5
Managing Scale-up of Antiretroviral Therapy
Antiretrovirals (ARVs) alone are not the answer to the HIV/AIDS pandemic. Linked inextricably to the ultimate success of these drug interventions are logistics systems that ensure the safe and timely procurement and delivery of the drugs and other commodities to their intended destinations, and to the people whose lives depend on them. Antiretrovial therapy (ART) scale-up will require tens of thousands of health care workers with the experience and training needed to treat so many people with a complex medical intervention. Well-functioning countrywide ART programs will also require significant investments to build the capacity of a broad range of other technical and managerial expertise, from data analysts to procurement strategists to supervisory personnel. Additionally, ART scale-up will require dedication of the necessary funds and other resources to the enormous task of securing and delivering effective drugs. Finally, both dedicated resources and processes will be needed to establish and maintain harmonized monitoring and evaluation systems that will not only measure the effectiveness of ART programs and outcomes, but also inform the ongoing improvement and optimization of the clinical and management operations of scale-up. An integrated management structure that includes these principal components will be necessary for the long-term success of ART programs.
BUILDING HUMAN RESOURCE CAPACITY
Although scientific data on health care personnel in resource-constrained settings, particularly sub-Saharan Africa, are extremely difficult
to collect, WHO surveys and general reports indicate that human resource capacity is generally extremely weak in such settings and in many places is a critically limiting factor in providing access to ART. In fact, some evidence suggests that ART scale-up could fail on these grounds alone (Kober and Van Damme, 2004). Many of those countries with the highest numbers of people living with HIV/AIDS have very few health care providers trained in comprehensive care for the disease (Liese et al., 2003; USAID, 2003). Many health workers have died as a result of untreated AIDS, and others have moved to wealthier countries in search of better pay and job security (Padarath et al., 2003; Pang et al., 2002; Tawfik and Kinoti, 2001). (For an extended review of human resource capacity considerations, see Appendix C.)
In acknowledgment of this situation, WHO’s 3-by-5 plan calls for the rapid training of tens of thousands of workers to aid in the delivery of ARVs. However, the medical complexity of HIV/AIDS therapy cannot be overestimated. Nor can the logistical complexity of reliably delivering ARVs to their intended destinations—a recurring process that can demand significant organizational skill and infrastructure—be ignored. Rapid scale-up will require sufficient expertise in all of the various nonmedical components of ART programming, as well as the more obvious health-sector roles. The problem is compounded not only by the shortage of trained workers with specific HIV/AIDS experience or expertise, but also by severe shortages in many resource-constrained settings of the well-trained professionals needed to handle other critical functions, such as commodity logistics, pharmaceutical regulation, laboratory support, information management, and operations research.
The seriousness of the situation is illustrated by an October 2003 report analyzing the cost and resource requirements associated with providing ART through the Zambian public health sector (Kombe and Smith, 2003). Despite key findings indicating that the provision of highly active antiretroviral therapy (HAART) to all clinically eligible patients will be prohibitively expensive, the report suggests that human resource capacity may become the most critical rate-limiting factor.
In the report, the estimated per-patient cost of the health care training necessary for public-sector ART scale-up in Zambia, with an initial goal of providing ARVs to 10,000 people, is US$3.70, which amounts to a total overall cost of $37,000 per year. That amount, which represents less than 1 percent of the estimated total per-patient cost (i.e., $488), would cover the marginal requirement for the estimated additional 13 full-time equivalent (FTE) doctors and nurses, 15 FTE pharmacists, and 32 FTE laboratory technicians needed to provide ART to 10,000 patients. Although the demand for laboratory technicians poses a challenge, meeting the overall workforce needs for achieving Zambia’s initial scale-up goal is quite fea-
sible, and the amount of funding necessary to bring the workforce to full capacity is relatively minimal. The low per-patient cost of training compared with the cost of the drugs and other components of scale-up suggests that serious, well-planned investments in health worker training would be an extremely cost-effective move.
On the other hand, 10,000 people still represent only about 10 percent of the total number of Zambians currently in need of ART, and many more infected but currently immunocompetent Zambians will join these ranks over the next decade. Providing full ARV coverage for the entire clinical population in need, as it stands now (i.e., about 100,000 people, rising to about 330,000 in 5 years, but also assuming a 20 percent mortality rate), would marginally require an additional 130 FTE nurses and physicians in the first year and 429 by the fifth year, and 316 laboratory technicians in the first year and more than a 1,000 by the fifth year. And these estimates do not even begin to address additional voluntary counseling and testing (VCT) staffing needs. Clearly, the human workforce needs for full coverage are immense.
Throughout sub-Saharan Africa in particular, the reality of the human resource situation is sobering, as these accounts and a wealth of qualitative reports attest (Kober and Van Damme, 2004). Recent data related to the overall health-sector human resource crisis in Africa and collected for the U.S. Agency for International Development (USAID) reveal that newly constructed health facility structures, including clinics and hospitals, remain unstaffed or understaffed throughout sub-Saharan Africa, as general efforts to expand the network of such facilities have greatly outpaced efforts to build human resource capacity. For example, despite vigorous efforts by the government of Mali to expand the number of its community health centers to 533, 43 percent of these centers were not functioning as of January 2001, with the remainder not operating because of a shortage of personnel to staff them (Lynch and Diallo, 2001; USAID, 2003). As it takes 3 to 4 years to train and deploy nurses and 5 or more years to train and deploy physicians, it is clear that without sufficient and aggressive training initiatives, this gap between physical infrastructure and human resource capacity will continue to widen.
Given the desperate and growing demand for health workers and the losses of trained workers to better jobs in more well-to-do countries, many African nations have reportedly been encouraged to adopt human resource policies that lead to the deliberate overproduction of health workers to fill the growing gaps in human resource capacity. Filling these gaps is not a simple task, however, as the African health sector’s human resource crisis is multidimensional and involves a complex set of underlying upstream and more-proximal causal factors (Puku, 2002; Narasimhan et al., 2004; Schwab, 2001). The problem encompasses not just the scarcity of well-
trained health workers, but also generally poor morale and staff motivation, insufficient management, an imbalance between urban and rural workforces, and strains on human resources caused by infrastructure changes and new, unfamiliar practices and technologies (see Table 5-1).
The burden of HIV/AIDS, which amounts to nearly one-fifth of the disease burden in sub-Saharan Africa, has not only dramatically increased the patient volume and associated workforce needs, but also led to the death of many health workers. According to one report, AIDS-related mortality accounts for 19 to 53 percent of all deaths among government staff, including public-sector health workers, in most African countries (USAID, 2003). Moreover, the number of hours or days of work lost due to AIDS-related illness can be substantial, further reducing actual workforce capacity.
Unfortunately, quantitative data and objective analyses of the situation are scarce. Most available data come from only three countries (Malawi, Zambia, and Zimbabwe), although these are by no means the only countries facing this critical problem. The lack of data is due in large part to a generally nonexistent personnel information system, which itself is indicative of how seriously neglected the issue is.
The human resource crisis in the health sectors of resource-constrained settings reflects the underlying crisis in tertiary education throughout the developing world, particularly in sub-Saharan Africa. The quality of such education tends to be low; access is limited; and as most health professional training is conducted under the auspices of national governments (through their ministries of health), there is not enough public money available to fund the numbers and types of formal preservice training programs that are needed (an issue discussed further below). In short, the production of new workers has not kept pace with the growing demand for greater workforce capacity. A recent report indicates that when countries do receive aid to build schools and training hostels, they often do not receive the funds needed to support the organizational programs those facilities house. Malawi, for example, has reportedly closed medical and nursing schools during midterm because of a lack of funds to support faculty and student services. Between 1996 and 1999, two of Zambia’s public universities reportedly only received 45 percent of expected funds from the treasury (USAID, 2003).
Over the last decade, the underfunding of preservice training for nurses, physicians, and other medical and allied professionals has contributed to a generally limited teaching capacity, significant curriculum gaps, and greater difficulty in enforcing qualification and practice standards. Graduates often are not well prepared to work in the field or at the front lines of public health services. Box 5-1 describes one intiative aimed at addressing this
TABLE 5-1 African Countries by Health Care Worker/Population Ratios, late 1990s
|
Population per Doctor |
Countries |
|
1 per 30,000 or more |
Burkina Faso, Central African Republic, Chad, Eritrea, Ethiopia, Gambia, Malawi, Mozambique, Niger, and Tanzania (10) |
|
1 per 20,000 |
Angola, Benin, Comoros, D.R. Congo, Lesotho, Mali, Rwanda, Sierra Leone, Somalia, Togo, Uganda, and Zambia (12) |
|
1 per 10,000 |
Burundi, Cameroon, Cote d’Ivoire, Djibouti, Ghana, Madagascar, Senegal, Sudan, and Swaziland (9) |
|
1 per 5,000 |
Botswana, Cape Verde, D.R. Congo, Equitorial Guinea, Gabon, Guinea, Guinea-Bissau, Kenya, Mauritania, Mauritius, Namibia, Nigeria, Sao Tome and Principe, Seychelles, South Africa, Swaziland, and Zimbabwe (16) |
|
Population per Nurse |
Countries |
|
1 per 10,000 or more |
Central African Republic, Gambia, and Mali (3) |
|
1 per 5,000 |
Benin, Burkina Faso, Chad, Eritrea, Madagascar, Niger, Senegal, Togo, and Uganda (9) |
|
1 per 2,000 |
Cape Verde, Comoros, Cote d’Ivoire, D.R. Congo, Equitorial Guinea, Ghana, Guinea, Lesotho, Sierra Leone, and Sudan (10) |
|
1 per 1,000 |
Angola, Botswana, Djibouti, D.R. Congo, Guinea-Bissau, Kenya, Mauritania, Mauritius, Namibia, Nigeria, Sao Tome and Principe, Seychelles, South Africa, Tanzania, Zambia, and Zimbabwe (16) |
|
Population per Midwife |
Countries |
|
1 per 20,000 |
Angola, Burkina Faso, Central African Republic, Chad, Equitorial Guinea, Eritrea, Guinea, Mali, Niger, and Sierra Leone (10) |
|
1 per 10,000 |
Benin, Gambia, Madagascar, Mauritania, Senegal, and Togo (6) |
|
1 per 5,000 |
Comoros, Congo, Cote d’Ivoire, Guinea-Bissau, and Uganda (5) |
|
1 per 2,000 |
Ghana, Lesotho, Namibia, Nigeria, Sao Tome and Principe, Seychelles, Tanzania, and Zimbabwe (8) |
|
Overall, the population per doctor in the developing world is 1:1,400; in industrialized nations, it is 1 per 300. Population per nurse in the developing world is 1:1,700; in the industrialized world, it is 1 per 170. |
|
|
SOURCE: USAID, 2003. |
|
|
BOX 5-1 The U.S. Health Resources and Services Administration and the Centers for Disease Control and Prevention established the International Training and Education Center on HIV (I-TECH) in 2002 to address human capacity development for care and treatment in the countries hardest hit by the AIDS epidemic. One goal of I-TECH is to support health care worker training programs that are locally determined and self-sustaining. Together with its domestic and international partners, I-TECH conducts needs assessments in high-priority areas; develops standards for education, training, and evaluation; disseminates best practices in human capacity development; assists local partners with training; and hosts study and exchange visits. I-TECH uses experienced clinicians, trainers, and program planners for a host of activities, including the following:
I-TECH currently works with the CDC Global AIDS Program and its collaborators in the Caribbean region, as well as in additional countries including Botswana, Ethiopia, India, Malawi, Namibia, South Africa, Thailand, and Zimbabwe. SOURCE: International Training and Education Center on HIV, 2004. |
need, while Box 5-2 reviews how the factors discussed above affect the potential role of nurse-based care.
