2
Benefits and Limitations of Mammography
Mammography is possibly the most intensely scrutinized and debated medical procedure of our time, but there is virtually no disagreement on two points. First, there is no other breast cancer screening tool that has a better combination of sensitivity and specificity. Second, as practiced today, mammography could be better. This chapter reviews the basic features of, and factors involved in, effective mammography screening and its benefits and limitations.
SCREENING VERSUS DIAGNOSIS
Mammography has two main uses, screening and diagnosis, and there are important medical and economic differences between the two. Screening mammography is an x-ray-based procedure applied to a woman who has no signs or symptoms of breast disease and is used for the early detection of breast cancer. The ultimate purpose of screening is not to detect breast cancer at an early stage, but to save lives. An added benefit of screening is that small, screen-detected tumors might be effectively treated with less aggressive and harsh regimens than larger tumors. Diagnostic mammography (also called problem-solving mammography) uses the same x-ray-based procedure but is tailored by the radiologist for specific patients’ signs or symptoms. This procedure is designed to diagnose previously observed signs or symptoms of breast disease in a man or woman, or to determine the presence or absence of breast cancer in someone with a personal history of breast cancer or biopsy-proven breast disease.
The fundamental tenet of screening for any disease is that finding the disease before symptoms develop enables detection at a less advanced stage, and that initiating treatment at that time will reduce the adverse effects of the disease.43
The World Health Organization (WHO) outlined the principles of effective screening in 1968 and they are as true today as they were then. In their simplest form, the WHO screening guidelines encompass five key points, each of which applies to breast cancer and mammography:
-
The disease being screened is serious and prevalent,
-
The test is sensitive and specific,
-
The test is well tolerated,
-
The test is inexpensive, and
-
The test changes therapy or outcome.
The implications of these principles are that the disease must be prevalent enough within the population or subpopulation being screened to warrant testing individuals who show no signs or symptoms of the diseases. The value of different screening schedules and/or different technologies are likely to be different for different subpopulations, and the determination of optimal strategies requires careful study. Methodological challenges and studies currently under way are discussed in Chapter 6.
STANDARDS OF EVIDENCE
The value of a screening tool is determined by the relationship between the nature of the disease being screened and the performance characteristics of the screening tool. Sensitivity and specificity are the two most commonly cited measures of a screening or diagnostic test, but the more informative measure is the positive predictive value, which incorporates both sensitivity and specificity (see Box 2-1a and 2-1b).
Sensitivity refers to the proportion of true-positive results; this is calculated by dividing the number of breast cancer cases that were detected by the total number of breast cancer cases in the population tested, which equals the sum of those that were detected plus those that were missed. Estimates of the sensitivity of screening mammography from different studies range from 83 to 95 percent.72
Specificity refers to the proportion of true-negative results, or tests that correctly indicate that a woman does not have breast cancer among screened women without breast cancer. Mammography specificities generally fall in the range of 90 to 98 percent.72 In other words, the risk of a false-positive mammogram is about 1 in 10. Two studies suggest that among women who receive annual mammograms for 10 years, half will have at least one suspi-
|
BOX 2-1a
Sensitivity (Se) refers to the proportion of true-positive results, or tests that correctly indicate a woman has breast cancer. Se = TP / (TP + FN) where TP = True Positives and FN = False Negatives (TP + FN) = Total number of cancer cases Specificity (Sp) refers to the proportion of true-negative results, or tests that correctly indicate that a woman does not have breast cancer. Sp = TN / (TN + FP) where TN = True Negatives and FP = False Positives (TN+FP) = Total number of cancer-free cases Positive Predictive Value (PPV) refers to the probability that a patient with a positive test actually has the disease. PPV = TP / (TP + FP) where TP = True Positives and FP = False Positive (TP+FP) = Total number of abnormal, or positive, mammograms |
|||||||||||
cious finding leading to additional tests, such as diagnostic mammography, ultrasound, or biopsy, but that are later shown to be false alarms.12,21
Positive predictive value measures the probability that a patient with a positive (abnormal) test result actually has the disease. The higher the positive predictive value, the lower the number of false-positive results. Predictive value is determined by the sensitivity and specificity of the test, and the prevalence of disease in the population being tested. (Prevalence is defined as the proportion of persons in a defined population at a given point in time with the condition in question.) The more sensitive a test, the less likely it is that an individual with a negative test will have the disease and thus the greater the negative predictive value. The more specific the
|
BOX 2-1b
In this example, the prevalence of breast cancer is 4%. Sensitivity is 90% and specificity is 96%. Overall, this results in a positive predictive value of 8%. This example assumes that out of 10,000 women who were screened, 436 had abnormal findings, 36 cancers were confirmed by biopsy, and the mammograms of 4 women appeared normal despite the presence of cancer. |
|||||||||||
test, the less likely an individual with a positive test will be free from disease and the greater the positive predictive value.
When the prevalence of disease in those without signs or symptoms is low, the positive predictive value will also be low, even using a test with high sensitivity and specificity. For such rare diseases where there will be few true positives, a large proportion of those with positive screening tests inevitably will be found not to have the disease upon further diagnostic testing (Box 2-1b). One way to increase the positive predictive value of a screening test is to target the screening test to those at high risk of developing the disease, based on considerations such as demographic factors, medical history, or occupation. For example, mammograms are recommended for women over age 40, because that population has a higher prevalence of breast cancer.
Because the ultimate purpose of screening is to save lives by detecting cancer sufficiently early for effective curative treatment to be administered, screening effectiveness must be measured in terms of reduction in cancer mortality. However, because the death rate from breast cancer in “healthy” women who qualify as participants in a screening trial is relatively low (around 1/10 of 1 percent per year) it requires many thousands of women
to be followed for many years before there are sufficient numbers of deaths from breast cancer to evaluate the impact of screening with adequate statistical power. Indeed, the mammography trials that have been conducted have involved a total of more than half a million participants. Methodological issues in cancer screening trials are reviewed in Chapter 6.
MAMMOGRAPHY UNDER FIRE
In what has been described as “the journalistic equivalent of shouting fire in a crowded theater,” The New York Times published a review in 2001 of a scientific article disputing the value of mammography, thereby igniting a year-long controversy whose ramifications continue. The basis of the controversy was a review conducted by Peter Gotzsche and Ole Olsen of the Nordic Cochrane Center in Copenhagen.39,74 Although both Gotzsche and Olsen are listed as authors on the primary papers and worked at the Nordic Cochrane Center, Olsen left in 2001 and Gotzsche is the lead proponent of the claims. They argued that several of the key mammography screening trials were scientifically flawed and concluded that there was no evidence of benefit from mammography. The first screening trial of mammography was initiated in 1963. Since then, seven have been carried out in four countries.a Most reported reductions in breast cancer mortality and more than a dozen countries have established breast cancer screening programs.
