2
Extent and Consequences of Childhood Obesity
Overall trend data clearly indicate that obesity prevalence in U.S. children and youth has risen to distressing proportions, but many questions remain about the nature, extent, and consequences of this problem. How much do we really know about how this epidemic is unfolding? Which population groups are most affected? What does the available evidence tell us about how to address this problem? Finally, what are the potential consequences of inaction with respect to social, developmental, and health outcomes and the associated health-care system costs? This chapter’s discussion of these questions informs the recommendations throughout the remainder of this report.
PREVALENCE AND TIME TRENDS
Because direct measures of body fat are neither feasible nor available for nationwide assessments of the prevalence of obesity, the National Health and Nutrition Examination Surveys (NHANES),1 conducted by the National Center for Health Statistics, have been using body mass index (BMI) as a surrogate measure for body fatness. The prevalence of childhood and
adolescent obesity is equated to the proportion of those who are in the upper end of the BMI distribution—specifically, at or above the age- and gender-specific 95th percentile of the Centers for Disease Control and Prevention’s (CDC’s) BMI charts for children and youth aged 2 through 19 years2 (Kuczmarski et al., 2000) (see Chapter 3 for a more extensive discussion about the use of terms for childhood overweight and childhood obesity).
If BMI is normally distributed and survey-specific percentile distributions are presented, then by definition, 5 percent of children in each survey will be above the 95th percentile BMI of the survey sample. Thus, reports based on the survey-specific BMI percentiles would always designate 5 percent of children as obese and would fail to detect any true increasing prevalence of obesity across surveys. The CDC therefore developed a revised growth reference in 2000 that established the age- and gender-specific 95th percentile of BMI. The growth reference data were based on BMI distributions from national surveys between 1963 and 1980 for children aged 6 to 19 years, and between 1971 and 1994 for children aged 2 through 5 years (Kuczmarski et al., 2002; Ogden et al., 2002b). There are no BMI-for-age references or accepted definitions for children younger than 2 years of age. However, the Special Supplemental Nutrition Program for Women, Infants and Children (WIC) has defined the term overweight for children under 2 years who are at or above the 95th percentile of weight-for-length and uses this standard for determining WIC program eligibility (Ogden et al., 2002a).
Overall Burden
The term “epidemic” suggests a condition that is occurring more frequently and extensively among individuals in a community or population than is expected. This characterization clearly appears to apply to childhood obesity. In 2000, obesity was two to three times more common in children and youth than in a reference period in the early 1970s. The increase in obesity prevalence has been particularly striking since the late 1970s. The obesity epidemic affects both boys and girls and has occurred in all age, race, and ethnic groups throughout the United States (Ogden et al., 2002a).
The 1999-2000 NHANES found that approximately 10 percent of 2-to 5-year-old children were at or above the 95th percentile of BMI, repre-
|
2 |
The NHANES series use the term “overweight” rather than “obese” to describe all children who are at or above the age- and gender-specific 95th percentile of BMI. However, this report uses the term “obese” to refer to those children (see Chapter 3). |
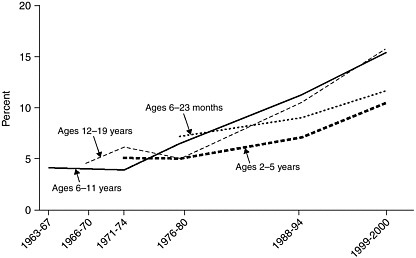
FIGURE 2-1 Age-specific trends in child and adolescent obesity.
NOTE: Obesity is defined as a BMI at or above the age- and gender-specific 95th percentile cutoff points from the 2000 CDC BMI charts. Weight-for-length is used to track children aged 6 to 23 months (under 2 years of age).
SOURCES: Ogden et al., 2002a; CDC, 2003.
senting twice the expected percentage; and that more than 15 percent of 6-to 19-year-olds met this criterion, representing about three times the expected percentage (Ogden et al., 2002a). No significant increases in obesity prevalence were reported between the 1999-2000 and the 2001-2002 NHANES (Hedley et al., 2004).
A significant, unabated increase in the prevalence of childhood obesity across all age groups is clearly seen in an analysis of serial national surveys from the early 1970s through the year 2000 (Figure 2-1). In the nearly 30 years between the 1971-1974 NHANES and the 1999-2000 NHANES, the prevalence of childhood obesity more than doubled for youth aged 12 to 19 years (from 6.1 percent to 15.5 percent) and more than tripled for children aged 6 to 11 years (4 percent to 15.3 percent). Even for preschool children, aged 2 to 5 years, the prevalence also more than doubled (5 percent to 10.4 percent) between these two national surveys (Ogden et al., 2002a). Data for children younger than 2 years of age, based on weight-for-length data available from NHANES II (6-23 months) onward also suggest an upward trend (Ogden et al., 2002a).
The same trends, stratified by gender, are shown in Figure 2-2 for infants and preschool children and in Figure 2-3 for school-aged children and adolescents. Among children older than 2 years of age, the increased prevalence of obesity over time has occurred to a similar degree in both
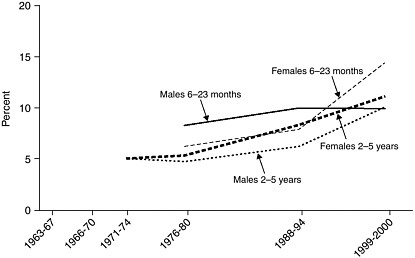
FIGURE 2-2 Trends in infant and child obesity, boys and girls aged 6 months through 5 years.
NOTE: Obesity is defined as a BMI at or above the age- and gender-specific 95th percentile cutoff points from the 2000 CDC BMI charts. Weight-for-length is used to track children aged 6 to 23 months (under 2 years of age).
SOURCE: Ogden et al., 2002a.
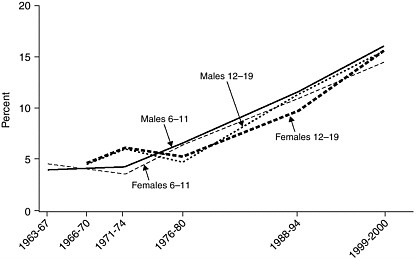
FIGURE 2-3 Trends in child and adolescent obesity, girls and boys aged 6 through 19 years.
NOTE: Obesity is defined as a BMI at or above the age- and gender-specific 95th percentile cutoff points from the 2000 CDC BMI charts.
SOURCES: Ogden et al., 2002a; CDC, 2003.
boys and girls. However, in those children under 2 years of age,3 the increased prevalence is more marked in girls than in boys.
High-Risk Population Subgroups
Although no demographic group in the United States has been untouched by the childhood obesity epidemic, there is evidence that some subgroups of the U.S. population have been affected more than others. As discussed below, certain ethnic minority populations, children in low-socioeconomic-status families, and children in the country’s southern region tend to have higher rates of obesity than the rest of the population. Either the factors driving the obesity epidemic are more pronounced in these high-risk populations and communities, or their children and adolescents may be more sensitive to, or less able to avoid, the causal factors when present. Additional efforts will be needed to identify the nature of the risk for obesity in these high-risk population subgroups.