To aid in the effort to bolster human resource capacity in resourceconstrained settings, multinational participation is encouraged. Although partnerships between institutions in the developed and developing worlds
|
BOX 5-2 It is estimated that some two-thirds of the burden of care for HIV/AIDS in Africa could potentially be addressed by community health nurses. The Médecins sans Frontières (MSF) program in Khayelitsha, South Africa, is a good example of a successful heavily nurse-based prevention and ART program. (For more detail on this program, see Chapter 2.) Each clinic team consists of one physician, two nurses, and two counselors. Although the physician plays a more prominent role initially, the nurses are becoming increasingly responsible for patient follow-up visits to the clinics (every 1 to 2 months), particularly as the number of people being treated increases. As of December 2003, there were 750 patients receiving ARVs through MSF; an additional 550 are expected to become part of the program this year. Another South African MSF program in Lusikisiki, which was initiated in January 2003 and aims to have 400 people on ART by December 2004, is operated entirely by nurses, counselors, and volunteers. Prior to MSF’s arrival, none of the country’s 12 rural nurse-run clinics had been visited by a physician in 5 years. Now doctors are responsible for training the nurses in ART, as well as OI therapy, prevention of mother-to-child transmission (PMTCT), and VCT, and for supervising newly trained nurses for 1 to 3 weeks before they work by themselves. Thereafter, doctors rotate through the clinics fortnightly. Yet despite this potential for nurse-based care to play a key role in ART scale-up, there are serious nursing shortages and problems with nurse training. Providers must be able to determine when to start, stop, or switch therapy; to explain the often complex dosing regimens and the side effects that may result; and to manage appropriate and adequate monitoring to slow the emergence of multidrug resistance. Knowledge and training for ARV providers are particularly important in settings not well equipped with sophisticated laboratory and monitoring equipment and resources. Although adherence and treatment success are possible based on clinical criteria alone, this is true only if health care providers are knowledgeable and capable with regard to monitoring and evaluating patient response to treatment in the absence of laboratory monitoring. There is an urgent need for an objective evaluation of the extent to which nurse-based care can fill the gaps in human resource capacity. |
will undoubtedly play a significant role in training, mentoring, and transferring knowledge, the value and usefulness of south–south partnerships should also be recognized.
Recommendation 5-1. Efforts should be made to augment mechanisms that can be used to mobilize larger numbers of trained professionals from resource-rich countries with extensive and relevant expertise to provide technical assistance and training to countries in need. Such an HIV/AIDS corps would serve to strengthen long-term ties among health professionals working to fight HIV/AIDS in all countries. A variety of
innovative governmental and private-sector mechanisms should be designed and expanded to bring qualified volunteer medical professionals into both urban and rural areas to support prevention, care, and training programs relevant to ART scale-up. The required expertise and skills and the areas for placement in country should be determined by local programs.
Recommendation 5-2. Donors and organizations with relevant expertise (e.g., academia, industry, public health agencies, nongovernmental organizations) should support active partnerships among all institutions possessing such expertise and those seeking to acquire the benefits of training; mentoring; and the transfer of antiretroviral therapy– related medical, technical, and managerial knowledge and skills. Partnerships among medical institutions within and across national borders should be encouraged by donors and governmental authorities. These twinning relationships should support the transfer of appropriate technology; expertise in medicine, monitoring and evaluation, and applied and operations research; and lessons learned. Physical and electronic means should be used to provide ongoing support for these partnerships.
Recommendation 5-3. Expertise within the AIDS Education and Training Center networks sponsored by the U.S. government and similar initiatives by other countries should be utilized to support the development of effective training programs in HIV care in order to prepare local physicians, nurses, community health workers, laboratory professionals, pharmacists, and logisticians in heavily HIV-afflicted countries facing severe human resource shortages.
DEVELOPING A SUSTAINABLE WORKFORCE
The Brain Drain
The brain drain (i.e., the departure of trained and educated individuals from one place to another) has had severe impacts on the health care sector of developing countries. Higher wages, better living conditions, and increased chances for career advancement are a few of the main reasons that health care workers are leaving their native countries (Dovlo, 2003; Padarath et al., 2003). The brain drain can occur domestically or internationally, with effects being felt at either the regional or national level. Not only are there not enough trained health care workers in most resourceconstrained settings, but the numbers are rapidly declining. As noted above, well-trained workers are leaving in search of better-paying jobs, both locally and abroad and in both the private and nongovernmental organiza-
tion (NGO) sectors, thus creating an even greater need for more trained personnel in the most resource-constrained settings (see Box 5-3). According to a recent USAID-sponsored report, data from Ghana, Zambia, and Zimbabwe show that annual losses from the public health sector range from 15 to 40 percent (USAID, 2003). These losses are due to emigration (in search of better-paying jobs), shifts from the public to the private sector, deaths from HIV/AIDS, and early retirement. The situation varies regionally and even within single countries, as the distribution of health workers is heavily skewed toward urban areas (see below). An even greater problem may be the loss of African-trained (and -financed) workers to industrial countries, where shortages of health-sector workers, particularly nurses, appear to be fueling the demand (Bundred and Levitt, 2000; Pang et al., 2002).
Although the loss of nurses and physicians may be the most obvious and commonly cited aspect of the human resource crisis in Africa and in the developing world generally, some experts argue that the loss of pharmacists is an even greater problem (Katerere and Matowe, 2003). Pharmacies are commonly considered the “poor man’s clinic” because they offer free consultations and are usually more accessible than primary health care facilities. As indicated in the previous chapter, pharmacist-led counseling is one of the few adherence interventions that are actually evidence-based. Thus the loss of pharmacists not only forces the closure of pharmacies, thereby reducing the accessibility of ARVs, but also comes at a time when the management and counseling skills of pharmacists are desperately needed to ensure the rational use of ARVs.
For example, the South African Pharmacy Council recently reported that 600 registered pharmacists emigrated in 2001 alone (Katerere and Matowe, 2003). This is alarming, as only 1,000 students graduate from South African pharmacy schools each year. Also in 2001, more than 60 pharmacists left Zimbabwe—an even more alarming statistic as that country produces only 40 pharmacists a year. Not only are practicing pharmacists and pharmacy school graduates emigrating, but so, too, are pharmacy school academic staff. According to one anecdotal report, many nonpharmacy graduates are teaching courses in South African pharmacy schools, and almost all of the academic staff of the University of Zimbabwe department of pharmacy have emigrated.
As most African governments already allocate 50 to 70 percent of their overall public health expenditures to salaries and wages, there is little money left over to address the problematic salary differences between local civil service and private, NGO, or foreign employment opportunities for physicians and other highly trained workers (Over, 2004; USAID, 2003). The pandemic of HIV/AIDS in developing countries has placed enormous strain
|
BOX 5-3 According to a USAID-sponsored report on the human resource crisis in Africa’s health sector (USAID, 2003), only 360 of the 1,200 doctors trained in Zimbabwe during the 1990s continue to practice within the country. A July 2003 article in Lancet (de Castella, 2003) reports that this country’s brain drain is particularly prevalent among doctors and anesthetists, who flee the country for the United Kingdom, New Zealand, and South Africa. A recent survey found that two-thirds of University of Zimbabwe medical students intended to leave the country after graduating, and one of the country’s major 1,000-bed hospitals lacks even a single qualified pharmacist. As the author of the Lancet article writes (p. 46), “If HIV/AIDS is the deadly cancer gnawing away at a population, then the brain drain is the medical profession’s own wasting disease—with particular specialists like pharmacists in very short supply, and an average vacancy rate of 24 percent across the medical spectrum.” The grounds for this exodus can be found in the current working conditions for members of the health professions. The monthly salary for a senior house officer working a 70- to 80-hour week, for example, is the equivalent of US$187, leading most to supplement their public-sector employment with private work. Many doctors report shortages of even basic drugs and medical supplies, such as needles and suture materials. Patients must pay out of pocket for some services, often forcing providers to withhold treatment until at least some level of payment has been provided. In addition to the demoralizing effects of working for so little money and with so few resources, there is the perceived threat of becoming infected oneself with HIV, as is believed to have happened to two doctors through needle-stick accidents at the university’s medical school. In an attempt to address medical staff shortages, the Ministry of Health recently ordered a two-fold increase in the number of medical students in training at the University of Zimbabwe. However, no corresponding increase was made in the size of the teaching staff. The situation in Zimbabwe is paralleled to varying degrees elsewhere on the continent. In other African nations, the USAID-sponsored report finds that:
As a result of these losses, many African countries are now actively trying to recruit health professionals through advertisements in foreign publications. This is a crisis that, at the very least, deserves further objective assessment so that the scope and urgency of local needs can be identified and addressed. |
on health care systems that are already severely underfunded; the brain drain is only worsening the problem.
