Executive Summary
PATIENT SAFETY CONTINUES TO BE THREATENED
In its report To Err Is Human: Building a Safer Health System, the Institute of Medicine (IOM) estimated that as many as 98,000 hospitalized Americans die each year—not as a result of their illness or disease, but as a result of errors in their care (IOM, 2000). This alarming number, which reflects only deaths occurring in hospital settings, exceeds the numbers of fatalities due to motor vehicle accidents, breast cancer, or AIDS. Moreover, this figure does not reflect the many patients who survive, but sustain serious injuries.
This high volume of errors was recently affirmed by some with firsthand knowledge of errors—practicing physicians, patients, and their families. Fully 35 percent of practicing physicians and 42 percent of members of the American public responding to a 2002 national survey reported having experienced an error either in their own care or in that of a family member. Moreover, 18 percent of the physicians and 24 percent of the members of the public responding cited an error that had serious health consequences, including death, long-term disability, and severe pain (Blendon et al., 2002).
This profusion of health care errors has received attention from federal and state policy makers, health care organizations (HCOs), individual health care practitioners, and experts on safety from a variety of disciplines. Key stimuli for this increased attention have included actions undertaken by the federal government to fund more research on why such errors occur and how to prevent them, to collect data on patient safety, to support new information technology for health care delivery, and to disseminate patient safety information to consumers and providers (Clancy and Scully, 2003).
In this context, and in recognition of evidence on the key role of nurses in patient safety, the U.S. Department of Health and Human Services’ (DHHS) Agency for Healthcare Research and Quality (AHRQ) asked the IOM to conduct a study to identify:
-
Key aspects of the work environment for nurses that likely have an impact on patient safety.
-
Potential improvements in health care working conditions that would likely increase patient safety.
AHRQ further directed that the study be conducted “in the context of current policy debates on regulation of nursing work hours and nursing workload … [and] cover such topics as: extended work hours and fatigue, including mandatory overtime; workload issues, including state regulation of nurse-to-bed ratios; workplace environmental issues, including poorly designed care processes; … workplace systems, including reliance on memory and lack of support systems for decision-making; and workplace communication, including social, physical, and other barriers to effective communication among care team members.” The IOM convened the Committee on the Work Environment for Nurses and Patient Safety to conduct this study.
THE CRITICAL ROLE OF NURSES IN PATIENT SAFETY
The 2.8 million licensed nurses and 2.3 million nursing assistants providing patient care in this country represent approximately 54 percent of all health care workers and provide patient care in virtually all locations in which health care is delivered—hospitals; nursing homes; ambulatory care settings, such as clinics or physicians’ offices; private homes; schools; and employee workplaces. When people are hospitalized, in a nursing home, having a baby, or learning to manage a chronic condition in their own home—at some of their most vulnerable moments—nurses are the health care providers they are most likely to encounter; spend the greatest amount of time with; and, along with other health care providers, depend on for their recovery.
Research is now beginning to document what physicians, patients, other health care providers, and nurses themselves have long known: how well we are cared for by nurses affects our health, and sometimes can be a matter of life or death. As physicians in the American College of Critical Care Medicine have noted: “Critical care nurses do the majority of patient assessment, evaluation, and care in the ICU [intensive care unit]” (Brilli et al., 2001:2011). Nursing actions, such as ongoing monitoring of patients’ health status, are directly related to better patient outcomes (Kahn et al., 1990;
Mitchell and Shortell, 1997; Rubenstein et al., 1992). Nursing vigilance also defends patients against errors. A study of medication errors in two hospitals over a 6-month period found that nurses were responsible for 86 percent of all interceptions of medication errors made by physicians, pharmacists, and others involved in providing medications for patients before the error reached the patient (Leape et al., 1995).
In reviewing evidence on acute hospital nurse staffing published from 1990 to 2001, the AHRQ report Making Health Care Safer: A Critical Analysis of Patient Safety Practices (Seago, 2001:430) concluded that “leaner nurse staffing is associated with increased length of stay, nosocomial infection (urinary tract infection, postoperative infection, and pneumonia), and pressure ulcers.… These studies … taken together, provide substantial evidence that richer nurse staffing is associated with better patient outcomes.” Subsequent studies have added to this evidence base and substantiate the observation that greater numbers of patient deaths are associated with fewer nurses to provide care (Aiken et al., 2002), and less nursing time provided to patients is associated with higher rates of infection, gastrointestinal bleeding, pneumonia, cardiac arrest, and death from these and other causes (Needleman et al., 2002). In caring for us all, nurses are indispensable to our safety.
NURSES’ WORK ENVIRONMENTS: A THREAT TO PATIENT SAFETY
In conducting this study, the committee reviewed evidence on the work and work environments of nurses; related health services, nursing, behavioral, and organizational research; findings from human factors analysis and engineering; and studies of safety in other industries. This evidence revealed that the typical work environment of nurses is characterized by many serious threats to patient safety. These threats are found in all four of the basic components of all organizations—organizational management practices, workforce deployment practices, work design, and organizational culture.
