11
What Makes a Place Healthy? Neighborhood Influences on Racial/ Ethnic Disparities in Health over the Life Course
Jeffrey D. Morenoff and John W. Lynch
Our main purpose in this chapter is to suggest a conceptual framework for better understanding how characteristics of neighborhoods can affect racial/ethnic differences in health, with a special emphasis on health in aging populations. At the outset we should recognize that the specific studies in this field are sparse. However, we will try to draw from the more diverse sociological and epidemiological literature on neighborhoods and health to illustrate the potential for certain characteristics of neighborhoods to affect racial/ethnic health differences in aging.
In recent years, epidemiologists and sociologists have become increasingly interested in studying the effects of local context on individual health and well-being. Although a long history of research shows that health status varies strongly across local, state, regional, and national settings (Murray, Michaud, McKenna, and Marks, 1998), what distinguishes the new generation of research on neighborhoods and health is its attention to investigating the multilevel causation of these differences. The basic premise is that both individual and contextual characteristics play a role in health. This concern is captured by the search for so-called “neighborhood effects,” which generally refers to the study of how local context influences the health and well-being of individuals in a way that cannot be reduced to the properties of the individuals themselves.
Most of the research on neighborhood effects has focused on social and behavioral outcomes, including child cognitive and behavioral development, school dropout, educational attainment, crime and delinquency, substance use, sexual activity, contraceptive use, childbearing, income, and
labor force participation (see recent reviews by Gephart, 1997; Leventhal and Brooks-Gunn, 2000; Sampson, Morenoff, and Gannon-Rowley, 2002). Until recently, health outcomes had been noticeably absent from this list, but multilevel studies are becoming increasingly popular in health research. This new multilevel research on local social context and health has garnered wide attention in social epidemiology, as evidenced by the publication of four reviews of this literature in the past 3 years (Diez-Roux, 2002; Ellen, Mijanovich, and Dillman, 2001; Pickett and Pearl, 2001; Robert, 1999).
One of the reasons that public health scientists have become so interested in local context is to better understand the striking and persistent racial and ethnic differences across a range of health outcomes that have eluded most efforts to explain them using data at the individual level (Krieger, 1994; Williams and Collins, 1995a). There are large racial/ethnic differences across many causes of morbidity and mortality, and even through casual observation it seems obvious that perhaps some of this health inequality is related to the different types of contexts, or “ecological niches,” into which different racial/ethnic groups are born, and within which they grow up, live, and work. As research on residential segregation demonstrates (Acevedo-Garcia, 2000; Cooper et al., 2001; Ellen, 2000; LaVeist and Wallace, 2000; Massey and Denton, 1993; Polednak, 1996) place-based disparities are of central importance to understanding race-based health disparities in the United States. Moreover, a better understanding of why place and context matter also promises to yield new insights and intervention strategies for addressing racial/ethnic inequalities in health. Thus, the potential of place-based research to inform health intervention strategies that target places as well as people has given further impetus to this research in public health (Macintyre, MacIver, and Sooman, 1993; Sooman, Macintyre, and Anderson, 1993).
At this point, research on local context and health remains somewhat disengaged from recent theoretical and methodological developments in the sociological literature on neighborhoods. For example, whereas the sociological literature on neighborhood effects has taken a “process turn” in recent years and begun to focus more on the mechanisms that explain why neighborhoods matter (Sampson et al., 2002), most research on the neighborhood context of health is still attempting to establish that context matters. This is partly because most health research is framed in a paradigm where individual-level proximal influences—such as behaviors or biomarkers of pathogenic processes—take precedence over contextual factors (Krieger, 1994; Palloni and Morenoff, 2001; Schwartz, Susser, and Susser, 1999; Susser, 1998).1
To some extent neighborhood effects research on health remains mired in a “poverty paradigm” (Rowley et al., 1993) focusing mostly on the
association between Census-based indicators of community socioeconomic position and individual health outcomes, with a heavy emphasis on the deleterious effects of concentrated poverty and other forms of disadvantage. The main thrust of such studies has been to show that poorer places are associated with worse health outcomes, above and beyond the characteristics of the individuals who live there (Robert, 1999). This emphasis on disadvantage, to the exclusion of other facets of neighborhood environments, is partly the result of a lack of appropriate data, but we argue that it also reflects a paucity theory that can inform questions about how neighborhoods may affect specific types of health outcomes.
In this chapter we discuss both the promises and shortcomings of this growing literature on local context and health. In doing so, we bring together epidemiological perspectives concerned with exposure measurement and mechanisms—what are the measurable characteristics of neighborhoods (exposures) that can plausibly influence different types of health-related outcomes (specific causal pathways)—with sociological concerns about how to conceptualize and analyze neighborhoods. Rather than engaging in a comprehensive literature review—excellent reviews already exist (e.g., Diez-Roux, 2001; Ellen et al., 2001; Pickett and Pearl, 2001; Robert, 1999; Yen and Syme, 1999)—in this chapter we will focus on issues relating to the current state of research on neighborhoods and health, the dimensions of neighborhood environments that may be related to health, the pathways through which neighborhoods translate into specific types of health outcomes, how neighborhood effects intersect with the study of aging and the life course, and selection processes relating to the sorting of individuals into neighborhoods. We also present an empirical analysis of the neighborhood context of mortality in Chicago neighborhoods and conclude by suggesting new directions for neighborhood research on health.
THE CONCEPT OF NEIGHBORHOOD
Robert Park and Ernest Burgess laid the foundation for urban sociology by defining local communities as “natural areas” that developed as a result of competition between businesses for land use and between population groups for affordable housing. A neighborhood, according to this view, is a subsection of a larger community—a collection of both people and institutions occupying a spatially defined area influenced by ecological, cultural, and sometimes political forces (Park, 1916). Suttles (1972) later refined this view by recognizing that local communities do not form their identities only as the result of free-market competition. Instead, some communities have their identity and boundaries imposed on them by outsiders. Suttles also argued that the local community is best thought of not as a single entity, but rather as a hierarchy of progressively more inclusive resi-
dential groupings. In this sense, we can think of neighborhoods as ecological units nested within successively larger communities.
In practice, most social scientists and virtually all studies we assess rely on “statistical” neighborhoods that depend on geographic boundaries defined by the Census Bureau or other administrative agencies (e.g., school districts, police districts). Although administratively defined units such as Census tracts and block groups are reasonably consistent with the notion of overlapping and nested ecological structures, they offer imperfect operational definitions of neighborhoods for research and policy. However, the term “neighborhood” has been defined quite broadly in health research, encompassing units as small as block groups and as large as counties. Thus far there has been little systematic research into how geographic scale affects contextual estimates, although there is some evidence that estimates of place effects are stronger when using smaller geographic areas (Boyle and Willms, 1999).
Increasingly, researchers have become interested in new methods that might help define neighborhoods in such a way that is more respectful of the logic of street patterns and possibly more reflective of the social networks of “neighboring” behavior (Coulton, Korbin, Chan, and Su, 2001; Grannis, 1998). One important avenue for future research is to explore whether and how such neighboring patterns vary across demographic subgroups. For example, children and the elderly may both face more geographical constraints on the range of social networks and routine activity patterns that could make the more proximate neighborhood environment more consequential in their daily lives (Booth, Owen, Bauman, Clavisi, and Leslie, 2000; Carstensen, Isaacowitz, and Charles, 1999). Race/ethnicity may also play a role in shaping the geographic reach of routine activities and social networks. Understanding how the concept of neighborhood varies across these demographic groups is critical in advancing research on neighborhood environments as sources of group disparities in health.
WHAT DO WE KNOW ABOUT NEIGHBORHOODS AND HEALTH?
One of the hallmarks of neighborhood effects research is its attention to the potentially confounding influences of individual-level attributes in making neighborhood-level inferences, either through the use of multilevel research designs and statistical methods, or through randomized experimental designs. Investigations in this field have attempted to unravel the extent to which characteristics of neighborhoods (contextual effects) influence health outcomes after accounting for the fact that neighborhoods are composed of people with different individual characteristics (compositional effects), who in some cases choose to live in different types of neighborhoods, or more likely are sorted into them by economic, political, and other
social processes. As we will discuss later, this beguilingly simple framing of the research objective raises important conceptual problems as to what should be considered a contextual or compositional effect. For example, at any one point in time an individual may “possess” a certain level of education, which could be considered an individual-level predictor of that person’s health status. Yet educational attainment is also the complex product of prior influences of the individual (e.g., innate characteristics), family (e.g., educational expectations), and social context (e.g., quality of schooling). Thus, the association between individual educational attainment and health could, in part, reflect the effects of prior social context, and yet its effect on health typically would be attributed to compositional rather than contextual factors. Thus, the line between compositional and contextual is conceptually very fuzzy, and is simultaneously a problem of not having appropriate data, appropriate methodology, and perhaps most importantly, appropriate sociological and epidemiological theory.
The literature on neighborhood effects and health is expanding rapidly. One recent review (Pickett and Pearl, 2001) identified 25 multilevel studies of neighborhood effects on health, 23 of which reported significant associations between health and at least one measure of neighborhood socioeconomic status. Even in the 2 years since the publication of that review, the literature has grown substantially. We have identified more than 60 multilevel studies of health that encompass the following array of outcomes:
-
Mortality: Specific outcomes include all-cause mortality (Anderson, Sorlie, Backlund, Johnson, and Kaplan, 1997; Bond Huie, Hummer, and Rogers, 2002; Bosma, van de Mheen, Borsboom, and MacKenbach, 2001; Ecob and Jones, 1998; Haan, Kaplan, and Camacho, 1987; Kaplan, 1996; LeClere, Rogers, and Peters, 1997; Malmstrom, Johansson, and Sundquist, 2001; Sloggett and Joshi, 1994, 1998; Veugelers, Yip, and Kephart, 2001; Waitzman and Smith, 1998a; Yen and Kaplan, 1999) and mortality due to specific causes, including heart disease, cancer, kidney disease, and injury (Alter, Naylor, Austin, and Tu, 1999; Cubbin, LeClere, and Smith, 2000; Garg, Diener-West, and Powe, 2001; LeClere et al., 1998; Waitzman and Smith, 1998a).
-
Adult physical health status: This category includes studies of blood pressure (Davey Smith, Hart, Watt, Hole, and Hawthorne, 1998; Diez-Roux et al., 1997; Krieger, 1992; Merlo et al., 2001; Wilson, Kliewer, Plybon, and Sica , 2000), cholesterol (Davey Smith et al., 1998; Diez-Roux et al., 1997), coronary heart disease (Diez-Roux et al., 1997; Lee and Cubbin, 2002), respiratory function (Ecob, 1996; Humphreys and Carr-Hill, 1991), height and waist-hip ratio (Ecob, 1996; Krieger, 1992), indicators of obesity (Davey Smith et al., 1998; Ecob, 1996; Marmot et al., 1998; Robert, 1998; Sundquist, Malmstrom, and Johansson, 1999), lead expo-
-
sure among older adults (Elreedy et al., 1999), and survey-reported conditions such as functional limitations, chronic conditions, and self-rated health (Balfour and Kaplan, 2002; Chandola, 2001; Ecob, 1996; Humphreys and Carr-Hill, 1991; Malmstrom et al., 2001; Malmstrom, Sundquist, and Johansson, 1999; Shouls, Congdon, and Curtis, 1996; Stafford, Bartley, Mitchell, and Marmot, 2001).
-
Infant and child health: Most of these studies are of birthweight (Buka, Brennan, Rich-Edwards, Raudenbush, and Earls, 2003; Ellen, 2000; Gorman, 1999; Morenoff, 2003; O’Campo, Xue, and Wang, 1997; Pearl, Braveman, and Abrams, 2001; Rauh, Andrews, and Garfinkel, 2001; Roberts, 1997; Sloggett and Joshi, 1998), but there are also some on infant mortality (Matteson, Burr, and Marshall, 1998), childhood asthma and respiratory illness (Morgan and Chinn, 1983), accidental injuries (Reading, Langford, Haynes, and Lovett, 1999), and emotional and behavioral problems (Caspi, Taylor, Moffitt, and Plomin, 2000; Kalff et al., 2001) among young children.
-
Mental health: This category includes measures of depression, anxiety, and various other outcomes (Aneshensel and Sucoff, 1996; Katz, Kling, and Liebman, 2001; Marmot et al., 1998; Reijneveld and Schene, 1998; Ross and Jang, 2000; Schulz et al., 2000).
-
Health behaviors: Outcomes in this group include substance use (Boardman et al., 2001; Diehr et al., 1993; Diez-Roux et al., 1997; Duncan, Jones, and Moon, 1998; Ecob and Macintyre, 2000; Finch, Vega, and Kolody, 2001; Ganz, 2000; Hart, Ecob, and Smith, 1997; Kleinschmidt, Hills, and Elliott, 1995; Krieger, 1992; Lee and Cubbin, 2002; Reijneveld and Schene, 1998; Robert, 1998; Schroeder et al., 2001; Sundquist et al., 1999), dietary practices (Diehr et al., 1993; Ecob and Macintyre 2000; Hart et al., 1997; Karvonen and Rimpela, 1996; Lee and Cubbin, 2002), and physical activity (Ecob and Macintyre, 2000; Lee and Cubbin, 2002; Robert, 1998; Ross, 2000b; Sundquist et al., 1999).
-
Health services: Some studies use multilevel data to examine neighborhood differences in the availability of health services, including cardiopulmonary resuscitation (Iwashyna, Christakis, and Becker, 1999), cardiac procedures (Alter et al., 1999), and kidney transplants (Garg et al., 2001).
