5
Poison Control Center Activities, Personnel, and Quality Assurance
Poison control centers were developed as sources of information about the management of pediatric poisonings, but have evolved to encompass a wide range of additional functions (Hoffman, 2002; Leikin and Krenzelok, 2001; Youniss et al., 2000; Zuvekas et al., 1997). Here we provide an overview of poison control center activities (Box 5-1) and the personnel who perform them (American Association of Poison Control Centers, 2002a; Poison Center Annual Reports, 2000–2002). Some of these activities are discussed only briefly here and covered more thoroughly in other chapters (e.g., public education, data collection and surveillance systems, and sentinel events).
Most activities discussed in this chapter are provided by all poison control centers, such as responding to telephone calls from the public or health care providers regarding poison exposures. Other activities are offered by only some poison control centers, depending on their interests, capabilities, affiliations, and the funding initiatives of sponsoring agencies. For example, centers affiliated with medical toxicology training programs serve as clinical training sites for medical toxicology residents. Collaboration between poison control centers and appropriate public health agencies, health care providers and provider groups, government agencies, and academic resources is embedded within the activities to be described, and is assumed throughout this discussion.
The first half of this chapter reviews the service and administrative/ research activities of the poison control centers. The professional education role of the centers, including the poison specialists who work for them, is emphasized in the latter half of the chapter.
|
BOX 5-1 Phone consultation regarding individual exposures, potential exposures, or information Public callers Health care professionals Capacity to respond to mass exposures or potential exposures HAZMAT/occupational Bioterrorism Nonpoisoning exposures for which the poison control center may be the default information source Contract services Industry support Data collection and reporting Systematic reporting of exposures to a collective poison prevention and control database Sentinel event reporting Research Toxicology Health care delivery Program evaluation Quality improvement Outcomes Public education, in collaboration with public health agencies Prevention Use of the health care system Professional education Specialist in poison information and poison information provider training Medical toxicologists Continuing education of health care professionals Other health care trainees |
ACTIVITIES
Telephone Consultation
The primary activity of poison control centers in the United States is telephone consultation, providing direct services to the public, emergency medical services personnel, health care providers, and public health agencies (Zuvekas et al., 1997). These services depend on the rapid, efficient call handling by specialists with training in clinical toxicology, supported by medical toxicologists, consultants in subspecialty areas, and poison information databases. The general process of call management is illustrated in Figure 5-1 and will be discussed. The skill sets and training of
personnel responding to telephone calls are reviewed later in this chapter under the section on health care professionals.
Table 5-1 presents an overview of poison control center direct services to patients; emergency medical services (EMS) personnel; medical staff in offices, clinics, and emergency departments; in-hospital staff; and local and state public health officials. Examples include providing (1) comfort to caregivers or patients; (2) advance notification and care guidance to EMS, emergency department, and in-hospital personnel; and (3) consultation on syndromal case clustering with public health officials.
Calls from the Public
Poison control centers provide information to the public regarding poisoning exposures and respond to requests for information about poisons—defined as calls in which there is no actual exposure discussed (Hoffman, 2002). Calls to poison control centers can be made directly by the public using a toll-free telephone number or through referrals to centers via 911 or other emergency numbers. Human exposures or suspected
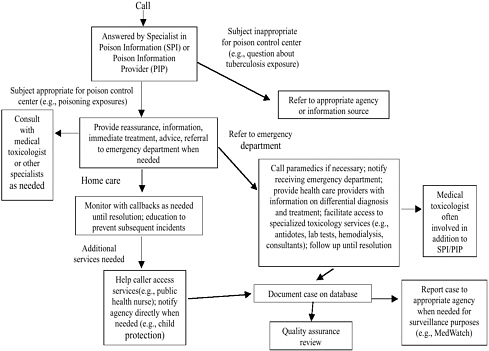
FIGURE 5-1 Typical sequence of events at poison control center handling a call from the public.
TABLE 5-1 Poison Control Center Direct Service Matrix
|
|
Service Recipient |
||||
|
Service Type |
Patient/Family Member |
EMS Personnel |
Office, Clinic, or Emergency Department Personnel |
In-Hospital Personnel |
County and Regional Public Health |
|
Comfort and reassure |
yes |
— |
— |
— |
— |
|
Identify products |
yes |
yes |
yes |
yes |
— |
|
Determine potential toxicity |
yes |
yes |
yes |
yes |
— |
|
Assist 911 response |
yes |
yes |
|
— |
— |
|
Direct poisoning first aid |
yes |
yes |
yes |
— |
— |
|
Guide prehospital triage decisions |
yes |
yes |
— |
— |
— |
|
Provide advance notification if care transferred |
— |
yes |
yes |
— |
— |
|
Offer continued care guidance and monitoring |
yes |
yes |
yes |
yes |
— |
|
Provide poison prevention education |
yes |
— |
— |
— |
— |
|
Guide advanced patient management and diagnostics |
— |
— |
yes |
yes |
— |
|
Guide caregiver protective actions |
— |
yes |
yes |
yes |
— |
|
Supply reference materials related to patient management |
— |
— |
yes |
yes |
— |
|
Link provider with special toxicology resources |
— |
— |
yes |
yes |
— |
|
Guide hazardous materials management |
— |
yes |
yes |
yes |
yes |
|
Consult on syndromal case clustering |
— |
— |
yes |
yes |
yes |
|
Participate in public health notifications as health threats emerge |
— |
— |
— |
yes |
yes |
exposures represent 68 percent of all calls, and requests for information represent 32 percent (Watson et al., 2003). In 2002, there were 2.38 million human exposure calls and 1.1 million information calls to poison control centers across the country (see Table 5-2 for the content of these calls). Approximately 85 percent of the human exposure calls were categorized as unintentional, 11.7 percent as intentional, and 2.4 percent as adverse reaction. Furthermore, most calls were judged to have little or minor effect, with 74 percent managed in the home (Watson et al., 2003).
Assistance to the public regarding human exposures includes assessment of the type and severity of poisoning, suggestions for at-home care when appropriate, reassurance to the caller, and referral to a health care provider when necessary. Follow-up is provided with callbacks as needed to assure satisfactory resolution of the episode. Preventive measures are suggested to avoid similar poisoning episodes, such as removing certain items from the home or placing them out of reach of children. When callers are referred to a health care facility, that facility is notified and information regarding the case and the relevant toxicology of the poison involved is made available. Access to the public is provided via around-the-clock toll-free telephone lines staffed by poison control center personnel. Most calls are answered by specialists in poison information (SPIs) or poison information providers (PIPs) (Zuvekas et al., 1997). Medical toxicologists are available at all times by telephone for backup consultation. Poison control centers also have consultants on call with specific areas of expertise, such as mycologists and herpetologists. Tables 5-2 and 5-3 present the most common reasons for exposure and information calls, respectively.