Gotzsche and Olsen’s analysis has been reviewed since then by a series of expert groups, including the Global Mammography Summit and the International Agency for Research on Cancer of the WHO, who met specifically to review these criticisms (Box 2-2). These and numerous other reviews concluded that many of Gotzsche and Olsen’s criticisms were unsubstantiated, and the remaining deficiencies in the screening trials were judged not to invalidate the trials’ findings that screening mammography reduces breast cancer mortality.73 Gotzsche and Olsen’s critique was based on judgments of the quality of the screening studies, but those judgments were based on misreading of the data and the literature.36,37 As is often the case, the eruption of a medical controversy receives more media attention than its resolution, and these expert reviews received relatively little media attention. It is thus not surprising that some members of the public continue to believe, incorrectly, that there is debate among the experts about whether screening mammography saves lives.
|
BOX 2-2 Physicians Data Query (PDQ) January 2002 The PDQ is an independent panel of cancer experts that regularly reviews evidence on cancer and prepares information for the National Cancer Institute (NCI). The PDQ posts its reports on the NCI website, but is independent of the NCI and does not issue guidelines or make official recommendations. It supported Gotzsche and Olsen’s criticism of mammography and concluded that “screening for breast cancer does not affect overall mortality, and that the absolute benefit for breast cancer mortality appears to be small.” International Agency for Research on Cancer of the WHO March 2002 The group, consisting of 24 experts from 11 countries, concluded that trials have provided sufficient evidence for the efficacy of mammography screening of women between 50 and 69 years. The reduction in mortality from breast cancer among women who chose to participate in screening programs was estimated to be about 35 percent. For women aged 40-49 years, there is only limited evidence for a reduction. The quality of the trials that were used to make these evaluations was carefully assessed. The working group found that the effectiveness of national screening programs varies due to differences in coverage of the female population, quality of mammography, treatment, and other factors. Organized screening programs are more effective in reducing the rate of death from breast cancer than sporadic screening of selected groups of women. Global Summit on Mammographic Screening June 2002 In response to the uncertainty over the efficacy of breast screening, a Global Summit on Mammographic Screening was organized at the European Institute of Oncology in Milan. The Summit was planned in association with the WHO, European Commission, American Cancer Society, U.S. Centers for Disease Control and Prevention, American Italian Cancer Foundation, European Society for Medical Oncology, American Society of Clinical Oncology, and International Union Against Cancer. The design and recent results from the seven randomized trials were presented and discussed in detail. Some of the criticisms put forward by Gotzsche and Olsen were discarded as being wrong; others had been addressed by new analyses and |
Although the debate on the benefits of mammography focused on the validity of the first seven clinical screening trials, these are only part of the evidence. A series of studies conducted in community settings that are more comparable to actual clinical practice have supported the conclusions of those earlier clinical screening trials.27 Overall, the evidence indicates that
|
shown to be of minor significance. The remaining minor considerations did not detract from the conclusion that screening mammography reduced the mortality from breast cancer in women receiving an invitation to be screened in well-organized clinical trials: The reduction in breast cancer mortality appeared to be between 21 and 23 percent, according to recent estimates. Those participating fully could expect greater benefit. There was unanimity that with the current evidence from randomized trials, taking full account of any limitations to their methodology, there were no grounds for stopping on-going screening programs or planned programs. The group also stated that mammographic screening is only one step in the total management of the woman with breast cancer. This goal can only be attained through rigorous, high-quality screening, diagnosis, and treatment. United States Preventive Services Task Force (USPSTF) September 2002 The USPSTF is an independent panel of experts in primary care and prevention that systematically reviews the evidence of effectiveness of clinical preventive services and develops recommendations for their use. The USPSTF concluded that the criticisms made against the Swedish trials by Gotzsche and Olsen are misleading and scientifically unfounded. “We found the same flaws [as Gotzsche and Olsen],” says Janet D. Allan, vice-chair of the task force and dean of the School of Nursing at the University of Texas Health Science Center in San Antonio. “They interpreted the flaws as being fatal flaws,” she says. “We did not interpret the flaws as fatal…and concluded that the studies were still valid and that mammography screening reduces deaths from breast cancer.” The USPSTF concluded that the absolute benefit among women in their 40s is smaller than it is among older women because the incidence of breast cancer is lower at the younger age. The USPSTF also concluded that the evidence is also generalizable to women aged 70 and older (who face a higher absolute risk for breast cancer) if their life expectancy is not compromised by comorbid disease. The absolute probability of benefits of regular mammography increase along a continuum with age, whereas the likelihood of harms from screening (false-positive results and unnecessary anxiety, biopsies, and cost) diminish from ages 40 to 70. The balance of benefits and potential harms, therefore, grows more favorable as women age. The precise age at which the potential benefits of mammography justify the possible harms is a subjective choice. |
the availability of screening reduces mortality from breast cancer by 20 to 30 percent (reviewed by Duffy and colleagues in 2003),19 and that in a population that actually participates in screening mammography, the reduction can be considerably greater, nearly 50 percent.18,97 This is not to say that every woman who undergoes screening mammography will ben-
efit. Most women will never develop breast cancer, but the lives of many of those who do will be saved even though it is not yet possible to identify them in advance.
BREAST DENSITY AFFECTS MAMMOGRAPHIC SENSITIVITY
Breast density varies widely among women, and cancer is more difficult to detect in mammograms of women with radiographically dense breasts. Mammographic density refers to the relative lightness of a mammogram, determined by the number of x-ray photons that penetrate the breast. Fat is radiographically translucent, so x-rays pass through it relatively unimpeded making it appear darker on x-ray images. Connective and epithelial tissue, which includes the mammary glands, is radiographically dense relative to fat and blocks x-rays to a greater extent, so it appears lighter. Breast cancers and microcalcifications generally appear as whiter areas on mammograms because they tend to absorb more x-ray photons; they can be difficult to detect against the relatively light background of dense breast tissue because of the lack of contrast between them and a dense breast background.
Breast density is usually measured as part of mammographic interpretation by classifying a mammogram according to the 4-point Breast Imaging Reporting and Data System™ (BI-RADS®) breast density scale established by the American College of Radiology (see Table 2-1). The scale was revised in 2003 and now asks radiologists to include the “percentage of glandular density,” or the percentage of breast tissue that is mammographically dense, when characterizing breast composition. Density level 1 indicates predominantly fatty tissue; 2 indicates scattered glandular tissue; 3 indicates heterogeneous density; and 4 indicates an extremely dense breast. Categories 3 and 4 indicate the possibility of reduced mammographic sensitivity. However, there is only moderate agreement among radiologists on these density readings,49 and several investigators have
TABLE 2-1 BI-RADS® (fourth edition) Scale for Characterizing Breast Composition
|
Category |
Description |
Glandular Density (percent of breast tissue that is mammographically dense) |
|
1 |
Predominantly fatty tissue |
Less than 25% |
|
2 |
Scattered glandular tissue |
25–50% |
|
3 |
Heterogeneously dense |
50–75% |
|
4 |
Extremely dense tissue |
More than 75% |
attempted to develop a standard quantitative approach to mammographic density measurement, such as by using x-ray digitizers and quantifiable detection systems using density algorithms. These have been carefully studied, but are not yet widely available for clinical purposes.4,79,102
Breast density is a risk factor for missed cancers, and both false-positive and false-negative mammographic interpretations are more likely with dense breasts.34 In a study of more than 11,000 women with no clinical symptoms of breast cancer, the sensitivity of mammography was only 48 percent for the subset of women with extremely dense breasts compared to 78 percent sensitivity for the entire sample of women in the study.53 Technologies that are not based on x-rays, such as magnetic resonance imaging and sonography (ultrasound), are less affected by breast density.
Many factors influence breast density, such as obesity, ethnicity, age, stage of menstrual cycle, and number of live births (parity). Overall, menopausal status, weight, and parity account for 20 to 30 percent of the age-adjusted variation in the percentage of dense breast tissue.5 Younger women tend to have more dense breasts and thus often have mammograms that are difficult to interpret. Hormone replacement therapy increases breast density, although few women show dramatic changes, and the changes depend on the particular hormone regime (reviewed by Slanetz, 2002).93 For example, estrogen and progestin combination therapy increases breast density to a greater degree than estrogen alone.15
Breast density varies within individual women as well as among different women. Breasts that are mammographically dense also tend to have areas that are not dense. Women are slightly more likely to have extremely dense breasts during the last 2 weeks of the menstrual cycle (luteal phase),103,111 although this is not generally clinically significant. Nevertheless, performing mammography during the first 2 weeks of the menstrual cycle may increase mammographic accuracy,111 probably because women do not feel as much discomfort during breast compression. This increases the probability of obtaining an examination without noticeable patient motion, which can degrade image quality and limit the ability to find cancers.
