2
Context for Community Effects: Uninsurance and the Financing and Delivery of Health Services
There is no guarantee that uninsured persons will be able to obtain the health care that they need and no guarantee that if they do get care, it will be adequate or affordable. Responsibility for financing and providing health care to uninsured persons in the United States is fragmented and ill-defined, to the extent that this responsibility exists at all. Many of the Committee’s hypothesized effects of uninsurance on communities stem from the structure of health care finance and the patterns of service provision for insured and uninsured Americans that have emerged over the past half-century. The current structure of safety net and non-safety net arrangements, along with the mix of public and private funding sources, was not envisioned or designed as an integrated system; rather, it has resulted from the aggregation, over time, of multiple initiatives and developments in both the private and the public sectors. Because the organization and delivery of care are closely linked to health insurance, the health care needs of persons who lack health insurance have been of secondary interest, often only as afterthoughts in the development of public policy.
In this chapter, the Committee describes the ad hoc nature of health care financing and services for the more than 41 million uninsured Americans. This information is drawn from both descriptive and analytic, empirical research sources. It frames the discussions in subsequent chapters of pathways through which community uninsurance is hypothesized to affect health care institutions, local economies, and population health. The chapter also documents the magnitude and distribution among providers of uncompensated care to the uninsured and considers who, if anyone, is responsible for providing that care.
The chapter is divided into four sections. The first section gives a historical account of the development of the current programs and arrangements for financ-
ing and providing health care to those without the means to pay (the “medically indigent”), including people without health insurance. The second and third sections describe the current mix of public and private financing and delivery arrangements involved in caring for uninsured persons, including the roles of government, health care institutions and professionals, and philanthropies and the issue of shifting costs to, or getting subsidies from, private payers (insurers and employers). The fourth section is a summary of what is known and what remains to be learned about how the present arrangements for financing and providing health care generally, and uninsured care in particular, have made uninsurance a critical and destabilizing factor in local health care markets and community economies today. Readers who are familiar with this historical background and policy context may want to turn immediately to the fourth section, which identifies research questions and data needs and then to Chapters 3 through 6, which provide the Committee’s findings and conclusions regarding community effects.
HISTORICAL AND ORGANIZATIONAL CONTEXT OF HEALTH CARE FOR UNINSURED AMERICANS
Over the past 25 years, federal and state policies to control health care costs and an increasingly competitive private market for health care services and coverage have constrained public payer and commercial reimbursement rates for care. As a result, there has been an erosion of the previous level of public support and private cross-subsidy for the uncompensated care costs associated with providing health services to uninsured persons. The effects of this erosion have been felt more strongly in communities with large or growing uninsured populations and by providers (e.g., public hospitals) that serve a high number or proportion of uninsured persons.
As health insurance has become more central both as a means to access care and to the support of health care providers and institutions, the presence of sizable uninsured populations in communities has become a common explanation for, or the most obvious proximal cause of, health system failings and inefficiencies. Understanding why and how this has happened requires some appreciation of the development of the present public and private structures for financing health services. This historical context also aids an objective appraisal of evidence as to what health system and community-wide effects can validly be attributed to local uninsured rates rather than to other aspects of the overall structure of health care finance.
The public–private amalgam of health insurance mechanisms and the mixed delivery system of private not-for-profit, private for-profit, and public health care institutions and services are a legacy of America’s particular history and notions of the public good. Over the past century in the United States, the concurrent development of private and public approaches to financing health care (and the
tension between them) have given shape to American health care services and institutions (Starr, 1982; Stevens, 1989).
The well-documented story of financing for hospitals illuminates the growing importance over time of health insurance as a revenue source for health care providers, the backdrop to the emergence of uninsurance as a health policy issue. Since the 1940s, hospitals have become increasingly reliant on revenues from patients to support their budgets and the financial margins on which their survival and development depend (Stevens, 1989). As health care costs have risen and coverage has become increasingly important for access to care by individuals and families, the presence of a sizable uninsured population has meant not only less access for uninsured persons but also the loss of potential revenues for health care providers. This section briefly traces the history of uninsurance in the context of changes in health care financing and delivery. The discussion is divided into three parts, following a typology proposed by Lynn Etheredge that includes an era in which health insurance became common (his era of fee-for-service reimbursement), an era of public regulation of pricing, and an era of managed care and market incentives (Etheredge, 2000).
The Rise of Health Insurance
Before the advent of Medicare and Medicaid in the mid-1960s, persons without the means to pay for their care relied for the most part on the charity of individual physicians, hospitals, and clinics in their communities. In the nineteenth century and into the early twentieth century, hospital dispensaries and public hospitals were important locations where medically indigent patients could obtain medical care, while patients with the means to hire physicians were treated in their homes. These practices reinforced a two-tier approach to medical care that was firmly established by the mid-1800s (Rosenberg, 1987).
During the first three decades of the twentieth century, profound changes in biomedical science and health professions education transformed hospitals into sites of care for middle-class persons, losing the stigma of the almshouse. The development of the new hospital and new standards of practice for providers brought higher prices for health care (Stevens, 1989). The financial consequences of paying for health care in hospitals became an issue for the middle class. In response, a variety of private health insurance plans were devised, some adapted from voluntary “sick funds” organized by immigrant benefit societies, fraternal orders, and unions. Others, such as Blue Cross, were newly created arrangements for individuals to pool their risk of incurring major hospital expenses through modest monthly payments that would relieve the individuals of further financial obligations should hospitalization be needed (Starr, 1982). Economic disparities in health services utilization among various income groups, documented by the Committee on the Costs of Medical Care in a series of studies between 1928 and 1931, were lessened by the 1950s, reflecting the expansion of health insurance more broadly among the population (Starr, 1982; Andersen and Anderson, 1999).
Enrollment in private health insurance plans expanded rapidly during the 1940s and 1950s, aided by workplace benefits and favorable federal tax treatment (Starr, 1982; Numbers, 1985; Gabel, 1999). By 1940, half of the states had enacted the legal framework for hospital service-benefit plans. These frameworks authorized state insurance commissioners to review the rates of such plans and also exempted the plans from taxes as charitable organizations. In that year, Blue Cross plans had a total enrollment of more than 6 million people and commercial insurers another 3.7 million subscribers (Starr, 1982). By the early 1950s, enrollment in commercial insurance plans and Blue Cross was comparable. In 1953, 29 percent of Americans were covered by commercial carriers, 27 percent by Blue Cross, and another 7 percent by independent plans, amounting to 63 percent of the U.S. population (Starr, 1982). Enrollment grew rapidly during the 1950s, then more slowly in the early 1960s.
As hospitals, physicians, and other providers of care during this era grew to rely on revenues generated from insurance payments, persons without insurance found themselves encountering arrangements for care that depended on public support or charitable donations to cover their unreimbursed expenses or on the ability of providers to cross-subsidize this care with revenues from insured patients. Then, as now, public and private nonprofit hospitals alike were widely considered to be obliged (ethically if not always legally) to provide community benefits, including uncompensated care to patients without the ability to pay, in exchange for their tax-supported or tax-exempt status (Clement et al., 1994; Buchmueller and Feldstein, 1996; Trocchio, 1996; Needleman, 2001). Another source of charitable care came from nonprofit community hospitals’ participation in the federal Hill-Burton hospital construction program, which from the late 1940s through the early 1970s (through a successor program) provided grants, loans, and loan guarantees for building and renovation, particularly in rural areas. Support through this program entailed a legal obligation to serve all community residents without regard to ability to pay and to provide a percentage of the value of their original Hill-Burton grant as uncompensated care (Stevens, 1989).1 A third source was federal vendor payments to the states to partially reimburse the care delivered to medically indigent persons, a predecessor to the Medicaid program (Stevens, 1989). Continued inflation in the costs of health care, however, brought new difficulties for uninsured persons in getting access to care and strained the capacity of these initiatives to accommodate growing volumes and costs of uncompensated care.
The passage of the Medicare and Medicaid programs as amendments to the
Social Security Act in the mid-1960s brought the promise of universal coverage and more stable financial footing for health care providers by filling significant gaps in coverage in the general population (Lewis, 1983; Stevens, 1989). Medicare and Medicaid expanded insurance-based financing for those over 65, the disabled, and single-parent families receiving income assistance. These programs preserved the ability of hospitals to charge and be reimbursed more than the direct costs involved in caring for the insured patient.2 However, because Medicare and Medicaid reimbursed for what were called contractual allowances (negotiated rates) rather than whatever fees a hospital might choose to charge for its services, implementation of these public insurance programs brought with it new concerns on the part of private payers that they would end up cross-subsidizing the unreimbursed expenses of publicly insured patients (Stevens, 1989).
The two programs filled some but not all existing gaps in coverage, with Medicare limited to persons at least 65 years of age and with categorical and income limits for Medicaid. Medicare was a nationally uniform program administered initially by Blue Cross and modeled after commercial health insurance plans. A federal entitlement program tied to the Social Security retirement and disability insurance program, Medicare specifically addressed the failure of the private market to supply health insurance to the elderly and the impoverishment of older Americans and their families that followed hospitalizations among this population (Marmor, 2000). Medicaid was enacted in conjunction with Medicare as a joint federal–state program entitling the very poorest Americans, through their eligibility for public assistance, to a broad scope of health care services. There was and continues to be much variation from state to state in the size and characteristics of Medicaid programs. Because Medicare and Medicaid left tens of millions of Americans uninsured, hospitals, physicians, and other providers who treated uninsured patients continued to incur costs that went unreimbursed.
In addition to expanding public coverage, efforts were made to meet the needs of uninsured and other medically underserved persons through a combination of dedicated health facilities, health professions education subsidies, and a clearer articulation and enforcement of hospital’s charitable obligations under Hill-Burton. Starting in the mid-1960s, the Office of Economic Opportunity awarded project grants to local community organizations to establish neighborhood health centers as innovative models of comprehensive health care delivery organized around primary care that also recognized the positive contributions of health care to local economic vitality and population health (Sardell, 1988). These neighborhood health centers eventually became community health centers. The National Health Services Corps, begun in the early 1970s, placed new physicians in medically underserved communities (Redman, 1973), and litigation in the early
1970s led to the requirement that hospitals explicitly document fulfillment of their Hill-Burton service obligations to medically indigent patients, a significant source of free care through the 1980s, when most Hill-Burton obligations ended (Blumstein, 1986; Stevens, 1989).
Federal reimbursement and purchasing policies related to Medicare and Medicaid set the stage for the current state of health care finance and the impact of uninsured patients and uncompensated care on health care institutions (Stevens, 1989). Implementation of Medicare and Medicaid was followed by a rapid rise in health care costs, attributable to greater use of hospital services. Public and private hospitals alike scrambled to secure reimbursement from third-party payers sufficient to keep revenue ahead of expenditures. As one observer of the time period notes. (Stevens, 1989, pp. 318-319):
Hospitals of all kinds made remarkable adjustments to changes in their environments in the years following Medicare and Medicaid. Some hospitals became aggressively profit-oriented, closing their emergency rooms and seeking maximum reimbursement rates. Others, seeking to maintain a traditional social role, became increasingly hard pressed… Taxing agencies, like their private counterparts, looked for ways to reduce demand for care by patients who were unable to pay. The dictates of the market seemed all-pervasive.
The influence of commercial payment, now joined by the interests of public payers, boosted the transformation of hospitals into vendors of services, with much potentially to be lost financially by caring for uninsured persons.
The role of public hospitals themselves was brought into question, as the availability of public financing through the Medicare and Medicaid program was posited to eliminate the need for tax-supported institutions (e.g., urban hospitals supported by local property taxes) to care for medically indigent persons who previously would not be seen by private hospitals or at least argue for the reallocation of public dollars for expanding coverage rather than expanding safety-net facilities (Blendon et al., 1986). Some have argued that, in fact, Medicaid actually fostered fragmentation of the health care system, for example, by not remedying existing racial segregation and segregation of the poor within health care facilities (Stevens, 1989).3 In the 1970s, public hospitals, particularly in urban areas, found themselves with many uninsured patients and inadequate reimbursement for many services, leading to great financial stress. By the early 1970s there were also efforts to constrain the huge increase in hospital expenditures by limiting expansion of Medicaid and by price controls (Etheredge, 2000). The failure of national health insurance proposals meant that Medicaid, with its limited income eligibility standards and frequently inadequate payment rates, marked the limits of greater access for the poor (Stevens, 1989).
