7
Immigrant Health: Selectivity and Acculturation
Guillermina Jasso, Douglas S. Massey, Mark R. Rosenzweig, and James P. Smith
Despite overall improvements in health, there is renewed concern that racial and ethnic disparities in health persist and in some cases may have expanded. Ethnic health disparities are inherently linked to immigration because ethnic identities are traced to the country of origin of an immigrant or his or her ancestors. The average healthiness of the original immigrants, the diversity in health status among immigrants, and the subsequent health trajectories following immigration both over the immigrants’ lifetime and that of their descendants all combine to produce the ethnic health disparities we observe at any point in time. Identifying the determinants of the original health selection of migrants and the forces that shape health paths following immigration is critical to understanding ethnic health differences.
According to the 2000 U.S. Census, there are 32 million foreign-born people now living in this country, constituting about one in nine of the total population. The foreign-born population has been growing rapidly as the numbers of immigrants has been rising in recent decades, reaching rates that rival the number of arrivals at the beginning of the 20th century. Moreover, immigration will be the driving force in accounting for the future growth of the American population. Recent estimates indicate that the American population will increase by 120 million people over the next 50 years, 80 million of who will be the direct or indirect consequence of immigration (see Smith and Edmonston, 1997). These demographic trends suggest that the health status of immigrants and their descendants will play an increasingly central role in shaping health outcomes of the American people. The importance of immigrant health is not limited to an American
setting. The United States is only an average country in terms of the fraction of its residents who are foreign born, and increasing rates of international migration make this issue one that transcends borders.
Immigrants potentially offer some significant analytical advantages for understanding the origins of health disparities in any population. Most importantly, by definition immigrants have changed regimes, moving from an environment with one set of health risks, behaviors, and constraints into another one that may contain a quite different mix. Given the number of sending countries, the diversity of health regimes from which immigrants flow may be enormous. Because isolating meaningful variation in health environments can be problematic within a domestic-born population, scholars from several disciplines have been eager to use immigrant samples to measure the impact of environmental factors such as diet, health care systems, and environmental risks. But these perceived advantages of immigrant samples do not come without a cost, as immigrant samples also raise difficult analytical issues about the extent of health selectivity and the nature of the appropriate counterfactual.
This paper is divided into six sections. The first, section one, provides a simple descriptive comparison of some salient health outcomes of foreign-born and domestic-born Americans. Relying on the existing scientific literature, the section that follows highlights some key findings and the hypotheses these findings generate about the health status of the foreign-born population. Two of the more central questions that have emerged involve the mechanisms shaping health selectivity and the determinants of health trajectories following immigration. With this in mind, the next section outlines some simple theoretical models of health selectivity of immigrants and their subsequent health trajectories following immigration. The following section uses data from the New Immigrant Survey to provide new information on the diversity of health outcomes of new legal immigrants to the United States. New empirical models that estimate the determinants of health selectivity and health trajectories following immigration are presented in the next section. The final section summarizes our views on the principal research and public policy questions about immigrant health that are high priority. It also contains our recommendations about how scientific funding agencies may best assist the research community in answering these questions.
HEALTH OF THE NATIVE BORN AND FOREIGN BORN: AN OVERVIEW
How do the native born and foreign born compare in terms of their overall health? Two widely used measures of health outcomes are self-reports of general health status based on a five-point scale ranging from
excellent to poor and prevalence rates of important chronic conditions. Table 7-1 compares the self-reports of native and foreign-born individuals using the 1996 National Health Interview Survey, and Table 7-2 provides a similar comparison for some common chronic conditions.1 Because immigrants are on average much younger than the native born and health is strongly related to age, the data in these tables are also stratified by age.
Using self-reports of general health status in Table 7-1, the foreign-born population in the United States appears to be in slightly worse health than the native born. These differences are concentrated in the higher end of this health scale. For example, conditioned on age, the fraction of foreign born who report themselves in either excellent or very good health is about four or five percentage points lower than that of the native born. The principal exception occurs among those ages 61 to 80; a considerably higher fraction of the foreign born say they are in either fair or poor health.
There is growing evidence that residents of different countries use different response thresholds when placing themselves within scales that involve ranking along general well-being criteria, including self-reported health (see Banks, Kapteyn, Smith, and Van Soest, 2004; King, Murray, Solomon, and Tandon, 2003). For this reason, it is useful to also examine other measures of health outcomes that may not be as susceptible to the problem of international differences in response thresholds.
The picture is quite different when disease prevalence rates are used instead as the health index. Across all conditions and in every age category listed in Table 7-2, the foreign born have much lower rates of chronic conditions than the native born. For example, for the two most prevalent chronic diseases—arthritis and hypertension—disease prevalence rates are nearly 50 percent higher among the native born. Although these differences
TABLE 7-1 Self-Reported Health Status of Native and Foreign-Born Individuals
|
|
Age Category |
||||
|
|
21-30 |
31-40 |
41-60 |
61-80 |
All Ages |
|
Born in United States |
|||||
|
Excellent or very good |
73.9 |
71.4 |
60.4 |
42.7 |
62.4 |
|
Good |
21.1 |
21.4 |
25.7 |
32.9 |
25.1 |
|
Fair or poor |
5.0 |
7.2 |
13.8 |
24.4 |
12.5 |
|
# of observations |
6,750 |
8,484 |
12,185 |
6,642 |
34,061 |
|
Foreign born |
|||||
|
Excellent or very good |
68.7 |
66.5 |
56.6 |
38.9 |
59.7 |
|
Good |
25.7 |
25.9 |
29.0 |
30.1 |
27.5 |
|
Fair or poor |
5.6 |
7.7 |
14.4 |
31.0 |
12.8 |
|
# of observations |
1,747 |
1,918 |
2,268 |
900 |
6,833 |
|
SOURCE: Calculations by authors from 1996 National Health Interview Survey. |
|||||
TABLE 7-2 Prevalence of Chronic Conditions by Nativity Status
|
|
Age Category |
||||
|
|
21-30 |
31-40 |
41-60 |
61-80 |
All Ages |
|
Arthritis |
|||||
|
U.S. born |
2.7 |
6.7 |
18.5 |
42.0 |
16.9 |
|
Foreign born |
2.1 |
2.2 |
11.4 |
41.9 |
11.2 |
|
Diabetes |
|||||
|
U.S. born |
0.4 |
1.5 |
4.1 |
11.0 |
4.1 |
|
Foreign born |
0.0 |
1.3 |
3.5 |
10.7 |
3.2 |
|
Hypertension |
|||||
|
U.S. born |
3.7 |
5.9 |
17.0 |
36.2 |
15.3 |
|
Foreign born |
1.4 |
4.6 |
12.9 |
34.7 |
10.8 |
|
Heart disease |
|||||
|
U.S. born |
3.5 |
5.1 |
8.7 |
19.5 |
8.9 |
|
Foreign born |
0.9 |
2.9 |
6.2 |
20.7 |
6.1 |
|
Asthma |
|||||
|
U.S. born |
6.9 |
5.3 |
4.6 |
5.5 |
5.4 |
|
Foreign born |
3.7 |
2.5 |
3.8 |
4.8 |
3.5 |
|
Diseases of the lung |
|||||
|
U.S. born |
9.1 |
7.3 |
9.9 |
13.1 |
9.7 |
|
Foreign born |
2.4 |
5.8 |
6.3 |
7.4 |
5.3 |
|
SOURCE: Calculations by authors from the 1996 National Health Interview Survey. Note that because questions on specific chronic conditions were given to one-sixth of the sample, the number of observations in this table are approximately one-sixth of those in Table 7-1. |
|||||
are smaller in the other conditions contained in this table (diabetes, heart disease, asthma, and diseases of the lung), in every case lower rates are found in the foreign-born population. When considered together, the data in Tables 7-1 and 7-2 suggest that foreign-born populations may self-report themselves in worse health than the native born do given their objective health circumstances. An alternative view is that self-reports of specific health conditions are underreported in foreign-born populations perhaps due to their less frequent contact with Western medical diagnostics. Cultural, language, and institutional differences across nations may also have a significant impact on what people know and what they report about their illnesses. We return to these issues later in this chapter.
Once again, there is some evidence in Table 7-2 of a reversal in ranking among older households. Reported rates of heart disease actually are slightly higher among the oldest foreign-born group listed, and there is a noticeable tendency for differences to converge to near equality among the older populations in all conditions other than diseases of the lung. This apparently more rapid disease progression across age groups among the foreign born in Tables 7-1 and 7-2 is one source of the view that immigrant populations tend to experience more rapid health deterioration over their stay in the United States than is typical of the native-born population.2
For several reasons, such a conclusion would be at best premature. As the demographic and labor economics literature has argued and demonstrated repeatedly, patterns obtained from cross-sectional age stratifications may not reveal actual lifecycle realities for anyone (see Smith and Edmonston, 1997). The within-age cell populations in Table 7-2 are members of distinct immigrant cohorts who may differ among other factors in their underlying health. A cross-sectional age pattern inherently cannot separate across-cohort differences from those that represent the pure effects of aging or staying longer in a location. Compounding this problem, there are nontrivial rates of emigration from these immigrant cohorts, and any health selectivity associated with such emigration would add more complexity. Finally, there is no obvious reason why health trajectories of the native-born U.S. population are representative of the health-age profiles that immigrants would have experienced if they had decided not to immigrate. We will return to a fuller discussion of these issues.
