6
Local Communities
Prevention of obesity in children and youth is, ultimately, about community—extending beyond individuals and families and often beyond geographic boundaries to encompass groups of people who share values and institutions (Pate et al., 2000). In recent years, many public health professionals and community leaders have recognized the need for community involvement in preventing disease and promoting healthful lifestyles. Consequently, they have attempted to capitalize on the naturally occurring strengths, capacities, and social structures of local communities to institute health-promoting change.
Many factors in the community setting affect the health of children and youth. Does the design of the neighborhood encourage physical activity? Do community facilities for entertainment and recreation exist, are they affordable, and do they encourage healthful behaviors? Can children pursue sports and other active-leisure activities without excessive concerns about safety? Are there tempting-yet-healthful alternatives to staying-at-home sedentary pastimes such as watching television, playing video games, or browsing the Internet? Are sound food choices available in local stores and at reasonable prices?
Communities can consist of people living or working in particular local areas or residential districts; people with common ethnic, cultural, or religious backgrounds or beliefs; or people who simply share particular interests. But intrinsic to any definition of a community is that it seeks to protect for its members what is shared and valued. In the case of obesity prevention in children and youth, what is “shared and valued” is the ability of children
to grow up with healthy and productive bodies and minds. But “to protect” is not necessarily a given. Achieving the vision of Healthy People 2010—“healthy people in healthy communities”—depends on the capacity of communities to foster social norms that support energy balance and a physically active lifestyle (DHHS, 2000b).
This report as a whole examines a variety of types of communities and the ways in which improvements can be made in order to foster and promote healthful food and physical activity choices and behaviors. This chapter focuses on the local community, using the term “community” to refer to the town, city, or other type of geographic entity where people share common institutions and, usually, a local government. Of course, within each local community there are many interdependent smaller networks of residential neighborhoods, faith-based communities, work communities, and social communities.
The intent of this chapter’s recommendations is not only to make a case for raising the priority of childhood obesity prevention in our communities, but also to identify common interests that can spark collaborative community initiatives for addressing that goal. Many communities and organizations across the United States are actively working to address physical activity and nutrition-related issues; examples are highlighted throughout the chapter (Boxes 6-1 through 6-5).
MOBILIZING COMMUNITIES
By stepping outside the traditional view of obesity as a medical problem, we may more fundamentally focus on the many institutions, organizations, and groups in a community that have significant roles to play in making the local environment more conducive to healthful eating and physical activity. Table 6-1 illustrates categories of many of the stakeholder groups that could be involved in obesity prevention efforts. For community efforts, key stakeholders include youth organizations, social and civic organizations, faith-based groups, and child-care centers; businesses, restaurants, and grocery stores; recreation and fitness centers; public health agencies; city planners and private developers; safety organizations; and schools.
Community-based obesity prevention efforts differ from those of school and home settings (Pate et al., 2000), but potentially supplement and reinforce the messages received in those settings. Young people, particularly adolescents, often spend a large part of their free time in community locales (e.g., recreational or entertainment centers, shopping areas, parks, fast food restaurants). These informal settings, which do not have the stresses of grades or other school situations, may offer environments that are more conducive to trying new activities and foods. Additionally, community settings offer the potential for involving parents and other adult role models in
TABLE 6-1 Examples of Stakeholder Groups in the Prevention of Childhood Obesity
|
Children, Youth, Parents, Families |
|
Child- and Youth-Centered Organizations Program, service, and advocacy organizations (e.g., Boys and Girls Clubs, 4H, Girl Scouts, Boy Scouts, YMCA, YWCA, National Head Start Association, Children’s Defense Fund, National Association for Family Child Care) |
|
Community-Based Organizations Community coalitions, civic organizations, faith-based organizations, ethnic and cultural organizations |
|
Community Development and Planning Architects, civil engineers, transportation and community planners, private developers, neighborhood associations |
|
Employers and Work Sites Employers and corporate policy makers, employee advisory committees |
|
Food and Beverage Industries, Food Producers, Advertisers, Marketers, and Retailers Corporate and local food producers and retailers (e.g., food and beverage industries, grocery stores, supermarkets, restaurants, fast food outlets, corner stores, farmers’ markets, community gardens) |
|
Foundations and Nonprofit Organizations Government Agencies and Programs Federal, state, county, and local elected or appointed decision-makers (e.g., education boards and agencies, public health agencies, parks and recreation commissions, planning and zoning commissions, law enforcement agencies) |
|
Health-Care Providers Pediatricians, family physicians, nurses and nurse practitioners, physician assistants, dietitians, occupational-health providers, dentists |
|
Health- and Medical-Care Professional Societies Disciplinary organizations and societies |
|
Health-Care Delivery Systems Hospitals, health clinics, school-based facilities, work-site health facilities |
|
Health-Care Insurers, Health Plans, and Quality Improvement and Accrediting Organizations Public and private health-care providers and insurance reimbursement institutions such as Medicaid and health maintenance organizations; quality improvement and accrediting organizations (e.g., National Committee for Quality Assurance) |
|
Mass Media, Entertainment, Recreation, and Leisure Industries Television, radio, movies, print, and electronic media; journalists; commercial sponsors and advertisers; Internet websites and advertisers; computer and video-entertainment industry representatives |
|
Public Health Professionals |
|
Recreation and Sports Enterprises Local, collegiate, and professional sports organizations; recreation facilities; recreation and sport equipment manufacturers, advertisers, marketers, and retailers |
|
Researchers Biomedical, public health, and social scientists; universities; private industry |
|
Schools, Child-Care Programs Educators and school administrators, food service personnel, after-school program providers, coaches, school boards, school designers (siting and construction), child-care providers |
promoting healthful behaviors (Pate et al., 2000). In enhancing local assets for promoting physical activity—that is, in designing and revamping community facilities and neighborhoods—communities should consider issues related to cultural and social acceptability, availability (proximity), affordability, and accessibility (ease of use).
Community Stakeholders and Coalitions
Community-Based Interventions: Framework and Evidence Base
“Ecological frameworks,” which have been applied across a variety of settings and public health issues to change people or change the environment (Glanz, 1997), suggest that it is important to involve individuals, organizations, communities, and health policy makers in producing desired effects on health (Baker and Brownson, 1998). Given the interactive nature of virtually all elements of a community, most effective interventions act at multiple levels. Moreover, tapping a wide range of local community leaders, organizations, businesses, and residents can result in local ownership of the issue and effectively leverage limited resources (Pate et al., 2000).
Community-wide campaigns and interventions. The most relevant evidence for large-scale community-wide efforts comes from studies aimed at reducing cardiovascular risk factors through dietary change and increased physical activity. These interventions have often used multiple strategies, including media campaigns (see Chapter 5), community mobilizations, education programs for health professionals and the general public, modifications of physical environments, and health screenings and referrals; in some cases, home- and school-based interventions were also incorporated (Shea and Basch, 1990).
The Stanford Three Community Study, Stanford Five-City Project, Minnesota Heart Health Program (MHHP), Pawtucket Heart Health Program, and North Karelia Project (in Finland) have demonstrated the feasibility of community-based approaches in promoting physical activity and changes in dietary intake (Farquhar et al., 1977, 1990; Maccoby et al., 1977; Luepker et al., 1994; Young et al., 1996; Puska et al., 2002). The results of these studies for adults have been somewhat inconsistent, although modest positive changes in diet and physical activity have generally been seen when a community that received the intervention was compared with one that had not. The strongest positive results were obtained by the extensive North Karelia project, which examined the effects of multiple interventions on the high incidence of coronary artery disease (Pietinen et
al., 2001; Puska et al., 2002). This study, being long-term and multifocal, may be the best model for childhood obesity prevention efforts.
MHHP’s Class of 1989 Study provides some insights into the potential impact of community-based programs focused on children and youth (Kelder et al., 1993, 1995). This study examined changes in nutrition and aerobic activity among groups of students, starting when they were sixth-graders and extending through 12th grade. Interventions included a school-based curriculum and a number of other community-based approaches that were not designed specifically for children (including labeling of heart-healthful restaurant and grocery store items; media campaigns; and screening for heart disease risk factors). Positive changes were seen in the young people’s levels of physical activity and their nutritional knowledge and decision-making.
Community campaigns aimed at preventing tobacco use by children and youth also provide evidence of the feasibility of using this approach for addressing major public health problems. The Midwestern Prevention Project, the North Karelia Youth Project, and MHHP’s Class of 1989 Study each found reductions in youth smoking rates that were maintained over time (IOM, 1994). It should be stressed that each of these studies had a strong school-based prevention intervention that complemented a community-wide program, and isolating the effects of the community-wide program was not possible.
Community programs for children and youth. Programs involving specific community-based organizations have also been found to aid health promotion efforts. Studies with civic, faith-based, and social organizations have established the feasibility of developing programs in a variety of settings that can be effective in improving nutritional knowledge and choices, increasing physical activity, and in some cases in reducing body weight or
|
BOX 6-1 Girls on the Run Girls on the Run is a nonprofit organization that works with local volunteers and community-level councils to encourage preteen girls to develop self-respect and healthful lifestyles through running (Girls on the Run, 2004). A 12-week, 24-lesson curriculum has been developed for use in after-school programs and at recreation centers and other locations. Evaluation of the program has found improvements in participants’ self-esteem, body-size satisfaction, and eating attitudes and behaviors (DeBate, 2002). |
maintaining healthy body weight (IOM, 2003). For example, Cullen and colleagues (1997) found that Girl Scouts who participated with their troop in nutrition classes including tasting sessions and materials sent home exhibited increased levels of fruit and vegetable consumption. Furthermore, community programs often are focused on high-risk populations and offer the opportunity to implement culturally appropriate interventions and evaluate their impact (Yancey et al., 2004).
Community coalitions. Building coalitions involves a range of public- and private-sector organizations that, together with individual citizens, focus on a shared goal and leverage the resources of each group through joint actions (Table 6-2). It has been pointed out, however, that while the strength of
TABLE 6-2 Unique Characteristics of Effective Community Coalitions
|
Characteristic |
Description |
|
Holistic and comprehensive |
Allows the coalition to address issues that it deems as priorities; well illustrated in the Ottawa Charter for Health Promotion |
|
Flexible and responsive |
Coalitions address emerging issues and modify their strategies to fit new community needs |
|
Build a sense of community |
Members frequently report that they value and receive professional and personal support for their participation in the social network of the coalition |
|
Build and enhance resident |
A structure is provided for renewed civic engagement in community life engagement; the coalition becomes a forum where multiple sectors can engage with each other |
|
Provide a vehicle for community empowerment |
As community coalitions solve local problems, they develop social capital, allowing residents to have an impact on multiple issues |
|
Allow diversity to be valued and celebrated |
As communities become increasingly diverse, coalitions provide a vehicle for bringing together diverse groups to solve common problems |
|
Incubators for innovative solutions to large problems |
Problem solving occurs not only at local levels, but at regional and national levels; local leaders can become national leaders |
|
SOURCE: Adapted from Wolff, 2001. |
|
coalitions is in mobilizing the community to work for change, they are not generally designed to develop or manage specific community services or activities (Chavis, 2001).
Community collaborative efforts focused on health are of growing interest across the United States. Models are being refined on ways to link community organizations, community leaders and interested individuals, health-care professionals, local and state public health agencies, and universities and research organizations (Lasker et al., 2001; Lasker and Weiss, 2003). Community coalitions have played significant roles in efforts to prevent or stop tobacco use. The American Stop Smoking Intervention Study (ASSIST), which was funded by the National Cancer Institute and featured the capacity building of community coalitions, targeted tobacco control efforts at the state and local levels. States with ASSIST programs had greater decreases in adult smoking prevalence than non-ASSIST states (Stillman et al., 2003); factors identified as contributing to participation and satisfaction with the ASSIST coalitions included skilled members and effective communication strategies (Kegler et al., 1998). Coalition building and community involvement also have been effective in community fluoridation efforts (Brumley et al., 2001).
Health Disparities
Although this report focuses primarily on population-wide approaches that have the potential to improve nutrition and increase physical activity among all children and youth, the committee recognizes the additional need for specific preventive efforts. Children and youth in certain ethnic groups including African-American, Mexican-American, American-Indian, and Pacific Islander populations, as well as those whose parents are obese and those who live in low-income households or neighborhoods, are disproportionately affected by the obesity epidemic (Chapter 2). Many issues—including safety, social isolation, lack of healthy role models, limited access to food supplies and services, income differentials, and the relative unavailability of physical activity opportunities—may be barriers to healthier lifestyles for these and other high-risk populations. Moreover, as discussed in Chapter 3, perceptions about body image and healthy weight can vary between cultures and ethnic groups, and these groups can manifest differing levels of comfort with having an elevated weight. Furthermore, there may be a “communication gap” in making information about the health concerns of childhood obesity widely available.