With only a few exceptions (e.g., Sloggett and Joshi, 1994; Veugelers et al., 2001), nearly all of the multilevel studies we reviewed found that after controlling for individual-level characteristics, there is still an association between neighborhood environments and health outcomes. However, these studies varied widely in the way they operationalized the concept of neighborhood and measured neighborhood characteristics, making it difficult to reach a conclusion about the magnitude and substantive importance of these effects.
The vast majority of the studies we reviewed focus on the deleterious effects of socioeconomic disadvantage using Census-based measures of local
area socioeconomic composition. The most common way to measure neighborhood socioeconomic status (SES) is through an index of socioeconomic deprivation/disadvantage (e.g., Boardman et al., 2001; Bosma et al., 2001; Caspi et al., 2000; Cubbin et al., 2000; Diez-Roux et al., 1997; Duncan et al., 1998; Ecob, 1996; Ecob and Jones, 1998; Ecob and Macintyre, 2000; Hart et al., 1997; Hart, Hole, and Smith, 2000; Malmstrom et al., 1999; Marmot et al., 1998; Morgan and Chinn, 1983; Reading et al., 1999; Reijneveld and Schene, 1998; Roberts, 1997; Sloggett and Joshi, 1994, 1998; Stafford et al., 2001; Sundquist et al., 1999; Wilson et al., 2000; Yen and Kaplan, 1999). However, some studies eschew the single index approach in favor of using single- or multiple-item indicators of neighborhood disadvantage, such as measures based on income, poverty, unemployment, public assistance, education, and occupational status (e.g., Ganz, 2000; Humphreys and Carr-Hill, 1991; Kaplan, 1996; Karvonen and Rimpela, 1996, 1997; LeClere et al., 1998; LeClere, Rogers, and Peters, 1997; Lee and Cubbin, 2002; O’Campo et al., 1997; Pearl et al., 2001; Robert, 1998; Ross, 2000a; Veugelers et al., 2001). Other studies take a categorical approach to measuring neighborhood disadvantage by constructing neighborhood typologies, such as the distinction between “poverty” and “nonpoverty” areas (Geis and Ross, 1998; Haan et al., 1987; Humphreys and Carr-Hill, 1991; Waitzman and Smith, 1998a).
A smaller number of studies have analyzed other neighborhood compositional/structural factors such as racial/ethnic composition (Bond Huie et al., 2002; Cubbin et al., 2000; LeClere et al., 1997, 1998; Lee and Cubbin, 2002; Roberts, 1997), family structure (Cubbin et al., 2000; LeClere et al., 1997, 1998; Lee and Cubbin, 2002; Ross, 2000a; Veugelers et al., 2001), residential stability (Cubbin et al., 2000; Kaplan, 1996; Lee and Cubbin, 2002; Roberts, 1997; Ross, Reynolds, and Geis, 2000), population density/ urbanization (Cubbin et al., 2000; Iwashyna et al.,1999; Lee and Cubbin, 2002), and housing condition/owner occupancy (Kaplan, 1996; Karvonen and Rimpela, 1997; Lee and Cubbin, 2002; O’Campo et al., 1997; Roberts, 1997; Stafford et al., 2001). However, the evidence on how these factors affect health is much less consistent across studies.
Neighborhood Context and Racial/Ethnic Disparities in Aging Health
Given that race/ethnic minority groups are disproportionately exposed to disadvantaged social environments, it is not surprising that many researchers have looked to neighborhood environmental factors, such as residential segregation and the concentration of poverty, as potential explanations for racial/ethnic disparities in health (e.g., Williams and Collins, 1995b). To this point, however, only a few studies have explicitly made this connection. Two such studies track the mortality of respondents to the
National Health Interview Survey (NHIS) using the National Death Index (NDI). In the first of these studies, LeClere and colleagues (1997) used tract-level contextual data from the 1990 Census to explain racial/ethnic disparities in all-cause mortality among NHIS respondents from 1986 to 1990. The authors found that after adjusting for individual-level indicators of SES (i.e., income, education, and marital status), neighborhood characteristics fully explain the remaining mortality differential between African Americans and non-Hispanic whites, but not the mortality differential between Mexicans and whites. (Mexicans had lower mortality rates than whites, and neighborhood characteristics do not explain Mexicans’ mortality advantage.) In this study, the main contextual factor driving the convergence in the mortality differential between African Americans and whites was neighborhood racial/ethnic composition.
In a follow-up study, Bond Huie and colleagues (2002) modified the NHIS-NDI data set by expanding the number of years of NHIS respondents (1986-1997), adding more individual-level control variables, and changing the definition of neighborhood from Census tracts to very small areas (VSAs). They found that the introduction of contextual variables reduced the mortality risk for African Americans and Puerto Ricans by 12 and 14 percent, respectively, but significant mortality disparities remained even after adjusting for neighborhood characteristics. As was the case in the study by LeClere and colleagues (1997), neighborhood characteristics explained fewer of the mortality disparities between whites and either Mexicans or other Hispanics.2 Although differences in model specification make it difficult to compare the results of the two NHIS-NDI studies, it does appear that neighborhood characteristics contribute substantially to the explanation of black-white mortality disparities in both studies, but less so to Mexican-white mortality differences.
Another issue that has also received relatively little attention is whether neighborhood context is more predictive of health outcomes for certain age groups. Most of the available evidence on this topic also comes from multilevel studies of mortality. Two of these studies (Haan et al., 1987; Waitzman and Smith, 1998a) show that residence in a poverty area is more predictive of mortality among younger age groups than older age groups. Using data from the National Health and Nutrition Examination Survey (1971-1974), Waitzman and Smith (1998a) found that poverty area residence is associated with elevated mortality risk among 25- to 54-year-olds, but reduced mortality risk among 55- to 74-year-olds. The authors attribute the counterintuitive effect of poverty in the older age group to a “crossover” effect in which elderly survivors living in poverty areas may be selectively less frail than their counterparts in nonpoverty areas. In another study showing that neighborhood effects on mortality may be less pronounced among the elderly, LeClere and colleagues (1997) found that con-
textual characteristics account for a greater reduction in racial/ethnic mortality disparities within younger age groups (18 to 44 and 45 to 64) than within the oldest group (65 and over). However, this study does not report the results of age-specific regression coefficients for neighborhood covariates, so it is not clear whether the neighborhood effects themselves are stronger among the younger groups.
Other mortality studies using the NHIS-NDI data set have failed to replicate the finding that neighborhood effects on mortality are weaker among the elderly. In one of these, Waitzman and Smith (1998b) showed that the metropolitan area-level concentration of poverty was associated with an elevated risk of mortality among respondents to the 1986-1994 NHIS in both the 30 to 44 and 65 and over age groups. In a more recent study using smaller geographic units to measure contextual effects (VSAs) and a longer time series of respondents to the NHIS (1986-1997), Bond Huie and colleagues (2002) found that most contextual covariates have slightly larger effects among the older age group (45 to 64) compared to the younger group (18 to 44). They also found interactions between age and some neighborhood covariates, such as immigrant composition, which is protective against mortality for the older group, but a risk factor for the younger group. Thus, the empirical evidence is mixed on the question of how contextual effects on mortality vary by age.
The view that neighborhood context may be more salient for the elderly is corroborated by multilevel research focusing on health outcomes other than mortality. For example, Balfour and Kaplan (2002) found that self-reported neighborhood problems, such as excessive noise, inadequate lighting, and heavy traffic, were strongly associated with functional loss among participants aged 55 and over in their sample of adults from Alameda County, California. In perhaps the most extensive investigation of age variation in neighborhood effects thus far, Robert and Li (2001) hypothesize that neighborhood effects should actually be stronger among older adults because they may be more vulnerable to negative exposures such as pollution, crime, and weak social and medical services. In keeping with this hypothesis, their findings show that the association between neighborhood socioeconomic characteristics and health (survey reports of self-rated health and the number of chronic conditions) is weakest in young adulthood, but becomes progressively stronger in successively older age groups, peaks between ages 60 and 69, then gets weaker again at ages 70 and older.
In sum, although there is relatively little research on how the relation between neighborhood environments and health may vary across demographic subgroups, the available evidence suggests that racial/ethnic differences in neighborhood context may account for a large proportion of racial/ethnic disparities in health (focusing primarily on mortality), but there is more disagreement on whether and how neighborhood effects vary across
age groups. A common limitation of the studies that have analyzed the connection between neighborhood environments and racial/ethnic health disparities is that they do not consider interactions between race/ethnicity and age. This is especially problematic in the case of mortality, where a large number of studies have found a black-white crossover in mortality curves at older ages (Hummer, Rogers, and Eberstein, 1998), implying that racial/ethnic disparities are not fixed entities, but moving targets that vary depending on which age groups are being compared. We will consider such interactions in an analysis of racial/ethnic disparities in mortality using multilevel data on all-cause mortality in Chicago neighborhoods.
UNDERSTANDING WHY NEIGHBORHOODS MATTER
Most of the previous research on neighborhood environments and health has been concerned with the question of whether neighborhoods, and specifically socioeconomic characteristics of neighborhoods, matter for the health of individuals. The overwhelming majority of these studies indicate that lower neighborhood socioeconomic status does appear to be related to poor health, net of individual characteristics. Without neglecting the importance of this question, we believe that research should begin to pay more attention to the question of why neighborhoods matter—what does the association between area socioeconomic status and individual health, even net of all other individual-level factors, mean? One way to answer this question is to explore interactions between neighborhood- and individual-level factors that might explain the individual circumstances under which neighborhoods influence individual health—or, considered another way, the neighborhood conditions under which individual-level factors influence health. Some studies have explored such “cross-level” interactions (e.g., Diez-Roux et al., 1997; Ecob and Macintyre, 2000; O’Campo et al., 1997; Rauh et al., 2001). Another strategy is to directly measure the neighborhood “mechanisms” that might explain the relationship between neighborhood SES and health (Morenoff, Sampson, and Raudenbush, 2001; Sampson et al., 2002). This calls for an infusion of new theory and new data.
One problem with the current state of this research is that neighborhood characteristics are used somewhat interchangeably and with little theoretical justification in the search for neighborhood effects. Whereas many frameworks have been proposed for organizing individual-level predictors of health status into conceptual categories and for determining the order in which they should be entered into statistical models, health researchers are much less accustomed to thinking about neighborhood-level mechanisms and how they are interrelated. We propose a conceptual framework, consistent with a stress and adaptation perspective on how social
environments come to affect health (House, 2002; Lin and Ensel, 1989), that highlights the importance of stressful neighborhood conditions that may deleteriously affect health and the availability of resources from social relations that may counteract or buffer the impact of contextual stressors on health.
Structural/Physical Environment
Structural characteristics refer to properties of a neighborhood’s population composition that are typically measured as aggregations of individual-level attributes. In the health literature, the most commonly studied structural measures are indicators of socioeconomic and racial/ethnic composition. In the case of socioeconomic composition, concentrated poverty may be a marker of institutional abandonment. For example, poor neighborhoods may lack access to quality health services, nutritional food, and well-maintained recreational areas (Sooman et al., 1993). Disadvantaged neighborhoods may also expose residents to more dilapidated housing, pollutants, and sources of stress that include crime, violence, and overcrowding. In contrast, affluent areas may offer access to better health care, stores with nutritional food, recreational areas, and other institutional resources that promote good health. Thus, measures of socioeconomic composition could be proxies for a bundle of health risks associated with the concentration of disadvantage and protective factors associated with the concentration of affluence.
The relationship between neighborhood racial/ethnic composition and health is more complex. On the one hand, measures of racial/ethnic composition are markers for residential segregation, and previous research demonstrates that segregation imposes multiple health risks on members of poor minority areas (Cooper et al., 2001; Ellen, 2000; LaVeist, 1993; Massey and Denton, 1993; Polednak, 1996). The health consequences of segregation are likely to overlap with those of concentrated disadvantage, but segregation could impose additional risks. For example, individuals who face barriers to residential mobility because of their race could face psychological risks associated with discrimination (Williams and Collins, 1995b). Moreover, studies have shown that African-American neighborhoods are more likely to suffer from institutional risk factors such as the proliferation of liquor stores and insufficient supplies of prescription drugs at local pharmacies (LaVeist and Wallace, 2000; Morrison, Wallenstein, Natale, Senzel, and Huang, 2000). On the other hand, ethnically homogeneous neighborhoods could also be havens for group resources. For example, some scholars have argued that Mexican culture emphasizes strong family support and reinforces healthy behaviors (Balcazar, Aoyama, and Cai, 1991; Scribner, 1996). Mexican women may be more likely to adhere
to traditional cultural practices when living in neighborhoods with higher concentrations of Mexicans. Thus, the expected association between racial/ ethnic composition and health is ambiguous—more homogeneous minority neighborhoods may present health risks associated with segregation, yet they also may produce important group resources through shared cultural experiences.
A testament to the power of structural characteristics to affect health can be seen in recent historical examples, where geographic distributions of poverty are overlaid on geographic distributions of health (Murray et al., 1998). For example, in London, neighborhoods identified as having high poverty and poorer health in 1900 were in almost exactly the same situation in 1999 (Dorling, Mitchell, Shaw, Orford, and Smith, 2000). The geographic pattern of economic and health disadvantage had changed little in 100 years—despite that fact that four or five generations of individuals had moved through those neighborhoods. The same processes can be seen in some U.S. cities (Sampson and Morenoff, 2001).
