|
Summary of Findings: Preventing Perinatal Transmission of HIV
|
8
Preventing Perinatal Transmission of HIV
The transmission of HIV from mother to fetus or infant presents a pressing challenge to improving birth outcomes in many developing countries. Since the start of the AIDS epidemic, an estimated 3.8 million children have died of the disease. The vast majority of these children acquired HIV from their mothers during pregnancy, at the time of childbirth, or during breastfeeding. Antiretroviral drugs that can be delivered to the mother during pregnancy and labor and to the child after birth, and which are widely used in the United States and other developed countries, have the potential to reverse the epidemic of pediatric AIDS in developing countries (Mofenson and McIntyre, 2000; Coll et al., 2002). Despite their promise, however, such interventions are not common in the developing world.
This chapter describes the scope of the HIV/AIDS epidemic, focusing on heavily infected populations where mother-to-child transmission occurs most frequently, and reviews the evidence for a variety of potential interventions to prevent perinatal transmission of HIV. It concludes with a description of an approach that would prevent new infections. Treatment of pregnant women for their own disease is clearly important, but beyond the scope of this report. The program of interventions described here can be accomplished ethically and at a reasonable cost compared with alternative treatments.
THE HIV/AIDS EPIDEMIC
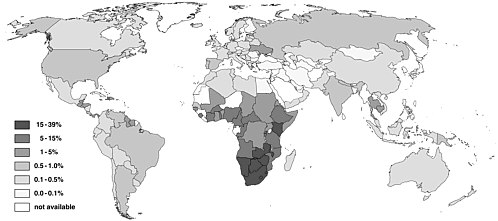
Since HIV/AIDS was recognized only two decades ago, the disease has reached epidemic proportions in many countries, especially in sub-Saharan
Africa (see Figure 8-1). Worldwide, approximately 3 million people died of AIDS during 2001. By the end of that year, an estimated 40 million people were living with HIV/AIDS—28 million in sub-Saharan Africa alone (Joint United Nations Programme on HIV/AIDS, 2001). In parts of southern Africa the prevalence of HIV in childbearing women may exceed 30 percent. The Joint United Nations Programme on HIV/AIDS estimates that about half of the 15-year-olds now living in the most heavily infected countries in Africa will eventually die of the disease and that it will reduce life expectancy in Southern Africa, which reached a high of 59 years in the early 1990s, to 45 years between 2005 and 2010 (Joint United Nations Programme on HIV/AIDS, 2000a, 1999). This represents a return to life expectancy rates not seen in the region since the early 1950s.
HIV/AIDS is killing large numbers of men and women in developing countries at the most productive time of their lives. They include doctors, farmers, and workers in agriculture, mining, and industry who not only support their families and raise children, but who make important contributions to the social and economic welfare of their countries. The loss of many teachers profoundly affects economic productivity, as it interferes with the development of human capital. Absenteeism, decreased productivity, worker turnover, training costs, funeral and death benefits are increasing across all sectors in many African countries, draining scarce public resources and impeding job creation and foreign investment (Joint United Nations Programme on HIV/AIDS, 2001). Many parents who have died of HIV/AIDS have orphaned children, some of them infected with HIV themselves, who are typically cared for by extended families (Mukwaya, 1999). UNAIDS estimates that there have been 13.2 million AIDS orphans in the world through 2000, 12.1 million in Sub-Saharan Africa (Joint United Nations Programme on HIV/AIDS, 2000a).
HIV in Women of Childbearing Age
In many developing countries, a high proportion of the female population is infected with HIV as compared with the global average. In sub-Saharan Africa, where heterosexual transmission predominates, women constitute 55 percent of the adults living with HIV/AIDS. In South and Southeast Asia and the Caribbean, women make up 30 percent to 50 percent of the HIV-infected adults. By comparison, women constitute about 20 to 40 percent of HIV-infected adults in North America, Western and Central Europe, Latin America, North Africa and the Middle East. The relatively high prevalence of HIV in women of childbearing age in developing countries increases the risk of perinatal transmission (Joint United Nations Programme on HIV/AIDS, 2001; Newell, 2000).
Biological and cultural factors help to explain the high prevalence of
HIV infection among women in the developing world. The subordinate sexual and economic status of women in many cultures contributes to the acquisition of HIV as well as of other sexually transmitted diseases, which also increase susceptibility to HIV infection (Joint United Nations Programme on HIV/AIDS, 2001). In Africa and South Asia, for instance, it is not uncommon for women to be coerced or seduced by older men into having sex. In some cultures there is a myth that if a man infected with an STD including HIV has sexual relations with a virgin, he can cure himself of his disease (Mukwaya, 1999).
In some populations, especially in sub-Saharan Africa, the estimated prevalence of HIV among pregnant women reaches 36 percent (Walker et al., 2002) (see Figure 8-1). In South and Southeast Asia, the overall prevalence in childbearing women is likely to be much lower than in Africa; there, HIV prevalence rates of up to 5 percent have been documented in antenatal clinics. The effects of high HIV prevalence on child mortality can be roughly estimated as follows: if one-third of the childbearing women in a population were infected with HIV, and the risk of mother-to-child transmission was one in three (as has been documented in some developing countries), then about 10 percent of children born in that population would be infected with HIV. Because nearly all HIV-infected children will die before they reach adulthood, these deaths would therefore raise child mortality by approximately 100 per thousand live births. And since maternal mortality negatively affects children’s survival, children who were not infected at birth would still face an increased risk of death after losing their mothers to AIDS.
Perinatal Transmission of HIV
Transmission of HIV from mother to child can take place in utero, intrapartum, or postpartum through breastfeeding (Mofenson, 1997). In sub-Saharan Africa and other developing countries, 25 to 35 percent of children born to HIV-infected mothers become infected at birth or shortly thereafter (De Cock et al., 2000; Brocklehurst, 2002). By contrast, the transmission rate in industrialized countries has been reduced to 5 percent or less through programs of antenatal counselling, testing, and antiretroviral treatment for infected women (Mofenson and McIntyre, 2000; Coll et al., 2002).
A series of maternal, obstetrical, and postpartum risk factors can affect the probability and the timing of mother-to-child transmission of HIV. The results of the European Collaborative Study demonstrated a linear relationship of transmission with decreasing maternal CD4+ cell counts, seemingly independent of other factors (European Collaborative Study, 1992). Other studies associate high maternal plasma HIV RNA levels with a significant
risk of perinatal HIV infection (Garcia et al., 1999; Mofenson et al., 1999), although transmission may occur even when the virus is undetectable. Separate studies of cohorts of pregnant women in Malawi and the United States have also found an association between low maternal vitamin A levels in pregnancy and increased risk of transmission (Semba, 1997; Greenberg et al., 1997). Other studies (Burns et al. 1999; Fawzi, 2000) did not detect such a trend, however.
Several obstetric factors also influence the rate of perinatal HIV transmission. Prolonged rupture of membranes, instrumentation, vaginal delivery, and birth trauma all increase the child’s risk of infection (International Perinatal HIV Group, 2001; Mofenson, 1997). Studies in both humans and primates demonstrate the transmission of HIV through maternal blood or secretions; thus if membranes rupture prematurely or if the mother hemorrhages, the child is at increased risk for infection (Mofenson, 1997). In the postpartum period, breastfeeding is the primary mode of mother-to-child HIV transmission. A randomized trial in Nairobi, Kenya, that compared breastfeeding and formula feeding found that breastfeeding increased the risk of HIV transmission by 16.2 percent, which accounted for 44 percent of HIV infection in the breastfeeding arm of that study. Most—75 percent—of the risk difference between the two arms of the study occurred in the first 6 months, but transmission continued throughout the duration of exposure (Nduati et al., 2000). Coutsoudis and colleagues (2001) have shown that mixed infant feeding (breast milk plus other liquids) is associated with higher rates of transmission than exclusive breastfeeding.