Urban–Rural Imbalance
The well-known health care disparities between the “urban poor” and the “rural poorer” that exist throughout the developing world are pronounced in sub-Saharan Africa. These disparities are due in part to a within-country brain drain. Most doctors and nurses are trained to work in hospitals (as opposed to rural clinics) and often find urban areas much more desirable than rural. Urban settings provide physicians with greater camaraderie, increased chances for promotion, and better living conditions (e.g., schools, housing, technology) than are available in rural areas (USAID, 2003). Also, many physicians moonlight from their low-paying daytime jobs with more lucrative private-practice appointments with those patients who are able to pay. This type of work is often easier to find in more heavily populated urban areas (USAID, 2003). Finally, as discussed above, the AIDS pandemic further infiltrates societies, health care workers themselves are often infected, and prefer to remain close to urban hospitals for their own treatment.
According to data from Malawi, Zambia, and Zimbabwe, in the late 1990s there were 2 to 10 times more professional health workers in central and provincial hospitals than in rural health centers (USAID, 2003). According to the Ghana Ministry of Health, in 2000 there were nearly 11 times as many doctors and more than 12 times as many nurses working in Greater Accra than in the Upper Western Region, even though there are more than 5 times as many people living in the latter (Ghana Ministry of Health, 2000).
Addressing such dramatic imbalances will not be an easy task, as urban settings are generally much more profitable, both salarywise and professionally, for practitioners. According to a survey conducted among government-employed Portuguese-speaking African doctors, their median monthly salary is equivalent to what they would earn from just 7 hours of private practice (Ferrinho et al., 1998). Thus it is clear that ART scale-up programs targeting rural areas will need to allocate funds specifically to ensure the availability of the necessary health care personnel. The need for rural service programs and incentives for health care workers to relocate or remain in traditionally underserved rural areas needs to be further evaluated and appropriately addressed.
In the developed world, various incentive programs are employed to maintain physician presence in rural areas. Some state-funded U.S. medical schools offer significant financial relief in the form of tuition benefits in exchange for the student’s future service in a rural part of the state. The
National Health Service Corps, run by the U.S. Department of Health and Human Services (DHHS), has a similar program designed to place future physicians in underserved areas in exchange for tuition scholarships. Large-scale efforts in this regard have not yet been tried in Africa (USAID, 2003). Inevitably, such staff retention programs and incentives will be necessary if trained personnel capacity is to be expanded and sustained in developing countries, particularly in rural areas.
Laboratory Technicians
In addition to physicians, pharmacists, nurses, and other health care workers directly involved in care and treatment for HIV/AIDS patients, laboratory technicians are essential to the actual administration and monitoring of ARVs. For example, as noted above, Zambia has estimated that its initial ART scale-up program (for 10,000 patients) will require 32 FTE laboratory technicians in addition to an estimated 13 FTE doctors and nurses and 15 FTE pharmacists.
The important role of laboratory technicians in ART scale-up suggests the need for more of these personnel and improvements in their training. Compliance with good laboratory practices is critical. Generally, problems with inaccurate laboratory analyses fall into one of three categories: preanalytical (e.g., improper labeling, specimen mix-ups), analytical, and postanalytical (i.e., when a test is done correctly, but the results are recorded incorrectly). It is essential to identify and evaluate deficiencies in training programs for laboratory technicians whose correction would minimize these errors. Other factors that may be contributing to poor laboratory compliance, such as not having clear laboratory procedures in place, should also be addressed.
Private Versus Public Sector
In resource-constrained settings, many people who suspect that they have a sexually transmitted disease seek care in the private sector, including private medical practitioners, pharmacists, traditional providers, and drug vendors. This fact raises several concerns about the regulation of the behavior of private providers and the proper use of ARVs. The report of a recent study in Zimbabwe, for example, describes prescribing practices as “therapeutic anarchy” (Nyazema et al., 2000). Reflecting a system without suitable controls, physicians and private pharmacies were found to be prescribing mono therapy to many patients, and most of the interviewed patients believed that the drugs actually cured HIV infection. In another survey of Ugandan private medical facilities, only 4 of 17 facilities prescribing ARVs had received CD4 and viral load results in the previous 2 months (i.e., for
only 38 of 450 patients) (Brugha, 2003). Even when users recognize that public services may be superior, they often select private providers for the sake of privacy and as a way to avoid the stigma associated with seeking treatment for HIV infection.
To circumvent such improper use of ARVs, better controls need to be instituted. Strategies need to be developed for providing treatment guidelines for private-sector practitioners, establishing links between private practitioners and specialists, and increasing private-sector access to information and research evidence. National tuberculosis programs have faced similar problems, presenting a potential opportunity to learn from those experiences (Caminero, 2003). (On the other hand, it should be noted that at least one study has indicated that private-sector care and ARV prescribing practices are consistent with international standards [Macharia, 2002].)
General Health-Sector Training
Clearly, given the decreasing number of well-qualified and highly trained health workers in resource-constrained settings, there is a need for cost-effective training programs that better prepare graduates for working in the field and on the front line. Ironically, however, donor support has generally tended to be overly skewed toward training as opposed to staff retention and human resource system improvement, such that the already financially strapped national governments are often left with the burden of bearing recurrent costs, such as salaries. Moreover, donor-supported training programs generally are not very well coordinated, are focused too heavily on in-service training as opposed to much-needed preservice training, and do not address the underlying causes of poor staff morale. In Malawi, 10 percent of all donor expenditures in fiscal year 1997 were dedicated to training (amounting to US$4.5 million, including $2.2 million for out-of-country workshops, $1.5 million for out-of-country short- and long-term training, and $0.8 million for other training initiatives). Alternatively, if this amount had been devoted toward supplementing the meager salaries of the civil service health-sector workforce, it would have translated into a US$473 salary increase for 1 year for each of Malawi’s 9,500 health-sector civil servants (a roughly 50 percent raise over the typical salary)—a comparison that did not go unnoticed among these civil servants (USAID, 2003).
Although there have been few quantitative assessments of the relative cost-effectiveness and value of preservice versus in-service training programs, the focus on in-service training (e.g., conferences, workshops, site visits) is questionable despite providing short-term solutions:
-
In-service training diverts attention away from preservice training
-
programs that create new practitioners and from the urgent needs of those programs.
-
It tends to cover only a certain proportion of the workforce.
-
It is usually not sustainable after donor funding ends.
-
In-service workshops tend to be held in hotels rather than out in the field, and are not exam based.
-
These workshops can be disruptive as they require workers to leave their posts in the field (although it can also be argued that the workshops could, if conducted appropriately, improve morale and provide a much-needed break for overworked staff).
Box 5-4 describes the efforts of one country—Botswana—to build health-sector human resource capacity to address the HIV/AIDS epidemic.
Donor-sponsored training programs tend to be focused on specific disease interventions while neglecting the support skills and services needed for the effective implementation of those interventions. These skills and services include pharmacy and pharmaceutical management, health facility management, health planning and administration, human resource planning and systems, accounting and finance, and procurement and logistics—in short, all of the components of ART scale-up not directly related to actually administering the drugs. Finally, the development of new technologies requires the acquisition of new skills and new training, creating yet another burden for already overtaxed training programs.
Management Challenges
The need for more trained workers with the skills necessary for administering and monitoring ART is not the only manpower demand related to scale-up. The managerial and supervisory capacity of the health care sector in many resource-constrained settings is also seriously lacking and in urgent need of improvement. Qualitative reports have pointed to various personnel-related and systematic causal factors:
-
As is the case with medical and technical positions, the above-noted loss of workers due to either death from HIV/AIDS or migration to higher-paying jobs, coupled with the slow production of new workers to fill open and needed positions, has resulted in many medical, technical, and managerial positions remaining vacant.
-
Already scarce medical personnel from other sectors, including physicians, are often misused for management tasks.
-
Health care management tends to be highly centralized, with little or weak supervision, monitoring, or communication with local providers. Consequently, local needs often go unnoticed.
|
BOX 5-4 Much of the HIV/AIDS-related human resource capacity building in Botswana is done through the African Comprehensive HIV/AIDS Partnerships (ACHAP). ACHAP runs several training programs throughout the country at many levels of the HIV/AIDS health care workforce. Teacher Capacity-Building Program—developed by ACHAP, the United Nations Development Program (UNDP), the United Nations Population Fund (UNFPA), the Bostwana Ministry of Education, and Botswana Television. The program is designed to improve schoolteachers’ ability to facilitate stigma reduction and HIV/AIDS discussion among their students. National Behavior Change Interventions Training Program—developed by ACHAP and the National AIDS Coordinating Agency (NACA) to provide behavior modification intervention skills to government workers, civil servants, and district level employees. The program encompasses six training sessions per year over 3 years. HIV/AIDS Training Clinical Preceptorship Program—developed by ACHAP to bring international experts to Botswana to provide hands-on training to local health care providers. Participants spend at least 3 months in the program. KITSO AIDS Training Program, Harvard—developed by the Botswana Ministry of Health, the Harvard AIDS Institute, and the Botswana–Harvard AIDS Institute Partnership to train health care professionals in HIV/AIDS care and ART. The program uses both classroom and clinic-based instruction. Participants must complete the four core modules and one of three elective modules, at which point they are awarded a certificate from the Harvard School of Public Health’s Center for Continuing Professional Education. KITSO AIDS Training Program, Baylor—developed by ACHAP, Baylor College of Medicine, and the University of Botswana to further enhance the existing KITSO curriculum. This program is currently in the development stages and is expected to begin in July 2004. SOURCES: See http://www.achap.org/Programmes.htm; http://www.hsph.harvard.edu/hai/kitso/; http://bayloraids.org/africa/kitso.shtml. |
-
Problems of favoritism and a lack of clear expectations and performance appraisal contribute to the problem. According to one report, many African countries foster a “supervisory culture of control, instruction-giving, and fault-finding . . . rather than one of facilitation and understanding what is happening so that the problems can be addressed” (USAID, 2003:20).