Cost Controls Shape the Health Care Marketplace, 1983–1992
The federal government’s reform of Medicare payments for hospital inpatient services from cost-based reimbursement to prospective payment in the early 1980s fundamentally transformed the economic incentives facing hospitals. Prospective payment was intended to standardize the payments made to hospitals all over the country so that reimbursement for an inpatient stay for a patient with a particular diagnosis (categorized under a diagnosis-related group, or DRG) would be tied to the average costs of treating that diagnosis and would be similar for every hospital. It was a response to the rapid increase in health care expenditures and resulting inflation in costs and health insurance premiums that had followed the introduction of Medicare and Medicaid 20 years earlier; Medicare and Medicaid spending increased by an average of 17 percent each year between 1965 and 1982 (Etheredge, 2000).
For hospitals, prospective payment exposed the economic differences between insured patients and uninsured patients even more starkly and heightened the importance of maximizing the hospital’s revenues, and its market position, through a variety of adaptive strategies (e.g., altering how its case mix is classified to receive higher reimbursements, earlier discharge of patients, shifting from inpatient admissions to outpatient visits) (Stevens, 1989). Third-party insurers followed Medicare’s lead in setting payment levels for services.
Prospective payment under Medicare had different economic impacts in different parts of the country and for different types of hospitals. Some hospitals found prospective payment to be profitable while others, for example public hospitals in large urban areas, lost revenue. With pressures on hospitals and providers to keep their costs low, the cross-subsidy or support of uncompensated care for uninsured patients became more difficult, especially for hospitals that disproportionately served the uninsured (Stevens, 1989). Public and private hospitals, and both nonprofit and for-profit hospitals, competed for patients whose health insurance coverage would yield the highest reimbursement for services and contribute the most to the facility’s revenues. Access to care for vulnerable groups, including the uninsured, was diminished (Stevens, 1989).
The federal government has responded to this situation through a series of subsidies and regulations grounded in its financing programs, including the following:
-
supplemental payments through the Medicare and Medicaid programs to hospitals serving a “disproportionate share” of low-income (and presumably higher-cost) program beneficiaries and for graduate medical education (these payments are discussed more fully later in this chapter) and
-
prohibition of “patient dumping,” the refusal to treat or the inappropriate transfer of patients unable to pay for their care, through the Emergency Medical Treatment and Labor Act (EMTALA), the federal law enacted as part of the
-
Consolidated Omnibus Budget Reconciliation Act of 1986 (COBRA). Structured as a hospital condition of participation in the Medicare program, EMTALA requires all hospitals with emergency departments to screen and stabilize all patients who present themselves for treatment, regardless of financial means or insurance status. Because EMTALA has not included provisions for reimbursing hospitals for the care they provide to uninsured patients, one consequence of the statute has been to make hospital emergency departments the providers of last resort and to place the departments at serious financial risk (Bitterman, 2002).
Since 1993: Hospital Margins Down, Number of Uninsured Persons Up
Prospective payment has proved unable to constrain costs in the long term (Etheredge, 2000; Aaron, 2002; Altman and Levitt, 2002). First private and then public purchasers have used managed care and selective contracting as ways to reduce their outlays for health services for their enrollees (Rundall et al., 1988; Etheredge, 2002). For example, state Medicaid programs have turned to managed care both to control costs and to provide enrollees in Medicaid with greater access to mainstream health care providers and potentially better integration of the delivery system. As Figure 2.1 shows, acute care, nonfederal hospitals saw their private payer surplus decline significantly over the course of the 1990s, from a high of nearly 12 percent in 1992 to about 5 percent in 2000. Over the same period, Medicare revenues first rose and then began to decline as a percent of Medicare costs. This contrasts with the trend for uncompensated care, which showed little change, while total margins for hospitals at first grew and then declined. There has been an erosion of the capacity of hospitals to cross-subsidize uncompensated care.
Figure 2.1 indicates a leveling off of the decline in hospital total margins, starting in 1999, reflecting a new period of growing inflation in the late 1990s in health care costs and health insurance premiums. In 2001, health care spending per capita increased by 10 percent (Strunk et al., 2002). More than half of this growth in total spending is attributable to spending on hospital inpatient and especially outpatient services. About one-third of the increasing spending on hospital services reflected higher payment rates and two-thirds reflected greater utilization of services (Strunk et al., 2002). Strunk and colleagues interpret the higher prices charged by hospitals as the outcome of hospital gains in market power (e.g., negotiating strength with health plans) and the loosening of managed care restrictions. They predict a slowing of growth in health care spending, as privately insured persons respond to increased cost-sharing (higher costs passed through their insurance plan) by dampening their use of services and as health care markets adjust to changes in managed care (Strunk et al., 2002).
Although this generation of cost-control efforts met with some success through the mid-to late 1990s, the number of uninsured persons has continued to increase, while remaining a relatively constant proportion of the general population. Health insurance coverage rates had first begun to increase substantially in
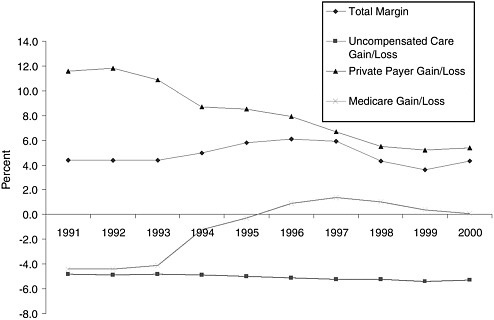
FIGURE 2.1 Hospitals’ total margins, with percent gains or losses by source of payment (private payer, uncompensated care, Medicare), 1991–2000.
NOTE: Gains or losses are the difference between the cost of providing care and the payment received.
SOURCE: Adapted from Hadley and Holahan, 2003, based on MedPAC, 2002a, pp. 156, 157.
the 1940s and 1950s, with the expansion of private and public insurance programs. By 1976, the number of uninsured Americans fell to between 24 million and 25 million (approximately 12 to 13 percent of the population under age 65) before increasing once again (HIAA, 2002).
Health insurance has played key roles in facilitating access to care and in securing a revenue stream for health care providers, roles that are rooted in the historical development of a third-party financing approach to paying for personal health services in the United States. The Committee considers the effects of uninsurance upon communities as growing out of the changes over time in the relationship among health insurance coverage, access to care, and the financing of health care services.
SAFETY NET SERVICES, PROVIDERS OF LAST RESORT, AND MAINSTREAM HEALTH CARE
Finding: Although the health care institutions and practitioners that serve the larger community of insured persons provide most of the
services that uninsured persons receive, the uninsured rely disproportionately on so-called safety-net providers and arrangements for care.
Finding: Rural and urban areas differ in the organization and delivery of care for uninsured persons. In urban areas, multiple tiers of providers and services tend to segregate patients by income level and coverage status, isolating insured patients from the experiences of uninsured patients. In rural areas, insured and uninsured patients may have more in common because a more limited set of providers typically serves all community members and safety-net arrangements tend to be less formal. At minimum, mainstream health care and safety-net arrangements are connected by their shared reliance on public and private financing streams.
Finding: Anticipated growth in the number and capacity of publicly supported ambulatory care clinics (under the Consolidated Health Centers program) is expected to be inadequate to meet the needs of the existing, as well as the projected future, number of uninsured persons.
A widely held misperception is that there are special programs and public facilities nationwide that give uninsured Americans adequate access to health care (Blendon et al., 1999; IOM, 2001a). This is a comforting but invidious myth. The provision and financing of health care for the uninsured are ill-defined, fragmented, and insufficient (Lewin and Altman, 2000; Hadley, 2002; IOM, 2002a). Perhaps more importantly, the metaphor of a safety net does not highlight the fact that all parts of this “net” are anchored, for better or worse, in the mainstream health care system (see Box 2.1). However, the term safety net has become established in public discourse about health services and other social welfare programs that serve vulnerable populations, including the uninsured. The Committee uses the phrase safety net only as an adjective, to refer to health care facilities and programs that disproportionately serve uninsured persons.4
Local safety-net arrangements commonly include services provided through health departments; federally sponsored clinics (e.g., community, migrant); other independent community, faith-based, or free clinics; hospital outpatient departments; public hospitals; and hospital emergency departments. In certain parts of the country, private hospitals may participate in safety net arrangements (Lewin and Altman, 2000). Like the broader health care market, the breadth and depth of
|
BOX 2.1 Certain health care institutions, including public hospitals and academic health centers, community health centers, other clinics, and health departments, because of their explicit missions and prominent roles in serving medically underserved or indigent groups have been labeled “core” safety net institutions. The Institute of Medicine (IOM) Committee on the Changing Market, Managed Care, and the Future Viability of Safety Net Providers, authors of America’s Health Care Safety Net, recognized both the unique role and mission of safety-net providers within communities and the highly variable configurations of safety-net services that exist across the country (Lewin and Altman, 2000, p. 47): The concept of a health care safety net conjures up the image of a tightly woven fabric of federal, state, and local programs stretched across the nation ready to catch those who slip through the health insurance system…. America’s safety net is neither secure nor uniform. Rather, it varies greatly from state to state, community to community…. These variations notwithstanding, most communities can identify a set of hospitals and clinics that by mandate or mission care for a proportionately greater share of poor and uninsured people. This earlier IOM Committee concludes that safety net arrangements are “intact but endangered,” threatened fiscally by a decline in support from public revenues, due particularly to the changes associated with state Medicaid managed care programs, and an increase in demand for services as reflected in an increasing number of uninsured persons nationally. SOURCE: Lewin and Altman, 2000. |
safety-net services are shaped by the local employment and tax base, the generosity of state Medicaid support, the community’s own history and performance in providing services to vulnerable groups, and the demand for services (Baxter and Mechanic, 1997; Lewin and Altman, 2000). Neither the existence of core safety-net providers nor the volume of care delivered outside formal safety net arrangements guarantees that there will be sufficient or adequate care for uninsured persons. There is considerable unmet need for health care in general in many communities around the United States (IOM, 1988, forthcoming 2003; Bovbjerg et al., 2000b).
Despite having distinctive characteristics and being identifiable within communities, safety-net providers and service arrangements may be interrelated with and sometimes part of mainstream health care providers and institutions. This blending of safety-net and mainstream health care services is particularly likely in rural areas and for specialty care in general.
There is significant heterogeneity across localities in the financing, function, and scope of safety-net arrangements, depending on factors such as the size of the
community and its uninsured population, population density, and state health services and financing programs (Baxter and Mechanic, 1997; Norton and Lipson, 1998; Lewin and Altman, 2000). Service configurations in rural areas differ from those in metropolitan areas, and urban center city safety-net arrangements differ from those that have emerged in suburban areas (Mueller et al., 1999; Ormond et al., 2000b; Taylor et al, 2001). The problems that rural communities face in terms of the absolute supply of services and further distances traveled to reach health care is magnified for uninsured rural residents, who may not have the economic means to travel out of their community in order to obtain greater access to care (Schur and Franco, 1999). Rural areas tend not to have dedicated safety net facilities. Physicians in private practice may provide the bulk of primary care to uninsured patients, and private hospitals may perform safety net functions that in a more urban community would be carried out by a public hospital (Taylor et al, 2001). In urban areas, in contrast, a tiered arrangement for health services tends to segregate patients by income level and coverage status, at separate institutions and through differential treatment within a single facility, such as a private nonprofit hospital. The sustainability of this tiered structure depends on patterns of insurance coverage within the community and additional support to reimburse providers for uncompensated care.5 Indeed, the threshold requirements of subsidies such as disproportionate share hospital payments by Medicare and Medicaid may promote the concentration of lower-income patients in some hospitals. If the need for care by uninsured patients substantially exceeds the capacity of local safety net arrangements, other health care providers in the community may be drawn on, even if they do not customarily participate in safety net care.
Although providers and institutions commonly considered to be parts of local safety-net arrangements are more likely than others to treat uninsured persons and members of partially uninsured families, most uninsured persons and their families obtain care not from formal safety-net arrangements but from mainstream health services providers and institutions (Cunningham and Tu, 1997; Lewin and Altman, 2000). In terms of the distribution of reported uncompensated care in 1994 as a rough proxy for services delivered to uninsured and other medically underserved groups, for example, private hospitals provided $10.6 billion in uncompensated care costs, while public hospitals provided $6.2 billion (Cunningham and Tu, 1997). For this reason, efforts to expand the capacity of safety net facility arrangements are unlikely to be successful as the sole strategy for providing adequate access and health care to uninsured Americans.
Uninsured patients comprise a relatively large proportion (40 percent) of the client base of federally supported primary care clinics (Cunningham and Tu, 1997; Bureau of Primary Health Care [BPHC], 2002). However, uninsured clients served by these clinics represent a relatively small proportion (between 6.5 and 10 percent) of the total uninsured population, and most uninsured persons do not live in the vicinity of a community health center (Cunningham and Tu, 1997; Cunningham and Kemper, 1998; Carlson et al., 2001; BPHC, 2002). Funding for community health centers and other primary care clinics has been limited and piecemeal, and health centers and clinics do not have the physical capacity to meet the projected unmet primary care needs of all of the uninsured persons in their area (Lewin and Altman, 2000).