Obesity is commonly associated with fatty breasts and accounts for more than 40 percent of the variance in breast density.6 Native American populations typically have lower density breast tissue, and Asian populations have greater density breast tissue than African American and white populations overall. One solution to the difficulties posed by dense breasts might be to perform ultrasound on all women with particularly dense breasts. This is standard practice in Korea and is done in many facilities in the United States, but, to date, no data have been published to indicate this would improve outcomes and which women would benefit.
THE HARMS OF MAMMOGRAPHY
Mammography has been criticized not only because of questions about its effectiveness, but for fear that it might actually cause harm. Harms that have been listed by Thornton and colleagues include physical, emotional, social, financial, intergenerational, or psychological harm.100 Although some authors suggest that these may be lifelong, the evidence collected thus far indicates that they are generally moderate and short-lived.
Financial harm refers to the cost of tests needed for definitive diagnosis following an abnormal mammogram. Retrospective studies indicate that the additional costs of evaluating false-positive results can add up to one-third of the total cost of screening for all women.21,63
Intergenerational harm refers to the possibility that insurance fees might be raised for daughters of women who were diagnosed with a condition that did not lead to adverse health outcomes and was detected only during a screening mammogram.14 However, the Committee is not aware of any published cases where this is documented.
Pain and Anxiety
Mammography requires compression of the breast, and is painful for some women primarily related to the timing of the last menstrual period or the anticipation of pain (reviewed by Drossaert and colleagues in 2002).17
Studies conducted prior to 1999 reported highly inconsistent results, ranging from only 1 percent to as many as 85 percent of women reporting pain during mammography. Given the known difficulty in reliably measuring pain, it is important to evaluate the methodologies used in these reports.1,85 For example, Kornguth and his colleagues found that only 2 percent of women reported pain using a 6-point pain scale, whereas 75 to 85 percent of the same women reported pain when using the two more complex measures of pain (McGill Pain Questionnaire and the Visual Analog Scale and Brief Pain Inventory).55
Recent, appropriately designed studies report that only 15 percent17 or 28 percent87 of women experienced moderate or severe pain. In the latter study, 200 women were asked to rate the pain associated with a screening mammogram on a 10-point scale, where 0 is “no pain at all”; 10 is “the worst pain you have ever felt”; and 5 is “about average: for example, a mild headache or shoes that are a little too tight.” Seventy-two percent of the women rated the pain at or less than 4. In general, these studies found no correlation between pain and age, breast size, or body mass index. In another recent study, 77 percent of women reported moderate or severe pain (lasting 10 minutes or less); 12 percent of them said they would be deterred from future screening, although less than 5 percent said they would like to receive pain medication prior to their next mammogram.85
Emotional harm includes the anxiety of waiting for results, which may take days to weeks. (The Mammography Quality Standards Act requires that women receive their mammogram results within 30 days of testing.) In one survey, women who were questioned immediately following screening mammography reported that the part of the procedure they found most stressful was waiting for results.87 Yet another study reported that 67 percent of women were unwilling to pay even a small fee of $25 for immediate results.81 In general, anxiety associated with waiting for mammography results does not appear to be significant for most women (reviewed in 2001 by Meystre-Agustoni and colleagues).67
False Alarms
An abnormal finding on a mammogram is cause for concern.b However, resulting psychological distress is usually transient84 and is generally resolved if a subsequent test indicates that the interpretation was, in fact, a false positive. Nevertheless, for some women, anxiety persists long after an initial false positive is resolved, although generally at moderate levels.
One study compared the anxiety levels of women who received negative results at their first screening with those who received false-positive results. The women’s anxiety levels were measured on a scale of 0 (not at all anxious) to 5 (very anxious). Depending on the measurement scale used and dimension of anxiety that was measured, the anxiety levels of the women who received false positives ranged from averages of 1.5 to 2.5. Their anxiety levels were consistently about three times higher than for women whose mammograms had been negative from the start, but they were still only “moderately anxious” and not “very anxious” (level 5) as much as eight weeks after the resolution of the false positive.67 The initial anxiety level of the women was a strong predictor of their anxiety levels after a negative result. Although this study measured anxiety levels in about 800 women, the results are based on the much smaller group of 36 women who received false-positive results. Furthermore, the study was conducted in Switzerland during the introduction of a pilot screening program and anxiety levels with mammography presumably were influenced by the unfamiliarity of these women with screening mammography.
Two studies report that the experience of a false-positive mammogram does not deter women from obtaining subsequent mammograms.16,80 A
third study reports the opposite—that fewer women who received false-positive results return for a screening mammogram within three years—but the difference between groups, although statistically significant was only 3 percent and of doubtful clinical relevance.66
Biopsies
In the event of a positive mammogram, a woman must undergo a secondary assessment phase involving needle and/or open surgical biopsy to establish a definitive diagnosis.c Exposure to unnecessary biopsies is a real danger. Biopsy rates for suspected cases of breast cancer vary considerably among countries, indicating that the technical limitations of mammography are only part of the reason for biopsies. The rates are influenced by multiple factors beyond screening, such as practice variation and risk assessment. For example, the physician must take into account not only a patient’s risk of breast cancer, but his or her confidence in the mammographic results (which can be influenced by patient characteristics such as breast density or previous surgeries), as well as risks associated with the health care system—such as the risk of malpractice suits. In principle, improved risk stratification should result in a lower rate of biopsies for benign conditions because there would be a smaller pool of low-risk women being screened. “Unnecessary” biopsies can also be reduced by the use of supplemental technologies.
Radiation Risk
High doses of radiation (0.2.5 to 20 Gy), such as those that occurred in the 1930s to 1950s due to atomic bomb radiation, multiple chest x-rays, and radiation treatment for breast disease, were associated with increased incidence of breast cancer in women below age 35 at exposure.29,59 However, radiation sensitivity among women drops precipitously after age 35,59 and although some caution may be warranted for regular mammographic screening of women below age 35,60 calculations indicate that radiation risk is extremely small compared with the benefits, even for women in their forties.28,29,48 Moreover, since the early days of mammography, image quality has improved markedly (Figure 2-1) and radiation exposure has been greatly reduced, so that the average amount of radiation absorbed during a mammogram is now very low.112 It is estimated that 100,000 women who were screened annually from ages 50 to 75 would lose about 13 years from
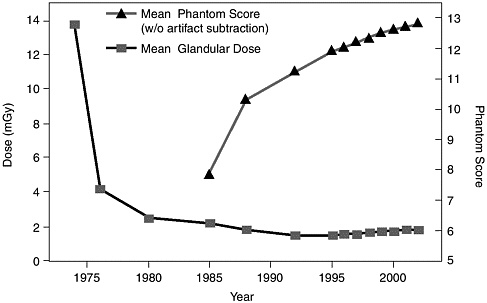
FIGURE 2-1 Trends in mammography dose and image quality. Radiation dose is shown in milliGray units. Phantom Score indicates image quality.95
radiation-induced cancers, but gain 12,600 years from an assumed 20 percent reduction in breast cancer mortality.28
Recent studies cited in the media have caused some alarm reporting greater DNA damage in human cells in cultures from low than from high x-ray doses.8,83 Also, because BRCA1 and BRCA2 mutations are associated with deficient DNA repair,11,56,78 it is theoretically possible that women with BRCA mutations might be more sensitive to the mutagenic effects of radiation. However, studies of mammalian cells in culture dishes have yielded inconsistent results,37,82 and isolated cells cannot be presumed to predict comparable effects on human health. No large-scale epidemiological studies have been able to detect an increase in cancer rate due to exposure to mammography,60 nor has a definitive correlation between BRCA1 or BRCA2 mutations and the induction of cancer (or even the induction of mutations) by the type of radiation used in mammography been demonstrated. (Other aspects of BRCA gene mutations are discussed in Chapter 4.)
