelines conclude, however, that there is currently insufficient evidence to support recommending for or against routine behavioral counseling to promote healthy diet or physical activity among general populations of primary care patients (United States Preventive Services Task Force, 2002a; 2003). Recent CDC (2001) data indicate that 58 percent of obese patients received no counseling about weight loss from their health care providers. Another study found that about a fifth of overweight and obese patients did not realize they had the problem-nor did their physicians-indicating that body mass index screening should be made routine (Caccamese et al., 2002).
Inclusiveness
The nation’s obesity epidemic has spared no region of the country or segment of the population (Mokdad et al., 2001). Obesity prevalence remains highest, however, among low-income Americans and members of underserved ethnic and racial minority groups. Specifically, the prevalence of obesity is greater among African American, Native American, and Hispanic populations as compared with Caucasians. Behavioral Risk Factor Surveillance System data from 2000 show that the proportion obese varied from 18.5 percent among Caucasians to 29.3 percent among African Americans and 23.4 percent among Hispanics. The contrasts are even greater for women. Among U.S. women aged 18–49, the prevalence of overweight or obesity was 59.9 percent for African American women, 61.7 percent for Mexican American women, and 39 percent for Caucasian women (Centers for Disease Control and Prevention, 2001a). Among children, the prevalence of overweight is increasing more rapidly for African Americans and Hispanics than for Caucasians. Between 1986 and 1998, the prevalence of overweight increased by more than 120 percent among African American and Hispanic children, compared with a 50 percent increase among Caucasians (Strauss and Pollack, 2001).
REFERENCES
Ades, P.A.2001. Cardiac rehabilitation and secondary prevention of coronary heart disease. N Engl J Med345 (12):892–902.
Administration on Aging. “A Profile of Older Americans: 2001.” Online. Available at http://www.aoa.gov/aoa/stats/profile/2001/1.html [accessed July 31, 2002].
Aligne, C.A., and J.J.Stoddard. 1997. Tobacco and children. An economic evaluation of the medical effects of parental smoking. Arch Pediatr Adolesc Med151 (7):648–53.
Allard, P., E.Maunsell, J.Labbe, and M.Dorval. 2001. Educational interventions to improve cancer pain control: A systematic review. J Palliat Med4 (2): 191–203.
American Academy of Pediatrics. 2002. “Flu Vaccine Encouraged for Kids 6–23 Months.” Online. Available at http://www.aap.org/advocacy/releases/decinfluenza.htm [accessed Dec. 3, 2002].
American Cancer Society. 2001. Guidelines on Screening and Surveillance for the Early Detection of Adenomatous Polyps and Colorectal Cancer. Atlanta, GA: American Cancer Society.
——. 2002. Cancer facts & figures 2002. Atlanta, GA: American Cancer Society.
American College of Physicians. 2002. Annals of Internal Medicine. Pp. 641, 648Interventions that Increase Use of Adult Immunization and Cancer Screening Services: A Meta-Analysis. Philadelphia, PA: American Society of Internal Medicine.
American Diabetes Association. “Facts & Figures: The Impact of Diabetes.” Online. Available at http://www.diabetes.org/main/application/commercewf;JSESSIONID_WLCS_DEFAULT http://www.diabetes.org/main/info/facts/impact/default2.jsp [accessed Aug. 6, 2002].
American Heart Association. 2001. 2002 Heart and Stroke Statistical Update.Dallas, TX: American Heart Association.
American Heart Association. 2002. “High Blood Pressure Statistics.” Online. Available at http://www.americanheart.org/presenter.jhtml?identifier=2139 [accessed Aug. 12, 2002].
American Hospital Association. 2001. “Fast Facts on U.S. Hosptials from Hostipal Statistics.” Online. Available at www.hospitalconnect.com/aha/resource_center/fastfacts/fast_facts_US_hospitals.html [accessed Sept. 4, 2002].
American Medical Association. “Health Literacy Introductory Kit.” Online. Available at http://www.ama-assn.org/ama/pub/printcat/8035.html [accessed Dec. 22, 2002].
American Medical Association white paper on elderly health. Report of the Council on Scientific Affairs. 1990. Arch Intern Med150 (12):2459–72.
American Psychiatric Association. 1994. Diagnostic and Statistical Manual of Mental Disorders.4th edition.Washington, D.C.:
Anderson, G., and J.R.Knickman. 2001. Changing the chronic care system to meet people’s needs. Health Aff (Millwood)20 (6): 146–60.
Anderson, G.F.2002a. Testimony by Dr. Gerard Anderson, Director of Partnership for Solutions at Johns Hopkins, before the House Ways and Means Health Subcommittee on April 16, 2002.
——. 2002b. Powerpoint Presentation: Multiple Chronic Conditions and Functional Limitations. Presented at May 9–10, 2002 Priority Areas for Quality Improvement Meeting .
Anderson, K.O., S.P.Richman, J.Hurley, G.Palos, V.Valero, T.R.Mendoza, I.Gning, and C.S. Cleeland. 2002. Cancer pain management among underserved minority outpatients: Perceived needs and barriers to optimal control. Cancer94 (8):2295–304.
Anderson, L.M., and D.S. May. 1995. Has the use of cervical, breast, and colorectal cancer screening increased in the United States?Am J Public Health85 (6): 840–2.
Antman, Mark. 2002. Personal Communication AMA. Personal communication to Kevin Weiss.
Bailit, J.L., J.M.Garrett, W.C.Miller, M.J. McMahon, and R.C.Cefalo. 2002. Hospital primary cesarean delivery rates and the risk of poor neonatal outcomes. Am J Obstet Gynecol 187 (3):721–7.
Baker, F.M., and C.C.Bell. 1999. Issues in the psychiatric treatment of African Americans. Psychiatr Serv50 (3):362–8.
Bastani, R., B.A.Berman, T.R.Belin, L.A.Crane, A.C.Marcus, K.Nasseri, N.Herman-Shipley, S.Bernstein, and C.E.Henneman. 2002. Increasing cervical cancer screening among underserved women in a large urban county health system: Can it be done? What does it take?Med Care40 (10):891–907.
Bates, D.W., D.J.Cullen, N.Laird, L.A.Petersen, S.D.Small, D.Servi, G.Laffel, B.J.Sweitzer, B.F.Shea, and R.Hallisey. 1995. Incidence of adverse drug events and potential adverse drug events. Implications for prevention. ADE Prevention Study Group. JAMA274 (1):29–34.
Bates, D.W., N.Spell, D.J.Cullen, E.Burdick, N. Laird, L.A.Petersen, S.D.Small, B.J. Sweitzer, and L.L.Leape. 1997. The costs of adverse drug events in hospitalized patients. Adverse Drug Events Prevention Study Group. JAMA277(4):307–11.
Bates, D.W., J.M.Teich, J.Lee, D.Seger, G.J. Kuperman , N. Ma’Luf, D.Boyle, and L.Leape. 1999. The impact of computerized physician order entry on medication error prevention. J Am Med Inform Assoc6 (4):313–21.
Bates-Jensen, B.M.2001. Quality indicators for prevention and management of pressure ulcers in vulnerable elders. Ann Intern Med135 (8 Pt 2):744–51.
Bauman, L.J., D.Drotar, J.M.Leventhal, E.C. Perrin, and I.B.Pless. 1997. A review of psychosocial interventions for children with chronic health conditions. Pediatrics100 (2 Pt 1):244–51.
Beck, A., J.Scott, P.Williams, B.Robertson, D. Jackson, G.Gade, and P.Cowan. 1997. A randomized trial of group outpatient visits for chronically ill older HMO members: The Cooperative Health Care Clinic. J Am Geriatr Soc45 (5):543–9.
Beck, L.F., B.Morrow, L.E.Lipscomb, C.H. Johnson, M.E.Gaffield, M.Rogers, and B.C. Gilbert. 2002. Prevalence of selected maternal behaviors and experiences. Pregnancy Risk Assessment Monitoring System (PRAMS), 1999. MMWR Surveill Summ51 (2): 1–27.
Becker, P.M., L.J.McVey, C.C.Saltz, J.R. Feussner, and H.J.Cohen. 1987. Hospital-acquired complications in a randomized controlled clinical trial of a geriatric consultation team. JAMA257 (17):2313–7.
Bernabei, R., G.Gambassi, K.Lapane, F.Landi, C. Gatsonis, R.Dunlop, L.Lipsitz, K.Steel, and V. Mor. 1998. Management of pain in elderly patients with cancer. SAGE Study Group. Systematic Assessment of Geriatric Drug Use via Epidemiology. JAMA279 (23): 1877–82.
Bero, L.A., R.Grilli, J.M.Grimshaw, E.Harvey, A. D.Oxman, and M.A.Thomson. 1998. Closing the gap between research and practice: An overview of systematic reviews of interventions to promote the implementation of research findings. The Cochrane Effective Practice and Organization of Care Review Group. BMJ317 (7156) :465–8.
Blazer, D.G., R.C.Kessler, K.A.McGonagle, and M.S.Swartz. 1994 . The prevalence and distribution of major depression in a national community sample: The National Comorbidity Survey. Am J Psychiatry151 (7):979–86.
Bodenheimer, T.1999. Long-term care for frail elderly people—the On Lok model. N Engl J Med341 (17):1324–8.
Bodenheimer, T., K.Lorig, H.Holman, and K. Grumbach. 2002. Patient self-management of chronic disease in primary care. JAMA288 (19):2469–75.
Boucher, J.L., J.D.Schaumann, and N.P.Pronk. 1999. The effectiveness of telephone-based counseling for weight management. Diab Spectrum12:121–23.
Breslau, N., K.S.Staruch, and E.A.Mortimer Jr. 1982. Psychological distress in mothers of disabled children. Am J Dis Child136(8):682– 6.
Brown, M.L., G.F.Riley, N.Schussler, and R. Etzioni. 2002. Estimating health care costs related to cancer treatment from SEER— Medicare data. Med Care40(8 Suppl):IV-104– 17.
Broyles, R.S., J.E.Tyson, E.T.Heyne, R.J.Heyne, J.F.Hickman, M.Swint, S.S.Adams, L.A. West, N.Pomeroy, P.J.Hicks, and C.Ahn. 2000. Comprehensive follow-up care and life-threatening illnesses among high- risk infants: A randomized controlled trial. JAMA284 (16):2070–6.
Buchner, D.M., and E.H.Wagner. 1992. Preventing frail health. Clin Geriatr Med8
Burgess, S., J.Geddes, K.Hawton, E.Townsend, K. Jamison, and G.Goodwin. 2001. Lithium for maintenance treatment of mood disorders. Cochrane Database Syst Rev(3):CD003013.
Burns, R.B., E.P.McCarthy, M.A.Moskowitz, A. Ash , R.L.Kane, and M.Finch. 1997. Outcomes for older men and women with congestive heart failure. J Am Geriatr Soc45 (3):276–80.
Burt, V.L., P.Whelton, E.J.Roccella, C.Brown, J. A.Cutler, M.Higgins, M.J.Horan, and D. Labarthe. 1995. Prevalence of hypertension in the US adult population. Results from the Third National Health and Nutrition Examination Survey, 1988–1991. Hypertension25 (3):305– 13.
