3
Current Financing and Delivery of HIV Care
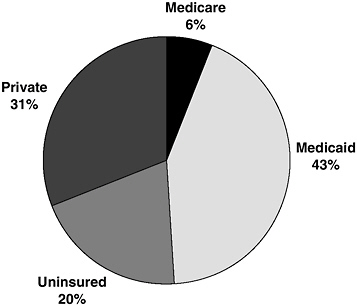
People living with HIV/AIDS rely on a variety of private and public payment mechanisms to obtain care. Thirty-one percent of people living with HIV/AIDS are covered by private insurance; the remaining individuals are covered through federal programs such as Medicaid and Medicare or are uninsured (Kates, 2004) (see Figure 3-1).1 Programs such as the Ryan White Comprehensive AIDS Resources Emergency (CARE) Act program, community and migrant health centers, private free clinics, and public hospitals provide a health care safety net for many individuals with HIV/AIDS who are uninsured and/or underinsured.
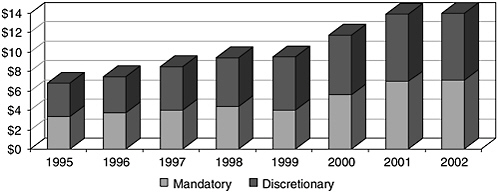
The federal programs that provide care to people living with HIV/AIDS operate through two financing mechanisms: mandatory spending programs, in the form of entitlements to the individual and to the states, and discretionary annual funding for specific services. These financing mechanisms have significant implications for individuals and governments in terms of stability of financing, access to care, durability of services, and costs. In 2002, 72 percent of the $8.7 billion spent on health care and related social support services for people with HIV/AIDS was spent under mandatory or entitlement programs. In fiscal year 2002, a total of $14.7 billion was spent by the federal government on HIV/AIDS medical care, research, prevention, and other activities (see Figure 3-2).
|
1 |
Portions of this chapter draw heavily from a paper commissioned by the Institute of Medicine Committee on Public Financing and Delivery of HIV/AIDS Care. The paper was written by Jennifer Kates, Kaiser Family Foundation, and is included in its entirety in Appendix D. |
FEDERAL FINANCING OF HIV CARE
Medicaid
Medicaid, Title XIX of the Social Security Act, is the largest source of public financing for HIV/AIDS care in the United States. Created in 1965, Medicaid is a jointly funded, jointly administered federal–state health insurance program for low-income people who meet one or more of several categorical eligibility requirements, including disability. The program is administered through the Centers for Medicare & Medicaid Services (CMS). Through Medicaid, the federal government provides matching funds to states that meet certain minimum federal standards in operating their Medicaid programs. States have broad flexibility in designing their Medicaid programs, and consequently there is significant variation in eligibility, benefits, provider payments, and other aspects of the program at the state level (Westmoreland, 1999; Kaiser Commission on Medicaid and the Uninsured, 2001). State Medicaid policies vary considerably even among similar-sized and or adjacent states. Thus, a person who is eligible for Medicaid in one state might not be eligible in another state; and the services provided by one state may differ from those of another state.2
Because many people with HIV/AIDS are low income—or become low income—and disabled, Medicaid is an important source of coverage. In FY 2002, Medicaid spending on AIDS care totaled $7.7 billion, including $4.2 billion in federal dollars and $3.5 billion in state funds (see Figure 3-3). Overall, the program is estimated to cover approximately 44 percent of people with HIV and 55 percent of those living with AIDS (CMS, 2002). Medicaid is also estimated to cover the health care costs of up to 90 percent of children with AIDS (CMS, 2002).3 Among those recently diagnosed with HIV (for whom coverage data were available), more than one-fifth (22 percent) were already covered by Medicaid at the time of diagnosis (Kates et al., 2002).
Eligibility
To be eligible for Medicaid, a person must meet the categorical and financial eligibility criteria in his or her state’s Medicaid program. Most
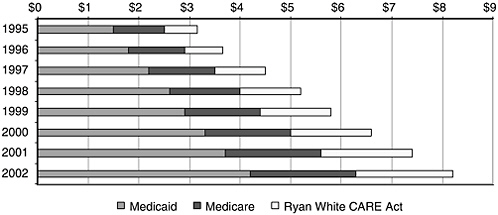
FIGURE 3-3 Federal spending on care: Ryan White CARE Act, Medicare, and Medicaid, fiscal years 1995–2002 (in billions).
adults with HIV/AIDS who qualify for Medicaid do so because they meet the disability and income and assets criteria of the federal Supplemental Security Income (SSI) program for persons who are aged, blind, or disabled. For purposes of SSI eligibility, a person is disabled if he or she is unable to engage in any gainful activity due to a medically determined physical or mental impairment expected to result in death or last for a continuous period of at least 12 months (Westmoreland, 1999).4 Some states, known as 209(b) states,5 may apply more restrictive eligibility rules under SSI.
People with HIV may also qualify for Medicaid through a state’s medically needy program that enables those who meet categorical eligibility requirements, such as disability, to spend-down their incomes to meet their state’s income eligibility threshold, which varies among states. Individuals must also meet a state’s resource test.
Benefits
Federal rules require states participating in Medicaid to cover a set of mandatory services to eligible people in order to receive federal matching payments (Box 3-1). States may also choose to provide optional services
|
BOX 3-1 Mandatory Services States Must Provide to Qualify for Federal Matching Payments Under Medicaid and Selected Optional Services That May Be Provided
|
||||||
and receive matching payments. Food and Drug Administration- (FDA) approved prescription drugs are an optional benefit that all states have chosen to provide. Medicaid coverage of prescription drugs includes all FDA-approved highly active antiretroviral therapy (HAART) drugs, but coverage of these drugs is at state option and subject to amount, duration, and scope limits (e.g., limit on the number of prescriptions), nominal copayments for adults, and prior authorization controls. Other optional services that can be important for people with HIV/AIDS include case management, prevention services, tuberculosis-related services, and hospice services.
States may also seek waivers to cover certain services that would not otherwise qualify for federal matching funds, and a number have done so (Kates, 2004).
Medicare: Coverage for Disabled and Elderly Persons with HIV/AIDS
Medicare (Title XVIII of the Social Security Act) is the nation’s federal health insurance program for the elderly and disabled. It was established in
1965 and is also administered by CMS. Medicare is an important source of coverage for people with HIV/AIDS who are disabled, have sufficient work history to qualify for disability insurance, and live long enough to qualify for Medicare. Medicare covers an estimated 6 percent of people with HIV/AIDS who are in care (CMS, 2002; Kates, 2004; Bozzette et al., 1998).
As people with HIV/AIDS live longer, the number of people with HIV/AIDS on Medicare is expected to grow, and Medicare spending is also expected to increase. Today, Medicare is the second largest source of federal financing of HIV/AIDS care, accounting for $2.1 billion in FY 2002. Medicare spending on HIV/AIDS has roughly doubled since FY 1995, when it was $1 billion (IOM, 2001; CMS, 2002; Kates, 2004). Some individuals with Medicare coverage also qualify for Medicaid because they have low income levels; they are considered to be dual-eligible.6 For these individuals, Medicaid provides varying levels of coverage, including payment of premiums, some cost sharing, coverage of services during the waiting period (for those under 65 years), and coverage of prescription drugs.
Eligibility
Most Americans ages 65 and older are entitled to Medicare as soon as they are eligible for Social Security payments. People under age 65 who receive Social Security Disability Insurance (SSDI) benefits and individuals with end-stage renal disease may also qualify for Medicare. People with HIV/AIDS who meet SSDI eligibility criteria are eligible for Medicare benefits. The Social Security Administration defines disabled to mean that an individual 18 years or older is unable to engage in any substantial gainful activity due to any medically determinable physical or mental impairment(s) that can be expected to result in death or that has lasted or can be expected to last for a period of not less than 12 months (SSA, 2004). In addition, individuals must have paid Social Security taxes through their workplace for a minimum number of fiscal quarters. Federal law, however, requires a 5-month waiting period after disability determination to receive SSDI benefits and then a 24-month waiting period before an SSDI beneficiary can join Medicare, resulting in a total of 29 months before receipt of health benefits (SSA, 2004; Schietinger and Schecter, 1998).
Benefits
Medicare as it currently exists is composed of three parts (KFF, 2004):
-
Part A covers inpatient hospital services, skilled nursing facilities, home health services, and hospice care.
-
Part B helps pay for the cost of physician services, outpatient hospital services, medical equipment and supplies, and other health services and supplies.
-
Part C allows beneficiaries to choose to enroll in a health maintenance organization or other managed care plan, a preferred provider organization or to chose a medical savings account.
Prescription drugs will not be a covered benefit under the Medicare program until January 1, 2006, when Medicare Part D takes effect as established by the Medicare Prescription Drug, Improvement and Modernization Act of 2003 (MPDIM) (PL. 108-173). A number of questions and concerns have already been raised about certain provisions of the legislation, its implementation, and its costs, including particular concerns for individuals who receive services as “dually eligible.” These concerns are related to the range of drugs offered, potential lapses in prescription drug coverage, difficulties navigating the enrollment process, out-of-pocket costs and the associated denial of prescription drugs if co-payment cannot be met. These issues are discussed in Kates (2004) in Appendix D.
