Appendix D
Financing HIV/AIDS Care: A Quilt with Many Holes1
Jennifer Kates
Kaiser Family Foundation
INTRODUCTION
There are multiple sources of insurance coverage and care for people with HIV/AIDS in the United States. Insurance coverage is important to help promote access to regular and high-quality care. Of those who are insured and in the care system, most are covered by public sector insurance programs (primarily Medicaid or Medicare or both). The uninsured and the underinsured rely on an array of safety net programs including the Ryan White Comprehensive AIDS Resources Emergency (CARE) Act, community and migrant health centers, private “free clinics,” and public hospitals. Some people with HIV/AIDS have private insurance but may still need to rely on the Ryan White CARE Act to fill in the gaps.
These multiple sources of coverage and care for people with HIV, however, are not well coordinated across programs, making it difficult for patients, their advocates, and providers to navigate access. Moreover, these programs often vary by state, resulting in differential access across the country. As such, the current system of financing for HIV care represents a complex patchwork that leaves some outside the system and presents others with financial barriers to accessing needed care.2,3,4,5
Indeed, despite the existence of national treatment guidelines6 calling for early access to medical care and treatment, including highly active antiretroviral therapy (HAART), an estimated 42% to 59% of the almost one million people living with HIV/AIDS in the U.S. are not in regular care7 (see Figure D-1). While a proportion of these individuals may not know
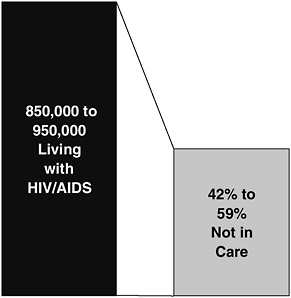
FIGURE D-1 Estimated number of people living with HIV/AIDS and proportion not in care, United States, 2000.
SOURCE: Fleming, P., et al., HIV Prevalence in the United States, 2000, 9th Conference on Retroviruses and Opportunistic Infections, Abstract #11, Oral Abstract Session 5, February 2002.
their HIV status (up to one-third of those living with HIV/AIDS8), others do not have access to insurance coverage (or face limits in their coverage) or care programs to help them afford the high cost of HIV treatment and services. The costs of HIV care present significant financial barriers to access for people with HIV/AIDS and strain the systems that serve them.
THE COST OF HIV CARE: A CONTINUING CONCERN
Financing care for people with HIV/AIDS has been of concern since early in the epidemic when people with HIV/AIDS often required expensive hospital inpatient and end-of-life care.9,10,11 The introduction of antiretroviral drug treatment in 1987 did not allay cost concerns—the very first FDA-approved AIDS drug, AZT, carried an initial pricetag of $10,000 a year.12 The current standard of care—combination antiretroviral therapy or HAART—calls for the use of expensive antiretrovirals in combinations of three, four, or even more medications.6 HAART has been largely responsible for significant declines in HIV-related deaths and improved health status for many.13,14 Combination therapy alone costs between $10,000
and $12,000 per patient per year depending on the regimen and payer (newer formulations of more than one antiretroviral drug may be priced as high as their component parts).15,16,17,29 When additional medical expenses for doctor’s visits, laboratory tests, and drugs to prevent or treat HIV-related opportunistic infections are taken into account, average annual costs rise to approximately $18,000 to $20,000 per patient, with even higher expenses for those with more advanced HIV-related illness.17,18,19,20,21
HIV is increasingly affecting people who are poor, outside the workforce, and have a history of barriers to access.14,22 Even among those individuals who have resources, the costs of HIV care can quickly exhaust their assets and may leave them impoverished. In addition, despite improvements in treatment, HIV/AIDS is often a disabling condition that forces individuals to leave the workforce (or be unable to enter the workforce) thereby losing access to both income and, eventually, private insurance. Indeed, many people with HIV in care are low-income (an estimated 46% have incomes below $10,000 a year) and unemployed (63%).19 Because of these factors, people with HIV rely heavily on the public sector for care.11,23,24
Expenditures for HIV/AIDS care, including public expenditures, have risen significantly over time.23,24 Spending increases largely reflect growing numbers of people living with HIV/AIDS in need of services and increasing health care costs, particularly for prescription drugs. A recent analysis by the National Institute for Health Care Management (NIHCM) Foundation, for example, found that national retail drug expenditures for antiretrovirals totaled $2,572.4 million in 2001, representing an almost 21 percent increase over 2000, compared to a 17% increase for all retail prescription drug sales over the same period.25 Analysis prepared for the Kaiser Family Foundation indicates that Medicaid spending on antiretrovirals increased significantly between 1991 and 1998, particularly after the introduction of HAART.26 Spending on HIV/AIDS treatments by AIDS Drug Assistance Programs (ADAPs) has also increased significantly over time.49
Despite the high costs to patients and the payers and programs that serve them, spending on HIV care (an estimated $6.1 billion in 1998)20 represents only a very small proportion—less than 1%—of estimated spending on overall direct personal health care expenditures in the United States.27 In addition, several studies have demonstrated the cost effectiveness of HIV care when compared to the treatment of many other disabling conditions.17,28,29,30 For example, a recent study found that the cost-effectiveness ratios of combination therapy for HIV infection ranged from $13,000 to $23,000 per quality-adjusted year of life gained (vs. no therapy) compared to $150,000 per quality-adjusted year of life gained for dialysis patients.29
INSURANCE COVERAGE OF PERSONS WITH HIV/AIDS
There are several challenges to assessing insurance coverage of persons with HIV/AIDS. These include difficulties in accessing the population of people with HIV/AIDS, given that a significant proportion is not in the care system and many do not know their HIV status, as well as limitations in data systems, methodological complexities, and the lack of capacity by major purchasers of care (e.g., state Medicaid programs) to perform client-level payer status analysis.
Coverage of Those in Care
The HIV Cost and Services Utilization Study (HCSUS), the only nationally representative study of people with HIV/AIDS in care, found that one-third to one-half of all people with HIV/AIDS were in regular care in 1996.19,31 More recent estimates from the Centers for Disease Control and Prevention (CDC) place this range slightly higher, between 41% and 58%.7
Most of those in care rely on public sector insurance programs or are uninsured, estimated to range between approximately 70%32 and 83%.33 HCSUS found that one-half are estimated to depend on the Medicaid (44%) or Medicare (6%) programs for coverage and one in five (20%) are uninsured32 (comparatively, among American adults overall, 6% are estimated to be covered by Medicaid, 2% by Medicare, and 19% are uninsured).34 Almost one-third have private insurance, a much smaller percentage than the U.S. adult population overall (31% of people with HIV compared to 73% of American adults overall).34 (See Figure D-2.) It is important to note that people with HIV/AIDS in care who are uninsured may be receiving care from Ryan White CARE Act programs or other safety net providers.
Many people with HIV/AIDS obtain their financing for care through multiple sources. For example, approximately 15% of those with Medicaid coverage also have other sources of coverage, primarily Medicare. About 12–13% of people with HIV/AIDS in care are estimated to be dual Medicaid and Medicare beneficiaries (called “dual eligibles” or “dual enrollees”).19,32,35 Viewed this way, Medicare covers approximately 19% of people with HIV/AIDS in care, including those also covered by Medicaid (6% with Medicare only and 12–13% with both Medicare and Medicaid).
More recent data on insurance coverage of people with HIV/AIDS in care are available from the HIV Research Network (HIVRN), a collaborative effort between the Agency for Healthcare Research and Quality (AHRQ), several other federal agencies, and the Johns Hopkins School of Medicine.36 While not national in scope, the HIVRN includes data from 1999 for 15 medical practices around the country, representing approximately 9,500 patients. Insurance coverage data were available for 42% of
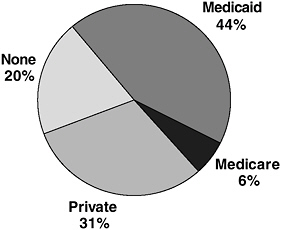
FIGURE D-2 Estimated insurance coverage of people living with HIV/AIDS in care, United States, 1996. Includes those with other coverage, primarily Medicare.
SOURCE: Fleishman, J., Personal communication, Analysis of HCSUS Data, January 2002.
HIVRN patients. Of the full sample, including those for whom coverage data were not available, 30% had Medicaid coverage, 5% had Medicare coverage, 4% were uninsured, and 3% were privately insured. Of the 42% for whom coverage data were available, 70% were covered by Medicaid, 13% by Medicare, 10% were uninsured, and 7% were privately insured.36
There are important differences in coverage by race, ethnicity, and sex (see Figure D-3). HSCUS found32 that African Americans and Latinos with HIV are much more likely to depend on Medicaid than whites (59% and 50% respectively, compared with 32% of whites). Minority Americans with HIV also are more likely to be uninsured than whites (22% of African Americans and 24% of Latinos compared with 17% of whites). Whites with HIV have the highest rate of private insurance across all racial and ethnic groups (44%). Women with HIV are also much more likely to rely on public insurance than their male counterparts, particularly Medicaid (61% of women compared with 39% of men), and less likely to be covered through the private sector (14% of women compared with 36% of men). This may be due in part to the fact that women are more likely to qualify for Medicaid as parents of dependent children or when pregnant. The intersection of race/ethnicity and sex is important here—most women newly infected with HIV and living with AIDS are women of color.13,37
Persons in care do not fare equally in the health care system. Analysis of data from HCSUS found that people with HIV who were covered by
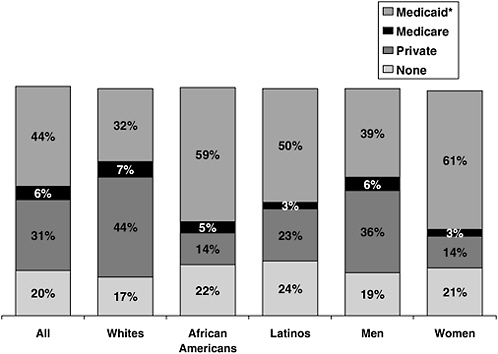
FIGURE D-3 Estimated insurance coverage of people living with HIV/AIDS in care by race/ethnicity and sex, United States, 1996. *Includes those with other coverage, primarily Medicare; May not total 100% due to rounding.
SOURCE: Fleishman, J., Personal communication, Analysis of HCSUS Data, January 2002.
Medicaid or were uninsured, and women and minority groups, fared more poorly on a range of access measures than those who were privately insured, male, and white.38 Other studies have found disparities as well.39,40,41,42 The reasons for this variation are not well understood but are likely due to a range of factors including the existence of historical barriers to access, disease stage at time of HIV diagnosis and at entrance into care, and HIV-related stigma.40,43,44
More recent analyses, including longitudinal analyses of the HCSUS national probability sample, have found that some of these differences have narrowed over time.38,40,41,42 In addition, findings related to differences in care vary by type of access measure. For example, while HCSUS findings indicate that those covered by Medicaid did not fare as well as those who were privately insured according to some measures of access (e.g., receipt of combination therapy, hospitalization rates),38 Medicaid coverage was also found to be a protective factor against delay in obtaining initial medical
care after HIV diagnosis, compared to other payers.45,46 Similarly, analysis of insurance coverage at time of initial HIV diagnosis indicates that those covered by Medicaid or by other public payers were less likely to be diagnosed late in illness than those who were privately insured (see discussion below).47
COVERAGE OF THOSE NOT YET IN CARE
Little is known about insurance coverage of people with HIV/AIDS who are not yet in regular HIV care. Recent analysis of the CDC’s HIV/AIDS Surveillance System (HARS) database provides the first assessment of payer status at time of initial HIV diagnosis, before entrance into HIV care.47 HARS data from 1994 through 1999 from 25 states with integrated HIV and AIDS surveillance were analyzed. Of the 104,780 persons diagnosed with HIV, data on insurance coverage were available for approximately half (52%). Of the full sample, including those for whom no coverage data were available, private coverage was the most common payer (17%); slightly more than one-third had public coverage or were uninsured—11% had Medicaid coverage, 10% had other public/government coverage, and 14% were uninsured. Of the 52% for whom insurance coverage data were available, 32% were privately insured, 22% had Medicaid coverage, 19% had other public coverage, and 27% were uninsured.47,48 (See Figure D-4.)
