1
Introduction
INSTITUTIONAL AND POLICY-LEVEL STRATEGIES FOR INCREASING THE DIVERSITY OF THE U.S. HEALTH-CARE WORKFORCE
The United States is rapidly transforming into one of the most racially and ethnically diverse nations in the world. Groups commonly referred to as minorities—including Asian Americans, Pacific Islanders, African Americans, Hispanics, American Indians, and Alaska Natives—are the fastest-growing segments of the population and are emerging as the nation’s majority. Since 2000, for example, Hispanics accounted for 3.5 million—or over one-half—of the population increase of 6.9 million individuals in the United States. The number of Asian Americans grew at a larger proportion (9 percent) than any other racial or ethnic group during this same time period. And in at least three states (California, Hawaii, and New Mexico) and the District of Columbia, these groups constitute a majority of the population (U.S. Bureau of the Census, 2003).
Despite the rapid growth of racial and ethnic minority groups in the United States, their representation among the nation’s health professionals has grown only modestly at best over the past 25 years, producing a trend in which the proportion of minorities in the population outstrips their representation among health professionals by several fold.1 Hispanics, for
example, comprise over 12 percent of the U.S population, but only 2 percent of the registered nurse population, 3.4 percent of psychologists, and 3.5 percent of physicians. Similarly, one in eight individuals in the United States is African American, yet less than one in twenty dentists or physicians is African American.
These stark figures, in part, have prompted many major health professions organizations and health professions educational institutions (HPEIs) to develop initiatives to increase the proportion of underrepresented minorities (URM)2 in health professions fields. These efforts, however, have met with limited success. To a great extent, efforts to diversify health professions fields have been hampered by gross inequalities in educational opportunity for students of minority racial and ethnic groups. Primary and secondary education for URM students is, on average, far below the quality of education for non-URM students. Proportionately fewer URM students enter higher education than their white or Asian American peers, and an even smaller percentage of these go on to graduate (post-baccalaureate) study. The “supply” of URM students who are well-prepared for higher education and advanced study in health professions fields has therefore suffered.
Equally important, however, are efforts to reduce policy-level barriers to URM participation in health professions training, and to increase the institutional “demand” for URM students. For example, several events—including public referenda (i.e., Proposition 209 in California and Initiative 200 in Washington state), judicial decisions (e.g., the Fifth District Court of Appeals finding in Hopwood v. Texas), and lawsuits challenging affirmative action policies in 1995, 1996, and 1997—forced many higher education institutions to abandon the use of race and ethnicity as factors in admissions decisions (in some cases temporarily, in light of the June 2003 Supreme Court decision in Grutter v. Bollinger, in which white plaintiffs sued—unsuccessfully—in an effort to halt the University of Michigan’s admissions policies that consider applicants’ race and ethnicity as one of
|
|
providers are less capable than minorities of providing high-quality care to these populations. Rather—as will be discussed later in this chapter and throughout the report—greater racial and ethnic diversity in health professions may offer broad benefits to help improve healthcare access for minorities and improve the cultural competency of all health-care providers and the health systems in which they work. |
many factors in the admissions process3), and to curtail race- and ethnicity-based financial aid.
Given these problems—an increasing need for minority health professionals, policy challenges to affirmative action, and little progress toward enhancing the numbers of URM students prepared to enter health professions careers—the W.K. Kellogg Foundation requested a study by the Institute of Medicine to assess institutional and policy-level strategies for achieving greater diversity among health-care professionals. Institutional and policy-level strategies are defined as specific policies or programs of health professions schools, associations, accreditation bodies, health-care organizations/systems, or state and federal governments, designed to increase access to health professions careers among underrepresented racial and ethnic minority groups, as a means of increasing the likelihood that “pipeline” efforts4 to increase diversity will succeed. Specifically, the IOM was asked to:
-
assess and describe potential benefits of greater racial and ethnic diversity among health professionals;
-
assess institutional and policy-level strategies that may increase diversity within the health professions, including:
-
modifying graduate health professions training programs’ admissions practices;
-
increasing the emphasis in health professions program accreditation on enhancing diversity in training programs and developing cross-cultural skills and competencies of health professions trainees;
-
improving the campus “climate” for diversity, including efforts to recruit and support URM students and faculty and facilitate learning within a context of diversity;
-
modifying the financing and funding of health professions training in order to reduce financial barriers to health professions training among minority and lower-income students; and
-
|
BOX 1-1
|
-
considering the application of community benefit principles to improve the accountability of nonprofit, tax exempt institutions (e.g., medical schools and teaching hospitals) to the diverse racial and ethnic communities they serve; and
-
identify mechanisms to garner broad support among health professions leaders, community members, and other key stakeholders to implement these strategies.
WHY EXAMINE INSTITUTIONAL AND POLICY-LEVEL STRATEGIES FOR INCREASING DIVERSITY IN HEALTH PROFESSIONS?
Historically, the efforts of HPEIs and professional associations to increase the presence of URM students in health professions careers have focused on enhancing students’ preparation to pursue these careers. Appro-
priately, many of these efforts have focused on improving URM students’ math and science education, particularly at the primary and secondary school levels, “bridging” K-12 training with undergraduate pre-health curricula and graduate training, and other academic and social supports. These programs have achieved some notable successes in a range of health disciplines. The Robert Wood Johnson Foundation-supported Minority Medical Education Program, for example, a 6-week summer intensive medical school preparatory program, has assisted 63 percent of its graduates to gain admission into medical school (Cantor et al., 1998).
Institutional and policy-level strategies for increasing diversity in health professions, however, have been relatively understudied. This lack of emphasis may lead to a void of strategies should future policy changes erode efforts to increase diversity (e.g., despite the U.S. Supreme Court decision in the Grutter case reaffirming the use of race/ethnicity in admissions decisions, some opponents of this decision plan to establish ballot initiatives in several states and localities to prohibit higher education institutions from adopting or continuing “race-conscious” admissions policies). As will be discussed in a later chapter (see “Reconceptualizing Admissions Policies and Practices”), “race-neutral” admissions policies, as have been practiced by some states over the past few years, have profoundly changed the land-scape for diversity and have adversely affected health professions’ efforts to increase minority representation in training programs. Failure to address these changes may therefore undercut some of the significant gains achieved by pipeline enhancement programs.
This focus is not to diminish the importance of pipeline development efforts. Rather, these strategies should be viewed as complementary. Strategies at the institutional and policy level, in conjunction with pipeline efforts, may have reciprocal effects; for example, the successful development and implementation of institutional and policy-level strategies to increase diversity in health professions may increase the demand for expanded emphasis and investment in pipeline enhancement strategies.
WHICH RACIAL AND ETHNIC GROUPS AND HEALTH PROFESSIONS ARE EXAMINED?
For purposes of this report, the study committee defines URMs as those racial and ethnic groups that are underrepresented in the heath professions relative to their numbers in the general population. This definition allows individual institutions to define which populations are underrepresented in its area of interest. It is also consistent with the definition of underrepresented minorities recently adopted by the Association of American Medical Colleges (AAMC). Previously, AAMC’s definition was limited to historically disadvantaged groups (i.e., African Americans, mainland Puerto
Ricans, and Native Americans, including American Indians, Alaska Natives, and Native Hawaiians). The new AAMC definition takes into account the fact that many other groups, such as subpopulations of Asian Americans, Pacific Islanders, and Latinos, are also poorly represented among health professionals, and many in these communities face barriers to accessing appropriate health care.