-
Weak personnel information systems technology and capacity contribute to the problem by making it difficult to retrieve data on employed staff, including their location. Although lower-level facilities often have
-
more complete information, the data are not typically sent to or available at central management locations.
The fact that personnel data are so incomplete not only creates management challenges, but also severely constrains efforts to change or develop human resource policy in ways that will maximally benefit the health care infrastructure. The lack of such data is also one of the reasons for the paucity of quantitative data on and objective assessment of the current human resource crisis in general.
Sometimes, deficiencies in management (and technical) expertise are addressed by hiring outside consultants or providing donor-sponsored advisors (e.g., World Bank implementation units). Although this type of quick fix may be necessary to address immediate crises, it is not sustainable over the long term and often complicates problems of motivation and morale by engendering jealousy (e.g., consultant and advisor salaries are often much higher than those of local workers). The number of such outside advisors is not trivial. In Zambia in the mid-1990s, there were apparently as many donor-funded positions as senior positions on the government payroll.
The current general move toward decentralization of health services, a strategy embraced by many African countries, may help alleviate some of these management problems. However, it also raises other, at least equally important, issues regarding local capacity and the need to develop new structures (e.g., budgeting and reporting mechanisms, new relationships among central ministries).
Given the critically important role of logistics, communications, and information management systems in ART scale-up, moreover, having people in place who can operate and manage such systems is critical. Additionally, the capacity to conduct credible monitoring and evaluation programs (described later in this chapter) requires human resources not involved with the operational aspects of scale-up. The people collecting and analyzing the data should not be those who are administering treatment and managing programs. Thus there is a need to mobilize data analysts and others to support monitoring and evaluation and to address associated operations research issues. The nature and extent of these skills will vary among different settings.
ART scale-up will rely on expertise from outside the clinical health sector as much as from within. Identifying specific deficiencies and needs is difficult, as there are scarce data from which to draw evidence-based conclusions. It is clear, however, that expertise will be needed in all areas of ART scale-up, including physicians; nurses; clinical officers; pharmacists; counselors; laboratory technicians; management personnel; information technologists; procurement and distribution professionals; drug regulatory
experts; data analysts; and experts in monitoring, evaluation, and operations research.
Recommendation 5-4. Countries should establish information systems at the regional and national levels so they can regularly assess and coordinate their evolving human resource needs. Both countries with relatively adequate human resources and those that are more resourceconstrained must pursue appropriate policies and programs to stem the “brain drain” of local expertise that is critically needed for the scale-up of ART programs. The current shortage of trained, dedicated personnel for monitoring and evaluation programs should be rectified in conjunction with meeting other training and personnel needs.
SECURING AND DELIVERING EFFECTIVE DRUGS
Purchasing drugs is about more than the price of the pills. Continuous drug availability and the safe, timely distribution of quality-assured drugs to the people who need them will be critical to the viability of any ART program, as interruptions in the drug supply can rapidly lead to treatment failure and the emergence of drug resistance even in the most motivated patients who are otherwise receiving good care. In many resource-limited areas, the requisite infrastructure for the regular procurement, distribution, regulation, and safe storage of ARVs may not be functional. The numerous problems currently facing many resource-limited countries include weak procurement strategies; a lack of sufficient and appropriate warehouse space for stocking drugs; too few people and vehicles to deliver the drugs to their intended, often remote, destinations in a timely manner; and poor communication along the drug delivery line. Addressing each of these components and ensuring the safe delivery of quality ARVs and related products to a number of sites across different sectors and for a growing number of people presents a much more complex set of challenges than those faced by pilot projects. Even in such projects, reports abound regarding the complications associated with the safe procurement, storage, and delivery of products. A well-planned and -executed logistics system can help alleviate many of these problems.
Procurement
For a number of reasons, ARV procurement is more challenging than is the case for other types of essential medicines. Cost issues aside, stock management is crucial for maintaining uninterrupted drug supplies; procurement systems must be flexible enough to adapt to the rapidly changing and wide range of treatment regimens; and a lack of quality reference
standards makes it difficult to assess the quality of generic ARVs (Médecins sans Frontières et al., 2003).
The main findings of a report examining the 2-year purchasing experience of Médecins sans Frontières (MSF) in 10 countries reveal that procurement works best when there is a well-supported and well-funded national HIV/AIDS strategy that includes ART. Although MSF advocates no single or best strategy for procurement, their experience suggests that the easiest and most effective procurement strategies involve a strong public procurement agency (e.g., as in Cameroon), local drug production (e.g., as in Thailand), and/or dynamic private-sector distributors (e.g., as in Malawi) (Campaign for Access to Essential Medicines, 2004; see also Box 5-5).
|
BOX 5-5 The World Health Organization’s (WHO) AIDS Medicines and Diagnostic Service (AMDS), operational since December 2003, is the access and supply arm of the UNAIDS/WHO 3-by-5 campaign. The AMDS was created to expand the access of developing countries to quality drugs and diagnostic services. To this end, it offers the following support:
As of mid-2004, 20 countries were using the AMDS for procurement and/or distribution of drugs and diagnostics. The AMDS is inviting participation by nongovernmental organizations, foundations, and governments. SOURCE: WHO, 2003c. |
|
BOX 5-6
SOURCE: Margherio, 2004. |
The development and implementation of procurement strategies should be informed by the market status of the desired drugs (i.e., generic, limited-source, or single-source, with the latter two indicating some degree of market exclusivity or patent protection); the characteristics of the medicines and associated suppliers (i.e., quality assurance, susceptibility to resistance, required cold-chain and expiration issues, need to monitor side effects); and the supplier’s timetable for drug delivery to ensure a match with treatment initiation and maintenance schedules. Key factors to which the Clinton Foundation attributes its recent success in procurement are described in Box 5-6 (see also the discussion of the the foundation’s program in Chapter 2).
Commodity Security
Commodity security, which ensures the long-term, continuous, and reliable availability of essential commodities (drugs, diagnostics, laboratory supplies, etc.) to those who need them, will be critical to the long-term sustainability of ART scale-up. At the program level, the consistent and secure delivery of high-quality drugs depends on five key components, a breakdown in any one of which could cause the entire system to collapse (Chandani, 2004; World Bank, 2004):
-
The capacity to forecast programmatic needs
-
The capacity to finance product requirements and to effectively coordinate funding for the purchase of required commodities
-
The capacity to procure the products in a timely and efficient manner
-
The capacity to deliver the products to those who need them on a reliable basis
-
The availability of good logistics data and an information system (e.g., to enable accurate forecasting)
The ability to forecast is particularly problematic, as there is a paucity of data on which to base accurate forecasting, and most programs have very little experience to guide their initial forecasts. Many assumptions must be made regarding not just the estimated need for first-line-regimen drugs, but also drug substitutions that will be required because of toxicity, treatment failure, and other problems.
As programs expand, it will be vital for logistics data to be collected, appropriately analyzed, and routinely available for the updating of forecasts so as to minimize the use of assumptions and maximize the utility of ARV purchases. The physical security of the supply chain in terms of protecting commodities from pilferage is another area of vital concern. Again, there are several ways in which a well-functioning logistics system can minimize this problem. For example, guidelines can be developed for transparency in such areas as procurement, inventory management procedures, routine tracking of stock levels and use, the use of secure vehicles, and requirements for storage conditions. Although an in-depth discussion of corruption is beyond the scope of this report, there is some concern that the problem, already entrenched in so many institutions worldwide, may become exacerbated as the global AIDS response infuses such large amounts of money and resources into communities with large, unemployed, desperate populations. A well-functioning logistics system (see below) can detect discrepancies and identify when and where leakage occurs.
Logistics Systems
DELIVER defines logistics as “the set of activities that move products through the supply chain to the ultimate customer” (DELIVER, 2000, 2004). These activities include the following:
-
Ensuring that ARVs reach the people being targeted
-
Providing a buffer against uncertainties in funding and procurement
-
Ensuring an uninterrupted supply of products so as to guard against the emergence of resistance, enhance treatment outcomes, and maximize investments
-
Securing the supply chain to minimize wastage or leakage of drugs
-
Providing data on ARV use for donors and program and logistics managers
-
Managing and delivering the approximately 120 other commodities necessary for ARV treatment (e.g., laboratory reagents and supplies, HIV diagnostic test kits)
Box 5-7 describes lessons learned about logistics systems during efforts to improve the delivery of drugs for sexually transmitted infections (STIs) in Kenya.
The importance of logistics systems to a smoothly operating drug supply chain raises questions about what can be done to improve already existing systems in some countries. In developing or assessing logistics systems, short- and long-term demands must be appropriately balanced. Although developing multiple parallel or separate systems may not be a desirable long-term solution, an emergency response may require initially bypassing existing structures or systems (e.g., those without the capacity to assume more responsibility). At the same time, ways to integrate the new parallel system, or components of that system, should be considered so that within 5 to 10 years, multiple systems will no longer exist. Several steps can be taken to improve existing logistics systems (Attawell and Mundy, 2003; Chandani, 2004):
-
Streamline supply chains, particularly public-sector systems, which tend to have many levels of authority, so that the system is more responsive, opportunities for leakage are minimized, and costs are reduced.
