4
Late Effects of Childhood Cancer
Childhood cancer survivors, though being “cured” of cancer, often experience late effects, both physical and psychological, secondary to their cancer or its treatment. Complications, disabilities, or adverse outcomes that are the result of the disease process, the treatment, or both, are generally referred to as “late effects.” Late effects may be easy to identify because of their visibility (e.g., amputation) or direct effects on function (e.g., severe cognitive impairment). Other late effects, however, can be subtle and apparent only to the trained observer (e.g., scoliosis or curvature of the spine) or not directly observable and identified only through screening or imaging tests (hypothyroidism, infertility). In addition to concerns about a recurrence of the cancer for which they were treated, cancer survivors are also at increased risk of developing a second type of cancer because of either their treatment for cancer (e.g., radiation), their genetic or other susceptibility, or some interaction between treatment and genetic susceptibility.
Some late effects of therapy are identified early in follow-up—during the childhood or adolescent years—and resolve without consequence. Others may persist, become chronic problems, and influence the progression of other diseases associated with aging. For example, renal dysfunction secondary to treatment with the chemotherapeutic agent ifosfamide may be accelerated if the survivor develops hypertension or diabetes mellitus, two common adult health problems (Prasad et al., 1996; Skinner et al., 2000).
Chemotherapy, radiation therapy, and surgery may all cause late effects involving any organ or system of the body. Effects of surgery with
implications for survivorship may include amputation, eye removal, disfigurement, or growth abnormalities. Exposure to therapeutic agents during the rapid and dramatic physiologic and psychologic changes occurring from infancy to early adulthood can result in specific tissue or organ damage, or alteration of normal patterns of growth and development. Long-term sequelae of chemotherapy and radiation are common, may be mild or severe, and may be asymptomatic for extended periods. As many as two-thirds of survivors will experience a late effect of chemotherapy or radiation, defined as any chronic or late occurring outcome—physical or psychosocial—that persists or develops beyond five years from the diagnosis of the cancer (Garre et al., 1994; Oeffinger et al., 2000; Stevens et al., 1998; Vonderweid et al., 1996). These late effects include cognitive impairment, fertility problems, alterations in growth and development, organ system damage, chronic hepatitis, and second malignant neoplasms (DeLaat and Lampkin, 1992; Donaldson, 1993; Dreyer et al., 2002; Friedman and Meadows, 2002; Marina, 1997; Meister and Meadows, 1993; Neglia and Nesbit, 1993; Schwartz, 1995). Survivors frequently have more than one late effect, with perhaps as many as a quarter of survivors experiencing one that is severe or life-threatening (Garre et al., 1994; Oeffinger et al., 2000; Stevens et al., 1998).
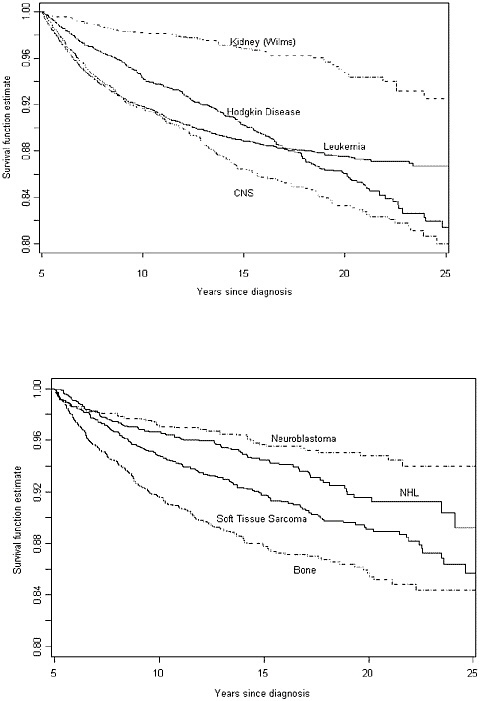
The seriousness of the consequences of late effects is evident in studies of premature death following cancer treatment. In one study of late mortality among 20,227 5-year survivors of childhood cancer diagnosed with cancer from 1970 to 1986, there was a 10.8-fold excess in overall mortality (Mertens et al., 2001). Ten percent of these individuals had died by 1996. Figure 4.1 shows all-cause mortality in this cohort as compared to age-adjusted expected survival rates for the U.S. population. Survival is shown by original cancer diagnosis in Figures 4.2a and 4.2b.
Among those for whom cause of death was ascertained, relapse of the primary cancer accounted for 67.4 percent of deaths and treatment-related consequences accounted for 21.3 percent of deaths. The remaining 11.3 percent of deaths were caused by non-treatment external causes (e.g., motor vehicle accidents) or medical conditions (e.g., HIV, pneumonia) (Table 4.1). The three most common treatment-related causes of death observed were (1) the development of a secondary or subsequent cancer, (2) cardiac toxicity, and (3) pulmonary complications.
Among the Childhood Cancer Survivor Study (CCSS) cohort, the overall all-cause absolute excess risk was 8.8 deaths per 1,000 person-years. Within treatment-related cause-specific categories (i.e., excluding recurrences and non-treatment-related deaths), the absolute excess risk was 1.26, 0.27, and 0.015 deaths per 1,000 person-years for secondary and subsequent cancers, cardiac causes, and pulmonary causes, respectively. These treatment-related deaths account for 18 percent of the excess risk of death
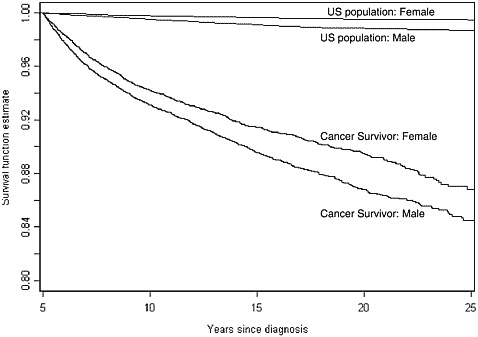
FIGURE 4.1 All-cause mortality, by sex (Childhood Cancer Survivor Study). US population: Age-adjusted expected survival rates. Cancer survivor: All-cause mortality experience from five years after inital canccer diagnosis.
SOURCE: Mertens et al., 2001. Reprinted with permission of the American Society of Clinical Oncology.
observed in this cohort. The risk was highest among females, those diagnosed with cancer before the age of 5, and those with an initial diagnosis of leukemia or central nervous system (CNS) tumor (Mertens et al., 2001; Moller et al., 2001).
The cumulative cause-specific mortality was highest for cancer recurrence (7 percent at 25 years from diagnosis) (Figure 4.2). Death rates due to subsequent cancers and other causes increased more rapidly in the time period 15 to 25 years after diagnosis than from 5 to 15 years after diagnosis.
Despite the relatively high prevalence of late effects, recent evidence suggests that survivors of childhood cancer view themselves as being in relatively good health. Only 11 percent of 9,434 members of the CCSS cohort reported that they were in fair or poor general health when recently surveyed (Kevin Oeffinger, personal communication to Maria Hewitt, August 16, 2002). This assessment may not necessarily indicate a lack of limitations or disability. People with serious chronic illness, recurring disease, or disability sometimes report being in good health because they
TABLE 4.1 Causes of Death in the Childhood Cancer Survivor Study Cohort
|
Cause of death |
Number of deaths |
Percent of deaths |
|
Total |
1,848 |
100.0 |
|
Recurrence |
1,246 |
67.4 |
|
Treatment-related consequences |
394 |
21.3 |
|
Subsequent neoplasm |
235 |
12.7 |
|
Cardiac |
83 |
4.5 |
|
Pulmonary |
33 |
1.8 |
|
Other sequelae |
43 |
2.3 |
|
Non-treatment related |
208 |
11.3 |
|
External causes |
94 |
5.1 |
|
Medical conditions |
114 |
6.2 |
|
SOURCE: Adapted from Mertens et al., 2001. |
||
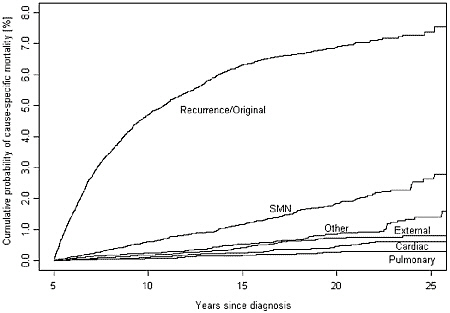
FIGURE 4.3 Cumulative cause-specific mortality (Childhood Cancer Survivor Study).
NOTE: SMN = second malignant neoplasm.
SOURCE: Mertens et al., 2001. Reprinted with permission of the American Society of Clinical Oncology.
experience benefits from their illness, for example, becoming closer to family, discovery of self and life priorities, and renewed spirituality (Justice, 1999; Kornblith et al., 1998). Researchers examined several health-related domains—general health, mental health, functional impairment, activity limitations, and pain or anxiety as a result of the cancer or its treatment— and found that 45 percent of the cohort members reported moderate to severe adverse outcomes in at least one of the domains (Kevin Oeffinger, personal communication to Maria Hewitt, August 16, 2002).
Table 4.2 summarizes some of the late effects associated with the more common childhood cancers. The next section describes how specific treatments can contribute to physical and psychosocial damage. Chapter 5 describes approaches to monitor late effects.
The most common late effects of childhood cancer include those that are neurocognitive and psychological, cardiopulmonary, endocrine (e.g., those affecting growth and fertility), musculoskeletal, and those related to second malignancies. The emergence of late effects depends on many factors, including age, exposures to chemotherapy and radiation during treatment (doses and parts of body exposed), and the severity of disease. The following section briefly reviews some of the late effects that occur following primary treatment. For a more complete discussion, see the background papers prepared for the Board (www.iom.edu/ncpb) and refer to comprehensive reviews that are available for both consumers (Keene et al., 2000; http://www.candlelighters.org) and providers (Dreyer et al., 2002; Friedman and Meadows, 2002; Schwartz, 1995, 1999; Schwartz et al., 1994; Ward, 2000).
NEUROCOGNITIVE LATE EFFECTS
Cognitive impairment is one of the most debilitating late effects among children whose cancer (or its treatment) involved the central nervous system. Learning problems, social difficulties, behavioral adjustment problems, and long-term education and vocational difficulties may be experienced.
There are five primary groups of children that may experience CNS-related cognitive impairments:
-
Children with tumors of the CNS
-
Children with leukemia or non-Hodgkin’s lymphoma who receive CNS prophylaxis involving chemotherapy and/or radiation therapy
-
Children with tumors of the face, eye, or skull that require localized, external beam radiation therapy
-
Children treated with whole body radiation and myeloablative che-
TABLE 4.2 Selected Physical Late Effects Associated with Childhood Cancer
|
Cancer |
Potential Late Effects |
|
|
Leukemias |
• Cognitive effects (e.g., learning disabilities) • Abnormal growth and maturation • Heart problems • Second cancers • Hepatitis C (effects of blood transfusion) |
• Weakness, fatigue • Obesity • Avascular necrosis of bone • Osteoporosis • Dental problems |
|
Brain cancer |
• Neurologic and cognitive effects (e.g., learning disabilities) • Abnormal growth and maturation • Hearing loss |
• Kidney damage • Hepatitis C • Infertility • Vision problems • Second cancers |
|
Hodgkin’s disease |
• Adhesions and intestinal obstruction (if spleen removed) • Decreased resistance to infection (potential for life-threatening sepsis) • Abnormal growth and maturation • Hypothyroidism (effects of neck radiation) |
• Salivary gland malfunctioning (effect of jawbone irradiation) • Lung damage • Heart problems • Infertility • Hepatitis C • Second cancers (e.g., breast cancer in females) |
|
Non-Hodgkin’s lymphoma |
• Heart problems • Hepatitis C • Cognitive effects |
• Infertility • Osteopenia/osteoporosis |
|
Bone tumor |
• Amputation/disfigurement • Functional, activity limitations • Damage to soft tissues and underlying bones (radiation may cause scarring, swelling, or inhibit growth) |
• Hearing loss • Heart problems • Kidney damage • Second cancers • Hepatitis C • Fertility problems |
|
Wilm’s tumor |
• Heart problems • Kidney damage • Damage to soft tissues and underlying bones (radiation may cause scarring, swelling, or inhibit growth) |
• Second cancers • Fertility problems • Scoliosis |
|
Cancer |
Potential Late Effects |
|
|
Neuroblastoma |
• Heart problems • Damage to soft tissues and underlying bones (radiation may cause scarring, swelling, or inhibit growth) |
• Neurocognitive effects • Hearing loss • Hepatitis C • Second cancers • Kidney damage |
|
Soft tissue sarcoma |
• Amputation/disfigurement • Functional, activity limitations • Heart problems • Damage to soft tissues and underlying bones (radiation may cause scarring, swelling, or inhibit growth) |
• Second cancers • Hepatitis C • Kidney damage • Cataracts • Infertility • Neurocognitive effects |
-
motherapy as part of a preparation regimen for allogeneic bone marrow transplantation (marrow is received from another person)
-
Children with solid tumors or leukemia who are treated during critical developmental periods and who require prolonged and repeated hospitalizations that interfere with the acquisition of normal developmental skills.
Since leukemias and lymphomas account for nearly 40 percent of childhood cancer diagnosed in the United States and tumors of the CNS account for nearly 20 percent, a total of about 50 to 60 percent of children treated for cancer will have at last some risk of neurocognitive impairment resulting from the cancer and/or its treatment. A number of factors can contribute to neurocognitive deficits: tumor characteristics (e.g., the location and extent of the tumor), surgery (e.g., bleeding or rarely, infection), radiation therapy (e.g., dose, volume, age at administration), and chemotherapy. Not all children with CNS exposure to radiation and chemotherapy will experience neurocognitive effects, and there is no certain way to predict which children will experience them. Factors associated with higher risk for cognitive impairment include younger age at the time of treatment, the intensity of treatment, the duration of time between treatment and evaluation, and the age of the child at the time he or she is evaluated. Absences from school during treatment can also contribute to impaired academic performance.