Children in developing countries who contract HIV at birth or shortly thereafter rarely live more than a few years. In several studies in Africa, the probability of death by the age of 12 months in HIV-infected children was found to be about 30 percent, and by the age of 5 years 60 to 90 percent had died (Joint United Nations Programme on HIV/AIDS Reference Group on Estimates, Modelling, and Projections, 2002; Adetunji, 2000; Tudor-Williams, 2000). A study in Malawi concluded that nearly 90 percent of African children infected with HIV do not survive beyond their third birthday (Taha et al., 2000).
INTERVENTIONS TO PREVENT HIV TRANSMISSION
Antiretroviral Strategies
Antiretroviral drugs that have proved effective in the treatment of adults and children with AIDS when administered either individually or in combination have also been tested and compared for their ability to prevent mother-to-child transmission of HIV. These medications include zidovudine (ZDV or AZT); ZDV in combination with lamivudine (3TC); and
nevirapine (NVP) (Nolan et al., 2002). Research indicates that with appropriate antiretroviral therapy and elective cesarean delivery, perinatal HIV transmission rates can be reduced to less than 2 percent (Mandelbrot et al., 2001). Table 8-1 summarizes the conditions and results of several key trials described below, many of which were conducted in developing countries.
Zidovudine (ZDV or AZT). A seminal study by the AIDS Clinical Trials Group (ACTG) in 1994 concluded that the antiretroviral drug zidovudine (ZDV), previously known to delay the progression of AIDS in persons with relatively advanced disease, was effective in reducing the risk of perinatal transmission (Connor et al., 1994). Based on these and subsequent results, the protocol used in that study—known as the ACTG 076 regimen—has become the minimum standard of care in industrialized countries (Institute of Medicine, 1999). In the United States, mother-to-child transmission of HIV has fallen by about 70 percent from its peak in the early 1990s (Centers for Disease Control and Prevention, 1999). However, while the ACTG 076 regimen is considered cost-effective in the industrialized world, it is considered too expensive and logistically difficult to establish in most developing countries.
As an alternative to the ACTG 076 regimen, a series of clinical trials of a shorter course of ZDV, which includes daily doses of the drug beginning late in pregnancy, have been carried out in Southeast Asia and sub-Saharan Africa. One of two short-course ZDV trials that have been conducted in Thailand, the Bangkok trial, found that a short-course regimen reduced mother-to-child HIV transmission by 50 percent, at a cost of about $200 to $400 per person (Shaffer et al., 1999; Mofenson and McIntyre, 2000). A follow-up study found that 81 percent of the children who received ZDV had no significant adverse events associated with treatment by 18 months (Chotpitayasunondh et al., 2001). The second Thai study, the Perinatal HIV Prevention Trial (PHPT), compared several different ZDV regimens using the same doses as one of the regiments in the Bangkok trial. A short prenatal/short postnatal arm of the trial was stopped early because the transmission rate was significantly higher than in the long prenatal/long postnatal arm. At 18 months, the transmission rate was found to be significantly lower in the long prenatal treatment arms (Lallemant et al., 2000; Mofenson and McIntyre, 2000).
Both African ZDV studies, which took place in Ivory Coast and Burkina Faso, were placebo-controlled trials in which the mothers breastfed. The Ivory Coast trial yielded a 37 percent reduction in the rate of transmission (Wiktor et al., 1999), while the DITRAME ANRS 049 study, conducted in Ivory Coast and Burkina Faso reported a 38 percent reduction in transmission (Dabis et al., 1999).
A recent Cochrane Review (Brocklehurst and Volmink, 2002) concluded that the effectiveness of zidovudine therapy from 28 weeks in preg-
nancy for the mother through 3 days for the infant (the long-short term course) and from 35 weeks in pregnancy for the mother to 6 weeks for the infant (the short-long term course) provided the same protection as the long-long course.
Combination therapy. With the advent of two- and three-drug combinations to reduce viral loads in people with AIDS, researchers began to evaluate benefits of combining ZDV with other antiretroviral agents to prevent perinatal HIV transmission. Mandelbrot and colleagues (2001) found, using retrospective controls, that a combination of ZDV and lamivudine (3TC) reduced the risk of HIV transmission by almost 80 percent in non-breastfeeding women compared with women taking only ZDV. However, concerns about possible side effects (see toxicity discussion below) and the fact that current treatment guidelines typically call for a three-drug regimen that includes a costly protease inhibitor limit the practical impact of this finding.
The PETRA trial in South Africa, Uganda, and Tanzania tested less intensive ZDV plus 3TC regimes than those used by Mandelbrot and colleagues (2001), and did so in women who mostly breastfed their infants (Petra Study Team, 2002). The study compared a three-part regimen (prepartum, intrapartum, and postpartum) to a combination of intrapartum and postpartum therapy and intrapartum therapy only. At 6 weeks postpartum, the rate of transmission was reduced by 50 percent in the three-part treatment group; the two-part regimen achieved a 37 percent reduction; and the intrapartum-only group was not significantly different from the placebo group. At 18 months the differences between the groups were less pronounced, probably due to the effects of breastfeeding.
A recent Cochrane Review (Brocklehurst and Volmink, 2002) concluded that the combination therapy using zidovudine and lamivudine (3TC) decreased the risk of transmission when the combination is given during the antenatal and intrapartum periods or the intrapartum and postpartum periods, but not when given only in the intrapartum period alone.
Nevirapine. The 1999 HIVNET 012 randomized controlled trial in Uganda found that nevirapine (NVP), a nonnucleoside reverse-transcriptase inhibitor that is rapidly absorbed orally, reduced the risk of perinatal transmission by 47 percent (Guay et al., 1999). This result, which is comparable to results achieved with a short course of ZDV, followed a single intrapartum dose of NVP for the mother and a single dose for the infant after birth. That regime costs about $4—a tiny fraction of the cost of ZDV treatment (Marseille et al., 1999).
The SAINT trial in South Africa compared NVP to a combination of ZDV and 3TC, both regimens administered intrapartum and postpartum. Preliminary results indicate that there was no significant difference in HIV infection in the two groups at 8 weeks postpartum (Moodley, 2000).
