Chapter 4
Care Coordination
DEFINITION AND OVERARCHING THEMES
The objective of the cross-cutting strategy session on care coordination was to identify ways in which communities can improve how care is coordinated––across settings and clinicians––for people with chronic and complex conditions. It was the universal belief of the participants that the current fragmented process of care delivery should be redesigned to enhance clinical outcomes and reduce expenditures. To frame this topic, the following definition of care coordination was accepted by the group (IOM, 2001, 2003b; Shortell et al., 2000):
To establish and support a continuous healing relationship, enabled by an integrated clinical environment and characterized by the proactive delivery of evidence-based care and follow-up. Clinical integration is further defined as the extent to which patient care services are coordinated across people, functions, activities, and sites over time so as to maximize the value of services delivered to patients. Coordination encompasses a set of practitioner behaviors and information systems intended to bring together health services, patient needs, and streams of information to facilitate the delivery of care in accordance with the six aims set forth in the Quality Chasm report. Such coordination can be facilitated by procedures for engaging community resources, including social and public health services.
At the summit, Martha Whitecotton, representing the voice of the consumer on the opening plenary panel, courageously shared her family’s experience navigating the turbulent waters of the health care delivery system with her son, who has major depression. She repeatedly emphasized the importance of care coordination across systems—health care and education—for individuals with depression and
extended her message to all chronic health conditions. Regrettably, her family’s experience was typical of many of those with chronic illness—one of disjointed care, spotty communication between primary care providers and specialists, and frustration over not knowing where to turn in the community for help. Her son’s case involved untimely diagnosis, failure to provide information on the evidence-based guidelines for depression treatment, lack of a centralized care plan shared among providers and the school system, and a myriad of health insurance obstacles. William Bruning, representing the Mid-America Coalition on Health Care Community Initiative on Depression, responded to the recurring themes in Whitecotton’s presentation and provided an overview of how the coalition is addressing many of these breakdowns in the system (see Box 4-1).
KEY STRATEGIES
Participants identified four key strategies to address the major barriers to achieving high-quality, well-coordinated care: (1) align financial incentives; (2) provide educational supports; (3) use patient-centered health records supported by information and communications technology; and (4) ensure accountability and define roles for care.
Align Financial Incentives
Aligning financial incentives to reward high-quality care was a resounding theme throughout the summit, but was viewed as particularly compelling by participants in the care coordination session. Currently, the health care financing system is oriented to reward care for acute episodes, administered by a single provider, as opposed to a continuum of care across multiple providers. The disconnect between a system designed for acute care and the needs of more than 125 million people in the United States with chronic conditions is profound (Partnership for Prevention, 2002). The session participants identified important opportunities to address this problem, underscoring the need for a shared vision around:
-
An operational construct—consistent with evidence-based medicine—of what good care coordination would be.
-
How care coordination would be measured.
-
How models of successful reimbursement for care coordination would be disseminated.
To initiate the identification of an operational construct of good care coordination, three elements of such a construct were identified: (1) technical quality or the comprehensiveness of care, (2) measures of efficiency, and (3) a patient-reported set of outcomes. Clearly, interdisciplinary teams of individuals with expertise in chronic diseases, in maximizing functional ability, in supporting family caregivers, in health education, and in social services are needed to specify these elements for chronic disease. Once these elements have been specified, internalized, and accepted by those who provide care, a reliable core set of measures and benchmarks can be established and serve as the basis for reimbursement, with financial incentives for more-effective implementation. This proposal parallels that of the finance group with regard to paying for performance and designing benefit packages around the creative accomplishment of better patient care.
