4
The Economics of Resistance
OVERVIEW
Microbes that are resistant to therapeutic agents arise and proliferate at a rate that is far faster than is socially desirable because individuals, as well as governments and institutions, make choices that fail to recognize the cost that use of such agents (including their overuse and misuse) exacts on society. Cost and choice, of course, are the coins of the realm in economics. The focus of this session of the workshop was to examine how economics can help in developing innovative responses to the problem of antimicrobial resistance. Participants identified several important roles for economic analysis.
First, economics can provide purely descriptive analysis, quantifying the phenomena which are of interest, such as national expenditure on health care and how much antimicrobial resistance costs individual hospitals. This is the most basic level of analysis, but nonetheless important in providing foundational information on which further analysis is based, as well as providing information on the consequence of choices that have already been made.
In this regard, various economic analyses indicate that antimicrobial resistance greatly increases the cost of health care, in a variety of ways. For example, treating individuals with alternative drugs is nearly always much more expensive than conventional treatment with generic drugs. Also, patients infected with resistant microorganisms may require extra investigations and treatment, and for some patients a cascade of drugs will be tried
before one is successful in eradicating the infection. The end result is longer and more expensive hospital stays. For the United States as a whole, the American Society for Microbiology estimated in 1995 that health care costs associated with treatment of resistant infections amounted to more than $4 billion annually. And this figure significantly underestimates the actual cost of resistance, since it includes only direct health care costs and excludes an array of other costs, such as lost lives and lost workdays. Moreover, these costs are expected to increase considerably given increasing rates of antimicrobial resistance.
In addition, economics can be used predictively to identify how changes in the health care system might affect the use of antimicrobial agents—and hence the emergence and spread of antimicrobial resistance. These analyses make use of descriptive data, together with conceptual models, to guide choices that are yet to be made.
Economics also can prove vital in developing specific strategies and policies to contain antimicrobial resistance. Key among current available strategies are regulation; charges (taxes) on the use of antimicrobials; and rights to trade (permits, licenses, or marketable property rights), which often are used in an attempt to combine the ease of regulation with the flexibility and efficiency of charges. To fill this role, however, the single biggest problem is lack of a comprehensive economic model for fully assessing the impact of antimicrobial resistance, as well as the cost and effectiveness of interventions to reduce the emergence and transmission of such resistance. Efforts are now under way to develop such a model. And while scientific and epidemiological development is vital, additional support also is required to advance understanding of the economics of resistance.
WHAT DOES ECONOMICS HAVE TO OFFER IN THE WAR AGAINST ANTIMICROBIAL RESISTANCE?
Richard D. Smith, M.Sc.
School of Medicine, Health Policy & Practice University of East Anglia, Norwich, United Kingdom
“We may look back at the antibiotic era as just a passing phase in the history of medicine, an era when a great natural resource was squandered, and the bugs proved smarter than the scientists” (Cannon, 1995).
We begin the 21st century in a position of retreat against infectious disease, with the latter half of the 20th century in danger of being consigned to the history books as the time when a valuable new resource in this battle was both discovered and squandered.
“Superbugs,” micro-organisms that have become resistant to the major
therapies used to treat them, present a major threat to current and future medical advances (Neu, 1992; Murray, 1994; Tomasz, 1994). Resistant bacteria causing global concern include multi-drug-resistant Mycobacte rium tuberculosis, penicillin-resistant Streptococcus pneumoniae, and methicillin-resistant Staphylococcus aureus (Neu, 1992; Tomasz, 1994; Cox et al., 1995). The effects of antimicrobial resistance (AMR) are documented in developed and developing nations alike, although arguably with greater potential for harm in the developing world, where many of the second- and third-line therapies for drug-resistant infections are unavailable, and many of the narrow spectrum antimicrobials available in the developed world are not affordable (Fasehun, 1999; Smith, 1999). However, despite increasing awareness, across both the medical (Levy, 2002) and lay communities (Cannon, 1995), of the rising prevalence of resistance, there is little evidence that the use of antimicrobials is changing.
The potential impact of this increasing antimicrobial resistance on health care expenditure and population morbidity and mortality is causing professional, government, and public concern (House of Lords Select Committee on Science and Technology, 1998; Standing Medical Advisory Committee Sub-Group on Antimicrobial Resistance, 1998; American Society for Microbiology, 1995; OTA, 1995; World Health Organization [WHO], 2001). Indeed, the United States considers the potentially destabilizing economic and social effects of antimicrobial resistance, as well as its potential in biological warfare, sufficient to classify antimicrobial resistance as a national security risk (Kaldec et al., 1997; CIA, 2000; World Bank, 2001).
The Discipline of Economics “in a Nutshell”
Economics is based on the fundamental premise that our resources (goods, services, time, raw materials, and all else that we use to make something else) are limited compared to what we want from them (which is virtually unlimited). On a personal level this means that one’s time and wealth are limited compared to what we would like to be able to do. Nationally, this also applies, with national resources limited compared to what they could be used for. At all levels this means that choices have to be made. As individuals we have to choose whether to have a new car or holiday, or spend time working or playing golf. Nationally, we have to decide whether to have more health care, more education, more defense, or more consumer items. Economics then is fundamentally the study of choice.
However, there are other disciplines that study choice, such as psychology and sociology, so what makes economics special? The “angle” of economics is that choice is studied from the perspective of efficiency. That is, that economists study choices that can be (have been) made with a view to assessing whether the most benefit will be (was) gained from the resources
used. What economics is fundamentally about then is quite simple: it is about assessing ways and means by which our choices, as individuals and nations, will lead to that allocation of resources amongst alternatives that will yield the most overall benefit. There are broader concerns than this of course, such as the equity of this resource allocation, but for the purposes of this paper, this simple definition provides the most important background to discussion.
Another important element of background to economics generally is the empirical manner in which economists approach the study of choice. Here there are three important categories of empirical activity, each of which will be considered in the paper with respect to the economic analysis of AMR.
