4
Socioeconomic Status
A considerable body of evidence has established that individuals of low socioeconomic status are more likely to suffer from disease, to experience loss of functioning, to be cognitively and physically impaired, and to experience higher mortality (Adler et al., 1993, 1994; Marmot et al., 1997b; Preston and Taubman, 1994; Rogers et al., 2000; Williams, 1990). As illustrated in Figure 4-1, this association holds true for nearly all major causes of morbidity, functioning loss, disability, and mortality. This figure uses education as an indicator of socioeconomic status; similar data using income, occupation, or wealth would generally show the same relationships. For instance, Table 4-1 shows that a similar relationship between wealth and self-reported health holds across adult ages.
THE HEALTH GRADIENT AND RECIPROCAL CAUSATION
The influence of socioeconomic status on health is assumed to begin in the prenatal environment and continue through life. Parents’ socioeconomic status affects childhood conditions, such as exposure to toxins and infectious agents. These conditions affect health immediately and possibly for years afterwards, the effects being only partly moderated by later changes in status (Blackwell et al., 2000; Hayward et al., 2000; Kuh and Davey-Smith, 1997; Preston et al., 1998). Childhood socioeconomic differences have been recently shown to account for a substantial part of the later mortality gap between blacks and whites (Warner and Hayward, 2002).
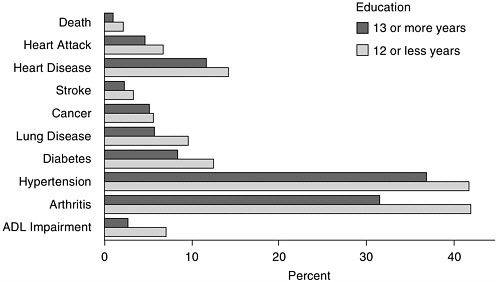
FIGURE 4-1 Death within 2 years and prevalence of various conditions, by years of education (in percent).
NOTE: ADL, activities of daily life.
SOURCE: Data from Health and Retirement Survey, as reported by Crimmins et al. (2004).
The health gradient by socioeconomic status widens through childhood and the adult working years and then contracts after retirement (Case et al., 2002; Crimmins et al., 2004; House et al., 1994). After some age, changes in some aspects of socioeconomic status have diminishing effects on health; it is unclear which changes in aspects of socioeconomic status continue to affect health in old age.
Assessing the effect of lifetime socioeconomic conditions on health is complicated by the fact that health also affects income and wealth, especially among adults (Smith, 1999). Table 4-1 shows that those with “fair” or “poor” self-reported health in 1984 not only had much lower wealth in that year but also saw their wealth grow less than that of others over the next 10 years. Though the table does not show it, smaller gains in wealth were associated with less favorable health outcomes.
Reciprocal causation has been one of the most difficult issues to deal with in this literature, and it is often ignored or dismissed as a minor factor. However, Smith and Kington (1997) show that much of the correlation between current income and health among males in their 50s appears to be the effect of health on income, rather than the reverse, and Adams et al. (2003) argue that among the retired population, there may be no income
TABLE 4-1 Median Household Wealth and Self-Reported Health Status
|
|
Wealth (in thousands)a |
||
|
Age Group and 1984 Health Status |
1984 |
1989 |
1994 |
|
All Households |
|||
|
Excellent |
68.3 |
99.3 |
127.9 |
|
Very good |
66.3 |
81.9 |
90.9 |
|
Good |
51.8 |
59.6 |
64.9 |
|
Fair/poor |
39.2 |
36.0 |
34.7 |
|
25-34 |
|||
|
Excellent |
28.5 |
51.5 |
84.3 |
|
Very good |
19.5 |
34.7 |
50.1 |
|
Good |
10.5 |
17.2 |
28.2 |
|
Fair/poor |
0.9 |
3.1 |
10.4 |
|
35-44 |
|||
|
Excellent |
100.1 |
150.1 |
194.7 |
|
Very good |
81.1 |
96.3 |
117.5 |
|
Good |
49.5 |
45.3 |
83.5 |
|
Fair/poor |
23.8 |
15.5 |
32.4 |
|
45-54 |
|||
|
Excellent |
164.2 |
198.3 |
255.8 |
|
Very good |
132.1 |
176.2 |
186.9 |
|
Good |
87.8 |
76.9 |
97.1 |
|
Fair/poor |
59.7 |
61.6 |
69.4 |
|
aIn 1996 dollars. SOURCE: Data from Panel Study of Income Dynamics, as reported by Smith (1999: Table 1, p. 147). |
|||
effects on health. The key question is not which of the two alternative pathways can be dismissed entirely. Rather, the more appropriate question may be which subset of the well-documented associations between socioeconomic status and health is most susceptible to interpretations that flow from health to status.