For children with CNS tumors or acute lymphocytic leukemia (ALL), the severity of cognitive impairment following radiation therapy has been associated with the dose of radiation that is administered. Higher doses of radiation (e.g., above 24 Gy) are associated with more significant impair-
ment, and these are the doses that are most frequently used in the treatment of children with CNS tumors. Studies of survivors of childhood CNS tumors have consistently shown substantial decreases in global IQ scores in the years following treatment, with declines of 20 to 50 full-scale IQ points noted. Lower doses of radiation (e.g., 18 Gy or less) are associated with less severe cognitive impairment. These doses are most frequently used in the treatment of children with CNS leukemia or as preparatory regimens for children treated with bone marrow transplantation. The addition of certain chemotherapeutic agents administered in high doses or injected into the spinal canal (e.g., methotrexate) significantly increases the risk for cognitive impairment. Females with ALL who received intrathecal methotrexate and cranial radiation as CNS prophylaxis have been shown to have lower levels of cognitive functioning than males. Preliminary reports suggest that cognitive dysfunction may also be more common when treatment for ALL includes dexamethasone instead of prednisone as the steroid (Waber et al., 2000).
Deficits in neurocognitive function may not be apparent in the immediate period following treatment. In one study, for example, there were no differences in the results on 16 standardized memory measures between patients randomized to receive CNS prophylaxis with either 18 Gy cranial irradiation or high-dose intravenous methotrexate (Mulhern et al., 1988). Subsequent periodic evaluation of these patients, however, showed declines in scores in both treatment groups (Ochs et al., 1991).
Studies of cognitive late effects in children treated for ALL and CNS tumors suggest that nonverbal abilities are most impaired, including short-term memory, processing speed, visual-motor integration, sequencing ability, and attention and concentration. These effects are common to other types of acquired brain injury. Such impairments can affect school performance, learning, and social function. Children may have difficulty completing work in the classroom, and may spend substantially more time completing homework assignments. There may also be difficulties with handwriting, organizing material on a page, lining up columns for arithmetic problems, and accurately responding to standardized testing forms that require shading responses on a computerized record. Problems with inattention may contribute to difficulties in completing tasks or following conversations. This complex of cognitive late effects contributes to educational difficulties with reading, language development, and complex mathematics (e.g., multiplication and division). Special education services are often required to overcome recognized learning difficulties.
A large retrospective cohort study of 593 adult survivors of childhood ALL and 409 sibling controls demonstrated that ALL survivors have a greater likelihood of being placed in special education or learning disabled programs than their siblings, but that most are able to compensate and
adapt to overcome these problems (Challinor and Karl, 1995; Haupt et al., 1994, 1995). On average, ALL survivors had lower grades, higher enrollment rates in special education or learning disability programs (four times greater than their siblings), and when enrolled, spent a longer time in these programs than did their siblings (Table 4.3). Cancer survivors were also at higher risk of missing school for long periods and repeating a year of school. Most ALL survivors had rates of high school graduation, college entry, and college graduation that were similar to those of their brothers and sisters, suggesting that remediation was successful. Only survivors treated with 24 Gy or more of cranial radiation and those diagnosed at a preschool age were at higher risk for poor educational performance; this group was identified by investigators as in need of targeting for remediation.
Participants in this study had to be at least 18 years old by 1990, to have been treated for ALL before age 20, to have survived at least 2 years after diagnosis, to be in remission, and to be receiving no leukemic therapy at follow-up. Nearly one-quarter (24 percent) of the sample had been diagnosed under age 6. Survivors were old enough to have finished high school and many had finished college. The educational outcomes of children currently treated on some of the intensive chemotherapy protocols in the 1990s are not yet available (D. Armstrong, University of Miami School of Medicine, personal communication to Maria Hewitt, March 28, 2002).
Some small single-institution studies have found relatively high rates of use of special education. In one study, 12 of 24 survivors of childhood ALL treated with 18 Gy of craniospinal irradiation and intrathecal chemotherapy (methotrexate) had received some type of special education service when assessed 4 to 5 years from the time of their diagnosis (Rubenstein et al., 1990). Another study conducted in The Netherlands found that 7 of 28 children treated for ALL with chemotherapy and radiation and assessed 10 years later had received special education services, a rate much higher than for their siblings (4 percent). There were no differences in special education placements between children treated with chemotherapy without radiation and their siblings. However, they had significant deficits in auditory memory and fine-motor functioning (Kingma et al., 2001). Some estimate that as many as 70 to 80 percent of high-risk children (e.g., those with CNS tumors treated with high-dose, whole-brain radiation under age 4) may need special education services (Armstrong et al., 1999; Packer et al., 1987).
As discussed above, neurocognitive deficits may not be evident in the period immediately following treatment. Studies of children with CNS tumors show that they generally do not lose abilities that had been acquired prior to treatment. Instead, the children appear to improve their skills in some areas, but at a substantially slower rate than healthy children. Other skills, which would be expected to emerge in a predictable developmental sequence in normal children, may not emerge because the underlying brain
structures fail to develop. Learning disabilities are defined in terms of recognized discrepancies between intellectual functioning and academic achievement. A discrepancy may not be observed shortly following treatment, but may become evident at a later time. Because the kinds of impairments experienced by children with cancer emerge over time, neurocognitive evaluations need to be conducted on a schedule that anticipates areas of deficit (Iuvone et al., 2002). Assessment tools used in these evaluations should focus on the specific areas of potential deficits that are associated with the type of brain injury resulting from cancer treatment. This may require neuropsychological testing that is typically not provided by the educational system and the use of tests that fall outside the scope of those routinely used in educational planning.
The evidence regarding neurocognitive deficits associated with cancer treatment is being used to moderate treatments to reduce these effects. The results of ongoing studies to maintain and improve survival while minimizing cognitive impairment, however, will not be available for another 5 to 10 years. Preliminary results of assessments of interventions to remediate treatment-related cognitive effects using a psychologically based outpatient rehabilitation program appear promising (Butler et al., 2002). Educational programs of relevance to cancer survivors are discussed in Chapter 6.
PSYCHOSOCIAL AND BEHAVIORAL LATE EFFECTS
“The experience of completing cancer treatment has two faces—one of celebration and hope, one of uncertainty and fear” (Haase and Rostad, 1994, p. 1490). Cancer may have psychological, social, and spiritual or existential effects secondary to worry about many aspects of survivorship, including the risk of relapses, dying, more treatments, potential problems with sexuality and fertility, body image, school and work performance, and social and family relationships (Gray et al., 1992; Rait et al., 1992; Roberts et al., 1998; Weigers et al., 1998). “Quality of life” studies assess the frequency of untoward consequences of disease and factors associated with them.
Despite periods of intense stress, most survivors achieve normal levels of psychological and social functioning, and families adapt well. All survivors, however, even those apparently doing quite well, experience at least occasional problems in social adjustment and continue to be concerned about their medical and social futures. There is a small but significant minority of survivors who remain seriously troubled and are impaired by their psychological problems. The size of this group, and the nature and extent of their problems are not fully known (Fritz et al., 1988; Gray et al., 1992; Greenberg et al., 1989; Hobbie et al., 2000; Kazak and Meadows, 1989; Koocher and O’Malley, 1981; Kupst et al., 1995; Moore et al., 1987;
TABLE 4.3 Enrollment in Special Education Programs Among Survivors of Childhood Acute Lymphoblastic Leukemia Relative to Sibling Controls, by Time from Diagnosisa
|
|
Before diagnosis |
After diagnosis |
||
|
Educational Outcome |
Event rateb |
RRc |
Event rateb |
RRc |
|
Special education |
||||
|
Total |
3.8 |
1.4 |
9.5 |
3.4* |
|
Age at diagnosis, y |
||||
|
0-5 |
|
|
12.3 |
4.5* |
|
≥6 |
|
|
7.7 |
2.8* |
|
Cranial radiation, Gy |
||||
|
None |
|
|
5.8 |
2.1 |
|
18 |
|
|
7.2 |
2.6* |
|
24 |
|
|
11.4 |
4.1* |
|
Intrathecal methotrexate, mg |
||||
|
None |
|
|
11.5 |
4.1* |
|
<83 |
|
|
11.2 |
4.1* |
|
≥83 |
|
|
5.5 |
2.0* |
|
Learning disabled |
||||
|
Total |
5.1 |
1.4 |
13.3 |
3.6* |
|
Age at diagnosis, y |
||||
|
0-5 |
|
|
17.5 |
4.7* |
|
≥6 |
|
|
10.8 |
2.9* |
|
Cranial radiation, Gy |
||||
|
None |
|
|
6.0 |
1.6 |
|
18 |
|
|
5.4 |
1.4 |
|
24 |
|
|
19.6 |
5.3* |
|
Intrathecal methotrexate, mg |
||||
|
None |
|
|
12.5 |
3.3* |
|
<83 |
|
|
18.2 |
4.9* |
|
≥83 |
|
|
6.9 |
1.9 |
|
Gifted and talented |
||||
|
Total |
7.0 |
1.0 |
7.0 |
1.0 |
|
Age at diagnosis, y |
||||
|
0-5 |
|
|
4.2 |
0.6 |
|
≥6 |
|
|
8.9 |
1.2 |
|
Cranial radiation, Gy |
||||
|
None |
|
|
5.7 |
0.8 |
|
18 |
|
|
8.5 |
1.2 |
|
24 |
|
|
6.2 |
0.9 |
|
Intrathecal methotrexate, mg |
||||
|
None |
|
|
8.0 |
1.1 |
|
<83 |
|
|
5.2 |
0.7 |
|
≥83 |
|
|
9.1 |
1.3 |
|
aOnly survivors diagnosed before 18 years of age were considered. bEvents per 1,000 person-years. |
||||
|
From diagnosis through 2 y after diagnosis |
After 3 y from diagnosis |
||
|
Event rateb |
RRc |
Event rateb |
RRc |
|
5.5 |
2.0 |
11.3 |
4.1* |
|
8.1 |
2.9 |
13.0 |
4.7* |
|
4.9 |
1.8 |
9.7 |
3.5* |
|
0 |
— |
8.8 |
3.2 |
|
1.4 |
0.5 |
11.2 |
4.0* |
|
10.8 |
3.9* |
11.6 |
4.2* |
|
16.2 |
5.9* |
10.3 |
3.7* |
|
4.9 |
1.8 |
13.6 |
4.9* |
|
3.0 |
1.1 |
7.5 |
2.7* |
|
13.2 |
3.5* |
13.4 |
3.6* |
|
24.7 |
6.6* |
16.3 |
4.4* |
|
0.9 |
2.9* |
10.7 |
2.9* |
|
0 |
— |
9.1 |
2.4* |
|
4.4 |
1.2 |
6.1 |
1.6 |
|
25.0 |
6.7* |
17.8 |
4.8* |
|
10.8 |
2.9 |
12.9 |
3.5* |
|
21.8 |
5.8* |
16.7 |
4.5* |
|
6.1 |
1.6 |
7.6 |
2.0 |
|
11.3 |
1.6 |
5.1 |
0.7 |
|
4.1 |
0.6 |
4.2 |
0.6 |
|
12.8 |
1.8 |
6.0 |
0.8 |
|
17.5 |
2.4 |
0 |
— |
|
15.2 |
2.1* |
4.0 |
0.6 |
|
6.2 |
0.9 |
6.2 |
0.9 |
|
10.8 |
1.5 |
7.3 |
1.0 |
|
10.0 |
1.4 |
3.5 |
0.5 |
|
12.7 |
1.8 |
6.3 |
0.9 |
|
cRR indicates relative risk and compares the event rate in survivors (shown) to the event rate in controls (not shown). *P < 0.05. SOURCE: Haup et al., 1994 (reprinted with permission). |
|||
Mulhern et al., 1989; Stuber et al., 1996; Van Dongen-Melman and Sanders-Woudstra, 1986; Wasserman et al., 1987). A syndrome similar to postraumatic stress disorder (PTSD)1 has been reported in adolescent and young adult survivors (Hobbie et al., 2000; Meeske et al., 2001) and in mothers, fathers, and siblings of childhood cancer survivors (Kazak et al., 199, 2002). Stress, either immediate or delayed, in response to childhood cancer is not surprising given the strenuous, invasive, and often painful nature of the treatments involved. PTSD is associated with anxiety and psychological distress, and may interfere with achievement of developmental milestones. Eiser and colleagues, however, in their systematic review of the literature on the psychological consequences of cancer found no higher prevalence of PTSD among childhood survivors in studies that included control groups (Eiser et al., 2000). More research in this area is needed to better understand the nature and extent of psychological distress among survivors of childhood cancer.
Some research has shown limitations of social functioning among children of school age. Survivors of CNS tumors, for example, have been shown to be less popular with other children (Noll et al., 1997). Studies of adult survivors of childhood cancer have shown poorer functioning in the areas of friendships and social contacts (Mackie et al., 2000). Preliminary results of a study of marriage among members of the Childhood Cancer Survivor Study suggest that adult survivors of childhood cancer marry at lower rates than expected, especially survivors of CNS tumors (Rauck et al., 1999).
Psychosocial interventions to address these concerns can include psychological, emotional, peer, or education support; social skills training; adjustment counseling; family counseling; therapeutic play; cognitive-behavioral interventions; and group or individual psychotherapy (Cohen and Walco, 1999; Kazak et al., 1999; Schwartz, 1999; Van Dongen-Melman, 2000; Walker, 1989). Applied research is needed to identify survivors and their families who are likely to benefit from services, and the relative success of interventions in improving quality of life. Also needed is research to identify the psychosocial issues and service needs of racial and ethnic minority populations and families of low socioeconomic status.