Frequent Failure to Follow Management Practices Necessary for Safety
Certain management practices are essential to the creation of safety within organizations and to the success of the organizational changes often needed to build stronger patient safety defenses. These practices include (1) balancing the tension between production efficiency and reliability (safety), (2) creating and sustaining trust throughout the organization, (3) actively managing the process of change, (4) involving workers in decision making pertaining to work design and work flow, and (5) using knowledge man-
agement practices to establish the organization as a “learning organization.” Evidence shows that these practices are not employed in many nursing work environments.
In particular, many hospital restructuring and redesign initiatives1 that have been widely adopted over the last two decades have changed the ways in which licensed nurses and nurse assistants are organized to provide patient care. Many of these changes have been focused largely on increasing efficiency and have been undertaken in ways that have damaged trust between nursing staff and management. Changes often have been poorly managed so that intended results have not been achieved, infrequently have involved nurses in decision making pertaining to the redesign of their work, and have not employed practices that encourage the uptake and dissemination of knowledge throughout the organization. The committee found, for example, that:
-
Loss of trust in hospital administration is widespread among nursing staff (Decker et al., 2001; Ingersoll et al., 2001; Kramer and Schmalenberg, 1993). This loss of trust stems in part from a perception that initiatives in patient care and nursing work redesign have emphasized efficiency over patient safety. Poor communication practices have also led to mistrust (Walston and Kimberly, 1997). This loss of trust has serious implications for the ability of hospitals and other HCOs to make the fundamental changes essential to providing safer patient care.
-
Clinical nursing leadership has been reduced at multiple levels, and the voice of nurses in patient care has diminished. Hospital reengineering initiatives often have resulted in the loss of a separate department of nursing (Gelinas and Manthey, 1997). At the same time, nursing staff have perceived a decline in chief nursing executives with power and authority equal to that of other top hospital officials, as well as in directors of nursing who are highly visible and accessible to staff (Aiken et al., 2000). These changes—along with losses of chief nursing officers without replacement; decreases in the numbers of nurse managers; and increased responsibilities of remaining nurse managers for more than one patient care unit, as well as for supervising personnel other than nursing staff (e.g., housekeepers, transportation staff, dietary aides) (Aiken et al., 2001; Sovie and Jawad, 2001)—have had the cumulative effect of reducing direct management support available to patient care staff. This situation hampers nurses’ ability to fix problems in their work environments that threaten patient safety (Tucker and Edmondson, 2002).
Unsafe Workforce Deployment
Despite the strong and accumulating evidence that higher nurse staffing levels in hospitals and nursing homes result in safer patient care, there is wide variation in nurse staffing levels across hospitals and nursing homes. Data from 135 hospitals contacted in 2002 show that although a nurse working in a medical–surgical unit on the day shift typically is assigned six patients to care for, that number is sometimes much higher for individual nurses. Fully 23 percent of hospitals reported that nurses in their medical–surgical units on the day shift were each responsible for caring for 7 to 12 patients (Cavouras and Suby, 2003). Nursing homes also vary in the number of patients assigned to nursing staff.
Currently available methods for achieving safer staffing levels in hospitals, such as authorizing nursing staff to halt admissions to their unit when staffing is inadequate for safe patient care, are not employed uniformly by hospitals or nursing homes. Federal regulations governing nursing home staffing are over a decade old and do not reflect new knowledge on safe staffing levels. Minimum standards for registered nurses require only the presence of one licensed nurse in a nursing home, regardless of its size. Moreover, the regulations do not specify minimum staffing levels for nurse assistants, who provide most of the nursing care in these facilities.
Additionally, not all HCOs have taken steps to compensate for the widely acknowledged fact that, like newly licensed physicians, newly licensed nurses need additional training and education once they enter the workforce, and that experienced nurses similarly need ongoing education and training to keep up with the continuing growth of new medical knowledge and technology. Surveys of nursing administrators from acute care hospitals and nursing homes and newly licensed nurses themselves report the same finding: many newly licensed nurses do not possess the overall educational preparation to provide safe, effective care. Registered nurses (RNs) are viewed as especially lacking skills in recognizing abnormal physical and diagnostic findings and responding to emergencies (Smith and Crawford, 2002a,b).
Despite these findings, hospitals are reported to have scaled back orientation programs for newly hired nurses, as well as ongoing in-service training and continuing education programs, as a result of financial pressures (Berens, 2000). A federally sponsored study of staffing in long-term care facilities similarly found that current initial certification education for nurse assistants is insufficient (CMS, 2002). The committee found evidence that all health care professionals (nurses and physicians alike) need better training, as well as organizational practices that promote and support interdisciplinary collaboration and teamwork. Decision support technology is also needed in all nursing work environments.