STATUS, RACE, AND ETHNICITY
The health gradient by socioeconomic status is important for racial and ethnic differences because socioeconomic status differs considerably by race and ethnicity. Table 4-2 shows some variations in socioeconomic status among older people. Older black and Hispanics are much less likely than whites to have a high school diploma or a college degree and much more likely to live in poverty. Older Asians have relatively more education, but compared with whites, twice the percentage of them live in poverty. Similar figures for American Indians and Alaska Natives are not available, but
TABLE 4-2 Socioeconomic Status by Race and Ethnicity Among Persons Aged 65 Years and Older
|
|
Percentage with |
Percentage in Poverty |
|||
|
Racial or Ethnic Group |
High School Diploma 1998 |
Bachelor’s Degree 1998 |
Both Sexes 1998 |
Men 1997 |
Women 1997 |
|
White |
71.6 |
16.0 |
8.2 |
5.6 |
11.5 |
|
Black |
43.7 |
7.0 |
26.4 |
21.8 |
28.8 |
|
Hispanic |
29.4 |
5.4 |
21.0 |
20.3 |
26.3 |
|
Asian or Pacific Islander |
65.1 |
22.2 |
16.0 |
—a |
—a |
|
aNo data. SOURCES: Data from Federal Interagency Forum on Aging Related Statistics (2000) and Kramarow et al. (1999). |
|||||
1990 household data suggest levels of poverty among American Indians similar to those for blacks, and levels for Alaska Natives similar to those for Asians (U.S. Census Bureau, 1990). Socioeconomic variations such as these, coupled with similar variations at younger ages, partly explain racial and ethnic differences in a number of health outcomes (Hayward et al., 2000; Smith and Kington, 1997).
When socioeconomic status is controlled, health differences between blacks and whites in mortality and functional limitations are sometimes eliminated (Kington and Smith, 1997), though differences may not disappear for specific diseases. Good examples of large racial or ethnic differences that are not explained by socioeconomic status are hypertension among black men and diabetes among black and Hispanic men (Crimmins et al., 2004). There also appear to be significant nonlinearities in the effects of income and wealth, as these factors have a much stronger effect on health in the bottom third of their respective distributions than in the top third. Taking these nonlinearities into account may help further explain black-white health differences. However, the role of socioeconomic status in explaining Asian-white differences is less clear, and it does not explain the relative health advantage of Hispanics.
One complication in any comparison is the possibility that socioeconomic measures may signify something different for each group (Kaufman et al., 1997; Williams and Collins, 1995). Black high school graduates, for instance, do not exhibit the same levels of knowledge and skills as whites (Maxwell, 1994). Equal incomes may not be truly equal if they do not translate into the same purchasing power in different communities (Alexis et al., 1980; Williams and Collins, 1995). The effect on health differences if
controls were possible with exactly equivalent socioeconomic measures is not known.
MECHANISMS
Socioeconomic status affects health through a variety of mechanisms, including psychosocial factors, health behaviors, and health care (Anderson, 1995; Hummer et al., 1998; Kington and Nickens, 2001; Seeman and Crimmins, 2001). In general, persons of higher socioeconomic status are less exposed to health-threatening conditions and have more resources to buffer health threats. For instance, persons with more education have greater ability to self-monitor and manage highly effective but complicated therapies for such conditions as diabetes and HIV (Goldman and Smith, 2002). Variation in this ability may involve other factors in addition to education, however. In general, the intervening mechanisms that have been studied through which socioeconomic status affects health—such as behavior risk factors (Lantz et al., 2001)—do not entirely account for the effects of socioeconomic status, leaving much of these effects still to be explained. In addition, these intervening mechanisms could operate independently of socioeconomic status.
Additional factors may also obscure the effects of status. For instance, recent immigrants often have lower incomes, at least initially, but enjoy health advantages for other reasons. Working-age immigrants, particularly those with employment visas or who enter as spouses of U.S. citizens, appear to be strongly selected for health (Jasso et al., 2004). Assessing the role of socioeconomic factors in group health, therefore, requires attention to health in countries of origin and to the average healthiness of the original immigrants, the diversity in health status among them, and their subsequent health trajectories over their lifetimes and those of their descendants.
