6
Work and Workspace Design to Prevent and Mitigate Errors
The largest, best-trained, and most dedicated workforce will still make errors; its fallibility is an immutable part of human nature. However, this innate fallibility can be compounded when the practices, procedures, tools, techniques, and devices used by workers are unreliable, complex, and themselves unsafe—having been designed, selected, and maintained by other fallible humans.
The two Institute of Medicine (IOM) reports discussed earlier in this report—To Err Is Human (IOM, 2000) and Crossing the Quality Chasm (IOM, 2001)—call for better design of work processes to improve patient care and safety. To Err Is Human recommends that health care organizations (HCOs) incorporate safety principles in work design. Crossing the Quality Chasm underscores this recommendation by observing that “health care has safety and quality problems because it relies on outmoded systems of work. Poor designs set up the workforce to fail, regardless of how hard they try (IOM, 2001:4).” The report reiterates that safer health care requires redesigned health care processes.
Some nursing processes, such as medication administration, are well documented to have multiple features conducive to the commission of health care errors. The long work hours of some nurses also cause fatigue and contribute to their making errors. Inefficient care processes and workspace design, while not intrinsically dangerous to patients, decrease patient safety to the extent that they reduce the time nurses have for monitoring patients and providing therapeutic care. Documentation and paperwork requirements are well known to involve such inefficiencies.
The committee agrees that nurses’ work processes and workspace need to be designed to make them more efficient, less conducive to the commission of errors, and more amenable to detecting and remedying errors when they occur. In addition, limiting the number of hours worked per day and consecutive days of work by nursing staff, as is done in other safety-sensitive industries, is a fundamental patient safety precaution. It is also essential to foster collaboration of nursing staff with other health care personnel in identifying high-risk and inefficient work processes and workspaces and (re)designing them for patient safety and efficiency. Redesign of patient care documentation practices, however, cannot be accomplished solely by nursing staff and internal HCO efforts. Because many documentation practices are driven by external parties, such as regulators and oversight organizations, these organizations will need to assist in the redesign of those practices.
This chapter reviews the evidence on the design of nurses’ work hours, work processes, and workspaces, primarily as they relate to patient safety, but also with respect to efficiency (which, as noted above, is a contributory factor in safety). We present findings and recommendations derived from this evidence on designing these elements of the nursing environment so as to enhance safety.
DESIGN OF WORK HOURS
This section reviews the evidence related to the design of nurses’ work hours: the effect of fatigue from shift work and extended work hours on work performance, the relationship between nurse work hours and the commission of errors, and data on hours worked by both hospital and nursing home nursing personnel. The committee’s responses to this evidence in the form of conclusions and a recommendation are then presented.
Effect of Fatigue from Shift Work and Extended Work Hours on Work Performance1
Fatigue results from continuous physical or mental activity, inadequate rest, sleep loss, or nonstandard work schedules (e.g., working at night). Whatever the origin of physical or mental fatigue, it is accompanied by a subjective feeling of tiredness and a diminished capacity to do work. The effects of fatigue include slowed reaction time, diminished attention to detail, errors of omission, compromised problem solving (Van-Griever and
|
1 |
This section incorporates content from a paper on “Work Hour Regulation in Safety-Sensitive Industries” commissioned by the committee and included in this report as Appendix C. |
Meijman, 1987), reduced motivation, and decreased vigor for successful completion of required tasks (Gravenstein et al., 1990). Thus, fatigue also causes decreased productivity. Tired workers accomplish less, especially if their tasks demand accuracy (Krueger, 1994; Rosa and Colligan, 1988). In nurses’ work environments, fatigue is produced by shift work and extended work hours.
Shift Work
Since almost all physiological and behavioral functions are affected by circadian rhythms, the time of day when work must be completed is important. The human circadian rhythm strongly favors sleeping during nighttime hours. Overall capacity for physical work is reduced at night (Cabri et al., 1988; Cohen and Muehl, 1977; Rosa, 2001; Wojtczak-Jaroszowa and Banaszkiewicz, 1974). Reaction times, visual search, perceptual–motor tracking, and short-term memory are worse at night than during the day (Folkard, 1996; Monk, 1990). On-the-job performance also deteriorates. At night, railroad signal and meter reading errors increase, minor errors occur more frequently in hospitals, and switchboard operators take longer to respond to phone calls (Monk et al., 1996).
Night shift workers also have difficulty staying awake. In a survey of nurses working in seven West Coast hospitals, 19.3 percent of those working night and rotating shifts reported struggling to stay awake at least once during the previous month while taking care of patients, compared with 3.8 percent of day and evening shift nurses (Lee, 1992). In a 1986 study of nurses in one hospital, 35.3 percent of those who routinely rotated to the night shift, 32.4 percent of those who always worked nights, and 20.7 percent of day/evening shift nurses who worked occasional nights reported falling asleep during the night shift at least once a week. Nurses working night shifts or rotating shifts also made more on-the-job procedural and medication errors due to sleepiness than did nurses working other shifts. Sleepiness appeared to be confined to the night shift, as none of the shift rotators or day/evening nurses who worked occasional nights reported significant difficulties remaining alert on other shifts (Gold et al., 1992). Likewise, objective findings of sleeping on duty were reported in a study of 15 French nurses working at night. Only 4 of the 15 were able to remain awake all night while at work as measured by activity (wrist actigraphy) and sleep (polysomnographic) recordings; the remaining nurses averaged 86.5 (standard deviation ± 77.6) minutes of sleep while on duty (Delafosse et al., 2000). Difficulties in maintaining alertness at night are not confined to nurses. Self-reported and objective measures of sleep were recorded in U.S. Air Force traffic controllers on duty at night (Luna et al., 1997). And the most consistent factor influencing truck driver fatigue and alertness over a
16-week study of 80 commercial truck drivers was time of day. Episodes of drowsiness at the wheel were observed in the majority of drivers. Drowsiness was markedly greater during nighttime than daytime driving (Wylie et al., 1996).
Coping with nonstandard work hours (nights or rotating shifts) is easier for someone fully rested. A person who is not sleep deprived performs tasks more efficiently after prolonged wakefulness (Dinges et al., 1996). However, individuals working nights and rotating shifts rarely obtain optimal amounts of quality sleep. Their sleep is shorter, lighter, more fragmented, and less restorative than sleep at night (Knauth et al., 1980; Lavie et al., 1989; Walsh et al., 1981).
A number of interventions have been proposed to mitigate the effect of shift work. Clockwise shift rotations—day shift, progressing to evening, then night shifts—appear to be tolerated more easily than the reverse. Scheduled, on-the-job naps and use of bright lighting also have been found to combat fatigue to some extent. However, the way in which they are best implemented has not been established. The speed of shift rotation, how to counteract the sleep inertia that commonly accompanies the taking of naps, and how to provide bright lighting for nurses while maintaining optimal darkness for patients are some of the issues not yet resolved. Consequently, experts on fatigue have recommended modifying work tasks and processes to reduce the risk for error and creating mechanisms to detect errors at the time they are committed to reduce their adverse effects (Office of Technology Assessment, 1991; Jha et al., 2001).
Extended Work Hours
Shifts of 12 or more hours with limited opportunity for rest and no opportunity for sleep are referred to as “sustained operations” (Kruger, 1989). Workers engaged in sustained operations in a variety of occupations report greater fatigue at the end of their shifts than do those who work 8-hour shifts (Mills et al., 1983; Rosa, 1995; Ugrovics and Wright, 1990).2
Studies in a variety of industries also show that accident rates increase during overtime hours (Kogi, 1991; Schuster, 1985); rates rise after 9 consecutive hours, double after 12 hours (Hanecke et al., 1998), and triple after 16 hours (Akerstedt, 1994). Data from aircraft accident investigations
conducted by the National Transportation Safety Board also show higher rates of error after 12 hours (National Transportation Safety Board, 1994). Finally, night shifts longer than 12 hours and day shifts longer than 16 hours have consistently been found to be associated with reduced productivity and more accidents (Rosa, 1995).
Laboratory studies have shown that moderate levels of prolonged wakefulness can produce performance impairments equal to or greater than those due to levels of intoxication deemed unacceptable for driving, working, and/or operating dangerous equipment. Prolonged periods of wakefulness (e.g., 17 hours without sleep) can produce performance decrements equivalent to a blood alcohol concentration (BAC) of 0.05 percent, the level defined as alcohol intoxication in many western industrialized countries.3 After 24 hours of sustained wakefulness, cognitive psychomotor performance decreases to a level equivalent to a BAC of 0.10 percent (Dawson and Reid, 1997; Lamond and Dawson, 1998). Performance on neurobehavioral tests decreases linearly after 17 hours of wakefulness, with the poorest performance occurring after 25–27 hours. Performance on the most complex task—grammatical reasoning—was found to be impaired several hours earlier than performance on vigilance accuracy and response latency (20.3 hours versus 22.3 and 24.9 hours, respectively) (Lamond and Dawson, 1998). Prolonged wakefulness also significantly impairs speed and accuracy, hand–eye coordination, decision making, and memory (Babkoff et al., 1988; Florica et al., 1968; Gillberg et al., 1994; Linde and Bergstrom, 1992; Mullaney et al., 1983). A nurse who worked on average one mandatory double shift (16 hours) every 2 weeks for a 2-month period reported, “By 4 a.m., I was so exhausted that I would stop between going from one baby to the next and completely forget why I was going to the other bedside. Another time, again about 4 a.m., I would sometimes stop in the middle of the floor and forget what I was doing” (California Nurses Association, 2003).
Fatigue is also exacerbated by working increased numbers of shifts without a day off (Dirks, 1993; Knauth, 1993) and by having only short durations between work shifts. Working more than four consecutive 12-hour shifts is associated with excessive fatigue and longer recovery times (Wallace and Greenwood, 1995). Very short off-duty periods—8 hours or less—do not provide enough time for commuting, recovery sleep, or time to take care of domestic responsibilities (Dinges et al., 1996; Rosa, 1995, 2001). Most adults require at least 6–8 hours of sleep to function adequately at work (Krueger, 1994). The loss of even 2 hours of sleep affects waking
performance and alertness the next day (Dinges et al., 1996). After 5 to 10 days of shortened sleep periods, the sleep debt (sleep loss) is significant enough to impair decision making, initiative, information integration, planning, and plan execution (Krueger, 1994). The effects of sleep loss are insidious and usually not recognized by the sleep-deprived individual until they have become severe (Dinges et al., 1996; Rosenkind et al., 1999). Schedules that require workers to return to work after an 8-hour rest period or to transition from night to day or evening shifts without at least 24 hours off are considered particularly dangerous (Olson and Ambrogetti, 1998; Rosa and Colligan, 1988).
Recovery from extended work periods requires more than 1 day. Off-duty intervals ranging from 10 to 16 hours are either suggested or already mandated for many transportation workers (Dinges et al., 1996; Gander et al., 1991; Mitler et al., 1997). Two consecutive nights of recovery sleep can return performance and alertness to normal levels, even following two or three 12-hour shifts (Dinges et al., 1996; Tucker et al., 1996); longer intervals between works days are even more beneficial. Workers obtain more sleep and start their next shift with less fatigue. The first or second night on a new series of night shifts, however, may be the most fatiguing because of circadian desynchrony (Rosa, 2001).
The combination of sustained wakefulness and working at night is particularly hazardous (Gold et al., 1992; Smith et al., 1994). When the Exxon Valdez ran aground around midnight on March 23, 1989, the third mate had been awake 18 hours and anticipated working several more hours (Alaska Oil Spill Commission, 1990). Although the explosion of the Challenger space shuttle occurred during the daytime, the decisions made the night before the launch by mission control staff have been cited as a major factor contributing to the explosion (Mitler et al., 1988). In a small study of the use of extended (16-hour) night shifts in seven wards of a Japanese university hospital, several compensatory measures were employed to protect against the dual effects of sustained operations and night shift work. These measures included increases in the numbers of night staff to allow all nursing staff to take a 2-hour nap in a dedicated resting room. Staff was also allowed to take at least one recovery day off after a 16-hour shift. The increase in staff, 2-hour nap, and day off were believed to contribute to the extended shift nurses’ less frequent complaints of fatigue and general decreased physical activity as compared with nurses working 8-hour shifts (Fukuda et al., 1999). The study also found that sleep inertia (characterized by sleepiness, fatigue, and dullness) increased immediately after the nap, but then decreased to the same levels as existed before the nap. The researchers concluded that nap length would need to be carefully regulated to avoid persistent sleep inertia and its attendant risks (Takahashi et al., 1999).
A review of evidence on the effects of worker fatigue on patient safety is included in the Agency for Healthcare Research and Quality’s (AHRQ) report Making Health Care Safer: A Critical Analysis of Patient Safety Practice (Jha et al. 2001). Consistent with the above evidence, the report notes that sleep deprivation leads to decreased alertness and poor performance on standardized testing, and that shift workers in particular experience disturbances in their circadian rhythms and tend to perform less well on reasoning and nonstimulating tasks.
Evidence on Nurse Work Hours and the Commission of Errors
Researchers conducting the evidence review presented in the AHRQ report cited above (Jha et al., 2001) were unable to locate research that could help identify the specific numbers of hours worked by health care personnel, including nurses, beyond which patient safety is threatened. These researchers noted inconsistent research findings with respect to ideal shift length for enhanced worker performance. The report suggests that while multiple studies have sought to document the impact of fatigue on the performance of medical personnel, these studies have been limited by poor design or outcomes that did not correlate well with medical error.
This situation has been improved by a 2002 study funded as part of AHRQ’s initiative to examine the effects of working conditions on patient safety. This study documented the work patterns of a sample of hospital staff nurses randomly selected from the membership of the American Nurses Association (ANA). The sample frame consisted of full-time hospital staff nurses (unit based, not working through a temporary agency) with no administrative or educational responsibilities. The study measured the effects of nurse work hours on patient safety by (1) documenting the total scheduled and unscheduled hours worked by nurses; (2) describing the nature of nurses’ overtime work hours in terms of what proportion of hours worked were overtime hours, how often nurses worked overtime, and whether overtime was voluntary or mandatory; and (3) determining whether there was an association between errors and near-errors and the numbers and types of hours worked by the nurses.
Study participants recorded information about their scheduled work hours, actual work hours, errors, and near-errors daily in a diary for 28 days. Nurses were also asked to describe all errors and near-errors. The researchers then categorized each error or near-error by type (e.g., medication administration, procedural, transcription) based on the nurse’s description. Error rates per hour were calculated according to the number of errors and hours worked, adjusting for multiple work shifts for the same nurse. The associations between error rates and both overtime and scheduled work
shift duration (in hours) were estimated using regression models. The p-values for the adjusted incidence rate ratios were constructed based on robust variance estimates, with α = 0.05. Near-errors were examined using the same procedures.
For all study nurses, the overall error rate was 0.00336 errors per hour worked. Working overtime—working longer than scheduled on a given day or working extra shifts (“scheduled overtime”)—had no effect on error rates unless shift durations exceeded 12 consecutive hours. Once shift durations exceed 12 consecutive hours, both voluntary and mandated overtime significantly increased error rates (0.00375/hour and 0.00490/hour, respectively) (p = 0.02 for voluntary overtime and 0.03 for mandated overtime). Results remained consistent when outliers (i.e., 54 extremely long shifts of more than 23 hours, nurses with more than 7 errors each) were removed from the analyses. Results were somewhat different for near-errors. Being mandated to work overtime was associated with significant increases in the rate of near-errors for shifts scheduled for 12 hours or more; however, the rate of near-errors associated with working voluntary overtime for periods exceeding 12 consecutive hours was not increased.4
Data on Nurse Work Hours
Nursing staff working in in-patient facilities have traditionally worked in 8-hour shifts, but increasingly work longer hours. Reasons for these increases include the desire for increased compensation (elective overtime), requirements by health care organizations to work overtime (mandatory overtime) to compensate for insufficient staffing, and the desire for more flexible work hours (e.g., 10- or 12-hour shifts) to accommodate either facility or individual nurse needs or both. Scheduled shifts may be 8, 10, or 12 hours and may not follow the traditional pattern of day, evening, or night shifts. Nurses working on specialized units, such as the operating room, dialysis units, and some intensive care units, may be required to be on call in addition to their regularly scheduled shifts (Rogers, 2002).
Representative, quantitative data describing the work hours of nurses are scarce. Evidence of the long hours worked by direct-care nurses working in hospitals and nursing homes was obtained from a random sample survey of nurses licensed to work in either Illinois or North Carolina5 as part of a longitudinal study of nurses’ worklife and health funded by the
National Institute for Occupational Safety and Health (NIOSH) of the U.S. Centers for Disease Control and Prevention (CDC). Of the 674 registered nurse (RN) respondents to this 2002–2003 survey who were employed as a full-time hospital or nursing home general-duty/staff nurse, 27.2 percent reported working more than 13 hours at a stretch one or more times a week, and an additional 18.9 percent reported doing so once a month or every other a week. Only 19.5 percent reporting never doing so, while 34.4 percent reported doing so only a few times per year.6 Extended work hours also are indicated by their frequently being cited by nurses as a key area of job dissatisfaction (U.S. General Accounting Office [GAO], 2001); by the extent to which nursing organizations have sought legislative, regulatory, and contractual relief from this practice; and by the few studies of hours worked by nursing staff in hospitals and nursing homes.