The immigrants who arrive in any year may also be influenced by forces unique to that year, such as the current state of relative economic conditions in the sending or receiving countries, new legislative changes in the rules governing immigration, or a specific refugee crisis. Consequently, the year immigrants migrate may matter in terms of their initial health outcomes. To illustrate this point, Table 7-3 lists self-reported health status in calendar years 1991 and 1996 among those who last immigrated to the Untied States less than 5 years ago. Health status appears to be lower among the immigrants of the early 1990s compared to those who immigrated during the late 1980s. In every instance in Table 7-3, the fraction that report in fair or poor health is larger in 1996 than in 1991. This variation in health status among immigrants arriving only 5 years apart
TABLE 7-3 Self-Reported Health Status by Time Since Immigration and Calendar Year
|
|
Age Category |
||||
|
|
21-30 |
31-40 |
41-60 |
61-80 |
All Ages |
|
0-5 years in United States in 1991 |
|||||
|
Excellent or very good |
71.9 |
67.2 |
52.9 |
40.6 |
65.7 |
|
Good |
23.3 |
26.9 |
30.9 |
34.4 |
26.2 |
|
Fair or poor |
4.8 |
5.9 |
16.2 |
25.1 |
8.2 |
|
# of observations |
702 |
364 |
273 |
62 |
1,401 |
|
0-5 years in United States in 1996 |
|||||
|
Excellent or very good |
68.3 |
61.7 |
43.1 |
47.6 |
60.9 |
|
Good |
24.3 |
30.3 |
37.8 |
14.7 |
27.9 |
|
Fair or poor |
7.4 |
8.1 |
19.1 |
37.7 |
11.2 |
|
# of observations |
521 |
256 |
182 |
42 |
1,001 |
|
SOURCE: Calculations by authors from 1996 National Health Interview Survey. |
|||||
sends a warning signal that research conclusions drawn from studies of immigrant cohorts from different times in American history may be generalized only with considerable risk.
Stratification by age does not provide a direct test of the impact on health of different levels of exposure by immigrants to the U.S. environment. Table 7-4 provides a more direct test by arraying prevalence rates of chronic conditions by length of reported stay in the United States. Because sample sizes are quite thin in any single NHIS year, the data are pooled across all years of the NHIS between 1991 and 1996 inclusive.3 If (controlling for age) all immigrant cohorts were identical at time of entry into the United States, then the patterns observed across time since immigration would inform us about the impact of different durations of exposure to the American health environment. Unlike the age patterns discussed earlier, these data do not speak unambiguously about any effects of differential duration of stay in the United States. For example, among those over age 50, hypertension is most prevalent among those in the 0 to 5 years since immigration group, lung disease is most prevalent among those in the 6- to 10-year group, and arthritis is most common among those with 11 to 15 years of exposure to the United States. In addition to sampling variability, this array is confusing partly because the ceteris paribus of all immigrant cohorts being alike at time of entry is unlikely to be correct. The relatively high rates of hypertension among recent immigrants over age 50 may simply indicate that there is differential health selection by age.
The availability of multiple cross-sections from the National Health Interview Surveys (NHIS) allows one to mimic an analysis that has become one of the mainstays in the labor economics literature regarding immigrant assimilation. By appropriately arraying the data by year since immigration and by age, one can in principle track cohorts as they age. This stratification is the basis of Table 7-5, which lists self-reported health status by time
TABLE 7-4 Rates of Chronic Conditions of New Immigrants
TABLE 7-5 Self-Reported Health Status by Time Since Immigration
since immigration and age where both are indexed by their 1991 values. To illustrate, the first entry in the 1991 column refers to those foreign born aged 21 to 30 in 1991 who had migrated to the United States within the previous 5 years. Of that group, 71.9 percent said they were in excellent or very good health. The number adjacent to it under the 1996 column (67.5) represents the self-reported health status of those who were 26 to 35 years old in 1996 and who had last migrated to the United States 6 to 10 years ago. Because both age and time since immigration have been incremented by 5 years, the 1991 and 1996 numbers would refer to the same group of people if the immigrant group was closed. Data are presented separately for those who in 1991 had migrated 0 to 5 years ago and 6 to 10 years ago. The final panel represents those born in the United States.
Not surprisingly given that respondents are necessarily getting older, the general tendency for all groups included in this table is that their health deteriorated somewhat between 1991 and 1996. More germane to our topic is the relative profiles of immigrants compared to those born in the United States. Although initial health levels are higher for the native born, there does not appear to be any systematic differential rate of deterioration at the higher health levels between the most recent arrivals (0 to 5 years) and the native born. However, there is some evidence of a greater movement of recent immigrants into the fair or poor category. When we compare the native born to those whose reported 1991 time of arrival was 6 to 10 years ago, if anything immigrant health deterioration may be less than the native born.
Table 7-6 performs a similar analysis using prevalence rates of chronic conditions. Two findings stand out from this table. First, by far the most
TABLE 7-6 Rates of Chronic Conditions of New Immigrants
|
Foreign Born |
||||
|
Age |
25-44 |
30-49 |
50+ |
55+ |
|
Years in United States |
0-5 |
6-10 |
0-5 |
6-10 |
|
Hypertension |
2.7 |
3.9 |
31.8 |
18.2 |
|
Diabetes |
0.8 |
1.7 |
6.1 |
8.8 |
|
Cancer |
0.1 |
0.0 |
1.3 |
0.7 |
|
Lung Disease |
1.9 |
2.6 |
3.7 |
8.1 |
|
Arthritis |
2.8 |
3.8 |
23.1 |
29.5 |
|
Heart Disease |
1.9 |
2.2 |
18.0 |
14.6 |
|
Asthma |
1.1 |
2.9 |
1.3 |
4.6 |
|
Age |
25-44 |
30-49 |
50+ |
55+ |
|
Years in United States |
6-10 |
11-15 |
6-10 |
11-15 |
|
Hypertension |
3.5 |
4.8 |
17.0 |
28.1 |
|
Diabetes |
1.0 |
1.2 |
8.2 |
11.2 |
|
Cancer |
0.0 |
0.7 |
1.2 |
0.8 |
|
Lung Disease |
3.2 |
3.5 |
5.9 |
3.1 |
|
Arthritis |
2.1 |
4.6 |
24.7 |
29.7 |
|
Heart Disease |
1.6 |
2.9 |
11.5 |
17.5 |
|
Asthma |
2.7 |
2.3 |
3.1 |
3.3 |
|
U.S. Born: Age |
25-44 |
30-49 |
50+ |
55+ |
|
Hypertension |
6.4 |
9.1 |
31.4 |
33.9 |
|
Diabetes |
1.5 |
2.0 |
8.8 |
9.8 |
|
Cancer |
0.6 |
0.9 |
0.8 |
6.8 |
|
Lung disease |
8.3 |
8.5 |
11.8 |
12.1 |
|
Arthritis |
6.3 |
8.7 |
37.0 |
40.6 |
|
Heart disease |
5.0 |
6.2 |
22.8 |
25.5 |
|
Asthma |
4.9 |
4.8 |
4.7 |
4.6 |
|
NOTE: See Table 7-4 for explanation on number of observations. SOURCE: 1991-1996 NHIS combined files. |
||||
salient pattern involves health selectivity of immigrants. No matter what duration since immigration is examined, prevalence rates among immigrants are much less than those for the U.S. born. As we will argue, strictly speaking the U.S. native-born population is not the appropriate comparison group to use when evaluating health selection of migrants. Rather, health selection of migrants involves a comparison between the health of migrants and stayers in the sending countries at the time of immigration. This comparison would be extraordinarily difficult given the number of sending countries and the state of health data in most of the sending countries. However, the United States can be used indirectly for this comparison. Because the health of the U.S. native born is so far in excess of those in most
migrant sending countries, if migrants to the United States have better health than the U.S. native born, they surely have better health than those who stayed in the sending countries.
Using this argument, the extent of this health selectivity is especially strong among younger migrants and for more serious health conditions. For example, prevalence rates for cancer, heart disease, and diseases of the lung are far less for recent migrants than for the U.S. born. Second, if we examine changes in prevalence rates with increasing age (and time since immigration), there is little evidence that the foreign born are doing worse compared to native-born Americans. An important caveat to the analysis contained in Tables 7-5 and 7-6 is that they are examining health changes over short increments in duration of stay. For many illnesses, one would want to examine health changes over much longer durations of stay than 5 years to better capture the impact of changing geographic location.
Moreover, the limitations of this analysis implicit in Tables 7-5 and 7-6 are serious when it comes to tracking immigrants. First, immigrant cohorts are not closed, because there is substantial emigration from the original immigrant cohort. For example, up to a third of Mexican immigrants who are in one decennial Census appear to have emigrated by the next. These rates of emigration differ significantly by nationality and across time. Second, the question on time since immigration asked in surveys is subject to considerable ambiguity. The specific question in the NHIS—“In what year did you come to the United States to stay?”—is quite ambiguous. Immigrants typically take many trips to the United States with uncertain intentions about how permanent their residence will be. For example, some may have come for temporary reasons, but subsequently decided to live permanently in the United States. Since they initially did not come to stay, it is unclear how they should answer the NHIS question.
MAIN FINDINGS FROM THE LITERATURE
There is a vast scientific literature on immigrant health differentials and their determinants that would be impossible to fully summarize here. Instead, we focus our review on that part of the literature that deals centrally with the main issues of the initial health selectivity of immigrants and the subsequent health trajectory following immigration.
Epidemiology has a long tradition of using migrant studies to isolate environmental effects on health. Put most simply, the basic notion is that if disease rates change when you move from one place to another, it is indicative of a role for environmental factors. A good example is Marmot’s observation that deaths by motor accidents are high both in France and among French immigrants to England, suggesting that the French bring their “accidents” with them (Marmot, Adelstein, and Bulusu, 1984).
A typical epidemiological study examines some health outcome in three populations that presumably differ in a significant way in their environments—people in the host country, the sending country, and migrants. Differences among them then are used to test the impact of some type of “environmental” exposure along a dimension where the groups are believed a priori to differ significantly. Although many differences may exist in their respective environments, the hope is that the design of the study has isolated and measured a small subset of salient differences. These epidemiological studies often examine patterns obtained from specific diseases where knowledge about the origins and progression of disease can be used to help isolate the migrant effect. As a practical matter, these comparisons are often limited to small geographical areas, especially in the host country. As we will see, the substantial heterogeneity in health among immigrants cautions that the use of small geographic areas to capture the representative migrant may be quite perilous.
A simple illustrative example of such studies is cited by Kasl and Berkman (1983) and relates to cancer. For example, mortality rates from breast cancer are low among both the Issei (Japanese migrants to the United States) and the Nisei (those born in the United States to Japanese parents), suggesting a genetic interpretation, while colon cancer rates among both the Issei and the Nisei are near the U.S. rates, from which a stronger environmental influence was inferred.