Ryan White CARE Act
Administered by the Health Resources and Services Administration (HRSA), the Ryan White CARE Act was designed to address the gaps in financing care for people with HIV/AIDS and to provide financial support to cities that were bearing a disproportionate burden of the cost of care. The CARE Act is intended to function as payer of last resort—that is, to provide care to individuals who are uninsured or underinsured and cannot cover the costs of care on their own, and who do not have another source of payment for services, public or private, available to them (HRSA, 2002j). Through the CARE Act, cities, states, and other public and private non-profit entities receive funds to develop, coordinate, and operate systems for the delivery of health and support services to medically underserved individuals and families affected by HIV disease.7 The CARE Act has helped to create an AIDS care infrastructure across the country.
|
7 |
See Appendix B for an overview of CARE Act funding allocation formulas. |
Ryan White CARE Act Title I and II
The CARE Act has several titles and components, which are described in Box 1-1. In FY 2003, federal spending for the CARE Act totaled $2.0 billion; it represents the third largest source of federal funding for HIV care in the United States (HRSA, 2003a). Title I ($626.7 million) and Title II ($1 billion) of the CARE Act provided the largest amount of grant funding to areas, states, and territories in FY 2003. The majority of Title I funds go to health care services, case management, and social support services (HRSA, 2002a). The majority of Title II funding is directed as an earmark to the AIDS Drug Assistance Progam (ADAP) ($714.3 million, a program that provides medications but can also be used to purchase private insurance with drug coverage benefits) (HRSA, 2002b). The remainder of ADAP funds is directed to states ($352.6 million) for services (HRSA, 2002c, 2003a). In recognition of the varying nature of the HIV/AIDS epidemic across the country, CARE Act grantees, including states and cities, are given broad discretion in designing local programs. As a result, there is significant variation in state funding, eligibility, services, and other aspects of CARE Act programs across the country.
Other Ryan White CARE Act Programs That Provide Care
Although much smaller in scope, three additional CARE Act programs provide funding for care services: Title III-Early Intervention Services, Planning and Capacity Grants (Title III); Title IV-Women, Children, Infants, and Youth (Title IV); and the HIV/AIDS Dental Reimbursement Program (Dental Reimbursement Program). In FY 2003, these programs had a cumulative appropriation of $288.8 million.
Title III of the CARE Act funds early-intervention HIV services provided by public and non-profit groups. Early-intervention services include counseling, testing, medical evaluation, primary care, antiretroviral therapies, medical and mental health care, case management, and other services. A smaller proportion of the Title III funds help such groups plan for the development of early-intervention services (one-year grants of $50,000) or build their capacity to provide services (up to $150,000 over a three-year period (HRSA, 2002d). In FY 2003, $200.9 million was appropriated for this program (HRSA, 2003a).
Title IV of the CARE Act addresses the specific needs of women, infants, and children and youth living with HIV. Title IV evolved from the Pediatric AIDS Demonstration Program which was established in 1988. The funds cover primary and specialty medical care, psychosocial services, logistical support and coordination, outreach, and case management (HRSA, 2002e). Title IV also provides clients with increased access to HIV/AIDS clinical
trials and research. In FY 2003, $74.5 million was appropriated for this program (HRSA, 2003a).
The Dental Reimbursement Program was added to the CARE Act in 1996. The program provides funding to improve access to oral health care for people with HIV/AIDS by providing reimbursement to educational programs. The funds help to offset the cost of uncompensated dental HIV care provided by the programs (HRSA, 2002f). The program was appropriated $13.4 million in FY 2003 (HRSA, 2003a).
In addition to these programs, two additional Ryan White CARE Act programs are designed to assist in improving the quality of care provided by the Ryan White programs and to assist community providers in improving the delivery of care. A total of $60.6 million was appropriated to these programs in FY 2003.
The AIDS Education and Training Centers (AETC) programs fund a network of 11 regional centers and associated sites that conduct multidisciplinary education and training for providers who care for persons with HIV/AIDS. The centers are designed to expand the number of providers who can counsel, diagnose, treat, and medically manage individuals with HIV, and who can help prevent high-risk behaviors that transmit HIV (HRSA, 2002g). The program disbursed $35.6 million in FY 2003 (HRSA, 2003a).
The Special Projects of National Significance (SPNS) Programs were established to advance knowledge and skills needed to deliver health and support services to underserved populations with HIV infection. SPNS programs evaluate the effectiveness of models of care, support the design of innovative care programs, and help replicate effective models (HRSA, 2002h). Funding for this program is provided through a set-aside from Titles I–V that cannot exceed $25 million (HRSA, 2003).
Clients Served by the Ryan White CARE Act
CARE Act providers serve an estimated 533,000 individuals each year (HRSA, 2003a).8 CARE Act providers, compared to non-CARE Act providers, typically serve more women, minorities (Ashman et al., 2000), and persons with no insurance (GAO, 2000). CARE Act providers also provide some services to Medicaid-only and dual-eligible beneficiaries whose needs are not met by these programs.
Data from HRSA’s Client Demonstration Project present similar findings. The project uses unique identifiers to track the service use of all HIV-
infected and -affected clients receiving services from Ryan White CARE Act-funded providers in specific Eligible Metropolitan Areas (EMAs) or states. More than 33,800 clients are tracked in five sites: Colorado; Michigan; Virginia; Orange County, CA; and Los Angeles, CA (HRSA, 2002i). Data from this tracking project indicate that the CARE Act served a much higher proportion of HIV-infected, African-American women than women from other racial/ethnic categories at these sites and that clients who received medical care services from Ryan White CARE Act providers were more likely to have no insurance coverage and less likely to have private insurance than clients who did not receive medical care from CARE Act providers.
Eligibility
CARE Act services are available to uninsured or underinsured individuals and families living with HIV/AIDS; states and municipalities determine eligibility for these services. Results from a 2000–2001 survey of Title I Planning Councils found that, in nearly all EMAs, medical eligibility required only that an individual be HIV positive. Some EMAs had additional medical eligibility criteria for specific services, for example, Social Security determination of disability to receive home health services. With respect to financial eligibility, at least 20 EMAs reported that they did not have income-related financial eligibility for Title I services. For those EMAs with financial eligibility criteria, the criteria tended to be higher than eligibility levels for Medicaid, and most were at least twice the federal poverty level (i.e., $8,980 for an individual in 2003). Some EMAs allowed client fees for some services. These were likely to be charged to individuals exceeding financial eligibility requirements. Client fees were typically based on a sliding-scale fee schedule (Buchanan, 2002).
Benefits
The CARE Act primarily funds outpatient care and support services and does not pay for hospitalizations and long-term institutional care (see Table 3-1). Services include outpatient medical and dental care, prescription drugs (through ADAP), case management, home health and hospice care, insurance continuation, and housing, transportation, and nutritional services.
Table 3-2 presents the distribution of dollars for CARE Act Titles I and II for Fiscal Years (FY) 1996, 1998, 2000, and 2001. The most notable trends in Title I spending are the level expenditures on health care since 1998 at 44 percent, and fairly level expenditures on case management and support services. Under Title II, spending on support services and case
TABLE 3-1 Services Available Through Ryan White CARE ACT Title I and II
|
Health Care Services Available Through CARE Act Titles I and II |
Support Services Available Through CARE Act Titles I and II |
|
Ambulatory medical care Medications Dental care Health insurance purchase Home health and hospice care Mental health therapy, counseling Nutritional services Rehabilitation care Substance abuse treatment Treatment adherence and counseling |
Case management Adoption/foster care assistance Buddy/companion services Client advocacy Counseling Day/respite care Direct emergency assistance Food bank, home meals Health education, risk reduction Housing assistance Outreach Primary care referrals Transportation |
TABLE 3-2 Percentage Distribution of CARE Act Title I and Title II Funds, FY 1996, 1998, 2000, 2001
|
Service |
1996 |
1998 |
2000 |
2001a |
||||
|
Ryan White Program |
Title I |
Title II |
Title I |
Title II |
Title I |
Title II |
Title I |
Title II |
|
Funding ($ millions) |
391.7 |
260.8 |
464.8 |
543.0 |
546.4 |
823.8 |
580.5 |
845.6 |
|
Percentage spent on service category |
||||||||
|
Health care (outpatient medical, dental, home health, hospice care) |
49 |
24 |
44 |
11 |
44 |
09 |
44 |
12 |
|
Case management |
12 |
11 |
11 |
06 |
12 |
05 |
12 |
08 |
|
Support services |
23 |
12 |
23 |
06 |
27 |
05 |
26 |
07 |
|
Medications/ADAP |
07 |
46 |
12 |
67 |
07 |
71 |
07 |
68 |
|
Administration, planning, evaluation, and program support |
09 |
07 |
10 |
10 |
10 |
09 |
11 |
07 |
|
a The most recent data available is for 2001 (Personal communication, Dr. Richard Conviser, HRSA, December 23, 2003). |
||||||||
management declined over the period, while spending on ADAP increased significantly, from 46 percent to 68 percent in response to the growing demand for antiretroviral therapy.