Caccamese, S.M., K.Kolodner, and S.M.Wright. 2002. Comparing patient and physician perception of weight status with body mass index. Am J Med112 (8):662–6.
Cadman, D., M.Boyle, P.Szatmari, and D.R. Offord. 1987. Chronic illness, disability, and mental and social well-being: Findings of the Ontario Child Health Study. Pediatrics79 (5):805–13.
Caro, J.J., A.J.Ward, and J.A.O’Brien. 2002. Lifetime costs of complications resulting from type 2 diabetes in the U.S.Diabetes Care25 (3):476–81.
Carraccio, C.L., K.S.Dettmer, M.L.duPont, and A.D.Sacchetti. 1998. Family member knowledge of children’s medical problems: The need for universal application of an emergency data set. Pediatrics102 (2 Pt 1):367–70.
Cassell, E.J.1992. The nature of suffering: Physical, psychological, social, and spiritual aspects. NLN Publ(15–2461): 1–10.
Center for Health Improvement. 2001. California Prevention Report: Delivery of High-Yield Clinical Preventive Services by Managed Health Care Plans in California.Sacramento, CA: CHI.
Centers for Disease Control and Prevention. 1998. Surveillance for Asthma—United States, 1960– 1995.Vol. 47 (SS-1). Atlanta, GA: MMWR.
——. 1999a. “National Hospital Ambulatory Medical Care Survey (NHAMCS).” Online. Available at http://www.cdc.gov/nchs/about/major/ahcd/nhamcsds.htm [accessed Nov. 13, 2002a].
——. 1999b. “National Hospital Discharge Survey (NHDS).” Online. Available at http://www.cdc.gov/nchs/about/major/hdasd/nhds.htm [accessed Nov. 13, 2002b].
——. 2000a. Behavioral Risk Factor Surveillance System Survey Data.Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention.
——. 2000b. “Guide to Community Preventive Services (Community Guide).” Online. Available at www.thecommunityguide.org/home_f.html
——. 2000c. “Guidelines & Recommendations: Overview of the 7 CDC Guidelines on Prevention of Healthcare-Associated Infections.” Online. Available at www.cdc.gov/ncidod/hip/guide/overview.htm [accessed Aug. 29, 2002c].
——. 2000d. Unrealized Prevention Opportunities: Reducing the Health and Economic Burden of Chronic Disease.Atlanta, GA: CDC, National Center for Chronic Disease Prevention and Health Promotion.
——. 2001a. Behavioral Risk Factor Surveillance System Survey Data.Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention.
——. 2001b. “About NNIS (National Nosocomial Infections Surveillance).” Online. Available at www.cdc.gov/ncidod/hip/nnis/@nnis.htm [accessed Aug. 29, 2002b].
——. 2001c. The Guide to Community Preventive Services: Tobacco Use Prevention and Control. Reviews, recommendations and expert commentary. Am J Prev Med(20(2)): Supplement.
——. 2001d. National Nosocomial Infections Surveillance (NNIS) System Report, Data Summary from January 1992-June 2001, Issued August 2001. Am J Infect Control29:404–21.
——. 2002a. Careful Antibiotic Use: Resistance and Antibiotic Use.
——. 2002b. State-specific mortality from stroke and distribution of place of death—United States, 1999. JAMA288 (3):309–10.
——. 2002c. “Surveillance and Research Fact Sheet: Increased Risk of Dying from Pregnancy among Hispanic Women in the United States.” Online. Available at http://www.cdc.gov/nccdphp/drh/surv_hispwus.htm [accessed Nov. 18, 2002c].
Chin, M.H., and L.Goldman. 1996. Correlates of major complications or death in patients admitted to the hospital with congestive heart failure. Arch Intern Med156 (16): 1814–20.
Chin, M.H., J.X.Zhang, and K.Merrell. 1998. Diabetes in the African-American Medicare population. Morbidity, quality of care, and resource utilization. Diabetes Care21 (7):1090–5.
Cifu, D.X., and D.G.Stewart. 1999. Factors affecting functional outcome after stroke: A critical review of rehabilitation interventions. Arch Phys Med Rehabil80 (5 Suppl 1):S35–9.
Ciota, R., and N.Singer. 1992. Steering Committee on Home Care for Chronically Ill Children, 1987–1992.Final Report.Syracuse, NY: Central New York Health Systems Agency, Inc.
Clark, C.M., J.E.Fradkin, R.G.Hiss, R.A.Lorenz, F.Vinicor, and E.Warren-Boulton. 2000. Promoting early diagnosis and treatment of type 2 diabetes: The National Diabetes Education Program. JAMA284 (3):363–5.
Clark, N.M., C.H.Feldman, D.Evans, Y. Wasilewski, and M.J.Levison. 1984. Changes in children’s school performance as a result of education for family management of asthma. J Sch Health54 (4): 143–5.
Classen, D.C.1998. Adverse drug events and medication errors: The scientific perspective. Enhancing Patient Safety and Reducing Errors in Health Care.
Classen, D.C., S.L.Pestotnik, R.S.Evans, J.F. Lloyd, and J.P.Burke. 1997. Adverse drug events in hospitalized patients. Excess length of stay, extra costs, and attributable mortality. JAMA277 (4):301–6.
Cleeland, C.S., R.Gonin, A.K.Hatfield, J.H. Edmonson, R.H.Blum, J.A.Stewart, and K.J. Pandya. 1994. Pain and its treatment in outpatients with metastatic cancer. N Engl J Med330 (9):592–6.
Coffield, A.B., M.V.Maciosek, J.M.McGinnis, J. R.Harris, M.B.Caldwell, S.M.Teutsch, D. Atkins, J.H.Richland, and A.Haddix. 2001. Priorities among recommended clinical preventive services. Am J Prev Med21 (1):1–9.
Cohen, D.J.2002. Invasive vs conservative management of acute coronary syndromes: Do the data support the guidelines?JAMA288 (15):1905–7.
Cole, S., N.Farber, J.Weiner, M.Sulfaro, A.Silver, and D.Katzelnick. 2002. Powerpoint Presentation: Depression in Congestive Heart Failure.
.2002Personal Conversation Steven Cole.
Cook, N.R., J.Cohen, P.R.Hebert, J.O.Taylor, and C.H.Hennekens. 1995. Implications of small reductions in diastolic blood pressure for primary prevention. Arch Intern Med155 (7):701–9.
Coupey, S.M., and M.I.Cohen. 1984. Special considerations for the health care of adolescents with chronic illnesses. Pediatr Clin North Am 31 (1):211–9.
Cringles, M.C.2002. Developing an integrated care pathway to manage cancer pain across primary, secondary and tertiary care. Int J Palliat Nurs8 (5):247–55.
Crismon, M.L., M.Trivedi, T.A.Pigott, A.J.Rush, R.M.Hirschfeld, D.A.Kahn, C.DeBattista, J. C.Nelson, A.A.Nierenberg, H.A.Sackeim, and M.E.Thase. 1999. The Texas Medication Algorithm Project: Report of the Texas Consensus Conference Panel on Medication Treatment of Major Depressive Disorder. J Clin Psychiatry60 (3): 142–56.
Cromwell, J., W.J.Bartosch, M.C.Fiore, V. Hasselblad, and T.Baker. 1997. Cost-effectiveness of the clinical practice recommendations in the AHCPR guideline for smoking cessation. Agency for Health Care Policy and Research. JAMA278 (21): 1759–66.
Cullen, D.J.1998. The effect of pharmacist participation as a member of the patient care team in reducing adverse drug events in a medical intensive care unit. Enhancing Patient Safety and Reducing Errors in Health Care.
Curry, S.J., L.C.Grothaus, T.McAfee, and C. Pabiniak. 1998. Use and cost effectiveness of smoking-cessation services under four insurance plans in a health maintenance organization. N Engl J Med339 (10):673–9.
Dacey, S.2000. Tobacco cessation program implementation-from plans to reality: skill building workshop-group model. Tob Control 9 Suppl 1:I30–2.
Dahl, J.L., M.E.Bennett, M.D.Bromley, and D.E. Joranson. 2002. Success of the state pain initiatives: Moving pain management forward. Cancer Pract10 Suppl 1:S9-S13.
Depression Guideline Panel. 1993. Depression in Primary Care.Rockville, MD: U.S. Dept. of Health and Human Agencies, Agency for Health Care Policy and Research.
Dewar, M.A., K.Hall, and J.Perchalski. 1992. Cervical cancer screening. Past success and future challenge. Prim Care19 (3):589–606.
Diette, G.B., E.A.Skinner, L.E.Markson, P. Algatt-Bergstrom, T.T.Nguyen, R.D.Clark, and A.W.Wu. 2001. Consistency of care with national guidelines for children with asthma in managed care . J Pediatr138 (1):59–64.
DiFranza, J.R., and R.A.Lew. 1996. Morbidity and mortality in children associated with the use of tobacco products by other people. Pediatrics 97 (4):560-8.
Dixon, L., L.Green-Paden, J.Delahanty, A. Lucksted, L.Postrado, and J.Hall. 2001. Variables associated with disparities in treatment of patients with schizophrenia and comorbid mood and anxiety disorders. Psychiatr Serv52 (9):1216–22.
Dosa, N.P., N.M.Boeing, N.Ms, and R.K.Kanter. 2001. Excess risk of severe acute illness in children with chronic health conditions. Pediatrics107 (3):499–504.
Drake, R.E., G.J.McHugo, R.R.Bebout, D.R. Becker, M. Harris, G. R. Bond, and E. Quimby. 1999. A randomized clinical trial of supported employment for inner-city patients with severe mental disorders. Arch Gen Psychiatry56 (7):627-33.
Drake, R. E., and K. T. Mueser. 2000. Psychosocial approaches to dual diagnosis. Schizophr Bull 26(1):105-18.
Druss, B.G., S.C.Marcus, M.Olfson, and H.A. Pincus. 2002. The most expensive medical conditions in America: This nationwide study fund that the most disabling conditions are not necessarity the ones we spend the most to treat. Health Aff (Millwood)21 (4):105–11.
Druss, B.G., S.C.Marcus, M.Olfson, T.Tanielian, L.Elinson, and H.A.Pincus. 2001a. Comparing the national economic burden of five chronic conditions. Health Aff (Millwood)20 (6):233–41.
Druss, B.G., R.M.Rohrbaugh, C.M.Levinson, and R.A.Rosenheck. 2001b. Integrated medical care for patients with serious psychiatric illness: A randomized trial. Arch Gen Psychiatry58 (9):861–8.
Egarter, C., H.Leitich, H.Karas, F.Wieser, P. Husslein, A.Kaider, and M.Schemper. 1996. Antibiotic treatment in preterm premature rupture of membranes and neonatal morbidity: A metaanalysis. Am J Obstet Gynecol174 (2):589–97.
Emergency Medical Services for Children, Task Force on Children with Special Health Care Needs. EMS for children: Recommendations for coordinating.
Epstein, L.H.1996. Family-based behavioural intervention for obese children. Int J Obes Relat Metab Disord20 Suppl 1:S14–21.
Epstein, L.H., J.N.Roemmich, and H.A.Raynor. 2001. Behavioral therapy in the treatment of pediatric obesity. Pediatr Clin North Am48 (4):981–93.