First, economics may provide purely “descriptive” analysis, quantifying the phenomena which are of interest, such as national expenditure on health care, how much AMR costs a hospital, and so on. This is the most basic level of analysis, but nonetheless an important one in providing foundational information on which further analysis is based, as well as providing information on the consequence of choices that have already been made.
Second, economics may be used “predictively,” identifying the impact of a change. For example, if health care expenditure rises, what will happen to physician income? How will user-charges for pharmaceuticals affect their use? These analyses make use of descriptive data, together with conceptual models, to guide choices that are yet to be made.
Third, economics may be used “evaluatively,” suggesting whether one situation is “preferable,” more efficient, to another; for example, whether national health insurance is better than private health insurance, competition between health care suppliers is more efficient or prevention is better than cure. Here, prediction is taken further to provide an assessment of what should be done if efficiency is to be maximized.
Economic Conceptualization of AMR
The use of antimicrobials can result in the unwanted “side effect” of the development of resistance. Economists conceptualize this side effect as a negative “externality” resulting from the consumption of antimicrobials. A negative externality refers to a situation where a cost is imposed on others not directly involved in the decision to produce or consume the commodity causing the pollution. A classic example of a negative externality is pollution, such as acid rain.
Antimicrobial resistance is an externality associated with the consumption of antimicrobials (as part of the production of health), and is a negative
externality because it has adverse consequences for society as a whole (Phelps, 1989).
The form of the externality may be specified as:
where ![]() is the extent of the (negative) externality in time t, At is the quantity of antimicrobials consumed in time t, and
is the extent of the (negative) externality in time t, At is the quantity of antimicrobials consumed in time t, and ![]() is a vector of other factors (e.g., background level of resistance, population mobility, and population density) which may determine the level of resistance in a community (Coast et al., 1998).
is a vector of other factors (e.g., background level of resistance, population mobility, and population density) which may determine the level of resistance in a community (Coast et al., 1998).
However, antimicrobials also have a positive impact, not just upon treated individuals, but also upon those individuals who would, in the absence of antimicrobials, have been infected by the treated individual. Thus, benefits from consumption include an improved outcome for the patient, reduced transmission of pathogens which would lead to disease in others, and a reduction in morbidity associated with sub-clinical infections which would otherwise be “accidentally” treated. The latter two benefits comprise a positive externality which results from taking antimicrobials. The format of this externality is:
where ![]() is the positive externality associated with reduced transmission and treatment of sub-clinical infections during time t, At is the quantity of antimicrobials used in time t,
is the positive externality associated with reduced transmission and treatment of sub-clinical infections during time t, At is the quantity of antimicrobials used in time t, ![]() (as before) is the extent of resistance in time t, and
(as before) is the extent of resistance in time t, and ![]() is a vector of exogenous factors which might influence the positive externality. It is important to note the presence of
is a vector of exogenous factors which might influence the positive externality. It is important to note the presence of ![]() in this equation. This represents the fact that, as time progresses and resistance increases, the positive externality associated with reduced transmission may in itself be reduced.
in this equation. This represents the fact that, as time progresses and resistance increases, the positive externality associated with reduced transmission may in itself be reduced.
Thus, the net benefit from antimicrobial usage in any period would therefore be:
where ![]() is the net benefit resulting from antimicrobial usage in time t,
is the net benefit resulting from antimicrobial usage in time t, ![]() ,
, ![]() , At, and
, At, and ![]() are defined as previously, Bt is the direct benefit to the patient of taking the antimicrobial, Ct is the drug plus administration cost, St is the cost associated with side effects, and Dt represents problems caused by difficulties in diagnosis.
are defined as previously, Bt is the direct benefit to the patient of taking the antimicrobial, Ct is the drug plus administration cost, St is the cost associated with side effects, and Dt represents problems caused by difficulties in diagnosis.
There are several important implications arising from this con
ceptualization. First, the balance between costs and benefits, and negative and positive externalities, means that we are not seeking the eradication of AMR, but rather the containment of AMR to an “optimal” level. Important here is the balance struck between securing the best interests of the individual patient presenting with an infection, versus the global need for sustainable antimicrobial use to ensure that benefits of these drugs are available for others.
Second is the importance of this optimization over time. The negative externality of AMR occurs in time t + 1 as a result of the consumption of antimicrobials in time t. This time period may vary from days, to months, to years, to decades. However, it is undoubtedly the case that many of the major effects of resistance are likely to be incurred by future generations, and policy decisions will therefore have to weigh current costs and benefits against those occurring to future generations.
Third, there is the obvious implication that one needs to assess all the relevant costs and benefits (direct and externality) of antimicrobial use, and thus strategies to contain AMR, as well as other strategies not primarily aimed at AMR, but which will impact upon AMR. For example, changes in user charges or reimbursement systems may impact levels of AMR.
Applications of Economics to AMR
There are several areas where economics may be, or have been, applied in the context of AMR. Most significantly, these include:
-
Assessment of the cost of AMR, by country, institution (e.g., hospital), and disease;
-
Assessment of the cost-effectiveness of strategies to contain AMR, including new and existing antimicrobial therapies;
-
Assessment of the value of the (cost and) benefit of AMR containment over time; and
-
Development of specific economic strategies/policies to contain AMR.
Work in these areas is summarized briefly here.
Assessment of the Cost of AMR
It is relatively easy to point to some of the likely consequences of AMR (Smith et al., 1996). Patients infected with a resistant microorganism are less likely than those infected with a sensitive microorganism to recover from infection with the first antimicrobial used in treatment. Patients with
resistant microorganisms may require extra investigations and treatment (usually more expensive), and for some patients a cascade of antimicrobial drugs will be tried before one is successful in eradicating the infection. This may result in longer hospital stays and longer periods of time away from work. Most seriously, of course, is that AMR will result in a greater likelihood of premature death. However, there has been little empirical research in this area, and estimates of the cost impact of AMR are therefore few and, inevitably, relatively crude.