While the study committee defines URMs broadly, it should be noted that the racial and ethnic groups identified in AAMC’s previous definition of URM groups (e.g., African Americans, some Hispanic/Latino groups, American Indians) are historically underrepresented and face long-standing barriers to greater inclusion among health professionals—including persistent discrimination, educational inequality, and few role models for students of these racial and ethnic groups. The persistent underrepresentation of these groups among health professionals suggests that a sustained emphasis on increasing access to health professions careers among historically underrepresented populations is critically important.
The study committee recognizes that a broad range of health professionals contribute invaluably to the health-care enterprise. These disciplines—including dental hygienists, pharmacists, allied health professionals, physician assistants, nutritionists, occupational therapists, and clinical social workers, among many others—are critically important to ensuring that America’s health-care systems provide the best quality health care, health promotion, and disease prevention services. This study, however, will focus on medicine, nursing, dentistry, and professional psychology. This is not to suggest that diversity is unimportant or has already been achieved in other health professions. Rather, this study is limited in its scope because a comprehensive analysis of all health-related fields is not feasible given the time frame of the current study. Over 15 million Americans work in over two-dozen health-care and health-related occupations and an even greater array of specialties and subspecialties (Matherlee, this volume), making the task of assessing health workforce trends daunting. In addition, medicine, nursing, dentistry, and professional psychology are among the largest health professions, and the availability and concentration of diverse professionals in these fields will therefore have significant implications for health service delivery. Furthermore, more complete data are available from these fields to evaluate minority participation and diversity efforts. It is the study committee’s expectation that strategies adopted to increase diversity in these fields may be applicable, in some cases, to other health professions.
WHY IS RACIAL AND ETHNIC DIVERSITY IMPORTANT IN HEALTH PROFESSIONS FIELDS?
The U.S. Supreme Court’s review of the University of Michigan admissions lawsuits prompted an avalanche of amicus brief filings from both proponents and opponents of affirmative action and the use of race and ethnicity in university admissions processes. Many of these arguments have been summarized elsewhere, particularly by the plaintiffs’ and defendants’ respective legal counsel (see especially amicus brief filings at the University of Michigan Internet website http://www.umich.edu/~urel/admissions/legal). The weight of scientific evidence, however, supports the necessity of ensuring that health professionals reflect the diversity of the U.S. population. This evidence (summarized below) demonstrates that greater diversity among health professionals is associated with improved access to care for racial and ethnic minority patients, greater patient choice and satisfaction, and better patient–clinician communication. In higher education settings, greater diversity is associated with improved student learning and community participation. Indirectly, evidence suggests that greater diversity can improve the cultural competence5 of health professionals and health systems, and that such improvements may be associated with better health-care outcomes. In addition, greater diversity among health professionals has the potential to improve the clinical research enterprise and to lead to new developments and improvements in health care and how care is delivered.
Racial and Ethnic Diversity Among Health Professionals and Access to Health Care for Minority Patients
Racial and ethnic minority health-care clinicians are significantly more likely than their white peers to serve minority and medically underserved communities, thereby helping to improve problems of limited minority access to care. Several studies document this trend across a range of health professions, although the bulk of this research has focused on the practice patterns of physicians.
Turner and Turner (1996), for example, studied the practice characteristics of psychological service providers, using a random sample of psychologists listing the National Register of Health Service Providers. Racial
and ethnic minority psychologists treated more than twice the proportion of racial and ethnic minority patients than nonminority psychologists (24.0 percent vs. 11.7 percent, respectively), and those psychologists who utilized cognitive/behavioral theoretical orientations saw a larger percentage of minority patients than psychologists who used psychoanalytic or other theoretical orientations. These findings are especially important in light of consistent findings that racial and ethnic minority patients underutilize mental health services (U.S. Surgeon General, 2001).
Moy and Bartman (1995), in a nationwide survey of households, found that minority patients were more than four times more likely than white patients to receive health care from nonwhite physicians. Medically indigent patients were also between 1.4 and 2.6 times more likely to receive care from minority physicians than were more affluent patients. In addition, minority physicians tended to see patients who were sicker than the patients seen by their white peers. Minority physicians’ patients were more likely to report being in poor health, with more acute complaints, more chronic conditions, and greater functional limitations. These findings held true even after controlling for physician gender, specialization, workplace, and geographic location.
Relative to nonminority communities, minority neighborhoods tend to face shortages of physicians, yet physicians of color are disproportionately more likely to serve in these communities. Komaromy et al. (1996), in a survey of over 1,000 physicians in California, found that African American and Hispanic physicians were five and two times more likely, respectively, than their white peers to practice in communities with high proportions of African American and Hispanic residents. Over half of the patients seen by African American and Hispanic physicians, on average, were members of these clinicians’ racial or ethnic group. Hispanic and black physicians tended to practice in areas with fewer primary care physicians per capita, but even after adjustment for the proportion of minority residents in the communities studied, African American and Hispanic physicians were more likely to care for African American and Hispanic patients, respectively. Similarly, Cantor et al. (1996) found that minority and women physicians, as well as those from lower socioeconomic backgrounds, were disproportionately more likely to serve minority, low-income, and Medicaid populations, even after adjustment for physician specialty, practice setting, and practice location.
Racial and ethnic minority dentists are also more likely than their white peers to practice in racial and ethnic minority communities. Solomon, Williams, and Sinkford (2001), in a study of African American and white dentists in Texas, found that a larger percentage of African American dentists practiced in communities with a high residential African American population than white dentists. African American dentists were also found
to be more likely to practice in communities characterized by lower levels of education and income than white dentists. Similarly, Mertz and Grumbach (2001), in an assessment of the availability of dental services in California, found that approximately one in five California communities—disproportionately minority, low-income, and rural—have a shortage of dentists and that minority dentists were more likely to practice in minority communities.
Diversity and Minority Patient Choice and Satisfaction
Minority patients who have a choice are more likely to select clinicians of their own racial or ethnic background. Lopez, Lopez, and Fong (1991), for example, in a study of Mexican-American college students, found that these students expressed a clear preference for ethnically similar mental health counselors or psychotherapists. These findings held among both men and women and among those who had and had not sought counseling. Similarly, Bichsel and Mallinckrodt (2001) surveyed a sample of American Indian women living in the Warm Spring (Oregon) Reservation regarding preferences for mental health counseling and found that respondents expressed preferences for female, ethnically similar counselors who understand and are sensitive to the respondents’ culture.
Saha et al. (2000) investigated whether minority patients tend to see physicians of their own race because of convenience (e.g., location) or as a matter of choice. Using data from a national survey of heath-care consumers, the authors found that African American and Hispanic patients who had a choice of clinician were more likely to choose a physician of their own race or ethnicity. Among Hispanic patients, over 40 percent responded that the physician’s ability to speak the patient’s language was a significant consideration in choosing a physician. These associations remained even after controlling for the physician’s office location (e.g., location in a predominantly minority neighborhood).
In light of these findings, it is not surprising that racial and ethnic minority patients are generally more satisfied with the care that they receive from minority physicians. Saha et al. (1999), for example, found that African American patients who receive care from physicians of the same race were more likely than African Americans with nonminority clinicians to rate their physicians as excellent in providing health care, in treating them with respect, in explaining their medical problems, in listening to their concerns, and in being accessible. In addition, the investigators found that although Hispanic patients who received care from Hispanic physicians did not rate their doctors as significantly better than Hispanic patients with non-Hispanic health-care clinicians, patients with an ethnically concordant provider were more likely to be satisfied with their overall health care.