Poison control centers also respond to calls from the public regarding animal exposures to poisons; exposures to chemicals at work or in the home; requests to evaluate symptoms that the caller believes may be related to poisoning; questions about environmental pollutants, plants, herbal medicines, drug interactions, or envenomations; or requests for general information about poisoning topics (e.g., first aid) (Leikin and Krenzelok, 2001). The range of topics is broad in part because people call the poison control center when they are not sure who else to call. Such calls may be referred to more appropriate agencies, for example, the local public health department for possible food poisoning. Nearly all of the poison control centers maintain websites with information on selected topics and links to other information sources, and callers may be referred to those websites when appropriate.
Calls from Health Care Professionals
Poison control centers provide information to a wide variety of health care providers regarding exposures and potential exposures. As the focus
TABLE 5-2 Exposure Call Content (most common agents involved in 2,380,028 exposure calls* reported to the TESS data collection system in 2002)
TABLE 5-3 Information Call Content to Poison Control Centers (most common topics involved in 1,110,635 information calls* reported to the TESS data collection system in 2002)
of poison control centers has shifted from pediatric exposures to include adult exposures, which are far more likely to result in significant morbidity and mortality, consultation with health care providers has become an increasingly important function. Users of this service include emergency medical technicians (EMTs) who obtain prehospital treatment guidance; first responders such as firefighters or HAZMAT teams; nurses and physicians in hospitals and clinics; nurses and social workers who staff advice lines; and physicians, nurses, or other professionals with public health agencies (Hoffman, 2001; Leikin and Krenzelok, 2001). Consultation with emergency department and intensive care unit staff has become an important role for poison control center staff. Emergency or critical care physicians or nurses managing poisonings in their clinic are given guidance related to poison identification, anticipated toxic effects, initial intervention, and whether transfer to an emergency department or inpatient facility is needed. Emergency physicians and nurses may receive suggestions regarding differential diagnosis, initial intervention, selection of laboratory tests, where to send nonstandard laboratory test requests, the need for consultation and the identification of appropriate consultants, and disposition of the patient.
Poison control center staff provide guidance regarding the indications for specific procedures such as hemodialysis, the availability and use of specific antidotes, or the need for transfer when the necessary facilities or expertise needed for patient management are not available. Staff assist with arranging patient transfers or putting physicians in contact with appropriate consultants. Specific reference materials or pertinent literature are provided. Calls from health care professionals are handled initially by SPIs or PIPs, but are often referred to medical toxicologists. Approximately 20 percent of the human exposure calls made to poison control centers come from health care facilities (Poison Control Center Annual Reports, 2000–2002).
Follow-up calls from the poison control center are used to ascertain patient status, symptom resolution, compliance with recommended therapy, and where appropriate, status after discharge. For both public and health care professional callers, health care agencies are contacted when they can assist with patient care or when reporting is required or appropriate. The adverse effect of Health Insurance Portability and Accountability Act regulations, or hospitals’ interpretations of these guidelines, on the ability to obtain follow-up information is an issue that poison control centers are currently addressing (http://fpicn.org/HIPAA_Compliant.htm).
Technology Support for Telephone Consultation
Since 2001, the American Association of Poison Control Centers (AAPCC) has been responsible for establishing and implementing a national toll-free telephone number (1-800-222-1212) that is advertised by all U.S. poison control centers. Individuals (either from the public or health care professionals) who wish to report a poisoning exposure or ask for information regarding a product or procedure can call this number and be routed to the local poison control center for a response. Centers may continue to maintain their own local and toll-free numbers because people in their service area are familiar with these numbers and have them posted at home. California maintains a separate toll-free number for use by health care professionals. Specialized telecommunication devices for communication with deaf individuals are used, and there are links to agencies that specialize in communicating with them. Translation services are available to ensure rapid and accurate communication with individuals who do not speak English or who speak English as a second language. Generally, these services are provided through a three-way conference call with a translation service equipped to translate several languages; however, four centers have bilingual speakers onsite 24 hours a day, 7 days a week (http://www.aapcc.org/pccsurveyresults/2002/2002Table4.pdf).
The primary information aid in exposure analysis and treatment is Poisindex® published by Micromedex. As noted in Chapter 4, Poisindex provides (1) information on the composition of most commercial and natural products; (2) a description of the toxicity of the products; and (3) suggested treatment options. Micromedex employs an internal staff to obtain and code products as well as to prepare the management documents for review by an outside editorial board. The embedded product codes are used by AAPCC to connect each poison control center case to a product or category.
As the call progresses, the certified specialist in poison information (CSPI) or SPI collects and records demographic information about the caller (e.g., age, gender, geographic location), notes the product code associated with the exposure, judges severity, and provides treatment recommendations using one of four commercially available data collection systems (discussed in Chapter 8) that automatically upload data every 4 to 10 minutes to the Toxic Exposure Surveillance System (TESS) housed at AAPCC headquarters in Washington, D.C. Electronic matching between the computerized case reports filled out by the specialists and the product and ingredient indexes of Poisindex® is automatic and works seamlessly with all four electronic data collection programs.
Capacity to Respond to Mass Exposures or Potential Exposures
HAZMAT, Occupational, or Environmental Exposures
Poison control centers are an integral part of most local HAZMAT (hazardous materials) response protocols, such as a chemical leak from an overturned tanker truck (Burgess et al., 1997; Mrvos et al., 1988). In this capacity, poison control centers work in close collaboration with local public health agencies and other agencies with responsibilities in this area, such as fire and police departments. Centers may be accessed in these situations by the public, responders at the incident scene, health care providers caring for exposed individuals, or public health agencies. The role of the poison control center includes providing information to individuals with exposures or potential exposures, assisting in triaging injured patients and notifying the receiving health care facility, providing information regarding the toxicology of the chemicals involved in the incident and the management of exposed patients, and gathering data regarding exposures (e.g., locations, types of injuries) that may be useful for managing the incident or for surveillance and follow-up. Poison control centers serve a similar role in acute or chronic occupational exposures, providing initial information regarding the toxicology of the exposure, assistance with initial triage and management, and coordination with responsible public health agencies (Blanc and Olson, 1986). Centers also have been accessed following natural disasters such as earthquakes to provide information on air and water quality (Nathan et al., 1992).