Perhaps the most influential of these studies has involved the health of Japanese immigrants to the United States.4 As a typical example of such studies, Marmot and Syme (1976) provide data showing that among men of Japanese ancestry, while all-cause mortality is higher among Japanese men (with cancer as the primary cause of death difference), the risks and occurrence of coronary heart disease (CHD) are lowest among those living in Japan, intermediate among those in Hawaii, and highest among those living in California. Moreover, while attenuated, these differences persisted among nonsmokers and among men with similar levels of cholesterol and/or blood pressure. Marmot hypothesized that the remaining differences may be due to cultural differences between the United States and Japan. Traditional Japanese culture is more characterized by group cohesion and social stability, which may be stress reducing and thus protective in reducing heart disease. Marmot examined health outcomes of Japanese living in and around the San Francisco Bay area, stratified by the degree of adherence to Japanese culture. Among these Japanese men, the more they adhered to the original Japanese culture, both during childhood and during adulthood, the lower the risks of CHD. This association prevails even when dietary preferences are controlled.5
Given its modern migration history with large numbers of migrants from quite diverse cultures (Europe, Asia, and Africa), it is not surprising
that Israel has been home to several important studies. The Israel Ischemic Heart Disease Project is a particularly influential research effort. In this study, 10,000 male Israeli government workers aged 40 and over were examined three times during a 5-year period, from 1963 to 1968. These government workers included first generation Israelis from many sending countries. According to the summary provided by Kasl and Berkman (1983), despite the large differences in culture and background across regions of birth, differences in disease rates were surprisingly small. In this case, either large differences in background did not translate into similarly significant health disparities or selection of a specific occupation (government employees) induced too much equality in health outcomes.
Finally, in another prospective epidemiological study of 1,001 middle-aged men of Irish ancestry, the relation between dietary information collected approximately 20 years ago and subsequent mortality from coronary heart disease was examined. Following the typical epidemiological protocol, the men were initially enrolled in three cohorts: one of men born and living in Ireland, another of those born in Ireland who had emigrated to Boston, and the third of those born in the Boston area of Irish immigrants. There were no differences in mortality from coronary heart disease among the three cohorts and only weak evidence that diet is related to the development of coronary heart disease.
In addition to using migrant samples to test the impact of differential environmental exposure, the second issue that has loomed large in the epidemiological studies concerns the health selection effect. In one of the most comprehensive studies of immigration selection, Marmot, Adelstein, and Bulusu (1984) compared mortality rates of migrants to England from Ireland, Poland, Italy, the Indian subcontinent, and the Caribbean to mortality rates for the sending countries. A summary of their findings is contained in Table 7-7, which lists age-standardized mortality rates compared to those who were born in the United Kingdom (UK). For all countries but Ireland, all-cause mortality rates were much lower among migrants compared to those of residents in the country of origin. While there are no controls for duration of stay, their data are suggestive of quite strong health
TABLE 7-7 Standardized Male Mortality Rates for Selected Immigrants to England and Wales (rates relative to United Kingdom)
|
|
Migrants |
Country of Origin |
|
Ireland |
114 |
99 |
|
Poland |
95 |
107 |
|
Italy |
77 |
91 |
|
Caribbean |
94 |
119 |
|
Indian subcontinent |
98 |
NA |
|
SOURCE: Adapted from Marmot et al. (1984, Table 1). |
||
selection effects among migrants to the UK. The exception of Ireland is also of interest in part because it indicates that health selection effects may vary systematically across countries. The cost of moving between the UK and Ireland is relatively low, and as we will demonstrate, in such situations health selection should be weaker. In addition, our model predicts that healthy Irish migrants should be found in much more distant places.
Latinos represent an important special case for research on immigrant health. In part the attention given to Latino health reflects their place as the numerically largest immigrant ethnic group, a dominance that will grow more pronounced in the future. But it also stems from scientific interest in the reasons for the so-called “Hispanic paradox”—by many measures Hispanic health is far superior to what one might expect given their socioeconomic status. In particular, although they share similar economic positions, Hispanic health levels are far better than those of African Americans and are often above those of non-Hispanic whites, whose economic resources are far superior. The Hispanic paradox is illustrated in Table 7-8. Age-adjusted death rates for the two leading causes of death—diseases of the heart and malignant neoplasms—are 50 percent lower among Hispanics than among African Americans. With the exception of diabetes, Hispanic age-adjusted death rates are actually lower for all diseases than those of non-Hispanic whites. The only group that outperforms Latinos on these measures is Asians/Pacific Islanders, whose overall lower mortality rate is due principally to low rates of death from heart disease.
The reasons underlying the Hispanic health paradox have been a source of considerable research and debate. Two themes have dominated that debate, but they are the same as those highlighted in this chapter. The first is the healthy migrant effect, where Latino migrants are seen as inherently healthier. This literature is largely silent on whether this better health due to selection mostly reflects the generally superior health habits, behaviors, and conditions in the Latino sending countries relative to the United States or
TABLE 7-8 Age-Adjusted Death Rates by Cause of Death: 1998
|
|
Hispanic |
Non-Hispanic White |
African American |
Asian/ Pacific Islander |
|
All |
596.4 |
862.7 |
1,135.7 |
516.8 |
|
Diseases of heart |
175.6 |
271.7 |
340.6 |
154.4 |
|
Malignant neoplasms |
123.7 |
203.0 |
255.1 |
124.2 |
|
Lower respiratory disease |
18.6 |
44.8 |
30.8 |
17.2 |
|
Cardiovascular diseases |
39.1 |
58.0 |
80.1 |
50.6 |
|
Diabetes |
32.1 |
21.1 |
22.1 |
16.9 |
|
Injuries |
30.2 |
34.6 |
39.5 |
17.6 |
|
Suicide |
6.3 |
12.8 |
5.8 |
6.6 |
|
Homicide |
8.8 |
3.1 |
22.6 |
3.5 |
|
SOURCE: Centers for Disease Control and Prevention (2001). |
||||
whether it is principally due to health selectivity among migrants compared to those who stayed. The problem with a heavy reliance on the generally superior health behaviors and conditions in the sending countries is that on standard health outcome measures such as mortality and morbidity, the major Latino sending countries rank below the United States.
The second theme concerns the protective effects of culture and norms within Latino families and communities. The argument is that there is cultural buffering, which is characterized by norms proscribing risky behaviors and promoting good ones, such as a healthier diet and stronger family support networks (Vega and Amaro, 1994). There is evidence that Latinos do have lower prevalence rates of some of the more common risk factors for good health. For example, rates of cigarette smoking are lower among foreign-born Latinos. The notable exception to better Latino health behaviors involves excessive weight and obesity. During the 1988-1994 time period, 24.4 percent of Mexican men and 36.1 percent of Mexican women were obese, much higher rates than observed among non-Hispanic whites. Similarly, 70 percent of Mexican women were reported as overweight compared to only 47 percent of non-Hispanic white women (see Centers for Disease Control and Prevention, 2001). Such weight-related problems no doubt have much to do with the high prevalence of diabetes among Hispanics.
With increased acculturation, however, the argument continues that the protective cultural buffering begins to dissipate, and with it Latino health deteriorates toward the U.S. norm. This deterioration becomes even more severe as we pass through the generations. As just one illustration among many, second generation Hispanic women fare worse than the first generation in terms of adolescent pregnancy and having low birthweight children (Vega and Amaro, 1994).
The final generic issue raised in the literature is that the very act of migration may also directly affect immigrant health. This effect is associated with the process of migration itself, which is often viewed as quite stressful with negative psychosocial impacts (Kasl and Berkman, 1983). This form of health impact of migration suggests that health problems of migrants should eventually be manifested in specific diseases. Cardiovascular diseases are known to be sensitive to prolonged exposure to high levels of stress, so that relatively high rates of heart disease among the foreign born associated with length of stay may be indicative of such a mechanism. More recently, heart disease has played an increased role in these studies. Migrants’ rates of heart disease are intermediate between sending and host country and converge with time since immigration (Kasl and Berkman, 1983). Repeated exposures of immigrants to prejudice and discriminatory acts in the host country are also cited as a reason for stress and its eventual toll on health (Vega and Amaro, 1994).
The emphasis in the epidemiological literature on specific diseases is important and should become a more standard part of analyses by social scientists. The early concerns about immigrant health had to do with the externalities associated with the spread of communicable diseases. Although this concern is much diminished today, tuberculosis tests and medical exams are required before admittance to permanent residence in the United States.
THEORETICAL ISSUES
There are two perennial themes to the literature on migration and health outcomes—the nature of the health selectivity of international migrants and the impact of migration on the subsequent health trajectory of migrants. Although these themes have appeared in the scientific literature for many decades and across several academic disciplines, there has been remarkably little theoretical guidance about the likely nature of the selectivity or on the mechanisms through which health trajectories may be altered by migration. In this section, we present a simple theoretical framework within which these questions can be investigated. A latter section summarizes our empirical estimates of these models.
Migration Model of Initial Health Selectivity
Will migrants be positively selected on their health, and if so what are the personal and environmental factors influencing the extent of this selection? Although one of the most often mentioned empirical findings regarding international migration concerns the possible health selectivity of migrants, there has been little formal theoretical investigation of this relationship. In this section, we develop a simple framework adapted from Jasso, Rosenzweig, and Smith (2001) that illustrates the main issues.
The decision to migrate can be viewed as a balance between the gains and costs of migration. For simplicity, these gains can be thought of as the difference in income received in the receiving and sending country. Income is the product of the skill of the individual (k), the rate of utilization of skill (or labor supply) (l), and a country-specific price of skill (w). All prices, skills, and utilization rates may be country specific.
Thus, an individual will migrate if:
(1)
where caj is the cost of moving from country j to country a. These costs may include not only any monetary costs associated with mobility, but also any nonpecuniary costs (utility), such as any cultural differences between the
sending and receiving country, the quality and availability of good health care, being away from family and friends, and the like. Individual skills may not be perfectly transferable across countries, a relationship that may be summarized by kia = αj kij where αj is index of transferability from country j to country a. Similarly, the relation of skill prices across countries can be written as wj = βo + βj wa and the relation of labor supply across countries is lia = cj lij. Substituting these intercounty associations into equation (1), an individual migrates if
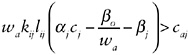
(2)
Before bringing health into this model, we mention some predictions for both number of migrants and skill selectivity of migrants who do come. First, an increase in the cost of migration (caj), whether due to monetary or nonmonetary factors, will reduce the number of migrants. Given skill prices, increases in migration costs also imply greater selectivity on either skill or labor supply. That is, when migration costs are greater, migrants must be either more skilled or harder workers or both. Second, countries with higher skill prices (βj) will also send fewer migrants to the United States, but once again these migrants should be more selective on labor effort or skill. Finally, migration rates will increase when rates of skill transferability (αj) are higher, but migrants who do come will be of lower skill or work effort.