Unsafe Work and Workspace Design
Several aspects of the way in which nurses’ work is designed pose threats to patient safety. The long work hours of some nurses represent one of the most serious threats. While most nurses typically work 8- or 12-hour shifts, some work much longer hours. In one study, 3.5 percent of scheduled shifts exceeded 12 hours, including “shifts” as long as 22.5 hours.2 In another study, 27 percent of full-time hospital and nursing home nurses reported working more than 13 hours at a stretch one or more times a week.3 The effects of fatigue on human performance are well known. Prolonged periods of wakefulness (e.g., 17 hours without sleep) can produce performance decrements equivalent to a blood alcohol concentration (BAC) of 0.05 percent, the BAC level defined as alcohol intoxication in many western industrialized countries (Dawson and Reid, 1997; Lamond and Dawson, 1998).4
Other nursing work processes, such as medication administration, are often carried out in ways that are conducive to the commission of errors and without the support of newer technologies that can prevent errors in medication administration. One study of preventable adverse drug events in hospitals found that 34 percent of medication errors took place in the course of administering the drug (a nursing role), as opposed to occurring as a part of ordering, transcribing, or dispensing the drug (Bates et al., 1995). A similar 6-month study of all adverse drug events in two tertiary care hospitals found that 38 percent occurred during the administration of the drug by nursing staff (Pepper, 1995).
Other inefficient care processes and workspace design features decrease patient safety by reducing the amount of time nurses have for monitoring patients and providing therapeutic care. For example, while not intrinsically dangerous to patients, documentation of patient information and care processes consumes an estimated 13–28 percent of a hospital nurse’s time (Pabst et al., 1996; Smeltzer et al., 1996; Upenieks, 1998; Urden and Roode, 1997). For home care nurses, the time required is estimated to be much greater as a result of regulatory requirements for patient information and assessment (Trossman, 2001). Other inefficiencies arise from interruptions
and distractions associated with nursing tasks; workspaces not designed to facilitate nursing organization and activities; limited access to information systems; and other common work practices, including using nurses to perform such non-nursing duties as picking up blood products and delivering laboratory specimens.
Punitive Cultures That Hinder the Reporting and Prevention of Errors
To Err Is Human also calls attention to the need to create organizational cultures of safety that promote the reporting, analysis, and prevention of errors within all HCOs. The committee finds that while some progress has been made in fostering such cultures, full implementation has not yet been achieved. Incidents have been reported in which nurses who were involved in the commission of an error but found blameless by a number of independent authoritative bodies were unjustly disciplined by state regulatory agencies. HCOs need the assistance of state and federal oversight organizations if they are to create fully effective programs for detecting and preventing patient care errors in their organizations.
NEED FOR BUNDLES OF MUTUALLY REINFORCING PATIENT SAFETY DEFENSES IN NURSES’ WORK ENVIRONMENTS
No single action can, by itself, keep patients safe from health care errors. Because multiple components and processes of HCOs create situations that nurture errors in the work environments of nurses, multiple, mutually reinforcing changes in those environments are needed to substantially reduce errors and increase patient safety. To this end, defenses must be created in all organizational components: (1) leadership and management, (2) the workforce, (3) work processes, and (4) organizational culture. Bundles of changes are needed within each of these components to strengthen patient safety.
Transformational Leadership and Evidence-Based Management
Creating work environments for nurses that are most conducive to patient safety will require fundamental changes throughout many HCOs in terms of how work is designed, how personnel are deployed, and how the very culture of the organization understands and acts on the science of safety. These changes require leadership capable of transforming not just physical environments, but also the beliefs and practices of both nurses and other health care workers providing patient care and those in the HCO who establish the policies and practices that shape those environments—the individuals who constitute the management of the organization.
Leadership will need to assure the effective use of practices that (1) balance the tension between production efficiency and reliability (safety), (2) create and sustain trust throughout the organization, (3) actively manage the process of change, (4) involve workers in decision making pertaining to work design and work flow, and (5) use knowledge management practices to establish the organization as a “learning organization.” To this end, the committee makes the following recommendations:
Recommendation 4-1.5 HCOs should acquire nurse leaders for all levels of management (e.g., at the organization-wide and patient care unit levels) who will:
-
Participate in executive decisions within the HCO.
-
Represent nursing staff to organization management and facilitate their mutual trust.
-
Achieve effective communication between nursing and other clinical leadership.
-
Facilitate input of direct-care nursing staff into operational decision making and the design of work processes and work flow.
-
Be provided with organizational resources to support the acquisition, management, and dissemination to nursing staff of the knowledge needed to support their clinical decision making and actions.
Recommendation 4-2. Leaders of HCOs should take action to identify and minimize the potential adverse effects of their decisions on patient safety by:
-
Educating board members and senior, midlevel, and line managers about the link between management practices and safety.
-
Emphasizing safety to the same extent as productivity and financial goals in internal management planning and reports and in public reports to stakeholders.
Recommendation 4-3. HCOs should employ management structures and processes throughout the organization that:
-
Provide ongoing vigilance in balancing efficiency and safety.
-
Demonstrate trust in workers and promote trust by workers.