All-Hazards and Other Public Health Emergencies
Poison control centers can play an important role in preparedness and response to acts of bioterrorism, chemical terrorism, or other public health emergencies. The efforts involved in the rapidly evolving, present-day building of capacity in the areas of bioterrorism and chemical terrorism preparedness and response is likely to strengthen the ability of centers to respond to natural disasters and other threats to public health. In 2001, 3,395 exposure calls regarding agents classified in TESS as “weapons of mass destruction” (WMD) were received and acted on by poison control centers. Examples include reports of anthrax, suspicious powder, chemical weapons, and other suspicious substances.
State plans for public health and hospital emergency preparedness are beginning to acknowledge roles for poison control centers. These state programs, funded by cooperative agreement grants from the Centers for Disease Control and Prevention (CDC) and the Health Resources and Services Administration (HRSA), help the public health system and hos-
pitals prepare for acts of bioterrorism, outbreaks of infectious disease, and other public health threats and emergencies. For a further discussion of state involvement, see Chapter 9.
To help describe the relevant services that poison control centers can provide, the following framework is adapted from the Haddon Matrix: Preevent, including planning, education, and surveillance; Event and Response, including detection, investigation, dissemination of information to the public, antidote distribution, and communication with agencies; and Recovery, including serving as an information resource for the public and health care providers.
Preevent activities include the following:
-
Preparedness planning: Poison control center personnel, particularly toxicologists and pharmacists, serve in multiple capacities related to local, regional, and national emergency preparedness planning; examples include service on state and local preparedness committees and advisory groups. CDC and HRSA guidance in 2003 to state and local applicants for cooperative agreement funding for public health preparedness and response to bioterrorism specifies that poison control centers be represented on advisory committees for these cooperative agreements. Centers also assist with Strategic National Stockpile planning; help with local and regional capacity assessments related to bioterrorism preparedness; and develop diagnostic and treatment protocols and associated standardized staff education programs. Poison control centers also maintain antidote supplies and/or facilitate local/regional inventory tracking for essential medicines and other supplies.
-
Surveillance: Poison control centers participate in toxicosurveillance for the identification of sentinel events that may represent intentional bioterrorist events or natural toxin exposures. Every 4 to 10 minutes, poison control centers upload case data to TESS. To assist in improving public health surveillance, CDC’s National Center for Environmental Public Health, the Agency for Toxic Substances and Disease Registry (ATSDR), and AAPCC are working to convert TESS into a real-time public health surveillance system. This conversion will generate more immediate and appropriate responses to public health threats that may be related to toxins or chemicals in the environment. In addition to a national toxicosurveillance effort performed in conjunction with AAPCC, poison control centers participate in local syndromic surveillance and report notifiable conditions affecting multiple individuals to local and/or state health officials.
-
Continuing education and research and preparation for bioterrorism through effective training programs: Poison control centers provide training to various groups (e.g., the public, emergency medicine residents, medical toxicology
-
fellows, emergency physicians and nurses, and public health officials) on the medical effects of WMD. Centers also serve as a repository for specialized databases regarding agents of bioterrorism and chemical terrorism.
Event and Response activities include the following:
-
Poison control centers can provide assistance with early recognition and notification of bioterrorism and chemical terrorism events; coordinate antidote distribution and guide appropriate antidote use; assist health care professionals with management of exposed patients and rescue personnel; disseminate threat and preventive/therapeutic information to the public; and provide consultative support to public health and law enforcement authorities.
Recovery activities include the following:
-
Poison control centers provide a single source (i.e., one telephone number) for coordinating exposure and treatment information; serve as an information resource to the public, media, and medical practitioners regarding existing health effects in the aftermath of a terrorist act; reassure these same groups to help minimize panic; and provide information to public health agencies about the long-term effects associated with a terrorist attack and how to respond to and treat those effects.
Case vignettes illustrative of how poison control centers contribute to the investigation and management of bioterrorism events are presented in Appendix 5-A. The case study of the Rocky Mountain Poison and Drug Center illustrates the integral involvement of a center into a public health system. The Texas Poison Control Center’s experience illustrates the role a poison control center can play in communicating with the public and provider community when an urgent health issue emerges, in this instance the receipt of hundreds of calls during the 2001 anthrax attacks. The Northern New England Poison Center vignette describes how a center works in the early identification of (i.e., toxicosurveillance) and response to a communitywide cluster of illness (i.e., arsenic exposure).
Nonpoisoning Exposure Information Requests to Poison Control Centers
Because of their well-publicized availability, poison control centers are often the default choice for the public to call regarding exposures to agents other than chemicals. For example, centers have received calls about Severe Acute Respiratory Syndrome and must be able to respond with appropriate information or referrals. In addition, incidents can occur
in which the nature of the offending agent is unknown and could be an infectious agent or a chemical. In this case, the public, health care professionals, and public health agencies may all access the poison control center for information (Geller and Lopez, 1999).
Industry Contracts
Poison control centers may contract with industry to provide poisoning information to the public and health care providers for a specific commercial product or group of products. For example, the toll-free number listed on a commercial product for information about poisoning may be answered by center staff, usually through a separate, dedicated telephone line. Summary information regarding the number, types, and outcomes of these exposures can assist companies with reporting requirements regarding adverse events associated with their products and guide reduction of the hazard. Poison control centers may also contract to provide material safety data sheets needed by an employer (Krenzelok and Dean, 1988). The number and extent of poison control center contracts with industry is not well documented.
Data Collection and Reporting
Data collection and reporting are critical activities of poison control centers. This topic is examined in detail in Chapter 7 along with the contribution of other data sources in developing an overall understanding of poisonings in the United States.
Systematic Reporting of Exposures to a Collective Poison Control Center Database
Poison control centers currently report all exposure data to the TESS database (Watson et al., 2003). These data are used to document the spectrum of exposures causing poisonings and their consequences. While this database represents only the fraction of all exposures that generate calls to centers (Blanc et al., 1995), the data may be used to identify trends and potential targets for education, surveillance, public health measures, or research. This type of database represents a unique opportunity to collect detailed data regarding certain types of poisoning exposures.