For example, estimates of the cost of AMR by country have been largely limited to work in the United States. The American Society for Microbiology (1995) have estimated the annual health care costs associated with treatment of resistant infections in the United States at over $4 billion (equivalent to approximately 0.5 percent of U.S. health care costs). More recent estimates suggest that, for the United States, the continued rise in use of antimicrobials has resulted in current costs of more than $7 billion annually, with up to $4 billion used for the treatment of nosocomial infections due to AMR bacteria (John and Fishman, 1997).
Estimates by institution have also been few. For example, in the United Kingdom in 1989 a five-week outbreak of MRSA was estimated to have cost £ 12,935 (Mehtar et al., 1989), excluding the costs of additional or lost bed days. In 1995, the cost of containing an MRSA outbreak in a district general hospital was estimated to be greater than £ 400,000 (Cox et al., 1995).
Estimates by disease are similarly limited. For example, recent work in the area of multi-drug-resistant tuberculosis has suggested that resistance effectively doubles the cost of standard treatment for sensitive tuberculosis, from around $13,000 to $30,000 (Wilton et al., 2001).
However, it is likely that these costs are an underestimate of the total current costs of resistance (as they include only health care costs) and that such costs will increase considerably in the future. Further, although AMR has a significant impact on current health care expenditure and health of the population, it is the potential long-term impact that resistance, and, specifically, failure to tackle resistance, will have which is arguably of greatest concern.
Assessment of the Cost-Effectiveness of Strategies to Contain AMR
There are a variety of strategies which may address resistance, that may be categorized according to two dimensions.
First, in terms of their focus—whether the strategy aims to decrease the transmission of resistance among organisms, individuals, and the environment (e.g., hand-washing, restriction on travel) or whether it aims to pre
vent or reduce the emergence of resistance, largely focused upon the appropriate use, and reduction in the level of use, of antimicrobials (e.g., cycling of drugs in the hospital).
Second, in terms of the level at which the strategy is focused—whether the strategy focuses on the “micro” level of an individual institution, for example, a “closed” environment such as a hospital, or whether it is a “macro” strategy focused at the broader community level.
A recent systematic literature review of studies assessing the cost and/or effectiveness of interventions specifically aimed at reducing the emergence and transmission of AMR, found only 127 studies of moderate to good quality, of which 68 were effectiveness studies, 10 economic evaluations, 2 cost studies, and 2 modeling studies (Smith et al., 2001; Wilton et al., 2002). The main conclusions of this study were that most studies:
-
are of poor methodological quality (i.e., at high risk of bias), which means that we cannot be confident of their results;
-
are from developed nations (principally the United States), although this could be a function of the search strategy which was restricted to papers published in English, or of research funding;
-
do not measure the impact on AMR in terms of costs, although this is not surprising as effectiveness studies always outnumber cost or cost-effectiveness studies;
-
are micro (institution) not macro (community) strategies, which may be because the strategy is more “contained” and the costs and effects are more observable, compared with the more diffuse impacts of the macro interventions focused on the community, and also because often hospitals and other institutions have financial incentives to try to control resistance; and
-
are concerned with transmission not emergence of AMR.
Assessment of the Value of the (Cost and) Benefit of AMR Containment over Time
The critical problem identified above is that although (macro) policies to contain emergence are likely to be optimal in the long term, (micro) policies to contain transmission are more likely to be rigorously evaluated. This is due to the problems caused by attempting to assess the costs and benefits of something which occurs now (i.e., reduced transmission has immediate and obvious effects) versus something which will occur in the future (i.e., reduced emergence has effects that will not be seen until sometime hence). This time-lag with containing emergence causes two main problems: (i) uncertainty with respect to effects occurring in the future; and (ii) discounting of costs and benefits in the future may result in such benefits
being given lower weight than equivalent benefits now. This means that there is a potential bias both against evaluating strategies aimed at emergence and in the cost-effectiveness result (Coast et al., 1996; Coast et al., 2002).
The issue of uncertainty can be addressed through the use of modeling, but really needs improved clinical and epidemiological evidence for the relevant relationships over time. The issue of discounting and time preference might be dealt with either through use of a zero discount rate, or perhaps through direct assessment of “option value.” That is, people may be willing to trade increases in morbidity, inconvenience, and cost incurred through reducing consumption of antimicrobials now in return for the option to consume them in the future. That is, maintain the effectiveness of treatment in case it is required in the future, at the expense of reduced use now, even if they do not in practice use them. Thus there may be a value attached to maintaining the option to benefit from antimicrobials in the future which would not be captured by valuations of the health impacts of different policies alone.
Development of Specific Economic Strategies/Policies to Contain AMR
The conceptualization of AMR as a negative externality allows the consideration of economic strategies (i.e., strategies designed to change incentive structures) developed to deal with similar instances of negative externalities in other areas. Key among these strategies are regulation, charges, and rights to trade. Each of these has been outlined in detail elsewhere (Coast et al., 1998; Smith and Coast, 1998), but a summary is provided below.
Regulation is the most obvious means of controlling the production of a negative externality, through control of the quantity produced (Turner et al., 1994; Hodge, 1995). However, although it is relatively easy to introduce and administer, it is less efficient than policies relying on price-based incentives, with evidence that regulation imposes considerable excess costs over these other policies (Tietenberg, 1990). In terms of AMR, the focus would be either on limiting the use of antimicrobials for particular types of patients or, alternatively, limiting the total supply of antimicrobials available to doctors for prescription to their patients. Issues arising in this would include heterogeneity of patients, enforcement (e.g., ensuring physicians were following the explicit rules about who should, and who should not, receive antimicrobial treatment), and cost of enforcement.