Although the expansion of the federally supported health centers is anticipated to improve their ability to meet a growing patient demand, given the limited capacity and geographical limits of community health centers (CHCs), providers such as hospital outpatient clinics and emergency departments are unlikely to be replaced by CHCs as providers of the greatest volume of primary care for uninsured persons. Through the Health Care Safety Net Amendments of 2002, the Bush Administration began a major effort to enlarge the CHC system, with a goal of doubling the capacity in CHCs from the current level of 11 million people served annually (4 to 5 million of whom are uninsured) to 22 million over a five-year period (NACHC, 2002). This expansion was accompanied by the defunding of Community Access Program grants to improve the coordination of safety-net services within communities.
Given a national uninsured population of 41 million persons as of 2001 and that 40 percent of CHC clients are uninsured, the projected capacity for CHCs is about one quarter of what would be needed, even if the number of uninsured Americans did not increase. This calculation assumes that all uninsured persons would receive primary and preventive care from CHCs and that CHCs would continue to serve both insured and uninsured clients as they do now. Over the next five to ten years, estimates of the projected number of uninsured persons range from a decrease to roughly 34 million in 2005, given a strong economic outlook, to an increase of up to 61 million uninsured by 2009 in the case of an economic recession (IOM, 2001a).
Major Providers of Safety-Net Care
In their participation in safety-net arrangements, physicians and health care institutions have taken some direct responsibility for providing care to the uninsured, on ethical as well as legal grounds. CHCs and public hospitals have mandates and some financial support earmarked for serving uninsured persons. Private hospitals are bound by the terms of their charters (e.g., provision of community benefits in exchange for tax-exempt status), by federal Hill-Burton grant and loan obligations, and by the requirements of the Emergency Medical Treatment and
Labor Act (EMTALA), to provide limited services regardless of patients’ ability to pay.
Physicians working in private practice, nonprofit clinics (such as federally qualified health centers and free clinics), and hospitals all provide significant amounts of subsidized or free care to uninsured persons. Information about the financial cost of services rendered to uninsured patients is often incomplete. Of the information available, more is known about hospitals’ provision of uncompensated care than about ambulatory care provided in doctors’ offices and clinics.
The amount and sources of uncompensated care generated within a particular community reflect economic and other factors beyond the uninsured rate within the community. Not all uncompensated or even charity care is generated by the uninsured, and not all care to the uninsured is uncompensated or subsidized. Some is traceable to insured patients who do not pay their copayments or deductibles. Three studies based on data from the 1980s estimate the share of hospital uncompensated care costs attributable to uninsured patients. These studies of Florida, Indiana, and Massachusetts hospitals report that 72, 72, and 59 percent, respectively, of uncompensated care costs were for services to uninsured patients (Duncan and Kilpatrick, 1987; Saywell et al., 1989b; Weissman et al., 1992).
Changes in the mix of services offered by hospitals and the overall trend toward outpatient instead of inpatient treatment have affected the level of uncompensated care as well as its distribution among different types of providers. Nationally, during the first half of the 1990s, there was an increasing concentration of uncompensated care among safety-net (public and academic health center) hospitals and a shift of uncompensated care burden from hospitals to private physicians and community health centers (Cunningham and Tu, 1997; Commonwealth Fund, 2001). In many rural communities, the hospital remains the source of ambulatory as well as institutional acute care. Overall, hospitals reported little change in their relative burden, although hospital care overall represented a smaller share of the health care dollar.6 Growing pressures on hospital financial margins due to competition within the private health insurance market and changing practice patterns contribute to this shift away from the hospital sector, as well as changes in the technology of medical care (Etheredge, 2000).
Physicians
By waiving or reducing fees to uninsured patients and others unable to pay the direct costs of their care and by donating their services in free clinics and
similar settings, physicians provide a significant amount of free or reduced-price charity care. One estimate of the value of charity care provided to uninsured patients by private practice physicians is $5.1 billion in 2001 dollars (Hadley and Holahan, 2003). This estimate reflects an adjusted midpoint from a range of survey results on physician-provided free and reduced-price care.
Both the American Medical Association (AMA) and the American Academy of Pediatrics (AAP) have surveyed their members about the provision of uncompensated care.
-
A recent AMA survey (1999) reports the responses of a nationally representative survey of nonfederal physicians involved in patient care (part of the AMA’s Socioeconomic Monitoring System), defining charity care as services provided at free or reduced price in light of a patient’s financial need. 7 Sixty-five percent of the surveyed physicians reported delivering charity care, averaging 8.8 hours per week or 14.4 percent of total patient hours among those who provide such care (Kane, 2002). Primary care physicians are less likely to provide charity care (62 percent) and provide fewer hours of care, on average (8.1 hours per week), than other physicians (67 percent, a weekly average of 9.3 hours); the latter category includes internal medicine subspecialties, surgeons, radiologists, psychiatrists, anesthesiologists, pathologists, and emergency medicine specialists. Emergency medicine physicians are reported to have experienced the greatest increase in the proportion providing charity care, from 48 percent in 1988 to 61 percent in 1999 (Kane, 2002). Of physicians in nonmetropolitan areas, 72 percent report providing charity care, compared with 64 percent of physicians in urban areas.
-
The most recent AAP survey of primary care pediatricians involved in direct provision of care finds that approximately 8 percent of these physicians’ patients are uninsured, on average, and that roughly 42 percent of services to uninsured patients are uncompensated (Yudkowski et al., 2000).
Another set of estimates comes from a nationally representative survey, the Community Tracking Study (CTS). CTS data show a decrease in the proportion of physicians providing charity care between 1997 and 2001, from 76.3 percent to 71.5 percent (Cunningham, 2002). Results from an earlier round of the CTS survey (1998-1999) indicate those physicians providing charity care report delivering an average of 2.5 hours weekly (Reed et al., 2001). Although the AMA and CTS survey results are quite disparate, both show a decrease in the number of physicians providing charity care in the mid-to-late 1990s (Cunningham et al., 1999).
Clinics
By mission, community health centers, other federally qualified health centers (FQHCs), and rural health clinics are devoted to improving access for medically underserved persons, including those who are uninsured. The FQHCs are considered “core” safety net institutions (Lewin and Altman, 2000). For the most part, FQHCs provide primary care and preventive and screening services, together with a small proportion of specialty services and referrals for specialty care.8 They fill a special niche, not only because of their location in underserved neighborhoods and communities but also because they offer enabling or wraparound services, such as transportation, translation, and case management, that facilitate access to health care (Davis et al., 1999). In addition, they frequently employ community residents. The unmet health needs that justify placement of a community health center vary regionally and may include a rural or frontier community’s isolation, resulting in lack of local physicians, an area’s high uninsured rate, or other impediments to access to care for low-income persons and recent immigrants (Clemmitt, 2000).
As of 2001, there were approximately 750 private nonprofit grantees operating clinics at more than 4,000 sites that served some 10 million people, 39 percent of whom were uninsured (BPHC, 2002). These health center grantees received approximately $1.2 billion in federal grants to support their operations. Federal grants supply just 25 percent of the centers’ operating funds, overall. Medicaid payments account for about 34 percent; state and local support, 14 percent; Medicare and other third-party payments, 15 percent; patient payments, 6 percent; and other sources, 6 percent (BPHC, 2002). There has been growth in the number of uninsured persons receiving free or reduced-price care from community health centers, from 2.2 million in the early 1990s to 4.0 million people in 2001.
Clinics have a limited capacity to care for their client base, and this capacity has been threatened in recent years. Many health centers and clinics that rely on federal section 330 grants for operating revenue are experiencing financial trouble (USGAO, 2000; McAlearney, 2002). Approximately 50 percent have fiscal or operating problems, with smaller clinics (those serving 5,000 or fewer patients annually) more likely to be experiencing trouble. In 1998, 50 percent of clinics had costs greater than or equal to revenues, and for 5 percent of clinics, costs exceeded revenues by 30 percent (USGAO, 2000). Since the 1970s, CHCs have become increasingly reliant on Medicaid reimbursement due to increasing enrollments in Medicaid. They have experienced little real increase in federal grants
over the past 20 years. After a period of growth through the mid-1990s, CHCs have experienced severe fiscal pressures from the combination of declining Medicaid revenues, in part connected with the spread of state Medicaid managed care contracting, and a rising uninsured population (Hawkins and Rosenbaum, 1998).
Rural health clinics do not receive federal operating grants and are under no legal obligation to care for underserved groups, yet they often function in this capacity (Gale and Coburn, 2001; Finerfrock, 2002; NARHC, n.d.). Because these rural clinics receive cost-based reimbursement from the Medicare and Medicaid programs, they are able to provide the facilities and administrative structure for bringing physicians, nurse practitioners, and other clinicians into rural areas, where a limited economic base may make it hard to recruit and retain health professionals in the community. During 2000, 55 percent of independent rural health clinics (RHCs) and almost 70 percent of provider-based (e.g., owned by physician or physician assistant) RHCs had free or reduced-price care policies. Four out of five RHCs accepted applications for such care, and most RHCs reported writing off uncompensated care (Coburn, 2002).
Hospitals
Estimates of hospital uncompensated care may be presented in several ways (Duncan, 1992):
-
the number of patients served
-
the dollar amount of care or the volume or amount of services provided
-
the total amount of care given that the patient does not pay for or the net dollar amount after a partial subsidy from other payers.
The estimates that result from these different metrics lead to varying interpretations of hospitals’ relative efforts and burdens. Although uncompensated care is often measured in terms of the individual physician or hospital, another perspective is provided when the volume of such care is cast in terms of overall community resources. The burden of providing free care is likely to be distributed unevenly and depends both on what individual providers choose to offer and from which institutions patients seek care (Duncan, 1992). The relative performance of nonprofit and for-profit hospitals in providing charity care varies by state and locality and reflects market circumstances and demographics as well as ownership type and explicit mission. The ownership profiles of hospitals in urban and rural areas also differ. Box 2.2 gives a national overview of hospitals by type of ownership and the relationship between ownership type, hospital mission, and obligations to serve the community as a whole. Box 2.3 defines some of the accounting terms used in discussion of uncompensated care and hospital finance.
Data from AHA annual surveys are the basis for recent national estimates of hospital uncompensated care. Over the past decade, uncompensated care expenditures at hospitals nationally have been relatively stable at about 6 percent of costs
|
BOX 2.2 Public hospitals may be sponsored directly by city, county, state, or federal governments or by local hospital districts independent of other government agencies or jurisdictions. In 1998, there were 651 city or county hospitals, 551 so-called district hospitals, 322 state hospitals, and 275 federal hospitals (Needleman, 2000). Federal hospitals usually are reserved for specific populations, for example, active and retired members of the military and their families through the Veterans Administration or American Indians through the Indian Health Service. State-owned facilities include psychiatric hospitals and university academic health centers. Private hospitals are greater in number and less likely to receive direct government subsidies to reimburse the uncompensated care costs incurred by uninsured persons. In 1998, there were 3,200 nonprofit and 1,182 for-profit hospitals nationally (Needleman, 2000). For-profit hospitals are assumed to set their prices with the goal of maximizing profits (Hoerger, 1991; Needleman, 1999; Zwanziger et al., 2000). They are less likely to serve as safety-net institutions or to provide care for uninsured persons (Hoerger, 1991; Mann et al, 1997). Because they are for profit, the prices charged to uninsured persons may be set differently than those charged by non-profit hospitals. Nonprofit hospitals vary widely in their provision of charity care, which depends upon the health insurance coverage rates in their service area, their mission, and whether there are public hospitals in their communities. Both public and private nonprofit hospitals are expected to provide community benefits, by virtue of their status as nonprofit and tax-exempt (Needleman, 2000; Nicholson et al., 2000). The term “community benefits” generally is understood to include
|
(Hadley and Holahan, 2003). In 1999, this translated into roughly $20.8 billion of care that was reported provided to patients who could not or did not pay their bills (MedPAC, 2001).9 The proportion of uncompensated care remained relatively
|
BOX 2.3
|
steady throughout the 1990s, although the national estimate masks important regional and local variations and trends (Cunningham and Tu, 1997). Specifically, the overall uncompensated care burden has become more concentrated in fewer hospitals, especially public hospitals. This has been attributed to new market pressures on hospitals and, consequently, a lessened ability to shift uncompensated care costs to insured patients, both public and private (Cunningham and Tu, 1997). These authors project that if Medicaid managed care patients go to private hospitals and uninsured patients are concentrated in public facilities, public hospitals will face increased fiscal pressure due to the combined impact of reduced revenue and uncompensated care. Gaskin and colleagues (2001) have documented this phenomenon in the case of low-risk Medicaid maternity patients, who are financially attractive, shifting from urban public hospitals to private hospitals.