Similarly, Cooper-Patrick and her colleagues (1999) found that minor-
ity patients’ ratings of the quality of their health care were generally higher in racially and ethnically concordant than racially and ethnically discordant settings. Using a measure of physicians’ participatory decision-making style, Cooper-Patrick surveyed over 1,800 adults who were seen in 1 of 32 primary care settings by physicians who were either African American (25 percent of the physician sample), white (56 percent), Asian American, (15 percent), or Latino (3 percent). Overall, African American patients rated their visits as significantly less participatory than whites, after adjusting for patient age, gender, education, marital status, health status, and length of the patient–physician relationship. Patients in race- and ethnic-concordant relationships, however, rated their visits as significantly more participatory than patients in race- and ethnic-discordant relationships. In addition, Cooper and Roter have found, through independent ratings of videotaped clinical encounters, that physician visits by African American patients were longer, were characterized by less physician dominance of the discussion, and were more patient-centered when the physician was African American than when the physician was white (Cooper and Roter, 2003).
Similarly, LaVeist and Nuru-Jeter (2002) examined predictors of racial concordance between patient and clinician and the effect of race concordance on satisfaction among a sample of white, African American, and Hispanic patients. Among all racial and ethnic groups, patients who reported having at least some choice in selecting a physician were more likely to have a race- or ethnic-concordant physician. Having a race-concordant physician was also associated with higher income for African Americans and not speaking English as a primary language among Hispanics. After adjusting for patients’ age, sex, marital status, income, health insurance status, and whether the respondent reported having a choice in physician, African American patients in race-concordant relationships were found to report higher satisfaction than those African Americans in race-discordant relationships. Furthermore, Hispanic patients in ethnic-concordant relationships reported greater satisfaction than patients from other racial and ethnic groups in similarly concordant relationships.
Diversity and Quality of Health Care for Minority Populations
Racial and ethnic minorities tend to receive a lower quality of health care than nonminorities. Much of this disparity may be explained by the overrepresentation of some minority groups among the uninsured, given that uninsured and underinsured individuals face greater difficulties in accessing care and are less likely to receive needed services. Yet a large body of research demonstrates that even when insured at the same levels as whites, minority patients receive fewer clinical services and receive a lower
quality of care (Institute of Medicine, 2003a). This disparity is apparent across a range of disease areas (e.g., diabetes, cancer, HIV/AIDS) and clinical services, and in a range of clinical settings (e.g., teaching and non-teaching hospitals, public and private clinics). At least some of these disparities may result from aspects of the clinical encounter and attitudes, both conscious and unconscious, of health-care clinicians (Institute of Medicine, 2003a), raising the question of whether greater diversity among health-care professionals may help to mitigate health-care disparities.
While no direct link has been established as yet between diversity among health-care clinicians and health outcomes for patients, research indicates that health-care processes and outcomes are influenced by cultural and linguistic barriers that minority clinicians are sometimes able to address. Perez-Stable, Napoles-Springer, and Miramontes (1997), for example, assessed the effects of ethnicity and language concordance between patients and their physicians on health outcomes, use of health services, and clinical outcomes among a sample of Spanish-speaking and non-Spanish-speaking Hispanic and non-Hispanic patients with hypertension or diabetes. Of the 74 Spanish-speaking Latinos, 60 percent were treated by clinicians who spoke Spanish, while 40 percent were treated by non-Spanish-speaking clinicians. After controlling for patient age, gender, education, number of medical problems, and number of prescribed medications, the authors found that having a language-concordant physician was associated with better patient self-reported physical functioning, psychological well-being, health perceptions, and lower pain.
In addition, as noted above, some research indicates that minority physicians display better process-of-care behaviors with minority patients than nonminority clinicians (Cooper-Patrick et al., 1999). Hispanic patients display better satisfaction and adherence to treatment plans when their physician not only speaks Spanish, but also shares the same cultural background (Perez-Stable et al., 1997). These “intermediate” outcomes may affect patients’ health care outcomes, in that patient satisfaction is associated with greater patient compliance with treatment regimens, participation in treatment decisions, and use of preventive care services (Betancourt et al., 2002).
Diversity and Quality of Training for All Health Professionals
Racial and ethnic minority patients, when given a choice, tend to choose health-care clinicians from similar backgrounds, as noted above. But because the proportion of racial and ethnic minority health-care clinicians is low relative to the proportion of racial and ethnic minorities in the general population (see below), it is clear that all health-care professionals must
develop the skills and competencies to serve diverse patient populations. Diversity in health professions training settings may therefore assist in efforts to improve the cross-cultural training and cultural competencies of all trainees. Students from diverse background interacting with each other in training settings may help to challenge assumptions and broaden students’ perspectives regarding racial, ethnic, and cultural differences (Whitla et al., 2003; Cohen, 2003). Whitla and colleagues (2003), for example, in a survey of medical school graduates’ attitudes regarding diversity in medical education, found that students reported experiencing greater levels of diversity in medical school than in their prior educational experiences, as the percentage of students reporting contact with other groups increased from 50 percent prior to college to 85 percent in medical school. Overwhelmingly, these students viewed diversity among their medical student peers as a positive; 86 percent thought that classroom diversity enhanced discussion and was more likely to foster serious discussions of alternate viewpoints. Over three-quarters of the students surveyed found that diversity helped them to rethink their viewpoints when racial and ethnic conflicts occurred, and the same percentage felt that diversity provided them with a greater understanding of medical conditions and treatments. The pattern of responses did not differ by respondents’ racial or ethnic group (Whitla et al., 2003).
In addition, diversity among students in training settings may enrich classroom discussions and spur changes in curriculums to address students’ cross-cultural education needs. There is growing evidence—primarily from studies of college students’ undergraduate experiences—that student diversity is associated with greater gains in students’ learning and community involvement (e.g., Gurin et al., 2002; Antonio et al., in press). Gurin and colleagues, for example, utilized data from longitudinal surveys of undergraduate students to assess whether students’ diversity experiences as undergraduates were related to their “learning outcomes” (defined as the use of active thinking, intellectual engagement and motivation, and academic skills) and “democracy outcomes” (i.e., citizenship engagement, belief in the compatibility of group differences and democracy, the ability to take the perspective of others, and cultural awareness and engagement). The investigators found that diversity experiences were significantly related to learning outcomes after graduation, even after adjusting for students’ academic and socioeconomic background (i.e., gender, SAT scores, high school grades, parents’ educational level, racial composition of high school and neighborhood growing up), institutional characteristics, and initial (pretest) scores on learning outcome measures. Informal interactions across racial and ethnic lines were especially significant for all racial/ethnic groups in predicting intellectual engagement and academic skills. Similarly, diver-
sity experiences were found to significantly predict students’ democracy outcomes, even after adjustment for students’ prior academic and socioeconomic background and pre-college racial exposure, as well as measures of democracy orientation upon initial assessment. For all racial groups, informal interactions across racial and ethnic lines were associated with higher levels of citizenship engagement and awareness and appreciation of racial and cultural diversity (Gurin et al., 2002).
These studies suggest that students’ classroom experiences and personal growth are enhanced by the presence of a diverse campus community. These benefits are explored in greater detail in Chapter 5, “Transforming the Institutional Climate for Diversity.”