Evans, R. 3rd, P.J.Gergen, H.Mitchell, M.Kattan, C.Kercsmar, E.Crain, J.Anderson, P. Eggleston, F.J.Malveaux, and H.J.Wedner. 1999. A randomized clinical trial to reduce asthma morbidity among inner-city children: Results of the National Cooperative Inner-City Asthma Study. J Pediatr135 (3):332–8.
Evans, R.S., S.L.Pestotnik, D.C.Classen, S.B. Bass, and J.P.Burke. 1992. Prevention of adverse drug events through computerized surveillance. Proc Annu Symp Comput Appl Med Care :437–41.
Fahey, T., N.Stocks, and T.Thomas. 1998. Quantitative systematic review of randomised controlled trials comparing antibiotic with placebo for acute cough in adults. BMJ316 (7135):906–10.
Ferrell, B.R., M.Rhiner, M.Z.Cohen, and M. Grant. 1991. Pain as a metaphor for illness. Part I: Impact of cancer pain on family caregivers. Oncol Nurs Forum18 (8): 1303–9.
Finkelstein, J.A., R.L.Davis, S.F.Dowell, J.P. Metlay, S.B.Soumerai, S.L.Rifas-Shiman, M. Higham, Z.Miller, I.Miroshnik, A.Pedan, and R.Platt. 2001. Reducing antibiotic use in children: A randomized trial in 12 practices. Pediatrics108 (1):1–7.
Finkelstein, J.A., P.Lozano, K.A.Streiff, K.E. Arduino, C.A.Sisk, E.H.Wagner, K.B.Weiss, and T.S.Inui. 2002. Clinical effectiveness research in managed-care systems: Lessons from the Pediatric Asthma Care PORT. Patient Outcomes Research Team . Health Serv Res37 (3):775–89.
Fiore, M.C., W.C.Bailey, and S.J.Cohen. 2000. Treating Tobacco Use and Dependence: Clinical Practice Guideline.Rockville, MD: U. S. Department of Health and Human Services, Public Health Service.
Fiore, M.C., T.E.Novotny, J.P.Pierce, G.A. Giovino, E.J.Hatziandreu, P.A.Newcomb, T. S.Surawicz, and R.M.Davis. 1990. Methods used to quit smoking in the United States. Do cessation programs help?JAMA263 (20):2760–5.
Fitzgibbon, D.R.2001. Cancer Pain: Management. Bonica’s Management of Pain.Philadelphia: Lippincott Williams & Wilkins.
Fleming, B.B., S.Greenfield, M.M.Engelgau, L. M.Pogach, S.B.Clauser, and M.A.Parrott. 2001. The Diabetes Quality Improvement Project: Moving science into health policy to gain an edge on the diabetes epidemic. Diabetes Care24 (10): 1815–20.
Fleming, B.E., and D.R.Pendergast. 1993. Physical condition, activity pattern, and environment as factors in falls by adult care facility residents. Arch Phys Med Rehabil74 (6):627–30.
Fontanarosa, P.B.1999. Patients, physicians, and weight control. JAMA282 (16):1581–2.
Forbes, S.A., P.W.Duncan, and M.K.Zimmerman. 1997. Review criteria for stroke rehabilitation outcomes. Arch Phys Med Rehabil78 (10):1112–6.
Frank, R.G., H.H.Goldman, and T.G.McGuire. 2001. Will parity in coverage result in better mental health care?N Engl J Med345 (23):1701–4.
Frank, R.G., H.A.Huskamp, T.G.McGuire, and J. P.Newhouse. 1996. Some economics of mental health ‘carve-outs’. Arch Gen Psychiatry 53 (10):933–7.
Freburger, J.K.1999. Analysis of the relationship between the utilization of physical therapy services and outcomes for patients with acute stroke. Phys Ther79(10):906–18.
Freedman, D.S., W.H.Dietz, S.R.Srinivasan, and G.S.Berenson. 1999. The relation of overweight to cardiovascular risk factors among children and adolescents: The Bogalusa Heart Study. Pediatrics103 (6 Pt 1): 1175–82.
Freemantle, N., J.Cleland, P.Young, J.Mason, and J.Harrison. 1999. Beta Blockade after myocardial infarction: Systematic review and meta regression analysis. BMJ318 (7200): 1730–7.
Fretwell, M.1993. Principles of Geriatric Medicine and Gerontology. Pp. 241–8. Vol. Acute Hospital Care for Frail Older Patients, Chapter 22. 3rd edition.McGraw Hill.
Fried, L.P., and J.M.Guralnik. 1997. Disability in older adults: Evidence regarding significance, etiology, and risk. J Am Geriatr Soc45 (1):92– 100.
Fried, L.P., C.M.Tangen, J.Walston, A.B. Newman, C.Hirsch, J.Gottdiener, T.Seeman, R.Tracy, W.J.Kop, G.Burke, and M.A. McBurnie. 2001. Frailty in older adults: Evidence for a phenotype. J Gerontol A Biol Sci Med Sci56 (3):M 146–56.
Fried, L.P., and J.Walston. 1998. Principles of Geriatric Medicine and Gerontology . Pp. 1387– 402. Vol. Frailty and Failure ot Thrive. Chapter 109. 4th edition. McGraw Hill.
Fried, T.R., E.H.Bradley, V.R.Towle, and H. Allore. 2002. Understanding the treatment preferences of seriously ill patients. N Engl J Med346 (14):1061–6.
Gandhi, T.K., H.R.Burstin, E.F.Cook, A.L. Puopolo, J.S.Haas, T.A.Brennan, and D.W. Bates. 2000. Drug complications in outpatients. J Gen Intern Med15 (3): 149–54.
Garner, J.S., W.R.Jarvis, T.G.Emori, T.C.Horan, and J.M.Hughes. 1996. CDC definitions for nosocomial infections. Pp. A-1-A-20. Olmsted RN edition . St Louis: Mosby.
Gaynes, R., C.Richards, J.Edwards, T.G.Emori, T. Horan, J.Alonso-Echanove, S.Fridkin, R. Lawton, G.Peavy, and J.Tolson. 2001. Feeding back surveillance data to prevent hospital-acquired infections. Emerg Infect Dis 7 (2):295–8.
Gaynes, R.P.1997. Surveillance of nosocomial infections: A fundamental ingredient for quality. Infect Control Hosp Epidemiol18 (7):475–8.
Gaynes, R.P., and S.Solomon. 1996a. Improving hospital-acquired infection rates: The CDC experience. Jt Comm J Qual Improv22 (7):457–67.
——. 1996b. Interhospital rate comparison issues: The CDC experience. Jt Comm J Qual Improv22 (7):457–67.
General Accounting Office. 1995. Prescription Drugs and the Elderly: Many Still Receive Potentially Harmful Drugs Despite Recent Improvements.GAO/HEHS-95–152. Washington, D.C.: U.S. General Accounting Office.
Gibson, P.G., J.Coughlan, A.J.Wilson, M. Abramson, A.Bauman, M.J.Hensley, and E.H. Walters. 2000. Self-management education and regular practitioner review for adults with asthma. Cochrane Database Syst Rev(2): CD001117.
Gibson, P.G., H.Powell, J.Coughlan, A.J.Wilson, M.J.Hensley, M.Abramson, A.Bauman, and E.H.Walters. 2002. Limited (information only) patient education programs for adults with asthma (Cochrane Review). Cochrane Database Syst Rev(2):CD001005.
Gill, T.M., D.I.Baker, M.Gottschalk, P.N. Peduzzi, H.Allore, and A.Byers. 2002. A program to prevent functional decline in physically frail, elderly persons who live at home. N Engl J Med347 (14):1068–74.
Gillum, R.F.1993. Epidemiology of heart failure in the United States. Am Heart J126(4):1042– 7.
Gilpin, E.A., S.L.Emery, and A.J.Farkas. 2001. The California Tobacco Control Program: A decade of progress, results from the California Tobacco Surveys, 1990–1999,La Jolla, CA: University of California San Diego.
Glasgow, R.E., M.M.Funnell, A.E.Bonomi, C. Davis, V.Beckham, and E.H.Wagner. 2002. Self-management aspects of the improving chronic illness care breakthrough series: Implementation with diabetes and heart failure teams. Ann Behav Med24 (2):80–7.
Glasgow, R.E., C.T.Orleans, and E.H.Wagner. 2001. Does the Chronic Care Model serve also as a template for improving prevention? Milbank Q79 (4):579–612, iv-v.
Glynn, T.J., M.W.Manley, L.I.Solberg, and J. Slade. 1993. Creating and maintaining an optimal medical practice environment for the treatment of nicotine addiction. Nicotine Addiction: Principles and Management.C.T. Orleans and J.Slade, eds. New York: Oxford University Press.
Goldberg, A.I., H.G.Gardner, and L.E.Gibson. 1994. Home care: The next frontier of pediatric practice. J Pediatr125 (5 Pt 1):686–90.
Goldfield, G.S., L.H.Epstein, C.K.Kilanowski, R. A.Paluch, and B.Kogut-Bossler. 2001. Cost-effectiveness of group and mixed family-based treatment for childhood obesity. Int J Obes Relat Metab Disord25 (12):1843–9.
Gonzales, R., J.F.Steiner, A.Lum, and P.H.Barrett Jr. 1999. Decreasing antibiotic use in ambulatory practice: Impact of a multidimensional intervention on the treatment of uncomplicated acute bronchitis in adults. JAMA281 (16):1512–9.
Gonzales, R., J.F.Steiner, and M.A.Sande. 1997. Antibiotic prescribing for adults with colds, upper respiratory tract infections, and bronchitis by ambulatory care physicians. JAMA278
Goodwin, M.A., S.J.Zyzanski, S.Zronek, M.Ruhe, S.M.Weyer, N.Konrad, D.Esola, and K.C. Stange. 2001. A clinical trial of tailored office systems for preventive service delivery: The Study to Enhance Prevention by Understanding Practice (STEP-UP). Am J Prev Med21 (1):20– 8.
Gortmaker, S.L., D.K.Walker, M.Weitzman, and A.M.Sobol. 1990. Chronic conditions, socioeconomic risks, and behavioral problems in children and adolescents. Pediatrics85 (3):267–76.
Grant, E.N., C.S.Lyttle, and K.B.Weiss. 2000. The relation of socioeconomic factors and racial/ethnic differences in US asthma mortality. Am J Public Health90 (12):1923–5.
Greineder, D.K., K.C.Loane, and P.Parks. 1999. A randomized controlled trial of a pediatric asthma outreach program. J Allergy Clin Immunol103 (3 Pt 1):436–40.
Grossman, D.C., L.M.Baldwin, S.Casey, B. Nixon, W.Hollow, and L.G.Hart. 2002. Disparities in infant health among American Indians and Alaska natives in US metropolitan areas. Pediatrics109 (4):627–33.
Guideline for the prevention of falls in older persons. American Geriatrics Society, British Geriatrics Society, and American Academy of Orthopaedic Surgeons Panel on Falls Prevention. 2001. J Am Geriatr Soc49 (5):664–72.