In rural areas, hospitals often anchor the web of relationships and institutions that comprise safety-net arrangements. Because there are fewer alternative providers of services in rural than urban areas, hospitals on average have greater burdens of uncompensated care and are more sensitive to fluctuations or changes in federal and state reimbursement policies for public insurance (e.g., Medicare, Medicaid,
State Children’s Health Insurance Program [SCHIP]). In urban areas, public and large teaching hospitals play a major role in serving uninsured patients, providing levels of uncompensated care much greater than their overall market share. The relationships among practitioners and institutions are more extensive, however, given the greater number of sites at which uninsured persons may be able to receive care (Lipson and Naierman, 1996; Bovbjerg et al., 2000a; Commonwealth Fund, 2001).
Providers of Last Resort
No single public entity functions nationally as a “provider of last resort” in the United States. Legal and financial responsibility for at least some of the care that uninsured persons need varies by locality. To the extent that states, counties, or municipalities do designate a provider of last resort, the services to be provided usually are not specified.
Unlike most developed countries and many developing nations, the United States does not guarantee its citizens or residents access to personal health care services beyond treatment to stabilize an emergency condition and care at child-birth. The minimal national standard of access to health services that has been established by EMTALA, a provision of the Omnibus Budget Reconciliation Act of 1986, is described in Box 2.4.
The facilities of states, counties, and municipalities are, often by default, providers of last resort for patients without the financial means to pay for their own care. Some states explicitly assign responsibility for this role in their constitutions or by statute, while others acknowledge the obligation implicitly through annual budgetary appropriations for personal health care services. Local agencies are more likely than state programs to be involved in the delivery of health services. Some states reimburse local health departments, public hospitals, or clinics for the direct provision of care; some reimburse all hospitals in the state for a percentage of their expenditures; some finance state and county catastrophic care funds; and others subsidize packages of services that resemble an insurance plan (IOM, 1988).
WHO PAYS FOR CARE FOR UNINSURED PERSONS?
Finding: Public support for the uncompensated care expenses incurred by uninsured persons is substantial. The public sector is estimated to finance up to 85 percent of the $34 billion to $38 billion in uncompensated care estimated to have been rendered to uninsured persons in 2001. The exact amount is unknown, because states and providers do not consistently document or report these public expenditures in ways that tie spending directly on behalf of unin-
|
BOX 2.4 EMTALA was enacted in 1986 to counter the practice of hospitals turning away or inappropriately transferring patients who did not have the means to pay for their care (a practice known as patient dumping) (Schiff et al., 1986; Ansell and Schiff, 1987; Friedman, 1987; Kellerman and Hackman, 1990; Bitterman, 2002). As a condition for participating in the federal Medicare program, hospitals must adhere to the requirements of EMTALA, which directs them to medically screen and stabilize all patients who present themselves to the emergency department for treatment and prohibits prescreening with regard to a patient’s insurance coverage or means to pay for care (Fields et al., 2001). The hospital is not precluded from billing the patient after the service has been provided, whether or not the patient has insurance or other resources to pay. EMTALA does not require any care beyond screening, stabilization, and, if necessary, hospitalization. Thus, uninsured persons who seek care in hospital emergency departments are unlikely to achieve continuity in their care over time, one hallmark of high-quality care (IOM, 2001b, 2002a). EMTALA is the single federal statutory provision that directly addresses the right to health care for uninsured persons (Fields et al., 2001). Most significantly for the financial viability of hospitals and emergency physicians, EMTALA does not authorize or appropriate any federal or other public funds to support its mandate. The requirements of EMTALA have ramifications not only for how emergency departments (EDs) function but also for the availability of inpatient beds and the willingness of specialists to serve on physician on-call panels to handle all cases within EDs and hospitals generally (Kamoie, 2000). |
sured persons. Many of the sources that do pay for services delivered to uninsured persons are not explicitly authorized or appropriated to do so, contributing to the uncertainty about the extent of public support for such care.
Finding: Although a larger scale and scope of public insurance programs (e.g., Medicaid, SCHIP) is sometimes associated with lower uninsured rates at the state level, it is the size of an area’s lower-income population (families with incomes of less than 200 percent of the federal poverty level, or FPL) that determines the relative need for public support for health care of all kinds (including both insurance and direct services). At the state level, higher uninsured rates tend to be associated with higher levels of public spending on coverage.
Finding: There is little direct evidence about the size of private payers’ cross-subsidy of the unreimbursed costs of care for uninsured persons.
There is no uniform public responsibility to subsidize or pay for the care delivered to uninsured persons. The financing that exists is diffuse, spread unevenly, and varies by locality.
The financial and organizational ties that bind safety-net arrangements to mainstream health care mean that unreimbursed expenditures for health services delivered to uninsured persons are borne by both public and private payers and by federal taxpayers as well as state and local ones. These expenditures, charges, or costs contribute to the total burden of uncompensated care shouldered by local providers and governments at all levels. It is hard to estimate the extent of uninsurance’s draw on public sector resources both because of the lack of explicit documentation and the lack of a comparison scenario (e.g., public expenditures if all uninsured persons were insured). It is likely that many of the same public funding streams would remain in place, especially because they do not target uninsured persons specifically. This topic, as well as the issue of what “true” costs of uninsurance may be estimated for the nation as a whole, will be discussed in greater depth in the Committee’s fifth report. It is introduced briefly here to give a more complete overview of health care financing for uninsured persons.
Even though individuals without health insurance are estimated to use only two-thirds of the care of comparable insured populations, the costs of the services that they do use are considerable (Marquis and Long, 1994–1995). Uninsured persons are more likely to forgo care until health conditions deteriorate, leading to more costly and less effective courses of treatment (IOM, 2002a, 2002b). Faced with a need for health care, some people without health insurance seek the care they need and pay for it out of pocket, and some try to obtain the care at subsidized rates or at public expense. Most people probably adopt some combination of these strategies. Given the limited incomes of most uninsured persons and the cost of health care, the costs borne societally (e.g., by taxpayers) for the care of uninsured persons is likely to be substantial.
One recent analysis of uncompensated care provided to uninsured Americans derived and compared estimates from two independent sources of information, one, the Medical Expenditures Panel Survey (MEPS) and the other, provider reports of uncompensated care. The authors of this study estimate the value of such care for 2001 in the range of $34 billion to $38 billion (Hadley and Holahan, 2003). For the estimate based on MEPS, the authors used reported expenditures, pooled for the years 1996 through 1998 and adjusted for an undercount of uninsured persons (care that is not billed is not recorded by MEPS) to arrive at an estimate of $34.5 billion in free care and $26.4 billion in out-of-pocket expenditures, for a total of $60.9 billion spent, in 2001 dollars. Their series of estimates about the providers and sources of financing for the proportion of uncompensated care delivered to uninsured persons is summarized in Table 2.1.
As described in Table 2.1, combined federal, state, and local spending is estimated at $30.6 billion, which the authors calculate equals about 5 percent of estimated public spending for Medicare, Medicaid, and the tax benefit of employment-based insurance plans in 2001 (Hadley and Holahan, 2003). The discussion
TABLE 2.1 Summary, Estimated Amounts and Sources of Payment for Free Care Delivered to Uninsured Persons, 2001
|
|
Est. Spending for Uninsured Persons ($$, billions) |
||||
|
Provider Type |
Source of Funds |
Federal |
State and Local |
Private |
Total |
|
Physicians (independent of health care facilities) |
Charity/practitioners |
|
|
5.1 |
5.1 |
|
Clinics and Government (direct care) |
Veterans Administration |
3.89 |
|
3.89 |
|
|
|
BPHC (e.g, CHCs) |
0.47 |
0.26 |
0.11 |
0.84 |
|
Indian Health Service |
0.67 |
0.02 |
|
0.69 |
|
|
HIV/AIDS Bureau |
0.59 |
0.09 |
|
|
|
|
Local health departments |
|
0.58 |
|
0.58 |
|
|
MCHB |
0.06 |
0.23 |
0.02 |
0.31 |
|
|
NHSC |
0.01 |
|
0.11 |
0.12 |
|
|
Totals, Support for Clinics |
|
5.69 |
1.29 |
0.13 |
7.11 |
|
Hospitals (nonfederal) |
Medicaid DSH |
6.7 |
1.7 |
|
8.4 |
|
|
Medicare DSH |
5.0 |
|
5.0 |
|
|
State and local indigent care |
|
4.3 |
|
4.3 |
|
|
State and local appropriations to hospitals |
|
3.1 |
|
3.1 |
|
|
Private (hospital surplus revenues) |
|
|
1.5-3.0 |
1.5-3.0 |
|
|
Medicare IME |
1.6 |
|
|
1.6 |
|
|
Private (philanthropy) |
|
|
0.8-1.6 |
0.8-1.6 |
|
|
Medicaid UPL |
0.9 |
0.3 |
|
1.2 |
|
|
Totals, Support for Hospitals |
|
14.2 |
9.4 |
2.3-4.6 |
25.9-28.2 |
|
NOTES: Definitions of acronyms follow; see glossary for explanations of programs. BPHC = Bureau of Primary Health Care; DSH = Disproportionate Share Hospital; IME = Indirect Medical Education; MCHB = Maternal and Child Health Bureau; NHSC = National Health Services Corps; UPL =Upper Payment Limit. SOURCE: Hadley and Holahan, 2003. |
|||||
and Table 2.1 that follow are not meant to be a comprehensive assessment of the adequacy or cost-effectiveness of current financing arrangements but rather to provide a sense of the magnitude of public and private supports for care to the uninsured persons.
Persons who are without health insurance for the entire year pay out of pocket an average of about 35 percent of the charges and payments for health care made on their behalf (Hadley and Holahan, 2003).10 The proportion paid out of pocket varies by the type of service (e.g., physician, inpatient hospital, prescriptions) (IOM, 2002b). If the provider who delivers the service is to remain financially viable, some or all of the remainder must be covered by federal, state, and local governmental funds or by charity.
While a significant proportion of the health care that uninsured persons receive is paid for by the uninsured themselves, an even greater share is subsidized either explicitly or implicitly. The distribution of this subsidy varies by locality, reflecting the different configurations of health services markets both among and within states, including which public entity or level of government, if any, has the responsibility to serve as a provider of last resort. The proportion of the subsidy borne by government, providers, and philanthropy also varies by type of service.
Explicit subsidies include public sources such as operating grants to community health centers and public hospitals and private sources such as philanthropic grants and hospital endowments for charity care. Examples of indirect subsidies include public subsidies for health professional education and research at safety net hospitals (e.g., Medicare graduate medical education payments), as well as higher charges for services provided to patients who are insured. Medicare and Medicaid disproportionate share hospital (DSH) payments are nominally implicit subsidies of care for uninsured persons because their explicit justification is the greater cost of caring for lower-income federal program beneficiaries; however, these payments are widely understood as compensating hospitals for the costs of their nonpaying patients as well.11
Public Payers
The role of federal, state, and local governments in supporting personal health services for uninsured persons is substantial:
-
Federal programs, funding, and regulation create the financial, legal, and organizational contexts within which care to the uninsured is provided. The federal government’s primary role is in financing health care services. It accom-
-
plishes this function largely through insurance mechanisms such as Medicare, Medicaid, and SCHIP and also through grant programs for service delivery (e.g., the Community Health Center program) and direct delivery (e.g., Department of Veterans Affairs facilities, Indian Health Service). These various programs are administered independently of each other, by different agencies within the Department of Health and Human Services and even by different departments (Veterans Affairs).
-
States determine eligibility standards and provide funding for health insurance programs (Medicaid, SCHIP, and similarly structured programs serving populations that do not qualify for federal matching funds) that directly affect the number and characteristics of uninsured residents.
-
Local governments, through the operation of public hospitals and clinics (and, increasingly, by contract) directly serve uninsured community members and, in some jurisdictions, also contribute to the financing of the state Medicaid program.
The sections that follow discuss the contributions of federal, state, and local governments in turn.
Federal Government
Through a variety of programs and funding mechanisms, different federal agencies support a portion of the health care services delivered to uninsured people and others unable to pay for their care. This support includes categorical and unrestricted grants; loans to public and private agencies, organizations, companies, and individuals; and the direct provision of care. Box 2.5 lists the major federal sources and mechanisms.
Monies for the care of uninsured people are provided largely through special financing provisions of the Medicaid program and by state and local tax revenues that subsidize uncompensated care for lower-income persons. States have employed a variety of approaches to raise the maximum amount of dollars that can be used to obtain federal matching funds through the Medicaid program, including the DSH payments (discussed below) and other financing mechanisms such as provider taxes and donations, administrative claims for school-based services, intergovernmental transfers, upper payment limits, and tobacco settlements (see Figure 2.2) (Schneider, 2002). In addition, federal Medicaid waivers to state governments have allowed states to redirect Medicaid monies toward the care of uninsured persons (Coughlin and Liska, 1997).