Sentinel Event Reporting
Sentinel events are initial cases or events indicating a more widespread problem. Poison control centers, because of their telephone con-
sultation function, may be the first part of the health care system to become aware of new types of poisonings in the community, such as previously unknown adverse reactions to a medication, the use of a new type of drug of abuse (e.g., scopolamine poisoning among heroin users [Morbidity and Mortality Weekly Report, 1996]), or an unusual illness suggestive of bioterrorism. Centers may also recognize clusters of cases that would otherwise go unnoticed as isolated events. Prompt reporting of these events to the appropriate public health agencies and in the medical literature can help provide an early warning and offer the option of generating a timely response. Poison control centers also notify public health agencies of reportable diseases or cases or incidents that may be of interest, such as suspected food poisoning.
Research
AAPCC (http://www.aapcc.org) considers research to be a part of the overall mission of poison control centers. Center research may be broadly divided into toxicology research, which focuses on the mechanisms, treatment, or prevention of poisonings; and poison control center clinical services research, which focuses on the role and contribution of centers to studying and managing these problems (North American Congress of Clinical Toxicology, 2003). Examples of poison control center clinical services research include the evaluation of different poison control center service models with regard to costs and outcomes; comparison of different data collection tools or models; efficacy of using center data for real-time surveillance of previously unrecognized toxic effects of medications or mass poisonings; effectiveness of education strategies; comparisons of treatments; or strategies for monitoring herbal medicine toxicities. Although any investigator, regardless of location or affiliation, could perform such research, poison control center staff are particularly well positioned to conduct research in these areas. Their involvement in the management of exposure and information calls provides a unique opportunity to identify important or emerging issues. Access to center data and familiarity with the health care delivery issues facing poison control centers provide staff with a unique perspective on issues surrounding the delivery of center services, and the means to study strategies for improving these services.
Despite these opportunities, the research output of poison control centers is generally modest. One survey of center research efforts, which included all types of research except for “bench science,” found that 5 percent of poison control center staff time (primarily non-SPI staff) was devoted to research and that centers published a mean of three journal articles yearly (Zuvekas et al., 1997). Some centers, such as those affiliated
with medical toxicology training programs, are more active in research. However, as noted in Chapter 6, they have little specific funding to conduct this research. Hence, presentations at the AAPCC annual meeting, the largest annual gathering of clinical toxicologists, tend to emphasize clinical observations. The abstracts accepted for the AAPCC meetings during the years 2001–2003 were tallied (Table 5-4), and results showed the vast majority of presentations were case reports and descriptive database summaries (some of the latter included prospective observational studies). True clinical trials, randomized or not, made up about 2 percent of the abstracts presented. This latter figure does not include a small number of human pharmacokinetic studies, which were generally observational and included only one to two subjects (these are listed separately). Laboratory-based or animal/tissue studies were the subject of about 11 percent of the abstracts. Clearly, the presentation of prospective interventional and laboratory-based research in poisoning mechanisms and management at this meeting was limited. Even research abstracts focusing on poison system impact made up less than 10 percent of the abstracts. Furthermore, only 1.5 percent of the abstracts addressed public/professional poison education programs.
TABLE 5-4 Summary of Research Abstract Contents, AAPCC Meetings, 2001–2003
|
Types of Studies |
2001 |
2002 |
2003 |
Total |
(%) |
|
Case series/report |
110 |
93 |
93 |
296 |
40.1% |
|
Descriptive database review |
38 |
58 |
64 |
160 |
21.7% |
|
Pharmacokinetic |
8 |
2 |
3 |
13 |
1.8% |
|
Survey |
0 |
2 |
11 |
13 |
1.8% |
|
Cohort analysis |
26 |
19 |
19 |
64 |
8.7% |
|
Case-control study |
4 |
5 |
5 |
14 |
1.9% |
|
Uncontrolled clinical trial |
2 |
0 |
3 |
5 |
0.7% |
|
Historically controlled clinical trial |
0 |
1 |
1 |
2 |
0.3% |
|
Nonrandomized controlled clinical trial |
2 |
1 |
3 |
6 |
0.8% |
|
Randomized controlled clinical trial |
1 |
1 |
0 |
2 |
0.3% |
|
Survey or administration |
24 |
22 |
28 |
74 |
10.0% |
|
Education |
1 |
5 |
5 |
11 |
1.5% |
|
Cell culture/biochemical |
5 |
2 |
1 |
8 |
1.1% |
|
Whole organ or whole animal study |
12 |
13 |
9 |
34 |
4.6% |
|
Laboratory research/product analysis |
4 |
12 |
20 |
36 |
4.9% |
|
Total |
237 |
236 |
265 |
|
|
|
(%) |
32.1% |
32.0% |
35.9% |
|
|
|
SOURCES: Journal of Toxicology, Clinical Toxicology (2001, 2002, 2003). |
|||||
Several factors may limit research activity. First, the common sources of funding for center services (federal, state, or local funds) neither support nor require research, and there is no research requirement for AAPCC certification of poison control centers (American Association of Poison Control Centers, 1998). Second, federal funding for poison control center-based research is limited. Research focusing on toxicologic mechanisms or specific poisons can be funded via programs with a related focus, such as drug abuse (e.g., phencyclidine toxicity [Hardin et al., 2002, p. 1642]), mental health (e.g., antidepressant overdose [Pentel et al., 1995, p. 817]), or environmental safety (e.g., lead poisoning [Osterloh and Kelly, 1999, p. 1980]).
By contrast, research focusing on poison control center health services delivery has not been a focus of programs within the National Institutes of Health (NIH). A search of NIH program announcements for 2003 using the keywords “poison system,” “poison control,” or “poison center” revealed only one announcement specifically relevant to poison control center services, and that announcement involves bioterrorism preparedness (http://grants1.nih.gov/grants/guide/index.html). A search using the term “poison” revealed 18 other announcements, none of these dealing with poison control center services delivery but rather focusing on specific areas such as drug abuse (alcohol, inhalants), environmental toxicology, or alternative medicines (chelation therapy). A search of the Computer Retrieval of Information on Scientific Projects (CRISP) database of current NIH grants for 2003 using the same terms revealed none dealing with general poison control center services issues, one each involving the utilization of poison control center surveillance to monitor gamma-hydroxybutyrate toxicity or foodborne illnesses, and one regarding antidote design for venomous bites (http://crisp.cit.nih.gov/). This indicates that sources of funding for research about poison control center services or general management issues in toxicology (such as the use of activated charcoal for drug ingestions) are limited.