Insurance coverage varied by race/ethnicity, sex, and exposure category at time of diagnosis. For example, while similar proportions of men and women were uninsured, women were more than twice as likely to be covered by Medicaid at time of diagnosis. African American and Latino women were more likely to be covered by Medicaid than white women. Latinos were least likely to be insured.47
In addition, insurance coverage and timing of initial HIV diagnosis (e.g., whether or not a diagnosis was “late,” defined as having an AIDS diagnosis made within one year of the first reported HIV diagnosis) appear to be related. For example, between 34% and 54% were diagnosed late, depending on coverage. Those with private insurance were more likely to receive a late diagnosis (54%) than not (46%), while those with Medicaid, other public insurance, and the uninsured were more likely to receive an HIV diagnosis more than 12 months before their AIDS diagnosis.47
FEDERAL SPENDING ON HIV/AIDS CARE
Data on federal spending on HIV/AIDS care are derived from analysis of funds specifically earmarked in appropriations legislation for HIV/AIDS care and from agency estimates.24 Actual HIV/AIDS care expenditures for the two largest care programs for people with HIV/AIDS, Medicaid and
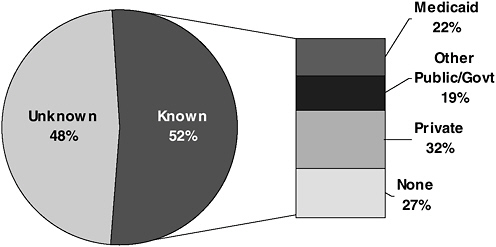
FIGURE D-4 Insurance coverage of persons with HIV/AIDS at time of diagnosis, 1994–1999.
SOURCE: Kates, J., Levi, J., Neal, J., Gallagher, K., “Learning More About the HIV-Infected Population Not IN Care in the United States: Using Public Health Surveillance Data to Inform Current Policy Challenges in Enhancing Access,” Poster TuPeG 5690, XIV International AIDS Conference, Barcelona, Spain, July 2002.
Medicare, are not available, and data presented here are based on actuarial estimates provided by the Centers for Medicare and Medicaid Services (CMS), the Department of Health and Human Services (DHHS) Agency that has responsibility for the Medicaid and Medicare programs. This is primarily due to the difficulties of assessing actual expenditures for people with HIV/AIDS within these two programs, since such spending data are not routinely collected; rather, to assess actual spending for people with HIV/AIDS, Medicaid and Medicare claims data would need to be analyzed using an algorithm specifically designed to identify claims for HIV-related care. Such algorithms have been developed, but are expensive and complex to implement at a national level and most states do not have the capacity to carry out these analyses on their own for their Medicaid programs. The advent of managed care presents additional challenges to collecting and analyzing actual spending data for people with HIV/AIDS.
In FY 2002, federal spending on HIV/AIDS-related medical care, research, prevention, and other activities was estimated to total $14.7 billion.23,24 Of that, more than half ($8.7 billion or 59%) was spent on health care and related support services for people with HIV/AIDS (an additional $1.6 billion was spent on disability income support provided through the Supplemental Security Income [SSI] and Social Security Disability Insurance
[SSDI] programs and housing assistance provided through the Housing Opportunities for Persons with AIDS [HOPWA] program). Not included in these care spending estimates is spending by state and local governments, although such spending represents an important component of public sector spending on HIV/AIDS care (for example, in FY 2002, the state share of Medicaid spending on AIDS was estimated by CMS to be $3.5 billion;23,24 in addition, in FY 2002, states reported that they provided $160 million to their AIDS Drug Assistance Programs).49
Medicaid is estimated to account for the federal government’s single largest expenditure on HIV/AIDS (29%). It also represents the largest amount of federal spending on health care for people with HIV/AIDS (48%), followed by Medicare (24%), and the Ryan White CARE Act (22%). The Department of Veterans Affairs accounts for another 4% of HIV/AIDS care spending, and remaining spending is spread among other agencies at the Department of Health and Human Services (e.g., the Substance Abuse and Mental Health Services Administration) and the Departments of Defense and Justice.24 (See Figure D-5.)
More than two-thirds (72% in FY 2002) of estimated federal spending on HIV/AIDS care is entitlement or mandatory spending, through the Medicaid and Medicare programs. (See Figure D-6.) This is in large part because many people with HIV/AIDS become low-income (or are already low-income) and disabled and qualify for the nation’s health insurance entitlement programs. Twenty-eight percent is discretionary spending, primarily through the Ryan White CARE Act, which is the third largest source of federal funding for HIV/AIDS care. These distinctions are important since most entitlement spending changes each year (increases or decreases) based on the need for and cost of services while discretionary spending is dependent on annual appropriations by Congress and may not correspond to the number of people who need care or the costs of that care.
Between FY 1995 and FY 2002, mandatory spending on HIV/AIDS care increased markedly (by 152%). Discretionary spending for HIV/AIDS care programs also increased significantly over this period (by 140%).24 As mentioned above, these increases largely reflect the advent of antiretroviral combination therapy, the rising cost of prescription drugs, and the growing numbers of people living with HIV/AIDS in need of care. Between FY 2001 and FY 2002, estimated mandatory spending on AIDS care increased by approximately 13% percent; it grew by 14% between FY 2002 and FY 2003.24,50,51 Federal funding for the Ryan White CARE Act increased by 6% between FY 2001 and FY 2002; it also grew by 6% between FY 2002 and FY 2003.24,52
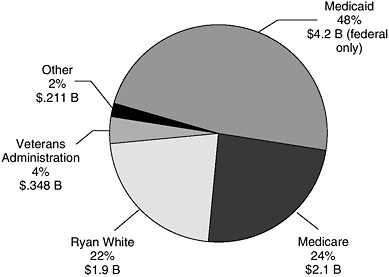
FIGURE D-5 Federal spending on HIV/AIDS care by program, FY 2002.
SOURCE: Kaiser Family Foundation, Federal HIV/AIDS Spending: A Budget Chartbook, FY 2002, September 2003.
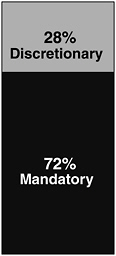
FIGURE D-6 Federal spending on HIV/AIDS care by type (mandatory or discretionary), FY 2002.
SOURCE: Kaiser Family Foundation, Federal HIV/AIDS Spending: A Budget Chartbook, FY 2002, September 2003.
HOW IS HIV/AIDS CARE FINANCED: MAJOR SOURCES OF COVERAGE AND CARE
There are several sources of coverage and care for people with HIV/AIDS, including insurance mechanisms such as Medicaid, Medicare, and private insurance, and publicly supported sources of care, such as the Ryan White CARE Act, the Veterans Health Administration, and community health centers.
The availability and accessibility of these programs vary significantly across the country. Eligibility depends on a variety of factors—including an individual’s health/disease status, family status, income, and assets—each of which may vary for a given individual over time. An individual may be eligible for more than one program in some states or none in others, and not all coverage and care programs are available in every state. Some programs are specifically designed for people with HIV/AIDS, such as those funded by the Ryan White CARE Act and HIV-specific Medicaid waivers. Others are more general coverage or care programs that are important for people with HIV/AIDS, particularly Medicaid and Medicare. Major sources of coverage and care are described below, and summary descriptions, as well as challenges, are provided in Table D-1. Table D-2 provides state-by-state data on variation in eligibility and other key characteristics for select programs.
Medicaid: Coverage for Low-Income Persons with HIV/AIDS
Medicaid (also known as Title XIX of the Social Security Act) is the largest source of public financing for HIV/AIDS care in the United States. Created in 1965, Medicaid is a jointly funded, jointly administered federal–state health insurance program for certain low-income people who meet one or more of several categorical eligibility requirements, including disability. Because many people with HIV/AIDS are low income—or become low-income—and disabled, Medicaid is a vital source of coverage for people with HIV. The program is estimated to cover approximately 44% of people with HIV, including those with AIDS, who are receiving care.32 As people progress in their illness, it is more likely they will become eligible for Medicaid. Among persons living with AIDS, 55% are estimated to be enrolled in Medicaid. Medicaid is also estimated to cover the health costs of up to 90% of children with AIDS.53 Among those recently diagnosed with HIV (for whom coverage data were available), more than one-fifth (22%) were already covered by Medicaid.47
CMS estimates that approximately 218,000 persons with AIDS were Medicaid beneficiaries in FY 2002 (due to the methodological challenges described above, the actual number of Medicaid beneficiaries with HIV/
AIDS is not currently known).53 Medicaid spending on AIDS care in FY 2002 was $7.7 billion, including $4.2 billion in federal dollars and $3.5 billion in state funds. In FY 2003, CMS estimates that federal Medicaid spending on AIDS care totaled $4.8 billion.50 Federal Medicaid spending on AIDS care more than tripled between FY 1995 and FY 2003, rising from $1.5 billion to $4.8 billion.23,24,50
At the federal level, the Medicaid program is administered by the Centers for Medicare & Medicaid Services of the Department of Health and Human Services. Through Medicaid, the federal government makes matching funds available to states that meet certain minimum federal standards in operating their Medicaid programs. Since 1982, all states have chosen to participate. States have broad flexibility in designing their Medicaid programs, and as a result there is significant variation in eligibility, benefits, provider payments, and other aspects of the program at the state level.54,55
Eligibility
To be eligible for Medicaid a person must have income, assets, and resources at or below a state’s standard and generally meet one of several other eligibility criteria. There are certain categories of individuals that all states participating in Medicaid must cover, including the disabled. Most adults with HIV/AIDS who qualify for Medicaid do so because they meet the disability and income criteria of the federal SSI program for persons who are aged, blind, or disabled. For purposes of SSI eligibility, a person is disabled if they are unable to engage in any “substantial gainful activity by reason of a medically determined physical or mental impairment expected to result in death, or that has lasted or can be expected to last for a continuous period of at least 12 months.”54 There are eleven states, known as 209B states, however, that may apply more restrictive eligibility rules than those under SSI.56