Work Hours of Hospital Nurses
Data collected from the 2000 National Sample Survey of Registered Nurses indicate that full-time hospital nurses (including direct-care, administrative, and other hospital nurses) worked on average 42.2 hours per week, in contrast to their average scheduled hours of 39.3 hours per week (Spratley et al., 2000). In 2001, 17 percent of a national representative sample of newly licensed RNs surveyed by the National Council of State Boards of Nursing in its twice yearly survey of entry-level nurses reported working (in all settings of care, full- and part-time) an average of 36.5 nonovertime hours per week and an average of 4.6 hours of overtime per week. Likewise, 17 percent of these newly licensed RNs reported working mandatory overtime (Smith and Crawford, 2002).
As the discussion of staffing levels in Chapter 5 indicates, however, averages do not tell the full story. The AHRQ-funded study of the work hours of a sample of members of the ANA documented the variation in the work patterns of full-time, direct-care hospital staff nurses in terms of hours worked, duration of shifts, and amount of overtime hours worked. The study found that although the majority (84.3 percent) of scheduled shifts were 8 or 12 hours in duration, 3.5 percent were for periods greater than 12 hours. Scheduled shift durations ranged from 2 to 22.5 hours (see Figure 6-1).
Furthermore, a comparison of scheduled and actual work times revealed that all nurses had started work earlier than scheduled, stayed later than scheduled, or both at least once during the 28-day period. Nurses reported working on average 13.4 days (range 1–24) during this 28-day data-gather-
ing period, and working beyond their scheduled shift times on average 10.9 days (range 1–24). Nurses started work early, left later than scheduled, or both on 81.4 percent of shifts. As a result, actual (as opposed to scheduled) work shift durations ranged from 1 hour, 15 minutes (an obstetrical nurse who was sent home because of a low census) to 23 hours, 57 minutes (see Figure 6-1). Almost half of the shifts worked (43 percent) exceeded 12 hours (1074 shifts), and one-quarter exceeded 12 hours, 50 minutes. There were 51 double (16-hour) shifts reported, 51 shifts in which participants worked more than 16 but less than 20 hours, and 103 shifts that exceeded 20 consecutive hours. A comparison of actual and scheduled work times revealed that participants worked on average 1 hour, 9 minutes extra per scheduled shift (range 18 minutes–19 hours, 30 minutes).
Work Hours of Nursing Staff in Nursing Homes
Research on the work hours of nursing staff in nursing homes also has revealed extended work hours. In site visits to 17 nursing homes in Ohio, Colorado, and Texas in 2001, researchers found that double shifts (i.e., two
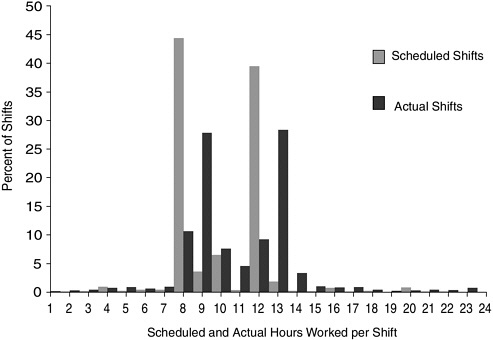
FIGURE 6-1 Scheduled and actual shift durations.
SOURCE: Ann Rogers, Ph.D., University of Pennsylvania (personal communication on July 4, 2003).
consecutive 8-hour shifts totaling 16 hours) and extra shifts were performed in many of these facilities on a regular basis. Double shifts in particular were pervasive. In 13 of the 17 nursing homes, at least one nursing staff member, but frequently more, had worked between one and three double shifts in the previous 7 days. In five nursing homes, at least one staff member had worked between four and seven double shifts in the last 7 days. In one of the facilities, more than a third of the interviewed nursing staff had worked between eight and eleven double shifts in the last 14 days. All direct-care nursing staff (RNs, licensed practical nurses [LPNs]/licensed vocational nurses [LVNs], and nursing assistants [NAs]) were engaged in these work practices; however, double shifts were performed most often by NAs (Centers for Medicare and Medicaid Services [CMS], 2002).
Responses to the Evidence
The committee finds the evidence that prolonged work hours and fatigue affect worker performance to be very strong. We also note that there is no evidence to suggest that any amount of training, motivation, or professionalism is able to overcome the performance deficits associated with fatigue, sleep loss, and the sleepiness associated with circadian variations in alertness (Battelle Memorial Institute, 1998; Dinges et al., 1996; Jha et al. 2001; McCartt et al., 2000). The recent AHRQ-funded study of nurse work hours and health care errors discussed above provides additional compelling evidence of the effect of nurses working long hours on patient safety.
The committee reviewed evidence on how other safety-sensitive industries—nuclear energy production, public and commercial transportation, the military, police, and firefighters—have responded to such evidence. All have placed some restrictions on the work hours of personnel (see Appendix C). The health care industry is notable in that, with few exceptions, it places no such limits on work hours. However, a number of organizations are beginning to respond to the evidence. As of 2002, eight states had enacted legislation or regulations prohibiting facilities from requiring nurses to work certain extended hours (ANA, 2002). Legislation also has been introduced federally and within additional states to ban mandatory overtime for nurses. The Safe Nursing and Patient Care Act of 2003 (HR 745 and SB 373), introduced in the 108th U.S. Congress, would, in part, prohibit mandatory overtime for nurses and other licensed health care providers. As part of the ANA’s nationwide state legislative agenda, other state nurses’ associations are pressing for prohibitions on mandatory overtime in state statutes and regulations. No proposals address how long nurses may work on a voluntary basis.
Jha et al (2001:530) note that “in most high-hazard industries the assumption is that fatigue and long, aberrant work hours leads to poor
performance, and the burden of proof is in the hands of those who believe that such work practices are safe.” They recommend that, “given that medical personnel, like all human beings, probably function suboptimally when fatigued, efforts to reduce fatigue and sleepiness should be undertaken, and the burden of proof should be in the hands of the advocates of the current system to demonstrate that it is safe.” Based on the evidence presented above, the committee concurs and makes the following recommendation:
Recommendation 6-1. To reduce error-producing fatigue, state regulatory bodies should prohibit nursing staff from providing patient care in any combination of scheduled shifts, mandatory overtime, or voluntary overtime in excess of 12 hours in any given 24-hour period and in excess of 60 hours per 7-day period. To this end:
-
HCOs and labor organizations representing nursing staff should establish policies and practices designed to prevent nurses who provide direct patient care from working longer than 12 hours in a 24-hour period and in excess of 60 hours per 7-day period.
-
Schools of nursing, state boards of nursing, and HCOs should educate nurses about the threats to patient safety caused by fatigue.
The committee calls attention to several parts of this recommendation. First, the recommendation calls for limiting the number of hours nurses spend in providing direct patient care. If for example, a nurse completes a 12-hour shift and needs to stay beyond this period to document care or attend a training or education activity, this time would not be included in the 12-hour limit. Rather, the recommendation is intended to limit the amount of time that fatigued nurses will have responsibility for direct patient care. We include clinical supervision in this definition of direct care because such supervision also requires the exercise of clinical judgment and often involvement in clinical care, both of which would be adversely affected by fatigue.
Second, the committee does not distinguish in this recommendation between voluntary and mandatory overtime. We note that personal strength of will and the exercise of free will are not effective countermeasures to the effects of sleep loss and fatigue. Consequently, while the committee believes HCOs might want to limit their use of mandatory overtime in the interest of nurse retention and recruitment, excessive hours endanger patient safety regardless of whether they are worked under a mandate or on a voluntary basis. The committee consequently recommends that working more than 12 hours in any 24-hour period and more than 60 hours in any 7-day pe-
riod be prevented except in case of an emergency, such as a natural disaster. In the event that nurses are required to work excessive hours because of an emergency, this information should be immediately disclosed to the public so that elective admissions can be postponed and other admissions diverted to different units or facilities. Similarly, in any instance where a nursing shortage prevents an HCO from securing sufficient nurses to prevent work hours in excess of 12 hours in any 24-hour period and more than 60 hours in any 7-day period, this information also should be disclosed to the public, so that elective admissions can be referred to other facilities or delayed until staffing is remedied. If an admission cannot be delayed or referred to another HCO, the patient and their family should be informed about the shortage of staffing and that nursing staff is working under conditions adverse to patient safety. Family members may want to attend to a patient for longer periods of his or her inpatient stay, when nursing staff is working longer work hours and there is a shortage of nursing staff.
Finally, by recommending a regulatory role in encouraging safe work hours, the committee does not intend to encourage the creation of burdensome oversight mechanisms that, for example, would require the submission or inspection of individual nurse time sheets. Rather, the committee encourages HCOs, state boards of nursing, and schools of nursing to educate nurses and themselves about the dangers of fatigue. We also recommend that HCOs, working with their labor partners, develop staffing and work-hour policies designed to prevent fatigue caused by excessive work hours. Such policies and procedures might include, for example:
-
Acknowledging the responsibility of nurses who work in more than one facility to ensure that their total patient care hours worked do not exceed the patient safety thresholds identified in the above recommendation.
-
Ensuring that any use of mandatory overtime by the facility will not require nurses to provide more than 12 hours of patient care in any 24-hour period or more than 60 hours of patient care in any 7-day period.
-
In health care organizations that allow nursing staff to self-schedule, preventing nursing staff from scheduling more than 12 hours of patient care in any 24-hour period or more than 60 hours of patient care in any 7-day period.
The committee anticipates these policies being facilitated by the authority of regulations promulgated by state boards of nursing, which license nurses and regulate the practice of nursing, and by other state agencies that have authority over the work of nurses and unlicensed NAs.
DESIGN OF WORK PROCESSES AND WORKSPACES
This section reviews the evidence on the design of work processes and workspaces, including the inherent risks to patient safety involved in certain nursing work processes, reduced patient safety due to inefficient nursing work processes, and the effect of the physical design of workspaces on both safety and efficiency. The final section examines how work processes and workspaces can be designed to enhance the safety and efficiency of the direct care provided by nursing staff to patients.
Inherent Risks to Patient Safety in Some Nursing Work Processes
Flaws in work or equipment design, equipment failures, and unanticipated interactions in work processes are recognized threats to safety in a many industries, including health care (Hyman, 1994; Senders, 1994). Medication administration and handwashing are two common nursing activities well documented as involving threats to patient safety.
Medication Administration
Medication administration is a high-frequency activity performed by nurses in every setting of care. It also is associated with great risks to patients. More than 770,000 people annually are estimated to suffer injury or death in hospitals as a result of adverse drug events (ADEs) (Kaushal and Bates, 2001). One study of preventable ADEs in hospitals found that 34 percent of such events occurred in connection with administering the drug (a nursing role), as opposed to ordering, transcribing, or dispensing of the drug (Bates et al., 1995). A 6-month study of all ADEs in two tertiary care hospitals found that 38 percent had resulted from administration by nursing staff (Pepper, 1995). The administration of medications is a complex process involving selecting the correct drug, dose, route, patient, and time, while also remaining alert to prescribing or dispensing errors. Consequently, errors in medication administration are enabled and caused by many factors.
Causes of medication administration errors The increasing numbers of new drugs available for administration are frequently cited as a factor in medication errors (O’Shea, 1999). With increased numbers of drugs for administration comes a concomitant increase in nurses’ responsibilities for knowledge of drug action, side effects, and correct dosage. Yet studies have documented that lack of knowledge about medications is a persistent problem—and a cause of ADEs. A systems analysis of ADEs occurring in 11 medical and surgical units in two tertiary care hospitals over a 6-month period found that lack of knowledge about the drug was the most common
cause of ADEs among both physicians and nurses. At the level of physician ordering, lack of awareness of drug interactions and correct dosing was the most frequent problem; at the nurse level, during administration of medications, overdosing of anti-emetics, mixing drugs in incompatible solutions, and overly rapid infusion of intravenous drugs were the most common errors (Leape et al., 1995).
Mathematical proficiency is a prerequisite for accurately performing many aspects of medication administration, such as intravenous regulation (Ashby, 1997; Calliari, 1995). Nurses’ poor mathematical and drug calculation skills have been linked to medication errors (Bindler and Bayne, 1991; O’Shea, 1999). Yet experts in human factors and ergonomics estimate that humans will normally (under conditions that do not involve any time pressures or stresses) make simple arithmetic errors at a rate of 3 per 100 calculations (Park, 1997). When nurses must calculate drug dosages under conditions of stress or time constraints, it is likely that this error rate will be higher.
Other causes of ADEs include stresses in the environment, including interruptions, fatigue, and overwork; miscommunication, including illegibility of written drug orders; lack of information about the patient; and problems with infusion pumps and IV delivery (Pape, 2001).
Potential remedies A number of strategies have been proposed to address the above problems, including ongoing in-service education, use of reference material as decision support, and medication administration assistance devices. The Institute for Safe Medication Practices and AHRQ have identified three medication administration technologies (in addition to computerized prescriber order entry at the point of prescribing) as important strategies for reducing medication errors at the point of medication administration by nurses: unit dose dispensing, bar-coding of medications, and use of “smart” infusion pumps.7
-
Unit dose dispensing—Murray and Shojania (2001) review the evidence associated with “unit dose dispensing”—the practice of having hospital pharmacies dispense medications to nursing stations in individually packaged doses ready to be given to the patient. Unit dose dispensing is common on general medical and surgical hospital units, but less so in intensive care units, operating rooms, and emergency departments. In the latter areas, bulk medication stock systems are still found. In a 1999 survey of hospital pharmacy directors, 80 percent reported that unit dose dispensing was used for 75 percent or more of oral doses and 52 percent of medications for injection. Murray and Shojania (2001:104-105) conclude that although the evidence for the effectiveness of unit dose dispensing is “modest,” studies evaluating the practice are “overall relatively consistent in showing a positive impact on error reduction.” The Institute for Safe Medication Practices notes, however, that the unavailability of unit dose packaging by manufacturers is becoming more widespread (Young, 2002). Information on the use of unit dose dispensing in nursing homes was not found.
-
Bar code medication administration—The Veterans Administration (VA) health system has used a bar code medication administration (BCMA) assistance device in almost all of its medical centers since 1999. This device, consisting of a wireless laptop computer atop a medication cart and a bar code reader, enables nurses to administer and document medications online at the point of administration. The nurse logs on to the BCMA computer, scans the patient’s ID bracelet, and brings the patient’s medication record up on the screen. The nurse then scans the medication bar code (placed there by the pharmacy) and verifies the patient’s identity and medications against active orders. If there are any issues, an alert appears. If not, the nurse administers the medication and documents this on the computer. A comparison of errors committed in 1993 (the last full year of completely manual drug administration) and those committed in 2001 at the VA medical center initiating the project revealed a 86 percent reduction in the overall medication error rate (Johnson et al., 2002). Despite similar findings at other VA facilities and endorsement by the Institute for Safe Medication Practices, a survey conducted by the American Society of Health Systems Pharmacists in 1999 found that only 1.1 percent of U.S. hospitals used bar code technology to scan a patient’s ID wristband, nurse’s badge, and prescribed drug at the bedside (Young, 2002). To encourage more widespread use of this practice, the U.S. Food and Drug Administration (FDA) proposed a new regulation on March 14, 2003, that would require human drug and blood products to be bar-coded. “The proposed rule would not require hospitals to introduce the new automated technologies, but the development of consistent bar codes on pharmaceutical and blood products would greatly encourage hospitals
-
to implement bar code based systems to reduce ADEs associated with medication errors.”8
-
Smart infusion pumps—Smart infusion pumps allow hospitals to enter various drug infusion protocols into a drug library with predefined limits. If a dose is programmed outside of established limits or clinical parameters, the pump halts or emits an alarm. Some pumps have the capability of integrating patient monitoring and other patient parameters, such as age or clinical condition. Clinical trials will soon be under way to assess the performance of these devices in reducing medication error rates (Institute for Safe Medication Practices, 2002).
In addition to the above remedies, low-tech strategies, such as decreasing interruptions and distractions, providing standardized protocols, and using checklists for drug administration, have been developed and used in efforts to reduce drug errors (Pape, 2003). Ensuring safe staffing levels (see Chapter 5) and preventing nurse fatigue as described earlier in this chapter can also reasonably be expected to help protect against medication administration errors. Effective redesign of medication administration also depends on the creation of a culture of safety and the establishment of a fair and just error-reporting system that is conducive to the discovery of medication errors (as discussed in Chapter 7).