-
Actively manage the process of change.
-
Engage workers in nonhierarchical decision making and in the design of work processes and work flow.
-
Establish the organization as a “learning organization.”
Because HCOs vary in the extent to which they currently employ the above practices and in their available resources, the committee also makes the following recommendation:
Recommendation 4-4. Professional associations, philanthropic organizations, and other organizational leaders within the health care industry should sponsor collaboratives that incorporate multiple academic and other research-based organizations to support HCOs in the identification and adoption of evidence-based management practices.
Maximizing Workforce Capability
Monitoring patient health status, performing therapeutic treatments, and integrating patient care to avoid health care gaps are nursing functions that directly affect patient safety. Accomplishing these activities requires an adequate number of nursing staff with the clinical knowledge and skills needed to carry out these interventions and the ability to effectively communicate findings and coordinate care with the interventions of other members of the patient’s health care team. Nurse staffing levels, the knowledge and skill level of nursing staff, and the extent to which workers collaborate in sharing their knowledge and skills all affect patient outcomes and safety.
Regulatory, internal HCO, and marketplace (consumer-driven) approaches are traditionally advocated as methods to achieve appropriate staffing levels. The committee determined that each of these approaches has limitations as well as strengths; their coordinated and combined use holds the most promise for achieving safe staffing levels. The committee also took particular note of the need for more accurate and reliable staffing data for hospitals and nursing homes to help make these efforts more effective and to facilitate additional needed research on staffing. Finally, the committee identified a need for more research on hospital staffing for specific types of patient care units, such as medical–surgical and labor and delivery units. The committee therefore makes the following recommendations:
Recommendation 5-1. The U.S. Department of Health and Human Services (DHHS) should update existing regulations established in 1990 that specify minimum standards for registered and licensed
nurse staffing in nursing homes. Updated minimum standards should:
-
Require the presence of at least one RN within the facility at all times.
-
Specify staffing levels that increase as the number of patients increase, and that are based on the findings and recommendations of the DHHS report to Congress, Appropriateness of Minimum Nurse Staffing Ratios in Nursing Homes—Phase II Final Report.
-
Address staffing levels for nurse assistants, who provide the majority of patient care.
Recommendation 5-2. Hospitals and nursing homes should employ nurse staffing practices that identify needed nurse staffing for each patient care unit per shift. These practices should:
-
Incorporate estimates of patient volume that count admissions, discharges, and “less than full-day” patients in addition to a census of patients at a point in time.
-
Involve direct-care nursing staff in determining and evaluating the approaches used to determine appropriate unit staffing levels for each shift.
-
Provide for staffing “elasticity” or “slack” within each shift’s scheduling to accommodate unpredicted variations in patient volume and acuity and resulting workload. Methods used to provide slack should give preference to scheduling excess staff and creating cross-trained float pools within the HCO. Use of nurses from external agencies should be avoided.
-
Empower nursing unit staff to regulate unit work flow and set criteria for unit closures to new admissions and transfers as nursing workload and staffing necessitate.
-
Involve direct-care nursing staff in identifying the causes of nursing staff turnover and in developing methods to improve nursing staff retention.
Recommendation 5-3. Hospitals and nursing homes should perform ongoing evaluation of the effectiveness of their nurse staffing practices with respect to patient safety, and increase internal oversight of their staffing methods, levels, and effects on patient safety whenever staffing falls below the following levels for a 24-hour day:
-
In hospital ICUs—one licensed nurse for every 2 patients (12 hours of licensed nursing staff per patient day).
-
In nursing homes, for long-stay residents—one RN for every 32 patients (0.75 hours per resident day), one licensed nurse for every 18 patients (1.3 hours per resident day), and one nurse assistant for every 8.5 patients (2.8 hours per resident day).
Recommendation 5-4. DHHS should implement a nationwide, publicly accessible system for collecting and managing valid and reliable staffing and turnover data from hospitals and nursing homes. Information on individual hospital and nursing home staffing at the level of individual nursing units and the facility in the aggregate should be disclosed routinely to the public.
-
Federal and state nursing home report cards should include standardized, case-mix–adjusted information on the average hours per patient day of RN, licensed, and nurse assistant care provided to residents and a comparison with federal and state standards.
-
During the next 3 years, public and private sponsors of the new hospital report card to be located on the federal government website should undertake an initiative—in collaboration with experts in acute hospital care, nurse staffing, and consumer information—to develop, test, and implement measures of hospital nurse staffing levels for the public.
Moreover, the knowledge base on effective clinical care and new health care technologies is increasing rapidly, making it impossible for nurses (and other clinicians) to incorporate this information into their clinical decision making and practice without organizational support. Organizational studies and research on exemplary work environments indicate the importance of investment in ongoing employee learning by employers. The committee therefore makes the following recommendation:
Recommendation 5-5. HCOs should dedicate budgetary resources equal to a defined percentage of nursing payroll to support nursing staff in their ongoing acquisition and maintenance of knowledge and skills. These resources should be sufficient for and used to implement policies and practices that:
-
Assign experienced nursing staff to precept nurses newly practicing in a clinical area to address knowledge and skill gaps.