Optional Medicaid eligibility categories are also important for people with HIV/AIDS, particularly the medically needy program. The medically needy program enables those who meet categorical eligibility requirements, such as disability, to spend-down their incomes on medical expenses to meet their state’s income eligibility threshold; these income thresholds vary significantly across states.56 Individuals qualifying as medically needy must also meet a resource test. Thirty-six states offer this optional program, 35 of which make it available to those who are disabled.57 Given the high costs of HIV care, the medically needy program can be an important option available to people with HIV/AIDS.54,57
The Omnibus Budget Reconciliation Act of 1986 (OBRA 86) gave states the option to provide full Medicaid benefits to all aged and disabled persons with incomes up to 100% of the federal poverty level (FPL). Nine-
TABLE D-1 Major Sources of Coverage and Care for HIV/AIDS Financing, with Benefits and Challenges
|
Source of Coverage/Care (funding source) |
Eligibility |
Benefits |
|
Medicaid (Federal and state funding) |
Individuals must have income and assets at or below a state’s standard and meet categorical eligibility criteria Mandatory groups include individuals who meet the disability and income criteria of the SSI program (some states use more restrictive criteria), certain low-income parents and children, low-income pregnant women, and certain low-income individuals who qualify for Medicare Optional groups include the medically needy and certain low-income working disabled Most people with HIV/AIDS who qualify for Medicaid meet income and disability criteria of the SSI program |
Mandatory services include Inpatient/outpatient hospital care Physician visits Lab and x-ray services Home health care Long-term care Optional benefits include: Prescription drugs Case management Dental services |
|
Medicare (Federal funding) |
Age 65+ Under 65 disabled who receive Social Security Disability Insurance (SSDI) benefits Individuals with end-stage renal disease Most people with HIV/AIDS who qualify for Medicare are disabled SSDI beneficiaries |
Part A Services include Inpatient hospital care Skilled nursing facilities Hospice care Home health care Part B Services include: Physician visits Outpatient hospital services Labs, x-rays, and medical equipment Medicare+Choice (M+C) plans contract with Medicare to provide both Part A and B services to enrolled beneficiaries. Part D adds outpatient prescription drug coverage, effective January 1, 2006. Beneficiaries entitled to Part A or enrolled in Part B are eligible to enroll in Part D. |
|
Challenges |
|
Eligibility “Catch-22”—SSI eligibility based on being disabled although therapies exist that can prevent disability, early care recommended Returning to work/entering workforce makes continuation of coverage uncertain Variation across states in eligibility, benefits, and other aspects of program Access to experienced HIV providers may be issue, particularly in Medicaid managed care context Need to ensure adequate capitation/reimbursement rates and services; historically low payment rates for providers and institutions HIV/AIDS drug prices higher than for other government purchasers |
|
Eligibility “Catch-22”—SSDI eligibility based on being disabled although therapies exist that can prevent disability, early care recommended Must also have sufficient work history to be eligible 29-month waiting period from determination of SSDI eligibility before coverage begins High cost-sharing requirements No cap on out-of-pocket spending Lack of outpatient prescription drug benefit currently; prescription drug coverage benefit as of January 1, 2006 Prescription drug benefit may present new challenges, particularly to the dually eligible, for whom Medicaid prescription drug benefits will end. Challenges may include difficulty navigating the enrollment process; the potential for temporary lapse in coverage; variation and limitation in formularies; out-of-pocket expenses, which may be higher than those paid under Medicaid; and denial of prescription drugs if co-payment cannot be met |
|
Source of Coverage/Care (funding source) |
Eligibility |
Benefits |
|
Ryan White CARE Act (Federal funding with some state and local funding) |
Uninsured and underinsured individuals and families living with HIV/AIDS Eligibility set by states and municipalities |
Primarily outpatient and related support services including Physician/clinic visits Prescription drugs (through ADAP) Case management Home health and hospice care Dental care Developmental and rehabilitation services Insurance continuation |
|
Private Health Insurance (Employer, employees, individuals) |
Group Coverage, primarily through an employer or association Individual coverage purchased through carrier/broker Most people with HIV/AIDS who are privately insured obtain group coverage through employer |
Group plans tend to cover Inpatient and outpatient hospital care Physician visits Prescription drugs Lab tests, x-rays, and durable medical equipment Inpatient and outpatient mental health services Individual plans vary from policy to policy |
|
Department of Veterans Affairs (Federal funding) |
Any veteran of the armed services, including disabled veterans |
Outpatient, inpatient, long-term care, prescription drugs, and range of other services VA operates AIDS service for veterans with HIV/AIDS |
|
Community Health Centers and Other Safety Net Providers (Federal, state, and local funding) |
Varies by type of provider Primarily serve low-income individuals, including uninsured or underinsured individuals and families; also serve many Medicaid beneficiaries |
Services vary by type of provider but can include Physician/clinic visits Inpatient/outpatient hospital care Emergency care Some preventive services |
|
Challenges |
|
Discretionary grant program dependent on annual appropriations by Congress and in some cases, states and municipalities Funding does not necessarily match need for or cost of care Variation in programs and services across the country More CARE dollars needed to fill gaps in jurisdictions with less generous access to other programs Allocation of most CARE Act dollars based on AIDS cases, not HIV infection and may not reflect current burden and recent trends |
|
Medical underwriting in the individual market may lead to denial of or limits on coverage—HIV generally considered uninsurable condition Premiums for individual policies often too high to afford Annual or lifetime caps on benefits may limit care for people with HIV/AIDS and other chronic conditions Limits may be placed on specific services (e.g., number of prescriptions filled, number of physician visits) May be other co-pays or deductibles |
|
Disability must be service-related and/or veteran must be poor to receive subsidized care, otherwise must pay share of costs Not all veterans live near VA facilities |
|
Most are discretionary grant funded and dependent on annual appropriations by Congress, states, and municipalities Funding does not necessarily match need for or cost of services Access to experienced HIV providers may be issue |
TABLE D-2 State Variation in Insurance Coverage and Care Programs for People with HIV/AIDS: Select Programs, Both HIV-Specific and General
|
State/Territory |
SSI Eligibility %FPL, 20001 |
Pregnant Women Eligibility, %FPL, 20001 |
Prescription Limitations per Month # per month 20033 |
|||
|
United States (Total number of states) |
— |
— |
36 states (35 for disabled) |
11 states |
14 states |
20 states (17 HCBW, 3 1115, 2 TWWIIA) |
|
Alabama |
74 |
133 |
— |
— |
— |
— |
|
Alaska |
74 |
200 |
— |
— |
— |
— |
|
Arizona |
74 |
140 |
— |
— |
— |
— |
|
Arkansas |
74 |
133 |
Yes (15) |
— |
6 |
— |
|
California |
74 |
300A |
Yes (83) |
— |
6 |
HCBS |
|
Colorado |
74 |
133 |
— |
— |
— |
HCBS |
|
Connecticut |
69 |
185 |
Yes (80/66) |
Yes |
— |
— |
|
Delaware |
74 |
200 |
— |
— |
— |
HCBS |
|
District of Columbia |
74 |
200 |
Yes (53) |
— |
— |
1115, TWWIIA, HCBS |
|
Florida |
74 |
185 |
Yes (25) |
— |
4 |
HCBS |
|
Georgia |
74 |
235 |
Yes (44) |
— |
5 |
— |
|
Hawaii |
Other |
185 |
Yes (51) |
Yes |
— |
HCBS |
|
Idaho |
74 |
133 |
— |
— |
— |
— |
|
Illinois |
41 |
200 |
Yes (40) |
Yes |
— |
HCBS |
|
Indiana |
76 |
150 |
— |
Yes |
— |
— |
|
Iowa |
74 |
200 |
Yes (67) |
— |
— |
HCBS |
|
Kansas |
74 |
150 |
Yes (66) |
— |
5 |
— |
|
Eligibility, %FPL, June 20026 |
Number of Drugs on Formulary, June 20026 |
Title I EMA(#), 20018 |
Title III EIS Site (#), 20018 |
Ryan White Health Insurance Continuation Program, 20018 |
State Pharmacy Assistance Programs for Non-Seniors—Subsidy (S) & Discount (D) Programs (not-HIV specific), 20029,10 |
State-Sponsored High-Risk Pool, (not HIV specific), 200111 |
|
|
— |
— |
16 states |
28 states (51 EMAs) |
50 states (310 EIS) |
37 states |
14 states |
29 states |
|
250 |
26 |
Waiting List |
— |
Yes (9) |
— |
— |
Yes |
|
300 |
62 |
Capped Enrollment |
— |
Yes (2) |
Yes |
— |
Yes |
|
300 |
27 |
— |
Yes (1) |
Yes (3) |
— |
Yes (S)C |
— |
|
300 |
43 |
Capped Enrollment |
— |
Yes (3) |
— |
— |
Yes |
|
400 |
144 |
— |
Yes (9) |
Yes (30) |
Yes |
Yes (D) |
Yes |
|
300 |
40 |
Waiting List |
Yes (1) |
Yes (2) |
Yes |
— |
Yes |
|
400 |
170 |
— |
Yes (2) |
Yes (6) |
— |
Yes (S) |
Yes |
|
500 |
137 |
— |
— |
Yes (1) |
Yes |
Yes (S) |
— |
|
300 |
65 |
— |
Yes (1) |
Yes (5) |
— |
Yes (S) |
— |
|
350 |
53 |
— |
Yes (6) |
Yes (19) |
Yes |
Yes (D) |
Yes |
|
300 |
47 |
— |
Yes (1) |
Yes (13) |
Yes |
— |
— |
|
400 |
85 |
— |
— |
Yes (1) |
Yes |
— |
— |
|
200 |
35 |
Capped Enrollment |
— |
Yes (1) |
— |
— |
— |
|
400 |
67 |
— |
Yes (1) |
Yes (13) |
Yes |
Yes (S) |
Yes |
|
300 |
67 |
Waiting List |
— |
Yes (2) |
Yes |
— |
Yes |
|
200 |
32 |
— |
— |
Yes (4) |
Yes |
Yes (D) |
Yes |
|
300 |
47 |
— |
YesB |
Yes (1) |
Yes |
— |
Yes |
|
State/Territory |
SSI Eligibility %FPL, 20001 |
Pregnant Women Eligibility, %FPL, 20001 |
Prescription Limitations per Month # per month 20033 |
|||
|
Kentucky |
74 |
185 |
Yes (30) |
— |
— |
— |
|
Louisiana |
74 |
133 |
Yes (14) |
— |
8 |
— |
|
Maine |
74 |
200 |
Yes (44) |
— |
— |
1115 |
|
Maryland |
74 |
200 |
Yes (49) |
— |
— |
— |
|
Massachusetts |
74 |
200 |
Yes (NA) |
— |
— |
1115 |
|
Michigan |
74 |
185 |
Yes (57) |
— |
— |
— |
|
Minnesota |
70 |
275 |
Yes (67) |
Yes |
— |
— |
|
Mississippi |
— |
185 |
— |
— |