Guidelines for home care of infants, children, and adolescents with chronic disease. American Academy of Pediatrics Committee on Children with Disabilities. 1995. Pediatrics96 (1 Pt 1):161–64.
Halar, E.M.1999. Management of stroke risk factors during the process of rehabilitation. Secondary stroke prevention. Phys Med Rehabil Clin N Am10 (4):839–56, viii.
Haley, R.W., D.H.Culver, J.W.White, W.M. Morgan, T.G.Emori, V.P.Munn, and T.M. Hooton. 1985. The efficacy of infection surveillance and control programs in preventing nosocomial infections in US hospitals. Am J Epidemiol121 (2): 182–205.
Harlan, L.C., A.B.Bernstein, and L.G.Kessler. 1991. Cervical cancer screening: Who is not screened and why?Am J Public Health81 (7):885–90.
Harris, J.R., H.H.Schauffler, A.Milstein, P. Powers, and D.P.Hopkins. 2001. Expanding health insurance coverage for smoking cessation treatments: Experience of the Pacific Business Group on Health. Am J Health Promot15 (5):350–6.
Hartert, T.V., A.Togias, B.G.Mellen, E.F. Mitchel , M.S.Snowden, and M.R.Griffin. 2000. Underutilization of controller and rescue medications among older adults with asthma requiring hospital care. J Am Geriatr Soc48 (6):651–7.
Health care reform for Americans with severe mental illnesses: Report of the National Advisory Mental Health Council. 1993. Am J Psychiatry 150 (10):1447–65.
HealthParmers. 2000. “News Release June 12, 2000: HealthPartners Medical Group Recognized by American Diabetes Association for Quality Diabetes Care.” Online [accessed Aug. 26, 2002].
Heidenreich, P.A., and M.McClellan. 2001. Trends in treatment and outcomes for acute myocardial infarction: 1975–1995. Am J Med 110 (3): 165–74.
Higgins, M.W.1989. Chronic airways disease in the United States. Trends and determinants. Chest96 (3 Suppl):328S-34S.
Hirschfeld, R.M., M.B.Keller, S.Panico, B.S. Arons, D.Barlow, F.Davidoff, J.Endicott, J. Froom, M.Goldstein, J.M.Gorman, R.G. Marek, T.A.Maurer, R.Meyer, K.Phillips, J. Ross, T.L.Schwenk, S.S.Sharfstein, M.E. Thase, and R.J.Wyatt. 1997. The National Depressive and Manic-Depressive Association consensus statement on the undertreatment of depression. JAMA277 (4):333–40.
Hodgson, D. C., C.S.Fuchs, and J.Z.Ayanian. 2001. Impact of patient and provider characteristics on the treatment and outcomes of colorectal cancer. J Natl Cancer Inst93 (7):501–15.
Hogan, M.F.1998. The public sector and mental health parity: Time for inclusion. J Ment Health Policy Econ1 (4): 189–98.
Hoyert, D.L., M.A.Freedman, D.M.Strobino, and B.Guyer. 2001. Annual summary of vital statistics: 2000. Pediatrics108 (6): 1241–55.
Hulscher, M.E., M.Wensing, R.P.Grol, T.van der Weijden, and C.van Weel. 1999. Interventions to improve the delivery of preventive services in primary care. Am J Public Health89 (5):737– 46.
Hunt, D.L., R.B.Haynes, S.E.Hanna, and K. Smith. 1998. Effects of computer-based clinical decision support systems on physician performance and patient outcomes: A systematic review. JAMA280 (15):1339–46.
Huntington, J., and F.A.Connell. 1994. For every dollar spent—the cost-savings argument for prenatal care. N Engl J Med331 (19):1303–7.
Hyman, D.J., and V.N.Pavlik. 2001. Characteristics of patients with uncontrolled hypertension in the United States. N Engl J Med 345 (7):479–86.
Ibrahim, J.K., H.H.Schauffler, D.C.Barker, and C. T.Orleans. 2002. Coverage of tobacco dependence treatments for pregnant women and for children and their parents. Am J Public Health92 (12): 1940–2.
Iezzoni, L.I., E.P.McCarthy, R.B.Davis, and H. Siebens. 2001. Mobility difficulties are not only a problem of old age. J Gen Intern Med 16 (4):235–43.
Implications of the Diabetes Control and Complications Trial . 2002. Diabetes Care 25Suppl 1
Implications of the United Kingdom Prospective Diabetes Study. 2002. Diabetes Care25 Suppl 1:S28–32.
Institute of Medicine. 1999. Ensuring Quality Cancer Care.M.Hewitt and J.V.Simone, eds. Washington, D.C.: National Academy Press.
——. 2000a. Calling the Shots: Immunization Finance Policies and Practices.Washington, D. C.: National Academy Press.
——. 2000b. To Err Is Human: Building a Safer Health System.L.T.Kohn,J.M.Corrigan, and M.S.Donaldson, eds. Washington, D.C: National Academy Press.
——. 2001a. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, D.C.: National Academy Press.
——. 2001b. Improving Palliative Care for Cancer.Washington, D.C.: National Academy Press.
——. 2002. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care.B. S.Smedley, A.Y.Stith, and B.D.Nelson, eds. Washington, D.C.: National Academy Press.
Ireys, H.T.1981. The Selected Panel on the Promotion of Child Health, Better Health for Our Children: A National Strategy. Pp. 321–53. Health Care for Chronically Disabled Children and Their Families.Washington, D.C.: U.S. Government Printing Office.
Ireys, H.T., G.F.Anderson, T.J.Shaffer, and J.M. Neff. 1997. Expenditures for care of children with chronic illnesses enrolled in the Washington State Medicaid program, fiscal year 1993. Pediatrics100 (2 Pt 1): 197–204.
Jaen, C.R., B.F.Crabtree, S.J.Zyzanski, M.A. Goodwin, and K.C.Stange. 1998. Making time for tobacco cessation counseling. J Fam Pract46 (5):425–8.
Jeffery, R.W., A.Drewnowski, L.H.Epstein, A.J. Stunkard, G.T.Wilson, R.R.Wing, and D.R. Hill. 2000. Long-term maintenance of weight loss: Current status. Health Psychol19 (1 Suppl):5–16.
Jinnett, K., J.A.Alexander, and E.Ullman. 2001. Case management and quality of life: Assessing treatment and outcomes for clients with chronic and persistent mental illness . Health Serv Res 36 (1 Pt 1):61–90.
Johnson, J.A., and J.L.Bootman. 1995. Drug-related morbidity and mortality. A cost-of-illness model. Arch Intern Med155 (18):1949– 56.
Joint National Committee on Prevention, Detection Evaluation and Treatment of High Blood Pressure. 1997. 6th report. 2413–46.
Jones, S.C., B.C.Brost, and W.T.Brehm. 2000. Should intravenous tocolysis be considered beyond 34 weeks’ gestation?Am J Obstet Gynecol183 (2):356–60.
Kanthor, H., B.Pless, B.Satterwhite, and G.Myers. 1974. Areas of responsibility in the health care of multiply handicapped children. Pediatrics 54 (6):779–85.
Katon, W., M.Von Korff, E.Lin, E.Walker, G.E. Simon, T.Bush, P.Robinson, and J.Russo. 1995. Collaborative management to achieve treatment guidelines. Impact on depression in primary care. JAMA273 (13):1026–31.
Kaushal, R., K.N.Barker, and D.W.Bates. 2001. How can information technology improve patient safety and reduce medication errors in children’s health care?Arch Pediatr Adolesc Med155 (9): 1002–7.
Kessler, R.C., P.A.Berglund, M.L.Bruce, J.R. Koch, E.M.Laska, P.J.Leaf, R.W. Manderscheid, R.A.Rosenheck, E.E.Walters, and P.S.Wang. 2001. The prevalence and correlates of untreated serious mental illness. Health Serv Res36 (6 Pt 1):987–1007.
King, P., I.Peacock, and R.Donnelly. 1999. The UK prospective diabetes study (UKPDS): Clinical and therapeutic implications for type 2 diabetes. Br J Clin Pharmacol48 (5):643–8.
Kogan, M.D., G.R.Alexander, B.W.Jack, and M. C.Allen. 1998. The association between adequacy of prenatal care utilization and subsequent pediatric care utilization in the United States. Pediatrics102 (1 Pt 1):25–30.
Kolarik, R.C., R.M.Arnold, G.S.Fischer, and B. H.Hanusa. 2002. Advance care planning. J Gen Intern Med17 (8):618–24.
Koutsky, L.A., K.A.Ault, C.M.Wheeler, D.R. Brown, E.Barr, F.B.Alvarez, L.M. Chiacchierini, and K.U.Jansen. 2002. A controlled trial of a human papillomavirus type 16 vaccine. N Engl J Med347 (21): 1645–51.
Kozak, L.J., and J.D.Weeks. 2002. U.S. trends in obstetric procedures, 1990–2000. Birth29 (3):157–61.
Kraus, W.E., J.A.Houmard, B.D.Duscha, K.J. Knetzger, M.B.Wharton, J.S.McCartney, C. W.Bales, S.Henes, G.P.Samsa, J.D.Otvos, K. R.Kulkarni, and C.A.Slentz. 2002. Effects of the amount and intensity of exercise on plasma lipoproteins. N Engl J Med347 (19):1483–92.
Kronenberger, W.G., and R.J.Thompson Jr.1992. Medical stress, appraised stress, and the psychological adjustment of mothers of children with myelomeningocele. J Dev Behav Pediatr 13 (6):405–11.
Krumholz, H.M., M.J.Radford, Y.Wang, J.Chen, A.Heiat, and T.A.Marciniak. 1998. National use and effectiveness of beta-blockers for the treatment of elderly patients after acute myocardial infarction: National Cooperative Cardiovascular Project. JAMA280 (7):623–9.
Kunin, C.M.1993. Resistance to antimicrobial drugs—a worldwide calamity. Ann Intern Med 118 (7):557–61.
Kuno, E., and A.B.Rothbard. 2002. Racial disparities in antipsychotic prescription patterns for patients with schizophrenia. Am J Psychiatry159 (4):567–72.
Kwakkel, G., R.C.Wagenaar, T.W.Koelman, G.J. Lankhorst, and J.C.Koetsier. 1997. Effects of intensity of rehabilitation after stroke. A research synthesis. Stroke28 (8):1550–6.
Kwakkel, G., R.C.Wagenaar, J.W.Twisk, G.J. Lankhorst, and J.C.Koetsier. 1999. Intensity of leg and arm training after primary middle-cerebral-artery stroke: a randomised trial. Lancet354 (9174):191–6.
Lamb, H.R., and L.L.Bachrach. 2000. Some perspectives on deinstitutionalization. Psychiatr Serv(52): 1039–45.
Lavigne, J.V., and J.Faier-Routman. 1993. Correlates of psychological adjustment to pediatric physical disorders: A meta-analytic review and comparison with existing models. J Dev Behav Pediatr14 (2): 117–23.
Law, M., and J.L.Tang. 1995. An analysis of the effectiveness of interventions intended to help people stop smoking. Arch Intern Med155 (18):1933–41.
