5
Options for Financing and Delivering HIV Care
Building on the findings and conclusions of previous chapters, the Committee considered a range of alternative approaches in developing its recommendations for improving the public financing of HIV care. This chapter presents the Committee’s analysis of the different options, while focusing on the concept of “Centers of Excellence” as a recommended method for improving HIV care.
The Committee considered a range of alternative approaches in developing its recommendations for improving the public financing of HIV care. Most of the approaches build on existing financing programs. One approach would expand the Ryan White Comprehensive AIDS Resource Emergency (CARE) Act. Another would expand Medicare to cover individuals with HIV infection. Three approaches would give states options for expanding their Medicaid programs to cover low-income individuals who have HIV but are not currently eligible. One of these approaches would facilitate Medicaid coverage through Section 1115 demonstration waivers; the other two would create a new optional Medicaid eligibility category of individuals with HIV, but with varying federal matching rates. The remaining approaches would create new federal programs. One would establish a federal block grant to allow states to purchase services for individuals with HIV. The other would establish a federally funded, state-administered entitlement to care for low-income individuals with HIV.
Each of these seven approaches was considered in light of the Committee’s goal to develop a comprehensive vision of a system of care that is accessible and efficient and that meets accepted standards of quality and
accountability for individuals with HIV who rely on public programs. From this goal, the Committee derived five assessment criteria:
-
Eligibility: Does the approach include a minimum, uniform standard for eligibility that ensures that low-income individuals with HIV (i.e., individuals with incomes at or below 250 percent of the federal poverty level, or FPL) have coverage for recommended services regardless of the state in which they reside?
-
Benefits: Does the approach include a benefit package that meets the standard of care for HIV/AIDS and that is uniform for all eligible individuals?
-
Provider reimbursement: Does the approach include payment rates that are adequate to enable providers to furnish services commensurate with the standard of care for HIV/AIDS?
-
Financing: Does the approach include a financing mechanism that is capable of supporting eligibility, benefits, and provider payment elements that meet the Committee’s criteria and that is stable over time?
-
Integrated and coordinated services that foster accountability: Does the approach include the integration and coordination of services that allows for administrative arrangements that are efficient and that support program accountability and evaluation?
The Committee applied these assessment criteria to each of the alternative approaches. The Committee’s findings are summarized in Table 5-1. The remainder of this chapter sets forth the Committee’s analysis of the advantages and disadvantages of these alternative approaches in light of these criteria. The recommendations that flow from this analysis are set forth in Chapter 6.
In the Committee’s judgment, the alternative that best fits the assessment criteria is a new federally funded, state-administered entitlement program for low-income individuals with HIV.
The Committee recognizes that the alternatives examined here do not represent the universe of policy options for financing and delivering HIV care. The Committee selected these particular options as broadly illustrative of the alternatives that federal policy makers are likely to explore given the current configuration of federal and state programs described in Chapter 3. For example, the most recent significant health care eligibility expansion at the federal level was the State Children’s Health Insurance Program (SCHIP), enacted in 1997. Although this program is targeted at a much different population than that to which this report is addressed, the structural features of SCHIP reflect some important policy preferences. The Committee therefore modeled one of its illustrative approaches on SCHIP.
The Committee notes that, in each approach presented (excluding the Medicare option), state participation is optional. In theory, the federal
TABLE 5-1 Alternative Options for Financing HIV Care by Assessment Criteria
|
Option |
Minimum Uniform Eligibility Rules for Individuals with HIV |
Benefit Package Meets Standard of Care for HIV/AIDS |
Provider Reimbursement Is Adequate to Standard of Care for HIV/AIDS |
Financing Mechanism Is Adequate to Standard of Care for HIV/AIDS over Time |
Integrated and Coordinated Services Fostering Accountability and Evaluation |
|
1: Expand Ryan White CARE Act |
No |
No |
— |
No |
No |
|
2: Medicare Eligibility for HIV |
Yes |
No |
Yes |
Yes |
Yes |
|
3A: Medicaid Budget-Neutral Waiver Expansion |
No |
No |
No |
No |
Yes |
|
3B: Medicaid Optional Eligibility, Regular Match |
No |
No |
No |
No |
Yes |
|
3C: Medicaid Optional Eligibility, Enhanced Match |
No |
No |
No |
No |
Yes |
|
4: Block Grant to States |
No |
No |
No |
No |
No |
|
5: New Federally Funded, StateAdministered Entitlement |
Yes |
Yes |
Yes |
Yes |
Yes |
government could attempt to require state participation in a program responding to a national epidemic, perhaps by conditioning the flow of federal grants-in-aid for highway construction or education upon state participation. However, the Committee believes such an approach does not merit consideration. Most states are currently experiencing substantial revenue shortfalls, and there is evidence that the imbalance between the demands on state budgets and available revenues is not temporary, but structural (Boyd, 2003). In these circumstances, reliance on any measure of required state financial participation seems to the Committee to be highly problematic. More fundamentally, forcing state participation would gener-
ate political tensions between federal and state governments that could compromise the accomplishment of the Committee’s objective: the financing of an accessible, efficient system of care for low-income individuals with HIV that meets accepted standards of quality and accountability.
FINANCING OPTIONS
Option 1: Expand Ryan White CARE Act
Under this approach, the Ryan White CARE Act programs discussed in Chapters 1 and 3 would be continued as currently structured, but annual appropriations would be increased to enable all CARE Act programs, ranging from Title I to Title IV, to expand their capacity to meet the medical and support service needs of low-income individuals with HIV.
Advantages
The primary advantage of working through the existing CARE Act programs is that these programs are already operational and have a track record of providing access to care for the uninsured and the poor. Since 1990, CARE Act programs have played a pivotal role in developing and strengthening the health care delivery infrastructure for individuals with HIV/AIDS. Though a substantial proportion of CARE Act funding is spent on medical treatment and drugs, a large proportion (27 percent) is also spent on local-level support services that are critical for individuals with HIV (GAO, 2000) but are often not covered by other programs (Levi and Kates, 2000).
This approach also has administrative advantages. The planning process within the Ryan White CARE Act is designed to allow local level flexibility in determining where funding should be directed. Planning councils established under Title I of the CARE Act are charged with monitoring local trends and assessing annual funding needs. These administrative structures provide the opportunity to address population-level issues and build capacity for services such as substance abuse treatment or outreach to immigrants. The planning process also allows members of the local community to have a voice in how funds are allocated and services are delivered.
Disadvantages
There are several disadvantages to an approach that relies on an expansion of the CARE Act. The first relates to eligibility for services, which now varies significantly from one state to the next and from one city to the next. As a “safety net program,” the CARE Act supplements other HIV/AIDS programs in a state or locality, most notably Medicaid; in practice, this
results in CARE Act programs with widely different eligibility criteria. This variation is inconsistent with a uniform, minimum standard of eligibility.
Similarly, CARE Act benefits vary substantially from state to state, for many of the same reasons that eligibility standards vary. Access to life-extending comprehensive antiretroviral therapy also varies significantly by state. Individuals in one state may be ineligible because of income level or have access to a fewer number of drugs or types of drugs than an individual with the same disease status in another state. This variation is also inconsistent with access to the standard of care for HIV/AIDS regardless of state of residence.
Another disadvantage of this approach concerns financing. As a discretionary program, the CARE Act program is subject to the uncertainties of the annual congressional appropriations process. States, localities, and private providers cannot predict with any confidence that the funds required to meet the standard of care for those with HIV in need of program assistance will be available in any given fiscal year. Currently, CARE Act dollars do not match the need for services, and some grantees have been unable to serve all those in need. Budget shortfalls for the AIDS Drug Assistance Program (ADAP) in particular have resulted in waiting lists, caps on enrollment, and/or limitations on benefits available to individuals already in the program. Although an expansion of federal appropriations consistent with this proposed approach could, if enacted, annually address these shortfalls, this would not resolve the related problem of allocation.
The community planning process associated with CARE Act Title I funds has provided important community input into how funds are allocated at the local level. This process does not, however, necessarily result in funding allocation decisions that reflect the greatest areas of need over time. This is partly because of inadequate and inconsistent data sources and measures used to describe severity of need for the Title I Supplemental Application (IOM, 2003b). Furthermore, current program data collection activities do not adequately support accountability or evaluation. It is currently impossible to determine national estimates of the number of clients served or the types of services received because programs do not provide unduplicated counts of clients and the services they receive. In short, there is no guarantee, even if the necessary funds were actually appropriated each year, that these funds would be allocated in a manner that enables the standard of care for HIV/AIDS for all those in need of public program assistance in each state.
Option 2: Extend Medicare to Individuals with HIV
Under this approach, individuals found to be infected with HIV would be eligible for Medicare coverage, subject to the same premium, deductible, and coinsurance requirements as other Medicare beneficiaries. This approach
would parallel the current coverage of individuals with end-stage renal disease (ESRD), who qualify for Medicare benefits even though they do not otherwise meet the Medicare eligibility requirements applicable to the aged (i.e., 65 or over and 40 quarters of payroll tax contributions) or the disabled (have received Social Security Disability Insurance payments for 24 months due to total and permanent disability) (CMS, 2003).