THE DCIS DILEMMA
Far outstripping the current rise in all breast cancers, the diagnosis of ductal carcinoma in situ (DCIS) has increased approximately 10-fold in the
United States and other developed countries since the advent of population-based mammographic screening, raising concerns of possible overtreatment (Figure 2-2).22,23,69
DCIS now represents about 14 percent, or 1 in 7, of all new breast cancer diagnoses in the United States.96,114 Among screen-detected breast cancers, 20 percent are DCIS and 1 in every 1,300 screening mammograms leads to a diagnosis of DCIS.22,d When younger women are diagnosed with breast cancer, it is somewhat less likely to be DCIS (Table 2-2). All breast cancers are more common among older women, so relatively and absolutely more of DCIS is found in older women.
Before the widespread use of screening mammography, many cases of DCIS went unrecognized; the increased numbers and proportion of DCIS cases that are now recognized do not necessarily mean that more women are developing DCIS. The reported incidence of DCIS is determined by the actual number of cases and also by the ability to detect them.
DCIS is not life-threatening per se, but it is a significant risk factor for invasive breast cancer. It is believed to precede the development, over time, of invasive breast cancer,54 although the rate of development can be so slow that it never becomes life threatening.46,77 Among women in an extensive mammography registry study who were initially diagnosed with DCIS between 1978 and 1983, 3.4 percent died of invasive breast cancer within 10 years; of those diagnosed between 1984 and 1989, the 10-year breast cancer mortality was 1.9 percent.22 These rates, which are approximately one-tenth those for women diagnosed with localized invasive breast cancer, may reflect the effectiveness of treatment for DCIS, the mildness of the condition, or both. Deaths from breast cancer among women with DCIS are thought to result from an invasive component that was not recognized at the time of the DCIS diagnosis or because of progression to an invasive cancer.
The most important issue for DCIS is not, however, the increased detection, but rather the information, which mammography cannot provide, that would permit optimally individualized treatments. Cessation of screening mammography, or any other screening modality, would not solve the problem of overtreatment.26 Instead, the solution lies in tailoring treatment to the biological characteristics of individual cases.
Diagnosis of DCIS
DCIS occurs when malignant epithelial cells proliferate within the breast ducts but remain confined by the basement membrane (a thin non-
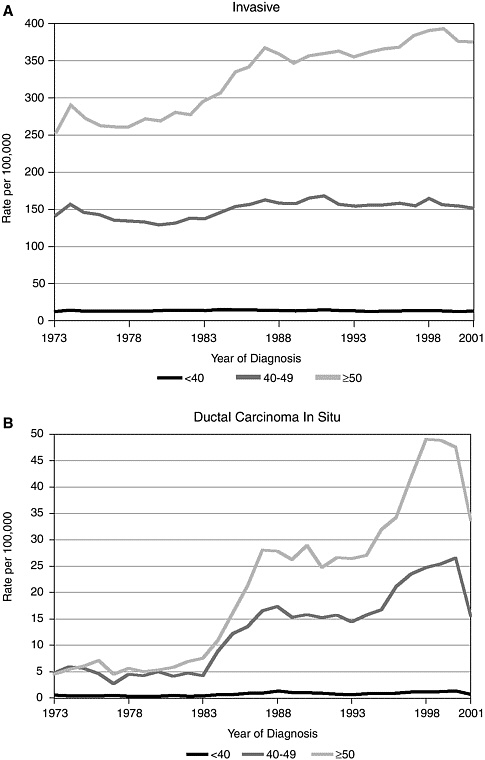
FIGURE 2-2 Female breast cancer incidence (invasive and DCIS) by age-adjusted rates from 1973 to 2001.96
TABLE 2-2 Age Differences in DCIS Detected by Screening Mammography22
|
Age |
Approximate Number of DCIS Cases Detected per Mammogram |
Approximate Incidence of DCIS Cases Detected by Mammography |
|
40-49 |
1 in 1800 |
0.06% |
|
50-59 |
1 in 1500 |
0.07% |
|
60-69 |
1 in 1000 |
0.1% |
|
70-84 |
1 in 900 |
0.1% |
cellular tissue underlying epithelial cells).40 The resulting disease ranges from low-grade lesions resembling atypical hyperplasia, to high-grade or anaplastic lesions. (Anaplastic lesions are made up of cells that have reverted to an immature or less differentiated form that is often indicative of invasive cancer.) The classification of different types of DCIS is described in Box 2-3.
The proliferation of epithelial cells in the lobules of the mammary ducts traditionally has been referred to as lobular carcinoma in situ (LCIS), but the current preferred term is lobular intraepithelial neoplasia (LIN), which includes both LCIS and atypical lobular hyperplasia.7 LIN and DCIS are neither invasive nor metastatic. In time, however, many DCIS lesions will become both invasive and metastatic.92 LIN, while an indicator of high risk for developing breast cancer, is not considered to be a pre-invasive cancer.106 It has no characteristic mammographic features and is typically detected by a biopsy performed for another reason,61 whereas the microcalcifications typical of many cases of DCIS are usually apparent on mammograms.
Only about 10 percent of mammographically detected DCIS will appear as a mass or asymmetry without calcifications; most DCIS is suspected on the basis of mammographic microcalcifications.22,71,109 This contrasts with invasive cancer, which usually appears as a mass or density on a mammogram. Mammograms frequently underestimate the extent of DCIS, particularly for larger lesions.41,42,43,71 Calcifications associated with DCIS vary in size, form and density, although they tend to be grouped in clusters, lines, or segmental arrangements that follow the morphology of the duct. Calcifications may also reflect the presence of benign conditions such as proliferative or nonproliferative fibrocystic change, although calcifications that result from these conditions are usually more rounded, more uniform in density, and more scattered in distribution than DCIS calcifications.71,88
A definitive diagnosis of DCIS requires pathologic evaluation of a biopsy specimen. To ensure complete accuracy of grading, a core or excisional biopsy must be performed.51 Stereotactic core biopsy is recommended and
|
BOX 2-3 Traditionally, the microscopic classification of DCIS has been based on the architecture of the lesion. Most simply, lesions are classified as either comedo or noncomedo, based on the presence or absence of plug-like necrotic material (dead tissue) filling the lumen of the affected ducts. This necrotic debris produces the typical fine, linear branching pattern of calcifications seen on mammography and is associated with more aggressive disease.20 DCIS is graded according to the Van Nuys classification, which combines nuclear grade and the presence or absence of necrosis to predict prognosis50,51,98 (see table below).90 Although the Van Nuys classification is used in clinical practice, it has never been validated in a prospective clinical trial. Comedo carcinoma or high-grade lesions are more aggressive and likely to progress to invasive disease. Studies of local recurrence rates (following local excision without subsequent radiotherapy) indicate that poorly differentiated, comedo-type tumors tend to recur earlier despite excision and radiotherapy (for excellent review, see Kessar et al., 2002).46,46,51,57,58,94 Van Nuys Prognostic Index
The Van Nuys Prognostic Index (VNPI). The first horizontal row represents VNPI scores and the index is calculated by adding the scores of the three parameters (VNPI varies between 3 and 9). For example, a 20-mm tumor would have a score of 2. If the margins were >10 mm (score =1) and there was no sign of necrosis or high-grade pathology in the nucleus (score =1), the total would give a VNPI of 4. The percent of women who had no recurrence after 8 years of the initial DCIS diagnosis was highest for low VNPI scores (97 percent for VNPI = 3-4; 77 percent for VNPI = 5-7; and 20 percent for VNPI = 8-9). |
||||||||||||||||||||
preferred for diagnosis of DCIS, but some patients with microcalcifications are poor candidates for this procedure due to the small size and/or thickness of their breasts, the location of the calcifications, or other factors that interfere with probe function.71 In these cases, image-directed open surgical biopsy is the preferred approach. Some facilities use vacuum-assisted bi-
opsy to obtain more tissue for analysis. Ultrasound-guided biopsy is useful for nonpalpable masses, but usually cannot be relied on for biopsy of microcalcifications.71
Although it was previously believed there was a general progression of genetic abnormalities from atypical ductal hyperplasia, to low-grade DCIS, to high-grade DCIS, and finally to invasive ductal carcinoma, this is no longer believed to be true.62,71
Is DCIS Overtreated?