A third possible reason for limited research is that poison control center staff have extensive clinical or administrative responsibilities that reduce the time they have available for research. Moreover, the training of poison control center staff is predominantly clinical.
Public Education
The following is a general statement of the types of public education currently provided by the poison control centers. A detailed discussion is provided in Chapter 8.
Primary Prevention: Public Education
Poison control centers provide public education on poisoning prevention (Zuvekas et al., 1997). This education may be offered in collaboration with public health agencies, nongovernment organizations, or industry. The role of the centers is to provide expertise in poisonings; the collaborator provides expertise in injury prevention, as well as offering the infrastructure for public education (see discussion in Chapter 8).
Secondary Prevention: Utilization of Health Care Resources
A potential benefit of having poison control centers available to answer poisoning calls is the appropriate triage of patients to health care facilities when needed (improving patient care), and avoiding the use of health care facilities when not needed (reducing costs). Poison control centers provide public education focused on facilitating these outcomes, such as calling the center for poisoning questions or exposures rather than calling physicians’ offices.
HEALTH CARE PROFESSIONALS AND THEIR TRAINING BY POISON CONTROL CENTERS
Poison control centers provide education for many categories of health care professionals. A critical component of this education is the training of the health care professionals who actually work in or with centers. To better describe how this training is provided, we begin with a description of the personnel who staff centers and the range of activities they perform. Activities include medical direction, center management, telephone consultation, professional training, public education, and research. A discussion of the specific contributions of poison control centers to their training follows.
Health Care Professionals
A wide variety of health care and public health professionals contribute to the recognition, prevention, and management of poisonings. This section focuses on those who staff or interact directly with poison control centers, recognizing that many other types of individuals contribute to poison control efforts in other capacities.
The term toxicologist is a general description of an individual dealing with any aspect of acute or chronic poisonings, and it does not have a specific definition or implication with regard to training or job description. For example, this term may be used to describe individuals whose
activities range from molecular biology to epidemiology, as long as they deal in some way with the toxic effects of chemicals. The term clinical toxicologist implies a more clinical orientation, but likewise has no specific definition or implications. Medical toxicologists are physicians with specific training and board certification in the subspecialty of medical toxicology, which focuses on the care of poisoned patients.
Specialists in poison information are health care professionals (primarily nurses or pharmacists) who serve as poison control center staff with the primary responsibility of responding to telephone calls regarding poisoning exposures or requests for information. Poison information providers are individuals who may lack training in nursing, pharmacy, or medicine but serve in a similar capacity to SPIs within poison control centers, but with supervision by an SPI or a medical or managing director.
Medical Toxicologists
Medical toxicology is a subspecialty for physicians defined by the Accreditation Council for Graduate Medical Education (ACGME) as a “clinical specialty that includes the monitoring, prevention, evaluation and treatment of injury and illness due to occupational and environmental exposures, pharmaceutical agents, as well as unintentional and intentional poisoning in all age groups” (Accreditation Council for Graduate Medical Education, 2003). Medical toxicologists first complete training in any primary medical specialty (usually emergency medicine, occupational medicine, pediatrics, internal medicine, or pathology), and then an additional 2-year fellowship in medical toxicology (Wax and Donovan, 2000).
AAPCC requires a board-certified medical toxicologist as medical director as a condition of poison control center certification. In this capacity, medical toxicologists provide overall clinical supervision and medical backup of poison control center personnel and contribute to teaching, administrative, and research efforts within the center. Medical toxicologists also serve as consultants to centers, providing medical backup, teaching, or research expertise.
Common roles for medical toxicologists outside poison control centers include direct care or consultation regarding poisoned patients, teaching of medical toxicology fellows and other health care professionals, toxicology research, and medicolegal consultation. A smaller number of medical toxicologists work in various capacities in public health or government agencies, including CDC and the U.S. Food and Drug Administration, or in industry (Wax and Donovan, 2000).
Managing Direction
According to the AAPCC criteria for certification, the managing director of a certified poison control center provides “direct supervision of poison center staff, strategic planning, and oversight of administrative functions of programs (e.g., staff training, quality assurance, budgeting, etc.)” (American Association of Poison Control Centers, 1998, p. 6). A managing director with responsibilities for toxicological supervision must be board certified or board prepared in applied toxicology. This position can be filled by a physician, a pharmacist, or a nurse. In some centers the managing director is also the medical director.
Specialists in Poison Information
Specialists in poison information are the primary poison control center staff who answer telephones and respond to callers wanting information regarding poisonings. A 1998 survey of centers in the United States reported that SPIs were nurses (53 percent), pharmacists (40 percent), or physicians (3.5 percent) or had other backgrounds (2 percent) (Youniss et al., 2000). A certification process for SPIs is offered by AAPCC, allowing them to become certified specialists in poison information (these procedures are discussed in the section on quality assurance).
In addition to their primary role in answering poison control center telephone calls from the public and professionals, SPIs may supervise PIPs (staff with less advanced training in health care), serve administrative functions, conduct public or professional education, or participate in research projects. However, most SPI time is spent responding to telephone calls (75 percent) or handling administrative tasks (20 percent), with little time devoted to education (3 percent) or research (1 percent) (Zuvekas et al., 1997).
Poison Information Providers
Like SPIs, the primary role of PIPs is answering poison control center telephone calls from the public and health care professionals. PIPs differ from SPIs in that they lack training as nurses, pharmacists, or physicians, but rather have a variety of other health-related backgrounds. Because they have less advanced training in health care, PIPs working in AAPCC-certified poison control centers are required to do so under the onsite supervision of a CSPI or the managing or medical director of the center. The addition of PIPs to the more traditional use of SPIs to answer center telephones serves to enlarge the pool of providers available for such employment and to reduce costs.
Health Educators
Most poison control centers have a full- or part-time health educator whose primary role is education of the public regarding poisoning prevention and promotion of poison control center use. These efforts are often focused on the pediatric age group. In some centers, SPIs contribute to public education (Zuvekas et al., 1997). The role of health educators is discussed in more detail in Chapter 8.
Consultants
A wide variety of consultants provide additional capacity and expertise to poison control centers. Centers have medical toxicologists who serve as consultants to provide additional medical backup to SPIs and PIPs, to share on-call responsibilities with the medical director, or to contribute to teaching or research. In addition, poison control centers have consultants with expertise in specialized areas, such as veterinary medicine, herpetology, or mycology. These individuals are important to centers because it is not possible for their staff to have the detailed knowledge needed to manage the wide variety of poisonings encountered. Consultants typically volunteer their services and represent backgrounds as diverse as their subject matter.