High-Risk Ethnic Groups
Cross-sectional population-based estimates of obesity prevalence at 6 to 19 years of age are available for U.S. children and adolescents overall, and specifically for non-Hispanic blacks, non-Hispanic whites, and Mexican Americans (Figure 2-4).4
Although obesity is prevalent among children and youth throughout the entire population, Hispanic, non-Hispanic black, and Native-American children and adolescents are disproportionately affected when compared to the general population (Ogden et al., 2002a). With both sexes combined, up to 24 percent of non-Hispanic black and Mexican-American adolescents are above the 95th percentile. Among boys, the highest prevalence of obesity is observed in Mexican Americans and among girls, the highest prevalence is observed in non-Hispanic blacks (Ogden et al., 2002a). American-
|
3 |
There are no BMI-for-age references or accepted definitions for children younger than 2 years of age. Weight-for-length greater than the 95th percentile is used by the CDC and the WIC program to define overweight in children under 2 years of age (see Chapter 3). |
|
4 |
Standard terms used in the NHANES series include non-Hispanic whites, non-Hispanic blacks, and Mexican Americans. The ethnic and racial categories discussed throughout this chapter use those that specific researchers used for different data sets. This report generally uses the terms African Americans to refer to non-Hispanic blacks; Hispanics to refer to Mexican Americans and populations from other Latin-American countries of Hispanic descent; American Indians to refer to Native Americans; and whites to refer to non-Hispanic whites. The report also uses the term Asian/Pacific Islanders (which includes Native Hawaiians). |
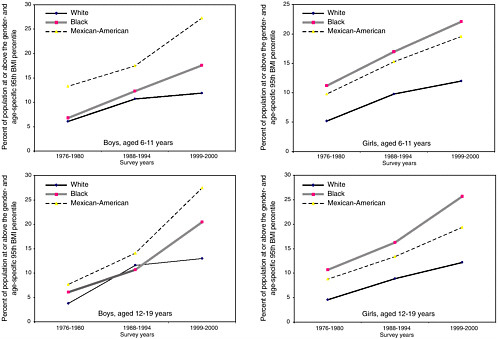
FIGURE 2-4 Trends in obesity prevalence for non-Hispanic white, non-Hispanic Black, and Mexican-American boys and girls.
NOTE: Obesity is defined as a BMI at or above the age- and gender-specific 95th percentile cutoff points from the 2000 CDC BMI charts. The following datapoints have a relative standard error of 20 to 30 percent: 1999-2000 boys, aged 6 to 11 years (white); 1999-2000 girls, aged 6 to 11 years (white); 1988-1994 girls, aged 6 to 11 years (white); 1988-1994 girls, aged 12 to 19 years (Mexican American).
Indian children and youth, although not reported separately in the NHANES data, are also particularly affected by obesity (Caballero et al., 2003). For example, the prevalence of obesity in 7-year-old American-Indian children has been estimated recently at nearly 30 percent, representing twice the current estimated prevalence among all U.S. children of that age (Caballero et al., 2003).
Moreover, ethnicity-specific plots of the cross-sectional NHES and NHANES data for children aged 6 to 19 years suggest accelerated rates of increase in obesity prevalence for non-Hispanic black and Mexican-American children of both sexes (Figure 2-4), creating a disparity in obesity prevalence between non-Hispanic white and black children (particularly among girls) (CDC, 2003).
Additional evidence that some ethnic disparities for obesity are increasing over time is drawn from the National Longitudinal Survey of Youth (NLSY). Between 1986 and 1998, the prevalence of obesity increased 120 percent among African Americans and Hispanics while it increased 50 percent among non-Hispanic whites (Strauss and Pollack, 2001).
Socioeconomic Difference
Evidence also suggests significant variation in BMI as a function of both socioeconomic status and ethnicity based on NHANES III in girls aged 6 to 9 years (Winkelby et al., 1999). An increase in obesity prevalence among African Americans appears greatest for those at the lowest income (Strauss and Pollack, 2001). But uncertainties remain. These disparities are not the same across ethnic groups and they do not emerge at comparable times during childhood. Also, there is almost no consensus, despite many theories, about the mechanisms by which they occur. For instance, analysis of the data from the 1988-1994 NHANES shows that the prevalence of obesity in white adolescents is higher among those in low-income families but there is no clear relationship between family income and obesity in other age or ethnic subgroups (Troiano and Flegal, 1998; Ogden et al., 2003).
Nonetheless, two analyses of nationally representative longitudinal data—the NLSY (Strauss and Knight, 1999; Strauss and Pollack, 2001) and the National Longitudinal Study of Adolescent Health (Goodman, 1999; Goodman et al., 2003)—have suggested that family socioeconomic status is inversely related to obesity prevalence in children and that the effects of socioeconomic status and race or ethnicity were independent of other variables.
One explanation is insurance status, which is related to socioeconomic status; the uninsured may face barriers to accessing health care (Haas et al., 2003). Insurance coverage has been associated with the prevalence of obe-
sity in youth. An analysis of the 1996 Medical Expenditure Panel Survey Household Component found that a combination of lacking health insurance and having public insurance (Medicaid, Medicare, or other public hospital coverage) were directly associated with obesity among adolescents (Haas et al., 2003).
Regional Differences
Regional differences in the prevalence of U.S. childhood obesity were already apparent in 1998 based on NLSY data (10.8 percent in western states and 17.1 percent in southern states) (Strauss and Pollack, 2001). However, most data available for regional differences are for adults. In 1998, adult obesity prevalence based on the CDC Behavioral Risk Factor Surveillance System (BRFSS) exceeded 20 percent in several states—Alabama (20.7 percent), Alaska (20.7 percent), Louisiana (21.3 percent), South Carolina (20.2 percent) and West Virginia (22.9 percent)—predominantly in the Southeast (Mokdad et al., 1999). By 2002, BRFSS data revealed that seven states had adult obesity prevalence rates greater than 25 percent: Alabama, Louisiana, Michigan, Mississippi, South Carolina, Texas, and West Virginia (CDC, 2002). Systematic data reflecting regional differences in obesity prevalence for children and youth are currently not available.
Shifts in the Population BMI Distribution
Researchers can monitor changes in the nature of the obesity epidemic by comparing the BMI distribution curves derived from population-based surveys and noting shifts in any particular distribution over time. A shift toward higher BMIs over the entire distribution would indicate that virtually everyone is becoming heavier, with lean individuals gradually moving into the overweight range, overweight individuals moving into the obese range, and the number of obese individuals becoming more severely obese. However, a graphical analysis comparing NHANES III (1988-1994) with earlier data found that the distributional patterns of BMIs differed among age groups (Flegal and Troiano, 2000).
For adults, there was a general shift upward in the BMI distribution, with the greatest shift occurring at the upper end of the distribution, reflected by the heaviest subgroups becoming heavier. For younger children aged 6 to 11 years, and to a lesser extent in adolescents, the distributions of BMI values were characterized by little or no difference in the lower part of the distribution, though there was also a greater shift at the upper end, as shown schematically in Figures 2.5a and 2.5b (Flegal and Troiano, 2000). The results of this study indicate that the heaviest children and youth were heavier in NHANES III than in earlier surveys; the authors caution, how-
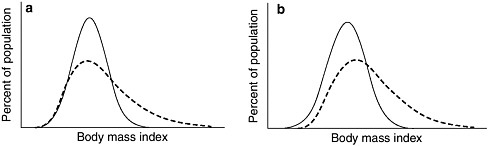
FIGURE 2-5 Schematic representations of BMI distribution models.