Charges, or taxes, on use of antimicrobials should, on the basis of economic theory, provide an efficient means of containing AMR, whereby the charge equates to the marginal external cost imposed. However, in practice, this is difficult to achieve because government would need infor
mation about this marginal external cost (Pearce and Turner, 1990). Application of charges on the basis of levels of AMR would almost certainly be impractical, and would be more likely to be levied on the consumption of antimicrobials, as a proxy for the generation of AMR. These products are easily identifiable, and the application of a charge relating to each antimicrobial would be relatively simple. The key issue then is who will pay this charge—the patient, the prescriber, or the manufacturer? In each case there would be implications for the effectiveness of the policy and equity of impact of any system of charges.
Rights to trade (permits, licenses, or marketable property rights) are used to try to combine the ease of regulation and flexibility and efficiency of charges. Here the total quantity is limited, but each consumer/producer may utilize any quantity up to that limit through the trade of that limited quantity. Thus, it uses regulation to set the overall level, and then the price mechanism to distribute that total most efficiently. This is a common method in the environment, such as for trading sulfur dioxide pollution (Winebrake et al., 1995) or fishery quotas (Turner et al., 1994), and has been proposed in the area of AMR (Smith and Coast, 1998).
What Does Economics Have to Offer in the War Against AMR?
As alluded to in this short paper, economics as a discipline has much to offer under three broad classifications.
Conceptualization of Problem
The economic conceptualization of AMR as a negative externality was highlighted. By concentrating upon efficiency—maximizing benefits for given resources—economists seek to determine the optimal rate at which resistance should be allowed to develop, balancing the costs and benefits of antimicrobial usage over time. This approach stresses, first, the importance of optimization and balance in the use of antimicrobial products, and thus in the level of AMR which exists, rather than eradication of AMR, and, second, the importance of this optimization and balance being one to be struck over time: that the balance is really against the (costs and benefits of) use of antimicrobial treatments now and their continued availability for use in the future.
Informing the policy options for the containment of AMR will thus require information relevant to these issues. The assessment of costs and benefits is discussed below, but the assessment of balance over time requires information about the development of new and/or alternative products to those currently being used, which is largely outside the sphere of economics, but also the perceptions of the public on their willingness to
trade current use and future availability. This is important, as it is the public who will be asked to forego some beneficial treatment if we are to constrain use of these treatments. There is much work to be done, therefore, on the assessment of “time preference” and discount rates used in economic analysis.
Technical Analysis
Economics can also assist with the development of an explicit basis for policy, through not only assessment of time preference rates, but also assessment of costs and benefits, and use of modeling to analyze the impact of a variety of policy options across various time periods.
A comprehensive economic model enabling assessment of the potential cost and impact of AMR containment strategies, and interventions upon antimicrobial use and AMR, is vital to the long-term management of antimicrobial use in two ways. First, it will enable estimates of the costs of resistance to be incorporated into economic evaluations of new antimicrobials, or other interventions, affecting AMR. In the absence of such information, current economic evaluations are mis-specifying the true cost of antimicrobial usage. Second, a model assessing the optimal use of antimicrobial drugs is essential for evaluating viable policy alternatives and prioritizing resource allocation between them.
However, the single biggest problem faced in the assessment of the economic impact of AMR, and the assessment of the cost and effectiveness of interventions to reduce the emergence and transmission of AMR, is the lack of a coherent and comprehensive economic model of AMR, although, together with colleagues, the author is currently seeking to develop one.
Strategies
Medical literature and research tends to focus on physical methods of reducing the transmission or emergence of resistance, such as through improved hygiene (for example, hand washing) or the cycling of antimicrobial treatments. Within economics, the focus tends to be upon developing policy responses which “internalize” the externality of resistance. In relation to antimicrobial resistance, this would mean, for example, providing incentives for consumers, prescribers, and/or producers to take account of the possible “externality” costs of the consumption of antimicrobials to society. Although work in this area has, to date, been relatively limited, there has been some discussion of policy instruments such as taxation and transferable permit markets, and a more extensive assessment of how such a permits system might operate in the United Kingdom (Smith and Coast, 1998).
A further consideration is the containment of AMR, on a global level, and the increasing interconnectedness of AMR meaning that no one country is likely to provide an effective policy response without considering the actions of neighboring countries. This has been considered from an economics perspective both within the “WHO Global Strategy for the Containment of AMR,” and more specifically with respect to the concept of “Global Public Goods” for health (Smith and Coast, 2001; 2002; in press).
Conclusion
Although further developments are undoubtedly required, economics can assist in clarifying the basis for policy development, can identify and develop policy options and, through the assessment of the cost and benefits of alternative options, can help to recognize optimal policy solutions. Although scientific and epidemiological development is vital, support is also required for development of the economics of resistance.
ECONOMIC INSTRUMENTS FOR THE CONTROL OF ANTIMICROBIAL RESISTANCE
William Jack, D.Phil.
Department of Economics, Georgetown University, Washington, DC
The mechanisms that govern the evolution of resistance of pathogens are subtle and complicated, depending on the individual- and population-level characteristics of the organisms and the interventions. These mechanisms can be studied, understood, and hopefully improved through scientific analysis. There is widespread agreement however, that a further determinant of the evolution of resistance is the behavior of the human host. Microeconomics—the study of the way people choose amongst alternatives—can provide a vehicle for understanding the behavior of people in disease environments, and hopefully (again) lead to suitable interventions to help control resistance.
A first question that can be posed is what outcome, in terms of drug resistance, is desired in a particular circumstance. Using economic language, it is possible to think of an existing drug as a capital asset—one that provides a flow of services over time, like a machine. Machines tend to run down as they are used more, and if they are used unwisely. Of course, one way of keeping a machine in good condition is to leave it unused. The extent to which one would want to allow depreciation of the physical asset depends crucially on how easy it is to replace it, or to innovate and make a better one.
Similarly, drugs can become less effective as they are used more, and if they are used unwisely. And drug resistance can be halted by discontinuing all drug therapy. Where to make the trade-off depends, as with a capital asset, on how easy it is to replace the drug, and on how likely a more effective intervention is to become available.
