13
Cumulative Psychosocial Risks and Resilience: A Conceptual Perspective on Ethnic Health Disparities in Late Life
Hector F. Myers and Wei-Chin Hwang
Over the past decade, concern has been growing about society’s ability to meet the mental health needs of elderly Americans in certain racial/ethnic groups. This issue has become particularly salient given the rapid increase in the U.S. elderly population. In fact, between the years of 1990 and 2000, the elderly population in the United States increased 12 percent, and elderly Americans currently comprise 12.4 percent of the U.S. population (U.S. Census Bureau, 2001). Moreover, the population of racial/ethnic elderly is estimated to be increasing at a faster rate than that of whites (Ruiz, 1995).
Despite these concerns, relatively little attention have been given to studying the mental health needs of aging ethnic minorities. In this chapter, we review the extant literature on ethnic disparities in mental health in late life, using depression as an illustrative disorder. We discuss methodological and conceptual gaps in the literature, and we review available clinical and epidemiological evidence. Moreover, we provide a conceptual framework for understanding the relationships among ethnicity, age, and well-being for elderly minority populations. Specifically, we present a biopsychosocial model of cumulative psychological and physical vulnerability and resilience in later life in which chronic stress burden and psychosocial resources for coping are hypothesized as playing a significant role in accounting for ethnic disparities in mental health. Implications and suggestions for future research are discussed.
AGING AND DEPRESSION
Because of a number of conceptual, diagnostic, and methodological challenges in studying depression in the elderly, findings from research
studies have been mixed, with most studies reporting lower prevalence of depression in the elderly (Regier et al., 1988), and some studies showing higher prevalence (Blazer, Burchett, Service, and George, 1991). Similar trends in low prevalence of mood disorders among ethnic elders also have been reported (Weissman, Bruce, Leaf, Florio, and Holzer, 1991), with no significant overall differences between groups in the Epidemiological Catchment Area (ECA) study (George, Blazer, Winfield-Laird, Leaf, and Fischbach, 1988). It would seem that healthy, functioning older adults are at no greater risk for becoming depressed. Instead, age-related effects may be attributable to physical health problems, functional and cognitive disability, chronic illness, low social support, and financial difficulties (Blazer et al., 1991; Roberts, Kaplan, Shema, and Strawbridge, 1997a).
Nevertheless, a number of methodological limitations may lead to underestimates in rates of depression in community studies. Karel (1997) noted that low prevalence rates of major depression among older adults may reflect (1) invalid measurement of depression in older adults (e.g., diagnostic difficulties, symptoms being misattributed to medical causes, symptom recall, and older adults being viewed as less likely to be functionally impaired by depressive symptoms), (2) sampling bias (e.g., older adults may have died, may be unable to participate due to illness and disability, and may be institutionalized or residing in community dwellings for the elderly), or (3) cohort effects due to sociocultural changes (i.e., rates of depression increase in cohorts born after World War II). Several studies have confirmed that rates of depression are increasing in the United States and worldwide (Cross-National Collaborative Group, 1992).
In examining depression in the elderly, it is also important to distinguish between recurrent illness that began earlier in life and first onset illness that manifests itself in late life. Early onset depression has been associated with a more malignant course (Klein et al., 1999; Lewinsohn, Fenn, Stanton, and Franklin, 1986; Sorenson, Rutter, and Aneshensel, 1991), greater vulnerability to chronic life stress (Hammen, Davila, Brown, Gitlin, and Ellicott, 1992), greater psychiatric comorbidity (Kasch and Klein, 1996; Lewinsohn, Rohde, Seeley, and Fischer, 1991), and greater genetic liability (Klein, Taylor, Harding, and Dickstein, 1988; Lyons et al., 1998). Early disorder onset is also associated with greater family psychiatric burden, neuroticism, and dysfunctional past maternal relationships (Brodaty et al., 2001; Van den Berg et al., 2001). On the other hand, first episode of depression in later life is associated with greater medical disability, and decreased neuropsychological and psychophysiological functioning (Lewinsohn et al., 1991). Therefore, it is important to distinguish between depressive subgroups that may possess different etiological pathways: (1) those with early onset and longstanding psychobiological and familial vulnerability, who carry this risk for recurrence into old age; (2) those who
become depressed as seniors, perhaps as a reaction to severe life stress; and (3) those whose depression may be associated with significant medical and vascular dysfunction and disability (Van den Berg et al., 2001).
ETHNIC DISPARITIES IN DEPRESSION
Results from large epidemiological studies on ethnic differences in the prevalence of major depression in the United States are mixed, with African Americans and Asian Americans showing lower rates of major depressive disorder (MDD), and Hispanics showing higher rates than whites (Blazer, Kessler, McGonagle, and Swartz, 1994; Somervell, Leaf, Weissman, Blazer, and Bruce, 1989; Zhang and Snowden, 1999). On the other hand, studies with smaller and less representative community samples report a greater prevalence of depressive symptoms in ethnic minorities (Kuo, 1984; Roberts, Roberts, and Chen, 1997b; Siegel, Aneshensel, Taub, Cantwell, and Driscoll, 1998), and more severe depression among ethnic minorities in treatment (Myers et al., 2002a). There has also been debate about the accuracy of these ethnic group differences, especially given the evidence for possible ethnic differences in symptom expression of depression. Although some studies have found similarities in the core features of major depression in all ethnic groups (Ballenger et al., 2001; Weissman et al., 1996), others have found a greater tendency among racial/ethnic minorities in the United States and nonwhites worldwide to somatize their psychological distress, which may also contribute to underestimates of disease prevalence (Kirmayer and Young, 1998; Kuo, 1984; Myers et al., 2002; Zheng, Lin, Takeuchi, Kurasaki, and Cheung, 1997). Several studies have reported that depressed African-American patients are more likely to report anxiety, anger, hostility, and suspiciousness than white patients (Fabrega, Mezzich, and Ulrich, 1988; Myers et al., 2002; Raskin, Crook, and Herman, 1975).
Cross-national studies reveal different rates of major depression in various countries around the world (Weissman et al., 1996). Although we can speculate that differences in risk factors or cultural differences in expression and/or reporting of symptoms may account for some of the differences, we cannot assume they account for all of the differences. Furthermore, no cross-national studies have specifically compared rates of depression among the elderly, with most including only participants up to age 65.
Findings from the ECA and National Comorbidity Study (NCS), the two largest epidemiological studies in the United States, have been mixed. ECA results indicated that whites and Hispanics evidenced higher rates of lifetime major depression (5.3 percent and 4.6 percent) than Asians and African Americans (3.6 and 3.4 percent) (Zhang and Snowden, 1999). Additionally, Hispanics reported higher rates of dysthymia than the other three groups, who reported comparable rates (4 percent, 2.6 percent, 3.2
percent, and 3 percent, respectively). African-American women between the ages of 18 and 24 were at particularly high risk in five ECA sites, and African-American men ages 18 to 24 were at lower risk compared with white men (Somervell et al., 1989).
The NCS also confirmed the existence of some ethnic and gender differences in the prevalence of MDD (Blazer et al., 1994), with whites and Hispanics evidencing higher current and lifetime rates than African Americans, and women in all ethnic groups evidencing consistently higher rates than men. African-American women between the ages of 35 and 44 were also at particularly high risk for becoming depressed.
Results from the more recent NCS also confirmed the existence of some ethnic and gender differences in the prevalence of MDD (Blazer et al., 1994), with whites and Hispanics evidencing higher lifetime rates of major depression than African Americans, and women in all ethnic groups evidencing consistently higher rates than men (see Table 13-1). Risk also varied by age groups, with African-American women between the ages of 35 and 44 and Hispanic women between the ages of 35 and 54 evidencing
TABLE 13-1 Prevalence of Lifetime Major Depressive Episode, by Race/ Ethnicity, Sex, and Age from the National Comorbidity Survey (N = 8,098)
|
|
Males |
Females |
Total |
|||
|
Race/Ethnicity |
% |
SE* |
% |
SE |
% |
SE |
|
White (years) |
||||||
|
15-24 |
11.6 |
2.1 |
23.1 |
2.3 |
16.9 |
1.5 |
|
25-34 |
14.0 |
1.4 |
19.6 |
1.5 |
17.0 |
1.1 |
|
35-44 |
15.2 |
2.0 |
24.2 |
2.4 |
19.5 |
1.8 |
|
45-54 |
12.7 |
2.0 |
23.1 |
2.9 |
17.9 |
1.6 |
|
Total |
13.5 |
1.0 |
22.3 |
1.0 |
17.9 |
0.8 |
|
Black |
||||||
|
15-24 |
4.7 |
2.2 |
9.2 |
2.7 |
7.1 |
1.8 |
|
25-34 |
9.0 |
4.1 |
18.6 |
4.4 |
14.5 |
3.3 |
|
35-44 |
5.9 |
1.8 |
21.1 |
4.5 |
14.9 |
3.3 |
|
45-54 |
10.2 |
6.2 |
9.0 |
3.9 |
9.6 |
4.1 |
|
Total |
7.2 |
1.9 |
15.5 |
2.2 |
11.9 |
1.6 |
|
Hispanic |
||||||
|
15-24 |
10.8 |
5.1 |
22.6 |
5.7 |
16.5 |
3.6 |
|
25-34 |
10.0 |
3.2 |
19.8 |
4.2 |
15.1 |
2.2 |
|
35-44 |
17.6 |
6.7 |
30.2 |
9.0 |
24.2 |
6.0 |
|
45-54 |
9.3 |
5.0 |
30.2 |
11.7 |
16.0 |
6.6 |
|
Total |
11.7 |
2.4 |
23.9 |
3.6 |
17.7 |
1.9 |
|
*Standard error. NOTE: Percentages are weighted to the population. |
||||||
particularly high risk. Although rates of 30-day current major depression proved to be less stable, they revealed similar trends.
Other studies have found no significant differences in prevalence of depression between African Americans and whites, but have found that depression in African Americans is associated with socioeconomic deprivation, including low urbanization, low education, chronic physical condition, uncertainty, job loss, money problems, and social isolation (Dressler and Badger, 1985), and that race interacts with socioeconomic status (SES) to increase psychological vulnerability among African Americans (Williams, Takeuchi, and Adair, 1992).
Because of methodological difficulties and the high cost of surveying the prevalence of psychiatric disorders among the heterogeneous mix of Asian Americans and Native Americans in the United States, we know less about the actual prevalence rates of depressive disorders in these populations. Studies on Chinese and Chinese Americans report lower prevalence rates for depression and lower treatment utilization rates than whites (Chen et al., 1993; Hwu, Yeh, and Chang, 1989; Snowden and Cheung, 1990; Sue, Fujino, Hu, Takeuchi, and Zane, 1991; Takeuchi et al., 1998). For example, lifetime and one-year prevalence of major depression among Chinese Americans as assessed by the University of Michigan-Composite International Diagnostic Interview was 6.9 percent and 3.4 percent, respectively (Takeuchi et al., 1998). Studies conducted in China and Hong Kong reveal even lower prevalence rates (Chen et al., 1993; Hwu et al., 1989). However, rates of dysthymia among Chinese Americans were comparable to the overall U.S. population (Takeuchi et al., 1998). In addition, some evidence indicates higher prevalence of psychiatric disorders among subgroups such as Southeast Asians who evidence high rates of posttraumatic stress disorder (PTSD) (Nicassio, 1985). Studies have also shown that Asian Americans seek treatment less often than other groups, and are more severely impaired at entry into treatment than whites. Therefore, treatment statistics may severely underestimate the need for mental health services in this population (Takeuchi, Leaf, and Kuo, 1988). In any event, mood disorders are the most prevalent psychiatric problem among Asian Americans and the main reason they seek treatment (Altschuler, Wang, Qi, Wang, and Xia, 1988; Flaskerud and Hu, 1994; Nakane et al., 1991). Moreover, there is evidence that Asians and Asian Americans report more severe distress and depressive symptoms in community and treatment settings (Kuo, 1984; Siegel et al., 1998; Sue and Sue, 1987), and that they tend to have worse treatment outcomes compared to whites (Zane, Enomoto, and Chun, 1994).
Immigrant status and acculturation further complicate risk associated with depression and other health and mental health problems in many ethnic minority groups. Some studies indicate that the risk for more severe depressive symptoms and/or syndromal depression increases as ethnic im-
migrants become more acculturated (Burnam, Hough, Karno, Escobar, and Telles, 1987; Escobar, 1998; Golding, Karno, and Rutter, 1990; Takeuchi et al., 1998; Vega et al., 1998), and that the age of onset for depression is later for those born outside the United States (Hwang, Chun, Takeuchi, Myers, and Prabha, in press; Sorenson et al., 1991). In addition, there is some evidence that gender differences become more pronounced as immigrants become more acculturated (Swensen, Baxter, Shetterly, Scarbro, and Hamman, 2000; Takeuchi et al., 1998). It is possible that when immigrants come to the United States, the increased stress and burden of adapting to a new place increases risk for becoming depressed, and/or that important cultural protective factors (e.g., large family and friend networks) become attenuated. It is also possible that as immigrant populations assimilate into the United States, they evidence a regression to the normative prevalence rates and age of onset patterns of the general U.S. population (Berry, 1998).
Even fewer studies have assessed the mental health needs of Native Americans. Large-scale epidemiological and community studies have failed to include significant numbers of Native Americans to permit meaningful comparisons, especially when the heterogeneity among Native American tribes is considered. Because of past discrimination and relocation, Native Americans remain plagued with economic disadvantage, poverty, physical and mental disability, and lack of access to care (Manson, 1995). In a study conducted by Kinzie et al. (1992), nearly 70 percent of Native Americans in their community sample had experienced a mental disorder in their lifetime. Among Vietnam veterans participating in the American Indian Vietnam Veterans Project, rates of PTSD among Northern Plains and Southwestern Vietnam vets ranged from 27 to 31 percent (current) and 45 to 57 percent (lifetime) (Beals et al., 2002; National Center for Post-Traumatic Stress Disorder and National Center for American Indian and Alaska Native Mental Health Research Center, 1996). Additionally, rates of current and lifetime alcohol abuse and/or dependence were 70 percent and 80 percent, respectively. These rates of PTSD and alcohol use and/or dependence are much higher than for whites, African Americans, and Japanese Americans.