Handwashing
Absence of handwashing is an example of a health care error of omission—an error that results from the failure to take an action, as opposed to an error of commission accompanying the performance of an action. Errors of omission are usually more difficult to detect than those of commission. However, the prevalence of the absence of handwashing is indicated by the tremendous morbidity, mortality, and health care costs resulting from hospital-acquired infections—found in 7–10 percent of hospitalized patients and causing approximately 80,000 deaths per year (Lautenbach, 2001). Infections are also are the major cause of transfer of nursing home residents to hospitals (CMS, 2002). It is also well established that (1) most hospital-acquired pathogens are transmitted from patient to patient via the hands of health care workers, and (2) handwashing is the simplest and most effective, proven method for reducing the incidence of nosocomial infections. Nevertheless, Lautenbach (2001) presents an array of evidence that handwashing by all health care workers is performed at very low rates. In the 11 studies reviewed, rates of handwashing ranged from 16 to 81 percent; only two studies noted compliance levels above 50 percent.
A number of causes have been identified for low rates of handwashing, some of which are a product of the work environment. Studies indicate that workers with the highest workload are the least likely to wash their hands; lack of time is one of the most commonly cited reasons for failure to wash hands. In a survey of health care workers, 75 percent stated that rewards or punishments would not increase handwashing, but 80 percent said that easy access to sinks and handwashing facilities would. Studies also have indicated that rubbing hands with a small amount of fast-acting antiseptic is more effective and takes less time than traditional soap-and-water handwashing. A recent study comparing alcohol hand rubs with soap-and-water handwashing found that hygienic hand rubs could reduce handwashing time by more than 75 percent Lautenbach (2001). A national stakeholders meeting convened in July 2003 by the U.S. Centers for Disease Control and Prevention (CDC) and the American Hospital Association (AHA) reaffirmed that alcohol-based hand rubs are more effective in reducing bacteria on workers’ hands, save workers’ time, and are associated with improved adherence to guidelines on handwashing. This stakeholder meeting was convened to identify ways that hospitals can fully use alcohol-based hand rubs and not jeopardize fire safety (CDC, 2003). Some also have suggested that the application of behavior theory and human factors approaches to infection control practices might help achieve sustained increases in handwashing rates (Lautenbach, 2001).
Reduced Patient Safety Due to Inefficient Nurse Work Processes
A number of studies provide evidence that nurses spend a significant portion of their time in activities that are inefficient and decrease the amount of time they have available to monitor patient status, provide therapeutic patient care, and educate patients. In a survey of 50 percent of RNs living in Pennsylvania, 34.3 percent of hospital nurses reported performing housekeeping duties, 42.5 percent delivering and retrieving food trays, and 45.7 percent transporting patients. Of these same nurses, 27.9 percent and 12.7 percent, respectively, reported leaving undone patient/family education and patient/family preparation for discharge (Aiken et al., 2001). When delivery of medications, medical equipment or supplies, blood products, or laboratory specimens is needed for the patient and transport staff are not available, this activity often is carried out by the nurse. Such practices occur frequently (Prescott et al., 1991; Upenieks, 1998). In separate studies comparing the efficiency of two different nurse call systems, 50 to 80 percent of calls were found not to require a response from a licensed nurse (Miller et al., 1997, 2001).
More recently, in a work sampling study involving 239 hours of observation of 26 hospital nurses at nine hospitals with a reputation among
industry experts for providing “excellent nursing care,” failures in the design or execution of hospital work processes were found to be so common that they were considered virtually routine. The nurses shadowed faced an average of one work design problem per hour in five broad categories of work problems: missing or incorrect information, missing or broken equipment, waiting for a (human or equipment) resource, missing or incorrect supplies, and simultaneous demands on their time. Of the problems observed, 39 percent caused, on average, a 90-minute delay in patient care, including delays in medication, treatment, food, transfer and discharge, laboratory results, and surgery. Numerous patients experienced long waits for transfer and had to have laboratory samples redrawn because earlier samples had been processed incorrectly. Researchers found that on average, 33 minutes was lost per 8-hour shift as a result of coping with work system failures (Tucker and Edmondson, 2002, 2003).
As discussed in earlier chapters, there is strong evidence that documenting patient care and large quantities of paperwork also consume very large amounts of nurses’ time.
Documentation and Paperwork
Nurses spend much time documenting patient care activities. Documenting patient care and completing other paperwork to meet facility, insurance, private accreditation, state, and federal requirements, as well as to furnish information needed by other providers, is uniformly cited as imposing a heavy demand on nurses’ time in hospitals, nursing homes, home health agencies, and community and public health settings. Estimates from work sampling studies and surveys of nurses within individual hospitals of the amount of time spent in patient care documentation range from 13 to 28 percent (Pabst et al., 1996; Smeltzer et al., 1996; Upenieks, 1998; Urden and Roode, 1997), although this proportion has also been shown to differ across shifts (Korst et al., 2003; Scharf, 1997). In a study in which the average time nurses spent in documentation was found to be 15.8 percent, day shift nurses spent 19.7 percent, while night shift nurses spent 12.4 percent (Korst et al., 2003). Completion of all required paperwork is cited as one reason nurses work overtime (see Chapter 5). As discussed earlier, because it cannot be accomplished in an 8-hour shift, it becomes a sort of “unofficial” mandatory overtime (Trossman, 2001).
Home care nurses are estimated to spend a much greater proportion of their time in documenting care. Although no work sampling studies of time spent in documentation among home health nurses were located, some have estimated that these nurses spend twice as much time in documenting patient care as do hospital nurses, in part because of more prescriptive federal
regulatory requirements for documentation in home health care than in hospital care (Trossman, 2001).
In addition to being time-consuming, required documentation is often redundant and irrelevant. Documentation redesign initiatives undertaken internally by hospitals have found an excess number of forms and duplication of patient information, such as vital statistics and allergies, in multiple locations throughout patients’ charts (Brunt et al., 1999). Moreover, in some HCOs, both nurses and other health professionals state that they rarely read nurses’ notes (Brooks, 1998; Brunt et al., 1999).
Multiple sources of demands for documentation and paperwork. The types of required documentation performed by nurses vary. Some may be characterized as “administrative,” that is, not treatment-specific (e.g., documentation of advance directives, permission for release of information, informing patients of their rights). Other documentation pertains to nursing care and typically includes patient care plans; progress notes, flow charts, and shift-to-shift documentation or reports; medication administration and treatment records; patient education; admission, discharge, and transfer notes; justification for use of restraints; and patient classification systems (Butler and Bender, 1999; Smeltzer et al., 1996). Nurses in particular settings must also complete setting-specific documentation. For example, home health care nurses utilize CMS’ Outcome and Assessment Information Set (OASIS)—a dataset sometimes more than 50 items long that is used in patient assessment. Nursing home nurses must complete CMS’ Minimum Data Set (MDS). Finally, nurses sometimes practice lengthy narrative charting as a defense against potential litigation and as a way to document professional practice. “If it isn’t charted, it didn’t happen,” is a well known nursing maxim (Trossman, 2001).
Internal and external solutions are needed. Because documentation demands arise from sources both internal and external to the HCO, strategies for reducing the documentation burden have been undertaken by both HCOs and external parties. Some HCOs have successfully employed work redesign and automation to reduce documentation demands.
With regard to work redesign, HCOs have reduced the amount of time nurses spend in documentation activities by eliminating documentation of the same information in multiple locations by multiple clinicians (Brunt et al., 1999; Zerwekh et al., 2000) and by using graphs, flow charts, and clinical algorithms or pathways to minimize the need for more time-consuming narrative notes (Bridgeman et al., 1997; Brunt et al., 1999). Efficient documentation practices also have been achieved by using “exception-based charting,” which focuses attention on abnormal or significant findings
rather than on documentation of normal findings (Blachly and Young, 1998; Murphy et al., 1988). Exception-based charting does not ignore normal findings; rather, it allows a notation (e.g., a check mark or caregiver initials) that care was provided in accordance with certain hospital-adopted standards of care, such as those found in clinical pathways. Narrative or more detailed notes are written when care and responses deviate from the expected:
For example, nurses formerly were asked to file an IV site check … every hour to “prove” that hourly checks were performed. Such documentation was mechanistic and was often entered all at once at the end of the shift. It did nothing to improve quality of care and provided no advantage. The new [charting by exception] approach allows the nurse to chart once, verifying the IV site was checked hourly … (LaDuke, 2001:285).
Exception-based charting is used more often in acute care settings than in long-term care (Blachly and Young, 1998). In both settings, it is associated with reducing the amount of time nurses spend in documenting care (Blachly and Young, 1998; Stephens and Mason, 1999; Wroblewski and Werrbach, 1999).
Some of the most effective strategies for achieving more-efficient documentation result from multidisciplinary documentation redesign initiatives (Brunt et al., 1999; Mosher et al., 1996; Smeltzer et al., 1996). For example, an interdisciplinary documentation work redesign and performance improvement initiative undertaken by Summa Health System in Akron, Ohio, found at baseline an excess number of forms, duplication of information throughout patient charts, poor use of data and information across disciplines, and large amounts of nursing time dedicated to patient care documentation. After a broad-based interdisciplinary initiative examining the processes and information flow needed to support interdisciplinary practice, Summa reengineered its patient care documentation processes.
Among the positive results of this initiative were the elimination of 80 forms; a decrease in multiple data entry (e.g., allergies were documented in 15 places prior to the redesign and in 2 places following the redesign; diagnoses were listed in 16 versus 4 places); and a decrease in the amount of time nurses spent in documentation from baseline survey reports of 25–40 percent to postimplementation survey reports of 10–20 percent. All these results were achieved by redesigning manual documentation processes; automated documentation was defined as a future goal (Brunt et al., 1999).
With regard to the use of automation, evidence exists that automated computer-based data entry, if carefully designed, can reduce the time required for documentation (Pabst et al., 1996), improve the quality of documentation (Nahm and Poston, 2000), or both. Some organizations have achieved cost savings as well (Baldwin, 1998; Weiss and Hailstone, 1993;
White and Hemby, 1997), sometimes through decreased use of overtime (Allan and Englebright, 2000; Smith et al., 1998). However, automation alone—without efficient underlying documentation processes and careful design of applications—will not always achieve these results (Allan and Englebright, 2000; Larrabee et al., 2001), as one hospital’s efforts illustrate:
Nurses complained about the length of time it now took them to document. They felt they were charting information that no one was reviewing or that was clinically irrelevant. Many of their complaints focused on the way the software worked, as opposed to the way it had been individualized by the facility. Frustration with … the number of screens that had to be traversed to enter the simplest data were often voiced. To reduce aggravation and documentation time, many nurses completely bypassed the structure provided by the care plan and wrote an electronic narrative note. Thus was lost much of the benefit of putting documentation online: clinical information systems do not have the sophistication to analyze a narrative note in a meaningful way.
Physicians were unhappy with the new nursing documentation … the medical staff simply could not find the information they wanted….
Medical records staff observed that the nursing documentation, when printed, was many pages long but did not offer a clear picture of the patient…
Eventually it was decided that the documentation structure...should be revisited … (LaDuke, 2001:284)
As the above case illustrates, carefully reviewing documentation requirements in combination with automating information input and access increases the likelihood of decreasing the time required for documentation while maintaining, if not improving, patient care documentation (Allan and Englebright, 2000; Butler and Bender, 1999). Successful automation initiatives also are associated with the use of computerized patient records (Clayton et al., 2003; Walker and Prophet, 1997).
As noted earlier, however, internal efforts by HCOs alone are not likely to maximize documentation efficiency and utility because many documentation demands are imposed by external entities, including regulators and payors. In recognition of this fact, in 2001 the Joint Commission on Accreditation of Healthcare Organizations (JCAHO) convened a 20-member task force of hospital leaders, clinicians, and other experts to conduct an in-depth review of its hospital standards and requirements for demonstrating compliance. The task force’s recommendations for streamlining standards and standards compliance requirements are scheduled to be formally implemented on January 1, 2004 (JCAHO, 2002). Similar actions by governmental regulators could be useful in decreasing the documentation burden on nurses, as several governmentally mandated reporting tools (e.g., OASIS) have been cited by nurses as requiring large amounts of time and not enabling adaptation to individual patient needs (Trossman, 2001).
Finally, nurses are also influenced by practices learned as a part of professional education and training. Yet documentation practices used to demonstrate critical thinking skills and knowledge to a preceptor may not always be necessary for effective documentation in clinical practice. Moreover, as noted above, some nurses practice detailed documentation as a proactive defense against litigation (Fiesta, 1993).
Effect of the Physical Design of Workspace on Efficiency and Safety9
The physical features of inpatient facilities can obstruct efficient nursing work and diminish patient safety. Poor layout of patient care units and patient rooms and poor design and deployment of communication technologies reduce the amount of time nurses have available to monitor patient status and provide direct care. The increasing practice of transferring patients to different care units also presents opportunities for inefficiencies, gaps in care, and care errors.
Design of Patient Care Units
The majority of hospital in-patient care is delivered on patient care units (also called “nursing units”), where patients are grouped according to age, diagnosis, or clinical condition (e.g., medical, surgical, pediatric, oncology, intensive care, or cardiology). Smaller community hospitals may have less specialization of patient care units and group more diverse populations into fewer units to respond to fluctuations in census. Although nursing units account for less than half of the total area of most hospital buildings, their size and shape still dictate the overall design of the entire structure.
Nursing units possess three to four distinct spaces: the patient space, the nursing station(s), the “core” space, and the hallway. The design and location of these spaces, the location and storage of equipment, the relationships of the patient rooms to the various supplies, the materials used, and the technology required to deliver care vary greatly from hospital to hospital:
-
Patient rooms—Patient rooms can be private or semiprivate. In some cases, “semi-private” can mean as many as four to six beds in one large room. In the last 10 years, in response to growing inpatient acuity and
-
scarcity of critical care beds, these four- to six-bed rooms increasingly have been used as “progressive care” rooms for patients with a level of acuity between critical care and medical–surgical to enable better nursing observation. Patient room assignment is guided by the sex of the patient, the presence or absence of an infectious process, and (when possible) patient preference. These factors can greatly decrease the efficiency of patient placement and nurse staffing in any hospital when the right “type” of room has to be located for a specific type of patient. Moreover, features of patient rooms can directly affect patient safety. For example, the majority of falls of hospitalized patients occur in the patient’s room, usually in association with elimination needs (Hendrich et al., 1995, 2003).
-
Nursing station—The nursing station is the hub of the nursing unit for both simple and complex communications in a multitude of care delivery processes. Some refer to it as the “so-called” nursing station, noting that it has become the location for the unit secretary as well as all health professionals who spend any time on the patient care unit, including physicians, pharmacists, respiratory therapists, physical therapists, dieticians, social workers, and pastoral care staff (Hamilton, 1999). The nursing station also is the point where nurses take and receive patient orders on paper or by phones; answer or initiate phone calls and pages; receive faxed reports; view orders and reported results (e.g., laboratory, x-ray); pick up stat pharmacy deliveries; document the care process; and collaborate and socialize with other nurses, physicians, and allied health care workers. The resultant milieu can be a chaotic work environment that introduces environmental factors, including high noise levels and simultaneous conversations, conducive to human errors. The most familiar nursing unit design has a centralized nursing station.
-
Core unit space—The core of a nursing unit, sometimes referred to as the “nursing space,” often consists of clean and dirty utility rooms (equipment/instruments); medication, treatment, and supply rooms; a pantry for food and beverages; staff lounge/locker space; medical equipment storage; a housekeeping closet; and staff and/or patient conference room(s).
-
Hallway—The hallway of a nursing unit is the necessary space between patient rooms and the nursing station and core unit. The hallway represents the total distance the nurse must travel between spaces, and it is heavily influenced by the size and class of patient rooms (private/semiprivate). The location of the patient rooms, nursing station, and core unit space relative to this hallway is critical to the overall time and distance nurses must travel to deliver patient care. Because of a lack of adequate storage space, medication carts, wheelchairs, isolation carts, and dietary carts are often found in the hallway, blocking travel for both patients and caregivers and introducing safety hazards (falls, fire, public access to medications and supplies) in the environment.
Nursing units have varying geometric designs (Bobrow, 1978; Bobrow and Thomas, 2000; Cox and Groves, 1990; Hamilton, 1990; James and Tatton-Brown, 1986). The most common designs are as follows:
-
Simple open or nightingale form—Consists of an open ward without individual patient rooms. Patient beds face inward toward a single walkway, with a nursing station located in the middle; support spaces (e.g., supplies) are located off the unit. Some trauma or cardiovascular intensive care units are still configured as open wards for high-acuity surgical patients. Critical-care unit shapes (e.g., circular, linear, horseshoe, triangle) have been developed on the premise that every patient should be observable from a central nursing station (Hamilton, 1999).