Leape, L.L., T.A.Brennan, N.Laird, A.G. Lawthers, A.R.Localio, B.A.Barnes, L. Hebert, J.P.Newhouse, P.C.Weiler, and H. Hiatt. 1991. The nature of adverse events in hospitalized patients. Results of the Harvard Medical Practice Study II . N Engl J Med324 (6):377–84.
Leatherman, S. and D.McCarthy. 2002. Quality of Health Care in the United States: A Chartbook. New York, NY: The Commonwealth Fund.
Legorreta, A.P., J.Christian-Herman, R.D. O’Connor, M.M.Hasan, R.Evans, and K.M. Leung. 1998. Compliance with national asthma management guidelines and specialty care: A health maintenance organization experience. Arch Intern Med158 (5):457–64.
Legorreta, A.P., X.Liu, C.A.Zaher, and D.E. Jatulis. 2000. Variation in managing asthma: Experience at the medical group level in California. Am J Manag Care6 (4):445–53.
Lehman, A.F., L.B.Dixon, E.Kernan, B.R. DeForge, and L.T.Postrado. 1997. A randomized trial of assertive community treatment for homeless persons with severe mental illness. Arch Gen Psychiatry54 (11):1038–43.
Lehman, A.F., R.Goldberg, L.B.Dixon, S. McNary, L.Postrado, A. Hackman, and K. McDonnell. 2002. Improving employment outcomes for persons with severe mental illnesses. Arch Gen Psychiatry59 (2): 165–72.
Levenson, J.W., E.P.McCarthy, J.Lynn, R.B. Davis, and R.S.Phillips. 2000. The last six months of life for patients with congestive heart failure. J Am Geriatr Soc48 (5 Suppl):S 101–9.
Leviton, L.C., R.L.Goldenberg, C.S.Baker, R.M. Schwartz, M.C.Freda, L.J.Fish, S.P.Cliver, D.J.Rouse, C.Chazotte, I.R.Merkatz, and J. M.Raczynski. 1999. Methods to encourage the use of antenatal corticosteroid therapy for fetal maturation: A randomized controlled trial. JAMA281 (1):46–52.
Levy, D., S.Kenchaiah, M.G.Larson, E.J. Benjamin, M.J.Kupka, K.K.Ho, J.M. Murabito, and R.S.Vasan. 2002. Long-term trends in the incidence of and survival with heart failure. N Engl J Med347 (18): 1397–402.
Levy, M.H.1996. Pharmacologic treatment of cancer pain. N Engl J Med335 (15):1124–32.3
Lifetime benefits and costs of intensive therapy as practiced in the diabetes control and complications trial. The Diabetes Control and Complications Trial Research Group. 1996. JAMA276 (17):1409–15.
Liptak, G.S., C.M.Burns, P.W.Davidson, and E. R.McAnarney. 1998. Effects of providing comprehensive ambulatory services to children with chronic conditions. Arch Pediatr Adolesc Med152 (10): 1003–8.
Lloyd-Jones, D.M., M.G.Larson, A.Beiser, and D. Levy. 1999. Lifetime risk of developing coronary heart disease. Lancet353 (9147):89– 92.
Lumley, J., S.Oliver, and E.Waters. 2000. Interventions for promoting smoking cessation during pregnancy. Cochrane Database Syst Rev (2):CD001055.
Lunney, J.R., J.Lynn, and C.Hogan. 2002. Profiles of older medicare decedents. J Am Geriatr Soc50 (6): 1108–12.
Lynn, J.2001. Perspectives on care at the close of life. Serving patients who may die soon and their families: The role of hospice and other services. JAMA285 (7):925–32.
Lynn, J., E.W.Ely, Z.Zhong, K.L.McNiff, N.V. Dawson, A.Connors, N.A.Desbiens, M. Claessens, and E.P.McCarthy. 2000. Living and dying with chronic obstructive pulmonary disease. J Am Geriatr Soc48 (5 Suppl):S91– 100.
Lynn, J., J.Lynch-Schuster, and A.Kabcenell. 2000. Improving Care for End of Life: A Sourcebook for Health Care Managers and Clinicians.New York: Oxford University Press.
Mahoney, E.M., C.T.Jurkovitz, H.Chu, E.R. Becker, S.Culler, A.S.Kosinski, D.H. Robertson, C.Alexander, S.Nag, J.R.Cook, L. A.Demopoulos, P.M.DiBattiste, C.P.Cannon, and W.S.Weintraub. 2002. Cost and cost-effectiveness of an early invasive vs conservative strategy for the treatment of unstable angina and non-ST-segment elevation myocardial infarction. JAMA288 (15):1851–8.
Manton, K.G.1989. Epidemiological, demographic, and social correlates of disability among the elderly. Milbank Q67 Suppl 2 Pt 1:13–58.
Marks, J.S., J.P.Koplan, C.J.Hogue, and M.E. Dalmat. 1990. A cost-benefit/cost-effectiveness analysis of smoking cessation for pregnant women. Am J Prev Med6 (5):282–9.
Marshall, M., and A.Lockwood. 2000. Assertive community treatment for people with severe mental disorders. Cochrane Database Syst Rev (2):CD001089.
Martin, J.A., B.E.Hamilton, S.J.Ventura, F. Menacker, and M.M.Park. 2001. Births: Final data for 2000. Natl Vital Stat Rep50 (5): 11–12.
Marx, A.J., M.A.Test, and L.I.Stein. 1973. Extrohospital management of severe mental illness. Feasibility and effects of social functioning. Arch Gen Psychiatry29 (4):505– 11.
Maternal mortality—United States, 1982–1996. 1998. MMWR Morb Mortal Wkly Rep47 (34):705–7.
Max, W.2001. The financial impact of smoking on health-related costs: A review of the literature. Am J Health Promot15 (5):321–31.
Mayo, P.H., J.Richman, and H.W.Harris. 1990. Results of a program to reduce admissions for adult asthma. Ann Intern Med112 (11):864–71.
McAfee, T., J.Wilson, S.Dacey, N.Sofian, S. Curry, and B.Wagener. 1995. Awakening the sleeping giant: mainstreaming efforts to decrease tobacco use in an HMO. HMO Pract 9 (3): 138–43.
McAlister, F.A., F.M.Lawson, K.K.Teo, and P. W.Armstrong. 2001. A systematic review of randomized trials of disease management programs in heart failure . Am J Med110 (5):378–84.
McBride, P., H.G.Schrott, M.B.Plane, G. Underbakke, and R.L.Brown. 1998. Primary care practice adherence to National Cholesterol Education Program guidelines for patients with coronary heart disease. Arch Intern Med158 (11):1238–44.
McCaig, L.F., R.E.Besser, and J.M.Hughes. 2002. Trends in antimicrobial prescribing rates for children and adolescents. JAMA287 (23):3096–102.
McCaig, L.F., and J.M.Hughes. 1995. Trends in antimicrobial drug prescribing among office-based physicians in the United States. JAMA 273 (3):214–9.
McGinnis, M.2002. Diabetes and physical activity: Translating evidence into action. Am J Prev Med22:1–2.
McGovern, P.G., D.R.Jacobs Jr, E.Shahar, D.K. Arnett, A.R.Folsom, H.Blackburn, and R.V. Luepker. 2001. Trends in acute coronary heart disease mortality, morbidity, and medical care from 1985 through 1997: The Minnesota Heart Survey . Circulation104 (1):19–24.
McMullin, S T., R.M.Reichley, L.A.Watson, S.A. Steib, M.E.Frisse, and T.C.Bailey. 1998. Experience with advanced technologies that reduce medication errors. Enhancing Patient Safety and Reducing Errors in Health Care.
McPherson, M., P.Arango, H.Fox, C.Lauver, M. McManus, P.W.Newacheck, J.M.Perrin, J.P. Shonkoff, and B.Strickland. 1998. A new definition of children with special health care needs. Pediatrics102 (1 Pt 1): 137–40.
McPhillips-Tangum, C.1998. Results from the first annual survey on addressing tobacco in managed care. Tob Control7 Suppl:S11–3.
McPhillips-Tangum C.2001. Year 2000 Addressing Tobacco in Managed Care Survey on Health Plans. Paper presented at the 4th Annual Addressing Tobacco in Managed Care Conference.Nashville, TN.
Melfi, C.A., T.W.Croghan, M.P.Hanna, and R.L. Robinson. 2000. Racial variation in antidepressant treatment in a Medicaid population. J Clin Psychiatry61 (1): 16–21.
Mercadante, S.1999. Pain treatment and outcomes for patients with advanced cancer who receive follow-up care at home. Cancer85 (8): 1849– 58.
Meredith, S., P.H.Feldman, D.Frey, K.Hall, K. Arnold, N.J.Brown, and W.A.Ray. 2001. Possible medication errors in home healthcare patients. J Am Geriatr Soc49 (6):719–24.
Minino, A.M. and B.L.Smith. 2001. National Vital Statistics Reports.Centers for Disease Control and Prevention.
Miranda, J., K.B.Wells, N.Duan, M.Jackson-Triche, I.Lagomasino, and C.D.Sherbourne. 2002. Can Quality Improvement Interventions Improve Care and Outcomes for Depressed Minorities? Results in a Randomized, Controlled Trial.Paper presented at the NIMH Mental Health Services Research Conference: July 18–20, 2002.
MMWR Weekly. 2000. Centers for Disease Control and Prevention—CDC49 (8): 149–53.
Mokdad, A.H., B.A.Bowman, E.S.Ford, F. Vinicor, J.S.Marks, and J.P.Koplan. 2001. The continuing epidemics of obesity and diabetes in the United States. JAMA286 (10): 1195–200.
Mokdad, A.H., E.S.Ford, B.A.Bowman, D.E. Nelson, M.M.Engelgau, F.Vinicor, and J.S. Marks. 2000. Diabetes trends in the U.S.: 1990–1998. Diabetes Care23 (9): 1278–83.
Moon, M.1996. The special health care needs of the elderly. Baxter Health Policy Rev2:317–49.
Must, A., J.Spadano, E.H.Coakley, A.E.Field, G. Colditz, and W.H.Dietz. 1999. The disease burden associated with overweight and obesity. JAMA282 (16):1523–9.
Nadel, M.R., D.K.Blackman, J.A.Shapiro, and L. C.Seeff. 2002. Are people being screened for colorectal cancer as recommended? Results from the National Health Interview Survey. Prev Med35 (3): 199–206.
NAEPP Expert Panel Report. 2002. Guidelines for the Diagnosis and Management of Asthma— Update on SelectedTopics.NHLBI, NIH.
Narrow, W.E., D.A.Regier, G.Norquist, D.S.Rae, C.Kennedy, and B.Arons. 2000. Mental health service use by Americans with severe mental illnesses. Soc Psychiatry Psychiatr Epidemiol35 (4): 147–55.
National Alliance for the Mentally Ill. “PACT: Program of Assertive Community Treatment.” Online. Available at http://www.nami.org/about/pactfact.html [accessed July, 2002].
National Asthma Education and Prevention Program. 1991. Guidelines for the Diagnosis and Management of Asthma.NIH/National Heart, Lung, and Blood Institute.
National Cancer Institute. 1996. “SEER Racial/ Ethnic Patterns of Cancer in the United States, 1988–1992.” Online. Available at http://seer.cancer.gov/publications/ethnicity/ [accessed Nov. 20, 2002].