NOTE: Figure 2-5a shows a schematic representation of increased skewness (lack of symmetry) at the upper end of the BMI distribution with little change at the lower end, as has been observed in U.S. children and adolescents. Figure 2-5b shows a schematic representation of both a rightward shift in the distribution and increased skewness at the upper end of the distribution, as has been observed in U.S. adults.
SOURCE: Reprinted, with permission, from Flegal and Troiano, 2000. Copyright 2000 by the International Journal of Obesity and Related Metabolic Disorders.
ever, that the unweighted sample sizes for 6- to 17-year-olds, particularly for adolescents, are small (Flegal and Troiano, 2000). Strauss and Pollack (2001) came to a similar conclusion based on their analyses of NLSY data.
Changes in BMI distributions have impacts on the population’s health. In adults, the major health-related co-morbidities that occur with obesity do not have a linear relationship with BMI. For example, although relationships between BMI and hypertension, diabetes, dyslipidemia, and even death occur across a wide range of BMIs, these relationships strengthen considerably at the highest levels of BMI (Solomon and Manson, 1997; Must et al., 1999).
Similarly, children at the highest levels of BMI are generally at the greatest risk of adverse health outcomes. Elevated blood pressure and insulin were both observed to be twice as common in children with BMIs above the 97th percentile as in children within the 95th to 97th percentile (Freedman et al., 1999). But the prevalence of these health outcomes is low between the 25th and 75th BMI percentiles, increasing modestly, if at all, across that span. Thus, with the childhood obesity epidemic characterized by a disproportionate number of children at the extreme ranges of BMI, there are likely to be higher obesity-related morbidity rates in children than if the epidemic mostly resulted from an upward shift in BMI across their entire population.
Relationship Between the Childhood and Adult Obesity Epidemics
The obesity epidemic that began in the early 1970s and escalated after 1980 for children and youth has progressed similarly in adults over the same time period. As depicted in Figures 2-6 and 2-7, between the 1971-1974 NHANES and the 1999-2000 NHANES the prevalence of obesity—defined as a BMI at or above 30 kg/m2—more than doubled (from 14.5
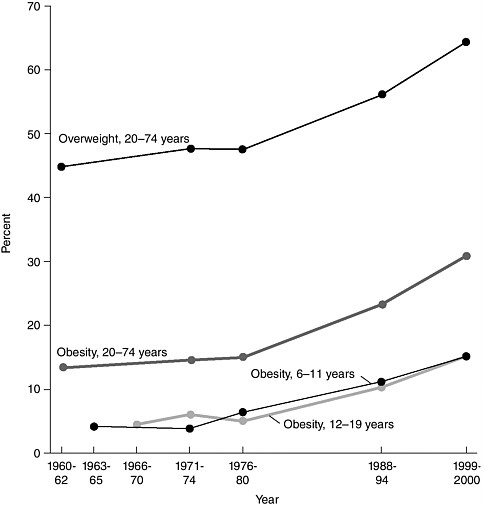
FIGURE 2-6 Overweight and obesity by age in the United States, 1960-2000.
NOTE: Percents for adults are age-adjusted. Obesity for children is defined as a BMI at or above the age- and gender-specific 95th percentile BMI cutpoints from the 2000 CDC BMI charts. Obesity for adults is defined as a BMI greater than or equal to 30. Obesity is a subset of the percent of overweight.
SOURCE: CDC, 2003.
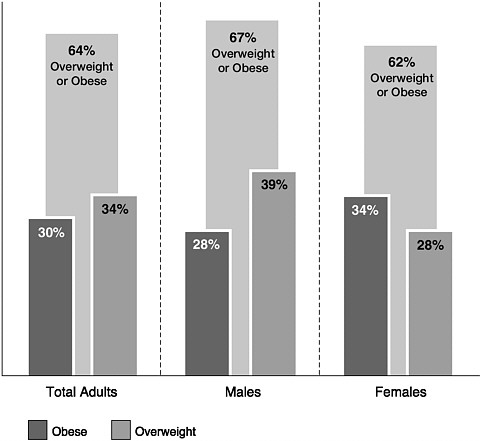
FIGURE 2-7 Prevalence of overweight and obesity among adults 20 years of age and older, NHANES 1999-2000.
SOURCE: CDC, 2003. Reprinted with permission from Salinsky and Scott, 2003. Copyright by the National Health Policy Forum.
percent to 30.5 percent) among 60 million U.S. adults. Between 1999-2000 and 2001-2002 there were no significant changes in the prevalence of obesity in adults (30.5 percent versus 30.6 percent) (Hedley et al., 2004). These trends, underscored by similar findings at the state level (Mokdad et al., 2001), have paralleled childhood and youth obesity prevalence, suggesting that the epidemics may be linked.
The observation that children and adults are both experiencing epidemics of obesity over the same time frame has important implications for understanding causes and formulating prevention interventions. Many of the same sociocultural factors that have contributed to the adult obesity epidemic have likely contributed to the childhood obesity epidemic.
The average parents today are twice as likely to be obese as 30 years
ago, even though their genetic susceptibility and that of their child has not changed over this period. Parental obesity more than doubles the risk of adult obesity among both obese and nonobese children under 10 years of age (Whitaker et al., 1997). For example, an obese preschool child with normal weight parents has approximately a 25 percent chance of being obese as an adult. However, this same preschool child with an obese parent has more than a 60 percent chance of being an obese adult (Whitaker et al., 1997). An additional implication of the adult and childhood obesity co-epidemics relates to intergenerational transmission. There are a number of potential mechanisms by which maternal obesity in pregnancy may promote offspring obesity (Whitaker and Dietz, 1998; Levin, 2000; Oken and Gillman, 2003), and further research is needed to examine these mechanisms.
Children can inherit obesity susceptibility genes from an obese parent or parents, or can be exposed, after birth, to diet and activity patterns that promote obesity. Moreover, recent research suggests that an altered intrauterine environment may be a third mechanism (see Chapter 8). For example, obese mothers are more likely to experience diabetes in pregnancy, and some evidence suggests that the offspring of mothers who have diabetes in pregnancy may have an increased risk of developing obesity later in life (Silverman et al., 1998).
In a study of low-income families enrolled in the WIC program, children born to mothers who were obese at the time of conception were twice as likely to be obese at 4 years of age (Whitaker, 2004b). Although much remains to be learned about the mechanisms of intergenerational obesity, these data suggest that it may be important to consider the promotion of healthy body weights among pregnant mothers as part of childhood obesity prevention efforts, and obesity research efforts should examine prevention interventions for pregnant mothers who are obese as well as for their children.