-
Corridor or continental form—Patients are located on one or both sides of a corridor with four to six beds in a room, for a total of up to 30 beds (can be in a “T”, “C”, or “L” shape).
-
Duplex or nuffield—Has Corridor characteristics, but is split into two sections containing up to 20 beds each. Each section has its own nursing station. Nursing and ancillary space is shared between the two sections.
-
Racetrack or double corridor—Patient rooms are farther apart, with support spaces between the two corridors. Cross-over hallways connect the two corridors at the ends and complete the loop or “racetrack.” This design can require that nurses spend much of their time traveling, since it utilizes only one clean and dirty utility room and a single nursing station. Travel distance from the nursing station to the utility room to the patient is very high, and visualization of the corridors is poor. A modified version of this unit design is one of the most common types found in acute care hospitals.
-
Courtyard—Sometimes referred to a “complicated racetrack,” this design has an open courtyard for ventilation in the middle of the unit (used in Europe in hospitals without air conditioning). The design creates a need for additional nursing stations with increased travel distances.
-
Cruciform or cluster—A modern Corridor ward plan that has more barriers, walls, doors, and toilets erected between the nursing station and patients. The shape is manipulated to group as many patients as possible around the nursing station and increase patient privacy.
-
Radial—A circle design that permits a “fishbowl” view of each patient room from the nursing station. Observation is maximized in a central location.
-
Triangle—The space in the middle of the triangle balances the support space and the number of beds (usually around 30 beds). Unlike the racetrack, this design attempts to minimize nursing travel distance.
Hybrids of these designs are created by varying their corners and lines.
Each of the above nursing unit designs has advantages and disadvantages depending on which single perspective is considered—the patient, the caregiver, or the hospital. Open ward or “fishbowl’ designs can maximize observation and staffing efficiencies, yet a patient’s privacy can be greatly decreased (Hamilton, 1999). The racetrack design can maximize the number of beds on a unit but significantly increase nurse travel times. The triangle can provide less travel distance but greatly reduces available square footage in the patient’s room, and affects family space and patient–family interaction.
A 1994–1996 time and motion study of more than 1,000 hours of nursing unit time on a medical–surgical unit in a comprehensive tertiary care hospital over an 18-month time period documented how nurses and other health care workers spend their time and provided insight into how the environmental design of the nursing unit can affect nursing workload (Hendrich and Lee, 2003a). Four cameras were installed to capture all nursing unit activities simultaneously in patient rooms, the nursing hallway, and the nursing station. A total of 978 hours was accepted into the study, with 3,690 events being measured in the patient rooms. In addition, a random 24-hour continuous sample of all activities in the nursing station was taken from the 978 hours. The analysis tracked excess motion, inefficiencies, health care worker patterns, ergonomics, workspace organization, safety, and how nurses spent their time. The study found that:
-
The total time all health care workers (not just nurses) spent in patient rooms on direct care and assessments ranged from only 1.1 to 3.3 hours (median 1.7) in a 12-hour period.
-
The majority of the nurses’ time was spent walking between the patient rooms and the nursing unit core, or in the nursing station.
Patient Transfers
The transfer or hand-off of patients from nurse to nurse, shift to shift, unit to unit, and HCO to HCO has also been identified as a potential source of errors and adverse patient events (Cook et al., 2000). These transfers create opportunities for gaps in the continuity of patient care through loss of information or interruptions in the care delivery. Most of these gaps in care are anticipated and addressed by the health care system through such mechanisms as shift-to-shift-reports by nurses, patient care planning and discharge instructions, and discharge summaries. When gaps are unanticipated or not well bridged or when events or conditions overwhelm usually effective bridging mechanisms, patient safety is threatened. Patient hand-offs also result in duplication of effort and waste.
Interunit patient transfers within acute care hospitals in particular are associated with risks to patients and require a significant amount of direct and indirect labor. Such transfers originated with the creation of the first coronary care units in the 1960s and the specialized intensive care units (e.g., neonatal, medical, and surgical) that followed. These higher levels of specialized care created the need to transfer patients to higher- or lower-acuity care units as their clinical condition worsened or improved (Gallant and Lanning, 2001). The number of transfers increased even more with the creation of progressive, step-down, or transition units, which offer an intensity of nursing service between that of an intensive care and a general medical–surgical unit. Thus, it is not unusual to see a patient cared for by five different nursing units—e.g., operating room, postanesthesia care unit, critical care unit, step-down unit, and general–medical surgical unit—during his or her hospital stay. Transferring patients to units with higher staffing levels and greater experience in caring for critically ill individuals offers advantages for the clinical care of patients, but the unintended consequences of these patient transfers are also worthy of study. For example, this increasing specialization of nursing units and the resulting increase in interunit patient transfers introduces disruption in patient care and creates patient flow bottlenecks due to waits and delays in bed assignments.
A 13-month (2000–2001) observational study of 200 patient transfers within a 500-bed tertiary-level hospital tracked time and tasks for each patient transfer between units (other types of transports to procedures or testing off the unit were not included) (Hendrich and Lee, 2003b). Each transport was observed in an effort to collect valid and reliable measures of the time and activities necessary for health care workers to move patients between nursing units. Among the study findings were the following:
-
The average elapsed time from the point at which the physician wrote a patient transfer order until the patient arrived in a new bed on another nursing unit was 306 minutes (5.1 hours), with a median of 250 minutes (4.16 hours).
-
The actual measured direct labor cost (based on the number of caregivers, their job class, and their hourly wage times the number of minutes involved in transport activity) was $35.17 an hour. (Subsequent nursing wage increases will increase this actual cost significantly).
-
Additional indirect hospital costs associated with patient transfers included lost nursing productivity, the cost of equipment required for transport, duplication and rework of the patient care process (documentation, forms, and assessments), errors, omissions or events that occurred as a result of the transfer, and laundry/linen and housekeeping expenses.
-
Patient length of stay was estimated to increase up to half a day for each transfer due to disruptions in the care process.
Other patient transfers occur between patient rooms in the same unit—sometimes for infection-control purposes, and at other times because of difficulties between roommates in semiprivate rooms. In a new 348-bed facility built by Bronson Methodist Hospital in Kalamazoo, Michigan, savings of about $500,000 per year were noted as a result of the use of all private rooms and not having to transfer patients because of infection control or roommate problems (Rich, 2002).
Other new technologies or work design strategies can create unintended gaps in care. Cook et al. (2000:792) cite the use of “patient care technicians” as an example of how new work design can actually create new opportunities for error:
… consider the effects of dividing nursing work between nurses and “patient care technicians.” The economic benefits of division are substantial: it allows the nurse to spend virtually the entire work shift concentrating on high level tasks that require certain credentials (giving intravenous drugs, for example) while other tasks are given to less skilled personnel. Among the side effects of such a change, however, are restrictions on the ability of the individual nurse to anticipate and detect gaps in the care of the patient. The nurse now has more patients to track, requiring more (and more complicated) inferences about which patient will next require attention, where monitoring needs to be more intensive, and so forth.
All of these patient hand-offs create opportunities for gaps in care, as well as the need for re-work and waste.
Poor Communication Technology
Nursing staff spend a great deal of time hunting down other nurses, physicians, and patient information. One hospital work sampling study of nurses across all hospital inpatient units found that nurses spent 10 percent of their time in patient-related communication. The major problem faced by these nurses was “looking for someone down the long halls to relay a message” (Linden and English, 1994). In a study of communication systems in a 56-bed neurological unit at a Midwest hospital, nurses estimated that they spent 25 percent of their time looking for another person, for example, the nurse with the narcotic keys or staff needed to help turn or transfer a patient or help with procedures (Miller et al., 1997).
Redesign of inefficient nurse call systems has been identified as an opportunity to decrease the amount of “non-value-added” time that nurses spend handling calls that do not require a response from a licensed nurse or responding to mistaken calls (i.e., the patient turned on the nurse call light by mistake). A study of nursing units at two large metropolitan hospitals found that almost 70 percent of nurse calls did not require a licensed nurse
to meet the patient’s needs (Miller et al., 1997). Design features to make nurse call systems more efficient and effective that have been identified by nurses include providing higher-quality audio, using medical secretaries to serve as the first responder and “triage” calls not requiring the assistance of a nurse, allowing nurse call lights to be turned off at the nursing station instead of requiring someone to go into the patient’s room for the purpose, providing room-to-room communication, using such devices as locator badges to locate needed personnel, and enabling hands-free operation of the system (Miller et al., 1997, 2001).
Providing the capability for computerized physician order entry and making patient education material available electronically to nurses also have been identified as strategies to facilitate communication. With computerized physician order entry, nurses do not have to engage in transcription or verification of orders. Electronic patient education materials, unlike printed materials, are easily modifiable to meet clinician and patient needs; it is also possible to track which materials were given and by whom, assess follow-up and comprehension, and link education activities and documentation (Case et al., 2002).
Sensory Interference
Sensory distractions and interference, such as noise, poor lighting, glare-producing surfaces, and clutter, can interfere with nurses’ work (Spath, 2000). Some hospitals further report that creating calming, “healing environments” through such design features as softer colors and indirect lighting has decreased patients’ use of pain medications and saved hospitalization costs (Rich, 2002).
Noise is recognized as a serious health hazard to hospital patients, but it is also recognized as interfering with worker performance. While most studies of the effects of noise in the work environment have been conducted in non–health care settings, the contribution of noise levels to nurse stress and work distractions is increasingly being documented (Morrison et al., 2003; Topf, 2000). In health care facilities, sources of noise can range from overhead paging systems and equipment alarms to heating, ventilation, and air-conditioning (HVAC) systems, plumbing, and ice machines. Reducing noise by installing materials that absorb sound, such as ceiling and wall materials and carpeting, can be accomplished at modest cost (Walsh-Sukys et al., 2001).
Noise and other sensory interference can be reduced by employing activities, tools, and principles developed by a number of different disciplines, including human factors, ergonomics, and engineering—many of which are already being used by some HCOs. New construction projects especially—whether a new building or an expansion or renovation of existing space—
present opportunities to improve workspace and work design. The effect of these and other design characteristics of nursing workspaces (and other aspects of health care facility design) on patient outcomes and facility performance are being studied under a research project (The Pebble Project) sponsored by The Center for Health Design, a nonprofit research and advocacy organization, and a network of 11 health care providers (The Center for Health Design, 2003a). Among the preliminary findings reported by the project are decreases in patient transfers, nosocomial infections, patient falls, medication usage, and medical errors (The Center for Health Design, 2003b).
Designing Work Processes and Workspaces to Enhance Safety and Efficiency
The Work Design Process10
Work design involves examining the various elements or factors that workers use, encounter, and experience in performing their work. In addition to the characteristics of the workers themselves, the elements considered include the nature of the task to be performed; the tools and technologies available for use; the physical environment in which the work is to be carried out (e.g., noise level, lighting, space, sources of distractions and interruptions); and organizational conditions, such as the level of communication and collaboration among the individual(s) who perform or use the work. These five elements are described as a work system because they interact with and influence each other. In examining these elements, questions such as the following are addressed:
-
What are the characteristics of the individual performing the work? Does the individual have the musculoskeletal, sensory, and cognitive abilities to do the required task? If not, can any of these gaps in ability be accommodated in the design of the task?
-
What tasks are being performed, and what characteristics of those tasks may contribute to unsafe patient care? What in the nature of the tasks allows the individual to perform them safely or assume risks in the process?
-
What tools and technologies are being used to perform the tasks, and do they increase or decrease the likelihood of untoward events?
-
What aspects of the physical environment can be sources of error or promote safety? What in the physical environment ensures safe behavior or allows room for unsafe behavior?
-
What in the organization prevents or allows exposure to hazard, and what promotes or hinders patient safety? What allows for assuming safe or unsafe behavior by the individual?
Because of their interrelatedness, work design needs to consider all these elements. Whenever one work element changes, there will be implications for the other elements (Carayon et al., 2003).
Work design is performed by collecting and analyzing data and information such as that listed above on the task or problem area, synthesizing the information, developing a proposed plan, and evaluating the plan once it has been implemented. Various approaches can be used to collect and analyze data and information: direct measurement, observation, surveys, interviews, review of organizational documents (e.g., position descriptions, organization chart), and analysis of archival data (e.g., patient satisfaction data, error reporting systems). Because each of these approaches has both weaknesses and strengths, multiple approaches provide the greatest confidence in the results obtained.
Several work and error analysis techniques also have been developed that can help individuals involved in work redesign initiatives discover more fully all contributing causes of adverse patient events, especially the latent conditions that contribute to the occurrence of such events.11 Three commonly used work redesign techniques are work sampling, root-cause analysis, and anticipatory failure analysis. Methods for achieving “LEAN” operations (defined below), widely used in other industries, are also beginning to be applied to work and workspace design in HCOs. These techniques are each discussed below.
Work and Error Analysis Techniques
Work sampling In work sampling studies, workers are observed a specified number of times at random or fixed intervals. For each observation, data are recorded on the task being performed (Carayon et al., 2003). Work sampling has been used to obtain insights into how nursing staff use their time, identify problem areas, and provide information for unit and work redesign (Linden and English, 1994; Pedersen, 1997; Scherubel and Minnick, 1994; Upenieks, 1998; Urden and Roode, 1997). However, work
|
11 |
As discussed in Chapter 1, latent conditions are usually less visible at the time an error occurs. |
sampling studies are limited in their power to accurately reflect all of nurses’ work (Carayon et al., 2003) because the method assumes that the tasks involved are observable, unambiguous, mutually exclusive, and exhaustive—not always the case with much of nursing work.
Root-cause analysis Root-cause analysis has long been used in engineering to examine organizational or system problems. It is a retrospective, qualitative process aimed at uncovering the underlying cause(s) of an error by looking past the “sharp end” of an error (see Chapter 1) to the enabling latent conditions that contributed to or enabled the occurrence of the error. Root-cause analysis involves a cycle of questions: What happened? Why did it happen? What were the most proximate factors causing it to happen? Why did those factors occur? and What systems and processes underlie those proximate factors? Answers to these questions help identify barriers and causes of problems so similar problems can be prevented in the future.
JCAHO requires that health care organizations perform root-cause analysis in response to all sentinel events. JCAHO also requires that HCOs, based on the results of this root-cause analysis, develop and implement an action plan consisting of improvements designed to reduce risk and monitor the effectiveness of those improvements (JCAHO, 2003). Wald and Shojania (2001) note that root-cause analysis is a labor-intensive process, and that there is not yet evidence that by itself it can improve patient safety. However, they also observe that the technique provides HCOs with a formal structure for learning from past mistakes.
Anticipatory failure analysis While root-cause analysis is performed in response to an adverse event that has already occurred, anticipatory failure analysis is used to identify and eliminate known and/or potential failures, problems, and errors from a system, design, process, and/or service before they occur. Failure modes and effects analysis (FMEA) is one technique used to conduct this type of analysis. Its goal is to prevent errors from occurring by attempting to identify all of the ways a device or process can fail, estimate the probability and consequence of each failure, and then take action to prevent the potential failures from occurring. Failure modes and effects analysis is typically conducted by multidisciplinary teams in an HCO on many different patient care processes, including device design. It is used to assess both existing and new products and processes (Carayon et al., 2003).
“LEAN” operations Root-cause analysis and anticipatory failure analysis are typically used to help nurses perform desirable, “value-added” nursing activities, such as medication administration, documentation, and patient monitoring, more efficiently or safely. LEAN operation techniques address not the enhancement of desirable, value-added activities, but the elimination of undesirable, often invisible activities—the waste inherent in
all work processes—through continuous improvement in pursuit of perfection (Alukal, 2003). The term is used in this country to refer to techniques pioneered in the Toyota Production System (described in Chapter 4), which are well known to most industrial engineers.
LEAN thinking is based on the premise that all processes are composed of value-added and non–value-added activities and time. In a hospital environment, value-added represents any activity that increases the health, healing, wellness, and satisfaction of the patient. These are activities that are patient-centric, timely, and not wasteful. Non–value-added activities are those that do not increase the health, wellness, and satisfaction of the patient, and thus should be eliminated, simplified, or reduced.
In attempts to increase efficiency and the quality of their products, most organizations typically focus on value-added activities and core competencies. Traditionally, very little consideration is given to the non–value-added activities that occur throughout the organization. The result is that the root causes of waste and inefficiency that result in poor performance are often nurtured by the organization and institutionalized in policies and procedures. LEAN techniques attempt to eliminate sources of waste through the use of such practices as the following:
-
Visual controls—keeping work processes and indicators in view so everyone can understand the status of the work system at a glance.
-
Streamlined physical plant layout—designing facility layout to optimize the sequencing of work processes.
-
Standardized work—using prescribed methods to perform routine tasks.