Advantages
This approach has four principal advantages. First, because Medicare is a national program, and because the presence of HIV infection is a standardized medical determination, this approach would ensure coverage of individuals with HIV infection regardless of the state in which they reside. Moreover, this approach would qualify an individual for coverage upon a medical determination of HIV infection, without a waiting period and without a disability determination or a financial means test.
Second, while the adequacy of Medicare payment rates for hospital, physician, and laboratory services is the subject of continuous analysis and political debate, there is little question that most providers participate in the program (MedPAC, 2003). In the Committee’s judgment, Medicare payment rates, as a general matter, would be adequate to enable providers to furnish services commensurate with the standard of care for HIV/AIDS.
Third, this approach offers sources of financing—federal payroll tax revenues (Medicare Part A), federal general revenues (Medicare Part B), and beneficiary premiums (Medicare Part B)—that are as broad in scope as the epidemic itself. These financing sources, while not without their challenges, are substantially more stable than the revenue bases of individual states, many of which are ill-equipped to absorb their portion of the costs of a national epidemic.
Finally, this approach relies on existing administrative structures that, while not without their shortcomings, are relatively efficient and have created a high level of uniformity in how the program is operated. The program’s national data collection requirements also allow for tracking, monitoring, and reporting on the program. To supplement the data systems and administrative capacity of the Centers for Medicare and Medicaid Services (CMS), the Congress has established an independent agency, the Medicare Payment Advisory Commission (MedPAC), the mission of which is to monitor, evaluate, and report on the operation of the Medicare program on a continuous basis. Program accountability is promoted by oversight from the Government Accountability Office (GAO) and the Office of Inspector General (OIG) of the Department of Health and Human Services (DHHS).
Disadvantages
Extending Medicare eligibility to individuals infected with HIV has two major disadvantages. First, because Medicare is a social insurance program and not a means-tested entitlement, it does not lend itself to a national program that focuses on low-income individuals with HIV. Just as Medicare now covers all individuals determined to have ESRD without regard to income or resources, so under this approach would Medicare cover all individuals with HIV without regard to income or resources. While the Committee does not object to universal eligibility in principle, the Committee recognizes that federal resources are limited, and that in the long run Medicare’s ability to finance current benefits is questionable (as of this writing the Medicare Part A Trust Fund is projected to remain solvent through 2026). In the Committee’s judgment, the federal resources potentially available to address the national HIV epidemic cannot realistically sustain an approach that offers universal eligibility of infected individuals through Medicare.
The second major disadvantage relates to Medicare’s benefits. As currently configured, Medicare’s benefits package does not include a number of services that are essential to the standard of care for HIV/AIDS, including outpatient prescription drugs and case management services. The current lack of coverage for HAART is especially problematic. As the Committee deliberated and reached its conclusions, the President signed into law the Medicare Prescription Drug, Improvement and Modernization Act of 2003 (MPDIM) (P.L. 108-173). One of the major features in the law is a prescription drug benefit (Medicare Part D, planned to take effect January 1, 2006) that allows beneficiaries to choose a drug benefit plan (the number of plans to choose from will vary by region). The standard benefit package of a Medicare Part D plan requires a $250 deductible, an average premium of $35 per month, and copayments. It offers coverage of 75 percent of prescription drug costs up to $2,250, no coverage for the next $3,600 in drug costs, and 100 percent coverage of costs above $5,850. Deductibles, premiums, copayments, and coverage thresholds are linked to inflation and will rise as time goes on. For individuals whose incomes are below 150 percent of FPL, cost-sharing and premium assistance is available and the $3,600 gap in coverage does not apply. This assistance does not reach those with incomes between 150 and 250 percent of FPL, however, leaving them with out-of-pocket drug costs that the Committee believes to be unacceptably high for individuals with HIV/AIDS. In addition, the new legislation requires that plans offer medications from each class of drugs, but state plans do not have to offer every drug within a class. Since treatment for HIV requires multiple drugs within a class and treatment regimens must be altered with some frequency, this leaves individuals with HIV vulnerable to
high, uncovered costs if all of the required drugs are not on the plan’s formulary (Kates, 2004).
Even with Medicare Part D supplying coverage of prescription drugs, the Medicare benefits package remains inadequate to the task of providing the standard of care for HIV/AIDS for low-income individuals. HAART therapy alone is not sufficient. The management of HIV/AIDS requires not only therapeutic services but also attention to the patient’s social and environmental circumstances to conserve levels of independence and slow the progression of disease and disability. Patients with HIV/AIDS, especially those with co-morbid conditions, require care from multiple clinicians and multiple systems. In addition to HAART and other drug therapies, a number of adjunct services and interventions have been identified as essential to the care process and necessary for optimal reductions in the rates of infection of HIV/AIDS. These services include but are not limited to primary medical care services (Ashman et al., 2002), substance abuse treatment (Turner et al., 2001), mental health services (Ashman et al., 2002; Davis, 2002), prevention counseling for the infected population (IOM, 2001a), and medical and social case management services (Laine et al., 1999; Ashman et al., 2002; Lo et al., 2002; Levi, 2002).
The current Medicare benefits package does not incorporate all of these services. Expanding the Medicare benefits package to include these services for all beneficiaries would represent a historic program expansion. Restructuring the benefits package just for one group of beneficiaries defined by HIV infection would represent a fundamental break from the Medicare program’s long-standing commitment to offering a uniform national benefit to all eligible individuals.
Option 3: Extend Medicaid to More Individuals with HIV
As discussed in Chapter 3, Medicaid is currently the nation’s largest source of public financing for HIV/AIDS care. The Committee considered three approaches to extending Medicaid to other individuals with HIV who are not currently eligible for the program. All three of these approaches are optional with the states, in recognition of the strong opposition on the part of many state policy makers to federal requirements. The approaches vary significantly in terms of potential cost to the federal government. The first is budget-neutral, the second would apportion the costs of HIV/AIDS care between federal and state governments as under current law, and the third would increase the federal financial responsibility. A discussion of each approach follows.
Option 3A: Budget-Neutral Medicaid Expansion
Under Section 1115 of the Social Security Act, the Secretary of Health and Human Services (the Secretary) has the authority to waive certain requirements of federal Medicaid law to enable states to engage in demonstrations that are likely to assist in promoting the objectives of the Medicaid program while continuing to receive federal Medicaid matching funds. Currently, Massachusetts, Maine, and the District of Columbia have been granted Section 1115 demonstration waivers to provide coverage to low-income individuals in the early stages of HIV disease, although Maine has not yet implemented its waiver (Shirk, 2003; Kates, 2004). Under this approach, the Secretary would set forth specifications for a national Section 1115 demonstration initiative to cover low-income individuals with HIV who otherwise would not be eligible for Medicaid prior to the onset of disability. The specifications would provide for uniform eligibility standards and a benefit package that meets the standard of care for HIV/AIDS, as well as a budget-neutrality test less stringent than applied currently (e.g., rather than focusing solely on federal Medical savings, the Secretary in applying the budget neutrality test could also consider savings to other federal programs). States seeking to operate a demonstration program consistent with the specifications and able to demonstrate budget neutrality would have their waiver applications processed and approved on an expedited basis. As under current law, the demonstrations would be subject to independent evaluation.
Advantages
The primary advantage to this approach is administrative. It would streamline the process of applying for and approving Section 1115 waivers, at least insofar as it applies to demonstrations involving low-income individuals with HIV who are not disabled by the disease and therefore ineligible for Medicaid. Making these waivers more readily available to states would in effect make federal Medicaid matching funds more available to assist them in meeting the treatment costs of this population. This approach would also allow for the addition of ancillary services such as substance abuse treatment and case management that would not necessarily be offered under a straight Medicaid expansion. In addition, because Section 1115 waivers by definition involve demonstrations, this approach maximizes the opportunity for the comparative evaluation of state coverage initiatives for this population.
Disadvantages
This approach has a number of disadvantages. First, although it specifies a uniform eligibility standard for state demonstrations, it does not ensure that all states would implement such waivers and adopt such eligibility policies. Similarly, although this approach specifies a uniform benefits package that meets the standard of care for HIV/AIDS, it does not ensure that all states would implement such waivers and establish such benefit packages. This approach is silent on the issue of provider reimbursement rates, which tend to be low in relation to the cost of caring for individuals with complex conditions like HIV/AIDS. In states where rates are low, however, raising them significantly would likely make it difficult for the state to satisfy the budget-neutrality requirements. Finally, this approach leaves Medicaid’s current federal–state financing arrangements in place. Thus, the federal government’s share of any state’s cost of treating individuals with HIV would vary inversely with the state’s per capita income, from a minimum of 50 percent to a maximum of 77 percent. State per capita income has no apparent relationship to the demands that the HIV epidemic places on any given state or to a state’s fiscal capacity to respond to the epidemic. Moreover, while Section 1115 demonstration projects must be budget neutral from the federal government’s standpoint over a five-year period, this does not necessarily ensure budget neutrality in state expenditures in any given year. In light of the current fiscal circumstances of most states, it seems unlikely that a majority of states would be willing to assume the risk that these demonstration projects might require additional state funds, at least in the short run.