CONSIDERING THE COSTS FOR CHILDREN AND FOR SOCIETY
The primary concern about childhood obesity is its potential impact on well-being, not only in childhood but into adulthood, with the term “well-being” reflecting the committee’s view that social and emotional health is as important as physical health. As discussed in Chapter 1, families may differ in the value they place on the different health outcomes of obesity, and the merits they attribute to certain benefits or drawbacks of changing behaviors to address it (Whitaker, 2004a). Research suggests that some parents do not perceive weight to be a health issue for their children (Baughcum et al., 2000; Jain et al., 2001; Borra et al., 2003), independent of their child’s physical and social functioning. Thus, individuals may differ in the value
they place on various aspects of their well-being (Buchanan, 2000). Depending on these values, childhood obesity may represent a greater concern to some than to others. Failing to reverse the trend in childhood obesity means that many obese children, over their lifetimes, could experience significant impairments in multiple domains of functioning. They are more likely to be chronically ill, to have a negative impact on their earning potential, and to even die prematurely.
Social and Emotional Health
While childhood obesity may not result in recognized clinical symptoms until later in life, the social and emotional correlates often have immediate effects on children’s lives. Research on the short- and long-term impacts of obesity on children’s emotional and social functioning has been extensively reviewed (French et al., 1995; Dietz, 1998b; Must and Strauss, 1999; Puhl and Brownell, 2001; Styne, 2001; Must and Anderson, 2003; Schwartz and Puhl, 2003), and the collective body of research clearly indicates that obese children and youth are stigmatized, and subject to negative stereotyping and discrimination by their peers (Schwartz and Puhl, 2003; Strauss and Pollack, 2003).
This sort of treatment, which is hypothesized to produce adverse emotional consequences such as low self-esteem, negative body image, and depressive symptoms for obese children, is not limited to peers; it may also come from adults, including parents, teachers, and health-care providers (Strauss et al., 1985). Even though obesity in children has become more common, such negative treatment has not diminished (Latner and Stunkard, 2003), as revealed by obese children who continue to be socially marginalized by their peers (Strauss and Pollack, 2003).
The results of studies on the emotional well-being of obese children are difficult to succinctly summarize, given the differences between studies. Variations include the outcome measures used, the characteristics of the study subjects (particularly age, gender, racial/ethnic status, and degree of obesity), and whether the samples were clinical or community-based. Furthermore, because many of the study designs are cross-sectional, it is often impossible to distinguish between time course, and impossible to determine whether the associations are causal. Nonetheless, a few general statements can be made.
In one longitudinal study, associations between obesity and low self-esteem appear to emerge by early adolescence and were strongest in Hispanic and white adolescent girls but not in African-American girls (Strauss, 2000). The emotional consequences are somewhat stronger in girls than in boys, increase with age, and may be greater in those obese children who seek treatment (Schwartz and Puhl, 2003). Having concerns about being
obese, regardless of actual body weight, appears to be a primary factor associated with depressive symptoms among preadolescent girls (Erickson et al., 2000).
The social and emotional impacts of obesity can also be long term. In a longitudinal U.S. cohort with a seven-year follow-up, women 16 to 24 years of age at baseline who had been overweight completed fewer years of school, earned less money, and were less likely to be married (Gortmaker et al., 1993). The impact of adolescent obesity on the subsequent lower earnings of women was also demonstrated in a British cohort study (Sargent and Blanchflower, 1994).
Physical Health
Several thorough reviews (Dietz, 1998a,b; Must and Strauss, 1999; Deckelbaum and Williams, 2001; Styne, 2001; Must and Anderson, 2003) have found childhood obesity to be associated with a wide array of disorders that affect multiple organ systems. These disorders include hypertension, dyslipidemia, glucose intolerance/insulin resistance, hepatic steatosis, cholelithiasis, sleep apnea, menstrual abnormalities, impaired balance, and orthopedic problems. Some of these conditions produce clinical symptoms in obese children, while others do not; however, the metabolic and physiologic changes associated with childhood obesity, along with the obesity itself, tend to track into adult life and eventually enhance the risks of disease, disability, and death.
In 2000, it was estimated that 400,000 deaths were attributed to poor diet and physical inactivity in the United States (Mokdad et al., 2004), an increase of one-third from 300,000 annual deaths attributed to diet and sedentary activities in 1990 (McGinnis and Foege, 1993). Although these risk factors represent the second leading cause of deaths among Americans, diet and physical inactivity are predicted to exceed tobacco as the leading cause of deaths in the future (Mokdad et al., 2004).
Of the multiple health correlates of the childhood obesity epidemic, perhaps the one that has received greatest attention is the increased prevalence of type 2 diabetes in children.5 By one population-based estimate from southwestern Ohio, a ten-fold increase in the prevalence of type 2 diabetes in children between 1982 and 1994 accounted for one-third of all new cases of diabetes (including type 1 and type 2) in children by 1994 (Pinhas-Hamiel et al., 1996). For individuals born in the United States in 2000, the lifetime risk of being diagnosed with diabetes at some point in their lives is estimated at 30 percent for boys and 40 percent for girls if
obesity rates level off (Narayan et al., 2003). Nearly all children with type 2 diabetes are obese, and a disproportionate number are Native American, African American, Hispanic, or Asian/Pacific Islander (Fagot-Campagna et al., 2000; Goran et al., 2003; Davis et al., 2004).
Several risk factors—including increased body fat (especially abdominal fat), insulin resistance, ethnicity, and the onset of puberty—have been identified as contributors to the development of type 2 diabetes, and they appear to have an additive influence (Goran et al., 2003). Accurate estimates of the prevalence of diabetes in U.S. children are difficult to determine. It has been estimated that the prevalence of diabetes is 0.41 percent in U.S. youth aged 12-19 years (approximately 100,000 U.S. adolescents) and the prevalence of impaired fasting glucose is 1.76 percent (approximately 500,000 U.S. adolescents) (Fagot-Campagna et al., 2001). Better estimates for children are not possible because the prevalence of type 2 diabetes in this population is still relatively low. NHANES is the only current national data collection effort that could potentially make such an estimate. However, the sample sizes from NHANES are not large enough to make a stable point estimate of the prevalence.
The childhood obesity epidemic may result in increased risk of type 2 diabetes. One study found that for each adolescent diagnosed with type 2 diabetes, there are 5 others with impaired fasting glucose, an indicator of insulin resistance below the diagnostic threshold for type 2 diabetes (Fagot-Campagna et al., 2001). Furthermore, the degree of insulin resistance in children increases with the severity of body fatness, as it does in adults (ADA, 2000). Thus, the combination of more obese children and the increased severity of obesity suggests that larger numbers of children will reach the diagnostic threshold for type 2 diabetes. Finally, it is estimated that approximately three-fourths of obese adolescents will be overweight as young adults (Guo et al., 2002) and will likely face the persistent risk of developing type 2 diabetes.
The increased prevalence of obesity among adults of all ages also has been associated with a similar increase in the prevalence of diabetes (Mokdad et al., 2001). In fact, the increase in diabetes prevalence has been greatest in young adults aged 30 to 39 years, with prevalence almost doubling between 1990 and 2001 (Mokdad et al., 2000, 2003). Moreover, the development of all of the major complications of diabetes, including retinopathy, nephropathy, and neuropathy, are related to duration of disease. Those who develop diabetes earlier in life generally will develop costly complications earlier with the potential for premature mortality. For example, among 79 individuals in a Canadian referral clinic who were diagnosed with type 2 diabetes before the age of 17 and who were followed up from ages 18 to 33 years, two had died suddenly while on dialysis and three more were currently receiving dialysis (Dean and Flett, 2002).