CARE Act Planning Bodies and Consortium
Title I funding is determined by a formula based on the estimated number of people living with AIDS in the EMA over the most recent 10-year period. Supplemental grants are awarded competitively by the U.S. Department of Health and Human Services (DHHS) on the basis of demonstrated severity of need and other criteria. Title II grants are also determined by a formula based on the estimated number of living AIDS cases in a state.9 The allocation of CARE Act Title I funds is guided by local planning councils. Councils have responsibility for assessing an EMA’s HIV/AIDS service needs, establishing priorities for the allocation of funds, developing a comprehensive plan for the organization and delivery of HIV services that is compatible with existing state and local plans, addressing the efficiency of the administering agency in rapidly allocating funds to areas of greatest need, and establishing operations to make planning tasks function smoothly (HRSA, 2003c). Planning council membership is determined by law and is intended to reflect the demographics of the population of individuals with HIV disease in the eligible area involved, with particular consideration given to disproportionately affected and historically underserved groups and subpopulations (HRSA, 2003c). It is required that 15 membership categories (see Box 3-2) be represented in the planning council.
CARE Act Title II funds are awarded to a state agency for administration. States use funds to provide services directly as well as through consortia. The Act defines consortia as “an association of one or more public, and one or more nonprofit private health care and support service providers and community based organizations operating within areas determined by the state to be most affected by HIV disease” (HRSA, 2003d). Consortia are responsible for assessing needs and contracting and coordinating a comprehensive continuum of outpatient health and related support services (HRSA, 2001). Furthermore, consortia are expected to promote the coordination and integration of available community resources, use case management to ensure continuity of services, and evaluate their effectiveness at meeting service needs. Consortia membership includes agencies with expe-
|
BOX 3-2
|
rience in HIV/AIDS delivery and populations and representatives of those groups of persons living with HIV disease who reflect the local incidence of HIV. In conducting their work, consortia members must also demonstrate that they have consulted with people affected by the disease, the public health agency providing HIV/AIDS-related health care, at least one community-based AIDS service provider, other CARE Act grantees, and Title I planning councils.
Private Coverage for HIV/AIDS Care
Private insurance represents a significant source of coverage for individuals with HIV/AIDS. According to the HIV Cost and Services Utilization Study (HCSUS), an estimated one-third of people in HIV/AIDS care are covered by private health insurance obtained through their employers (Kates, 2004; Bozzette et al., 1998) (see Box 3-3). Those who are insured in the group market tend to have the most comprehensive coverage and have less difficulty obtaining and keeping that coverage. The insurance market is largely regulated at the state level; however, the Health Insurance Portability and Accountability Act of 1996 (P.L. 104-191), also known as HIPAA, established basic national standards for insurance regulation in the small-group market (firms with 2 to 50 workers) and, to a lesser extent, in the
|
BOX 3-3 The HIV Cost and Services Utilization Study (HCSUS) was the first major research effort to collect information on a nationally representative sample of people in care for HIV infection. HCSUS is sponsored by the federal government and is centered at RAND. The core study enrolled a national probability sample of 2,864 HIV-infected adults who were receiving ongoing or regular medical care in the first two months of 1996. Respondents were sampled from 28 urban areas and 24 clusters of rural counties in the continental United States. Patients receiving services in hospitals, clinics, and private staff model practice settings were enrolled. HCSUS oversampled women and members of health maintenance organizations to obtain more precise information on these specific populations. The HCSUS design includes a baseline in-person interview with sampled patients, two follow-up interviews scheduled for 6 months and 12 months after the baseline interview, and abstractions of data from patients’ medical, pharmaceutical, and billing records. All baseline and followup interviews were completed as of January1998. In addition, a supplemental interview containing a standardized instrument to diagnose psychiatric disorders was administered to a subsample of approximately 1,500 HCSUS respondents in conjunction with the first followup interview. Additional blood samples have been collected from a majority of HCSUS respondents, and virological analyses are being initiated. Supplemental studies are examining HIV care delivery in rural areas, prevalence of mental and substance abuse disorders, oral health of HIV-positive individuals, and issues related to HIV-infected persons over 50 years of age. A supplemental sample of persons receiving care in rural areas was obtained to augment the core rural sample and to provide a basis for studies focused on the rural population with HIV infection. Another supplemental project is collecting data from the providers of care to HCSUS respondents. The study continues to add to our understanding of AIDS. Although the original data collection activities are now several years old, the point estimates for a large number of values are still robust. Values for social situations and access issues within subpopulations, for example, have not changed much: most of those in care now were in care then (because of longer survival), and most people entering care still enter care with advanced disease. Point estimates for changes in clinical practices resulting from new information such as the proportion of persons on four or more antiretroviral therapies are less robust. However, this study remains the most diverse cohort ever, and the relationships found between predictor variables (e.g., demographics, insurance, region, etc.) and status or outcomes are not only robust but very unlikely to have changed over time (Personal communication, Sam Bozzette). Results from the HCSUS appear in a number of peer-reviewed journal articles. SOURCE: AHRQ, 2004. |
individual market. Protections covered in HIPAA included the following (Pollitz et al., 2000; Kates, 2004):
-
Portability. Exclusions of preexisting medical conditions are limited to a maximum of 12 months.
-
Nondiscrimination. Insurers in the group market are prohibited from conditioning persons’ eligibility for group coverage on their health status. This does not apply to individual policies.
-
Guaranteed issue. Insurers must offer all of their small-group policies to any small employers that want to purchase coverage for their workers.
-
Guaranteed renewal. Insurers must allow all policies—group and individual—to be renewed.
Although private insurance represents a significant source of coverage for individuals with HIV/AIDS, its importance as a source of coverage diminishes as the disease progresses. A recent analysis of HCSUS data found that private insurance covered 42 percent of individuals with HIV infection in the early asymptomatic stage of the disease. Medicare, Medicaid, or a combination of the two programs provided coverage for 31 percent of those with asymptomatic disease, and the remaining 26 percent of individuals were uninsured. During the symptomatic stage, private insurance coverage dropped to 31 percent, federal programs provided coverage for 44 percent of symptomatic individuals, and the percentage of uninsured individuals remained virtually unchanged (25 percent). In the most advanced stage of the disease—full-blown AIDS—private insurance bears a proportionately small burden for providing coverage. At this stage, private insurance covers 26 percent of individuals, federal entitlement programs cover 62 percent of individuals, and 12 percent are uninsured. The study authors note that there is a close link between insurance coverage and HIV disease progression. Patients with private insurance are able to start treatment early but tend to lose insurance coverage as their disease worsens, and the uninsured must delay treatment until their health deteriorates enough for them to be deemed disabled and eligible for public insurance coverage under Medicare or Medicaid (Goldman et al., 2003).
DELIVERY OF HIV/AIDS CARE SERVICES
During the first two decades of the epidemic, hospitals served as the backbone of the HIV/AIDS delivery system. At that time, AIDS patients required the expertise of hospital-based infectious disease specialists for the majority of their clinical care, including palliative medical interventions.
Organizations, some linked to hospitals and some not, provided AIDS patients with supportive and other palliative care services.
By the end of the epidemic’s second decade (1990s), revolutionary and increasingly more simplified HAART medical therapy was successful in preventing disease progression, death, and disability. Today, patients who know their status, enter care, and stay in continuous care over their lifetime experience HIV/AIDS as a lifetime chronic disease that most often allows them to continue to make productive contributions to society (Gifford and Groessl, 2002). Changes in understanding of the disease and improvements in therapeutic technology have required significant changes in delivery system structure, moving the primary locus of care from the hospitals, hospital providers, and end-of-life social supports like buddy and nutrition services to outpatient medical care systems and medical providers supported by social services providers. While care still includes specialized inpatient care when needed, outpatient clinical services are now the backbone of the HIV/AIDS care system. Care services are organized and coordinated by outpatient infectious disease specialists, primary care physicians, or nonphysician case managers from community-based organizations that provide social support.
The shift from inpatient to outpatient care is consistent with the shift in the goals of therapy for HIV-infected patients. Until the advent of HAART, the goals of treatment were to manage the acute conditions associated with immune system deficiencies and provide supportive and palliative care services so as to minimize suffering and maximize functional status through a period of decline and ultimately death. With the introduction of HAART, survival times are longer and the primary treatment goals are to reduce viral loads to low levels, maintain immune system function, and delay or prevent the progression from HIV to AIDS. Today, HIV/AIDS is managed much like a serious chronic condition (e.g., diabetes, asthma) rather than a terminal disease such as cancer (Gifford and Groessl, 2002). The shift in care emphasis—from acute to chronic—has important implications for managing the condition. As discussed in the section on adherence in Chapter 2, diabetes in particular provides important lessons in the management of HIV. These lessons include the importance of developing a collaborative relationship between the patient and the health care provider and implementing financing mechanisms that allow for continuity of care and adequate reimbursement of time spent on the part of the health care provider (APHA, 2002). In addition, experience with the management of diabetes has highlighted the importance of provider training in promoting adherence to treatment (APHA, 2002).
The Committee reviewed current guidelines and standards of care for HIV-infected individuals to understand what an appropriate level of care would include. Eight broad areas of standard care surfaced that capture the critical components of HIV care. These critical components of HIV care
will reduce mortality, extend the lives of people with HIV, and, when combined with prevention services, assist in controlling the epidemic. They include HAART, other drug therapies, primary care services, obstetrics and reproductive health services for HIV-infected women, substance abuse treatment, treatment for mental illness, case management services, and HIV prevention services.
Highly Active Antiretroviral Therapy
As noted in Chapter 2, access and adherence to life-sustaining comprehensive antiretroviral therapy is the cornerstone of HIV care. Without it, patients experience a rapid death. HAART is described as a standard of care in the Guidelines for the Use of Antiretroviral Agents in HIV-Infected Adults and Adolescents (DHHS, 2004). The guidelines recommend that HAART be offered to all patients with symptoms of HIV infection, especially those with with a CD4 cell count below 350 or viral load exceeding 55,000 copies/mL. To assist in managing the disease, the International AIDS Society-USA Panel developed new guidelines recommending antiretroviral resistance testing to better manage HAART therapy and minimize the risk of viral drug resistance (Hirsch et al., 2003).
