Appendix F
Conference Prework and Sample Matrices
The following letter and accompanying matrices were sent to the community participants in advance of the summit.
Dear Community Participant:
As a participating community at the Institute of Medicine’s Quality Chasm Summit on January 6-7, 2004, you will be actively involved in developing high-level work plans (including metrics) to redesign care in one of the following five clinical areas: asthma, depression, diabetes, chronic heart failure, and pain control in advanced cancer. Prior to the Summit, as shared with you in your invitation letter, your group will need to complete some preparatory work so that the condition-specific working groups can be as productive as possible. We will make every effort to facilitate this process in a manner that is sensitive to your time constraints. Your commitment will be as follows:
-
Participation by at least one member of your community team in a conference call to receive guidance in completion of pre-work materials.
-
Completion of two matrices to assess gaps in care and barriers/opportunities for improvement.
-
Follow-up conference call with committee content experts to agree upon assumptions derived from the data that will help inform the Summit work plans.
The IOM Next Steps Summit is intended to support communities of care providers in “Crossing the Chasm” to delivering high-quality care in one or more of the aforementioned five priority areas. This document lays the foundation for the condition-specific working groups. By investing in a modest amount of preparatory work, the participants should be able to maximize their time at the conference so that unique and valuable insights into how best to improve care within each community can be learned and deployed.
The first step towards optimizing the quality of care for the five conditions being targeted is to visualize the process of ideal care and to understand potential impediments to delivering that care. Figure 1 below represents the cycle of “ideal” care.
Using chronic heart failure as an example, the initial step is to recognize that the patient suffers from the syndrome of heart failure and to make a proper diagnosis. These diagnostic steps are outlined in the first column of the attached grids and include an assessment of left ventricular function, the use of laboratory tests to exclude other etiologies for these symptoms, and the exclusion of significant ischemic coronary disease. The next step of the care process is to educate patients about the nature of heart failure and what to expect regarding treatment (including lifestyle interventions) and prognosis. The third phase of care is to recommend initial treatment. Current standards of care for patients with left ventricular dysfunction include the use of angiotensin converting enzyme inhibitors, beta-blockers and anti-coagulation for those with atrial fibrillation. Ensuring that treatment recommendations are followed is the next step along the path of ideal care and includes teaching patients techniques of self-management such as monitoring weight and medication compliance. Finally, serial assessments of patients’ responses to treatment and monitoring the status of their heart failure are needed to continually optimize the other aspects of their heart failure care. This can be done through the serial assessment of patients’ symptoms, function and quality of life. Sub-optimal health status (symptoms, function and quality of life) should trigger a repeated pursuit, using the same steps outlined above, of opportunities to improve the patient’s condition. Naturally, it should be emphasized that this pursuit is one of shared management.
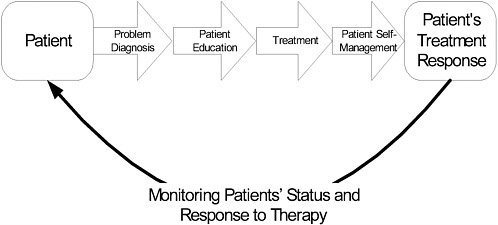
Figure F-1. Cycle of “Ideal” Care
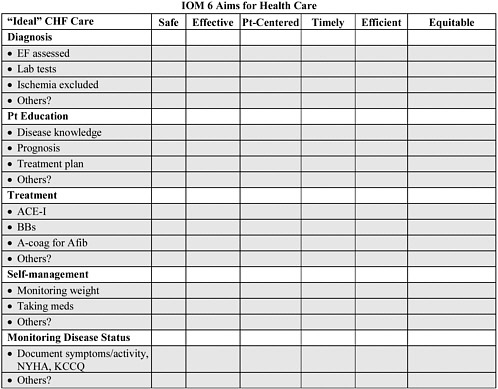
Rendering optimal care for patients with chronic conditions requires the efficient coordination of multiple components of the health care system and its environment. Towards that end, the Next Steps Summit is designed to identify those aspects of care that are most rate limiting in achieving a system that is safe, effective, patient-centered, timely, efficient and equitable. To identify the most pressing components of care for emphasis during the summit, we have designed the first of the attached worksheets. This matrix aligns each component of the process of “ideal” care against the six aims of high-quality healthcare described in the IOM’s Crossing the Quality Chasm. Please rank each process of care from 1-5, where a score of 5 indicates complete satisfaction of the goal and lower scores represent an increasing gap between current and ideal care. We will use these scores to identify the areas most in need of improvement.
The second matrix is designed to illuminate strategies currently being implemented at your institution to support high-quality care in each of these aspects of the desired “ideal” care process. We intend to share strategies from communities successful in certain aspects of care delivery with those struggling in those areas. Conversely, we hope to identify areas where all are suffering and to brainstorm solutions, through the use of national experts, for how to overcome these challenges. Your thoughtful and detailed completion of these grids is very much appreciated and the best possible investment that you could make in ensuring a successful conference in January. Thank you again for your participation and commitment to this process.