Diversity and Research on Racial and Ethnic Minority Health Disparities
Diversity among health professionals may improve scientific understanding of the causes and consequences of racial and ethnic health disparities and may help to eliminate these gaps. Minority scientists and researchers bring a wide range of cultural perspectives and experiences to research teams, which increases the likelihood that sociocultural issues influencing health outcomes will be addressed in research design and study questions (Institute of Medicine, 1999). In turn, a greater examination of health status and health risks among some racial and ethnic minorities will likely yield information that may prove helpful to improve health outcomes among all racial and ethnic groups. For example, public health scholars and epidemiologists have noted that some racial and ethnic minorities experience better health status than the majority population, despite relatively less advantaged environmental and socioeconomic circumstances (e.g., the “epidemiologic paradox” of better health status among new immigrant Latino populations, relative to second- and third-generation Latinos living in the United States), suggesting that these groups possess culturally determined coping styles, social supports, or health attitudes and behaviors that may reduce risks for poor health (Institute of Medicine, 1999).
Minority investigators may also prove valuable in efforts to increase the enrollment of minority patients in clinical trials. Minority participation in clinical research as human subjects is typically lower than among nonminority populations, even though some minorities experience higher rates of chronic and infectious diseases than whites. Low participation rates among minorities may be traced to a variety of historic and cultural factors (e.g., the legacy of abuse and mistreatment of minorities at the hands of the scientific and medical establishment, as exemplified in the infamous Tuskegee syphilis experiment). Yet more minorities are needed to participate in clinical research to better understand how to improve the health of
these populations and close the health gap. As a result of their generally broader cross-cultural experiences, minority investigators are often able to address minority patient mistrust and improve communication between the scientific and lay communities (Institute of Medicine, 1999).
Equally important, minority scientists and researchers, because of their personal experiences and interests, are more likely to study health needs of minority and underserved populations. As Jordan Cohen has noted,
Our country’s research agenda is influenced significantly by those who choose careers in investigation. It is also true that individual investigators tend to research problems that they see and feel. Since what people see as problems depends greatly on their particular cultural and ethnic filters, it follows that finding solutions to some of our country’s most recalcitrant heath problems, even being able to conceptualize what the real problems actually are, will require a research workforce that is much more diverse racially and ethnically than we now have (Cohen, 2003, p. 1144).
The nation’s premiere health research institution, the National Institutes of Health, has recognized the need for greater racial/ethnic diversity among health researchers and offers a number of grant programs to enhance the career development of minority health researchers.
Diversity and Health Policy and Health Research Leadership
Racial and ethnic diversity in health professions is also critical to enhance the representation of minority groups among the leadership in the health policy and health research enterprises. Racial and ethnic minority health professionals are often able to bring diverse and underrepresented perspectives to both health policy and health systems leadership, which may lead to organizational and programmatic changes that can improve the accessibility and cultural competence of health systems. Diversity in health systems leadership should not, however, be assumed to (in and of itself) lead to more culturally competent health systems; such diversity merely increases the likelihood that broader systems change will include and be guided by diverse perspectives.
Similarly, URM representation among health research policy leadership is important to broaden and improve the nation’s health research agenda. Minority researchers often bring a sensitivity to and understanding of minority health concerns that can significantly influence the design and interpretation of minority health research. This sensitivity can also significantly influence decisions regarding resource allocation and research priorities, particularly with regard to the priorities of the nation’s leading health research agency, the National Institutes of Health (NIH). Many NIH scientific advisory boards and councils lack significant racial and ethnic diversity
(Institute of Medicine, 1999), which NIH has attempted to address by identifying URM health researchers, policy analysts, and others who might be willing to serve in advisory capacities. Analogously, women’s health research has grown exponentially and has benefited from the increased presence of women among health researchers and policy makers. As a result, scientific knowledge of women’s health (and subsequent breakthroughs in the understanding and treatment of women’s health concerns) has improved dramatically over the past several decades. As above, this is not to suggest that women and minority scientists and clinicians should be expected to work exclusively in women’s and minority health domains; rather, it suggests that gender and racial/ethnic diversity in the health research enterprise can lead to important development and expansion of these fields.
Diversity and Quality of Care for All Americans
While few empirical data bear directly upon the question, indirect evidence suggests that diversity among health professionals may bring fresh approaches to health care and new problem-solving skills that can enrich and improve health care for all Americans. Anecdotal evidence suggests that the skills and resources of many diverse groups can help to address the nation’s health-care needs. Scientists and clinicians of color have contributed to many medical breakthroughs (e.g., Dr. Daniel Hale Williams, the African American physician credited with performing the first successful surgical repair of a heart wound; Dr. Charles R. Drew, the African American physician responsible for organizing the concept of the Blood Bank; Organ and Kosiba, 1987). As the U.S. Surgeon General’s report on mental health, culture, and diversity notes, “Diversity has enriched our Nation by bringing global ideas, perspectives, and productive contributions to all areas of contemporary life” (U.S. Surgeon General, 2001).
TRENDS IN MINORITY PARTICIPATION IN NURSING, MEDICINE, DENTISTRY, AND PROFESSIONAL PSYCHOLOGY—WHERE ARE THE GAPS?
While the need for and benefits of a racially and ethnically diverse workforce are clear, nursing, medicine, dentistry, and psychology have yet to reflect the diversity of the nation among their clinicians, faculty, and students. Given the changing demographic composition of the United States and current trends in minority underrepresentation in the health-care workforce, the health professions appear to be in sharp contrast with broader population changes in the country. This section will review, where
the data exist, a demographic profile of clinicians, faculty, and health professions students.6 In this section, “URM” groups are defined as African Americans, American Indians and Alaska Natives, and Latinos, because most data collection efforts until recently used this definition. This is consistent with definitions used by AAMC prior to announcing its new, broader definition of URM in June 2003.
Nurses
The Nursing Workforce
In recent years, the nursing profession has seen modest growth in the number of underrepresented racial and ethnic minorities entering its ranks. Findings from the National Sample Survey of Registered Nurses (HRSA, 2002) indicate that the percentage of minority nurses increased from 7 percent in 1980 to 12 percent in 2000. These data must be interpreted with caution, however, because of a change in questionnaire construction in 2000 to reflect revisions in the Office of Management and Budget’s (OMB) designated racial and ethnic categories. While the percentage of minority nurses increased, this percentage is still far below the minority representation in the population, which is approximately 30 percent (see Figure 1-1).
Rates of growth in the registered nurse (RN) workforce vary among racial and ethnic groups. Between 1977 and 1997, the percentage of African Americans among the nursing workforce increased from 2.6 to 4.2 percent, a 62 percent increase, while the representation of Hispanic RNs increased by 1.4 percent to 1.6 percent during the same period (a 17 percent increase; Buerhaus and Auerbach, 1999). During this same period, all “other ethnic groups”—including Asian Americans, Pacific Islanders, American Indians and Alaska Natives—increased among the RN workforce by over one-third (Buerhaus and Auerbach, 1999).
Despite these modest gains in URM representation among nurses, the nursing profession faces a critical shortage of nurses that threatens to impair the quality of care in many health-care settings (Kimball and O’Neil, 2002). In 2000, the estimated shortage of full-time equivalent RNs was
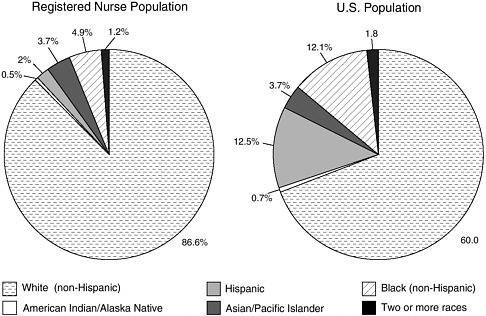
FIGURE 1-1 Distribution of registered nurses by racial/ethnic background: March 2000.