National Committee for Quality Assurance. 1997. HEDIS 3.0. What’s In It and Why It Matters. Washington, D.C.: NCQA.
——. 2002. State of Health Care Quality Report. Washington, D.C.: NCQA.
National Conference of State Legislatures. “Influenza Vaccine Rates Among People Age 65 and Older.”Imunization Project.Washington, D.C.
National Heart Lung and Blood Institute (NHLBI). 1998. “The NHLBI Clinical Guidelines.” Online. Available at www.nhlbi.nih/.gov/guileines/obesity/e.textbk/index/htm [accessed Aug. 26, 2002].
National Institutes of Health. 2002. State-of-the-Science Conference Statement. State-of-the- Science Conference on Symptom Management in Cancer: Pain, Depression, and Fatigue. National Institutes of Health
Newacheck, P.W., M.A.McManus, and H.B.Fox. 1991. Prevalence and impact of chronic illness among adolescents. Am J Dis Child145 (12):1367–73.
Newacheck, P.W., B.Strickland, J.P.Shonkoff, J. M.Perrin, M.McPherson, M.McManus, C. Lauver, H.Fox, and P.Arango. 1998. An epidemiologic profile of children with special health care needs. Pediatrics102 (1 Pt 1):117– 23.
Newacheck, P.W., and W.R.Taylor. 1992. Childhood chronic illness: Prevalence, severity, and impact. Am J Public Health82 (3):364–71.
NHLBI USPHS. 1997. Expert Panel Report 2. Guidelines for the Diagnosis and Management of Asthma.Bethesda, MD: National Institutes of Health.
Ni, H., D.J.Nauman, and R.E.Hershberger. 1998. Managed care and outcomes of hospitalization among elderly patients with congestive heart failure. Arch Intern Med158 (11):1231–6.
NIH Consensus Statement. 1996. Cervical cancer. 14(1):1–38.
Nolan, T., I.Zvagulis, and B.Pless. 1987. Controlled trial of social work in childhood chronic illness. Lancet2 (8556):411–5.
Norman, D.C.2002. Management of antibioticresistant bacteria. J Am Geriatr Soc50 (7 Suppl):S242–6.
Norris, S.L., M.M.Engelgau, and K.M.Narayan. 2001. Effectiveness of self-management training in type 2 diabetes: A systematic review of randomized controlled trials. Diabetes Care 24 (3):561–87.
Nyquist, A.C., R.Gonzales, J.F.Steiner, and M.A. Sande. 1998. Antibiotic prescribing for children with colds, upper respiratory tract infections, and bronchitis. JAMA279 (11):875– 7.
O’Connor, G.T., H.B.Quinton, N.D.Traven, L.D. Ramunno, T.A.Dodds, T.A.Marciniak, and J. E.Wennberg. 1999 . Geographic variation in the treatment of acute myocardial infarction: The Cooperative Cardiovascular Project. JAMA 281 (7):627–33.
Olivarius, N.F., H.Beck-Nielsen, A.H.Andreasen, M.Horder, and P.A.Pedersen. 2001. Randomised controlled trial of structured personal care of type 2 diabetes mellitus. BMJ 323 (7319):970–5.
Oliveria, S.A., P.Lapuerta, B.D.McCarthy, G.J. L’Italien, D.R.Berlowitz, and S.M.Asch. 2002. Physician-related barriers to the effective management of uncontrolled hypertension. Arch Intern Med162 (4):413–20.
Ornish, D., L.W.Scherwitz, J.H.Billings, S.E. Brown, K.L.Gould, T.A.Merritt, S.Sparler, W.T.Armstrong, T.A.Ports, R.L.Kirkeeide, C.Hogeboom, and R.J.Brand. 1998. Intensive lifestyle changes for reversal of coronary heart disease. JAMA280 (23):2001–7.
Ossip-Klein, D.J., T.A.Pearson, S.McIntosh, and C.T.Orleans. 1999. Smoking is a geriatric health issue. Nicotine Tob Res1 (4):299–300.
Partnership for Prevention. 1999. Why Invest in Disease Prevention? It’s a Good Business Decision. And It’s Good for American Business.
——. 2002. Prevention Priorities: A Health Plan’s Guide to the Highest Value Preventive Health Services.
Partnership for Solutions, The Johns Hopkins University. 2001. “Partnership for Solutions: A National Program of The Robert Wood Johnson Foundation.” Online. Available at http://www.partnershipforsolutions.org/statistics/prevalence.htm [accessed Dec. 12, 2002].
Perez-Stable, E.J., and E.Fuentes-Afflick. 1998. Role of clinicians in cigarette smoking prevention. West J Med169 (1):23–9.
Perz, J.F., A.S.Craig, C.S.Coffey, D.M. Jorgensen, E.Mitchel, S.Hall, W.Schaffher, and M.R.Griffin. 2002. Changes in antibiotic prescribing for children after a community-wide campaign . JAMA287 (23):3103–9.
Petersen, L.A., S.M.Wright, E.D.Peterson, and J. Daley. 2002. Impact of race on cardiac care and outcomes in veterans with acute myocardial infarction. Med Care40 (1.Supp):86–96.
Pfizer. 1998. “Promoting Health Literacy: A Call to Action.” Online. Available at http://www.pfizerhealthliteracy.com [accessed July 11, 2002].
Phillips, D.M.2000. JCAHO pain management standards are unveiled. Joint Commission on Accreditation of Healthcare Organizations. JAMA284 (4):428–9.
Phillips, D.P., N.Christenfeld, and L.M.Glynn. 1998. Increase in US medication-error deaths between 1983 and 1993. Lancet351 (9103):643–4.
Phillips, J., S.Beam, A.Drinker, C.Holquist, P. Honig, L.Y.Lee, and C.Pamer. 2001. Retrospective analysis of mortalities associated with medication errors. Am J Health Syst Pharm58 (19):1835–41.
Pignone, M., C.Phillips, and C.Mulrow. 2000. Use of lipid lowering drugs for primary prevention of coronary heart disease: Meta-analysis of randomised trials. BMJ321 (7267):983–6.
Pignone, M., S.Saha, T.Hoerger, and J. Mandelblatt. 2002. Cost-effectiveness analyses of colorectal cancer screening: A systematic review for the U.S. Preventive Services Task Force. Ann Intern Med137 (2):96–104.
Pilote, L., R.M.Califf, S.Sapp, D.P.Miller, D.B. Mark, W.D.Weaver, J.M.Gore, P.W. Armstrong, E.M.Ohman, and E.J.Topol. 1995. Regional variation across the United States in the management of acute myocardial infarction. GUSTO-1 Investigators. Global Utilization of Streptokinase and Tissue Plasminogen Activator for Occluded Coronary Arteries. N Engl J Med333 (9):565–72.
Pincus, H.A., T.L.Tanielian, S.C.Marcus, M. Olfson, D.A.Zarin, J.Thompson, and J.Magno Zito. 1998. Prescribing trends in psychotropic medications: Primary care, psychiatry, and other medical specialties. JAMA279 (7):526–31.
Pless, I.B. and M.E.Wadsworth. 1988. The unresolved question: Long-term psychological sequelae of chronic illness in childhood. In: R. E.K.Stein ed. Caring for Children with Chronic Illness: Issues and Strategies.New York, NY: Springer Publishing Company.
Post-stroke Rehabilitation Panel, GE Gresham Chair. 1995. Post-stroke Rehabilitation.Rockville, MD: Agency for Health Care Policy and Research.
Prevention Program Reduces Incidences of Pressure Ulcers by Up to 87%. 2002. Dermatol Nurs14 (4):286.
Psaty, B.M., N.L.Smith, D.S.Siscovick, T.D. Koepsell, N.S.Weiss, S.R.Heckbert, R.N. Lemaitre, E.H.Wagner, and C.D.Furberg. 1997. Health outcomes associated with antihypertensive therapies used as first-line agents. A systematic review and meta-analysis. JAMA277 (9):739–45.
Rathore, S.S., J.D.McGreevey 3rd, K.A. Schulman, and D.Atkins. 2000. Mandated coverage for cancer-screening services: Whose guidelines do states follow?Am J Prev Meet19 (2):71–8.
Renders, C.M., G.D.Valk, S.J.Griffin, E.H. Wagner, J.T.Eijk Van, and W.J.Assendelft. 2001. Interventions to improve the management of diabetes in primary care, outpatient, and community settings: A systematic review. Diabetes Care24 (10): 1821–33.
Rennels, M.B., and H.C.Meissner. 2002. Technical report: Reduction of the influenza burden in children. Pediatrics110(6):e80.
Reogowski J.1998. Cost-effectiveness of care for very low birth weight infants. Pediatrics (102):35–43.
Rich, M.W.1997. Epidemiology, pathophysiology, and etiology of congestive heart failure in older adults. J Am Geriatr Soc45 (8):968–74.
——. 1999. Heart failure disease management: a critical review. J Card Fail5 (1):64–75.
Richards, C., T.G.Emori, J.Edwards, S.Fridkin, J. Tolson, and R.Gaynes. 2001. Characteristics of hospital and infection control professionals participating in the National Nosocomial Infections Surveillance System 1999. Am J Infect Control29 (6):400–403.
Ries, L.A., M.P.Eisner, and C.L.Kosary. 2002. SEER Cancer Statistics Review, 1973–1999. Bethesda, MD: National Cancer Institute, 2002.
Rimer, B.K., C.T.Orleans, M.K.Keintz, S. Cristinzio, and L.Fleisher. 1990. The older smoker. Status, challenges and opportunities for intervention. Chest97 (3):547–53.
Rodewald, L.E., P.G.Szilagyi, S.G.Humiston, R. Barth, R.Kraus, and R.F.Raubertas. 1999. A randomized study of tracking with outreach and provider prompting to improve immunization coverage and primary care. Pediatrics103
Rogowski, J.1998. Cost-effectiveness of care for very low birth weight infants. Pediatrics102 (1 Pt 1):35–43.
Rosenberg, C.H., and G.M.Popelka. 2000. Post-stroke rehabilitation. A review of the guidelines for patient management. Geriatrics55 (9): 75– 81; quiz 82.
Rosenheck, R.A., and D.Dennis. 2001. Time-limited assertive community treatment for homeless persons with severe mental illness. Arch Gen Psychiatry58 (11):1073–80.
Roth, E.J., A.W.Heinemann, L.L.Lovell, R.L. Harvey, J.R.McGuire, and S.Diaz. 1998. Impairment and disability: Their relation during stroke rehabilitation. Arch Phys Med Rehabil 79 (3):329–35.
Roth, K., J.Lynn, Z.Zhong, M.Borum, and N.V. Dawson. 2000. Dying with end stage liver disease with cirrhosis: Insights from SUPPORT. Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatment. J Am Geriatr Soc48 (5 Suppl): S122–30.
Saaddine, J.B., M.M.Engelgau, G.L.Beckles, E. W.Gregg, T.J.Thompson, and K.M.Narayan. 2002. A diabetes report card for the United States: Quality of care in the 1990s. Ann Intern Med136 (8):565–74.