As a result, culturally appropriate and targeted intervention strategies are needed to reach high-risk populations. There are examples of these types of strategies having positive results. For example, a 10-county study of churches participating in the North Carolina Black Churches United for
Better Health project found that church-based interventions (including group activities, changes in food served at church events, and dissemination of educational materials) resulted in increased fruit and vegetable consumption by adults participating in the intervention (Campbell et al., 1999). Pilot studies from the Girls Health Enrichment Multi-site Study (GEMS), a research program designed to develop and test interventions for preventing overweight and obesity in African-American girls, have included a variety of community, after-school, and family-based components in a range of settings (Baranowski et al., 2003; Beech et al., 2003; Robinson et al., 2003; Story et al., 2003). For example, the Stanford GEMS pilot study in 61 families tested a model that combined after-school dance classes for girls with family-based efforts to reduce time spent watching television. Positive trends were observed regarding body mass index (BMI), waist circumference, physical activity, and television viewing in the treatment group when compared to the control group (Robinson et al., 2003). These studies demonstrate the feasibility of implementing relevant community programs; two of these studies have been expanded to evaluate programs with larger study populations over a 2-year period (Kumanyika et al., 2003).
However, much remains to be learned about interventions that can reduce or alleviate the risk factors for childhood obesity in high-risk populations. Prevention efforts must be considerate of culture, language, and inequities in social and physical environments (PolicyLink, 2002). Furthermore, because these populations traditionally have been disenfranchised, special efforts must be made to gain their trust, both among individuals and at the community level. The 39-community Partnership for the Public’s Health project in California and other community-centered public health initiatives have demonstrated that the most progress is made when an intervention engages community members themselves in the program’s assessment, planning, implementation, and evaluation (Partnership for the Public’s Health, 2004).
Private and public efforts that work to eliminate health disparities should include obesity prevention as one of their primary areas of focus. Some of the many ongoing efforts span the public and private sectors as well as the local, regional, state, and national levels and focus on diabetes and other chronic diseases for which obesity is a risk factor. For example, the Centers for Disease Control and Prevention’s (CDC’s) REACH 2010 initiative has broad-based collaboration within the U.S. Department of Health and Human Services (DHHS) and the private sector (CDC, 2004b) to fund and support demonstration projects and community coalitions focused on eliminating health disparities. Each coalition includes community-based organizations and the local or state health department or a university or research organization. Efforts to date have included community and tribal efforts to address diabetes and cardiovascular disease risk factors.
These efforts should aim to increase access to culturally and linguistically appropriate nutritional and physical activity information and skills and should support community-based collaborative programs that address the inequities in obesity rates between populations.
The communities themselves, meanwhile, need to involve all segments of the local population in developing both community-wide interventions and those that focus on high-risk populations. Furthermore, local communities—with the assistance of state and federal governments, nonprofit organizations, and the private sector—need to grapple with the underlying and long-standing socioeconomic barriers that result in limited opportunities for physical activity (e.g., safe parks and playgrounds) and affordable healthful foods (e.g., produce markets or large grocery stores). Opportunities to foster such coalitions and to develop effective programs for high-risk populations will be widened if there is grassroots participation by the citizens most affected by the problem.
Next Steps for Community Stakeholders
Many community organizations are currently involved in efforts to improve the well-being of their children and youth regarding a number of health and safety concerns, such as tobacco and alcohol abuse, sexually transmitted diseases, pedestrian and bike safety, and prevention of motor
|
BOX 6-2 Kids Off the Couch Kids Off the Couch is a community collaborative pilot project in Modesto, California, that works with parents and caregivers to prevent obesity in children up to 5 years of age. The project’s goal is to influence behavioral changes in food selection and physical activity among parents and primary caregivers. The program provides parents and caregivers with:
This project is a collaborative effort of numerous partners including the local school system, health services agency, hospitals, and health clubs; the American Cancer Society; Blue Cross of California; and the University of California Cooperative Extension. |
vehicle injuries. Increased media coverage and the voices of concerned individuals and groups should now be prompting these community groups and others, including the broad range of stakeholders they work with, to focus on childhood obesity prevention. In particular, there is a need to galvanize action and expand opportunities for healthful eating and physical activity at the community level.
Community youth organizations can have an impact not only by adapting their own programs to include emphasis on healthful eating and physical activity, but also by joining with other organizations to form coalitions to promote community-wide efforts. Additionally, innovative approaches to community recreational programs are needed. Traditional organized competitive sports programs are an important facet of the community and offer physical activity opportunities for many children and adolescents. However, competitive sports programs are not of interest to all individuals and it is important to expand the range of options to include not only team and individual sports but also other types of physical activity (e.g., dance, martial arts) (CDC, 1997b). It will also be important to help families overcome potential obstacles—including transportation, fees, or special equipment—to program participation (CDC, 1997b).
Community youth organizations (such as Boys and Girls Clubs, Girls Scouts, Boy Scouts, 4H, and YMCA) should expand existing programs and establish new ones that widen children’s opportunities to be physically active and maintain a balanced diet. These programs should complement and seek linkages with similar efforts by schools, local health departments, and other community organizations. Furthermore, evaluation of these programs should be encouraged.
Employers and work sites are another important component of community coalitions. The work site affects children’s health both indirectly, through its influence on employed parents’ health habits, and directly, through programs that may engage the entire family. Workplaces should offer healthful food choices and encourage physical activity. In businesses where on-site child care is provided, attention should be paid to ensuring that children have a balanced diet and adequate levels of physical activity.
Local organizations, businesses, local public health agencies, and other stakeholders increasingly have been joining together to address health issues through community coalitions, wherein the sum is greater than the parts, and meaningful progress on an issue becomes more likely. Coalitions can make obesity prevention a local priority and can design and implement programs that best fit the local area. It is important for coalitions to be inclusive, promote broad involvement, and represent as many constituencies as possible (see Table 6-2). As coalitions become established, it is also important for them to periodically reassess their status to ensure they remain inclusive and do not outlive their usefulness. Because of their nature,
coalitions exhibit wide variation in their structure and in the range of organizations, agencies, and individuals involved. However, to be sustained all require strong and ongoing leadership that is selected by coalition members.
Communities should establish and promote coalitions of key public and private stakeholders (including community youth organizations, local government, state and local public health agencies, civic and community groups, businesses, faith-based groups) to address the problem of childhood obesity by increasing the opportunities for physical activity and a balanced diet. Partnering with academic centers will be important for community-based research.
To have a long-term and significant impact on the public’s health, community health initiatives should include programs that work towards initiating changes at many levels including changes in individual behaviors, family environments, schools, workplaces, the built environment, and public policy (Kaiser Permanente, 2004). This ecologic approach (see Chapter 3) is a critical part of a framework for community-level initiatives that support a health-promoting environment. Communities should seek to undertake a comprehensive, interrelated set of interventions operating at each ecological level and in multiple sectors and settings. Factors that have been found to be involved in sustaining successful community change efforts include a large number of environmental changes focused on a small number of categorical outcomes; intensity of behavior change strategy; duration of interventions; and use of appropriate channels of influence to reach appropriate targets (Fawcett et al., 2001).
Community-level approaches are among the most promising strategies for closing the disparities gap (PolicyLink, 2002; Prevention Institute, 2002). These strategies include improvements in the social and economic environment (e.g., through the creation of health-promoting social norms, economic stability, and social capital development), the physical environment (e.g., access to affordable healthful food and physical activity resources), and community services (e.g., after-school programs) (Prevention Institute, 2003). The goals of improving community health and addressing racial and ethnic health disparities are closely aligned.
The committee acknowledges the limited amount of empirical research that directly examines the effects of changes in community programs or formation of coalitions on obesity prevalence. However, interventions such as GEMS demonstrate the feasibility of these interventions, and the experience gained in other public health areas provides additional support for recommendations in these areas. As with other types of obesity prevention interventions (noted throughout this report), there is a critical need to ensure that community intervention programs are thoroughly evaluated. The impacts of coalitions have sometimes gone undetected because of inap-
propriate (or weak) evaluation plans. This is most likely to occur when (1) the evaluation timeline is too short, (2) the evaluation strategy focuses on unrealistic or distant health outcomes instead of intermediate indicators that can be influenced by coalition activity, (3) measures are incapable of detecting valid indicators of change, or (4) alternative explanations for effects are not taken into account (Kreuter and Lezin, 2002). In order to assess a community coalition’s level of change, and to allow communities elsewhere to profit from its experience (good, bad, or in between), realistic evaluation plans must be set up and be incorporated into the initial planning and implementation of coalitions and interventions. Ongoing evaluation that relies on learning and feedback is also an integral component of the community change process. Community health initiatives by their nature are confronted with unpredictable variables; feedback should be used to adjust subsequent efforts.
The standard of practice in comprehensive community health improvement efforts is to fully engage community organizations and community residents, not just as subjects of research but as the drivers and owners of evaluation—“community-based participatory research” (Minkler and Wallerstein, 2003). Using this approach, community members are involved in identifying and framing of the problem or goals; developing a logic model or framework for achieving success; identifying research questions and appropriate research methods; documenting the intervention and its effects; understanding the data; and using the data to make midcourse adjustments (Fawcett et al., 2004).
To provide the impetus for community programs and efforts, a coordinated network of community-based demonstration projects should be established. These projects would be run by community organizations linked with public health departments and in partnership with academic institutions to provide support, training, and evaluation. Seed funding for the projects could come from an expansion of federal programs, particularly CDC’s state-based Nutrition and Physical Activity Program to Prevent Obesity and Other Chronic Diseases (see Chapter 4) and the DHHS Steps to a Healthier U.S. initiative.
Built Environment
Designing Communities and Neighborhoods to Encourage Physical Activity
Communities should provide places where children can play outside, particularly within their residential neighborhoods, and where they can safely walk, bike, or travel by other self-propelled means to destinations such as the park, playground, or school. Hoefer and colleagues (2001)
found that local neighborhood and parks were the most frequent settings for physical activity among middle school students. Three studies of young children found that the amount of time a child spent outside was the most powerful correlate of his or her physical activity level (Klesges et al., 1990; Baranowski et al., 1993; Sallis et al., 1993). However, pedestrian injuries that result from collisions with automobiles are a leading cause of injury death for children aged 5 years and older (Grossman, 2000), and traffic speed is a key determinant of their injury risk (Jacobsen et al., 2000). The challenge is thus to create places where children are safe to walk, bike, and play, so that the benefits of increased physical activity are not offset by increases in injuries.
Because changes to the built environment can enhance opportunities for children and youth to safely play outside and be more physically active, such changes are a critical component of any action plan to prevent childhood obesity. Interest in the role of the built environment in determining levels of physical activity has grown over the past decade, and renewed efforts are currently under way to reconnect the goals of urban planning and public health and to identify the factors that influence physical activity and travel behavior (Handy et al., 2002; Hoehner et al., 2003; Corburn, 2004). A concurrent study by the Transportation Research Board is examining issues regarding transportation, land use, and health in greater depth than this report, though for the population as a whole.
Encouraging children and youth to be physically active involves providing them with opportunities to walk, bike, run, skate, play games, or engage in other activities that expend energy. However, in many neighborhoods children do not have safe places—because of vehicular traffic, or high crime rates, or both—in which to play outside. In other locales, children may lack adequate sidewalks or paths on which to bike, skate, or simply walk to local destinations such as schools, parks, or grocery stores. This is a result of regulations and practices that guide the development of transportation systems and design of neighborhoods. The needs of the car have often been emphasized over the needs of pedestrians and bicyclists.