-
Annually ensure that each licensed nurse and nurse assistant has an individualized plan and resources for educational development within health care.
-
Provide education and training of staff as new technology or changes in the workplace are introduced.
-
Provide decision support technology identified with the active involvement of direct-care nursing staff to enable point-of-care learning.
-
Disseminate to individual staff organizational learning as captured in clinical tools, algorithms, and pathways.
Finally, in response to evidence on inconsistent interprofessional collaboration among nursing staff and other health care providers, the committee makes the following recommendation:
Recommendation 5-6. HCOs should take action to support interdisciplinary collaboration by adopting such interdisciplinary practice mechanisms as interdisciplinary rounds, and by providing ongoing formal education and training in interdisciplinary collaboration for all health care providers on a regularly scheduled, continuous basis (e.g., monthly, quarterly, or semiannually).
Design of Work and Workspace to Prevent and Mitigate Errors
Nurses’ work processes and workspaces need to be designed to make them more efficient, less conducive to the commission of errors, and more amenable to detecting and remedying errors when they occur. The work hours of a minority of nurses, in particular, are identified as a serious threat to the safety of patients. The effects of fatigue include slowed reaction time, lapses of attention to detail, errors of omission, compromised problem solving, reduced motivation, and decreased energy for successful completion of required tasks. Other safety-sensitive industries have acknowledged and taken action to defend against these effects by limiting the number of shifts or hours worked in a week.
Changing work patterns will require attention from HCOs, regulatory bodies, state boards of nursing, schools of nursing, and nurses themselves. Accordingly, the committee makes the following recommendation:
Recommendation 6-1. To reduce error-producing fatigue, state regulatory bodies should prohibit nursing staff from providing patient care in any combination of scheduled shifts, mandatory over-
time, or voluntary overtime in excess of 12 hours in any given 24-hour period and in excess of 60 hours per 7-day period. To this end:
-
HCOs and labor organizations representing nursing staff should establish policies and practices designed to prevent nurses who provide direct patient care from working longer than 12 hours in a 24-hour period and in excess of 60 hours per 7-day period.
-
Schools of nursing, state boards of nursing, and HCOs should educate nurses about the threats to patient safety caused by fatigue.
Enabling nursing staff to collaborate with other health care personnel in identifying high-risk and inefficient work processes and workspaces and (re)designing them for patient safety and efficiency is also essential. Moreover, documentation practices are in great need of redesign. However, this cannot be accomplished solely by nursing staff and internal HCO efforts. Because many documentation practices are driven by external parties, such as regulators and oversight organizations, these entities will need to assist in the redesign of documentation practices. To address these needs, the committee makes the following recommendations:
Recommendation 6-2. HCOs should provide nursing leadership with resources that enable them to design the nursing work environment and care processes to reduce errors. These efforts must directly involve direct-care nurses throughout all phases of the work design and should concentrate on errors associated with:
-
Surveillance of patient health status.
-
Patient transfers and other patient hand-offs.
-
Complex patient care processes.
-
Non–value-added activities performed by nurses, such as locating and obtaining supplies, looking for personnel, completing redundant and unnecessary documentation, and compensating for poor communication systems.
Recommendation 6-3. HCOs should address handwashing and medication administration among their first work design initiatives.
Recommendation 6-4. Regulators; leaders in health care; and experts in nursing, law, informatics, and related disciplines should jointly convene to identify strategies for safely reducing the burden associated with patient and work-related documentation.
Creating and Sustaining a Culture of Safety
Employing a nursing workforce strong in numbers and capabilities and designing their work to prevent errors will not be sufficient to fully safeguard patients. The largest and most capable workforce is still fallible, and the best-designed work processes are still designed by fallible individuals. Patient safety also requires an organizational commitment to vigilance to prevent potential errors, and to the detection, analysis, and redress of errors when they occur.
A variety of safety-conscious industries have made such a commitment and achieved substantially lower rates of errors by doing so. These organizations place as high a priority on safety as they do on production; all employees are fully engaged in the process of detecting high-risk situations before an error occurs. Management is so responsive to employees’ detection of risk that it dedicates time, personnel, budget, and training resources to bring about changes needed to make work processes safer. Employees also are empowered to act in dangerous situations to reduce the likelihood of adverse events. These attitudes and employee engagement are so pervasive and observable in the behaviors of these organizations and their employees that an actual culture of safety exists within the organization. These organizational cultures are effective because they (1) recognize that the majority of errors are created by systemic organizational defects in work processes, not by blameworthy individuals; (2) support staff; and (3) foster continuous learning by the organization as a whole and its employees.