Sacchetti, A., M.Gerardi, R.Barkin, J.Santamaria, R.Cantor, J.Weinberg, and M.Gausche. 1996. Emergency data set for children with special needs. Ann Emerg Med28 (3):324–7.
Sadur, C.N., N.Moline, M.Costa, D.Michalik, D. Mendlowitz, S.Roller, R.Watson, B.E.Swain, J.V.Selby, and W.C.Javorski. 1999. Diabetes management in a health maintenance organization. Efficacy of care management using cluster visits. Diabetes Care22
Samsa, G.P., D.B.Matchar, L.B.Goldstein, A.J. Bonito, L.J.Lux, D.M.Witter, and J.Bian. 2000. Quality of anticoagulation management among patients with atrial fibrillation: Results of a review of medical records from 2 communities. Arch Intern Med160 (7):967–73.
Saslow, D., C.D.Runowicz, D.Solomon, A.-B. Moscicki, R.A.Smith, H.J.Eyre, and C. Cohen . 2002. American Cancer Society Guideline for the Early Detection of Cervical Neoplasia and Cancer. CA Cancer J Clin52 (6):342–62.
Sawaya, G.F., and D.A.Grimes. 1999. New technologies in cervical cytology screening: A word of caution. Obstet Gynecol94 (2):307–10.
Schappert, S.M.1997. Ambulatory care visits of physician offices, hospital outpatient departments, and emergency departments: United States, 1995. Vital Health Stat13 (129):1–38.
Schillinger, D., K.Grumbach, J.Piette, F.Wang, D. Osmond, C.Daher, J.Palacios, G.D.Sullivan, and A.B.Bindman. 2002. Association of health literacy with diabetes outcomes. JAMA 288 (4):475–82.
Schlesinger, M., R.Dorwart, C.Hoover, and S. Epstein. 1997. The determinants of dumping: A national study of economically motivated transfers involving mental health care. Health Serv Res32 (5):561–90.
Schneider, E.C., A.M.Zaslavsky, and A.M. Epstein. 2002. Racial disparities in the quality of care for enrollees in medicare managed care. JAMA287 (10):1288–94.
Schoenbaum, M., J.Unutzer, C.Sherbourne, N. Duan, L.V.Rubenstein, J.Miranda, L.S. Meredith, M.F.Carney, and K.Wells. 2001. Cost-effectiveness of practice-initiated quality improvement for depression: Results of a randomized controlled trial. JAMA286 (11):1325–30.
Schulberg, H.C., W.Katon, G.E.Simon, and A.J. Rush. 1998. Treating major depression in primary care practice: An update of the Agency for Health Care Policy and Research Practice Guidelines. Arch Gen Psychiatry55 (12):1121– 7.
Schulman, K.A., J.A.Berlin, W.Harless, J.F. Kerner, S.Sistrunk, B.J.Gersh, R.Dube, C.K. Taleghani, J.E.Burke, S.Williams, J.M. Eisenberg, and J.J.Escarce. 1999. The effect of race and sex on physicians’ recommendations for cardiac catheterization. N Engl J Med340 (8):618–26.
Schwartz, C.E., H.B.Wheeler, B.Hammes, N. Basque, J.Edmunds, G.Reed, Y.Ma, L.Li, P. Tabloski, and J.Yanko. 2002. Early intervention in planning end-of-life care with ambulatory geriatric patients: Results of a pilot trial. Arch Intern Med162 (14):1611–8.
Scott, J.G., D.Cohen, B.DiCicco-Bloom, A.J. Orzano, C.R.Jaen, and B.F.Crabtree. 2001. Antibiotic use in acute respiratory infections and the ways patients pressure physicians for a prescription. J Fam Pract50 (10):853–8.
Seeff, L.C., J.A.Shapiro, and M.R.Nadel. 2002. Are we doing enough to screen for colorectal cancer? Findings from the 1999 Behavioral Risk Factor Surveillance System. J Fam Pract51 (9):761–6.
Senate report number 102–397.
Serdula, M.K., A.H.Mokdad, D.F.Williamson, D. A.Galuska , J.M.Mendlein, and G.W.Heath. 1999. Prevalence of attempting weight loss and strategies for controlling weight. JAMA282 (14):1353–8.
Sheikh, K., and C.Bullock. 2001. Urban-rural differences in the quality of care for medicare patients with acute myocardial infarction. Arch Intern Med161 (5):737–43.
Shipp, M., M.S.Croughan-Minihane, D.B.Petitti, and A.E.Washington. 1992. Estimation of the break-even point for smoking cessation programs in pregnancy. Am J Public Health82 (3):383–90.
Shortell, S.M., R.R.Gillies, and D.A.Anderson. 2000. Remaking Health Care in America.2nd edition. San Francisco, CA: Jossey-Bass.
Silber, J.H., S.P.Gleeson, and H.Zhao. 1999. The influence of chronic disease on resource utilization in common acute pediatric conditions. Financial concerns for children’s hospitals. Arch Pediatr Adolesc Med153 (2): 169–79.
Simon, G.E., D.Goldberg, B.G.Tiemens, and T.B. Ustun. 1999. Outcomes of recognized and unrecognized depression in an international primary care study. Gen Hosp Psychiatry21 (2):97–105.
Simon, G.E., M.VonKorff, C.Rutter, and E. Wagner. 2000. Randomised trial of monitoring, feedback, and management of care by telephone to improve treatment of depression in primary care. BMJ320 (7234):550–4.
Sloan, P.A., B.L.Vanderveer, J.S.Snapp, M. Johnson, and D.A.Sloan. 1999. Cancer pain assessment and management recommendations by hospice nurses. University of Kentucky, Lexington, KY. J Pain Symptom Manage18 (2):103–10.
Solberg, L.I., T.E.Kottke, S.A.Conn, M.L. Brekke, C.A.Calomeni, and K.S.Conboy. 1997. Delivering clinical preventive services is a systems problem. Ann Behav Med19 (3):271–8.
Sperl-Hillen, J., P.J.O’Connor, R.R.Carlson, T.B. Lawson, C.Halstenson, T.Crowson, and J. Wuorenma. 2000. Improving diabetes care in a large health care system: an enhanced primary care approach. Jt Comm J Qual Improv26
Spore, D.L., V.Mor, P.Larrat, C.Hawes, and J. Hiris. 1997. Inappropriate drug prescriptions for elderly residents of board and care facilities. Am J Public Health87 (3):404–9.
Squires, S. Dec. 13, 2001. Surgeon General Outlines National Plan on Obesity. The Washington Post.
St Lawrence, J.S., D.E.Montano, D.Kasprzyk, W. R.Phillips, K.Armstrong, and J.S.Leichliter. 2002. STD screening, testing, case reporting, and clinical and partner notification practices: A national survey of US physicians. Am J Public Health92 (11):1784–8.
Standards for the diagnosis and care of patients with chronic obstructive pulmonary disease. American Thoracic Society. 1995. Am J Respir Crit Care Med152 (5 Pt 2):S77–121.
STAR*D Program. “Sequenced treatment alternatives to relieve depression.” Online. Available at http://www.edc.gsph.pitt.edu/stard [accessed July, 2002].
Stein, R.1983. A home care program for children with chronic illness. Child Health Care12 (2):90–2.
Stone, E.G., S.C.Morton, M.E.Hulscher, M.A. Maglione, E.A.Roth, J.M.Grimshaw, B.S. Mittman, L.V.Rubenstein, L.Z.Rubenstein, and P.G.Shekelle. 2002. Interventions that increase use of adult immunization and cancer screening services: A meta-analysis. Ann Intern Med136 (9):641–51.
Strauss, R.S., and H.A.Pollack. 2001. Epidemic increase in childhood overweight, 1986–1998. JAMA286 (22):2845–8.
Stuck, A.E., M.H.Beers, A.Steiner, H.U.Aronow, L.Z.Rubenstein, and J.C.Beck. 1994. Inappropriate medication use in community-residing older persons. Arch Intern Med154 (19):2195–200.
Sturm, R.1999. Tracking changes in behavioral health services: How have carve-outs changed care?J Behav Health Serv Res26 (4):360–71.
Sturm, R.2002. The effects of obesity, smoking, and drinking on medical problems and costs. Obesity outranks both smoking and drinking in its deleterious effects on health and health costs. Health Aff (Millwood)21 (2):245–53.
Tamminga, C.A.1997. Gender and schizophrenia. J Clin Psychiatry58Suppl 15:33–7.
Taylor, D.H. Jr, V.Hasselblad, S.J.Henley, M.J. Thun, and F.A.Sloan. 2002. Benefits of smoking cessation for longevity. Am J Public Health92 (6):990–6.
Testa, M.A., and D.C.Simonson. 1998. Health economic benefits and quality of life during improved glycemic control in patients with type 2 diabetes mellitus: A randomized, controlled, double-blind trial. JAMA280 (17): 1490–6.
The Commonwealth Fund. 2002. Quality of Health Care in the United States: A Chartbook.
The National Coalition on Health Care and the Institute for Healthcare Improvement. 2002. Curing the System: Stories of Change in Chronic Illness Care.The National Coalition on Health Care and the Institute for Healthcare Improvement.
The Robert Wood Johnson Foundation. 2001. Substance Abuse: The Nation’s Number One Health Problem.Princeton, NJ: Robert Wood Johnson Foundation .
——. 2002. National Partnership to Help Pregnant Smokers Quit: Action Plan.Princeton, NJ: Robert Wood Johnson Foundation.
The sixth report of the Joint National Committee on prevention, detection, evaluation, and treatment of high blood pressure. 1997. Arch Intern Med 157 (21):2413–46.
Thompson, R.S.1996. What have HMOs learned about clinical prevention services? An examination of the experience at Group Health Cooperative of Puget Sound. Milbank Q74 (4):469–509.
Thorndike, A.N., N.A.Rigotti, R.S.Stafford, and D.E.Singer. 1998. National patterns in the treatment of smokers by physicians. JAMA 279 (8):604–8.
Thornley, B., C.E.Adams, and G.Awad. 2000. Chlorpromazine versus placebo for schizophrenia. Cochrane Database Syst Rev (2):CD000284.
Tinetti, M.E., and C.S.Williams. 1998. The effect of falls and fall injuries on functioning in community- dwelling older persons. J Gerontol A Biol Sci Med Sci53 (2):M112–9.
Tomar, S.L., C.G.Husten, and M.W.Manley. 1996. Do dentists and physicians advise tobacco users to quit?J Am Dent Assoc127 (2):259–65.
Trepka, M.J., E.A.Belongia, P.H.Chyou, J.P. Davis, and B.Schwartz. 2001. The effect of a community intervention trial on parental knowledge and awareness of antibiotic resistance and appropriate antibiotic use in children. Pediatrics107 (1):E6.
United States Department of Health and Human Services. 1990. The Health Benefits of Smoking Cessation: A Report of the Surgeon General. Vol. Rockland, MD: U.S. Govenment Printing Office.
——. 1998. “National Vital Statistics Reports.” Washington, D.C.: Department of Health and Human Services.
——. 2000. Healthy People 2010: Understanding and Improving Health.2nd edition. Washington, D.C.: U.S. Government Printing Office.