A recently published observational study examined the associations between community physical activity-related settings (e.g., sports areas, public pools and beaches, parks and green space, and bike paths) and race, ethnicity, and socioeconomic status in 409 communities throughout the United States (Powell et al., 2004). The researchers found that higher median household income and lower poverty rates were associated with increasing levels of available physical activity-related facilities and settings. Communities with higher proportions of ethnic minorities had fewer physical activity-related settings. There are many communities and neighborhoods where access to facilities for physical activity is an issue that needs to be addressed.
|
BOX 6-3 Discovering Public Spaces as Neighborhood Assets in Seattle Feet First, a Seattle-area nonprofit organization, is using its Active Living by Design grant from the Robert Wood Johnson Foundation to help neighborhood residents take a closer look at their streets. As part of their project’s activities, Feet First staff organize neighborhoods through monthly walking audits. On these walks, the staff train groups of up to 40 neighbors to see their streets as an untapped resource with potential for physical activity. At the end of the one-mile, two-hour inspections, participants receive notes with photos and maps documenting assets, possible improvements, and needed policy changes. The organization assists citizens in working with city agencies and departments to address the neighborhood concerns. Evaluation has been built into the design and implementation of the Feet First program and is now in progress. Results will be used to assess next steps and inform the planning of future programs. |
Correlational studies. Convenient access to recreational facilities emerges as a consistent correlate of physical activity, although most research has been conducted with adults (Sallis et al., 1998; Humpel et al., 2002). A 2002 review by Humpel and colleagues summarized the results of 16 cross-sectional studies, published between 1990 and 2001, on the link between physical activity and the physical environment. Access to facilities such as bicycle paths or parks showed significant positive associations with physical activity, while measures of a lack of facilities (or inadequate facilities) showed significant negative associations. Awareness of and satisfaction with facilities also showed significant associations with physical activity, as did measures of local aesthetics, such as attractive neighborhoods or enjoyable scenery.
Although there are fewer studies on the relationships between young people’s access to recreational facilities and their levels of physical activity, they are nevertheless consistent with the findings for adults. A comprehensive review by Sallis and colleagues (2000a) on the correlates of physical activity among children found a significant positive association with access to recreational facilities and programs, and two out of three studies involving adolescents found a significant positive association as well. However, a study of the neighborhoods of low-income preschoolers in Cincinnati, Ohio, found that overweight was not associated with proximity to playgrounds (Burdette and Whitaker, 2004). These results suggest that access to recreational facilities may be more important for youth than for young children or that reported physical activity may not always translate into differences in weight.
Available evidence (limited to the behavior of all residents or of adults
only) shows that the design of streets and neighborhoods is correlated with walking. A recent review of studies (Saelens et al., 2003) comparing “high-walkable” and “low-walkable” neighborhoods found that among persons aged 18 to 65 years, the frequency of walking trips was twice as high in the high-walkable locales. The high-walkable neighborhoods were characterized as those that had higher residential density, street connectivity (few cul-de-sacs), aesthetics, safety, and mixed land use (stores and services located within close proximity to residential areas).
Safety is often an important consideration in decisions by parents and children regarding outside activity. Safety concerns pertain to the speed and proximity of nearby traffic and to fears of crime; but other factors, such as unattended dogs and lack of street lighting, may also be pertinent. Research has shown that parents are more likely now than in the past to restrict their children’s use of public spaces because of fear for their safety (Loukaitou-Sideris, 2003). Concerns about “traffic danger” and “stranger danger” have been reported as important influences on the decisions by parents to drive their children to school or not allow them to walk to the neighborhood park (Roberts, 1993; DiGuiseppi et al., 1998); furthermore, parents report that safety considerations are the most important factor in selecting play spaces for their young children (Sallis et al., 1997).
Among adults, data from five states (Maryland, Montana, Ohio, Pennsylvania, and Virginia) document a higher level of physical inactivity among persons who perceive their neighborhoods to be unsafe (CDC, 1999). There also appear to be large gaps in neighborhood safety across socioeconomic groups. For example, a national study found that perception of neighborhood crime was almost twice as great among lower income populations as in higher income populations (Brownson et al., 2001). Thus, the crime rate, or the perception of crime, is likely to affect the likelihood of people walking or bicycling in their neighborhoods.
Studies on the link between neighborhood crime and rates of physical activity among children and youth have shown inconsistent results. Gordon-Larsen and colleagues (2000) studied a large adolescent cohort and found that living in a high-crime neighborhood was associated with a decreased likelihood that teenagers would participate in moderate-to-vigorous physical activity at high levels. However, a study by Zakarian and colleagues (1994) looking at physical activity among minority adolescents or children, who were predominantly of low socioeconomic status, found no association with convenient facilities or neighborhood safety; another study found no association between these factors and overweight (Burdette and Whitaker, 2004). On the other hand, Romero and colleagues (2001) studied fourth-grade students of diverse economic backgrounds and found that children from families of lower socioeconomic status perceived more neighborhood hazards (including crime and traffic), but that this percep-
tion was significantly associated with more reported physical activity rather than less. This finding points to a problem documented by others (Doxey et al., 2003): children from families with lower socioeconomic status are more dependent on walking as a means of transportation than are children from families with higher socioeconomic status, but they also live in neighborhoods where walking is not as safe.
Intervention studies. Research that directly examines the impact of changes made in the built environment on physical activity has been limited simply because increasing physical activity is often not the primary goal of these interventions and “pre-/post-” studies are difficult to conduct. Instead, changes to the built environment are often made because of safety concerns and the need to reduce the likelihood of traffic-related injuries. For example, the primary goal of traffic-calming programs—such as speed humps, traffic diverters, and “bulb-outs” (pavement structures that extend from the sidewalk at an intersection to force cars to take slower turns around corners)—has been to reduce speeds and to lower the levels of traffic on residential streets. Studies have been conducted of traffic levels and speeds, pedestrian-vehicle crashes, and pedestrian behavior both before and after the installation of traffic-calming devices (Huang and Cynecki, 2000, 2001; Retting et al., 2003). One recent study, for example, showed that speed humps were associated with a lower probability of children being injured within their neighborhood (Tester et al., 2004). However, no studies of the impact of the installation of such devices on the physical activity of residents in the area are available.
A small group of studies has used a pretest/posttest design to test the impact of a specific change to the built environment in a relatively limited area (e.g., street-scale interventions). Painter (1996) examined the impact of improved lighting on the use of footpaths in London and found an intervention effect ranging from 34 percent to 101 percent increases in footpath use, depending on the location. Similarly, a 23 percent increase in bicycle use was found with the addition of bike lanes (Macbeth, 1999). Researchers examining the impact of the redesign of two residential streets in Hannover, Germany, into “Woonerven” (designed for shared use by cars and people) observed 11 percent to 100 percent more children on the street and 53 percent to 206 percent more incidents of street play after the changes in street design (Eubanks-Ahrens, 1987).
The research needs in this area are many. Most obviously, future studies should determine the specific elements of the built environment that influence physical activity in children and youth. DHHS and the Department of Transportation should fund community-based research to examine the impact of changes to the built environment on the levels of physical activity in the relevant communities; in addition, population-wide demon-
stration projects should be funded and carefully evaluated, as should studies of natural experiments.1 In addition, carefully designed intervention studies together with studies using longitudinal designs are needed to improve our understanding of the relationships between changes to the built environment and resulting physical activity behavior in youth; such studies will require collaborations between researchers and the responsible public officials. Furthermore, better measures of physical activity collected through travel diary surveys (widely used in transportation planning) and ongoing surveillance systems such as the Youth Risk Behavior Surveillance System are needed, as are better measures of the built environment itself.
The Guide to Community Preventive Services, a systematic review of population-based interventions, strongly recommends the “creation of and enhanced access to places for physical activity combined with informational outreach activities” (p. 91) as an approach to promote physical activity, though the focus of this review was on adults (Kahn et al., 2002). But it is clear that improvements to many different elements of the built environment—parks, hike/bike trails, sidewalks, traffic-calming devices, pedestrian crossings, bicycle-route networks, street connections, and mixed land-use developments—will contribute to the solution.
Next steps. It is incumbent upon local governments to find ways to increase the opportunities for physical activity in local communities and neighborhoods. Achieving this goal may involve revising zoning and subdivision ordinances, where necessary, to ensure that new neighborhoods provide opportunities and facilities for physical activity. For example, a growing number of communities are revamping their local development codes to adhere to smart-growth principles (see Box 6-4) (Local Government Commission, 2003).
To enhance the quality and extent of opportunities for physical activity within existing neighborhoods, local governments will need to prioritize such projects in their capital improvement programs. Federal, state, and regional policies can also contribute to these efforts, primarily by providing the funding necessary to effect physical changes to the built environment. The Federal Transportation Enhancements Program, for example, funded $1.9 billion in pedestrian and bicycle projects throughout the United States between 1992 and 2002 (Federal Highway Administration, 2004). As a
|
BOX 6-4 Trends in City Planning
|
result, many Metropolitan Planning Organizations, agencies responsible for implementing federal transportation programs in metropolitan areas, now put significant emphasis on bicycle and pedestrian planning (Chauncey and Wilkinson, 2003). Professional organizations such as the Institute of Traffic Engineers and the American Planning Association should also work to assist the efforts of local governments by developing and disseminating best practices for expanding opportunities for physical activity.
Citizens themselves have a responsibility to advocate for changes in policy so that the built environment may ultimately offer increased opportunities for physical activity among children and youth. The public may bring significant influence to bear over policy, particularly if a large and vocal constituency urges change and if prominent community groups, nonprofit organizations, and business organizations lend their support. In many communities, neighborhood associations play a formal role in the planning process and have successfully advocated for new or improved parks, additional side walks, traffic-calming programs, and other changes in the built
environment. In addition, legal approaches may be useful (Perdue et al., 2003; Mensah et al., 2004).
Local governments, in partnership with private developers and community groups, should ensure that every neighborhood has safe and well-designed recreational facilities and other places for physical activity for children and youth. Communities can require such environmental characteristics in new developments and use creative approaches to retrofit existing neighborhoods. Furthermore, local governments should ensure that streets are designed to encourage safe walking, bicycling, and other physical activities within the neighborhood and the larger community. Child-safe street design includes well-maintained sidewalks, safe places for crossing, adequate bike lanes, and features that slow traffic.
Walking and Bicycling to School
Compared with 30 years ago, few students in the United States are walking or bicycling to school. In 1969, an average of 48 percent of all students walked or biked to that destination; among those living no more than a mile away, nearly 90 percent did so (EPA, 2003). In comparison, the 1999 HealthStyles Survey found that of the participating households, 19 percent reported that their children walked to or from school at least once a week in the preceding month and that 6 percent rode their bikes (CDC, 2002a). Similar results were seen in a study by the Georgia Division of Public Health, which found that fewer than 19 percent of the state’s school-aged children who lived a mile or less from school commuted by foot most days of the week (CDC, 2002b).
The HealthStyles Survey households reported that barriers to their children’s walking or bicycling to school included: long distances (noted by 55 percent of respondents), traffic-related safety concerns (40 percent), adverse weather conditions (24 percent), crime danger (18 percent), school policy (7 percent), or other reasons (26 percent) (CDC, 2002a). Sixteen percent acknowledged that there were no barriers to walking or bicycling to school.
Two other studies also identified distance as a determinant. In one small study of six school sites, respondents said that it was more likely that their children would walk or bike to school if their home was a mile or less away (McMillan, 2002), while the other found that the probability of walking or bicycling declined with travel time (EPA, 2003). The situation at present is that the majority of children arrive and leave school in automobiles, vans, trucks, and buses (Figure 6-1) (TRB, 2002). Research also suggests that parents, students, and school officials often select or encourage motorized travel because of convenience, flexibility, budget, or expectation rather than to maximize safety (TRB, 2002).
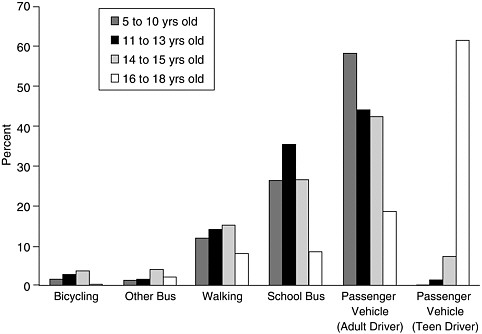
FIGURE 6-1 Percentage of trips during normal school travel hours, Nationwide Personal Transportation Survey, 1995.
SOURCE: Special Report 269: The Relative Risks of School Travel. Transportation Research Board, National Research Council, Washington, D.C., 2002, Figure 3-1(a), p. 88. Reproduced with permission.
Because the majority of children and youth attend school five days per week, throughout a large part of the year, trips to and from school offer a potential opportunity to substantially increase their daily physical activity and energy expenditure. Observational studies have in fact demonstrated that children can get some of their most vigorous school-day physical activity during the times they travel between home and school (Cooper et al., 2003; Tudor-Locke et al., 2003). Cooper and colleagues (2003) found, in a study of 114 British children aged 9 to 11 years, that the boys who walked to school were generally more active than those who were transported by car (although similar results were not seen for girls).