ETHNIC DIFFERENCES IN DEPRESSION AMONG THE ELDERLY
There is a surprising lack of research available on the psychological well-being of older ethnic minorities. Although the NCS did not include those over 54 years of age, the ECA did survey the prevalence of psychiatric disorders in those 65 years and older. Findings revealed that 25- to 44-year-olds were at highest risk for experiencing a major depressive episode, while those over 65 were at lowest risk (Regier et al., 1988, 1993). Again, women evidenced highest risk for all age groups, and age trends were consistent across ethnic groups (Weissman et al., 1991).
On the other hand, in a community study of African Americans, Brown, Ahmed, Gary, and Milburn (1995) found that the one-year prevalence of major depression was highest among those 20 to 29 years old (5.6 percent), decreased among those 30 to 44 years old (2.2 percent) and 45 to 64 (1.2 percent) years old, but then increased among those over age 65 (3.2 percent). Additionally, the large majority of African Americans with major depression did not seek or receive mental health treatment (over 90 percent). Among elderly inpatient veterans at the Veterans Administration hospital, both African-American and Hispanic elderly evidenced significantly higher rates of psychotic disorders than whites (Kales, Blow, Bingham, Copeland, and Mellow, 2000). Although African-American elderly had significantly higher cognitive disorder and substance abuse rates than white and Hispanic elderly, they evidenced lower rates of mood and anxiety disorders. African-American elderly also have been found to report lower levels of depressive symptoms than whites, but report more functional impairment, unmet needs, losses, and physical illnesses, and fewer formal sources of support (Turnbull and Mui, 1995). Common predictors for both groups included the loss of significant others and the loss of a sense of control. Poor perceived health, physical illnesses, and fewer social contacts were significant predictors for frail white elders, but not for African-American elders. Similarly, poor ego strength and chronic medical problems were associated with greater depressive symptoms among African-American elderly in Tennessee (Husaini et al., 1991). Additionally, females were found to be more reactive to life events and to decreases in social support.
Epidemiological evidence also notes significant black-white differences in rates of suicide among the elderly, with rates in white men and women (33.1 and 4.85 per 100,000, respectively) significantly higher than for African-American men and women (11.7 per 100,000 for men and rates that are too low for women for a reliable estimate) (Centers for Disease Control and Prevention, 2001). The rates of passive and active suicide ideation among African-American elderly are also reported to be equally low, with 2.5 percent and 1.4 percent for men and women respectively (Cook, Pearson, Thompson, Black, and Rabins, 2002).
Among Hispanic elderly, Bastida and Gonzalez (1995) suggested that the stresses of migration, relocation, and adapting to a new cultural environment act as chronic stressors that increase risk for mental health problems. Canino et al. (1987) found that lifetime and 6-month prevalence rates for affective, anxiety, and substance abuse disorders increased with age in Puerto Ricans. However, their study did not examine Puerto Rican elders over age 65. Escobar, Karno, Burnam, Hough, and Golding (1988) also found higher rates of phobic and dysthymic disorders in Mexican women over 40, but again, their study did not include those over age 65. In a study of elderly Hispanics living in the San Luis Valley, no difference in risk of
depression was found among men (Swenson et al., 2000). However, Hispanic women evidenced greater depressive symptoms than non-Hispanic women. Additionally, elderly Hispanics who were less acculturated were at greater risk than those who were more acculturated. Female gender, chronic diseases, dissatisfaction with available social support, living alone, and lower income and education enhance risk for more severe depressive symptoms.
There are relatively few studies on psychological distress and depression in elderly Asians and Asian Americans. The most frequently cited of these studies is the Chinese American Psychiatric Epidemiological Study, which found that Chinese Americans between the ages of 50 and 65 were at the greatest risk for becoming depressed (Takeuchi et al., 1998). Those who immigrated at a later stage in their lives were especially vulnerable to the deleterious risks of immigrating to a new country (Hwang et al., in press).
Most of the major epidemiological studies of depression on Asians in Asia also exclude persons over age 65. However, there is some evidence for high prevalence of affective disorders among Asian elderly. For example, Lee et al. (1990) found a high prevalence of major depression among Koreans in Korea ages 18 to 24 (3.8 percent), a decreased prevalence in 25- to 44-year-olds (3 percent), and an increase in those 45 to 65 years old (3.5 percent). In addition, rates of dysthymia increased with age. Rates of major depression in Korean-American elderly in Los Angeles were similar to American elderly in the ECA sample in St. Louis, but lower than elderly Koreans in Korea (Yamamoto, Rhee, and Chang, 1994). However, the rate of alcohol abuse/dependence in Korean Americans was more than twice that of other elderly Americans. Cooper and Sartorius (1996) also found a gradual increase with age in the prevalence of neurotic disorders among Chinese in 12 areas of China. However, Chen et al. (1993) found that the prevalence of major depression was lower among Chinese ages 45 to 64, but that rates of dysthymia were higher compared to younger Chinese. Depression among Chinese elderly has been found to be associated with poor physical health, financial strains, lack of social support and resources, and stressful family environments (Chou and Chi, 2000; Krause and Liang, 1993; Kua, 1990; Woo, Ho, Lau, and Yuen, 1994). Furthermore, depression among elderly immigrants is often associated with social alienation and isolation, disempowerment, loss of support, and increased risk for suicide. In fact, elderly Chinese Americans, especially women, have been found to have higher rates of suicide than elders from other ethnic groups (Yamamoto et al., 1997; Yu, 1986).
Depression in Native American elders is also a common problem. Manson (1992) found significant depressive symptoms in more than 30 percent of elderly Native American adults visiting an urban outpatient medical facility. In addition, nearly 20 percent of Native American elders
seeking treatment in primary care settings reported significant psychiatric difficulties (Goldwasser and Badger, 1989; Wilson, Civic, and Glass, 1995), and more than 18 percent of Great Lakes Native Americans endorsed clinically significant levels of depression as measured by the Center for Epidemiologic Study-Depression (Curyto, Chapleski, and Lichtenberg, 1999; Curyto et al., 1998). High prevalence rates of suicide, homelessness, alcohol and drug abuse, poverty, domestic violence, trauma exposure, and comorbidity of health and mental health problems also reflect the significant need for mental health services in this population.
In summary, few studies have examined mental health issues among ethnic minorities, especially ethnic elders. The available evidence is mixed, revealing a higher prevalence of affective disorders among Hispanic Americans and Native Americans across the life course. On the other hand, African Americans and Asian Americans seem to have lower rates of diagnosable disorders, but higher rates of depressive symptomatology overall. Differences in the samples studied (i.e., community versus clinical samples), in the assessment measures used (i.e., symptom measures versus diagnostic interviews), as well as possible differences in expression of distress may partially account for these discrepancies. It is also possible that age-related effects and differences in risk for mental health problems in ethnic elderly may be attributable to a disproportionate burden of accumulated stress, physical health problems, functional and cognitive disability, chronic illness, low social support, and financial difficulties (Blazer et al., 1991; Roberts et al., 1997a). In any event, more systematic research examining the prevalence of psychiatric disorders among ethnic elderly is an important priority.
CONCEPTUAL MODEL OF CUMULATIVE BIOPSYCHOSOCIAL VULNERABILITY AND RESILIENCE IN LATE LIFE
The previous review indicates that the available research on the different ethnic groups is uneven, with limited information on Native Americans and on many racial/ethnic subgroups. Furthermore, few studies of depression and psychological well-being take a developmental life-course perspective in investigating possible ethnic group differences and factors that contribute to such differences. Finally, there is little synergy among the biological, psychosocial, and behavioral explanations that have been offered in accounting for ethnic differences in distress and depression in the elderly. To advance our understanding of the role psychosocial factors might play in ethnic differences in depression and well-being in late life, we offer an integrative biopsychosocial model as a heuristic for organizing our review and discussion of how psychosocial stress and related factors might account for ethnic differences in functional health outcomes. We use de-
pression as an illustrative disorder, but acknowledge that there is substantial evidence that the biopsychosocial factors included in this conceptual model may also apply to many other health outcomes, including but not limited to hypertension, cancer, chronic pain and disability, cognitive decline, and immune-mediated disorders. It is also important to acknowledge that depression is often co-morbid with chronic illnesses (e.g., advanced heart disease, diabetes, cancer), and is often a consequence of the anxiety, pain, and disability associated with these chronic conditions. Therefore, this conceptual framework may have broader applicability to both psychiatric and medical illnesses. We also acknowledge that the evidence supporting many of the hypothesized pathways varies in quality and relevance to explaining ethnic group differences in the health of the elderly. Nevertheless, we believe this model can be helpful in guiding future research efforts.
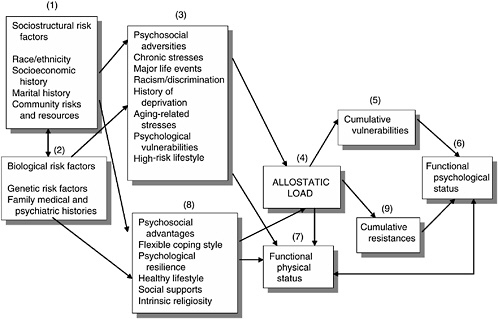
The proposed model, depicted in Figure 13-1, makes explicit that (1) sociostructural factors, such as race/ethnicity, social class, environmental factors (e.g., community, family), and (2) biological factors such as genetic vulnerabilities and family medical and psychiatric histories, interact over time to increase (3) burden of psychosocial adversities, which is hypothesized to be the primary predictor of risk. Primary among these adversities are a cluster of life stresses that include chronic life stresses, major life events, ethnicity-related stresses, and age-related stresses. Over the life course, we hypothesize that these stresses will accumulate and contribute to vulnerability to disease and dysfunction. The impact of this stress burden is further exacerbated by personality characteristics, such as anger/hostility, neuroticism, and pessimism, and by the clustering of health-endangering behaviors, such as smoking, alcohol and drug abuse, sedentary lifestyle, and obesity (Contrada et al., 2000; Krieger, Rowley, Herman, Avery, and Phillips, 1993; Myers, Kagawa-Singer, Kumanyika, Lex, and Markides, 1995; Williams, Yu, Jackson, and Anderson, 1997).
Our conceptual model builds on the work of several stress and life-course theorists, including McEwen and colleagues’ (McEwen, 1998; McEwen and Seeman, 1999) work on “allostatic load,” the work by Elder and colleagues (Elder, 1998; Elder and Crosnoe, 2002; Wickrama, Conger, Wallace, and Elder, 1999) on “life course and intergenerational transmission of risk,” Singer and Ryff’s (1999) work on “life history methodology,” and Geronimus’s (1992) work on the “weathering hypothesis.” These earlier models identify factors that serve as (4) biobehavioral mediators and moderators of risk for adverse psychological and health outcomes. Furthermore, lifetime burden of adversities is hypothesized as contributing to disease through biological and behavioral pathways that include the chronic triggering of physiological response mechanisms (i.e., allostasis), constitutional predispositions or vulnerabilities, and allostatic load (i.e., wear and tear on the system). In turn, allostatic load is hypothesized to contribute
over time to (5) cumulative vulnerability, and ultimately to (6) functional outcomes such as physical and psychological distress and dysfunction (Blanchard, 1996; Geronimus, 1992; Lestra et al., 1998; McEwen, 1998; McEwen and Stellar, 1993; Seeman, Singer, Rowe, Horwitz, and McEwen, 1997). In addition, this burden of biological hyperreactivity is compromised by the clustering of health-endangering behaviors that further enhance risk for adverse health outcomes (Myers et al., 1995; Wickrama et al., 1999).
Furthermore, and consistent with evidence of reciprocal effects between current illness and future stress exposure (McLean and Link, 1994; Harkness, Monroe, Simons, and Thase, 1999), (7) poor health and functional limitations are likely to exacerbate the burden of adversities over time by generating new stresses, increasing the demands on coping resources, and increasing the likelihood of greater distress, depression, and functional impairment.
However, the model also acknowledges that the stress-biological processes-disease pathways are influenced by a number of psychosocial and behavioral factors that serve as (8) psychosocial assets or advantages that have been shown to moderate risk. These include psychological characteristics, such as dispositional optimism and perceived control (Eizenman, Nesselroade, Featherman, and Rowe, 1997; Holahan and Holahan, 1987; Seeman, Unger, McAvay, and Mendez de Leon, 1999), healthy lifestyles (McEwen, 1998; Myers et al., 1995; Shiono, Rauh, Park, Lederman, and Suskar, 1997), flexible stress appraisal and coping strategies (Stern, Dhanda, and Hazuda, 2001; Wong and Reker, 1985), and the availability and use of adequate social support resources (Kelley, Whitley, Sipe, and Yorke, 2000; Seeman, Lusignolo, Albert, and Berkman, 2001; Walen and Lachman, 2000).
Consistent with the evidence reported by Singer and Ryff (1999) and Elder and Crosnoe (2002), the model therefore hypothesizes that it is the balance between (5) cumulative adversities or vulnerabilities and (9) cumulative advantages or assets over the life-course and the life transitions experienced that ultimately contributes to differences in functional status and health trajectories in the elderly, both overall and as a function of ethnicity, gender, and social class. Limitations in the available evidence for all pathways as well as space constraints preclude a detailed discussion of all aspects of this conceptual model. Therefore, we give special attention to discussing (1) the role of chronic stress, especially age- and ethnicity-related stressors, as adversities that can enhance risk for depression and other adverse health outcomes, (2) allostatic load and “weathering” or premature aging as hypothesized mediators of disease and dysfunction, and (3) stress coping, perceived control and self-efficacy, social supports, and religiosity
as psychosocial advantages that have been shown to moderate the stress-depression relationship.