Some researchers contend that the routine biopsy and follow-up of mammographically detected DCIS constitutes overtreatment, because many such tumors would not progress to invasive disease.33,44,51,99 This argument is based on (1) autopsy studies that indicate a significant prevalence of undetected DCIS in women who died of other causes, and (2) the observation that most women with DCIS do not experience invasive recurrence within 10 to 15 years following treatment (reviewed in Ernster et al., 2002).22,24,108,110 However, neither of these arguments is conclusive. First, the series of studies that estimated a 30 to 50 percent risk of developing invasive cancer within 10 years of a DCIS diagnosis (and in the absence of any treatment besides surgical biopsy)2,86 was based on cases that occurred before the widespread use of mammography and were detected by other means.76 Second, many more cases are detected, presumably at earlier stages, and few go untreated. As a result, there are no definitive estimates of the natural course of DCIS (see Box 2-4). Moreover, later review of the earlier autopsy studies revealed that many of the DCIS cases had been overdiagnosed and failed to meet current criteria for DCIS diagnosis.91
Other lines of evidence suggest that DCIS is not overtreated. A small series of untreated women with DCIS, who were diagnosed before mammographic screening became widespread, were found to have more than the expected number of invasive breast cancers when compared to the general population.2,22,25,75 Similarly, increased risk for both DCIS and invasive breast cancer also has been reported in larger, more recent studies of women treated for DCIS.22,35,36,68,104 Findings from randomized trials indicate that the addition of radiotherapy and tamoxifen to breast-conserving surgery (BCS) reduces the chance of future invasive disease recurrence compared with BCS alone.22,31,32,47 Finally, recent molecular genetic studies suggest that most invasive ductal breast cancers arise from DCIS (reviewed by Feig, 2000).9,10,26,64,65,70,107 Overall, most cases of DCIS are high grade, regardless of how they were detected. Fifty-four percent of screen-detected cases and 62 percent of non-screen-detected cases were high grade.51 High-grade tumors have a greater potential to progress to invasive disease than low-
|
BOX 2-4 Women with biopsy-proven DCIS are typically treated surgically with either mastectomy or BCS (also known as lumpectomy). Along with BCS, treatment often includes adjuvant radiotherapy (RT) and in some cases, hormone therapy (tamoxifen).22,24 Although BCS is recommended for the majority of DCIS cases, mastectomy remains the treatment of choice for many women in the United States. Mastectomy is specifically indicated for women with two or more primary tumors in the breast or with diffuse malignant-appearing microcalcifications, and also when persistent positive tumor margins remain after reasonable surgical attempts.26,71,114 Mastectomy may also be more appropriate in cases of extensive DCIS that can be removed with only a small negative margin, particularly in small-breasted patients. Total mastectomy is associated with very low rates of local recurrence (1.4 percent) and breast cancer-specific mortality (0.6 percent).69 Treatment guidelines recommend BCS plus RT for localized DCIS (that is, for single, nondiffuse loci) less than or equal to 4 cm, meanwhile acknowledging the inherent difficulty of accurately measuring DCIS lesions.71 Younger women tend to have a greater risk of local recurrence after BCS plus RT, which results at least in part from the biological characteristics of disease in younger women.105 Although no randomized trials have yet been published, retrospective studies indicate that total mastectomy improves disease-free survival of DCIS as compared with BCS plus RT, but there is no evidence to suggest the superiority of mastectomy over BCS plus RT in terms of overall and breast-cancer-specific survival.3,69,89 There have been some reports of low recurrence rates following BCS alone for small-volume lesions with clear margins, but the maximum size of DCIS for which RT could be safely omitted is unknown.69,71 Three recent randomized controlled trials demonstrated that BCS plus RT significantly reduces the incidence of local recurrence of DCIS.30,31,38,47,69 Most nonrandomized trials reported findings consistent with these randomized trials and showed that adjuvant RT after BCS significantly decreased the incidence of ipsilateral (same side) breast tumor recurrence.13,52,69,89,101 Randomized trials show that recurrence with lumpectomy alone is approximately 30 percent at 10 years and reduced by half with radiotherapy. Despite the higher rates of recurrence, there is no difference in the mortality rates for lumpectomy alone versus lumpectomy with RT; rates for both are in the range of mortality for mastectomy, which is about 2 percent. Fifty percent of recurrences are DCIS and the other 50 percent are invasive breast cancer. Although not considered a mandatory part of treatment for DCIS, tamoxifen therapy appears to benefit some patients.32,69,114 |
grade tumors. DCIS is now recognized to be very heterogeneous is its clinical behavior.46
Although there is an element of overdiagnosis of DCIS in breast cancer screening, this appears to be relatively small. For example, a recent study reported that the average incidence of nonprogressive DCIS is about 1 in
100,000 per year and estimated that only 4 percent of DCIS cases detected during incidence screening represent overdiagnosis that would not progress if left untreated.113,e
Thus, although most experts accept that a significant fraction of DCIS will remain noninvasive, many agree that until clinicians can distinguish among the heterogeneous types of DCIS and recognize those that are likely to progress to invasive, metastatic breast cancer, mammography-detected DCIS requires full diagnostic workup and treatment.51 A critically important focus of future research will be to identify those cases of DCIS that are unlikely to progress, as well as more effective ways to arrest the development of more dangerous lesions.45
REFERENCES
1. Andrews FJ. 2001. Pain during mammography: implications for breast screening programmes. Australas Radiol 45(2):113-117.
2. Betsill WL Jr, Rosen PP, Lieberman PH, Robbins GF. 1978. Intraductal carcinoma. Long-term follow-up after treatment by biopsy alone. JAMA 239(18):1863-1867.
3. Boyages J, Delaney G, Taylor R. 1999. Predictors of local recurrence after treatment of ductal carcinoma in situ: a meta-analysis. Cancer 85(3):616-628.
4. Boyd NF, Byng JW, Jong RA, Fishell EK, Little LE, Miller AB, Lockwood GA, Tritchler DL, Yaffe MJ. 1995. Quantitative classification of mammographic densities and breast cancer risk: results from the Canadian National Breast Screening Study. J Natl Cancer Inst 87(9):670-675.
5. Boyd NF, Dite GS, Stone J, Gunasekara A, English DR, McCredie MR, Giles GG, Tritchler D, Chiarelli A, Yaffe MJ, Hopper JL. 2002. Heritability of mammographic density, a risk factor for breast cancer. N Engl J Med 347(12):886-894.
6. Boyd NF, Lockwood GA, Byng JW, Little LE, Yaffe MJ, Tritchler DL. 1998. The relationship of anthropometric measures to radiological features of the breast in premenopausal women. Br J Cancer 78(9):1233-1238.
7. Bratthauer GL, Tavassoli FA. 2002. Lobular intraepithelial neoplasia: previously unexplored aspects assessed in 775 cases and their clinical implications. Virchows Arch 440(2):134-138.
8. Brenner DJ, Sawant SG, Hande MP, Miller RC, Elliston CD, Fu Z, Randers-Pehrson G, Marino SA. 2002. Routine screening mammography: how important is the radiation-risk side of the benefit-risk equation? Int J Radiat Biol 78(12):1065-1067.
9. Buerger H, Otterbach F, Simon R, Poremba C, Diallo R, Decker T, Riethdorf L, Brinkschmidt C, Dockhorn-Dworniczak B, Boecker W. 1999. Comparative genomic hybridization of ductal carcinoma in situ of the breast-evidence of multiple genetic pathways. J Pathol 187(4):396-402.
10. Bur ME, Zimarowski MJ, Schnitt SJ, Baker S, Lew R. 1992. Estrogen receptor immunohistochemistry in carcinoma in situ of the breast. Cancer 69(5):1174-1181.