While the committee acknowledges that there is no direct evidence that walking or bicycling to school will reduce the prevalence of obesity in children, clear evidence does exist that increases in physical activity can have positive impacts on weight loss or on maintaining a healthy weight. Further, there are potential ancillary benefits, which include enhancing the neighborhood environment (e.g., so that families may walk or bike more
often during after-school hours), lowering busing costs, and fostering social interaction within the community.
Interventions to promote safe walking and bicycling to schools have already become popular in some communities, thereby demonstrating a broader potential for feasibility and acceptability (Box 6-5). In Chicago, for example, 90 percent of the nearly 422,000 public school children walk to school and the city has encouraged a Walking School Bus program in which one or more adults walk to school with and supervise a small group of children from the neighborhood (Chicago Police Department, 2004). Since 1997,2 National Walk Our Children to School Day and a similar international effort have attracted substantial interest.
Safe Routes to School programs have produced increases in the number of students walking or bicycling between home and school. Demonstration projects in 10 British towns showed an increase in walking and bicycling among children and reductions in car use (Sustrans, 2001). An evaluation of the Safe Routes to School programs in seven schools in Marin County, California, found that from fall 2000 to spring 2002, there was a 64 percent increase in the number of children walking to school and a 114 percent increase in the number of students bicycling (Staunton et al., 2003). Another evaluation of the California program, which focused on schools in Southern California, showed strong evidence of success in five schools, weak evidence in one school, and no evidence in three schools (success was defined as improvements in safety conditions as well as increases in the numbers of children walking or bicycling to school) (Boarnet et al., 2003). These data suggest that Safe Routes to School programs show promise in promoting physically active means for children traveling to and from school.
Locating schools in close proximity to the neighborhoods they serve is another opportunity for increasing the likelihood that children and youth will walk or bike between them (EPA, 2003). Annual school construction costs in the United States (including new school construction and school building rehabilitation) were estimated to have grown from about $18 billion in 1990 to $25 billion in 1997 (GAO, 2000) and continue to increase. Given the scale of this spending and the numerous projects involved, school construction projects provide a tremendous opportunity for locating at least some new schools within walking or biking distance of the residential areas from which they draw their students.
Local governments and school districts should ensure that children and youth have safe walking and bicycling routes between their homes and schools and that they are encouraged to use them. Realizing this objective
|
BOX 6-5 Safe Routes to School Safe Routes to Schools was initiated in Western Europe and the United Kingdom. As its name implies, the program promotes walking and bicycling to school, and it does so through education and incentives that show how much fun it can be. The program also addresses the safety concerns of parents by encouraging greater enforcement of traffic laws, educating the public, and exploring ways to create inherently safer streets. In the United States, the California legislature established a Safe Routes to School program in 1999 and extended it for three more years in 2001. This program provides $25 million in state and federal transportation funds to projects that improve the safety of walking and bicycling to schools. Administered by the state Department of Transportation, Safe Routes to School funded 268 projects in its first 4 years (Caltrans, 2004). Other programs are emerging across the United States to promote safe walking and bicycling to school, and the nonprofit organization Transportation Alternatives provides a toolkit to help communities in starting their own Safe Routes to School-type programs (Transportation Alternatives, 2004). The U.S. programs incorporate one or more of the following four key elements:
|
will involve the efforts of many groups in local communities. Schools and school districts, in collaboration with community partners, need to develop and implement policies and programs that promote walking and bicycling (Chapter 7). Local governments need to allocate the resources to make the necessary improvements to sidewalks, crosswalks, signals, signs, and other traffic control devices. Collaborations between law enforcement officials and schools are needed to deploy pedestrian safety measures at the beginning and end of each school day; crossing guards are an important part of this process. Additionally, decisions regarding the locations of new schools need to carefully consider the benefits of being close enough to the neighborhoods they serve to facilitate students’ walking or bicycling from one site to the other.
When interventions that promote walking or bicycling to school are implemented, it is crucial that researchers evaluate their effects on total
daily physical activity and energy expenditure, and on changes in weight over time. Programs promoting safe routes to school, as well as other efforts to increase students’ walking and bicycling, should include funding for evaluation, and the organizations that implement these programs should work with researchers to develop rigorous evaluation designs. Because so much remains to be learned about the various approaches to increasing walking and bicycling to school, thorough evaluations of such initiatives are critical.
Community Food Environment
All members in a community need access3 to affordable and healthful food on a regular basis. Food security is commonly defined as “access by all people at all times to enough food for an active, healthy life and includes at a minimum: a) the ready availability of nutritionally adequate and safe foods, and b) the assured ability to acquire acceptable foods in socially acceptable ways (p. 1560)” (LSRO, 1990). Food security is one of the necessary conditions to ensure the health of a population.
In 2002, 11.1 percent of U.S. households, representing more than 35 million people, experienced food insecurity—that is, their access to nutritious food on a regular basis was limited or uncertain (Nord et al., 2003). In general, households with children report food insecurity at more than twice the rate of households without children (16.5 percent versus 8.1 percent, respectively) (Nord et al., 2003). Children living in food-insecure households are more likely to have compromised well-being than children living in food-secure households (Alaimo et al., 2001); evidence has linked food insecurity to declines in children’s health, mental and psychological functioning, and academic achievement (ADA, 2004). As discussed in Chapter 3, however, evidence linking childhood food insecurity to obesity is inconclusive.
In 2002, a food-secure household in the United States spent 35 percent more on food than the typical food-insecure household of the same size and composition (Nord et al., 2003), though food accounted for a greater proportion of the latter’s budget (Lang and Caraher, 1998). Thus, it stands to reason that food cost is a significant predictor of dietary choices and health outcomes, particularly in low-income ethnic minority urban communities (Perry, 2001; Morland et al., 2002a; Pothukuchi et al., 2002; Sloane et al., 2003) and rural communities (Holben et al., 2004). At the same time, while
it is acknowledged that consumer food choices are shaped by taste, cost, and convenience, it has been suggested that high-fat, energy-dense foods and diets are often less expensive on a cost-per-calorie basis and are more palatable than high-fiber low-energy-dense foods such as the lean meats, fish, fresh fruits, and vegetables that comprise a healthful diet (Drewnowski and Specter, 2004). However, based on the ACNielsen Homescan 1999 data for household food purchases from all types of retail outlets, a price analysis of 154 types of fruits and vegetables found that more than one-half of the produce items were estimated to cost less than 25 cents per serving. The study concludes that all consumers, including low-income households, can meet the recommendations of three servings of fruit and four servings of vegetables for 64 cents per day (Reed et al., 2004). However, it is difficult to predict or understand consumer behavior from these types of analyses, as discussed in Chapters 3 and 5.
The availability and affordability of energy-dense foods has increased in recent years in low-income neighborhoods (Morland et al., 2002a,b; Sloane et al., 2003). This situation is associated with several trends: fewer supermarkets being located within a reasonable walking distance, supermarket relocation to the suburbs (Cotterill and Franklin, 1995; Shaffer, 2002; Bolen and Hecht, 2003), the lack of transportation to supermarkets offering a variety of healthful choices at affordable prices (Urban and Environmental Policy Institute, 2002; Bolen and Hecht, 2003), and the local proliferation of gas stations and convenience stores that often have a limited selection of healthful foods and at higher prices (Alwitt and Donley, 1997; Perry, 2001; Morland et al., 2002a).
Community food-security assessment toolkits and other methods, such as community mapping, have been used to assist communities throughout the United States in undertaking community assessments and inventories to identify the type and range of locally available food resources, including supermarkets, corner grocery stores, full-service and fast food restaurants, food banks, food pantries, farmers’ markets, and community gardens (Perry, 2001; Cohen, 2002; Pothukuchi et al., 2002; Sloane et al., 2003). Knowing the inventory and its gaps, communities may then take appropriate action, and in fact they are addressing their food insecurity problems in a variety of ways.
For example, local governments are offering financial incentives such as grants, loans, and tax benefits to stimulate the development of neighborhood groceries in underserved urban neighborhoods (Shaffer, 2002; Bolen and Hecht, 2003; Baltimore Healthy Stores Project, 2004; Clark, 2004). Some communities are initiating farmers’ markets or enhancing the existing Farmers’ Market Nutrition Programs offered to participants in Special Supplemental Nutrition Program for Women, Infants, and Children and the Food Stamp Program (Connecticut Food Policy Council, 1998; Fisher,
1999; Kantor, 2001; Conrey et al., 2003). Others are promoting community gardens (Kantor, 2001; Twiss et al., 2003), school gardens (Edible Schoolyard, 2004; see Chapter 7), and farm-to-school and farm-to-cafeteria programs (Kantor, 2001; Bellows et al., 2003; Center for Food and Justice, 2004; Sanger and Zenz, 2004; see Chapter 7).
Recent research has demonstrated that children who grow some of their own food in school gardens have an increased preference for certain vegetables (Morris and Zidenberg-Cherr, 2002). Recent federal legislation (Public Law 108-265) includes provisions designed to strengthen partnerships between local agriculture and schools to ensure that fresh local produce can go from farms directly to schools.
These initiatives to enhance the community food environment and promote household and community food security are promising to expand healthful food choices, especially for neighborhoods that are now limited in their ability to obtain healthful and affordable food on a regular basis. However, evaluations will be required to determine the programs’ effectiveness in meeting these goals.
Local governments should work with community groups, nonprofit organizations, local farmers and food processors, and local businesses to support multisectoral partnerships and networks that expand the availability of healthful foods within walking distance, particularly in low-income and underserved neighborhoods. Such efforts will expand healthful food choices at local grocery stores, supermarkets, and fast food restaurants, and they will encourage a broad range of community food-security initiatives that improve access to highly nutritional foods.
Health Impact Assessments and Community Health Evaluations
Evaluation of community-wide efforts can be a challenge, given the typically wide age range among members of the population; their ethnic, racial, and social diversities; the differences in settings of various community interventions; and the numerous barriers involved.
Nevertheless, it is important to assess the potential impact of proposed programs and changes as well as to conduct evaluations of recent and ongoing efforts. A prospective approach to community evaluation efforts involves a “health impact assessment” that gauges the potential effects of a proposed policy or intervention on the health of the population (WHO, 1999). Much as environmental impact assessments examine the potential effects of a new construction project on such indicators as an area’s air and water quality, health impact assessments are used to evaluate and then modify a proposed action—that is, to remove or minimize that action’s negative public health impacts, and to help enhance its positive effects (Taylor and Quigley, 2002). The health impact assessment may also be
particularly useful in bringing potential health impacts to the attention of policy makers.
A major value of this approach is its focus on considering the input of multiple stakeholders, including those who would be directly affected by the project under consideration. As changes are proposed to the built environment, communities should consider this tool for examining how proposed changes in the community would affect health issues such as access to and availability of healthful foods and opportunities for physical activity. It will be important to identify and examine natural experiments in which initiatives based on health-impact assessments could be compared to those undertaken without such an assessment.
For an overall assessment of a community’s health improvement efforts that are already underway, community health “report cards” (also termed community health assessments or health profiles) are an excellent tool, both to assess and convey progress (CDC, 1997a). A variety of approaches have been used, all with the goal of providing a concise and consistent collection of data that can be formatted for dissemination to the community. For example, state, county, and community health profiles have been developed using CDC’s Healthy Days Measures among other community performance indicators (CDC, 2004a). In addition, the Community Health Status Indicators Project (CHSI)—a collaborative effort of the Association of State and Territorial Health Officials, the National Association of County and City Health Officials (NACCHO), and the Public Health Foundation—has developed report indicators and formats for county-specific information that allows comparisons with similar “peer” counties throughout the country (NACCHO, 2004). A CHSI report contains information on behavioral risks, preventive services use, access, and summary health measures. To assist in obesity prevention efforts, community health report cards should use measures that assess the community’s progress toward encouraging good nutrition and physical activity. These measures could rate the built and social environments, local school policies and practices (Chapter 7), the community food environment, and the degree of involvement of local businesses, organizations, and other groups in supporting and participating in obesity prevention efforts.
To streamline efforts and encourage communities to engage in these types of evaluation efforts, common evaluation tools should be developed and shared, while also ensuring that evaluation tools have the flexibility to be sensitive to the needs of local communities. This is an area where it will be important to build on tools (those discussed above and others) that have already been developed. Leadership for these efforts should involve CDC, NACCHO, the American Planning Association, and other relevant organizations, including foundations such as the Robert Wood Johnson Foundation, with interests in community-based obesity prevention efforts.