Even though uninsured persons by definition are not enrolled in Medicaid, their care is subsidized by Medicaid payments, a substantial portion of which are made to public hospitals, academic health centers, and other hospitals that disproportionately serve uninsured people. In addition, there is considerable overlap between the uninsured and Medicaid-enrolled populations, given the high turnover rates in the enrolled population and the similar demographic characteristics
|
BOX 2.5 Subsidies Through Public Insurance Programs
Programs Targeted at the Uninsured and Medically Underserved
Direct Provision of Health Services to Entitled Categories of People
Grants for Categorical Services
|
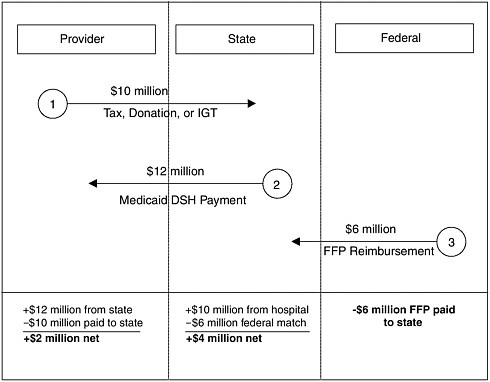
FIGURE 2.2 How a DHS program can work.
NOTE: IGT = intergovermmental transfer, FFP = federal financial participation.
SOURCE: Coughlin and Liska, 1997.
for Medicaid enrollees and uninsured people (e.g., family or household income of less than 200 percent FPL).
Both the Medicare and the Medicaid programs are significant sources of indirect financing for care to the uninsured. The Medicare and Medicaid DSH provisions, which provide for additional payments to hospitals that serve a “disproportionate share” of low-income patients, are particularly important in this context. The Medicare DSH payment provision (see Box 2.6) was authorized originally by the 1983 legislation establishing prospective payment for hospital inpatient services under Medicare, to allow payment adjustments to take account of the special needs of public and other hospitals serving low-income patients (Schneider, 2002). The Medicaid DSH (see Box 2.7) program was created in 1981 as part of the Omnibus Budget Reconciliation Act (Schneider, 2002). It required hospitals to establish payment rates that take into account the situation of hospitals serving a disproportionate share of low-income patients. Although the nominal purpose of Medicare and Medicaid DSH payments was to compensate hospitals for the additional costs of serving low-income program beneficiaries, the original impetus for the programs included a recognition of the need for additional rev-
|
BOX 2.6 In fiscal year 2001, Medicare DSH payments to hospitals amounted to an estimated $5.0 billion (Hadley and Holahan, 2003). Medicare DSH payments are allocated among hospitals according to an index that sums two ratios: the share of total patient days represented by Medicaid patients and the share of Medicare patient days represented by patients receiving Supplemental Security Income (and who are thus also Medicaid enrollees) (Nicholson, 2002). Hospitals with index values that exceed certain thresholds (different for rural and urban hospitals and for hospitals of varying size) are eligible for DSH payments. One recent analysis of Medicare DSH payments concludes that, although the Medicare DSH formula rewards hospitals for high proportions of Medicaid and Medicare patients, it does not result in higher payments to hospitals that actually have relatively high uninsured patient loads (Nicholson, 2002). The Medicare Payment Advisory Commission (MedPAC) has recommended that the Medicare DSH index be revised to take uncompensated patient careloads directly into account (Nicholson, 2002). |
|
Box 2.7 Medicaid DSH payments, both federal and state shares, amounted to $15 billion in 1998, of which $9billion were federal funds (Schneider, 2002). For 2002, the federal share of DSH payments is projected to exceed $9 billion (Miller, 2002a). Only about 75 percent of federal DSH payments are estimated to go to general hospitals, however, since a significant portion of these monies support state mental hospitals and some of the monies are returned by the institutions receiving them to state treasuries in the form of provider tax payments (Schneider, 2002). States have a great deal of discretion in determining how Medicaid DSH payments are distributed among hospitals. Federal statute requires that states have a program of DSH payments and that, at a minimum, they make such payments to hospitals whose share of Medicaid patient days is at least one standard deviation above the average (mean) for the state or whose low-income patient use rate is 25 percent or more (Coughlin et al., 2000). However, states may make DSH payments to hospitals with Medicaid patient day shares as low as 1 percent. |
enues by hospitals caring for a high volume of uninsured patients and a relatively low volume of privately insured patients (Coughlin and Liska, 1997; Fagnani and Tolbert, 1999; Coughlin et al., 2000; Nicholson, 2002).
Medicaid and Medicare DSH payments shape local capacity to provide services for uninsured persons, even though the number of uninsured patients and the amount of care provided them are not taken directly into account when allocating these funds (Fagnani and Tolbert, 1999). Past decreases in DSH funding
levels due to the Balanced Budget Amendments of 1997 have increased the financial pressures on hospitals that disproportionately serve Medicaid and uninsured patients, while recent legislative changes in the Medicare, Medicaid, and SCHIP Benefits Improvement and Protection Act of 2000 are likely to lead to increased DSH payments.
States vary greatly in their participation in Medicaid DSH, the extent to which they draw down the maximum amounts they are allowed under the program, and their reallocation of other public funds in response to DSH payments. On average, Medicaid DSH payments account for 6.6 percent of federal Medicaid grants to the states. Eight states have federal DSH grants that account for more than 10 percent of federal grants for Medicaid inpatient services, while 19 states have DSH grants amounting to less than 3 percent of that total (Miller, 2002a). Only a small proportion of state Medicaid DSH payments is assumed to be funding available to cover uncompensated care (Ku and Coughlin, 1995). If states or localities reduce their own support of hospitals for uncompensated care and simply allow federal payments to replace what they had previously supported, the value of the DSH payments to providers is obviously less than if the federal support augments state and local funding. Table 2.2 represents a regional summary of federal payments to the states under the Medicare and Medicaid DSH programs in 1998, compared to the relative size of the target population (uninsured persons and Medicaid enrollees) within the region. See Table C.4 in Appendix C for a summary by state.
TABLE 2.2 Combined Federal Medicare and Medicaid Disproportionate Share Hospital (DSH) Payments by Census Region, 1998
|
|
Population <65 yrs, 1998 (millions) |
No. of Uninsured 1998 (millions) |
Uninsured, Rate, 1998 (%) |
No. of Medicaid 1998 (millions) |
Medicaid, Rate, 1998 (%) |
|
Total |
238.6 |
43.9 |
18.4 |
24.9 |
10.4 |
|
New England |
11.7 |
1.5 |
12.6 |
1.3 |
11.1 |
|
Middle Atlantic |
33.5 |
5.7 |
17.0 |
4.0 |
12.0 |
|
East North Central |
39.4 |
5.7 |
14.6 |
3.7 |
9.4 |
|
West North Central |
16.3 |
1.9 |
11.6 |
1.4 |
8.8 |
|
South Atlantic |
41.4 |
7.8 |
18.9 |
3.7 |
9.0 |
|
East South Central |
14.4 |
2.5 |
17.6 |
2.0 |
13.7 |
|
West South Central |
26.8 |
6.7 |
25.2 |
2.6 |
9.8 |
|
Mountain |
15.5 |
3.3 |
21.5 |
1.2 |
7.4 |
|
Pacific |
39.6 |
8.7 |
22.0 |
5.0 |
12.6 |
|
SOURCE: Fronstin, 2000; Wynn et al., 2002. |
|||||
The table gives a rough approximation of the marked variation across regions in state participation in the DSH programs, participation that may not necessarily correlate with the need for public support, as indicated by the size of the target population:
-
The West South Central region has the highest proportion of the target population for public support (35 percent either uninsured or enrolled in Medicaid, which is 122 percent of the average nationally), and states in this region receive on average 104 percent of the national average combined DSH payment per member of the target group ($301). The Pacific region has almost as high a proportion of the target population as the West South Central region (34.6 percent either uninsured or enrolled in Medicaid), and states in this region receive on average 96 percent of the national average combined DSH payment ($276).
-
The New England states, whose proportion of uninsured and Medicaid-enrolled persons (23.7 percent) is 82 percent of the national average, receive on average 172 percent of the national average DSH payment ($495).
-
For states in the Mountain region, the proportion of the target population is comparable to the national average (28.9 percent), but the combined DSH payments per member of the target group fall short, with the region’s states receiving on average 40 percent of the national average DSH payment ($114).
|
Sum No. (Uninsured and Medicaid), 1998 (millions) |
Sum Rate (Uninsured and Medicaid), 1998 (%) |
Sum Rate/ Total, (%) |
Combined Medicare and Medicaid DSH Payment, 1998 (millions) |
Combined DSH/Sum No. ($$) |
Combined DSH/ Sum No./ Total (%) |
|
68.8 |
28.8 |
100 |
19,844 |
288 |
100 |
|
2.8 |
23.7 |
82 |
1,387 |
495 |
172 |
|
9.7 |
29.0 |
100 |
4,391 |
453 |
157 |
|
9.4 |
24.0 |
83 |
1,843 |
196 |
68 |
|
3.3 |
20.4 |
71 |
961 |
291 |
101 |
|
11.5 |
27.9 |
97 |
3,012 |
262 |
91 |
|
4.5 |
31.3 |
109 |
1,154 |
256 |
89 |
|
9.3 |
35.0 |
122 |
2,795 |
301 |
104 |
|
4.5 |
28.9 |
100 |
514 |
114 |
40 |
|
13.7 |
34.6 |
120 |
3,787 |
276 |
96 |
State Government
Health activities within a state reflect budgetary priorities set by both the state and the federal government. The federal government supports almost half of all health care spending by state governments, with the proportion of federal funds varying by program (NACCHO, 2001). Federal grant dollars are a large part of state public health budgets (50 to 85 percent in the mid-1990s in the 13 states studied in the Urban Institute’s Assessing the New Federalism project) (Wall, 1998).12 For state governments as for the federal government, health care is the single largest budget item (NACCHO, 2001).
In addition to state constitutional or delegated responsibilities for public health and welfare, state budget decisions have important implications for all of the health activities within the state. States administer and share the financing of their own Medicaid program, in conjunction with the federal government. Each state has its own health department, as well as local health departments. While state agencies may provide health services directly to vulnerable populations, including uninsured persons, they more often provide financial support, both through the operation of public insurance programs such as Medicaid and SCHIP and through grants and revenue sharing to counties and other jurisdictions. Forty-two states have general assistance programs for medically indigent persons, including the uninsured, and fourteen states have other subsidy programs (Rajan, 1998). A recent study divides state-supported programs into two groups: (1) those that pay for or subsidize coverage of uninsured persons, including subsidy of employment-based coverage, and support for persons who are not eligible for public coverage or who are deemed medically uninsurable, and (2) those that pay subsidies directly to health care providers, using general revenues or dedicated taxes (Seifert, 2002).
State Policy Choices for Public Insurance Programs
The choices states make about Medicaid influence the size of their uninsured population. Although the federal government provides well over half of the costs of Medicaid and SCHIP, states have discretion in their programs’ eligibility criteria, benefits, and payment rates beyond minimum federal standards.13 In addition to determining what proportion of their low-income population is eligible for Medicaid, states vary widely in payment rates for services. Both the extensiveness of their public insurance programs and the level of payments for services under these programs affect the financial status of health care providers that serve unin-
sured persons. They also affect whether hospitals and physicians serve the uninsured at all because if Medicaid payment rates are too low, providers cannot afford to offer uncompensated care. Box 2.8 describes the distinctive experiences of Medicaid waiver programs in Oregon and Tennessee that extended coverage to previously ineligible state residents, ostensibly financed in both cases by reduced payments for services.
Although local (county, city, district) tax revenues are the primary source of support for public hospitals and clinics, state dollars may also come from separate payments for medical education (supplementing those made by Medicare), appropriations to medical schools, and state-sponsored uncompensated care pools (discussed below) that reimburse hospitals. The state and local tax base, along with the state’s level of “fiscal effort,” account for much of the funding differences among states (Trenholme and Kung, 2000). See Appendix B for further discussion of how differences in state spending contribute to differences in uninsured rates.
State Uncompensated Care Pools
In Maryland, Massachusetts, New Jersey, and New York, an uncompensated or free care pool redistributes some of the disproportionate burden of uncompensated care borne by some hospitals more equitably among all hospitals in the state (Needleman, 1999; Bovbjerg et al., 2000a). Box 2.9 describes the operation of Massachusetts’ pool as a case in point. Pools have the potential to facilitate greater access to care for uninsured persons who do not live near public hospitals (Bovbjerg et al., 2000a). The pool of funds for uncompensated care is raised by surcharges on payments to hospitals by insurers and patients.