LIFETIME BURDEN OF ADVERSITIES
A primary hypothesis in our model is that the differential burden of lifetime stresses is responsible for ethnic disparities in health. The additional stress burden that ethnic groups face has yet to be studied thoroughly, but includes racism-related stresses, acculturative stress, and stresses that are particularly salient to ethnic elderly. Although there is a substantial body of evidence linking exposure to many sources of stress to depression, relatively few studies have specifically addressed the particular hypothesized associations between several of these sources of stress and ethnic differences in risk for depression. We suggest that future studies aim toward testing pathways in the proposed model.
Chronic Stress Burden
There is a large and rich interdisciplinary body of research on the complex relationships between stress, generally defined as “environmental demands that tax or exceed the adaptive capacity of an organism, resulting in biological and psychological changes that may be detrimental and place the organism at risk for disease” (Cohen, Kessler, and Gordon, 1995), and functional health outcomes. Most models of stress and disease distinguish among stress exposure, the context of stress exposure, stress appraisal, and stress response (Lobel, Dunkel-Schetter, and Scrimshaw, 1992). Meaningful distinctions are also made among types of stressors, including discrete life changes or events, chronic unresolved stresses and daily hassles, as well as the role that personal predisposition (e.g., anger/hostility, cognitive schemas) (Monroe and Simons, 1991) and situational diatheses (e.g., socioeconomic deprivation, limited social supports) (Dohrenwend et al., 1992) play in increasing vulnerability to physical and psychiatric disorders.
There is also a growing body of evidence that has specifically tested the hypothesis that ethnic differences in physical health may be due, at least in part, to differential exposure to chronic and acute life stressors (Geronimus, 1992; Williams et al., 1997). Ethnic minorities, especially those from lower social classes, often report a greater number of negative life events, greater and more frequent exposure to “generic life stressors” (i.e., stressors that are a usual part of modern life, including those that are financial, occupational, relationship oriented, or parental), and greater psychological distress from these stressful life experiences than their white counterparts (Myers, Lewis, and Parker-Dominguez, 2002b). Therefore, they are likely to be particularly vulnerable to the long-term effects of high chronic stress
burden and presumably higher allostatic load. Chronic stressors due to financial strain, inadequate housing, crowding, and violence may also contribute to more frequent activation of stress-response systems and prolonged exposure to stress hormones (Anderson, McNeilly, and Myers, 1992; McEwen, 1998).
In a recent review, Myers, Lewis, and Parker-Dominguez (2002b) discuss the evidence linking psychosocial stress and other factors in accounting for ethnic disparities in a variety of chronic illnesses and adverse health outcomes. For example, studies by Orr et al. (1996) found that exposure to high psychosocial stressors was related to low birthweight for African Americans. Shiono et al. (1997) reported in their study of ethnic differences in birthweight that living in public housing and believing that one’s health was largely determined by chance were negatively related to birthweight, and that having a stable residence was associated with higher birthweight. Furthermore, Zambrana and colleagues (1999) found that prenatal stress, drug use and smoking, and attitudes toward the pregnancy accounted for ethnic differences in birthweight between African Americans and Hispanics.
Such differences in exposure to generic life stressors probably account for some of the ethnic disparities in health. However, we argue that such a simple explanation of differential stress burden underestimates the true complexity of the minority stress-health relationships. For example, it has been argued that race conditions social class such that exposure to life stressors are not only greater among the poor, but also that racial/ethnic minorities experience greater stress burden and poorer health outcome at all equivalent levels of SES (Krieger et al., 1993; Williams, 1999). This race-SES relationship can have direct effects on health through additional stress burden and higher allostatic load, as well as indirect effects through structural barriers of access to health care and other social resources (i.e., housing, employment, safety); acceptance of societal stigma of inferiority (i.e., acceptance of minority status); high risk and unhealthy lifestyles (Kumanyika, 1998; Myers et al., 1995; see also Chapter 9, this volume); coercive, restrictive, or neglectful parenting; ineffective coping and negative affective states (e.g., depression, hostility, dispositional pessimism) (Clark, Anderson, Clark, and Williams, 1999; Kreiger et al., 1993; Williams, 1999); and lack of perceived control (Shaw and Krause, 2001).
Minorities, and the elderly in particular, also face a number of neighborhood stresses that add to their stress burdens. These include greater vulnerability to violence, especially from neighborhood youth, inadequate transportation, poor housing, limited access to recreation and other social services geared to the needs of the elderly (e.g., senior centers), as well as increased vulnerability to swindles and other financial schemes. These factors, in addition to their growing burden of health and functional limitations, often contribute to greater sense of lack of control. Some studies
suggest there are racial disparities in feelings of perceived control that persist across all age groups (Shaw and Krause, 2001). For a more detailed discussion of these issues, see Chapter 11.
In addition to greater burden of these generic life stresses, persons of color also experience additional stresses related to their race/ethnicity, such as racism-related and acculturative stresses that add to their overall stress burden. Therefore, assessment of stress burden for populations of color will be incomplete without the inclusion of these additional sources of stress.
Racism-Related Stresses
In their recent review of the literature on racism and its effects on African Americans, Clark et al. (1999) discussed the empirical evidence verifying the effects racism has on mental and physical health. They acknowledge that both intergroup and intragroup racism, as well as attitudinal (i.e., prejudice) and behavioral (i.e., overt discrimination) racism, are significant stressors and offer a biopsychosocial model to account for its effects.
Minority elderly may be less likely to experience overt acts of racism and discrimination because they pose less of a threat and are no longer serious competitors for social resources. The one area in which there may be an exception is in access to quality health care (see Smedley, Stith, and Nelson, 2002, for a more detailed discussion of this issue). However, experiences with discrimination over the life course, including exposure to the most blatant forms of discrimination (i.e., discrimination in education, housing, employment, and transportation, and within the legal/judicial system), may have long-term deleterious effects that may become evident in their later years. Elderly African Americans were young adults during the Jim Crow years and the civil rights struggles, many elderly Japanese experienced internment camps, many elderly Mexican Americans experienced the Bracero Movement and the Zoot Suit riots in California, Cuban elders experienced economic losses when forced to leave Cuba followed by racism when they arrived in the United States, and most Native American elders experienced some of the worst treatment by the U.S. government. In addition, many older minority men experienced significant discrimination in the military during World War II and Korea. How they coped with these past and current experiences and how they have resolved these conflicts may have, at least, indirect effects on their current health and functioning. The work by Elder and Crosnoe (2002) on the influence of early behavior patterns on later life illustrates this point. Using data from men born between 1905 and 1914 and tracking their life trajectories in terms of emotional health, career achievement, and civic involvement, Elder and Crosnoe were able to differentiate five
behavioral types in terms of overall success and life achievement, and identified factors associated with these life trajectories. Similar longitudinal studies of the life course of racial/ethnic minority men and women would be especially helpful in testing the hypothesized relationship in this conceptual model. For example, it would be especially useful for future research to determine whether there is a measurable difference in health status in minority elderly who experienced more race-related traumas compared to those who were spared such experiences.
One of the methodological challenges facing research on the experience and impact of racism on health is the fact that racism is a “perceived stressor” (i.e., the subjective experience of prejudice or discrimination), and that people of different ethnicities may differ in how they interpret and respond to racist experiences. Clark et al. (1999) argue that traditional models of stress focus primarily on more “objective” stressors such as life events and role strains, and in doing so ignore or underestimate the importance of exposure to more subtle racism because it involves some degree of subjectivity. However, Lazarus and Folkman (1984) note that it is the subjective appraisal of events as stressful that determines the magnitude of a stress response. Therefore, we would expect greater psychological and physiological reactivity and greater allostatic load in those who report greater exposure to both objectively measurable stressors as well as subjectively experienced greater exposure to racism-related stresses (Anderson, McNeilly, and Myers, 1993; Fang and Myers, 2001; Krieger and Sidney, 1996). We might also expect that greater exposure to racism and discrimination will be associated with more health-damaging behaviors and a poorer lifetime health trajectory. Additional studies are needed to investigate these hypotheses and to consider possible ethnic differences in exposure to and impact of racism-related stresses.
Acculturative Stress
Another major source of stress for racial/ethnic minority groups, especially those who are immigrants, is acculturative stress. There is a substantial and growing body of research on acculturation and its effect on psychological and physical health (see Berry, 1998, and Chun, Organista, and Marin, 2002, for a comprehensive review of this literature). Berry (1998) argues that investigations of relationships among acculturation, adjustment, and health need to consider the influences of social and personal variables from the society of origin (i.e., social class, sex roles, opportunity structures for social mobility, and other factors), the society of settlement (i.e., receptivity of cultural differences), and phenomena that exist both prior to (e.g., trauma) and during the process of acculturation. Despite continued debates about how to conceptualize and measure acculturation, the available evi-
dence suggests that acculturation to the majority society has both costs and benefits. For example, research indicates that recent Hispanic and Asian immigrants evidence better mental and physical health than U.S.-born members of the same group (Rogler, Cortes, and Malgady, 1991; Vega et al., 1998), except for those who are refugees, who evidence higher rates of trauma and PTSD (Nicholson, 1997). However, this initial advantage is lost during the early phases of acculturation, primarily through stresses associated with acculturation (e.g., learning a new language, exposure to immigrant-related discrimination, changes in social roles, family disintegration, changes in health behaviors) (Balcazar, Peterson, and Krull, 1997; Nicholson, 1997).
Contrada et al. (2000, p. 138) also note that own-group conformity pressures, defined as “the experience of being pressured or constrained by one’s ethnic group’s expectations specifying appropriate or inappropriate behavior for the group,” are independent of discrimination and are an additional source of stress for those who are upwardly mobile and acculturating, and for children and adults who may be acculturating at different rates. Also, while those who learn to balance their bicultural status (i.e., integrate into majority society yet retain their ethnic identity and cultural roots) seem to reobtain health losses due to acculturation (Cortes, Rogler, and Malgady, 1994; LaFromboise, Coleman, and Gerton, 1995; Moyerman and Forman, 1992; Roysircar-Sodowsky and Maestas, 2000), those who are bicultural but have not learned to negotiate the demands from both worlds may be at increased risk (Hwang et al., 2000).
For minority elderly, acculturation may pose unique challenges. On the one hand, elders are the guardians and conveyors of the culture of origin, and therefore, they are the primary socialization agents and source of knowledge about the cultural values, beliefs, and norms of the group. Thus, they are often at the center of generational conflicts that inevitably emerge as the younger generations embrace the values, beliefs, and norms of the new culture and challenge, adhere less rigidly, or discard those of the culture of origin (e.g., centrality of family loyalty and obligations versus the desire to pursue personal goals). On the other hand, and depending on when minority elders immigrated, they are often the ones who experienced the greatest obstacles and harshest forms of discrimination, and therefore struggle with the competing goals of maintaining cultural integrity versus encouraging the next generation to acculturate (i.e., learn the language and customs of the new society) as quickly as possible in order to improve their odds. This may pose more of a problem for the oldest old, who are either recent immigrants or remain enculturated (e.g., they never learned English or adopted American culture) and are likely to have the greatest difficulty making necessary changes, despite living in the
United States for a significant part of their adult lives. The latter group is more likely to be poorer, to be less educated, to rely entirely on their native community for resources, to have poorer health, and to have less access to health care and other resources of the larger society (Wong and Ujimoto, 1998). Additional studies are needed to explore these issues across different ethnic groups who may differ in their immigration experiences in the United States.
Aging-Related Stresses
In addition to the stresses already described, the elderly face a number of additional stressors related to their life stage. These include adequacy and stability of financial resources, coping with chronic illnesses and the attendant pain and physical limitations, social isolation, assuming caretaking responsibilities for ill spouses or custodial responsibilities for grandchildren, loss of meaningful social roles, decreasing cognitive functioning and dementia, and reductions in their social networks due to death, especially of spouses and friends (Karel, 1997). All of these stresses contribute to enhanced risk for depression and lower life satisfaction in the elderly (Burnette, 1999; Karel, 1997; Kelley et al., 2000; Newsom and Schulz, 1996).
One of the major stressors faced by the elderly is the anxiety over the adequacy and stability of their fixed income. This is especially true for minority elders, who may have experienced lifetime financial obstacles that limited their ability to accumulate savings and who must now rely on Social Security, disability payments, pensions, or veteran’s benefits, or on the generosity of family and social services (Gibson, 1993). This is a particularly salient issue for undocumented immigrants as they grow older because they are often not able to capitalize on retirement benefits and may not have been able to accumulate enough savings because many held jobs with low pay and low status.
Ethnic elderly from low socioeconomic backgrounds are also at greater risk for acute and chronic physical illnesses and their sequelae. In Karel’s (1997) comprehensive review of the literature on aging and depression, she notes that these functional limitations are more important than life events and psychological factors in contributing to risk for depression and low life satisfaction. She also concludes that these depressogenic effects are greatest in elderly who experience serious illnesses, severe pain, greater functional impairment, and more social isolation, and who must commit more of their limited financial resources to health care. This effect is evident in all ethnic groups, but minority elderly who generally experience greater lifetime socioeconomic deprivation and carry a heavier burden of lifetime medical morbidity are expected to be at higher risk.