A closely related group of neighborhood characteristics includes physical and geographic features of the local environment, such as natural amenities, street layout, and pollution. The importance of local toxic environmental exposures for health is clear. There is evidence of negative health effects from a variety of such exposures, including diesel exhaust, lead, and water quality—PCBs, toxic waste dumps, chemical releases, and airborne particulates (Bjorksten, 1999; Burns, Baghurst, Sawyer, McMichael, and Tong, 1999; Eggleston et al., 1999; Howel, Darnell, and Pless-Mulloli, 2001; Northridge et al., 1999; Pandya, Solomon, Kinner, and Balmes, 2002). By their very nature, some of these exposures are inherently “local” and thus are potentially important sources of racial/ethnic differences in health. Balanced against this is the fact that some of the more extreme exposures are quite rare and so are unlikely to aid in explaining the systematic and wide-ranging differences in health across race/ethnic groups. However, we also need to consider that it may not only be the independent effects of the relatively more common exposures—such as geographically specific poor air quality—but their capacity to interact with other exposures to produce poorer health. For example, environmental exposures involved in the pathogenesis of asthma may interact with lack of adequate medical management of the disease to exacerbate its effects. These are clearly important areas for research on context effects on racial/ethnic differences in certain outcomes.
Mounting evidence also exists that physical characteristics of neighborhoods can be crucial determinants of health behaviors. Humpel, Owen, and Leslie (2002) show that accessibility to bicycle paths, parks, walkways, and even local shopping facilities all positively affect deliberate and incidental physical activity. Recent research also suggests that certain physical charac-
teristics of neighborhoods promote outdoor activity and may also afford opportunities for social interaction among area residents (Balfour and Kaplan, 2002; Humpel et al., 2002). Neighborhood characteristics that discourage residents from leaving their homes to interact with neighbors may be especially relevant to the elderly in light of recent evidence showing that diverse social interactions are crucial to maintaining cognitive functioning among the elderly (Fratiglioni, Wang, Ericsson, Maytan, and Winblad, 2000). Thus, it is possible that the physical characteristics of neighborhoods affect cognitive decline among the elderly.
Stressful Social Conditions
One of the main reasons that lower SES neighborhoods may be unhealthy places to live is that they expose residents to stressful conditions, such as violent crime. Repeated exposure to stress fosters a condition known as allostatic load, which refers to the physiological costs of chronic overactivity or underactivity of systems within the body (e.g., the hypothalamic-pituitary-adrenal axis or the autonomic nervous system) that fluctuate to meet demands of repeated exposure to environmental stressors (McEwen, 1998). Geronimus (1992) argues that prolonged exposure to high-stress neighborhood environments can take a cumulative toll on maternal health in the form of “weathering.”
Although there is relatively little research on crime and health, some evidence shows that fear of crime may be a key mechanism in explaining the effects of neighborhood structural characteristics on self-rated health and mental health (Aneshensel and Sucoff, 1996; Chandola, 2001; Cutrona, Russell, Hessling, Adama Brown, and Murray, 2000; Geis and Ross, 1998; Ross and Jang, 2000; Ross et al., 2000) and that higher neighborhood crime is associated with a greater risk of low birthweight (Collins and David, 1997; Morenoff, 2003; Zapata, Rebolledo, Atalah, Newman, and King, 1992). There are also strong theoretical reasons to believe that violent crime is a primary source of stress in many urban neighborhoods. First, research on the fear of crime shows that people tend to perceive crime largely in geographic terms (Warr, 1994), which makes the neighborhood environment a particularly salient context for generating fear, and hence stress. Moreover, neighborhood crime can be stressful not only for people who perceive high personal risks of victimization, but also for those who fear for the safety of family members and friends, which Warr and Ellison (2000) call “altruistic fear.”
Second, research shows that people who perceive more crime and disorder in their neighborhoods have a higher risk of mental health problems related to stress, such as anxiety, depression, powerlessness, fear, and mistrust (Aneshensel and Sucoff, 1996; Cutrona et al., 2000; Geis and Ross,
1998; Ross and Jang, 2000; Ross et al., 2000). By promoting distrust of others, neighborhood crime can also lead to social isolation from close social relationships (Krause, 1991), which in turn has been linked to adverse physical health outcomes (Berkman and Glass, 2000; House, Landis, and Umberson, 1988).
Third, research on exposure to violence among children and adolescents has linked repeated encounters with violence (both direct and indirect) to the development of emotional problems, posttraumatic stress syndrome, substance use, and increasing pessimism in one’s own ability, and that of health professionals, to improve health (Fick and Thomas, 1995; Margolin and Gordis, 2000; Selner-O’Hagan, Kindlon, and Buka, 1998).
Finally, some scholars suggest that in addition to fostering stress, neighborhood crime also promotes risky behaviors, such as substance use, because residents of crime-ridden neighborhoods perceive themselves to have relatively short life expectancies, leaving them less concerned with the long-term health consequences of their actions (Ellen et al., 2001; Ganz, 2000).
Social Relations/Engagement
How people adapt to stressful environments depends, in part, on their access to informal resources such as those produced through social relationships and institutions (i.e., social capital). In places where neighbors are more engaged in the social life of their community, residents are more likely to generate informal resources by assisting one another with favors; providing each other with health-related advice and other information; aiding one another with everyday tasks, such as childcare; monitoring each others’ property; and participating in local voluntary associations, such as block clubs, tenants’ associations, and religious organizations (Morenoff, 2003).
Thus far, most of the research on social relations/engagement and health has focused on individual-level measures of social ties and social support. A major finding from this research is that social isolation—the relative lack of social relationships—is a risk factor for mortality, with a relative risk ratio comparable to that of cigarette smoking (Berkman and Glass, 2000; House et al., 1988; Singer and Ryff, 2001). A related line of research finds that participation in voluntary organizations, a form of social engagement, may promote both physical and mental health (Wilson and Musick, 1999).
Relatively few studies have analyzed the connection between neighborhood-level measures of social relations/engagement and health. Those that have focus mainly on mental health (Aneshensel and Sucoff, 1996; Cutrona et al., 2000; Geis and Ross, 1998; Ross and Jang, 2000; Ross et al., 2000), and most of these studies characterize neighborhood social processes by relying on only a single individual’s report of what happens in his or her neighborhood. A more reliable approach to measuring neighborhood social
processes is to aggregate the reports of multiple respondents living in the same neighborhood (Raudenbush and Sampson, 1999; Sampson et al., 2002), but this strategy has not been used in many health studies (for an exception, see Cutrona et al., 2000).
Sampson and colleagues use such an approach to measure neighborhood “collective efficacy,” defined as the shared willingness of residents to actively cooperate in pursuit of commonly held goals (Sampson, Morenoff, and Earls, 1999; Sampson, Raudenbush, and Earls, 1997), but most of their research focuses on crime-related outcomes, not health.3 This research shows that neighborhoods with higher levels of collective efficacy have lower levels of violent crime (Morenoff et al., 2001; Sampson et al., 1997) and disorder (Sampson and Raudenbush, 1999), and that collective efficacy—as well as other social processes, such as reciprocal exchange—is predicted by structural factors, such as concentrated disadvantage and residential stability (Morenoff et al., 2001; Sampson et al., 1999). In related work, Morenoff (2003) found that the neighborhoods with higher levels of reciprocal exchange among neighbors and participation in local voluntary associations are protective against the risk of low birthweight, even after adjusting for a large set of sociodemographic, behavioral, and biomedical individual-level risk factors. A recent study of middle-aged women in Sweden shows that greater levels of neighborhood social participation also increases the use of hormone replacement therapy (HRT) net of individual socioeconomic, behavioral, and other risk factors (Merlo et al., 2001). The authors speculate that greater social participation in neighborhoods may reflect communication processes whereby women living in neighborhoods with higher levels of social participation influence each other’s use of HRT or unmeasured characteristics such as different prescribing patterns of physicians in those neighborhoods.
Influences from Outside the Neighborhood
The social environment and context in which individuals live their lives comprises not only their own immediate neighborhood, but also surrounding neighborhoods in which people work, shop, attend school, visit with friends, travel, and conduct other activities in the course of their daily lives. Most previous research on neighborhoods and health focuses exclusively on the “internal” properties of neighborhoods, but does not consider the possible influences that the wider social environment surrounding a given neighborhood may have on the health of its residents. The tendency to abstract the idea of “neighborhood” from its broader spatial context runs counter to the long theoretical tradition in urban sociology, dating back to the Chicago School, that views neighborhoods as spatially interrelated parts of a broader social system that Park, Burgess, and McKenzie (1967, p. 54)
characterized as a “moving equilibrium of social order.” Thus far, only a few studies have explored the wider spatial context of neighborhood effects (e.g., Baller, Anselin, and Messner, 2001; Morenoff and Sampson, 1997; Morenoff et al., 2001; Sampson et al., 1999; Smith, Frazee, and Davison, 2000), and most of these are ecological-level studies that do not control for characteristics of individuals. However, in his study of birthweight in Chicago neighborhoods, Morenoff (2003) found that after adjusting for potentially confounding covariates at both the individual and neighborhood levels, there was strong spatial autocorrelation in birthweight such that the incidence of low birthweight in a given neighborhood was correlated .69 with the rate of low birthweight in adjacent neighborhoods.
A key issue in spatial analysis is how to conceptualize and model the spatial process under study (Anselin, 2001). Some outcomes diffuse over space, such as acts of violence in one neighborhood that instigate retaliatory acts in nearby neighborhoods or an infectious disease that is spread from one area to another through social networks (Cohen and Tita, 1999). Such diffusion processes apply to the case of infectious disease, but noninfectious health outcomes do not diffuse over space in the sense that the occurrence of the event/disease in one neighborhood does not directly affect the likelihood of a similar outcome occurring in a geographically proximate area. In the case of noninfectious health outcomes, spatial dependence can still arise as a result of “spillover” effects from nearby neighborhoods, also known as spatial externalities. For example, crime in nearby areas may provoke fear in a given neighborhood, regardless of the level of crime in that neighborhood (Morenoff and Sampson, 1997). Likewise, informal social resources generated through social relations and collective engagement may accrue not just to the residents of a particular neighborhood, but potentially to residents in adjacent areas as well (Sampson et al., 1999). The general point is that neighborhood conditions may be reinforced, exacerbated, moderated, or counteracted by the characteristics of adjacent and proximate neighborhoods.
PATHWAYS TO HEALTH: SPECIFICITY, NATURAL HISTORY, AND LIFE COURSE
We now consider how future research could improve our understanding of the pathways through which neighborhoods come to affect health by proposing three related ideas that we believe are useful for better understanding how neighborhoods might affect racial/ethnic disparities in aging and health: (1) why we need to think about specific outcomes related to neighborhood effects on health, (2) how the timing of neighborhood exposures intersects with the natural history of health outcomes, and (3) how neighborhood effects may vary over the life course.
Neighborhood Effects and the Specificity of Health Outcomes
The first idea involves conceptualizing “health.” Obviously health is multidimensional and cannot be captured in a single outcome, although there are many useful summary measures of health, such as overall mortality and life expectancy, and measures that tap into disease burden as well as death, such as disability-adjusted life years (DALY) and quality-adjusted life years (QALY). In considering how neighborhoods may affect aging, we are concerned with the major chronic disease conditions and their sequelae, such as heart disease, diabetes, stroke, cancer, and respiratory disease. We are also concerned with mental health; aspects of physical, social, emotional, and cognitive functioning; and health-related behaviors, such as exercise, diet, and medication and health care utilization. This list is not intended to be exhaustive or exclusive. Rather, it serves to illustrate our first principle, that in thinking about how neighborhood processes could affect health outcomes, we need to think about how specific types of neighborhood processes link to specific types of health outcomes.
For example, the proximal neighborhood exposures causing falls among the elderly, such as uneven or broken pavements, are not the same causal exposures implicated in respiratory disease. Although sometimes we may be forced to pragmatically use a count of uneven or broken pavements as a surrogate for the causal exposures for respiratory disease that are present in a neighborhood—indeed, tallies of dilapidated buildings and broken windows have been used as surrogate measures of neighborhood environment linked to certain health outcomes (Cohen et al., 2000)—it is important nevertheless to be clear on what the relevant causal exposures are for each type of health outcome. Broken windows do not cause heart disease, unless they contribute to a complicated miasma of “stressful environment” that affects heart disease risk through cognitively mediated psychoneuroendocrine and immunologic processes. On the other hand, general aspects of the appearance of the environment may be important for mental health. The point is that unless we attempt to study specific outcomes, it will be difficult to know which neighborhood characteristics are important for which outcomes.
As another example of this specificity criterion, it is relatively easy to understand how “collective efficacy” might be associated with outcomes such as juvenile delinquency, violent behavior, or perhaps even behaviors such as smoking. It is less clear how the same neighborhood-level exposure might affect the pathogenesis of breast cancer or depression among the elderly. In fact, one of the strengths of the concept of collective efficacy is that it was formulated as a task-specific construct, meaning that what constitutes collective efficacy may differ depending on the outcome or age group in question (Sampson et al., 1999). This specific outcome/mechanism
approach is, in our opinion, one way forward and needs to be applied more rigorously across a range of potential health outcomes relevant to disparities in aging. Such a recognition may also mean that general health outcomes such as self-rated health or functional health indicators that mix physical, psychological, and functional morbidity are potentially of less interest in regard to understanding the specific mechanisms of health-related neighborhood processes, simply because there are so many potential pathways to individuals rating their general state of health. This is not meant to imply that such investigations are uninformative—instead they are limited in the extent to which they can provide clues to the ways in which specific neighborhood processes affect different health outcomes.