A potentially even more important complication of childhood obesity may be the metabolic syndrome, diagnosed when a person has at least three of five metabolic abnormalities: glucose intolerance, abdominal obesity, hypertriglyceridemia, low high-density lipoprotein (HDL) cholesterol, and high blood pressure (NHLBI, 2002). The metabolic syndrome is now present in approximately one-quarter of all U.S. adults (Ford et al., 2002; Park et al., 2003) and in nearly 30 percent of U.S. children and youth who are obese (Cook et al., 2003).
Among adults, the metabolic syndrome is associated not only with type 2 diabetes (Haffner et al., 1992; Cook et al., 2003) but also with cardiovascular disease (Isomaa et al., 2001; Cook et al., 2003) and a higher mortality rate (Lakka et al., 2002; Cook et al., 2003). Even among those obese youth who do not yet have clinical diabetes, components of the metabolic syndrome appear to contribute to the development of atherosclerosis (Mahoney et al., 1996; Berenson et al., 1998; McGill et al., 2002). Ultimately, it may be the association of childhood obesity with the metabolic syndrome, rather than exclusively with diabetes, that may comprise the greatest physical health threat of childhood obesity.
It is possible that if the childhood obesity epidemic continues at its current rate, conditions related to type 2 diabetes—such as blindness, amputation, coronary artery disease, stroke, and kidney failure—will become ordinary in middle-aged people. Additionally, risk factors for cancer in obese adults, such as hormone alterations, may be present in obese children and contribute to a higher incidence of certain types of cancer later in life (Gascon et al., 2004). Thus, these conditions may affect a greater proportion of the population than current morbidity. This is a serious prospect given that obesity accounts for a level of morbidity comparable to that of smoking and poverty (Sturm and Wells, 2001).
Integrated View of the Consequences of Childhood Obesity
In reviews of the correlates of childhood obesity, discussions of the physical impacts and of the social and emotional impacts are often separate. But this distinction may be artificial. First, although the brain plays a central role in the regulation of energy balance and obesity (Schwartz et al., 2000), it is also the central organ for integrating social stimuli, regulating emotion, and executing social interaction. Not surprisingly, cues that affect both eating and activity behaviors are often social in nature, ranging from sadness to anxiety to boredom.
Social and emotional factors must therefore be recognized not only as potential consequences of obesity but also as potential causes. For example, depressed mood in children and adolescents may precede the development of obesity and not just follow it (Pine et al., 2001; Goodman and Whitaker,
2002; Richardson et al., 2003). In a nationally representative sample of 8-to 11-year-olds, clinically meaningful behavioral problems have been shown to be associated with the development of obesity over a 2-year period among children not obese at baseline (Lumeng et al., 2003). Affective factors, such as depressive symptoms, are also the likely mediators of the observed association between adult obesity and traumatic childhood experiences (e.g., physical abuse, sexual abuse) (Williamson et al., 2002).
There is accruing evidence that even the metabolic syndrome itself may be a consequence of how the brain processes environmental stimuli that are social in nature. For instance, the brain’s response to stress may alter the hypothalamic-pituitary-adrenal (or gonadal) axis in a way that promotes central fat deposition and insulin resistance in adults (Bjorntorp, 2001). Because children also experience stress, the part of the brain that regulates emotion may not only influence whether a child overeats, but also the metabolic consequences of that excess energy.
The fact that the physiologic response to stress is conditioned in childhood (Gunnar and Donzella, 2002) emphasizes the potential importance of optimizing the social and emotional health of children as a strategy for preventing obesity over a lifetime. Failure to recognize this connection between social or emotional health and physical health could result in prevention strategies that are poorly conceptualized, and underscores the need to consider the broadest possible definition of health to include the physical, mental, and emotional aspects (Table 2-1), because the foundations of all three develop during childhood and are interconnected.
Health-Care Costs
A RAND study has calculated that the costs imposed on society by people with sedentary lifestyles (i.e., the “external” costs generated) may be greater than those imposed by smokers (Keeler et al., 1989). More recent computations of national health-care expenditures related to obesity and overweight in adults showed large lifetime external costs related to these conditions. After adjusting for inflation and converting estimates to 2004 dollars, the national direct and indirect health-care costs related to overweight and obesity range from $98 billion (Finkelstein et al., 2003) to $129 billion (DHHS, 2001a).6 It has been suggested that overweight and obesity may account for nearly one-third (27 to 31 percent) of total direct costs related to 15 co-morbid diseases (Lewin Group, 2000) and account for 9
TABLE 2-1 Physical, Social, and Emotional Health Consequences of Obesity in Children and Youth
|
Physical Health
|
|
Emotional Health
|
|
Social Health
|
percent of total U.S. medical spending (Finkelstein et al., 2003). Less than a decade ago, by contrast, the estimated direct health-care costs attributable to obesity ranged from 1 to 6 percent of total health-care expenditures, depending on the definition of obesity and the methods of calculation used (Seidell, 1995; Wolf and Colditz, 1998). Annual medical expenditures in the United States related to obesity are estimated at $75 billion (in 2003 dollars) with approximately half of the expenditures financed by Medicaid and Medicare (Finkelstein et al., 2004). California, the most populous state, spent the most in public funds on health care for obese people in that year, a total of $7.7 billion (Finkelstein et al., 2004).
The direct health-care costs of physical inactivity, which contribute to the obesity epidemic, have been estimated to exceed $77 billion annually (Pratt et al., 2000). In addition, there are indirect costs of physical inactivity, such as those associated with dependence on motorized travel. For example, the national cost of traffic congestion in 2002 was estimated at 3.5 billion hours of delay, costing the nation $69.5 billion—an increase of $4.5 billion from the previous year (Schrank and Lomax, 2003).
Additionally, the estimated national health-care expenditures for Americans with diabetes exceeded $132 billion in 2002, and it has been suggested
that people with diabetes have health-care costs that are on average 2.4 times higher than those of people without diabetes (ADA, 2003). Obesity-linked type 2 diabetes, by far the most common form of the disease, is largely preventable. The cost of obesity has recently been compared to other health-care costs, and research suggests that it outranks both smoking and drinking in adverse health effects and health-care costs, adding an average of $395 per patient per year to health-care costs (Sturm, 2002).
The direct economic burden of obesity in youth aged 6 to 17 years has been estimated, based on the 1979-1999 National Hospital Discharge Survey (Wang and Dietz, 2002). Obesity-associated hospital costs were determined from hospital discharges that listed obesity as either the primary or secondary diagnosis. Results indicate that the percentage of discharges with obesity-related diseases increased dramatically from 1979-1981 to 1997-1999. Discharges for diabetes doubled, gallbladder disease tripled, and sleep apnea increased five-fold during this time frame. In 2001 dollars, obesity-associated annual hospital costs for children and youth were estimated to have more than tripled from $35 million (1979-1981) to $127 million (1997-1999) (Wang and Dietz, 2002).