Like the finance group, the care coordination group embraced the concept of budget neutrality. It was collectively acknowledged that effective care coordination could facilitate achieving the mandates of the Quality Chasm report to provide care “based on continuous healing relationships,” support “decision making [that] is evidence-based,” and “anticipate patients’ needs, rather than simply reacting to events” (IOM, 2001:8). Care could also be provided in a more cost-effective manner. For example, a heart failure patient who was gaining weight and becoming increasingly symptomatic could be recognized by means of a patient-initiated phone call and
|
Box 4-1. The Mid-America Coalition on Health Care Community Initiative on Depression initially began as a cooperative effort with 8 Kansas City employers in 1998 and has grown to encompass 15 employers—now impacting 140,000 lives. To identify the greatest health risks to employees and their families, the Behavioral Risk Factor Surveillance System survey was administered to 45,000 area residents by the Kansas Department of Health and Environment (Centers for Disease Control and Prevention, 2004). Based on the survey results, the founding group strongly endorsed targeting improved quality of care for depression, and thus focused on creating community and clinical support for timely diagnosis and treatment, destigmatization, and identification of the direct and indirect costs attributable to this disease. Some examples of interventions currently under way include the following: Lack of care coordination
Need for a patient-centered approach to care
Failure to provide information about best practices
Note: Additional information on the coalition can be found at its website (Mid-America Coalition on Health Care, 2004). |
treated, rather than progressing to the point of requiring hospitalization. Thus the participants were not proposing payment for another layer of care, but suggesting a coordinated care approach that would yield savings to support this new structure of care. Three mechanisms were discussed for stimulating change in the current payment system: (1) direct payments for care coordination, (2) pay for performance, and (3) capitation.
To accelerate such changes, Don Berwick in his keynote address called for a dialogue among communities, Medicare, and Medicaid to institute cost-neutral flexibility in the use of funds for the treatment of chronic illnesses. Specific strategies discussed during this crosscutting session that could be used by national leadership organizations to facilitate and simplify local efforts included granting waivers, collaborating with experts who perform quality measurement and data collection, and linking disparate parts of the system that currently benefit from the lack of coordination.
Provide Educational Supports
The session participants suggested that a major barrier to providing care consistent with the six aims of the Quality Chasm report is the difficulty of integrating multiple health providers to develop and communicate a common care plan for patients with chronic conditions. To do so becomes even more challenging as the number of individuals with multiple chronic conditions—now one in five Americans—continues to grow (Wu and Green, 2000). Thus, much attention was paid to the strategy of educational supports, which encompasses the following: (1) multidisciplinary health professions education; (2) teaching of care coordination principles in academic settings; and (3) development of care teams.
The ability to work in interdisciplinary teams—to “cooperate, collaborate, communicate and integrate care in teams to ensure that care is continuous and reliable”—is a core competency recommended for all clinicians in the IOM report, Health Professions Education: A Bridge to Quality (IOM, 2003a:4). Yet concern was expressed by several of the condition-specific working groups that the health care workforce is not adequately trained to meet such demands of the changing practice environment. Overcoming this gap in knowledge requires redesigning both didactic and clinical components of professional training. Indeed, a survey of more than a thousand physicians revealed that two-thirds of respondents felt their training in care coordination and patient education had been inadequate (Anderson, 2003).
The depression working group suggested broadening the scope of training and increasing the knowledge base for that condition in the areas of screening, referral, and treatment. Accomplishing this will require a coordinated effort across the spectrum of mental health providers, including physicians, nurses, social workers, and psychologists. A dual strategy was proposed, beginning with practicing clinicians, managers, and educational leaders, and then progressing through faculty to currently enrolled students. A core set of competencies would need to be developed in these domains of care and then linked to ongoing licensing and certification programs. These competencies would be relevant across various chronic conditions in which depression is a prevalent comorbidity. Implementation of this strategy would begin at the local level in the first year and expand within 3 years to a national-level initiative. For example the depression group proposed:
-
Educational credentialing organizations developing a nationally recognized systems-oriented approach to education and training for depression.
-
Increased emphasis on these competencies embedded in licensing, certification, and recertification programs.
-
Enhanced focus on system-based and practice-based approaches to the evolution of communication and collaboration as a core competency.