Grandparenting Stresses
Minority elderly, especially African-American and Hispanic elderly, are disproportionately burdened by custodial and caretaking responsibilities of grandchildren. The increase in the number of grandparents who are raising grandchildren is one of the unanticipated and underrecognized fallouts of the cocaine/crack abuse, HIV/AIDS, and teen pregnancy epidemics of the 1980s and 1990s (Burnette, 1997; Minkler and Fuller-Thompson, 1999). Data from the U.S. Census reported by Minkler and Fuller-Thompson (1999) indicated that in 1997, approximately 4 million children were living with grandparents, including 4.1 percent of white children, 6.5 percent of Hispanic children, and 13.5 percent of African American children. This is a 44 percent increase from 1980 (Lugaila, 1998), with the greatest increase in skipped-generation families in which the birthparents were not co-resident (Casper and Bryson, 1998). Szinovacz (1998) noted from his analyses of the Wave II data in the National Survey of Families and Households (NSFH) that Census data underestimate the true prevalence of grandchildren living with grandparents. He found custodial grandparenting rates in the NSFH as high as 26 percent in African-American grandmothers and 7.3 percent in white grandmothers.
There is also substantial evidence that caregiving grandparents are especially vulnerable to a host of problems, including depression, social isolation, poverty, and reduced quality of life (Minkler and Fuller-Thompson, 1999; Minkler, Fuller-Thompson, Miller, and Driver, 1997; Rodgers-Farmer, 1999). In their secondary analysis of the NSFH data, Minkler and Fuller-Thompson found that caregiving grandparents were 50 percent more likely to have activities of daily living limitations and lower self-reported satisfaction with health than noncustodial grandparents. Similarly, these grandparents were almost twice as likely as noncaregiving grandparents to report clinically significant levels of depressive symptoms, even after controlling for precaregiving depression and demographic characteristics (Minkler et al., 1997). However, this greater vulnerability to depression cannot be attributed entirely to caregiving per se. Rather, other factors contribute to enhanced risk for depression, such as female gender (Minkler et al., 1997), recency of caregiving, younger age of the dependent child (Strawbridge, Wallhagen, Shema, and Kaplan, 1997), older age and poorer health of the caregiving grandparent (Minkler et al., 1997), having to care for children with special needs (Jendrek, 1994), inadequacy of available social supports (Sands and Goldberg-Glen, 2000), and the reasons for having to assume this responsibility (Minkler and Roe, 1993). Grandparents who had to step in to care for their grandchildren because of parental incarceration due to drug addiction and incapacitation, or death due to AIDS or violent crime, report feeling more anger, shame, and percep-
tions of entrapment in this “time disordered role” (Minkler et al., 1997). In addition, they may also experience greater feelings of failure in raising their own children, and create more pressure on themselves to do well in raising their grandchildren while trying to adapt to the financial, physical, and mental transitions of growing old.
Several studies have noted, however, that although the additional stress burden associated with assuming caregiving responsibilities for grandchildren increases risk for psychological distress and depression in all groups, there are notable ethnic differences in the relative impact this new source of stress appears to have. In a recent report, Pruchno (1999) compared the experiences of 398 white and 319 African-American caretaking grandmothers and found that the latter reported less distress and less negative impact of their caretaking responsibilities on their mental health and social lives than the former. White grandmothers were more likely to feel trapped in their role; to feel tired, isolated, and alone; and to have less personal time and greater interference with their social lives, and more negative relationships with family members. These differences were evident even though the African-American grandmothers were more likely to be widowed or divorced and to have lower per capita incomes and more children in their households.
The lower impact of childcare burden on African-American grandmothers may be explained by the fact that they traditionally play key roles as support for African-American families during times of crisis. Many African-American grandmothers reported being embedded in large, supportive social networks (e.g., other parenting grandmothers and other sources of support) that provided emotional and other tangible assistance. The same was not true for white grandmothers.
Burnette (1999) reported similar results in her study of Hispanic grandparent caregivers. Using social role theory as a framework, Burnette investigated the effects of caretaking responsibilities on Latina grandmothers. She noted that Hispanic elders tend to have larger families, stronger family bonds, and more interactions with and support from adult children than either African-American or white elders, which may moderate risk for negative outcomes (Lubben and Becerra, 1987; Sabogal, Marin, and Otero-Sabogal, 1987). Older Latinas serve an important central role in kinkeeping, and may identify with this role more than women in other ethnic groups (Kornhaber, 1996; Padgett, 1998). However, while this family status affords them considerable prestige and domestic authority, differences in gender role status also disproportionately burden Latinas with caretaking responsibilities (Hurtado, 1995).
Results from the Burnette (1999) sample of Puerto Rican and Dominican women, most of whom were unmarried, undereducated, and low income, indicated that assuming the responsibility of primary caretaker for
grandchildren had significant detrimental effects on their mental health and social lives, such as giving up their jobs, loss of autonomy, and loss of social ties.
In summary, although the evidence clearly indicates that a heavier burden of aging-related stresses is associated with enhanced risk for depression and related dysfunction in both younger and older adults (Bazargan and Hamm-Baugh, 1995; Holahan, Holahan, and Belk, 1984; Karel, 1997; Markides, 1986), stress-depression and well-being relationships are complex and moderated by social class, ethnicity, and a number of psychosocial factors, including social supports, coping, religiosity, and personality traits (Karel, 1997). Most of the available evidence appears to suggest that African-American grandparents who have caretaking responsibilities for their grandchildren may be less vulnerable to the depressogenic effects of this additional source of role strain. The effects for Latina grandmothers, however, appear to be less clear. In any event, simple generalizations to these ethnic groups would be premature. Additional research is still needed to determine to what extent aging-related stresses may contribute to ethnic differences in functional status and health outcomes and for which ethnic groups.
Unfortunately, relatively little research is available on these issues in Asian American or Native American elderly. Therefore, an important priority for future research is to investigate the contributions of chronic stress burden from multiple sources to the health trajectory and functional status of these understudied populations.
ALLOSTATIC LOAD AS A BIOBEHAVIORAL MEDIATOR OF RISK
Modern models of stress, disease, and functional status all acknowledge the importance of identifying the biological pathways through which the burden of life stresses contributes to differences in functional status and health outcomes. The work by McEwen (1998) on allostatic load and by Geronimus (1992) on the weathering hypothesis are especially useful in this regard. In addition, the work by Thayer on heart rate variability (see Chapter 15, this volume, for a review) is a promising alternative mediating mechanism that might be especially useful in future large-scale longitudinal studies.
McEwen and Stellar (1993) coined the term “allostasis” to refer to the normal fluctuations of the autonomic nervous system, the hypothalamic-pituitary-adrenal axis, and the metabolic, cardiovascular, and immune systems that maintain stability and protect the body by responding to stress. However, these normal allostatic responses can become dysregulated, which subsequently overtaxes the system and results in physiologic wear and tear, which they defined as “allostatic load.” A good example of this model is
essential hypertension, which is conceptualized as a disease that results from the dysregulation of blood pressure control mechanisms due to persistent and pathological autonomic hyperreactivity to stress (Myers, Anderson, and Strickland, 1996).
According to McEwen (1998), allostatic load increases under four conditions: (1) frequent stress exposure, with attendant frequent exposure to stress hormones; (2) exaggerated reactivity and/or inadequate habituation to stressful experiences, which also results in prolonged exposure to stress hormones; (3) inability to recover, where physiological arousal and reactivity continue even after the stressor has been removed or terminated; and (4) an inadequate response to stress because of system fatigue or dysfunction, which triggers pathological compensatory responses in other systems. Recent studies by McEwen and Seeman (1999) and Singer and Ryff (1999) provide compelling empirical support for this argument. In their review, McEwen and Seeman (1999) argue for a more comprehensive model of the effect of stress on disease that includes genetic load, life experiences, individual health habits, and physiological reactivity, all of which interact over time to produce gradients of risk for disease. Specific attention is given to increasing mortality and morbidity rates as one descends the socioeconomic gradient, which reflects the cumulative burden of coping with life demands with inadequate resources for coping. In the case of the elderly, this social class differential, and possible racial/ethnic differential as well, would be expected to be greater given the greater cumulative allostatic load attributable to lifetime accumulation of disadvantage.
Singer and Ryff (1999) tested this hypothesis using data from the predominantly white sample of adults in the Wisconsin Longitudinal Study. Using social relationships (i.e., parental bonding in childhood and relationship intimacy as adults) and household income in childhood and adulthood as their measures of adversity and advantage, and a rating system that characterized distinct life histories based on positive and negative ratings on these two dimensions, they demonstrated that there was a strong direct association between the extent of lifetime adversity relative to advantages in ordering life histories. Those with higher relative disadvantages (i.e., negative economic and social relationships, at each measurement point), especially those with persistent negative social relationships, evidenced higher allostatic loads (i.e., impaired immune function, elevated blood pressure, and later life illness and chronic disease propensity) compared to those with balanced (+, − or −, +) or more advantaged (+, +) histories. Their analyses also confirmed that downward social mobility was more adverse than upward mobility, which provides a more textured glimpse of the substantial variation in the SES-health relationship than is possible using the usual single point in time (i.e., current) measure of SES.
These findings complement the results of the studies by Elder and Crosnoe (2002), who used life-course development methods to track the developmental trajectories of men born in the early 1900s from childhood through later life. They were able to demonstrate that historical events and life transitions exert powerful effects of the life trajectory of these men.
In their more recent work, Elder and colleagues (Wickrama et al., 1999) also demonstrated that health-risk behaviors and health-risk lifestyles are transmitted intergenerationally between parents and teens. These parent health-risk effects were moderated by family social status and by family structure such that parental health-risk lifestyle affected their sons and mothers’ health-risk lifestyle affected their daughters. This suggests possible gender-related modeling of health behaviors. Unfortunately, these studies did not specifically address any ethnic differences in these processes, but their findings are somewhat congruent with other studies that indicate a clustering of risk behaviors within minority families, and the role such clustering plays in accounting for the greater burden of illness and disability observed in many racial/ethnic populations (Harris et al., 1997; Moore and Chase-Landsdale, 2001; Myers and Taylor, 1998).
Singer and Ryff (1999) also identified a group of resilient elderly who evidenced lower allostatic loads despite relatively disadvantaged histories, which they attributed to the presence of compensatory social relationship histories. This is an understudied group, especially resilient minority elders, which could yield valuable information for programs designed to foster healthy aging and that might help to close the health disparities gap.
These intriguing ideas and methodologies have not yet been directly applied to investigating ethnic differences in health and well-being in adults and the elderly. However, Geronimus’s (1992) “weathering hypothesis,” which is hypothesized to account for some of the persistent African-American versus white differences in birth outcomes, demonstrates the utility of investigating health differentials at different developmental stages. Using national infant mortality data comparing African-American and white mothers by age cohorts, Geronimus found that these groups differed in patterns of neonatal mortality rates over the predominant age of having a first child. Her results indicated, as shown in Table 13-2, that compared to white infants, African-American infants of teen mothers experienced a survival advantage relative to infants whose mothers were older and in the prime childbearing years (i.e., 20s and 30s). A similar but weaker trend was also observed for Mexican and Puerto Rican women.
She argued that this evidence indicates that there may be population differences in prime childbearing years, and suggested that African-American (and perhaps also Puerto Rican) women appear to experience an earlier aging or “weathering process.” She speculated that this difference was probably a consequence of prolonged, effortful coping with socioeconomic
TABLE 13-2 Neonatal Mortality Rates and Rate Ratios by Maternal Age and Ethnicity: First Births, United States, 1983
|
|
Neonatal Mortality Rates* |
Rate Ratios |
|||||
|
Age (years) |
White |
Black |
Mexican |
Puerto Rican |
Black-white |
Mexican-white |
Puerto Rican-white |
|
15-19 |
7.2 |
9.8 |
5.3 |
8.5 |
1.4 |
0.7 |
1.2 |
|
20-29 |
4.6 |
10.4 |
4.7 |
9.2 |
2.3 |
1.0 |
2.0 |
|
30-34 |
5.6 |
15.0 |
7.9 |
11.9 |
2.7 |
1.4 |
2.1 |
|
Total |
5.4 |
10.6 |
5.2 |
9.0 |
1.9 |
0.9 |
1.7 |
|
*Deaths per 1,000 live births. NOTE: Presented by Geronimus (1992, p. 209). SOURCE: National Linked Birth/Death Files (1983). |
|||||||
inequality, racial discrimination, and greater risk of exposure to environmental hazards. This burden of risk is likely to be exacerbated as these women get older by the development and untreated progression of chronic illnesses (e.g., hypertension, diabetes), by the development of behavior patterns that are adversarial to health (e.g., obesity, alcohol and drug use), and by increasing stress burden.
It is also important to note that the African-American versus white differentials in adverse birth outcomes, especially low birthweight and infant mortality, are smaller among the less educated and larger among the most educated (Kleinman, Fingerhut, and Prager, 1991; Shiono et al., 1997). This suggests that African-American women may derive less reproductive benefit from upward mobility than white women. Additional research is needed to explore this hypothesis with the other ethnic groups and to determine whether women who experience adverse birth outcomes during their childbearing years evidence early aging in the form of more health difficulties and a heavier burden of medical morbidity in later years.
We believe our understanding of the health disparities would be greatly enhanced by lifespan developmental studies that apply the concepts and methodologies used to test the allostatic load and weathering hypotheses to investigate ethnic differences in health trajectories.
LIFETIME ADVANTAGES AS PSYCHOSOCIAL MODERATORS OF RISK
Substantial empirical evidence shows that a number of psychosocial factors—including psychological resilience, stress appraisal and coping style, the availability of social supports, and religiosity—serve to moderate the stress-health and functional status relationships in adults and the elderly.
Psychological Resilience
In her comprehensive review of depression and aging, Karel (1997) notes that adults appear to become less psychologically vulnerable to depression as they age. This may be because personality characteristics that enhance risk for depression, such as pessimism, self-criticism, interpersonal dependence, and preoccupation with failure (Akiskal, 1991) may be less common among the elderly, despite stereotypes to the contrary (Jones and Meredith, 1996). In fact, Jones and Meredith found patterns of longitudinal changes over 30 to 40 years that indicated stability of personality traits across ages, along with slight increases in self-confidence, extroversion, and dependability as people matured.