In 2000, the United States spent approximately 14 percent of its gross national product on health care—representing the largest share for any developed country over the past decade—and its per capita health-care expenditures were greater than those of any other nation (OECD Health Data, 2003). But although it is estimated that preventive measures could impact 70 percent of the causes of early deaths in the United States (McGinnis et al., 2002), most of the $1.4 trillion that the United States spends per year on health is used for direct medical care service. The national investment in preventing disease and promoting health is estimated to be only 5 percent of the total annual health-care costs (DHHS, 2001b; Kelley et al., 2004). This imbalance underscores the need for the health-care systems in the United States to establish a greater preventive orientation (Mokdad et al., 2004), particularly for childhood obesity, a largely preventable condition that has been shown to be a major determinant of healthcare costs.
SUMMARY
Representative population surveys have found significant increases in the prevalence of obesity in U.S. children and youth. In 2000, childhood obesity was two to three times more common than in the early 1970s. Certain subpopulations of children, including those in several ethnic minority populations, in low-socioeconomic-status families, and in the southern region of the United States, tend to be most affected. Furthermore, there are
particular concerns that the heaviest children are becoming heavier (i.e., a skewing of the population BMI distribution).
Obesity can have adverse impacts on a child’s physical, social, and emotional well-being. It increases the incidence of type 2 diabetes and other chronic medical and psychosocial conditions. Furthermore, the metabolic and physiologic changes associated with childhood obesity, along with obesity itself, tend to track into adult life and eventually increase the individual’s risk of disease, disability, and death.
Poor diet and physical inactivity contributed to an estimated 400,000 deaths that occurred in the U.S. population in 2000 (Mokdad et al., 2004); predictions indicate that diet and physical inactivity will ultimately overtake tobacco as the leading cause of death in the future. Obesity-associated annual hospital costs for children and youth were estimated to have more than tripled over a two-decade period, rising from $35 million (1979-1981) to $127 million (1997-1999).7 Meanwhile, after adjusting for inflation and converting estimates to 2004 dollars, the national direct and indirect healthcare expenditures related to adult obesity and overweight range from $98 billion to $129 billion. These figures clearly implicate obesity as a major determinant of health-care costs.
REFERENCES
ADA (American Diabetes Association). 2000. Type 2 diabetes in children and adolescents. Pediatrics 105(3):671-680.
ADA. 2003. Economic costs of diabetes in the U.S. in 2002. Diabetes Care 26(3):917-932.
Baughcum AE, Chamberlin LA, Deeks CM, Powers SW, Whitaker RC. 2000. Maternal perceptions of overweight preschool children. Pediatrics 106(6):1380-1386.
Berenson GS, Srinivasan SR, Bao W, Newman WP 3rd, Tracy RE, Wattigney WA. 1998. Association between multiple cardiovascular risk factors and atherosclerosis in children and young adults: The Bogalusa Heart Study. N Engl J Med 338(23):1650-1656.
Bjorntorp P. 2001. Do stress reactions cause abdominal obesity and comorbidities? Obes Rev 2(2):73-86.
Borra ST, Kelly L, Shirreffs MB, Neville K, Geiger CJ. 2003. Developing health messages: Qualitative studies with children, parents, and teachers help identify communications opportunities for healthful lifestyles and the prevention of obesity. J Am Diet Assoc 103(6):721-728.
Buchanan DR. 2000. An Ethic for Health Promotion. New York: Oxford University Press.
Caballero B, Himes JH, Lohman T, Davis SM, Stevens J, Evans M, Going S, Pablo J. 2003. Body composition and overweight prevalence in 1704 schoolchildren from 7 American Indian communities. Am J Clin Nutr 78:308-312.
CDC (Centers for Disease Control and Prevention). 2002. Behavioral Risk Factor Surveillance System Survey Data: Risk Factors and Calculated Variables–2002. Atlanta, GA: U.S. Department of Health and Human Services, CDC. [Online]. Available: http://apps.nccd.cdc.gov/brfss/list.asp?cat=RF&yr=2002&qkey=4409&state=All [accessed June 11 2004].
CDC. 2003. Health, United States, 2003 with Chartbook on Trends in the Health of Americans. [Online]. Available: http://www.cdc.gov/nchs/data/hus/hus03.pdf [accessed May 17, 2004].
Cook S, Weitzman M, Auinger P, Nguyen M, Dietz WH. 2003. Prevalence of a metabolic syndrome phenotype in adolescents: Findings from the Third National Health and Nutrition Examination Survey, 1988-1994. Arch Pediatr Adolesc Med 157(8):821-827.
Davis J, Busch J, Hammatt Z, Novotny R, Harrigan R, Grandinetti A, Easa D. 2004. The relationship between ethnicity and obesity in Asian and Pacific Islander populations: A literature review. Eth Dis 14(1):111-118.
Dean HJ, Flett B. 2002. Natural history of type 2 diabetes diagnosed in childhood: Long-term follow-up in young adult years. Diabetes 51:A24-A25.
Deckelbaum RJ, Williams CL. 2001. Childhood obesity: The health issue. Obes Res 9(S4):239S-243S.
DHHS (U.S. Department of Health and Human Services). 2001a. The Surgeon General’s Call to Action to Prevent and Decrease Overweight and Obesity. Rockville, MD: Public Health Service, Office of the Surgeon General.
DHHS. 2001b. Steps to a Healthier U.S. Washington, DC: Office of Public Health Promotion. [Online]. Available: http://www.healthierus.gov/steps/steps_brochure.pdf [accessed June 18, 2004].
Dietz WH. 1998a. Childhood weight affects adult morbidity and mortality. J Nutr 128(2S):411S-414S.
Dietz WH. 1998b. Health consequences of obesity in youth: Childhood predictors of adult disease. Pediatrics 101(3):518-525.
Erickson SJ, Robinson TN, Haydel KF, Killen JD. 2000. Are overweight children unhappy? Body mass index, depressive symptoms, and overweight concerns in elementary school children. Arch Pediatr Adolesc Med 154(9):931-935.
Fagot-Campagna A, Saaddine JB, Engelgau MM. 2000. Is testing children for type 2 diabetes a lost battle? Diabetes Care 23(9):1442-1443.
Fagot-Campagna A, Saaddine JB, Flegal KM, Beckles GL. 2001. Diabetes, impaired fasting glucose, and elevated HbA1c in U.S. adolescents: The Third National Health and Nutrition Examination Survey. Diabetes Care 24(5):834-837.
Finkelstein EA, Fiebelkorn IC, Wang G. 2003. National medical spending attributable to overweight and obesity: How much, and who’s paying? Health Aff (Millwood) 22:W3-219-226.
Finkelstein EA, Fiebelkorn IC, Wang G. 2004. State-level estimates of annual medical expenditures attributable to obesity. Obes Res 12(1):18-24.
Flegal KM, Troiano RP. 2000. Changes in the distribution of body mass index of adults and children in the US population. Int J Obes Relat Metab Disord 24(7):807-818.
Ford ES, Giles WH, Dietz WH. 2002. Prevalence of the metabolic syndrome among US adults: Findings from the Third National Health and Nutrition Examination Survey. J Am Med Assoc 287(3):356-359.
Freedman DS, Dietz WH, Srinivasan SR, Berenson GS. 1999. The relation of overweight to cardiovascular risk factors among children and adolescents: The Bogalusa Heart Study. Pediatrics 103(6):1175-1182.