The asthma working group highlighted opportunities for expanding such training efforts by targeting office staff and other caregivers, with emphasis on completing and utilizing asthma action plans. For example, the Children’s Mercy Hospital/Kansas City Asthma Coalition, a community participating in the summit, provides an excellent example of an office-based training program designed to improve care coordination while engaging patients and their caregivers. The coalition has taken a proactive approach to educating and training physicians to help them properly diagnose and deliver high-quality asthma care. One of its interdisciplinary interventions involves placing certified asthma educators into primary care offices for 8 weeks to provide instruction on evidence-based asthma care, practice role modeling, and stimulate behavior modification. The focus is on teaching clinicians to fully engage patients in the decision-making process and providing timely feedback on performance on key asthma indicators.
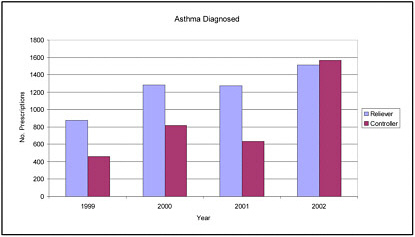
Outcomes from this intervention have been positive. A foundation of good asthma care is to emphasize the use of treatments that control/prevent asthma attacks, rather than bronchodilators that relieve symptoms once they have developed. Graph 1 in Box 4-2 demonstrates that from 1999 to 2001, very few controllers were prescribed as compared with relievers.
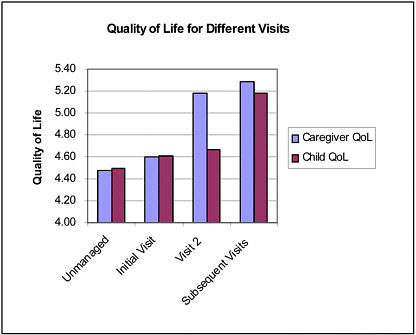
In 2002, however, after the intervention had been introduced, this ratio shifted favorably. As illustrated by Graph 2 in Box 4-2, quality-of-life scores (with higher numbers indicating better quality of life) were also found to increase postintervention for both patients with asthma and their caregivers (Jones and Portnoy, 2003; Miller et al., 2003).
Richard Brumley, representing the Kaiser Permanente TriCentral Palliative Care Program community, shared with summit participants how that program developed a multidisciplinary care team to provide compassionate, patient-centered care for patients with chronic diseases approaching the end of life. See Box 4-3 for an overview of this program.
|
“As part of a team we think of all of us as having equal status—physicians, nurses, social workers, volunteers, chaplains, home health aides, the whole gamut. We all work together.” —Richard Brumley, summit participant |
|
Box 4-3. The Kaiser Permanente TriCentral Palliative Care Program uses a multidisciplinary approach to coordinate care in the home for patients transitioning from acute to palliative care during the last 12 months of life. After statistics showed that more than 50 percent of Kaiser Permanent TriCentral patients with heart failure, chronic obstructive pulmonary disease, and cancer died in either the medical/surgical unit or the intensive care unit, this program was developed to remedy the mismatch between patient preferences to die peacefully at home and the tendency for the health care system, as currently structured, to steer care at the end of life to the inpatient setting. In this home-based care program, the patient and the family are considered an integral part of the care team and are supported by an array of professionals, including a physician, nurse, and social worker, while also receiving other psychosocial supports, such as from a chaplain or a volunteer. Making the patient the central focus with a radiating comprehensive care team encouraging active communication among all involved can heighten awareness of patient and family treatment preferences. The program places a strong emphasis on evidence-based medicine and has developed protocols and care guidelines to reduce variability in practice. For example, it has implemented a checklist of the most important things team members must cover, such as pain management and advanced care planning, to ensure successful management of home-based care. The program has also incorporated continuous quality improvement (QI) into its daily practice. Thus when a problem arises, it is designated as a “QI Indicator” and is monitored monthly, with outcomes being shared within the program. Results of a recent study, which included a comparison group, demonstrated that program participants had significantly higher satisfaction ratings and fewer emergency department visits, hospital days, skilled nursing facility days, and physician visits. Notably, 88 percent of patients receiving palliative care died at home. Additionally, on average those enrolled in the program experienced a 45 percent decrease in cost as compared with patients who received routine care (Brumley et al., 2003). |
Use Patient-Centered Health Records
Recognizing that more than half of people with chronic conditions have three or more different physicians, the participants in this session stressed that an easily accessible, patient-centered health record is critical to ensure communication of treatment plans across providers (The Gallup Organization, 2002). Additionally, as patients are often shuttled to and from multiple care settings—hospitals, nursing homes, and home health—seamless transfer of heath information during these transitions is vital, as this is when patient are most vulnerable to breakdowns in care (Coleman et al., 2003).