Option 3B: Optional Medicaid Eligibility Group
Another approach would allow states to extend Medicaid coverage to low-income individuals with HIV who otherwise would not be eligible for Medicaid without obtaining a demonstration waiver or maintaining budget neutrality. Instead, states would be allowed to amend their state Medicaid plans to cover a new optional category of low-income individuals infected with HIV. (Conceptually, this parallels the current state option to cover individuals infected with tuberculosis.1) A minimum eligibility standard
would be established at 250 percent of the federal poverty level. The costs of this eligibility expansion would be matched by the federal government at the same rate as the costs of most other eligibility groups (e.g., 50 percent to 77 percent depending on state per capita income). States electing this option would be required to offer the full range of current Medicaid benefits to individuals enrolling under the expansion. Current Medicaid rules governing provider reimbursement rates would continue to apply.
Advantages
Relative to Option 3A, this option would make it significantly less difficult for states interested in expanding coverage for low-income individuals with HIV to obtain federal Medicaid matching funds to defray the costs of such coverage. States would not have to demonstrate to the Secretary of HHS that the federal government would not spend more over a five-year demonstration period than it would if the expansion did not occur. Instead, this option would make additional federal matching funds available to states willing to put additional funds of their own into such an expansion. In those states electing the option, a uniform standard for eligibility could be achieved, and the benefits provided to individuals with HIV would at least meet the standard of care offered currently under Medicaid programs.
Disadvantages
As in the case of Option 3A, this approach has a number of disadvantages that stem from its optional nature and the current fiscal pressures on the states. If all states were to elect this option, a minimum uniform standard of eligibility would be achieved but variations in the scope of benefits would continue. However, given the revenue shortfalls being experienced by most states, widespread state participation in an option that involves the outlay of additional state funds seems unlikely. Even in those states that elect to cover this optional group, low provider reimbursement rates may constrain provider capacity to meet the standard of care and may limit participation by providers qualified to do so. Moreover, individuals enrolled under this expansion would have access only to those benefits offered under the state’s existing Medicaid program, which may not provide coverage for the ancillary services necessary for optimal HIV care. Finally, this option does not alter the current distribution of financial responsibility between the federal government and the states. Although the HIV epidemic is national in scope, the federal government’s share of the costs of treating individuals infected with HIV under this approach would vary from state to state, from a low of 50 percent to a high of 77 percent, depending on the state’s per capita income. Many states, regardless of their relative per capita
incomes, will find it difficult to generate their share of the costs of an eligibility expansion in the face of revenue shortfalls.
Option 3C: Optional Medicaid Eligibility Group with Increased Federal Match
This approach follows Option 3B, with one exception. As in Option 3B, states would be allowed to amend their state Medicaid plans to cover a new optional category of low-income individuals infected with HIV. States electing this option would be required to cover individuals with incomes up to 250 percent of the FPL and to furnish benefits to such individuals that meet the current scope of benefits offered under Medicaid. States could continue to use their existing provider reimbursement rates. Unlike Option 3B, however, the costs of covering this new optional group would be matched by the federal government at an enhanced rate ranging from 65 to 84 percent, depending on state per capita income. (In this regard, this approach parallels the current law option for covering uninsured women diagnosed with breast or cervical cancer.2)
Advantages
This approach has the same advantages compared with Option 3A as does Option 3B. States would be able to obtain federal matching funds for the costs of covering low-income individuals with HIV who are currently ineligible for Medicaid without having to satisfy the Secretary that their eligibility expansion would be budget neutral to the federal government over a five-year period. Additionally, as in the case of Option 3B, this approach would ensure that, in states electing the option, the minimum eligibility standard would be uniform although variations in the scope of benefits would remain.
This approach would have one additional advantage. By increasing the federal financial share of the costs of coverage, this approach would reduce the state share of costs for treating individuals with HIV, both those newly eligible and those already covered by Medicaid under existing rules. In all likelihood, state participation in this option would be greater than state participation under either Option 3A or 3B, resulting in the coverage of a greater number of low-income individuals with HIV.
Disadvantages
This approach has the same generic disadvantages as Options 3A and 3B, but they are somewhat mitigated by the enhanced federal matching rate feature. The Committee’s criteria of a minimum uniform standard of eligibility would be achieved only if all states participated. The enhanced federal matching rate would increase state participation compared with the other Medicaid options, but universal state participation still seems a remote possibility in light of the revenue pressures under which most states are operating. Even in those states that choose to participate, there would be no requirement that provider reimbursement rates be adequate for maintaining appropriate levels of provider participation. In states with low rates, this would limit the ability or willingness of providers to deliver covered services. Finally, although this option recognizes that the federal government has a greater financial responsibility for the costs of responding to a national epidemic, it still requires a significant state contribution, ranging from 17 to 35 percent, depending on state per capita income. Many states, particularly those hard hit by the epidemic, will have difficulty sustaining their state contribution toward the costs of an eligibility expansion over time, regardless of their relative per capita incomes.
Option 4: Federal Block Grant to States for HIV Care
Under this approach, the federal government would establish a block grant to states for HIV care modeled on the State Children’s Health Insurance Program block grant. SCHIP was enacted in 1997 as a means of providing health benefits coverage to uninsured children living in families whose incomes exceed their state’s eligibility limits for Medicaid, but do not exceed 200 percent of the FPL.3 The SCHIP block grant is a federal entitlement to states subject to a cap; that is, federal matching funds are made available to participating states based on costs incurred up to the state’s allocation for a given fiscal year. The state’s allocation, in turn, is determined under a statutory formula that distributes a fixed federal dollar amount for a fiscal year among states based on the number of low-income children with and without health insurance coverage, as well as geographic variations in health care costs. The rate at which the federal government matches state costs up to the allocation varies from 65 to 84 percent, depending on the state’s per capita income. Uninsured children have no individual entitlement to a defined package of services; instead, states have
discretion to limit enrollment of otherwise eligible children (GAO, 2001). States also have discretion, within broad federal guidelines, to design their own SCHIP benefits packages, which may be less generous than those available to children enrolled in their Medicaid programs. States have complete discretion with respect to provider reimbursement rates; they can pay more or less than their state Medicaid program pays for comparable services. They may administer SCHIP through their Medicaid program, through a separate free-standing program, or through a combination of the two (Lambrew, 2001).
Following this model, a federal HIV block grant would make matching funds available to each state opting to participate, up to a specified dollar amount each fiscal year. The allocation to each state would be determined by distributing the fixed federal amount for a fiscal year among participating states based on the estimated number of individuals with HIV and the costs of health care services. The federal matching rate would be the same as that under the SCHIP block grant, a reduction of 30 percent in the state share under the Medicaid matching rate formula. States could use the funds to purchase services for individuals with HIV who are ineligible for Medicaid and have incomes up to 250 percent of the FPL. States would be able to offer benefits that meet the standard of care for HIV/AIDS, but would have the discretion to design their own alternative benefits package. States would have complete discretion in setting provider payment rates and in establishing their own administrative structures.
Advantages
The principal advantage to this approach is that it makes additional federal resources available to states to furnish the standard of care for HIV/AIDS to low-income individuals infected with HIV who cannot now qualify for Medicaid. Because of the enhanced federal matching rate, states would be required to contribute a significantly smaller share of the costs of caring for these newly eligible individuals with HIV than the proportion that they contribute to the costs of caring for Medicaid patients with HIV/AIDS. In addition, a state would have broad flexibility to design its own benefits package and to establish its own provider payment levels, allowing for innovation in the design of an HIV delivery system. Finally, states would have the discretion to cap enrollment of otherwise eligible individuals in the event that their expenditures exceed the available federal funds. For all of these reasons, participation in such a block grant might be more attractive to some states than participation in an optional Medicaid expansion of the kind described in Option 3C. To the extent that more states participate, more state resources would be brought to bear on the epidemic and its victims.
Disadvantages
This approach has a number of disadvantages, most of which stem from the inherent structural characteristics of a block grant approach. The total federal financial contribution in any given fiscal year would be fixed in advance (the total funding levels for the SCHIP block grant were specified in 1997 for each fiscal year through 2007). This fixed total amount must be allocated among states each year based on a formula rather than on the basis of actual costs incurred by states in treating eligible individuals. Because the federal funds available to any given state in a fiscal year are fixed, each state that elects to participate is given broad discretion in determining eligibility, benefits, and provider reimbursement.
This approach would not ensure the adoption of a minimum standard of eligibility for low-income individuals with HIV from state to state. Not all states would necessarily participate, and those opting to participate would be likely to set different eligibility thresholds. Even among states with comparable eligibility thresholds, some states might impose enrollment caps, leaving some eligible individuals without coverage, while other states might not. In short, considerable variation in eligibility would be likely from state to state.