TABLE 8-1 Trials of Antiretroviral Treatments to Prevent Mother-to-Child HIV Transmission
|
Study Name and Reference |
Population Characteristics |
Treatment (Pre- and Intrapartum to Mother, Postpartum to Child) |
|
ACTG 076 (Connor et al., 1994) |
Nonbreastfeeding women in US and France |
Pre: 100 mg ZDV orally 5x daily starting at 14-34 weeks gestation Intra: 2 mg/kg ZDV IV for 1 hour, then 1 mg/kg ZDV IV per hour until delivery Post: 2 mg/kg orally 4x daily for 6 weeks |
|
Bangkok trial (Shaffer et al., 1999) |
Nonbreastfeeding women in Thailand |
Pre: 300 mg ZDV orally 2x daily starting in 36th week of pregnancy Intra: 300 mg ZDV every 3 hours |
|
Perinatal HIV Prevention Trial (PHPT) (Lallemant et al., 2000) |
Nonbreastfeeding women in Thailand |
Short Pre: 300 mg ZDV orally 2x daily starting at 35 weeks gestation Intra: 300 mg ZDV every 3 hours Short Post: 2 mg/kg ZDV orally every 6 hours for 3 days |
|
|
Long Pre: 300 mg ZDV orally 2x daily starting at 28 weeks gestation Intra: 300 mg ZDV every 3 hours Short Post: 2 mg/kg ZDV orally every 6 hours for 3 days |
|
|
Short Pre: 300 mg ZDV orally 2x daily starting at 35 weeks gestation Intra: 300 mg ZDV every 3 hours Long Post: 2 mg/kg ZDV orally every 6 hours for 6 weeks |
||
|
Long Pre: 300 mg ZDV orally 2x daily starting at 28 weeks gestation Intra: 300 mg ZDV every 3 hours Long Post: 2 mg/kg ZDV orally every 6 hours for 6 weeks |
||
|
RETROCI (Wiktor et al., 1999) |
Breastfeeding women in Ivory Coast |
Pre: 300 mg ZDV orally 2x daily starting at 36 weeks gestation Intra: 300 mg ZDV every 3 hours |
|
DITRAME ANRS 049 (Dabis et al., 1999) |
Mostly breastfeeding women in Ivory Coast and Burkina Faso |
Pre: 300 mg ZDV orally 2x daily starting at 36-38 weeks gestation Intra: 600 mg ZDV at onset of labor Post (maternal): 300 mg ZDV orally 2x daily for 1 week |
|
|
Risk of Transmission (% of Children) |
|
|
|
HIV Status Evaluated |
Control |
Treatment |
Relative Reduction in Risk (in %) |
|
18 mo. |
25.5 |
8.3 |
67 |
|
6 mo. |
18.9 |
9.4 |
50.0 |
|
6 mo. |
— |
10.5 |
Stopped early |
|
18 mo. |
— |
4.7 |
In utero transmission higher with short maternal treatment |
|
|
— |
8.6 |
|
|
|
— |
6.5 |
|
|
3 mo. |
24.9 26.1 |
15.7 16.5 |
37 37 |
|
6 mo. |
27.5 |
18.0 |
35 |
|
|
|
Treatment (Pre- and Intrapartum to Mother, Postpartum to Child) |
|
Study Name and Reference |
Population Characteristics |
|
|
|
||
|
RETROCI and DITRAME pooled analysis (Peiperl, 2001) |
|
As above |
|
|
||
|
|
||
|
|
||
|
|
Nonbreastfeeding women in France |
ACTG 076 regimen (historical controls) |
|
|
ACTG 076 regimen plus 150 mg 3TC orally 2x daily starting at 32 weeks gestation and 2 mg/kg orally 2x daily for 6 weeks to child |
|
|
PETRA (Petra Study Team, 1999) |
Mostly breastfeeding women in South Africa, Tanzania, and Uganda |
Intra: 300 mg ZDV every 3 hours and 150 mg 3TC orally every 12 hours |
|
|
Intra: as above Post (maternal): 300 mg ZDV and 150 mg 3TC orally 2x daily for 1 week |
|
|
Pre: 300 mg ZDV and 150 mg 3TC orally 2x daily starting at 36 weeks gestation Intra: as above Post (maternal): as above |
||
|
Intra: 300 mg ZDV every 3 hours and 150 mg 3TC orally every 12 hours |
||
|
Intra: as above Post (maternal): 300 mg ZDV and 150 mg 3TC orally 2x daily for 1 week |
||
|
Pre: 300 mg ZDV and 150 mg 3TC orally 2x daily starting at 36 weeks gestation Intra: as above Post (maternal): as above |
||
|
|
Risk of Transmission (% of Children) |
|
|
|
HIV Status Evaluated |
Control |
Treatment |
Relative Reduction in Risk (in %) |
|
15 mo. |
30.6 |
21.5 |
30 |
|
6 mo. |
26.1 |
16.9 |
|
|
12 mo. |
28.5 |
18.5 |
|
|
18 mo. |
30.1 |
21.6 |
|
|
24 mo. |
30.1 |
22.1 |
27 |
|
18 mo. |
6.8 |
|
|
|
|
|
1.6 |
78 |
|
6 wk. |
17.2 |
17.1 |
0 |
|
|
17.2 |
10.8 |
37 |
|
17.2 |
8.6 |
50 |
|
|
18 mo. |
26.6 |
25.7 |
3 |
|
|
26.6 |
24.4 |
8 |
|
26.6 |
20.7 |
22 |
|
|
|
|
Treatment (Pre- and Intrapartum to Mother, Postpartum to Child) |
|
Study Name and Reference |
Population Characteristics |
|
|
HIVNET 012 (Guay, 1999) |
Breastfeeding women in Uganda |
Intra: 600 mg ZDV orally at onset of labor and 300 mg ZDV every 3 hours Post: 4 mg/kg orally 2x daily for 1 week |
|
|
Intra: 200 mg NVP orally at onset of labor Post: 200 mg/kg NVP orally at 48-72 hours postpartum |
|
|
Intra: 600 mg ZDV orally at onset of labor and 300 mg ZDV every 3 hours Post: 4 mg/kg orally 2x daily for 1 week |
||
|
Intra: 200 mg NVP orally at onset of labor Post: 200 mg/kg NVP orally at 48-72 hours postpartum |
||
|
SAINT (Moodley, 2000) |
Mostly breastfeeding women in South Africa |
Intra: 600 mg ZDV and 150 mg 3TC orally at onset of labor and 300 mg ZDV and 150 mg 3TC orally every 3 hours Post: 12 mg ZDV and 6 mg 3TC orally 2x daily for 1 week Post (maternal): 300 mg ZDV and 150 mg 3TC orally 2x daily for 1 week |
|
|
Intra: 200 mg NVP orally at onset of labor Post: 6 mg NVP orally at 24-48 hours postpartum Post (maternal): 200 mg NVP orally at 24-48 hours postpartum |
|
A recent Cochrane Review (Brocklehurst and Volmink, 2002) stated that one large randomized trial demonstrates that nevirapine given to the mother as a single dose at the onset of labor and to the infant as a single dose within 72 hours of birth is more effective than an intrapartum and post partum regime of zidovudine.
Toxicity and risks associated with antiretroviral therapy. Given the
|
|
Risk of Transmission (% of Children) |
|
|
|
HIV Status Evaluated |
Control |
Treatment |
Relative Reduction in Risk (in %) |
|
14-16 weeks |
25.1 |
— |
47 |
|
|
— |
13.1 |
|
|
1 yr. |
24.1 |
— |
35 |
|
|
— |
15.7 |
|
|
8 weeks |
10.8 |
— |
Difference not significant |
|
|
— |
14.0 |
|
known vulnerability of the developing fetus to toxicity, the potential side effects of any drug used in utero must be investigated. While some antiretroviral drugs have been shown to be carcinogenic in rodents, no such effects have been detected in short-term human studies or reported to a registry maintained by the drugs’ manufacturers (Culnane et al., 1999; Mofenson and McIntyre, 2000). Overall, it is likely that the risk of serious
drug-associated side effects to the child is small compared with the averted risk of HIV infection and death.
Based on eight cases in France, researchers have postulated a link between mitochondrial dysfunction and exposure to ZDV or a combination of ZDV and 3TC (Blanche et al, 1999). These authors have recommended that antiretroviral treatment to prevent perinatal HIV transmission be limited to ZDV alone to minimize the dangers of mitochondrial damage or toxicity. Recent evidence of toxic side effects from NVP, including severe liver damage in health care workers who took the drug for postexposure prophylaxis, has been attributed to taking multiple doses of the drug; a single dose is typically used to prevent perinatal HIV transmission. Having compared the costs and benefits of NVP use in both situations, the Centers for Disease Control and Prevention (CDC) has advised against using the drug for postexposure prophylaxis while continuing to recommend it for the prevention of perinatal transmission (Centers for Disease Control and Prevention, 2001).