Survivors with substantial physical late effects, learning problems, or relapse are more likely than survivors without late effects to show evidence of lower self-esteem, poorer adjustment, and worse quality of life (Chen et al., 1998; Fritz et al., 1988; Kazak et al., 1994; Koocher et al., 1980; Kupst and Schulman, 1988; Moore et al., 1987; Mulhern et al., 1989; Van Dongen-Melman and Sanders-Woudstra, 1986; Zebrack and Chesler, 2002; Zeltzer, 1993). Other research suggests that survivors diagnosed at an older age (Kupst et al., 1995) or who are older at the time of inquiry (Barakat et al., 1997; Elkin et al., 1997) show more negative psychosocial outlooks, as do those who are from families of lower socioeconomic status (Greenberg et al., 1997; Kupst and Schulman, 1988) or who have experienced more concurrent stress (Barakat et al., 1997). Others have identified high dose radiation, younger age at diagnosis, and female gender as risk factors for mood disturbance in long-term survivors (Zeltzer et al., 1997).
A recent report from the Childhood Cancer Survivor Study indicates that certain sociodemographic characteristics (i.e., female gender, lower household income, lower educational attainment, not being employed) are associated with an increased risk for depression and somatic distress among both leukemia and lymphoma survivors and their sibling controls (Zebrack et al., 2002). These sociodemographic characteristics are generally recognized as risk factors for mental illness in the general population. Only exposure to intensive chemotherapy added to childhood cancer survivors’ risk for reporting somatic distress. These findings from the largest cohort of childhood cancer survivors to date (over 16,000 survivors diagnosed before age 18 and ranging in age from 14 to 52 at time of study) have led the authors to theorize that psychosocial distress results from limited educational and employment opportunities that are secondary to late effects of chemotherapy and cancer-related social disruptions at critical developmental life stages (Zebrack et al., 2002). Other investigators examining outcomes among cancer survivors have suggested that increased anxiety and depression in children who have had treatment for childhood cancer may be a consequence of perceived or real academic underachievement (Brouwers et al., 2002).
There are anecdotal reports of psychological growth among survivors in response to childhood cancer (Eiser and Havermans, 1994), and in several studies childhood cancer survivors were significantly healthier in psychosocial terms or more appreciative of life than population norms or healthy controls (Arnholt et al., 1993; Cella and Tross, 1986; Elkin et al., 1997; Maggiolini et al., 2000; Weigers et al., 1998). These findings suggest a degree of resiliency and positive adaptation among some long-term survivors of childhood cancer. However, the extent to which psychological growth and meaning attributed to the cancer experience exists among survivors has yet to be determined and deserves further research.
Childhood cancer affects entire families (Chesler and Barbarin, 1987), and the health and well-being of the childhood cancer survivor is inextricably linked to the health and well-being of his or her own parents, siblings, and eventually spouses and significant others, as well as offspring. An example of the familial effect of childhood cancer is the finding that siblings of children with cancer have more somatic symptoms and poorer health care than healthy controls (Barbarin et al., 1995; Dolgin et al., 1997; Sahler et al., 1994; Sargent et al., 1995; Zeltzer et al., 1996). The long-term implications for siblings of childhood cancer survivors are unknown, and studies using these siblings as control groups may in fact lead to underestimation of problems among survivors.
Risky Behaviors
Some evidence suggests that childhood cancer survivors engage in behaviors that are likely to further increase their risk of subsequent cancer and other chronic illnesses. In one study, survivors had higher rates of alcoholism than the general population (Lansky et al., 1986). Despite their increased risks for second cancers, smoking rates among survivors were equal to those in the general U.S. population according to some studies (Emmons et al., 2002; Hollen and Hobbie, 1993; Hollen and Hobbie, 1996; Tao et al., 1998; Troyer and Holmes, 1988). Certain survivors are at particularly high risk for smoking-related health effects, especially individuals who received potentially pulmonary-damaging treatments such as bleomycin, or cardiotoxic treatments such as anthracyclines. According to a survey of 40 young adult survivors, 47 percent reported trying tobacco, 17 percent continued to smoke, and 12 percent reported binge drinking (Mulhern et al., 1995).
Survivors were less likely to quit smoking as compared with sibling controls according to one study (Haupt et al., 1992); however, another study showed no significant differences among quit rates between survivors and sibling controls (Tao et al., 1998). Survivors were significantly less likely to initiate smoking, but once having started, they were as likely as controls to become regular smokers (Tao et al., 1998). Furthermore, both survivor and sibling smokers reported substantial habits (greater than 1/2 pack per day). Childhood cancer survivors, particularly if they are male, with high rates of anxiety, depression, or self-esteem deficits, limited vocational potential, and physical health or functioning deficits may be especially likely to engage in risk-taking behaviors. In contrast, females in the general population are more likely to experience anxiety or depression, low self-esteem, and low vocational potential (Nolen-Hoeksema, 1987), which may secondarily increase their risk-taking behaviors. Treatment variables, such as exposure to cranial irradiation and demographic variables such as
age at diagnosis, have been demonstrated to significantly and negatively affect educational attainment in long-term survivors of childhood leukemia (Haupt et al., 1994). Treatment intensity during childhood may serve as a risk factor for adult survivors’ health-compromising behaviors as the result of neuropsychological deficits that arise from cancer treatment (Chen et al., 1998; Hollen, 2000).
It is still unclear which treatment factors (type and level of chemotherapy or radiation therapy) and quality of life issues (psychological distress, vocational potential, or physical health and functioning) will best predict high-risk behavior. Investigators have found lower risk-taking behaviors (i.e., smoking, alcohol use, illicit drug use) among resilient adolescents, those with good decision-making abilities, and those described as having an easygoing temperament, high self-esteem, and a sense of control and autonomy (Hollen et al., 1997; Hollen et al., 2001).
It is also not well understood how sociodemographic variables such as age at diagnosis, gender, ethnicity or socioeconomic status influence risk behavior. Limited investigations into the role of race and ethnicity in health behavior outcomes for childhood cancer survivors have not demonstrated ethnic differences in health behavior outcomes (Mulhern et al., 1995); yet, race/ethnicity and socioeconomic status are considered predisposing (as well as confounding) factors for increased vulnerability of young people engaging in risk-taking behaviors (Irwin, 1993). It may be that small sample size in reported survivor studies has limited the power for examining race and ethnicity as risk factors.
Some adult survivors engage in behaviors that increase their risk of disease and disability. Adult survivors of childhood cancer were less likely to smoke than the general population, but 17 percent were still current smokers according to an analysis of behaviors of 9,709 adult survivors participating in the Childhood Cancer Survivor Study (Emmons et al., 2002). Survivors who had received chest radiation or anthracyclines were no less likely to smoke than other survivors. These studies underscore the need for survivors to receive counseling regarding high-risk behaviors. Preliminary results from studies of smoking cessation interventions among childhood cancer survivors show success in helping smokers to quit (Emmons et al., 2002).
HEART AND LUNG LATE EFFECTS
Childhood cancer survivors with a history of exposure to certain chemotherapeutic agents (i.e., anthracyclines, notably daunomycin and doxorubicin) or thoracic radiotherapy are at increased risk for late-onset cardiac and pulmonary toxicity. According to recent studies of the CCSS cohort, 18 percent of survivors of childhood brain tumors
reported one or more cardiovascular condition (Gurney et al., 2003). Among the entire cohort, survivors faced an increased risk of a number of pulmonary complications including lung fibrosis, recurrent pneumonia, chronic cough, use of supplemental oxygen, abnormal chest wall, exercise-induced shortness of breath, and bronchitis (Mertens et al., 2002). Chest radiation was associated with a 3.5 percent cumulative incidence of lung fibrosis at 20 years after diagnosis.
Chemotherapy-Induced Heart Damage
Anthracyclines have been used in the treatment of several childhood cancers, including Hodgkin’s and non-Hodgkin’s lymphomas, soft tissue sarcoma, ALL, and Wilms’ tumor. Being female, young age at treatment, higher rate of administration or cumulative dose, and concurrent treatment with chest (mantle) radiation are independent risk factors that contribute to the development of heart abnormalities. The use of drugs that protect the heart (e.g., dexrazoxane) is under investigation and appears to decrease acute toxicity secondary to anthracyclines (Wexler, 1998). Further longitudinal studies will be needed to ascertain their long-term protective action.
Most survivors who develop echocardiographic evidence of left ventricular dysfunction after treatment with an anthracycline will likely remain asymptomatic, but longitudinal studies suggest that a significant proportion of those treated will experience progressive changes and may develop congestive heart failure (Grenier and Lipshultz, 1998; Lipshultz et al., 1995). Within the first 10 years after treatment, about 4 to 5 percent of survivors will have overt congestive heart failure (Lipshultz et al., 1991; Steinherz et al., 1991). However, the incidence of echocardiographically demonstrated severe left ventricular dysfunction increases with the duration of follow-up, and thus, the long-term incidence of survivors who will become symptomatic is likely considerably higher. Late cardiac failure may be induced among those with heart damage by alcohol consumption, physical inactivity, or rapid growth. Importantly, in female survivors, the initial presentation of congestive heart failure may be abruptly precipitated by pregnancy or delivery (Grenier and Lipshultz, 1998; Shan et al., 1996).
In the general population, early identification and aggressive management of left ventricular dysfunction contribute to reductions in morbidity and mortality and improved quality of life. Treatment of asymptomatic patients is associated with a delay in the onset of symptomatic disease, improvement in ejection fractions (percentage of blood ejected from the heart with each beat), and lower rates of death or hospitalization for heart failure (Exner et al., 1999). Treatment of co-morbid conditions and risk factors, such as hypertension, diabetes mellitus, dyslipidemia, and smoking, has been shown to reduce the risk for developing heart failure (McKelvie et
al., 1999). Treatment of congestive heart failure with either an angiotensin-converting enzyme inhibitor or a beta-adrenergic blocking agent (standard drug therapy) results in improved quality of life and reduced mortality rates.
Based on the benefits of early identification, risk modification, and aggressive management of adults in the general population with cardiomyopathy, there is general consensus that periodic monitoring of left ventricular function of asymptomatic survivors who were treated with moderate to high doses of anthracyclines is appropriate, especially for females and those treated at a younger age or with chest radiation (Grenier and Lipshultz, 1998; Lipshultz et al., 1991).
Chemotherapy can also damage the lung (Abid et al., 2001; Ginsberg and Comis, 1982; Mertens et al., 2002; O’Driscoll et al., 1990, 1995). Bleomycin, for example, causes fibrosis of the lung that reduces lung function. Pulmonary toxicity, when it occurs, can cause significant disability. For individuals treated with bleomycin, there is a subsequent risk posed by oxygenation after anesthesia (Goldiner et al., 1978; Goldiner and Schweizer, 1979).
Radiation-Induced Heart and Lung Damage
Radiation damage to the heart has been recognized since the 1960s, and consequently, total pericardial (tissue covering the heart) radiation doses have been reduced to minimize cardiovascular effects. A cohort of patients who survived radiation treatment administered before 1974 suffered high rates of cardiovascular damage. Among 635 pediatric Hodgkin’s disease patients (under age 21) treated using radiotherapy at Stanford University between 1961 and 1991, 7 of 12 deaths observed 3 to 22 years after radiation were due to acute myocardial infarction (Hancock et al., 1993; Leonard et al., 2000). Radiation-related valvular disease (Carlson et al., 1991), pericardial thickening, and ischemic heart disease have been observed among those with radiation exposure to the heart. Investigators have concluded that symptomatic disease may not appear for many years following mediastinal irradiation (Green et al., 1987). Little is known of the effects of lower dose radiation therapy currently in use (from 15 to 25 Gy).
Radiation therapy and chemotherapy (carmustine [BCNU], high dose cyclophosphamide) can also contribute to lung dysfunction and disease. Chest and thoracic irradiation can adversely affect lung function, for example, by inhibiting chest wall growth that may in turn diminish lung volume. These pulmonary effects may be subtle and may be only indirectly associated with cancer treatment. Lung volume may be reduced, for example, if individuals avoid exercise that has become difficult.
LATE EFFECTS INVOLVING ENDOCRINE FUNCTION AND FERTILITY
Endocrine complications are among the most prevalent late effects experienced by survivors of childhood cancer, affecting 20 to 50 percent of survivors who have been followed into adulthood (Friedrich, 2001; Gurney et al., 2003; Oberfield and Sklar, 2002). A common delayed effect of radiation therapy for Hodgkin’s disease, brain tumors, and ALL is thyroid dysfunction, including hypothyroidism, hyperthyroidism, goiter, or nodules (Sklar et al., 2000). The high risk of thyroid disease persists more than 25 years after patients receive radiation therapy for Hodgkin’s disease. The consequences of cranial irradiation can include growth hormone deficiency, delayed or precocious puberty, and hypopituitarism. Effects depend on dose, age at time of exposure, and gender. Hormonal alterations can be successfully treated, but concerns have been raised that such treatment may, in some cases, increase the risk of the development of second cancers. A recent study, for example, found an increased risk of second malignant neoplasms in childhood cancer survivors who had received growth hormone therapy for growth hormone deficiency following cranial irradiation for childhood cancer (Sklar et al., 2002). Other studies of more heterogeneous populations have not identified an increased risk of leukemia among patients treated with growth hormone, an unknown number of whom were childhood cancer survivors (Fradkin et al., 1993). Additional research is needed to clarify the risks associated with hormone therapy.
Growth
Linear growth (height) may be inhibited by cranial irradiation through its effect on the hypothalamic/pituitary axis (see also effects on the skeleton and muscles below). The effect is dose- and age-dependent. Patients treated with large doses of whole-brain radiotherapy, usually for brain tumors, are likely to have severe growth hormone deficiency necessitating hormone replacement. Lower doses of radiation, those typical for treatment of leukemia, may result in less dramatic retardation of growth. The growth of children treated for leukemia is often impaired when exposed to total body radiation and/or high-dose chemotherapy prior to bone marrow transplantation (Clement-De Boers et al., 1996; Hovi et al., 1990; Huma et al., 1995; Sanders et al., 1986; Wingard et al., 1992).