We do not wish to appear as overly reductionist, and we hold open the possibility that some neighborhood factors may be implicated in a range of outcomes. For example, it would not be a surprise to find that neighborhood poverty was associated with higher infant mortality, homicide, and heart disease—three disparate outcomes, with biologically different causal mechanisms, primarily affecting different age groups in the population. We would all recognize that poverty is a multidimensional construct that implicates a variety of more specific exposures such as poor housing, pollution, lack of education, unemployment, inadequate diet, and so on. The fact that these specific exposures cluster in certain geographic spaces—and so appear to be empirically associated with all the outcomes—should not be confused with the idea that they all have specific, proximal mechanistic pathways to different health outcomes. It simply means that neighborhoods that have poor-quality housing are also more likely to have more pollution, unsafe playgrounds, and no places to buy fresh fruit and vegetables. Thus, poverty is a convenient marker of many more specific damaging neighborhood exposures of which we are either ignorant or unable to measure directly. We should also be aware of the potential for such clusters of exposures to interact in producing disease, so that it is the spatial aggregation of a series of negative neighborhood forces that act synergistically to magnify the total exposure load and/or increase susceptibility to certain outcomes. However, the general principle of moving toward a search for greater conceptual and mechanistic specificity—in both social and biological domains—of neighborhood influences on health remains important.
Neighborhood Effects and the Natural History of Different Health Outcomes
The second and related principle is to consider the natural history of different types of health outcomes and at which stage in the natural history of an outcome neighborhood environments might be most relevant. For many health outcomes, especially chronic disease outcomes,
there is a natural history, which may begin with exposure to certain risk factors such as high-fat diet or smoking, metabolic or hemostatic changes, and the appearance of subclinical manifestations that increase susceptibility, such as asymptomatic atherosclerosis or elevated blood pressure. Then some triggering mechanism may come that leads to a clinically defined event (such as a heart attack), and assuming survival, the consequences of the disease where afflicted individuals learn to live on a day-to-day basis with any physical, social, behavioral, and psychological limitations imposed by their condition. It seems likely that different aspects of neighborhoods could affect these processes differently depending on which stage of the natural history of the particular disease is of concern. For example, it is possible that neighborhood characteristics may play little immediate role in the pathogenesis of stroke, but neighborhood factors may be very important in the quality of life and access to resources of people who have survived stroke and are living with some of the functional limitations that can impose.
Our point here is to suggest that there is no single pathway to health and thus no unique set of neighborhood characteristics that will be universally important for all health outcomes or at all stages of the outcomes. While this may be seen as lurching toward reductionism, we think it is an appropriate recognition of potential complexity. These two principles are important in guiding the next phase of research on health-related neighborhood effects, and this recognition is motivated by the overwhelming body of knowledge that suggests that there are indeed different pathways to different types and stages of health outcomes. Our specific topic here is to better understand racial/ethnic differences in health and aging. This clearly implicates disparities in a large array of different health outcomes and implicates different mechanisms.
Neighborhood Effects and the Life Course
The third principle also relates to the first two and involves considering life-course processes (Kuh and Ben Shlomo, 1997). If research on neighborhoods is to fulfill its promise for better understanding racial/ethnic disparities in major aging outcomes such as chronic disease, then it may be misleading to look for “explanations” of these disparities based on contemporaneous neighborhood exposures. As we have discussed, chronic diseases have latency periods, which implies that exposures from across the life course may be important in the pathogenesis and progression of these diseases (Barker, 1998; Davey Smith, Gunnell, and Ben Shlomo, 2000; Davey Smith et al., 1998; Hertzman, Power, Matthews, and Manor, 2001; Leon, 2001b; Leon and Davey Smith, 2000).
One way that research on neighborhoods and health could move forward is to better conceptualize how measured exposures to neighborhood conditions match up with the temporal logic of the stage of the outcome. In simple terms this means that we should start thinking about the potential effects of neighborhoods through a life-course perspective. It is possible that exposure to current neighborhood conditions per se has little to do with the current distribution of disparities in the incidence of chronic disease outcomes, such as rates of heart disease or cancer. Rather, these probably reflect neighborhood and individual influences from earlier in the life course. This recognition means that both individual and neighborhood life-course exposures are of interest in better understanding contemporary racial/ethnic differentials in some outcomes such as heart disease, cancer, chronic lung disease, and diabetes.
In its broadest conceptualization, a life-course approach recognizes that:
-
exposures in early life can have both direct and indirect long-term effects on health;
-
there may be genetic, biological, and social intergenerational inheritance of risk factors;
-
biological and social exposures coevolve over the life course, so that contextual exposures at one point of the life course may be literally “embodied”; and
-
the effects of exposures can accumulate over time.
Space limitations constrain our discussion of these principles here, but they have been well elaborated in previous work (Aboderin et al., 2002; Davey Smith, Ben-Shlomo, and Lynch, 2002; Davey Smith, Gunnell, and Ben Shlomo, 2000; Harding, 2001; Kuh and Ben Shlomo, 1997; Leon, 2001a).
Consider the example of neighborhood effects on coronary heart disease (CHD). CHD is a major cause of morbidity and mortality in the United States, and there are large and potentially widening racial/ethnic disparities in heart disease (Barnett and Halverson, 2001; Schalick, Hadden, Pamuk, Navarro, and Pappas, 2000). The long incubation period for CHD has been recognized for many years, and a life-course approach to its etiology is a natural extension of this view. Most of the important risk factors identified for CHD are socially patterned. Davey Smith and Lynch (2002) have detailed the risk factors for incident coronary heart disease according to stages of the life course:
-
Maternal health, development, and diet before and during pregnancy
-
Parental history of CHD
-
Low birthweight
-
Socioeconomic deprivation from childhood onward
-
Stress from childhood onward
-
Poor growth in childhood
-
Short leg length in childhood
-
Obesity in childhood
-
Certain infections acquired in childhood
-
Poor diet from childhood onward
-
High blood pressure in late adolescence
-
High serum cholesterol in late adolescence
-
Smoking from late adolescence onward
-
Little physical activity from late adolescence onward
-
High blood pressure in adulthood
-
High serum cholesterol in adulthood
-
Obesity in adulthood
-
Job insecurity and unemployment in adulthood
-
Short stature in adulthood
-
Binge alcohol drinking in adulthood
-
Diabetes and components of syndrome X in adulthood
-
Elevated fibrinogen and other acute phase reactants in adulthood
-
Certain infections acquired in adulthood
This list summarizes factors that are putative CHD risk factors and of particular interest from a life-course perspective, according to their period of influence. It is clear that CHD can be considered the archetype of diseases whose determinants should be sought across the entire life course—from conditions existing at the time of conception and during intrauterine development, through nutrition, growth, and health in childhood, to social conditions, occupation, diet, physical activity, and smoking throughout adult life. Applied to the potential for neighborhood characteristics to affect CHD, it is obvious that many of the factors listed are influenced by the contexts in which people have lived and that these contextual influences may be expressed at many stages of the life course.
Even greater complexity is added when we consider that these contextual effects may differ by birth cohort. The life-course conditions and exposures of individuals born into a poor neighborhood in Detroit in the 1940s may be very different from those born into the same conditions in the same city today. Poor neighborhoods in the 1940s may have implied greater exposure to environmental conditions conducive to undernutrition, while today they may be more likely to increase the risk of obesity. Yet it is the health of that cohort born in the 1940s that we are now beginning to observe in population health statistics. So, to explain current racial/ethnic disparities in health, we may need—depending on the outcome—to con-
sider the complex coevolution of individual and neighborhood processes over time that may in some cases be specific to birth cohort and the outcome being studied.
If we consider the schema presented in Figure 11-1 as a representation of some of the factors involved in the natural history of CHD across the life course, we could ask many questions about the potential for neighborhood processes to affect CHD at one or more points in time. Neighborhood effects on CHD are likely to be stronger at some stages than others. For example, we could hypothesize that neighborhood factors may be very important in dealing with the functional consequences of CHD.
Although our specific focus here is on neighborhood processes, we should also remember that neighborhoods might not be the relevant dimension of context for all stages of all health outcomes. For example, families, peers, schools, and workplaces may be more relevant dimensions of context than neighborhoods when considering the adoption, maintenance, and extinction of known behavioral CHD risk factors such as smoking. Nevertheless, neighborhoods lacking the infrastructure for healthy eating and exercise may impact the development of health behaviors, metabolic changes, and the subclinical development of atherosclerosis. Neighborhoods with high levels of crime and social stress could help trigger a heart attack. Neighborhoods with inadequate health care infrastructure probably affect
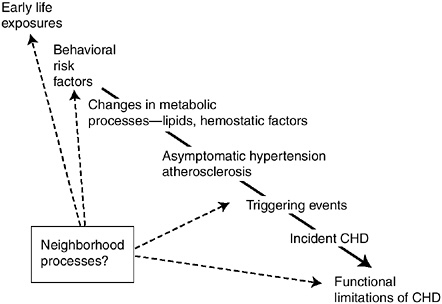
FIGURE 11-1 Neighborhood effects and the natural history of coronary heart disease.
access to emergency services, and the proper and timely diagnosis and immediate management of the condition. Finally, it is conceivable that neighborhoods also differ in their capacity—through such factors as housing, social networks, and transport—to foster adequate levels of physical and social functioning of individuals living with various degrees of CHD-induced disability. This approach raises more questions than it answers, but it does suggest a framework within which to examine such issues.
The life-course approach to chronic diseases such as CHD in adulthood—and therefore the life-course approach to disparities in the distribution of chronic diseases in adulthood—attempts to move beyond an epidemiology that concentrates on individual-level risk factors acting in a relatively instantaneous and supposedly independent manner. This search for instantaneous and independent contributors to risk is partly an outcome of the underlying model of disease causation, captured in the well-known metaphor of the “web of causation.” Although the idea of a complex web of causal components—even a web of multilevel contextual causal components—is certainly useful, it does not explicitly include a temporal component and masks the fact that what we observe at any point in time as an array of adult risk factors for CHD is the result of interlacing multilevel chains of biological and social exposures that have coevolved over time. Many of these risk factors have come from previous contextual exposures. In this way the life-course approach addresses the recent debate regarding the individualistic focus of much epidemiology, which concentrates on the lifestyles or physiological risk factor profiles of people abstracted from their social and temporal contexts (Krieger, 1999; Pearce, 1996; Susser, 1998; Weed, 1998). The many weaknesses of epidemiological approaches, which fail to locate exposure-disease associations within their historical, political, and social contexts, have been convincingly elaborated elsewhere (Koopman and Lynch, 1999; Leon, 2001a; McMichael, 1999; Palloni and Morenoff, 2001; Schwartz et al., 1999).
A life-course approach attempts not to abstract individual life trajectories from their contexts; indeed the long-term and sometimes irreversible outcomes of social circumstances at different stages of life can be seen as becoming literally embodied. Human bodies and minds in different social locations become crystallized reflections of the social experiences within which they have developed. Such biological and psychosocial development occurs within contexts of families, peers, and schools and thus also implies the potential for neighborhood influences.
The socially patterned nutritional, health, and environmental experiences of parents influence birthweight, height, weight, and lung function of their children, what are in turn important indicators of future health prospects. The life-course approach to health disparities views the physical and the social as being mutually constitutive, because aspects of bodily form can
influence social trajectory in the same way as social experiences become embodied. Low birthweight, growth patterns through childhood into adulthood, persistent infections acquired in early life (such as Helicobacter pylori) or the failure to acquire certain infections (leading to immunological programming and increased risk of atopy), lung function, degree of adiposity, and a habitus that embraces particular dispositional characteristics (including attitudes, health-related behaviors, and mood) and ways of dealing with misfortune may seem to fall within different categories, but they are all essential components of life trajectories that influence health. These trajectories are subject to the influence of context.
Better understanding racial/ethnic health disparities means we have to consider both contextual and individual processes acting over the life course of particular birth cohorts to affect racial/ethnic differences in particular outcomes. This implies a potentially important role for neighborhood influences on these processes over time and raises several methodological problems in studying the effects of contemporary indicators of neighborhood on outcomes that we know develop over time. For example, how should we interpret cross-sectional studies that show “small” effects of current neighborhood conditions on chronic disease or mortality after adjusting for individual factors such as behaviors and health indicators? It is precisely these “individual” risk factors that may be partly the result of a complex dynamic of life trajectories influenced by contexts that are now embodied as high lipid levels, obesity, or a positive history of hypertension. For example, evidence shows that individual dietary patterns are determined, at least in part, early in life and may be related to aspects of the neighborhoods in which individuals were raised. Thus, a study of obesity may find no evidence of contemporaneous neighborhood effects after controlling for individual dietary patterns, but these dietary patterns may carry with them the indirect effects of prior exposure to neighborhoods in which fresh fruit and vegetables were not widely available and dietary norms promoted less healthy nutritional practices.
SELECTION PROCESSES
Tilly (2002) argues that all empirical social research rests on two types of theories: one theory that explains the substantive phenomenon under study and a second theory that explains the generation of evidence concerning that phenomenon. Thus far our discussion of neighborhood environments and health has focused solely on the first type of theory—substantive explanations for how neighborhood environments may be related to health and well-being.4 Both sociologists and epidemiologists who study neighborhoods and health have been far less attentive to Tilly’s second type of theory—one that focuses on the processes that generate the empirical data,
which in this case means how individuals get sorted into neighborhoods. Such explanations generally fall under the rubric of selection arguments because they seek to understand how individuals and/or neighborhoods are “selected” into certain environmental contexts.
In fact, one of the major critiques of research on “neighborhood effects,” generally made by economists (e.g., Ludwig, 2002; Manski, 1993), is that it ignores potentially important selection processes that could generate empirical associations between neighborhood properties and individual health outcomes that are mere artifacts of individual-level causal processes. For example, individual-level health status may play an important role in determining how individuals sort themselves (or are sorted by broader macrosocial forces) into neighborhoods, such that less healthy people are selectively sorted into more disadvantaged neighborhood environments. As a result, the apparent associations between ecological properties of neighborhood environments, such as socioeconomic disadvantage, and individual-level health outcomes could be mere reflections of individual-level factors that are causally related to both health outcomes and sorting into residential neighborhood of residence. In other words, the correlation between disadvantaged neighborhoods and worse health outcomes could reflect compositional differences between neighborhoods rather than true contextual effects.