French SA, Story M, Perry CL. 1995. Self-esteem and obesity in children and adolescents: A literature review. Obes Res 3(5):479-490.
Gascon F, Valle M, Martos R, Zafra M, Morales R, Castano MA. 2004. Childhood obesity and hormonal abnormalities associated with cancer risk. Eur J Cancer Prev 13(3):193-197.
Goodman E. 1999. The role of socioeconomic status gradients in explaining differences in US adolescents health. Am J Public Health 89(10):1522-1528.
Goodman E, Whitaker RC. 2002. A prospective study of the role of depression in the development and persistence of adolescent obesity. Pediatrics 109(3):497-504.
Goodman E, Slap GB, Huang B. 2003. The public health impact of socioeconomic status on adolescent depression and obesity. Am J Public Health 93(11):1844-1850.
Goran MI, Ball GD, Cruz ML. 2003. Obesity and risk of type 2 diabetes and cardiovascular disease in children and adolescents. J Clin Endocrinol Metab 88(4):1417-1427.
Gortmaker SL, Must A, Perrin JM, Sobol AM, Dietz WH. 1993. Social and economic consequences of overweight in adolescence and young adulthood. N Engl J Med 329(14):1008-1012.
Gunnar MR, Donzella B. 2002. Social regulation of the cortisol levels in early human development. Psychoneuroendocrinology 27(1-2):199-220.
Guo SS, Wu W, Chumlea WC, Roche AF. 2002. Predicting overweight and obesity in adulthood from body mass index values in childhood and adolescence. Am J Clin Nutr 76(3):653-658.
Haas JS, Lee LB, Kaplan CP, Sonneborn D, Phillips KA, Liang S-Y. 2003. The association of race, socioeconomic status, and health insurance status with the prevalence of overweight among children and adolescents. Am J Public Health 93(12):2105-2110.
Haffner SM, Valdez RA, Hazuda HP, Mitchell BD, Morales PA, Stern MP. 1992. Prospective analysis of the insulin-resistance syndrome (syndrome X). Diabetes 41(6):715-722.
Hedley AA, Ogden CL, Johnson CL, Carroll MD, Curtin LR, Flegal KM. 2004. Prevalence of overweight and obesity among US children, adolescents, and adults, 1999-2002. J Am Med Assoc 291(23):2847-2850.
Isomaa B, Almgren P, Tuomi T, Forsen B, Lahti K, Nissen M, Taskinen MR, Groop L. 2001. Cardiovascular morbidity and mortality associated with the metabolic syndrome. Diabetes Care 24(4):683-689.
Jain A, Sherman SN, Chamberlin DL, Carter Y, Powers SW, Whitaker RC. 2001. Why don’t low-income mothers worry about their preschoolers being overweight? Pediatrics 107(5):1138-1146.
Keeler EB, Manning WG, Newhouse JP, Sloss EM, Wasserman J. 1989. The economic costs of a sedentary life-style. Am J Public Health 79(8):975-981.
Kelley E, Moy E, Kosiak B, McNeill D, Zhan C, Stryer D, Clancy C.2004. Prevention health care quality in America: Findings from the First National Healthcare Quality and Disparities Reports. Preventing Chronic Disease 1(3). [Online]. Available: http://www.cdc.gov/pcd/issues/2004/jul/cover.htm [accessed June 18, 2004].
Kuczmarski RJ, Ogden CL, Grummer-Strawn LM, Flegal KM, Guo SS, Wei R, Mei Z, Curtin LR, Roche AF, Johnson CL. 2000. CDC growth charts: United States. Adv Data 8(314):1-27.
Kuczmarski RJ, Ogden CL, Guo SS, Grummer-Strawn LM, Flegal KM, Mei Z, Wei R, Curtin LR, Roche AF, Johnson CL. 2002. Data from the National Health Survey. 2000 CDC Growth Charts for the United States: Methods and Development. Hyattsville, MD: National Center for Health Statistics.
Lakka HM, Laaksonen DE, Lakka TA, Niskanen LK, Kumpusalo E, Tuomilehto J, Salonen JT. 2002. The metabolic syndrome and total and cardiovascular disease mortality in middle-aged men. J Am Med Assoc 288(21):2709-2716.
Latner JD, Stunkard AJ. 2003. Getting worse: The stigmatization of obese children. Obes Res 11(3):452-456.
Levin BE. 2000. The obesity epidemic: Metabolic imprinting on genetically susceptible neural circuits. Obes Res 8(4):342-347.
Lewin Group. 2000. The Costs of Obesity. Paper presented at Obesity: The Public Health Crisis Conference, Washington, DC, American Obesity Association, September 13, 2000.
Lumeng JC, Gannon K, Cabral HJ, Frank DA, Zuckerman B. 2003. Association between clinically meaningful behavior problems and overweight in children. Pediatrics 112(5):1138-1145.
Mahoney LT, Burns TL, Stanford W, Thompson BH, Witt JD, Rost CA, Lauer RM. 1996. Coronary risk factors measured in childhood and young adult life are associated with coronary artery calcification in young adults: The Muscatine Study. J Am Coll Cardiol 27(2):277-284.
Manning WG, Keeler EB, Newhouse JP, Sloss EM, Wasserman J. 1989. The taxes of sin. Do smokers and drinkers pay their way? J Am Med Assoc 261(11):1604-1609.
McGill HC Jr, McMahan CA, Herderick EE, Zieske AW, Malcom GT, Tracy RE, Strong JP. 2002. Obesity accelerates the progression of coronary atherosclerosis in young men. Circulation 105(23):2712-2718.
McGinnis JM, Foege WH. 1993. Actual causes of death in the United States. J Am Med Assoc 270(18):2207-2212.
McGinnis JM, Williams-Russo P, Knickman JR. 2002. The case for more active policy attention to health promotion: To succeed, we need leadership that informs and motivates, economic incentives that encourage change, and science that moves the frontiers. Health Aff (Millwood) 21(2):78-93.
Mokdad AH, Serdula MK, Dietz WH, Bowman BA, Marks JS, Koplan JP. 1999. The spread of the obesity epidemic in the United States, 1991-1998. J Am Med Assoc 282(16):1519-1522.
Mokdad AH, Ford ES, Bowman BA, Nelson DE, Engelgau MM, Vinicor F, Marks JS. 2000. Diabetes trends in the U.S.: 1990-1998. Diabetes Care 23(9):1278-1283.
Mokdad AH, Bowman BA, Ford ES, Vinicor F, Marks JS, Koplan JP. 2001. The continuing epidemics of obesity and diabetes in the United States. J Am Med Assoc 286(10):1195-1200.
Mokdad AH, Ford ES, Bowman BA, Dietz WH, Vinicor F, Bales VS, Marks JS. 2003. Prevalence of obesity, diabetes, and obesity-related health risk factors, 2001. J Am Med Assoc 289(1):76-79.
Mokdad AH, Marks JS, Stroup DF, Gerberding JL. 2004. Actual causes of death in the United States, 2000. J Am Med Assoc 291(10):1238-1245.
Must A, Anderson SE. 2003. Effects of obesity on morbidity in children and adolescents. Nutr Clin Care 6(1):4-12.