11. Chen JJ, Silver D, Cantor S, Livingston DM, Scully R. 1999. BRCA1, BRCA2, and Rad51 operate in a common DNA damage response pathway. Cancer Res 59(7 Suppl):1752s-1756s.
12. Christiansen CL, Wang F, Barton MB, Kreuter W, Elmore JG, Gelfand AE, Fletcher SW. 2000. Predicting the cumulative risk of false-positive mammograms. J Natl Cancer Inst 92(20):1657-1666.
13. Cutuli B, Cohen-Solal-Le Nir C, De Lafontan B, Mignotte H, Fichet V, Fay R, Servent V, Giard S, Charra-Brunaud C, Auvray H, Penault-Llorca F, Charpentier JC. 2001. Ductal carcinoma in situ of the breast results of conservative and radical treatments in 716 patients. Eur J Cancer 37(18):2365-2372.
14. Davey C, White V, Ward JE. 2002. Insurance repercussions of mammographic screening: what do women think? Med Sci Monit 8(12):LE54-LE55.
15. Dixon JM. 2003. Hormone replacement therapy and the breast. Surg Oncol 12(4):251-263.
16. Drossaert CH, Boer H, Seydel ER. 2001. Does mammographic screening and a negative result affect attitudes towards future breast screening? J Med Screen 8(4):204-212.
17. Drossaert CH, Boer H, Seydel ER. 2002. Monitoring women’s experiences during three rounds of breast cancer screening: results from a longitudinal study. J Med Screen 9(4):168-175.
18. Duffy SW, Tabar L, Chen HH, Holmqvist M, Yen MF, Abdsalah S, Epstein B, Frodis E, Ljungberg E, Hedborg-Melander C, Sundbom A, Tholin M, Wiege M, Akerlund A, Wu HM, Tung TS, Chiu YH, Chiu CP, Huang CC, Smith RA, Rosen M, Stenbeck M, Holmberg L. 2002. The impact of organized mammography service screening on breast carcinoma mortality in seven Swedish counties. Cancer 95(3):458-469.
19. Duffy SW, Tabar L, Vitak B, Day NE, Smith RA, Chen HH, Yen MF. 2003. The relative contributions of screen-detected in situ and invasive breast carcinomas in reducing mortality from the disease. Eur J Cancer 39(12):1755-1760.
20. Dummin L. Pathology Seen in Breast Imaging: DCIS. Web Page. Available at: http://medrad.city.unisa.edu.au/Breast/DCIS.html.
21. Elmore JG, Barton MB, Moceri VM, Polk S, Arena PJ, Fletcher SW. 1998. Ten-year risk of false positive screening mammograms and clinical breast examinations. N Engl J Med 338(16):1089-1096.
22. Ernster VL, Ballard-Barbash R, Barlow WE, Zheng Y, Weaver DL, Cutter G, Yankaskas BC, Rosenberg R, Carney PA, Kerlikowske K, Taplin SH, Urban N, Geller BM. 2002. Detection of ductal carcinoma in situ in women undergoing screening mammography. J Natl Cancer Inst 94(20):1546-1554.
23. Ernster VL, Barclay J, Kerlikowske K, Grady D, Henderson C. 1996. Incidence of and treatment for ductal carcinoma in situ of the breast. JAMA 275(12):913-918.
24. Ernster VL, Barclay J, Kerlikowske K, Wilkie H, Ballard-Barbash R. 2000. Mortality among women with ductal carcinoma in situ of the breast in the population-based surveillance, epidemiology and end results program. Arch Intern Med 160(7):953-958.
25. Eusebi V, Foschini MP, Cook MG, Berrino F, Azzopardi JG. 1989. Long-term follow-up of in situ carcinoma of the breast with special emphasis on clinging carcinoma. Semin Diagn Pathol 6(2):165-173.
26. Feig SA. 2000. Ductal carcinoma in situ. Implications for screening mammography. Radiol Clin North Am 38(4):653-668, vii.
27. Feig SA. 2002. Effect of service screening mammography on population mortality from breast carcinoma. Cancer 95(3):451-457.
28. Feig SA, Ehrlich SM. 1990. Estimation of radiation risk from screening mammography: recent trends and comparison with expected benefits. Radiology 174(3 Pt 1):638-647.
29. Feig SA, Hendrick RE. 1997. Radiation risk from screening mammography of women aged 40-49 years. J Natl Cancer Inst Monogr (22):119-124.
30. Fisher B, Constantino J, Redmond C, et al. 1993. Lumpectomy compared with lumpectomy and radiation therapy for the treatment of intraductal breast cancer. N Engl J Med 328:1581-1586.
31. Fisher B, Dignam J, Wolmark N, Mamounas E, Costantino J, Poller W, Fisher ER, Wickerham DL, Deutsch M, Margolese R, Dimitrov N, Kavanah M. 1998. Lumpectomy and radiation therapy for the treatment of intraductal breast cancer: findings from National Surgical Adjuvant Breast and Bowel Project B-17. J Clin Oncol 16(2):441-452.
32. Fisher B, Dignam J, Wolmark N, Wickerham DL, Fisher ER, Mamounas E, Smith R, Begovic M, Dimitrov NV, Margolese RG, Kardinal CG, Kavanah MT, Fehrenbacher L, Oishi RH. 1999. Tamoxifen in treatment of intraductal breast cancer: National Surgical Adjuvant Breast and Bowel Project B-24 randomised controlled trial. Lancet 353(9169):1993-2000.
33. Fletcher SW. 1995. Why question screening mammography for women in their forties? Radiol Clin North Am 33(6):1259-1271.
34. Fletcher SW, Elmore JG. 2003. Clinical practice. Mammographic screening for breast cancer. N Engl J Med 348(17):1672-1680.
35. Fonseca R, Hartmann LC, Petersen IA, Donohue JH, Crotty TB, Gisvold JJ. 1997. Ductal carcinoma in situ of the breast. Ann Intern Med 127(11):1013-1022.
36. Franceschi S, Levi F, La Vecchia C, Randimbison L, Te VC. 1998. Second cancers following in situ carcinoma of the breast. Int J Cancer 77(3):392-395.
37. Frankenberg-Schwager M, Garg I, Fran-Kenberg D, Greve B, Severin E, Uthe D, Gohde W. 2002. Mutagenicity of low-filtered 30 kVp X-rays, mammography X-rays and conventional X-rays in cultured mammalian cells. Int J Radiat Biol 78(9):781-789.
38. George WD, Houghton J, Cuzick J, et al. 2000. Radiotherapy and tamoxifen following complete local excision in the management of ductal carcinoma in situ: preliminary results from the UK DCIS trial. Proc Am Soc Clin Oncol Abstract 270.
39. Gotzsche PCOO. 2000. Is screening for breast cancer with mammography justifiable? Lancet 355:129-133.
40. Harris JR, Lippman ME, Veronesi U, Willett W. 1992. Breast cancer (2). N Engl J Med 327(6):390-398.
41. Holland R, Hendricks JH, Verbeek AL, et al. 1990. Extent, distribution, and mammographic/histological correlations of breast ductal carcinoma in situ. Lancet 335:519-522.
42. Holland R, Hendriks JH. 1994. Microcalcifications associated with ductal carcinomain-situ: mammographic-pathological correlation. Semin Diag Pathol 11:181-192.
43. Institute of Medicine. 2003. Fulfilling the Potential of Cancer Prevention and Early Detection. Washington DC: The National Academies Press.
44. Jatoi I, Baum M. 1995. Mammographically detected ductal carcinoma in situ: are we overdiagnosing breast cancer? Surgery 118(1):118-120.
45. Jeffrey SS, Pollack JR. 2003. The diagnosis and management of pre-invasive breast disease: promise of new technologies in understanding pre-invasive breast lesions. Breast Cancer Res 5(6):320-328.