A recent report from the Kaiser Commission on Medicaid and the Uninsured (Ross and Cox, 2003) on strategies states are implementing under SCHIP found that enrollment freezes in six states (Alabama, Colorado, Florida, Maryland, Montana, and Utah) have resulted in tens of thousands of eligible children going without health insurance. These enrollment freezes are creating inequities among children eligible for health coverage programs. In some states, inequities relate to policies that bar newborn children from the program (Alabama, Florida, Maryland, and Utah), such as an age-based eligibility structure for health coverage programs that puts young children enrolled in Medicaid at increased risk of becoming uninsured if a SCHIP enrollment freeze is in effect. In Alabama and Montana, children who are subject to the freeze may lose the value of 12-month “continuous eligibility” and remain uninsured for part of the year (Ross and Cox, 2003).
The same can be said with respect to benefits. Some participating states would likely adopt a benefit package that meets the standard of care for HIV/AIDS. Others might design a less comprehensive package or might offer different packages in different parts of the state. In short, this approach would not ensure the use of a benefits package that meets the standard of care for HIV/AIDS and that is uniform for all eligible individuals. In addition, because the new HIV block grant would affect benefits only for low-income individuals not eligible for Medicaid, the benefits available to individuals with HIV/AIDS enrolled in Medicaid would be likely to remain
the same as under current policy, often departing from the standard of care for HIV/AIDS.
Under this approach, states would have even more discretion in establishing provider reimbursement rates than the considerable discretion they are currently allowed under Medicaid. Some states would likely set payment rates that are adequate to enable providers to furnish services consistent with the standard of care for HIV/AIDS. Other states would likely set payment rates that are not adequate, potentially undermining provider participation in the program and patient access to services. The rates set by a state under its HIV block grant program may or may not be the same as the rates used by the state under its Medicaid program. If the rates under the HIV block grant program are significantly higher (or lower) than those under the state’s Medicaid program, providers may have an incentive to favor the treatment of those individuals covered by the higher paying program.
As discussed earlier, the availability of federal matching funds to states on an entitlement basis has advantages over funding that is subject to annual appropriations. However, the signature feature of the block grant is that this federal funding would be subject to a limit in each state for each fiscal year, regardless of the number of uninsured low-income individuals infected with HIV or the actual cost of providing the standard of care for HIV/AIDS to these individuals through qualified providers. These annual limits would be determined 5 to 10 years in advance and likely would be based not just on projections of the epidemic and its costs, but also on competing federal budget priorities (the SCHIP block grant was enacted as part of the deficit reduction agreement in the Balanced Budget Act of 1997). Multiple factors—not the least of which is the difficulty in developing accurate population estimates of HIV—make predicting what resources each state will need in any given year particularly daunting. As noted previously, up to one-third of the HIV-infected population is unaware of their HIV status, and as many 30 percent of those people with HIV who are aware of their status are not in care. Because of the difficulties in developing information for allocation formulas, block grants have not been found to be effective in achieving equity among states (NRC, 2001; IOM, 2003b). Thus, the annual limits on federal funds might or might not be capable of supporting, over time, the eligibility, benefits, and provider payment policies that meet the Committee’s criteria for the financing of HIV care.
A related disadvantage has to do with the differential federal matching rates that this approach implies. Under this block grant, state expenditures would be matched (up to each state’s allocation for the fiscal year) at an enhanced rate compared with the matching rate under Medicaid. Thus, in a state with a relatively high per capita income, the federal government would pay 50 percent of the costs of treating Medicaid beneficiaries with HIV/
AIDS, but 65 percent of the costs of treating individuals with HIV who are eligible for the block grant. Similarly, in a state with relatively low per capita income, if the federal government paid 70 percent of the costs of treating Medicaid beneficiaries, it would pay 79 percent of the costs of treating individuals with HIV who are eligible for the block grant. These differential matching rates are difficult to justify: Why should the federal government assume a greater share of the cost of treating individuals with HIV who are less poor than those eligible for Medicaid? In addition, differential matching rates create a risk of manipulation of the system by fiscally pressed states seeking to maximize federal revenues.
Finally, the block grant approach has potential administrative disadvantages. States that opt to participate by establishing a new program separate from their Medicaid program will incur some administrative costs that duplicate those already assumed by their Medicaid programs. In addition, because of the emphasis on state flexibility under a block grant, obtaining comparable, accurate, and timely program data is likely to be more difficult for the federal government than it would be under Medicaid or another entitlement program, where reporting is tied to state claims for federal matching funds for costs incurred on behalf of specific individuals. Difficulty in tracking how federal block grant funds are being spent or even how many individuals are being served would be particularly counter-productive in a program designed to control the proliferation of infection and achieve specified targets in reduced mortality.
Option 5: New Federal HIV Entitlement Program Administered by States
The final approach the Committee considered is the implementation of a federally funded, state-administered program for the coverage of HIV/AIDS care. Under this option, the federal government would establish eligibility requirements, specifications for benefits, and standards for provider reimbursement designed to ensure that individuals with HIV and family incomes at or below 250 percent of the FPL receive the services needed to meet the standard of care for the treatment of HIV infection. State participation would be optional; however, all costs incurred by a state in furnishing covered services to eligible individuals, including reasonable administrative expenses, would be reimbursed by the federal government at a 100 percent matching rate.4 Federal funding for this program would be available to states on an entitlement basis and would not be subject to annual appropriation or to an upper limit in any fiscal year. Individuals eligible under the
federal standards who reside in participating states, including individuals currently eligible for Medicaid or for Ryan White CARE Act services, would have an individual entitlement to the federally defined set of benefits under the new program. States electing to participate would have the option of administering the new national program as a free-standing program or through their Medicaid program, so long as they meet the federal requirements relating to eligibility, scope of benefits, and adequacy of provider reimbursement.
The Committee also considered a similar program that was not only federally financed but also federally administered—a program that did not rely on any state Medicaid or other administrative structures. In states with dysfunctional administration, the creation of new beneficiary enrollment and provider claims processing capacity through federal contracting with private entities could potentially improve program implementation and outcomes. However, the Committee determined that a new “stand-alone national program” would create administrative challenges not presented by other alternatives. For example, a new, separate administrative structure would be required to receive and disburse program funds, determine eligibility, certify and contract with providers, and monitor quality. The creation of a new structure would unnecessarily duplicate costs built into the management of existing programs. The Committee did not pursue this option.
Advantages
This approach has a number of advantages. First, of all the approaches considered by the Committee, this approach has the greatest likelihood of ensuring that all individuals with HIV and family incomes below 250 percent of the poverty level have coverage for services that meet the standard of care for HIV/AIDS, regardless of the state in which they reside. As will be noted, this approach does not guarantee this result because it does not compel state participation; however, the incentives for state participation are quite powerful.
With respect to benefits, this approach would give federal policy makers the ability to design a comprehensive benefit package that includes the necessary mix of medical and social services for effective HIV/AIDS management. Federal policy makers would also set minimum payment standards to ensure participation by qualified providers to an extent sufficient to meet the demand for services by eligible individuals. Because participating states would be reimbursed for the full cost of paying qualified providers adequate rates for furnishing the specified benefits to eligible individuals, there is a strong likelihood that most low-income individuals with HIV would have access to the standard of care for HIV/AIDS.
Another advantage of this approach lies in its financing mechanism.
Currently, the costs of treating individuals with HIV/AIDS are paid for in significant part by those states (and localities) in which large numbers of individuals with HIV/AIDS are concentrated. Under this federally funded approach, the scope of the revenue base would be aligned with the scope of the epidemic. The federal government’s national revenue base is not limit-less, but it is significantly more capable of supporting an effective program of care for HIV/AIDS over the course of the epidemic than are the revenue bases of individual states.
This approach also offers two significant advantages with respect to administration. First, rather than creating a new and potentially redundant set of federal administrative structures, this approach would rely on participating states to select the most effective set of administrative arrangements. Some states may elect to use their Medicaid agencies and program administrative contractors; others may decide to establish a new program, either using another state agency or contracting out to a private vendor (or both). Because the federal government would pay 100 percent of the administrative costs incurred by states, it could specify reporting requirements that would ensure program accountability and facilitate evaluation, regardless of the particular administrative arrangement a state chooses to put in place.
Second, because the federal government would finance the entire cost of covered services for all eligible individuals in participating states, it would have purchasing leverage that could be used to generate considerable efficiencies in the purchase of prescription drugs used in highly active antiretroviral therapy (HAART). As discussed in Chapter 6, the Medicaid program, ADAP, and the Veterans Administration (VA) all obtain discounts on HIV/AIDS drugs. These discounts vary from program to program and, in the case of ADAP, from state to state. The creation of a national program that entitles more individuals with HIV to HAART would provide an opportunity for the federal government to achieve greater program efficiencies by negotiating lower prices with manufacturers in exchange for the increased volume of sales that the new program will bring.
Disadvantages
This approach is not without its disadvantages. First, as in the case of all the approaches considered by the Committee, participation in this new program would be optional on the part of the states. Thus, there is no guarantee that the Committee’s criteria of a national, uniform standard of eligibility and a national, uniform benefits package meeting the standard of care for HIV/AIDS will be met in practice. However, the availability of federal matching funds for 100 percent of the costs of covered services and administration would be a powerful incentive for every state to participate, particularly in the cases of those states that currently spend significant
amounts of state funds purchasing services for individuals with HIV/AIDS through their Medicaid programs. By participating in this new program, these states would be able to replace these state dollars with federal funds without simultaneously incurring any additional state costs for expanding eligibility to individuals with incomes at or below 250 percent of the FPL.