This qualitative similarity between physical equipment and drugs can help rationalize public interventions aimed at affecting drug use. The underlying reason that there is a potential role for government aimed at controlling drug use is that, while we expect individuals to have appropriate incentives to “wisely use” their physical assets, there are reasons to expect them to (rationally) overuse drug therapies. The simple reason is that the costs of overuse by one person are borne by all other individuals who might one day need the drug, while the costs of running a machine into the ground are borne primarily by the owner of that machine. Another way of saying this is that an effective drug has some of the characteristics of what economists call a public good, incentives for the maintenance of which might be attenuated at the individual level.
Societies respond to public good problems by sometimes agreeing to limit the use of a resource. Thus, numerous international agreements concerning, for example, fisheries, aim to limit the amount each nation will exploit a reserve, given that individually rational behavior would lead to depletion that is too rapid. Economists also like to rely on the price mechanism (as opposed to quotas) to implement such contractions in use, for example by levying a tax on use. In international settings, deciding which body collects (and keeps) the revenue from such taxes is politically dicey, and quotas are often employed instead.1
When dealing with a large population of individuals using drugs, the price mechanism seems to have important advantages over quotas. For one thing, many individuals will not need to use the drug, so allocating a fixed number of units to them, and the same number to an individual in dire need, is inefficient. On the other hand, trying to pick the right number to allocate to each person as a function of his/her health status could quickly become hopelessly complicated. “Getting the price right” is a potentially more fruitful approach.
That, at least, is the theory. The problem with this story is that it assumes that resistance is caused simply by overuse. However, there are two margins on which decisions are made by individuals (and their doctors) regarding drug use: the number of treatments (e.g., the number of prescriptions filled), and the extent to which the treatment is completed. In richer
countries, drug resistance is blamed in part on excessive prescribing behavior, but in poorer parts of the world, incomplete treatment and/or inappropriate self-medication with readily available, cheap, but often ineffective generic old-line therapies is often identified as the culprit.
Decisions on both of these margins could be controlled if it were possible to charge a certain price for a prescription, and a separate price for use of the drug. Other things being equal, we would want to set the first price on the high side, so as to reduce the number of prescriptions, and the second price on the low side, so as to encourage completion of the course. However, if only a single price instrument is available (e.g., the prescription charge), then raising it will tend to reduce both the number of prescriptions (which is good for controlling use and resistance), and the likelihood that an individual will complete a course (which is bad for controlling resistance). The reason that increasing the prescription price may reduce completion rates is that individuals who expect to contract the illness again will have an incentive to save some of the medication as a contingency against such an event. The higher the price of getting a new prescription in the future, the greater this incentive will be.
The net effect of a price increase on resistance is thus ambiguous. Indeed, it is possible that reducing the prescription charge could reduce the rate at which the drug became ineffective. If the two effects happen to offset each other exactly, the optimum tax would be zero. That is, it might be best to leave the price unchanged.
The impact of prescription charges on completion rates is likely to be more prevalent in environments where the likelihood of reinfection is higher, and for drugs that are more easily storable. One interesting implication of this is that it might be desirable to design therapies that depreciate quickly once a course is begun, thus lowering the value of saving some of the medication for future use. The trouble with such a policy is that it might also reduce the shelf-life of the drug before treatment, thus making it difficult for clinics and hospitals to manage their pharmaceutical stocks. These concerns would seem to be particularly relevant in developing countries, where, also, the chance of reinfection is typically higher.
Instead of relying on price instruments alone, WHO has addressed the problem of incomplete treatment of tuberculosis by developing and advocating the use of the DOTS (directly observed treatment [short course]) protocol. Individuals are induced to complete the course of medication not by being charged a low price per pill (conditional on obtaining a prescription), but by being directly monitored and encouraged by an outside agent. This kind of intervention is expensive, however, in terms of the labor costs incurred by the monitoring agent.
Finally, the issue of equity must be addressed in the context of contemplating price increases. To a first approximation, in order to correct a
market imperfection associated with overuse, the same price increase should apply to all individuals, simply because it is aggregate use that affects resistance and needs to be controlled, not use by say the rich or the poor.2 Policies that relate charges to income exist in other cases however: for example, in some countries (e.g., Sweden), speeding tickets, which presumably are meant to reduce the amount of speeding, are sometimes proportional to an individual’s income.3
This prescription of uniform pricing is appropriate either if the distribution of income and well-being in society is of little concern to policy makers, or if that distribution can be improved through direct income transfers and other poverty alleviation programs. The institutional capacity to implement such transfers and programs in poor countries may be sufficiently weak however, that exempting the poor from higher prices may be attractive. Of course, such an exemption policy in itself will require a level of institutional capacity and targeting capability that may be beyond the reach of some countries. Applying different taxes to drug sales in urban and rural areas might represent a very blunt instrument to effect an appropriate targeting policy, but the possibility of resale and trade between rural and urban centers would weaken the implementability of such a scheme.
ECONOMIC RESPONSES TO THE PROBLEM OF DRUG RESISTANCE
Ramanan Laxminarayan, Ph.D., M.P.H.*
Resources for the Future, Washington, DC
The increasing resistance of bacteria to antibiotics is a consequence of selection pressure placed by the use of antibiotics on susceptible organisms to the benefit of resistant organisms. Addressed as a behavioral problem, resistance is, at least in part, a consequence of missing economic incentives. Resistant bacteria arise and proliferate at a rate faster than is socially desirable because individuals fail to recognize the cost imposed by their use
or misuse of antibiotics on the rest of society. For this reason, economists are often asked what they bring to the table in terms of innovative responses to the problem of resistance. Broadly speaking, there are two fronts along which we can consider strategies to counter drug resistance, and economics can help on both. First, we can manage our existing arsenal of drugs and antibiotics carefully so as to maximize the value derived from their use by intervening on the demand side of the antibiotics market. Second, we can develop (or encourage the development of) new drugs and pesticides that could replace old products that resistance has rendered ineffective by intervening on the supply side.4
On the demand side, measures to encourage more efficient antibiotic use include both price and non-price measures. Price measures involve increasing the cost of antibiotics for patients to discourage their use. Non-price measures include patient counseling on the societal effects of antibiotic use, physician education, and so forth. These could also include measures to encourage the use of an economically efficient variety of drugs.