5 |
TWWIIA |
|
Missouri |
74 |
185 |
— |
Yes |
5 |
HCBS |
|
Montana |
74 |
133 |
Yes (73) |
— |
— |
HCBS |
|
Nebraska |
74 |
185 |
Yes (55) |
— |
— |
— |
|
Nevada |
74 |
133 |
— |
— |
— |
— |
|
New Hampshire |
76 |
185 |
Yes (76) |
Yes |
— |
— |
|
New Jersey |
74 |
185 |
Yes (51) |
— |
— |
HCBS |
|
New Mexico |
74 |
185 |
— |
— |
— |
HCBS |
|
New York |
74 |
200 |
Yes (87) |
— |
Yes - Annual Limit |
— |
|
North Carolina |
74 |
185 |
Yes (34) |
— |
6 |
HCBS |
|
North Dakota |
65 |
133 |
Yes (66) |
Yes |
— |
— |
|
Ohio |
64 |
150 |
— |
Yes |
— |
— |
|
Oklahoma |
74 |
185 |
Yes (36) |
Yes |
3 |
— |
|
Oregon |
74 |
170 |
Yes (58) |
— |
— |
— |
|
Pennsylvania |
74 |
185 |
Yes (59) |
— |
— |
HCBS |
|
Eligibility, %FPL, June 20026 |
Number of Drugs on Formulary, June 20026 |
Title I EMA(#), 20018 |
Title III EIS Site (#), 20018 |
Ryan White Health Insurance Continuation Program, 20018 |
State Pharmacy Assistance Programs for Non-Seniors—Subsidy (S) & Discount (D) Programs (not-HIV specific), 20029,10 |
State-Sponsored High-Risk Pool, (not HIV specific), 200111 |
|
|
300 |
30 |
Waiting List |
— |
Yes (4) |
Yes |
— |
Yes |
|
200 |
18 |
— |
Yes (1) |
Yes (8) |
Yes |
— |
Yes |
|
300 |
38 |
— |
— |
Yes (2) |
— |
Yes (S, D)C |
— |
|
400 |
85 |
— |
Yes (1) |
Yes (3) |
Yes |
Yes (S,D) |
— |
|
less than $50,000 per yr |
open |
— |
Yes (1) |
Yes (16) |
Yes |
Yes (S) |
— |
|
450 |
160 |
— |
Yes (1) |
Yes (4) |
Yes |
— |
— |
|
300 |
112 |
— |
Yes (1) |
Yes (2) |
Yes |
— |
Yes |
|
400 |
43 |
— |
— |
Yes (7) |
— |
— |
Yes |
|
300 |
270 |
— |
Yes (2) |
Yes (4) |
Yes |
— |
Yes |
|
300 |
49 |
Waiting List |
— |
Yes (1) |
Yes |
— |
Yes |
|
200 |
18 |
Waiting List |
— |
Yes (2) |
Yes |
— |
Yes |
|
400 |
55 |
— |
Yes (1) |
Yes (2) |
Yes |
— |
— |
|
300 |
32 |
— |
YesB |
— |
Yes |
— |
Yes |
|
500 |
open |
— |
Yes (5) |
Yes (8) |
Yes |
Yes (S) |
— |
|
300 |
60 |
— |
— |
Yes (3) |
Yes |
— |
Yes |
|
less than $44,000 per yr |
463 |
— |
Yes (3) |
Yes (41) |
Yes |
— |
— |
|
125 |
51 |
Capped Enrollment |
— |
Yes (9) |
— |
— |
— |
|
400 |
86 |
— |
— |
— |
— |
— |
Yes |
|
300 |
69 |
— |
Yes (1) |
Yes (7) |
Yes |
— |
— |
|
200 |
65 |
Other |
— |
Yes (2) |
— |
— |
Yes |
|
200 |
56 |
Waiting List |
Yes (1) |
Yes (1) |
Yes |
— |
Yes |
|
less than $30,000 per yr |
69 |
— |
Yes (1) |
Yes (18) |
— |
— |
— |
|
State/Territory |
SSI Eligibility %FPL, 20001 |
Pregnant Women Eligibility, %FPL, 20001 |
Prescription Limitations per Month # per month 20033 |
|||
|
Rhode Island |
74 |
250 |
Yes (87) |
— |
— |
— |
|
South Carolina |
74 |
185 |
— |
— |
4 |
HCBS |
|
South Dakota |
74 |
133 |
— |
— |
— |
— |
|
Tennessee |
74 |
185 |
Yes (34) |
— |
— |
— |
|
Texas |
74 |
185 |
Not for disabled |
— |
3 |
— |
|
Utah |
74 |
133 |
Yes (53) |
— |
— |
— |
|
Vermont |
74 |
200 |
Yes (111/102) |
— |
— |
— |
|
Virginia |
74 |
133 |
Yes (47) |
Yes |
— |
HCBS |
|
Washington |
74 |
185 |
Yes (78) |
— |
>4 brand review |
HCBS |
|
West Virginia |
74 |
150 |
Yes (28) |
— |
|
— |
|
Wisconsin |
74 |
185 |
Yes (83) |
— |
— |
— |
|
Wyoming |
74 |
133 |
— |
— |
— |
— |
|
Puerto Rico |
— |
— |
— |
— |
— |
— |
|
Virgin Islands |
— |
— |
— |
— |
— |
— |
|
Guam |
— |
— |
— |
— |
— |
— |
|
NOTES: A California’s Medicaid program covers pregnant women with incomes up to 200%FPL; The Access for Infants and Mothers (AIM) program covers pregnant women between 200%FPL and 300%FPL. B The Eligible Metropolitan Area (EMA) in this state is part of another state’s EMA. C Arizona program not yet operational. Maine discount program halted pending legal action. Vermont discount program not yet operational. D Coverage for high-risk individuals is now provided under TennCare, the state’s Medicaid program. The Tennessee Comprehensive Health Insurance Pool ceased operations on June 30, 1996. |
||||||
|
Eligibility, %FPL, June 20026 |
Number of Drugs on Formulary, June 20026 |
Title I EMA(#), 20018 |
Title III EIS Site (#), 20018 |
Ryan White Health Insurance Continuation Program, 20018 |
State Pharmacy Assistance Programs for Non-Seniors—Subsidy (S) & Discount (D) Programs (not-HIV specific), 20029,10 |
State-Sponsored High-Risk Pool, (not HIV specific), 200111 |
|
|
400 |
57 |
— |
— |
Yes (2) |
Yes |
— |
— |
|
300 |
48 |
— |
— |
Yes |
(7) Yes |
— |
Yes |
|
300 |
41 |
Waiting List |
— |
Yes (1) |
Yes |
— |
— |
|
300 |
43 |
— |
— |
Yes (4) |
Yes |
— |
See note D |
|
200 |
36 |
— |
Yes (5) |
Yes (9) |
Yes |
— |
Yes |
|
200 |
18 |
— |
— |
Yes (1) |
Yes |
— |
Yes |
|
200 |
69 |
— |
— |
Yes (1) |
Yes (S,D)C |
Yes |
— |
|
300/333 |
51 |
— |
Yes (1) |
Yes (5) |
— |
— |
— |
|
300 |
137 |
Other |
Yes (1) |
Yes (5) |
Yes |
— |
Yes |
|
250 |
27 |
Waiting List |
YesB |
Yes (1) |
Yes |
— |
— |
|
300 |
43 |
— |
YesB |
Yes (4) |
Yes |
— |
Yes |
|
200 |
51 |
Other |
— |
— |
— |
Yes (S) |
Yes |
|
certified as indigent |
115 |
— |
Yes (3) |
Yes (9) |
— |
— |
— |
|
200 |
26 |
— |
— |
Yes (2) |
— |
— |
— |
|
200 |
26 |
— |
— |
— |
— |
— |
— |
|
SOURCES: 1 Kaiser Family Foundation, State Health Facts Online, Medicaid & SCHIP, Eligibility Levels for Other Medicaid Enrollment Groups as Percent of Federal Poverty Level, www.statehealthfacts.org (Accessed January 18, 2003). See website for specific notes on state eligibility levels. 2 Analysis prepared for the Kaiser Commission on Medicaid and the Uninsured by Jeff Crowley, Georgetown University, 2003. 3 Kaiser Commission on Medicaid and the Uninsured, Medicaid Outpatient Prescription Drug Benefits: Findings from a National Survey, 2003, December 2003. continued |
|||||||
|
4 Centers for Medicare & Medicaid Services, Personal communication, August 2002 5 Kaiser Family Foundation, State Health Facts Online, HIV/AIDS, Status of State Medicaid Expansion Efforts for People with HIV, www.statehealthfacts.org (Accessed January 18, 2003). 6 National Alliance of State and Territorial AIDS Directors/Kaiser Family Foundation/AIDS Treatment Data Network, National ADAP Monitoring Project, Annual Report, April 2003. 7 National Alliance of State and Territorial AIDS Directors, ADAP Watch, September 2003. Other restrictions include reduced formularies, annual expenditure caps, cost-sharing, and lowering financial eligibility criteria. 8 Health Resources and Services Administration, HIV/AIDS Bureau, http://hab.hrsa.gov/ (Accessed August 30, 2002); Personal communication, HIV/AIDS Bureau, August and November 2002. 9 Kaiser Family Foundation, State Health Facts Online, Medicare, State Pharmaceutical Assistance Programs, www.statehealthfacts.org (Accessed January 18, 2003). 10 National Conference of State Legislatures, State Pharmaceutical Assistance Programs, http://www.ncsl.org/programs/health/drugaid.htm (Accessed January 18, 2003). 11 Kaiser Family Foundation, State Health Facts Online, Managed Care and Health Insurance, State Sponsored High Risk Insurance Pools, www.statehealthfacts.org (Accessed January 18, 2003). |
teen states use this option (17 have expanded Medicaid elig|ibility up to the poverty level and 2 have raised the income standard but not to the poverty level).58
Some children and adults with HIV/AIDS also qualify for Medicaid before they are disabled if they are poor and meet other program eligibility categories. The primary non-disabled categories are for low-income children and their parents and pregnant women. The income limits for each of these different eligibility criteria vary. Some Medicaid beneficiaries are also covered by Medicare, as discussed below.19,32,54
Benefits
Federal rules require states participating in Medicaid to cover a set of mandatory services to the categorically needy in order to receive federal matching payments. States may also choose to provide optional services and receive matching payments. One of the most important benefits for people with HIV/AIDS, prescription drugs,59 is an optional benefit that all states have chosen to provide. Other optional services that can be important for people with HIV/AIDS include targeted case management, prevention services, and hospice services. Currently, 17 states have developed home and community based services (HCBS) programs for people with
AIDS using Section 1915(c) waivers. HCBS waiver programs are for individuals determined to be at risk for institutional care and have been used for people with AIDS to maximize their independence through the use of services such as case management, adult day health care, and hospice care.60
States may place limits on some Medicaid services, and several limit the number of prescriptions allowed per month, the length of hospital inpatient services, and the number of physician visits (these limits cannot, however, be applied selectively to one group of beneficiaries). In 2003, for example, 14 states limited the number of prescriptions per month or year.61 States may also impose “nominal” cost-sharing requirements on most nonemergency mandatory or optional services with respect to adults (other than pregnant women and institutionalized patients). Emergency care, hospice care, and family planning services are excluded from cost-sharing.
Challenges
Certain aspects of the Medicaid program present challenges to people living with HIV/AIDS, as well as to low-income adults more generally (since low-income adults mainly qualify for Medicaid after they are disabled). These include the following:
Eligibility “Catch-22”
One main challenge facing low-income people with HIV/AIDS is a Medicaid eligibility “Catch-22”—many are not eligible for Medicaid until they become disabled, despite the availability of therapies that may prevent disability. Several options are being considered to address this, including:
-
Section 1115 Waivers. Several states have applied for or are considering Medicaid Section 1115 waivers to expand Medicaid eligibility to low-income people with HIV prior to disability.62 To date, three states—Maine, Massachusetts, and the District of Columbia—have received federal approval to operate such waivers. Only the Massachusetts and District of Columbia waiver is currently operational. A major barrier to the 1115 waiver strategy is that 1115 waivers must be “budget neutral” (i.e., the costs of the expansion over a designated period of time, usually 5 years, cannot exceed the costs to Medicaid in the absence of the expansion). This standard has been hard for states to meet. While analyses have shown that additional, non-Medicaid savings will accrue through such expansions (e.g., to SSI, SSDI, Medicare, and the Ryan White AIDS Drug Assistance Program), these savings cannot be included in budget neutrality calculations under current policy.17,30
-
The Ticket to Work/Work Incentives Improvement Act of 1999.