Another key moderator of risk for depression is sense of perceived control. Although aging exposes the elderly to more uncontrollable events (i.e., declining physical health and cognitive functioning), this does not appear to result in a decreased sense of overall control. Instead, factors such as an increasing ability to make psychological compensations and accommodations (e.g., adjusting one’s goals, making more downward social comparisons to those less well off, seeking assistance from others, and using aids such as wheelchairs and hearing aids to compensate for functional limitations) contribute to protect the elderly from perceived loss of control and corresponding increase in risk for depression (Aldwin, 1992; Heckhausen and Schulz, 1993; Karel, 1997).
Unfortunately, there continues to be inadequate representation of minority elderly in studies investigating factors associated with psychological resilience, especially groups other than African Americans. Therefore, although there is little reason to expect that these factors are likely to operate differently in these populations, current evidence does not allow us to draw any firm conclusions about their effects across ethnic and social class groups.
Stress Appraisal
The impact of exposure to chronic stress on health is moderated by how one interprets or appraises and responds to the stressful experience (Lazarus and Folkman, 1984). Stress appraisal involves the weighing of one’s resources against the demands of the stressor in order to determine how large a threat the stressor is to well-being. For ethnic minority elderly, stress appraisal is likely to involve not only the subjective examination of resources versus demands, but also the filtering of stressful experiences through one’s unique cultural lens. For example, women of all ethnic groups typically serve as the traditional center of families, and are responsible for the emotional, physical, and spiritual well-being of family members, and in some cases, sharing or carrying the major responsibility for the economic
viability of the family, coping with their own burden of life stresses, and moderating the impact stresses have on other family members (Burnette, 1999; Chisholm, 1996; Minkler and Roe, 1993; Reid and Bing, 2000). This is illustrated in the acceptance of the primary responsibility for the care of grandchildren in response to major family crises (Minkler et al., 1997). Accepting this “strong woman” image is an additional burden of stress, and cultural expectations that they should be able to handle life challenges may hinder some minority women (and men) from seeking help with problems from professionals and/or formal assistance programs. On the other hand, fulfilling strong traditional roles may contribute to their resilience, resourcefulness, and flexibility in dealing with stressful situations (Reid and Bing, 2000).
However, and contrary to popular belief, evidence regarding ethnic differences in seeking help is somewhat mixed. Some studies suggest that minorities evidence greater reliance on informal sources of help than whites (Harden, Clark, and Maguire, 1997; Zhang, Snowden, and Sue, 1998), while others indicate that some groups, especially African Americans, tend to rely more on both formal and informal sources of support for mental health needs than whites (Snowden, 1998). More well-designed studies with diverse populations are clearly needed to clarify these apparently contradictory findings, and to identify which factors in which ethnic groups are associated with timely health care seeking versus delayed care seeking.
Coping
As a byproduct of experience and maturity, older adults have been found to use more adaptive coping strategies, including anticipation, sublimation, humor, altruism, and spirituality in coping with life changes (Diehl, Coyle, and Labouvie-Vief, 1996; McCrae, 1982). They may also have a greater ability to accept and reinterpret adverse situations in more positive ways (Diehl et al., 1996), have greater emotional stability and less emotional reactivity (Lawton, Kleban, Rajagopal, and Dean, 1992), and to be more thoughtful and flexible in their response to stress (Diehl et al., 1996).
Again, our ability to investigate the role of coping and psychological distress in minority elderly is severely limited by the dearth of studies that specifically address this issue (Markides, 1986). Nevertheless, useful inferences can be drawn from studies on other populations. For example, in a theoretical discussion of issues surrounding coping in women, Banyard and Graham-Bermann (1993) argued that coping as it is traditionally measured is largely influenced by education and income, such that those with more resources typically cope “better.” In this respect, an individual’s social position and environment can either constrain or enhance his or her resources and choice of coping strategies (Taylor, Repetti, and Seeman, 1997).
Members of marginalized groups, because of ethnicity, social class, gender, and/or age, may face special challenges to active coping. Limitations in finances, knowledge, access to requisite technical expertise, or other resources and cultural, social, or psychological barriers may discourage active coping. In the case of minority adult men and women, assertiveness is often misperceived as aggressiveness or arrogance, and responded to with fear or punitive action. In the case of the elderly, however, active, assertive coping may not pose the same threat and may not trigger the same adverse outcome. Instead, they may derive greater benefits by being more assertive (e.g., gaining access to needed services). Additional research is needed to investigate this hypothesis and to determine under what conditions and for which ethnic, gender, and age groups does assertive versus emotion-focused coping yield more positive health outcomes.
Ethnic minority status can also influence the efficacy of certain coping strategies, especially when SES is considered. For example, the work by James (1994) on John Henryism illustrates this relationship. John Henryism is defined as active, effortful coping with adversity marked by attitudes that reflect (1) efficacious mental and physical vigor, (2) a strong commitment to hard work, and (3) a single-minded determination to succeed. When compared to higher SES African Americans and whites from all SES groups, John Henryism has been shown to predict higher blood pressure and greater risk for hypertension only in young African-American men with low socioeconomic resources (Dressler, Bindon, and Neggers, 1998; James, 1994). Thus, John Henryism appears to be relatively benign for higher SES African Americans and whites. However, for African-American men with limited resources, the benefits of effortful coping (i.e., economic survival) appear to be tempered by increased health risks.
Given that ethnic minorities are often confronted with chronic stressors that are not easily ameliorated, it is not surprising that effortful, active coping strategies such as John Henryism are likely to yield mixed results. Such coping strategies may not produce the desired changes in status and opportunity and may in fact produce high levels of anger and frustration, which might account for the higher levels of blood pressure seen in these individuals. Unfortunately, we do not know how prevalent this coping strategy is among African-American elderly or what effect long-term use has on their health and well-being. We also do not know whether members of other racial/ethnic minorities use this coping strategy, and whether the effects obtained with low-SES, younger African-American adults will be observed in older and higher SES adults in the other ethnic groups.
Limited attention has been given to identifying coping strategies that are most adaptive for ethnic minority adults and the elderly, especially those with limited resources. It is very likely that healthy functioning in the face of chronic stress exposure from low SES and/or older age requires
the development of a different array of active and passive coping strategies than is the case for those who are younger and/or who have more resources.
Religiosity
A substantial literature indicates the salience of religion and religious participation in the lives of the elderly, especially for African Americans, Hispanics, Native Americans, and Asian Americans (Mattis, 1997; McAuley, Pecchioni, and Grant, 2000; Nelson, 1989; Taylor, 1993; Villarosa, 1994; Wade-Gayles, 1995). In addition, both cross-sectional and longitudinal studies indicate that there are aging-related changes in the pattern of predominant religious behaviors, with participation in organized religious activities remaining high until late old age, then dropping off due to increased physical disability. However, religious attitudes and private religious behaviors (i.e., prayer, reading religious materials, watching or listening to religious programs) actually increase with age (Koenig, Smiley, and Gonzalez, 1988).
There is also growing evidence of a positive relationship between religious practices, spirituality, and health. In their recent review of the evidence of the role of spirituality, health, and aging, Musick, Traphagan, Koenig, and Larson (2000) generally conclude that greater religious participation and higher self-rated spirituality have been associated with lower mortality rates (Helm, Hays, Flint, Koenig, and Blazer, 2000; McCullough, Hoyt, Larson, Koenig, and Thoresen, 2000); better self-rated health, both cross-sectionally and over time; and lower risk for hypertension and lower cancer rates, especially in those religions that have strong dietary and other lifestyle restrictions. The evidence for participation and functional status are less clear because of possible reverse causation, but longitudinal studies do suggest that service attendance does influence functional health.
The beneficial effects of religion on health are believed to occur through several mechanisms, including supporting a healthier lifestyle (i.e., proscriptions against smoking, drinking, illicit drug use, more physical activity, and diet) (Idler and Kasl, 1997; Strawbridge et al., 1997), by fostering greater social integration, more social contacts, and the provision of more instrumental and emotional support (Ellison, 1995), greater marital satisfaction and stability, and greater comfort, meaning, and effective coping with major life challenges and transitions (George, Larson, Koenig, and McCullough, 2000; Harrison, Koenig, Hays, Eme-Akwari, and Pargament, 2001; Pargament, Smith, Koenig, and Perez, 1998). (See Musick et al., 2000, for a detailed discussion of this evidence.)
Several authors also note, however, that greater religiosity and religious coping can also have negative health and mental health effects, especially
because of ideological rigidity, spiritual discontent, demonic reappraisal, and negative reappraisal of God and his powers (Pargament et al., 1998).
This literature also suggests that there are important ethnic differences in religiosity between ethnic minority versus white elderly. Historically, African Americans and Hispanics have relied on religion and on the church as important sources of spiritual, emotional, and material support in coping with life stresses. In the case of African Americans, the church has also served as a powerful political force for social change and an opportunity for social status (Ellison, 1995). Thus, the prevailing view is that religion is a powerful resource for coping for all groups (George et al., 2000), especially for marginalized minority groups; that ethnic groups may engage in more religious coping with adversity than whites, and that African Americans have a more personal relationship with God (McAuley et al., 2000) and report greater satisfaction with the results of their religious coping efforts (Neighbors, Jackson, Bowman, and Gurin, 1983). For example, in a study of African-American and white elderly women with medical problems, Conway (1985) found that the majority (64 percent) of African-American women employed prayer as a coping strategy, compared to only a third of their white counterparts. Similarly, in a comparative analysis of intrinsic versus extrinsic religious orientation in African-American and white seniors, Nelson (1989) found that although religion was important for both groups, the groups differed in their religious orientation and behaviors. Compared to whites, African-American elders were more intrinsically oriented to religion (i.e., stronger spiritual beliefs and faith and more emphasis on prayer), but there were no differences in extrinsic orientation (i.e., active religious participation). These findings were also confirmed by Ellison (1995) using data from the ECA sample in the southeastern United States, which showed significantly higher rates of church attendance and religious devotion among African Americans compared to their white counterparts.
However, the evidence on the effect of religiosity on well-being, both overall and as a function of ethnicity, is mixed, suggesting the need for better designed studies and more critical analysis (Ellison, 1995; Mickley, Carson, and Soeken, 1995). Many studies suggest that religious beliefs and practices are associated with enhanced health and life satisfaction (Koenig, Siegler, and George, 1989; Levin, Chatters, and Taylor, 1995), greater perceived control (Koenig, Smiley, and Gonzalez, 1989), and greater mobility, less depression, and greater social integration in the elderly (Idler, 1987; Miller, 1998). A number of other studies have suggested, however, that the relationship among religiosity, depression, and well-being is more complex than is generally believed. For example, Nelson (1989) found that African-American elderly who were more active in church attendance and engaged in more private religious practices were more depressed than white elderly. On the other hand, in his sample of adult and elderly southerners, Ellison
(1995) found that religious coping was associated with lower depression in white respondents, but was unrelated to depression in African Americans. He argued that this unexpected finding suggests that other factors might temper the effectiveness of religious experiences and practices in moderating risk for depression in this sample of elderly southern African Americans. Unfortunately, we cannot determine from the data in either the Nelson or Ellison studies whether religious coping was ineffective in preventing depression or whether those who were depressed were simply more likely to engage in more religious coping in an effort to deal with their distress.
Additional evidence in support of the complex relationships between religiosity and health is provided by Strawbridge, Shema, Cohen, Roberts, and Kaplan (1998). They contrasted nonorganizational religiosity (i.e., prayer, importance of religious and spiritual beliefs) versus organizational religiosity (i.e., attendance at services and other religious activities) as moderators on stress and depression in the Alameda County, California Health Survey of adults ages 50 to 102. Their results indicated that although religiosity is protective for mortality and morbidity, it buffers some stressors but appears to exacerbate others. They found that nonorganizational religiosity was unrelated to depression, while organizational religiosity had a weak negative association with depression. However, while both forms of religiosity buffered the effect of nonfamily stressors (i.e., financial, health), nonorganizational religiosity exacerbated the effects of child problems, and organizational religiosity exacerbated the effects of marital problems, child and/or spousal abuse, and caregiving. Thus, religiosity may benefit those facing nonfamilial stressors, but may make coping with family crises worse.
Recent studies of African-American and Hispanic women suffering from chronic illness also found that religious coping was associated with less depression and anxiety, but did not find a similar association with physical health outcomes (Alferi, Culver, Carver, Arena, and Antoni, 1999; Woods, Antoni, Ironson, and Kling, 1999). In this respect, religious coping may be effective in reducing the psychological distress associated with chronic stressors, but may not be effective in ameliorating the negative effects of chronic stressors on health outcomes.
Taken as a whole, the evidence suggests that religion is an important spiritual and social resource for the elderly of all ethnic groups, and that African Americans and other minority elderly evidence greater religious involvement and use of religious coping than white elderly. However, the evidence also indicates that religion does not yield uniformly positive effects, especially as a buffer for depression and feelings of well-being. In fact, several studies indicate higher rates of depression and psychological distress in persons who report high religious participation. It is unclear, however, whether this reflects the ineffectiveness of religious coping or the fact that depressed individuals are more likely to seek more spiritual and social
support. Additionally, most of the comparison studies of religiosity and health have been conducted on African Americans and whites, and there are comparatively fewer empirical studies that examined the effects of religiosity on mental health in Native Americans and Asian Americans, which should be an important priority for future research.