On the supply side, measures to address the resistance problem would include incentives that not only encourage drug firms to develop new antibiotics, but also give them a greater incentive to care about the impact of drug resistance. We discuss each of these measures in turn.
Intervening on the Demand Side
Price Measures
The most reliable axiom in economics is that as the price of any commodity goes up, the quantity of that commodity that people will consume declines, all else being equal. Therefore, if our objective is to reduce the use of antibiotics, then the most reliable way of doing so without second-guessing physicians’ decision-making is by raising the cost of using antibiotics to the patient. One solution might be to impose a tax on antibiotics. However, a tax may be undesirable for two reasons. First, a tax may not discourage antibiotic use if insurance coverage shields many patients from drug costs and physicians are relatively insensitive to these costs. Second, the burden of a tax may be disproportionately borne by poorer patients
who are less likely to have health insurance to cover the cost of antibiotic prescriptions.
A logical alternative would be to mandate an increase in the extent of cost-sharing for antibiotics. This could be accomplished by increasing co-payments for antibiotic prescriptions for certain conditions where a regulatory or scientific body believes that antibiotics are overprescribed (such as for the treatment of ear infections).5 Such a measure would not hurt the majority of economically disadvantaged patients who currently lack prescription drug coverage, but would effectively tax antibiotic use. Figure 4-1 shows how an increase in the cost-share borne by patients would decrease the quantity of antibiotics consumed from Q1 to Q2.
Empirical evidence on the effect of cost-sharing on antibiotic use is limited but consistent. For instance, a large randomized study conducted in 1985 showed that people who received free medical care used 85 percent more antibiotics than those required to pay for at least some portion of their medical care (Foxman et al., 1987). However, the same study found that cost-sharing was likely to equally reduce both appropriate as well as inappropriate antibiotic use.
To be sure, a price-based policy intervention is a blunt instrument, and may, in some instances, discourage the use of antibiotics even when their use is justified. However, targeted cost-sharing efforts aimed at certain diagnoses may be preferable to an across-the-board increase in mandatory cost-sharing for all antibiotics. Increased cost-sharing for antibiotics, or other methods of raising the cost of antibiotics to the patient may not be popular. However, short of direct case-by-case oversight of antibiotic prescriptions, there are few other alternative strategies that can effectively lower antibiotic use. Policy makers in the antibiotic resistance arena would do well to learn from the use of tobacco taxes in the United States. The tremendous success of higher tobacco taxes on lowering smoking in this and other countries is self-evident.
Non-Price Measures
While price measures could be effective in lowering antibiotic use, their effectiveness may be enhanced when used in combination with non-price measures as part of an overall strategy to fight resistance. Increasing patient awareness of the drawbacks of antibiotic use and improving physician education could promote judicious antibiotic use; much has been written
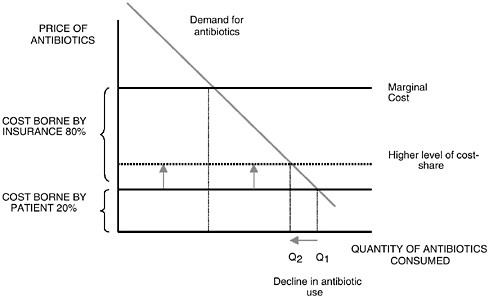
FIGURE 4-1 Increasing share of costs borne by patients decreases the quantity of antibiotics consumed from Q1 to Q2.
about these interventions and therefore these topics are not covered in this paper. Non-price measures could also include other innovative strategies, such as increasing treatment heterogeneity, that have received relatively less attention from the public health and medical communities. Treatment heterogeneity refers to the policy option of treating different patients afflicted with the same disease with antibiotics that have unrelated modes of action.
The rationale for treatment heterogeneity follows from the notion that the likelihood that bacteria will develop resistance to any single antibiotic can be reduced by treating fewer patients with that antibiotic. This is achieved by using a larger variety of antibiotics (Laxminarayan and Weitzman, 2002). Variety reduces the selection pressure for resistance to evolve to any single drug class. However, one is struck by the degree of homogeneity in antibiotic treatment, a fact that is attributable to industry concentration, uniform treatment guidelines, and to some extent, emphasis on providing the safest, and most cost-effective treatment to all patients. For instance, in 1997, nearly 60 percent of all cases of acute otitis media in the United States were treated with amoxicillin (Laxminarayan et al., 1998).6 In fact, an earlier study found that in 1992, amoxicillin accounted
for 39 percent of all antibiotics prescribed in the United States, and the five most commonly used antibiotics accounted for 80 percent of all antibiotics prescribed (McCaig and Hughes, 1995). The degree of treatment uniformity is even more striking in infectious disease treatment in the developing world. In most African countries, chloroquine has been the most commonly used drug to treat malaria for more than five decades.
To the extent that most patients in a region or country are treated with the same drug for a given infectious disease, the use of a single drug places excessively high selection pressure on organisms that are susceptible to that particular drug and increases the likelihood that a resistant strain will evolve and proliferate. As resistance to the recommended first-line drug builds up, that drug is replaced by an alternative that is used until resistance to this second drug also increases, and so on in succession. Therefore, the optimal solution may be to use not just a single drug throughout the population as first-line agent, but to prescribe a variety of drugs, randomized over patients, to ensure that inordinate selection pressure is not placed on any single drug, or class of drugs.