-
Limit the number of logistics systems by establishing partnerships (i.e., public–private partnerships among different donors and national governments). The more systems are in place, the greater will be the overall cost and the extent of regulation required, and the less efficient will be the operation of the country’s overall drug supply.
|
BOX 5-7 Although not a “how-to” guide for logistics practitioners, DELIVER’s Programs That Deliver: Logistics’ Contribution to Better Health in Developing Countries is intended to serve as an overview for policy makers on all of the various components of a logistics system. While its focus is on family planning programs, the concepts, approaches, and lessons outlined provide a strategic framework that could readily be adapted to ART scale-up. The following example illustrates how improving just one aspect of a country’s logistics system can improve program outcomes. In 1995, Kenya received a US$600,000 donation of more than 2,500 sexually transmitted infection (STI) kits from the British Department for International Development. At that time, it was estimated that the kits could supply 163 sites for 1 year (i.e., all of Kenya’s hospitals and one-third of its health clinics). Meanwhile, also in 1995, the Family Planning Logistics Management Project, the predecessor to DELIVER, started providing technical assistance and software to Kenya for the tracking of customer symptoms and the number of STI drugs consumed by each customer. The resulting information was used to estimate when each site would need its next supply of drugs. Within 5 months of implementation, this new tracking system had produced enough information to permit redesign of the kits such that they, and the drugs they contained, could be redistributed. Instead of serving 163 sites for 12 months, the kits ended up serving 500 sites for 29 months for the same amount of money. Thus the same budget was used to serve three times as many people for twice the amount of time—all because of the implementation of a logistics management information system. (The cost of the logistics and additional clinical support was estimated to be 22 percent of the cost of the drugs themselves.) SOURCE: DELIVER, 2003. |
-
Invest in building logistics information systems that provide the necessary data for forecasting and long-term planning.
-
Develop flexible procurement mechanisms, such as framework contracts, so that countries are not stuck with unneeded products when uptake is low, while countries in need can readily obtain more products.
-
Consider logistics issues when selecting products. For example, the use of fixed-dose combinations (FDCs), blister packs, and cold-chain independent drugs will greatly enhance program implementation.
-
Consider the regionalization of logistics system and whether and how that strategy could strengthen country systems.
Information Systems
ART scale-up is a complex systems problem involving a multitude of interacting components, people, and sectors. Consequently, the vital but often overlooked role of data and information must not be underestimated. Data and information necessary for managing all aspects of ART scale-up will need to be standardized, compiled, and made easily accessible. Information systems will be essential to meet these needs.
Information systems comprise two main components. The first is information management, which encompasses data collection and analysis. The second is information technology, which includes the telecommunications network in the country in which the system is being implemented (e.g., telephones, fax service), Internet access technologies (varying, for example, between capital cities and remote locations), bandwidth, and service reliability. Also, at a more basic level, power supply availability and stability are critical; anecdotal reports about having all of the pieces in place but no power to run the system abound. Finally, the cost of information technology and cultural considerations (e.g., attitudes toward the use of technology) need to be addressed.
Brazil provides an excellent example of how a well-functioning information system can dramatically ease ART scale-up (see Box 5-8). A key component of scale-up in that country was a targeted effort to address and strengthen the country’s information management and information technology needs. There was an awareness that, in a country the size of Brazil, the logistical demands of ART scale-up would require the ready availability and usability of valuable, accurate information pertaining to all aspects of drug delivery—from procurement to patient adherence. Thus the demand was recognized for the creation and implementation of two computerized systems: SICLOM (Sistema de Controle Logistico de Medicamentos, or System of Logistical Control of ARV) (Viols et al., 2000), to register and track the distribution of ARVs; and SISCEL (Sistema de Controle de Exames Laboratoriais, or Systems for Control of Laboratory Exams) (Lima and Veloso, 2000), to track CD4 and viral load laboratory test results.
The design and implementation of appropriate information systems requires a thorough information technology site assessment beforehand. This effort must include obtaining any special licenses needed for uplinking and permission for using the Internet, forming strategic partnerships when possible, conducting on-site evaluations in person, verifying customer service satisfaction, and evaluating met and unmet financial needs.
Recommendation 5-5. To provide continuous, secure delivery of quality drugs, diagnostics, and other products, national and international program managers of antiretroviral scale-up efforts should ensure that
|
BOX 5-8 SICLOM: Sistema de Controle Logistico de Medicamentos In 1998, the National AIDS Programme in Brazil developed a computerized system to control drug logistics. This system allows for the registration of drug distribution, which helps authorities maintain stock information and track prescriptions. The drug dispensing unit has at least one computer and one attendant staff person to run SICLOM. By registering the distribution of ARVs, SICLOM helps maintain needed stocks at 486 AIDS drugs dispensing units (ADDUs) located throughout the country and assists in tracking prescriptions (Lima and Veloso, 2000; Veloso et al., 2000). The largest unit, in San Paulo, serves 7,000 enrolled people living with HIV/ AIDS. Some 285 ARV-dispensing units use SICLOM to track about 118,000 enrolled patients. The system tracks prescriptions issued to establish whether they fall within treatment guidelines established by the National AIDS Programme. At the end of each day, the prescription information from each drug dispensing unit is sent via modem, online connection, email, or CD-ROM to the office of the National AIDS Programme in Brasilia. At this main center, the data are synchronized, allowing analysis of problems or errors in drug prescriptions; a report indicating any problems or errors detected is generated. For example, from November 1999 to January 2000, SICLOM detected and rejected 9 percent of prescriptions as being outside the Brazilian guidelines for ART. If 5 percent of these rejected prescriptions had been filled as written, patients could have developed serious side effects. Not only do the data indicate correctable errors and thereby aid in reducing side effects or other complications that might have resulted from the incorrect or nonrecommended use of ARVs, but they are also used to indicate areas in which further training of health care providers is needed. SISCEL: Sistema de Controle de Exames Laboratoriais One year after instituting widespread and free access to ART, the Brazilian Ministry of Health established a network of public laboratories to monitor patients clinically. Patients could use these laboratories to receive CD4 and viral load testing free of charge. As of 2004, 94 of these public laboratories were in operation and had issued more than 500,000 test results. The data gathered from these laboratories are sent via online Internet connection or dial-up modem to the National AIDS Programme in Brasilia. Clinicians can access the database to review SISCEL-generated graphs of changes in CD4 and viral loads. SISCEL maintains Brazil’s guidelines for laboratory testing and also is integrated with SICLOM. SOURCES: Galvão, 2002; Lima, 2004. |
well-coordinated commodity and logistics systems are in place from the outset of program initiation. Technical leadership, governmental commitment, and institutional support are needed to ensure the secure delivery of quality drugs and supplies. Methods to avert the interruption of drug supplies include information systems to facilitate the projection of needs and track the distribution of available stocks. Such planning and investment should also account for the consequences of civil disruption or natural disasters, which would require adequate contingencies to avoid disruption to the supply and treatment systems.
Quality Assurance of Antiretroviral Drugs
The benefits of high levels of adherence to ARV regimens would be illusory if those drugs were not themselves efficacious, safe, and of consistent quality. The extension of these treatments to millions of persons in need over the next several years will involve a growing number of established and new manufacturers. Ongoing, rigorous quality assurance throughout the manufacturing and distribution chain is essential, especially as less experienced manufacturers enter the global market to produce ARVs. As more and more drug producers enter the market to produce ARVs at the lowest possible cost, the oversight system will need to be especially vigilant to ensure that cost savings are not routinely or intermittently sought at the expense of quality.
As noted in the World Bank’s 2004 technical guide on ARV procurement, an additional risk faced in dealing with commodities of significant market value such as ARVs is that of counterfeit products (World Bank, 2004). Counterfeit products may contain the wrong components or insufficient active ingredients, or may be contained in fake packaging. Temptations to divert very low-cost generic ARVs meant for use in resource-poor settings to more lucrative markets should be anticipated as a factor that could promote the downstream substitution of counterfeits and other forms of corruption. The World Bank guidelines emphasize that competent national authorities must have the capacity to enforce the laws and regulations designed to prevent fake or substandard medicines from reaching patients.
As noted by the World Bank, a systematic approach to procurement includes four elements: (1) prequalifying suppliers and products through evaluation of product dossiers and assessment of the use of good manufacturing practices; (2) well-crafted procurement contracts that detail supplier conditions, including technical specifications; (3) quality monitoring including laboratory testing; and (4) the installation of systems for continuous evaluation of supplier performance (World Bank, 2004).
The World Health Organization’s (WHO) Essential Drugs and Medi-
cines Policy Department embarked in 2001 on an important prequalification project to provide governments and pharmaceutical manufacturers with the first step toward establishing and maintaining mechanisms to ensure the quality, safety, efficacy, and rational use of pharmaceutical products (WHO, 2004a). The prequalification efforts have encompassed not only the assessment of pharmaceutical and diagnostics manufacturers, but also work on standards for procurement systems and quality assurance laboratories. Recognizing the extreme limitations of many resource-poor countries with respect to ensuring that their citizens obtain quality-assured pharmaceuticals and enjoy the advantages of consolidated and harmonized quality assessment procedures, WHO has laudably undertaken this prequalification endeavor. WHO does note, however, that its efforts are not a substitute for regulation by competent national authorities that need to address the remaining elements of procurement.
WHO does not regard inclusion on the prequalification list to be a warranty of the fitness of a product for treatment of HIV/AIDS with regard safety and/or efficacy. WHO also points out that its processes do not guarantee that “the products and manufacturing sites which have been found to meet the standards recommended by WHO, will continue to do so” (WHO, 2004a). In addition, WHO cautions that downstream issues such as the improper storage, handling, and transportation of drugs may affect their quality, efficacy, and safety (WHO, 2004a). For these reasons, national capacity building must be supported in parallel with the valuable first step taken by WHO.
As noted by WHO (2004a):
… the [prequalification] process began with a public invitation, to suppliers of pharmaceutical products, for their Expression of Interest (EOI). Evaluation of the product quality [has been] based on product data and information provided by the suppliers, followed by inspections of manufacturing sites. Guidelines on the contents of product data dossiers for quality assurance and on inspection of manufacturing sites are available from special section of EDM web site and WHO publications, which are in the public domain. Quality control analysis of selected samples of drugs was carried out.
Products meeting all quality criteria can be prequalified within 120 days of application. When suppliers and products fail to meet standards, WHO offers the opportunity to improve dossiers or compliance with Good Manufacturing Practices.