Spinal radiotherapy can compound loss in stature secondary to the direct inhibition of vertebral body growth (Donaldson et al., 1988; Probert and Parker, 1975; Riseborough et al., 1976). Early onset of puberty is common after cranial radiation, further reducing ultimate height. The younger the child is at the time of radiation, the earlier the onset of puberty.
Growth hormone treatment increases growth velocity in patients at risk for growth retardation (Giorgiani et al., 1995; Leiper et al., 1987; Papadimitriou et al., 1991). Growth hormone administration beginning shortly after completion of therapy is being assessed. Close monitoring of growth is recommended but may not be sufficient. Early onset of puberty with consequent early epiphyseal fusion will prevent successful interventions.
The sensitivity of adipose tissue to radiation may lead to asymmetric fat distribution with weight gain later in life. Breast asymmetry may occur among females unilaterally irradiated prior to maturity. High doses may stop breast development completely. These effects are decreased or eliminated by reducing radiation doses or fields.
Obesity
Adult survivors of childhood acute lymphoblastic leukemia, particularly females treated at a younger age and previously treated with cranial radiotherapy with cumulative doses of 20 Gy or more have been found to be at a marked increased risk for obesity (Didi et al., 1995; Schell et al., 1992; Van Dongen-Melman et al., 1995; Zee and Chen, 1986). Adult survivors were at two to three times the risk for obesity, relative to sibling controls (i.e., the age- and race-adjusted odds ratio (OR) was 2.59 for females and 1.86 for males). Adult leukemia survivors appear to be more likely to be physically inactive and have reduced exercise capacity, further increasing their risk for obesity (Black et al., 1998; Jenney et al., 1995; Oeffinger et al., 2001; Warner et al., 1998).
A study of both children and adult survivors of ALL found a higher risk of obesity (Mayer et al., 2000). In the cranially irradiated patients, the likely causes of this increased risk included low physical activity, low resting metabolic rate, and hormonal insufficiency.
Interventions to prevent obesity and promote physical activity have been shown to reduce cardiovascular morbidity and mortality and improve quality of life in the general population, and likewise should lower risk in adult survivors. Periodic follow-up to assess weight and physical activity levels and to screen for potential obesity-related diseases is important for adult survivors of childhood cancer, especially those who were treated with cranial irradiation.
Fertility and Reproduction
Treatment with radiation therapy or chemotherapy may have adverse effects on germ cell survival (i.e., ova and sperm), fertility, and the health of offspring (Green et al., 2002a; Green et al., 2002b). Most girls whose
entire abdomen or craniospinal area was irradiated fail to enter puberty. Females who maintain or recover ovarian function may enter menopause prematurely. For these women, family planning discussions are important because they may be fertile for only a relatively short period of time. Exposure of the ovary and the dose of radiation affect subsequent ovarian function. Ovarian damage results in both sterilization and loss of hormone production. Ovulating females who receive total body irradiation prior to bone marrow transplantation develop amenorrhea and fewer than 10 percent of women recover normal ovarian function. Reduction in doses of chemotherapeutic agents responsible for ovarian damage has led to improvements in female fertility. Procedures to move the ovaries out of the field of radiation (oophoropexy) have also been used to avoid reproductive late effects.
Males can become infertile following treatment with chemotherapy and radiation, but usually maintain normal hormonal production. Changes in chemotherapy (reduction or elimination of use of alkylating agents) have reduced male infertility following treatment. Sexually mature males about to begin any treatment that could adversely impact fertility should be informed and offered the option of preserving sperm prior to treatment so that the option of artificial insemination is available later.
Hyperprolactinemia, characterized by problems with fertility, growth, and libido, can result after radiation to the hypothalamic-pituitary axis. Some of those treated with high-dose radiotherapy for CNS tumors (not involving the hypothalamic-pituitary axis) were also found to have this hormonal imbalance (Constine et al., 1993; Duffner et al., 1983). Hyperprolactinemia is treatable if identified.
A review of the pregnancy outcomes of female participants in the CCSS showed no adverse outcomes associated with chemotherapeutic agents, but pelvic irradiation increased the risk for low birth weight (Green et al., 2002b). The contribution of somatic or germ cell damage following therapy to the occurrence of low birth weight among offspring of survivors of childhood cancer is not known. Female survivors of Wilms’ tumor treated with radiation of the kidney are at increased risk of fetal malposition and premature labor. The offspring of female Wilms’ tumor survivors are at risk for low birthweight, premature birth, and the occurrence of congenital malformations (Green et al., 2002a). There were fewer males among the offspring of the partners of the male CCSS participants, as compared with the offspring of the partners of the male siblings, raising the possibility that therapy preferentially interferes with the progression of male fetuses in pregnancies in partners of these survivors (Green et al., 2003 [in press]).
Several recent studies did not identify an increased frequency of major congenital malformations (Byrne et al., 1998; Dodds et al., 1993; Green et al., 1991, 1997; Hawkins, 1991; Janov et al., 1992; Kenney et al., 1996;
Nygaard et al., 1991), genetic disease (Byrne et al., 1998) or childhood cancer (Green et al., 1997; Hawkins et al., 1989; Mulvihill et al., 1987) in the offspring of former pediatric cancer patients, including those conceived after bone marrow transplantation (Sanders et al., 1996), suggesting that the health of offspring appears to be normal.
MUSCULOSKELETAL LATE EFFECTS
Growing children are vulnerable to the effects on their bones of radiation and chemotherapy. Radiation can cause soft tissue hypoplasia (growth impairment), diminution of bone growth, avascular necrosis (circulatory-related tissue damage) (Donaldson and Kaplan, 1982; Libshitz and Edeiken, 1981; Mauch et al., 1983), and epiphyseal slippage (slippage of the bone growth plate) (Dickerman et al., 1979; Silverman et al., 1981). Asymmetric radiation exposure can result in differential growth and lead to functional disabilities, pain, and asymmetric appearance, for example, secondary to scoliosis. These effects of radiation may not be apparent at the end of therapy but emerge with growth, especially during the pubertal growth spurt. Some chemotherapeutic agents (e.g., corticosteroids, methotrexate) also directly affect bone growth. Other agents can indirectly affect growth through damage to hormonal systems (e.g., pituitary-hypothalamic or gonadal dysfunction) (see section above). Treatment regimens for ALL, lymphomas, brain tumors, Wilms’ tumor, and sarcomas make survivors particularly vulnerable to these musculoskeletal effects.
Decreased bone mineral density is a multifactorial disorder that is being recognized with increased frequency among survivors of brain tumors (Barr et al., 1998), acute lymphoblastic leukemia (Aisenberg et al., 1998; Arikoski et al., 1998; Nysom et al., 1998), lymphoma (Aisenberg et al., 1998), and solid tumors (Aisenberg et al., 1998). Important risk factors include gonadal dysfunction (Aisenberg et al., 1998), male gender (Arikoski et al., 1998), and prior cranial irradiation (Arikoski et al., 1998; Nysom et al., 1998). Treatment with corticosteroids and methotrexate may impair mineralization (Leiper et al., 1998). These patients may be at increased risk for pathologic fractures as the result of failure to achieve maximal bone mineral accretion during adolescence (Carrascosa et al., 1995). The value of treatment with calcium supplementation, growth hormone, and androgen or estrogen replacement therapy is unknown.
Measures to prevent or reverse bone loss are needed to counter the development of osteoporosis and subsequent bone fractures. Long-term survivors of childhood cancer should be periodically assessed to determine risk for osteoporosis and counseled regarding adequate calcium intake and the benefits of exercise and avoidance of smoking. Exercise, in particular,
is known to be effective in increasing bone density among children (Gutin et al., 1999) and young adults (Valdimarsson et al., 1999).
SECOND MALIGNANCIES
The cumulative risk of second malignant cancers 20 years following primary treatment for childhood cancer varies between 3 and 10 percent and is 5 to 20 times greater than that expected in the general population. Radiation therapy is associated with the development of thyroid cancer, breast cancer, melanoma and other skin cancers, brain tumors, and bone and soft tissue sarcomas. Certain types of chemotherapy (i.e., alkylating agents, topoisomerase II inhibitors) are associated with the development of leukemia. Reductions in dose or elimination of radiation for certain embryonal tumors and the reduction in use and alteration in schedule of certain specific drugs may reduce the risk of second malignant cancers. Certain high-risk groups of patients have been identified as those for whom therapy should be modified. An estimated 10 percent of children with ALL, for example, have a defect in a drug-metabolizing enzyme (thiopurine methyltransferase [TPMT]), which places them at increased risk for the development of a second cancer (McLeod et al., 2000).
Women who were treated with chest (mantle) irradiation for childhood Hodgkin’s disease face a significant increase in risk for development of breast cancer, with a cumulative incidence of about 35 percent at 20 to 25 years post therapy (Aisenberg et al., 1997; Bhatia et al., 1996). Onset of breast cancer has been noted as early as eight years post radiation, with a median age at diagnosis of 31.5 years (Bhatia et al., 1996) and a median interval from radiation of 15.7 years (Neglia et al., 2001). It appears that pathologic features and prognosis for breast cancer in Hodgkin’s survivors are similar to those for the general population (Wolden et al., 2000). Like-wise, 5-year survival is strongly associated with stage of disease at time of diagnosis (Cutuli et al., 2001).
There is no consensus about when women who were treated with thoracic radiation therapy should initiate mammographic screening and how frequently they should be screened. The issues surrounding this controversy—usefulness of mammography in dense premenopausal breast, enhancement of breast cancer risk with irradiation exposure by mammography (and the potential for a synergistic effect of irradiation following cancer and its treatment), when to screen girls irradiated in childhood—are areas that require further study.
Children who received radiation or chemotherapeutic agents with known carcinogenic effects should be informed of their risk and should be seen regularly by a health care provider familiar with their treatment and
risks who can evaluate early signs and symptoms appropriately. Some survivors of childhood cancers are at increased risk because they have a genetic form of a disease that predisposes them to other cancers. Survivors of the genetic form of retinoblastoma, for example, face risks as high as 50 percent of subsequent secondary cancers over their lifetime. Other rare syndromes predispose survivors to second malignancies (e.g., Li-Fraumeni syndrome, familial polyposis coli).
Skin is sensitive to radiation carcinogenesis, especially at a young age. Doses of radiation used in the treatment of childhood cancers, such as Hodgkin’s and non-Hodgkin’s lymphomas, soft tissue sarcoma, and Wilms’ tumor, are associated with an increased risk for basal cell carcinoma and squamous cell carcinoma (Meadows et al., 1985; Olsen et al., 1993; Swerdlow et al., 1997). Although some follow-up studies of cancer patients have demonstrated an increased risk for malignant melanoma, it is not clear how much, if any, of the excess risk is due to radiation therapy (Shore, 2001). Cancers occur on areas of the skin that were exposed to the radiation. Whether sun protection will lower risk is not known (Lichter et al., 2000; Ron et al., 1991; Ron et al., 1998). However, in recognition of the increased risk for skin cancer after radiation and the benefits of early diagnosis and treatment, it is recommended that health care providers counsel survivors regarding methods of sun protection, the ABCD (Asymmetry, Border, Color, Diameter) rule for early detection of skin cancer, and the importance of periodic examination of the skin in and around the radiation field. Among the general population, public education regarding sun protection and self-examination has been associated with earlier stage of disease at diagnosis (Rhodes, 1995).
OTHER ORGAN DAMAGE
Liver
Because many children with cancer receive blood products during therapy, patients treated before adequate blood donor screening for hepatitis C was initiated in the early 1990s are at risk for chronic liver disease. Estimates of prevalence of exposure to hepatitis C (i.e., as evidenced by presence of hepatitis C viral [HCV] RNA) among ALL and other pediatric cancer patients treated before 1990 ranges from 7 to 49 percent, with an unknown, and likely sizable, percentage of survivors never having been tested or aware of their risk (Dibenedetto et al., 1994; Locasciulli et al., 1997; Paul et al., 1999; Strickland et al., 2000). The health consequences of exposure to hepatitis C among ALL survivors are not well understood. In an Italian study, only two of the 56 HCV-RNA seropositive patients had persistently elevated alanine aminotransferase (ALT) tests for liver inflam
mation over the course of a mean follow-up of 17 years (Locasciulli and Alberti, 1995). In contrast, Paul et al. reported more serious progression— 12 percent of 75 leukemia survivors were HCV seropositive, 6 of 9 had liver biopsies that showed at least moderate portal inflammation, and half had bridging scarring, consistent with early cirrhosis (Paul et al., 1999).
In the general population, chronic HCV infection develops in 75 to 85 percent of persons infected with hepatitis C (Alter et al., 1992; Shakil et al., 1995). About 30 to 40 percent of chronically infected persons have persistently normal ALT levels and tend to have indolent disease. The course of progressive liver dysfunction is usually insidious, progressing at a slow rate without symptoms or physical signs in the majority of patients during the first two or more decades after infection. Over a 20- to 30-year period, 20 to 30 percent of patients with untreated HCV will develop cirrhosis or extrahepatic sequelae, such as cryoglobulinemia, porphyria cutanea tarda, or membranoproliferative glomerulonephritis (Fattovich et al., 1997; Poynard et al., 1997; Tong et al., 1995). Alcohol consumption, even in moderate amounts, increases the risk of progression to cirrhosis (Pianko et al., 2000; Wiley et al., 1998).
Successful long-term treatment prior to liver decompensation has rapidly improved in the past decade (e.g., treatment with interferon alpha2b and ribavirin) (Lindsay et al., 2001; Poynard et al., 1998). Thus, identification of survivors who were treated with blood products prior to July 1992, determination of their HCV-RNA status, assessment of the liver function of those infected, counseling regarding alcohol consumption, and appropriate treatment and follow-up are essential to reduce the risk for potentially life-threatening sequelae.