Uncompensated care pools began in the 1970s, in response to growing uncompensated care costs and health care inflation spurred by an economic recession. They were incorporated into these four states’ hospital rate-setting regulations during the 1980s (Bovbjerg et al., 2000a). With the deregulation of hospital payment practices in the early 1990s (except in Maryland), the states turned to Medicaid DSH payments and Medicaid waivers as additional revenue sources for their pools. States have narrowed the scope of the care that qualifies for payment through the pools, targeting only charity (rather than all) uncompensated care and only those hospitals providing the greatest volume of such services. As uncompensated care expenditures continued to rise during the 1990s, pool resources were exhausted.
Like Medicaid DSH payments, state uncompensated care pools are an indirect means of financing care for uninsured persons and, as such, have similar problems with inefficiencies. Increasingly competitive hospital markets have spurred greater resistance by hospitals to assessments levied by the state, and fair and efficient targeting of pool funds is made more difficult by lack of information about actual amounts of charity care provided to uninsured patients. Hospitals that provide uncompensated care but are not recognized as safety-net institutions (i.e., are not public or teaching hospitals) are less likely to receive compensation from pools.
|
BOX 2.8 In 1994, Oregon and Tennessee each began a major expansion of their Medicaid programs, using federal waivers (which required that the new program be budget neutral) and managed care contracting. All persons at or below 100 percent of the federal poverty level became eligible for public coverage or for employer-subsidized coverage. Expanding Medicaid to decrease uninsurance has involved hard choices for these demonstration states, and their success has been mixed and limited. In 2001, both states had uninsured rates below the national average. Still, each had a sizable uninsured population: 443,000 uninsured persons in Oregon (12.8 percent of the state’s population of 3.5 million persons) and 640,000 uninsured persons in Tennessee (11.3 percent of the state’s population of 5.7 million) (Mills, 2002). Oregon Since the 1980s, health reformers have attempted to implement universal coverage in the state incrementally, by means of a series of coordinated measures. These include the Oregon Health Plan, which is a Medicaid expansion to all persons at or below 100 percent of FPL, an employer mandate (which has not been implemented), a public subsidy for workers to purchase employment-based coverage, and a state high-risk pool for persons unable to purchase coverage privately due to their medical conditions (medically uninsurable persons). The immediate spur to action was the highly publicized death of a 7-year-old boy from leukemia following the state Medicaid program’s rejection of a proposed transplant to treat the child’s disease. A unique political and technical strategy for engaging public and legislative discussion about the cost of the Medicaid expansion was to make decisions about the scope of Medicaid benefits explicit. Conditions for which treatment would be covered under the program were ranked in order of priority, an approach described as rationing care. Ostensibly, the goal of this approach has been a budget-neutral program expansion. In reality, there is little evidence of cost savings under the new list-based approach to Medicaid benefits, given federal limits placed on changes to Medicaid’s benefit package and anecdotal evidence that uncovered care has been provided, if not reimbursed, through other means. The Medicaid expansion has been underwritten by new state general revenues and proceeds from a new tax on cigarette sales. The Oregon Health Plan has lowered the state’s uninsured rate, covering an estimated additional 130,000 low-income persons who would otherwise be uninsured, improved access to care and quality of care for low-income residents, and reduced uncompensated care. In addition, the process of developing and revising the list of benefits that Medicaid covers has fostered social cohesion, building popular support for the Medicaid program.1 |
|
Tennessee Tennessee’s reforms were motivated by an imminent fiscal crisis in the state’s Medicaid program after challenges to its use of a provider tax to raise state matching funds for Medicaid (a situation somewhat unique to Tennessee, which does not levy an income tax). A federal Medicaid waiver moved all of the state’s Medicaid enrollees into private sector managed care, doubled the size of the Medicaid program to make eligible all persons at or below 100 percent of FPL; and extended public coverage to all uninsured children through age 17. Benefits were made more generous than under the Medicaid program, with some cost-sharing and premiums tied to income. Despite the large increase in enrollment that followed expanded eligibility and the greater volume of services delivered by providers at lower reimbursement rates, there was a relatively small increase in new funds to support TennCare. Dollars have come from federal and a variety of state and local revenue streams, including DSH payments to hospitals and annual insurer assessments that had been supporting a state high-risk pool. Capitation resulted in lower per-enrollee payments. One study estimates that during the TennCare’s first five years, state and federal government spent about $700 million less than would have been predicted for the Medicaid program without the waiver but that TennCare’s expansion of eligibility cost approximately $3.8 billion more, when predicted changes in charity care, patients’ cost-sharing, and local government spending were considered. In the first year after TennCare began, the state’s uninsured rate shrank by one-third to one-half, putting the state well below the national average uninsured rate, and there was greater coverage of medically uninsurable persons. This dramatically lower rate has not been maintained, although Tennessee continues to have a lower-than-average uninsured rate. After the first year, fiscal constraints led state officials to close further enrollment of uninsured persons ineligible for Medicaid. In the years since, problems related to TennCare’s relatively low capitation rates and potential for adverse risk selection of chronically ill patients have meant further financial stresses and less progress in reducing uninsurance. Lower reimbursement rates have contributed to financial losses that have fiscally destabilized public hospitals and academic health centers, community health centers, and physicians in private practice that serve Medicaid and uninsured patients, and uncompensated care has continued to grow. Although TennCare has improved access to care, quality of care, and consumer satisfaction, and has introduced some efficiencies, it has also fueled tensions between providers and state Medicaid administrators and among beneficiaries, providers, and the state. This has resulted in a decline in social cohesion and a relative lack of popular support that have made it more difficult to secure funding for the program.2 |
|
BOX 2.9 The Commonwealth of Massachusetts has operated an uncompensated or free care pool since 1985. The goal of the pool is to lighten the burden of uncompensated care related to charity at hospitals and freestanding community health centers that serve large numbers of uninsured and medically indigent persons, by redistributing a portion of the costs incurred in providing these services across all hospitals in the state. For persons judged to be medically indigent (medical expenses greater than 30 percent of income and insufficient assets to cover the expenses) and for lower-income uninsured patients (less than 200 percent of FPL), care is free to the patient and eligible to be fully reimbursed through the pool if funds are available. Care provided to moderate-income (between 200 and 400 percent of FPL) uninsured patients is partially free to the patient and eligible for reimbursement. Although both clinics and hospitals participate in the pool, hospitals are the primary beneficiary, for both inpatient and outpatient services. Allowable free care does not include prescription drugs, physician care outside of what is billed through hospitals or clinics, or services provided by nonacute care hospitals. The pool is financed by hospital assessments ($170 million in fiscal year 2002); surcharges on payments for hospital and ambulatory surgery center services by private payers (e.g., health plans), including individuals with medical bills over $10,000 ($100 million); and annual state appropriations comprised of federal matching dollars through the Medicaid DSH program ($30 million; the remaining $120 million to $130 million in matching Medicaid DSH dollars goes into state general revenues). Additional state contributions to the pool may also include in |
Finally, the pool may unintentionally encourage poor management practices or poor quality of care at hospitals, for example, by offering financial incentives to provide hospital inpatient rather than outpatient care for conditions that may not require hospitalization (Dunn and Chen, 1994; Spencer, 1998; Bovbjerg et. al, 2000a).
City and County Governments
There are approximately 3,000 local health agencies across the country. These include county, city, combined city–county, township, and district or regional organizations. Sixty percent of local public health agencies are at the county level, and 69 percent of local agencies are in jurisdictions of fewer than 50,000 persons (NACCHO, 2001). Annual spending varies from zero to more than $836 million (1999–2000 figures), with median annual expenditures of $621,000 in 1999 dollars (NACCHO, 2001). The largest proportion (average of 44 percent) of total budgets for these health departments comes from local funds (county, city, town), with an average of 30 percent from state funds and federal funds passed through by
|
tergovernmental transfers from public hospitals in Boston and Cambridge ($70 million in fiscal year 2002), surplus funds from a payroll tax-supported Medical Security Trust Fund that finances coverage for unemployed workers ($90 million), and proceeds from the Tobacco Settlement Fund. On a monthly basis, hospitals submit information to the state about charges incurred by private sector payers, bad debt connected with the provision of emergency department services, and free care delivered to persons qualified to receive such care on the basis of income and residency criteria. Each hospital is credited or reimbursed a portion of the costs, adjusted for an assessment based on the proportion of private sector charges and a proportion of the fund’s anticipated shortfall. Demands on the pool have outpaced available funds in all but two of the past ten years, and current budget trends indicate continuing pressures from state fiscal cutbacks and pressures related to the functioning of the pool and its relationship to the state’s Medicaid program (MassHealth). Unanticipated stress on pool resources may result from unintended incentives for hospitals to turn to the pool as a first-dollar payer rather than as a payer of last resort, despite pool regulations stipulating that hospitals screen patients for public coverage eligibility, because of higher reimbursement for services compared with public health insurance reimbursements. The pool’s viability also depends in part on the status of MassHealth. For the first three years following expansion of MassHealth in the latter part of the 1990s, draws on the free care pool declined, although increasing health care inflation countered this decline in subsequent years. Also, a planned cutback in MassHealth eligibility, expected to result in 50,000 newly uninsured adults in 2003, is likely to result in greater demand on free care pool resources as well as the loss of federal Medicaid DSH matching dollars available to the pool. SOURCES: Bovbjerg et al., 2000a; Bovbjerg and Ullman, 2002; Seifert, 2002. |
the state to localities. Three percent comes to localities directly from the federal government. Overall, local health departments receive an average of 19 percent of their budgets as reimbursement for direct health services delivery (Medicare, Medicaid, third-party insurers, fees) (NACCHO, 2001).
Local health departments deliver primary care and categorically funded services that are both public health activities and personal health care services (e.g., maternal and child health, immunizations, family planning clinics). In areas with a high uninsured rate, local health departments frequently have absorbed the increases in demand for services from medically indigent residents. Since the late 1980s, health departments have shifted away from the direct provision of personal health services and toward privatizing or contracting out services delivery (Wall, 1998; NACCHO, 2001). At the same time, health departments have become more reliant on Medicaid reimbursements for services they previously provided without charge. However, this source of funds began to decline in the early 1990s, as Medicaid programs entered into managed care contracts with private sector health care providers (Martinez and Closter, 1998; Wall, 1998; Fairbrother et al., 2000).
The degree to which health departments directly provide or arrange for the delivery of health services varies by region and urban versus rural location. Urban health departments are more likely than rural agencies to be involved in the delivery of primary care services and often provide primary care, maternal and child health services, and sexually transmitted disease screening and treatment. Thirty-seven percent of health departments serving more than 500,000 people are involved in direct delivery of health services, compared with 11 percent of agencies serving fewer than 25,000 people (NACCHO, 2001). County health departments in California and Florida and in the South are more likely than health departments in other areas of the country to be involved in direct provision of service. In California and Florida, this involvement stems from the sizable unmet need due in part to high levels of uninsurance, while in the South it reflects historical shortages of private health facilities and providers, particularly in lower-income and rural communities (Needleman et al., 1999).
Public hospitals receive much of their nonoperating revenue from local (municipal and county) dollars (Bovbjerg et al., 2000b). State support may be less important than local public funding for public and other facilities that disproportionately serve uninsured patients. In one study of safety-net capacity in five urban areas, four of the sites had city or county subsidies for general health services (in addition to support for the local health department) through contracts with a city health department or academic health center to provide services, a managed care program sponsored by the county, or support for a public hospital (Felt-Lisk et al., 2001). Box 2.10 details the financing and organization of care for uninsured persons in a number of states and localities to illustrate the variety of arrangements and extensiveness of programs across locales.
Interactions Between Coverage and Services for the Uninsured
As discussed earlier, the size and impacts of a community’s uninsured population are closely related to the scope and scale of the state’s Medicaid program, as well as its spending on direct services and the size of its lower-income population. For example, Massachusetts’ expansion of its Medicaid program to cover childless adults (MassHealth) is estimated to have contributed to a 10 percent decrease in the state’s uninsured rate between 1997 and 1999 (Zuckerman et al., 2001b).
Medicaid payments underpin the financial operations of providers that serve the uninsured and public program beneficiaries alike. Yet the extent of employment-based health insurance coverage has an even greater effect on state-level uninsured rates than does the expansiveness of the state’s Medicaid program (Holahan, 2002). Some researchers have investigated whether the availability of publicly provided services within a community influences local uninsured rates. Rask and Rask (2000) found, using 1987 data, that counties with public hospitals also had higher uninsured rates than counties that did not have their own hospitals. The direction of causality in this study cannot be determined. Another study using more recent national survey data found that, as measured by a composite of
aggregate uncompensated hospital care, physician charity care, and presence of community health centers, low-income workers in cities with a greater safety net capacity to provide charity care are less likely to have an offer of workplace health insurance coverage, although they are just as likely to take up coverage if offered by their employer (Herring, 2001).