Sincerely,
John Spertus, M.D., M.P.H.
Chair, Community Pre-work Subgroup Quality Chasm Summit
MATRIX # 1 CHRONIC HEART FAILURE
Please list each of the components of ideal chronic heart failure care below and rate on a scale of 1-5 (where 5 means that the aim is completely satisfied and 1 represents an enormous gap) how well each component is performing in your community* in attaining each of the IOM 6 Aims for healthcare. We have provided examples under each heading. You may enter not applicable “N/A” where appropriate.
Institute of Medicine Aims for the 21st-Century Health Care System
Health care should be:
-
Safe—avoiding injuries to patients from the care that is intended to help them.
-
Effective—providing services based on scientific knowledge to all who could benefit and refraining from providing services to those not likely to benefit (avoiding underuse and overuse, respectively).
-
Patient-centered—providing care that is respectful of and responsive to individual patient preferences, needs, and values and ensuring that patient values guide all clinical decisions.
-
Timely—reducing waits and sometimes harmful delays for both those who receive and those who give care.
-
Efficient—avoiding waste, including waste of equipment, supplies, ideas, and energy.
-
Equitable—providing care that does not vary in quality because of personal characteristics such as gender, ethnicity, geographic location, and socioeconomic status.
MATRIX # 2 Strategies for Achieving High-Quality CHF Care
This grid is to illustrate how improving CHF outcomes relates to five areas in need of “System Improvement.” We have purposefully written it as a series of questions to help in defining various system interventions. For many, there is no single “right answer.” Rather, these are suggestions your community** should use to guide your responses to the worksheet accompanying this grid.
|
“Ideal” care |
Examples |
Clinical Information Systems |
Delivery System Redesign |
Decision Support |
Self-management Support |
Community Resources and Policies |
|
Diagnosis |
|
Does your community have a database to identify patients with heart failure? Does your community have a mechanism for enrolling heart failure patients into a database so that the processes and results of their care can be measured? How do you track test results? |
Who reviews the registry to insure complete workup? How does an efficient work-up, convenient to patients occur? |
Does your community have an evidence-based guideline for heart failure diagnosis? How is the guideline disseminated to providers? How is the guideline “embedded” into your system? How are recommendations for further care (Patient education, treatment, self-management, monitoring) facilitated? For Group A patients, at risk for but without HF, how are primary prevention practices supported? |
How is the import of a complete work-up communicated to patients? |
What links does your community have set up to provide information for patients about heart failure diagnoses? |
|
Patient Education |
|
How is it known whether patients have an adequate understanding of HF, its treatment and their prognosis? |
Are ‘education clinics’ available to provide this information? Are patient groups so that newly diagnosed patients can learn form other patients available? |
What tools are available to allow patients to select among different therapies and treatment environments? What process is in place to facilitate patient decisions about living wills and end of life care? |
Is there support for patients to create living wills? How are lifestyle changes (smoking cessation, exercise programs, etc.) supported? |
What links does your community have set up to provide information for patients about treatment? |
Adapted w/ permission from Ed Wagner, MacColl Institute for Health Care Innovation at Group Health Cooperative
|
“Ideal” care |
Examples |
Clinical Information Systems |
Delivery System Redesign |
Decision Support |
Self-management Support |
Community Resources and Policies |
|
Treatment for systolic left ventricular dysfunction (i.e. EF < 40-45%, moderate LV dysfunction or worse by qualitative assessment) |
|
How does your community track general measures, such as diet, physical activity, and immunizations? How does your community monitor the initiation and titration of needed medications? How are contraindications for certain medicines identified? How are medication dosages and medication changes tracked? |
Who reviews the registry for these general aspects of care? Are titration clinics available to adjust and monitor medications? Who provides patients with the means to monitor and follow treatment plans at home? |
Does your community have an evidence-based guideline for general measures in heart failure management, such as sodium restriction, fluid intake, physical activity, immunizations and avoidance of NSAIDs? Do guidelines describe optimal doses of ACE inhibitors (ex: captopril 150 mg/d, enalapril 20 mg/d or equivalent) and substitutes for ACE inhibitors? Beta blockers? Anti-coagulation? Do guidelines address the role of diuretics in maintaining euvolemia and minimizing symptoms? Do guidelines address the use of digoxin? How is the guideline disseminated to providers? How is the guideline “embedded” into your community system? |
Do you have documentation of collaborative goal setting and shared treatment plans for general measures? What ways and means are available to provide self-management support to patients? What incentives does your community have to encourage patients? What methods are there to assist patients with medication management? What methods are used in teaching patients about medication adjustments? Are patients encouraged to report medication effects? |
What links does your community have set up to: Financial support for medications? Transportation to appointments? Home health agencies? What programs are available to assist patients in obtaining medications? What programs are available to assist the patient and caregiver in medication management? |
|