Reflecting on the first few years of the prequalification program, WHO (2004a) found that “it took a long time for many of the suppliers to submit product data to the specifications requested. Data on product quality and on bioequivalence were often inadequate and some manufacturing sites requested postponement of scheduled site inspections.” As the project has
progressed, however, “an improvement in the quality of product dossiers submitted by suppliers and a voluntary willingness to upgrade manufacturing sites have been observed. This may result in an improvement in the quality of HIV/AIDS drugs that are being traded in international commerce” (WHO, 2004a).
A challenge for ARV assessment is the fact that publicly available quality control and analytic methods or reference standards generally are not available for these often relatively new medicines. As a result, original methods developed and validated by the manufacturer are frequently used. A common basis for concluding that these in-house assay methods are valid is necessary across these manufacturers. Periodically, product dossiers and manufacturers must be reassessed, while changes in manufacturing methods or facilities require immediate review. Samples tested for qualification and regulatory purposes should be from actual production lots rather than pilot test lots. Periodic random representative sampling and quality control analysis of production lots, preferably downstream near the end user, are an essential supplement to impressions drawn from the prequalification of suppliers.
Beyond proper manufacture critical to appropriate care will be the construction of reliable distribution systems to ensure that drugs flow steadily and in sufficient quantity and that consistent quality is maintained until the point of use. Also essential to quality assurance are a country’s development of quality assurance laboratory resources and other regulatory mechanisms to guarantee quality across time and geographically dispersed distribution points, as well as the introduction of postmarketing surveillance programs. Some countries do not now possess the capacity to monitor ARV quality and need relevant training and other support. Box 5-9 describes one example of a strategy that can be employed by countries without established, reliable regulatory systems in place: the use of foreign procurement agencies.
FDCs raise some challenging quality assurance issues. While holding promise as means to simplify treatment regimens and improve patient adherence, FDCs add complexity to the quality assurance challenge because generic FDCs rarely can draw on experience with a fully evaluated, innovator-originated equivalent FDC product. At times, simultaneous use of the individual components has been characterized as safe and effective, but in other instances, the FDC represents combinations never before used together or used according to a novel dosing scheme. Moreover, an FDC might incorporate an entirely new molecule.
In recognition of the need for uniform principles to guide the formulation and evaluation of FDCs, WHO and DHHS have been developing guidelines or international standards to support FDC development. Reflecting the multidimensional complexity of the matter, WHO reports that
|
BOX 5-9 An option for countries lacking the regulatory systems necessary to provide quality assurance for ARVs is to rely, at least initially, on foreign procurement agencies. For example, an increasing number of countries are expressing interest in becoming involved with the Clinton Foundation’s strategic procurement partnership program (described in Chapter 2). An important component of the foundation’s procurement process is assuring good drug quality by prequalifying suppliers. To that end, the foundation focuses on manufacturers that meet drug quality criteria as defined by WHO and by the South African Medicines Control Council. The foundation also provides technical assistance through its country teams to ensure that drug distribution systems are secure and that inventory is properly maintained. It also reportedly is going to begin sample testing of shipped materials and is exploring the branding of the Clinton Foundation project so that drug leakage can be readily detected and addressed (Margherio, 2004). Despite the success of the Clinton Foundation’s procurement work thus far, as well as the initial value of WHO’s prequalification guidelines and other similar resources and options, the capacity of national regulatory agencies to conduct ongoing quality monitoring both at the point of entry and throughout the supply chain must be enhanced as ART programs expand—particularly if national governments are expected to eventually procure ARVs on their own. It is not well understood whether sufficient procedures are in place to ensure ongoing drug quality after initial qualification (through such methods as random specimen inspection) or to identify the emergence of drug-related adverse events or ineffectiveness that could result from drug combinations or interactions (postmarket surveillance). SOURCE: Margherio, 2004. |
“work is proceeding to resolve a few remaining clinical, public health, adherence, patent, production, regulation, and other issues” (WHO, 2004a).
The WHO- and DHHS-coordinated guidelines should encompass the need in specific circumstances for microbiologic and toxicologic studies of the proposed combinations. Rigorous assessment of bioequivalence of the FDC to the individual components is central to the acceptability of FDCs. As noted by the World Bank, therapeutic equivalence, as determined through in vivo bioequivalence studies, is especially important for FDCs given the seriousness of the condition being treated and the complex pharmacokinetic and physicochemical properties of these drug combinations. Of course, the drugs used in these studies must be essentially the same as those used in actual mass production for sale. Moreover, when simultaneous use of the individual components of FDCs is not standard, one must
consider not only the safety and efficacy of each component, but also the safety and efficacy of their simultaneous use and possible interactions—both favorable and unfavorable. The value of each component individually and in combined form must be clear. Inactive ingredients not present in single drugs may be a factor in the use of combinations as well.
Recommendation 5-6. The committee endorses as critical the use of the cheapest, safest, most effective high-quality antiretroviral drugs that can be procured. Fixed-dose combinations are recommended as most desirable if they are also of high quality, safe, effective, and inexpensive. The committee also strongly endorses a rigorous, standardized international mechanism to support national quality assurance programs for antiretroviral drugs. This mechanism should be timely, transparent, and independent of conflicts of interest; employ evidence-based standards; and provide ongoing assurance of consistent high-quality manufacture and handling. In particular, the pharmacological issues associated with fixed-dose combinations must be rigorously and rapidly addressed.
This Institute of Medicine (IOM) committee was asked to discuss the essential components and related general principles of a systematic framework to achieve a balance between the development of resistance and the need to scale up ART rapidly in resource-constrained settings. Yet it was not constituted with the particular technical expertise nor did it have the time to provide the sort of in-depth, independent, evidence-based examination necessary to critique or endorse specific drug quality assurance programs. Nevertheless, the committee commends the efforts of WHO, the U.S. government, and other international partners to facilitate and expedite the manufacture, procurement, distribution, and administration of consistently safe quality pharmaceuticals. Now that attempts to assure the quality of FDCs for AIDS treatment have highlighted the need for specific guidelines for particular component scenarios, publication of final expert consensus guidance is urgently needed. Organizations and governments working toward this goal should collaborate energetically and with the highest possible level of transparency to support each other’s efforts. The bottom line is that the approval process for ARVs must be swift while not compromising the quality and efficacy of the drugs.
MONITORING AND EVALUATION
Given the unprecedented magnitude of global ART scale-up and the paucity of data on how to provide ART safely and effectively in resourceconstrained settings, scale-up programs must be based on a learn-by-doing
approach as capacity is built and programs are continually reworked. The urgent need to deliver life-saving drugs to millions demands reliance on continuous monitoring and evaluation (M&E), rather than exhaustive up-front studies, to identify optimal outcomes and processes. One important function of M&E is to help ensure that programmatic goals are being met and, most important, that the greatest numbers of patients are being treated effectively to ensure that mortality and morbidity from HIV/AIDS are reduced. M&E also helps identify efficient, effective programmatic activities that warrant expansion and underperforming programs that should be either discontinued or improved.
Another important role for M&E is to ensure that funded ART programs are sensitive to ongoing country activities and are not negatively impacting HIV/AIDS prevention or other public health initiatives or programs. Not only does well-planned and well-executed M&E benefit programs in place, but a rigorous evaluation of the impact of initial ART efforts will be critical to the long-term sustainability of ART scale-up—particularly from a donor perspective, as there will be reluctance to continue funding programs that are not cost-effective or otherwise successful. This point is especially important in light of the long-term commitment required for ART scale-up.
What exactly is M&E? As defined in the National AIDS Council’s manual for use by practitioners in the design and implementation of M&E programs (National AIDS Council, 2002:3):
Monitoring is the routine, daily assessment of ongoing activities and progress. In contrast, evaluation is the episodic assessment of overall achievements. Monitoring looks at what is being done, whereas evaluation examines what has been achieved or what impact has been made.
With regard to examining health outcomes and impacts for both patients and services, M&E can be used to address any of a number of questions, depending on the specific goals of a program or intervention, as well as the needs and interests of the organization or authority requesting the information. For example:
-
What is the impact of ART on the health of patients treated? This question is addressed using such indicators as weight gain, functional status, incidence of opportunistic infections, mortality, and CD4 and viral load measurements (when available).
-
What is the impact of ART in reducing the age-specific HIV-related mortality rate, the mother-to-child transmission rate, and the age-specific prevalence of HIV infection?
-
What is the impact of ART on the ability to return to work?
-
What is the impact on both individual and societal productivity?
-
What is the impact on health care utilization (e.g., hospitalizations, clinic visits)?
-
What is the impact on prophylaxis for opportunistic infections?
Given that ART scale-up is only just beginning, it is difficult to find examples of how M&E could be used by treatment programs in resourceconstrained settings to identify practices that are working versus those that need to be improved. Countries’ efforts to evaluate their national AIDS programs have varied. Some experts have expressed concern that M&E for existing programs has generally been highly inadequate, and that programs in the process of being rolled out have no formal M&E mechanisms in place and insufficient staffing for evaluating programmatic impact. This situation may be due in part to the fact that until recently, the conceptual framework for M&E was not very solid, and there have been few M&E tools available for countries to use.
Recommendation 5-7. Monitoring and evaluation processes should be put in place by program managers at all levels at the start of scale-up initiatives. A fixed percentage (approximately 5–10 percent) of ART program funding should be budgeted strictly for monitoring and evaluation (exclusive of support for hypothesis-driven operations research).
Recommendation 5-8. Program managers should measure the effectiveness of HIV prevention and treatment efforts by means of scientifically valid and systematically conducted surveys of HIV prevalence and incidence, HIV morbidity and mortality, and risk behaviors. ART programs should be designed to improve the quality of life and add many years of productivity for as many people as possible. The success of ART scale-up should be evaluated on the basis of the extent to which these specific goals are achieved.
Monitoring and Evaluation Challenges
As described earlier in this chapter, the lack of trained health care and ancillary personnel is one of the greatest challenges to successful ART scale-up. In this regard, the dearth of M&E expertise is not an exception. Such expertise is not widely or uniformly available, and training at the outset of scale-up programs will be necessary to ensure that efforts and investments in M&E foster the expected returns.