Role of Poison Control Centers in Training Their Personnel and Other Health Care Providers
All poison control centers provide training for their own SPI and PIP staff because no other means of training is available. Clinical experience in the setting of a center is required for the training of medical toxicologists, and centers affiliated with such training programs are involved extensively in the education of these physicians. Thus, poison control centers play an essential role in the education of each of the major categories of center personnel and they also provide continuing medical education in their service area to health care professionals and to groups such as fire or police departments. Additionally, centers with affiliations or geographic proximity to training programs for physicians, nurses, dentists, pharmacists, or emergency medical technicians also provide some experience in toxicology as part of their training.
SPIs and PIPs
The training of both SPIs and PIPs is accomplished by the poison control center via lectures, assigned readings, observing center staff, par-
ticipating in hospital rounds, and responding to poison information or exposure telephone calls under supervision. There is no standard curriculum or published description for such training. AAPCC requires of certified poison control centers only that such training be under the supervision of the center medical director. SPI training takes from 3 months to a year to allow the SPI to answer center telephones independently (Committee briefings from Dart, 2003; Heard, 2003; and Trestrail, 2003).
Medical Toxicologists
Poison control centers provide an essential part of the training of medical toxicology fellows. ACGME specifically requires that accredited fellowship programs have an affiliation and geographic proximity to a poison control center for the clinical portion of their training. This center-based training includes answering telephones, providing medical backup to SPIs and PIPs, providing direct consultation to health care professionals calling the center, interacting with health care agencies that collaborate with or use the center, understanding center data collection and reporting, and gaining experience in center administration. A survey of medical toxicologists indicated that 46 percent of their clinical experience during training involved center-based activities (Wax and Donovan, 2000).
Currently, 12 poison control centers (ACGME-accredited programs) offer medical toxicology fellowships. In some cases, medical toxicology fellows spend time at a second center that serves a different geographic area or patient population or has staff with different expertise in order to gain a broader range of experience.
Clinical Toxicology Fellowships
Several poison control centers offer 1- or 2-year clinical toxicology fellowship training programs for clinical pharmacists (e.g., see http://www.pharmacy.umaryland.edu/pps/residents/toxicology.htm and http://www.hscj.ufl.edu/pharmacy/residency/index.html). There are no uniform criteria, curricula, or accreditation processes for such fellowships. The purpose of these fellowships is to prepare clinical pharmacists for careers focusing on the management of the poisoned patient, but their content may vary depending on the institution and the interests of the trainee.
Professional Continuing Education
Poison control centers provide professional continuing education in their service area. The type and extent varies greatly, reflecting the needs
of the community, the availability and funding of center staff, and the particular expertise of the staff (Zuvekas et al., 1997). Courses or individual lectures may be located at or near the poison control center, or in communities throughout the service area. The target audience may include physicians, nurses, pharmacists, emergency medical technicians, veterinarians, dentists, public health workers, or government employees who share responsibility for some aspect of poisoning prevention or management, such as HAZMAT responders. Poison control center staff often share the podium with other professionals at such conferences because the range and scope of toxicology is broad and collaboration with other professionals and agencies is an integral part of both center service and educational efforts.
Poison control center staff also contribute to professional continuing education via publications, including editing toxicology textbooks, writing book chapters or review articles, contributing sections to references such as Poisindex®, and preparing review or teaching documents for government agencies such as ATSDR.
Education of Other Health Care Professionals
Poison control centers contribute to the education of a wide variety of health care professionals, including medical, nursing, pharmacy, and dental students; medical and pharmacy residents and fellows; and EMTs. Training may include rotations through the centers where they observe or assist with call management or information retrieval, lectures in formal courses, or the participation of poison control center personnel in hospital rounds. Education of these trainees is important as a means of disseminating standards of care for the poisoned patient, and in creating interest in this field among younger trainees who might later choose to obtain further training in toxicology or careers involving poison control centers.
Poison control center education of trainees also contributes to the scope of their education. However, there are many more training programs for health care professionals than there are poison control centers, and not all training programs are located near a center. Thus the extent to which poison control centers contribute to the education of health care professionals varies greatly (Zuvekas et al., 1997). For example, a survey of emergency medical technician training programs showed that 81 percent of such programs had access to a regional poison control center, and 11 percent offered rotations in centers to trainees (Davis et al., 1999). Where such relationships are established, poison control centers can contribute to the education of health care professional students, residents, or fellows through lectures incorporated into their required courses (e.g., a lecture on management of overdose as part of a pharmacology course for
medical students), as clinical rotations in which students spend time in the center, or as participants in center research projects. This form of poison control center educational involvement is not mandated for any health care professional training (other than that of medical toxicologists).
QUALITY ASSURANCE
There are both external and internal evaluation mechanisms for assuring the quality of poison control centers. Externally, a certification process is offered by AAPCC for poison control centers or systems (see Box 5-2), defined as two or more poison control centers functionally and electronically linked to provide services (http://www.aapcc.org/MEM-BERS/center.htm). Fifty-two of the existing 63 poison control centers in the United States are currently certified. Although certification is voluntary, some funding sources (e.g., states, HRSA) require AAPCC certification as a condition of funding. The key elements of certification are as follows:
-
Providing free 24-hour-a-day, 365-days-a-year telephone service to a defined geographic area designated by the involved state(s) in order to respond to calls from the public and health professionals regarding poisoning exposures or information;
-
Offering access to hearing-impaired and non-English-speaking callers;
-
Providing staffing by qualified SPIs, PIPs, a managing director, and a medical director, and other medical backup as needed;
-
Achieving a minimum penetrance of 7 human poison exposure calls per 1,000 population served each year;
-
Developing comprehensive public and professional education plans;
-
Submitting all exposure data to the TESS database;
-
Having written operational guidelines and a disaster plan;
-
Providing quality assurance monitoring; and
-
Maintaining current institutional membership in AAPCC.