Health can enter this model in several ways. The most direct pathway is that health enhances earnings capacity. It is widely acknowledged that health is an important component of an individual’s human capital (Grossman, 1972), so that skill levels are generally greater among healthier people. Healthier individuals are generally more energetic and robust, so that skill utilization (or labor supply) and health are also positively correlated. Because health increases both kij and lij, healthier individuals will gain more from migration and migrants will be positively selected on their health.
Health will interact with the other determinants of migration we have mentioned. Where the costs of migration between two countries are greater, migrants will self-select on better health to a greater extent. Thus, countries that are more distant from each other, either geographically or culturally, will (other things equal) be more positively selected on migrant health. Similarly, migrants from countries with lower skill prices relative to those in the United States will be less positively selected on migrant health. Finally, when skill transferability is lower, migrants will more positively select on health.
Holding everything else equal, equation (2) indicates that there is a minimum health level that would make migration worthwhile. Because
health varies so much among sending countries, this implies that the dispersion in health outcomes among migrants should be less than that which exists across sending countries and that the magnitude of health selection is negatively related to health levels in the sending countries.
To this point, we have highlighted health effects that operate principally through labor market earnings. Migrants may also be attracted to countries with higher quality health care or healthier environments. These factors may be incorporated into the model as part of the nonpecuniary costs of migration. For example, if the United States offers a healthier environment or lower cost health care of a given quality than that which exists in the sending country, more migrants will come, but the marginal migrant will be less healthy.
Labor market considerations are less important for older migrants who may have either short or no remaining tenure in the labor market. The factors relating to skill levels, utilization, and prices may be of no importance for new migrants over age 60 who do not plan to work. In contrast, the better health care available in the United States may be of far greater concern among older migrants. This indicates that health selection effects may be quite different among older migrants, a point consistent with the age stratifications in the data presented earlier.6 It also suggests the importance of time because migration is a key control in examining the health of older migrants. Older migrants consist of two groups—those who have migrated at a much younger age and who were presumably positively selected on their health and those who migrated at much older ages, when the migration selection may have been reversed.
Comprehensive evidence on the extent of health selection of migrants is difficult to obtain. In principle we would like to know how migrants compare at the time of their initial migration with residents in their sending country. The data contained in Table 7-7 do suggest that the migrant health selection effect may be strong, but there is no control for duration of stay in the United Kingdom.
As a first step toward gauging the importance of health selectivity, Table 7-9 ranks countries by numbers of legal male migrants to the United States in 1995, and then provides for each country the levels of male life expectancy and the probability of a male dying between ages 15 and 59. The later index is provided because it is presumably less affected by infant mortality and more closely approximates the ages when migration takes place. The story told by these two death indexes is quite similar, so we will concentrate our discussion on the more conventional life-expectancy measure. The variance in male life expectancy across these major sending countries is enormous, with a range of more than 25 years. Three countries have higher life expectancy than the United States, while overall life expectancy in 14 of the countries is lower than in the United States. A weighted (by
TABLE 7-9 Life Expectancies of Major Sending Countries
number of migrants) average of life expectancies from these major sending countries is 67.1 years, nearly 7 years less than that in the United States.
Thus, the typical legal migrant comes from a country where average health is far below that in the United States, but the typical migrant to the United States is much healthier than the typical native-born resident. In our view, this is convincing evidence not only that there is a health selection effect for migrants to the United States, but also that the average magnitude of the health selection effect is very large. For some countries, the presumption must be that health selection is even larger. For example, the average male life expectancy in India is less than 60 years. The typical Indian migrants to the United States would clearly not expect such a life expectancy either in India or in the United States. Table 7-9 also suggests that the extent of health selection varies considerably across sending countries. The real question is whether that variability is systematically related to the factors highlighted in the model outlined in this section.
Progress on this issue has been limited because we typically do not know the health of immigrants at time of first arrival, which is the only time when selectivity can be unambiguously evaluated. Health selectivity involves a com-
parison at the time of immigration between the health of movers and the health of stayers in the sending country; it has nothing directly to do with health of the native born of those in the receiving country.
Table 7-10 attempts to partially remedy this situation by placing the 17 countries listed in Table 7-9 into three groups based on the average male life expectancy in the sending country. Group 1 includes migrants from the five countries with the longest male lifespan, while Group 3 includes migrants from the six countries with the shortest male lifespan. Group 2 includes those from countries that fall between the other groups. This grouping discriminates well among the sending countries in this dimension. Men in Group 2 countries live an average of nearly 5 fewer years than men in Group 1 countries, while those in Group 3 countries live almost 9 fewer years than those in Group 2.
The remaining columns in Table 7-10 measure health outcomes of new legal immigrants to the United States approximately at the time of their arrival. Using the general health status scale, new immigrants from Group 1 countries self-report themselves in much better health than the two other country groups. However, the difference between Group 2 and 3 immigrants is not large (and may even slightly favor Group 3) in spite of the 8-year difference in male life expectancy between them. Moreover, there appear to be very small differences between these three groups in the overall prevalence rates of conditions.7 These data suggest that especially among Group 2 and 3 countries, there is considerably less heterogeneity among new immigrants than there is among health outcomes in the sending countries. This confirms the theoretical prediction that the variance in health among migrants is much smaller than the variance in health in sending countries.
Table 7-11 provides additional evidence on the issue of health selection. Swallen (2002) has computed male life expectancy by ethnic group for the native born and foreign born in the United States. Her data demonstrate
TABLE 7-10 Comparisons of New Legal Immigrants with Life Expectancy in Country of Origin
|
Country of Origin Grouping |
Male Life Expectancy |
% in Excellent or Very Good Health |
% in Fair or Poor Condition |
% with any Chronic Condition |
% with any Serious Condition |
|
1 |
72.3 |
57.1 |
14.1 |
20.6 |
7.0 |
|
2 |
67.5 |
43.4 |
29.4 |
23.9 |
6.4 |
|
3 |
58.7 |
52.9 |
22.1 |
23.4 |
6.9 |
|
NOTE: The three country groupings are based on the list of 17 countries in Table 7-9, ordered by levels of male life expectancy. Group 1 includes the five sending countries that rank highest in male LE while Group 3 includes the six countries that rank lowest in male LE. The health outcome measures in the 3rd through 6th columns are from the New Immigrant Survey-Pilot. |
|||||
TABLE 7-11 Life Expectancies by Nativity
|
|
White male |
Asian male |
Hispanic male |
|||||
|
Age |
U.S born |
Foreign born |
U.S. born |
Foreign born |
Home country |
U.S. born |
Foreign born |
Home country |
|
5 |
68.2 |
66.9 |
73.5 |
74.2 |
65.2 |
68.1 |
70.3 |
67.5 |
|
45 |
30.8 |
31.6 |
35.2 |
35.7 |
29.8 |
31.8 |
34.1 |
32.5 |
|
65 |
15.1 |
15.9 |
15.8 |
18.7 |
14.3 |
16.1 |
18.0 |
17.0 |
|
SOURCES: Data for U.S. born and foreign born are obtained from Swallen (2002). These data are for 1990 life tables. Data for Home Country are immigrant weighted averages of the data contained in Table 7-9. These data are for 2000 life tables. |
||||||||
that within broad ethnic categories, the foreign born have longer life expectancies than the U.S. born and implicitly the foreign born have longer expectancies than residents in the sending countries (by comparison with Table 7-9). This comparison is made more explicit by including immigrant-weighted average life expectancies in the sending countries for Asians and Hispanics. The latter numbers are for calendar year 2000, while the nativity numbers for the United States are for 1990, so the home country numbers are inflated by a few years of mortality improvement compared to the nativity life expectancy (LE) numbers. These comparisons show that for Asian immigrants life expectancies in the United States (at age 5) may be as much as 10 years greater than the average in the Asian sending countries. This must mean that health selection among Asians is very large or that the United States is a much healthier place to live than the typical Asian sending country. Although Asian life expectancies are lower in the second generation, they remain much higher than in the Asian sending countries.
The data in Table 7-11 show that positive health selection also exists among Latino immigrants, but that it is much smaller in magnitude. Adjusting for the secular improvements in mortality, the LE differential between Latino migrants and their home countries is about 5 years. Once again, LE falls in the second generation, but would still remain above the sending countries after adjusting for the secular improvements in mortality.
Migration Model of Subsequent Health Trajectory
The second most prominent subject concerns what happens to immigrants’ health subsequent to their arrival in the United States. The dominant empirical conclusion appears to be that trajectories of immigrant health are less positive than they would have been if they had not migrated. Once again, these findings coexist with little assistance from formal theory, but the usual reasons cited include a less healthy environment in the United
States or the adoption by migrants of the alleged poorer health habits that exist in America.
A useful place to introduce some theory is the health production function—the relationship between various inputs and the stock or commodity “health” (Ht):
(3)
Health in time period t, Ht, is the result of the stock of health in the time period t–1, Ht–1, depreciation, and investments to improve health in the previous time period. Health is produced by several different inputs, including the use and quality of medical care (MCt), the adoption of good personal health behaviors (good diet, exercise), and the avoidance of bad ones (smoking, excessive drinking) (Bt), and a vector of country-specific environmental factors (Et), such as the air pollution level or prevalence rates of contagious diseases.
Education may enter this production function because it affects the way individuals can transform inputs into good health. For example, more educated households may choose more qualified doctors, be more aware of the harmful health effects of behaviors such as smoking or environmental risks, or be better able to provide preventive self-care to prevent illness or to mitigate its more harmful effects. Finally, family background or genetic endowments (Go), which are typically unobserved by the researcher, have played an important role in contemporary research on this topic. For example, Rosenzweig and others have argued that the existence of these unobserved background factors that can often be traced to early childhood may seriously bias estimates of this production function.8
In this framework, health changes over the life course and the trajectory of these changes are the result of the stock of health in the time period t–1, Ht–1, depreciation over the previous time period, and investments to improve health in the previous time period.9 The current inputs and behaviors chosen are investments that produce increments to the stock of health. These inputs, such as the demand for medical care, are “derived” demands: valued not directly but only because of their impact on health. Because the purchase of these inputs or the adoption of health-related behaviors are choices individuals or families can make, they are, in the parlance of economics, “endogenous” variables.