There are also concerns about the development of resistance to antiretrovirals (Mandelbrot et al., 2001; Morris et al., 2001; Hirsch, 2002; Euroguidelines Group for HIV Resistance, 2001). It is unlikely that NVP-resistant strains of the virus would be tramsmitted during labor or delivery (Joint United Nations Programme on HIV/AIDS, 2000b). Transmission during breastfeeding is a greater concern, however, as NVP-resistant virus has been observed in adults receiving chronic NVP treatment as a single agent and after single dose prophylaxis (Eshelman and Jackson, 2002). This possibility would be minimized through the use of combination therapies which include NVP or another nonnucleoside reverse transcriptase inhibitors (NNRTIs) (Mandlebrot et al., 2001).
Cost of antiretroviral drugs. Recently, pharmaceutical companies that produce anti-AIDS medicines responded to concerns about the prices of these drugs. The companies agreed to offer ZDV, NVP and other AIDS drugs—at prices discounted by up to 90 percent—to developing countries that have been severely affected by the AIDS epidemic, and Roxane Laboratories, the manufacturer of NVP, has offered to provide it free to some countries. The governments of some African nations were originally reluctant to accept these offers, however, due to the cost of developing the necessary infrastructure for drug distribution, patient education, and laboratory monitoring. Moreover, a Washington Post article (Gellman, 2000) reports that Secretary-General of the United Nations Kofi Annan’s advisers said in a memo that even at a 90 percent discount, treatments to save the lives of people with AIDS can cost hundreds to thousands of dollars per person, an amount that is unrealistic in developing countries. However, the simple courses of ZDV and NVP that are necessary to prevent perinatal
transmission are far less costly than treatment regimens for HIV-infected adults and children.
Cost of programs to administer ART. Introducing and sustaining programs to administer antiretroviral therapy in resource poor countries, even short-term therapies, involves resources well beyond the cost of the drugs. These programs involve the counseling and testing of pregnant women: those who are infected with HIV need information and support in dealing with their own infection, while those who are not infected should be provided with information and support to avoid future infection. Although the cost of the drugs has become more affordable, development of appropriate infrastructure including trained staff is a separate and substantial challenge.
Nonantiretroviral Strategies
Cesarean section. A meta-analysis of North American and European studies found that elective cesarean section reduces the risk of mother-to-child transmission of HIV by more than 50 percent, independent of treatment with ZDV (International Perinatal HIV Group, 1999). It is postulated that the reduced risk of perinatal HIV transmission is the result of minimizing the infant’s exposure to body fluids in the maternal genital tract. However, safe and effective cesarean sections are not available to many women in the developing world, and some studies in both developing and industrialized countries have found an increased rate of maternal complications in HIV-infected women who have undergone the procedure (Mofenson and McIntyre, 2000). Thus, cesarean section may be an appropriate strategy for preventing perinatal transmission of HIV, but only when performed in appropriately staffed and equipped health facilities, where the risks associated with cesarean section are low.
Vaginal lavage. Viricidal cleansing of the birth canal and the infant’s skin immediately after delivery has been examined as a potentially inexpensive, low-technology method of reducing perinatal HIV transmission. To date, its efficacy has not been demonstrated. Therefore, additional research and well designed randomized, controlled trials are needed.
Vitamin A therapy. Therapeutic doses of vitamin A have been shown to be ineffective in preventing perinatal transmission of HIV, so vitamin therapy is not recommended at this time (Kumwenda et al., 2002; Fawzi et al., 2002b).
Breast milk substitutes. The HIV epidemic has raised difficult questions about breastfeeding in areas where there is a high prevalence of HIV among lactating women and where infants are at high risks for diarrhea and malnutrition (Fowler et al., 1999). The rate of postnatal transmission of HIV through breastfeeding is high (Fawzi et al., 2002a). While early weaning
may reduce transmission, this must be balanced against risks of malnutrition and diarrhea in a particular setting. Antiretroviral drugs to the mother may also reduce risk of breast milk transmission. Breastfeeding by HIV-positive mothers is discouraged in industrialized countries, where safe and affordable alternatives to breast milk are available. The choice is complicated in developing countries, where breastfeeding has proven benefits and artificial feeding has established risks. In 1998, UNAIDS, WHO, and UNICEF issued a joint statement that supports breastfeeding, but also encourages voluntary and confidential testing for both men and women of reproductive age, and promotes education regarding the implications of their HIV status for the health and welfare of their children. “When children born to women with HIV can be ensured uninterrupted access to nutritionally adequate breast milk substitutes that are safely prepared, they are at less risk of illness and death if they are not breast fed. However, when these conditions are not fulfilled, in particular in an environment where infectious diseases and malnutrition are the primary causes of death during infancy, artificial feeding substantially increases children’s risk of illness or death” (World Health Organization, Joint United Nations Programme on HIV/AIDS, 1998).
Breastfeeding has been promoted for many years for its reduction of mortality due to infectious diseases including neonatal sepsis, acute respiratory infections, and diarrhea (Arifeen et al., 2001; Ashraf et al., 1991; World Health Organization Collaborative Study Team, 2000). Discouraging breastfeeding now may be both unsafe and socially unacceptable in certain settings. Programs to reduce breastfeeding or limit its duration among HIV-infected women (and thus decrease transmission to their infants) must not reduce breastfeeding among women who are not infected with HIV, and must ensure that safe and affordable breast milk substitutes are available as long as needed (World Health Organization, 2000). In addition, maternal antibodies in breast milk confer immunity to the child (Nicoll et al., 1995), so breastfeeding can protect against infectious diseases. Finally, since breastfeeding is the norm for infant feeding in the developing world, a woman who does not breastfeed tacitly admits that she is HIV-positive, which in turn may cause her to be rejected by her mate and community.
Comparing Preventive Interventions
Of all of the options discussed, it appears that treating pregnant women who are HIV-positive, and their infants, with simple low-cost regimens of antiretroviral drugs is the most effective and feasible means to prevent perinatal transmission in developing countries. The success of this strategy depends upon access to antenatal care, so that HIV-positive women can be identified before (or at least by) the time of delivery. To increase the effec-
tiveness of antiretroviral treatment, infants of HIV-positive mothers should be fed a breast milk replacement where safe, appropriate, and feasible.
A number of available antiviral regimens for preventing perinatal HIV transmission are known to be safe and effective (World Health Organization, 2000). Although less effective than the ACTG 076 regimen used in developed countries (see Table 8-1), short-course ZDV and intrapartum NVP have both been shown to reduce the HIV transmission rate by up to 50 percent at a much lower cost. The choice of regimen should be determined according to local circumstances on the grounds of costs and practicality, particularly as related to the availability and quality of antenatal care (World Health Organization, 2000).
Unlike most types of interventions that could improve birth outcomes in developing countries, AIDS prevention programs—including those to prevent perinatal HIV transmission—have been the subject of many cost-benefit analyses. Table 8-2 summarizes the results of several studies that examine antenatal HIV screening and the subsequent treatment of women who test positive, as well as their infants, to prevent HIV infection. Although the details of these studies differ, all indicate that perinatal HIV prevention programs can be effective at a relatively low cost. Given the high opportunity cost to the economy of losing a life at a young age, antenatal HIV screening appears to cost-effective even at low prevalence rates. Where prevalence is high, the cost-effectiveness of antenatal HIV prevention programs can be substantially less than $100 per disability-adjusted life years (DALY) saved, and may actually save money for the health care system (Stoto and Goldman, 2003). This compares favorably with the four most effective public health interventions for children under 5 years of age in developing countries: control of respiratory and perinatal infections, diarrheal diseases, and vaccine-preventable diseases (World Bank, 1993).