In addition to certifying centers, AAPCC provides the certification process for SPIs, allowing them to become certified specialists in poison information. To be eligible for this certification, a SPI must be trained as a nurse, pharmacist, or physician, and must acquire experience at a poison control center, consisting of 2,000 hours answering poison information or exposure calls, and 2,000 calls answered. One AAPCC requirement of certified poison control centers is that all SPIs acquire CSPI certification within 2 years of achieving eligibility. AAPCC considers certification by the American Board of Applied Toxicology to be an acceptable alternative
|
BOX 5-2 Provide evidence that the center/system adequately serves its entire region. Where multiple states are involved, designation from each state is necessary. Where a state declines to designate any poison center/system, designation by other political or health jurisdictions may be an alternative. In instances where more than one center or system is designated to serve the same area, evidence of cooperative arrangements must be provided. Direct incoming telephone system that is extensively publicized throughout the region to both health professionals and the public. Must use AAPCC nationwide toll-free number (1-800-222-1222). May not impose a direct fee to individual members of the lay public (either by direct billing or pay-for-call services) for emergency calls received within its region. Must be able to respond to inquiries in languages other than English as appropriate to the region. Access for hearing-impaired individuals must be provided. A plan to provide poison center services in response to natural and technological disasters must be in place. Provide a Medical Director certified by the American Board of Medical Toxicology. Medical Director full-time equivalent to be determined by call volume. Staff certification and roles are as follows: For certification of center, 50 percent of staff must have passed exam. Provide triage and treatment for individual calls. Provide follow-up at appropriate intervals, validate cases, provide caller education. Obtain specific data for data collection and poison prevention. Provide education for other health care providers. Provide poison prevention education for public. Collect prehospital care and triage data; some hospitalized data may be obtained, but this is primarily the role of the Medical Director. A managing director with toxicological supervision must be board prepared or board certified. For physicians the board can be ABMT or ABMS; for non-physicians the board must be ABAT. SOURCE: American Association of Poison Control Centers (2003a, pp. 16–23). |
to CSPI certification to satisfy this requirement or, for physicians, certification in medical toxicology by the American Board of Medical Toxicology or American Board of Medical Specialists.
Internally, poison control centers have instituted programs consisting of case reviews, call monitoring, and other measures designed to evaluate
the quality of service provided (McGuigan, 1997). A quality improvement program focusing on “high risk, high volume or problem-prone cases” is required for AAPCC certification of poison control centers (American Association of Poison Control Centers, 1998). Centers collect data through callbacks to individuals or to the health care facility caring for them to assess outcomes of cases (Zuvekas et al., 1997).
Data are limited regarding the evaluation of poison control center performance for the purposes of ongoing quality assurance of case management, assessing the impact of the larger poison control system, or assessing various poison control strategies. Most such data (reviewed in Chapter 6) focus on poison center utilization or cost-effectiveness, specifically the role of poison control centers in reducing health care costs by reducing unneeded emergency department or primary care visits. Some studies have examined the performance of poison control center personnel in managing structured simulated cases (e.g., Thompson et al., 1983). This mechanism potentially could be used for ongoing quality control of poison control centers, but has not been specifically studied for this purpose. Essentially no data are available regarding the impact of poison control centers, individually or in aggregate, on health outcomes (morbidity or mortality). The lack of such data is partly because of the following factors:
-
The incompatibility of existing databases (nonuniform methods of data collection, disease definitions, and reporting) that makes population-based data collection and evaluation difficult;
-
Low rates of some outcomes such as mortality from poisonings, as well as the wide variety of types of poisonings managed by poison control centers, such that very large samples are needed to examine trends or make comparisons; and
-
A lack of funding for outcomes-based quality assurance activities or research, and the resulting lack of data on whether these are feasible or how to accomplish them.
Data regarding the effectiveness of poison education by poison control centers are discussed in Chapter 8. As with poisoning management data, these are largely limited to intermediate outcomes, such as the retention of the education messages or short-term changes in behaviors (e.g., safe storage of hazardous household products), rather than to health outcomes, such as a reduction in incidence of poisoning, morbidity, or mortality.
OPPORTUNITIES
-
Poison control centers have developed an infrastructure to respond to calls from the public or professionals regarding poisoning exposures or to obtain information about poisonings. This infrastructure has been adapted successfully to respond to HAZMAT incidents, and is now being further developed to contribute to all-hazards emergency preparedness and response, including biological or chemical terrorism. The latter role represents a significant opportunity to use the unique capabilities and expertise of poison control centers to support our national capacity to prevent, recognize, or respond to such incidents.
-
There are few specific funding opportunities available for research regarding poison control center services delivery. Dedicated funding for such studies, and for analysis of the data generated by poison control centers, would provide important and much needed information for the further development of poison prevention and control programs.
-
A certification process exists for poison control centers and for SPIs to become CSPIs; however, there is no certification for PIPs. Development of certification for PIPs could help to assure the competence of this expanding role. Certification of SPIs is currently the responsibility of the professional organization (AAPCC) to which these same individuals belong and which represents their interests. Certification of poison control centers is also the responsibility of AAPCC. Poison control centers are in fact required to join AAPCC to become certified. AAPCC assumed this dual role of professional organization and certifying body out of necessity because no other agency expressed an interest in acquiring the required expertise or developing such a process. A more common model for certification of health care professionals or programs is for certification to be the responsibility of an independent agency, rather than an organization to which the applicants belong. For example, medical toxicologists are certified by the American Board of Medical Specialties rather than by a toxicology organization. With the continued development of poison control centers and their increased integration into the public health system, alternative certification processes may offer advantages over the current system. Certification of centers, SPIs, and PIPs by an independent organization would offer greater independence of the process from the participants, wider input from the health care community, and wider recognition of their skills and contributions.
SUMMARY
Poison control centers perform a wide variety of activities related to the prevention, recognition, and management of poisonings. The types of
poisonings addressed include commercial products, medications, drugs of abuse, plants, venomous animals, industrial chemicals, and potential agents of bioterrorism. Because accessibility is widely publicized and available around the clock and free, centers are used extensively as sources of information or advice regarding actual or potential poisoning exposures. Poison control centers may also be accessed when the nature of the exposure (e.g., chemical versus infectious agent) is uncertain, and perform a triage function by either providing information or referring the call to an appropriate agency. Poison control centers have evolved a common set of activities to deal with these needs, primarily centered around telephone lines staffed by specialists with training in clinical toxicology and backed up by medical toxicologists, a wide range of consultants, and extensive collaborations with public health agencies and first responders. Complementary educational efforts are also offered by most poison control centers. Some centers provide training of medical toxicology residents, research, surveillance to detect emerging syndromes or bioterrorism events, or contracts to provide information services to industry.