(4)
Equation (4) expresses current health as a function of the price of medical care (Pmc), the price of other inputs (Po), education of each family member (ED), and household income (Yt).
If we let period t–1 be the time of immigration, we can solve equation (4) sequentially to obtain the health trajectory subsequent to immigration. Conditional on health at the point of immigration, this health trajectory is a function of all relevant prices and incomes subsequent to immigration. Solving sequentially
(5)
(where ~ indicates a time series vector of values).
Because equation (5) describes the health trajectory if a person immigrates, the relevant prices, incomes, and environmental factors are those that exist in the United States. There is a corresponding equation that would be obtained if the person chose not to immigrate:
(5’)
(where prices, incomes, and environmental influences are now those that exist in the sending country).
Combined, equations (5) and (5’) suggest that there are several pathways through which health may be altered by immigration. First, higher incomes may promote better health. Jasso et al. (2001) show that the typical economic gain from legal immigration to the United States is large but quite variable across immigrant attributes. For example, the mean economic gain at the time of green card receipt was about $15,000 per year. Economic gains of this magnitude could eventually translate into improved health trajectories. The variability of economic gains suggests similar variability in improved health outcomes.
An advantage of immigrant samples for this issue concerns its ability to separate out the effects of changes in relative and absolute incomes, two quite distinct hypotheses of why income may affect health. Relative income position is thought to affect health by the stress associated with lower hierarchical position, while absolute income may alter health through access to care. Many immigrants may experience a large absolute increase in income while finding themselves at a lower point in the income distribution in the United States than they were in their country of origin. These distinct effects of relative and absolute income position are quite difficult to separate in domestic population samples.
Turning to country-level environmental attributes, equations (5) and (5’) represent a comparison of country-specific attributes that promote or hinder health. Because there are more than 100 different sending countries, it indicates that individual studies such as those of Japanese immigrants are
not capable of being informative about the experiences of other immigrants from other countries or of those who arrived at a different time. A good deal of the emphasis in the Japanese studies rests on the comparative benefits of a Japanese diet or culture over an American one, a comparison that would not carry over to other side-by-side contrasts.
Equations (5) and (5’) also indicate that simple summary statements—such as that living in the United States is bad for immigrant health—are misplaced. Across all the environmental factors that influence health, America is unlikely to rank as either the best or worst health environment. What is more relevant is measuring the specific environmental factors—diet, specific health behaviors, health environment, health care system—that distinguish subsequent health outcomes.
Equations (5) and (5’) raise the fundamental question of what the appropriate counterfactual is. We are interested in a comparison of what happens to an immigrant as he/she stays in the United States compared to what would have happened in the sending country if no migration had taken place. Although often used in the literature, an appropriate counterfactual is not what is happening to the health of a native-born U.S. resident. Rather, the effect on the health of an immigrant changing countries involves a comparison of the health trajectory of an immigrant in the receiving country with the health trajectories of “similar” people in the sending countries.
Equations (5) and (5’) do not represent a complete characterization of the problem, which has a form similar to that developed by Willis and Rosen (1979), where individuals now self-select as migrants or nonmigrants. The migrant selection rule was described in equations (1) and (2), earlier illustrating that although often discussed separately, health selection and subsequent health trajectories are not orthogonal processes. Current and perhaps expected future health profiles influence the decision to migrate so that migrants are not a random sample of the population at risk either in terms of their current health or its expected trajectory.
Finally, health selection is not independent of the subsequent health trajectory. To this point we have modeled selection in a cross-section. But consider a sending country with the exact same distribution of health as that which exists in the United States. In our theoretical model (supported by the empirical facts to follow), immigrants of working age still should be quite positively selected on their health—so we see very low rates of serious illness (heart disease, cancer, diabetes, and the like) among new immigrants to the United States. But because you can only self-select based on something you know about or at least suspect, differences in health outcomes of immigrants and the native born in onset of disease 10 or 20 years after immigration should show much smaller differences, or maybe none at all. Therefore, by a simple process of regression toward the mean, disease rates of the foreign born will necessarily converge to the U.S. norm. For a similar reason, the
health of the second generation will tend to fall relative to the first generation. A good deal of the current literature interprets a decline in immigrant health, with length of stay or across generations as indicative of problems in American health environments.10 But all it may be is the necessary consequence of strong health selection effects and regression toward the mean.
THE HEALTH OF NEW LEGAL IMMIGRANTS
In this section, we present results obtained from the New Immigrant Pilot Survey (NIS-P), a panel survey of a nationally representative sample of new legal immigrants. These legal immigrants were admitted to legal permanent residence to the United States during the months of July and August of 1996 (for details, see Jasso, Massey, Rosenzweig, and Smith, 2000). This sample was based on probability samples of administrative records of the U.S. Immigration and Naturalization Service (INS) representing all those who received their green cards during those months. The NIS-P links survey information about immigrants’ pre- and postimmigration labor market, schooling, health, and migratory experiences with data available from INS administrative records, including the visa type under which the immigrant was admitted. The NIS-P consists of a baseline survey, a 3-month follow-up of half of the original sample (to evaluate whether periodicity affected attrition), a 6-month follow-up of all original sample members, and a 1-year follow-up, also of all original sample members.11
Given the brief 15-minute telephone interviews, the health information collected in the NIS-P was limited—largely self-reported general health status, the prevalence of selected chronic conditions, some health behaviors, the utilization of medical services, and how that care was paid. Yet, even this limited health information proves to be quite valuable. The reason is that the problems that plagued monitoring the economic success of new legal immigrants also have affected current research findings on immigrant health. These problems include the lack of any true national representative samples and the inability to follow this appropriate sample over time.
Table 7-12 lists the distribution of self-reported health status of these new legal immigrants alongside distributions for the native born obtained in the same year from the NHIS. Using this index, once again the health of new legal immigrants to the United States is generally quite good. Fewer than one in seven report themselves as being in fair or poor health. If we compare all adult immigrants to native-born Americans, the data indicate that the only noticeable difference that emerges takes place among older immigrants. This age pattern among legal immigrants is additional evidence that the nature of health selection is very different among older immigrants.
Table 7-13 lists rates of chronic conditions for respondents in the NIS-P. To examine the possibility that any disparities with the native born are
TABLE 7-12 Health Status of New Legal Immigrants and the U.S. Native Born
|
|
NIS |
1996 NHIS: Born in U.S. |
||||
|
All |
25-44 |
50+ |
All |
25-44 |
50+ |
|
|
Excellent or very good |
59.6 |
66.2 |
29.9 |
62.4 |
71.2 |
46.8 |
|
Good |
26.8 |
26.9 |
27.7 |
25.1 |
21.5 |
30.9 |
|
Fair or poor |
13.6 |
7.0 |
42.5 |
12.5 |
7.3 |
22.3 |
|
# of observations |
972 |
588 |
127 |
34,061 |
16,024 |
13,105 |
|
SOURCES: New Immigrant Pilot Survey and born in the United States from 1996 NHIS. |
||||||
due to age, rates are also listed for those 25 to 44 years old and for those over age 50. To provide a benchmark, the middle three columns provide rates for native-born Americans from the 1996 NHIS and the last three columns for those who said they had arrived within the past 5 years. The latter group is most similar to respondents in the NIS-P in terms of duration of stay in the United States, but will include, in addition to legal immigrants, nonimmigrants (e.g., students, those on temporary visa) and illegal immigrants. Reported rates of chronic conditions of new legal immigrants are quite low, especially compared to the native born. Among the younger sample (those between ages 25 and 44), these differences are particularly large in the more severe conditions. For some diseases such as hypertension and diabetes, health selection may actually reverse among older, new legal immigrants.
It is sometimes argued that these low rates of chronic conditions among the foreign-born population simply reflect the lower degree of contact with doctors and hospitals. Without such contact, a condition would not be diagnosed. To check this possibility, we look in Table 7-14 at rates conditional on having seen a physician or having been hospitalized during the past year. In fact, rates of contact with Western medicine among new legal
TABLE 7-13 Rates of Chronic Conditions of New Legal Immigrants
|
|
NIS |
Native Born |
0-5 |
||||||
|
All |
25-44 |
50+ |
All |
25-44 |
50+ |
All |
25-44 |
50+ |
|
|
Hypertension |
10.8 |
4.6 |
40.6 |
16.9 |
6.0 |
33.3 |
6.3 |
1.4 |
31.6 |
|
Diabetes |
2.5 |
0.6 |
13.3 |
4.1 |
1.5 |
8.9 |
1.4 |
0.0 |
3.4 |
|
Cancer |
0.7 |
0.6 |
1.8 |
2.3 |
0.6 |
5.9 |
0.2 |
0.1 |
1.3 |
|
Lung disease |
1.9 |
1.4 |
4.6 |
9.7 |
4.1 |
12.4 |
2.1 |
2.0 |
0.0 |
|
Arthritis |
7.4 |
3.1 |
27.3 |
16.9 |
6.3 |
36.3 |
5.3 |
3.1 |
21.4 |
|
Heart disease |
3.0 |
1.0 |
15.1 |
8.9 |
5.9 |
19.9 |
3.7 |
0.0 |
19.9 |
|
Asthma |
3.4 |
2.8 |
3.6 |
5.4 |
6.0 |
5.0 |
1.1 |
1.3 |
0.0 |
|
SOURCES: Native born and 0-5 from NHIS and from New Immigrant Pilot Survey. For number of observations, see Table 7-12. |
|||||||||
TABLE 7-14 Prevalence Rates of Chronic Conditions for Those Who Saw a Doctor or Were Hospitalized During the Past Year
|
|
25-44 |
50+ |
||
|
0-5 Years |
U.S. Born |
0-5 Years |
U.S. Born |
|
|
Hypertension |
3.9 |
7.7 |
38.1 |
35.7 |
|
Diabetes |
1.4 |
1.9 |
7.1 |
10.2 |
|
Cancer |
0.2 |
0.8 |
1.1 |
6.7 |
|
Lung disease |
2.7 |
10.4 |
4.7 |
13.2 |
|
Arthritis |
3.2 |
7.3 |
31.2 |
40.1 |
|
Heart disease |
2.7 |
6.1 |
23.9 |
26.1 |
|
Asthma |
2.3 |
5.9 |
1.4 |
5.3 |
immigrants are quite high; 62 percent of the new legal immigrants said they had seen a doctor during the past year. Even among those who had such contact, reported rates of chronic conditions are much lower among new immigrants than among the native born. This indicates that this source of reporting bias may not be able to explain the better health of immigrants.12
This comparison with native-born Americans hides the far more interesting story about the considerable variation in health that exists among immigrants. One dimension of that diversity concerns the countries from which they came. These data are listed for general health status in panel A of Table 7-15 and for the more important chronic conditions in panel B of
TABLE 7-15 Diversity of Immigrant Health Outcomes by Place of Last Residence
|
A. Self-Reported Health Status |
|||
|
Place of origin |
Excellent or Very Good |
Good |
Fair or Poor |
|
Europe |
52 |
30 |
19 |
|
South America |
69 |
18 |
13 |
|
Asia |
57 |
29 |
14 |
|
Africa |
70 |
29 |
1 |
|
Mexico |
49 |
34 |
16 |
|
Other North America |
74 |
16 |
10 |
|
B. Prevalence Rates of Selected Chronic Conditions |
|||
|
Place of origin |
Hypertension |
Arthritis |
Diabetes |
|
Europe |
17.4 |
12.0 |
3.7 |
|
South America |
8.5 |
4.6 |
3.0 |
|
Asia |
5.5 |
6.6 |
1.4 |
|
Africa |
9.5 |
2.4 |
2.4 |
|
Mexico |
11.0 |
7.1 |
4.8 |
|
Other North America |
13.5 |
6.2 |
1.0 |
|
SOURCE: New Immigrant Pilot Survey. |
|||
the same table. While nearly three quarters of immigrants from North America (except Mexico) are in excellent or very good health, this fraction drops to about half among Europeans and Mexicans. A similar degree of heterogeneity holds when we examine type of visa. For example, hypertension is particularly common among Europeans (about 1 in 6) and much more rare among new Asian migrants (about 1 in 20).