Social Support Resources
There is a substantial body of evidence examining the importance of social relationships and availability of adequate instrumental and emotional support on health. The evidence indicates that social supports can serve as both a protector against adverse health outcomes as well as a moderator of stress in reducing its impact on health (Cohen, Underwood, and Gottlieb, 2000; Leppin and Schwarzer, 1990), including improved functional status and quality of life (Seeman, Bruce, and McAvay, 1996; Unger, McAvay, Bruce, Berkman, and Seeman, 1999) and slower cognitive aging in the elderly (Seeman et al., 2001). In addition, social support can also serve as a mediator for depression in the elderly, with lower social support leading to both decreased life satisfaction and increased depressive symptoms (Newsom and Schulz, 1996). Similarly, social isolation, inadequate social support, and problematic interpersonal relationships can have adverse effects on health and well-being, especially for women (Bazargan and Hamm-Baugh, 1995; Burg and Seeman, 1994; Newsom and Schulz, 1996), as well as for those with debilitating physical illnesses, depression, or cognitive decline (Karel, 1997; Musick, Koenig, Hays, and Cohen, 1998; Unger et al., 1999). In fact, there appears to be a reciprocal relationship between physical impairment and social support, such that the availability of social support reduces functional impairment in those with significant chronic illnesses, and in turn, functional impairment is associated with an attenuation of support or reduction in access to supports (e.g., fewer friendship contacts, inability to attend religious services or other social functions, and reduction in perceived self-efficacy) (Holahan and Holahan, 1987; Newsom and Schulz, 1996).
Evidence of the positive effects of social support have been obtained with white and ethnic minority elderly populations, and many studies have reported that ethnic minority adults and elderly tend to rely more on larger family and other informal social networks for support than whites (Antonucci and Jackson, 1987; Delgado and Humm-Delgado, 1982; Lubben and Becerra, 1987; Neighbors et al., 1983; Pruchno, 1999). However, it is unclear whether, after controlling for social class, ethnic differences continue in the number, type, quality, and efficacy of available supports. It is also unclear whether different types of social support and how this variable is conceptualized and measured (e.g., size, type of support
received, satisfaction with support received, social network composition, frequency of social contacts) have the same impact on the well-being of elders from diverse ethnic and sociocultural backgrounds. It is also important to note that reliance on informal social networks may exacerbate the stress burden of the elderly by adding to their role demands, by interfering with their autonomy and self-sufficiency, and/or by encouraging greater dependency (Coyne, Wortman, and Lehman, 1988).
Ideally, however, social support serves a positive function across the lifespan and helps maintain an individual’s sense of well-being, self-efficacy, and control (Antonucci and Jackson, 1987). In a prospective cohort study of the elderly, instrumental and subjective social support were predictors of longer time to depression remission (Bosworth, McQuoid, George, and Steffens, 2002). Absence of support from a relative or friend also has been found to predict late-life suicide among the elderly (Turvey et al., 2002). Furthermore, being married or unmarried with social support has been found to significantly reduce the impact of functional disabilities on the incidence of depression in the elderly (Schoevers et al., 2000). The role of social support, health, and well-being is addressed in greater detail in Chapter 10.
SUMMARY AND RECOMMENDATIONS FOR FUTURE RESEARCH
In summary, our goal was to offer a multidimensional biopsychosocial framework for understanding the complex relationships among psychosocial, biological, and behavioral adversities and advantages that operate over the lifespan to impact the health and well-being of the elderly. Special attention was paid to identifying some of the primary risks and resources that are likely to be implicated in racial/ethnic differences in health and well-being in late life. The available evidence suggests that adults of color, especially the elderly, carry a disproportionate burden of chronic and life-change stresses compared to white elders, and that lifetime exposure to racism and discrimination (Williams, 1999; Clark et al., 1999), stresses from acculturation (Bastida and Gonzalez, 1995; Contrada et al., 2000; Vega et al., 1998), and the greater likelihood that they will assume caretaking responsibilities for grandchildren and other relatives, should be included in assessments of their stress burdens (Burnette, 1999; Minkler et al., 1997). However, additional caregiving responsibilities do not appear to cause as much distress to minority elders compared to whites, perhaps because of greater cultural congruence of the role, greater access to larger support networks, and exposure to other seniors in their peer group who are also caring for their grandchildren (Pruchno, 1999).
The evidence also suggests that despite overall greater socioeconomic deprivation and stress in this population, there are important differences
among ethnic groups in vulnerability to distress and depression, with higher overall rates in whites and Hispanics and lower overall rates in African Americans and Asian Americans (Somervell et al., 1989; Zhang and Snowden, 1999). These ethnic group differences vary by gender, social class, geography, and age of immigration, and there is some evidence that those who immigrate during old age may be at enhanced risk relative to those who immigrated at younger ages. Regardless of ethnicity, greater psychological distress and depression are found in elderly who are older, carrying a heavier burden of medical morbidity and functional impairment, more socially isolated, and who have few family and friend social supports. Higher rates are also found in those who have little perceived control over their circumstances, who fail to use more adaptive and flexible coping strategies, whose autonomy is constrained by their circumstances, who cope with frequent interpersonal conflicts, and who rely heavily on religious coping or have little or no religious or spiritual connections (Diehl et al., 1996; Karel, 1997; Musick et al., 2000; Nelson, 1989).
In addition, the common assumptions that social supports and religiosity have uniformly positive effects for the elderly are not justified. Several studies indicate that although religiosity is protective of mortality and morbidity and appears to buffer nonfamilial stresses, it may exacerbate family conflict stresses (Pargament et al., 1998; Strawbridge et al., 1998), and may yield different results for different ethnic groups depending on what measures of religiosity are used (Ellison, 1995; Nelson, 1989).
Unfortunately, and as in other areas, there is a dearth of information on psychosocial and behavioral issues on racial/ethnic elderly, especially for Native Americans and subgroups of Hispanics and Asian Americans (Markides, 1986). Thus, a major need in the field is for more studies that focus specifically on the psychosocial and behavioral predictors of health and well-being in elderly from these understudied groups. Also, while ethnic comparison studies that investigate group differences in these factors continue to be needed, there is also a substantial need for ethnic-specific studies that can clarify which psychosocial and behavioral factors are most important in increasing and reducing risk for health outcomes in each racial/ethnic group. The latter approach will encourage more focused attention on developing and testing methodologies and measures that are most appropriate for the different ethnic groups.
In this chapter, we also argue for the need for studies that take a lifetime perspective in investigating ethnic disparities in psychological well-being and functioning. To date, most studies are cross-sectional and focus on differences in current or proximal risks and resources in accounting for differences in health and well-being. However, as argued by Geronimus (1992), Elder and Crosnoe (2002), and Singer and Ryff (1999), studies
testing such concurrent effects hypotheses are necessarily limited, and substantial additional information can be obtained by investigating the cumulative effects of lifetime advantages and adversities in predicting individual and group differences in health trajectories.
We offer one cumulative advantages and vulnerabilities model as a conceptual tool to guide future studies. This model builds on and expands on the life history approach by Singer and Ryff (1999) and the developmental perspective of Elder and Crosnoe (2002) and Geronimus (1992) by including consideration of lifetime exposure to additional sociostructural and psychosocial adversities and advantages that have specific relevance to ethnic minority elderly. In addition, the model recognizes that these risk and protective factors exert their effects through biological pathways, including genetic predispositions, allostatic load, medical burden, and psychiatric history. Finally, consistent with Singer and Ryff (1999), the model argues that it is the balance between lifetime advantages and adversities that is likely to predict psychological health and well-being over time, with a greater burden of lifetime adversities resulting in greater psychological distress and dysfunction, and an imbalance in favor of assets and advantages resulting in better overall psychological functioning. This approach also should allow for better identification of minority elders who are psychologically resilient despite high lifetime burdens of adversity.
As noted previously, although our review focused specifically on the role these hypothesized risk and protective factors play in accounting for individual and group differences in psychological distress, depression, and well-being, the proposed conceptual perspective should also be useful in investigating health disparities for a variety of other chronic diseases, including but not limited to essential hypertension and other cardiovascular diseases, chronic pain, cognitive decline and dementia, and functional impairment. Future research should consider the following priority issues:
-
Ethnic-specific studies are needed that investigate which psychosocial risk and protective factors are the most important contributors to psychological well-being and resilience in each racial/ethnic group. Specific attention is needed to estimate the relative contribution of each risk factor, to include culture-specific variables, and to determine whether there are within-group differences in the relative importance of risk and protective factors. In addition, special focus should be given to problems of particular importance to specific communities (e.g., prevention and intervention research for alcohol and drug abuse, crime and violence, and HIV/AIDS are important for low-SES communities).
-
Cross-cultural studies are needed to help us understand the differential roles each risk and protective factor might play in health outcomes for different ethnic groups. Such comparison studies should include representation from as many of the major ethnic groups in the United States as reasonable. Understanding etiological processes across ethnicities may provide additional information and understanding of how early risk exposure predicts differences in health trajectories and what resources are needed to increase resilience in these groups.
-
In conducting ethnic-specific and cross-cultural research, measurement issues need to be considered. Basic questions about the validity and generalizability of assessment instruments have yet to be resolved. For example, ethnic differences in the way social support and other coping resources are perceived and utilized have yet to be explicated. Debate also continues regarding differences in the experience, expression, and construct of mental illness, and how such illness should be treated in different ethnic groups. Our ability to understand and treat mental illness will be challenged by our ability to create new assessment measures, verify the reliability and generalizability of existing instruments, and adequately capture the differences and similarities of such constructs.
-
Longitudinal studies are also needed that test the hypothesized cumulative effects of lifetime adversities and advantages in predicting functional status in minority elderly. Particular attention should be given to the relationships among lifetime exposure to chronic life stresses, personality dispositions, coping styles, access to and utilization of social supports and formal services, and spirituality and religious participation.
-
Additionally, the investigation of ethnic disparities in health also raises a number of important statistical issues. Testing comprehensive, longitudinal models such as the one proposed will require more advanced statistical techniques. One approach that lends itself to this task is multivariate causal modeling that allows the testing of the full model as well as the separate hypothesized pathways within the model. In addition, separate models can be developed and tested for each ethnic group, thus allowing for the possibility that there are ethnic differences in the relative contributions these variables make in predicting health outcomes. For example, exposure to racism and discrimination may have different effects on health in different ethnic groups, perhaps because of differences in appraisal and coping strategies used in coping with this source of stress. This approach also allows other alternative relationships among the variables to be considered. For example, models could test whether race/ethnicity affects SES, and both SES and race/ethnicity in turn affect health.
-
Although the evidence is clear that ethnic health disparities are evident at each step in the SES gradient (Williams, 1999), debate continues about what is the best analytic approach to test the interfaces among SES,
-
ethnicity, and health. For example, while conventional practice is to statistically control for SES before testing for ethnic differences on outcomes of interest, many have argued that this may be inappropriate because it assumes that the relationship between SES and health is the same regardless of ethnicity. However, there is ample evidence that race/ethnicity conditions SES such that low SES is associated with greater functional disability and distress in populations of color compared to whites (Kessler and Neighbors, 1986), and persons of color may derive comparatively less health benefit from higher socioeconomic status than whites (Geronimus, 1992). Thus, as suggested by Kessler and Neighbors (1986), it is advisable to test for an SES X ethnicity interaction in order to determine whether the joint effect of SES and ethnicity is most adverse to health.
-
Little will be accomplished if most of our attention is focused on studies of group differences that do not inform interventions. A need continues for studies that develop and test interventions that enhance resilience by improving coping, and fostering the development of more effective social support resources, especially among the poorest minority elderly and those who immigrated at older ages. Minority groups who evidence the most difficulty are often underrepresented in research, and their needs are inadequately addressed because interventions used are not specifically tailored to their needs. More studies are needed that investigate psychosocial predictors of risk and resilience in Native American, Asian American, and Hispanic American elderly. Such research needs to recognize the heterogeneity within these larger panethnic or pancultural groups, and test for both within- and between-group differences.
-
Finally, studies are also needed to identify factors that predict successful aging and healthy functional status in populations of color. This is perhaps the most understudied issue in the field.
ACKNOWLEDGMENTS
The authors express their appreciation to Carolyn Melton, MSW, for her assistance with the review of the literature on grandparenting stresses, and to the National Research Council Panel on Race, Ethnicity and Health in Later Life and external reviewers for their feedback and recommendations on previous drafts of this manuscript.
REFERENCES
Akiskal, H.S. (1991). An integrative perspective on recurrent mood disorders: The mediating role of personality. In J. Becker and A. Kleinman (Eds.), Psychosocial aspects of depression (pp. 215-235). Hillsdale, NJ: Lawrence Erlbaum Associates.
Aldwin, C.M. (1992). Aging, coping, and efficacy: Theoretical framework for examining coping in life-span developmental context. In M.L. Wykle, E. Kahana, and J. Kowal (Eds.), Stress and health among the elderly (pp. 96-113). New York: Springer.
Alferi, S.M., Culver, J.L., Carver, C.S., Arena, P.L., and Antoni, M.H. (1999). Religiosity, religious coping, and distress: A prospective study of Catholic and Evangelical Hispanic women in treatment for early-stage breast cancer. Journal of Health Psychology, 4(3), 343-356.
Altschuler, L.L., Wang, X.D., Qi, H.Q., Wang, W.Q., and Xia, M.L. (1988). Who seeks mental health care in China? Diagnoses of Chinese outpatients according to DSM-III criteria and the Chinese classification system. American Journal of Psychiatry, 145, 872-875.
Anderson, N.B., McNeilly, M., and Myers, H.F. (1992). Autonomic reactivity and hypertension in blacks: Toward a contextual model. In E.H. Johnson, W.D. Johnson, and S. Julius (Eds.), Personality, elevated blood pressure and essential hypertension (pp. 197-216). New York: Hemisphere.
Anderson, N.B., McNeilly, M., and Myers, H.F. (1993). A biopsychosocial model of race differences in vascular reactivity. In J.J. Blascovich and E.S. Katkin (Eds.), Cardiovascular reactivity to psychological stress and disease (pp. 83-108). Washington, DC: American Psychological Association.
Antonucci, T.C., and Jackson, J.S. (1987). Social support, interpersonal efficacy, and health: A life course perspective. In L.L. Carstensen, B.A. Edelstein, and L. Dornbrand (Eds.), Handbook of clinical gerontology (pp. 21-31). New York: Pergamon Press.