46. Jensen RA, Page DL. 2003. Ductal carcinoma in situ of the breast: impact of pathology on therapeutic decisions. Am J Surg Pathol 27(6):828-831.
47. Julien JP, Bijker N, Fentiman IS, Peterse JL, Delledonne V, Rouanet P, Avril A, Sylvester R, Mignolet F, Bartelink H, Van Dongen JA. 2000. Radiotherapy in breast-conserving treatment for ductal carcinoma in situ: first results of the EORTC randomised phase III trial 10853. EORTC Breast Cancer Cooperative Group and EORTC Radiotherapy Group. Lancet 355(9203):528-533.
48. Jung H. 2001. Is there a real risk of radiation-induced breast cancer for postmenopausal women? Radiat Environ Biophys 40(2):169-174.
49. Kerlikowske K, Grady D, Barclay J, Frankel SD, Ominsky SH, Sickles EA, Ernster V. 1998. Variability and accuracy in mammographic interpretation using the American College of Radiology Breast Imaging Reporting and Data System. J Natl Cancer Inst 90(23):1801-1809.
50. Kerlikowske K, Molinaro A, Cha I, Ljung B-M, Ernster VL, Stewart K, Chew K, Moore D2, Waldman F. 2003. Characteristics associated with recurrence among women with ductal carcinoma in situ treated by lumpectomy. J Natl Cancer Inst 95(22):1692-1702.
51. Kessar P, Perry N, Vinnicombe SJ, Hussain HK, Carpenter R, Wells CA. 2002. How significant is detection of ductal carcinoma in situ in a breast screening programme? Clin Radiol 57(9):807-814.
52. Kestin LL, Goldstein NS, Martinez AA, Rebner M, Balasubramaniam M, Frazier RC, Register JT, Pettinga J, Vicini FA. 2000. Mammographically detected ductal carcinoma in situ treated with conservative surgery with or without radiation therapy: patterns of failure and 10-year results. Ann Surg 231(2):235-245.
53. Kolb TM, Lichy J, Newhouse JH. 2002. Comparison of the performance of screening mammography, physical examination, and breast US and evaluation of factors that influence them: an analysis of 27,825 patient evaluations. Radiology 225(1):165-175.
54. Kopans DB. 2003. Re: Detection of ductal carcinoma in situ in women undergoing screening mammography. J Natl Cancer Inst 95(6):487; author reply 487-488.
55. Kornguth PJ, Keefe FJ, Conaway MR. 1996. Pain during mammography: characteristics and relationship to demographic and medical variables. Pain 66(2-3):187-194.
56. Kote-Jarai Z, Eeles RA. 1999. BRCA1, BRCA2 and their possible function in DNA damage response. Br J Cancer 81(7):1099-1102.
57. Lagios MD. 1990. Duct carcinoma in situ. Pathology and treatment. Surg Clin North Am 70(4):853-871.
58. Lagios MD, Margolin FR, Westdahl PR, Rose MR. 1989. Mammographically detected duct carcinoma in situ. Frequency of local recurrence following tylectomy and prognostic effect of nuclear grade on local recurrence. Cancer 63(4):618-624.
59. Land CE, Tokunaga M, Koyama K, Soda M, Preston DL, Nishimori I, Tokuoka S. 2003. Incidence of female breast cancer among atomic bomb survivors, Hiroshima and Nagasaki, 1950-1990. Radiat Res 160(6):707-717.
60. Law J, Faulkner K. 2001. Cancers detected and induced, and associated risk and benefit, in a breast screening programme. Br J Radiol 74(888):1121-1127.
61. Li CI, Anderson BO, Daling JR, Moe RE. 2003. Trends in incidence rates of invasive lobular and ductal breast carcinoma. JAMA 289(11):1421-1424.
62. Liberman L. 2000. Ductal carcinoma in situ: Percutaneous biopsy considerations. Semin Breast Dis 3:14-25.
63. Lidbrink E, Elfving J, Frisell J, Jonsson E. 1996. Neglected aspects of false positive findings of mammography in breast cancer screening: analysis of false positive cases from the Stockholm trial. BMJ 312(7026):273-276.
64. Liu E, Thor A, He M, Barcos M, Ljung BM, Benz C. 1992. The HER2 (c-erbB-2) oncogene is frequently amplified in in situ carcinomas of the breast. Oncogene 7(5):1027-1032.
65. Maguire HC Jr, Hellman ME, Greene MI, Yeh I. 1992. Expression of c-erbB-2 in in situ and in adjacent invasive ductal adenocarcinomas of the female breast. Pathobiology 60(3):117-121.
66. McCann J, Stockton D, Godward S. 2002. Impact of false-positive mammography on subsequent screening attendance and risk of cancer. Breast Cancer Res 4(5):R11.
67. Meystre-Agustoni G, Paccaud F, Jeannin A, Dubois-Arber F. 2001. Anxiety in a cohort of Swiss women participating in a mammographic screening programme. J Med Screen 8(4):213-219.
68. Mirza NQ, Vlastos G, Meric F, Sahin AA, Singletary SE, Newman LA, Kuerer HM, Ames FC, Ross MI, Feig BW, Pollock RE, Buchholz TA, McNeese MD, Strom EA, Hortobagyi GN, Hunt KK. 2000. Ductal carcinoma-in-situ: long-term results of breast-conserving therapy. Ann Surg Oncol 7(9):656-664.
69. Mokbel K. 2003. Towards optimal management of ductal carcinoma in situ of the breast. Eur J Surg Oncol 29(2):191-197.
70. Moore E, Magee H, Coyne J, Gorey T, Dervan PA. 1999. Widespread chromosomal abnormalities in high-grade ductal carcinoma in situ of the breast. Comparative genomic hybridization study of pure high-grade DCIS. J Pathol 187(4):403-409.
71. Morrow M, Strom EA, Bassett LW, Dershaw DD, Fowble B, Harris JR, O’Malley F, Schnitt SJ, Singletary SE, Winchester DP. 2002. Standard for the management of ductal carcinoma in situ of the breast (DCIS). CA Cancer J Clin 52(5):256-276.
72. Mushlin AI, Kouides RW, Shapiro DE. 1998. Estimating the accuracy of screening mammography: a meta-analysis. Am J Prev Med 14(2):143-153.
73. Nystrom L, Andersson I, Bjurstam N, Frisell J, Nordenskjold B, Rutqvist LE. 2002. Long-term effects of mammography screening: updated overview of the Swedish randomised trials. Lancet 359(9310):909-919.
74. Olsen O, Gotzsche PC. 2001. Cochrane review on screening for breast cancer with mammography. Lancet 358(9290):1340-1342.
75. Page DL, Dupont WD, Rogers LW, Jensen RA, Schuyler PA. 1995. Continued local recurrence of carcinoma 15-25 years after a diagnosis of low grade ductal carcinoma in situ of the breast treated only by biopsy. Cancer 76(7):1197-1200.
76. Page DL, Dupont WD, Rogers LW, Landenberger M. 1982. Intraductal carcinoma of the breast: follow-up after biopsy only. Cancer 49(4):751-758.
77. Page DL, Gray R, Allred DC, Dressler LG, Hatfield AK, Martino S, Robert NJ, Wood WC. 2001. Prediction of node-negative breast cancer outcome by histologic grading and S-phase analysis by flow cytometry: an Eastern Cooperative Oncology Group Study (2192). Am J Clin Oncol 24(1):10-18.
78. Patel KJ, Yu VP, Lee H, Corcoran A, Thistlethwaite FC, Evans MJ, Colledge WH, Friedman LS, Ponder BA, Venkitaraman AR. 1998. Involvement of Brca2 in DNA repair. Mol Cell 1(3):347-357.
79. Pawluczyk O, Augustine BJ, Yaffe MJ, Rico D, Yang J, Mawdsley GE, Boyd NF. 2003. A volumetric method for estimation of breast density on digitized screen-film mammograms. Med Phys 30(3):352-364.