Clearly, the reduction of AIDS-related morbidity and mortality is the most important outcome of ART programs, and the measure of this outcome is the most obvious indicator of program success. However, there are other important components of ART scale-up that require similar levels of M&E and financing, such as measurement of the cost-effective impact of
certain projects, efforts, or decisions); issues related to commodities (e.g., how decisions impact the availability of certain commodities); the provision of services and coverage; the quality of service delivery; operations research (e.g., how scale-up impacts operations research, whether enough funds have been directed toward such research, how results of the research are being fed back into systems); behavioral components (e.g., adherence); biological and epidemiological components (e.g., prevalence, incidence); and policy. Much of the data needed to monitor these components of scale-up are generally not available or of poor quality in most settings. Where they are generated, few such data are actually used by program managers.
Related to these concerns is the current lack of effective mechanisms to rapidly apply the lessons learned from M&E to improve the quality of care and the effectiveness of clinical and procedural management and training programs within scale-up efforts. Information platforms that can be used to identify initial data and information needs, along with methods for effectively assessing and implementing improvements, have not been widely incorporated into developing-country settings. One such method that might be considered is the Breakthrough Series system for learning and improvement developed by the Institute for Healthcare Improvement (IHI) (2003)—a collaborative learning model that incorporates multiple sites (e.g., regional hospitals, primary health care centers, rural clinics) in the study, testing, and implementation of best-practice knowledge to produce rapid improvement in health care delivery or management systems. As noted earlier, effective ART scale-up in resource-constrained settings will have to rely heavily on a learning-by-doing approach. These programs must also ensure that they “do what they learn” (Massoud, 2004). (See Box 5-10 for further information on the IHI model.)
To address multiple challenges, M&E information systems should (Delay, 2004):
-
Complement existing information systems.
-
Utilize simplified, harmonized, and prioritized data and data collection techniques.
-
Contribute to the improvement of patient management (in addition to providing useful information to the donor).
-
Build local capacity and incentives to collect, interpret, and disseminate the data in an appropriate form.
-
Support a culture of strategic information sharing (e.g., with respect to translating knowledge).
-
Protect the confidentiality of all health information.
-
Maintain individual patient records using unique patient identifiers.
-
Involve people living with HIV/AIDS.
|
BOX 5-10 IHI’s Model for Improvement requires collaborative teams to ask three fundamental questions: (1) What are we trying to accomplish? (Aim), (2) How will we know that a change is an improvement? (Measures), (3) What changes can we make that will result in improvement? (Changes) (Langley et al., 1996; WHO, 2004b). By addressing these questions, teams establish which specific outcomes they are trying to effect, identify appropriate measures to track their success, and determine key changes they will implement for testing (Plan). Key changes are then tested in a cyclical fashion that recognizes cultural and organizational characteristics. Change is implemented, and progress, problems, and unanticipated outcomes are documented (Do). The collaborative site teams complete data analysis and comparison of outcomes and initial objectives (Study). (See the figure below.) 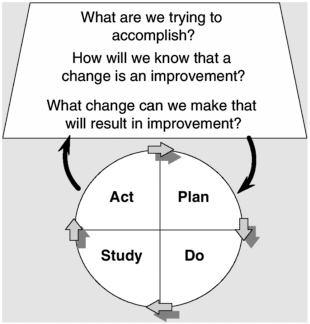 SOURCE: WHO, 2004b. |
-
Collect information from all providers of ART, including public, private, NGO, workplace, and other sites.
-
Ensure that the data gathering and analysis methodologies used are flexible, adaptable, and acceptable.
It is essential to select good indicators for use in M&E—data that are
|
Decisions are then made regarding how to implement and refine successful changes and abandon unsuccessful efforts (Act). Critical to this collaborative improvement approach is that participating health care teams contribute to adapting the new approaches for care. Real-time interactive operations research is designed to capture local knowledge and experience by making health care teams active partners in the refinement and improvement of care process. (See the figure below.) 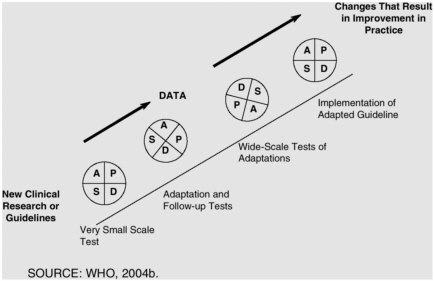 SOURCE: WHO, 2004b. |
relevant, easy to collect, and easy to interpret and that reflect changes that are easy to track over time and can be quantified. Measures should reflect both quantitative and qualitative aspects of programmatic management and patient-level quality of care. A number of core ART evaluation indicators have been identified that, if measured every year or two, would probably be sufficient for donor-related evaluation purposes (see Box 5-11).
That having been said, depending on the specific scale-up objectives, even these core indicators may not be sufficient for all donors. The fact that different donors may have differing objectives, and thus differing M&E requirements, raises important concerns about the impact of the resulting lack of standardized metrics and harmonization of M&E procedures. The more donors have a presence in a country, the higher will be the potential transaction costs involved with M&E and the higher the burden on resource-strapped host country programs.
WHO’s Health Metrics Network, supported by the Gates Foundation, was developed in recognition of the fact that most developing countries are overwhelmed by reporting requirements. For example, the Tanzanian Ministry of Health once filed 5,000 pages of reports, including different sets of measurements for different donors in the same areas. WHO was asked by donors to serve as a secretariat and develop a single set of measurements such that satisfying the criteria of the Health Metrics Network would meet the requirements of multiple organizations (Kim, 2004) (see Box 5-12 for some recommended M&E outcome indicators).
The standardization and harmonization of foreign-donor M&E efforts is only one of several political challenges to collecting, analyzing, and interpreting accurate data and unbiased results:
-
Because of widespread denial of the severity of the HIV/AIDS pandemic, data may be suppressed.
-
The needs of funding agencies often conflict with those of program managers (e.g., the former may be interested in outcomes to which the latter does not give priority or vice versa).
-
Collecting data on marginalized or illegal populations is difficult.
-
There may be resistance to tracking resources, as doing so may expose corruption and inequitable distribution.
-
Service delivery statistics are often perceived by staff as punitive.
-
The selective use of evaluation data may skew M&E efforts and bias analyses.
-
Performance-based disbursement policies can have a dramatic effect on data collection, analysis, and accuracy.
Another important challenge to M&E of ART scale-up will be monitoring long-term sustainability and impact. Tracking resources, including the cost per unit service and cost per commodity, will become more difficult as the number of people being treated increases. The same is true for tracking and monitoring staffing patterns (whether human resource capacity is really increasing, or ART scale-up is diverting staff from malaria control, childhood immunization, and other programs). Measures of logistics capacity, overall public health capacity, ARV resistance patterns, sur-
|
BOX 5-11 Community Level
ART Site Level
District/Region Level
Central/National Level
SOURCE: Delay, 2004. |
vival patterns, infection incidence, and economic productivity (i.e., whether the economic impact of HIV/AIDS is really changing over time) will also pose increasing challenges. Assuming that incidence is cut by half to 2.5 million cases per year and assuming that the goal will continue to be to treat only half of all clinically eligible HIV-infected individuals, the target will be
|
BOX 5-12
|
to treat 6 to 9 million people by 2010. A global program of that magnitude will require extraordinary M&E efforts.
Finally, programs should be monitored at optimum frequency, which may differ for different types of interventions. And a mechanism for regular international communication of M&E results, inspired by the regular international rounds conducted during the SARS crisis, needs to be established. Box 5-13 summarizes some important features of M&E for ART scale-up.
Measuring Success
What defines programmatic success for ART? The number of drugs distributed is not the best measure, as the numerous problems elucidated earlier attest. There are too many things that can go wrong during the drug
|
BOX 5-13
|
delivery process and far too few management information systems in place to track drug delivery in a way that would provide meaningful information on the number of drugs distributed. Nor is measuring the number of people treated necessarily the best way to monitor progress, as both the individual clinical benefit (reduced toxicity and mortality) and population-level benefit (decreased morbidity and mortality) of therapy depend on adherence and the success of chosen adherence interventions.
A definition of treatment success needs to be formulated, with an awareness that it will likely change over time. It must also be realized that success can be defined from several different vantage points, including the patient, physician, community health system, nation, and donor agency.
What many U.S. clinicians considered successful a decade ago would not be considered successful today. Just 6 years ago, success was declared if 50 percent of ARV-treated patients showed complete viral suppression at the end of the first year or 18 months of treatment. Now, clinicians strive for 85 or 90 or even 95 percent as a sign of success. It is critical for ART scale-up programs in resource-constrained settings to strive for a very high—for example, 90 percent—success rate for initial regimens and that treatment regimens and care delivery systems be planned accordingly. Some experts argue that it is not fair to set the bar higher than it has been set in the United States or other resource-rich countries. If this is not done, however, the long-term sustainability of donor support in combination with the durability of inexpensive drug regimens will be at serious risk. Most resource-constrained countries simply cannot afford the flexibility in treatment regimen—in terms of both drug cost and the necessary expertise and
human resource capacity—required to individualize treatment when complications arise, as can the United States and other resource-rich countries (Redfield, 2004).
Within 10 years, ART scale-up will have evolved into a US$30–100 billion annual effort, demanding an enormous amount of program success to meet donor goals. In the rush to achieve a quick fix, initial expectations should not be set too low such that they compromise the long-term sustainability of ART scale-up. At the same time, there can be no delay in responding to the ethical imperative to act now.
Recommendation 5-9. Monitoring and evaluation measures and requirements, as directed by various donors and other stakeholders, should be harmonized across programs to minimize time-consuming inefficiencies in data collection and program management. Additional efficiencies would be achieved if these efforts were coordinated by a single national ministry or agency. Donors should avoid attempting to ascribe results solely to individual funding sources in order to minimize the in-country confusion and inefficiency created by mandates to conduct multiple, uncoordinated monitoring and evaluation efforts in the midst of rapid scale-up.
REFERENCES
Attawell K, Mundy J. 2003. Provision of Antiretroviral Therapy in Resource-Limited Settings: A Review of Experience up to August 2003. London: DFID Health Systems Resource Centre.