-
The Ticket to Work/Work Incentives Improvement Act (TWWIIA) included an option for states to launch demonstration projects to provide Medicaid to workers with potentially severe disabilities, including HIV/AIDS, who are not yet disabled but whose health conditions could be expected to cause disability. This demonstration is funded at a total of $250 million over the FY 2001–2006 period. Mississippi and the District of Columbia have been awarded approval for HIV-related demonstrations under the Act.62
-
The Early Treatment for HIV Act. Because of the many barriers faced by states through the 1115 process and the limited nature of the TWWIIA demonstration, Congress is considering the Early Treatment for HIV Act (ETHA). ETHA would create a new state option to expand Medicaid coverage to low-income people living with HIV who are not disabled, similar to legislation passed in 2000 by Congress that gave states the option to provide Medicaid coverage to women diagnosed with breast and cervical cancer.63
Returning to/Entering the Workforce
While new treatments are enabling more Medicaid beneficiaries with HIV to enter or return to the workforce, the continuation of their Medicaid coverage is uncertain. Current Medicaid rules do not allow beneficiaries to keep their health coverage when they earn income above the eligibility level. This may present a barrier to working since the cost of treatments that allow people with HIV to enter the workforce may be prohibitive without Medicaid coverage. In addition, people with HIV/AIDS who re-enter or enter the workforce for the first time may not be able to get insurance through the workplace. The Balanced Budget Act of 1997 gave states the option to allow low-income disabled individuals to keep their Medicaid coverage while working and earning income up to 250 percent of poverty. The TWWIIA also made several changes designed to encourage low-income individuals with disabilities to work while allowing them to keep their Medicaid coverage.64 In both these cases, however, relatively few states have exercised these options.65
Variation in state Medicaid programs resulting in different levels of access across the states
In states with less generous Medicaid programs (e.g., states with limits on the number of prescriptions filled per month or states with lower income eligibility thresholds), low-income people with HIV may have to rely on other programs to fill the gaps or may not have access to needed services.66
Medicaid payment rates to providers and institutions
Historically low payment rates have been shown to affect access to care for Medicaid beneficiaries.67
Medicaid managed care
Medicaid managed care also presents new challenges to the financing and delivery of HIV care. These include the difficulties of developing adequate capitation and reimbursement rates in the context of rapidly changing standards of care; the need to ensure access to the continuum of care, including full access to prescription drugs within managed care plan formularies; and the need to ensure access to experienced HIV providers.54,68
Different prices paid by different government purchasers for the same medications
A recent analysis indicates that Medicaid, despite being the largest public purchaser of HIV/AIDS drugs, pays higher prices for these medications than other government purchasers, including the VA and ADAP programs.69
Finally, in addition to these challenges, states are experiencing increasingly difficult fiscal situations, with most facing budget shortfalls. As states struggle to balance their budgets, many are seeking ways to reduce their Medicaid spending, the second-largest expenditure in most state budgets, and the one that has grown faster than many other state programs. States are exploring or have already implemented several strategies for controlling Medicaid costs, including controlling pharmacy costs and provider payments, increasing cost sharing, eliminating optional benefits, and reducing eligibility. These strategies may limit beneficiary access to Medicaid, including for beneficiaries with HIV/AIDS, and limit the revenue flows to experienced HIV providers, including individual practitioners, clinics, and hospitals.70,71
Medicare: Coverage for Disabled and Elderly Persons with HIV/AIDS
Also created in 1965 and administered by CMS, Medicare (Title XVIII of the Social Security Act) is the nation’s federal health insurance program for the elderly and disabled. Medicare is an important source of coverage for people with HIV/AIDS who are disabled, have sufficient work history to qualify for disability insurance, and live long enough to qualify for Medicare. Many of these individuals also qualify for Medicaid because they are low-income. Medicare is estimated to cover approximately 19% of
people with HIV/AIDS who are receiving regular care, including an estimated 6% covered by Medicare alone and an additional 12–13% covered by both Medicare and Medicaid (a small percentage may also have private coverage).19,32,35 CMS estimates that Medicare served approximately 44,000 persons with AIDS in 2001 and 46,000 persons with AIDS in 2002.72
Forecasting the growth in the number of Medicare beneficiaries with HIV/AIDS is difficult—on the one hand, the number of beneficiaries may grow as more people with HIV/AIDS live longer; on the other, the success of combination antiretroviral therapy may keep people with HIV from meeting the SSDI eligibility criteria needed to receive Medicare coverage. In addition, an increasing proportion of those becoming newly infected with HIV are estimated to be low income and may therefore be less likely to have sufficient work history to meet eligibility criteria.
Medicare spending on HIV/AIDS is estimated to have increased over time. Today, Medicare is the second largest source of federal financing for HIV/AIDS care, after Medicaid, accounting for an estimated $2.1 billion in FY 2002 and $2.4 billion in FY 2003, according to CMS.50 Estimated Medicare spending on people with AIDS has more than doubled since FY 1995, when it was $1 billion.23,24,50
Eligibility
Most Americans ages 65 and older are entitled to Medicare as soon as they are eligible for Social Security payments. People under age 65 who receive SSDI benefits and individuals with end-stage renal disease may also qualify for Medicare. Most people with HIV/AIDS who receive Medicare benefits do so as a result of their SSDI status. Eligibility for SSDI, however, is limited to those who have sufficient work histories and who are permanently disabled. In addition, federal law requires a 5-month waiting period after disability determination to receive SSDI benefits and then a 24-month waiting period before an SSDI beneficiary can join Medicare, resulting in a total of 29 months before receipt of health benefits.73
For those Medicare beneficiaries with HIV who are low income, Medicaid coverage is critical, filling in the gaps in coverage for these beneficiaries. Depending on income, Medicaid provides varying levels of coverage to low-income Medicare beneficiaries including payment of premiums, some cost-sharing, and coverage of services during the 29-month waiting period. In addition, Medicaid has been a critical source of prescription drug coverage for dual beneficiaries because outpatient prescription drugs are not covered by Medicare.65,74 With the passage of the Medicare Prescription Drug, Improvement, and Modernization Act of 2003 (P.L. 108-173) in December 2003, the role of Medicaid as a provider of prescription drug
coverage to the dually eligible will be eliminated when the new law goes into effect in 2006 (see discussion below).
Benefits
Medicare is comprised of the following parts:75
-
Part A covers inpatient hospital services, skilled nursing facilities, home health services, and hospice care.
-
Part B helps pay for the cost of physician services, outpatient hospital services, medical equipment and supplies, and other health services and supplies.
-
Medicare+Choice (M+C) plans contract with Medicare to provide both Part A and B services to enrolled beneficiaries.
-
Part D adds outpatient prescription drug coverage to the Medicare program, effective January 1, 2006. This new drug benefit would be delivered through private risk-bearing entities under contract with DHHS, and drug benefits would be provided through stand-alone prescription drug plans (PDPs) or comprehensive managed care plans, known as Medicare Advantage Plans. Beneficiaries entitled to Part A or enrolled in Part B will be eligible to enroll in Part D. The law establishes a new Medicare Prescription Drug Discount Card and Transitional Assistance Program to provide relief to beneficiaries before the benefit is fully implemented in 2006.74,76
Challenges
People with HIV/AIDS, as well as people with disabling conditions more generally, face certain challenges in accessing Medicare or needed benefits through the Medicare program. One such challenge is the 29-month waiting period for benefits. Early on in the AIDS epidemic, people with HIV who otherwise might have been eligible for Medicare benefits often did not live long enough to begin receiving them. Even though people with HIV are now living longer, the waiting period still presents a barrier to accessing Medicare coverage and during that 29-month period, they have to find care elsewhere. In addition, to be eligible for benefits, a person with HIV must have sufficient work history and, as with Medicaid, must meet federal disability criteria. In the case of the former, because HIV is increasingly affecting people who are poor and outside the workforce, it may be difficult for some to meet the work history requirements needed to access the program. In the case of the latter, even people with HIV who have sufficient work history may find themselves facing a similar “Catch-22” in eligibility that is encountered with the Medicaid program, since they cannot become eligible for SSDI benefits until they are disabled.
There are also limitations to the Medicare program that present particular problems to people with HIV/AIDS and others with serious illness and high care costs. Although Medicare provides broad coverage of basic health care services, it has high cost-sharing requirements, no cap on out-of-pocket spending, and does not cover outpatient prescription drugs, one of the most important benefits for people with HIV (this will change with the passage of the new Medicare prescription drug law). As a result, many Medicare beneficiaries have to rely on supplemental insurance or programs to fill in the gaps. For example, people with HIV/AIDS who cannot afford prescription drugs have had to rely either on Medicaid or the AIDS Drug Assistance Program of the Ryan White CARE Act in order to receive medications. Others may receive prescription drug benefits by purchasing a private “Medigap” policy or by enrolling in a Medicare managed care plan, although these benefits are severely limited and the recent withdrawals, service area reductions, and benefit limitations by Medicare plans in many markets have affected Medicare beneficiary access.77,78
While the recently enacted Medicare legislation adds a drug benefit for the more than 40 million seniors and people with disabilities who have Medicare, a number of questions and concerns have been raised about certain provisions of the legislation, its implementation, and its costs, including particular concerns for dual eligibles:74,79
-
Range of drugs offered. Beneficiaries who participate in Part D will receive their drug coverage through private stand-alone drug-only plans or Medicare Advantage plans (offering comprehensive benefits). Plans can choose to establish formularies, and while they must follow certain rules to do so, they will have broad flexibility to determine formularies. A provision in the law allows plans to limit the number of drugs offered per therapeutic class to two. For people with HIV/AIDS who must rely on multiple medications, many of which are from the same therapeutic class (or could be depending on the definition used by the plan), this could present access and quality barriers. In addition, the range of drugs offered may vary by plan and could differ (be less or more generous) from that which beneficiaries may have had through prior coverage (e.g., what dual beneficiaries had under Medicaid).
-
Potential lapse in prescription drug coverage. The new Medicare law eliminates prescription drug coverage for the dually eligible on January 1, 2006, regardless of whether they have actually enrolled in Part D. States can no longer receive Medicaid matching funds to provide any drugs that could be covered by a Medicare Part D plan, even if eligibles have not yet enrolled in Part D. While the law requires the Secretary of Health and Human Services to develop a plan to automatically sign up dual eligibles for Part D, that plan has not yet been formulated, and it is unclear how dual
-
eligibles will be identified for this purpose. This could mean that some dual eligibles might experience a lapse in prescription drug coverage if they have not yet enrolled in Part D, a situation that could be particularly problematic for people with HIV/AIDS on HAART regimens for which adherence is critical and for those fighting opportunistic infections.
-
Difficulties navigating the enrollment process. It is also likely that the enrollment process for Part D will present challenges, particularly for low-income populations and this too could delay enrollment.
-
Out of pocket costs. Co-payments may also pose barriers for some beneficiaries, particularly low-income beneficiaries, despite the law’s provision for a low-income subsidy program. In some cases, co-payments may be higher under the new law than what dual beneficiaries were required to pay under Medicaid. In addition, beneficiaries will have to pay 100% of the costs of any drug not covered by their plan.
-
Denial of prescription drugs if co-payment cannot be met. Under the new law, beneficiaries can be denied a prescription if they cannot meet the co-payment. This kind of restriction is barred under current Medicaid law.
Ultimately, how the new law will play out and what effect it will have on people with HIV/AIDS and the other programs that serve them (e.g., will it lead to increased demand for ADAP? increased costs? reduced access to prescription drugs?) remains unclear.
Ryan White CARE Act: A Payer of Last Resort for People with HIV/AIDS
First enacted in 1990 and reauthorized in both 1996 and 2000, the Ryan White CARE Act provides funding to cities, states, and other public and private nonprofit entities to develop, coordinate, and operate systems for the delivery of health and support services to medically underserved individuals and families affected by HIV disease. The Ryan White CARE Act is administered by the Health Resources and Services Administration (HRSA) of the Department of Health and Human Services. The CARE Act functions as the payer of last resort—that is, providing care to individuals who are uninsured or underinsured and cannot cover the costs of care on their own, and because no other source of payment for services, public or private, is available to them.80
The CARE Act was first designed to fill the gaps in financing care for people with HIV/AIDS and to relieve cities that were bearing a disproportionate burden of the cost of care. It has since grown into a major program that has helped create an AIDS care infrastructure across the country. In FY 2003, federal funding for Ryan White was approximately $2 billion, about three times its funding level in FY 1995 ($657 million), largely
reflecting increases in funding for medications through the AIDS Drug Assistance Program.23,24,52 The Ryan White program represents the third largest source of federal funding for HIV care in the United States.
Data on state-only spending for Ryan White programs are generally not available with the exception of state contributions to ADAP programs, which states report totaled $160 million in FY 2002, and state matching contributions to Title II HIV Care Grants, which are estimated to total approximately $400 million in FY 2002.49,81
HRSA’s HIV/AIDS Bureau estimates that more than 500,000 people receive Ryan White-funded services each year, but it is impossible to obtain an unduplicated count of users, many of whom receive services from multiple parts of the CARE Act (unique client-level data are not reported for most parts of the CARE Act).80
In recognition of the varying nature of the HIV/AIDS epidemic across the country, Ryan White grantees, including states and cities, are given broad discretion in designing local programs. As a result, there is significant variation in state funding, eligibility, services, and other aspects of Ryan White programs across the country. For example, the number of drugs covered by state AIDS Drug Assistance Programs varies from a low of 18 to a high of 463. Another reason for variation across states is that Ryan White dollars are sometimes inadequate to fill the gaps in states with less generous Medicaid or other programs.66
Eligibility
CARE Act services are available to uninsured or underinsured individuals and families living with HIV/AIDS, and eligibility for services is determined by states and municipalities.