Balcazar, H., Peterson, G.W., and Krull, J.L. (1997). Acculturation and family cohesiveness in Mexican American pregnant women: Social and health implications. Family and Community Health, 20, 16-31.
Ballenger, J.C., Davidson, J.R., Lecrubier, Y., Nutt, D.J., Kirmayer, L.J., Lepine, J.P., Lin, K.M., Tajima, O., and Ono, Y. (2001). Consensus statement on transcultural issues in depression and anxiety from the International Consensus Group on Depression and Anxiety. Journal of Clinical Psychiatry, 62(Suppl. 13), 47-55.
Banyard, V.L., and Graham-Bermann, S.A. (1993). Can women cope? A gender analysis of theories of coping with stress. Psychology of Women Quarterly, 17, 303-318.
Bastida, E., and Gonzalez, G. (1995). Mental health status and needs of black and white elderly: Differences in depression. In D.K. Padgett (Ed.), Handbook on ethnicity, aging, and mental health (pp. 99-112). Westport, CT: Greenwood Press.
Bazargan, N., and Hamm-Baugh, V.P. (1995). The relationship between chronic illness and depression in a community of urban black elderly persons. Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 50(2), S119-S127.
Beals, J., Manson, S., Shore, J.H., Friedman, M., Ashcraft, M., Fairbanks, J.A., and Schlenger, W.E. (2002). The prevalence of posttraumatic stress disorder among American Indian Vietnam veterans: Disparities and context. Journal of Traumatic Stress, 15(2), 89-97.
Berry, J.W. (1998). Acculturation and health: Theory and research. In S. Kazarian and D. Evans (Eds.), Cultural clinical psychology: Theory, research, and practice (pp. 39-57). New York: Oxford University Press.
Blanchard, M. (1996). Old age depression—a biological inevitability? International Review of Psychiatry, 8(4), 379-385.
Blazer, D., Burchett, B., Service, C., and George, L.K. (1991). The association of age and depression among the elderly: An epidemiologic exploration. Journal of Gerontology, 46, 210-215.
Blazer, D.G., Kessler, R.C., McGonagle, K.A., and Swartz, M.S. (1994). The prevalence and distribution of major depression in a national community sample: The National Comorbidity Survey. American Journal of Psychiatry, 151, 979-986.
Bosworth, H.B., McQuoid, D.R., George, L.K., and Steffens, D.C. (2002). Time-to-remission from geriatric depression: Psychosocial and clinical factors. American Journal of Geriatric Psychiatry, 10(5), 551-559.
Brodaty, H., Luscombe, G., Parker, G., Wilhelm, K., Hickie, I., Austin, M., and Mitchell, P. (2001). Early and late onset depression in old age: Different aetiologies, same phenomenology. Journal of Affective Disorders, 66, 225-236.
Brown, D.R., Ahmed, F., Gary, L.E., and Milburn, N.G. (1995). Major depression in a community sample of African Americans. American Journal of Psychiatry, 152(3), 373-378.
Burg, M.M., and Seeman, T.E. (1994). Families and health: The negative side of social ties. The Society of Behavioral Medicine, 16(2), 109-115.
Burnam, M.A. Hough, R.L., Karno, M., Escobar, J.I., and Telles, C. (1987). Acculturation and lifetime prevalence of psychiatric disorders among Mexican Americans in Los Angeles. Journal of Health and Social Behavior, 28, 89-102.
Burnette, D. (1997). Grandparents raising grandchildren in the inner-city. Families in Society, 78, 489-499.
Burnette, D. (1999). Social relationships of Hispanic grandparent caregivers: A role theory perspective. The Gerontologist, 39(1), 49-58.
Canino, G.J., Bird, H.R., Shrout, P.E., Rubio-Stipec, M., Bravo, M., Martinez, R., Sesman, M., and Guevara, L.M. (1987). The prevalence of specific psychiatric disorders in Puerto Rico. Archives of General Psychiatry, 44, 727-735.
Casper, L.M., and Bryson, K.R. (1998). Coresident grandparents and their grandchildren: Grandparent-maintained families. Population Division Working Paper No. 26. Washington, DC: U.S. Bureau of the Census.
Centers for Disease Control and Prevention. (2001). Health, United States: 2001 with urban and rural health chartbook. Hyattsville, MD: National Center for Health Statistics.
Chen, C.N., Wong, J., Lee, N., Chan-Ho, M.W., Lau, J.T., and Fung, M. (1993). The Shatin community mental health survey in Hong Kong II: Major findings. Archives of General Psychiatry, 50, 125-133.
Chisholm, J.F. (1996). Mental health issues in African-American women. Annals of the New York Academy of Sciences, 789, 161-179.
Chou, K., and Chi, I. (2000). Stressful events and depressive symptoms among old women and men: A longitudinal study. International Journal of Aging and Human Development, 51(4), 275-293.
Chun, K.M., Organista, P.M., and Marin, G. (2002). Acculturation: Advances in theory, measurement, and applied research. Washington, DC: American Psychological Association.
Clark, R., Anderson, N.B., Clark, V.R., and Williams, D.R. (1999). Racism as a stressor for African Americans: A biopsychosocial model. American Psychologist, 54(10), 805-816.
Cohen, S., Kessler, R.C, and Gordon, L.U. (1995). Strategies for measuring stress in studies of psychiatric and physical disorders . In S. Cohen, R.C. Kessler, and L.U. Gordon (Eds.), Measuring stress: A guide for health and social scientists (pp. 3-26). New York: Oxford University Press.
Cohen, S., Underwood, L.G., and Gottlieb, B.H. (2000). Social support measurement and intervention: A guide for health and social scientists. New York: Oxford University Press.
Contrada, R.J., Ashmore, R.D., Gary, M.L., Coups, E., Egeth, J.D., Sewell, A., Ewell, K., Goyal, T.M., and Chasse, V. (2000). Ethnicity-related sources of stress and their effects on well-being. Current Directions in Psychological Science, 9(4), 136-139.
Conway, K. (1985). Coping with the stress of medical problems among black and white elderly. International Journal of Aging and Human Development, 21, 39-48.
Cook, J.M., Pearson, J.L., Thompson, R., Black, B.S., and Rabins, P.V. (2002). Suicidality in older African Americans: Findings from the EPOCH study. American Journal of Geriatric Psychiatry, 10(4), 437-446.
Cooper, J.E., and Sartorius, N. (1996). Mental disorders in China: Results of the national epidemiological survey in 12 areas. London: Gaskell.
Cortes, D.E., Rogler, L.H., and Malgady, R.G. (1994). Biculturality among Puerto Rican adults in the United States. American Journal of Community Psychology, 22, 707-721.
Coyne, J.C., Wortman, C.B., and Lehman, D.R. (1988). The other side of support: Emotional overinvolvement and miscarried helping. In B.H. Gottlieb (Ed.), Marshalling social support: Format, process, and effects (pp. 305-330). Thousand Oaks, CA: Sage.
Cross-National Collaborative Group. (1992). The changing rate of major depression: Cross-national comparisons. Journal of the American Medical Association, 268, 3098-3105.
Curyto, K.J., Chapleski, E.E., Lichtenberg, P.A., Hodges, E., Kaczynski, R., and Sobeck, J. (1998). Prevalence and prediction of depression in American Indian elderly. Clinical Gerontologist, 18, 19-37.
Curyto, K.J., Chapleski, E.E., and Lichtenberg, P.A. (1999). Prediction of the presence and stability of depression in the Great Lakes Native American elderly. Journal of Mental Health and Aging , 5, 323-340.
Delgado, M., and Humm-Delgado, D. (1982). Natural support systems: Source of strength in Hispanic communities. Social Work, 27, 83-89.
Diehl, M., Coyle, N., and Labouvie-Vief, G. (1996). Age and sex differences in strategies of coping and defense across the life span. Psychology and Aging, 11, 127-139.
Dohrenwend, B.P., Levav, I., Shrout, P.E., Schwartz, S., Naveh, G., Link, B.G., Skodol, A.E, and Stueve, A. (1992). Socioeconomic status and psychiatric disorders: The causation-selection issue. Science, 255(5047), 946-952.
Dressler, W.W., and Badger, L.W. (1985). Epidemiology of depressive symptoms in black communities: A comparative analysis. Journal of Nervous and Mental Disorders, 173, 212-220.
Dressler, W.W., Bindon, J.R., and Neggers, Y.H. (1998). John Henryism, gender, and arterial blood pressure in an African American community. Psychosomatic Medicine, 60, 620-624.
Eizenman, D.R., Nesselroade, J.R., Featherman, D.L., and Rowe, J.W. (1997). Intraindividual variability in perceived control in an older sample: The MacArthur successful aging studies. Psychology and Aging, 12(3), 489-502.
Elder, G.H. Jr. (1998). The life course as developmental theory. Child Development, 69(1), 1-12.
Elder, G.H., Jr., and Crosnoe, R. (2002). The influence of early behavior patterns on later life. In L. Pulkkinen and A. Caspi (Eds.), Paths to successful development: Personality in the life course (pp. 157-176). New York: Cambridge University Press.
Ellison, C.G. (1995). Race, religious involvement and depressive symptomatology in a southeastern U.S. community. Social Science and Medicine, 40(11), 1561-1572.
Escobar, J.E., Karno, M., Burnam, A., Hough, R.L., and Golding, J. (1988). Distribution of major mental disorders in a U.S. metropolis. Acta Psychiatrica Scandinavica (Suppl. 344), 45-53.
Escobar, J.I. (1998). Immigration and mental health: Why are immigrants better off? Archives of General Psychiatry, 55, 781-782.
Fabrega, H., Mezzich, J., and Ulrich, R.F. (1988). African American-white differences in psychopathology in an urban psychiatric population. Comprehensive Psychiatry, 29, 285-297.
Fang, C.Y., and Myers, H.F. (2001). The effects of racial stressors and hostility on cardiovascular reactivity in African American and white men. Health Psychology, 20(1), 64-70.
Flaskerud, J.H., and Hu, L.T. (1994). Participation in and outcome of treatment for major depression among low income Asian Americans. Psychiatry Research, 53, 289-300.
George, L.K., Blazer, D., Winfield-Laird, I., Leaf, P.J., and Fischbach, R.I. (1988). Psychiatric disorders and mental health service use in later life: Evidence from the Epidemiologic Catchment Area program. In J. Brody and G. Maddox (Eds.), Epidemiology and aging (pp. 189-219). New York: Springer.
George, L.K., Larson, D.B., Koenig, H.G., and McCullough, M.E. (2000). Spirituality and health: What we know, what we need to know. Journal of Social and Clinical Psychology, 19(1), 102-116.
Geronimus, A.T. (1992). The weathering hypothesis and the health of African-American women and infants: Evidence and speculations. Ethnicity and Disease, 2, 207-221.
Gibson, R.C. (1993). The Black American retirement experience. In J.S. Jackson, L.M. Chatters, and R.J. Taylor (Eds.), Aging in black America (pp. 277-297). Thousand Oaks, CA: Sage.
Golding, J.M., Karno, M., and Rutter, C.M. (1990). Symptoms of major depression among Mexican-Americans and non-Hispanic whites. American Journal of Psychiatry, 147, 861-866.
Goldwasser, H.D., and Badger, L.W. (1989). Utility of the psychiatric screen among the Navajo of Chinle: A fourth-year clerkship experience. American Indian Alaska Native Mental Health Research, 3, 6-15.
Hammen, C.L., Davila, J., Brown, G.P., Gitlin, M.J., and Ellicott, A. (1992). Stress as a mediator of the effects of psychiatric history on severity of unipolar depression. Journal of Abnormal Psychology, 101, 45-52.
Harden, A.W., Clark, R., and Maguire, K. (1997). Informal and formal kinship care. Report for the Office of the Assistant Secretary for Planning and Evaluation (Task Order HHS-100-95-0021) . Washington, DC: U.S. Department of Health and Human Services.
Harkness, K.L., Monroe, S.M., Simons, A.D., and Thase, M. (1999). The generation of life events in recurrent and non-recurrent depression. Psychological Medicine, 29, 135-144.
Harris, T.B., Savage, P.J., Tell, G.S., Haan, M., Kumanyika, S., and Lynch, J.C. (1997). Carrying the burden of cardiovascular risk in old age: Associations of weight and weight change with prevalent cardiovascular disease, risk factors, and health status in the Cardiovascular Health Study. American Journal of Clinical Nutrition, 66(4), 837-844.
Harrison, M.O., Koenig, H.G., Hays, J.C., Eme-Akwari, A.G., and Pargament, K.I. (2001). The epidemiology of religious coping: A review of recent literature. International Review of Psychiatry, 13(2), 86-93.
Heckhausen, J., and Schulz, R. (1993). Optimization by selection and compensation: Balancing primary and secondary control in life span development. International Journal of Behavioral Development, 16, 287-303.
Helm, H.M., Hays, J.C., Flint, E.P., Koenig, H.G., and Blazer, D.G. (2000). Does private religious activity prolong survival? A six-year follow-up study of 3,851 older adults . Journals of Gerontology, Series A: Biological Sciences and Medical Sciences, 55(7), M400-M405.
Holahan, C.K., and Holahan, C.J. (1987). Life stresses, hassles, and self-efficacy in aging: A replication and extension. Journal of Applied Social Psychology, 17(6), 574-592.
Holahan, C.K., Holahan, C.J., and Belk, S.S. (1984). Adjustment in aging: The roles of life stresses, hassles, and self-efficacy. Health Psychology, 3(4), 315-328.
Hurtado, A. (1995). Variations, combinations, and evolutions: Hispanic families in the United States. In R.E. Zanbrana (Ed.), Understanding Hispanic families: Scholarship, policy, and practice (pp. 40-61). Thousand Oaks, CA: Sage.
Husaini, B.A., Moore, S.T., Castor, R.S., Neser, W., Whitten-Stovall, R., Linn, J.G., and Griffin, D. (1991). Social density, stressors, and depression: Gender differences among the black elderly. Journal of Gerontology: Psychological Sciences, 46(5), 236-242.