Both the core activities shared by most poison control centers and the additional activities offered by some centers fill distinct needs in the nation’s public health system. Opportunities for enhancing poison control center effectiveness exist in the potential for further expansion of efforts in the area of emergency preparedness and response. There is a need for funding to support data analysis and research regarding center services delivery and further development of the certification process for SPIs and PIPs.
Appendix 5-A
Case Studies of Poison Control Centers in Emerging Health Situations
Three brief examples are provided. The first focuses on the development of cooperative arrangements between a poison control center and other local and state organizations involved in preparedness. The second provides general steps taken by a poison control center in response to calls about anthrax. The third illustrates the interaction between a poison control center and other health care agencies in diagnosing a threat and providing a response.
ROCKY MOUNTAIN POISON AND DRUG CENTER: INTEGRATION INTO PUBLIC HEALTH SYSTEM
The Rocky Mountain Poison and Drug Center (RMPDC) is the designated regional poison control center for Colorado; Montana; Las Vegas, Nevada; Idaho; and Hawaii. RMPDC is the coordinator for the Metropolitan Medical Response System (MMRS) for Denver County and works with the Denver Health Center for Public Health Preparedness. RMPDC’s ability to bring groups together as a neutral third party within a competitive health care market led to its selection as the coordinator for the MMRS in 1997. RMPDC personnel are members of the HRSA-supported hospital preparedness advisory committee and work closely with the activities established via the CDC’s Public Health Preparedness and Response for Bioterrorism Cooperative Agreement with the state of Colorado.
Specific public health preparedness activities undertaken by RMPDC include:
-
Establishment of a set of emergency response procedures for call center workers, located on workstation desktops.
-
Use of the nurse advice line to assist Denver Health with syndromic surveillance.
-
Use of the nurse advice line to assist Denver Health with handling calls from the public regarding public health topics, including emerging problems, smallpox vaccination, and West Nile virus.
-
Creation of stockpiles of antidotes and ability to survey for inventory levels of local/regional supplies of antidotes.
-
Involvement in drills within Colorado (but not with other states served by RMPDC), including TOPOFF (top officials).
-
Provision of training, including development of Web-based training modules in emergency preparedness and response.
TEXAS: ANTHRAX CALLS
(Note: The following is based on material provided to committee by Doug Borys, Director, Central Texas Poison Control Center; also, an article on anthrax calls to the Texas Poison Control Center is forthcoming, which will be authored by M. Forrester.)
The Texas Poison Control Center’s (TPCC’s) response to bioterrorism is focused on three areas: incident response, emergency preparedness, and professional and public education. Under incident response, TPCC reported receipt of hundreds of calls during the 2001 anthrax attack. Medical staff at TPCC wrote a public education piece on anthrax that was distributed on state and other Internet sites, and copies were distributed to health care providers and the public throughout Texas. Local emergency preparedness activities include the participation of TPCC staff in emergency planning committees of their own host institution, the city in which they are located, and in groups located throughout the state of Texas. At the state level, TPCC staff are members of the following organizations:
-
Texas Department of Health, Hospital Preparedness Planning Committee
-
Texas Department of Health Preparedness Coordinating Council
-
Texas Institute for Health Policy Research, Policy Advisory Committee, Disaster Response Project
-
Texas Medical Association, Bioterrorism Task Force
Also, the West Texas Poison Center serves as an active member of the El Paso/Ciudad Juarez-binational local emergency planning committee.
In terms of professional and public education, staff members of the six TPCCs are involved in a variety of terrorism-related panels, programs, and lectures, including:
-
Chaired and lectured on a panel on biochemical weapons and the Latino community in Washington, D.C., at a national Latino health leadership conference.
-
Served as regional director of advanced HAZMAT life support course (Texas, Louisiana, Oklahoma, and Arkansas) that included chemical terrorism preparedness; medical director for several courses.
-
Participated in dozens of training sessions related to weapons of mass destruction (non-Advanced HAZMAT Life Support).
NORTHERN NEW ENGLAND POISON CENTER: ARSENIC EXPOSURE1
The Northern New England Poison Center (NNEPC) received a call from a rural hospital in the northeast corner of Maine requesting epidemiological assistance with what hospital staff thought was an outbreak of infectious disease or foodborne illness. One hour later, the hospital called the NNEPC staff on the poison control center hotline for information regarding the possibility that this incident involved poisoning—not an infectious disease or foodborne illness outbreak.
The staff reviewed potential causes and requested that the beverage and foods potentially linked to the exposures be secured for later evaluation, and paged the center’s two boarded toxicologists for consultation. More patients had presented to the rural emergency department for treatment of severe symptoms of dehydration and hypotension. The most serious cases were transferred to a larger hospital. A differential diagnosis of possible toxins, including arsenic, paraquat, and ricin, was discussed and laboratory evaluation arranged with the state Environmental Testing Lab. A diagnosis of arsenic was confirmed and supported. AAPCC called NNEPC to investigate because all NNEPC cases had been automatically uploaded to TESS in Washington, DC. AAPCC notified CDC and the Department of Homeland Security.
NNEPC and the Maine Medical Center, the poison control center’s host institution, had developed mechanisms for locating and delivering antidotes throughout the state. After September 11, 2001, NNEPC developed a state antidote stockpile to provide initial doses of antidotes for attacks with weapons of mass destruction. The state police and a plane normally used to transport critically ill patients transported the antidotes. NNEPC staff provided antidote administration and dosing guidelines to the clinicians involved in treatment, and worked at the treating hospital regarding emergency use of unapproved drugs. The center developed information materials for the health care professionals involved in treatment to help explain the therapy to patients and to obtain legal consent, as well as fact sheets for patients and their families to explain the effects of acute arsenic poisoning. At the request of treating health care professionals, NNEPC drafted a letter outlining appropriate monitoring and admission/discharge information. This information was used to guide physician management and satisfy insurers, who were calling the hospitals daily.
Multiple media requests were made of NNEPC. Toxicologists provided more than 20 interviews discussing arsenic toxicity in general and used the opportunity to raise awareness of unrelated but regionally significant chronic arsenic exposure through well water. The center staff followed these patients over subsequent weeks.
During this time, the poison control center continued to manage approximately 100 other hotline calls daily, and the publicity of the cases led to an increased number of calls about food poisoning and potential chronic heavy metal exposure. Information will be shared with the Maine Bureau of Health and the involved hospitals to furnish data that will be useful to others treating patients poisoned with arsenic in the future.






