Must A, Strauss RS. 1999. Risks and consequences of childhood and adolescent obesity. Int J Obes Relat Metab Disord 23(2S):S2-S11.
Must A, Spadano J, Coakley EH, Field AE, Colditz G, Dietz WH. 1999. The disease burden associated with overweight and obesity. J Am Med Assoc 282(16):1523-1529.
Narayan KM, Boyle JP, Thompson TJ, Sorensen SW, Williamson DF. 2003. Lifetime risk for diabetes mellitus in the United States. J Am Med Assoc 290(14):1884-1890.
NHLBI (National Heart, Lung, and Blood Institute). 2002. Third Report of the Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Publication No. 02-5215. Rockville, MD: NIH.
OECD Health Data. 2003. A Comparative Analysis of 30 Countries. [Online]. Available: http://www.fedpubs.com/subject/health/oecdhealth.htm [accessed June 6, 2004].
Ogden CL, Flegal KM, Carroll MD, Johnson CL. 2002a. Prevalence and trends in overweight among US children and adolescents, 1999-2000. J Am Med Assoc 288(14):1728-1732.
Ogden CL, Kuczmarski RJ, Flegal KM, Mei Z, Guo S, Wei R, Grummer-Strawn LM, Curtin LR, Roche AF, Johnson CL. 2002b. Centers for Disease Control and Prevention 2000 growth charts for the United States: Improvements to the 1977 National Center for Health Statistics version. Pediatrics 109(1):45-60.
Ogden CL, Carroll MD, Flegal KM. 2003. Epidemiologic trends in overweight and obesity. Endocrinol Metab Clin North Am 32(4):741-760, vii.
Oken E, Gillman MW. 2003. Fetal origins of obesity. Obes Res 11(4):496-506.
Park YW, Zhu S, Palaniappan L, Heshka S, Carnethon MR, Heymsfield SB. 2003. The metabolic syndrome: Prevalence and associated risk factor findings in the US population from the Third National Health and Nutrition Examination Survey, 1988-1994. Arch Intern Med 163(4):427-436.
Pine DS, Goldstein RB, Wolk S, Weissman MM. 2001. The association between childhood depression and adulthood body mass index. Pediatrics 107(5):1049-1056.
Pinhas-Hamiel O, Dolan LM, Daniels SR, Standiford D, Khoury PR, Zeitler P. 1996. Increased incidence of non-insulin-dependent diabetes mellitus among adolescents. J Pediatr 128(5):608-615.
Pratt M, Macera CA, Wang G. 2000. Higher direct medical costs associated with physical inactivity. Physician Sportsmed 28(10):63-70.
Puhl R, Brownell KD. 2001. Bias, discrimination, and obesity. Obes Res 9(12):788-805.
Richardson LP, Davis R, Poulton R, McCauley E, Moffitt TE, Caspi A, Connell F. 2003. A longitudinal evaluation of adolescent depression and adult obesity. Arch Pediatr Adolesc Med 157(8):739-745.
Salinsky E, Scott W. 2003. Obesity in America: A Growing Threat. NHPF Background Paper. Washington, DC: The George Washington University.
Sargent JD, Blanchflower DG. 1994. Obesity and stature in adolescence and earnings in young adulthood: Analysis of a British birth cohort. Arch Pediatr Adolesc Med 148(7):681-687.
Schrank D, Lomax T. 2003. The 2003 Urban Mobility Report. Texas Transportation Institute. College Statation, TX: Texas A&M University System.
Schwartz MB, Puhl R. 2003. Childhood obesity: A societal problem to solve. Obes Rev 4(1):57-71.
Schwartz MW, Woods SC, Porte D Jr, Seeley RJ, Baskin DG. 2000. Central nervous system control of food intake. Nature 404(6778):661-671.
Seidell JC. 1995. The impact of obesity on health status: Some implications for health care costs. Int J Obes Relat Metab Disord 19(6S):S13-S16.
Silverman BL, Cho NH, Rizzo TA, Metzger BE. 1998. Long-term effects of the intrauterine environment: The Northwestern University Diabetes in Pregnancy Center. Diabetes Care 21(S2):B142-B149.
Solomon CG, Manson JE. 1997. Obesity and mortality: A review of the epidemiologic data. Am J Clin Nutr 66(4S):1044S-1050S.
Strauss CC, Smith K, Frame C, Forehand R. 1985. Personal and interpersonal characteristics associated with childhood obesity. J Pediatr Psychol 10(3):337-343.
Strauss RS. 2000. Childhood obesity and self-esteem. Pediatrics 105(1):E15.
Strauss RS, Knight J. 1999. Influence of the home environment on the development of obesity in children. Pediatrics 103(6):E85.
Strauss RS, Pollack HA. 2001. Epidemic increase in childhood overweight, 1986-1998. J Am Med Assoc 286(22):2845-2848.
Strauss RS, Pollack HA. 2003. Social marginalization of overweight children. Arch Pediatr Adolesc Med 157(8):746-752.
Sturm R. 2002. The effects of obesity, smoking, and drinking on medical problems and costs: Obesity outranks both smoking and drinking in its deleterious effects on health and health costs. Health Aff (Millwood) 21(2):245-253.
Sturm R, Wells KB. 2001. Does obesity contribute as much to morbidity as poverty or smoking? Public Health 115(3):229-235.
Styne DM. 2001. Childhood and adolescent obesity. Prevalence and significance. Pediatr Clin North Am 48(4):823-854.
Troiano RP, Flegal KM. 1998. Overweight children and adolescents: Description, epidemiology, and demographics. Pediatrics 101(3):497-504.
U.S. Bureau of Labor Statistics. 2004. Consumer Price Indexes. [Online]. Available: http://www.bls.gov/cpi/home.htm [accessed September 3, 2004].
Wang G, Dietz WH. 2002. Economic burden of obesity in youths aged 6 to 17 years: 1979-1999. Pediatrics 109(5):E81-E86.
Whitaker RC. 2004a. Informational Report on Evidence-Based Literature for Development of a Childhood Obesity Interactive Tool. Princeton, NJ: Mathematica Policy Research.
Whitaker RC. 2004b. Predicting preschooler obesity at birth: The role of maternal obesity in early pregnancy. Pediatrics 114(1):e29-e36.
Whitaker RC, Dietz WH. 1998. Role of the prenatal environment in the development of obesity. J Pediatr 132(5):768-776.
Whitaker RC, Wright JA, Pepe MS, Seidel KD, Dietz WH. 1997. Predicting obesity in young adulthood from childhood and parental obesity. N Engl J Med 337(13):869-873.
Williamson DF, Thompson TJ, Anda RF, Dietz WH, Felitti V. 2002. Body weight and obesity in adults and self-reported abuse in childhood. Int J Obes Relat Metab Disord 26(8):1075-1082.
Winkleby MA, Robinson TN, Sundquist J, Kraemer HC. 1999. Ethnic variation in cardiovascular disease risk factors among children and young adults: Findings from the Third National Health and Nutrition Examination Survey, 1988-1994. J Am Med Assoc 281(11):1006-1013.
Wolf AM, Colditz GA. 1998. Current estimates of the economic cost of obesity in the United States. Obes Res 6(2):97-106.

