HCOs should redouble their efforts to create such cultures of safety within their work environments. Such efforts require a long-term commitment because they necessitate changes in the attitudes and behaviors of both organizations and people. Time is needed to enact an initial change, evaluate, refine, and enact further change. Strong organizational leadership is also essential. The safety of patients needs to be a stated and visible priority, with every organizational member understanding that each is fallible, even with the best of intentions, as are the processes used. Moreover, establishing a fair and just culture in responding to errors reduces workers’ fear and disincentives to report errors and near misses. As a result, all nursing staff are more inclined to be vigilant for errors and near misses, with a view toward learning from each event and strengthening the culture of safety accordingly. Action also is needed from state boards of nursing and Congress to enable strong and effective cultures of safety to exist. To these ends, the committee makes the following recommendations:
Recommendation 7-1. HCO boards of directors, managerial leadership, and labor partners should create and sustain cultures of safety by implementing the recommendations presented previously and by:
-
Specifying short- and long-term safety objectives.
-
Continuously reviewing success in meeting these objectives and providing feedback at all levels.
-
Conducting an annual, confidential survey of nursing and other health care workers to assess the extent to which a culture of safety exists.
-
Instituting a deidentified, fair, and just reporting system for errors and near misses.
-
Engaging in ongoing employee training in error detection, analysis, and reduction.
-
Implementing procedures for analyzing errors and providing feedback to direct-care workers.
-
Instituting rewards and incentives for error reduction.
Recommendation 7-2. The National Council of State Boards of Nursing, in consultation with patient safety experts and health care leaders, should undertake an initiative to design uniform processes across states for better distinguishing human errors from willful negligence and intentional misconduct, along with guidelines for their application by state boards of nursing and other state regulatory bodies having authority over nursing.
Recommendation 7-3. Congress should pass legislation to extend peer review protections to data related to patient safety and quality improvement that are collected and analyzed by HCOs for internal use or shared with others solely for purposes of improving safety and quality.
Summary
Implementing all of the above recommendations will create the necessary bundles of mutually reinforcing patient safeguards in the work environments of nurses listed in Box ES-1.
IMPLEMENTING THE COMMITTEE’S RECOMMENDATIONS
The Recommendations Build on Two Prior IOM Reports
The committee’s recommendations build on those contained in two prior IOM reports: To Err Is Human: Building a Safer Health System (IOM, 2000) and Crossing the Quality Chasm: A New Health System for the 21st
|
BOX ES-1 Governing Boards That Focus on Safety
Leadership and Evidence-Based Management Structures and Processes
Effective Nursing Leadership
Adequate Staffing
|
Century (IOM, 2001). The authors of the Quality Chasm report identify four different levels for intervening in the delivery of health care: (1) the experience of patients; (2) the functioning of small units of care delivery (“microsystems”), such as surgical teams or nursing units; (3) the functioning of organizations that house the microsystems; and (4) the policy, payment, regulation, accreditation, and other external factors that shape the environment in which HCOs deliver care. To Err Is Human speaks mainly
Organizational Support for Ongoing Learning and Decision Support
Mechanisms That Promote Interdisciplinary Collaboration
Work Design That Promotes Safety
Organizational Culture That Continuously Strengthens Patient Safety
|
to the fourth level (i.e., policy, payment, regulation, accreditation, and other external factors) in its articulation of a national agenda for patient safety. Crossing the Quality Chasm addresses primarily how the experiences of patients and the work of microsystems of care should be changed (Berwick, 2002). The present report, which focuses on the third level (i.e., HCOs and their work environments), complements the work of the two prior IOM reports in three ways:
-
It provides greater detail about how HCOs can and should implement key recommendations from To Err Is Human and Crossing the Quality Chasm in such areas as creating cultures of safety and addressing work design.
-
It addresses aspects of the work environment that are critical to patient safety but are not addressed in either of the two prior reports, such as the adequacy of staffing levels and worker fatigue.
-
It unifies the work of the prior two IOM reports and this report into a framework that all HCOs can use to construct work environments more conducive to patient safety.
Piecemeal Approaches Will Not Be Successful
With respect to this report’s recommendations, the committee wishes to underscore that none of these recommendations is “less important.” Redesigned work practices will still be unsafe if the number of nurses available to perform the work as designed is insufficient. Nor will an apparently sufficient number of nurses perform as needed if they are suffering from the effects of fatigue, inexperienced in a given work process, or unfamiliar with the work processes because they have been secured from a temporary agency. Moreover, even when the most capable workforce provides care using the best-designed work processes, errors will still occur because neither the nurse nor the work process is perfect. Defenses against human errors can be developed and put in place only if nursing staff are not afraid of reporting those errors and are involved in designing even stronger defenses. Finally, instituting all of these defense strategies can be accomplished only by individuals who have a vision of and command resources for the organization as a whole—an organization’s leadership and management. Their actions are the essential precursor to creating safer health care environments by addressing all sources of threats to patient safety (see Figure ES-1).