A related disadvantage arises from the strong financial incentive for states to participate: federal expenditures for HIV/AIDS care will increase substantially. This increase has two principal sources. First, the federal government will be paying 100 percent of the costs of covering all the newly eligible individuals with HIV in those states electing to participate. Second, the federal government will also be paying what is currently the state share of the cost of treating Medicaid beneficiaries with HIV/AIDS (on average, 43 percent of the costs). The federal government can realize some offsetting savings by redirecting the federal Medicaid funds and a portion of the Ryan White CARE Act funds now being spent on individuals who qualify under the new program. Nonetheless, a significant net increase in federal spending will occur. There are three broad options for addressing this net increase in federal outlays: reducing other entitlement programs, increasing federal revenues, or further increasing the federal budget deficit.
Another disadvantage is that any state funds now being applied to the provision of services for low-income individuals with HIV that are replaced by the new federal funds would not necessarily remain available to combat the epidemic. This option does not contain a maintenance of effort (MOE) requirement under which states would have to continue their current level of spending on HIV/AIDS care. Although the absence of an MOE requirement makes participation in the program considerably more attractive to the states, and although there is a strong logic to the federal government’s assumption of the costs of a national epidemic, the disadvantage remains that significant public resources now being applied to HIV/AIDS care would be applied to other purposes.
A final disadvantage arises from the federal–state nature of this program. Because the federal government would match state rather than local expenditures for covered services on behalf of eligible individuals, there would be less opportunity for local policy makers to address issues specific to providing services in their communities. The role of Ryan White Planning Councils, in particular, would be reduced, and the program would likely require the redistribution of dollars in ways that may reduce funding for certain community-based services.
IMPROVING THE DELIVERY OF HIV CARE
In addition to considering options to improve the public financing of HIV care, the Committee was asked to consider what improvements could be made
in the delivery of HIV care. In this section, the Committee provides a framework for redesigning an improved health care system for people with HIV.
The complexity of HIV disease—lifelong need for treatment and prevention, coordination of medical treatment with social support and mental health and substance abuse services, and chronic care management requirements—calls for the development of an improved HIV/AIDS care delivery structure. This is essential if the goals of preventing death and disability associated with HIV infection, controlling the epidemic spread of HIV, and improving quality of life for those affected by the disease are to be achieved. These goals can be accomplished within the broader context of care systems that are organized to provide effective and efficient services that are accessible, comprehensive, and coordinated, with high quality maintained within an environment of accountability. The Committee drew from two bodies of literature—chronic disease and quality care—to develop a framework for considering ways to improve the delivery of HIV care. The concepts and principles supported in this literature guided the Committee to examine the concept of “Centers of Excellence” as a means to improve the delivery of HIV care.
HIV/AIDS as a Chronic Condition
Chronic illnesses, as defined by the National Center for Health Statistics of the Centers for Disease Control and Prevention, are “illnesses that are prolonged, do not resolve spontaneously, and are rarely cured completely” (McKenna et al., 1998). There is no cure for HIV disease; however, as noted earlier, access to HAART early in the course of HIV disease has been shown to delay the onset of AIDS and is associated with decreased mortality from HIV disease (Palella et al., 1998, 2003; Moore and Chaisson, 1997, 1999; DHHS, 2004). Once treatment has begun, an individual can expect to be on antiretroviral medication for the remainder of his or her life. Under these conditions, HIV/AIDS squarely meets the definition of a chronic illness (Gifford and Groessl, 2002).
As noted in Chapter 2, HAART requires a high level of management to ensure adherence (Garcia de Olalla et al., 2002; Bangsberg et al., 2001; McNabb et al., 2001; Paterson et al., 2000). However, HAART alone is not sufficient. The management of HIV/AIDS requires not only therapeutic services but also attention to the patient’s social and environmental circumstances to conserve levels of independence and slow the progression of disease and disability and the prevention of new infections. Patients with HIV/AIDS, especially those with co-morbid conditions, require care from multiple clinicians and multiple systems. In addition to HAART and other drug therapies, a number of adjunct services and interventions have been identified as essential to the care process and necessary for optimal reduc-
tions in the rates of infection of HIV/AIDS. These services include, but are not limited to, primary medical care services (Ashman et al., 2002), substance abuse treatment (Turner et al., 2001), mental health services (Ashman et al., 2002; Davis, 2002), prevention counseling for the infected population (IOM, 2001a), and medical and social case management services (Laine et al., 1999; Ashman et al., 2002; Lo et al., 2002; Levi, 2002).
To fully support the management of chronic illnesses, a “chronic care model” has been developed and described more fully by Wagner (2001), Wagner et al. (1996, 2001), and Bodenheimer et al. (2002). In this model, chronic care takes place within three spheres: the community, the health care system, and the provider organization. The workings of each sphere can help or hinder optimal care. In the community sphere, community-based resources such as community support, social service resources, and policies provide critical linkages to provider organizations. In the health care system and provider spheres, the structure, goals, and values of the provider organization and its relationship with purchasers, insurers, and other providers are established. These spheres support critical dimensions of chronic care, including recognition of the patient and family as the source of control with the practice team collaborating and providing expertise and tools, the creation of a care delivery structure that is appropriate to the planned management of patients with chronic illness with clear roles for all staff, the integration of evidence-based guidelines into daily practice, and the development of clinical information systems that allow clinicians to plan care for both individuals and whole populations of patients and to monitor and receive appropriate feedback (Bodenheimer et al., 2002; IOM, 2002).
The management of HIV/AIDS is very similar to that of other chronic diseases. It requires coordination of care, clinical integration of services, and development of delivery system and community relationships. The management of HIV/AIDS also differs in important ways from the management of other chronic diseases. In this section, the Committee illuminates some of the similarities and differences in the managing adherence to diabetes and HIV/AIDS treatment.
In 2003, the American Public Health Association developed a comparison of the management of diabetes and HIV/AIDS as part of a Web-based document on Treatment Adherence to Antiretroviral Therapies: Recommendations for Best Practices (APHA, 2003). The comparison highlighted shared features and influences that influence adherence or utilization of treatment and features that distinguish between the two diseases that may complicate adherence. Table 5-2 provides an overview of these similarities and differences.
Experiences in promoting adherence in diabetes provide some lessons for promoting treatment adherence in HIV. The report identifies several
TABLE 5-2 Managing Adherence Case Study Contrasting Diabetes and HIV/AIDS
|
Shared Features |
Distinguishing Features |
|
|
conditions of care management that support treatment adherence. Especially important among these conditions is care that is based on a collaborative model where the provider’s role is to apply technical knowledge and skill, and to assist patients to develop self-management skills. Continuing contact and support is another critical condition of care that supports sustained adherence. Well-trained providers organized in multidisciplinary teams and skilled to deal with adherence problems are other conditions that support treatment adherence.
Lessons learned from the broader chronic care management literature highlight five important elements of chronic care programs. These elements include evidenced-based planned care, a multidisciplinary team approach, systematic approaches to providing patient information (counseling, education, information feedback), clinical knowledge and expertise (available to
both patients and clinicians), and supportive information systems that allow sharing of information among team members and between patients and team members (IOM, 2003a). Chronic disease management programs have been implemented by a number of health care providers, states, and public health agencies for a number of disease states; common among these are programs for asthma, diabetes, and hypertension (Wheatley, 2002). The Task Force on Community Preventive Services (CDC, 2001) strongly recommended disease and case management as an effective strategy for reducing morbidity and mortality from diabetes. The Committee concludes that the chronic care model is an appropriate framework for redesigning an improved delivery system for HIV care.
Quality Care
In 2001, an Institute of Medicine (IOM) study committee charged with “developing a strategy that would result in a substantial improvement of health care over the next 10 years” issued its report, Crossing the Quality Chasm: A New Health System for the 21st Century (IOM, 2001b). This report followed that of a 2000 IOM study, To Err Is Human: Building a Safer Health Care System, which focused on a specific quality concern—patient safety. These two reports have focused significant attention on organizational management issues related to improving the health care sector.
In Crossing the Quality Chasm (IOM, 2001b), the Committee on Quality of Health Care proposed specific aims for health care system improvement and for meeting patient needs. Several of these aims are consistent with the chronic care model—providing care that is patient centered, effective, safe, and timely. The Committee on Quality of Health Care also recognized that the challenge health care organizations face is fundamentally an issue of the current failings of systems of providers; and hence, the need to redesign the process of clinical care delivery. To this end, the Committee identified specific challenges for the design of health care organizations and systems that are also challenges for care provided under a chronic care model. These challenges include redesigning care processes based on best practices; making effective use of information technologies; managing clinical knowledge and skills; developing effective teams; coordinating care across patient conditions, services, and settings over time; and incorporating performance and outcome measurements for improvement and accountability.