A recent body of research has taken up this issue directly by examining an ongoing housing program in five major cities across the United States (Boston, Baltimore, New York, Chicago, and Los Angeles) called the Moving to Opportunity program (Katz et al., 2001; Ludwig, Duncan, and Hirschfield, 2001). Participants were randomly assigned to one of two treatment groups—both groups received housing vouchers, but one group could use the voucher only to move to a neighborhood that had a sufficiently low poverty rate, while the other group could use the voucher to move to any neighborhood—or a control group, which received no voucher. Although this experimental design does not eliminate all sources of selection (for example, there is still selection in who takes up the treatment), issues of selective neighborhood sorting are much less of a concern because of the random assignment to treatment and control groups. Results from the Boston study reveal that adults in the experimental group (those who were given vouchers to move to more affluent neighborhoods) experienced improvements in self-rated health and mental health after they moved, and children in these families experienced fewer injuries and a lower probability of having an asthma attack (Katz et al., 2001).
In the following section we consider how selection processes may distort estimates of neighborhood effects and racial/ethnic health disparities in nonexperimental research through a case study of mortality in Chicago neighborhoods. Surprising patterns of racial/ethnic mortality disparities
across neighborhood contexts defined by socioeconomic disadvantage suggest that neighborhood selection processes may be more complex than commonly believed. In addition to the possibility that less healthy people are selectively sorted into the most disadvantaged neighborhood environments, we argue that in some contexts it is equally possible that less healthy people may be selectively sorted into more affluent neighborhood environments.
A Case Study of Mortality in Chicago Neighborhoods
In this section we present the results of a multilevel analysis on mortality in Chicago neighborhoods to illustrate the connection between neighborhood environments and racial/ethnic disparities in mortality, and also to suggest how attending to selection processes may be critical to advancing our understanding of these disparities. Our data set consists of vital statistics on all deaths in Chicago during 1990 and aggregate Census data from the same year. One obstacle to performing a multilevel analysis with vital statistics data is that there is no variation on the dependent variable because the records only include information on individuals who died, not survivors. However, by combining the vital statistics with Census data from the same year, we obtain information on cases of both mortality and survival within 144 sociodemographic strata, defined through a cross-classification of age (18 categories, as presented in Table 11-1), race/ethnicity (4 categories), and gender (2 categories).5 We can thus perform a two-level analysis of mortality rates for the age-, race-, and sex-specific demographic strata, which, in turn, are nested within 342 neighborhood clusters (aggregates of Census tracts).6 Henceforth we refer to the characteristics of each stratum (age, race/ethnicity, and sex) as “individual-level” covariates in our analysis.
Descriptive statistics on population and death counts by race/ethnicity, age, and gender are reported in Table 11-1. Whites are the largest racial/ ethnic group in the sample, accounting for just over 35 percent of the population and 50 percent of all deaths, followed by African Americans. The crude death rate is higher for whites than any other group, which, in part, is attributable to a higher number of whites at older, high-mortality risk ages. The age distributions for each racial/ethnic group are displayed in Table 11-2. Whites have the oldest age structure of all racial/ethnic groups, while Hispanics have the youngest.
Table 11-3 presents the results of our multilevel analysis of mortality. The first model contains only individual-level covariates for race/ethnicity (whites are the reference group), age (linear, squared, and cubed), and gender (males are the reference group).7 The results show that mortality is significantly higher among African Americans compared to whites, while
TABLE 11-1 Descriptive Statistics on Population and Deaths by Race/ Ethnicity, Age, and Gender
|
|
Population Frequency |
(%) |
Death Frequency |
(%) |
Crude Death Rate (per 1,000) |
|
N |
4,013,165 |
|
27,630 |
|
|
|
Race/ethnicity |
|||||
|
White |
1,407,925 |
(35.08) |
14,078 |
(50.95) |
10.00 |
|
African American |
1,271,609 |
(31.69) |
11,345 |
(41.06) |
8.92 |
|
Hispanic |
720,535 |
(17.95) |
1,894 |
(6.85) |
2.63 |
|
Other race |
613,096 |
(15.28) |
313 |
(1.13) |
0.51 |
|
Age |
|||||
|
<5 |
312,822 |
(7.79) |
806 |
(2.92) |
2.58 |
|
5-9 |
296,656 |
(7.39) |
232 |
(0.84) |
0.78 |
|
10-14 |
287,105 |
(7.15) |
159 |
(0.58) |
0.55 |
|
15-19 |
291,709 |
(7.27) |
350 |
(1.27) |
1.20 |
|
20-24 |
324,459 |
(8.08) |
383 |
(1.39) |
1.18 |
|
25-29 |
345,344 |
(8.61) |
513 |
(1.86) |
1.49 |
|
30-34 |
344,237 |
(8.58) |
693 |
(2.51) |
2.01 |
|
35-39 |
294,651 |
(7.34) |
809 |
(2.93) |
2.75 |
|
40-44 |
244,601 |
(6.09) |
821 |
(2.97) |
3.36 |
|
45-49 |
202,636 |
(5.05) |
918 |
(3.32) |
4.53 |
|
50-54 |
184,359 |
(4.59) |
1,137 |
(4.12) |
6.17 |
|
55-59 |
166,311 |
(4.14) |
1,488 |
(5.39) |
8.95 |
|
60-64 |
167,392 |
(4.17) |
2,289 |
(8.28) |
13.67 |
|
65-69 |
155,348 |
(3.87) |
2,883 |
(10.43) |
18.56 |
|
70-74 |
131,579 |
(3.28) |
3,205 |
(11.60) |
24.36 |
|
75-79 |
110,305 |
(2.75) |
3,403 |
(12.32) |
30.85 |
|
80-84 |
82,818 |
(2.06) |
3,217 |
(11.64) |
38.84 |
|
85+ |
70,833 |
(1.77) |
4,324 |
(15.65) |
61.04 |
|
Gender |
|||||
|
Male |
1,960,974 |
(48.86) |
14,888 |
(5,388.35) |
7.59 |
|
Female |
2,052,191 |
(51.14) |
12,742 |
(4,611.65) |
6.21 |
|
SOURCE: Chicago Vital Statistics and Census (1990). |
|||||
Hispanics and members of other races have significantly lower mortality rates than whites. In model 2, we introduce three neighborhood-level covariates, which are based on a principal components analysis (with a varimax rotation) of ten Census variables. These factor scores have been used in previous research on Chicago neighborhoods and the details of the principal components analysis are reported elsewhere (Sampson et al., 1997). The first neighborhood covariate represents the concentration of disadvantage and racial segregation (variables loading highly onto this factor include the percentage of poor families, families on public assistance, female-headed families, individuals in the labor force who are unemployed, individuals under the age of 18, and individuals who are African American). It has a significant positive effect on mortality, indicating that after controlling for age, race/ethnicity, and gender, the risk of mortality is still higher in
TABLE 11-2 Age Distribution of Chicago Population by Race/Ethnicity
|
|
Relative Frequency (%) |
|||
|
Age |
White |
African American |
Hispanic |
Other |
|
<5 |
5.9 |
8.3 |
9.4 |
8.2 |
|
5-9 |
5.4 |
8.0 |
8.9 |
8.0 |
|
10-14 |
5.0 |
8.1 |
8.5 |
7.8 |
|
15-19 |
5.2 |
8.2 |
8.3 |
8.1 |
|
20-24 |
7.6 |
7.4 |
8.9 |
8.8 |
|
25-29 |
8.3 |
8.0 |
9.1 |
8.9 |
|
30-34 |
8.9 |
8.0 |
8.3 |
8.4 |
|
35-39 |
7.8 |
6.9 |
7.0 |
7.1 |
|
40-44 |
6.5 |
5.9 |
5.6 |
5.9 |
|
45-49 |
5.4 |
5.1 |
4.6 |
4.9 |
|
50-54 |
5.0 |
4.9 |
4.0 |
4.2 |
|
55-59 |
4.8 |
4.3 |
3.5 |
3.7 |
|
60-64 |
5.2 |
4.3 |
3.2 |
3.4 |
|
65-69 |
5.2 |
3.8 |
2.7 |
3.1 |
|
70-74 |
4.8 |
3.0 |
2.2 |
2.6 |
|
75-79 |
4.1 |
2.4 |
2.1 |
2.4 |
|
80-84 |
2.9 |
1.8 |
1.9 |
2.3 |
|
85+ |
2.3 |
1.6 |
1.9 |
2.1 |
|
SOURCE: Chicago Vital Statistics and Census (1990). |
||||
disadvantaged neighborhoods. The second variable represents the concentration of Hispanic and immigrant populations, which is significantly protective against the risk of mortality in model 2. The third variable represents residential stability (based on the percentage of individuals who lived in the same house in 1985 and the percentage of homes that are owner occupied), and it also has a significant protective effect. Adding the three neighborhood-level covariates in model 2 reduces the estimated risk of being African American compared to white (as represented by the individual-level coefficient) by 79 percent, making it statistically nonsignificant, but it does not significantly change the protective effects associated with being Hispanic or belonging to another race.
In model 3, we allow racial/ethnic status to interact with age, gender, and neighborhood characteristics. Because race/ethnicity is now fully interacted with the other characteristics in the model, the racial/ethnic group coefficients in model 3 are no longer comparable to those in models 1 and 2. We focus our discussion of these results on the association between neighborhood disadvantage and mortality, and its implications for racial/ ethnic mortality disparities, because concentrated disadvantage is such a pivotal construct in neighborhood health research. An important result from model 3 is that the effect of neighborhood disadvantage varies signifi-
TABLE 11-3 Individual- and Neighborhood-Level Coefficients from Hierarchical Poisson Regressions of Mortality
|
|
(1) |
(2) |
(3) |
|||
|
Variable |
Coefficient |
T-ratio |
Coefficient |
T-ratio |
Coefficient |
T-ratio |
|
Individual level |
||||||
|
African American |
0.20 |
(701.16) |
0.04 |
(0.95) |
0.55 |
(8.15) |
|
Hispanic |
–0.95 |
(–1,722.91) |
–0.95 |
(–21.12) |
0.02 |
(0.32) |
|
Other race |
–2.70 |
(–2,124.74) |
–2.72 |
(–27.56) |
–2.22 |
(–16.37) |
|
Age |
0.07 |
(4,502.69) |
0.07 |
(64.65) |
0.08 |
(82.77) |
|
African American |
|
–0.02 |
(–22.03) |
|||
|
Hispanic |
–0.03 |
(–23.22) |
||||
|
Other |
–0.01 |
(–2.81) |
||||
|
Age squareda |
0.39 |
(1,586.70) |
0.38 |
(17.57) |
0.49 |
(17.34) |
|
African American |
|
–0.27 |
(–6.78) |
|||
|
Hispanic |
–0.40 |
(–8.17) |
||||
|
Othera |
–0.36 |
(–3.16) |
||||
|
Age cubed |
–0.01 |
(–1,084.13) |
–0.01 |
(–17.50) |
–0.01 |
(–19.39) |
|
Female |
–0.44 |
(–1,621.79) |
–0.45 |
(–30.32) |
–0.47 |
(–26.44) |
|
African American |
|
–0.07 |
(–2.53) |
|||
|
Hispanic |
0.02 |
(0.46) |
||||
|
Other |
0.07 |
(0.76) |
||||
|
Neighborhood level |
||||||
|
Concentrated disadvantage |
|
0.06 |
(3.76) |
–0.5 |
(–10.38) |
|
|
African American |
|
0.89 |
(15.68) |
|||
|
Hispanic |
0.66 |
(11.93) |
||||
|
Other |
0.02 |
(0.25) |
||||
|
Hispanic immigrant concentration |
|
–0.11 |
(–6.89) |
0.25 |
(8.26) |
|
|
African American |
|
–0.71 |
(–10.83) |
|||
|
Hispanic |
–0.14 |
(–3.20) |
||||
|
Other |
–0.38 |
(–4.97) |
||||
|
Residential stability |
–0.04 |
(–2.37) |
–0.07 |
(–2.20) |
||
|
African American |
|
–0.02 |
(–0.37) |
|||
|
Hispanic |
–0.03 |
(–0.76) |
||||
|
Other |
–0.50 |
(–6.50) |
||||
|
Intercept |
–4.88 |
(–16,266.80) |
–4.83 |
(–193.61) |
–5.60 |
(–101.67) |
|
aCoefficients have been multiplied by 1,000. SOURCE: Chicago Vital Statistics and Census (1990.) |
||||||
cantly across racial/ethnic groups. Among whites (the reference group), concentrated disadvantage is negatively related to mortality, which means that white mortality rates are actually higher in less disadvantaged (i.e., more affluent) neighborhoods—a very counterintuitive result that we will attempt to explain. However, for African Americans and Hispanics, concentrated disadvantage is associated with higher levels of mortality, a result that would be expected based on previous research.
To better illustrate what the results in model 3 imply about the neighborhood context of racial/ethnic disparities in mortality, we graph the age-mortality hazard curves by race/ethnicity and levels of neighborhood disadvantage in Figure 11-2. The main point of Figure 11-2 is that racial/ethnic mortality disparities vary as a function of both individual age and neighborhood disadvantage. As is the case in previous mortality research, we observe a black-white crossover in the mortality hazard curves, but with a distinctive twist involving the level of neighborhood disadvantage. At younger ages, African Americans living in highly disadvantaged neighborhoods (75th percentile of disadvantage) have the highest risk of mortality, but at about age 67, this risk is surpassed by whites living in low-disadvantage
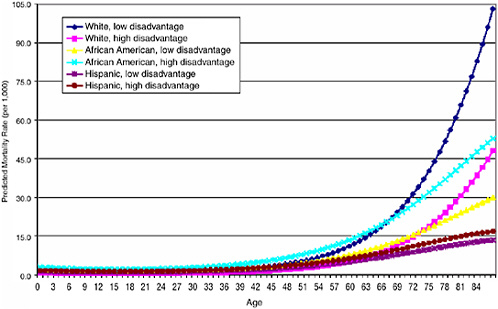
FIGURE 11-2 Model-based mortality rates by race/ethnicity and neighborhood disadvantage.