SOURCE: HRSA, 2002.
110,000, or 6 percent of the workforce. An initial slow rate of growth of this shortage is anticipated, reaching 12 percent of the workforce by 2010. At that point, the shortage will grow at an accelerated rate, reaching 20 percent by 2015. If trends continue and the problem remains unaddressed, the shortage will grow to 29 percent by 2020. Not unexpectedly—given their underrepresentation in the current nursing workforce—the shortage of minority nurses will be particularly difficult to address; an increase of more than 20,000 minority nurses is needed to increase the proportion of minority nurses by just 1 percent (National Advisory Council on Nurse Education and Practice, 2000).
The increased demand for nurses will be caused by increases in the population, growth of the elderly population, and medical advances that increase the need for nurses. The supply of potential nurses is affected by a decrease in the number of nursing graduates, decrease in relative earnings for nurses, aging of the workforce, and new and alternative job opportunities for nurses (HRSA, 2002). The shortage of nurses may have implications for patient safety in terms of hospital deaths and injuries and increased costs (through replacing nurses lost through turnover and caring for patients with poor outcomes (Institute of Medicine, 2003b).
URM Participation in Nursing Education
Among recent nursing graduates (those whose degrees were awarded in 2002), white nurses constituted the largest percentage of graduates in baccalaureate, associate, diploma, and RN programs, earning between 60–70 percent of diploma, associate, basic B.S.N., and all basic RN degrees (National League for Nursing, 2003) (Figure 1-2). Among minorities, African American and those nurses who classified their ethnicity as “other” received the largest percentage of degrees. More African American nurses received nursing diplomas than nursing degrees (B.S.N. and above). Less than 10 percent of degrees were awarded to Hispanic, Asian, and American Indian nurses.
Figure 1-3 presents enrollment trends for students in baccalaureate nursing programs (national annual data on other degree nursing programs were not available for all the years studied). URM enrollment has steadily increased between 1991 and 1999, increasing 48 percent from 11,661 to 17,303 baccalaureate nursing students.
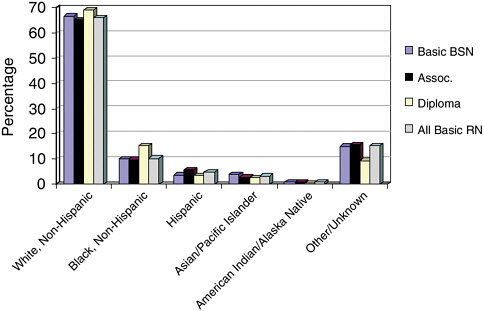
FIGURE 1-2 Estimated minority nursing graduations: baccalaureate, associate, diploma programs, 2001–2002 (preliminary and unpublished data).
SOURCE: National League for Nursing (2003). Figure included, with permission, from the National League for Nursing, New York, NY. Copyright 2004 by NLN.
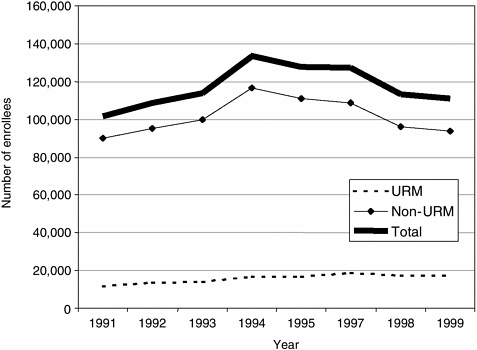
FIGURE 1-3 Enrollment in U.S. baccalaureate nursing programs.
SOURCE: Grumbach et al., 2001.
Both URM and non-URM enrollment in baccalaureate programs began to decline in the mid-1990s, although non-URM enrollment declined more sharply.
Nursing Faculty
Nursing faculty, like the broader population of nurses, does not reflect the nation’s diversity (Figure 1-4). Data indicate geographic variations in faculty diversity, as the largest percentage of African American nursing faculty are represented among faculty in the south (nearly 10 percent). In addition, there are slightly more American Indian nursing faculty in the Midwest region of the country, while the representation of Asian American nursing faculty is only slightly larger in the West than in the rest of the nation (National League for Nursing, 2002). While minorities are starkly underrepresented among nursing faculty, opportunities to increase the presence of racial and ethnic minority nursing faculty may increase in the near future, as their will be a significant need to replace the current nursing faculty, whose average age is 51.2 years (American Association of Colleges of Nursing, 2003).
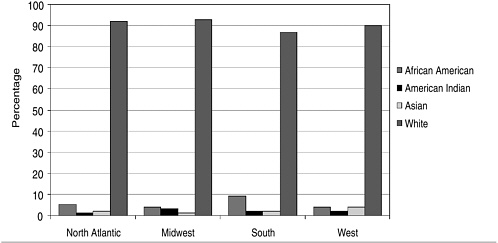
FIGURE 1-4 Racial background of full-time nursing faculty by region, 2002.
SOURCE: National League for Nursing (2003). Reproduced, with permission, from the National League for Nursing, New York, NY. Copyright 2004 by NLN.
Physicians
URM Representation in the Physician Workforce
African Americans, Latinos, and American Indians, and Alaska Natives are underrepresented among United States physicians (Figure 1-5), as these groups constitute less than 8 percent of the physician population. Of these, Hispanics/Latinos are the largest URM group, constituting approximately 3.5 percent of the physician population, followed by African Americans, who represent approximately 2.6 percent of physicians. The majority of United States physicians are white, a percentage that has slowly declined over the past several decades.
URM Representation Among Medical School Faculty
URM representation among medical school faculty increased between 1980 and 2001, as the percentage of URM faculty increased while the percentage of white faculty declined slightly (Figure 1-6; AAMC, 2002). Whites, however, remain disproportionately the largest racial or ethnic group among medical school faculty, composing just less than four of five medical school faculties in 2001. The number of full-time clinical and non-clinical URM faculty increased from 1,140 to 4,060 between 1981 and 2001, although they represent only 4.2 percent of current medical school
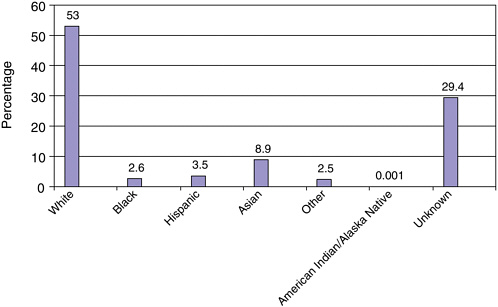
FIGURE 1-5 Total physicians by race/ethnicity, 2000.
SOURCE: AMA, Physician Characteristics and Distribution in the US 2002–2003.
faculties. Approximately 20 percent of these URM faculty members are located at Howard University School of Medicine, Meharry Medical College, Morehouse School of Medicine, and three Puerto Rican medical schools (Universidad Central del Caribe School of Medicine, Ponce School of Medicine, and the University of Puerto Rico School of Medicine).
In recent years, significant progress has been made in increasing the presence of URM faculty at many nonminority medical schools, while at other institutions their presence remains rare. Overall, the percentage of URM faculty has more than tripled in the past 20 years. In 1981, the majority of medical schools (82 of 111) had between one and nine URM faculty members and none had more than 39. In 2001, 22 (out of 112) schools had more than 40 URM faculty members, yet 27 had between one and nine URM faculty. There are still few schools that have a “critical mass” of URM faculty (AAMC, 2002).