The Committee on the Public Financing and Delivery of HIV Care fully embraces the principles of quality and strategies for quality improvement as outlined in the previous IOM reports and believes that publicly funded programs of HIV care should support delivery system redesign in order to
improve the quality of the services they provide. Some of these steps are being taken already. The Health Resources and Services Administration (HRSA) and CMS have been working to improve the quality oversight of their programs and to support quality improvement programs. In particular, HRSA’s HIVQUAL Continuous Quality Improvement Program seeks to improve quality of care for people with HIV by building knowledge, skills, and capacity through system improvement, information management, and performance measurements (New York State Department of Health, no date).
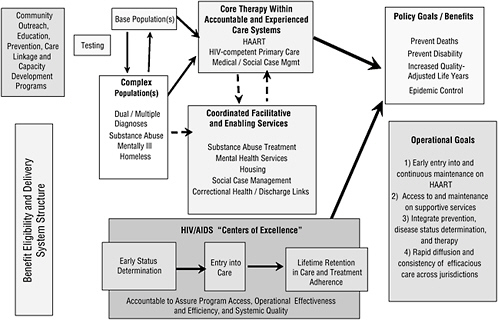
Delivery System for HIV/AIDS Care
Drawing from the review of the chronic care literature and the Quality Chasm report in particular, the Committee acknowledges that the HIV/AIDS care system—like the American health care delivery system in general—is in need of fundamental redesign, not just minor correction. When applied to HIV/AIDS care, that idea suggests that allocating new funds to the current system will not necessarily achieve better results; what is needed is fundamental change in the design of the delivery system and a redesigned financing system. Toward that end, the Committee is convinced that HIV/AIDS patients need to be cared for in a system that is specifically designed around the core concepts of the chronic care model and of the Quality Chasm report. That system does not exist today. In the next section, the Committee discusses the characteristics of a delivery system that would better integrate these two conceptual areas for HIV/AIDS care (Figure 5-1).
Figure 5-1 provides a broad overview of the Committee’s view of the logic of integrated and coordinated care for individuals with HIV. If HIV-infected patients know their status, enter care, and stay in continuous care over their lifetime, a previously fatal disease is converted into a lifetime chronic disease, allowing those afflicted to maintain productive contributions to society. Appropriate medical management of the disease requires coordinated and integrated expert care. Such medical care may be more effectively provided through organized and accountable systems of care such as Centers of Excellence. Early infection status determination rather than AIDS determination leads to early therapy and prevention of both epidemic spread and progression to serious disability for those infected. Changes in the understanding of the disease and improvements in therapeutic technology also require significant changes in delivery system structure such as moving the primary locus of care from social settings and providers supported by medical providers to medical care systems, settings, and providers supported by social systems and providers. The integrated and coordinated model also acknowledges that the development of “rapid testing” technology and availability of newer and easier to use HAART thera-
pies, combined with a significant number of HIV-positive individuals who do not know their disease status, creates an increased need for community outreach to achieve early status determination and referral to care.
Delivery System Functions
The Committee identified two key functions of an HIV/AIDS care system: (1) the provision of HAART in order to delay or prevent progression of the disease and minimize infection of others, and (2) the provision and coordination of other medical care and ancillary support services necessary to ensure that patients adhere to HAART. The evidence reviewed by the Committee in earlier chapters and much of the public testimony heard by the Committee indicate that the delivery of services for patients with HIV/AIDS falls far short of optimal. Many patients do not have a regular “medical home”; many (particularly those in rural areas) receive care from physicians with little experience in treating HIV (Cohn et al., 2001); coordination of care plans and other information among medical, mental health, and substance abuse providers is often minimal or nonexistent; and many patients face significant barriers in trying to make and keep appointments with multiple providers in multiple organizations with multiple medical records systems and phone numbers to remember. The need for medical or social case management systems comes largely from the administrative complexity of the current “system” for providing HIV/AIDS care.
Boiled down to its administrative essentials, an improved delivery system for HIV/AIDS care in the public sector must have the ability to engage experienced HIV/AIDS providers and coordinate their activities in service of the two key functions described above. More specifically, the system should be made up of entities capable of
-
identifying highly qualified, experienced providers of HIV-related services and entering into contracts with those providers for the provision of care to a defined set of patients;
-
managing patients’ clinical information (i.e., medical records) and making that information available as needed to the range of health care providers involved in patient care;
-
measuring and monitoring access to care, quality of care provided, and outcomes of care, and reporting that information to the public entities providing funds for HIV-related services; and
-
receiving and managing public funds allocated for HIV/AIDS care and distributing those funds to individual providers and provider organizations in exchange for services rendered.
The Committee considered several types of delivery models, and heard
testimony from a number of organizations that have done exemplary jobs of providing and/or coordinating HIV-related services. No single organizational model has become clearly established as superior to all others. There is great variety in the organizational structure of those models—some are large integrated medical care systems such as the VA; others are smaller, HIV/AIDS-focused organizations whose roots are in social services rather than medical care. Successful organizations have all, to some extent, adapted themselves to local and geographic circumstances that are unique and therefore not precisely replicable elsewhere.
Centers of Excellence
In spite of this variety in current models, the Committee remains convinced that some modification to the current system for delivering HIV/AIDS services would be essential to ensure that patients receive the maximum possible benefit of the enhanced financing being recommended. The Committee focused its discussion on the concept of Centers of Excellence (CoEs) to provide high-quality, chronic care services to patients with HIV/AIDS.
The CoE concept implies a system of care that offers access to clinical and support services that are comprehensive, integrated across providers, and seamless. Centers of Excellence generally include clinicians who are highly trained and experienced in providing care to a specific set of patients. Typically, CoEs focus on particular diseases that are high cost or high volume (cancer) or affect a specific population (e.g., women). CoEs often integrate or bridge the multiple services and multidisciplinary providers whose services are not necessarily coordinated. CoEs, as part of their responsibility to recruit and maintain a highly trained and experienced staff (physicians, mental health and substance abuse providers, case managers, etc.), often implement strategies for training and continuing education. Through these strategies, staff are kept abreast of changing therapies and evolving knowledge on HIV and care for HIV patients. Some CoEs are also organized to conduct research to improve the care delivery system for their target population. An administrative structure assumes responsibility for ensuring access to services and for the quality, outcomes, and cost of services provided. CoEs may receive special reimbursement consideration and/or may be involved in reimbursing participating providers through a salary or other mechanisms.
The Medicaid program has some experience with disease-focused CoEs, but not with CoEs for HIV care. The state of New York, however, has been experimenting with the CoE concept since 1986 through its Designated AIDS Center Program (DACs). The 44 centers designated under the program are hospital based and state certified. These centers serve as the hub
for a continuum of hospital- and community-based care for persons with HIV infection and AIDS. DACs provide multidisciplinary inpatient and outpatient care coordinated through hospital-based case management. The centers are held to HIV-specific care standards to ensure uniform and quality care, and an AIDS Intervention Management System is used to collect, organize, and evaluate data for utilization monitoring and quality of care reviews. Enhanced funding is provided for services delivered through the program. The program, originally established when hospital-based care was the norm, is in the process of review now that the hub of care is no longer hospital based (New York State Department of Health, 1993, 2003).
CoEs for chronic conditions such as HIV/AIDS will have to be different in some respects from those for acute illnesses. The need to coordinate services from many different providers over extended periods of time, to maintain patient tracking systems and promote adherence to therapy, and to integrate with community-based programs and services will all require somewhat different organizational forms than those found in hospital-based CoEs for acute conditions.
Organizing Centers of Excellence
The Committee discussed a variety of structural models that a CoE might adopt. The Committee chose not to recommend one specific model over the others, recognizing that local circumstances (e.g., existing organizations, community preferences, geographical considerations) will favor one model over another in those circumstances. Furthermore, current models have not been specifically designed with the needs of individuals with HIV in mind. The Committee recognizes that testing and experimentation will need to occur before the best ways to serve people with HIV are identified. Thus, the committee remains open to different approaches for providing the most appropriate and feasible care for people with HIV/AIDS. Testing of these alternatives will require mechanisms for ensuring accountability. Experimentation with alternatives will require data collection, especially analysis and reporting related to assessing access, cost, quality, and patient satisfaction.
The range of potential structural models for a CoEs is quite broad. Models can range from highly integrated systems exemplified by the VA or Kaiser Permanente to very loosely structured organizations in which there is no central administrative entity. In the former model, a single organization provides the entire range of medical and support services and receives payment for that entire range of services. The organization may occasionally contract with outside providers for a limited set of highly specialized services, but for the most part services are provided by employees of the integrated system. It is likely, but not guaranteed, that each patient will
have a single medical record (perhaps in electronic form) and a care plan that is shared among all types of service providers. In some instances, the entire range of medical, mental health, substance abuse, and social services will be available at a single physical facility; in other instances, the organization may have multiple physical facilities that are closely linked in terms of medical records, appointments, and billing systems.
In the latter model, the CoE concept comes to life primarily through a process of selecting only high-quality, experienced providers to participate in the public financing system. There would not be a mechanism for formally assigning patients to individual providers or to the system as a whole, but only designated providers would be able to receive payment for services to individuals with HIV/AIDS. Structurally, there is no distinction between this model and an unstructured fee-for-service delivery system. Payment in this model is made directly by the public entity (e.g., Medicaid program) to individual providers, including providers of case management or care coordination services. Payment for services may be made on the basis of fee-for-service, capitated, or any other model mutually agreeable between the provider and the payer.