Compelling cost-effectiveness evidence also supports the need to provide HIV-infected individuals with HAART. Studies by numerous researchers have demonstrated that HAART use is cost effective in that it significantly reduces hospital inpatient costs and community costs (Gebo et al., 1999; Bozzette et al., 2001; Moore, 2000; Keiser et al., 2001; Freedberg et al., 2001) and improves the health-related quality of life of patients with HIV infection (Hays et al., 2000). 10
As noted earlier, HAART is available through Medicaid and the ADAP portion of the CARE Act programs. The extent to which individuals receive appropriate prescribed drugs, however, varies significantly for each program.
Other Drug Therapies That Prevent Complications and Support Retention in Care
Although antiretroviral therapy can reduce opportunistic infections in HIV-infected people, some will still develop a variety of infections that complicate their care. Many of these illnesses are very serious, and they
need to be prevented or, when they occur, treated. Opportunistic infections seen in individuals with HIV infection include those that are bacterial and mycobacterial (Mycobacterium avium complex or MAC, tuberculosis, syphilis), fungal (candidiasis, coccidioidomycosis, histoplasmosis), protozoal (cryptosporidiosis, cryptococcosis, toxoplasmosis), and viral (cytomegalovirus or CMV, herpes zoster). The U.S. Public Health Service and Infectious Diseases Society of America (2001) (CDC, 1998) have developed guidelines for preventing exposure to infections, disease, and recurrence of these opportunistic infections among HIV-infected persons. Specific guidelines for the prevention and treatment of tuberculosis in HIV patients have been published by CDC (1998, 2003d).
Obstetrics and Reproductive Health Services for HIV-infected Women and Pediatric Care for Infants with HIV
As stated in Reducing the Odds: Preventing Perinatal Transmission of HIV in the United States (IOM, 1999),“One of the most promising victories in the battle against AIDS was the finding in 1994 that administration of the antiretroviral drug zidovudine (ZDV) during pregnancy and childbirth could reduce the chance that the child of an HIV-positive mother would be infected by two thirds.” Since then, epidemiologic data have since confirmed the efficacy of ZDV for reduction of perinatal transmission. In 1998, the Public Health Service Task Force recommended that all pregnant HIV-1 infected women should be offered HAART to maximally suppress viral replication, to reduce the risk of perinatal transmission, and to minimize the risk of development of resistant viruses. These recommendations were revised in June 2003 to update recommendations on antiretroviral chemoprophylaxis for reducing perinatal transmission. The recommendations also state that all women should receive comprehensive health care services that continue after pregnancy for their own medical care and for assistance with family planning and contraception (U.S. Public Health Service Task Force, 2003).
Similar guidelines for the use of antiretroviral agents for the treatment of pediatric HIV infection were developed by the Working Group on Antiretroviral Therapy and Medical Management (WGATMM) of HIV-Infected Children (revised June 2003). The guidelines provide the standard of care for the management of an estimated 300 infants who contract HIV from their mothers each year (CDC, 2003a; WGATMM, 2004). Supervising the HIV Perinatal and Pediatric guidelines is a new initiative launched by CDC and other DHHS agencies: Advancing HIV Prevention: New Strategies for a Changing Epidemic (CDC, 2003b). One of the initiative’s four key strategies is to further decrease mother-to-child HIV transmission by
incorporating HIV testing in the routine battery of prenatal tests (CDC, 2003b).
Care for Individuals with HIV/AIDS, Substance Abuse, and Mental Illness
Care of the HIV-infected individual requires specific attention to the interplay of co-occurring diseases of substance abuse and mental illness (Douaihy et al., 2003a, 2003b; Bruce and Altice, 2003; Bing et al., 2001; Altice and Friedland, 1998; CSAT, 1995, 2000). Several reasons support the need to provide care delivery strategies that are comprehensive and that meet the standards of care for these three diseases. First, adherence to antiretroviral treatment may be undermined by co-occurring substance abuse and mental illness and could lead to the development of drug resistance. Second, the clinical management of HIV-infected individuals must take into account the impact of substance abuse and mental illness and their treatment on the expression of symptoms, the development of drug interactions, progression of HIV disease, the utilization of care services, and high-risk HIV behaviors (see Box 3-4).
Drug treatment adherence. As noted in Chapter 2, adherence to antiretroviral therapy is critical for therapeutic effectiveness (Harrigan et al., 2003; Garcia de Olalla et al., 2002; Bangsberg et al., 2001; McNabb et al., 2001; Paterson et al., 2000). However, an individual’s ability to adhere to a treatment regimen may be related to co-occurring substance abuse and mental illness (Ferrando et al., 1996; Sternhell and Corr, 2002; Starace et al., 2002). A longitudinal study of the effects of continued drug use on the treatment of HIV infection in patients who attend an urbanized HIV clinic (Lucas et al., 2002) found that switching from non-use to substance abuse was strongly associated with worsening antiretroviral therapy use and adherence, less frequent HIV-1 RNA suppression, and blunted CD4 cell increases. The researchers also found that switching from substance abuse to non-use was strongly associated with improvements in antiretroviral therapy use and adherence, and HIV-1 treatment.
Tucker and colleagues (2003) analyzed data from the HCSUS study to investigate the association of antiretroviral medication nonadherence with specific types of psychiatric disorders and drug use, and with varying level of alcohol use. The researchers found that patients with depression, generalized anxiety disorder, or panic disorder were more likely to be nonadherent than those without a psychiatric disorder. Nonadherence was also associated with use of cocaine, marijuana, amphetamines, or sedatives in the previous months. Moderate and heavy alcohol use compared with no alcohol use was also found to be associated with nonadherence (Tucker et al., 2003). Researchers in Canada (Palepu et al., 2003) made similar find-
|
BOX 3-4 “Although discussions regarding triple diagnosis began more than 10 years ago, the interrelated nature of substance abuse, mental illness, and HIV infection has been highlighted in the last several years with the understanding that adherence to antiretroviral therapy must approach 100 percent to be most effective. Both active substance abuse and mental illness in a HIV infected persons make the attainment of high adherence difficult, though not impossible. Among substance abusers, especially injection users, there is a high prevalence of social instability, which exacerbates the effects of substance abuse on adherence. Poor adherence to antiretroviral may result in the development of drug resistance and poor virologic outcomes. In addition, persons with triple diagnosis, especially those not receiving treatment, are also more likely to engage in high risk behaviors and thus fuel the HIV epidemic through the transmission of the virus, particularly multidrug-resistant strains. “Clinically, it is unrealistic to address each of these diagnoses individually. Because of the overlapping natures of these 3 diagnoses, triple diagnosis should be viewed as 3 overlapping spheres of influence, with each diagnosis affecting the others. Conceptually this is important because successful therapy will treat all spheres of influence rather than ignore any single area. Consider the case of the heroin-dependent woman with bipolar disorder and advanced HIV disease. It would not be feasible to expect that one condition must be treated before addressing the others. Such an approach would likely result in a stalemate in which none of the conditions would be adequately treated. While the psychiatrist might argue that her drug use must be stabilized first, the drug treatment provider might insist that her untreated bipolar disorder compromises successful drug treatment. The HIV clinician might fear poor adherence to HAART and forego treatment until both the mental illness and substance abuse are controlled. This approach might result in significant morbidity and mortality as a result of opportunistic infections. “Recognition of the interplay between substance abuse and mental illness in HIV-infected patients remains a focal point for the organization of health care and public health services. Models of integrated health care must continually be developed using innovative approached to address this complex problem….” R. Douglas Bruce, M.D. Fredrick L. Altice, M.D. SOURCE: Bruce and Altice, 2003. |
ings. In a study of injection drug use and virologic response to HAART, current injection drug users were significantly less likely to suppress their HIV-1 RNA while former injection drug users were not significantly different from non-drug users. The researchers also found a significant interaction between drug use and adherence. The adherence of former drug users and non-drug users was positively associated with HIV-1 RNA sup-
pression, whereas for current drug users it was not. Enhancing adherence to HAART would require careful assessment and treatment of co-occurring drug use and mental illness.
Expression of symptoms. The differential diagnosis and treatment of individuals with HIV-infection, substance abuse, and mental illness is complicated by the overlap of some symptoms and medical complications associated with the three disease entities (CSAT, 2000). Anorexia and weight loss, for example, may be directly related to HIV infection or associated with cocaine and methamphetamine use. Similarly, neurological symptoms such as peripheral neuropathy can be associated with HIV infection, AIDS dementia complex, and with other opportunistic infections such as toxoplasmosis. Peripheral neuropathy is also associated with the abuse of alcohol (alcohol polyneuropathy). Similarly, altered mental states can be associated with mental illness, HIV infection, opportunistic infection with cryptococcosis, and with the use of methamphetamine and other recreational drugs.