Another dimension of this heterogeneity exists by visa category. This dimension is important because visa status—the legal reason why an immigrant was allowed into the United States—is one of the principal policy levers that can be used to change the types of immigrants who arrive. The A panel of Table 7-16 lists the distribution of self-reported health status by the major categories of admission to legal status in the United States. The health of immigrants in the two largest visa categories—employment and spouses of U.S. citizens—is generally excellent and much better than that of the typical native-born American (see Table 7-1). The situation is not as sanguine in the other groups listed in this table. To illustrate, the other immigrant visa category where individuals qualify through marriage—spouses of permanent resident aliens—report themselves in much poorer health than those people who married U.S. citizens. However, one group of immigrants stands out in terms of their relatively bad health status—refugees and asylees. Shortly after the time of their green card receipt, one-third of refugees self-report as being in fair or poor health.
Panel B of Table 7-16 illustrates this diversity by visa status by listing prevalence rates for the more common chronic conditions. As before,
TABLE 7-16 Diversity of Immigrant Health Outcomes by Visa Status
|
A. Self-Reported Health Status |
|||
|
Visa status |
Excellent or Very Good |
Good |
Fair or Poor |
|
Principal employment |
76 |
18 |
6 |
|
Spouse of U.S. citizen |
74 |
20 |
6 |
|
Spouse of permanent resident |
51 |
37 |
14 |
|
Diversity |
46 |
38 |
17 |
|
Refugee or asylee |
38 |
30 |
32 |
|
B. Prevalence Rates of Selected Chronic Conditions |
|||
|
Visa status |
Hypertension |
Arthritis |
Diabetes |
|
Principal employment |
5.3 |
4.2 |
0.5 |
|
Spouse of U.S. citizen |
4.8 |
4.0 |
0.0 |
|
Spouse of permanent resident |
9.7 |
4.8 |
3.2 |
|
Diversity |
14.6 |
4.1 |
4.2 |
|
Refugee or asylee |
25.3 |
17.7 |
5.1 |
|
SOURCE: New Immigrant Pilot Survey. |
|||
chronic conditions vary across types of immigrants. In every single visa category, prevalence rates are smaller—and often considerably smaller—among new immigrants. For example, a quarter of all refugees and asylees have hypertension, while nearly one in five were diagnosed with arthritis. The ability of such data to isolate health problems of some immigrants by a known characteristic may turn into an important public health tool in targeting health interventions.
To this point, our data on the health status of new legal immigrants has concentrated on when they arrived. The question of what happens subsequently has absorbed much recent research on immigrant health. Most scholarship in this field argues that on average, immigrant health actually deteriorates with length of stay in the United States. The reasons for this relative deterioration are debated, but there is general acceptance that living in the United States may not be all that good for your health.
The difficulty with the “years” is that we do not have good national data that track immigrants over time. Although the NIS-P only monitors health changes over a short period of about a year, these early years may be a critical time in health evolution. The “all” row in Table 7-17 examines changes in self-reported health status for the full NIS sample. Contrary to the widespread view, on average immigrant health actually improved during the first year of the survey. For example, at the time of the 6-month interview, 18 percent of respondents reported themselves in fair or poor health. Roughly 9 months later, only 14 percent reported the same status.
There are two main hypotheses about our two salient findings: First, immigrant health is better than that of native-born Americans, and second, it actually improves over time. The explanations generically fall into two
TABLE 7-17 Short-Run Changes in Health Status
|
|
Initial |
Final |
||||
|
Excellent or Very Good |
Good |
Fair or Poor |
Excellent or Very Good |
Good |
Fair or Poor |
|
|
All |
56 |
26 |
18 |
59 |
27 |
14 |
|
Saw doctor |
||||||
|
Yes |
56 |
25 |
19 |
60 |
26 |
14 |
|
No |
66 |
28 |
16 |
70 |
28 |
12 |
|
Place of origin |
||||||
|
Asia |
53 |
24 |
23 |
54 |
29 |
14 |
|
Europe |
54 |
28 |
19 |
52 |
30 |
18 |
|
South America |
63 |
23 |
13 |
71 |
17 |
10 |
|
Other North America |
63 |
25 |
13 |
74 |
16 |
10 |
|
Mexico |
42 |
38 |
19 |
49 |
34 |
16 |
camps. The first explanation is that it is a real phenomenon and immigrants are much healthier. Just as immigrants were highly selective on other traits, this explanation claims that immigrants are selective on their health. In part, this health selectivity may result from medical screening exams given prior to entry, although there is some legitimate question about how rigorous those exams are. More importantly, immigrants may self-select themselves on their health.
One explanation for this improvement is that it results from reporting biases, of which three are often mentioned. The first reporting issue relates to language—the effect of limited English-language ability and changes in that ability over time. Some immigrants may not fully understand the question and as their language ability improves, they report health improvements even though no change has occurred. To examine this possibility, the next row in Table 7-17 examines only immigrants whose English ability was very good when they arrived and did not change. Even in this sample where language is good and unchanging, health status got better over time. The second reporting bias concerns contact with Western medical diagnosis. The next two rows in Table 7-17 list changes in health status by whether or not the respondent had seen a health care provider in the past year. Once again, short-run improvements in health appear to exist independently of physician contact.
The third type of reporting bias involves the reference comparison implicitly being made. If a person says his or her health is very good, the natural question is compared to whom? This is a particularly salient issue for immigrants, whose reference group may be changing with the very act of migration. For example, if an immigrant comes from a place where the average health is much worse than in the United States, he or she may downgrade this evaluation when he or she begins to discover that average health is much better in the United States. A symmetric argument holds for places where average health is above that in the United States. One way of testing this hypothesis is to examine changes across place of origin. The final rows in this table do exactly that. Health status improves across all countries of origin. Moreover, there does not appear to be any relation of health change to whether one arrives from a place where the average health was either low or high. The arguments were not meant to imply that reporting biases in health do not exist. However, these biases appear not able to explain the principal health patterns observed for immigrants. In general, immigrant health is quite good and it appears to improve over time, at least in the short run.
EMPIRICAL MODELS OF HEALTH SELECTIVITY AND HEALTH TRAJECTORIES
In this section, we present new empirical models estimating the determinants of health selectivity of migrants to the United States. and short-run health changes subsequent to immigration. Both models rely on data obtained from the New Immigrant Pilot Survey, which was described in detail in the previous section. We first present our analysis of health selectivity of migrants and conclude this section with a simple model of short-run health changes following immigration. The basic idea behind these analyses is that skill and health are complements—those factors that induce more skilled immigrants to emigrate to the United States also induce healthier immigrants. Skill and health go together for two reasons. First, those immigrants with more skill have higher incomes and thus can “purchase” better health, a proposition we will test directly based on the change in income of the immigrants. Second, those who tend to invest in human capital do so with respect to both investments in health and in labor market skills.
Health Selectivity of Immigrants
The theoretical model in an earlier section highlighted some central factors that should influence both the skill and health selectivity of immigrants. The parallel nature of the predictions for skill and health argues for the estimation of models of both outcomes at the same time with the same set of covariates. Therefore, to carry out an analysis motivated by the theoretical framework discussed earlier, we focus on the home country earnings and health outcomes of adult immigrants aged 21 through 64 who obtained visas as employment immigrants or as spouses of U.S. citizens or U.S. permanent resident aliens. We chose these categories principally because such immigrants are able to immigrate without having a blood relative in the United States—a very different kind of selection effect than the one that concerns us here. This nonnepotistic immigration is thus an option for all individuals born and residing outside the United States. In contrast, the left-out group is very heterogeneous, including refugees, parents, and adult unmarried children. In addition, we select people within this working-age group (ages 21 to 64) because the data presented earlier indicate that the health selection process is quite different for older immigrants.