Brugha R. 2003. Antiretroviral treatment in developing countries: The peril of neglecting private providers. British Medical Journal 326:1382–1384.
Bundred P, Levitt C. 2000. Medical migration: Who are the real losers? Lancet 356:245–246.
Caminero JA. 2003. Is the DOTS strategy sufficient to achieve tuberculosis control in low-and middle-income countries? 2. Need for interventions among private physicians, medical specialists and scientific societies. International Journal of Tuberculosis and Lung Disease 7(7):623–630.
Campaign for Access to Essential Medicines. 2004. Surmounting Challenges: Procurement of Antiretroviral Medicines in Low- and Middle-Income Countries. [Online]. Available: http://www.accessmed-msf.org/prod/publications.asp?scntid=201120031530452&contenttype=PARA& [accessed January 5, 2004].
Chandani Y. 2004 (January 28). Distribution of ARVs: Issues of Security, Logistics, and Quality. Paper presented at the Institute of Medicine Workshop on Antiretroviral Scale-up in Resource Constrained Settings, Washington, DC. Institute of Medicine Committee on Antiretroviral Drug Use in Resource-Constrained Settings.
de Castella T. 2003. Health workers struggle to provide care in Zimbabwe. Lancet 362(9377): 46–47.
Delay P. 2004 (January 28). Monitoring and Evaluation for ARV Programs in Resource Poor Settings. Paper presented at the Institute of Medicine Workshop on Antiretroviral Scale-up in Resource Constrained Settings, Washington, DC. Institute of Medicine Committee on Antiretroviral Drug Use in Resource-Constrained Settings.
DELIVER. 2000. Programs that Deliver: Logistics’ Contribution to Better Health in Developing Countries. [Online]. Available: http://www/fplm.jsi.com/2002/Pubs/Pubs_Policy/Programs_That_Deliver/TOC/index.cfm [accessed August 30, 2004].
DELIVER. 2003. In Kenya, Logistics Project Helps to Extend the Coverage of STI Drugs. [Online]. Available: http://www.deliver.jsi.com/2002/PUBS/pubs_success/ontrack_archives/index.cfm [accessed February 22, 2004].
DELIVER. 2004. DELIVER Homepage. [Online]. Available: http://www.deliver.jsi.com [accessed February 22, 2004].
Dovlo D. 2003 (September 23–25). The Brain Drain and Retention of Health Professionals in Africa. Case study prepared for a regional training conference on Improving Tertiary Education in Sub-Saharan Africa: Things That Work, Accra.
Ferrinho P, Van Lerberghe W, Julien MR, Fresta E, Gomes A, Dias F, Goncalves A, Backstrom B. 1998. How and why public sector doctors engage in private practice in Portuguese-speaking African countries. Health Policy and Planning 13:322–338.
Galvão J. 2002. Access to antiretroviral drugs in Brazil. Lancet 360(9348):1862–1865
Ghana Ministry of Health. 2000. Consolidating the Gains, Managing the Challenges: 1999 Health Sector Review. Ghana: Ghana Ministry of Health.
Institute for Healthcare Improvement. 2003. The Breakthrough Series: IHI’s Collaborative Model for Achieving Breakthrough Improvement (Innovation Paper). Boston, MA: Institute for Healthcare Improvement.
International Training and Education Center on HIV. 2003. [Online]. Available: http://ww.gotditech.org [accessed August 30, 2004].
Katerere DR, Matowe L. 2003. Effect of pharmacist emigration on pharmaceutical services in southern Africa. American Journal of Health-System Pharmacy 60:1169–1170.
Kim J. 2004. The Challenge of HIV in 2004 and the UNAIDS/WHO “3 by 5” Program. Paper presented at the Institute of Medicine Workshop on Antiretroviral Scale-up in Resource Constrained Settings, Washington, DC. Institute of Medicine Committee on Antiretroviral Drug Use in Resource-Constrained Settings.
Kober K, Van Damme W. 2004. Scaling up access to antiretroviral treatment in southern Africa: Who will do the job? Lancet 364:103–107.
Kombe G, Smith O. 2003. The Costs of Anti-Retroviral Treatment in Zambia, Technical Report No. 029. The Partners for Health Reformplus Project, Abt Associates Inc.
Langley G, Nolan K, Nolan T, Norman C, Provost L. 1996. The Improvement Guide: A Practical Approach to Enhancing Organizational Performance. San Francisco, CA: Jossey-Bass Publishers.
Liese B, Blanchet N, Dussault G. 2003. The Human Resource Crisis in Health Services in SubSaharan Africa. Washington, DC: World Bank.
Lima R. Information Management and Technology Considerations for ARV Programs in Resource-Constrained Settings. Paper presented at the Institute of Medicine Workshop on Antiretroviral Scale-Up in Resource Constrained Settings. Washington, DC. Institute of Medicine Committee on Antiretroviral Drug Use in Resource-Constrained Settings.
Lima RM, Veloso V. 2000. SICLOM: Fistruicao informatizada de medicamentos para HIV/ AIDS. Acao Anti-AIDS 43:6–7.
Lynch E, Diallo I. 2001. Donor Mapping. USAID. [Online]. Available: http://mali.viky.net/usaid/mes_photos/donor_mapping_part3.doc [accessed August 30, 2004].
Macharia D. 2002. Antiretroviral Chemotherapy in Resource Limited Settings: A Review of ARV Therapy in the Private Sector in Nairobi, Kenya. Paper presented at the 9th Conference on Retroviruses and Opportunistic Infections in Seattle, WA. [Online]. Available: http://www.retroconference.org/2002/Abstract/13602.htm [accessed August 30, 2004].
Margherio L. 2004. Perspectives on Purchasing First and Second Line ARVs. Paper presented at the Institute of Medicine Workshop on Antiretroviral Scale-up in Resource Constrained Settings, Washington, DC. Institute of Medicine Committee on Antiretroviral Drug Use in Resource-Constrained Settings.
Massoud R. 2004. Principles of Design and Scale-up for National Clinical Care Programs and Applications to the WHO 3×5 Targets. Paper presented at the Institute of Medicine Workshop on Antiretroviral Scale-up in Resource Constrained Settings, Washington, DC. Institute of Medicine Committee on Antiretroviral Drug Use in Resource-Constrained Settings.
Médecins sans Frontières, World Health Organization, and UNAIDS. 2003. Surmounting Challenges: Procurement of Antiretroviral Medicines in Low- and Middle-Income Countries. The Experience of Médecins sans Frontières. Geneva: Médecins sans Frontières.
Narasimhan V, Brown H, Pablos-Mendez A, Adams O, Dussault G, Elzinga G, Nordstrom A, Habte D, Jacobs M, Solimano G, Sewankambo N, Wilbulpolprasert S, Evans T, Chen L. 2004. Responding to the global human resources crisis. Lancet 363(9419):1469–1472.
National AIDS Councils. 2002. Monitoring and Evaluation Operations Manual. Geneva: UNAIDS.
Nyazema NZ, Khoza S, Landman I, Sibanda E, Gael K. 2000. Antiretroviral (ARV) drug utilisation in Harare. Central African Journal of Medicine 46:89–93.
Over M. 2004 (January 28). An Overview of Health Care Manpower, Health Care Infrastructure and Economics in Select Resource-Poor Countries. Paper presented at the Institute of Medicine Workshop on Antiretroviral Scale-up in Resource Constrained Settings, Washington, DC. Institute of Medicine Committee on Antiretroviral Drug Use in Resource-Constrained Settings.
Padarath A, Chamberlain C, McCoy D, Ntuli A, Rowson M, Loewenson R. 2003. Health Personnel in Southern Africa: Confronting Maldistribution and Brain Drain. Equinet Discussion Paper #3. Regional Network for Equity in Health in Southern Africa.
Pang T, Lansang MA, Haines, A. 2002. Brain drain and health professionals. British Medical Journal 324(7336):499–500.
Puku N. 2002. Poverty, debt, and Africa’s HIV/AIDS crisis. International Affairs 78(3):531–546.
Redfield R. 2004 (January 27). Durability of ARV Therapy: US Experience and its Implications for Resource-Constrained Settings. Paper presented at the Institute of Medicine Workshop on Antiretroviral Scale-up in Resource Constrained Settings, Washington, DC. Institute of Medicine Committee on Antiretroviral Drug Use in Resource-Constrained Settings.
Schwab P. 2001. Africa: A Continent Self-Destructs. New York: Palgrave, Macmillan.
Tawfik L, Kinoti S. 2001. The Impact of HIV/AIDS on the Health Sector in Sub-Saharan Africa: The Issue of Human Resources. Washington, DC: USAID.
USAID (U.S. Agency for International Development). 2003. The Health Sector Human Resource Crisis in Africa: An Issues Paper. Washington, DC: USAID.
Veloso V, Sudo E, Lima RM et al. 2000. Promoting the Rational Use of Antiretrovirals through a Computer Aided System for the Logistical Control of AIDS Medications in Brazil. Paper presented at the 13th International AIDS Conference in Durban, South Africa.
Viols V et al. 2000. Promoting the rational use of antiretrovirals through a computer aided system for the logistical control of AIDS medications in Brazil. Presentation at the 13th International AIDS Conference in Durban, South Africa.
WHO (World Health Organization). 2004a. World Health Organization Prequalification Project . [Online]. Available: http://mednet3.who.int/prequal/ [accessed August 2, 2004].
WHO. 2004b. An Approach to Scaling Up: Using HIV/AIDS Care as an Example. Draft Document.
WHO. 2004c. 3 by 5 Technical Brief: AIDS Medicines and Diagnostic Service (AMDS). [Online]. Available: http://www.who.int/3by5/publications/briefs/amds/en/ [accessed August 24, 2004].
World Bank. 2004. HIV/AIDS Medicines and Related Supplies: Contemporary Context and Procurement. Technical Guide. Washington, DC: World Bank.










