Additional Research Necessitates Ongoing Change
Finally, the committee notes that changing health care delivery practices to increase patient safety must be an ongoing process. Research findings and dissemination of practices that other HCOs have found successful in improving patient safety will help HCOs as learning organizations add to their repertoire of patient safety practices. This report calls attention to several areas in which, at present, information is limited about how to design nurses’ work and work environments to make them safer for patients. Research is needed to provide better information on nursing-related errors, means of achieving safer work processes and workspace design, a standard-
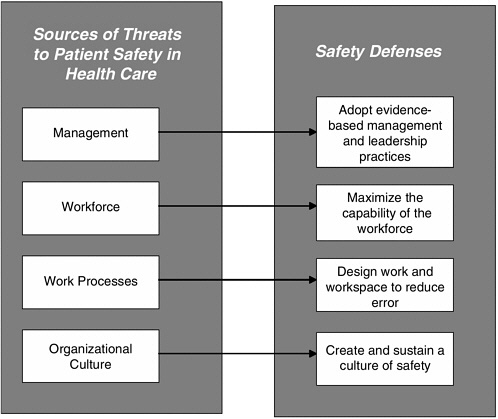
FIGURE ES-1 Sources of threats to patient safety in the work environment and corresponding safety defenses.
ized approach to measuring patient acuity, safe staffing levels for different types of patient care units, effective methods to help night shift workers compensate for fatigue, what limits should be imposed on successive days of working sustained work hours, and collaborative models of care. Accordingly, the committee makes the following recommendation:
Recommendation 8-1. Federal agencies and private foundations should support research in the following areas to provide HCOs with the additional information they need to continue to strengthen nurse work environments for patient safety:
-
Studies and development of methods to better describe, both qualitatively and quantitatively, the work nurses perform in different care settings.
-
Descriptive studies of nursing-related errors.
-
Design, application, and evaluation (including financial costs and savings) of safer and more efficient work processes and workspace, including the application of information technology.
-
Development and testing of a standardized approach to measuring patient acuity.
-
Determination of safe staffing levels within different types of nursing units.
-
Development and testing of methods to help night shift workers compensate for fatigue.
-
Research on the effects of successive work days and sustained work hours on patient safety.
-
Development and evaluation of models of collaborative care, including care by teams.
REFERENCES
Aiken L, Clarke S, Sloane D. 2000. Hospital restructuring: Does it adversely affect care and outcomes? Journal of Nursing Administration 30(10):457–465.
Aiken L, Clarke S, Sloane D, Sochalski J, Busse R, Clarke H, Giovannetti P, Hunt J, Rafferty A, Shamian J. 2001. Nurses’ reports on hospital care in five countries. Health Affairs 20(3):43–53.
Aiken L, Clarke S, Sloane D, Sochalski J, Silber J. 2002. Hospital nurse staffing and patient mortality, nurse burnout, and job dissatisfaction. Journal of the American Medical Association 288:1987–1993.
Bates D, Cullen D, Laird N, Petersen L, Small S, Servi D, Laffel G, Sweitzer B, Shea B, Hallisey R, Vander Vleit M, Nemeskal R, Leape L. 1995. Incidence of adverse drug events and potential adverse drug events: Implications for prevention. Journal of the American Medical Association 274:29–34.
Berens M. 2000, September 11. Training often takes a back seat; budget pressures, lack of state laws aggravate trend. Chicago Tribune. News. p. 7.
Berwick D. 2002. A user’s manual for the IOM’s “Quality Chasm” report. Health Affairs 21(3):80–90.
Blendon R, DesRoches C, Brodie M, Benson J, Rosen A, Schneider E, Altman D, Zapert K, Herrmann M, Steffenson A. 2002. Views of practicing physicians and the public on medical errors. The New England Journal of Medicine 347(24):1933–1940.
Brilli R, Spevetz A, Branson R, Campbell G, Cohen H, Dasta J, Harvey M, Kelley M, Kelley K, Rudis M, St. Andre A, Stone J, Teres D, Weled B, Peruzzi W, the members of the American College of Critical Care Medicine Task Force on Models of Critical Care Delivery, the members of the American College of Critical Care Medicine Guidelines for the Definition of an Intensivist, and the Practice of Critical Care Medicine. 2001. Critical care delivery in the intensive care unit: Defining clinical roles and the best practice model. Critical Care Medicine 29(10):2007–2019.
Cavouras C, Suby C. 2003. Perspectives on Staffing and Scheduling. 2003 Survey of Hours Report: Direct and Total Hours per Patient Day (HPPD) by Patient Care Units. Phoenix, AZ: Labor Management Institute.
Clancy C, Scully T. 2003. A call to excellence. Health Affairs 22(2):113–115.
CMS (Centers for Medicare and Medicaid Services). 2002. Report to Congress: Appropriateness of Minimum Nurse Staffing Ratios in Nursing Homes—Phase II Final Report: U.S. Department of Health and Human Services. [Online]. Available: www.cms.gov/medicaid/reports/rp1201home.asp “last modified on Wednesday, June 12, 2002” [accessed on June, 25, 2002].