We examine two outcomes that address the selectivity of immigrants—their last earnings in the sending countries and their self-reported health status indexed by an ordinal five-point scale ranked from excellent to poor. We use the immigrant’s earnings in his or her home country rather than the U.S. wage because the former is not affected by possibly imperfect skill
transferability. A unique feature of the NIS-P is that it provides information on the earnings of the immigrants in their last job before coming to the United States. More than 77 percent of the immigrants had worked in a foreign country in the 10 years prior to the survey. We converted the earnings in the last job abroad, provided by the immigrants in native currency units, to dollar amounts based on estimates of the country-specific purchasing power of the currencies from the Penn International Comparisons Project, described by Summers and Heston (1991). These conversion factors are explicitly designed to take into account differences in the “cost of living” across countries and to avoid the distortions associated with exchange rate regimes in order to facilitate cross-country comparisons. Table 7-18 contains our estimated models for these two outcomes—Generalized Least Squares (GLS) estimation for the ln of purchasing power parity (PPP)-full time earnings in the sending country and ordered logit estimation for the self-reported health index (scaled from 1 = excellent to 5 = poor). This scale is used to parallel work where mortality is the health outcome.
Our basic migration model with worker skill heterogeneity and country skill-price differentials implies that high skill-price countries will send fewer but more skilled and healthier immigrants. How can we measure variation across countries in skill prices? In terms of the observable correlates of skill prices, among workers residing in countries with the same output per worker, those workers residing in countries where workers have higher average skill levels receive lower skill prices, while among workers in countries with the same average worker skill levels, those in countries with higher output per worker will receive higher skill prices. Given immigrant skill heterogeneity and selectivity due to home country skill-price variation, these results imply that immigrants from countries with high output per worker and with low average levels of schooling will have the highest skill levels and best health among immigrants with identical own schooling levels.
To measure skill prices in accordance with the model, we used the real (PPP-converted) Gross Domestic Product (GDP) per worker estimates from the Penn World Table, Mark 5.6 supplemented with updated 1995 estimates from the ICP, and estimates of the average schooling levels of the population aged 25 and over in origin countries from Barro and Lee (1993). Average schooling estimates are available for a large but not complete subset of countries for which there are PPP GDP estimates. For those countries for which there are no schooling stock estimates, we constructed a variable indicating that schooling was missing and set the schooling variable to zero. Similarly, home country average health is indexed by female life expectancy, with an indicator variable for the few countries for which we were unable to obtain a value.
TABLE 7-18 Determinants of Log of Immigrants’ Home Country Earnings and Health Status
|
Sample |
Home Country Earners |
Health Status from Excellent (1) to Poor (5) |
|
Variable/Estimation Procedure |
GLS |
Ordered Logit |
|
Home country characteristic |
||
|
Ln (real GDP/worker) |
1.27 (7.71)* |
–.4329 (1.92) |
|
Ln (average schooling in years) |
–0.91 (2.55) |
0.6527 (1.85) |
|
Distance to closest U.S. port of entry (miles × 10–4) |
0.157 (0.42) |
0.429 (0.68) |
|
Border country |
–0.258 (1.22) |
1.014 (2.93) |
|
U.S. military base |
–0.0751 (0.31) |
0.4748 (1.51) |
|
English an official language |
0.719 (3.89) |
–1.138 (3.44) |
|
Schooling missing |
–1.00 (1.76) |
1.607 (2.17) |
|
Ln life expectancy |
0.372 (0.42) |
–3.197 (2.11) |
|
Life expectancy missing |
2.088 (0.42) |
–12.73 (1.91) |
|
Characteristic of worker |
||
|
Schooling (years) |
0.0441 (2.79) |
–0.0788 (2.94) |
|
Years in the United States |
0.1237 (1.43) |
–0.0221 (0.17) |
|
Years in the United States squared |
–0.0182 (1.86) |
0.0051 (0.41) |
|
Age |
0.0763 (2.17) |
–0.0367 (0.64) |
|
Age squared |
–0.00061 (1.52) |
0.0009 (1.29) |
|
Year last worked in home country |
0.0464 |
— (2.42) |
|
Female |
–0.114 (0.90) |
0.0620 (0.30) |
|
Visa |
||
|
Spouse of U.S. citizen |
–0.575 (3.13) |
0.2551 (0.85) |
|
Spouse of U.S. permanent resident alien |
–0.331 (1.11) |
1.728 (4.17) |
|
Spouse of employment immigrant |
–0.393 (2.24) |
0.1599 (0.55) |
|
Constant |
(1.87) –9.53 |
|
|
Number of immigrants |
342 |
327 |
|
Number of countries |
58 |
|
|
Adjusted R2 |
0.445 |
0.1065 |
|
*Absolute value of t-ratio adjusted for country cluster effects in parentheses in column. |
||
We have several measures related to the costs of immigration. The first is whether the immigrant is from a border country to the United States (Mexico or Canada), while the second variable is the distance of the origin country’s capital to the closest major entry city in the United States. The third is an indicator variable taking on the value of one if the country was a host to a U.S. military base in the 5 years preceding the NIS-P survey. Military bases are enclaves of U.S. citizens abroad, many of whom are young and single so that the cost of obtaining entry by marrying a U.S. citizen is lower. The selection framework suggests that countries with military bases, border countries (Mexico and Canada), and countries generally not located at great distances from the United States have lower U.S. immigration barriers or costs and should, given skill prices, be disproportionately sending countries for low-skill and less healthy immigrants.
Worker attributes included in these models include own schooling measured in years, number of years in the United States because some of these immigrants obtained their green cards while living in this country, a quadratic in age, sex (an indicator variable set to one for women), and the year last worked in the home country (for the home country earnings equation model only). In addition, three indicator variables for type of visa are included: whether the immigrant obtained a visa as a spouse of a U.S. citizen, a spouse of a permanent resident alien, or a spouse of a principal employment visa immigrant.
In column 2 of Table 7-18, we report GLS estimates of ln (national log) home country earnings in a model that includes the country-specific skill price determinants—the log of real GDP per worker and the log of the average schooling of workers—and the individual worker’s individual observable skill attributes. A parallel ordered logit model for self-reported health status is listed in the third column. These specifications also include visa category variables, geographic proximity variables, and years of U.S. residence as determinants of home country earnings to assess how earnings and health selectivity can obscure interpretations of the determinants of the U.S. earnings and health of immigrants. Because the geographic location of a country relative to the United States, the U.S. visa status of an immigrant, and his or her U.S. experience are unlikely to have direct effects on home country earnings or health, the coefficients on these variables mainly reflect selectivity.
In conformity to the model, the coefficient on the log of per-worker country output is positive for home country earnings and negative for our health index (with poor health at the top of this index). Similarly, the sign of the coefficient on the measure of average worker skill in the country is negative for ln earnings and positive for health status. Combined, these results indicate that immigrants from countries with high skill prices are, as predicted, positively selected both on their skill and their overall health.
Not surprisingly, immigrants from countries where the average health status is better (as measured by average life expectancy) are healthier. These effects are not quantitatively trivial. For example, a doubling of GDP/ worker (holding everything the same), which is equivalent to a doubling in the skill price, would increase the proportion of immigrants in “excellent” health by 20 percent and reduce the proportion in “fair” health by 25 percent. Similarly, a much smaller 10 percent increase in the price of skill increases the proportion of immigrants in “excellent” health by 3 percent and reduces the proportion in fair health by 4 percent.
In contrast, there appears to be no relation between country-specific average life expectancy and home country earnings. This may reflect two offsetting forces. First, average life expectancy is correlated with own health, which should increase earnings. But in the formulation in Table 7-18, average life expectancy also is a (negative) proxy for unobserved skill prices, which should reduce earnings.
There are several measures of the cost of immigration included in these models. A simple measure of geographic distance does not matter in either equation, perhaps because the distance to the nearest point of entry may not be the most relevant measure given the existence of ethnic enclaves in the United States. In contrast, other things equal, immigrants from the two border countries (Canada and Mexico), where the cost of migration is presumably less, send less skilled and less healthy migrants to the United States. We also estimate poorer health status among migrants from countries with military bases, although this effect is not statistically significant at conventional levels.
With respect to effects of personal attributes, our estimates support the conventional finding that own schooling is positively associated with both last home country earnings and with self-assessed health status. Both estimates are statistically significant. The interpretation of the coefficient on U.S. experience is not whether increased time in the United States increases or decreases home country earnings, because home country earnings are measured prior to coming to the United States. Rather, this variable should be interpreted as measuring whether immigrants, of given age, who came to the United States earlier have higher or lower levels of skills. Our results indicate no statistically significant effect of time in the United States on home country earnings.
This interpretation is not possible for health status, which is measured instead after arrival in the United States. However, because our results will indicate that health status improves after arrival in the United States, our estimate of a zero net effect of U.S. experience on health in Table 7-18 may indicate that those who come to this country earlier also had worse health on average.
Visa status also captures some aspects of immigrant selection. All effects are estimates compared to the left-out group—those who obtained
principal employment visas. Although spouses of U.S. citizens and spouses of those who obtained principal employment visas appear to be negatively selected on their labor market skills, there does not seem to be any selectivity on their health status. In contrast, spouses of permanent resident aliens are in significantly poorer health than immigrants on employment visas.
In sum, the results in Table 7-18 indicate that there exists systematic variation in the skill and health selectivity of immigrants to the United States that in large part conforms remarkably well with the theoretical predictions outlined earlier. In particular, the country-specific factors that positively select on the skills of new immigrants also appear to positively select on their health status. The results imply that increases in the price of skills in countries outside the United States, a common result of economic development, will lead to a more skilled and healthier immigrant population in the United States.
Short-Run Health Trajectories
Although it receives almost no mention in the existing literature on health trajectories, one of the biggest changes attributable to immigration is a very large income gain (Jasso et al., 2001). To the extent that income is an important determinant of health status, there is reason to believe that the economic gains of immigrants can result in health improvements. In this section we use new data on immigrants to examine how economic gains from immigration affect health change. Because long-term panel data that follow immigrants from the start of their immigration process are simply not available, estimating models of health change subsequent to immigration is difficult. Once again a data source that offers some potential for examining health change is the New Immigrant Pilot Survey. The random sample of new legal immigrants of the NIS-P was followed up at three subsequent waves. Self-assessed health status, rated from excellent to poor, was reported by all respondents at the 6-month and 12-month interviews, which were actually about 9 months to 1 year apart. In this analysis, we examine changes in self-reported health status ranked as improved, stayed the same, and deteriorated, again using an ordered logit model. We can think of this model as a fixed effects equation. For example, suppose that health is a lagged function of income and other fixed traits (such as schooling, visa, country of origin attributes). Because we have health and income at two points in time, differencing gives the change in health as a function of the lagged change in income. Age is added to the model to capture nonlinearities in age.