Drug interactions. Treatment of HIV, substance abuse, and mental illness often require the use of prescription medication; thus, a clinician is faced with managing the potential of serious pharmacokinetic drug interactions (Faragon and Pilliero, 2003; CSAT, 2000). These interactions can affect absorption, distribution, metabolism, and elimination of concurrently administered drugs. The use of the recreational drug ecstasy (3,4 methylenedioxymeth; MDMA), for example, can lead to significant toxicity when combined with antiretroviral therapy. The combination of heroin and ritonar and nelfinavir may enhance the effect of heroin. The medical or recreational use of barbituates is also problematic because it can reduce the levels of protease inhibitors and increase the risk of virologic failure and/or resistance. Alcohol use by patients with HIV has been shown to alter drug metabolism and to increase the risk of drug-induced hepatotoxicity, especially in patients co-infected with hepatitis C.
Similarly, prescribed medications used in the treatment of substance abuse and mental illness can produce drug interactions with the medications used in the treatment of HIV infection. The concentration of methadone, used in the treatment of heroin addiction, has been found to be significantly reduced when combined with certain HAART drugs—efavirenz and nevirapine (Faragon and Pilliero, 2003). Medications used to treat psychiatric disorders such as benzodiazepines can interact with some antiretrovirals in a negative way. Antiretrovials may increase the risk of benzodiazepine toxicity. HIV disease management would require an assessment of potential drug interactions.
Complication and progression of HIV disease. The course of HIV disease can be mediated by state of mind. Researchers investigating depression as a risk factor in HIV disease found that among women whose CD4 was
less than 200, HIV-related mortality of those with chronic or intermittent depressive symptoms was 54 percent and 48 percent compared with 21 percent for those with limited or no depressive symptoms. The study’s findings provide evidence that depression may alter the function of killer lymphocytes in HIV-infected women and suggests that depression may decrease natural killer cell activity and lead to an increase in activated CD8 T lymphocytes, and that viral load may decrease natural killer cell activity and lead to an increase in activated CD8 lymphocytes and viral load (Evans et al., 2002).
Another study addressing the impact of depression and mortality among women with HIV found that women with chronic depressive symptoms were two times more likely to die than women with limited or no depressive symptoms. Women with chronic depressive symptoms also had a more rapid decline in CD4 counts compared with women with limited or no depressive symptoms (Ickovics et al., 2001). Additional research investigating whether psychological distress was independently associated with rapid progression to AIDS among HIV-infected injection drug users found similar results. Psychological distress was found to be associated with more rapid time to AIDS. The strongest association was observed in individuals with the lowest CD4 cell counts (Golub et al., 2003).
High risk behavior. As noted in Chapter 2, HIV-infected individuals who abuse substances or are mentally ill are at a higher risk of transmitting HIV infection to others. For some, substance abuse and mental illness placed them at risk for becoming infected with HIV. Use of injection drugs and associated practices such as the sharing of needles and other injection equipment is an efficient method for transmitting HIV. Similarly, the exchange of bodily fluids through unprotected sexual activity increases the risk of transmitting HIV infection to others (IOM, 2001; Friedman et al., 1999; CSAT, 2000). Individuals with mental illnesses—including mood disorders, schizophrenia, and personality disorders—are at higher risk of engaging in behaviors that increase HIV risk. Risky behavior has been noted to be related to illness severity and psychiatric symptoms (Otto-Salaj and Stevenson, 2001).
Utilization of services. In addition to reducing adherence to antiretroviral therapy, substance abuse may also impact the use of other medical services. Arici et al. (2002) found that HIV-infected active injection drug users tend to be less compliant with keeping medical appointments, taking medications, and obtaining regular laboratory testing. Depression may also interfere with treatment of HIV and utilization of care services. Depressed patients are often more difficult to engage in and maintain in treatment because of the associated anergy, hopelessness, and negativism associated with their disorder (Hsu, 2002).
The complex nature of treating individuals with co-occurring HIV, substance abuse and mental illness has given rise to rethinking the way care is provided. Consensus groups, researchers, care providers, and government officials have begun to consider integrated treatment approaches that integrate services of medical providers, psychiatrists, substance abuse counselors, therapists, and social workers. The Center for Substance Abuse and Treatment (CSAT), in its Treatment Improvement Protocol on Substance Abuse Treatment for persons with HIV/AIDS (CSAT, 2000), for example, notes that the treatment of substance abuse and HIV/AIDS should reflect the interconnected relationship they share and be coordinated as much as possible to maximize care for persons with both HIV/AIDS and substance abuse disorders. CSAT recommends that “integrated treatment is the best option” for this population and that substance abuse treatment programs should incorporate primary care. CSAT also recommends that substance abuse treatment centers screen for HIV (CSAT, 2000). Two federal programs that focus on this population, the HIV set-aside in Substance Abuse Prevention and Treatment Block Grants and the CARE Act, are mandated to seek collaboration between substance abuse treatment providers and medical care providers and to seek to establish service linkages between the two systems (CSAT, 1995). Both of these programs, however, are relatively small compared with other parts of the HIV care system. Medicaid, the care provider with which the majority of people with HIV/AIDS in care interact, provides highly variable and at times restricted access to substance abuse treatment and offers few incentives to integrate care (Lubinski et al., 2002).
The Substance Abuse and Mental Health Services Administration (SAMHSA) in collaboration with HRSA and the CDC have been working on developing more effective services to integrate HIV prevention and care, substance abuse prevention and treatment, and mental health services (SAMHSA Funding FY 2004 Budget Narrative). Integration of services is an important focus of HRSA projects under its SPNS program. The HIV/AIDS Treatment Adherence Health Outcomes and Cost Study, for example, is a collaborative effort of six U.S. Department of Health and Human Service components to study integrated mental health, substance use, and primary medical HIV treatment interventions.
The HIV/AIDS Mental Health Services Demonstration Program, a joint federal project that offered mental health care to PLWH/A, found that individuals with comorbid substance abuse disorders and HIV were more likely to seek primary health care if they received mental health services and that early intervention with mental health services can improve adherence to HIV medications (SAMHSA, 1997). In short, individuals with HIV infection and severe and persistent mental illness often are inhibited by their mental illness from seeking care and from adhering to medication regimens that could help them lengthen and improve the quality of their lives.
Case Management Services
While there is no set definition for “case management,” the Ryan White CARE Act Title I Manual (HRSA, 2001) defines case management for the Title I and Title II programs as:
A range of client centered services that link clients with health care, psychosocial and other services to insure timely, coordinated access to medically appropriate levels of health and support services, continuity of care, on-going assessment of the client’s and other family members’ needs and personal support systems, and inpatient case management services that prevent unnecessary hospitalizations or that expedite discharge, as medically appropriate, from inpatient facilities. Key activities include: initial comprehensive assessment of the client’s needs and personal support systems; development of a comprehensive, individualized service plan; coordination of the services required to implement the plan; client monitoring to assess the efficacy for the plan; and periodic re-evaluation and revision of the plan as necessary over the life of the client. May include client-specific advocacy and/or review of utilization of services.
More simply put, the main purpose of case management is to coordinate care, decrease barriers to medical and support services, and increase quality of life (HRSA, 2001).
Growing evidence shows that HIV-positive individuals who have case managers are more likely to use life-prolonging HIV medications and to have their needs met for income support, health insurance, home health care, and emotional counseling than those without case managers (Katz et al., 2001; McKinney and Marconi, 2002). Specifically, case management was found to have a positive effect on retaining people in appropriate HIV medical care (Conviser and Pounds, 2002; Ashman et al., 2002; Sherer et al., 2002; Messeri et al., 2002; Magnus et al., 2002). In one study, individuals who received case management were more than twice as likely to be retained in appropriate medical care than were those who did not (Messeri et al., 2002).
A debate is ongoing, however, about how case management services are best delivered. In one delivery model, case management services are co-located or intensely related to medical care. In another model, services are established in community service organizations that lack tight ties to clinical providers. Many medical providers of HIV services prefer models in which case management services are closely related to primary care, so that these services can directly support treatment adherence.
Case management service visits account for the largest number of visits made by Ryan White CARE Act clients under Title I and Title II non-ADAP services (HRSA, 2002j). Case management services are optional services under Medicaid.
HIV Prevention Services
Antiretroviral therapy can help prevent transmission of HIV because it reduces a person’s viral load and renders the person less infectious (Vernazza et al., 1999; Staszewski et al., 1999; Barroso et al., 2000). However, an HIV-infected person receiving antiretroviral therapy can still spread infection to others, thus risk reduction interventions among HIV-infected individuals is considered an important part of overall HIV prevention. The U.S. Preventive Services Task Force Guide to Clinical Preventive Services (1996) makes HIV prevention recommendations for providers in clinical care settings. Specifically, the task force recommends that clinicians take a complete sexual and drug history to help determine patient risk and the appropriate prevention intervention. The recommendations, though, do not target individuals who are already HIV infected and who may still engage in risky behavior. In 1997, a National Institutes of Health consensus statement concluded that there was a need to develop programs to help HIV-infected individuals avoid risky behavior over long periods of time (NIH, 1997). A 2001 Institute of Medicine report, No Time to Lose: Getting More from HIV Prevention, noted this deficiency and recommended that HIV prevention services for HIV-infected persons and those at high risk should be a standard of care in all clinical settings. There is no mandatory or optional Medicaid service category that specifically covers HIV prevention services in the clinical setting (IOM, 2001).
More recently, CDC’s Advancing HIV Prevention: New Strategies for a Changing Epidemic identified preventing new infections among persons diagnosed with HIV and their partners as a key element of its new prevention strategy. CDC has made a commitment to publishing (along with other federal agency partners) Recommendations Incorporating HIV Prevention into the Medical Care of Persons with HIV Infection (CDC, 2003c).