Benefits
The CARE Act primarily funds outpatient care and related support services and does not pay for hospitalizations and long-term institutional care. Services include outpatient medical and dental care, prescription drugs (through the ADAPs), case management, home health and hospice care, insurance continuation, and housing and transportation services. The CARE Act is comprised of several titles and components, including82
-
Title I ($619 million in FY 2002) provides emergency assistance to eligible metropolitan areas (EMAs) most severely affected by the HIV/AIDS epidemic. Federal funding is awarded on a formula and supplemental basis to EMAs. Title I funds may be used to provide a wide range of services including outpatient medical and dental care and support services such as
-
case management. Title I grantees must establish HIV Health Services Planning Councils to set service priorities for the allocation of funds. In FY 2001, there were 51 EMAs in 28 states/territories.
-
Title II ($977 million in FY 2002, including ADAP funds) grants are awarded on a formula basis to states, the District of Columbia, Puerto Rico, and eligible U.S. territories and associated jurisdictions to provide health care and support services for people living with HIV disease, including home- and community-based services, continuation of health insurance coverage, prescription drugs (states receive earmarked funds to support ADAP), and direct health and support services. Some states are required to provide matching funds, depending on their AIDS case burden. In FY 2002, these matching funds are estimated to total close to $400 million.81 As part of the year 2000 reauthorization, supplemental funds are also available through Title II for “emerging communities,” urban areas within states that are not eligible for Title I funds but have a certain level of reported AIDS cases.
-
AIDS Drug Assistance Programs ($639 million in FY 2002, included in Title II funding above). Title II funds also support ADAPs, which provide prescription medications to individuals with HIV disease who have limited or no coverage for medications through other insurance mechanisms. ADAPs began serving clients in 1987, when Congress first appropriated funds to help states purchase AZT, the only approved antitretroviral at that time. In 1990, Congress incorporated ADAP into Title II of the Ryan White CARE Act and, since 1995, Congress has specifically earmarked funding for ADAP, and states are permitted to spend some of their general Title II funds to support these programs. There are 56 ADAPs in all 50 states, the District of Columbia, Puerto Rico, Guam, the U.S. Virgin Islands, the Northern Mariana Islands, and the Marshall Islands. Each state administers its own ADAP program including establishing financial and clinical eligibility criteria and ADAP formularies.
-
Title III ($194 million in FY 2002) supports early intervention services (EIS) for individuals who have been diagnosed with HIV disease. Currently, there are 310 Title III EIS-funded programs in 50 states/territories.
-
Title IV ($71 million in FY 2002) provides community-based, and family centered services to children, youth, and women living with HIV and their families. Services include primary and specialty medical care, psychosocial services, and outreach and prevention services.
-
Dental Assistance ($13 million in FY 2002). The dental reimbursement program assists accredited dental schools, post-doctoral dental programs, and dental hygiene education programs by reimbursing them for nonreimbursed costs incurred in the provision of oral health care to patients with HIV infection.
-
AIDS Education and Training Centers (AETCs) ($35 million in FY 2002) support a network of 14 regional centers (and over 70 associated sites) that conduct targeted, multidisciplinary education and training programs for health care providers of clinical care for persons with HIV/AIDS.
-
Special Projects of National Significance (SPNS) (funded through set-aside from Titles I–IV not to exceed $25 million annually; as of FY 2003, SPNS is being funded through DHHS evaluation set-asides) are funded to establish innovative demonstration projects that respond to the challenge of HIV/AIDS service provision to underserved and vulnerable populations.
Challenges
People with HIV also face challenges in accessing CARE services. As the number of people living with HIV/AIDS continues to grow and the cost of care increases, demand for CARE Act services is also increasing. Because the CARE Act is a discretionary grant program that depends on annual appropriations by Congress (and often by states and municipalities), CARE Act dollars do not necessarily match the need for services and some grantees have been unable to serve all those in need. For example, several state ADAP programs have had to place clients on waiting lists to access prescription drugs, or limit such access in other ways (16 as of September 2003)83 and, as mentioned above, ADAP formularies vary significantly across the country—while almost all ADAPs cover all FDA-approved antiretrovirals, only 15 states cover the full set of drugs highly recommended for the prevention and treatment of opportunistic infections (OIs); 39 states cover 10 or more of these drugs.49,84
In addition, CARE Act programs and services vary across the country, due to local flexibility in designing programs, different levels of funding, and the CARE Act’s role as gap filler. Much of the federal funding for the CARE Act is allocated by formula, based largely on local AIDS case burden. Yet health care system capacity and the availability of other programs vary across jurisdictions and more CARE dollars must be used to fill the gaps in jurisdictions with less generous access to other programs.66 In addition, because the current allocation formula relies on AIDS cases, not HIV infection, allocations may not reflect recent trends in the epidemic and the full burden of affected individuals in all jurisdictions. The 2000 reauthorization of the CARE Act calls for the incorporation of reported HIV cases into the Title I and II formulas as early as FY 2005, if accurate and reliable data exist (a recently released Institute of Medicine report found, however, that HIV case reporting is not yet reliable enough for this purpose. See: Institute of Medicine, Measuring What Matters: Allocation, Planning, and Quality Assessment for the Ryan White CARE Act, 2004).
Private Health Insurance
Almost one-third (31%) of people with HIV/AIDS who are in care are estimated to be covered by private health insurance,32 as are a significant proportion of those newly diagnosed with HIV.47 As new treatments allow people with HIV to more fully participate in the workforce, private insurance will likely continue to play an important role in HIV/AIDS care.
Like most Americans, the vast majority of privately insured individuals with HIV obtain their insurance through their employers. Those who are insured in the group market tend to have the most comprehensive coverage and have much less difficulty obtaining and keeping that coverage. People with HIV/AIDS who must purchase coverage in the individual insurance market often face barriers to obtaining a policy. A recent study of the accessibility of the individual insurance market for those in less than perfect health found that people with HIV are generally considered “uninsurable” and are routinely rejected when they apply for coverage (some states require certain carriers in the individual market to offer coverage to all applicants).85 Those who have limits in their private coverage may need to rely on safety net programs, such as the Ryan White CARE Act, to fill the gaps. Some states have implemented insurance reforms to enhance access to the individual insurance market, although these reforms vary and have different implications for people with HIV.85,86 If recent trends indicating reductions in employer-sponsored health insurance coverage continue,87 people with HIV/AIDS may increasingly need to rely on other safety net programs for care.
While the insurance market is largely regulated at the state level, the Health Insurance Portability and Accountability Act of 1996 (P.L. 104-191), also known as HIPAA, established basic national standards for insurance regulation in the small-group (firms with 2 to 50 workers) market and, to a lesser extent, in the individual market. Among the protections included in HIPAA were88,89
-
Portability. Exclusions of pre-existing medical conditions are limited to a maximum of 12 months. In other words, if a person with HIV/AIDS changes jobs and insurers and has already experienced a 12-month coverage exclusion of that condition, the new insurer cannot exclude them again. Workers with previous coverage receive credit for each month of coverage to reduce the exclusion period. The portability protection only applies to group coverage and only if the period of time between coverage was less than 63 days.
-
Non-discrimination. Insurers in the group market are prohibited from conditioning a person’s eligibility for group coverage on their health status and worker contributions cannot be varied based on health status.
-
However, HIPAA does not prohibit an insurer from charging a higher premium to an employer based on the health status of workers. Nondiscrimination protections do not apply to individual policies.
-
Guaranteed issue. Insurers must offer all of their small-group policies to any small employer that wants to purchase coverage for their workers. While HIPAA does not extend guaranteed issuance to the nongroup market, it does require that each state have in place a policy that permits individuals losing coverage in the group market to get access to a non-group policy, either through an insurer or through another mechanism such as the state’s high-risk pool. Although HIPAA does not limit the premiums that can be charged, many states do.
-
Guaranteed renewal. Insurers must allow all policies—group and individual—to be renewed.
Those individuals who lose private group coverage in firms with more than 20 employees can continue that coverage for a specified period of time under the terms of the Consolidated Omnibus Budget Reconciliation Act of 1986 (P.L. 99-272), also known as COBRA. For those who are disabled, coverage can be extended for up to 29 months, designed to provide coverage until Medicare eligibility begins.86,90 Employers are required to notify workers who are eligible for COBRA coverage and workers have 60 days to exercise their benefits. People who exercise their COBRA benefits must pay a monthly premium. A number of states apply COBRA-like laws to group plans that are exempt from COBRA.
Under a provision added to the Ryan White CARE Act in 1996, states can use Ryan White funds to help people with HIV/AIDS who are eligible for COBRA pay their premiums or buy private insurance. In addition, since 1993, Medicaid has given states the option to receive federal matching funds for the costs of COBRA premiums for individuals with incomes at or below 100 percent of the federal poverty level and countable resources under $4,000.
Challenges
Even with the protections offered by HIPAA, people with HIV face barriers to accessing private insurance, particularly in the individual insurance market. First, HIPAA does not include any limits on insurance rates and people can effectively be priced out of the market. Some states—most notably New York, New Jersey, Maine, and Vermont—have adopted community rating; others have utilized “rating bands” to limit the size of premium increases. Some states have also chosen to purchase new policies for people with HIV, using Ryan White CARE Act funds or broader programs that target low-income or uninsured people. Second, HIPAA does not
improve access to the individual market for those without prior group coverage and, as noted above, HIV is generally considered an “uninsurable” condition by most carriers in the individual market. In addition, private insurance plans often have annual or lifetime caps on benefits, copayments and deductibles, and limits on services that may limit access in the private market. Finally, the insurance market and insurance reforms vary significantly by state, presenting different options and limitations across the country.85,86
Department of Veterans Affairs
Acting as both insurer and provider of care, the VA is the largest single provider of comprehensive HIV/AIDS care in the United States. In FY 2001, the VA provided care to approximately 18,500 veterans with HIV/AIDS; since 1982, the agency has served a total of 50,000 persons with HIV/AIDS.91,92 In FY 2002, the VA spent $348 million on HIV/AIDS care, representing 4% of federal spending on HIV care.23,24 VA HIV/AIDS care is financed through annual appropriations out of general tax revenues. Any veteran of the armed services is eligible to receive HIV/AIDS care through the Veterans Health Administration. Under VA guidelines, private insurers must pay for care where appropriate, and veterans contribute based on a system of service-based ranking and means-testing screens. Disabilities, including HIV-related disability, must be service-related or a veteran must be low-income to receive subsidized care; otherwise, veterans must pay a share of costs.
HIV/AIDS care is provided at the VA’s 163 hospitals, more than 850 primary care clinics, 137 nursing homes, 43 domiciliary centers, 73 home care programs, and 206 Vietnam Veteran Outreach Centers.91,92,93 The VA has an HIV/AIDS Coordinator at every VA hospital and the VA’s AIDS Service coordinates HIV/AIDS care throughout the VA system. In addition to providing care, the VA provides HIV prevention services to veterans, providing approximately 50,000 HIV tests per year, and conducts clinical research on HIV/AIDS.92 Not all veterans, however, live near a VA facility, which could inhibit access.
Community Health Centers and Other Safety Net Providers
Those who are uninsured and underinsured also rely on an array of other safety net providers for care. These include community and migrant health centers, public hospitals, private “free clinics,” and individual health care providers who offer free care. Services vary across these different types of providers.
Community health centers serve a large number of people living with
HIV, with both CARE Act dollars and community health center grant funding.4 They can also directly bill Medicaid for eligible beneficiaries. In 2000, community health centers provided almost 250,000 HIV-related encounters to more than 48,000 people. In addition, they provided more than 270,000 HIV tests to approximately 231,000 people.94
Most of these safety net programs are funded through discretionary grants, and are dependent upon annual appropriations for funding. As such, funding does not necessarily match the need for or cost of care. In addition, people with HIV/AIDS may not always have access to experienced HIV providers through these mechanisms.