In addition to these individual-level mechanisms, considerable research in the last decade argues that macrolevel socioeconomic factors affect individual health outcomes (Marmot, 2000; Wilkinson, 1997). One form of the hypothesis is that inequality, as measured in various ways, has a negative effect on individual health outcomes, especially for those at the bottom of the social and economic hierarchy. In this view, the cumulative stress of being at the bottom of the hierarchy eventually takes a toll in poorer health. This is an important scientific hypothesis with far-reaching implications. However, much of the influential early work on this subject suffered from severe limitations, including inadequate conceptualization of and difficulties in separating individual from macrolevel influences. Recent work by Deaton and Paxson (2001) argues that, at least for U.S. blacks and whites, the evidence that rising levels of income inequality have negative health consequences is dubious.
Another factor strongly linked to socioeconomic status is the quality of one’s physical environment (Adler and Newman, 2002; Evans and Kantrowitz, 2002). U.S. data indicate that substandard housing, crowding, elevated noise levels, limited ability to regulate temperature and humidity, and exposure to noxious pollutants and allergens (including lead, smog, particulates, and dust mites) are all common in poor, segregated communities (Been, 1997; Bullard, 1994; Evans and Saegert, 2000; Mohai and Bryant, 1992, 1998; Pearlin et al., 2001). For both adults and children, increased respiratory and other health problems result from residing near hazardous waste sites (Dolk et al., 1998; Goldberg et al., 1999), residential exposure to air pollution (Keeler et al., 2002; Pope et al., 2002; Thurston and Ito, 2001), and deteriorated housing conditions (Peat et al., 1998; Rauh et al., 2002). However, the exact contribution of such environmental conditions to racial and ethnic differences in health status, and the extent to which they add to other socioeconomic effects or possibly explain them, is still unclear.
NEEDED RESEARCH
Although socioeconomic status is strongly linked to health, many research questions remain about the nature of this linkage and the contribution of socioeconomic status to racial and ethnic health differences.
Research Need 6: Clarify the degree to which socioeconomic status accounts for racial and ethnic differences in health outcomes over the life course.
Some differences are not explained by socioeconomic status, or even run counter to the expected. Would better measures of education, or other aspects of status, provide clarification? Would incorporating measures of earlier socioeconomic status, perhaps status prior to immigration, explain more of the differences? Is better modeling needed of presumed nonlinear relationships? What differences in health outcomes would still not be explained even if all these questions could be answered? The possibility that the effects of socioeconomic factors are misestimated because of differential survival by race and ethnic group also requires consideration.
One complication is that dimensions of socioeconomic status are not identical in their effects on racial and ethnic health differences. Analysts need to know the most appropriate aspect of status to consider—income, wealth, education, or occupation. Health differences by race or ethnicity will look different if one or the other indicator is controlled. Policy makers need to know which aspect of status matters most. It makes a great deal of difference to policy whether differences are largely due to income, in which case increasing the income of the poor gains greater weight from its possible
effect on health; or education, in which case equality of educational opportunity, or affecting the outcomes of education—improving individual access to information and the ability to process it effectively—become long-term priorities. That identical levels on the same indicators may have different implications across groups also requires attention.
Variability in the effect of socioeconomic status over the life course is an additional complication. In late life, which aspects of status have the most influence on health? At the start of the life course, socioeconomic status is acquired from one’s parents, who not only provide financial support but also influence the education of their children. Children may also acquire from their parents habits and personal characteristics that directly affect health. How intergenerational transmission of all these factors is patterned by race or ethnicity may be important, given the influence of early life factors on late-life health. Reciprocal causation between socioeconomic status and health is an important aspect of the lifelong effect of status, and whether it operates similarly across the life course for different racial and ethnic groups needs study.
Research Need 7: Identify the mechanisms through which socioeconomic status produces racial and ethnic differences in health among the elderly, and identify other factors that complicate its effects.
Socioeconomic status may have an effect because of its links to commonly recognized health behaviors, other psychosocial factors, multiple dimensions of access to health care, geographic residence, environmental conditions, and nativity and duration of residence, especially for Hispanics and other immigrant groups. In what circumstances, or for which subgroups, are racial and ethnic differences robust to controls for such variables? Which controls are most important and why? If none of them adequately explain the effects of status, how does it come to modify health outcomes?
This analysis will require attending not just to socioeconomic variation in disease prevalence but to variation in the disease process: the onset of conditions, their severity, duration, and effects on survival (Crimmins et al., 2004). The relevant mechanisms may differ at each stage.
Whether macrolevel mechanisms are important is another aspect worth studying. Can aggregate effects be verified, and is income inequality the most appropriate aggregate indicator? If such aggregate effects exist, how do they work—at the local, regional, or societal levels, or even at the workplace level, and through what mechanisms? How are such aggregate macromarkers related to other aggregate variables, such as social capital and group cohesion, and how do such factors vary by race and ethnicity?