URM Participation in Medical Education
Among medical students and recent graduates of medical schools, URM student enrollment and graduation rates generally show steady increases through the early and mid-1990s, followed by declines. URM students
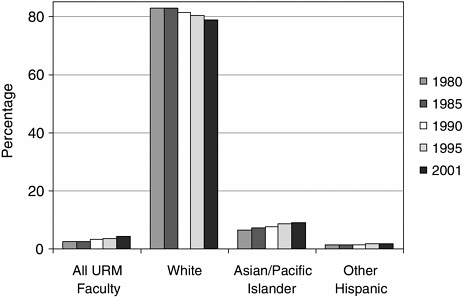
FIGURE 1-6 Distribution of U.S. medical school faculty by race/ethnicity, 1980 to 2001.
SOURCE: AAMC Faculty Roster System, December 2001. Reprinted, with permission, from the Association of American Medical Colleges, 2004. Copyright 2004 by AAMC.
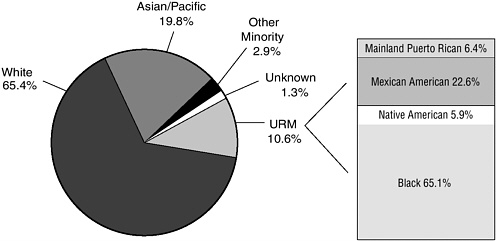
FIGURE 1-7 U.S. medical school graduates, 2001.
SOURCE: AAMC Student Record System, April 2002. Reprinted, with permission, from the Association of American Medical Colleges, 2004. Copyright 2004 by AAMC.
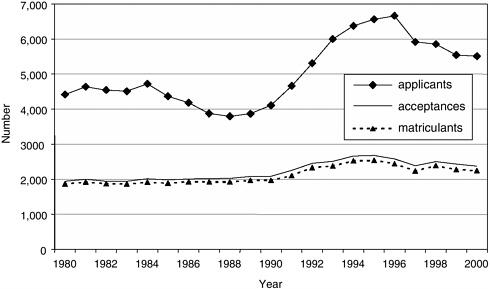
FIGURE 1-8 Allopathic medical school URM application, acceptance, and matriculation trends.
SOURCE: Grumbach et al., 2001.
constituted approximately 10 percent of medical graduates in 2001 (Figure 1-7; AAMC, 2002). The majority of these URM students (65 percent) were African American, with smaller percentages of Mexican American students (22.6 percent), mainland Puerto Ricans (6.4 percent), and Native Americans (5.9 percent). Trends from 1980 to 2001 revealed an increase in the number of URM graduates until 1998, with a gradual decline since that year. Trends in URM medical school applicants indicate an increase from the late 1980s to the mid-1990s (Figure 1-8). Since 1996–1997, there has been a steady decline. There were 6,663 URM applicants in 1996. By 2000, the number of applicants decreased to 5,511, which represents a 17 percent decrease. The decline in applicants corresponds to a decline in the number of acceptances and matriculants during the same period of time.
Dentists
URM Participation in the Dental Workforce
As in nursing and medicine, racial and ethnic minorities in dentistry are underrepresented compared to their proportions in the general population. Approximately 13 percent of dentists are nonwhite (Mertz and O’Neil, 2002), and African Americans, American Indians, and Hispanics constitute only 6.8 percent of the dental workforce (see Figure 1-9).
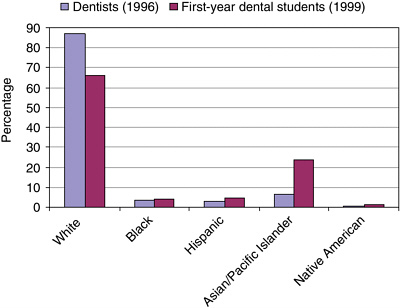
FIGURE 1-9 Variations in racial/ethnic representation in dentistry, 1996–1999.
SOURCE: Valachovic et al., 2001. Reprinted, with permission, from the American Dental Education Association, 2004. Copyright 2004 by ADEA.
URM Participation in Dental Education
Among first-year dental students in 1999, 34 percent were nonwhite. Of this percentage, however, less than one-third (10.2 percent of the total student enrollment) were from URM groups. As in medicine, the number of URM matriculants in dentistry has declined in recent years. Matriculants dropped by 23 percent: from 525 in 1989 to 404 in 1999 (Figure 1-10). Other figures indicate a slight increase in the percent of URM graduates since 1999 (Figure 1-11).
URM Participation Among Dental School Faculty
Trends in the percentage of minority full-time faculty indicate that the number of URM faculty remained low and relatively stable during the 1990s (Figure 1-12). Between 1990 and 1998, the percentage of Native American faculty increased very slightly, from 0.3 percent to 0.6 percent. The percentage of African American faculty hovered around 5 percent during these 8 years and the percentage of Hispanic faculty remained stable at approximately 3 percent.
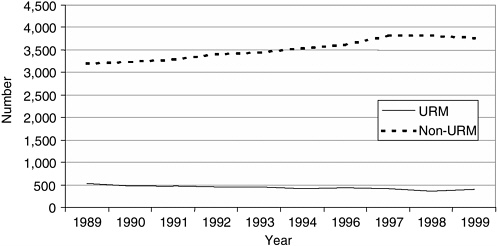
FIGURE 1-10 Dental school matriculants.
SOURCE: Grumbach et al., 2001.
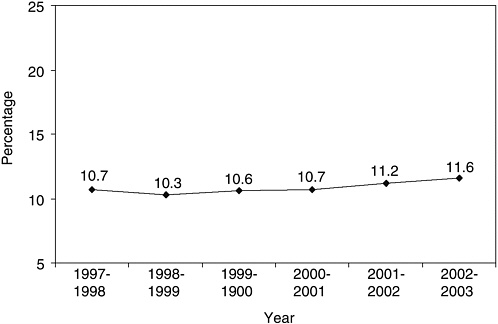
FIGURE 1-11 Underrepresented minority graduates in U.S. dental education programs: Black, Hispanic, Native American.
SOURCE: Total Minority Enrollment in U.S. Dental Education Programs, 1997–2003. American Dental Association Survey Center, Surveys of Predoctoral Dental Education. Reprinted, with permission, from American Dental Association, 2004. Copyright 2004 by ADA.
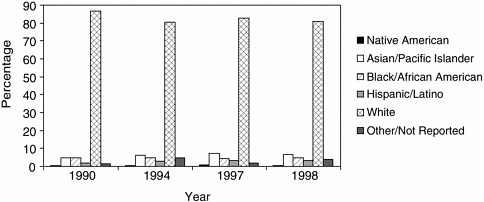
FIGURE 1-12 Minority full-time faculty in U.S. dental schools. SOURCE: Haden et al., 2000. Reprinted, with permission, from the American Dental Education Association, 2004. Copyright 2004 by ADEA.
Psychologists
URM Participation in the Psychology Workforce
Minority representation in the field of psychology is disproportionately low (Figure 1-13; Rapopor et al., 2000). Among all psychologists, 3.4 percent are African American, 3.4 percent are Hispanic, and 2.2 are Asian/ Pacific Islander. The percentage of American Indian/Alaska Native psychologists is less than 1 percent.