A number of caveats, however, must be heeded when interpreting such economic analyses. First, because many assumptions must be made without hard data, there is a large amount of uncertainty in the results. These educated guesses, however, do establish the order of magnitude of the results, which sometimes is enough for policy comparisons. Second, new developments with respect to the cost and efficacy of the medication, as well as efficiencies in counseling and testing and other aspects of screening and treatment, are likely to make the economic comparisons more favorable, so the cost estimates presented here should be seen as conservative.
Barriers to Implementing Antenatal Screening
Despite evidence of the cost-effectiveness of antenatal HIV screening, few developing countries have decided to implement national screening programs. Some countries have pilot programs underway; others have con-
TABLE 8-2 Cost-Effectiveness Analyses of Antenatal HIV Screening Programs
Several published cost-effectiveness analyses have evaluated antenatal HIV screening programs on the individual, health sector, and social level. Program costs include counseling women in antenatal care, testing them for HIV, and treating those who are found to be positive to prevent transmission to their children (except for one study of NVP treatment provided to all pregnant women). All costs are based upon actual local costs for program administration, but are expressed in terms of U.S. dollars.
|
Population Characteristics |
HIV prevalence in pregnant women (percent) |
Treatment regimen(s) |
Cost per case averted |
Reference |
|
Sub-Saharan Africa |
12.5 |
Two doses of 300 mg ZDV/day beginning 2 to 6 weeks before delivery and 300 mg per 3 three hours in labor |
$1,269 (a savings of $1.06 million per 100,000 births) |
Mansergh et al. (1996, 1998) |
|
Sub-Saharan Africa |
15 |
ZDV and 3TC daily starting at the 36th week of pregnancy and continuing for 1 week postpartum |
$5,134 |
Marseille et al. (1998) |
|
Sub-Saharan Africa |
15 |
ZDV and 3TC starting at delivery, continuing through 1 week postpartum |
$2,680 |
Marseille et al. (1998) |
|
Sub-Saharan Africa |
15 |
ZDV and 3TC administered intrapartum only |
$1,129 |
Marseille et al. (1998) |
|
Rural South Africa (KwaZulu/Natal district) |
26 |
ACTG 076 (see Table 8-1) |
$5,806 ($5,591 with enhanced service infrastructure) |
Wilkinson et al. (1998) |
|
Rural South Africa (KwaZulu/Natal district) |
26 |
Short course of ZDV with 3TC |
$2,492 |
Wilkinson et al. (1998) |
|
Sub-Saharan Africa |
15, 30 |
NVP administered 200 mg oral dose given to all women in labor and 2 mg given to infant after birth |
$276, $138 |
Marseille et al. (1999) |
|
Sub-Saharan Africa |
15, 30 |
NVP administered 200 mg oral dose given to HIV-positive mother (identified through counseling and testing) in labor and 2 mg given to infant after birth |
$506, $298 |
Marseille et al. (1999) |
|
Urban, working-class South Africa (Soweto) |
15 |
Short course ZDV before and during birth plus formula supplied |
less than $100 (formula (formula supplied) recommended); $669 |
Söderlund et al. (1999) |
sidered implementing such programs but have declined to do so, citing their cost as well as social, cultural, and ethical concerns.
Cost. The cost of treating individuals with HIV may exceed a developing country’s national health budget on a per capita basis. In sub-Saharan Africa, for instance, the annual budget for health care averages $24 per capita (World Bank, 1993). Antenatal screening and treatment with NVP costs less than $10 per pregnant woman, most of which pays for counseling and HIV testing; however, only pregnant women (not the whole population) incur costs. A more relevant comparison, therefore, might be made with antenatal and delivery care, which typically costs $90 per woman in the poorest developing countries (World Bank, 1993); that figure would increase by less than 10 percent were it to include the cost of HIV screening.
Social, cultural, and ethical concerns. In light of the evidence that a program of antenatal HIV screening and prophylaxis of infected mothers to prevent transmission is both effective and cost-efficient under most if not all circumstances, one might argue that not to implement antenatal HIV screening is unethical. However, acceptability of HIV counseling and testing has limited implementation for treatment programs in some settings (Meda et al., 2002). If stigma and discrimination associated with HIV infection is high—if women who are known to have AIDS or HIV infection endure beatings and may be disowned by their families (Berer, 1999; Mukwaya, 1999)—it is understandable that women might want to avoid HIV testing, especially during pregnancy, a time of great vulnerability. Concerns about stigma and discrimination also interfere with women’s ability to accept antiviral treatment for themselves and bottle-feeding for their infants. A study in Rwanda suggested that women 35 years and older and those whose partners had skilled and well-paid jobs were more likely to accept HIV testing (Kowalczyk et al., 2002). Clearly, the stigma associated with HIV status must be removed through extensive social programs if efforts to prevent transmission are to succeed, but such changes will take time. Women must meanwhile be counseled frankly about the costs and benefits of HIV testing and treatment if necessary for themselves and their children and be allowed to make their own decisions.
Policy makers in developing countries have also questioned the appropriateness of treating women to prevent transmission of HIV at birth if (a) there is a high risk of transmission later through breastfeeding and (b) parents are likely to die of HIV disease before the infant reaches adulthood. Many observers believe that a life is worth saving whatever the risks that the child faces later in life, and that antenatal HIV screening with prophylaxis offers many children a chance to live into adulthood. Moreover, it can be argued that the main risks facing children saved from HIV infection can themselves be mitigated. The risk of transmission through breastfeeding can be eliminated or reduced through the provision of alter-
natives such as formula, and most AIDS orphans can be raised by extended families, as they are today in many developing countries. Children saved from HIV infection through antenatal screening programs may represent a burden on society and especially their relatives during early life, but they have the potential to contribute significantly to society and the economy, as well as to the welfare of their extended families. If resources are not sufficient to provide treatment to all HIV-infected citizens, treatment of pregnant women should be considered seriously in setting priorities, because of transmission from mother to baby.
One might also ask whether it is ethically appropriate to treat a mother with a short course or a single dose of drugs that would benefit her child, but not the mother herself. Many observers have argued that it is, given the inability of many developing countries to pay for lifelong therapy for people with HIV, the tangible benefits to the child, and the satisfaction that many women get from selflessly protecting their children. Prophylaxis of pregnant women also can be distinguished from other treatment programs in that it aims to prevent new AIDS cases, and is far more effective in doing so than other measures.
In the United States, where HIV prevalence rates in childbearing women are low and many women are well informed about HIV and AIDS, the Institute of Medicine has recommended that prenatal care for all women include HIV testing, with notification of results to the patient (Institute of Medicine, 1999). In developing countries, where women might be less aware of HIV/AIDS, for example among women in India (Chaterjee, 1999), and where prevalence rates may be higher, counseling and informed consent for HIV testing in antenatal care should be more intensive and focused on helping women make informed choices for themselves.
Guidelines for Antenatal HIV Screening
A recent summary of the characteristics of a well-organized perinatal public health screening program (Institute of Medicine, 1999), which draws upon earlier principles developed by WHO (Wilson and Jungner, 1968), is relevant to countries considering antenatal HIV screening programs:
-
The goals of a screening program must be clearly specified and achievable.
-
The natural history of the condition should be adequately understood, treatment for those found positive must be widely accepted by the medical community, and there should be evidence that early intervention improves health outcomes.
-
The screen should be able to distinguish individuals likely to have the condition from those not likely to have it.
-
There must be adequate resources to diagnose and treat every person with the condition.
-
The test and intervention should be acceptable to the affected population.
Given the evidence discussed in this chapter, and understanding “treatment” as short-course ZDV or intrapartum NVP intended to prevent transmission to the infant, antenatal HIV screening programs would likely be judged to be ethically appropriate in most developing countries where the prevalence of HIV in childbearing mothers is high and where resources exist to treat them.