Information and communications technology, in the form of electronic health records (EHRs) and patient registries, was proposed as a viable solution to facilitate rapid retrieval and sharing of patient data and address the problems associated with traditional paper health records that inhibit good care coordination, such as charts being misplaced and missing data (Tang et al., 1994). A fundamental concept articulated by many of the working groups was that patients should play a central role in the diffusion and exchange of their health data. To this end, patients should have total access to their records, with some suggesting that they be the ultimate locus of control. Succinctly stated, the overarching message from this session was to provide a common health record, preferably in electronic format, and complete with relevant patient information, to all those involved in care, and to empower patients to be in charge of their records.
In its action plan shared with the plenary session, the diabetes working group proposed specific parameters for EHRs, including standardization of data elements to allow for the flow of information among clinicians and patients. The group also proposed that patients be provided with a portable health record, such as a “smart card” containing their data and/or a web-based repository (see Box 4-4).
Ensure Accountability and Define Roles for Care
Successful management of chronic conditions requires the delivery of a vast array of services, hand-offs to other specialists, and aggressive follow-up. Given this complexity of care, it is essential that the care team’s roles be clearly delineated and that administrative support be provided for new functions and responsibilities assumed by staff. In essence, this strategy holds each team member accountable for ensuring that a patient’s care is properly managed.
The Chronic Care Model (see Chapter 1) supports this type of delivery system redesign at the micro-system level—the “front line” where small groups interact closely with patients. The model identifies the following elements as essential to the delivery of effective and
|
Box 4-4.
|
efficient care: (1) define roles and allocate tasks among team members; (2) plan interactions between informed, activated patients and a prepared practice team to support care that is evidence-based; (3) ensure regular follow-up by the care team; (4) provide more intense case management for more complex cases; and (5) administer care to patients that is culturally sensitive (Improving Chronic Illness Care, 2004; Quinn, 1992; Wagner et al., 2001).
In addition to defining providers’ roles, it was suggested across the working groups that the community’s role should be articulated in the overall care plan. The asthma working group encouraged health care practices to partner with community resources to foster two-way communication and sharing of expertise. For example, leaders from churches and social organizations could be targeted to provide peer education for chronic conditions prevalent in their communities in a comfortable, nearby setting. Both the pain control and heart failure working groups called for the development of media campaigns to raise public awareness of their respective conditions.
The Philadelphia Department of Health—recently awarded a Department of Health and Humans Services Steps to a HealthierUS grant (see Box 1-5 in Chapter 1)—described its initiative to coordinate care for children with asthma across multiple systems and link them to resources in the community (Steps to a HealthierUS Initiative, 2004). Box 4-5 provides a description of this program.
CLOSING STATEMENT
The participants in this session outlined several strategies for achieving good care coordination. First, financial incentives need to be in place to reward and encourage care coordination. Implementing this strategy will require conceptualizing and operationalizing what care coordination is so it can be measured and reimbursed accordingly. Second, well-trained interdisciplinary teams of diverse practitioners—physicians, nurses, allied health professionals, social workers, and others—are critical to delivering high-quality, well-orchestrated care. To meet this need, current approaches to clinical training must be redesigned to address the necessary skills. Third, a patient-centered EHR is a viable mechanism for facilitating care coordination. Finally, accountability to the patient is paramount, necessitating clearly defined roles for clinicians, as well as mobilization of community resources.