Communities should use evaluation tools (e.g., health impact assessments, audits, or report cards) to assess the availability and impact of local opportunities for physical activity (e.g., sidewalks, parks, recreational facilities) and for healthful eating (e.g., grocery store access, farmers’ markets).
Recommendations
Mobilizing communities to address childhood obesity will involve changes in the social and built environment. Several large-scale community-based interventions—primarily focused on improving diet and physical activity levels to address cardiovascular outcomes—show the feasibility of such efforts, although much remains to be learned about how to increase their effectiveness, particularly with regard to obesity prevention in youth. Efforts to address other public health issues such as tobacco prevention and control provide models for community coalition efforts.
A relatively new field of research is merging urban planning, transportation, and public health research tools to examine the impact of the built environment on human health. Observational and correlational studies, primarily conducted in adult populations, have shown that features in the built environment such as the walkability of neighborhoods or availability of recreational facilities are associated with level of physical activity. A few small-scale intervention studies have examined the effects of changes to the built environment; however, research is needed to explore what specific changes to the built environment will be the most effective in preventing childhood obesity. The committee recommends the implementation and evaluation of a range of community changes to facilitate improved nutrition and increased physical activity. These efforts are an integral part of a comprehensive approach to create healthier environments for children and youth.
Recommendation 6: Community Programs
Local governments, public health agencies, schools, and community organizations should collaboratively develop and promote programs that encourage healthful eating behaviors and regular physical activity, particularly for populations at high risk of childhood obesity. Community coalitions should be formed to facilitate and promote cross-cutting programs and community-wide efforts.
To implement this recommendation:
-
Private and public efforts to eliminate health disparities should include obesity prevention as one of their primary areas of focus and
-
should support community-based collaborative programs to address social, economic, and environmental barriers that contribute to the increased obesity prevalence among certain populations.
-
Community child- and youth-centered organizations should promote healthful eating behaviors and regular physical activity through new and existing programs that will be sustained over the long term.
-
Community evaluation tools should incorporate measures of the availability of opportunities for physical activity and healthful eating.
-
Communities should improve access to supermarkets, farmers’ markets, and community gardens to expand healthful food options, particularly in low-income and underserved areas.
Recommendation 7: Built Environment
Local governments, private developers, and community groups should expand opportunities for physical activity including recreational facilities, parks, playgrounds, sidewalks, bike paths, routes for walking or bicycling to school, and safe streets and neighborhoods, especially for populations at high risk of childhood obesity.
To implement this recommendation:
Local governments, working with private developers and community groups, should:
-
Revise comprehensive plans, zoning and subdivision ordinances, and other planning practices to increase availability and accessibility of opportunities for physical activity in new developments
-
Prioritize capital improvement projects to increase opportunities for physical activity in existing areas
-
Improve the street, sidewalk, and street-crossing safety of routes to school, develop programs to encourage walking and bicycling to school, and build schools within walking and bicycling distance of the neighborhoods they serve
Community groups should:
-
Work with local governments to change their planning and capital improvement practices to give higher priority to opportunities for physical activity
DHHS and the Department of Transportation should:
-
Fund community-based research to examine the impact of
-
changes to the built environment on the levels of physical activity in the relevant communities and populations.
HEALTH CARE
Because health care is usually provided at the local level, it is best addressed in a community context. Health-care professionals have frequent opportunities to encourage children and youth to engage in healthful lifestyles. Unfortunately, treatment of obesity per se is rarely considered a reimbursable interaction between patient and doctor, and our current health-care system is not yet focused on preventive measures for childhood obesity. But the health-care delivery system can still have a significant impact on this issue. It is now up to health-care professionals and their professional organizations, as well as health insurers and quality improvement and accrediting agencies, to make obesity prevention a part of routine preventive health care.
Health-Care Professionals
Health-care professionals—physicians, nurses, and other clinicians—have an influential role to play in preventing childhood obesity. As healthcare advisors both to children and their parents, they have the access and the influence to make key suggestions and recommendations on dietary intake and physical activity throughout children’s lives. They also have the authority to elevate concern about childhood obesity and advocate for preventive efforts.
The 2002 National Health Interview Survey found that 74.5 percent of children (aged 18 years or younger) had seen a health-care professional at some time during the past six months (Dey et al., 2004), thereby providing numerous opportunities for doctors and other clinicians to measure and track height, weight, and BMI and to counsel the children—as well as their parents or other caregivers—about proper nutrition and physical activity. Measuring height and weight and plotting these measures on growth charts is already a standard part of children’s health care, and recent recommendations by the American Academy of Pediatrics have added BMI to this list (AAP, 2003). Although there is little direct evidence of the impact of height, weight, and BMI screening and tracking on preventing obesity in children, BMI measures for adults have been found to be both easy to measure and a highly reliable method for identifying patients at risk of morbidity and mortality due to obesity (McTigue et al., 2003). The U.S. Preventive Services Task Force (USPSTF) recommends that clinicians use BMI to screen all adult patients for obesity (USPSTF, 2003). A survey of 940 pediatric health-care providers, however, found that more used clinical impression
and weight-for-age or weight-for-height measures than used BMI or BMI percentiles (Barlow et al., 2002).
Because there are standardized BMI charts for children, and given that BMI is a reasonably good surrogate for adiposity, it is sensible to include BMI calculations in all health supervision visits for children. By routinely measuring height and weight and calculating BMI, clinicians communicate that this is an important matter, just as important as routine immunizations or screening tests in protecting children’s health (see Chapter 8). Furthermore, BMI measures on an annual or similarly regular basis allow assessment of the individual child’s growth trajectory, which offers better insights, and on an earlier basis, than height or weight measurement alone (see Chapter 3).
After determining the child’s weight status, health-care professionals have a responsibility to carefully communicate the results to parents and, in an age-appropriate manner, to the children themselves; provide the information that the families need to make informed decisions about physical activity and nutrition; and explain the risks associated with childhood overweight and obesity. Behaviors that can be targeted include those most closely associated with improved nutrition and increased physical activity: increased breastfeeding, limited consumption of sweetened beverages, reduced television viewing or other screen time, and a greater amount of outdoor play (Whitaker, 2003). Careful attention should be paid to minimizing the stigmatization of obesity (Schwartz and Puhl, 2003).
Studies of such counseling on obesity-related issues have shown positive results. In one trial, African-American families were randomized to receive primary-care-based counseling alone or counseling plus a behavioral intervention (including goal-setting and an electronic television-time manager) as part of their regular clinic visits (Ford et al., 2002). Both groups reported similar within-group decreases (from baseline) in children’s television, videotape, and video game use. In the between-group comparison, the behavioral intervention group reported medium to large (and statistically significant) increases in organized physical activity and increases in playing outside. There was also a slight decrease for the intervention group in the number of meals eaten in front of the television, though the differences were not statistically significant (Ford et al., 2002). A four-month primary-care-based assessment and counseling intervention involving adolescents showed the feasibility of such efforts and found short-term improvements in dietary and physical activity outcome measures (Patrick et al., 2001).
More generally, studies of counseling for adults may provide insights into the potential effectiveness of counseling for children and their parents. The USPSTF review of dietary intake counseling for adults in primary-care settings found it to be effective in reducing dietary fat consumption and
increasing fruit and vegetable consumption (Pignone et al., 2003). The best evidence was for patients with known risk factors for cardiovascular and other chronic diseases, but there was also fair evidence that brief counseling in primary care can produce some improvements in diet among unselected patients as well.
Similar reviews of studies that focused on physical activity counseling of adults in primary care found mixed results, although most of the studies showed a trend toward increased physical activity in the intervention groups (Sallis et al., 2000b; Eden et al., 2002). For example, a nonrandomized controlled trial in healthy sedentary adults found short-term increases in moderate physical activity, particularly walking, among those who had received three to five minutes of physical activity counseling by their physician (Calfas et al., 1996).
Although research on the effectiveness of counseling children and their caregivers about obesity prevention is limited to date, and much remains to be learned, the seriousness of the problem and the emergence of tested strategies argue for routine counseling. The evidence that routine smoking-cessation counseling is effective, at least in changing adult behaviors, is another precedent for this kind of guidance (DHHS, 2000a).
Additionally, as visible and influential members of their communities, health-care professionals can serve as role models for good nutrition, for being physically active, and for maintaining a healthy weight. Health-care professionals can also have influential voices in increasing community awareness and advocating for actions to prevent childhood obesity. By giving speeches or conducting workshops at schools, testifying before legislative bodies, working in community organizations, or speaking out in any number of other ways, health-care professionals can press for changes to make the community one that supports and facilitates healthful eating and physical activity. A notable precedent is that physicians and other healthcare professionals have played crucial roles in changing tobacco-related behaviors; they have been advocates both at the local and national levels, and they have served as personal role models by quitting smoking or by not starting in the first place.
Pediatricians, family physicians, nurses, and other clinicians should take active roles in the prevention of obesity in children and youth. As discussed above, this includes routinely measuring height and weight; tracking BMI; and providing feedback, interpretation, counseling, and guidance on obesity prevention to children, parents, and other caregivers. This assumes that clinicians will have learned the appropriate skills to deliver these preventive services, which has implications for training at all levels (see below). They should also serve as role models for healthful eating and regular physical activity and take leadership roles in advocating for childhood obesity prevention in local schools and communities.
Similarly, health-care professional organizations and their members have important roles to play in advocating across the range of community institutions for obesity prevention activities and policies (AAP, 2003). Areas of possible involvement include health insurance coverage policies, school nutrition and physical education, and community recreation and zoning policies. Professional organizations can also be influential in encouraging their members to adopt a more healthful lifestyle and serve as role models to their patients as well as to become more active in their offices and communities in working to prevent obesity. For example, the leadership of the American Academy of Family Physicians (AAFP) has recently challenged all of its members to increase their personal physical activity levels in order to serve as role models for their patients (as well as improve their own health); additionally, AAFP has initiated a program called “Americans in Motion” to help patients, their families, and communities fight obesity (AAFP, 2004).
Furthermore, many professional organizations are providing information on topics relevant to obesity prevention. The American Academy of Pediatrics has issued position statements on children’s television viewing and on physical fitness and activity in schools (AAP, 2000, 2001). The American Medical Association recently published a 10-part monograph on assessment and treatment of adult obesity (Kushner, 2003); similar materials on children should also be prepared. Collaboration between groups could broaden their effectiveness; if health-care professional organizations work together to implement obesity prevention programs and initiatives and develop clinical guidance, they would help ensure that consistent messages are reaching both health-care professionals and their patients.
Health- and medical-care professional organizations should make childhood obesity prevention a high-priority goal for their organizations. This includes creating and disseminating evidence-based clinical guidance and other materials on obesity prevention; establishing programs to encourage members to be role models for proper nutrition and physical activity; advocating for childhood obesity prevention initiatives; and coordinating their efforts, wherever possible, with other health-care professional organizations.
It is also critical to address current limitations in health-care training with regard to obesity prevention, nutrition, and physical activity. Medical and other health-care students have traditionally received little education in nutrition and physical activity; further, instruction on counseling about these topics generally has not been included either in medical school or primary-care residency training curricula (Taren et al., 2001). Such omissions should be corrected in curricula at all levels, from preclinical science through the clinical training years and into postgraduate training programs and continuing medical education for practicing clinicians. In addition, if
certifying entities such as medical specialty boards included questions about these areas in their formal examinations, this would provide an incentive to students and residents to master the associated material. Programs such as the Nutrition Academic Award Program sponsored by the National Heart, Lung, and Blood Institute have begun to focus attention on improving nutrition education efforts in medical schools (Pearson et al., 2001), and further efforts are needed regarding other relevant areas. A recent Institute of Medicine report confirms the need for expanding behavioral and social-science content in medical schools’ curricula (IOM, 2004). Health-care professional schools, postgraduate training programs, continuing professional education programs, professional organizations, and certifying entities should require knowledge and skills related to obesity prevention (e.g., child and adolescent BMI interpretation, nutritional and physical activity counseling) in their curricula and examinations.