The literature reports at least two randomized trials for a risk reduction intervention for HIV-positive injection drug users (Kalichman et al., 2001; Margolin et al., 2003). In the first study, HIV-infected individuals were randomly assigned to an intervention to reduce the risk of HIV transmission. The risk reduction intervention resulted in less unprotected intercourse and greater condom use at follow-up. Transmission-risk behaviors with non-HIV-positive sexual partners and estimated HIV transmission rates were also significantly lower for the behavior risk-reduction intervention group. Authors of the second study (Margolin et al., 2003) found that enhancing methadone maintenance with interventions targeting HIV-seropositive injection drug users increases both harm reduction and health promotion behaviors. HRSA, under its CARE Act SPNS program, has two studies underway exploring prevention with HIV-infected persons seen in primary care settings and a demonstration project on prevention for HIV-positive persons (HRSA, 2003a).
Primary Care Services
HIV/AIDS is a complex multi-system illness. Patients with HIV/AIDS require a broad range of services and care from a number of providers. A primary care services approach to managing the complexity of services and providers who provide care to people with HIV infection has been an important foundation of the CARE Act and the federal Medicaid program.
Generally, primary care is understood as the provision of integrated, accessible health care services by clinicians who are accountable for addressing a large majority of personal health care needs, developing a sustained partnership with patients, and practicing in the context of family and community (IOM, 1996). The elements of primary care include first contact care, continuity of care or one individual or team of associated individuals serving as the source of care over a defined period of time, comprehensiveness of services and the need to provide them directly or arrange for their provision when needed, and coordination of providers and referral services. The value of primary care for individuals is that it provides a place to which patients can bring a wide range of health problems for appropriate attention, guides patients through the health care system, provides opportunities for disease prevention and health promotion as well as early detection of problems, and helps to build bridges between personal health care services and providers and patients’ families and communities that can assist in meeting the health needs of the patient (IOM, 1996).
Under the CARE Act, the primary care approach is used to provide and coordinate providers and such services as diagnostic testing, early intervention and risk assessment, preventive care and screening, practitioner examination, medical history taking, diagnosis and treatment of common physical and mental conditions, prescribing and managing medication therapy, education and counseling on health issues, well-baby care, continuing care and management of chronic conditions, and referral to and provision of specialty care (includes all medical subspecialties) (HRSA, 2003b, 2003c).
Primary care services also include primary oral health care. The first signs of HIV infection are often found in the oral cavity. As the disease progresses and the immune system deteriorates, AIDS patients are more susceptible to mouth infections such as oral herpes, fungal diseases, and gum disease. Thus, primary oral care is a critical component of primary care for HIV/AIDS.
Coverage for primary care services is mandatory under Medicaid. Primary care services are supported by the CARE Act but are available in varying degrees; services vary significantly from state to state and city to city depending on local resource allocation decisions. Acknowledging that HIV/AIDS patients suffer a high incidence of oral disease and many low-
income people with HIV need assistance covering their dental costs, the Ryan White HIV/AIDS Dental Reimbursement Program was established in 2000. The program is directed at dental institutions (dental schools, dental hygiene schools, and postdoctoral dental education programs) to cover their non-reimbursed costs of providing oral health care to individuals with HIV.
Where HIV/AIDS Patients Receive Care
The most comprehensive source of information on the delivery of HIV care comes from the HIV Costs and Service Utilization Study. The survey is based on a representative sample of individuals receiving medical care for HIV infection in January and February of 1996.11 An analysis of survey data found that 30 percent of patients received care at major teaching hospitals, and the balance received care from office-based physicians and community hospitals and clinics. Data also show that one-third of patients made at least one visit to an emergency room and 20 percent were hospitalized every six months.
One of the survey’s most disturbing findings underscored the lack of regular care by individuals with HIV infection. Survey results suggest that an estimated two-thirds of HIV-infected adults do not receive medical care on a regular basis. Furthermore, most infected adults who do not receive medical care on a regular basis are in the early stages of disease (Shapiro et al., 1999).
With the spread of HIV infection outside large metropolitan areas, the delivery of care in smaller cities and less urbanized areas has become a growing concern. HCSUS data were analyzed to assess the delivery of care in rural areas. Results of the analysis revealed significant disparities between rural and urban areas. Patients in rural HIV care were more likely than patients in urban care to receive care from providers seeing few infected patients, and were also less likely than urban patients to have taken HAART (Cohn et al., 2001). This finding is significant given the recognition that greater physician and hospital experience with HIV/AIDS treatment has been linked to improved outcome—that is, longer survival after AIDS diagnosis (Laine et al., 1998). Other study findings have shown that patients in clinics with HIV expertise rely less on the emergency department for care (Markson et al., 1998).
|
Findings:
|
REFERENCES
AHRQ (Agency for Health, Research and Quality). 2004. HCSUS: HIV Cost and Services Utilization Study. Fact sheet. Rockville, MD: Agency for Health Care Policy and Research. [Online]. Available: http://www.ahrq.gov/data/hcsus.htm [accessed January 3, 2004].
Altice FL, Friedland GH. 1998. The era of adherence to HIV therapy. Annals of Internal Medicine 129(6):503–505.
APHA (American Public Health Association). 2002. Adherence to HIV Treatment Regimens: Recommendations for Best Practices. Pp. 126–130. [Online]. Available: http://www.apha.org/PPP/HIV/Best_Practices.pdf [accessed March 14, 2004].
Arici C, Ripamonti D, Maggiolo F, Rizzi M, Finazzi MG, Pezzotti P, Suter F. 2002. Factors associated with the failure of HIV-positive persons to return for scheduled medical visits. HIV Clinical Trials 3(1):52–57.
Ashman JJ, Conviser R, Pounds MB. 2002. Associations between HIV-positive individuals’ receipt of ancillary services and medical care receipt and retention. AIDS Care 14(Suppl. 1):S109–S118.
Ashman JJ, Marconi KM, McKinney MM, O’Neill JF. 2000. Who receives Ryan White CARE Act Services? A demographic comparison of CARE Act clients and the general AIDS population. AIDS Patient Care STDS 14(10):561–565.
Bangsberg DR, Perry S, Charlesbois ED, Clark RA, Robertson M, Zolopa AR, Moss A. 2001. Non-adherence to highly active antiretroviral therapy predicts progression to AIDS. AIDS 15(9):1181–1183.
Barroso PF, Schecter M, Gupta P, Melo MF, Viera M, Murta FC, Sourza Y, Harrison LH. 2000. Effect of antiretroviral therapy on HIV shedding in semen. Annals of Internal Medicine 133(4):280–284.
Bing EG, Burnam MA, Longshore D, Fleishman JA, Sherbourne CD, London AS, Turner BJ, Eggan F, Beckman R, Vitiello B, Morton SC, Orlando M, Bozzette SA, Ortiz-Barron L, Shapiro M. 2001. Psychiatric disorders and drug use among human immunodeficiency virus-infected adults in the United States. Archives of General Psychiatry 58(8):721–728.
Bozzette S, Berry SH, Duan N, Frankel MR, Leibowitz AA, Lefkowitz D, Emmons CA, Senterfitt JW, Berk ML, Morton SC, Shapiro MF. 1998. The care of HIV-infected adults in the United States. HIV Cost and Services Utilization Study Consortium. New England Journal of Medicine 339(26):1897–1904.
Bozzette SA, Joyce G, McCaffrey DF, Leibowitz AA, Morton SC, Berry SH, Rastegar A, Timberlake D, Shapiro MF, Goldman DP. 2001. Expenditures for the care of HIV-infected patients in the era of highly active antiretroviral therapy. HIV Cost and Services Utilization Study Consortium. New England Journal of Medicine 344(11):817–823.
Bruce RD, Altice FL. 2003. Editorial Comment. Why treat three conditions when it is one patient? AIDS Reader 13(8):375–382.
Buchanan RJ. 2002. Ryan White CARE Act and eligible metropolitan areas. Health Care Financing Review 23(4):149–157.
CDC (Centers for Disease Control and Prevention). 1998. Prevention and treatment of tuberculosis among patients infected with human immunodeficiency virus: principles of therapy and revised recommendations. MMWR 47(RR–20):1–26.
CDC. 2003a. Advancing HIV prevention: new strategies for a changing epidemic—United States, 2003. MMWR 52(15):329–332.
CDC. 2003b. Advancing HIV Prevention: The Science Behind the Initiative. [Online]. Available: http://www.cdc.gov/hiv/partners/ahp_science.htm [accessed October 14, 2003].
CDC. 2003c. Incorporating HIV prevention into the medical care of persons living with HIV. Recommendations of CDC, Health Resources and Services Administration, National Institutes of Health, and HIV Medicine Association of the Infectious Diseases Society of America. MMWR 52(R12):1–24.
CDC. 2003d. Treatment of tuberculosis. Official statement of the American Thoracic Society, CDC, and Infectious Diseases Society of America. MMWR 52(R11):1–77.
CMS (Centers for Medicare & Medicaid Services). 2002. Fact Sheet: Medicaid and Acquired Immunodeficiency Syndrome (AIDS) and Human Immunodeficiency Virus (HIV) Infection. [Online]. Available: http://cms.hhs.gov.hiv/hivfs.asp [accessed July 8, 2003].