The notion that there is a single cost-effective treatment for an infectious disease fails to consider the effect of homogenous drug use on the evolution of resistance. Consequently, the standard cost-effectiveness method may lead to flawed conclusions in the case of drugs such as antibiotics and anti-malarials since it has no way of capturing the notion that using the same drug on all patients may be undesirable from a societal perspective. Encouraging treatment heterogeneity may not require any specific policy beyond issuing treatment guidelines that recognize this aspect of infectious disease treatment. There may be sufficient heterogeneity in physicians’ preferences and patients’ willingness to pay that will bring about sufficient variation in drug choice. However, treatment heterogeneity necessarily requires the availability of a variety of drugs, and this may require regulatory intervention.
Supply Side
While increasing treatment heterogeneity and lowering the demand for unnecessary antibiotics through both price and non-price measures comprise one side of the solution, the other side deals with increasing incentives for pharmaceutical firms to increase research spending on new antibiotics as well as to care about resistance to existing drugs.
The fundamental policy objective is not just to increase incentives for firms to develop and introduce any new antibiotics, but to specifically develop new products or classes of antibiotics that are significantly different from existing ones in their mechanisms of action. This minimizes the common property problem that arises when different firms make products
with similar modes of action and, consequently, no single firm has sufficient incentive to care about declining product effectiveness. If one were to use the analogy of thinking about product effectiveness as a resource, like oil for instance, then an optimal policy would encourage drug firms to search for new “wells” of effectiveness against bacteria, rather than to drill new wells to extract existing reserves, thereby competing with other producers. Given this latter criterion, standard policy solutions such as research investment tax credits, and longer-duration patents may not solve the problem of incentives.
One policy option that may address this problem is to extend patent breadth (or scope) for antibiotics as a way of encouraging innovation. To be sure, this is a more difficult policy to implement. While patent lengths can be easily extended by legislative action or administrative fiat, patent breadths are more difficult to change. Patent offices are reluctant to alter the rules that guide their decisions. However, one might argue that there are few, if any, innovations that are in need of such alterations to patent breadth. Under this proposed policy, the scope of antibiotics patents could be increased so they cover an entire class of compounds and preempt “me too” antibiotics that increase competition for the same mechanism of action. This may be a good idea for three reasons.
First, increasing patent scope gives firms an incentive to care about the evolution of resistance since the firm owning the patent would have nearly complete control over the stock of effectiveness. The common property problem arises with antibiotics because different firms sell similar antibiotics with similar modes of action, and no firm bears the full resistance cost of its production decisions. Indeed, the quantity of antibiotics sold is only one factor, albeit an important one, that influences the growth of resistance. For instance, the care that a drug firm might take in selecting the indications that an antibiotic will be marketed for can play an important role in influencing the growth in resistance. These and other strategies to reduce resistance are more likely to be employed by a firm if it has a broader patent on the antibiotic, and is likely to reap the benefits of sustained effectiveness to a greater extent.
Second, increasing breadth would dramatically increase the returns from investing in new compounds rather than just tinkering with existing compounds. The returns from new discoveries would dramatically increase since the innovator will have broad rights over the newly innovated class of antibiotics rather than just the narrow chemical entity. The third reason for increasing patent breadth is that we attain the basic objective of focusing new drug research on increasing the variety of modes of action of antibiotics. Variety has social value that is not fully compensated for in the current market for antibiotics, and increasing patent breadths would encourage variety (Ellison and Hellerstein, 1999).
There are drawbacks of broader patent scope for antibiotics that would need to be considered as well. First, increasing the allowable breadth of antibiotics patents increases the social welfare costs associated with greater imperfect competition. Second, broader patents may discourage potentially valuable innovations such as new drugs that are closely related to existing antibiotics, but which are easier to administer and have fewer side-effects. These drawbacks should be addressed by other policies where possible, and balanced against the benefits of broader patents.
Recommendations
-
The problem of reducing inappropriate antibiotic use calls for a combination of price and non-price measures. The appropriate mix will have to be tailored to the particular cultural and medical context. Patient and physician education, better surveillance data, increasing antibiotic heterogeneity, providing warning labels on antibiotics are all part of the policy response mix. However, they are likely to be ineffective without a compelling economic incentive for patients and physicians to face the cost they impose on the rest of society in the form of resistance when they use or misuse antibiotics.
-
While lowering the demand for antibiotics is one part of the solution, further research should also look at incentives faced by pharmaceutical firms with respect to research and development expenditure on new classes of antibiotics, as well as resistance to existing products.
REFERENCES
American Society for Microbiology. 1995. Report of the ASM task force on antibiotic resistance. Antimicrobial Agents and ChemotherapySupplement:1–23.
Cannon G. 1995. Superbug. Nature’s revenge. London: Virgin Publishing. P. 189.
CIA (Central Intelligence Agency). 2000. The Global Infectious Disease Threat and Its Impli cations for the United States. [Online]. Available: http://www.odci.gov/nic/graphics/infectiousdiseases.pdf.
Coast J and Smith RD. 2001. Antimicrobial resistance: can economics help?Eurohealth 7:32–33.
Coast J, Smith RD, Karcher AM, Wilton P, Millar M. 2002. Superbugs II: How should economic evaluation be conducted for interventions which aim to reduce antimicrobial resistance?Health Economics11:637–647.
Coast J, Smith R, Millar MR. 1996. Superbugs: should antimicrobial resistance be included as a cost in economic evaluation?Health Economics5:217–226.
Coast J, Smith RD, Millar MR. 1998. An economic perspective on policy antimicrobial resistance. Social Science and Medicine46:29–38.
Cox RA, Conquest C, Mallaghan C, Marples RR. 1995. A major outbreak of methicillin-resistant Staphylococcus aureus caused by a new phage-type (EMRSA-16). Journal of Hospital Infection29:87–106.