Health-Care Insurers, Health Plans, and Quality Improvement and Accrediting Organizations
Until recently, health-care concerns had largely focused on the treatment—as opposed to the prevention—of obesity, particularly the severe forms of adult obesity. But epidemiologic data showing increases in the numbers of obese children and youth, along with a rise in the prevalence of type 2 diabetes (formerly termed “adult onset diabetes”) and increased hypertension in children (Muntner et al., 2004), have raised awareness that childhood obesity might be best addressed from a prevention perspective. Furthermore, the high economic costs of obesity (Chapter 2) provide incentives to health-care insurers and health plans to encourage healthful lifestyles and thereby reduce their costs.
The health-care insurance industry in particular has several paths by which it may address obesity prevention. For individuals and their families, health insurance companies and health plans can develop innovative strategies for encouraging policy holders and their children to maintain a healthy weight, increase their levels of physical activity, and improve the quality of their diet. Creative options may include incentives for participating in and documenting regular physical activity, or programs that provide discounts or other incentives for wellness-related products. For example, one insurance company includes discounts on health and wellness magazines as well as lowered fees for health club memberships and weight-reduction programs for adults (CIGNA, 2004). Furthermore, health-care insurers can take an active role in community coalitions and other activities; one example is the Jump Up and Go Program in Massachusetts (Blue Cross Blue Shield of Massachusetts, 2004). It will be particularly important for healthcare insurers and health plans to consider incentives that are useful to high-
risk populations, who often live in areas where easy access to recreational facilities is lacking or where costs are prohibitive.
For the providers of health-care services, it is important that obesity prevention (including assessment of weight status as well as counseling on nutrition and physical activity) become a routine part of clinical care. Moreover, measures related to successful delivery of clinical preventive services, such as rates of screening tests, should be important components of healthcare quality-improvement programs that are promoted by health plans. The National Committee for Quality Assurance (NCQA) and other national quality-improvement and accrediting organizations should add obesity prevention efforts—such as routine measurement and tracking of BMI, counseling of children and their parents on diet and exercise—to the measures they develop and assess.
There may also be opportunities for incorporating obesity prevention measures and counseling into ongoing federal, state, and local programs that provide disease prevention and health promotion services to children. For example, Medicaid’s Early and Periodic Screening, Diagnostic, and Treatment program offers preventive screenings for eligible children (generally in underserved populations) and it includes a comprehensive health and developmental history. More than 8.7 million children participated in the screening program in 1998 (CMS, 2004), thus offering many potential opportunities for obesity prevention in children.
As with other sectors, those involved in delivering and paying for health care need to become more proactive, preferably through a multifocal, coordinated set of initiatives, in working with families to promote physical activity and healthful diets among children. Medicare has recently removed barriers to coverage for obesity-related services (DHHS, 2004). Although this, of course, does not relate directly to children, it is an action that may well be emulated by other insurers and for preventive services as well as for treatment.
Health insurers, health plans, and quality-improvement and accrediting organizations should designate childhood obesity prevention as a priority health promotion issue. Furthermore, health plans and health-care insurers should provide incentives to individuals and families to maintain healthy body weight and engage in routine physical activity. Health insurers, health plans, and quality improvement and accrediting organizations (such as NCQA) should include screening and obesity prevention services (e.g., routine assessment of BMI or other weight-status measures, counseling of children and their parents on nutrition and physical activity) in routine clinical practice and in quality assessment measures relating to health care.
Recommendation
The health-care community offers a range of opportunities for interactions with children and youth regarding obesity prevention. Several controlled trials of counseling by health-care providers have resulted in patient improvements in physical activity levels or diet, although these studies have generally been conducted with small numbers of patients and have focused on counseling of adult patients. Further research is needed on effective counseling or other types of obesity prevention interventions that could be provided in health-care settings. Improved professional education regarding obesity prevention is an important next step, as is the active involvement of health professional organizations, insurers, and accrediting organizations, in making childhood obesity prevention efforts a priority.
Recommendation 8: Health Care
Pediatricians, family physicians, nurses, and other clinicians should engage in the prevention of childhood obesity. Health-care professional organizations, insurers, and accrediting groups should support individual and population-based obesity prevention efforts.
To implement this recommendation:
-
Health-care professionals should routinely track BMI, offer relevant evidence-based counseling and guidance, serve as role models, and provide leadership in their communities for obesity prevention efforts.
-
Professional organizations should disseminate evidence-based clinical guidance and establish programs on obesity prevention.
-
Training programs and certifying entities should require obesity prevention knowledge and skills in their curricula and examinations.
-
Insurers and accrediting organizations should provide incentives for maintaining healthy body weight and include screening and obesity preventive services in routine clinical practice and quality assessment measures.
REFERENCES
AAFP (American Academy of Family Physicians). 2004. Americans in Motion. [Online]. Available: http://www.aafp.org/x22874.xml [accessed May 14, 2004].
AAP (American Academy of Pediatrics), Committee on Sports Medicine and Fitness and Committee on School Health. 2000. Physical fitness and activity in schools. Pediatrics 105(5):1156-1157.
AAP. 2001. Children, adolescents, and television. Pediatrics 107(2):423-426.
AAP, Committee on Nutrition. 2003. Prevention of pediatric overweight and obesity. Pediatrics 112(2):424-430.
ADA (American Dietetic Association). 2004. Position of the American Dietetic Association: Dietary guidance for healthy children ages 2 to 11 years. J Am Diet Assoc 104(4):660-677.
Alaimo K, Olson CM, Frongillo EA Jr, Briefel RR. 2001. Food insufficiency, family income, and health in US preschool and school-aged children. Am J Public Health 91(5):781-786.
Alwitt LF, Donley TD. 1997. Retail stores in poor urban neighborhoods. J Consumer Affairs 31(1):139-164.
Baker EA, Brownson CA. 1998. Defining characteristics of community-based health promotion programs. J Public Health Manag Pract 4(2):1-9.
Baltimore Healthy Stores Project. 2004. Baltimore Healthy Stores Project. [Online]. Available: http://www.healthystores.org/BHS.html [accessed June 8, 2004].
Baranowski T, Thompson WO, DuRant RH, Baranowski J, Puhl J. 1993. Observations on physical activity in physical locations: Age, gender, ethnicity, and month effects. Res Q Exerc Sport 64(2):127-133.
Baranowski T, Baranowski JC, Cullen KW, Thompson DI, Nicklas T, Zakeri IE, Rochon J. 2003. The Fun, Food, and Fitness Project (FFFP): The Baylor GEMS pilot study. Ethn Dis 13(1 Suppl 1):S30-S39.
Barlow SE, Dietz WH, Klish WJ, Trowbridge FL. 2002. Medical evaluation of overweight children and adolescents: Reports from pediatricians, pediatric nurse practitioners, and registered dietitians. Pediatrics 110(1):222-228.
Beech BM, Klesges RC, Kumanyika SK, Murray DM, Klesges L, McClanahan B, Slawson D, Nunnally C, Rochon J, McLain-Allen B, Pree-Cary J. 2003. Child- and parent-targeted interventions: The Memphis GEMS pilot study. Ethn Dis 13(1 Suppl 1):S40-S53.
Bellows BC, Dufour R, Bachmann J. 2003. Bringing Local Food to Local Institutions. A Resource Guide for Farm-to-School and Farm-to-Institution Programs. [Online]. Available: http://attra.ncat.org/attra-pub/PDF/farmtoschool.pdf [accessed June 8, 2004].
Blue Cross Blue Shield of Massachusetts. 2004. Jump Up and Go! [Online]. Available: http://www.bcbsma.com/common/en_US/myWellbeingIndex.jsp [accessed August 5, 2004].
Boarnet MG, Day K, Anderson C, McMillen T, Alfonzo M. 2003. Urban Form and Physical Activity: Insights from a Quasi-Experiment. [Online]. Available: http://www.activelivingresearch.org/downloads/boarnet_presentation.pdf [accessed June 3, 2004].
Bolen E, Hecht K. 2003. Neighborhood Groceries: New Access to Healthy Food in Low-Income Communities. California Food Policy Advocates. [Online]. Available: http://www.cfpa.net/Grocery.PDF [accessed January 8, 2004].
Brownson RC, Baker EA, Housemann RA, Brennan LK, Bacak SJ. 2001. Environmental and policy determinants of physical activity in the United States. Am J Public Health 91:1995-2003.
Brumley DE, Hawks RW, Gillcrist JA, Blackford JU, Wells WW. 2001. Successful implementation of community water fluoridation via the community diagnosis process. J Public Health Dent 61(1):28-33.
Burdette HL, Whitaker RC. 2004. Neighborhood playgrounds, fast food restaurants, and crime: Relationships to overweight in low-income preschool children. Prev Med 38(1):57-63.
Calfas KJ, Long BJ, Sallis JF, Wooten WJ, Pratt M, Patrick K. 1996. A controlled trial of physician counseling to promote the adoption of physical activity. Prev Med 25(3):225-233.
Caltrans. 2004. Safe Routes to School Program. [Online]. Available: http://www.dot.ca.gov/hq/LocalPrograms/saferoute2.htm [accessed April 22, 2004].
Campbell MK, Demark-Wahnefried W, Symons M, Kalsbeek WD, Dodds J, Cowan A, Jackson B, Motsinger B, Hoben K, Lashley J, Demissie S, McClelland JW. 1999. Fruit and vegetable consumption and prevention of cancer: The Black Churches United for Better Health project. Am J Public Health 89(9):1390-1396.
CDC (Centers for Disease Control and Prevention). 1997a. Characteristics of community report cards, United States, 1996. MMWR 46(28):647-648.
CDC. 1997b. Guidelines for school and community programs to promote lifelong physical activity among young people. MMWR 46(RR-6):1-36.
CDC. 1999. Neighborhood safety and prevalence of physical inactivity-selected states. MMWR 48(7):143-146.
CDC. 2002a. Barriers to children walking and bicycling to school—United States, 1999. MMWR 51(32):701-704.
CDC. 2002b. School transportation modes—Georgia, 2000. MMWR 51(32):704-705.
CDC. 2004a. State and Community Health Profiles. [Online]. Available: http://www.cdc.gov/hrqol/community.htm [accessed July 6, 2004].
CDC. 2004b. REACH: Racial and Ethnic Approaches to Community Health. [Online]. Available: http://www.cdc.gov/reach2010/ [accessed August 4, 2004].
Center for Food and Justice. 2004. Farm to School Projects: Improving School Food While Helping Local Farmers. Urban and Environmental Policy Institute. [Online]. Available: http://www.farmtoschool.org/ [accessed June 8, 2004].
Chauncey B, Wilkinson B. 2003. An Assessment of MPO Support for Bicycling and Walking. Washington DC: National Center for Bicycling and Walking.
Chavis DM. 2001. The paradoxes and promise of community coalitions. Am J Community Psychol 29(2):309-320.
Chicago Police Department. 2004. Protecting Our Children—Working Together for a Safer Chicago. [Online]. Available: http://www.cityofchicago.org/cp/Alerts/SafetyTips/ChildSafety/WalkingSchoolbus.html [accessed May 21, 2004].
CIGNA. 2004. Member Discounts from Healthy Rewards. [Online]. Available: http://www.cigna.com/health/consumer/medical/discount.html [accessed April 22, 2004].
Clark V. 2004. Plan would add supermarkets in city: The $100 million statewide proposal is intended to promote healthy eating in low-income areas. Philadelphia Inquirer. News release. May 5.
CMS (Centers for Medicare & Medicaid Services). 2004. Annual EPSDT Participation Report, All States. [Online]. Available: http://www.cms.hhs.gov/medicaid/epsdt/ep1998n.pdf [accessed May 14, 2004].
CNU (Congress for the New Urbanism). 2004. About CNU. [Online]. Available: http://www.cnu.org/aboutcnu [accessed April 22, 2004].
Cohen B. 2002. Community Food Security Assessment Toolkit. Washington, DC: USDA, Economic Research Service. E-FAN-02-013. [Online]. Available: http://www.ers.usda.gov/publications/efan02013/efan02013.pdf [accessed June 8, 2004].
Connecticut Food Policy Council. 1998. Making Room at the Table: A Guide to Community Food Security in Connecticut. Hartford, CT: CFPC.
Conrey EJ, Frongillo EA, Dollahite JS, Griffin MR. 2003. Integrated program enhancements increased utilization of a farmers’ market nutrition program. J Nutr 133(6):1841-1844.
Cooper AR, Page AS, Foster LJ, Qahwaji D. 2003. Commuting to school: Are children who walk more physically active? Am J Prev Med 25(4):273-276.