Radiation at high doses can also lead to liver damage (e.g., fibrosis).
Kidney and Bladder
Chemotherapy (e.g., cisplatin, ifosfamide), aminoglycoside antibiotics, and some antifungal agents, such as amphotericin B can cause renal failure or damage. Other renal late effects occur secondary to radiation exposure.
Cystitis may occur following treatment with oxazaphosphorine alkylating agents. In one study, the frequency of bladder toxicity was 34 percent among 50 patients treated with pelvic irradiation and cyclophosphamide, compared with 8 percent among 60 patients who received extrapelvic irradiation and cyclophosphamide (Jayalakshmamma and Pinkel, 1976). Medications are now used to protect the bladder from chemotherapy damage, but patients treated before these bladder-protective drugs became available in the late 1990s sometimes sustained damage to the bladder.
Wilms’ tumor may be treated by nephrectomy, which sometimes leads to the need for dialysis and transplantation. This occurs rarely and is a
greater risk in children with tumors involving both kidneys and those with aniridia or Denys-Drash syndrome (Breslow et al., 2000; Ritchey et al., 1996).
Gastrointestinal
Chemotherapy, radiation therapy, and surgery can contribute to fibrosis (scarring) or inflammation that can interfere with the function of the intestine. Fibrosis and inflammation can also be caused by chronic graft-versus-host disease following allogenic bone marrow transplant. Adhesions, obstructions, ulcers, diarrhea, constipation, and malabsorption can result.
Dental
Radiation therapy that includes the mandible, as for some head and neck cancers and for upper cervical radiation therapy for Hodgkin’s disease, can disturb the growth of teeth and affect tooth enamel (e.g., cause pitting) (Jaffe et al., 1984). Dry mouth (xerostomia) due to damage to salivary glands is a common side effect of radiation to the head and neck and medication (Marks et al., 1981; Mira et al., 1981). Lack of saliva predisposes the mouth to oral infection and increases the risk of caries. Administration of amifostine appears to decrease the frequency of chronic xerostomia following irradiation for head and neck cancer (Wasserman et al., 2000). Dry mouth and tooth decay also occur as a consequence of chronic graft-versus-host disease following allogeneic bone marrow transplants.
Sensory Loss
Primary tumors of the CNS, middle ear, and orbital area may be associated with loss of vision and hearing. Radiation therapy may injure the eye lens, retina, or optic nerve and contribute to the formation of cataracts. Prolonged steroid use may also cause cataracts. Hearing loss, which may be reversible, is associated with radiation and long-term administration of several chemotherapies, including cisplatin. The aminoglycoside antibiotics may also produce ototoxicity.
Immune Function
Radiation, chemotherapy, bone marrow transplantation, and removal (or irradiation) of the spleen can impair immune function and decrease the production of blood cells (myelosuppression). The risks of infection among
survivors of Hodgkin’s disease following removal or irradiation of the spleen are well documented. Children with non-Hodgkin’s lymphoma treated with high-dose radiation to the spleen may also face a higher risk of subsequent infections. Total body irradiation prior to bone marrow transplantation may also impair immune system function. In general, the long-term effects of chemotherapy on bone marrow function have not been evaluated exhaustively, but may result in myelosuppression. Administration of the pneumococcal vaccine and the use of prophylactic antibiotics for indefinite periods diminish the risk of infections among those whose spleen has been removed or damaged. Monitoring survivors for immunohematologic dysfunction includes eliciting a detailed history and conducting physical exams for signs and symptoms of recurrent infection, anemia, or bleeding easily.
LATE EFFECTS EMERGING IN ADULTHOOD
Some late effects occur many years after treatment, have an asymptomatic interval, and then become symptomatic only with end-stage or progressive disease, often with devastating consequences. Because the population of adult survivors of childhood cancer is still relatively young, with only a small percentage over the age of 40, very little is known of the eventual effects of cancer and its treatment in older age. Will survivors who experience cognitive dysfunction and neuropathologic changes from cranial irradiation experience premature dementia-type illnesses? Will survivors of soft tissue sarcoma who often experience skeletal problems and asymmetric growth secondary to radiation be at increased risk for premature joint deterioration and chronic muscle spasm and pain? Will clinical or subclinical organ toxicity predispose survivors to premature organ dysfunction/ failure? How persistent is the risk of second cancers? Only through long-term follow-up of adult survivors will the impact of these types of late effects on the aging process become evident.
SUMMARY AND CONCLUSIONS
Complications, disabilities, or adverse outcomes that are the result of the disease process, the treatment, or both, are generally referred to as “late effects.” Estimates are that as many as two-thirds of survivors will experience a late effect, with perhaps a quarter of survivors experiencing one that is severe or life-threatening. The most common late effects of childhood cancer include those that are neurocognitive and psychological, cardiopulmonary, endocrine (e.g., those affecting growth and fertility), musculoskeletal, and recurrent or second malignancies. The emergence of late effects
depends on many factors, including age, exposures to chemotherapy and radiation during treatment (doses and parts of body exposed), and the severity of disease. Complicating the management of late effects is their variable nature. Some may be identified and treated early in follow-up or during the childhood or adolescent years, and resolve without consequence. Others may persist from childhood or arise in adulthood to become chronic problems or influence the progression of other diseases associated with aging. Evidence is lacking for many aspects of care, but does suggest that at least some late effects can be successfully prevented, some can be treated, and others can be managed with expert care.
Assessments of neurocognitive late effects have often been made among ALL survivors. These survivors have a greater likelihood of being placed in special education or learning disabled programs than their siblings, but most are able to compensate and adapt to overcome these problems. Survivors with substantial physical late effects, learning problems, or relapse are more likely than survivors without late effects to show evidence of lower self-esteem, poorer adjustment, and worse quality of life. Some recent research points to psychological problems (Zeltzer et al., 1997) as a result of poor academic achievement secondary to neurocognitive late effects. Psychosocial effects extend to the entire family with recent evidence pointing to significant dysfunction among both siblings and parents of survivors.
The cumulative risk of second malignant cancers 20 years following primary treatment for childhood cancer varies between 3 and 10 percent and is 5 to 20 times greater than that expected in the general population. Despite their increased risks for second cancers, smoking rates among survivors of childhood cancer appear to be equal to those in the general population. Preliminary evidence suggests that there are ways to intervene with tailored smoking cessation interventions in this high-risk population.
Other commonly reported late effects include late-onset cardiac and pulmonary disease among childhood cancer survivors with a history of exposure to certain chemotherapeutic agents (i.e., anthracyclines, notably daunorubicin and doxorubicin) or thoracic radiotherapy; thyroid dysfunction following radiation therapy for Hodgkin’s disease, brain tumors, and ALL; alterations in growth and maturation (e.g., growth hormone deficiency, delayed or precocious puberty, hypopituitarism) following cranial irradiation; obesity among survivors of ALL; and fertility problems following radiation therapy or chemotherapy. Not well understood are the consequences of late effects among the aging population of childhood cancer survivors. Research is needed to identify these consequences and effective methods to ameliorate them.
REFERENCES
Abid SH, Malhotra V, Perry MC. 2001. Radiation-induced and chemotherapy-induced pulmonary injury. Curr Opin Oncol 13(4):242-8.
Aisenberg AC, Finkelstein DM, Doppke KP, Koerner FC, Boivin JF, Willett CG. 1997. High risk of breast carcinoma after irradiation of young women with Hodgkin’s disease. Cancer 79(6):1203-10.
Aisenberg J, Hsieh K, Kalaitzoglou G, Whittam E, Heller G, Schneider R, Sklar C. 1998. Bone mineral density in young adult survivors of childhood cancer. J Pediatr Hematol Oncol 20(3):241-5.
Alter MJ, Margolis HS, Krawczynski K, Judson FN, Mares A, Alexander WJ, Hu PY, Miller JK, Gerber MA, Sampliner RE, et al. 1992. The natural history of community-acquired hepatitis C in the United States. The Sentinel Counties Chronic non-A, non-B Hepatitis Study Team. N Engl J Med 327(27):1899-905.
American Psychiatric Association. 1998. Diagnostic and Statistical Manual of Mental Disorders. Amer Psych Assn.
American Cancer Society. 2000. Cancer Facts and Figures, 2000. Atlanta, GA: American Cancer Society.
Arikoski P, Komulainen J, Voutilainen R, Riikonen P, Parviainen M, Tapanainen P, Knip M, Kroger H. 1998. Reduced bone mineral density in long-term survivors of childhood acute lymphoblastic leukemia. J Pediatr Hematol Oncol 20(3):234-40.
Armstrong FD, Blumberg MJ, Toledano SR. 1999. Neurobehavioral issues in childhood cancer. School Psychology Review 28(2):1940-2203.
Arnholt UV, Fritz GK, Keener M. 1993. Self-concept in survivors of childhood and adolescent cancer. Journal of Psychosocial Oncology 11(1):1-16.
Barakat LP, Kazak AE, Meadows AT, Casey R, Meeske K, Stuber ML. 1997. Families surviving childhood cancer: a comparison of posttraumatic stress symptoms with families of healthy children. J Pediatr Psychol 22(6):843-59.
Barbarin OA, Sargent JR, Sahler OJZ, Carpenter PJ, Copeland DR, Dolgin MJ, Mulhern RK, Roghmann KJ, Zeltzer LK. 1995. Sibling adaptation to childhood cancer collaborative study: Parental views of pre- and postdiagnosis adjustment of siblings of children with cancer. Journal of Psychosocial Oncology 13(3):1-20.
Barr RD, Simpson T, Webber CE, Gill GJ, Hay J, Eves M, Whitton AC. 1998. Osteopenia in children surviving brain tumours. Eur J Cancer 34(6):873-7.
Bhatia S, Robison LL, Oberlin O, Greenberg M, Bunin G, Fossati-Bellani F, Meadows AT. 1996. Breast cancer and other second neoplasms after childhood Hodgkin’s disease. N Engl J Med 334(12):745-51.
Black P, Gutjahr P, Stopfkuchen H. 1998. Physical performance in long-term survivors of acute leukaemia in childhood. Eur J Pediatr 157(6):464-7.
Breslow NE, Takashima JR, Ritchey ML, Strong LC, Green DM. 2000. Renal failure in the Denys-Drash and Wilms’ tumor-aniridia syndromes. Cancer Res60(15):4030-2.
Brouwers P, Neelam J, Krull K, Law R, Fruge E, Bottonley S, Dreyer Z. 2002. Academic and Neurobehavioral Functioning in Long-Term Survivors of Childhood Cancer: Relation to Depression and Anxiety. Cancer Survivorship: Resilience Across the Lifespan, June 2-4, 2002. Washington, DC: National Cancer Institute and American Cancer Society.
Butler R, Copeland D, Fairclugh D, Katz E, Kazak A, Mulhern R, Noll R, Sahler OJ. 2002. Neuropsychological Processes and Their Remediation in Children Treated for Cancer. Cancer Survivorship: Resilience Across the Lifespan, June 2-4, 2002. Washington, DC: National Cancer Institute and American Cancer Society.
Byrne J, Rasmussen SA, Steinhorn SC, Connelly RR, Myers MH, Lynch CF, Flannery J, Austin DF, Holmes FF, Holmes GE, Strong LC, Mulvihill JJ. 1998. Genetic disease in offspring of long-term survivors of childhood and adolescent cancer. Am J Hum Genet 62(1):45-52.
Carlson RG, Mayfield WR, Normann S, Alexander JA. 1991. Radiation-associated valvular disease. Chest 99(3):538-45.
Carrascosa A, Gussinye M, Yeste D, del Rio L, Audi L. 1995. Bone mass acquisition during infancy, childhood and adolescence. Acta Paediatr Suppl 411:18-23.
Cella DF, Tross S. 1986. Psychological adjustment to survival from Hodgkin’s disease. J Consult Clin Psychol 54(5):616-22.
Challinor J, Karl D. 1995. Educational attainment in survivors of ALL. JAMA 274(14):1134-5.
Chen E, Zeltzer LK, Bentler PM, Byrne J, Nicholson HS, Meadows AT, Mills JL, Haupt R, Fears TR, Robison LL. 1998. Pathways linking treatment intensity and psychosocial outcomes among adult survivors of childhood leukemia. Journal of Health Psychology 3(1):23-38.
Chesler M, Barbarin O. 1987. Childhood Cancer and the Family: Meeting the Challenge of Stress and Support. New York: Brunner/Mazel.
Clement-De Boers A, Oostdijk W, Van Weel-Sipman MH, Van den Broeck J, Wit JM, Vossen JM. 1996. Final height and hormonal function after bone marrow transplantation in children. J Pediatr 129(4):544-50.
Cohen SO, Walco GA. 1999. Dance/movement therapy for children and adolescents with cancer. Cancer Pract 7(1):34-42.
Constine LS, Woolf PD, Cann D, Mick G, McCormick K, Raubertas RF, Rubin P. 1993. Hypothalamic-pituitary dysfunction after radiation for brain tumors. N Engl J Med 328(2):87-94.
Cutuli B, Borel C, Dhermain F, Magrini SM, Wasserman TH, Bogart JA, Provencio M, de Lafontan B, de la Rochefordiere A, Cellai E, Graic Y, Kerbrat P, Alzieu C, Teissier E, Dilhuydy JM, Mignotte H, Velten M. 2001. Breast cancer occurred after treatment for Hodgkin’s disease: analysis of 133 cases. Radiother Oncol 59(3):247-55.
DeLaat CA, Lampkin BC. 1992. Long-term survivors of childhood cancer: evaluation and identification of sequelae of treatment. CA Cancer J Clin 42(5):263-82.
Dibenedetto SP, Ragusa R, Sciacca A, Di Cataldo A, Miraglia V, D’Amico S, Lo Nigro L, Ippolito AM. 1994. Incidence and morbidity of infection by hepatitis C virus in children with acute lymphoblastic leukaemia. Eur J Pediatr 153(4):271-5.