Ellison SF and Hellerstein J.1999. The economics of antibiotics: an exploratory study. In: Triplett JE, ed. Measuring the Prices of Medical Treatment.Washington, DC: Brookings Institution Press. Pp. 118–151.
Fasehun F. 1999. The antibacterial paradox: essential drugs, effectiveness and cost. Bulletin of the World Health Organization77:211–216.
Foxman B, Valdez RB, Lohr KN, Goldberg GA, Newhouse JP, Brook RH. 1987. The effect of cost sharing on the use of antibiotics in ambulatory care: results from a population-based randomized controlled trial. Journal of Chronic Diseases40:429–437.
Hodge I. 1995. Environmental Economics.Basingstoke, UK: MacMillan. House of Lords Select Committee on Science and Technology. 1998. Seventh Report. [Online]. Available: http://www.parliament.the-stationery-office.co.uk/pa/ld199798/ldselect/ldsctech/081vii/st0701.htm.
John J and Fishman NO. 1997. Programmatic role of the infectious diseases physician in controlling antimicrobial costs in the hospital. Clinical Infectious Diseases24:471–485.
Kaldec R, Zelicoff A, Vrtis A. 1997. Biological weapons control: prospects and implications for the future. Journal of the American Medical Association278:351–356.
Laxminarayan R, ed. 2002. Battling Resistance to Antibiotics and Pesticides: An Economic Approach.Washington, DC: Resources for the Future Press.
Laxminarayan R and Weitzman ML. 2002. On the implications of endogenous resistance to medications . Journal of Health Economics21:709–718.
Laxminarayan R, Jernigan DB, et al. 1998. Using Antibiotic Resistance Surveillance Data in the Optimal Treatment of Acute Otitis Media.Paper presented at the Infectious Diseases Society of America 36th Annual Meeting, Denver.
Levy S. 2002. The Antibiotic Paradox. How the Misuse of Antibiotics Destroys Their Cura tive Powers. Cambridge, MA: Perseus Publishing.
McCaig LF and Hughes JM. 1995. Trends in antimicrobial drug prescribing among office-based physicians in the United States. Journal of the American Medical Association 273:214–219.
Mehtar S, Drabu YJ, Mayet F. 1989. Expenses incurred during a 5-week epidemic methicillin-resistant Staphylococcus aureus outbreak. Journal of Hospital Infection13(2):199–200.
Murray BE. 1994. Can antibiotic resistance be controlled?New England Journal of Medicine 330:1229–1230.
Neu HC. 1992. The crisis in antibiotic resistance. Science257:1064–1073.
OTA (Office of Technology Assessment). 1995. Impacts of Antibiotic-Resistant Bacteria. OTA-H-629. Washington, DC: OTA.
Pearce D and Turner R.1990. Economics of Natural Resources and the Environment. London: Harvester Wheatsheaf.
Phelps C. 1989. Bug-drug resistance. Medical Care27:194–203.
Smith RD. 1999. Antimicrobial resistance: the importance of developing long term policy. Bulletin of the World Health Organization77:862.
Smith RD and Coast J. 1998. Controlling antimicrobial resistance: a proposed transferable permit market. Health Policy43:219–232.
Smith RD and Coast J. 2001. Global Responses to the Growing Threat of Antimicrobial Resistance.Working Paper prepared for Commission on Macroeconomics and Health, WHO. [Online]. Available: http://www3.who.int/whosis/cmh/cmh_papers/e/pdf/wg2_paper16.pdf.
Smith RD and Coast J. 2002. Antimicrobial resistance: a global response. Bulletin of the World Health Organization80:126–133.
Smith RD and Coast J. In press. Antimicrobial resistance and global public goods for health. In: Smith RD, Beaglehole R, Drager N, eds. Global Public Goods for Health: A Health Economic and Public Health Perspective.Oxford: Oxford University Press.
Smith RD, Coast J, Millar MR. 1996. Over-the-counter antimicrobials: the hidden costs of resistance. Journal of Antimicrobial Chemotherapy37:1031–1032.
Smith RD, Coast J, Millar MR, Wilton P, Karcher A-M. 2001. Interventions Against Anti-Microbial Resistance: a Review of the Literature and Exploration of Modelling Cost- Effectiveness. Report to: Global Forum for Health Research.Geneva: World Health Organization.
Standing Medical Advisory Committee Sub-Group on Antimicrobial Resistance. 1998. The Path of Least Resistance. [Online]. Available: http://www.doh.gov.uk/smac1.htm.
Tietenberg T. 1990. Economic instruments for environmental regulation. Oxford Review of Economic Policy6:17–33.
Tomasz A. 1994. Multiple-antibiotic resistant pathogenic bacteria. A report on the Rockefeller University workshop. New England Journal of Medicine330:1247–1251.
Turner R, Pearce D, Bateman I. 1994. Environmental Economics. An Elementary Introduc tion.London: Harvester Wheatsheaf.
Weitzman M. 1974. Prices versus quantities. Review of Economic Studies41:477–491.
WHO (World Health Organization). 2001. Global Strategy for the Containment of Antimi crobial Resistance.WHO/CDS/CSR/DRS/2001.2. Geneva: WHO.
Wilton P, Smith RD, Coast J, Millar M. 2002. Strategies to contain the emergence of antimicrobial resistance: a systematic review of effectiveness and cost-effectiveness. Journal of Health Services Research and Policy7:111–117.
Wilton P, Smith RD, Coast J, Millar M, Karcher A. 2001. Directly observed therapy for multi-drug resistant tuberculosis: an economic evaluation in the United States of America and South Africa. The International Journal of Tuberculosis and Lung Disease5:1137– 1142.
Winebrake J, Farrell A, Bernstein M. 1995. The Clean Air Act’s sulfur dioxide emissions market: estimating the costs of regulatory and legislative intervention. Resource and Energy Economics17:239–260.
World Bank. 2001. World Development Report 2000/01. New York: Oxford University Press.