Corburn J. 2004. Confronting the challenges in reconnecting urban planning and public health. Am J Public Health 94(4):541-546.
Cotterill RW, Franklin AW. 1995. The Urban Grocery Store Gap. Storrs, CT: Food Marketing Policy Center, University of Connecticut.
Cullen KW, Bartholomew LL, Parcel GS. 1997. Girl Scouting: An effective channel for nutrition education. J Nutr Educ 92(5):86-91.
DeBate RD. 2002. Girls on the Run International. Evaluation Report, Spring 2002. Charlotte, NC: University of North Carolina.
Dey AN, Schiller JS, Tai DA. 2004. Summary health statistics for U.S. children: National Health Interview Survey, 2002. Vital Health Statistics 10(221).
DHHS (U.S. Department of Health and Human Services), USPHS Guideline Panel. 2000a. Treating Tobacco Use and Dependence. Washington, DC: DHHS.
DHHS. 2000b. Healthy People 2010: Understanding and Improving Health. 2nd edition. Washington, DC: U.S. Government Printing Office. [Online]. Available: http://www.healthypeople.gov/document/tableofcontents.htm [accessed April 9, 2004].
DHHS. 2004. HHS Announces Revised Medicare Obesity Coverage Policy. [Online]. Available: http://www.hhs.gov/news/press/2004pres/20040715.html [accessed August 4, 2004].
DiGuiseppi C, Roberts I, Li L, Allen D. 1998. Determinants of car travel on daily journeys to school: Cross sectional survey of primary school children. Br Med J 316(7142):1426-1428.
Doxey J, Tran T, Kimball K, Corliss J, Mercer M. 2003. Can’t Get There from Here: The Declining Independent Mobility of California’s Children and Youth. A Joint Project of the Surface Transportation Policy Project, Transportation and Land Use Coalition, Latino Issues Forum. [Online]. Available: http://www.transcoalition.org/reports/kids/kids_report.pdf [accessed April 18, 2004].
Drewnowski A, Specter SE. 2004. Poverty and obesity: The role of energy density and energy costs. Am J Clin Nutr 79(1):6-16.
Eden KB, Orleans CT, Mulrow CD, Pender NJ, Teutsch SM. 2002. Does counseling by clinicians improve physical activity? A summary of the evidence for the U.S. Preventive Services Task Force. Ann Intern Med 137(3):208-215.
Edible Schoolyard. 2004. The Edible Schoolyard. [Online]. Available: http://www.edibleschoolyard.org [accessed June 4, 2004].
EPA (U.S. Environmental Protection Agency). 2003. Travel and Environmental Implications of School Siting. EPA 231-R-03-004. Washington, DC: EPA.
Eubanks-Ahrens B. 1987. A closer look at the users of Woonerven. In: Moudon AV, ed. Public Streets for Public Use. New York: Van Nostrand Reinhold.
Farquhar JW, Maccoby N, Wood PD, Alexander JK, Breitrose H, Brown BW Jr, Haskell WL, McAlister AL, Meyer AJ, Nash JD, Stern MP. 1977. Community education for cardiovascular health. Lancet 1(8023):1192-1995.
Farquhar JW, Fortmann SP, Flora JA, Taylor CB, Haskell WL, Williams PT, Maccoby N, Wood PD. 1990. Effects of communitywide education on cardiovascular disease risk factors. The Stanford Five-City Project. J Am Med Assoc 264(3):359-365.
Fawcett SB, Paine-Andrews A, Francisco VT, Schultz J, Richter KP, Berkley-Patton J, Fisher JL, Lewis RK, Lopez CM, Russos S, Williams EL, Harris KJ, Evensen P. 2001. Evaluating community initiatives for health and development. WHO Reg Publ Eur Ser 92:241-270.
Fawcett SB, et al. 2004. Understanding and Improving the Work of Community Health and Development. Paper presented at the VIII Biannual Symposium on the Science of Behavior. As cited in: Kaiser Permanente. 2004. Kaiser Permanente’s Framework for Community Health Initiatives. [Online]. Available: http://www.kpihp.org/publications/briefs/chi_Framework.pdf.
Federal Highway Administration. 2004. Federal–Aid Highway Program Funding for Pedestrian and Bicycle Facilities and Programs. [Online]. Available: http://www.fhwa.dot.gov/environment/bikeped/bikepedfund.htm [accessed July 15, 2004].
Fisher A. 1999. Hot Peppers and Parking Lot Peaches: Evaluating Farmers’ Markets in Low Income Communities. Venice, CA: Community Food Security Coalition. [Online]. Available: http://www.foodsecurity.org/executive.html [accessed April 22, 2004].
Ford BS, McDonald TE, Owens AS, Robinson TN. 2002. Primary care interventions to reduce television viewing in African-American children. Am J Prev Med 22(2):106-109.
GAO (U.S. General Accounting Office). 2000. School Facilities: Construction Expenditures Have Grown Significantly in Recent Years. HEHS-00-41. Washington, DC: GAO.
Girls on the Run. 2004. Girls on the Run International. [Online]. Available: http://www.girlsontherun.org/ [accessed May 14, 2004].
Glanz K. 1997. Perspectives on using theory. In: Glanz K, Lewis FM, Rimer BK, eds. Health Behavior and Health Education. 2nd ed. San Francisco, CA: Jossey-Bass Publishers. Pp. 441-449.
Gordon-Larsen P, McMurray RG, Popkin BM. 2000. Determinants of adolescent physical activity and inactivity patterns. Pediatrics 105:E83.
Grossman DC. 2000. The history of injury control and the epidemiology of child and adolescent injuries. Future Child 10(1):23-52.
Handy S, Boarnet MG, Ewing R, Killingsworth RE. 2002. How the built environment affects physical activity: Views from urban planning. Am J Prev Med 23(2 Suppl):64-73.
Handy S, Paterson R, Butler K. 2003. Planning for Street Connectivity: Getting from Here to There. Planning Advisory Service Report. Chicago, IL: American Planning Association.
Hoefer WR, McKenzie TL, Sallis JF, Marshall SJ, Conway JL. 2001. Parental provision of transportation for adolescent physical activity. Am J Prev Med 21(1):48-51.
Hoehner CM, Brennan LK, Brownson RC, Handy SL, Killingsworth R. 2003. Opportunities for integrating public health and urban planning approaches to promote active community environments. Am J Health Promot 18(1):14-20.
Holben DH, McClincy MC, Holcomb JP Jr, Dean KL, Walker CE. 2004. Food security status of households in Appalachian Ohio with children in Head Start. J Am Diet Assoc 104(2):238-241.
Huang HF, Cynecki MJ. 2000. Effects of traffic calming measures on pedestrian and motorist behavior. Transp Res Rec 1705:26-31.
Huang HF, Cynecki MJ. 2001. The Effects of Traffic Calming Measures on Pedestrian and Motorist Behavior. McLean, VA: Federal Highway Administration.
Humpel N, Owen N, Leslie E. 2002. Environmental factors associated with adults’ participation in physical activity: A review. Am J Prev Med 22(3):188-199.
IOM (Institute of Medicine). 1994. Growing Up Tobacco Free: Preventing Nicotine Addiction in Children and Youth. Washington, DC: National Academy Press.
IOM. 2003. Fulfilling the Potential of Cancer Prevention and Early Detection. Washington, DC: The National Academies Press.
IOM. 2004. Improving Medical Education: Enhancing the Behavioral and Social Science Content of Medical School Curricula. Washington, DC: The National Academies Press.
ITE (Institute of Transportation Engineers). 1999. Traditional Neighborhood Development Street Design Guidelines: Recommended Practice. Washington, DC: ITE.
Jacobsen P, Anderson CL, Winn DG, Moffat J, Agran PF, Sarkar S. 2000. Child pedestrian injuries on residential streets: Implications for traffic engineering. Inst Traffic Eng J Web 70:71-75.
Kahn EB, Ramsey LT, Brownson RC, Heath GW, Howze EH, Powell KE, Stone EJ, Rajab MW, Corso P. 2002. The effectiveness of interventions to increase physical activity. A systematic review. Am J Prev Med 22(4 Suppl):73-107.
Kaiser Permanente. 2004. Kaiser Permanente’s Framework for Community Health Initiatives. [Online]. Available: http://www.kpihp.org/publications/briefs/chi_Framework.pdf.
Kantor LS. 2001. Community food security programs improve food access. Food Rev 24(1):20-26.
Kegler MC, Steckler A, McLeroy K, Malek SH. 1998. Factors that contribute to effective community health promotion coalitions: A study of 10 Project ASSIST coalitions in North Carolina. American Stop Smoking Intervention Study for Cancer Prevention. Health Educ Behav 25(3):338-353.
Kelder SH, Perry CL, Klepp KI. 1993. Community-wide youth exercise promotion: Long-term outcomes of the Minnesota Heart Health Program and the Class of 1989 Study. J Sch Health 63(5):218-223.
Kelder SH, Perry CL, Lytle LA, Klepp KI. 1995. Community-wide youth nutrition education: Long-term outcomes of the Minnesota Heart Health Program. Health Educ Res 10(2):119-131.
Klesges RC, Eck LH, Hanson CL, Haddock CK, Klesges LM. 1990. Effects of obesity, social interactions, and physical environment on physical activity in preschoolers. Health Psychol 9(4):435-449.
Kreuter M, Lezin N. 2002. Coalitions, consortia and partnerships. In: Last J, Breslow L, Green LW, eds. Encyclopedia of Public Health. London, UK: MacMillan Publishers.
Kumanyika SK, Obarzanek E, Robinson TN, Beech BM. 2003. Phase 1 of the Girls health Enrichment Multi-site Studies (GEMS): Conclusion. Ethn Dis 13(1 Suppl 1):S88-S91.
Kushner RF. 2003. Assessment and Management of Adult Obesity: A Primer for Physicans. Chicago, IL: American Medical Association.
Lang T, Caraher M. 1998. Food poverty and shopping deserts: What are the implications for health promotion policy and practice? Health Educ J 58(3):202-211.
Lasker RD, Weiss ES. 2003. Broadening participation in community-problem solving: A multidisciplinary model to support collaborative practice and research. J Urban Health 80(1):14-47.
Lasker RD, Weiss ES, Miller R, Community-Campus Parternerships for Health. 2001. Promoting collaborations that improve health. Educ Health 14(2):163-172.
Local Government Commission.2003. Overcoming Obstacles to Smart Growth Through Code Reform. Sacramento, CA: Local Government Commission.
Loukaitou-Sideris A. 2003. Transportation, Land Use, and Physical Activity: Safety and Security Considerations. Draft paper presented at a workshop of the Transportation Research Board and the Institute of Medicine Committee on Physical Activity, Health, Transportation, and Land Use. Washington, DC.
LSRO (Life Sciences Research Organization). 1990. Core indicators of nutritional state for difficult to sample populations. J Nutr 120(Suppl 11):1559-1660.
Luepker RV, Murray DM, Jacobs DR Jr, Mittelmark MB, Bracht N, Carlaw R, Crow R, Elmer P, Finnegan J, Folsom AR, Grimm R, Hannan PJ, Jeffrey R, Lando H, McGovern P, Mullis R, Perry CL, Pechacek T, Pirie P, Sprafka JM, Weisbrod R, Blackburn H. 1994. Community education for cardiovascular disease prevention: Risk factor changes in the Minnesota Heart Health Program. Am J Public Health 84(9):1383-1393.
Macbeth AG. 1999. Bicycle lanes in Toronto. ITE J 69:38-40, 42, 44, 46.
Maccoby N, Farquhar JW, Wood PD, Alexander J. 1977. Reducing the risk of cardiovascular disease: Effects of a community-based campaign on knowledge and behavior. J Community Health 3(2):100-114.
McMillan TE. 2002. The influence of urban form on a child’s trip to school. Presented at the Association of Collegiate Schools of Planning Annual Conference, Baltimore. Cited in: EPA. 2003. Travel and Environmental Implications of School Siting. EPA 231-R-03-004. Washington, DC: EPA.
McTigue KM, Harris R, Hemphill B, Lux L, Sutton S, Bunton AJ, Lohr KN. 2003. Screening and interventions for obesity in adults: Summary of the evidence for the U.S. Preventive Services Task Force. Ann Intern Med 139(11):933-949.
Mensah GA, Goodman RA, Zaza S, Moulton AD, Kocher PL, Dietz WH, Pechacek TF, Marks JS. 2004. Law as a tool for preventing chronic diseases: Expanding the spectrum of effective public health strategies [Part 2]. Preventing Chronic Disease [Online]. Available: http://www.cdc.gov/pcd/issues/2004/apr/04_0009.htm [accessed April 20, 2004].