——. 2001a. The Surgeon General’s Call to Action to Prevent and Decrease Overweight and Obesity.Vol. Rockville, MD: U.S. Department of Health and Human Services, Public Health Services, Office of the Surgeon General.
——. 2001b. Women and Smoking : A Report of the Surgeon General.Vol. Rockland, MD: U.S. Govenment Printing Office.
——. 2002. “National Vital Statistics Reports.” Washington, D.C.: CDC—Centers for Disease Control and Prevention.
United States General Accounting Office. 2000. Medicaid Managed Care: Challenges in Implementing Safeguards for Children with Special Needs.Washington, D.C.: U.S. Goverment Printing Office.
United States Preventive Services Task Force. 1996. Guide to Clinical Preventive Services. Baltimore, MD: Williams and Wilkins.
United States Preventive Services Task Force. 2002a. Behavioral counseling in primary care to promote a physical activity: Recommendation and rationale. Ann Intern Med137:205–8.
United States Preventive Services Task Force. 2002b. “Recommendations and Rationale: Screening for Colorectal Cancer.” Online. Available at http://www.ahrq.gov/clinic/3rduspstf/colorectal/colorr.htm [accessed Nov. 20, 2002b].
United States Preventive Services Task Force. 2003. Behavioral counseling primary care to promote a healthy diet. Recommendation and rationale. Am J Prev Med24(1):93–100
United States Public Health Service. 1999. Office of the Surgeon General Mental Health: A Report of the Surgeon General, pp 244–68.
van der Lee, J.H., R.C.Wagenaar, G.J.Lankhorst, T.W.Vogelaar, W.L.Deville, and L.M. Bouter. 1999. Forced use of the upper extremity in chronic stroke patients: Results from a single-blind randomized clinical trial . Stroke30 (11):2369–75.
Vasan, R.S., A.Beiser, S.Seshadri, M.G.Larson, W.B.Kannel, R.B.D’Agostino, and D.Levy. 2002. Residual lifetime risk for developing hypertension in middle-aged women and men: The Framingham Heart Study. JAMA287 (8):1003–10.
Verschuren, W.M., D.R.Jacobs, B.P.Bloemberg, D.Kromhout, A.Menotti, C.Aravanis, H. Blackburn, R.Buzina, A.S.Dontas, and F. Fidanza. 1995. Serum total cholesterol and long-term coronary heart disease mortality in different cultures. Twenty-five-year follow-up of the seven countries study. JAMA274 (2): 131–6.
Vintzileos, A.M., C.V.Ananth, J.C.Smulian, W. E.Scorza, and R.A.Knuppel. 2002. The impact of prenatal care on neonatal deaths in the presence and absence of antenatal high-risk conditions. Am J Obstet Gynecol186 (5):1011– 6.
Vishnu-Priya, S., H.Izurieta, C.Bridges, E.Bolyard, D.Johnson, and M.Hoyt. 2000. Prevention and Control of Vaccine-Preventable Diseases in Long-Term Care Facilities. Journal of American Medical Directors Association :S2-S37.
Viskin, S., and H.V.Barron. 1996. Beta blockers prevent cardiac death following a myocardial infarction: So why are so many infarct survivors discharged without beta blockers?Am J Cardiol 78 (7):821–2.
Von Korff, M., J.Gruman, J.Schaefer, S.J.Curry, and E.H.Wagner. 1997. Collaborative management of chronic illness. Ann Intern Med 127 (12):1097–102.
Von Korff, M., G.Nestadt, A.Romanoski, J. Anthony, W.Eaton, A.Merchant, R.Chahal, M. Kramer, M.Folstein, and E.Gruenberg. 1985. Prevalence of treated and untreated DSM-III schizophrenia. Results of a two-stage community survey. J Nerv Ment Dis173 (10):577–81.
Wadden, T.A., and G.D.Foster. 2000. Behavioral treatment of obesity. Med Clin North Am84 (2):441–61, vii.
Wagner, E.H., S.J.Curry, L.Grothaus, K.W. Saunders, and C.M.McBride. 1995. The impact of smoking and quitting on health care use. Arch Intern Med155 (16):1789–95.
Wagner, E.H., B.T.Austin, and M.Von Korff. 1996. Organizing care for patients with chronic illness. Milbank Q74 (4):511–44.
Wagner, E.H., R.E.Glasgow, C.Davis, A.E. Bonomi, L.Provost, D.McCulloch, P.Carver, and C.Sixta. 2001a. Quality improvement in chronic illness care: A collaborative approach. Jt Comm J Qual Improv27 (2):63–80.
Wagner, E.H., N.Sandhu, K.M.Newton, D.K. McCulloch, S.D.Ramsey, and L.C.Grothaus. 2001b. Effect of improved glycemic control on health care costs and utilization. JAMA285 (2): 182–9.
Wagner, E.H., B.T.Austin, C.Davis, M. Hindmarsh, J.Schaefer, and A.Bonomi. 2001c. Improving chronic illness care: Translating evidence into action. Health Aff (Millwood)20 (6):64–78.
Wahlbeck, K., M.Cheine, and M.A.Essali. 2000. Clozapine versus typical neuroleptic medication for schizophrenia. Cochrane Database Syst Rev (2):CD000059.
Wallander, J.L., J.W.Varni, L.Babani, H.T.Banis, and K.T.Wilcox. 1988. Children with chronic physical disorders: Maternal reports of their psychological adjustment. J Pediatr Psychol13 (2): 197–212.
Wallander, J.L., J.W.Varni, L.Babani, C.B. DeHaan, K.T.Wilcox, and H.T.Banis. 1989. The social environment and the adaptation of mothers of physically handicapped children. J Pediatr Psychol14 (3):371–87.
Walston, J., and L.P.Fried. 1999. Frailty and the older man. Med Clin North Am83 (5): 1173–94.
Wang, P.S., P.Berglund, and R.C.Kessler. 2000. Recent care of common mental disorders in the United States: Prevalence and conformance with evidence-based recommendations. J Gen Intern Med15 (5):284–92.
Wang, P.S., O.Demler, and R.C.Kessler. 2002. Adequacy of treatment for serious mental illness in the United States. Am J Public Health92 (1):92–8.
Weaver, W.D., R.J.Simes, A.Betriu, C.L.Grines, F.Zijlstra, E.Garcia, L.Grinfeld, R.J.Gibbons, E.E.Ribeiro, M.A.DeWood, and F.Ribichini. 1997. Comparison of primary coronary angioplasty and intravenous thrombolytic therapy for acute myocardial infarction: A quantitative review. JAMA278 (23):2093–8.
Weiland, S.K., I.B.Pless, and K.J.Roghmann. 1992. Chronic illness and mental health problems in pediatric practice: Results from a survey of primary care providers. Pediatrics89 (3):445–9.
Weinstein, R.A.1998. Nosocomial infection update. Emerg Infect Dis4 (3):416–20.
Weiss, K.B., and S.D.Sullivan. 2001. The health economics of asthma and rhinitis. I. Assessing the economic impact. J Allergy Clin Immunol 107 (1):3–8.
Weiss, K.B., S.D.Sullivan, and C.S.Lyttle. 2000. Trends in the cost of illness for asthma in the United States, 1985–1994. J Allergy Clin Immunol106 (3):493–9.
Wells, K.B.2002a. Mental Disorders and Candidate Quality Improvement Conditions. Presented at May 9–10, 2002 Priority Areas for Quality Improvement Meeting.
Wells, K.B.2002b. The story and findings of Partners in Care. From Jackson-Triche M, Wells KB, Minnium K. Beating Depression: The Journey to Hope. New York: McGraw Hill.
Wells, K.B., C.Sherbourne, M.Schoenbaum, N. Duan, L.Meredith, J.Unutzer, J.Miranda, M.F. Carney, and L.V.Rubenstein. 2000. Impact of disseminating quality improvement programs for depression in managed primary care: A randomized controlled trial . JAMA283 (2):212–20.
Wells, K.B., A.Stewart, R.D.Hays, M.A.Burnam, W.Rogers, M.Daniels, S.Berry, S.Greenfield, and J.Ware. 1989. The functioning and well-being of depressed patients. Results from the Medical Outcomes Study. JAMA262 (7):914– 9.
Wenzel, R.P., and M.B.Edmond. 2001. The impact of hospital-acquired bloodstream infections. Emerg Infect Dis7 (2): 174–7.
Whelton, P.K., J. He, L.J.Appel, J.A.Cutler, S. Havas, T.A.Kotchen, E.J.Roccella, R.Stout, C.Vallbona, M.C.Winston, and J.Karimbakas. 2002. Primary prevention of hypertension: Clinical and public health advisory from the national high blood pressure education program. JAMA288 (15):1882–8.
Whitney, C.G., M.M.Farley, J.Hadler, L.H. Harrison, C.Lexau, A.Reingold, L.Lefkowitz, P.R.Cieslak, M.Cetron, E.R.Zell, J.H. Jorgensen, and A.Schuchat. 2000. Increasing prevalence of multidrug-resistant streptococcus pneumoniae in the United States. N Engl J Med 343 (26):1917–24.
Willcox, S.M., D.U.Himmelstein, and S. Woolhandler. 1994. Inappropriate drug prescribing for the community-dwelling elderly. JAMA272 (4):292–6.
Wisborg, K., T.B.Henriksen, C.Obel, E.Skajaa, and J.R.Ostergaard. 1999. Smoking during pregnancy and hospitalization of the child. Pediatrics104 (4):e46.
World Health Organization. 1996. With a guide to opioid availability. Cancer Pain Relief.2nd edition. Geneva: World Health Organization.
——. 2000. “Global Burden of Disease 2000 Version 1 Estimates.” Online. Available at http://www3.who.int/whosis/menu [accessed May 29, 2002].
Yanovski, S.Z., and J.A.Yanovski. 2002. Obesity. N Engl J Med346 (8):591–602.
Young, A.S., R.Klap, C.D.Sherbourne, and K.B. Wells. 2001. The quality of care for depressive and anxiety disorders in the United States. Arch Gen Psychiatry58 (1):55–61.
Yusuf, S., R.Peto, J.Lewis, R.Collins, and P. Sleight. 1985. Beta blockade during and after myocardial infarction: An overview of the randomized trials. Prog Cardiovasc Dis27 (5):335–71.
Zech, D.F., S.Grond, J.Lynch, D.Hertel, and K.A. Lehmann. 1995. Validation of World Health Organization Guidelines for cancer pain relief: A 10-year prospective study. Pain63 (1):65– 76.
Zeiger, R.S., S.Heller, M.H.Mellon, J.Wald, R. Falkoff, and M.Schatz. 1991. Facilitated referral to asthma specialist reduces relapses in asthma emergency room visits. J Allergy Clin Immunol87 (6): 1160–8.
Zhan, C., J.Sangl, A.S.Bierman, M.R.Miller, B. Friedman, S.W.Wickizer, and G.S.Meyer. 2001. Potentially inappropriate medication use in the community-dwelling elderly: Findings from the 1996 Medical Expenditure Panel Survey. JAMA286 (22):2823–9.










































