RECOMMENDATIONS
Antenatal screening and prophylaxis programs represent the most immediate means to reducing perinatal HIV transmission. The reduced cost of drug therapy makes them more comparable with other health and economic investments. The most significant cost is, however, that associated with building the health care infrastructure needed to deliver testing, counselling, and drugs.When the social costs of AIDS are considered, especially in populations with a high prevalence of HIV1 in childbearing women, antenatal screening programs in developing countries appear to be cost-saving; in populations with low prevalence rates, the per capita cost can be low. In order to implement antenatal HIV screening programs as quickly as possible, international support should be organized to supplement limited resources of developing countries.
The social cost of HIV/AIDS is very high in terms of the stigma and discrimination borne by women who test positive, especially those who have little power. Fear of the consequences of a positive test and the lack of resources to treat HIV infection in developing countries turn women away from testing. In addition, relatively few women in developing countries realize that HIV can be transmitted to their children, or that effective measures to reduce the risk of transmission are available. Thus education regarding the risks and benefits of antenatal HIV screening and treatment must be incorporated into antenatal care along with options for HIV screening and antiretroviral prophylaxis.
There are inadequate data on which to base specific recommendations on breastfeeding or formula feeding by HIV-infected women in developing countries. Although formula feeding eliminates the risk of vertical trans-
mission of HIV, the use of unsafe water to reconstitute infant formula poses an even greater hazard to neonates in most settings. Accordingly, the benefits and disadvantages of breast and formula feeding need to be assessed simultaneously, and HIV-infected women should receive counseling on infant feeding options appropriate to the woman’s cultural, social, and economic circumstances and support for her individual choice.
Recommendation 4. The following strategy is recommended for incorporation into preconceptional and antenatal care in all settings:
-
In areas where HIV is a public health problem (seroprevalence exceeds 1 percent), antenatal screening for HIV should be provided to women who, after counseling, give their informed consent. Women who test positive should receive antiretroviral prophylaxis to prevent mother-to-child transmission of the virus, along with appropriate counseling on infant feeding options.
The success of programs to prevent perinatal HIV transmission—and indeed of all efforts to reduce the global impact of AIDS—rests on the longer-term prospect of removing the stigma associated with the disease. Countries should use every means possible to reduce this stigma, which presents a major barrier to the prevention and treatment of HIV/AIDS. It is possible that incorporating HIV screening as a routine part of antenatal care for all women will contribute to that goal.
RESEARCH NEEDS
Despite considerable progress over the last decade, optimizing the prevention of perinatal HIV infection, especially in low-resource settings, will require ongoing study. The committee therefore recommends research on the following topics to support the previous recommendation.
-
Identifying effective and efficient ways to implement antenatal HIV screening programs in developing country settings.
-
Discovering effective counseling techniques that increase women’s awareness of the risks and benefits of antenatal HIV screening and encourage them to make informed choices regarding testing.
-
Identifying barriers to women accepting HIV testing and discovering means to overcome them.
-
Developing and testing rapid HIV diagnostic tests suitable for field settings to be used late in pregnancy or in the intrapartum period.
-
Selecting the most effective antiretroviral drugs, doses, and regimens for reducing perinatal HIV transmission, and determining the extent to which the effectiveness of treatments can be preserved while reducing duration of therapy, drug dose, and cost.
-
Identifying effective alternatives to antiretroviral medications for reducing the risk of transmission from mother to child, especially during breast feeding.
-
Finding effective ways to reduce the stigma associated with AIDS.
CONCLUSION
Preventing perinatal HIV transmission will not substantially reduce mortality in the target populations served by this study (mothers, fetuses, and neonates). However, as the swiftest and most affordable means of reducing the number of new AIDS cases in developing countries, prevention of mother-to-child infection represents a key opportunity for antenatal care in developing countries. Because stigma and discrimination associated with HIV infection may pose a considerable barrier to diagnosis, successful programs to prevent perinatal transmission will need to educate pregnant women about the risks and benefits of antenatal HIV screening and prophylaxis.
Clearly, the most reliable means of preventing perinatal HIV transmission is to prevent infection among women of childbearing age. Achieving this long-term objective will require the implementation of primary prevention strategies, as well as the education and empowerment of women. For the near term, the evidence and analyses reviewed in this chapter demonstrate that the goal of preventing HIV infection in substantial numbers of children born to infected women in developing countries is well within reach.
REFERENCES
Adetunji J. 2000. Trends in under-5 mortality rates and the HIV/AIDS epidemic. Bulletin of the World Health Organization 78(10):1200–1206.
Arifeen S, Black RE, Antelman G, Baqui A, Caulfield L, Becker S. 2001. Exclusive breastfeeding reduces acute respiratory infecton and diarrhea deaths among infants in Dhaka slums. Pediatrics 108(4):E67.
Ashraf RN, Jalil F, Zaman S, Karlberg J, Khan SR, Lindblad BS, Hanson LA. 1991. Breast feeding and protection against neonatal sepsis in a high risk population. Archives of Diesase in Childhood 66(4):499–490.
Berer M. 1999. Reducing perinatal HIV transmission in developing countries through antenatal and delivery care, and breastfeeding: supporting infant survival by supporting women’s survival. Bulletin of the World Health Organization 77(11):871–877.
Blanche S, Tardieu M, Rustin P. 1999. Persistent mitochondrial dysfunction and perinatal exposure to antiretroviral nucleoside analogues, Lancet 354(9184):1084–1089.
Brocklehurst P. 2002. Interventions aimed at decreasing the risk of mother-to-child transmission of HIV infection (Cochrane Review). Cochrane Library, Issue 2.
Brocklehurst P, Volmink J. 2002. Antiretrovirals for reducing the risk of mother-to-child transmission of HIV infection (Cochrane Review). Cochrane Library, Issue 2.
Burns DN, FitzGerald G, Semba R, Hershow R, Zorrilla C, Pitt J, Hammill H, Cooper ER, Fowler MG, Landesman S. 1999. Vitamin A deficiency and other nutritional indices during pregnancy in human immunodeficiency virus infection: prevalence, clinical correlates, and outcome. Women and Infants Transmission Study Group. Clinical Infectious Diseases 29(2):328–334.
Centers for Disease Control and Prevention (CDC). 1999. HIV/AIDS Surveillance Report 11(2).
Centers for Disease Control and Prevention (CDC). 2001. Serious adverse events attributed to nevirapine regimens for postexposure prophylaxis after HIV exposures—Worldwide, 1997–2000. Mortality and Morbidity Weekly Review 49(51):1153–1156.
Chatterjee N. 1999. They have not heard of AIDS: HIV/AIDS awareness among married women in Bombay. Public Health 113(3):137–140.
Coll O, Fiore S, Floridia M, Giaquinto C, Grosch-Worner I, Guiliano M, Lindgren S, Lyall H, Mandelbrot L, Newell ML, Peckham C, Rudin C, Semprini AE, Taylor G, Thorne C, Tovo PA. 2002. Pregnancy and HIV infection: a European consensus on management. AIDS 16(Suppl)2:S1-S18.
Chotpitayasunondh T, Vanprapar N, Simonds RJ, Chokephaibulkit K, Waranawat N, Mock P, Stat MA, Chuachoowong R, Young N, Mastro TD, Shaffer N. 2001. Safety of late in utero exposure to zidovudine in infants born to human immunodeficiency virus-infected mothers: Bangkok. Bangkok Collaborative Perinatal HIV Transmission Study Group. Pediatrics 107(1):E5.
Connor E, Sperling R, Gelber R, Kiselev P, Scott G, O’Sullivan MJ, VanDyke R, Bey M, Shearer W, Jacobson RL, et al. 1994. Reduction of maternal-infant transmission of human immunodeficiency virus type 1 with zidovudine treatment. New England Journal of Medicine 331(18):1173–1180.