SOURCE: Chicago Vital Statistics and Census (1990).
neighborhoods (25th percentile of disadvantage), and these low-disadvantage whites continue to display the highest mortality rates at successively older ages. Waitzman and Smith (1998a) report a similar finding that mortality risk is lower in the 65-and-over age group for residents of poverty areas, except that they did not report interactions between poverty area residence and race, so it is not clear whether this effect is driven largely by older whites, as it is in our sample.
Needless to say, the finding that whites living in more affluent neighborhoods have the highest risk of mortality at older ages is somewhat counterintuitive, but at the same time it suggests some intriguing hypotheses about possible selection processes that could account for such results. Most speculation about the direction of selection bias in research on neighborhood effects and health presumes that estimates of their association may be overstated because of the potential for less healthy individuals to selectively reside in more disadvantaged neighborhoods. In other words, the correlation between disadvantaged neighborhoods and worse health outcomes could reflect compositional differences between neighborhoods rather than true contextual effects.
Our findings suggest that it may be equally important to consider selection processes through which less healthy individuals, particularly at older ages, are selected into more affluent neighborhood environments. For example, it is possible that nursing homes in Chicago and other cities may be located predominantly in more affluent neighborhoods, attracting a selectively frail older age population to these neighborhoods that is reflected in a higher risk of mortality. At the same time, those who survive to older ages in more disadvantaged neighborhoods may be selectively less frail because they have had to overcome greater ecological risks. These are examples of selection processes that would result in the counterintuitive greater mortality risk in affluent compared to disadvantaged neighborhood environments. Such processes could also vary across racial/ethnic groups if, for example, there is selective out-migration of healthier whites away from the city, particularly at older ages, but less out-migration for African Americans due to the constraints of a segregated housing market. In sum, there are plausible reasons why the surviving population of whites at older ages in more affluent neighborhoods may be selectively more frail than similarly situated African Americans. Ironically, the net effect of such adverse forms of selection among elderly residents of affluent neighborhoods could be to understate the risk associated with disadvantaged neighborhood environments.
We present this case study not only to underscore the importance of selection bias in neighborhood research, but also to suggest that much remains to be learned about the direction of this bias and its consequences for causal inferences about neighborhoods. Our analysis raises questions
about selection bias that we are admittedly not equipped to answer with our current data set, but it also poses a challenge for future research to better understand the ways in which health status may play a role in the processes through which individuals are sorted into neighborhoods. In short, research on neighborhoods and health could benefit from further development of Tilly’s second type of theory.
CONCLUSION
The recent explosion of studies on neighborhood environments and health has provided strong initial evidence that characteristics of neighborhood environments, particularly those relating to the concentration of disadvantage and segregation, are associated with a wide array of health outcomes and may also be implicated in explaining why there are persisting racial/ethnic disparities in so many health outcomes even after controlling for sociodemographic and behavioral characteristics of individuals. Yet much remains to be learned in this area of research. We now conclude with several suggestions on avenues for future research that require the most attention:
-
Collecting data on neighborhood mechanisms for health: One of the top priorities is to better understand the specific exposures that neighborhood environments offer and how they may be related to health. Socioeconomic disadvantage and segregation are undoubtedly key dimensions of neighborhood life, but researchers need to better understand how they are connected to social processes, institutions, sources of stress, and characteristics of the physical environment that may be more directly relevant to health. Some of the most notable advances in neighborhood research in recent years have been the development of research designs and methods that enable researchers to measure neighborhood social and institutional processes either through surveys or systematic social observation (Raudenbush and Sampson, 1999). This research has shown that community-based surveys can indeed yield reliable and valid measures of neighborhood characteristics when surveying multiple respondents living in the same ecological areas and using their collective assessment to build neighborhood indicators (e.g., Cook, Shagle, and Degirmencioglu, 1997; Elliott et al., 1996; Sampson et al., 1997), as opposed to a strategy of constructing neighborhood indicators based on a single individual’s report of his or her neighborhood. Another trend in this direction is the recent advance in collecting observational data on the physical and social features of neighborhood environments. This strategy, known as “systematic social observation” (Sampson and Raudenbush, 1999), is important for health research because it more directly captures the sights, sounds, and feel of neighbor-
-
hood environments that may be important for some health outcomes, particularly among children and the elderly, whose routine activity patterns may depend heavily on the microlevel conditions of the blocks in and around where they live. By observing block faces (one side of a street within a block), data can be aggregated to any level of analysis desired (e.g., block, block group, housing project, or neighborhood) to characterize social and physical characteristics. Such data can be exploited to build new measures of “microneighborhood” contexts.
-
Age- and race/ethnic-specific effects: By and large, most research on neighborhood context and health has focused on the main effects of neighborhood characteristics. Only a few studies have considered interactions between neighborhood characteristics and individual-level race/ethnicity (Pearl et al., 2001) and age (Bond Huie et al., 2002; Haan et al., 1987; LeClere et al., 1997, 1998; Rauh et al., 2001; Robert and Li, 2001; Waitzman and Smith, 1998a, 1998b). In our analysis of mortality, interactions revealed that racial/ethnic disparities in mortality vary as a function of both neighborhood characteristics and age. More research on how neighborhood effects vary across demographic subgroups could yield new insights into the connection between neighborhood environments and racial/ ethnic disparities in health and aging.
-
Selection processes and life-course perspectives: The issue of selection bias should be understood not only as a threat to causal inference, but also an opportunity to better understand important socioeconomic processes that may underlie racial/ethnic disparities in health (Palloni and Morenoff, 2001), such as the sorting of individuals into neighborhoods. Our multilevel analysis of mortality produced results that appeared to be counterintuitive until they were cast in the light of possible selection processes that could operate in some contexts to channel less healthy people from older age groups into more affluent urban neighborhoods and other forms of selection that may produce a selectively more healthy stock of survivors in poor urban environments. Researchers should thus attempt not only to control for selection, but also to study such processes more directly by collecting information on residential histories and integrating this analysis into the study of neighborhood effects on health. Understanding residential histories would also address concerns we have raised about the life course and timing of an individual’s exposure to neighborhood environments. Some sociologists have begun to consider the enduring effects of childhood community context and independent effects of adult community context on health-related outcomes (Axinn and Yabiku, 2001). This is precisely the kind of research that promises to yield a richer understanding of the multiple developmental influences that neighborhood environments may have across the life course. Investigating neighborhood effects on health from a life-course perspective requires the collection of longitudinal data on
-
both individuals and their neighborhoods. Some existing data sets offer these possibilities, including national studies, such as the Panel Study of Income Dynamics (http://www.isr.umich.edu/src/psid/), and local area studies, such as the Project on Human Development in Chicago Neighborhoods (http://phdcn.harvard.edu/).
-
Spatial perspectives on health: To gain a fuller appreciation of contextual effects on health it is also necessary to widen the geographic lens beyond the often arbitrary boundaries of statistically defined neighborhoods. A wider spatial perspective on health may also shed new light on racial/ethnic health disparities. For example, if African-American neighborhoods are embedded in more disadvantaged environments than are similarly endowed white neighborhoods, then the consequences of racial segregation may be greater and more systemic than previously thought (Morenoff et al., 2001). Patillo-McCoy’s (1999) ethnographic study of “Groveland,” a community in Chicago, suggests that black middle-class families face such a spatial (and structural) disadvantage. Despite networks of social control, she found that black middle-class families must constantly struggle to escape the problems of drugs, violence, and disorder that spill over from neighboring communities. Finally, from a public health viewpoint, understanding how and why spatial externalities occur may be critical in designing community intervention strategies. These findings carry with them both a caution that treating neighborhoods as “islands unto themselves” for the purposes of intervention is potentially misguided, but also the promise that if interventions can foster protective factors, such as social resources, they may spawn positive spatial externalities and thus benefit a wider geographic area.
ENDNOTES
REFERENCES
Aboderin, I., Kalache, A., Ben-Shlomo, Y., Lynch, J.W., Yajnik, C.S., and Kuh, D. (2002). Life course perspectives on coronary heart disease, stroke and diabetes. The evidence and implications for policy and research. Geneva, Switzerland: World Health Organization.
Acevedo-Garcia, D. (2000). Residential segregation and the epidemiology of infectious diseases. Social Science and Medicine, 6(1), 45-72.
Alter, D.A., Naylor, C.D., Austin, P., and Tu, J.V. (1999). Effects of socioeconomic status on access to invasive cardiac procedures and on mortality after acute myocardial infarction. New England Journal of Medicine, 341, 1359-1367.
Anderson, R.T., Sorlie, P., Backlund, E., Johnson, N., and Kaplan, G.A. (1997). Mortality effects of community socioeconomic status. Epidemiology, 8, 42-47.
Aneshensel, C.S., and Sucoff, C.A. (1996). The neighborhood context of adolescent mental health. Journal of Health and Social Behavior, 37, 293-310.
Anselin, L. (2001). Spatial externalities, spatial multipliers, and spatial econometrics. Unpublished manuscript, University of Illinois, Urbana-Champaign.
Axinn, W.G., and Yabiku, S.T. (2001). Social change, the social organization of families, and fertility limitation. American Journal of Sociology, 106, 1219-1261.
Balcazar, H., Aoyama, C., and Cai, X. (1991). Interpretative views on Hispanics’ perinatal problems of low birth weight and prenatal care. Public Health Reports, 106, 420-426.
Balfour, J.L., and Kaplan, G.A. (2002). Neighborhood environment and loss of physical function in older adults: Evidence from the Alameda County study. American Journal of Epidemiology, 155, 507-515.
Baller, R.D., Anselin, L., and Messner, S.F. (2001). Structural covariates of U.S. county homicide rates: Incorporating spatial effects. Criminology, 39, 561-590.
Barker, D.J.P. (1998). Mothers, babies, and health in later life. Edinburgh, Scotland: Churchill Livingstone.
Barnett, E., and Halverson, J. (2001). Local increases in coronary heart disease mortality among blacks and whites in the United States, 1985-1995. American Journal of Public Health, 91, 1499-1506.
Berkman, L.F., and Glass, T. (2000). Social integration, social networks, social support, and health . In I. Kawachi (Ed.), Social epidemiology (pp. 137-173). Oxford, England: Oxford University Press.
Bjorksten, B. (1999). The environmental influence on childhood asthma. Allergy, 54, 17-23.
Boardman, J.D., Finch, B.K., Ellison, C.G., Williams, D.R., and Jackson, J.S. (2001). Neighborhood disadvantage, stress, and drug use among adults. Journal of Health and Social Behavior, 42, 151-165.
Bond Huie, S.A., Hummer, R.A., and Rogers, R.G. (2002). Individual and contextual risk factors of death among race and ethnic groups in the United States. Journal of Health and Social Behavior, 43, 359-381.
Booth, M.L., Owen, N., Bauman, A., Clavisi, O., and Leslie, E. (2000). Social-cognitive and perceived environment influences associated with physical activity in older Australians. Preventive Medicine, 31, 15-22.
Bosma, H., van de Mheen, H.D., Borsboom, G.J. and Mackenbach, J.P. (2001). Neighborhood socioeconomic status and all-cause mortality. American Journal of Epidemiology, 153(4), 363-371.
Boyle, M.H., and Willms, J.D. (1999). Place effects for areas defined by administrative boundaries. American Journal of Epidemiology, 149, 577-585.
Buka, S.L., Brennan, R.T., Rich-Edwards, J.W., Raudenbush, S.W., and Earls, F. (2003). Neighborhood support and the birth weight of urban infants. American Journal of Epidemiology, 157(1), 1-8.
Burns, J.M., Baghurst, P.A., Sawyer, M.G., McMichael, A.J., and Tong, S.L. (1999). Lifetime low-level exposure to environmental lead and children’s emotional and behavioral development at ages 11-13 years: The Port Pirie Cohort Study. American Journal of Epidemiology, 149, 740-749.
Carstensen, L.L., Isaacowitz, D.M., and Charles, S.T. (1999). Taking time seriously: A theory of socioemotional selectivity. American Psychologist, 54, 165-181.
Caspi, A., Taylor, A., Moffitt, T.E., and Plomin, R. (2000). Neighborhood deprivation affects children’s mental health: Environmental risks identified in a genetic design. Psychological Science, 11, 338-342.
Chandola, T. (2001). The fear of crime and area differences in health. Health and Place, 7, 105-116.
Cohen, D., Spear, S., Scribner, R., Kissinger, P., Mason, K., and Wildgen, J. (2000). “Broken windows” and the risk of gonorrhea. American Journal of Public Health, 90, 230-236.
Cohen, J., and Tita, G. (1999). Diffusion in homicide: Exploring a general method for detecting spatial diffusion processes. Journal of Quantitative Criminology, 15, 451-493.
Collins, J.W., Jr., and David, R.J. (1997). Urban violence and African-American pregnancy outcome: An ecologic study. Ethnicity and Disease, 7, 184-190.
Cook, T.D., Shagle, S.C., and Degirmencioglu, S.M. (1997). Capturing social process for testing mediational models of neighborhood effects. In J. Brooks-Gunn, G.J. Duncan, and J. L. Aber (Eds.), Neighborhood poverty: Policy implications in studying neighborhoods (pp. 94-119). New York: Russell Sage Foundation.