Dickerman JD, Newberg AH, Moreland MD. 1979. Slipped capital femoral epiphysis (SCFE) following pelvic irradiation for rhabdomyosarcoma. Cancer 44(2):480-2.
Didi M, Didcock E, Davies HA, Ogilvy-Stuart AL, Wales JK, Shalet SM. 1995. High incidence of obesity in young adults after treatment of acute lymphoblastic leukemia in childhood. J Pediatr 127(1):63-7.
Dodds L, Marrett LD, Tomkins DJ, Green B, Sherman G. 1993. Case-control study of congenital anomalies in children of cancer patients. BMJ 307(6897):164-8.
Dolgin MJ, Blumensohn R, Mulhern RK, Orbach J, Sahler OJ, Roghmann KJ, Carpenter PJ, Barbarin OA, Sargent JR, Zeltzer LK, Copeland DR. 1997. Sibling Adaptation to Childhood Cancer Collaborative Study: cross-cultural aspects. Journal of Psychosocial Oncology 15 (1):1-14.
Donaldson SS. 1993. Lessons from our children. International Journal of Radiation Oncology, Biology, Physics 26(5):739-749.
Donaldson SS, Kaplan HS. 1982. Complications of treatment of Hodgkin’s disease in children. Cancer Treat Rep 66(4):977-89.
Dreyer ZE, Blatt J, Bleyer A. 2002. Late Effects of Childhood Cancer and its Treatment. Pizzo PA, Poplack DG, Eds. Principles and Practice of Pediatric Oncology. 4th ed. Philadelphia: Lippincott Williams & Wilkins.
Duffner PK, Cohen ME, Anderson SW, Voorhess ML, MacGillivray MH, Panahon A, Brecher ML. 1983. Long-term effects of treatment on endocrine function in children with brain tumors. Ann Neurol 14(5):528-32.
Eiser C, Havermans T. 1994. Long term social adjustment after treatment for childhood cancer. Archives of Disease in Childhood 70(1):66-70.
Eiser C, Hill JJ, Vance YH. 2000. Examining the psychological consequences of surviving childhood cancer: systematic review as a research method in pediatric psychology. J Pediatr Psychol 25(6):449-60.
Elkin TD, Phipps S, Mulhern RK, Fairclough D. 1997. Psychological functioning of adolescent and young adult survivors of pediatric malignancy. Med Pediatr Oncol 29(6): 582-8.
Emmons K, Li FP, Whitton J, Mertens AC, Hutchinson R, Diller L, Robison LL. 2002. Predictors of smoking initiation and cessation among childhood cancer survivors: a report from the childhood cancer survivor study. J Clin Oncol 20(6):1608-16.
Exner DV, Dries DL, Waclawiw MA, Shelton B, Domanski MJ. 1999. Beta-adrenergic blocking agent use and mortality in patients with asymptomatic and symptomatic left ventricular systolic dysfunction: a post hoc analysis of the Studies of Left Ventricular Dysfunction. J Am Coll Cardiol 33(4):916-23.
Fattovich G, Giustina G, Degos F, Tremolada F, Diodati G, Almasio P, Nevens F, Solinas A, Mura D, Brouwer JT, Thomas H, Njapoum C, Casarin C, Bonetti P, Fuschi P, Basho J, Tocco A, Bhalla A, Galassini R, Noventa F, Schalm SW, Realdi G. 1997. Morbidity and mortality in compensated cirrhosis type C: a retrospective follow-up study of 384 patients. Gastroenterology 112(2):463-72.
Fradkin JE, Mills JL, Schonberger LB, Wysowski DK, Thomson R, Durako SJ, Robison LL. 1993. Risk of leukemia after treatment with pituitary growth hormone. JAMA 270(23): 2829-32.
Friedman DL, Meadows AT. 2002. Late effects of childhood cancer therapy. Pediatr Clin North Am 49(5):1083-106.
Friedrich MJ. 2001. Lowering risk of second malignancy in the survivors of childhood cancer. JAMA 285(19):2435-7.
Fritz GK, Williams JR, Amylon M. 1988. After treatment ends: psychosocial sequelae in pediatric cancer survivors. Am J Orthopsychiatry 58(4):552-61.
Garre ML, Gandus S, Cesana B, Haupt R, De Bernardi B, Comelli A, Ferrando A, Stella G, Vitali ML, Picco P, et al. 1994. Health status of long-term survivors after cancer in childhood. Results of an uniinstitutional study in Italy. Am J Pediatr Hematol Oncol 16(2):143-52.
Ginsberg SJ, Comis RL. 1982. The pulmonary toxicity of antineoplastic agents. Semin Oncol 9(1):34-51.
Giorgiani G, Bozzola M, Locatelli F, Picco P, Zecca M, Cisternino M, Dallorso S, Bonetti F, Dini G, Borrone C, et al. 1995. Role of busulfan and total body irradiation on growth of prepubertal children receiving bone marrow transplantation and results of treatment with recombinant human growth hormone. Blood 86(2):825-31.
Goldiner PL, Schweizer O. 1979. The hazards of anesthesia and surgery in bleomycin-treated patients. Semin Oncol 6(1):121-4.
Goldiner PL, Carlon GC, Cvitkovic E, Schweizer O, Howland WS. 1978. Factors influencing postoperative morbidity and mortality in patients treated with bleomycin. Br Med J 1(6128):1664-7.
Gray RE, Doan BD, Shermer P, FitzGerald AV, Berry MP, Jenkin D, Doherty MA. 1992. Psychologic adaptation of survivors of childhood cancer. Cancer 70(11):2713-21.
Green DM, Gingell RL, Pearce J, Panahon AM, Ghoorah J. 1987. The effect of mediastinal irradiation on cardiac function of patients treated during childhood and adolescence for Hodgkin’s disease. J Clin Oncol 5(2):239-45.
Green DM, Zevon MA, Lowrie G, Seigelstein N, Hall B. 1991. Congenital anomalies in children of patients who received chemotherapy for cancer in childhood and adolescence. N Engl J Med 325(3):141-6.
Green DM, Fiorello A, Zevon MA, Hall B, Seigelstein N. 1997. Birth defects and childhood cancer in offspring of survivors of childhood cancer. Arch Pediatr Adolesc Med 151(4): 379-83.
Green DM, Peabody EM, Nan B, Peterson S, Kalapurakal JA, Breslow NE. 2002a. Pregnancy outcome after treatment for Wilms tumor: a report from the National Wilms Tumor Study Group. J Clin Oncol 20(10):2506-13.
Green DM, Whitton JA, Stovall M, Mertens AC, Donaldson SS, Ruymann FB, Pendergrass TW, Robison LL. 2002b. Pregnancy outcome of female survivors of childhood cancer: a report from the Childhood Cancer Survivor Study. Am J Obstet Gynecol 187(4): 1070-80.
Green DM, Whitton JA, Stovall M, Mertens AC, Donaldson SS, Ruymann FB, Pendergrass TW, Robison LL. 2003. Pregnancy outcome of partners of male survivors of childhood cancer: a report from the Childhood Cancer Survivor Study. J Clin Oncol, Feb. 15; 21(4):716-21.
Greenberg DB, Kornblith AB, Herndon JE, Zuckerman E, Schiffer CA, Weiss RB, Mayer RJ, Wolchok SM, Holland JC. 1997. Quality of life for adult leukemia survivors treated on clinical trials of Cancer and Leukemia Group B during the period 1971-1988: predictors for later psychologic distress. Cancer 80(10):1936-44.
Greenberg HS, Kazak AE, Meadows AT. 1989. Psychologic functioning in 8- to 16-year-old cancer survivors and their parents. J Pediatr 114(3):488-93.
Grenier MA, Lipshultz SE. 1998. Epidemiology of anthracycline cardiotoxicity in children and adults. Semin Oncol 25(4 Suppl 10):72-85.
Gurney JG, Kadan-Lottick NS, Packer RJ, Neglia JP, Sklar CA, Punyko JA, Stovall M, Yasui Y, Nicholson HS, Wolden S, McNeil DE, Mertens AC, Robison LL. 2003. Endocrine and cardiovascular late effects among adult survivors of childhood brain tumors. Cancer 97(3):663-73.
Gutin B, Owens S, Okuyama T, Riggs S, Ferguson M, Litaker M. 1999. Effect of physical training and its cessation on percent fat and bone density of children with obesity. Obes Res 7(2):208-14.
Haase JE, Rostad M. 1994. Experiences of completing cancer therapy: children’s perspectives. Oncol Nurs Forum 21(9):1483-92; discussion 1493-4.
Hancock SL, Tucker MA, Hoppe RT. 1993. Breast cancer after treatment of Hodgkin’s disease. J Natl Cancer Inst 85(1):25-31.
Haupt R, Byrne J, Connelly RR, Mostow EN, Austin DF, Holmes GR, Holmes FF, Latourette HB, Teta MJ, Strong LC, et al. 1992. Smoking habits in survivors of childhood and adolescent cancer. Med Pediatr Oncol 20(4):301-6.
Haupt R, Fears TR, Robison LL, Mills JL, Nicholson HS, Zeltzer LK, Meadows AT, Byrne J. 1994. Educational attainment in long-term survivors of childhood acute lymphoblastic leukemia. JAMA 272(18):1427-32.
Haupt R, Zeltzer L, Byrne J. 1995. In reply to educational attainment in survivors of ALL. JAMA 274(14):1135.
Hawkins MM. 1991. Is there evidence of a therapy-related increase in germ cell mutation among childhood cancer survivors? J Natl Cancer Inst 83(22):1643-50.
Hawkins MM, Draper GJ, Smith RA. 1989. Cancer among 1,348 offspring of survivors of childhood cancer. Int J Cancer 43(6):975-8.
Hobbie WL, Stuber M, Meeske K, Wissler K, Rourke MT, Ruccione K, Hinkle A, Kazak AE. 2000. Symptoms of posttraumatic stress in young adult survivors of childhood cancer. J Clin Oncol 18(24):4060-6.
Hollen PJ. 2000. A clinical profile to predict decision making, risk behaviors, clinical status, and health-related quality of life for cancer-surviving adolescents. Part 1. Cancer Nurs 23(4):247-57.
Hollen PJ, Hobbie WL. 1993. Risk taking and decision making of adolescent long-term survivors of cancer. Oncol Nurs Forum 20(5):769-76.
Hollen PJ, Hobbie WL. 1996. Decision making and risk behaviors of cancer-surviving adolescents and their peers. J Pediatr Oncol Nurs 13(3):121-33; discussion 135-7.
Hollen PJ, Hobbie WL, Finley SM. 1997. Cognitive late effect factors related to decision making and risk behaviors of cancer-surviving adolescents. Cancer Nurs 20(5):305-14.
Hollen PJ, Hobbie WL, Finley SM, Hiebert SM. 2001. The relationship of resiliency to decision making and risk behaviors of cancer-surviving adolescents. J Pediatr Oncol Nurs 18(5):188-204.
Hovi L, Rajantie J, Perkkio M, Sainio K, Sipila I, Siimes MA. 1990. Growth failure and growth hormone deficiency in children after bone marrow transplantation for leukemia. Bone Marrow Transplant 5(3):183-6.
Huma Z, Boulad F, Black P, Heller G, Sklar C. 1995. Growth in children after bone marrow transplantation for acute leukemia. Blood 86(2):819-24.
Irwin CE. 1993. Adolescence and risk taking: How are they related? Bell NJ, Bell RW, eds. Adolescent Risk Taking.: Newbury Park, CA: Sage Publications. Pp. 1-28.
Iuvone L, Mariotti P, Colosimo C, Guzzetta F, Ruggiero A, Riccardi R. 2002. Long-term cognitive outcome, brain computed tomography scan, and magnetic resonance imaging in children cured for acute lymphoblastic leukemia. Cancer 95(12):2562-70.
Jaffe N, Toth BB, Hoar RE, Ried HL, Sullivan MP, McNeese MD. 1984. Dental and maxillo-facial abnormalities in long-term survivors of childhood cancer: effects of treatment with chemotherapy and radiation to the head and neck. Pediatrics 73(6):816-23.
Janov AJ, Anderson J, Cella DF, Zuckerman E, Kornblith AB, Holland JC, Kantor AF, Li FP, Henderson E, Weiss RB, et al. 1992. Pregnancy outcome in survivors of advanced Hodgkin disease. Cancer 70(3):688-92.
Jayalakshmamma B, Pinkel D. 1976. Urinary-bladder toxicity following pelvic irradiation and simultaneous cyclophosphamide therapy. Cancer 38(2):701-7.
Jenney ME, Faragher EB, Jones PH, Woodcock A. 1995. Lung function and exercise capacity in survivors of childhood leukaemia. Med Pediatr Oncol 24(4):222-30.
Justice B. 1999. Why do women treated for breast cancer report good health despite disease or disability? A pilot study. Psychol Rep 84(2):392-4.
Kazak A, Christakis D, Alderfer MCM. 1994. Young adolescent cancer survivors and their parents: adjustments, learning problems, and gender. Journal of Family Psychology 8 (1):74-84.
Kazak AE, Meadows AT. 1989. Families of young adolescents who have survived cancer: social-emotional adjustment, adaptability, and social support. J Pediatr Psychol 14(2): 175-91.
Kazak AE, Barakat LP, Meeske K, Christakis D, Meadows AT, Casey R, Penati B, Stuber ML. 1997. Posttraumatic stress, family functioning, and social support in survivors of childhood leukemia and their mothers and fathers. J Consult Clin Psychol 65(1):120-9.
Kazak AE, Simms S, Barakat L, Hobbie W, Foley B, Golomb V, Best M. 1999. Surviving cancer competently intervention program (SCCIP): a cognitive-behavioral and family therapy intervention for adolescent survivors of childhood cancer and their families. Fam Process 38(2):175-91.