URM Participation among Psychology Faculty
URMs are similarly underrepresented among faculty in departments of psychology (Figure 1-14). Among full professors, 94.1 percent are white, 1.7 percent are Asian, 2 percent are Hispanic, 1.9 percent are African American, and 0.3 percent are American Indian. Among all tenured professors, 2.5 percent are African American, 2.3 percent Hispanic, and 0.3 percent American Indian. However, URM faculty have slightly higher representation among tenure track professors (5.1 percent black, 4.6 percent Hispanic, and 0.9 percent American Indian).
URM Participation in Psychology Graduate Education
The percentage of URM graduate students in departments of psychology is greater than percentage of URM faculty. During the 2002–2003 academic year, 7 percent of first-year students in programs that offered a Ph.D. were African American, 6 percent were Hispanic, 1 percent were
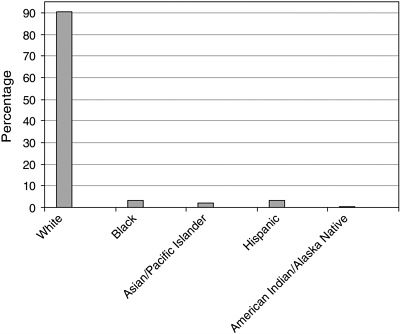
FIGURE 1-13 Employed doctoral psychologists (percent), 2001.
SOURCE: National Science Foundation/Division of Science Resources Statistics, 2001 Survey of Doctorate Recipients.
Native American, and 1 percent classified themselves as multiracial (Figure 1-15). Among 2000 graduates from clinical psychology programs, the largest subfield of practitioners, 5 percent were African American, 7 percent were Hispanic, and less than 1 percent were Native American.
SUMMARY
African Americans, American Indians and Alaska Natives, and many Hispanic/Latino populations are grossly underrepresented among the nation’s physicians, nurses, dentists, and psychologists. These populations also experience generally poorer health status and face greater difficulties in accessing health care. Consequently, many health professions leaders have called for an expansion of efforts to increase diversity among health-care professionals as one means of assisting in the effort to increase access to health care for all populations and to close the health gap between minorities and nonminorities.
Recent policy developments, however, have had and may continue to have a significant negative impact on the ability of health professions train-
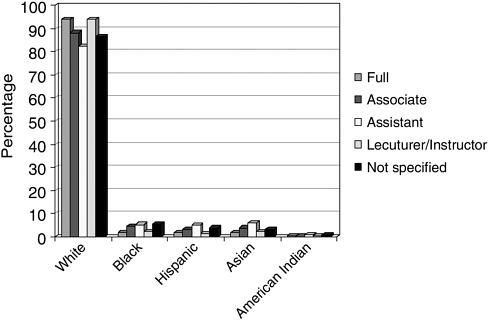
FIGURE 1-14 Academic rank of faculty in departments of psychology by race/ ethnicity, 2002–2003.
SOURCE: Faculty Salary Survey, 2002–2003. Academic Rank and Tenure Status of Faculty in Graduate Departments of Psychology by Race/Ethnicity, 2002–2003. Reprinted, with permission, from the American Psychological Association, 2004. Copyright 2004 by APA.
ing programs and higher education institutions to admit URM students into the health professions training pipeline. The U.S. Supreme Court decision in the Grutter v. Bollinger lawsuit reaffirmed that higher education institutions may consider applicants’ race or ethnicity as one of many factors in admissions decisions. But as a result of public referenda, judicial decisions, and lawsuits challenging affirmative action policies in 1995, 1996, and 1997, many higher education institutions abandoned (in some cases, temporarily) the use of race and ethnicity as factors in admissions decisions. To add to this challenge, significant financial disparities persist between minority and nonminority students, leaving many URM students with fewer financial resources to pursue careers in health professions. It is therefore important to assess whether opportunities exist at the level of higher education institutions, health professions leadership and accrediting bodies, and state and federal policy to reduce barriers to minority participation in health professions.
This chapter has presented a review of evidence regarding the impor-
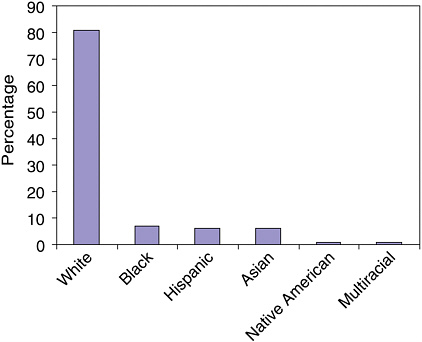
FIGURE 1-15 Race/ethnicity of newly enrolled students in doctoral departments of psychology, 2002–2003.
SOURCE: Graduate Study in Psychology, 2004. Compiled by APA Research Office. Reprinted, with permission, from the American Psychological Association, 2004. Copyright 2004 by APA.
tance of diversity in health professions. This evidence demonstrates that greater diversity among health professionals is associated with improved access to care for racial and ethnic minority patients, greater patient choice and satisfaction, and better patient–clinician communication. Indirectly, this evidence suggests that greater diversity can improve the cultural competence of health professionals and health systems and that such improvements may be associated with better health-care outcomes. In addition, greater diversity among health professionals has the potential to improve the clinical research enterprise and to lead to new developments and improvements in health care and how care is delivered.
Subsequent chapters of this report will explore the potential value of specific institutional and policy-level strategies to increase diversity in the health professions. These strategies include efforts to reconceptualize admissions procedures for health professions education programs, to improve public and private financing of health professions education, to place greater emphasis on faculty and student diversity in program accreditation stan-
dards, and to improve the campus climate for diversity. Finally, the study committee considers the potential application of community benefit principles to improve the accountability of nonprofit, tax-exempt institutions to the diverse racial and ethnic communities they serve.
REFERENCES
American Association of Colleges of Nursing. 2003. AACN’s Nursing Faculty Shortage Fact Sheet. [Online]. Available: http://www.aacn.nche.edu/Media/Backgrounders/facultyshortage.htm [accessed January 16, 2004].
American Medical Association (AMA). 2003. Physician Characteristics and Distribution in the US, 2002-2003. Chicago: American Medical Association.
Anderson LM, Scrimshaw SC, Fullilove MT, Fielding JE, Normand J. 2002. Culturally competent healthcare systems: A systematic review. American Journal of Preventive Medicine 24(3 Suppl):68–79.
Antonio AL, Chang MJ, Hakuta K, Kenny DA, Levin SL, Milem JF. In press. Effects of racial diversity on complex thinking in college students. Psychological Science.
Association of American Medical Colleges (AAMC). 2002. Minority Students in Medical Education: Facts and Figures XII. Washington, DC: Association of American Medical Colleges.
Betancourt JR, Green AR, Carrillo JE. 2002. Cultural Competence in Health Care: Emerging Frameworks and Practical Approaches. New York: The Commonwealth Fund.
Bichsel RJ, Mallinckrodt B. 2001. Cultural commitment and the counseling preferences and counselor perceptions of Native American women. The Counseling Psychologist 29(6): 858–881.
Buerhaus PI, Auerbach D. 1999. Slow growth in the United States of the number of minorities in RN workforce. Journal of Nursing Scholarship 31(2):179–183.
Cantor JC, Bergeisen L, Baker L. 1998. Effect of intensive educational program for minority college students and recent graduates on the probability of acceptance into medical school. Journal of the American Medical Association 280:772–776.
Cantor JC, Miles EL, Baker LC, Barker DC. 1996. Physician service to the underserved: Implications for affirmative action in medical education. Inquiry 33:167–181.