Cooper, R.S., Kennelly, J.F., Durazo-Arvizu, R., Oh, H., Kaplan, G., and Lynch, J. (2001). Relationship between premature mortality and socioeconomic factors in black and white populations of US metropolitan areas. Public Health Reports, 116, 464-474.
Coulton, C.J., Korbin, J., Chan, T., and Su, M. (2001). Mapping residents’ perceptions of neighborhood boundaries: A methodological note. American Journal of Community Psychology, 29, 371-383.
Cubbin, C., LeClere, F.B., and Smith, G.S. (2000). Socioeconomic status and injury mortality: Individual and neighbourhood determinants. Journal of Epidemiology and Community Health, 54, 517-524.
Cutrona, C.E., Russell, D.W., Hessling, R.M., Adama Brown, P., and Murry, V. (2000). Personality processes and individual differences—direct and moderating effects of community context on the psychological well-being of African American women. Journal of Personality and Social Psychology, 79, 1088-1101.
Davey Smith, G., and Lynch, J.W. (2002). Socioeconomic differentials. In D. Kuh and Y. Ben-Shlomo (Eds.), A life course approach to chronic disease epidemiology. Oxford, England: Oxford University Press.
Davey Smith, G., Hart, C., Watt, G., Hole, D., and Hawthorne, V. (1998). Individual social class, area-based deprivation, cardiovascular disease risk factors, and mortality: The Renfrew and Paisley study. Journal of Epidemiology and Community Health, 52, 399.
Davey Smith, G., Gunnell, D., and Ben Shlomo, Y. (2000). Life course approaches to socioeconomic differentials in cause-specific adult mortality. In D. Leon and G. Walt (Eds.), Poverty, inequality and health (pp. 88-124). Oxford, England: Oxford University Press.
Davey Smith, G., Ben-Shlomo, Y., and Lynch, J.W. (2002). Life course approaches to inequalities in coronary heart disease risk. In S. Stansfeld and M. Marmot (Eds.), Stress and the heart: Psychosocial pathways to coronary heart disease (pp. 20-49). London: British Medical Journal Books.
Diehr, P., Koepsell, T., Cheadle, A., Psaty, B.M., Wagner, E., and Curry, S. (1993). Do communities differ in health behaviors? Journal of Clinical Epidemiology, 46, 1141-1149.
Diez-Roux, A.V. (2001). Investigating neighborhood and area effects on health. American Journal of Public Health, 91, 1783-1789.
Diez-Roux, A.V. (2002). Invited commentary: Places, people, and health. American Journal of Epidemiology, 155, 516-519.
Diez-Roux, A.V., Nieto, F.J., Muntaner, C., Tyroler, H.A., Comstock, G.W., Shahar, E., Cooper, L.S., Watson, R.L., and Szklo, M. (1997). Neighborhood environments and coronary heart disease: A multilevel analysis. American Journal of Epidemiology, 146, 48-63.
Dorling, D., Mitchell, R., Shaw, M., Orford, S., and Smith, G.D. (2000). The ghost of Christmas past: Health effects of poverty in London in 1896 and 1991. British Medical Journal, 321, 1547-1551.
Duncan, C., Jones, K., and Moon, G. (1998). Smoking and deprivation: Are there neighbourhood effects? Social Science and Medicine, 48(4), 497-507.
Ecob, R. (1996). A multilevel modelling approach to examining the effects of area of residence on health and functioning. Journal of the Royal Statistical Society, Series A (General), 159, 61.
Ecob, R., and Jones, K. (1998). Mortality variations in England and Wales between types of place: An analysis of the ONS longitudinal study. Social Science and Medicine, 47(12), 2055-2067.
Ecob, R., and Macintyre, S. (2000). Small area variations in health related behaviours: Do these depend on the behaviour itself, its measurement, or on personal characteristics? Health and Place, 6, 261-274.
Eggleston, P.A., Buckley, T.J., Breysse, P.N., Wills-Karp, M., Kleeberger, S.R., and Jaakkola, J.J. (1999). The environment and asthma in U.S. inner cities. Environmental Health Perspectives, 107, 439-450.
Ellen, I.G. (2000). Is segregation really bad for your health? The case of low birthweight. Brookings-Wharton Papers on Urban Affairs, 1, 203-229.
Ellen, I.G., Mijanovich, T., and Dillman, K.-N. (2001). Neighborhood effects on health: Exploring the links and assessing the evidence. Journal of Urban Affairs, 23, 391-408.
Elliott, D.S., Wilson, W.J., Huizinga, D., Sampson, R.J., Elliott, A., and Rankin, B. (1996). The effects of neighborhood disadvantage on adolescent development. Journal of Research in Crime and Delinquency, 33, 389-427.
Elreedy, S., Krieger, N., Ryan, P.B., Sparrow, D., Weiss, S.T., and Hu, H. (1999). Relations between individual and neighborhood-based measures of socioeconomic position and bone lead concentrations among community-exposed men: The Normative Aging Study. American Journal of Epidemiology, 150, 129-141.
Fick, A.C., and Thomas, S.M. (1995). Growing up in a violent environment: Relationship to health-related beliefs and behaviors. Youth and Society, 27(2), 136-148.
Finch, B.K., Vega, W.A., and Kolody, B. (2001). Substance use during pregnancy in the state of California, USA. Social Science and Medicine, 52, 571-583.
Fratiglioni, L., Wang, H.X., Ericsson, K., Maytan, M., and Winblad, B. (2000). Influence of social network on occurrence of dementia: A community-based longitudinal study. Lancet, 355, 1315-1319.
Ganz, M.L. (2000). The relationship between external threats and smoking in central Harlem. American Journal of Public Health, 90, 367-371.
Garg, P.P., Diener-West, M., and Powe, N.R. (2001). Income-based disparities in outcomes for patients with chronic kidney disease. Seminars in Nephrology, 21, 377-385.
Geis, K.J., and Ross, C.E. (1998). A new look at urban alienation: The effect of neighborhood disorder on perceived powerlessness. Social Psychology Quarterly, 61, 232-246.
Gephart, M.A. (1997). Neighborhoods and communities as contexts for development. In J. Brooks-Gunn, G.J. Duncan, and J.L. Aber (Eds.), Neighborhood poverty: Volume II. Context and consequences for children (pp. 1-43). New York: Russell Sage Foundation.
Geronimus, A.T. (1992). The weathering hypothesis and the health of African-American women and infants: Evidence and speculations. Ethnicity and Disease, 2, 207-221.
Geronimus, A., and Bound, J. (1998). Use of Census-based aggregate variables to proxy for socioeconomic group: Evidence from national samples. American Journal of Epidemiology, 148, 475-486.
Gorman, B.K. (1999). Racial and ethnic variation in low birthweight in the United States: Individual and contextual determinants. Health and Place, 5, 195-207.
Grannis, R. (1998). The importance of trivial streets: Residential streets and residential segregation. American Journal of Sociology, 103, 1530-1564.
Haan, M., Kaplan, G.A., and Camacho, T. (1987). Poverty and health: Prospective evidence from the Alameda County study. American Journal of Epidemiology, 125, 989-998.
Harding, J.E. (2001). The nutritional basis of the fetal origins of adult disease. International Journal of Epidemiology, 30, 15-23.
Hart, C., Ecob, R., and Smith, G.D. (1997). People, places and coronary heart disease risk factors: A multilevel analysis of the Scottish Heart Health Study archive. Social Science and Medicine, 45, 893-902.
Hart, C.L., Hole, D.J., and Smith, G.D. (2000). Influence of socioeconomic circumstances in early and later life on stroke risk among men in a Scottish cohort study. Stroke, 31, 2093-2097.
Hertzman, C., Power, C., Matthews, S., and Manor, O. (2001). Using an interactive framework of society and life course to explain self-rated health in early adulthood. Social Science and Medicine, 53, 1575-1585.
House, J.S. (2002). Understanding social factors and inequalities in health: 20th century progress and 21st century prospects. Journal of Health and Social Behavior, 43, 125-143.
House, J.S., Landis, K.R., and Umberson, D. (1988). Social relationships and health. Science, 241, 540-554.
Howel, D., Darnell, R., and Pless-Mulloli, T. (2001). Children’s respiratory health and daily particulate levels in 10 nonurban communities. Environmental Research, 87, 1-9.
Hummer, R.A., Rogers, R.G., and Eberstein, I.W. (1998). Sociodemographic differentials in adult mortality: A review of analytic approaches. Population and Development Review, 24(3), 553-578.
Humpel, N., Owen, N., and Leslie, E. (2002). Environmental factors associated with adults’ participation in physical activity: A review. American Journal of Preventive Medicine, 22, 188-199.
Humphreys, K., and Carr-Hill, R. (1991). Area variations in health outcomes: Artifact or ecology. International Journal of Epidemiology, 20, 251-258.
Iwashyna, T.J., Christakis, N.A., and Becker, L.B. (1999). Neighborhoods matter: A population-based study of provision of cardiopulmonary resuscitation. Annals of Emergency Medicine , 34, 459-468.
Kalff, A.C., Kroes, M., Vles, J.S., Hendriksen, J.G., Feron, F.J., Steyaert, J., van Zeben, T.M., Jolles, J., and van Os, J. (2001). Neighbourhood level and individual level SES effects on child problem behaviour: A multilevel analysis. Journal of Epidemiology and Community Health, 55, 246-250.
Kaplan, G.A. (1996). People and places: Contrasting perspectives on the association between social class and health. International Journal of Health Services, 26, 507-521.
Karvonen, S., and Rimpela, A. (1996). Socio-regional context as a determinant of adolescents’ health behaviour in Finland. Social Science and Medicine, 43, 1467-1474.
Karvonen, S., and Rimpela, A.H. (1997). Urban small area variation in adolescents’ health behaviour. Social Science and Medicine, 45, 1089-1098.
Katz, L.F., Kling, J.R., and Liebman, J.B. (2001). Moving to opportunity in Boston: Early results of a randomized mobility experiment. Quarterly Journal of Economics, 116, 607-654.
Kleinschmidt, I., Hills, M., and Elliott, P. (1995). Smoking behavior can be predicted by neighborhood deprivation measures. Journal of Epidemiology and Community Health, 49, S72-S77.
Koopman, J.S., and Lynch, J.W. (1999). Individual causal models and population system models in epidemiology. American Journal of Public Health, 89, 1170-1174.
Krause, N. (1991). Stress and isolation from close ties in later life. Journals of Gerontology, 46, S183-S194.
Krieger, N. (1992). Overcoming the absence of socioeconomic data in medical records: Validation and application of a Census-based methodology. American Journal of Public Health, 82, 703-710.
Krieger, N. (1994). Epidemiology and the web of causation: Has anyone seen the spider? Social Science and Medicine, 39, 887-903.
Krieger, N. (1999). Sticky webs, hungry spiders, buzzing flies, and fractal metaphors: On the misleading juxtaposition of “risk factor” versus “social” epidemiology. Journal of Epidemiology and Community Health, 53, 678-680.
Kuh, D., and Ben Shlomo, Y. (1997). A life course approach to chronic disease epidemiology. Oxford, England: Oxford University Press.
LaVeist, T.A. (1993). Segregation, poverty, and empowerment: Health consequences for African Americans. Milbank Quarterly, 71, 41-64.
LaVeist, T.A., and Wallace, J.M., Jr. (2000). Health risk and inequitable distribution of liquor stores in African American neighborhoods. Social Science and Medicine, 51, 613-617.
LeClere, F.B., Rogers, R.G., and Peters, K.D. (1997). Ethnicity and mortality in the United States: Individual and community correlates. Social Forces, 76, 169-198.
LeClere, F.B., Rogers, R.G., and Peters, K. (1998). Neighborhood social context and racial differences in women’s heart disease mortality. Journal of Health and Social Behavior, 39, 91-108.
Lee, R.E., and Cubbin, C. (2002). Neighborhood context and youth cardiovascular health behaviors. American Journal of Public Health, 92, 428-436.
Leon, D. (2001a). Common threads: Underlying components of inequalities in mortality between and within countries. In D. Leon and G. Walt (Eds.), Poverty, inequality and health (pp. 58-87). Oxford, England: Oxford University Press.
Leon, D.A. (2001b). Commentary: Getting to grips with fetal programming—aspects of a rapidly evolving agenda. International Journal of Epidemiology, 30, 96-98.
Leon, D.A., and Davey Smith, G. (2000). Infant mortality, stomach cancer, stroke, and coronary heart disease: Ecological analysis. British Medical Journal, 320, 1705-1706.
Leventhal, T., and Brooks-Gunn, J. (2000). The neighborhoods they live in: The effects of neighborhood residence on child and adolescent outcomes. Psychological Bulletin, 126(2), 309-337.
Lin, N., and Ensel, W.M. (1989). Life stress and health: Stressors and resources. American Sociological Review, 54, 382-399.
Ludwig, J. (2002). Neighborhood effects and self-selection. Unpublished manuscript, Georgetown Public Policy Institute.
Ludwig, J., Duncan, G.J., and Hirschfield, P. (2001). Urban poverty and juvenile crime: Evidence from a randomized housing-mobility experiment. Quarterly Journal of Economics, 116, 655-679.
Macintyre, S., MacIver, S., and Sooman, A. (1993). Area, class and health: Should we be focusing on places or people? Journal of Social Policy, 22, 213-234.
Malmstrom, M., Sundquist, J., and Johansson, S.E. (1999). Neighborhood environment and self-reported health status: A multilevel analysis. American Journal of Public Health, 89, 1181-1186.