Coutsoudis A, Pillay K, Spooner E, Kuhn L, Coovadia HM. 1999. Randomized trial testing the effect of vitamin A supplementation on pregnancy outcomes and early mother-to-child HIV-1 transmission in Durban, South Africa. South African Vitamin A Study Group. AIDS 13(12):1517–1524.
Coutsoudis A, Pillay K, Kuhn L, Spooner E, Tsai WY, Coovadia HM, South African Vitamin A Study Group. 2001. Method of feeding and transmission of HIV-1 from mothers to children by 15 months of age: prospective cohort study from Durban, South Africa. AIDS 15(3):379–387.
Culnane M, Fowler M, Lee SS, McSherry G, Brady M, O’Donnell K, Mofenson L, Gortmaker SL, Shapiro DE, Scott G, Jimenez E, Moore EC, Diaz C, Flynn PM, Cunningham B, Oleske J. 1999. Lack of long-term effects of in utero exposure to zidovudine among uninfected children born to HIV-infected women. Journal of the American Medical Association 281(2):151–157.
Dabis F, Msellati P, Meda N, Welffens-Ekra C, You B, Manigart O, Leroy V, Simonon A, Cartoux M, Combe P, Ouangre A, Ramon R, Ky-Zerbo O, Montcho C, Salamon R, Rouzioux C, Van de Perre P, Mandelbrot L. 1999. Six–month efficacy, tolerance, and acceptability of a short regimen of oral zidovudine to reduce vertical transmission of HIV in breastfed children in Cote d’Ivoire and Burkina Faso: a double-blind placebo-controlled multi-center trial. Lancet 353(9155):786–792.
De Cock KM, Fowler MG, Mercier E, de Vincenzi I, Saba J, Hoff E, Alnwick DJ, Rogers M, Shaffer N. 2000. Prevention of mother-to-child HIV transmission in resource-poor countries. Journal of the American Medical Association 283(9):1175–1182.
Eshleman SH, Jackson JB. 2002. Nevirapine resistance after single dose prophylaxis. AIDS Review 4(2):59–63
European Collaborative Study. 1992. Risk factors for mother-to-child transmission of HIV-1. Lancet 339(8800):1007–1012
Euroguidelines Group for HIV Resistance. 2001. Clinical and laboratory guidelines for the use of HIV-1 drug resistance testing as part of treatment management: recommendations for the European setting. The EuroGUidelines Group for HIV resistance. AIDS 15(3):309–320.
Fawzi W. 2000. Nutritional factors and vertical transmission of HIV-1. Epidemiology and potential mechanisms. Annals of the New York Academis of Science 918:99–114.
Fawzi W, Msamanga G, Spiegelman D, Renjifo B, Bang H, Kapiga S, Coley J, Hertzmark E, Essex M, Hunter D. 2002a. Transmission of HIV-1 through breastfeeding among women in Dar es Salaam, Tanzania. Journal of Acquired Immune Deficiency Syndrome 31(3):331–338.
Fawzi WW, Msamanga GI, Hunter D, Renjifo B, Antelman G, Bang H, Manji K, Kapiga S, Mwakagile D, Essex M, Spiegelman D. 2002b. Randomized trial of vitamin supplements in relation to transmission of HIV-1 through breastfeeding and early child mortality. AIDS 16(14)1935–1944.
Fowler MG, Bertolli J, Nieburg P. 1999. When is breastfeeding not best? The dilemma facing HIV-infected women in resource-poor settings. Journal of the American Medical Association 282(8):781–783.
Garcia PM, Kalish LA, Pitt J, Minkoff H, Quinn TC, Burchett SK, Kornegay J, Jackson B, Moye J, Hanson C, Zorrilla C, Lew JF. 1999. Maternal levels of plasma human immunodeficiency virus type 1 RNA and the risk of perinatal transmission. New England Journal of Medicine 341(6):394–402.
Gellman B. 2000. A turning point that left millions behind. The Washington Post December 28.
Greenberg BL, Semba RD, Vink PE, Farley JJ, Sivapalasingam M, Steketee RW, Thea DM, Schoenbaum EE. 1997. Vitamin A deficiency and maternal-infant transmissions of HIV in two metropolitan areas in the United States. AIDS 11(3):325–332.
Guay LA, Musoke P, Fleming T, Bagenda D, Allen M, Nakabiito C, Sherman J, Bakaki P, Ducar C, Deseyve M, Emel L, Mirochnick M, Fowler MG, Mofenson L, Miotti P, Dransfield K, Bray D, Mmiro F, Jackson JB. 1999. Intrapartum and neonatal single-dose nevirapine compared with zidovudine for prevention of mother-to-child transmission of HIV-1 in Kampala, Uganda: HIVNET 012 randomized trial. Lancet 354(9181):795–802.
Hirsch MS. 2002. HIV drug resistance—a chink in the armor. New England Journal of Medicine 347(6):438–439.
Institute of Medicine (IOM). 1999. Reducing the Odds: Preventing Perinatal Transmission of HIV in the United States.Washington, DC: National Academy Press.
International Perinatal HIV Group. 1999. The mode of delivery and the risk of vertical transmission of human immunodeficiency virus type 1—a meta-analysis of 15 prospective cohort studies. New England Journal of Medicine 340(13):977–987.
International Perinatal HIV Group. 2001. Duration of ruptured membranes and vertical transmission of HIV-1: a meta-analysis from 15 prospective cohort studies. AIDS 15(3):357–368.
Joint United Nations Programme on HIV/AIDS (UNAIDS). 1999. Statement of the Joint United Nations Programme on HIV/AIDS (UNAIDS) at the Third WTO Ministerial Conference, Seattle.
Joint United Nations Programme on HIV/AIDS (UNAIDS). 2000a. New UN report estimates over one-third of today’s 15-year-olds will die of AIDS in worst affected countries. Press release, 27 June 2000. Geneva: WHO.
Joint United Nations Programme on HIV/AIDS (UNAIDS). 2000b. Use of nevirapine to reduce mother-to-child transmission of HIV (MTCT). WHO report of Reported Drug Resistance. Geneva: WHO.
Joint United Nations Programme on HIV/AIDS (UNAIDS). 2001. AIDS Epidemic Update: December 2001. Geneva: UNAIDS/WHO.
Joint United Nations Programme on HIV/AIDS (UNAIDS). 2002. Report on the Global HIV/ AIDS Epidemic, 2002. Geneva: UNAIDS.
Joint United Nations Programme on HIV/AIDS Reference Group on Estimates, Modelling and Projections. 2002. Improved methods and assumptions for estimation of the HIV/ AIDS epidemic and its impact: recommendations of the UNAIDS Reference Group on Estimates, Modelling and Projections. AIDS 16(9):W1–W14
Kowalczyk J, Jolly P, Karita E, Nibarere JA, Vyankandondera J, Salihu H. 2002. Voluntary counseling and testing for HIV among pregnant women presenting in labor in Kigali, Rwanda. Journal of Acquired Immune Deficiency Syndrome 31(4):408–415.
Kumwenda N, Miotti PG, Taha TE, Broadhead R, Biggar RJ, Jackson JB, Melikian G, Semba RD. 2002. Antenatal vitamin A supplementation increases birth weight and decreases anemia among infants born to human immunodeficiency virus-infected women in Malawi. Clinical Infectious Diseases 35(5):618–624.
Lallemant M, Jourdain G, Le Coeur S, Kim S, Koetsawang S, Comeau AM, Phoolcharoen W, Essex M, McIntosh K, Vithayasai V. 2000. A trial of shortened zidovudine regimens to prevent mother-to-child transmission of human immunodeficiency virus type I. New England Journal of Medicine 343(14):982–991.