There are other models in the middle of this continuum of administrative integration. For example, there could be a “managed care model,” exemplified by many health maintenance organizations (HMOs) and other forms of managed-care or “carve-out” plans. In this model, a single entity would receive payment (almost always on a capitated basis) for the entire range of necessary services. That entity would generally not provide services directly, but would contract with a network of medical and social service providers to ensure that members/patients receive necessary services in a timely fashion. In many state Medicaid programs, individuals with HIV/AIDS are assigned to managed-care plans and receive services through this model.
One might also envision a “care coordination model,” in which a defined entity is responsible for providing case management/care coordination services in the context of a loosely connected network of medical and social services providers. The care coordination entity would not receive payment for the complete range of medical and social services, though, and would not pay the other providers. An outside entity (e.g., state Medicaid program) would pay the other providers on the basis of whatever payment model(s) it can negotiate with each type of provider. In this model, the case management/care coordination entity can be (but does not have to be) given authority to set quality standards, develop and enforce coordinated care plans for individual patients, collect and analyze data on quality of care, and select the members of the provider network.
Regardless of the specific organizational form used in a given area, though, the Committee believes that the key functions for CoEs are those
identified earlier in this section: assembling a set of highly trained, experienced HIV/AIDS providers; coordinating their activities in order to achieve the highest possible levels of adherence to HAART; and providing necessary medical and nonmedical services to complement and support HAART. The Committee assumes that a wide range of providers, including community-based providers who have experience and expertise in working with the new populations affected, will be considered when organizing Centers of Excellence.
Mechanisms of Accountability
Any of the potential structural models for an HIV/AIDS Center of Excellence can support mechanisms of accountability to the public funders of HIV/AIDS care. That is, there can be mechanisms to collect, analyze, and report data related to standards for access, cost, quality, and patient satisfaction.
Each CoE would be organized as an accountable health enterprise. Individual providers within each designated CoE would be reimbursed at a level to attract and retain the complete range of excellent providers required to meet the comprehensive service needs of the eligible HIV/AIDS population. Each designated CoE would be responsible for assuring that individual providers meet ongoing quality and service standards to maintain their individual eligibility to participate in the CoE. The designated CoE organization, itself, would receive compensation from the state Medicaid agency to support network management, quality management, and network care coordination expenses required to assure long-term efficacy and cost effectiveness of care services.
Each designated CoE would be accountable for assuring appropriateness of fund expenditures and for the cost and quality of services rendered. Expenditures, service levels, and quality levels would be reported to the state Medicaid agency by each designated CoE on an annual basis. The national Medicaid program would assume responsibility for compiling and reporting program access, cost, and quality results to all participants, to the Centers for Disease Control and Prevention, and to Congress on a regular basis. Where deficiencies are deemed to exist, the national Medicaid program would ensure that plans are placed in effect to correct the deficiencies at the state level. A general overall program accountability concept is summarized in Figure 5-2.
For true accountability to exist in the system, though, there must be consequences for good or poor performance that have the net effect of improving quality and efficiency. Most systems of accountability in health care involve consequences in either “market share” or funding. The former involves incentives that move members/patients to better performing orga-
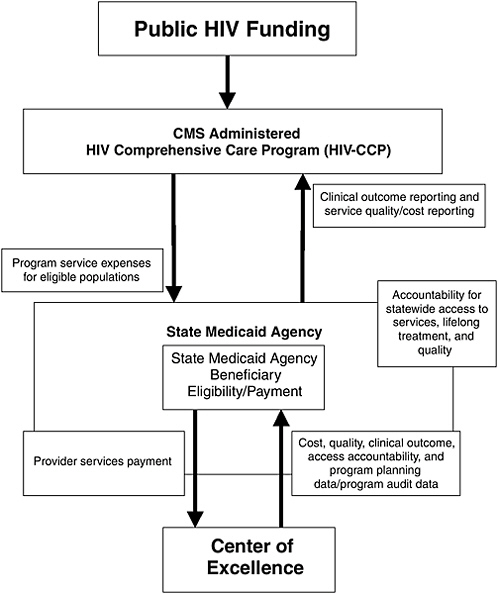
FIGURE 5-2 Overall program accountability concept.
nizations or away from poorer performing organizations. The latter involves financial rewards (either supplemental payments or higher rates of basic payment) to better performing organizations and financial disincentives (e.g., no return of “withholds”) for poorer performing organizations or individual providers.
In the context of a CoEs model for HIV/AIDS care, both types of
approaches can be used within states, but each will have a mix of strengths and weaknesses. Reward in the form of increased market share can be effective for CoEs that are performing well, but only if those organizations have room to grow and the payment system is set so that the CoE at least breaks even on additional patients. If the CoE is already at capacity in terms of its providers or inpatient capacity, additional patients are a problem rather than a reward. If the payment model produces a predictable loss for each new patient seen, more patients are not a reward. This type of reward is also not effective in a region or community with only one CoE and a fixed number of HIV/AIDS patients to see. There is no way of increasing market share over 100 percent.
Disincentives in the form of reduced (or possibly completely eliminated) market share are generally more effective because organizations typically depend on a predictable flow of patients to keep providers busy and facilities full. A mechanism through which patients can be reassigned from one CoE to another as a consequence of poor performance (or if patients are allowed to choose among competing CoEs) can provide a strong incentive for improvement in poor-performing organizations. This mechanism would work more effectively in moderate to large urban areas where more than one CoE is possible. A similar incentive can be provided through fixed-term contracts between individual providers and CoEs, or between competing CoEs and the state, if the contracts involve a reassessment of performance and the tangible prospect of nonrenewal. These types of incentives and disincentives, however, may not be implementable in some areas, for example rural areas, because the poor-performing entity may be the sole provider in that area.
Financial rewards for excellent performance can be effective, but rarely have been used in health care, particularly in the context of HIV/AIDS care or Medicaid (IOM, 2003a). Potential models can take the form of either “bonus payments” at the end of a period of time if certain quality or efficiency targets are achieved, or higher fee-for-service or capitation payments in future time periods if performance targets are reached in a current period. These models can only be implemented if the state or other public payer has funds available that are not already committed to the basic payment model for services and if clear performance measures, data collection, and analysis systems are available to assess performance on a regular basis (Kates et al., 2001). Some models may also require an amendment of legislation or regulation that defines levels of provider payment and the extent that payment can vary from provider to provider.
Financial disincentives for poor performance are typically the mirror image of financial rewards—they either involve a “take-back” of funds on the basis of poor performance or a lower rate of payment in the future if performance is poor in the recent past. These models have been imple-
mented in the context of “withholds” in the payment agreements between HMOs and physicians, but have not been widely used in the context of publicly financed HIV/AIDS care. If base reimbursements are already low, any form of take-back or lower payment may have the effect of driving a particular provider out of the program entirely. In some instances, this may be an acceptable consequence of a financial disincentive system, but it will not allow poorer performing providers time or opportunity to improve and remain in the system. This may be a significant concern in situations where many of the HIV/AIDS service providers are not financially stable and not able to withstand any cuts in payment levels or are unable to meet all performance criteria because of having to make tradeoffs among different aspects of care (e.g., good care is provided when the patient sees the physician, but a waiting time may not meet standards because of budget constraints).
At a higher level of oversight, the federal government, through CMS, can define standards of performance for the state Medicaid programs (or other public entities) that will be asked to administer the new HIV/AIDS care program. Theoretically, the federal government can create a system of accountability by providing more or less funding to states with better or poorer performance according to those standards. In practice, though, this ability is limited by the language of legislation and regulation that sets rates of federal payments to states, and by the ability of CMS staff to make and enforce decisions that would be highly visible and strongly opposed by elected officials from adversely affected states.
A system of accountability based on market share is essentially impossible to implement in the context of federal–state relationships because the population of HIV/AIDS patients in a given state is essentially fixed in the short run, and it is unlikely that patients would ever be asked to travel to a different state to receive services. It is conceivable that in some regions, with large metropolitan areas that cross state boundaries, the federal government could encourage individuals to seek care in one state rather than another and allocate funds accordingly, but the Committee views this as not being feasible.
SUMMARY
The Committee is convinced that implementing a redesign of the HIV delivery system would result in an improved system of HIV care based on the chronic care model and driven by the six aims for health system improvement: safe, effective, patient centered, timely, efficient, and equal. The Committee also recognizes that it is almost certainly impossible to create systems of care with all these attributes in all regions of the country in a short time frame. However, the Committee believes it is possible to modify
current relationships among providers of services in order to create systems of care that have more of these attributes than are currently experienced by most patients.
REFERENCES
APHA (American Public Health Association). 2003. Treatment Adherence to Anitretroviral Therapies: Recommendations for Best Practices. [Online]. Available: http://www.apha.org/ppp/hiv [accessed March 22, 2004].