Other Sources of Coverage and Care
While there are several other mechanisms available for coverage and care, they provide access to only limited numbers of people with HIV/AIDS. These include high-risk pools, designed for people with significant health risks who have been denied coverage in the private market85,86,95,96,97 and pharmacy assistance programs offered by states98,99,100 and pharmaceutical manufacturers101 to low-income individuals (with varying other eligibility requirements). Twenty-nine states currently operate high-risk pools95 and 14 states have state pharmacy assistance programs available to non-seniors, either through subsidies or discounts.99,100 Finally, the Department of Defense provides care to a small number of active duty service personnel69 and the federal government, as an employer, provides care to federal employees with HIV/AIDS through the Federal Employee Health Benefits program.24,51
POLICY CHALLENGES
The patchwork of financing for HIV/AIDS care presents barriers to accessing care. As policymakers search for ways to improve access, they face several important challenges, many of which cut across the multiple sources of financing and care, including
Reaching Those Not in Care
A significant proportion (42% to 59%) of people living with HIV/AIDS are not in regular care. While some may not know their HIV status, many face financial and other barriers to access. More research is needed to identify the barriers to care. Outreach is also needed both to help bring people who know their HIV status into care early and to encourage others to get tested and learn their status. This will require better linkages between HIV testing and treatment facilities and services.
Enhancing Care for Those Who Are Uninsured or Publicly Insured, Minority Americans, and Women
Recent data indicate that although quality of HIV care has improved over time, there are still differences in quality and access by insurance status, race/ethnicity, and sex. These findings call for further research to understand better the underlying causes of these differences and identify ways to enhance access to and quality of care for different populations.
Improving Insurance Coverage
Current eligibility rules for Medicaid and Medicare make it difficult for many people with HIV to gain coverage before their health status worsens and they are disabled. Most people with HIV become eligible for Medicaid through SSI, after they are disabled, yet national treatment guidelines call for early access to treatment to prevent or delay disability (this eligibility limitation also present barriers to Medicare access, through SSDI). A few states are attempting to address this through Medicaid 1115 waivers and provisions of the TWWIIA, but most will need to continue to rely on discretionary grant funding, particularly the AIDS Drug Assistance Program and other parts of the CARE Act, to do so. Medicaid and Medicare eligibility may also be jeopardized for those beneficiaries with HIV who have benefited from new treatments and wish to enter or re-enter the workforce. The BBA and TWWIIA each had provisions designed to address some of these concerns, but challenges still remain and few states have exercised these options. The 29-month waiting period for Medicare eligibility also presents a challenge to coverage for people with HIV/AIDS. Finally, the current lack of a prescription drug benefit in the Medicare program and potential limitations of the new Medicare prescription drug law could present new challenges for people with HIV/AIDS.
Reducing Variation in Access Across States
Many of the programs that provide care to people with HIV have significant variation in eligibility, benefits, and other program components across states. This is particularly true for the Ryan White CARE Act and Medicaid, two of the most important sources of financing for HIV care. As a result, people with HIV face highly uneven access to coverage across the country.
Enhancing Coordination Across Programs
There is limited coordination across the multiple funding streams that finance HIV care. Yet these programs greatly impact one another and the
level of access available to people with HIV across the country. More information is needed to understand how these financing systems interact and how they can better work together to increase program efficiency and enhance access to care for people with HIV. A recently proposed “HIV/AIDS Integrated Services Project,” a joint initiative of HRSA, CMS, and CDC, will explore ways to blend federal funding streams and better coordinate care for people with HIV/AIDS on a demonstration basis; however, when exploring options to blend federal funding streams, it is important to maintain the level of individual entitlement to coverage for basic health services that each Medicaid or Medicare beneficiary now has.
Addressing the Cost of Prescription Drugs
Prescription drugs are one of the fastest growing components of health care spending. They also represent a key component of HIV/AIDS care. As such, rising prescription drug costs will continue to present challenges to people with HIV and the programs that provide for their care, especially Medicaid and the AIDS Drug Assistance Program, which have already seen sharp rises in expenditures for AIDS drugs. As a result, some state Medicaid programs and ADAPs have taken steps to control drug expenditures, which could limit access (e.g, Medicaid prescription drug limits and cost controls, ADAP waiting lists). Analysis indicating that Medicaid, the largest public purchaser of HIV/AIDS drugs, is paying higher prices for these drugs than other government purchasers also presents challenges for policymakers seeking to balance cost containment and access. It is also unclear how incentives in the new Medicare prescription drug law will impact drug prices over the long-term, particularly for breakthrough drugs for which there is little competition, and if the new law will affect the price paid for drugs by Medicaid (as it stands to lose purchasing power after prescription drug benefits for dual eligibles are transferred to Medicare in 2006).
Financing Prevention Services
Current care financing mechanisms do not offer clear incentives to provide prevention services in the clinical setting. Yet an estimated 40,000 people still become infected with HIV each year in the United States, indicating the importance of continued prevention efforts targeting those at risk. In addition, people already infected with HIV need access to prevention services to help prevent the further spread of HIV, which is the focus of the CDC’s Serostatus Approach to Fighting the Epidemic (SAFE) and the CDC’s new prevention initiative, Advancing HIV Prevention. A recent study showing that a significant proportion of people with HIV are already covered by Medicaid or other public payers at time of diagnosis underscores
the important role public payers can play in the delivery of prevention services within the care setting.47
These policy issues are often heightened in the context of the HIV/AIDS epidemic due to shifting demographics and rapidly changing clinical standards of care. People with HIV/AIDS are increasingly likely to be members of already disadvantaged groups who are more likely to rely on the public sector for financing their care and face historical barriers to access. African Americans and Latinos, for example, represent the majority of new HIV infections and women now comprise almost a third (30%) of new HIV infections in the United States; most women newly infected are minority women.37
In addition, HIV care has grown increasingly complex, requiring rapid dissemination of new standards to diverse groups of providers. Moreover, to support receipt of and adherence to complex treatment and help them navigate the financing and health care delivery systems, people with HIV/AIDS need access to a comprehensive continuum of care and experienced providers. Yet some needed services, such as case management or prevention, are not always financed through the same mechanism as medical care or may not be financed at all. Together, these aspects of the epidemic mean that policymakers will be faced with continued challenges to financing HIV-related care in the future, particularly as the number of people with HIV/AIDS continues to grow, as do health care costs. These challenges may be exacerbated during tough economic times.
CONCLUSION
Despite the existence of multiple sources of financing, many people with HIV/AIDS are not in regular care and a significant proportion does not know they are infected. Even among those who are in care, numerous barriers may impede their access to needed treatments. The high cost of care poses challenges for individuals and caregivers, as well as state and federal governments. Eligibility rules create barriers to coverage and care. Existing programs vary significantly across the states and are often poorly coordinated. As the HIV epidemic continues to shift towards those who have always had a more difficult task gaining access to and paying for care, these policy challenges are certain to grow.
ENDNOTES
|
4. |
Levi, J. and Kates, J., “HIV: Challenging the Health Care Delivery System,” American Journal of Public Health, Vol. 90, No. 7, 2000. |
|
5. |
Kates, J., Sorian, R., Crowley, C., Summers, T., “Critical Policy Challenges in the Third Decade of the HIV/AIDS Epidemic,” American Journal of Public Health, Vol. 92, No.7, July 2002. |
|
6. |
Department of Health and Human Services/Kaiser Family Foundation, Guidelines for the Use of Antiretroviral Agents in HIV-infected Adults and Adolescents, February 2002, http://www.hivatis.org. |
|
7. |
Fleming, P., et al., HIV Prevalence in the United States, 2000, 9th Conference on Retroviruses and Opportunistic Infections, Abstract #11, Oral Abstract Session 5, February 2002. |
|
8. |
It is estimated that between 19% and 33% of those infected with HIV in the United States do not know their status. See Fleming, P. et al., note #7. |
|
9. |
Scitovsky, A. and Rice, D., “Estimates of the Direct and Indirect Costs of Acquired Immunodeficiency Syndrome in the United States, 1985, 1986, 1991,” Public Health Reports, Vol. 102, No. 1, 1987. |
|
10. |
Sisk, J., “The Costs of AIDS: A Review of The Estimates,” Health Affairs, Summer 1987. |
|
11. |
Green, J. and Arno, P., “The ‘Medicaidization’ of AIDS: Trends in the Financing of HIV-Related Medical Care,” Journal of the American Medical Association, Vol. 264, No. 10, 1990. |
|
12. |
Arno, P. and Feiden, K., Against the Odds: The Story of AIDS Drug Development, Politics, and Profits, Harper Collins, New York, 1992. |
|
13. |
Centers for Disease Control and Prevention, HIV/AIDS Surveillance Report, Vol. 13, No. 2, 2002. |
|
14. |
Centers for Disease Control and Prevention, “Update: AIDS—United States, 2000,” MMWR, Vol. 51, No. 27, July 2002. |
|
15. |
This is based on average wholesale price (AWP). The price Medicaid pays for prescription drugs includes a rebate off the average manufacturers price (AMP), which itself is less than the AWP. The rebate received is defined as the greater of 15.1% of AMP or AMP minus the Best Price (BP) for brand name drugs. The rebate for generic drugs is 11% of AMP. |
|
16. |
Bartlett, J., Medical Management of HIV Infection, 2001-2002 Edition, 2001. |
|
17. |
Kahn, J., Haile, B., Kates, J., Chang, S., “Health and Federal Budgetary Effects of Increasing Access to Antiretroviral Medications for HIV by Expanding Medicaid,” American Journal of Public Health, Vol. 91, No. 9, September 2001. |
|
18. |
This represents an average estimate across all payers and all HIV disease stages, based on several studies. Personal communication, James G. Kahn, January 2003. |
|
19. |
Bozzette, S., et al., “The Care of HIV Infected Adults in the United States,” New England Journal of Medicine, Vol. 339. No. 26, December 1998. |
|
20. |
Bozzette, S., et al., “Expenditures for the Care of HIV-Infected Patients in the Era of Highly Active Antiretroviral Therapy,” New England Journal of Medicine, Vo. 334, No. 11, March 2001. |
|
21. |
University of Alabama (UAB), Press Release: UAB Announces Results of First HIV Patient Care Cost Analysis, July 2002. In the UAB study, the average annual cost of patient care ranged from $14,000 for those at early stage HIV infection to $34,000 for those with advanced-stage disease. |
|
22. |