|
Box 4-5. The Philadelphia Department of Health’s Child Asthma Link Line targets children who present to local pediatric emergency departments with an acute exacerbation of asthma. The visit is viewed as a sentinel event and triggers immediate intervention, including a follow-up phone call to the parent or guardian, referral to a specialist, and enrollment in an asthma disease management education program for both caregiver and patient. Educational programs use a train-the-trainer approach, with parents and children who have been through the program serving as mentors to newcomers. Additional interventions include an environmental assessment for asthma triggers, partnering with the school system to ensure that an asthma action plan is in place, and coordination of medical insurance benefits to help families obtain coverage for uninsured children. This multilevel initiative brings all providers together to center care on the child’s needs. |
REFERENCES
Anderson G. 2003. Chronic care. Advanced Studies in Medicine 3(2):110–111. [Online]. Available: http://www.jhasim.com/files/articlefiles/pdf/journal_p110(V3-2)MC_health.pdf [accessed April 30, 2004].
Brumley RD, Enguidanos S, Cherin DA. 2003. Effectiveness of a home-based palliative care program for end-of-life. Journal of Palliative Medicine 6(5):715–724.
Centers for Disease Control and Prevention. 2004. CDC’s Behavioral Risk Factor Surveillance System. [Online]. Available: http://www.cdc.gov/brfss/ [accessed March 23, 2004].
Coleman EA, Boult C, American Geriatrics Society Health Care Systems Committee. 2003. Improving the quality of transitional care for persons with complex care needs. Journal of the American Geriatrics Society 51(4):556–557.
Improving Chronic Illness Care. 2004. ICIC: The Chronic Care Model: Delivery System Design. [Online]. Available: www.improvingchroniccare.org/change/model/deliv_design.html [accessed February 26, 2004].
IOM (Institute of Medicine). 2001. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academy Press.
IOM. 2003a. Health Professions Education: A Bridge to Quality. Greiner AC, Knebel E, eds. Washington, DC: National Academy Press.
IOM. 2003b. Priority Areas for National Action: Transforming Health Care Quality. Adams K, Corrigan JM, eds. Washington, DC: National Academy Press.
Jones EM, Portnoy JM. 2003. Modification of provider behavior to achieve improved asthma outcomes. Current Allergy and Asthma Reports 3(6):484–490.
Mid-America Coalition on Health Care. 2004. Mid-America Coalition on Health Care. [Online]. Available: http://www.machc.org/ [accessed April 30, 2004].
Miller K, Ward-Smith P, Cox K, Jones EM, Portnoy JM. 2003. Development of an asthma disease management program in a children’s hospital. Current Allergy and Asthma Reports 3(6):491–500.
Partnership for Prevention. 2002. Better Lives for People with Chronic Conditions. Baltimore, MD: John Hopkins University, Robert Wood Johnson Foundation.
Portnoy JM. 2004 (January 6). Patient Self Management: Asthma. Presentation at the Institute of Medicine 1st Annual Crossing the Quality Chasm Summit, Washington, DC. Institute of Medicine Committee on Crossing the Quality Chasm.
Quinn JB. 1992. Intelligent Enterprise: A Knowledge and Service Based Paradigm for Industry. New York, NY: New York Free Press.
The Gallup Organization. Serious Chronic Illness Survey. 2002. The Gallup Organization.
Shortell SM, Gillies RR, Anderson DA. 2000. Remaking Health Care in America. 2nd Edition. San Francisco, CA: Jossey-Bass.
Steps to a HealthierUS Initiative. 2004. Grantees, Steps to a HealthierUS Initiative. [Online]. Available: http://www.healthierus.gov/steps/grantees.html [accessed March 24, 2004].
Tang P, Fafchamps D, Shortliffe EH. 1994. Traditional Hospital Records as a Source of Clinical Data in the Outpatient Setting. Eighteenth Annual Symposium on Computer Applications in Medical Care, Washington, DC. Pp. 575–579.
Wagner EH, Austin BT, Davis C, Hindmarsh M, Schaefer J, Bonomi A. 2001. Improving chronic illness care: Translating evidence into action. Health Affairs (Millwood, VA) 20(6):64–78.
Wu SY, Green A. 2000. Projection of Chronic Illness Prevalence and Cost Inflation. Santa Monica, CA: RAND Corporation.