Our results are reported in Table 7-19. The main explanatory variable is the economic gain from immigration—the difference between the earnings received in the United States and amount earned in the last job in the
TABLE 7-19 Ordered Logit of Whether Self-Reported Health Status Improved, Stayed Same, or Deteriorated
|
|
Coefficient |
Z |
|
Economic gain |
0.0716 |
3.23 |
|
Age |
–0.0189 |
1.23 |
|
Cut 1 |
–2.3600 |
|
|
Cut 2 |
0.3231 |
|
sending country. To make earnings in different countries as comparable as possible, as explained earlier, all sending country earnings are adjusted for purchasing power parity. The size and variability of the economic gain from immigration is not trivial. According to the estimates contained in Jasso et al. (2001), the mean economic gain from immigration was about $21,000, around which there was enormous variability. Moreover, the results in Table 7-19 indicate that the income gain associated with immigration positively affects health, so that big gainers are more likely to have subsequently improved health.
Recognizing the real possibility of dual causality, one should be cautious about any interpretation dealing with the relation between health and income (Smith, 1999). But given the magnitude of the gains in income due to immigration, it would be difficult to argue that health changes associated with immigration “caused’ these income changes. Most important, the results in Table 7-19 add more reasons for some skepticism about the widely held view that health will decline due to immigration. The impact on one’s health of living in a particular place is probably slow and cumulative, and the results in Table 7-19 only measure short-run changes. However, these economic gains at the time of immigration are unlikely to dissipate over time; in fact, the evidence shows that they will most likely expand over time (Jasso et al., 2001). Thus, even though the model estimated in Table 7-19 only predicts short-run health changes, the persistence of these large economic gains over the long term makes one suspect that on this mechanism at least health improvements might also persist. There is a vast literature spanning several disciplines that argues that income strongly promotes improved health. Why the force of this literature is ignored when the topic shifts to immigration is an interesting question.
RECOMMENDATIONS ON RESEARCH PRIORITIES AND FUNDING
There are several recommendations for research priorities and funding that are suggested by the findings in this chapter. First, the data have highlighted the enormous heterogeneity that exists within the foreign-born
population. This heterogeneity appears in many dimensions, and immigrant health is certainly no exception. The most direct implication of this heterogeneity is that researchers need data with larger sample sizes of immigrants so that they can conduct country-specific analyses. The current, prominent national social science surveys contain immigrant samples as an addendum, roughly in proportion to their role in the overall population. Consequently, sample sizes for even the larger individual immigrant groups are often severely inadequate for meaningful analysis on the topic of immigrant health. If processes of health selection and acculturation vary across immigrant groups, our current data would not be able to detect either for many ethnic groups.
Second, it is essential that surveys be designed that capture immigrants at the start of the immigrant process. There are several key advantages to such a design. It allows one to more accurately access the extent of health selectivity at the time of immigration, before the environment in the receiving country has had any significant impact on the immigrant’s health. It also permits an assessment of subsequent health trajectories from the beginning of the immigration process. Currently available immigrant samples are, at best, representative samples of the currently resident foreign-born population—those members of past immigrant cohorts who remained in the United States. Because we know little about the nature of the health selection of those who emigrated, it is impossible to deduce what health trajectories were for the typical immigrant. The New Immigrant Survey is an important step in the direction of obtaining a sample of immigrants at the beginning of a well-defined point—the receipt of a green card—and following all members of that cohort, whether or not they subsequently emigrated.
Third, in order to investigate the principal unanswered questions about immigrant health, it is necessary to integrate health, economic, social, and demographic measures within a single survey. Although they are quite useful for documenting health disparities, traditional health surveys such as NHIS or the National Health and Nutrition Environmental Survey are not ideal vehicles for understanding root causes because their measures of the economic, social, and demographic environment are quite limited. Similarly, current economic and demographic surveys are too narrow in the scope and depth of the health information they contain. These new surveys must also incorporate measures of the principal pathways that affect health trajectories. Such measures would include diet, income, and cultural support networks. Finally, it would be quite desirable to supplement observational health measures with physical measurements of health conditions.
Fourth, studies of the health outcomes of immigrant children and the children of immigrants also merit high priority on the research agenda. Such research adds an intergenerational component that speaks to possible
alternative pathways of health acculturation across generations. Because the outcomes of children are closely tied to the behaviors and constraints faced by their immigrant parents, it is important to include children in the same surveys as their parents. These children are the eventual future legacy of immigration so understanding the determinants of their health addresses the issue of the long-term impact of immigration on the health of the American population.
Fifth, an important insight from the epidemiology literature is that investigations of specific diseases can help elucidate the pathways through which immigration affects health. For example, models that emphasize the impact of psychosocial stress associated with the process of immigration often see the main manifestations of this stress showing up later in diseases of the heart. Similarly, exposures to certain environmental or behavioral risks such as smoking may lead to increased risks of cancers or other diseases of the lung. Consequently, it is important to be able to track specific disease progressions of immigrants that can then be contrasted to those that characterize their native-born counterparts.
Sixth, the subject of immigrant health argues for the value of comparable international comparison studies. One of the arguments in favor of studies of immigrant health is that the diversity of health environments represented by the many sending countries offers an important analytical tool for studying effects of geographical environment on health. A similar agreement can be made about the receiving countries. The United States is not a unique country in terms of its position as an immigrant-receiving nation, and the considerable diversity among receiving countries will also provide much useful information.
Conclusions
In this chapter, we have explored some salient issues concerning immigrant health. Ethnic health disparities are inherently linked to immigration because ethnic identities often are traced to the country of origin of one’s immigrant ancestors. Two of the central questions that have dominated the medical and social science literature on immigrant health are the central focus of this chapter. These issues involve the magnitude and mechanisms shaping health selectivity and the determinants of health trajectories following immigration. Health selection—the propensity of immigrants to be much healthier than a representative person in the sending country—is a quantitatively important phenomenon that is fundamental to understanding the most basic patterns that emerge about immigrant health. Immigrants are quite healthy and are very positively selected on this trait. However, great diversity exists among immigrants in the extent of health selection. In addition, the nature of health selection of immigrants appears
to be fundamentally different among older immigrants, who have largely passed their prime working years. As part of this chapter, we also developed a theoretical model that attempts to explain the diversity in health selection among immigrants.
One of the consequences of this strong health selection effect is that it makes current evidence of health trajectories following immigration very problematic. For example, the general theme in the literature appears to be that immigration to the United States may have deleterious health consequences. However, this pattern is also easily explained simply by positive health selection on currently observed health traits and outcomes and then the subsequent necessary regression toward the mean. Research on health trajectories following immigration also frequently suffers from some confusion on what the appropriate comparison group should be. The issue is what an immigrant health profile is following immigration compared to what it would have been if he or she did not migrate. Comparisons that have dominated the existing literature that rely principally on how immigrants fare relative to native-born populations do not directly speak to the issue of the effects of immigration on lifetime health profiles.
ACKNOWLEDGMENT
Paper prepared for National Academy of Sciences Conference on Racial and Ethnic Disparities in Health. This research was supported by grants from the National Institutes of Health.
ENDNOTES
REFERENCES
Banks, J., Kapteyn, A., Smith, J.P., and Van Soest, A. (2004, February). International comparisons of work and disability. Paper presented at NBER conference on disability, Charleston, South Carolina.
Barro, R., and Lee, J.W. (1994). International comparisons of educational attainment. Journal of Monetary Economics, 32(December), 363-394.
Centers for Disease Control and Prevention. (2001). Health: United States: 2001 with urban and rural health chartbook. Hyattsville, MD: National Center for Health Statistics.
Grossman, M. (1972). The demand for health: A theoretical and empirical investigation. New York: National Bureau of Economic Research.
Jasso, G., Massey, D., Rosenzweig, M., and Smith, J.P. (2000). The new immigrant pilot survey (NIS): Overview and findings about U.S. immigrants at admission . Demography, 37(1), 127-138.
Jasso, G., Rosenzweig, M., and Smith, J.P. (2001). The earnings of U.S. immigrants: World skill prices, skill transferability and selectivity. Unpublished manuscript.
Kasl, S.V., and Berkman, L. (1983). Health consequences of the experiences of migration. Annual Review of Public Health, 4, 69-90.
King, G., Murray, C. Solomon, J., and Tandon, A. (2003). Enhancing the validity and cross-cultural comparability of measurement in survey research. American Political Science Review, 98(1), 567-583.
Kitagawa, E., and Hauser, P. (1973). Differential mortality in the United States: A study in socioeconomic epidemiology. Cambridge, MA: Harvard University Press.
Marmot, M.G., and Syme, S.L. (1976). Acculturation and coronary heart disease in Japanese-Americans. American Journal of Epidemiology, 104(3), 225-247.
Marmot, M.G., Adelstein, A.M., and Bulusu, L. (1984). Lessons from the study of immigrant mortality. Lancet, 2, 1455-1457.
National Research Council. (2002). Emerging issues in Hispanic health: Summary of a workshop. Center for Social and Economic Studies, Committee on Population, Commission on Behavioral and Social Sciences and Education. Washington, DC: National Academy Press.
Smith, J.P. (1999). Healthy bodies and thick wallets: The dual relation between health and economic status. Journal of Economic Perspectives, 13(2), 145-167.
Smith, J.P., and Edmonston, B. (1997). The new Americans: Economic, demographic, and fiscal effects of immigration. Washington, DC: National Academy Press.
Summers, R., and Heston, A. (1991). The Penn World Table (Mark 5): An expanded set of international comparisons, 1950-1988. Quarterly Journal of Economics, 106, 327-368.
Swallen, K.C. (2002). Mortality in the U.S.: Comparing race/ethnicity and nativity. Unpublished manuscript, University of Wisconsin.
Vega, W., and Amaro, H. (1994). Latino outlook: Good health, uncertain prognosis. Annual Review of Public Health, 15, 39-67.
Willis, R.J., and Rosen, S. (1979). Education and self-selection. Journal of Political Economy, 87(5), S7-S37.








