CSAT (Center for Substance Abuse Treatment). 1995. Treatment for HIV-Infected Alcohol and other Drug Abusers: Treatment Improvement Protocol Series 15. DHHS Publication No. (SMA) 95-3038. Rockville, MD: Substance Abuse and Mental Health Services Administration.
CSAT. 2000. Substance Abuse Treatment for Persons with HIV/AIDS: Treatment Improvement Protocol Series 37. DHHS Publication No. (SMA) 00-3410. Rockville, MD: Substance Abuse and Mental Health Services Administration.
Cohn SE, Berk ML, Berry SH, Duan N, Frankel MR, Klein JD, McKinney MM, Rastegar A, Smith S, Shapiro MF, Bozzette SA. 2001. The care of HIV-infected adults in rural areas of the United States. Journal of Acquired Immune Deficiency Syndrome 28(4):385–392.
Conviser R, Pounds MB. 2002. The role of ancillary services in client-centered systems of care. AIDS Care 14(Suppl. 1):119–132.
DHHS (U.S. Department of Health and Human Services). 2004. Guidelines for the Use of Antiretroviral Agents in HIV-1-Infected Adults and Adolescents. [Online]. Available: http://aidsinfo.nih.gov/guidelines/default_db2.asp?id=50 [accessed April 15, 2004].
Douaihy AB, Jou RJ, Gorske T, Salloum IM. 2003a. Triple diagnosis: dual diagnosis and HIV disease, part 1. AIDS Reader 13(7):331–341.
Douaihy AB, Jou RJ, Gorske T, Salloum IM. 2003b. Triple diagnosis: dual diagnosis and HIV disease, part 2. AIDS Reader 13(8):375–382.
Evans DL, Ten Have TR, Douglas SD, Genes DR, Morrison M, Chiappini MS, Brinker Spence P, Job C, Mercer DE, Wang YL, Cruess D, Dube B, Dalen EA, Brown T, Bauer R, Petitto JM. 2002. Association of depression with viral load, CD8 I lymphocytes, and natural killer cells in women with H infection. American Journal of Psychiatry 159(10):1752–1759.
Faragon JJ, Pilliero PJ. 2003. Drug interactions associated with HAART: focus on treatment for addiction and recreational drugs. AIDS Reader 13(9):433–450.
Ferrando SJ, Wall TL, Batki SL, Sorensen JL. 1996. Psychiatric morbidity, illicit drug use and adherence to zidovudine (AZT) among injection drug users with HIV disease. American Journal of Drug & Alcohol Abuse 22(4):475–487.
Freedberg KA, Losina E, Weinstein MC, Paltiel AD, Cohen CJ, Seage GR, Craven DE, Zhang H, Kimmel AD, Goldie SJ. 2001. The cost effectiveness of combination antiretroviral therapy for HIV disease. New England Journal of Medicine 344(11):824–831.
Friedman SR, Curtis R, Neaigus A, Benny J, Des Jarlais DC. 1999. Social Networks, Drug Injectors’ Lives, and HIV/AIDS. New York: Kluwer Academic/Plenum Publishers.
GAO (General Accounting Office). 2000. Ryan White CARE Act: Opportunities to Enhance Funding Equity. GAO/T-HEHS-00-150. Washington, DC: GAO.
Garcia de Olalla P, Knobel H, Carmona A, Guelar A, Lopez-Colomes J, Cayla JA. 2002. Impact of adherence and highly active antiretroviral therapy on survival in HIV-infected patients. Journal of Acquired Immune Deficiency Syndromes 30(1):105–110.
Gebo KA, Chaisson RE, Folkemer JG, Bartlett JG, Moore RD. 1999. Costs of HIV medical care in the era of highly active antiretroviral therapy. AIDS 13(8):963–999.
Gifford AL, Groessl EJ. 2002. Chronic disease self-management and adherence to HIV medications. Journal of Acquired Immune Deficiency Syndrome 31:S163–S166.
Goldman DP, Leibowitz AA, Joyce GF, Fleishman JA, Bozzette SA, Duan N, Shapiro MF. 2003. Insurance status of HIV-infected adults in the post-HAART era: evidence from the United States. Applied Health Economics and Health Policy 2(1):85–91.
Golub ET, Astemborski JA, Hoover DR, Anthony JC, Vlahov D, Strathdee SA. 2003. Psychological distress and progression to AIDS in cohort of injection drug users. Journal of Acquired Immune Deficiency Syndromes 32(4):429–434.
Harrigan PR, Dong WY, Alexander C, Yip B, Ting L, Wynhoven B, Woodward J, Mo T, Hogg R, Montaner J. 2003. The association between drug resistance and adherence determined by two independent methods in a large cohort of drug naïve individuals starting triple therapy. The 2nd International AIDS Society Conference on HIV Pathogenesis and Treatment. Abstract no. LB12. [Online]. Available: http://www.ias.se/abstract/show.asp?abstract_id=11066 [accessed September 28, 2003].
Hays RD, Cunningham WE, Sherbourne CD, Wilson IB, Wu AW, Cleary PD, McCaffery DF, Fleischman JA, Crystal S, Collins R, Eggan F, Shapiro MF, Bozzette SA. 2000. Health-related quality of life in patients with human immunodeficiency virus infection in the United States: results from the HIV Cost and Services Utilization Study. American Journal of Medicine 108:714–722.
Hirsch MS, Bru-Vezinet F, Clotet B, Conway B, Kuritzkes DR, D’Aquila RT, Demeter LM, Hammer SM, Johnson VA, Loveday C, Mellors JW, Jacobson DM, Richman DD. 2003. Antiretroviral drug resistance testing in adults infected with human immunodeficiency virus type 1:2003 recommendations of an International AIDS Society-USA Panel. Clinical Infectious Disease 37(1):113–128.
HRSA (Health Resources and Services Administration). 2001. Outcome Evaluation Technical Assistance Guide: Case Management Outcomes, Titles I and II of the Ryan White CARE Act. Rockville, MD: HRSA.
HRSA. 2002a. Title I: Grants to Eligible Metropolitan Areas. [Online]. Available: http://hab.hrsa.gov/programs/factsheets/title1fact.htm [accessed April 14, 2004].
HRSA. 2002b. Title II: AIDS Drug Assistance Program. [Online]. Available: http://hab.hrsa.gov/programs/factsheets/adap1.htm [accessed April 14, 2004].
HRSA. 2002c. Title II: Grants to States and Territories [Online]. Available: http://hab.hrsa.gov/programs/factsheets/titleiifact.htm [accessed April 14, 2004].
HRSA. 2002d. Title III: Capacity Building Grant Program. [Online]. Available: http://hab.hrsa.gov/programs/factsheets/titleiiicap.htm [accessed April 14, 2004].
HRSA. 2002e. Title IV Services or Women, Infants, Children, Youth, and their Families. [Online]. Available: http://hrsa.gov/hab/titleiv.htm [accessed April 14, 2004].
HRSA. 2002f. Dental Reimbursement Program. [Online]. Available: http://hab.hrsa.gov/programs/factsheets/drpfact.htm [accessed April 14, 2004].
HRSA. 2002g. AIDS Education and Training Centers Program. [Online]. Available: http://hab.hrsa.gov/programs/factsheets/aetc.htm [accessed April 14, 2004].
HRSA. 2002h. Special Projects of National Significance Program. [Online]. Available: http://hab.hrsa.gov/programs/factsheets/spnsfact.htm [accessed April 14, 2004].
HRSA. 2002j. Ryan White CARE Act Annual Administrative Report 2000: Title I, Title II, AIDS Drug Assistance Program, Health Insurance Program. Rockville, MD: HRSA.
HRSA. 2003a. Ryan White CARE Act Appropriations for Fiscal Years 1991-2003. [Online]. Available: ftp://ftp.hrsa.gov/hab/findinghis03.xls. [accessed April 14, 2004].
HRSA. 2003b. HRSA CARE ACTION: Prevention Is Treatment: Prevention with Positives in Clinical Care. [Online]. Available: ftp://ftp.hrsa.gov/hab/march2003.pdf [accessed April 27, 2004].
HRSA. 2003c. Title I Manual. [Online]. Available: http://hab.hrsa.gov/tools/title1/ [accessed October 29, 2003].
HRSA. 2003d. Title II Manual. [Online]. Available: http://hab.hrsa.gov/tools/title2/ [accessed October 29, 2003].
Hsu JH. 2002. Substance Abuse and HIV. The Hopkins HIV Report. [Online]. Available: http://www.Hopkins-aids.edu/publications/report/july02_5.html [accessed April 14, 2004].
Ickovics JR, Hamburger ME, Vlahov D, Schoenbaum BE, Schuman P, Boland RJ, Moore J, HIV Epidemiology Research Study Group. 2001. Mortality, CD4 cell count decline, and depressive symptoms among HIV-seropositive women: longitudinal analysis from the HIV Epidemiology Research Study. Journal of the American Medical Association 285(11):1466–1474.
IOM (Institute of Medicine). 1996. Primary Care: America’s Health in a New Era. Donaldson MS, Yordy KD, Lohr KN, Vaneslow NA, eds. Washington, DC: National Academy Press.
IOM. 1999. Reducing the Odds: Preventing Perinatal Transmission of HIV in the United States. Stoto MA, Almario DA, McCormick MC, eds. Washington, DC: National Academy Press.