-
Point-of-use storage—locating supplies, equipment, information, and procedure rules where they will be used, thus saving the time otherwise involved in locating and obtaining them.
The Toyota Production System identifies seven categories of waste attributable to a manufacturing facility. A brief summary of those seven categories, modified for the hospital environment and design of nursing workspace, is shown in Table 6-1 (Hendrich and Lee, 2003c). LEAN techniques and other work analysis approaches (e.g., total quality management, continuous quality improvement, and six sigma DMAIC [define, measure, analyze, improvement control]) are not mutually exclusive. Rather, they are complementary and can be used together (Alukal, 2003; Smith, 2003).
Work design principles Regardless of the resources, approaches, and sources of expertise an HCO is able to bring to bear on a specific work design effort, principles for effective and safe work design have been identified that can guide all work (re)design initiatives. These principles, detailed
TABLE 6-1 Seven Categories of Waste as Applied to the Hospital Environment
|
Category |
Root Causes of Hospital Waste |
|
Poor Utilization of Resources |
People, resources, and supplies are deployed or stored in the hospital at the wrong place, at the wrong time, and in the wrong quantities. Time must be spent in locating and obtaining those items needed to provide care. |
|
Excess Motion |
Poorly designed workspaces and units, process complexity, and discontinuous processes contribute to excess caregiver motion in the workspace, patient room, and/or nursing hallway. |
|
Unnecessary Waiting |
Delays involving patients, nurses, and resources are caused by process complexity and interdependency, poor execution, organizational misalignment, and inaccessible information. Nurses must wait to provide care because necessary personnel, supplies, authorizations, or patients are not where they need to be. |
|
Transportation |
Movement of resources and inventory is inefficient because of policy and process inefficiencies, intra-unit patient transfers, and inefficient layout and unit organization. |
|
Process Inefficiency |
Unnecessary steps in the patient care process, poor execution, and unplanned interruptions take health care workers away from the patient. |
|
Excess Inventory |
More supplies and inventory are on hand than are needed, creating waste. This includes waste of nursing personnel when, for example, nurses are called in to work, but then sent home because of low census. |
|
Defects/Quality Control |
Mistakes, omissions, and accidents are caused by distractions, discontinuous processes, and nonconformance or lack of standardization. |
in the following subsections, aim to create reliable and safe patient care processes by:
-
Eliminating errors—changing work processes so errors cannot be made. While the total elimination of all errors is impossible, work design principles should aim to continuously eliminate errors consistent with principles of continuous quality improvement, the defect-free goals of the Toyota Production System described in Chapter 4, six sigma DMAIC approaches to error reduction, and other improvement approaches that have “zero errors” as their goal.
-
Reducing error occurrence—redesigning processes so that errors are less likely.
-
Detecting errors early—catching errors early before patient harm occurs.
-
Containing the effects of errors—designing features to mitigate the consequences of errors once they occur (Spath, 2000).
Directly involving workers throughout the design process The workers who currently perform the activity to be redesigned or will perform a new activity are the users, beneficiaries, and consumers of work design. Therefore, their active participation in all aspects and stages of work (re)design is essential. Active participation, in which employees are directly involved in the work redesign activity, is distinguished from passive participation, whereby the organization communicates with employees regarding the work redesign (Carayon et al., 2003). As discussed in Chapter 4, employee participation is a key ingredient in successful organizational change, improving the outcome of work (re)design, and facilitating its successful implementation. Benefits include more thorough diagnosis of and formulation of solutions for problems and more rapid implementation of technological and organizational change, as well as increased employee motivation, job satisfaction, and performance (Lawler, 1986; Noro and Imada, 1991; Wilson and Haines, 1997).
Nursing units are organized in a variety of ways, reflecting different decision-making, work allocation, communication, and management approaches (Kovner, 2001). Resources and work processes also differ on nursing units, as do patient levels of care and the experience level of nurses (Deutschendorf, 2003). Evidence does not yet exist for identifying any one best model for providing nursing care (Seago, 2001). A unit with highly experienced RNs may need a different structure from one with novice nurses. As the nature of nurses’ work changes, new models will need to be developed and deployed (Kimball and O’Neil, 2002). Thus work processes need to be designed with consideration of unit-specific structures and processes (Deutschendorf, 2003), something that is best accomplished through the active involvement of nursing unit staff.
Simplifying and standardizing common work procedures and equipment Simplifying key work processes can greatly reduce the likelihood of error and facilitate the formulation of solutions when problems occur (IOM, 2000). Standardizing processes reduces the need for workers to rely on memory and allows new workers unfamiliar with a procedure or device to employ it safely. The increasing use of clinical pathways in many hospitals (see Chapter 5) is an example of standardizing patient care to reduce variation in practice and opportunities for error. Simplifying and standardizing routine procedures, such as IV insertion, catheter insertion, dressing changes, care for decubiti, tracheotomy care, and other nursing treatments
and procedures, minimizes opportunities for slips and lapses.12 Standardization also can be used for both facility and room design (e.g., location of electrical outlets, bed controls, and equipment cupboards), medical equipment (e.g., IV pumps, hand disinfection products, and sinks), and location of monitors and other equipment. Standardization of patient care environments and equipment decreases the cognitive load on nurses, making slips and lapses less likely to occur during routine tasks by minimizing decision time and manipulation time.
Avoiding reliance on individual worker memory Given the enormous and expanding body of health care knowledge, and the great variation in patients’ health status and needs, as well as the very nature of the human condition, individual nurses cannot be expected to retain all the information necessary to provide state-of-the-science health care. Both automated and hard-copy memory aides, such as procedure checklists and protocols, clinical pathways, drug reference databases, and computerized decision aids, can help compensate for the limitations of human memory (Spath, 2000).
Decreasing interruptions, distractions, and interferences An interruption has been defined as the cessation of a task before its completion as the result of any external factor, and a distraction as an external stimulus causing a human response but not cessation of a task (Flynn et al., 1999). Interference denotes competition for the cognitive resources required for the performance of simultaneous tasks, which often occurs in busy work settings. Errors attributed to interference appear to be more likely with novel or difficult tasks (Dornheim, 2000).
Most evaluations of the effects of interruptions, distractions, and interference on human performance have been conducted in industries other than health care. These factors have been found to be important contributors to nearly one-half of significant aviation flight crew incidents (Dornheim, 2000). When health professionals have been asked to report their perceptions of why medical errors occur, interruptions and distractions have frequently been cited (Ely et al., 1995).
Nurses frequently cite distractions and interruptions as contributing to their commission of medication errors (Wakefield et al., 1998; Walters, 1992). Interruptions and interference are also reported by nurses in nursing
homes as occurring frequently and requiring them to repeatedly revise plans, alter directions, and cease activities prior to completion (Bowers et al., 2001). In a random sample survey of nurses licensed to work in Illinois and North Carolina, conducted as part of a longitudinal study of nurses’ worklife and health funded by the National Institute for Occupational Safety and Health (NIOSH) of the U.S. Centers for Disease Control and Prevention (CDC), 75 percent of the 674 RN respondents who were currently employed as a full-time hospital or nursing home general-duty/staff nurse agreed or agreed strongly that “my job requires long periods of intense concentration”; 82 percent similarly agreed that “I work very fast”; and 79.6 percent agreed that “tasks are often interrupted without being completed.”13
Studies of crew resource management in aviation provide insight into how to limit the effects of interruptions and distractions in that setting (Dismukes et al., 1998). Similar strategies have been employed for evaluating errors in operating rooms (Cooper et al., 1984). However, strategies for reducing interruptions and distractions in nursing settings have not been well developed. A quasi-experimental study of two interventions in a medical–surgical unit (an active avoidance protocol for staff and wearing of a color-coded vest with a warning to avoid interrupting a nurse who is administering medications) found that interruptions and distractions could be significantly reduced (Pape, 2003). Other strategies include closing the patient’s door while conducting bedside care and using manual or electronic message boards to convey nonurgent requests.
Instilling redundancy and back-up systems High-reliability organizations and other safety-conscious organizations design redundancy into their production processes to ensure that there are several ways to identify problems before they become catastrophic. For example, the control tower of a navy aircraft carrier, which is responsible for all activity on the flight deck and hangar, uses more than 20 devices to ensure communication with critical parts of the ship. The landing signal officer on the flight deck is connected directly to the air commander in five different ways: a regular telephone, two sound-powered hot lines, two radios, and a public address system. These multiple communication channels are supplemented by the tower’s capability to call the deck “foul” or not ready to receive an airplane, which serves as one final way to communicate with the landing signal officer. Similarly, airlines have two qualified pilots on each commercial flight, and air traffic controllers work in pairs. Members of such organiza-
tions learn what is important by observing where the organization focuses its time, energy, and resources. When an organization spends the money to create redundancy, there is no question in anyone’s mind that the organization takes the possibility of errors very seriously (Roberts and Bea, 2001).
In manufacturing industries, a person or machine may be unable to respond to a request on demand because of an unexpected mechanical breakdown. For this reason, surplus stocks of parts and equipment are maintained. When customer needs are so large and unpredictable that it is impossible for a plant to adjust production in a timely manner, “buffer stock” is kept at or near the shipping point as a countermeasure (Spear and Bowen, 1999). In the work environment of nurses, redundant staffing or “slack” in staffing is recommended (see Chapter 5) as one way to ensure the ability to respond to unexpected variations in need for additional staff.
Using constraint and forcing functions The most unambiguous way to design work so as to prevent a worker from making an error is to render the worker incapable of taking the erroneous action (referred to as a constraint) (Reason, 1990). For example, the design of certain vehicles prevents automatic door devices from being deployed accidentally when the vehicle is in motion. Conversely, a forcing function forces a worker to take a correct action.
Avoiding reliance on individual vigilance Because of the limits of humans’ ability to maintain a high intensity of vigilance over prolonged periods of time, it is important not to rely on a single individual’s vigilance to monitor for threats to safety. A good example of how equipment has been engineered to decrease the need for extensive vigilance on the part of a nurse is the use of alarms on automatic IV pumps and other patient care and patient monitoring devices. The patient and family members can provide additional monitoring assistance. When patients and their families are knowledgeable about any treatment protocols and prescribed medications, they can take a more active role in monitoring care, as well as providing self-care.
Reducing and compensating for hand-offs A number of strategies to address issues associated with patient hand-offs (see the discussion earlier in this chapter) are being implemented today. “Universal rooms,” single-stay units, and acuity-adaptable rooms all aim to place a single patient in a care room or nursing unit for his/her entire hospital stay (Gallant and Lanning, 2001). The room or unit adapts to the changing health status of the patient, eliminating the need for patient transfers. However, early testing of acuity-adaptable rooms has indicated that several factors are critical to their appropriate use.
The first of these factors is the environmental design component—an acuity-adaptable headwall (e.g., one that includes additional gas and line outlets). The second is advanced medical–surgical skills on the part of the nurse. The third is identifying the subset of intensive care unit patients appropriate for care in an acuity-adaptable unit. While trauma patients in an intensive care unit typically require highly specialized, intensive interventions, a more hemodynamically stable group, such as coronary care patients, may be able to receive better care on an acuity-adaptable unit that provides both step-down and general medical care. Finally, there needs to be a sufficient number of patients in a like disease state to justify consolidating multiple levels of care into one unit (Gallant and Lanning, 2001).
The committee found only one study that tested the application and safety of acuity-adaptable rooms. This study found significant improvements in quality and operational costs, including a large reduction in clinician hand-offs and transfers, reductions in medication and patient falls, improvements in patient satisfaction, and an increase in patient days per bed on a base of fewer beds (more efficient use of beds) (Hendrich et al., 2004). Further testing is needed on the use of acuity-adaptable rooms as an alternative to transferring patients to a unit staffed with specially trained nurses and other care providers who have benefited from experience with a high volume of intensive care unit interventions.
There are other ways to decrease the risks of hand-offs. They include hospital-wide automated patient records so that there is no temporary loss of patient care information (as can occur when a patient’s hard-copy record is transferred to a new unit), and providing ample space in the patient care room for family to accompany the patient.
Improving information access Good decision making requires good information. This information can best be provided through automated and integrated clinical information systems that provide access to patient information, together with clinical decision support systems (Ball et al., 2003) (see Chapter 5). Information technology used in this way can reduce work errors and inefficiencies.
The increase in safety and efficiency achieved through automated patient records integrated with other clinical information systems is well illustrated by the automated information systems in place at Intermountain Health Care in Salt Lake City (Peck et al., 1997). Access to patient information is facilitated through automated patient records. Patient histories, physical exams, vital signs, and other clinical data are documented on line. When patient records are automated in this way, all patient data are easily accessed and viewed. The nurse can see the patient’s longitudinal history. Little time is wasted in calling to see whether a laboratory test or radiology result is available, because the patient record is linked to the laboratory or
radiology department, and test results are entered immediately. Allergy information is always accessible, so that caregivers are aware of preexisting conditions. Clinicians need not be physically or temporally co-located to collaborate since they can view and discuss data simultaneously. Providers with a legitimate need to know can access the record anytime, anywhere.
Intermountain Health Care identifies other benefits of automated patient records integrated with automated clinical information systems. These benefits include the following:
-
Data that are organized and legible—The nurse can see all of the prescribed drugs for a patient in one location; the doses are written clearly, and names are spelled correctly. Data are grouped to ensure that important data are not buried among the more routine. A problem list shows acute and chronic conditions and complete known allergies. Other health care team members can view the nurse’s concerns and respond to them. Abnormal findings are highlighted, and trends can be graphed and compared with interventions (e.g., temperature spikes correlated with drug administration). An integrated plan allows all members of the collaborative care process to see what is happening and decide what should occur in the future. Everyone knows who is responsible for the patient and who needs to communicate about the patient’s care.
-
Support for ongoing knowledge acquisition—The patient’s clinical data can be linked to reference literature to answer questions about policies, procedures, prognosis, diagnoses, educational material, appropriate drug dose, drug contraindications, and the like.
-
Generation of alerts, reminders, or suggestions when standards of care are not being followed—Rules can be implemented to address changes in the patient’s condition or to remind providers of process issues. For instance, Intermountain Health Care (IHC) manages patients receiving the medication coumadin by having the computer screen show the results of the most recent clotting factor test or the unanticipated absence of such results to see which patients are out of acceptable blood value ranges and need dosage adjustments or another test. Similar messages for ventilator management are sent directly to the provider. Intermountain Health Care also manages populations of people with diabetes by reminding providers which patients have not had glycosalated hemoglobin tests, retinal exams, and so on. Similar reminders are sent about pap smears, mammograms, and immunizations. Process reminders are also used. When documentation is not recorded that a wound dressing has been changed according to schedule, IV tubing has been changed, or drugs have been administered, the automated patient record generates reminders according to rules that are agreed upon by providers. These measures help integrate evidence-based medicine into the process of care.
-
Asynchronous messaging—This technique allows team members to communicate with one another without each member having to be present at the same exact location at the same point in time. This prevents wasting large amounts of time trying to track down a busy physician during office hours or a nurse on the following shift. Things that should be communicated do not slip between the cracks. At Intermountain Health Care, 2,568 staff voluntarily chose to start using a message log in the first year after the message log application was made available. These users are primarily in the ambulatory arena; application to Intermountain Health Care acute care facilities is now under way. Other applications, such as personal radio transceivers, also facilitate instant messaging.
In general, an electronic information database aids patient care, quality assessment, and research. The hallmark of quality improvement is feedback to users on the results of their activities. With the ability, for example, to assess how often different nursing divisions use restraints for similar populations, one can begin to assess processes that lead to improved outcomes. The degree to which skin breakdowns occur in patients being cared for on different units can be assessed and the results fed back. Ultimately, much of patient safety derives from this process of analysis. Paper abstraction of handwritten charts is highly laborious and prevents large-scale analyses of nursing care. Automated record systems offer the potential to manage and assess the care provided to a much larger population on a routine basis.
As the discussion in earlier chapters on paperwork and documentation practices makes clear, automating patient records and clinical information also can reduce costs. Moreover, the nurse does not spend as much time in the find-and-fetch mode. Inventories are updated when supplies are used, so new supplies can be on hand when needed; charges are generated by the entry of point-of-care documentation rather than by the filling out of billing slips. Filing activities by ward clerks are reduced, allowing more time to help the nurse. Educational materials can be printed for the patient in multiple languages (Clayton, 2001).
Remaining alert to the limitations of and risks created by technology In searching for ways to improve patient safety, technology is often proposed as a strategy. Despite its potential, however, patient safety experts caution that technology by itself is not a panacea. While able to remedy some problems, technology may also generate new forms of error and failure (Battles and Keyes, 2002; Cook, 2002; Reason, 1990). Fundamental to the successful introduction of technology is a thorough understanding of the work flow and work processes involved in patient care (Cook, 2002; Goldberger and Kremsdorf, 2001). The expected benefits of a new technology may not occur if the technology is not designed appropriately (i.e.,
according to human factors and ergonomic principles) or does not fit with the rest of the work system.