Malmstrom, M., Johansson, S., and Sundquist, J. (2001). A hierarchical analysis of long-term illness and mortality in socially deprived areas. Social Science and Medicine, 53(3), 265-277.
Manski, C.F. (1993). Identification of endogenous social effects—the reflection problem. Review of Economic Studies, 60, 531-542.
Margolin, G., and Gordis, E.B. (2000). The effects of family and community violence on children. Annual Review of Psychology, 51, 445-479.
Marmot, M.G., Fuhrer, R., Ettner, S.L., Marks, N.F., Bumpass, L.L., and Ryff, C.D. (1998). Contribution of psychosocial factors to socioeconomic differences in health. Milbank Quarterly, 76, 403-448.
Massey, D.S., and Denton, N.A. (1993). American apartheid: Segregation and the making of the underclass. Cambridge, MA: Harvard University Press.
Matteson, D., Burr, J., and Marshall, J. (1998). Infant mortality: A multi-level analysis of individual and community risk factors. Social Science and Medicine, 47, 1841-1854.
McEwen, B.S. (1998). Protective and damaging effects of stress mediators. New England Journal of Medicine, 338, 171-179.
McMichael, A.J. (1999). Prisoners of the proximate: Loosening the constraints on epidemiology in an age of change. American Journal of Epidemiology, 149, 887-897.
Merlo, J., Ostergren, P.O., Hagberg, O., Lindstrom, M., Lindgren, A., Melander, A., Rastam, L., and Berglund, G. (2001). Diastolic blood pressure and area of residence: Multilevel versus ecological analysis of social inequity. Journal of Epidemiology and Community Health, 55, 791-798.
Morenoff, J.D. (2003). Neighborhood mechanisms and the spatial dynamics of birthweight. American Journal of Sociology, 108, 976-1017.
Morenoff, J.D., and Sampson, R.J. (1997). Violent crime and the spatial dynamics of neighborhood transition: Chicago, 1970-1990. Social Forces, 76, 31-64.
Morenoff, J.D., Sampson, R.J., and Raudenbush, S.W. (2001). Neighborhood inequality, collective efficacy, and the spatial dynamics of urban violence. Criminology, 39, 517-559.
Morgan, M., and Chinn, S. (1983). ACORN group, social class, and child health. Journal of Epidemiology and Community Health, 37, 196-203.
Morrison, R.S., Wallenstein, S., Natale, D.K., Senzel, R.S., and Huang, L.L. (2000). “We don’t carry that”—Failure of pharmacies in predominantly nonwhite neighborhoods to stock opioid analgesics. New England Journal of Medicine, 342, 1023-1026.
Murray, C.J.L., Michaud, C.M., McKenna, M.T., and Marks, J.S. (1998). U.S. patterns of mortality by county and race: 1965-1994. Harvard Center for Population and Development Studies (Monograph Series). Cambridge, MA.
Northridge, M.E., Yankura, J., Kinney, P.L., Santella, R.M., Shepard, P., Riojas, Y., Aggarwal, M., and Strickland, P. (1999). Diesel exhaust exposure among adolescents in Harlem: A community-driven study. American Journal of Public Health, 89, 998-1002.
O’Campo, P., Xue, X., and Wang, M.C. (1997). Neighborhood risk factors for low birthweight in Baltimore: A multilevel analysis . American Journal of Public Health, 87, 1113-1118.
Palloni, A., and Morenoff, J.D. (2001). Interpreting the paradoxical in the Hispanic paradox: Demographic and epidemiologic approaches. Annals of the New York Academy of Sciences, 954, 140-175.
Pandya, R.J., Solomon, G., Kinner, A., and Balmes, J.R. (2002). Diesel exhaust and asthma: Hypotheses and molecular mechanisms of action. Environmental Health Perspectives, 110, 103-112.
Park, R. (1916). Suggestions for the investigations of human behavior in the urban environment. American Journal of Sociology, 20, 577-612.
Park, R.E., Burgess, E.W., and McKenzie, R.D. (1967). The city. Chicago: University of Chicago Press.
Patillo-McCoy, M. (1999). Black picket fences: Privilege and peril among the black middle class. Chicago: University of Chicago Press.
Pearce, N. (1996). Traditional epidemiology, modern epidemiology, and public health. American Journal of Public Health, 86, 678-683.
Pearl, M., Braveman, P., and Abrams, B. (2001). The relationship of neighborhood socioeconomic characteristics to birthweight among 5 ethnic groups in California. American Journal of Public Health, 91, 1808-1814.
Pickett, K.E., and Pearl, M. (2001). Multilevel analyses of neighbourhood socioeconomic context and health outcomes: A critical review. Journal of Epidemiology and Community Health, 55, 111-122.
Polednak, A.P. (1996). Trends in US urban black infant mortality, by degree of residential segregation. American Journal of Public Health, 86, 723-726.
Raudenbush, S.W., and Sampson, R.J. (1999). Ecometrics: Toward a science of assessing ecological settings, with application to the systematic social observation of neighborhoods. Sociological Methodology, 29, 1-41.
Rauh, V.A., Andrews, H.F., and Garfinkel, R.S. (2001). The contribution of maternal age to racial disparities in birthweight: A multilevel perspective. American Journal of Public Health, 91, 1815-1824.
Reading, R., Langford, I.H., Haynes, R., and Lovett, A. (1999). Accidents to preschool children: Comparing family and neighbourhood risk factors. Social Science and Medicine, 48, 321-330.
Reijneveld, S.A., and Schene, A.H. (1998). Higher prevalence of mental disorders in socioeconomically deprived urban areas in The Netherlands: Community or personal disadvantage? Journal of Epidemiology and Community Health, 52, 2-7.
Robert, S.A. (1998). Community-level socioeconomic status effects on adult health. Journal of Health and Social Behavior, 39, 18-38.
Robert, S.A. (1999). Socioeconomic position and health: The independent contribution of community socioeconomic context. Annual Review of Sociology, 25, 489-516.
Robert, S.A., and Li, L.W. (2001). Age variation in the relationship between community socioeconomic status and adult health. Research on Aging, 23(2), 234-259.
Roberts, E.M. (1997). Neighborhood social environments and the distribution of low birthweight in Chicago. American Journal of Public Health, 87, 597-603.
Ross, C.E. (2000a). Neighborhood disadvantage and adult depression. Journal of Health and Social Behavior, 41, 177-187.
Ross, C.E. (2000b). Walking, exercising, and smoking: Does neighborhood matter? Social Science and Medicine, 51, 265-274.
Ross, C.E., and Jang, S.J. (2000). Neighborhood disorder, fear, and mistrust: The buffering role of social ties with neighbors . American Journal of Community Psychology, 28, 401-420.
Ross, C.E., Reynolds, J.R., and Geis, K.J. (2000). The contingent meaning of neighborhood stability for residents’ psychological well-being. American Sociological Review, 65, 581-597.
Rowley, D.L., Hogue, C.J.R., Blackmore, C.A., Ferre, C.D., Hatfield-Timajchy, K., Branch, P., and Atrash, H.K. (1993). Preterm delivery among African-American women: A research strategy. American Journal of Preventive Medicine, 9, 1-6.
Sampson, R.J., and Morenoff, J.D. (2001, July). Durable inequality: Spatial dynamics, social processes, and the persistence of poverty in Chicago neighborhoods. Paper presented at “Poverty Traps” Conference, Santa Fe Institute, CA.
Sampson, R.J., and Raudenbush, S.W. (1999). Systematic social observation of public spaces: A new look at disorder in urban neighborhoods. American Journal of Sociology, 105, 603-651.
Sampson, R.J., Raudenbush, S.W., and Earls, F. (1997). Neighborhoods and violent crime: A multilevel study of collective efficacy. Science, 277, 918-924.
Sampson, R.J., Morenoff, J.D., and Earls, F. (1999). Beyond social capital: Spatial dynamics of collective efficacy for children. American Sociological Review, 64, 633-660.
Sampson, R.J., Morenoff, J.D., and Gannon-Rowley, T. (2002). Assessing “neighborhood effects”: Social processes and new directions in research. Annual Review of Sociology, 28, 443-478.
Schalick, L.M., Hadden, W.C., Pamuk, E., Navarro, V., and Pappas, G. (2000). The widening gap in death rates among income groups in the United States from 1967 to 1986. International Journal of Health Services, 30, 13-26.
Schroeder, J.R., Latkin, C.A., Hoover, D.R., Curry, A.D., Knowlton, A.R., and Celentano, D.D. (2001). Illicit drug use in one’s social network and in one’s neighborhood predicts individual heroin and cocaine use. Annals of Epidemiology, 11, 389-394.
Schulz, A., Williams, D., Israel, B., Becker, A., Parker, E., James, S.A., and Jackson, J. (2000). Unfair treatment, neighborhood effects, and mental health in the Detroit metropolitan area. Journal of Health and Social Behavior, 41, 314-332.
Schwartz, S., Susser, E., and Susser, M. (1999). A future for epidemiology? Annual Review of Public Health, 20, 15-35.
Scribner, R. (1996). Editorial: Paradox as paradigm—the health outcomes of Mexican Americans. American Journal of Public Health, 86, 303-305.
Selner-O’Hagan, M.B., Kindlon, D.J., and Buka, S.L. (1998). Assessing exposure to violence in urban youth. The Journal of Child Psychology and Psychiatry and Allied Disciplines, 39, 215-224.
Shouls, S., Congdon, P., and Curtis, S. (1996). Modelling inequality in reported long term illness in the UK: Combining individual and area characteristics. Journal of Epidemiology and Community Health, 50, 66-76.
Singer, B.H., and Ryff, C.D. (Eds.). (2001). New horizons in health: An integrative approach. Washington, DC: National Academy Press.
Sloggett, A., and Joshi, H. (1994). Higher mortality in deprived areas: Community or personal disadvantage? British Medical Journal, 309, 1470-1474.
Sloggett, A., and Joshi, H. (1998). Deprivation indicators as predictors of life events 1981-1992 based on the UK ONS Longitudinal Study. Journal of Epidemiology and Community Health, 52, 228-233.
Smith, W.R., Frazee, S.G., and Davison, E.L. (2000). Furthering the integration of routine activity and social disorganization theories: Small units of analysis and the study of street robbery as a diffusion process. Criminology, 38, 489-523.
Sooman, A., Macintyre, S., and Anderson, A. (1993). Scotland’s health—a more difficult challenge for some? The price and availability of healthy foods in socially contrasting localities in the west of Scotland. Health Bulletin, 51, 276-284.
Stafford, M., Bartley, M., Mitchell, R., and Marmot, M. (2001). Characteristics of individuals and characteristics of areas: Investigating their influence on health in the Whitehall II study. Health and Place, 7, 117-129.
Sundquist, J., Malmstrom, M., and Johansson, S.E. (1999). Cardiovascular risk factors and the neighbourhood environment: A multilevel analysis. International Journal of Epidemiology, 28, 841-845.
Susser, M. (1998). Does risk factor epidemiology put epidemiology at risk? Peering into the future. Journal of Epidemiology of Community Health, 52, 608-611.
Suttles, G.D. (1972). The social construction of communities. Chicago: University of Chicago Press.
Tilly, C. (2002). Event catalogs as theories. Sociological Theory, 20, 248-254.
Veugelers, P.J., Yip, A.M., and Kephart, G. (2001). Proximate and contextual socioeconomic determinants of mortality: Multilevel approaches in a setting with universal health care coverage. American Journal of Epidemiology, 154, 725-732.
Waitzman, N.J., and Smith, K.R. (1998a). Phantom of the area: Poverty-area residence and mortality in the United States. American Journal of Public Health, 88, 973-976.
Waitzman, N.J., and Smith, K.R. (1998b). Separate but lethal: The effects of economic segregation on mortality in metropolitan America. Milbank Quarterly, 76, 341-373.
Warr, M. (1994). Public perceptions and reactions to violent offending and victimization. In A.J. Reiss, Jr., and J.A. Roth (Eds.), Understanding and preventing violence. Vol. 4: Consequences and control (pp. 1-66). Washington, DC: National Academy Press.
Warr, M., and Ellison, C.G. (2000). Rethinking social reactions to crime: Personal and altruistic fear in family households. American Journal of Sociology, 106, 551-578.
Weed, D.L. (1998). Beyond black box epidemiology. American Journal of Public Health, 88, 12-14.
Williams, D.R., and Collins, C. (1995a). US socioeconomic and racial differences in health: Patterns and explanations. Annual Review of Sociology, 21, 349-386.
Williams, D.R., and Collins, C. (1995b). Racial residential segregation: A fundamental cause of racial disparities in health. Public Health Reports, 116, 404-416.
Wilson, D.K., Kliewer, W., Plybon, L., and Sica, D.A. (2000). Socioeconomic status and blood pressure reactivity in healthy black adolescents. Hypertension, 35, 496-500.
Wilson, J., and Musick, M. (1999). The effects of volunteering on the volunteer. Law and Contemporary Problems, 62(4), 141-168.
Winship, C. (2002, July). Counterfactual models of causal inference: Useful or useless? Presentation made at University of Michigan, Department of Sociology Colloquium.
Yen, I.H., and Kaplan, G.A. (1999). Neighborhood social environment and risk of death: Multilevel evidence from the Alameda County study. American Journal of Epidemiology, 149, 898-907.
Yen, I.H., and Syme, S.L. (1999). The social environment and health: A discussion of the epidemiologic literature. Annual Review of Public Health, 20, 287-308.
Zapata, B.C., Rebolledo, A., Atalah, E., Newman, B., and King, M.C. (1992). The influence of social and political violence on the risk of pregnancy complications. American Journal of Public Health, 82, 685-690.












