Community health centers and other federally supported clinics are in a double bind with regard to Medicaid managed care. Because they have grown to rely on Medicaid revenues in lieu of operating grants, they have an incentive to serve patients who are Medicaid beneficiaries. However, when costs of providing care under Medicaid managed care contracts exceed their capitation payments, the centers’ financial condition worsens. Consequently, they have less revenue with which to provide care to uninsured patients (Shi et al., 2001; Rosenbaum et al., 2002). Financial losses and the loss of capacity are likely to diminish access for all health center clients, insured as well as uninsured—for example, pregnant women and young children covered through SCHIP, low-income members of racial and ethnic minority groups, and low-income seniors enrolled in Medicare.
When legislation in the late 1980s established special cost-based reimbursement for FQHCs, these centers were able to increase their capacity to serve uninsured clients substantially, by 1.6 million persons between 1989 and 1999 (BPHC, 2001). In 1997 the Balanced Budget Act stipulated that the special FQHC provision be phased out. However, consequent to the Benefits Improvement and Protection Act of 2000 (BIPA), the federal government adopted a prospective payment system for Medicaid managed care contracts with CHCs, based on each center’s cost experience, which is expected to ameliorate some of the adverse effects of managed care contracting for health centers (USGAO, 2001; Schneider, 2002).
Private Payers
Philanthropy
Private charitable contributions play a small but important role in financing health care services for uninsured and other medically indigent individuals. Private nonprofit hospitals and health care networks operated by charitable organizations (e.g., Catholic Health Association members) constitute one type of philanthropic support (Catholic Health Association, 2002). Hospital charity care funds also include the endowments of and relatively small contributions to not-for-profit institutions and community foundations established in the conversion of not-for-profit hospitals and health plans to for-profit status (Grantmakers in Health, 2002b). One estimate puts the total value of private philanthropy at between 1 and 3 percent of hospital revenues, of which only a portion is available for the care of uninsured patients (Davison, 2001).
Regional, community-based, and national foundations also play a role in underwriting care to those who are uninsured. For example, the W.K. Kellogg
|
BOX 2.10 Texas In Texas, counties can discharge their duty as provider of last resort by participating in a hospital taxing district (87 counties) that raises funds for indigent care, operating a public hospital (32 counties) or an indigent care program (138 counties), or some combination of these options. Hospital districts levy local property taxes, which account for about one-quarter of the revenue devoted to indigent care, with the remainder financed by the state, out-of-pocket payments, and third-party payers (including Medicaid and Medicare). The state’s Tertiary Care Fund (unclaimed lottery prizes) partially reimburses hospital districts for trauma care provided to residents from outside the district and is received mostly by larger urban districts. Federal Medicaid DSH and Medicare graduate medical education (GME) dollars also support hospital districts—again, often larger urban teaching hospitals. In addition, counties and cities may operate their own public hospitals, without the benefit of a hospital district’s taxing authority or dedicated local tax revenues, and some rural counties operate their own indigent care programs. Texas also has an array of publicly supported safety net arrangements similar to those found in other parts of the country, involving academic health centers, state tuberculosis and psychiatric hospitals, and the criminal justice system (about $270 million spent annually on health care, funded solely by state general revenue because prisoners are ineligible for public coverage). Federal matching and block grants, together with state dollars, support specialty services for uninsured persons as well as for the underinsured, chiefly in the areas of family planning ($65 million annually), substance abuse treatment ($85 million annually), and HIV/AIDS treatment ($56 million annually). Finally, uninsured persons are served by 163 federally qualified health centers (FQHCs), an undetermined number of free clinics, more than 450 rural health clinics, and clinics operated or contracted for by local health departments.1 Colorado With its relatively high 17.8 percent uninsured rate in 1998, the 2.2 million person Denver metropolitan area includes the 500,000 residents of the city and county of Denver as well as five adjacent suburban counties. Financing for services for uninsured residents is more secure in the city and county of Denver and less stable in the suburbs, which are experiencing population growth. In both urban and suburban areas, state Medicaid DSH funds and local funds are critical sources of support for this care. The state finances health care for uninsured persons through the Medicaid DSH program ($174.9 million in 2001), grants for primary and preventive care and for essential community providers ($4.8 million), and the state’s indigent care programs (Denver Indigent Care, University Hospital, and Outstate Medically Indigent Care, $79.6 million altogether), which are also supported through the Medicaid DSH program. The indigent care programs are open to uninsured residents or migrant workers who are either U.S. citizens or legal residents and who meet certain income and assets guidelines (sliding scale for copayments). They reimburse up to 30 percent of costs for a broad range of services delivered by qualified |
|
providers and are supported by the state’s Medicaid program. During 1999, 150,000 Coloradans participated in the state’s indigent care programs. The city and county of Denver support an integrated set of safety-net arrangements through the Denver Health and Hospitals authority, which includes a hospital, 11 FQHCs, a local health department, and 12 school-based clinics, with coordination of services and information across the system. In 1999, Denver’s hospital authority provided close to 40 percent of all inpatient visits under the state’s indigent care program and more than 40 percent of all indigent care program outpatient visits, delivering about half of all uncompensated care in the larger metropolitan area. The state’s Medicaid DSH program and support from the city or county of Denver are major and essential revenue sources for the authority. In 2000, net revenues came from the Medicaid program (33 percent), private insurers (22 percent), the city (11 percent), and Medicare (10 percent). Other sources (e.g., grants, teaching funds) comprised smaller percentages. The city’s annual payment to Denver Health in recent years has averaged about half of Denver Health’s charity care expenses (not including bad debt, expenses reimbursed through Medicaid DSH, federal operating grants, and revenue from patients). In 1999, Denver contributed $26 million toward Denver Health’s estimated $57 million in uncompensated care expenditures. In addition, Denver Health has cultivated new revenue streams from Medicaid managed care (as a partner in statewide Medicaid managed care contracting through Colorado Access); from contracts to care for state and local prisoners and to provide local indigent care and emergency medical services; and from payments made by SCHIP enrollees and paying patients from outside the combined city and county jurisdiction. Compared with the city of Denver, the suburban counties surrounding it have been less successful in financing care for uninsured persons. Safety-net arrangements include three nonprofit clinic networks at 11 sites (coordinated through the Colorado Community Health Network), county health departments, and private hospitals, with University Hospital as the provider of last resort for inpatient care. Population growth has been more rapid in the suburbs than in the city of Denver itself, and with this growth have come relatively greater numbers of uninsured persons who are ineligible for the indigent care programs (undocumented immigrants). In recent years, University Hospital has accumulated losses that administrators attribute to an increasing load of uninsured patients without a sufficient increase in funding, leading to the rationing of available sources and plans for future cutbacks in the amount of charity care to be given.2 Idaho In Idaho, both the state and the counties finance care for the medically indigent. The state operates a Catastrophic Health Care Cost program that reimburses hospitals for individual patients’ bills greater than $10,000 in a one-year period, drawing on a state general fund and a $4.50 per capita fee assessment on each county. Each county functions as the provider of last resort for residents and operates a Medical Indigency Care Program (MICP), supported by local property taxes. At the discretion of the county commissioners, the local MICP may pay bills for less than $10,000 to reimburse necessary care for eligible county residents who apply and are accepted into the program. The structure of the program, eligibility guide- |
|
lines, and reimbursement amounts and schedules vary from county to county. Recipients are expected to reimburse the MICP for at least a portion of their covered expenses according to a payment schedule. To enforce this provision, at the time a resident applies to MICP, a lien is placed on the recipient’s real and personal property and future potential insurance benefits that remains until the payback is completed. A survey of 11 Idaho counties finds that between 1995 and 1999, few of the counties spent the full amount that had been budgeted for MICP, limited reimbursement was collected, and there were no foreclosures on property. In 1999, budgets for 10 of these counties ranged between $123,000 and $5.8 million, with expenditures of between 50 and 90 percent and paybacks of between 4 and 53 percent.3 New Mexico In New Mexico, a state with a high uninsured rate (and no state income tax), some care for uninsured persons is covered through County Indigent Fund programs. Although participation is not required, most of New Mexico’s 33 counties take part in the state’s County Indigent Fund program, which finances payments for health care largely through a gross receipts tax. The counties also collect funds and may use their County Indigent Fund program to support county Medicaid (25 percent of County Indigent Fund expenditures overall) and Sole Community Provider (40 percent of expenditures) programs, both of which receive federal matching funds. The eligibility criteria (including residency and documentation of legal immigration status) and benefits vary from county to county and tend to be limited. County indigent hospital and health care boards have administrative oversight of the funds. In state fiscal year 2001, the participating counties collected about $26.3 million and spent about $28.5 million (including funds carried over from previous years), with a median expenditure of about $570,000 and a range in expenditures from $55,000 for De Baca County to $3.8 million for Dona Ana County on the southwestern border and $3.7 million for San Juan County. In addition, six counties finance indigent care outside the County Indigent Fund, drawing for the most part on property taxes and collecting about $46.1 million in 2001. A closer look at one county gives a sense of the balance of funding streams and expenditures. In urban Bernalillo County, for example, which includes the Albuquerque metropolitan area, during state fiscal year 2001 the county collected $1 |
Foundation’s six-year program of grants to 13 communities through its Community Voices program supports collaborative efforts to expand access to care through expanded insurance coverage (Kellogg Foundation, 2002). Local foundations in California, Rhode Island, New Hampshire, New York, and Kansas have funded programs to expand coverage, both alone and together with national foundations including The Robert Wood Johnson Foundation (Grantmakers in Health, 2002a).
One new source of support for regional or statewide charitable health foun-
|
million in gross receipts tax to pay providers under its County Indigent Fund. In addition, the county collected $31.4 million in property taxes and $5.1 million in a General Fund Health Care Account, which were applied toward support for the University of New Mexico’s County Medical Center, a county mental health center, health care at the county’s detention denter, and service for the debt on a public health facility bond.4 Indianapolis, Indiana Marion County, Indiana, which is contiguous with the city of Indianapolis, operates a managed care program, Wishard Advantage, that enrolls 20,000 of an estimated 40,000 to 60,000 lower-income uninsured persons (earning less than 200 percent of FPL) living in the county. The municipal Health and Hospital Corporation, which oversees the county health department, the county public hospital (Wishard Memorial Hospital), and affiliated health clinics, began this program in 1997 as a way to improve access to primary and preventive services, reduce inappropriate and often costly utilization of the hospital’s emergency department, and put the public hospital on a more sound financial footing in an increasingly competitive hospital market. The number of uninsured persons in the county was also increasing at the time the program began. Benefits are similar to those offered through Indiana’s Medicaid managed care programs, although enrollees have access only to providers in the Wishard Advantage network (e.g., a physicians group practice affiliated with Indiana University Medical School, Wishard Memorial Hospital, a neighborhood health clinic). The Corporation has the authority to levy property taxes and generates roughly $70 million annually in revenues, of which $56 million supports Wishard Advantage. State and federal dollars through the Medicaid DSH payment amounted to almost $52 million in 1997. Funding is considered stable, given the stable tax rate since 1992 and rising property values.5 |
dations is the conversion of nonprofit health plans to for-profit status (analogous to the conversion of nonprofit hospitals) and the creation of local foundations (Grantmakers in Health, 2002b). In California, not-for-profit health plans converting to for-profit status are required by the state to transfer the not-for-profit’s assets into a charitable foundation (California Wellness Foundation, n.d.). A number of foundations have been created in this way, including The California Wellness Foundation (established in 1992 with the assets from the conversion of
the Health Net health maintenance organization [HMO]) and two foundations created from the 1996 conversion of Blue Cross of California into WellPoint Health Networks (The California Endowment and the California HealthCare Foundation) (California Endowment, n.d.; California HealthCare Foundation, 2001; California Wellness Foundation, n.d.). These foundations have supported care to the uninsured through operating grants, but some devote the bulk of their funding to research, technical support, and education.
The pro bono services of physicians and other health professionals in treating uninsured patients, both within their private practices and at specially established clinics, also fall within the category of philanthropy. The extent of such care provided by physicians has been discussed in a previous section.