Mandelbrot L, Landreau-Mascaro A, Rekacewicz C, Berrebi A, Benifla JL, Burgard M, Lachassine E, Barret B, Chaix ML, Bongain A, Ciraru-Vigneron N, Crenn-Hebert, C, Delfraissy JF, Rouzioux C, Mayaux MJ, Blanche S, Agence Nationale de Recherches sur le SIDA (ANRS) 075 Study Group. 2001. Lamivudine-zidovudine combination for prevention of maternal-infant transmission of HIV-1. Journal of the American Medical Association 285(16):2083–2093.
Mansergh G, Haddix AC, Steketee RW, Nieburg PI, Hu DJ, Simonds RJ, Rogers M. 1996. Cost-effectiveness of short-course zidovudine to prevent perinatal HIV Type I infection in a sub-Saharan African developing country setting. Journal of the American Medical Association 276(2):139–145.
Mansergh G, Haddix AC, Steketee RW, Simonds RJ. 1998. Cost-effectiveness of zidovudine to prevent mother-to-child transmission of HIV in sub-Saharan Africa. Journal of the American Medical Association 280(1):30–31.
Marseille E, Kahn JG, Saba J. 1998. Cost-effectiveness of antiviral drug therapy to reduce mother-to-child HIV transmission in sub-Saharan Africa. AIDS 12:939–948.
Marseille E, Marseille E, Kahn JG, Mmiro F, Guay L, Musoke P, Fowler MG, Jackson JB. 1999. Cost-effectiveness of single-dose nevirapine regimen for mothers and babies to decrease vertical HIV-1 transmission in sub-Saharan Africa. Lancet 354(9181):803–809.
Meda N, Leroy V, Viho I, Msellati P, Yaro S, Mandelbrot L, Montcho C, Manigart O, Dabis F. 2002. Field acceptability and effectiveness of the routine utilization of zidovudine to reduce mother-to-child transmission of HIV-1 in West Africa. AIDS 16(17):2323–2328.
Mofenson, L. 1997. Mother-child HIV-1 transmission: timing and determinants, Obstetrics and Gynecology Clinics of North America 24(4):759–784.
Mofenson LM, McIntyre JA. 2000. Advances and research directions in the prevention of mother-to-child HIV-1 transmission. Lancet 355(9222):2237–2244.
Mofenson LM, Lambert JS, Stiehm ER, Bethel J, Meyer WA 3rd, Whitehouse J, Moye J Jr, Reichelderfer P, Harris DR, Fowler MG, Mathieson BJ, Nemo GJ. 1999. Risk factors for perinatal transmission of human immunodeficiency virus type 1 in women treated with zidovudine. New England Journal of Medicine 341(6):385–393.
Moodley D. 2000. The SAINT trial: nevirapine (NVP) versus zidovudine (ZDV) + lamivudine (3TC) in prevention of peripartum HIV transmission. Paper read at 13th International AIDS Conference, Durban, South Africa, July 9–14, 2000. Abstract LbOr2. Available online at http://www.iac2000.org/abdetail.asp?ID=LbOr2.
Morris L, Pillay C, Gray G, McIntyre J. 2001. HIV-1 drug resistance and mother-to-child transmission. South African Dental Association 56(12):614–616.
Mukwaya J. 1999. The AIDS Emergency. In: The Progress of Nations. New York: UNICEF 1999. Pp. 17–19. Available online at http://www.unicef.org/pon99/.
Newell M. 2000. Vertical transmission of HIV-1 infection. Transactions of the Royal Society of Tropical Medicine and Hygiene 94(1):1–2.
Nduati R, John G, Mbori-Ngacha D, Richardson B, Overbaugh J, Mwatha A, Ndinya-Achola J, Bwayo J, Onyango FE, Hughes J, Kreiss J. 2000. Effect of breastfeeding and formula feeding on transmission of HIV-1. Journal of the American Medical Association 283(9):1167–1174.
Nicoll A, Newell ML, Van Praag E, Van de Perre P, Peckham C. 1995. Infant feeding policy and practice in the presence of HIV-1 infection. AIDS 9(2):107–119.
Nolan ML, Greenberg AE, Fowler MG. 2002. A review of clinical trials to prevent mother-to-child HIV-1 transmission in Africa and inform rational intervention strategies. AIDS 16(15):1991–1999.
Peiperl L. 2001. Antiretroviral treatments to reduce mother-to-child transmission of HIV. HIV Clinical Trials 2(1):46–55.
Petra Study Team. 2002. Efficacy of three short-course regimens of zidovudine and lamivudine in preventing early and late transmission of HIV-1 from mother to child in Tanzania, South Africa, and Uganda (Petra study): a randomised, double-blind, placebo-controlled trial. Lancet 359(9313):1178–1186.
Semba RD. 1997. Overview of the potential role of vitamin A in mother-to-child transmission of HIV. Acta Paediatrica Supplement 421:107–112.
Shaffer N, Chuachoowong R, Mock PA, Bhadrakom C, Siriwasin W, Young NL, Chotpitayasunondh T, Chearskul S, Roongpisuthipong A, Chinayon P, Karon J, Mastro TD, Simonds RJ. 1999. Short-course zidovudine for perinatal HIV-1 transmission in Bangkok, Thailand: a randomised controlled trial. Lancet 353(9155):773–780.
Söderlund N, Zwi K, Kinghorn A, Gray G. 1999. Prevention of vertical transmission HIV: analysis of cost effectiveness options available in South Africa. British Medical Journal 318(7199):1650–1656.
Stoto MA, Goldman AS. 2003. Preventing Perinatal Transmission of HIV. RAND, DRU-3071.
Taha TE, Graham SM, Kumwenda NI, Broadhead RL, Hoover DR, Markakis D, van Der Hoeven L, Liomba GN, Chiphangwi JD, Miotti PG. 2000. Morbidity among human immunodeficiency virus-1-infected and -uninfected African children. Pediatrics 106(6):E77.
Tudor-Williams G. 2000. HIV infection in children in developing countries. Transactions of the Royal Society of Tropical Medicine and Hygiene 94(1):3–4.
Walker N, Schwartlander B, Bryce J. 2002. Meeting international goals in child survival and HIV/AIDS. Lancet 360(9329):284–289.
Wiktor S, Ekpini E, Karon J. 1999. Short-course oral zidovudine for prevention of mother-to-child transmission of HIV-1 in Abidjan, Cote d’Ivoire: a randomised trial. Lancet 353:781–785.
Wilkinson D, Floyd K, Gilks CF. 1998. Antiretroviral drugs as a public health intervention for pregnant HIV-infected women in rural South Africa: an issue of cost-effectiveness and capacity. AIDS 12(13):1675–1682.
Wilson JMG, Jungner F. 1968. Principles and practice of screening for disease. Public Health Paper 34. Geneva: WHO.
World Bank. 1993. World Development Report 1993: Investing in Health. New York: Oxford University Press.
World Health Organization (WHO), Joint United Nations Programme on HIV/AIDS. 1998. HIV and Infant Feeding, Guidelines for Decision Makers. Geneva: WHO. Available online at http://www.unaids.org/publications/documents/mtct/infantpolicy.html.
World Health Organization (WHO). 2000. New Data on the Prevention of Mother-to-Child Transmission of HIV and Their Policy Implications: Conclusions and Recommendations. Geneva, 11–13 October 2000. Available online at http://www.unaids.org/publications/documents/.
World Health Organization Collaborative Study Team, 2000. Effect of breastfeeding on infant and child mortality due to infectious diseases in less developed countries: a pooled analysis. WHO Collaborative Study Team on the Role of Breastfeeding on the Prevention of Infant Mortality. Lancet 355(9202):451–455.