Treatment for Diastolic Heart Failure (LVEF > or = 45%, normal or mild LV dysfunction by qualitative assessment) |
|
How are medication dosages and changes tracked? |
Who monitors medication adjustment? What intervals are established to review medications? How is care for underlying illnesses coordinated with heart failure care? |
Do guidelines address optimization of BP control (140/90 or less), aggressive treatment of coronary artery disease and maintenance of sinus rhythm? Do guidelines address the role of diuretics in maintaining euvolemia and minimizing symptoms, nitrates for preload reduction, other therapeutic options (such as ACE inhibitors, beta blockers, calcium channel blockers and ARBs) and digoxin in patients who continue to have symptoms despite the above? |
What methods are there to assist patients with medication management? What methods are used in teaching patients about medication adjustments? Are patients encouraged to report medication effects? |
What programs are available to assist patients in obtaining medications? What programs are available to assist the patient and caregiver in medication management? |
Adapted w/ permission from Ed Wagner, MacColl Institute for Health Care Innovation at Group Health Cooperative
|
“Ideal” care |
Examples |
Clinical Information Systems |
Delivery System Redesign |
Decision Support |
Self-management Support |
Community Resources and Policies |
|
Treatment for Refractory Heart Failure |
|
How does your community track which heart failure patients need referral? |
How do case managers, primary care providers and cardiologists interact? |
Does the guideline include the decision to refer? |
How is care coordinated from the patient’s perspective? |
What assistance is provided to complete referrals? |
|
Self-management |
|
How is it known whether patients have an adequate understanding of HF and their role in managing their disease? How do you document changes to the care plan? How is the need for case management identified? How is information shared across practice settings? |
Are ‘education clinics’ available to provide this information? Who reviews the collaborative goals? Who calls the patients to discuss monitoring, diet, exercise, medication use? Who determines discharge from follow-up care? How do case managers interact with primary care providers and specialists? What methods and schedules are used to contact patients? |
What techniques for teaching patients appropriate guidelines for how to adjust diuretics, when to call for additional input, and how to arrange follow-up appointments for changes in their condition? Do you utilize behavior change and motivational techniques in patient interactions? How are providers trained in motivational techniques? How are patients assisted to make informed decisions about their care? Does your community have evidence-based protocols for the case managers? How are the protocols disseminated to case managers? How is the protocol “embedded” into your community’s system? |
Is there a mechanism for patients to make appointments promptly? What tools are available to assist patients with their self-management? What “menus” of self-management support are available to patients? (Class, telephone, peer, case management.) What incentives does your community have to encourage patients? Does self-management support address all conditions experienced by the patient and their interactions? |
What assistance is provided to patients for ensuring home monitoring, such as scales or caregivers? What links does your community have set up to: Home health programs? Support groups? Internet links? Transportation programs? Financial assistance? When one is involved, how does the case manager interact with other health care providers in the community? |
|
Monitoring |
|
How does your community track periodic assessments of symptoms and function? How do you track laboratory tests? What ICT tools are available to facilitate the use of patient-centered health status measures? |
Who monitors signs, symptoms, medication side effects and daily weights? What intervals are established to review laboratory tests? What methods are used to monitor patients (phone, fax, email)? |
Do guidelines include periodic assessment of signs, symptoms, weight and medications? Do guidelines include intervals for monitoring laboratory tests? |
What methods are there to assist patients with monitoring? What methods are used in teaching patients about monitoring? |
What assistance is provided to patients for ensuring home monitoring, such as scales or caregivers? |
Adapted w/ permission from Ed Wagner, MacColl Institute for Health Care Innovation at Group Health Cooperative
|
“Ideal” care |
Examples |
Clinical Information Systems |
Delivery System Redesign |
Decision Support |
Self-management Support |
Community Resources and Policies |
|
End of Life Issues |
When no other options are available to improve the health status of severely debilitated patients, end of life care should be pursued |
How do you track patient preferences for end of life care? Is this information available across multiple settings? |
Who discusses end of life issues with patients? When and where do discussions occur? Which team members can be helpful to the patient and family and how are they involved? |
Do protocols and guidelines address advance planning such as living will, durable power of attorney for health care or other appropriate legal documents? |
How are patient and family members provided with helpful information and support? |
What links do you have set up to community programs to assist patients, such as legal aid? |
|
Sharing successes/ failures across institutions |
|
|
|
|
|
|
|
Engendering involvement of practitioners |
|
|
|
|
|
|
|
Care delivery by clinicians other than cardiologists |
|
|
|
|
|
|
|
Other Please consider any unique attributes of your community initiative not addressed above, and capture those efforts in the worksheet. |
|
|
|
|
|
|
Adapted w/ permission from Ed Wagner, MacColl Institute for Health Care Innovation at Group Health Cooperative