Dawson D, Reid K. 1997. Fatigue, alcohol and performance impairment. Nature 388:235.
Decker D, Wheeler G, Johnson J, Parsons R. 2001. Effect of organizational change on the individual employee. The Health Care Manager 19(4):1–12.
Gelinas L, Manthey M. 1997. The impact of organizational redesign on nurse executive leadership. Journal of Nursing Administration 27(10):35–42.
Ingersoll G, Fisher M, Ross B, Soja M, Kidd N. 2001. Employee response to major organizational redesign. Applied Nursing Research 14(1):18–28.
IOM (Institute of Medicine). 2000. To Err Is Human: Building a Safer Health System. Washington, DC: National Academy Press.
IOM. 2001. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academy Press.
Kahn K, Rogers W, Rubenstein L, Sherwood M, Reinisch E, Keeler E, Draper D, Kosecoff J, Brook R. 1990. Measuring quality of care with explicit process criteria before and after implementation of the DRG-based prospective payment system. Journal of the American Medical Association 264(15):1969–1973.
Kramer M, Schmalenberg C. 1993. Learning from success: Autonomy and empowerment. Nursing Management 24(5):58–64.
Lamond N, Dawson D. 1998. Quantifying the Performance Impairment Associated With Sustained Wakefulness. South Australia: The Centre for Sleep Research, The Queen Elizabeth Hospital. [Online]. Available: http://cf.alpha.org/internet/projects/ftdt/backgr/Daw_Lam.html [accessed July 7, 2003].
Leape L, Bates D, Cullen D, Cooper J, Demonaco H, Gallivan T, Hallisey R, Ives J, Laird N, Laffel G, Nemeskal R, Petersen L, Porter K, Servi D, Shea B, Small S, Sweitzer B, Thompson B, Vander Vleit M. 1995. Systems analysis of adverse drug events. Journal of the American Medical Association 274(1):35–43.
Mitchell P, Shortell S. 1997. Adverse outcomes and variations in organization of care delivery. Medical Care 35:NS 19–32.
Needleman J, Buerhaus P, Mattke S, Stewart M, Zelevinsky K. 2002. Nurse-staffing levels and the quality of care in hospitals. The New England Journal of Medicine 346(22):1715–1722.
Pabst M, Scherubel J, Minnick A. 1996. The impact of computerized documentation on nurses’ use of time. Computers in Nursing 14(1):25–30.
Pepper G. 1995. Errors in drug administration by nurses. American Journal of Health-System Pharmacy 52:390–395.
Rubenstein L, Chang B, Keeler E, Kahn K. 1992. Measuring the quality of nursing surveillance activities for five diseases before and after implementation of the drug-based prospective payment system. In: Patient Outcomes Research: Examining the Effectiveness of Nursing Practice. Proceedings of the State of the Science Conference. Bethesda, MD: NIH, National Center for Nursing Research. Washington, DC: U.S. Government Printing Office.
Seago J. 2001. Nurse staffing, models of care delivery, and interventions. In: Shojania K, Duncan B, McDonald K, Wachter R, eds. Making Health Care Safer: A Critical Analysis of Patient Safety Practices. Evidence Report/Technology Assessment No. 43. Rockville, MD: AHRQ.
Smeltzer C, Hines P, Beebe H, Keller B. 1996. Streamlining documentation: An opportunity to reduce costs and increase nurse clinicians’ time with patients. Journal of Nursing Care Quality 10(4):66–77.
Smith J, Crawford L. 2002a. Report of Findings from the 2001 Employers Survey. NCSBN Research Brief. 3. Chicago, IL: National Council of State Boards of Nursing, Inc.
Smith J, Crawford L. 2002b. Report of Findings from the Practice and Professional Issues Survey—Spring 2001. NCSBN Research Brief. 2. Chicago, IL: National Council of State Boards of Nursing, Inc.
Sovie M, Jawad A. 2001. Hospital restructuring and its impact on outcomes. Journal of Nursing Administration 31(12):588–600.
Trossman S. 2001. The documentation dilemma: Nurses poised to address paperwork burden. The American Nurse, 33(5): 1, 9, 18.
Tucker A, Edmondson A. 2002. Managing routine exceptions: A model of nurse problem solving behavior. Advances in Health Care Management 3:87–113.
Upenieks V. 1998. Work sampling: Assessing nursing efficiency. Nursing Management 29(4): 27–29.
Urden L, Roode J. 1997. Work sampling: A decision-making tool for determining resources and work redesign. Journal of Nursing Administration 27(9):34–41.
Wagenaar A, O’Malley P, LaFond C. 2001. Lowered legal blood alcohol limits for young drivers: Effects on drinking, driving, and driving-after-drinking behaviors in 30 states. American Journal of Public Health 91(5):801–804.
Walston S, Kimberly J. 1997. Reengineering hospitals: Evidence from the field. Hospital and Health Services Administration 42(2):143–163.






