Karon, J. et al., “HIV in the United States at the Turn of the Century: An Epidemic in Transition,” American Journal of Public Health, Vol. 91, No. 7, July 2001. |
|
23. |
Kaiser Family Foundation, Federal HIV/AIDS Spending: A Budget Chartbook, Fiscal Year 2002, September 2003. |
|
24. |
Alagiri, P., Summers, T., Kates, J., Trends in U.S. Spending on HIV/AIDS, Kaiser Family Foundation, July 2002. |
|
25. |
National Institute for Health Care Management Foundation, Prescription Drug Expenditures in 2001: Another Year of Escalating Costs, Revised May 2002. |
|
26. |
Kaiser Family Foundation, unpublished data. |
|
27. |
Centers for Medicare & Medicaid Services, Office of the Actuary, National Health Statistics Group, National Health Expenditures, 2002 (www.cms.hhs.gov/statistics/nhe/historical/ (Accessed January 18, 2003). |
|
28. |
GAO, HIV/AIDS Drugs: Funding Implications of New Combination Therapies for Federal and State Programs, GAO/HEHS-99-2, 1998. |
|
29. |
Freedberg, et al., “The Cost Effectiveness of Combination Antiretroviral Therapy For HIV Disease,” New England Journal of Medicine, Vol. 344, No. 11, March 2001. |
|
30. |
Shackman, et. al., “Cost-Effectiveness of Earlier Initiation of Antiretroviral Therapy for Uninsured HIV-Infected Adults,” American Journal of Public Health, Vol. 91, No. 9, September 2001. |
|
31. |
Data are for those ages 18 and older. |
|
32. |
Fleishman, J., Personal communication, Analysis of HCSUS Data, January 2002. |
|
33. |
Nakashima AK. “Who Will Pay for HIV Treatment? Health Insurance Status of HIV-Infected Persons.” In: Proceedings of the 1997 Meeting of the Infectious Diseases Society of America; September 13-16, 1997; San Francisco, CA. Abstract 293. |
|
34. |
Kaiser Family Foundation, State Health Facts Online, Health Coverage & Uninsured, Distribution of Adults, 19-64 by Insurance Status, 2000-2001, www.statehealthfacts.org (Accessed February 7, 2004). |
|
35. |
A small number may have other forms of coverage, such as private coverage. |
|
36. |
HIVnet, HIV Resource Utilization Data Coordinating Center (DCC) project, July 2002. Agency for Healthcare Research and Quality, Rockville, MD. www.ahrq.gov/data/HIVnet.htm (Accessed January 18, 2003). Data are for those ages 18 and older. |
|
37. |
Centers for Disease Control and Prevention, HIV/AIDS Update: A Glance at the Epidemic, 2002. |
|
38. |
Shapiro, et al., “Variations in the Care of HIV-Infected Adults in the United States,” Journal of the American Medical Association, Vol. 281, No. 24, June 1999. |
|
39. |
Sambamoorthi, U., et. al., “Use of Protease Inhibitors and Non-Nucleoside Reverse Transcriptase Inhibitors Among Medicaid Beneficiaries with AIDS,” American Journal of Public Health, Vol. 91, No. 9, September 2001. |
|
40. |
Health Resources and Services Administration, Press Release: HRSA Welcomes HIV/AIDS Health Care Providers to Biennial Conference; Studies Find that While Patients in Federal Programs are Mostly Minorities, Those Groups Still Face Barriers to Accessing HIV/AIDS Care, August 2002. |
|
41. |
Keruly, J., Conviser, R, and Moore, R., “Association of Medical Insurance and Other Factors With Receipt of Antiretroviral Therapy,” American Journal of Public Health, Vol. 92, No. 5, May 2002. |
|
42. |
Cunningham, W. et al., “Prevalence and Predictors of Highly Active Antiretroviral Therapy Use in Patients with HIV Infection in the United States,” Journal of Acquired Immune Deficiency Syndromes, Vol. 25, No. 2, October 2000. |
|
43. |
Campsmith, M., Burgess, D., “Race/Ethnicity and Gender Differences in Late HIV Testing—Results from a Supplemental HIV/AIDS Surveillance Project,” HIV Prevention Conference, August 2001. |
|
44. |
Neal, J., Fleming, P., “Frequency and Predictors of Late HIV Diagnosis in the United States, 1994 through 1999,” 9th Conference on Retroviruses and Opportunistic Infections, Abstract #474M, February 2002. |
|
45. |
Cunningham, W., et al., “Delayed Medical Care After Diagnosis in a U.S. National Probability Sample of Persons Infected With Human Immunodeficiency Virus,” Archives of Internal Medicine, Vol. 160, September 2000. |
|
46. |
It is important to note that the HCSUS analysis of variation in care by insurance status included analysis of those covered by Medicaid only. Those who were dual Medicaid/Medicare beneficiaries were counted in the Medicare category. See, Shapiro, et al., 1999 note 38. |
|
47. |
Kates, J., Levi, J., Neal, J., Gallagher, K., “Learning More About the HIV-Infected Population Not IN Care in the United States: Using Public Health Surveillance Data to Inform Current Policy Challenges in Enhancing Access,” Poster TuPeG 5690, XIV International AIDS Conference, Barcelona, Spain, July 2002. Data are for those ages 13 and older. |
|
48. |
It is important to note that the insurance profile of those for whom such data are not available may differ from the insurance profile of those for whom data are available. |
|
49. |
National Alliance of State and Territorial AIDS Directors/Kaiser Family Foundation/AIDS Treatment Data Network, National ADAP Monitoring Project, Annual Report, April 2003. |
|
50. |
Centers for Medicare &Medicaid Services, Office of the Actuary, personal communication, February 2003. |
|
51. |
Department of Health and Human Services, Office of Budget, Total Federal Government Spending (by Function), February 2004. |
|
52. |
U.S. Congress, Consolidated Omnibus Bill & Conference Report, February 2003. |
|
53. |
Centers for Medicare & Medicaid Services, Fact Sheet: Medicaid and Acquired Immunodeficiency Syndrome (AIDS) and Human Immunodeficiency Virus (HIV) Infection, January 2002. |
|
54. |
Kaiser Family Foundation, Medicaid and HIV/AIDS Policy: A Basic Primer, 1999. |
|
55. |
Kaiser Commission on Medicaid and the Uninsured, Medicaid: A Primer, March 2001. |
|
56. |
Kaiser Commission on Medicaid and the Uninsured, Fact Sheet: Medicaid’s Role for the Disabled Population Under Age 65, April 2001. |
|
57. |
Analysis prepared for the Kaiser Commission on Medicaid and the Uninsured by Jeff Crowley, Georgetown University, 2003. |
|
58. |
National Association of State Medicaid Directors, Aged, Blind, and Disabled Medicaid Eligibility Survey, www.nasmd.org/eligibility/optional.asp (Accessed June 2003). |
|
59. |
FDA-approved prescription drugs. |
|
60. |
Centers for Medicare & Medicaid Services, Personal communication, August 2002. |
|
61. |
Kaiser Commission on Medicaid and the Uninsured, Medicaid Outpatient Prescription Drug Benefits: Findings from a National Survey, 2003, December 2003. |
|
62. |
Kaiser Family Foundation, State Health Facts Online, HIV/AIDS, Status of State Medicaid Expansion Efforts for People with HIV, www.statehealthfacts.org (Accessed January 18, 2003). |
|
63. |
The Breast and Cervical Cancer Prevention and Treatment Act of 2000 (P.L. 106-354). |
|
64. |
Kaiser Commission on Medicaid and the Uninsured, Medicaid Related Provisions in the Ticket To Work and Work Incentives Improvement Act of 1999, 2000. |
|
65. |
Kaiser Commission on Medicaid and the Uninsured, The Medicaid Resource Book, July 2002. |
|
66. |
Levi, J., Hidalgo, J., Wyatt, S., “The Impact of State-by-State Variability in Entitlement Programs on the Ryan White Care Act and Access to Services for Underserved Populations,” Prepared for the Health Resources and Services Administration, March 2000. |
|
67. |
Rowland, D. and Tallon, J., Medicaid: Lessons From a Decade, 2002. |
|
68. |
National Association of People with AIDS, Building Strong Medicaid Managed Care Programs: A Guide to Help Consumer Advocates Participate in Strengthening HIV/AIDS Provisions in Managed Care Contracts, 2000. |
|
69. |
Department of Health and Human Services, Office of Inspector General, Cost Containment of Medicaid HIV/AIDS Drug Expenditures, OEI-05-99-00611, July 2001. |
|
70. |
Kaiser Commission on Medicaid and the Uninsured, State Budgets Under Stress: How are States Planning to Reduce The Growth in Medicaid Costs?, July 2002. |
|
71. |
Kaiser Commission on Medicaid and the Uninsured, Medicaid Spending Growth: A 50 State Update for FY 2003, December 2002. |
|
72. |
Centers for Medicare & Medicaid Services, Office of the Actuary, Personal communication, September 2002. |
|
73. |
Schietinger, H. and Schecter, C., Medical Coverage for Medicare Beneficiaries with HIV/AIDS: Issues and Implications, Academy for Educational Development, 1998. |
|
74. |
Kaiser Commission on Medicaid and the Uninsured, Fact Sheet: Dual Eligibles: Medicaid’s Role for Low-Income Medicare Beneficiaries, January 2004. |
|
75. |
Kaiser Family Foundation, Fact Sheet: Medicare at a Glance, April 2003. |
|
76. |
Kaiser Family Foundation, Prescription Drug Coverage for Medicare Beneficiaries: An Overview of the Medicare Prescription Drug, Improvement, and Modernization Act of 2003 (Public Law 108-173). Prepared by Health Policy Alternatives, Inc., January 2004. |
|
77. |
Kaiser Family Foundation, Medicare+Choice Withdrawals: Understanding Key Factors, June 2002. |
|
78. |
Kaiser Family Foundation, Medicare+Choice Fact Sheet, April 2003. |
|
79. |
Kaiser Commission on Medicaid and the Uninsured, Implications of the New Medicare Law for Dual Eligibles: 10 Key Questions and Answers, December 2003. |
|
80. |
Health Resources and Services Administration, HIV/AIDS Bureau website, Care Act Overview, http://hab.hrsa.gov/programs/factsheets/programfact.htm (Accessed January 18, 2003). |
|
81. |
National Alliance of State and Territorial AIDS Directors, FY 2002 Ryan White CARE ACT Title II HIV Care Grants (Proposed), February 2002. |
|
82. |
Health Resources and Services Administration, HIV/AIDS Bureau website, http://hab.hrsa.gov (Accessed January 18, 2003). |
|
83. |
National Alliance of State and Territorial AIDS Directors, ADAP Watch, September 2003. |
|
84. |
National Alliance of State and Territorial AIDS Directors/Kaiser Family Foundation/AIDS Treatment Data Network, Issue Brief: Trends in Opportunistic Infection Drug Coverage and Spending, February 2003. |
|
85. |
Kaiser Family Foundation, How Accessible is Individual Health Insurance for Consumers in Less-Than-Perfect Health?, June 2001. |
|
86. |
Levi, J,. et al., Can Access to the Private Individual Insurance Market be Increased for People Living With HIV?, George Washington University Medical Center, 1999. |
|
87. |
Kaiser Family Foundation and HRET, 2002 Employer Health Benefits Survey, September 2002. |
|
88. |
Pollitz, K. et al., “Early Experience with ‘New Federalism’ in Health Insurance Regulation,” Health Affairs, July/August 2000. |
|
89. |
Kaiser Family Foundation, How Private Insurance Works: A Primer, April 2002. |
|
90. |
U.S. Department of Labor, Pension and Welfare Benefits Administration, Health Benefits Under the Consolidated Omnibus Budget Reconciliation Act, COBRA, www.dol.gov/pwba/pdf/cobra99.pdf. |
|
91. |
Department of Veterans Affairs, Veterans Health Administration, The VA HIV Prevention Handbook: A Guide for Clinicians, January 2002. |
|
92. |
Veterans Administration, Public Health Strategic Health Care Group, HIV/AIDS Program Fact Sheet, 2002. |
|
93. |
Veterans Health Administration, Overview, Department of Veterans Affairs, August 2002. |
|
94. |
Health Resources and Services Administration, Bureau of Primary Health Care, 2000 Uniform Data System, data extracted in August 2002. |
|
95. |
Kaiser Family Foundation, State Health Facts Online, Managed Care and Health Insurance, State Sponsored High Risk Insurance Pools, 2001, www.statehealthfacts.org (Accessed January 18, 2003). |
|
96. |
Communicating for Agriculture & the Self Employed, Comprehensive Health Insurance for High-Risk Individuals: A State-by-State Analysis, Fifteenth Edition, 2001/2002, 2001. |
|
97. |
Achman, L., Chollet, D., Insuring the Uninsurable: An Overview of State High-Risk Health Insurance Pools, The Commonwealth Fund, August 2001. |
|
98. |
GAO, State Pharmacy Programs: Assistance Designed to Target Coverage and Stretch Budgets, GAO/HEHS-00-162, 2000. |
|
99. |
Kaiser Family Foundation, State Health Facts Online, Medicare, State Pharmaceutical Assistance Programs, 2001, www.statehealthfacts.org (Accessed January 18, 2003). |
|
100. |
National Conference of State Legislatures, State Pharmaceutical Assistance Programs, January 2003, www.ncsl.org/programs/health/drugaid.htm (Accessed January 18, 2003). |
|
101. |
Pharmaceutical Research and Manufacturers of America, Directory of Prescription Drug Patient Assistance Programs, 2002. |













