For example, while microprocessor-controlled medication infusion pumps eliminate many cumbersome processes that are often the source of errors, they also introduce new demands, such as complicated set-up and operation procedures, that can lead to new sources of error. Bar coding technology can prevent patient misidentification, but the possibility exists that an error committed during patient registration may be disseminated throughout the information system and may be more difficult to detect and correct than with conventional systems (Wald and Shojania, 2001). Whenever a technology is implemented, then, the human factors characteristics of its design and its potential positive and negative influences on other work system elements should be studied.
Paying ongoing attention to work design Successful implementation of work redesign is not a one-time effort. Few changes in complex organizations work perfectly when first introduced; virtually all require modification over time to achieve optimum results. Ongoing monitoring, feedback, and redesign are therefore needed to create and sustain effective change (Goodman, 2001). Work (re)design should be considered a continuous process.
Moreover, it is not unusual for organizations or departments that have implemented innovations most recently to perform worse than those that implemented comparable innovations a year or two before. Macduffie and Pil (1996) point out that in the automobile industry, plants struggle in the first year following adoption of a new work system with the right mix of incentives, managerial supports, and training needs, as well as coordination difficulties with other units. Those that sustain the change into the second year begin to see cost and quality improvements. New practices often initially undermine existing routines and competencies and require ongoing learning, redesign of the change, and creation of support practices to capture the promised benefits.
Workspace Design for Safety and Efficiency
An example: Methodist Hospital, Clarian Health Partners In the mid-1990s, the Methodist campus of Clarian Health had two floors of nursing unit shell space available as the result of a consolidation process. An interdisciplinary planning effort employed continuous quality improvement principles and systems thinking, along with evidence from the literature, to determine how to best use this space. In addition, two work process and patient flow studies were conducted. The first was a 1,000-hour video capture of time and motion on a medical–surgical unit that simultaneously
detailed all activities in the patient room, nursing hallway, and nursing station. The second was an observational study of internal patient transfers.
As a result of these efforts, the interdisciplinary team determined that it was possible to redesign workspaces to (1) eliminate resource waste (caregiver and fiscal), (2) improve caregiver work environment and personal satisfaction, (3) improve patient care, (4) employ healing environment concepts, and (5) support future care delivery while solving patient flow problems. To these ends, it would be necessary to shift indirect time back to the nurse and patient care by reducing the steps necessary for nursing staff to obtain supplies, reduce transfers of patients, rework the care delivery model, minimize delays in patient placement and waits in holding areas, eliminate equipment duplication, maximize technology for efficiency, and have patient and caregiver information readily available at the point of care.
In 1999, the resulting Cardiac Comprehensive Critical Care unit was opened. It contains 56 acuity-adaptable, 400-square-foot patient rooms (28 per floor) designed to offer three main zones: the family zone, the patient zone, and the caregiver zone. The patient zone includes patient beds with acuity-adaptable headwalls and advanced computer technology directly at the patient’s bed, allowing staff to record weight and other vital data without disturbing the patient. Patients are admitted to and discharged from the same patient room. The family zone (150 square feet) offers such features as a chair-bed for nighttime visitation, a refrigerator, a computer hook-up, voice mail and TV/VCR, and customized educational kiosks and computer-based patient education. The staff zone offers similar conveniences. Because most of the distance traveled by nurses consists of going back and forth to the nursing or supply station, necessary supplies are maintained in the patient room. Nursing stations with computer access and servers for supplies are decentralized just outside the patient room. Corridor design allows for emergency equipment, such as defibrillators, to be hidden behind doors. Additional features for staff include a computerized education center for uninhibited access to e-learning and hospital information. Personal paging and an ID tracking system also pinpoint staff locations.
A comparison of 2 years of predesign baseline data with 3 years of data following the redesign found statistically significant changes in pre and post measures, including:
-
A 90 percent reduction in patient transports. The two units had averaged 200+ interunit transfers per month in the 2 years prior to the new design. With the new design, patient days per bed increased, although the units had fewer beds than previously.
-
A 70 percent reduction in medication errors.
-
A decrease in the cardiac population’s fall index to a national benchmark level of two falls per 1,000 patient days.
-
A decrease in nurses’ walking time and trips to obtain supplies. These and other efficiencies significantly increased available nursing time and permitted a reduction in budgeted staff care hours while increasing direct patient care time.
-
A decrease in patient dissatisfaction.
The Cardiac Comprehensive Critical Care Unit has been recognized by the American Association of Critical Care Nurses/Society for Critical Care Medicine/American Institute of Architects as “best design in a critical care nursing unit” (Hendrich et al., 2004).
Potential workspace design elements for safety Workspace design initiatives, such as that of Methodist Hospital and those undertaken by the Pebble Project, aim to improve efficiency, safety, and overall patient and workforce experiences in care delivery. Several workspace design elements (shown in Table 6-2) based on LEAN operation and other work design principles can potentially achieve workload reductions and more efficient and safer care delivery in general patient care rooms (Hendrich and Lee, 2003c; Ulrich, 1991). Similar concepts apply to the design of adult critical care units (Hamilton, 1999) although there are special considerations for neonatal intensive care units (Graven, 1997). The committee notes that little research has been conducted establishing the efficiency and effectiveness of these measures in improving patient safety. However, the committee also notes the evidence in support of their use as LEAN practices, as well as their beneficial effect on patients, and strongly urges further implementation and evaluation of these interventions.
Getting started in work redesign Some of the principles and methods of work design are relatively intuitive and easy to apply. Many HCOs already practice root-cause analysis; others have used work sampling and failure modes and effects analysis to redesign work. Work redesign is sometimes undertaken using quality improvement approaches such as the plan-do-check-act cycle (Carayon et al., 2003). Many of the documentation redesign initiatives described earlier were undertaken by interdisciplinary teams without the use of professional experts in work redesign. Other HCOs, including small community hospitals, have reported the use of internal work teams composed of existing staff to redesign work processes (Doerge and Hagenow, 1995; Fletcher, 1997). However, work design initiatives can be enhanced when individuals with knowledge of different disciplines, such as environmental design, human factors, and industrial relations, are involved. Sometimes this specialized knowledge can be supplied only by experts in work design with these areas of expertise.
TABLE 6-2 Workspace Design Elements for General Patient Care Rooms Based on LEAN Principles
|
Nursing Unit Design |
Elements of Workspace Design |
LEAN Principles |
|
The patient room |
Divide the room into workspace zones of care (Gallant and Lanning, 2001): • Patient • Caregiver • Family |
Maximize zones for order, efficiency, and standardization with an integrated approach. Direct caregivers should determine how this is best accomplished. |
|
Acuity-adaptable headwall |
An ambidextrous (each side of the bed) headwall is equipped with gases, lines, and electrical ports to accommodate advanced medical surgical acuity (Gallant and Lanning, 2001; Hendrich et al., 2004). Electrical plug-in locations are provided at varying heights on the wall (low/mid/high) to decrease back strain. |
Maximize the flexibility of care levels within the same patient room. Eliminate nursing trips around the bed to access a singular port. Eliminate the need for many intra-unit patient transfers, reduce the workload index; conserve critical care beds; and improve the throughput and capacity of the hospital. |
|
Bed types |
Beds with built-in functionality (scales, fall monitors, chair–bed status, motorized drives) can eliminate lifting and transfers and increase nursing efficiency and workload. |
Eliminate or reduce redundant devices (scales, restraints). Reduce the opportunity for caregiver injuries. |
|
A staff observation window for each patient room with acuity-adaptable headwalls |
This feature supports the acuity-adaptable care model, in which high observation must be balanced with privacy as patient acuity changes. This element is believed to be a requirement if different levels of patient acuity are to be handled in the same patient room. A full or half window on the inboard side of the patient room permits observation of two to three patients at a time when decentralized nursing stations are used. A blind, curtain, or opaque glass can be used for privacy. |
Eliminate many interunit transfers, thereby improving the workload index. Reduce the need for low-risk monitored patients to occupy critical care beds. |
|
Nursing Unit Design |
Elements of Workspace Design |
LEAN Principles |
|
Family zone |
A dedicated space is provided within the room with adequate chair, sofa, or bench seating to permit overnight stays (Gallant and Lanning, 2001; Ulrich, 1991), as well as a small locker or storage space. A mini-refrigerator in the family zone can provide access to nutritional supplements for the patient, and the family/significant other can participate in family-centered care, with the nurse as caregiver. |
Social supports tend to decrease stress and improve outcomes (Ulrich 1991). Many nursing call lights meet simple nutrition needs. Through self/family-centered care, nursing time can be preserved for activities requiring advanced skills. |
|
Private, adequate patient room |
An ideal room size has not been determined. Private, ample-size rooms ensure family space, adequate caregiver space, and appropriate space for safe patient mobility. The minimum space to meet these requirements, as well as to anticipate emerging, acuity-adaptable technology for the patient room, is probably at least 250 square feet (Hendrich et al., 2004). |
Accommodate the family, the acuity-adaptable headwall, and anticipated future technologies. Improve workspace conditions by promoting an organized work area. Potentially reduce patient risk of infection and errors when only one patient is in a room. |
|
Patient beds positioned to enable patients to see out a window, preferably providing visual exposure to everyday nature; exterior windows designed to distribute |
Views of nature provide positive distractions that can decrease stress and aid healing. Natural lighting provides a connection with nature. Staff lounges should be a respite for stress reduction and socialization if desired. |
Reduce worker stress and errors and promote patient healing and comfort through the provision of natural light and a connection with nature (Ulrich,1991). |
|
Nursing Unit Design |
Elements of Workspace Design |
LEAN Principles |
|
natural light into the patient’s room and the nursing workspace and staff lounge whenever possiblea |
|
|
|
An enlarged door entrance to the patient’s toilet |
The door should be large enough to accommodate two caregivers and the patient or a patient with an assistive device (walker, cane, wheelchair). |
Provide adequate maneuvering space for proper body mechanics to reduce opportunities for caregiver or patient injury. Locate the toilet close enough to the patient’s bed to permit patient transfers to the toilet without additional lifting or equipment, thus reducing caregiver injuries and skin friction for the patient. Eliminate or greatly reduce the need for bedside commodes, provide patient privacy in a safer toilet area with appropriate grab bars, and reduce caregiver contact with human waste. |
|
Equipment and supplies |
Locate small supplies used most frequently by nurses inside the patient’s room. |
Reduce workload and improve productivity by using a small equipment cart or built-in cabinetry in the patient’s room to safely store supplies that represent 80 percent of caregiver trips outside the room. |
|
Nursing Unit Design |
Elements of Workspace Design |
LEAN Principles |
|
Servers |
Cabinetry or drawers are designed to be “served ” or filled from outside the patient’s room by non-nursing personnel (care partners). |
Provide immediate access to laundry and linen. Allow for transfer of soiled and clean materials and keep the hallway clear. Conserve scarce nursing resources and time. |
|
Nursing call light system |
A multifunctional communication network can optimize communication (Miller et al., 1997, 2001). Nursing unit communication systems utilize voice, phone, and staff tracking capabilities based on digital and infrared technology to enable communication between the patient and nurse and among caregivers. |
Reduce travel time and caregiver response times to call lights. Support decentralized nursing stations for maximum efficiency. Eliminate non – value-added nursing time and motion. |
|
Patient education systems |
Standardized programming is available on diseases, procedures, and self-care. These programs can be delivered via the hospital intranet or television network. |
Use patient/family education to enhance outcomes, enable early discharges, and reduce readmissions. Prepare the patient for discharge planning and self-care. Conserve nursing time for advanced, one-on-one, individualized responses to patient questions. Ensure that all patients have access to fundamental medical information as a standard of care. |
|
Lighting and temperature controls |
These should be accessible and controlled by the patient within his/her room. |
Enable patients to control their own climate and environmental comfort without depending solely upon the nurse or other caregiver. Control over environment decreases stress and promotes wellness (Ulrich,1991). |
|
Nursing Unit Design |
Elements of Workspace Design |
LEAN Principles |
|
Standardized patient rooms with acuity-adaptable headwall |
Acuity-adaptable private rooms are standardized in design, equipment, and supplies. The design provides maximum flexibility for future care needs. |
Minimize variation, enhance efficiency, and promote error reduction. Support principles of just-in-time inventory, and meet the immediate needs of caregiver and patient. Anticipate additional shifts in patient acuity and workforce shortages; potentially may reduce future design needs. |
|
Ergonomics • Noise • Seating • Flooring • Colors • Workstation furniture |
Silent paging systems; reduce or eliminate unnecessary bedside alarms; build acoustical characteristics into the environment; use full-spectrum colors found in nature; provide a variety of adequate seating choices to match an aging workforce with individual preferences and needs; anticipate a variety of emergency medical response devices; employ low-resistance carpet in the hallway or flooring with noise and stress reduction qualities;and eliminate or improve noisy carts and vibrations. |
Create a safe, pleasant working environment to retain a highly skilled, aging, and scarce workforce. Increase productivity. |
|
Positive distractions for the patient |
A positive distraction is an environmental element or situation that increases positive feelings; effectively holds attention or interest; may block or reduce worrisome thoughts; and produces desirable physiologic changes, such as decreased blood pressure (Ulrich, 1997). |
Provide scenes of nature, laughter/comedy, human contact, music. |
|
Decentralized nursing stations |
Distribute the workstations outside each patient room or set of patient rooms. |
Reduce the chaotic milieu often found in the nursing station. Eliminate steps, time, and distance. Place the nurse at the point of patient care. Improve patient safety (enhanced observation/fall reduction/reduced waits and delays). |
|
Nursing Unit Design |
Elements of Workspace Design |
LEAN Principles |
|
Learning center |
Such a center provides electronic access to hospital policies/procedures/nursing information if possible, as well as access to e-learning and reference material on nursing units. |
Improve knowledge among nursing staff, and provide immediate access to reference materials in a timely fashion to reduce errors. |
|
Staff lounge |
The staff lounge provides private space with adequate accommodations. When possible, it has a window to the outside. The lounge supports caregivers by providing an “off-stage” area for downtime. |
Reduce caregiver stress; offer caregivers privacy. |
|
Physician–nurse collaboration areas |
Private areas for consultation and collaboration are needed to promote professional interdisciplinary practice. Decentralized nursing stations can detract from staff privacy; an alternative area is needed for compliance with HIPAAb patient privacy provisions as well. |
Provide space for team-centered care. Reduce errors and improve care processes through collaboration. |
|
Supplies and equipment |
Adequate space for storage of patient equipment should be conveniently located in the core space out of the hallway. Automated supply systems should be standardized and matched against patient populations. |
|
|
Medication delivery |
Robotic, automated, or mobile carts should be conveniently distributed on the unit with adequate ratios to nursing unit size. |
Eliminate the need to stand in line to get drugs. Prevent nurse “pocket storage” from automated systems by eliminating lines for access. |
|
aThis does not apply to neonatal intensive care units, where exposure to direct sunlight has risks for the pre-term infant (Graven, 1997). bHealth Insurance Portability and Accountability Act of 1996. |
||
The role of the ergonomist is the subject of debate in the field of human factors and ergonomics. Drury (1995:66–67) argues that “there is no substitute for the ergonomist’s knowledge and understanding of both the system under study and the ergonomics literature.” Gosbee (2002:354) argues that “[human factors engineering] must become a core competency of anyone who has significant involvement in patient safety activities.” Corlett (1991:418) states that “[we must] give ergonomics away, … transfer our knowledge and methods to others who are closer to the places where changes have to be made, so that they do much of the ergonomics for themselves…. Until ergonomics is widely practiced by other than professional ergonomists, it is likely to remain something to be added on at the end.”
The committee concludes that the dissemination and application of work design knowledge and skills throughout individual HCOs needs to be achieved through multiple mechanisms, including trial and error, creation of in-house expertise, use of consultants, and various education and training mechanisms. HCOs should undertake efforts to increase the knowledge of end users—the nurses whose work is being redesigned—about work design through, for example, on-the-job coaching or continuing education programs. As the complexity of work design initiatives increases, however, there is likely to be a commensurate increased need for professional consultation. The committee makes the following recommendations:
Recommendation 6-2. HCOs should provide nursing leadership with resources that enable them to design the nursing work environment and care processes to reduce errors. These efforts must directly involve direct-care nurses throughout all phases of the work design and should concentrate on errors associated with:
-
Surveillance of patient health status.
-
Patient transfers and other patient hand-offs.
-
Complex patient care processes.
-
Non–value-added activities performed by nurses, such as locating and obtaining supplies, looking for personnel, completing redundant and unnecessary documentation, and compensating for poor communication systems.
The committee notes that “resources” should include time and financial and consultant resources, as necessary.
Recommendation 6-3. HCOs should address handwashing and medication administration among their first work design initiatives.