Minkler M, Wallerstein N. 2003. Community-Based Participatory Research for Health. San Francisco, CA: Jossey-Bass.
Morland K, Wing S, Diez Roux A, Poole C. 2002a. Neighborhood characteristics associated with the location of food stores and food service places. Am J Prev Med 22(1):23-29.
Morland K, Wing S, Diez Roux A. 2002b. The contextual effect of the local food environment on residents’ diets: The atherosclerosis risk in communities study. Am J Public Health 92(11):1761-1767.
Morris J, Zidenberg-Cherr S. 2002. Garden-enhanced nutrition curriculum improves fourth-grade school children’s knowledge of nutrition and preferences for some vegetables. J Am Diet Assoc 102(1):91-93.
Muntner P, He J, Cutler JA, Wildman RP, Whelton PK. 2004. Trends in blood pressure among children and adults. J Am Med Assoc 291(17):2107-2113.
NACCHO (National Association of County and City Health Officials). 2004. Community Health Status Indicators Project. [Online]. Available: http://www.naccho.org/project2.cfm [accessed July 6, 2004].
Nord M, Andrews M, Carlson S. 2003. Household Food Security in the United States, 2002. Alexandria, VA: USDA, Economic Research Service. Food Assistance and Nutrition Research Report 35.
Painter K. 1996. The influence of street lighting improvements on crime, fear, and pedestrian street use, after dark. Landsc Urban Plan 35:193-201.
Partnership for the Public’s Health. 2004. The Power of Partnership: Improving the Health of California’s Communities. 2003 Annual Report. [Online]. Available: http://www.partnershipph.org/col4/ar/ar03.pdf [accessed July 6, 2004].
Pate RR, Trost SG, Mullis R, Sallis JF, Wechsler H, Brown DR. 2000. Community interventions to promote proper nutrition and physical activity among youth. Prev Med 31:S138-S148.
Patrick K, Sallis JF, Prochaska JJ, Lydston DD, Calfas KJ, Zabinski MF, Wilfley DE, Saelens BE, Brown DR. 2001. A multicomponent program for nutrition and physical activity change in primary care: PACE+ for adolescents. Arch Pediatr Adolesc Med 155(8):940-946.
Pearson TA, Stone EJ, Grundy SM, McBride PE, Van Horn L, Tobin BW, NAA Collaborative Group. 2001. Translation of nutritional sciences into medical education: The Nutrition Academic Award Program. Am J Clin Nutr 74(2):164-170.
Perdue WC, Stone LA, Gostin LO. 2003. The built environment and its relationship to the public’s health: The legal framework. Am J Public Health 93(9):1390-1394.
Perry D. 2001. The Need for More Supermarkets in Philadelphia. Philadelphia, PA: The Food Trust.
Pietinen P, Lahti-Koski M, Vartiainen E, Puska P. 2001. Nutrition and cardiovascular disease in Finland since the early 1970s: A success story. J Nutr Health Aging 5(3):150-154.
Pignone MP, Ammerman A, Fernandez L, Orleans CT, Pender N, Woolf S, Lohr KN, Sutton S. 2003. Counseling to promote a healthy diet in adults: A summary of the evidence for the U.S. Preventive Services Task Force. Am J Prev Med 24(1):75-92.
PolicyLink. 2002. Reducing Health Disparities Through a Focus on Communities. Oakland, CA: PolicyLink. [Online]. Available: http://www.policylink.org/pdfs/HealthDisparities.pdf [accessed July 6, 2004].
Pothukuchi K, Joseph H, Burton H, Fisher A. 2002. What’s Cooking in Your Food System? A Guide to Community Food Assessment. Venice, CA: Community Food Security Coalition.
Powell LM, Slater S, Chaloupka FJ. 2004. The relationship between community physical activity settings and race, ethnicity and socioeconomic status. Evidence-Based Prev Med 1(2):135-144.
Prevention Institute. 2002. Eliminating Health Disparities: The Role of Primary Prevention. [Online]. Available: http://www.preventioninstitute.org/pdf/Health_Disparities.pdf [accessed August 23, 2004].
Prevention Institute. 2003. Environmental and Policy Approaches to Promoting Healthy Eating and Activity Behaviors. Oakland, CA: Prevention Institute.
Puska P, Pietinen P, Uusitalo U. 2002. Influencing public nutrition for non-communicable disease prevention: From community intervention to national programme—Experiences from Finland. Public Health Nutr 5(1A):245-251.
Reed J, Frazao E, Itskowitz R. 2004. How Much Do Americans Pay for Fruits and Vegetables? Agriculture Information Bulletin Number 790. Washington, DC: USDA, Economic Research Service. [Online]. Available: http://www.ers.usda.gov/publications/aib790/aib790.pdf [accessed August 4, 2004].
Retting RA, Ferguson SA, McCartt AT. 2003. A review of evidence-based traffic engineering measures designed to reduce pedestrian-motor vehicle crashes. Am J Public Health 93(9):1456-1463.
Roberts I. 1993. Why have child pedestrian death rates fallen? Br Med J 306(6894):1737-1739.
Robinson TN, Killen JD, Kraemer HC, Wilson DM, Matheson DM, Haskell WL, Pruitt LA, Powell TM, Owens AS, Thompson NS, Flint-Moore NM, Davis GJ, Emig KA, Brown RT, Rochon J, Green S, Varady A. 2003. Dance and reducing television viewing to prevent weight gain in African-American girls: The Stanford GEMS pilot study. Ethn Dis 13(1 Suppl 1):S65-S77.
Romero AJ, Robinson TN, Kraemer HC, Erickson SJ, Haydel KF, Mendoza F, Killen JD. 2001. Are perceived neighborhood hazards a barrier to physical activity in children? Arch Pediatr Adolesc Med 155(10):1143-1148.
Saelens BE, Sallis JF, Black JB, Chen D. 2003. Neighborhood-based differences in physical activity: An environment scale evaluation. Am J Public Health 93(9):1552-1558.
Sallis JF, Nader PR, Broyles SL, Berry CC, Elder JP, McKenzie TL, Nelson JA. 1993. Correlates of physical activity at home in Mexican-American and Anglo-American preschool children. Health Psychol 12(5):390-398.
Sallis JF, McKenzie TL, Elder JP, Broyles SL, Nader PR. 1997. Factors parents use in selecting play spaces for young children. Arch Pediatr Adolesc Med 151(4):414-417.
Sallis JF, Bauman A, Pratt M. 1998. Environmental and policy interventions to promote physical activity. Am J Prev Med 15(4):379-397.
Sallis JF, Prochaska JJ, Taylor WC. 2000a. A review of correlates of physical activity of children and adolescents. Med Sci Sports Exerc 32(5):963-975.
Sallis JF, Patrick K, Frank E, Pratt M, Wechsler H, Galuska DA. 2000b. Interventions in health care settings to promote healthful eating and physical activity in children and adolescents. Prev Med 31(2):S112-S120.
Sanger K, Zenz L. 2004. Farm-to-Cafeteria Connections. Marketing Opportunities for Small Farms in Washington State. Washington State Department of Agriculture, Small Farm and Direct Marketing Program. [Online]. Available: http://agr.wa.gov/Marketing/SmallFarm/102-FarmToCafeteriaConnections-Web.pdf [accessed June 8, 2004].
Schwartz MB, Puhl R. 2003. Childhood obesity: A societal problem to solve. Obes Rev 4(1):57-71.
Shaffer A. 2002. The Persistence of L.A.’s Grocery Gap: The Need for a New Food Policy and Approach to Market Development. Los Angeles, CA: Center for Food and Justice, Urban and Environmental Policy Institute.
Shea S, Basch CE. 1990. A review of five major community-based cardiovascular disease prevention programs. Part II: Intervention strategies, evaluation methods, and results. Am J Health Promot 4(4):279-287.
Sloane DC, Diamant AL, Lewis LB, Yancey AK, Flynn G, Nascimento LM, McCarthy WJ, Guinyard JJ, Cousineau MR. 2003. Improving the nutritional resource environment for healthy living through community-based participatory research. J Gen Intern Med 18(7):568-575.
Smart Growth America. 2004. Smart Growth America. [Online]. Available: http://www.smartgrowthamerica.com/ [accessed April 22, 2004].
Staunton CE, Hubsmith D, Kallins W. 2003. Promoting safe walking and bicycling to school: The Marin County success story. Am J Public Health 93(9):1431-1434.
Stillman FA, Hartman AM, Graubard BI, Gilpin EA, Murray DM, Gibson JT. 2003. Evaluation of the American Stop Smoking Intervention Study (ASSIST): A report of outcomes. J Natl Cancer Inst 95(22):1681-1691.
Story M, Sherwood NE, Himes JH, Davis M, Jacobs DR Jr, Cartwright Y, Smyth M, Rochon J. 2003. An after-school obesity prevention program for African-American girls: The Minnesota GEMS pilot study. Ethn Dis 13(1 Suppl 1):S54-S64.
Sustrans. 2001. Safe Route to Schools. Sustrans Information Sheet FS01. [Online]. Available: http://www.saferoutestoschools.org.uk/imagprod/downloads/fs01.pdf [accessed August 4, 2004].
Taren DL, Thomson CA, Koff NA, Gordon PR, Marian MJ, Bassford TL, Fulginiti JV, Ritenbaugh CK. 2001. Effect of an integrated nutrition curriculum on medical education, student clinical performance, and student perception of medical-nutrition training. Am J Clin Nutr 73(6):1107-1112.
Taylor L, Quigley R. 2002. Health Impact Assessment: A Review of Reviews. London: Health Development Agency. [Online]. Available: http://www.hda-online.org.uk/evidence [accessed May 26, 2004].
Tester JM, Rutherford GW, Wald Z, Rutherford MW. 2004. A matched case-control study evaluating the effectiveness of speed humps in reducing child pedestrian injuries. Am J Public Health 94(4):646-650.
Transportation Alternatives. 2004. Safe Routes to School. [Online]. Available: http://www.saferoutestoschools.org [accessed April 20, 2004].
TRB (Transportation Research Board). 2002. The Relative Risks of School Travel. A National Perspective and Guidance for Local Community Risk Assessment. Washington, DC: TRB.
Tudor-Locke C, Ainsworth BE, Adair LS, Popkin BM. 2003. Objective physical activity of Filipino youth stratified for commuting mode to school. Med Sci Sports Exerc 35(3):465-471.
Twiss J, Dickinson J, Duma S, Kleinman T, Paulsen H, Rilveria L. 2003. Community gardens: Lessons learned from California healthy cities and communities. Am J Public Health 93(9):1435-1438.
Urban and Environmental Policy Institute. 2002. Transportation and Food: The Importance of Access. [Online]. Available: http://departments.oxy.edu/uepi/cfj/resources/TransportationAndFood.htm#_edn2 [accessed June 8, 2004].
USPSTF (U.S. Preventive Services Task Force). 2003. Screening for obesity in adults: Recommendations and rationale. Ann Intern Med 139(11):930-932.
Whitaker RC. 2003. Obesity prevention in pediatric primary care: Four behaviors to target. Arch Pediatr Adolesc Med 157(8):725-727.
WHO (World Health Organization). 1999. Health Impact Assessment: Main Concepts and Suggested Approach. Brussels, Belgium: European Centre for Health Policy.
Wolff T. 2001. Community coalition building—Contemporary practice and research: Introduction. Am J Community Psychol 29(2):165-172, 205-111.
Yancey AK, Kumanyika SK, Ponce NA, McCarthy WJ, Fielding JE, Leslie JP, Akbar J. 2004. Population-based interventions engaging communities of color in healthy eating and active living: A review. Prev Chronic Dis 1(1):1-18. [Online]. Available: http://www.cdc.gov/pcd [accessed August 26, 2004].
Young DR, Haskell WL, Taylor CB, Fortmann SP. 1996. Effect of community health education on physical activity knowledge, attitudes, and behavior. The Stanford Five-City Project. Am J Epidemiol 144(3):264-274.
Zakarian JM, Hovell MF, Hofstetter CR, Sallis JF, Keating KJ. 1994. Correlates of vigorous exercise in a predominantly low SES and minority high school population. Prev Med 23(3):314-321.












