80. Pinckney RG, Geller BM, Burman M, Littenberg B. 2003. Effect of false-positive mammograms on return for subsequent screening mammography. Am J Med 114(2):120-125.
81. Raza S, Rosen MP, Chorny K, Mehta TS, Hulka CA, Baum JK. 2001. Patient expectations and costs of immediate reporting of screening mammography: talk isn’t cheap. Am J Roentgenol 177(3):579-583.
82. Rothfuss A, Schutz P, Bochum S, Volm T, Eberhardt E, Kreienberg R, Vogel W, Speit G. 2000. Induced micronucleus frequencies in peripheral lymphocytes as a screening test for carriers of a BRCA1 mutation in breast cancer families. Cancer Res 60(2):390-394.
83. Rothkamm K, Lobrich M. 2003. Evidence for a lack of DNA double-strand break repair in human cells exposed to very low x-ray doses. Proc Natl Acad Sci USA 100(9):5057-5062.
84. Sandin B, Chorot P, Valiente RM, Lostao L, Santed MA. 2002. Adverse psychological effects in women attending a second-stage breast cancer screening. J Psychosom Res 52(5):303-309.
85. Sapir R, Patlas M, Strano SD, Hadas-Halpern I, Cherny NI. 2003. Does mammography hurt? J Pain Symptom Manage 25(1):53-63.
86. Schwartz GF, Patchefsky AS, Finkelstein SD, et al. 1989. Non-palpable in situ ductal carcinoma of the breast: predictors of multicentricity and microinvasion and implication for treatment. Arch Surg 124:29-32.
87. Sharp PC, Michielutte R, Freimanis R, Cunningham L, Spangler J, Burnette V. 2003. Reported pain following mammography screening. Arch Intern Med 163(7):833-836.
88. Sigfusson BF, Andersson I, Aspegren K, Janzon L, Linell F, Ljungberg O. 1983. Clustered breast calcifications. Acta Radiol Diagn (Stockh) 24(4):273-281.
89. Silverstein MJ, Barth A, Poller DN, Gierson ED, Colburn WJ, Waisman JR, Gamagami P. 1995. Ten-year results comparing mastectomy to excision and radiation therapy for ductal carcinoma in situ of the breast. Eur J Cancer 31A(9):1425-1427.
90. Silverstein MJ, Lagios MD, Craig PH, Waisman JR, Lewinsky BS, Colburn WJ, Poller DN. 1996. A prognostic index for ductal carcinoma in situ of the breast. Cancer 77(11):2267-2274.
91. Silverstein MJ, Recht A, Lagios MD. 2002. Ductal Carcinoma in Situ of the Breast. second ed. Philadelphia: Lippincott Williams and Wilkins.
92. Skinner KA, Silverstein MJ. 2001. The management of ductal carcinoma in situ of the breast. Endocr Relat Cancer 8(1):33-45.
93. Slanetz PJ. 2002. Hormone replacement therapy and breast tissue density on mammography. Menopause 9(2):82-83.
94. Solin LJ, Yeh IT, Kurtz J, Fourquet A, Recht A, Kuske R, McCormick B, Cross MA, Schultz DJ, Amalric R, et al. 1993. Ductal carcinoma in situ (intraductal carcinoma) of the breast treated with breast-conserving surgery and definitive irradiation. Correlation of pathologic parameters with outcome of treatment. Cancer 71(8):2532-2542.
95. Spelic DC. Dose and Image Quality in Mammography: Trends During the First Decade of MQSA. Accessed December 3, 2003. Web Page. Available at: http://www.fda.gov/cdrh/mammography/scorecard-article5.html.
96. Surveillance Epidemiology and End Results (SEER) Program (www.seer.cancer.gov). 2003. SEER*Stat Database: Incidence—SEER 9 Registry Public-Use, Nov. 2002 Submission (1973-2000), National Cancer Institute, DCCPS, Surveillance Research Program, Cancer Statistics Branch.
97. Tabar L, Vitak B, Chen HH, Yen MF, Duffy SW, Smith RA. 2001. Beyond randomized controlled trials: organized mammographic screening substantially reduces breast carcinoma mortality. Cancer 91(9):1724-1731.
98. The Consensus Conference Committee. 1997. Consensus Conference on the classification of ductal carcinoma in situ. Cancer 80(9):1798-1802.
99. Thornton H. 2000. Consequences of breast screening. Lancet 356(9234):1033.
100. Thornton H, Edwards A, Baum M. 2003. Women need better information about routine mammography. BMJ 327(7406):101-103.
101. Tunon-de-Lara C, de-Mascarel I, Mac-Grogan G, Stockle E, Jourdain O, Acharian V, Guegan C, Faucher A, Bussieres E, Trojani M, Bonichon F, Barreau B, Dilhuydy MH, Dilhuydy JM, Mauriac L, Durand M, Avril A. 2001. Analysis of 676 cases of ductal carcinoma in situ of the breast from 1971 to 1995: diagnosis and treatment—the experience of one institute. Am J Clin Oncol 24(6):531-536.
102. Ursin G, Astrahan MA, Salane M, Parisky YR, Pearce JG, Daniels JR, Pike MC, Spicer DV. 1998. The detection of changes in mammographic densities. Cancer Epidemiol Biomarkers Prev 7(1):43-47.
103. Ursin G, Parisky YR, Pike MC, Spicer DV. 2001. Mammographic density changes during the menstrual cycle. Cancer Epidemiol Biomarkers Prev 10(2):141-142.
104. Van Zee KJ, Liberman L, Samli B, Tran KN, McCormick B, Petrek JA, Rosen PP, Borgen PI. 1999. Long term follow-up of women with ductal carcinoma in situ treated with breast-conserving surgery: the effect of age. Cancer 86(9):1757-1767.
105. Vicini FA, Recht A. 2002. Age at diagnosis and outcome for women with ductal carcinoma-in-situ of the breast: a critical review of the literature. J Clin Oncol 20(11):2736-2744.
106. Viehweg P, Lampe D, Buchmann J, Heywang-Kobrunner SH. 2000. In situ and minimally invasive breast cancer: morphologic and kinetic features on contrast-enhanced MR imaging. MAGMA 11(3):129-137.
107. Walker RA, Dearing SJ, Lane DP, Varley JM. 1991. Expression of p53 protein in infiltrating and in-situ breast carcinomas. J Pathol 165(3):203-211.
108. Warnberg F, Bergh J, Holmberg L. 1999. Prognosis in women with a carcinoma in situ of the breast: a population-based study in Sweden. Cancer Epidemiol Biomarkers Prev 8(9):769-774.
109. Wazer DE, Gage I, Homer MJ, Krosnick SH, Schmid C. 1996. Age-related differences in patients with nonpalpable breast carcinomas. Cancer 78(7):1432-1437.
110. Welch HG, Black WC. 1997. Using autopsy series to estimate the disease “reservoir” for ductal carcinoma in situ of the breast: how much more breast cancer can we find? Ann Intern Med 127(11):1023-1028.
111. White E, Velentgas P, Mandelson MT, Lehman CD, Elmore JG, Porter P, Yasui Y, Taplin SH. 1998. Variation in mammographic breast density by time in menstrual cycle among women aged 40-49 years. J Natl Cancer Inst 90(12):906-910.
112. White SC. 1992. 1992 assessment of radiation risk from dental radiography. Dentomaxillofac Radiol 21(3):118-126.
113. Yen MF, Tabar L, Vitak B, Smith RA, Chen HH, Duffy SW. 2003. Quantifying the potential problem of overdiagnosis of ductal carcinoma in situ in breast cancer screening. Eur J Cancer 39(12):1746-1754.
114. Zellars R, Wolff AC. 2003. Local failure and prognostic factors in ductal carcinoma in situ: concentration on recent publications. Curr Opin Obstet Gynecol 15(1):9-12.


