Recommendation 6-4. Regulators; leaders in health care; and experts in nursing, law, informatics, and related disciplines should jointly convene to identify strategies for safely reducing the burden associated with patient and work-related documentation.
REFERENCES
Aiken L, Clarke S, Sloane D, Sochalski J, Busse R, Clarke H, Giovannetti P, Hunt J, Rafferty A, Shamian J. 2001. Nurses’ reports on hospital care in five countries. Health Affairs 20(3):43–53.
Akerstedt T. 1994. Work injuries and time of day—national data. Proceedings of a Consensus Development Symposium Entitled Work Hours, Sleepiness, and Accidents. Stockholm, Sweden.
Alaska Oil Spill Commission. 1990. Spill: The Wreck of the Exxon Valdez. [Online]. Available: http://www.oilspill.state.ak.us/facts/details.html [accessed July 29, 2003].
Allan J, Englebright J. 2000. Patient-centered documentation: An effective and efficient use of clinical information systems. Journal of Nursing Administration 30(2):90–95.
Alukal G. 2003. Create a lean, mean machine. Quality Progress 36(4):29–35.
ANA (American Nurses Association). 2002. State Legislative Trends and Analysis. Washington, DC: ANA.
Anonymous. 2000. Automation can reduce errors, but don’t jump before looking, ISMP says. Healthcare Risk Management 59.
Ashby D. 1997. Medication calculation skills of the medical–surgical nurse. MEDSURG Nursing 6(2):90–94.
Babkoff H, Mikulincer M, Caspy T, Kempinski D, Sing H. 1988. The typology of performance curves during 72 hours of sleep loss. The Quarterly Journal of Experimental Psychology 324:737–756.
Baldwin D. 1998. Implementation of computerized clinical documentation. Home Health Care Management & Practice 10(2):43–51.
Ball M, Weaver C, Abbott P. 2003. Enabling technologies promise to revitalize the role of nursing in an era of patient safety. International Journal of Medical Informatics 69:29–38.
Bates D, Cullen D, Laird N, Petersen L, Small S, Servi D, Laffel G, Sweitzer B, Shea B, Hallisey R, Vander Vleit M, Nemeskal R, Leape L. 1995. Incidence of adverse drug events and potential adverse drug events: Implications for prevention. Journal of the American Medical Association 274:29–34.
Battelle Memorial Institute, JIL Information Systems. 1998. An Overview of the Scientific Literature Concerning Fatigue, Sleep and the Circadian Cycle. Prepared for the Office of the Chief Scientific and Technical Advisor for Human Factors, Federal Aviation Administration. [Online]. Available: http://www.unionepiloti.it/diparti/technico/Documenti_dt/studio_Battelle.pdf [accessed July 29, 2003].
Battles J, Keyes M. 2002. Technology and patient safety: A two-edged sword. Biomedical Instrumentation and Technology 36(2):84–88.
Bindler R, Bayne T. 1991. Medication calculation ability of registered nurses. Image: Journal of Nursing Scholarship 23(4):221–224.
Blachly B, Young H. 1998. Reducing the burden of paperwork: Modified charting by exception for medications. Journal of Gerontological Nursing 24(6):16–20.
Bobrow M. 1978. The Evolution of Nursing Space Planning for Efficient Operations. In: Redston L, ed. Hospitals and Health Care Facilities: An Architectural Record Book. New York, NY: McGraw-Hill.
Bobrow M, Thomas J. 2000. Inpatient Care Facilities. In: Kliment S, ed. Building Type Basics for Health Care Facilities . New York, NY: John Wiley and Sons.
Bowers B, Lauring C, Jacobson N. 2001. How nurses manage time and work in long term care facilities. Journal of Advanced Nursing 33:484–491.
Bridgeman T, Flores M, Rosenbluth J, Pierog J. 1997. One emergency department’s experience: Clinical algorithms and documentation. Journal of Emergency Nursing 23(4):316–325.
Brooks J. 1998. An analysis of nursing documentation as a reflection of actual nurse work. MEDSURG Nursing 7(4):189–198.
Brunt B, Gifford L, Hart D, McQueen-Goss S, Siddall D, Smith R, Weakland R. 1999. Designing interdisciplinary documentation for the continuum of care. Journal of Nursing Care Quality 14(1):1–10.
Butler M, Bender A. 1999. Intensive care unit bedside documentation systems: Realizing cost savings and quality improvements. Computers in Nursing 17(1):32–41.
Cabri J, De Witt B, Clarys J. 1988. Circadian variation in blood pressure responses to muscular exercises. Ergonomics 31:1559–1566.
California Nurses Association. 2003. Mandatory Overtime Is Detrimental to Patient Care and the Health of Nurses. [Online]. Available: http://www.calnurse.og/cna/patient/nursespeak.html [accessed June 16, 2003].
Calliari D. 1995. The relationship between a calculation test given in nursing orientation and medication errors. Journal of Continuing Education in Nursing 26(1):11–14.
Carayon P, Alvarado C, Hundt A. 2003. Center for Quality and Productivity Improvement and Department of Industrial Engineering, University of Wisconsin-Madison. Reducing Workload and Increasing Patient Safety through Work and Workspace Design. Paper commissioned by the Institute of Medicine Committee on the Work Environment for Nurses and Patient Safety
Case J, Mowry M, Welebob E. 2002. The Nursing Shortage: Can Technology Help? Oakland, CA: California Heathcare Foundation.
CDC (Centers for Disease Control and Prevention). 2003 (July 22). Hand Hygiene in Healthcare Settings. National Stakeholders Meeting on Alcohol-Based Hand-Rubs and Fire Safety in Healthcare Facilities. Executive summary. [Online]. Available: http://www.cdc.gov/handhygiene/firesafety/aha_meeting.htm [accessed September 30, 2003].
Clayton P. 2001. The state of clinical information systems, after four decades of effort. In: Clayton P. IMIA Yearbook of Medical Informatics—2001. Stuttgart, Germany: Shattauer Publishing Company. Pp. 333–337.
Clayton P, Hougaard J, Rhodes J, Narus S, Wilcox A, Wallace J, Miller S, Evans R, Hales R, Rowan B, Johnson K, Boyce J, Calder C. 2003. Improving the Nursing Environment: Reducing the Documentation Burden. Unpublished paper.
CMS (Centers for Medicare and Medicaid Services). 2002. Report to Congress: Appropriateness of Minimum Nurse Staffing Ratios in Nursing Homes—Phase II Final Report. [Online]. Available: www.cms.gov/medicaid/reports/rp1201home.asp [accessed June 25, 2002].
Cohen C, Muehl G. 1977. Human circadian rhythms in resting and exercise pulse rates. Ergonomics 20:475–479.
Cook R. 2002. Safety technology: Solutions or experiments? Nursing Economics 20(2):80–82.
Cook R, Render M, Woods D. 2000. Gaps in the continuity of care and progress on patient safety. British Medical Journal 320(7237):791–794.
Cooper J, Newbower R, Kitz R. 1984. An analysis of major errors and equipment failures in anesthesia management: Considerations for prevention and detection. Anesthesiology 60(1):34–42.
Corlett E. 1991. Some future directions for ergonomics. In: Kumashiro M, Megaw E, eds. Towards Human Work: Solutions to Problems in Occupational Health and Safety. London: Taylor & Francis.
Cox A, Groves P. 1990. Hospitals and Health-Care Facilities: A Design and Development Guide. London: Butterworth and Company, Ltd.
Dawson D, Reid K. 1997. Fatigue, alcohol, and performance impairment. Nature 388:235.
Delafosse J, Leger D, Quera-Salva M, Samson O, Adrien J. 2000. Comparative study of actigraphy and ambulatory polysomnography in the assessment of adaptation to night shift work in nurses. Revue Neurologique (Paris) 156(6-7):641–645.
Deutschendorf A. 2003. From past paradigms to future frontiers: Unique care delivery models to facilitate nursing work and quality outcomes. Journal of Nursing Administration 33(1):52–59.
Dinges D, Graeber R, Rosenkind M, Samuel A, Wegman H. 1996. Principles and Guidelines for Duty and Rest Scheduling in Commercial Aviation. NASA Technical Memorandum 110404. Moffett Field, CA: National Aeronautics and Space Administration, Ames Research Center. [Online]. Available: http://olias.arc.nasa.gov/zteam/PDF_pubs/p-g1.pdf [accessed October 4, 2003].
Dirks J. 1993. Adaptation to permanent night work: The number of consecutive work nights and motivated choice. Ergonomics 36:29–36.
Dismukes K, Young G, Sumwalt R. 1998. Cockpit interruptions and distractions: Effective management requires a careful balancing act. ASRS Directline 4–9.
Doerge J, Hagenow N. 1995. Patient-centered process of work redesign: Arizona hospital reengineers with no outside help. Health Progress 76(8):28–32.
Dornheim M. 2000. Crew distractions emerge as new safety focus. Aviation Week & Space Technology 60:153–158.
Drury C. 1995. Methods for direct observation of performance. In: Wilson J, Corlett E, eds. Evaluation of Human Work (2nd Edition). London: Taylor & Francis. Pp. 45–68.
Duchon J, Keran C, Smith T. 1994. Extended workdays in an underground mine: A work performance analysis. Human Factors 36:258–269.
Ely J, Levinson W, Elder N, Mainous A, Vinson D. 1995. Perceived causes of family physicians’ errors. Journal of Family Practice 40(4):337–344.
Fiesta J. 1993. Charting: One national standard, one form. Nursing Management 24(6):22–24.
Fletcher C. 1997. Failure mode and effects analysis: An interdisciplinary way to analyze and reduce medication errors. Journal of Nursing Administration 27(12):19–26.
Florica V, Higgins E, Iampietro P, Lategola M, Davis A. 1968. Physiological responses of man during sleep deprivation. Journal of Applied Physiology 24:169–175.
Flynn E, Barker K, Gibson J, Pearson R, Berger B, Smith L. 1999. Impact of interruptions and distractions on dispensing errors in an ambulatory care pharmacy. American Journal of Health-System Pharmacy 56(13):1319–1325.
Folkard S. 1996. Effects on performance efficiency. In: Colquhoun W, Costa G, Kolkard S, Knauth P, eds. Shiftwork: Problems and Solutions. Frankfurt am Main: Peter Lang Publishing. Pp. 65–87.
Fukuda H, Takahashi M, Airto H. 1999. Nurses’ workload associated with 16-h night shifts on the 2-shift system. I: Comparison with the 3-shift system. Psychiatry and Clinical Neurosciences 53(2):219–221.
Gallant D, Lanning K. 2001. Streamlining patient care processes through flexible room and equipment design. Critical Care Nursing Quarterly 24(3):1–20.
Gander P, McDonald J, Montgomery J, Paulin M. 1991. Adaptation of sleep and circadian rhythms to the Antarctic summer: A question of zeitgeber strength. Aviation, Space and Environmental Medicine 62:1019–1025.
GAO (U.S. General Accounting Office). 2001. Nursing Workforce: Emerging Nurse Shortages Due to Multiple Factors. GAO-01-944. Washington, DC: GAO.
Gillberg M, Kecklund G, Akerstadt T. 1994. Relations between performance and subjective ratings of sleepiness during a night awake. Sleep 17:236–241.
Gold D, Rogacz S, Bock N, Tosteson T, Baum T, Speizer F, Czeisler C. 1992. Rotating shift work, sleep, and accidents related to sleepiness in hospital nurses. American Journal of Public Health 82(7):1011–1014.
Goldberger D, Kremsdorf R. 2001. Clinical information systems: Developing a systematic planning process. Journal of Ambulatory Care Management 24(1):67–83.
Goodman P. 2001. Missing Organizational Linkages: Tools for Cross-Level Organizational Research. Thousand Oaks, CA: Sage Publications.
Gosbee J. 2002. Human factors engineering and patient safety. Quality & Safety in Health Care 11(4):352–354.
Graven, S. 1997. Pre-symposium workshop: Clinical research data illuminating the relationship between the physical environment and patient medical outcomes. Journal of Healthcare Design IX:15–20. Volume IX contains the proceedings of the Ninth Symposium of Healthcare Design, held on November 14–17, 1996, in Boston, Massachusetts. Copyright 1997 by The Center for Health Design, Inc.
Gravenstein J, Cooper J, Orkin F. 1990. Work and rest cycles in anesthesia practice. Anesthesiology 72:737–742.
Hamilton D. 1999. Design for flexibility in critical care. New Horizons 7(2):205–217.
Hamilton K. 1990. Unit 2000: Patient Beds for the Future. Bel Air, TX: Watkins, Carter, Hamilton Publications.
Hanecke K, Tiedemann S, Nachreiner F, Grzech-Sukalo H. 1998. Accident risk as a function of hour at work and time of day as determined from accident data and exposure models for the German working population. Scandinavian Journal of Work Environment Health 24(Supplement 3):43–48.
Hendrich A, Lee N. 2003a. A Time and Motion Study of Health Care Workers: Tribes of Hunters and Gatherers. Unpublished data.
Hendrich A, Lee N. 2003b. The Cost of Intra-unit Hospital Patient Transfers. Unpublished data.
Hendrich A, Lee N. 2003c. Evidence-Based Design on Nursing Workspace in Hospitals. Report commissioned by the IOM Committee on the Work Environment for Nurses and Patient Safety.
Hendrich A, Nyhuis A, Kippenbrock T, Soja M. 1995. Hospital falls: Development of a predictive model for clinical practice. Applied Nursing Research 8(3):129–139.
Hendrich A, Nyhuis A, Bender P. 2003. Validation of the Hendrich II fall risk model: A large concurrent case/control study of hospitalized patients. Applied Nursing Research 16(1):9–21.
Hendrich A, Fay J, Sorrels A. 2004 (forthcoming). Cardiac comprehensive critical care: Effects of acuity-adaptable rooms on flow of patients and delivery of care. American Journal of Critical Care 13(1).
Hyman W. 1994. Errors in the use of medical equipment. In: Bogner M, ed. Human Error in Medicine. Hillsdale, NJ: Lawrence Erlbaum Associates. Pp. 327–347.
Institute for Safe Medication Practices. 2002. “Smart” infusion pumps join CPOE and bar coding as important ways to prevent medication errors. ISMP Medication Safety Alert. [Online]. Available: www.ismp.org/MSAarticles/Smart.htm [accessed June 27, 2003].
IOM (Institute of Medicine). 2000. To Err Is Human: Building a Safer Health System. Washington, DC: National Academy Press.
IOM. 2001. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academy Press.
James P, Tatton-Brown W. 1986. Hospitals: Design and Development. New York, NY: Van Nostrand Reinhold Co.
JCAHO (Joint Commission on Accreditation of Healthcare Organizations). 2002. Health Care at the Crossroads: Strategies for Addressing the Evolving Nursing Crisis. Oakbrook Terrace, IL: JCAHO.
JCAHO. 2003. 2003 Hospital Accreditation Standards. Oakbrook Terrace, IL: Joint Commission Resources.
Jha A, Duncan B, Bates D. 2001. Fatigue, sleepiness, and medical errors. In: Shojania K, Duncan B, McDonald K, Wachter R, eds. Making Health Care Safer: A Critical Analysis of Patient Safety Practices. AHRQ Publication No. 01-E058. Rockville, MD: AHRQ.
Johnson C, Carlson R, Tucker C, Willette C. 2002. Using BCMA software to improve patient safety in Veterans Administration Medical Centers. Journal of Healthcare Information Management 16(1):46–51.
Kaushal R, Bates, D. 2001. Computerized physician order entry (CPOE) and clinical decision support systems (CDSSs). In: Shojania K, Duncan B, McDonald K, Wachter R. eds. Making Health Care Safer: A Critical Analysis of Patient Safety Practices. Rockville, MD: AHRQ. Pp. 59–69.
Kimball B, O’Neil E. 2002. Health Care’s Human Crisis: The American Nursing Shortage: The Robert Wood Johnson Foundation. [Online]. Available: www.rwjf.org/news/nursing_report.pdf [accessed October 4, 2003].
Knauth P. 1993. The design of shift systems. Ergonomics 36:29–36.
Knauth P, Landau K, Droge C, Schwitteck N, Widynski M, Rutenfranz J. 1980. Duration of sleep depending on the type of shift work. International Archives of Occupational and Environmental Health 46:167–177.
Kogi K. 1991. Job content and working time: The scope for joint change. Ergonomics 34:757–773.
Korst L, Eusebio-Angeja A, Chamorro T, Aydin C, Gregory K. 2003. Nursing documentation time during implementation of an electronic medical record. Journal of Nursing Administration 33(1):24–30.
Kovner C. 2001. The impact of staffing and organization of work on patient outcomes and health care workers in health care organizations. The Joint Commission Journal on Quality Improvement 27(9):458–468.