Privately established free clinics, sponsored variously by faith-based institutions, medical societies, and community coalitions, provide a growing but poorly documented share of services to uninsured persons (Grantmakers in Health, 2002a). A study of changing safety-net capacity in the mid-1990s finds volunteer-staffed free clinics at three of five sites studied (Detroit, Michigan; Columbus, Ohio; and Oklahoma City, Oklahoma) (Felt-Lisk et al., 2001). The clinics have limited hours, are supported by donations, tend to provide primary care and pharmaceuticals for adults, and are often connected with churches. They may be affiliated with local hospitals, but the relationship can be tenuous, with the hospital unwilling to accept referrals. These clinics provide greater access for vulnerable groups, particularly uninsured persons who are ineligible for public coverage (i.e., undocumented immigrants) but are limited in resources and unlikely to be able to sustain continuity of care. Like soup kitchens in church basements for homeless people, the need for and existence of community free clinics point up the inadequacies of local public services and provisions for vulnerable community residents.
Third-Party Payers and Cross-Subsidization
An earlier section of this chapter describes the public subsidies that reimburse some of the uncompensated care expenditures incurred by uninsured persons. Private sector payers may also contribute to the reimbursement of providers’ uncompensated care costs. This section explores how one might think about such a private “cross” subsidy from commercial or private sector payers (e.g., insurers, employers who sponsor employment-based coverage, and covered workers, whose insurance represents part of their compensation package). The extent of private cross-subsidy of the uninsured has not been systematically investigated. Aside from Massachusetts, where provider surcharges finance a free care pool for hospitals and some clinics (Seifert, 2002), such cross-subsidy is expected to be implicit rather than explicit. There is, however, research literature about physician and hospital pricing policy with regard to the “shifting” of incurred costs from public to private payers that suggests how a similar mechanism for private cross-subsidy of a portion of the unreimbursed costs of the uninsured would work.
The term cost-shifting has been defined in a number of ways. Some studies consider shifting in a static sense (e.g., price discrimination, when a hospital charges different prices of different payers, without any particular relationship between the different prices). Others, which look at shifting in a dynamic sense (e.g., when the price charged to one payer is higher because a lower price is charged to another payer or because of a shortfall in revenue from the other payer), are more relevant to understanding potential cross-subsidies of uncompensated care (Morrisey, 1996). In the early 1980s, the term described how, after the advent of Medicare prospective payment, hospitals sought to “shift” what they considered unreimbursed expenditures for Medicare patients to private payers by means of higher billed rates for health services (Morrisey, 1994; Clement, 1997– 1998). In the first half of the 1990s, attention focused on cost-shifting from private (managed care contracting for employment-based coverage) to public payers.
Changes in hospital margins over time give a rough sense of the extent to which private cross-subsidies affect hospitals’ capacity to absorb uncompensated care expenditures. Figure 2.1 depicts the simultaneous decline in private payer surpluses for hospital payments over the past 10 years with little change in reported (net) uncompensated care and change in hospitals’ financial margins; the trends could be interpreted as evidence that hospitals have actually been able to raise their charges to private payers in order to cover uncompensated care costs. It is difficult to interpret the changes in hospital pricing because published studies have examined individual hospitals, rather than the overall relationship between uncompensated care, uninsured rates, and pricing trends in the hospital services market overall.
There is little published evidence about cross-subsidizing uncompensated care among for-profit hospitals. To the extent that such institutions conform to standard economic models of profit maximization, they would be predicted to minimize their provision of uncompensated care (Needleman, 2000; Zwanziger et al., 2000). One analyst argues that there was little or no cross-subsidization from private payers during the 1990s, despite the potential for it, because of “price sensitive employers, aggressive insurers, and excess capacity in the hospital industry,” all of which imply a relative lack of market power on the part of hospitals (Morrisey, 1996). Older data (from the 1980s) yields somewhat more evidence for cross-subsidization among nonprofit hospitals than among for-profit hospitals (Hadley and Feder, 1985; Frank and Salkever, 1991; Morrisey, 1993, 1994; Gruber, 1994; Hadley et al., 1996; Dranove and White, 1998; Needleman, 1999). Hospitals have been less able to shift costs among payers as health services markets have become more competitive (Morrisey, 1993; Bamezai et al., 1999; Keeler et al., 1999). In some circumstances (e.g., California in the 1980s and early 1990s), uncompensated care has declined in response to increased market pressures and to public policy (Gruber, 1994; Rundall et al., 1988; Mann et al., 1995). Instead of shifting costs, hospitals are cutting costs and reducing uncompensated care (Campbell and Ahern, 1993; Gruber, 1994; Zwanziger et al., 1994; Hadley et al., 1996;
Morrisey, 1996; Dranove and White, 1998). Some analysts argue, however, that the ability to cross-subsidize care remains substantial (Zwanziger et al., 2000).
Institutional efforts to reduce private cross-subsidy can result in the transfer of the burden of uncompensated care from private hospitals to public institutions, which has been facilitated by the increasingly competitive market for hospital services and managed care contracting (Morrisey, 1996). As discussed earlier in this chapter, in some urban areas there is evidence that uninsured patients are being even more concentrated at safety-net facilities and that, as a result, there is less opportunity for private cross-subsidy of their care. The closing or ownership conversion to private status of public hospitals, a topic to be taken up in Chapter 3, can effect a reverse transfer, from public to private institutions, depending on local public financing arrangements.
Efforts to increase, decrease, or maintain private cross-subsidies may have a particular impact in rural areas. The smaller the provider, the less ability it has to cross-subsidize. Coburn (2002) argues that physicians in private practice are able to provide the 20 to 40 percent of uncompensated care in rural communities that they do because they are supported or subsidized by their community’s hospital. For employers in rural areas, the importance of cross-subsidy is a function of scale. It is a greater burden in small towns, where there are fewer employers across whom to spread the financial burden when it occurs in the form of higher costs for health care and health insurance premiums. As a result, there is a competitive disadvantage that accrues to employers who offer more generous or greater subsidies of their employment-based coverage (Morrisey, 1994). A hospital’s ability to cross-subsidize uncompensated care costs is affected by the percentage of the revenue base to which uncompensated expenses may be shifted. Rural hospitals tend to have a smaller-than-average private payer revenue base because Medicare constitutes a higher-than-average proportion of their payer mix (MedPAC, 2001). Similarly, hospitals that disproportionately serve Medicaid and uninsured patients by definition have a smaller private payer base that could potentially cross-subsidize the care provided to uninsured patients.
RESEARCH QUESTIONS
2.1 Local Patterns of Unmet Need and Utilization by Uninsured Persons
What are the unmet needs for care of uninsured persons and families?
Do they differ geographically both within and among states?
Basic to almost all the proposed research in this chapter is the need for reliable and current local estimates of uninsured rates and measures of the dispersion or concentration of uninsured persons within local health services markets and among the providers within a market. Until the late 1990s most estimates of uninsured rates were available only at the national, state, or major metropolitan statistical area (MSA) level, most notably through the U.S. Census Bureau’s March Current
Population Survey (CPS).14 In recent years, the Health Resources and Services Administration’s State Planning Grant program, together with the State Health Access Data Assistance Center (SHADAC), has facilitated the creation of uninsured rate surveys at the county or regional level within states, although these estimates tend not to be comparable across surveys. Enhanced data collection and coordination of existing surveys are needed, as well as the development of new methods to allow generation of more precise and reliable local uninsured rates and for the comparison of these estimated rates across jurisdictions.
A local uninsured rate can be the basis for estimating the unmet need or health services utilization of uninsured persons, but more direct measures are preferable. Programs to provide and pay for uninsured care are often stretched to their resource limits, with existing dollars outstripped by the perceived health needs of this population (Lewin and Altman, 2000; Felt-Lisk et al., 2001; IOM, forthcoming 2003). Evaluative research is needed to understand how uninsurance at a local level influences the organization and delivery of health care. How have communities that have been substantially effective in meeting the needs for health care of uninsured and other underserved populations proceeded, and what financing and services strategies have they employed?
2.2 Public Subsidy of Health Services Delivered to Uninsured Persons
What are the sources of public support for care to uninsured persons?
How much does each source contribute and how efficiently are the funds allocated?
The Committee relies on Hadley and Holahan (2003) for a working set of rough estimates about the extent of public subsidy. More complete and consistent documentation of existing federal, state, and local supports for the provision of care to uninsured persons is needed. The levels of such payments to hospitals alone, for example, are substantial and may even be adequate in total to cover the costs of uncompensated hospital care for those completely without health insurance (Hadley and Holohan, 2003). However, more research is needed to pinpoint administrative barriers and inefficiencies in the allocation of funds that result in inadequate or poorly targeted subsidies for the care of uninsured persons. For example, the formulas used to calculate Medicare and Medicaid DSH payment rates do not take the number of uninsured patients into account. In addition, it is difficult if not impossible to compare the relative amounts spent by states through the Medicaid DSH program because states use a variety of methods to generate their match (e.g., tax revenues, intergovernmental transfers from public hospitals) and report different types of data.
|
14 |
Appendix B in the Committee’s first report, Coverage Matters, reviews the major surveys that give estimates of uninsured rates (IOM, 2001a). |
2.3 Private Subsidy of Care Delivered to Uninsured Persons
To what extent does uncompensated care by doctors, hospitals, and other entities support care for uninsured persons? To what degree do private cross-subsidies support the care of uninsured persons?
It is widely assumed that private payers (e.g., employers, insurers) and private sector health care providers (e.g., nonprofit hospitals, physician practices) cross-subsidize the costs of care for uninsured patients. However, the size of this subsidy is difficult to estimate and the mechanisms through which this uncompensated care is subsidized are complex and not explicitly addressed or documented in the research literature. To the extent that private cross-subsidies occur, what are the implications for health care costs, for local businesses and employers who offer employment-based coverage, and for economic activity in the community?
The literature on hospital cost-shifting presents a useful approach to proposed research on private cross-subsidy. One way to gauge the extent of cross-subsidy, for example, is depicted in Figure 2.1, which compares the contributions of uncompensated care, Medicare margins, and private payer surpluses to hospitals’ total margins over time. A longitudinal analysis of changes in payment-to-cost ratios or prices for each payer to an individual provider, correlated with changes in the provider’s total margin and in the cost of unreimbursed care provided to uninsured persons, would yield more precise information about the amount and sources of private subsidy (Dobson, 2002; Morrissey, 2002). Both quantitative and qualitative studies would likely be needed to tease out the extent of private cross-subsidy, with much regional and market variation related to the market position of both insurers and health care providers (e.g., ability to negotiate discounted charges, anticipated revenue from a hospital’s patient case mix, the amount of hospital revenues across which an uncompensated care burden could be spread).
SUMMARY
As one historian of health care financing in twentieth-century America has observed, hospitals have proven to be quite efficient in their adaptive responses to changed fiscal incentives but not nearly as efficient in meeting changing public needs for health care (Stevens, 1989). The growth of insurance-based means for financing care, the federal government’s approach to shaping health policy through payment policies, increasing price competition in the market for health services, and erosion of the cross-subsidies afforded by private payer reimbursements for care have meant that persons who lack health coverage are less able than insured persons to gain access to affordable care and to be able to pay for the care that they receive. As a result, health care providers who treat uninsured persons are likely to
accumulate uncompensated costs that may impair their ability to continue delivering care.
Governments, health care practitioners and institutions, philanthropies, and private payers all play a part in serving or paying for the care of uninsured Americans. The implicit subsidies are considerable, and their target efficiency and adequacy are difficult to judge. Ultimately, there is no comprehensive or coordinated approach to caring for uninsured persons. The financial implication of this reality—namely, uncompensated care—sets into motion a number of potential community effects of uninsurance.
The growth over the past several decades in the importance of health finance in the U.S. economy and government finances magnifies market distortions and inequities and inefficiencies in the allocation of public resources. Hospital uncompensated care was much easier for both governments and the institutions themselves to address when Medicaid and Medicare together accounted for much less of the national spending on hospital care than the 48 percent that they currently do (Cowan et al., 2001). The DSH payments under those two federal programs, although substantial and essential supports for institutions that are major providers of care to the uninsured, are blunt tools.
Mainstream health services delivery and the provision of care to and financing of care for uninsured Americans are fundamentally interrelated. Although these two components of the health care enterprise are often treated as separate entities with distinct constituencies governed by separate policies, they cannot be understood in isolation from one another. This is especially evident when tracing the funding streams that pay for the care the uninsured receive and the impacts on health care institutions and providers locally when the proportion of uninsured residents is relatively high or increasing. Despite the relatively stable proportion of the national population without health insurance over the past two decades, major changes in the financing and organization of health care services in both the public and the private sectors have changed the significance and impact of uninsured populations for health care providers and governments at all levels.
The next three chapters examine community health care services and access, social and economic institutions, and population health in conjunction with local uninsurance.
















