Kazak AE, Alderfer M, Rourke M, Simms S, Streisand R. 2002. Posttraumatic Stress in Adolescent Survivors of Childhood Cancer and Their Mothers, Father, and Siblings, Poster Presentation. Cancer Survivorship: Resilience Across the Lifespan, June 2-4, 2002. Washington, DC: National Cancer Institute and American Cancer Society.
Keene N, Hobbie W, Ruccione K. 2000. Childhood Cancer Survivors: A Practical Guide to Your Future. Sebastopol, CA: O’Reilly and Associates, Inc.
Kenney LB, Nicholson HS, Brasseux C, Mills JL, Robison LL, Zeltzer LK, Meadows AT, Reaman GH, Byrne J. 1996. Birth defects in offspring of adult survivors of childhood acute lymphoblastic leukemia. A Childrens Cancer Group/National Institutes of Health Report. Cancer 78(1):169-76.
Kingma A, van Dommelen RI, Mooyaart EL, Wilmink JT, Deelman BG, Kamps WA. 2001. Slight cognitive impairment and magnetic resonance imaging abnormalities but normal school levels in children treated for acute lymphoblastic leukemia with chemotherapy only. J Pediatr 139(3):413-20.
Koocher GP, O’Malley JE. 1981. The Damocles Syndrome: Psychosocial Consequences of Surviving Childhood Cancer. New York: McGraw-Hill.
Koocher GP, O’Malley JE, Gogan JL, Foster DJ. 1980. Psychological adjustment among pediatric cancer survivors. Journal of Child Psychology & Psychiatry & Allied Disciplines 21(2):163-73.
Kornblith AB, Herndon JE 2nd, Zuckerman E, Cella DF, Cherin E, Wolchok S, Weiss RB, Diehl LF, Henderson E, Cooper MR, Schiffer C, Canellos GP, Mayer RJ, Silver RT, Schilling A, Peterson BA, Greenberg D, Holland JC. 1998. Comparison of psychosocial adaptation of advanced stage Hodgkin’s disease and acute leukemia survivors. Cancer and Leukemia Group B. Ann Oncol 9(3):297-306.
Kupst MJ, Schulman JL. 1988. Long-term coping with pediatric leukemia: a six-year follow-up study. J Pediatr Psychol 13(1):7-22.
Kupst MJ, Natta MB, Richardson CC, Schulman JL, Lavigne JV, Das L. 1995. Family coping with pediatric leukemia: ten years after treatment. J Pediatr Psychol 20(5):601-17.
Lansky SB, List MA, Ritter-Sterr C. 1986. Psychosocial consequences of cure. Cancer 58(2 Suppl):529-33.
Leiper AD, Stanhope R, Lau T, Grant DB, Blacklock H, Chessells JM, Plowman PN. 1987. The effect of total body irradiation and bone marrow transplantation during childhood and adolescence on growth and endocrine function. Br J Haematol 67(4):419-26.
Leonard GT, Green DM, Spengenthal EL, et al. 2000. Cardiac mortality and morbidity after treatment for Hodgkin disease during childhood or adolescence. Pediatrc Res 47(46A).
Libshitz HI, Edeiken BS. 1981. Radiotherapy changes of the pediatric hip. AJR Am J Roentgenol 137(3):585-8.
Lichter MD, Karagas MR, Mott LA, Spencer SK, Stukel TA, Greenberg ER. 2000. Therapeutic ionizing radiation and the incidence of basal cell carcinoma and squamous cell carcinoma. The New Hampshire Skin Cancer Study Group. Arch Dermatol 136(8):1007-11.
Lindsay KL, Trepo C, Heintges T, Shiffman ML, Gordon SC, Hoefs JC, Schiff ER, Goodman ZD, Laughlin M, Yao R, Albrecht JK. 2001. A randomized, double-blind trial comparing pegylated interferon alfa-2b to interferon alfa-2b as initial treatment for chronic hepatitis C. Hepatology 34(2):395-403.
Lipshultz SE, Colan SD, Gelber RD, Perez-Atayde AR, Sallan SE, Sanders SP. 1991. Late cardiac effects of doxorubicin therapy for acute lymphoblastic leukemia in childhood. N Engl J Med 324(12):808-15.
Lipshultz SE, Lipsitz SR, Mone SM, Goorin AM, Sallan SE, Sanders SP, Orav EJ, Gelber RD, Colan SD. 1995. Female sex and drug dose as risk factors for late cardiotoxic effects of doxorubicin therapy for childhood cancer. N Engl J Med 332(26):1738-43.
Locasciulli A, Alberti A. 1995. Hepatitis C virus serum markers and liver disease in children with leukemia. Leuk Lymphoma 17(3-4):245-9.
Locasciulli A, Testa M, Pontisso P, Benvegnu L, Fraschini D, Corbetta A, Noventa F, Masera G, Alberti A. 1997. Prevalence and natural history of hepatitis C infection in patients cured of childhood leukemia. Blood 90(11):4628-33.
Mackie E, Hill J, Kondryn H, McNally R. 2000. Adult psychosocial outcomes in long-term survivors of acute lymphoblastic leukaemia and Wilms’ tumour: a controlled study. Lancet 355(9212):1310-4.
Maggiolini A, Grassi R, Adamoli L, Corbetta A, Charmet GP, Provantini K, Fraschini D, Jankovic M, Lia R, Spinetta J, Masera G. 2000. Self-image of adolescent survivors of long-term childhood leukemia. J Pediatr Hematol Oncol 22(5):417-21.
Marina N. 1997. Long-term survivors of childhood cancer. The medical consequences of cure. Pediatr Clin North Am 44(4):1021-42.
Marks JE, Davis CC, Gottsman VL, Purdy JE, Lee F. 1981. The effects of radiation on parotid salivary function. Int J Radiat Oncol Biol Phys 7(8):1013-9.
Mauch PM, Weinstein H, Botnick L, Belli J, Cassady JR. 1983. An evaluation of long-term survival and treatment complications in children with Hodgkin’s disease. Cancer 51(5): 925-32.
Mayer EI, Reuter M, Dopfer RE, Ranke MB. 2000. Energy expenditure, energy intake and prevalence of obesity after therapy for acute lymphoblastic leukemia during childhood. Horm Res 53(4):193-9.
McKelvie RS, Benedict CR, Yusuf S. 1999. Evidence based cardiology: prevention of congestive heart failure and management of asymptomatic left ventricular dysfunction. BMJ 318(7195):1400-2.
McLeod HL, Krynetski EY, Relling MV, Evans WE. 2000. Genetic polymorphism of thiopurine methyltransferase and its clinical relevance for childhood acute lymphoblastic leukemia. Leukemia 14(4):567-72.
Meadows AT, Baum E, Fossati-Bellani F, Green D, Jenkin RD, Marsden B, Nesbit M, Newton W, Oberlin O, Sallan SG, et al. 1985. Second malignant neoplasms in children: an update from the Late Effects Study Group. J Clin Oncol 3(4):532-8.
Meeske KA, Ruccione K, Globe DR, Stuber ML. 2001. Posttraumatic stress, quality of life, and psychological distress in young adult survivors of childhood cancer. Oncol Nurs Forum 28(3):481-9.
Meister LA, Meadows AT. 1993. Late effects of childhood cancer therapy. Curr Probl Pediatr 23(3):102-31.
Mertens AC, Yasui Y, Neglia JP, Potter JD, Nesbit ME Jr, Ruccione K, Smithson WA, Robison LL. 2001. Late mortality experience in five-year survivors of childhood and adolescent cancer: the Childhood Cancer Survivor Study. J Clin Oncol 19(13):3163-72.
Mertens AC, Yasui Y, Liu Y, Stovall M, Hutchinson R, Ginsberg J, Sklar C, Robison LL. 2002. Pulmonary complications in survivors of childhood and adolescent cancer. A report from the Childhood Cancer Survivor Study. Cancer 95(11):2431-41.
Mira JG, Wescott WB, Starcke EN, Shannon IL. 1981. Some factors influencing salivary function when treating with radiotherapy. Int J Radiat Oncol Biol Phys 7(4):535-41.
Moller TR, Garwicz S, Barlow L, Falck Winther J, Glattre E, Olafsdottir G, Olsen JH, Perfekt R, Ritvanen A, Sankila R, Tulinius H. 2001. Decreasing late mortality among five-year survivors of cancer in childhood and adolescence: a population-based study in the Nordic countries. J Clin Oncol 19(13):3173-81.
Moore I, Glasser M, Ablin A. 1987. Late psychosocial consequences of childhood cancer. Journal of Pediatric Nursing 3(3):150.
Mulhern RK, Wasserman AL, Fairclough D, Ochs J. 1988. Memory function in disease-free survivors of childhood acute lymphocytic leukemia given CNS prophylaxis with or without 1,800 cGy cranial irradiation. J Clin Oncol 6(2):315-20.
Mulhern RK, Wasserman AL, Friedman AG, Fairclough D. 1989. Social competence and behavioral adjustment of children who are long-term survivors of cancer. Pediatrics 83(1):18-25.
Mulhern RK, Tyc VL, Phipps S, Crom D, Barclay D, Greenwald C, Hudson M, Thompson EI. 1995. Health-related behaviors of survivors of childhood cancer. Med Pediatr Oncol 25(3):159-65.
Mulvihill JJ, Myers MH, Connelly RR, Byrne J, Austin DF, Bragg K, Cook JW, Hassinger DD, Holmes FF, Holmes GF, et al. 1987. Cancer in offspring of long-term survivors of childhood and adolescent cancer. Lancet 2(8563):813-7.
Neglia JP, Nesbit ME Jr. 1993. Care and treatment of long-term survivors of childhood cancer. Cancer 71(10 Suppl):3386-91.
Neglia JP, Friedman DL, Yasui Y, Mertens AC, Hammond S, Stovall M, Donaldson SS, Meadows AT, Robison LL. 2001. Second malignant neoplasms in five-year survivors of childhood cancer: Childhood Cancer Survivor Study. J Natl Cancer Inst 93(8):618-29.
Nolen-Hoeksema S. 1987. Sex differences in unipolar depression: evidence and theory. Psychological Bulletin 101(2):259-82.
Noll RB, MacLean WE Jr, Whitt JK, Kaleita TA, Stehbens JA, Waskerwitz MJ, Ruymann FB, Hammond GD. 1997. Behavioral adjustment and social functioning of long-term survivors of childhood leukemia: parent and teacher reports. J Pediatr Psychol 22(6):827-41.
Nygaard R, Clausen N, Siimes MA, Marky I, Skjeldestad FE, Kristinsson JR, Vuoristo A, Wegelius R, Moe PJ. 1991. Reproduction following treatment for childhood leukemia: a population-based prospective cohort study of fertility and offspring. Med Pediatr Oncol 19(6):459-66.
Nysom K, Holm K, Michaelsen KF, Hertz H, Muller J, Molgaard C. 1998. Bone mass after treatment for acute lymphoblastic leukemia in childhood. J Clin Oncol 16(12):3752-60.
O’Driscoll BR, Hasleton PS, Taylor PM, Poulter LW, Gattameneni HR, Woodcock AA. 1990. Active lung fibrosis up to 17 years after chemotherapy with carmustine (BCNU) in childhood. N Engl J Med 323(6):378-82.
O’Driscoll BR, Kalra S, Gattamaneni HR, Woodcock AA. 1995. Late carmustine lung fibrosis. Age at treatment may influence severity and survival. Chest 107(5):1355-7.
Oberfield SE, Sklar CA. 2002. Endocrine sequelae in survivors of childhood cancer. Adolesc Med 13(1):161-9, viii.
Ochs J, Mulhern R, Fairclough D, Parvey L, Whitaker J, Ch’ien L, Mauer A, Simone J. 1991. Comparison of neuropsychologic functioning and clinical indicators of neurotoxicity in long-term survivors of childhood leukemia given cranial radiation or parenteral methotrexate: a prospective study. J Clin Oncol 9(1):145-51.
Oeffinger KC, Eshelman DA, Tomlinson GE, Buchanan GR, Foster BM. 2000. Grading of late effects in young adult survivors of childhood cancer followed in an ambulatory adult setting. Cancer 88(7):1687-95.
Oeffinger KC, Buchanan GR, Eshelman DA, Denke MA, Andrews TC, Germak JA, Tomlinson GE, Snell LE, Foster BM. 2001. Cardiovascular risk factors in young adult survivors of childhood acute lymphoblastic leukemia. J Pediatr Hematol Oncol 23(7):424-30.
Olsen JH, Garwicz S, Hertz H, Jonmundsson G, Langmark F, Lanning M, Lie SO, Moe PJ, Moller T, Sankila R, et al. 1993. Second malignant neoplasms after cancer in childhood or adolescence. Nordic Society of Paediatric Haematology and Oncology Association of the Nordic Cancer Registries. BMJ 307(6911):1030-6.
Packer RJ, Meadows AT, Rorke LB, Goldwein JL, D’Angio G. 1987. Long-term sequelae of cancer treatment on the central nervous system in childhood. Med Pediatr Oncol 15(5): 241-53.
Papadimitriou A, Urena M, Hamill G, Stanhope R, Leiper AD. 1991. Growth hormone treatment of growth failure secondary to total body irradiation and bone marrow transplantation. Arch Dis Child 66(6):689-92.
Paul IM, Sanders J, Ruggiero F, Andrews T, Ungar D, Eyster ME. 1999. Chronic hepatitis C virus infections in leukemia survivors: prevalence, viral load, and severity of liver disease. Blood 93(11):3672-7.
Pianko S, Patella S, Sievert W. 2000. Alcohol consumption induces hepatocyte apoptosis in patients with chronic hepatitis C infection. J Gastroenterol Hepatol 15(7):798-805.