IOM. 2001. No Time to Lose: Getting More from HIV Prevention. Ruiz MS, Gable AR, Kaplan EH, Stoto MA, Fineberg H, Trussell J, eds. Washington, DC: National Academy Press.
Kaiser Commission on Medicaid and the Uninsured. 2001. Medicaid: A Primer. Washington, DC: Henry J. Kaiser Family Foundation.
KFF (Kaiser Family Foundation). 2004. Medicare: Medicare at a Glance. Washington, DC: Kaiser Family Foundation.
Kalichman SC, Rompa D, Cage M, DiFonzo K, Simpson D, Austin J, Luke W, Buckles J, Kyomugisha F, Benotsch E, Pinkerton S, Graham J. 2001. Effectiveness of an intervention to reduce HIV transmission risks in HIV-positive people. American Journal of Preventive Medicine 21(2):84–92.
Kates J. 2004. Financing HIV/AIDS Care: A Quilt with Many Holes. Paper prepared for the Committee on Public Financing and Delivery of HIV Care, Institute of Medicine. Washington, DC: Kaiser Family Foundation.
Kates J, Levi J, Neal J, Gallagher K. 2002. Learning more about the HIV-infected population not in care in the United States: using public health surveillance data to inform current policy challenges in enhancing access. Poster TuPeG 5690, XIV International AIDS Conference, Barcelona, Spain.
Katz MH, Cunningham WE, Fleishman JA, Andersen RM, Kellogg T, Bozzette SA, Shapiro MF. 2001. Effect of case management on unmet needs and utilization of medical care and medications among HIV-infected persons. Annals of Internal Medicine 135(8 Pt. 1):557–565.
Keiser P, Nassar N, Kvanli MB, Turner D, Smith JW, Skiest D. 2001. Long-term impact of highly active antiretroviral therapy on HIV-related health care costs. Journal of Acquired Immune Deficiency Syndromes and Human Retrovirology. 27:14–19.
Laine C, Markson LE, McKee LJ, Hauck WW, Fanning TR, Turner BJ. 1998. The relationship of clinical experience with advanced HIV and survival of women with AIDS. AIDS 12(4):417–424.
Lubinski C, Weddle A, Grayer C. 2002. Medicaid Financing of HIV care: An Analysis of Five State Programs. Paper prepared for the Committee on the Public Financing and Delivery of HIV Care, Institute of Medicine. Washington, DC: Unpublished.
Lucas GM, Gebo KA, Chaisson RE, Moore RD. 2002. Longitudinal assessment of the effects of drug and alcohol abuse on HIV-1 treatment outcomes in an urban clinic. AIDS 16(5):767–774.
Magnus M, Schmidt N, Brown B, Kissinger PJ. 2002. A profile of an HIV- and child-specific programme in New Orleans, Louisiana, USA. AIDS Care 14(Suppl. 1):85–94.
Margolin A, Avants SK, Warbourton LA, Hawkins KA, Shi J. 2003. A randomized clinical trial of a manual-guided risk reduction intervention for HIV-positive injection drug users. Health Psychology 22(2):223–228.
Markson L, Houchens R, Fanning TR, Turner BJ. 1998. Repeated emergency department use by HIV infected persons: effect of clinic accessibility and expertise in HIV care. Journal of Acquired Immune Deficiency Syndromes 17(1):35–41.
McKinney MM, Marconi KM. 2002. Delivering HIV services to vulnerable populations: A review of CARE Act-funded research. Public Health Reports 117:99–113.
McNabb J, Ross JW, Abriola K, Turley C, Nightingale CH, Nicolau DP. 2001. Adherence to highly active antiretroviral therapy predicts virologic outcome at an inner-city human immunodeficiency virus clinic. Clinical Infectious Diseases 33(5):700–705.
Messeri PA, Abramson DM, Aidala AA, Lee F, Lee G. 2002. The impact of ancillary HIV services on engagement in medical care in New York City. AIDS Care 14(Suppl. 1):15–29.
Moore RD. 2000. Cost effectiveness of combination HIV therapy: 3 years later. Pharmacoeconomics 17(4):325–330.
NIH (National Institutes of Health). 1997. Interventions to Prevent HIV Risk Behaviors. NIH Consensus Statement. [Online]. Available: http://consensus.nih.gov/cons/104/104_statement.htm [accessed April 27, 2004].
Otto-Salaj LL, Stevenson Y. 2001. Influence of psychiatric diagnoses and symptoms on HIV risk behavior in adults with serious mental illness. AIDS Reader 11(4):197–208.
Palepu A, Tyndall M, Yip B, O’Shaughnessy MV, Hogg RS, Montaner JSG. 2003. Impaired virologic response to highly active antiretroviral therapy associated with ongoing injection drug use. Journal of Acquired Immune Deficiency Syndromes 32(5):522–526.
Paterson DL, Swindells S, Mohr J, Brester M, Vergis EN, Squier C, Wagener MM, Singh N. 2000. Adherence to protease inhibitor therapy and outcomes in patients with HIV infection. Annals of Internal Medicine 133(1):21–30.
Pernice C, Wysen K, Riley T, Kaye N. 2001. Charting SCHIP: Report of the Second National Survey of the State Children’s Health Insurance Program. Portland, ME: National Academy for State Health Policy.
Pollitz K, Tapay N, Hadley E, Specht J. 2000. Early experience with ‘new federalism’ in health insurance regulation. Health Affairs 19(4):7–22.
SAMHSA (Substance Abuse and Mental Health Services Administration). 1997. HIV/AIDS: Initial findings from the field. Information Center Bulletin 1(1). National Mental Health Information Center. [Online]. Available: http://www.mentalhealth.org/publications/allpubs/KEN96-0040/ken96-0040-05.asp [accessed May 7, 2004].
Schietinger H, Schecter C. 1998. Medical Coverage for Medicare Beneficiaries with HIV/AIDS: Issues and Implications. Washington, DC: Academy for Educational Development.
Shapiro MF, Morton SC, McCaffrey DF, Senterfitt JW, Fleishman JA, Perlman JF, Athey LA, Keesey JW, Goldman DP, Berry SH, Bozzette SA. 1999. Variations in the care of HIV-infected adults in the United States: results from the HIV Cost and Services Utilization Study. Journal of the American Medical Association 281(24):2305–2315.
Sherer R, Stieglits K, Narra J, Jasek J, Green L, Moore B, Short S, Cohen M. 2002. HIV multidisciplinary teams work: support services improve access to and retention in HIV primary care. AIDS Care 14(Suppl. 1):31–44.
SSA (Social Security Administration). 2004. Supplemental Security Income (SSI): understanding Supplemental Security Income if You are Disabled or Blind. [Online]. Available: http://www.ssa.gov/notices/supplemental-security-income/text-disable-ussi.htm [accessed February 3, 2004].
Starace F, Anmassari A, Trotta MP, Murri R, Dc Longis P, Izzo C, Sca A, d’Arminio Monforte A, Wu AW, Antinori A; Ad Study Group; NeurolCoNa Study Group. 2002. Depression is a risk factor for suboptimal adherence to highly active antiretroviral therapy. Journal of Acquired Immune Deficiency Syndrome 31(Suppl 3):S136–S139.
Staszewski S, Morales-Ramires J, Tashima KT, Rachlis A, Skiest D, Stanford J, Stryler R, Johnson P, Labriola DF, Farina, D Manion DJ, Ruiz N, for the Study 006 Team. 1999. Efavirenz plus Zidouvudine and Lamivudine, Efavirenz plus Indavir, and Indavir plus Zidovudine and Lamivudine in the treatment of HIV-1 infection in adults. New England Journal of Medicine 341(25):1865–1873.
Sternhell PS, Corr MJ. 2002. Psychiatric morbidity and adherence to antiretroviral medication in patients with FHV/AIDS. Australian & New Zealand Journal of Psychiatry 36(4): 528–533.
Tucker JS, Burnarn MA, Sherbourne CD, Kung FY, Gifford AL. 2003. Substance use and mental health correlates of nonadherence to antiretroviral medications in a sample of patients with human immunodeficiency virus infection. American Journal of Medicine 114(7):573–580.
U.S. Preventive Services Task Force. 1996. Guide to Clinical Preventive Services. 2nd ed. Washington, DC: U.S. Department of Health and Human Services.
U.S. Public Health Service Task Force. 2003. Recommendations for Use of Antiretroviral Drugs in Pregnant HIV-1-Infected Women for Maternal Health and Interventions to Reduce Perinatal HIV-1 Transmission in the United States. Washington, DC: U.S. Department of Health and Human Services.
U.S. Public Health Service Task Force and Infectious Diseases Society of America. 2001. Guidelines for the Prevention of Opportunistic Infections in Persons Infected with HIV. Washington, DC: U.S. Department of Health and Human Services.
Vernazza PL, Eron JJ, Fiscus SA, Cohen MS. 1999. Sexual transmission of HIV: infectiousness and prevention. AIDS 13(2):155–166.
Westmoreland T. 1999. Medicaid and HIV/AIDS Policy: A Basic Primer. Washington, DC: Henry J. Kaiser Family Foundation.
WGATMM (Working Group on Antiretroviral Therapy and Medical Management of HIV-Infected Children). 2004, January 20. Guidelines for the Use of Antiretroviral Agents in Pediatric HIV Infection. [Online]. Available: http://aidsinfo.nih.gov/guidelines/pediatric/PED_012004.pdf [accessed April 15, 2004].