Cohen JJ. 2003. The consequences of premature abandonment of affirmative action in medical school admissions. Journal of the American Medical Association 289(9):1143–1149.
Collins KS, Hall A, Neuhaus C. 1999. U.S. Minority Health: A Chartbook. New York: The Commonwealth Fund.
Cooper L, Roter D. 2003. Patient–provider communication: The effect of race and ethnicity on process and outcomes of health care. In: Smedley BD, Stith AY, Nelson AR, eds. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: The National Academies Press.
Cooper-Patrick L, Gallo JJ, Gonzales JJ, Vu HT, Powe NR, Nelson C, Ford DE. 1999. Race, gender, and partnership in the patient–physician relationship. Journal of the American Medical Association 282(6):583–589.
Grumbach K, Coffman J, Rosenoff E, Muñoz C. 2001. Trends in underrepresented minority participation in health professions schools. In: Smedley BD, Stith AY, Colburn L, Evans CH, eds. The Right Thing to Do, The Smart Thing to Do: Enhancing Diversity in the Health Professions. Washington, DC: National Academy Press.
Gurin P, Dey EL, Hurtado S, Gurin G. 2002. Diversity and higher education: Theory and impact on educational outcomes. Harvard Education Review 72(3):330–366.
Haden NK, Beemsterboer PL, Weaver RG, Valachovic RW. 2002. Dental school faculty shortages increase: An update on future dental school faculty. Journal of Dental Education 64(9):666–682.
Health Resources and Services Administration (HRSA). 2002. Projected Supply, Demand, and Shortages of Registered Nurses: 2000–2020. [Online]. Available: http://bhpr.hrsa.gov/healthworkforce/rnproject/default.htm [accessed December 2, 2003].
Institute of Medicine (IOM). 1999. The Unequal Burden of Cancer: An Assessment of NIH Programs and Research for Minorities and the Medically Underserved. Haynes AM, Smedley BD, eds. Washington, DC: National Academy Press.
Institute of Medicine (IOM). 2001. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academy Press.
Institute of Medicine (IOM). 2003a. Unequal Treatment: Confronting Racial and Ethnic Disparities in Healthcare. Smedley BD, Stith AY, Nelson AR, eds. Washington, DC: The National Academies Press.
Institute of Medicine (IOM). 2003b. Keeping Patients Safe: Transforming the Work Environment of Nurses. Page A, ed. Washington, DC: The National Academies Press.
Kaiser Daily Health Policy Report. 2003. California seniors who are Latino or have limited English language skills more likely to report being in fair or poor health, study says. [Online]. Available: www.kaisernetwork.org/daily_reports [accessed October 31, 2003].
Kimball B, O’Neil E. 2002. Health Care’s Human Crisis: The American Nursing Shortage. Princeton, NJ: The Robert Wood Johnson Foundation. [Online]. Available: http://www.rwjf.org/news/special/nursing_report.pdf [accessed January 16, 2004].
Komaromy M, Grumbach K, Drake M, Vranizan K, Lurie N, Keane D, Bindman AB. 1996. The role of black and Hispanic physicians in providing health care for underserved populations. New England Journal of Medicine 334(20):1305–1310.
LaVeist TA, Nuru-Jeter A. 2002. Is doctor–patient race concordance associated with greater satisfaction with care? Journal of Health and Social Behavior 43(3):296–306.
Lopez SR, Lopez AA, Fong KT. 1991. Mexican Americans’ initial preferences for counselors: The role of ethnic factors. Journal of Counseling Psychology 38(4):487–496.
Matherlee K. This volume. The role of public financing in improving diversity in the health professions. In Smedley BD, Stith-Butler A, Bristow LR, eds. In the Nation’s Compelling Interest: Ensuring Diversity in the Health-Care Workforce. Washington, DC: The National Academies Press.
Mertz E, O’Neil E. 2002. The growing challenge of providing oral health care services to all Americans. Health Affairs 21(5):65–77.
Mertz EA, Grumbach K. 2001. Identifying communities with low dentist supply in California. Journal of Public Health Dentistry 61(3):172–177.
Moy E, Bartman A. 1995. Physician race and care of minority and medically indigent patients. Journal of the American Medical Association 273(19):1515–1520.
National Advisory Council on Nurse Education and Practice. 2000. A National Agenda for Nursing Workforce Racial/Ethnic Diversity. Report to the Secretary of Health and Human Services and Congress. Washington, DC: U.S. Department of Health and Human Services.
National League for Nursing 2003. Nurse Educators 2002: Report of the Faculty Census Survey of RN and Graduate Programs. New York: National League for Nursing.
Nettles MT, Millet CM. 2001. Toward diverse student representation and higher achievement in higher levels of the educational meritocracy. In: Smedley SB, Stith AY, Colburn L, Evans CH, eds. The Right Thing to Do, The Smart Thing to Do: Enhancing Diversity in Health Professions. Washington, DC: National Academy Press.
Organ CH, Kosiba MM. 1987. A Century of Black Surgeons—The U.S.A. Experience. Volume I. Norman, OK: Transcript Press.
Perez-Stable EJ, Napoles-Springer A, Miramontes JM. 1998. The effects of ethnicity and language on medical outcomes of patients with hypertension or diabetes. Medical Care 35(12):1212–1219.
Rapoport AI, Kohout J, Wicherski M. 2000. Psychology doctorate recipients: How much financial debt at graduation? Issue Brief: Division of Science Resources Studies, National Science Foundation. [Online]. Available: http://www.nsf.gov/sbe/srs/issuebrf/sib00321/htm [accessed August 18, 2003].
Robert Wood Johnson Foundation. 2001. New survey shows language barriers causing many Spanish-speaking Latinos to skip care. [Online]. Available: www.rwjf.org/news [accessed January 26, 2003].
Saha S, Taggart S, Komaromy K, Bindman AB. 2000. Do patients choose physicians of their own race? Health Affairs 19(4):76–83.
Saha S, Komaromy, M, Koepsell TD, Bindman AB. 1999. Patient–physician racial concordance and the perceived quality and use of health care. Archives of Internal Medicine 159:997–1004.
Sinkford JC, Harrison S, Valachovic W. 2001. Underrepresented minority enrollment in U.S. dental schools—The challenge. Journal of Dental Education 65(6):564–570.
Solomon ES, Williams CR, Sinkford JC. 2001. Practice location characteristics of black dentists in Texas. Journal of Dental Education 65(6):571–574.
Turner CB, Turner BF. 1996. Who treats minorities? Cultural diversity in mental health. Cultural Diversity in Mental Health 2(3):175–182.
U.S. Bureau of the Census. 2003. Hispanic population reaches all-time high of 38.8 million, new Census Bureau estimates show. [Online]. Available: www.census.gov/press-release/www/2003/cb03-100.html [accessed September 24, 2003].
U.S. Surgeon General. 2001. Mental Health: Culture, Race, and Ethnicity. A Supplement to Mental Health: A Report of the Surgeon General. Washington, DC: U.S. Department of Health and Human Services.
Valachovic RW, Weaver RG, Sinkford JC, Haden K. 2001. Trends in dentistry and dental education. Journal of Dental Education 65(6):539–561.
Whitla DK, Orfield G, Silen W, Teperow C, Howard C, Reede J. 2003. Educational benefits of diversity in medical school: A survey of students. Academic Medicine 78(5):460–466.
