Poynard T, Bedossa P, Opolon P. 1997. Natural history of liver fibrosis progression in patients with chronic hepatitis C. The OBSVIRC, METAVIR, CLINIVIR, and DOSVIRC groups. Lancet 349(9055):825-32.
Poynard T, Marcellin P, Lee SS, Niederau C, Minuk GS, Ideo G, Bain V, Heathcote J, Zeuzem S, Trepo C, Albrecht J. 1998. Randomised trial of interferon alpha2b plus ribavirin for 48 weeks or for 24 weeks versus interferon alpha2b plus placebo for 48 weeks for treatment of chronic infection with hepatitis C virus. International Hepatitis Interventional Therapy Group (IHIT). Lancet 352(9138):1426-32.
Prasad VK, Lewis IJ, Aparicio SR, Heney D,Hale JP, Bailey CC, Kinsey SE. 1996. Progressive glomerular toxicity of ifosfamide in children. Med Pediatr Oncol 27(3):149-55.
Probert JC, Parker BR. 1975. The effects of radiation therapy on bone growth. Radiology 114(1):155-62.
Rait DS, Ostroff JS, Smith K, Cella DF, Tan C, Lesko LM. 1992. Lives in a balance: perceived family functioning and the psychosocial adjustment of adolescent cancer survivors. Fam Process 31(4):383-97.
Rauck AM, Green DM, Yasui Y, Mertens A, Robison LL. 1999. Marriage in the survivors of childhood cancer: a preliminary description from the Childhood Cancer Survivor Study. Med Pediatr Oncol 33(1):60-3.
Rhodes AR. 1995. Public education and cancer of the skin. What do people need to know about melanoma and nonmelanoma skin cancer? Cancer 75(2 Suppl):613-36.
Riseborough EJ, Grabias SL, Burton RI, Jaffe N. 1976. Skeletal alterations following irradiation for Wilms’ tumor: with particular reference to scoliosis and kyphosis. J Bone Joint Surg Am 58(4):526-36.
Ritchey ML, Green DM, Thomas PR, Smith GR, Haase G, Shochat S, Moksness J, Breslow NE. 1996. Renal failure in Wilms’ tumor patients: a report from the National Wilms’ Tumor Study Group. Med Pediatr Oncol 26(2):75-80.
Roberts CS, Turney ME, Knowles AM. 1998. Psychosocial issues of adolescents with cancer. Soc Work Health Care 27(4):3-18.
Ron E, Modan B, Preston D, Alfandary E, Stovall M, Boice JD Jr. 1991. Radiation-induced skin carcinomas of the head and neck. Radiat Res 125(3):318-25.
Ron E, Preston DL, Kishikawa M, Kobuke T, Iseki M, Tokuoka S, Tokunaga M, Mabuchi K. 1998. Skin tumor risk among atomic-bomb survivors in Japan. Cancer Causes Control 9(4):393-401.
Rourke MT, Stuber ML, Hobbie WL, Kazak AE. 1999. Posttraumatic stress disorder: understanding the psychosocial impact of surviving childhood cancer into young adulthood. J Pediatr Oncol Nurs 16(3):126-35.
Rubenstein CL, Varni JW, Katz ER. 1990. Cognitive functioning in long-term survivors of childhood leukemia: a prospective analysis. J Dev Behav Pediatr 11(6):301-5.
Sahler OJ, Roghmann KJ, Carpenter PJ, Mulhern RK, Dolgin MJ, Sargent JR, Barbarin OA, Copeland DR, Zeltzer LK. 1994. Sibling adaptation to childhood cancer collaborative study: prevalence of sibling distress and definition of adaptation levels. J Dev Behav Pediatr 15(5):353-66.
Sanders JE, Pritchard S, Mahoney P, Amos D, Buckner CD, Witherspoon RP, Deeg HJ, Doney KC, Sullivan KM, Appelbaum FR, et al. 1986. Growth and development following marrow transplantation for leukemia. Blood 68(5):1129-35.
Sanders JE, Hawley J, Levy W, Gooley T, Buckner CD, Deeg HJ, Doney K, Storb R, Sullivan K, Witherspoon R, Appelbaum FR. 1996. Pregnancies following high-dose cyclophosphamide with or without high-dose busulfan or total-body irradiation and bone marrow transplantation. Blood 87(7):3045-52.
Sargent JR, Sahler OJ, Roghmann KJ, Mulhern RK, Barbarian OA, Carpenter PJ, Copeland DR, Dolgin MJ, Zeltzer LK. 1995. Sibling adaptation to childhood cancer collaborative study: siblings’ perceptions of the cancer experience. J Pediatr Psychol 20(2):151-64.
Schell MJ, Ochs JJ, Schriock EA, Carter M. 1992. A method of predicting adult height and obesity in long-term survivors of childhood acute lymphoblastic leukemia. J Clin Oncol 10(1):128-33.
Schwartz C, Hobbie W, Constine L, Ruccione K. 1994. Survivors of Childhood Cancer: Assessment and Management. St. Louis, MO: Mosby.
Schwartz CL. 1995. Late effects of treatment in long-term survivors of cancer. Cancer Treat Rev 21(4):355-66.
Schwartz CL. 1999. Long-term survivors of childhood cancer: the late effects of therapy. Oncologist 4(1):45-54.
Shakil AO, Conry-Cantilena C, Alter HJ, Hayashi P, Kleiner DE, Tedeschi V, Krawczynski K, Conjeevaram HS, Sallie R, Di Bisceglie AM. 1995. Volunteer blood donors with anti-body to hepatitis C virus: clinical, biochemical, virologic, and histologic features. The Hepatitis C Study Group. Ann Intern Med 123(5):330-7.
Shan K, Lincoff AM, Young JB. 1996. Anthracycline-induced cardiotoxicity. Ann Intern Med 125(1):47-58.
Shore RE. 2001. Radiation-induced skin cancer in humans. Med Pediatr Oncol 36(5):549-54.
Silverman CL, Thomas PR, McAlister WH, Walker S, Whiteside LA. 1981. Slipped femoral capital epiphyses in irradiated children: dose, volume and age relationships. Int J Radiat Oncol Biol Phys 7(10):1357-63.
Skinner R, Cotterill SJ, Stevens MC. 2000. Risk factors for nephrotoxicity after ifosfamide treatment in children: a UKCCSG Late Effects Group study. United Kingdom Children’s Cancer Study Group. Br J Cancer 82(10):1636-45.
Sklar C, Whitton J, Mertens A, Stovall M, Green D, Marina N, Greffe B, Wolden S, Robison L. 2000. Abnormalities of the thyroid in survivors of Hodgkin’s disease: data from the Childhood Cancer Survivor Study. J Clin Endocrinol Metab 85(9):3227-32.
Sklar CA, Mertens AC, Mitby P, Occhiogrosso G, Qin J, Heller G, Yasui Y, Robison LL. 2002. Risk of disease recurrence and second neoplasms in survivors of childhood cancer treated with growth hormone: a report from the Childhood Cancer Survivor Study. J Clin Endocrinol Metab 87(7):3136-41.
Smith MA, Ries LAG. 2002. Childhood Cancer: Incidence, Survival, and Mortality. Pizzo PA, Poplack DG, Eds. Principles and Practice of Pediatric Oncology. 4th ed. Philadelphia: Lippincott Williams & Wilkins.
Steinherz LJ, Steinherz PG, Tan CT, Heller G, Murphy ML. 1991. Cardiac toxicity 4 to 20 years after completing anthracycline therapy. JAMA 266(12):1672-7.
Stevens MC, Mahler H, Parkes S. 1998. The health status of adult survivors of cancer in childhood. Eur J Cancer 34(5):694-8.
Strickland DK, Riely CA, Patrick CC, Jones-Wallace D, Boyett JM, Waters B, Fleckenstein JF, Dean PJ, Davila R, Caver TE, Hudson MM. 2000. Hepatitis C infection among survivors of childhood cancer. Blood 95(10):3065-70.
Stuber ML, Christakis DA, Houskamp B, Kazak AE. 1996. Posttrauma symptoms in childhood leukemia survivors and their parents. Psychosomatics 37(3):254-61.
Swerdlow AJ, Barber JA, Horwich A, Cunningham D, Milan S, Omar RZ. 1997. Second malignancy in patients with Hodgkin’s disease treated at the Royal Marsden Hospital. Br J Cancer 75(1):116-23.
Tao ML, Guo MD, Weiss R, Byrne J, Mills JL, Robison LL, Zeltzer LK. 1998. Smoking in adult survivors of childhood acute lymphoblastic leukemia. J Natl Cancer Inst 90(3):219-25.
Tong MJ, el-Farra NS, Reikes AR, Co RL. 1995. Clinical outcomes after transfusion-associated hepatitis C. N Engl J Med 332(22):1463-6.
Troyer H, Holmes G. 1988. Cigarette smoking among childhood cancer survivors. American Journal of Disease of Childhood 142:123.
Valdimarsson O, Kristinsson JO, Stefansson SO, Valdimarsson S, Sigurdsson G. 1999. Lean mass and physical activity as predictors of bone mineral density in 16-20-year old women. J Intern Med 245(5):489-96.
Van Dongen-Melman JE. 2000. Developing psychosocial aftercare for children surviving cancer and their families. Acta Oncol 39(1):23-31.
Van Dongen-Melman JE, Sanders-Woudstra JA. 1986. Psychosocial aspects of childhood cancer: a review of the literature. J Child Psychol Psychiatry 27(2):145-80.
Van Dongen-Melman JE, Hokken-Koelega AC, Hahlen K, De Groot A, Tromp CG, Egeler RM. 1995. Obesity after successful treatment of acute lymphoblastic leukemia in childhood. Pediatr Res 38(1):86-90.
Vonderweid N, Beck D, Caflisch U, Feldges A, Wyss M, Wagner HP. 1996. Standardized assessment of late effects in long-term survivors of childhood cancer in Switzerland: results of a Swiss Pediatric Oncology Group (SPOG) pilot study. International Journal of Pediatric Hematology/Oncology 3:483.
Waber DP, Carpentieri SC, Klar N, Silverman LB, Schwenn M, Hurwitz CA, Mullenix PJ, Tarbell NJ, Sallan SE. 2000. Cognitive sequelae in children treated for acute lymphoblastic leukemia with dexamethasone or prednisone. J Pediatr Hematol Oncol 22(3):206-13.
Walker C. 1989. Use of art and play therapy in pediatric oncology. J Pediatr Oncol Nurs 6(4):121-6.
Ward, JD. 2000. Pediatric cancer survivors: assessment of late effects. Nurse Pract. 25(12):18, 21-8, 35-7; quiz 38-9.
Warner JT, Bell W, Webb DK, Gregory JW. 1998. Daily energy expenditure and physical activity in survivors of childhood malignancy. Pediatr Res 43(5):607-13.
Wasserman AL, Thompson EI, Wilimas JA, Fairclough DL. 1987. The psychological status of survivors of childhood/adolescent Hodgkin’s disease. American Journal of Diseases of Children 141(6):626-31.
Wasserman T, Mackowiak JI, Brizel DM, Oster W, Zhang J, Peeples PJ, Sauer R. 2000. Effect of amifostine on patient assessed clinical benefit in irradiated head and neck cancer. Int J Radiat Oncol Biol Phys 48(4):1035-9.
Weigers ME, Chesler MA, Zebrack BJGS. 1998. Self-reported worries among long-term survivors of chilodhood cancer and their peers. Journal of Psyhosocial Oncology 16(2): 1-24.
Wexler LH. 1998. Ameliorating anthracycline cardiotoxicity in children with cancer: clinical trials with dexrazoxane. Semin Oncol 25(4 Suppl 10):86-92.
Wiley TE, McCarthy M, Breidi L, McCarthy M, Layden TJ. 1998. Impact of alcohol on the histological and clinical progression of hepatitis C infection. Hepatology 28(3):805-9.
Wingard JR, Plotnick LP, Freemer CS, Zahurak M, Piantadosi S, Miller DF, Vriesendorp HM, Yeager AM, Santos GW. 1992. Growth in children after bone marrow transplantation: busulfan plus cyclophosphamide versus cyclophosphamide plus total body irradiation. Blood 79(4):1068-73.
Wolden SL, Hancock SL, Carlson RW, Goffinet DR, Jeffrey SS, Hoppe RT. 2000. Management of breast cancer after Hodgkin’s disease. J Clin Oncol 18(4):765-72.
Zebrack BJ, Chesler MA. 2002. Quality of life in childhood cancer survivors. Psychooncology 11(2):132-41.
Zebrack BJ, Zeltzer LK, Whitton J, Mertens AC, Odom L, Berkow R, Robison LL. 2002. Psychological outcomes in long-term survivors of childhood leukemia, Hodgkin’s disease, and non-Hodgkin’s lymphoma: a report from the Childhood Cancer Survivor Study. Pediatrics 110(1 Pt 1):42-52.
Zee P, Chen CH. 1986. Prevalence of obesity in children after therapy for acute lymphoblastic leukemia. Am J Pediatr Hematol Oncol 8(4):294-9.
Zeltzer LK. 1993. Cancer in adolescents and young adults psychosocial aspects. Long-term survivors. Cancer 71(10 Suppl):3463-8.
Zeltzer LK, Dolgin MJ, Sahler OJ, Roghmann K, Barbarin OA, Carpenter PJ, Copeland DR, Mulhern RK, Sargent JR. 1996. Sibling adaptation to childhood cancer collaborative study: health outcomes of siblings of children with cancer. Med Pediatr Oncol 27(2):98-107.
Zeltzer LK, Chen E, Weiss R, Guo MD, Robison LL, Meadows AT, Mills JL, Nicholson HS, Byrne J. 1997. Comparison of psychologic outcome in adult survivors of childhood acute lymphoblastic leukemia versus sibling controls: a cooperative Children’s Cancer Group and National Institutes of Health study. J Clin Oncol 15(2):547-56.