Krueger G. 1994. Fatigue, performance and medical error. In: Mary Sue Bogner, ed. Human Error in Medicine. Hillsdale, NJ: Lawrence Erlbaum Associates.
Kruger G. 1989. Sustained work, fatigue, sleep loss and performance. Work & Stress 3:287–298.
LaDuke S. 2001. Online nursing documentation: Finding a middle ground. Journal of Nursing Administration 31(6):283–286.
Lamond N, Dawson D. 1998. Quantifying the Performance Impairment Associated with Sustained Wakefulness. South Australia: The Centre for Sleep Research, The Queen Elizabeth Hospital. [Online]. Available: http://cf.alpha.org/internet/projects/ftdt/backgr/Daw_Lam.html [accessed July 7, 2003].
Larrabee J, Boldreghini S, Elder-Sorrells K, Turner Z, Wender R, Hart J, Lenzi P. 2001. Evaluation of documentation before and after implementation of a nursing information system in an acute care hospital. Computers in Nursing 19(2):56–65.
Lautenbach E. 2001. Practices to improve handwashing compliance. In: Shojania K, Duncan B, McDonald K, Wachter R, eds. Making Health Care Safer: A Critical Analysis of Patient Safety Practices. Rockville, MD: AHRQ. Pp. 119–126.
Lavie P, Chillag N, Epstein R, Tzischinsky O, Givon R, Fuschs S, Shahal B. 1989. Sleep disturbance in shift workers: A marker for maladaptation syndrome. Work Stress 3:33–40.
Lawler III E. 1986. High Involvement Management: Participative Strategies for Improving Organizational Performance. San Francisco, CA: Jossey-Bass.
Leape L, Bates D, Cullen D, Cooper J, Demonaco H, Gallivan T, Hallisey R, Ives J, Laird N, Laffel G, Nemeskal R, Petersen L, Porter K, Servi D, Shea B, Small S, Sweitzer B, Thompson B, Vander Vleit M. 1995. Systems analysis of adverse drug events. Journal of the American Medical Association 274(1):35–43.
Lee K. 1992. Self-reported sleep disturbances in employed women. Sleep 15:493–498.
Linde L, Bergstrom M. 1992. The effect of one night without sleep on problem-solving and immediate recall. Psychological Research 54:127–136.
Linden L, English K. 1994. Adjusting the cost-quality equation: Utilizing work sampling and time study data to redesign clinical practice. Journal of Nursing Care Quality 8(3):34–42.
Luna T, French J, Mitcha J. 1997. A study of USAF air traffic controller shiftwork: Sleep, fatigue, activity, and mood analyses. Aviation, Space and Environmental Medicine 68:18–23.
Macduffie J, Pil F. 1996. “High involvement” work practices and human resource policies: An international overview. In: Kochan T, Lansbury R, Macduffie J, eds. Evolving Employment Practices in the World Auto Industry. New York, NY: Oxford University Press.
McCartt A, Rohrbaugh J, Hammer M. 2000. Factors associated with falling asleep at the wheel among long-distance truck drivers. Accident Analysis and Prevention 32:493–504.
Miller E, Deets C, Miller R. 1997. Nurse call systems: Impact on nursing performance. Journal of Nursing Care Quality 11(3):36–43.
Miller E, Deets C, Miller R. 2001. Nurse call and the work environment: Lessons learned. Journal of Nursing Care Quality 15(3):7–15.
Mills M, Arnold B, Wood C. 1983. Core 12: A controlled study of the impact of 12-hour scheduling. Nursing Research 32:356–361.
Mitler M, Carskadon M, Czeisler C, Dement W, Dinges D, Graeber R. 1988. Catastrophes, sleep, and public policy: Consensus report. Sleep 11:100–109.
Mitler M, Miller J, Lipsitz J, Walsh J, Wylie C. 1997. The sleep of long-haul truckers. The New England Journal of Medicine 337:755–761.
Monk T. 1990. Shiftworker performance. In: Scott A, ed. Occupational Medicine State of the Art Reviews. Volume 5. Philadelphia, PA: Hanley and Belfus, Inc. Pp. 183–198.
Monk T, Folkard S, Wedderburn A. 1996. Maintaining safety and high performance on shiftwork. Applied Ergonomics 27:17–23.
Morrison W, Haas E, Shaffner D, Garrett E. 2003. Noise, stress, and annoyance in a pediatric intensive care unit. Critical Care Medicine 31(1):113–119.
Mosher C, Rademacher K, Day G, Fanelli D. 1996. Documenting for patient-focused care. Nursing Economics 14(4 ):218–223.
Mullaney D, Kripke D, Fleck P, Johnson L. 1983. Sleep loss and nap effects on sustained continuous performance. Psychophysiology 20:643–651.
Murphy J, Beglinger J, Johnson B. 1988. Charting by exception: Meeting the challenge of cost containment. Nursing Management 19(2):56–72.
Murray M. 2001. Automated medication dispensing devices. In: Shojania K, Duncan B, McDonald K, Wachter R, eds. Making Health Care Safer: A Critical Analysis of Patient Safety Practices. Rockville, MD: AHRQ. Pp. 111–117.
Murray M, Shojania K. 2001. Unit-dose drug distribution systems. In: Shojania K, Duncan B, McDonald K, Wachter R, eds. Making Health Care Safer: A Critical Analysis of Patient Safety Practices. Rockville, MD: AHRQ. Pp. 101–109.
Nahm R, Poston I. 2000. Measurement of the effects of an integrated, point-of-care computer system on quality of nursing documentation and patient satisfaction. Computers in Nursing 18(5):220–229.
National Transportation Safety Board. 1994. A Review of Flight Crew-Involved Major Accidents of U.S. Air Carriers, 1978 Through 1990. NTSB #SS-94-01/PB94-917001. Washington, DC: National Transportation Safety Board.
Noro K, Imada A. 1991. Participatory Ergonomics. London: Taylor and Francis.
Office of Technology Assessment, U.S. Congress. 1991. Biological Rhythms: Implications for the Worker. OTA-BA-463. Washington, DC: U.S. Government Printing Office.
Olson L, Ambrogetti A. 1998. Working harder: Working dangerously? Fatigue and performance in hospitals. Medical Journal of Australia 168(12):614–616.
O’Shea E. 1999. Factors contributing to medication errors: A literature review. Journal of Clinical Nursing 8(5):496–505.
Pabst M, Scherubel J, Minnick A. 1996. The impact of computerized documentation on nurses’ use of time. Computers in Nursing 14(1):25–30.
Pape T. 2001. Searching for the final answer: Factors contributing to medication administration errors. Journal of Continuing Education in Nursing 32(4):152–160, 190–191.
Pape T. 2003. Applying airline safety practices to medication administration. MEDSURG Nursing 12(2):77–93.
Park K. 1997. Human error. In: Salvendy G, ed. Handbook of Human Factors and Ergonomics. New York, NY: John Wiley & Son, Inc. Pp. 150–170.
Peck M, Nelson N, Buxton R, Bushnell J, Dahle M, Rosebrock B, Ashton C. 1997. LDS Hospital: A facility of Intermountain Health Care, Salt Lake City, UT. Nursing Administration Quarterly 21(3):29–49.
Pedersen A. 1997. A data-driven approach to work redesign in nursing units. Journal of Nursing Administration 27(4):49–54.
Pepper G. 1995. Errors in drug administration by nurses. American Journal of Health-System Pharmacy 52:390–395.
Prescott P, Phillips C, Ryan J, Thompson K. 1991. Changing how nurses spend their time. Image 23(1):23–28.
Reason J. 1990. Human Error. Cambridge, UK: Cambridge University Press.
Rich M. 2002 (November 27). Healthy hospital designs: Improving decor and layout can have impact on care; fewer fractures and infections. The Wall Street Journal. Pp. B-1, B-4.
Roberts K, Bea R. 2001. Must accidents happen? Lessons from high-reliability organizations. Academy of Management Executive 15(3):70–78.
Rogers A. 2002. Work Hour Regulation in Safety-Sensitive Industries. Paper commissioned by the Institute of Medicine Committee on the Work Environment for Nurses and Patient Safety. Presented to the Committee on November 19, 2002.
Rosa R. 1995. Extended workshifts and excessive fatigue. Journal of Sleep Research 4(Supplement 2):51–56.
Rosa R. 2001. Examining work schedules for fatigue: Its not just hours of work. In: Hancock P, Desmond P, eds. Stress, Workload, and Fatigue. Mahwah, NJ: Lawrence Earlbaum Associates. Pp. 513–528.
Rosa R, Colligan M. 1988. Long workdays vs. restdays: Assessing fatigue and alertness with a portable performance battery. Human Factors 30:305–317.
Rosenkind M, Gander P, Connell L, Co E. 1999. Crew Factors in Flight Operations X: Alertness Management in Flight Operations. NASA/FAA.
Scharf L. 1997. Revising nursing documentation to meet patient outcomes. Nursing Management 28(4):38.
Scherubel J, Minnick A. 1994. Implementation of work sampling methodology. Nursing Research 43(2):120–123.
Schuster M. 1985. The impact of overtime work on industrial accident rates. Industrial Relations 24(2):234–246.
Seago J. 2001. Nurse staffing, models of care delivery, and interventions. In: Shojania K, Duncan B, McDonald K, Wachter R. eds. Making Health Care Safer: A Critical Analysis of Patient Safety Practices. Evidence Report/Technology Assessment No. 43. Rockville, MD: AHRQ.
Senders J. 1994. Medical devices, medical errors, and medical accidents. In: Bogner M, ed. Human Error in Medicine. Hillsdale, NJ: Lawrence Erlbaum Associates.
Smeltzer C, Hines P, Beebe H, Keller B. 1996. Streamlining documentation: An opportunity to reduce costs and increase nurse clinicians’ time with patients. Journal of Nursing Care Quality 10(4):66–77.
Smith B. 2003. Lean and six sigma: A one-two punch. Quality Progress 36(4).
Smith D, Rogers S, Hood E, Phillips D. 1998. Overtime reduction with the press of a button: An unexpected outcome of computerized documentation. Nursing Case Management 3(6):266–270.
Smith J, Crawford L. 2002. Report of Findings from the Practice and Professional Issues Survey—Spring 2001. NCSBN Research Brief 2. Chicago, IL: National Council of State Boards of Nursing, Inc.
Smith L, Folkard S, Poole C. 1994. Increased injuries on the night shift. Lancet 344:1137–1139.
Spath P. 2000. Reducing errors through work system improvements. In: Spath P, ed. Error Reduction in Health Care. San Francisco, CA: Jossey Bass. Pp. 199–234.
Spear S, Bowen H. 1999. Decoding the DNA of the Toyota Production System. Harvard Business Review 77(5):97–106.
Spratley E, Johnson A, Sochalski J, Fritz M, Spencer W. 2000. The Registered Nurse Population: Findings from the National Sample Survey of Registered Nurses: DHHS, HRSA. [Online]. Available: http://bhpr.hrsa.gov/healthworkforce/reports/rnsurvey/rnss1.htm [accessed October 4, 2003].
Stephens S, Mason S. 1999. Putting it together: A clinical documentation system that works. Nursing Management 30(3):43–47.
Takahashi M, Arito H, Fukuda H. 1999. Nurses’ workload associated with 16-h night shifts. II: Effects of a nap taken during the shifts. Psychiatry and Clinical Neurosciences 53(2):223–225.
The Center for Health Design. 2003a. What Is the Pebble Project? [Online]. Available: http:www.pebbleproject.org/pebble_faq.php [accessed July 5, 2003].
The Center for Health Design. 2003b. Pebble Project: Selected Preliminary Data. [Online]. Available: http://www.pebbleproject.org/pebble_data.php [accessed July 5, 2003].
Topf M. 2000. Hospital noise pollution: An environmental stress model to guide research and clinical interventions. Journal of Advanced Nursing 31(3):520–528.
Trossman S. 2001. The documentation dilemma: Nurses poised to address paperwork burden. The American Nurse 33(5):1, 9, 18.
Tucker A, Edmondson A. 2002. Managing routine exceptions: A model of nurse problem solving behavior. Advances in Health Care Management 3:87–113.
Tucker A, Edmondson A. 2003. Why hospitals don’t learn from failures: Organizational and psychological dynamics that inhibit system change. California Management Review 45(2):1–18.
Tucker P, Barton J, Folkard S. 1996. Comparison of eight and 12 hour shifts: Impacts on health, wellbeing, and alertness during the shift. Occupational and Environmental Medicine 53:767–772.
Ugrovics A, Wright J. 1990. 12-hour shifts: Does fatigue undermine ICU nursing judgments? Nursing Management 21:64A–64G.
Ulrich R. 1991. Effects of interior design on wellness: Theory and recent scientific research. Journal of Health Care Interior Design 3:97–109.
Ulrich R. 1997. Pre-symposium workshop: A theory of supportive design for healthcare facilities. Journal of Healthcare Design Volume IX:3-7. Volume IX contains the proceedings of the Ninth Symposium of Healthcare Design, held on November 14–17, 1996, in Boston, Massachusetts. Copyright 1997 by The Center for Health Design, Inc.
Upenieks V. 1998. Work sampling: Assessing nursing efficiency. Nursing Management 29(4):27–29.
Urden L, Roode J. 1997. Work sampling: A decision-making tool for determining resources and work redesign. Journal of Nursing Administration 27(9):34–41.
Van-Griever A, Meijman T. 1987. The impact of abnormal hours of work on various modes of information processing: A process model on human costs of performance. Ergonomics 30:1287–1299.
Wagenaar A, O’Malley P, LaFond C. 2001. Lowered legal blood alcohol limits for young drivers: Effects on drinking, driving, and driving-after-drinking behaviors in 30 states. American Journal of Public Health 91(5):801–804.
Wakefield B, Wakefield D, Uden-Holman T, Blegen M. 1998. Nurses’ perceptions of why medication administration errors occur. MEDSURG Nursing 7(1):39–44.
Wald H, Shojania K. 2001. Root cause analysis. In: Shojania K, Duncan B, McDonald K, Wachter R, eds. Making Health Care Safer: A Critical Analysis of Patient Safety Practices. Evidence Report/Technology Assessment No.43. AHRQ Publication Number: 01-E058. Rockville, MD: AHRQ.
Walker K, Prophet C. 1997. Nursing documentation in the computer-based patient record. Studies in Health Technology & Informatics 46:313–317.
Wallace M, Greenwood K. 1995. Twelve-hour shifts [editorial]. Work and Stress 9:105–108.
Walsh J, Tepas D, Moss P. 1981. The EEG sleep of night and rotating shift workers. In: Johnson L, Tepas D, Colquhon W, Colligan M, eds. Biological Rhythms, Sleep, and Shift Work. New York, NY: Spectrum. Pp. 371–381.
Walsh-Sukys A, Reitenbach A, Hudson-Barr D, DePompei P. 2001. Reducing light and sound in the neonatal intensive care unit: An evaluation of patient safety, staff satisfaction and costs. Journal of Perinatology 21:230–235.
Walters J. 1992. Nurses’ perceptions of reportable medication errors and factors that contribute to their occurrence. Applied Nursing Research 5(2):86–88.
Weiss D, Hailstone S. 1993. Hospital saves with bedside point-of-care system. Computers in Healthcare 14(1):28–32.
White C, Hemby C. 1997. Automating the bedside. Healthcare Informatics 14(2):68–70.
Williamson A, Gower C, Clarke B. 1994. Changing the hours of shiftwork: A comparison on 8 and 12-hour shift rosters in a group of computer operators. Ergonomics 37:287–298.
Wilson J, Haines H. 1997. Participatory ergonomics. In: Salvendy G, ed. Handbook of Human Factors and Ergonomics. New York, NY: John Wiley and Sons. Pp. 490–513.
Wojtczak-Jaroszowa J, Banaszkiewicz A. 1974. Physical work capacity during the day and at night. Ergonomics 17:193–198.
Wroblewski M, Werrbach K. 1999. Nurses gain more time with patients. Nursing Management 30(9):35.
Wylie C, Schultz T, Miller J, Mitler M, Mackie R. 1996. Commercial Motor Vehicle Driver Fatigue and Alertness Study. FHWA Report number: FHWA-MC-97-001, TC Report Number TP12876E. Montreal, Canada: Transportation Development Center. Prepared for the Federal Highway Administration, U.S. Department of Transportation; Trucking Research Institute, American Trucking Associations Foundation; and the Transportation Development Centre, Safety and Security, Transport Canada.
Young D. 2002. Health care industry informs FDA of bar-code needs. American Journal of Health Systems Pharmacists 59:1592, 1594, 1600.
Zerwekh J, Thibodeaux R, Plesko R. 2000. Chart it once: Innovation in public health documentation. Journal of Community Health Nursing 17(2):75–83.




























