Ashman JJ, Conviser R, Pounds MB. 2002. Associations between HIV-positive individuals’ receipt of ancillary services and medical care receipt and retention. AIDS Care 14:S109–S118.
Bangsberg DR, Perry S, Charlebois ED, Clark RA, Robertson M, Zolopa AR, Moss A. 2001. Non-adherence to highly active antiretroviral therapy predicts progression to AIDS. AIDS 15(9):1181–1183.
Bodenheimer T, Wagner EH, Grumbach K. 2002. Improving primary care for patients with chronic illness. Journal of the American Medical Association 288(14):1775–1779.
Boyd DJ. 2003. The bursting state fiscal bubble and state Medicaid budgets. Health Affairs 22(1):46–61.
Cohn SE, Berk ML, Berry SH, Duan N, Frankel MR, Klein JD, McKinney MM, Rastegar A, Smith S, Shapiro MF, Bozzette SA. 2001. The care of HIV-infected adults in rural areas of the United States. Journal of Acquired Immune Deficiency Syndromes 28(4):385–392.
CDC (Centers for Disease Control and Prevention). 2001. Strategies for reducing morbidity and mortality from diabetes through health-care system interventions and diabetes self-management education in community settings: a report on recommendations of the Task Force on Community Prevention Services. MMWR 50(RR-16):1–15. Atlanta, GA: CDC.
CMS (Centers for Medicare & Medicaid Services). 2003. Medicare General Information, Eligibility and Entitlement Manual. [Online]. Available: http://www.cms.hhs.gov/manuals/101_general/ge101index.asp [accessed February 20, 2004].
Davis M. 2002. Mental Illness and HIV Comorbidity: A Large and Vulnerable HIV Subpopulation. Paper prepared for the Committee on Public Financing and Delivery of HIV Care, Institute of Medicine. Washington, DC: unpublished.
DHHS (U.S. Department of Health and Human Services). 2004. Guidelines for the Use of Antiretroviral Agents in HIV-1-Infected Adults and Adolescents. [Online]. Available: http://aidsinfo.nih.gov/guidelines/default_db2.asp?id=50 [accessed March 23, 2004].
Garcia de Olalla P, Knobel H, Carmona A, Guelar A, Lopez-Colomes JL, Cayla JA. 2002. Impact of adherence and highly active antiretroviral therapy on survival in HIV-infected patients. Journal of Acquired Immune Deficiency Syndromes 30(1):105–110.
GAO (General Accounting Office). 2000. Ryan White CARE Act: Opportunities to Enhance Funding Equity. GAO/T-HEHS-00-150. Washington, DC: GAO.
GAO. 2001. Medicaid and SCHIP: States’ Enrollment and Payment Policies Can Affect Children’s Access to Care. GAO-01-883. Washington, DC: GAO.
Gifford AL, Groessl EJ. 2002. Chronic disease self-management and adherence to HIV medications. Journal of Acquired Immune Deficiency Syndromes 31:S163–S166.
IOM (Institute of Medicine). 2000. To Err Is Human: Building a Safer Health System. Washington, DC: National Academy Press.
IOM. 2001a. No Time to Lose: Getting More from HIV Prevention. Washington DC: National Academy Press.
IOM. 2001b. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: The National Academies Press.
IOM. 2002. Fostering Rapid Advances in Health Care: Learning from Systems Demonstration. Washington, DC: The National Academies Press.
IOM. 2003a. Priority Areas for National Action: Transforming Health Care Quality. Washington, DC: The National Academies Press.
IOM. 2003b. Measuring What Matters: Allocation Planning and Quality Assurance for the Ryan White CARE ACT. Washington, DC: The National Academies Press.
Kates J. 2004. Financing HIV/AIDS Care: A Quilt with Many Holes. Paper prepared for the Committee on Public Financing and Delivery of HIV Care, Institute of Medicine. Washington, DC: Kaiser Family Foundation.
Kates J, Marconi K, Mannle TE. 2001. Developing a performance management system for a federal public health program: the Ryan White CARE Act Titles I and II. Evaluation and Program Planning 24:145–155.
Laine C, Markson LE, Fanning TR, Turner BJ. 1999. Relationship between ambulatory care accessibility and hospitalization for persons with advanced HIV disease. Journal of Health Care for the Poor & Underserved. 10(3):313–327.
Lambrew J. 2001. Section 1115 Waivers in Medicaid and the State Children’ Health Insurance Program an Overview. Washington DC: Kaiser Commission on Medicaid and the Uninsured, Kaiser Family Foundation.
Levi J. 2002. The Response of Programs That Finance HIV Care and Services to an Evolving Continuum of Services Needs for People Living with HIV. Paper prepared for the Committee on Public Financing and Delivery of HIV Care, Institute of Medicine. Washington, DC: Unpublished.
Levi J, Kates J. 2000. HIV: Challenging the health care delivery system. American Journal of Public Health 90(7):1033–1036.
Lo W, MacGovern T, Bradford J. 2002. Association of ancillary services with primary care utilization and retention for patients with HIV/AIDS. AIDS Care 14:S45–S57.
McKenna MT, Taylor WR, Marks, JS. 1998. Current issues and challenges in chronic disease control. In: Chronic Disease Epidemiology and Control. 2nd edition. Washington, DC: United Book Press. Pp. 1–26.
McNabb J, Ross JW, Abriola K, Turley C, Nightengale CH, Nicolau DP. 2001. Adherence to highly active antiretroviral therapy predicts virologic outcome at an inner-city human immunodeficiency virus clinic. Clinical Infectious Diseases 33(5):700–705.
MedPAC (Medicare Payment Advisory Commission). 2003. Assessing payment adequacy and updating payment for physician services. In: Report to the Congress: Medicare Payment Policy. Washington, DC: Medicare Payment Advisory Commission. Pp. 105–118.
Moore RD, Chaisson RE. 1997. Costs to Medicaid of advancing immunosuppression in an urban HIV-infected patient population in Maryland. Journal of Acquired Immune Deficiency Syndromes and Human Retrovirology 14(3): 223–231.
Moore RD, Chaisson RE. 1999. Natural history of HIV infection in the era of combination antiretroviral therapy. AIDS 13(14):1933–1942.
NRC (National Research Council). 2001. Choosing the Right Formula: Initial Report. Washington, DC: National Academy Press.
New York State Department of Health. 1993. Supplement to DOH Memorandum 86-32 Update of Program Standards for Designated AIDS Center Hospitals. Health Facilities Series: H-22-93-25. Albany, NY: New York State Department of Health.
New York State Department of Health, AIDS Institute. No date. HIVQUAL Fact Sheet. Albany, NY: New York State Department of Health.
New York State Department of Health, AIDS Institute. 2003. Designated AIDS Center Program Description, and AIDS Intervention Management System, Program Description. Albany, NY: New York State Department of Health.
Palella FJ Jr, Delaney KM, Moorman AC, Loveless MO, Fuhrer J, Satten GA, Aschman DJ, Holmberg SD. 1998. Declining morbidity and mortality among patients with advanced human immunodeficiency virus infection. HIV Outpatient Study Investigators. New England Journal of Medicine 338(13):853–860.
Palella FJ Jr, Deloria-Knoll M, Chmiel JS, Moorman AC, Wood KC, Greenberg AE, Holmberg SD, HIV Outpatient Study Investigators. 2003. Survival benefit of initiating antiretroviral therapy in HIV-infected persons in different CD4+ cell strata. Annals of Internal Medicine 138(8):620–626.
Paterson DL, Swindells S, Mohr J, Brester M, Vergis EN, Squier C, Wagener MM, Singh N. 2000. Adherence to protease inhibitor therapy and outcomes in patients with HIV infection. Annals of Internal Medicine 133(1):21–30.
Ross DC, Cox L. 2003. Out in the Cold: Enrollment Freezes in Six State Children’s Health Insurance Programs Withhold Coverage from Eligible Children. Washington, DC: Kaiser Commission on Medicaid and the Uninsured, Kaiser Family Foundation.
Shirk C. 2003. Shaping Public Programs through Medicare, Medicaid, and SCHIP Waivers: The Fundamentals. National Health Policy Forum Background Paper. Washington, DC, National Health Policy Forum, George Washington University.
Turner BJ, Fleishman JA, Wenger N, London AS, Burnam MA, Shapiro MF, Bing EG, Stein MD, Longshore D, Bozzette SA. 2001. Effects of drug abuse and mental disorders on use and type of antiretroviral therapy in HIV-infected persons. Journal of General Internal Medicine 16(9):625–633.
Wagner EH. 2001. Meeting the needs of chronically ill patients. British Medical Journal 323(7319):945–946.
Wagner EH, Austin BT, Von Korff M. 1996. Organizing care for patients with chronic illness. Milbank Quarterly 74(4):511–544.
Wagner EH, Austin BT, Davis C, Hindmarsh M, Schaefer J, Bonomi A. 2001. Improving chronic illness care: translating evidence into action. Health Affairs 20(6):64–78.
Wheatly B. 2002. Issue Brief: Disease Management: Findings from Leading State Programs, Vol. 3, No. 3. Washington, DC: Academy Health State Coverage Initiatives.