Hwang, W., Myers, H., and Takeuchi, D. (2000). Psychosocial predictors of first-onset depression in Chinese Americans. Social Psychiatry and Psychiatric Epidemiology, 35, 133-145.
Hwang, W., Chun, C., Takeuchi, D.T., Myers, H.F., and Prabha, S. (in press). Age at first-onset depression among Chinese Americans. Journal of Consulting and Clinical Psychology.
Hwu, H., Yeh, E., and Chang, L. (1989). Prevalence of psychiatric disorders in Taiwan defined by the Chinese Diagnostic Interview Schedule. Acta Psychiatrica Scandinavica, 79, 136-147.
Idler, E.L. (1987). Religious involvement and the health of the elderly: Some hypotheses and an initial test. Social Forces, 66(1), 226-238.
Idler, E.L., and Kasl, S.V. (1997). Religion among disabled and nondisabled persons II: Attendance at religious services as a predictor of the course of disability. Journal of Gerontology, Series B: Psychology and Social Science, 52(6), S306-S316.
James, S.A. (1994). John Henryism and the health of African-Americans. Culture, Medicine and Psychiatry, 18(2), 163-182.
Jendrek, M.P. (1994). Grandparents who parent their grandchildren: Circumstances and decisions. Gerontologist, 34, 206-216.
Jones, C.J., and Meredith, W. (1996). Patterns of personality change across the life span. Psychology and Aging, 11, 57-65.
Kales, H.C., Blow, F.C., Bingham, C.R., Copeland, L.A., and Mellow, A.M. (2000). Race and inpatient psychiatric diagnoses among elderly veterans. Psychiatric Services, 51(6), 795-800.
Karel, M.J. (1997). Aging and depression: Vulnerability and stress across adulthood. Clinical Psychology Review, 17(8), 847-879.
Kasch, K.L., and Klein, D.N. (1996). The relationship between age of onset and comorbidity in psychiatric disorders. Journal of Nervous and Mental Disease, 184(11), 703-707.
Kelley, S.J., Whitley, D., Sipe, J., and Yorke, B.C. (2000). Psychological distress in grandmother kinship care providers: The role of resources, social support, and physical health. Child Abuse and Neglect, 24(3), 311-321.
Kessler, R.C., and Neighbors, H.W. (1986). A new perspective on the relationships among race, social class and psychological distress. Journal of Health and Social Behavior, 27, 107-115.
Kinzie, J.D., Leung, P.K., Boehnlein, J., Matsunaga, D., Johnson, R., Manson, S., Shore, J.H., Heinz, J., and Williams, M. (1992). Psychiatric epidemiology of an Indian village: A 19-year replication study. Journal of Nervous and Mental Disease, 180(1), 33-39.
Kirmayer, L.J., and Young, A. (1998). Culture and somatization: Clinical, epidemiological, and ethnographic perspectives. Psychosomatic Medicine, 60, 420-430.
Klein, D.N., Taylor, E.B., Harding, K., and Dickstein, S. (1988). Double depression and episodic major depression: Demographic, clinical, familial, personality, and socioenvironmental characteristics and short-term outcome. American Journal of Psychiatry, 145, 1226-1231.
Klein, D.N., Schatzberg, A.F., McCullough, J.P., Dowling, F., Goodman, D., Howland, R.H., Markowitz, J.C., Smith, C., Thase, M.E., Rush, A.J., LaVange, L., Harrison, W.M., and Keller, M.B. (1999). Age of onset in chronic major depression: Relation to demographic and clinical variables, family history, and treatment response. Journal of Affective Disorders, 55, 149-158.
Kleinman, J.C., Fingerhut, L.A., and Prager, K. (1991). Differences in infant mortality by race, nativity status, and other maternal characteristics. American Journal of Diseases of Childhood , 145, 194-195.
Koenig, H., Smiley, M., and Gonzalez, J.A.P. (1988). Religion, health, and aging. Westport, CT: Greenwood Press.
Koenig, H.G., Siegler, I.C., and George, L.K. (1989). Religious and non-religious coping: Impact on adaptation in later life. Journal of Religion and Aging, 5, 73-94.
Kornhaber, A. (1996). Contemporary grandparenting. Thousand Oaks, CA: Sage.
Krause, N., and Liang, J. (1993). Stress, social support, and psychological distress among the Chinese elderly. Journal of Gerontology, 48(6), 282-291.
Krieger, N., and Sidney, S. (1996). Racial discrimination and blood pressure: The CARDIA study of young black and white adults. American Journal of Public Health, 86, 1370-1378.
Krieger, N., Rowley, D.L., Herman, A.A., Avery, B., and Phillips, M.T. (1993). Racism, sexism, and social class: Implications for studies of health, disease, and well-being. American Journal of Preventive Medicine, 9(Suppl. 6), 82-122.
Kua, E.H. (1990). Depressive disorder in elderly Chinese people. Acta Psychiatrica Scandinavica, 81(4), 386-388.
Kumanyika, S.K. (1998). Obesity in African Americans: Biobehavioral consequences of culture. Ethnicity and Disease, 8(1), 93-96.
Kuo, W. (1984). Prevalence of depression among Asian-Americans. Journal of Nervous and Mental Disease, 172, 449-457.
LaFromboise, T., Coleman, H.L.K., and Gerton, J. (1995). Psychological impact of biculturalism: Evidence and theory. In N.R. Goldberger, J.B. Veroff et al. (Eds.), The culture and psychology reader (pp. 489-535). New York: New York University Press.
Lawton, M.P., Kleban, M.H., Rajagopal, D., and Dean, J. (1992). Dimensions of affective experience in three age groups. Psychology and Aging, 7, 171-184.
Lazarus, R.S., and Folkman, S. (1984). Stress, appraisal and coping. New York: Springer.
Lee, C.K., Kwak, Y.S., Yamamoto, J., Rhee, H., Kim, Y.S., Han, J.H., Choi, J.O., and Lee, Y.H. (1990). Psychiatric epidemiology in Korea, Part I: Gender and age differences in Seoul. Journal of Nervous and Mental Disease, 175(4), 242-246.
Leppin, A., and Schwarzer, R. (1990). Social support and physical health: An updated meta-analysis. In L.R. Schmidt, P. Schwenkmezzger, P.J. Weinman, and S. Maes (Eds.), Theoretical and applied aspects of health psychology (pp. 185-202). Chur, Switzerland: Harwood Academic Press.
Lestra, C., D’Amato, T., Ghaemmaghami, C., Perret-Liaudet, A., Broyer, M., Renaud, B., Dalery, J., and Chamba, G. (1998). Biological parameters in major depression: Effects of paroxetine, viloxazine, moclobemide, and electroconvulsive therapy: Relation to early clinical outcome. Biological Psychiatry, 44(4), 274-280.
Levin, J.S., Chatters, L.M., and Taylor, R.J. (1995). Religious effects on health status and life satisfaction among black Americans. Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 50(3), S154-S163.
Lewinsohn, P.M., Fenn, S., Stanton, A.K., and Franklin, J. (1986). Relation of age at onset to duration of episode in unipolar depression. Journal of Psychology and Aging, 1(1), 63-68.
Lewinsohn, P.M., Rohde, P., Seeley, J.R., and Fischer, S.A. (1991). Age and depression: Unique and shared effects. Psychology and Aging, 6(2), 247-260.
Lobel, M., Dunkel-Schetter, C., and Scrimshaw, S. (1992). Prenatal maternal stress and prematurity: A prospective study of socioeconomically disadvantaged women. Health Psychology, 11(1), 32-40.
Lubben, J.E., and Becerra, R.M. (1987). Social support among black, Mexican, and Chinese elderly. In D.E. Gelfand and C.M. Barresi (Eds.), Ethnic dimensions in aging (pp. 18-34). New York: Springer.
Lugaila, T. (1998). Marital status and living arrangements: March, 1997. Current Population Reports Series. Washington, DC: U.S. Bureau of the Census.
Lyons, M.J., Eisen, S.A., Goldberg, J., True, W., Lin, N., Meyer, J.M., Toomey, R., Faraone, S.V., Merla-Ramos, M., and Tsuang, M.T. (1998). A registry-based twin study of depression in men. Archives of General Psychiatry, 55(5), 468-472.
Manson, S.M. (1992). Long-term care of older American Indians: Challenges in the development of institutional services. In C. Barresi and D.E. Stull (Eds.), Ethnicity and long-term care (pp. 130-143). New York: Springer.
Manson, S.M. (1995). Mental health status and needs of the American Indian and Alaska Native elderly. In D.K. Padgett (Ed.), Handbook on ethnicity, aging, and mental health (pp. 132-141). Westport, CT: Greenwood Press.
Markides, K.S. (1986). Minority status, aging, and mental health. International Journal of Aging and Human Development, 23(4), 285-300.
Mattis, J. (1997). Spirituality and religiosity in the lives of black women. African American Research Perspectives, 3, 56-60.
McAuley, W.J., Pecchioni, L., and Grant, J.A. (2000). Personal accounts of the role of God in health and illness among older rural African American and white residents. Journal of Cross-Cultural Gerontology, 15(1), 13-35.
McCrae, R.R. (1982). Age differences in the use of coping mechanisms. Journal of Gerontology, 37, 454-460.
McCullough, M.E., Hoyt, W.T., Larson, D.B., Koenig, H.G., and Thoresen, C. (2000). Religious involvement and mortality: A meta-analytic review. Health Psychology, 19(3), 211-222.
McEwen, B.S. (1998). Stress, adaptation, and disease: Allostasis and allostatic load. In S.M. McCann, J.M. Lipton et al. (Eds.), Annals of the New York Academy of Sciences. Vol. 840. Neuroimmunomodulation: Molecular aspects, integrative systems, and clinical advances (pp. 33-44). New York: New York Academy of Sciences.
McEwen, B.S., and Seeman, T. (1999). Protective and damaging effects of mediators of stress: Elaborating and testing the concepts of allostasis and allostatic load. In N.E. Adler, M. Marmot, B.S. McEwen, and J. Stewart (Eds.), Socioeconomic status and health in industrial nations: Social, psychological, and biological pathways (pp. 30-47). New York: New York Academy of Sciences.
McEwen, B.S., and Stellar, E. (1993). Stress and the individual mechanisms leading to disease. Archives of Internal Medicine, 153, 2093-2101.
McLean, D.E., and Link, B.G. (1994). Unraveling complexity: Strategies to refine concepts, measures, and research designs in the study of life events and mental health. In W.R. Avison and I.H. Gotlib (Eds.), Stress and mental health: Contemporary issues and prospects for the future (pp. 15-42). New York: Plenum Press.
Mickley, J.R., Carson, V., and Soeken, K.L. (1995). Religion and mental health: State of the science in nursing. Issues in Mental Health Nursing, 16(4), 345-366.
Miller, K.J. (1998). Life satisfaction in older adults: The impact of social support and religious maturity. Dissertation Abstracts International: Section B: The Sciences and Engineering, 59(6-B), 3067.
Minkler, M., and Fuller-Thompson, E. (1999). The health of grandparents raising grandchildren: Results of a national study. American Journal of Public Health, 89(9), 1384-1389.
Minkler, M., and Roe, K.M. (1993). Grandparents as surrogate parents. Generation, 20, 304-338.
Minkler, M., Fuller-Thompson, E., Miller, D., and Driver, D. (1997). Depression in grandparents raising grandchildren: Results of a national longitudinal study. Archives of Family Medicine, 6, 445-452.
Monroe, S.M., and Simons, A.D. (1991). Diathesis-stress theories in the context of life stress research: Implications for the depressive disorders. Psychology Bulletin, 110(3), 406-425.
Moore, M.R., and Chase-Landsdale, P.L. (2001). Sexual intercourse and pregnancy among African American girls in high-poverty neighborhoods: The role of family and perceived community environment. Journal of Marriage and the Family, 63(4), 1146-1157.
Moyerman, D.R., and Forman, B.D. (1992). Acculturation and adjustment: A meta-analytic study. Hispanic Journal of Behavioral Sciences, 14, 163-200.
Musick, M.A, Koenig, H.G., Hays, J.C, and Cohen, H.J. (1998). Religious activity and depression among community-dwelling elderly persons with cancer: The moderating effect of race. Journal of Gerontology, Series B: Psychology and Social Science, 53(4), S218-227.
Musick, M.A., Traphagan, J.W., Koenig, H.G., and Larson, D.B. (2000). Spirituality in physical health and aging. Journal of Adult Development, 7(2), 73-86.
Myers, H.F., and Taylor, S. (1998). Family contributions to risk and resilience in African American children . Journal of Comparative Family Studies, 29(1), 215-229.
Myers, H.F., Kagawa-Singer, M., Kumanyika, S.K., Lex, B.W., and Markides, K.S. (1995). Panel III: Behavioral risk factors related to chronic diseases in ethnic populations. Health Psychology, 14(7), 613-621.
Myers, H.F., Anderson, N.B., and Strickland, R. (1996). Biobehavioral perspective for research on stress and hypertension in black adults. Theoretical and empirical issues. In R. Jones (Ed.), African American mental health (pp. 1-36). Hampton, VA: Cobb and Henry.
Myers, H.F., Lesser, I., Rodrigues, N., Mira, C.B., Hwang, W., Camp, C., Anderson, D., Erickson, L., and Wohl, M. (2002a). Ethnic differences in clinical presentation of depression in adult women. Cultural Diversity and Ethnic Minority Psychology, 8(2), 138-156.
Myers, H.F., Lewis, T.T., and Parker-Dominguez, T. (2002b). Stress, coping and minority health: Biopsychosocial perspective on ethnic health disparities. In G. Bernal, J. Trimble, K. Burlew, and F. Leong (Eds.), Handbook of racial and ethnic minority psychology. Thousand Oaks, CA: Sage.
Nakane, Y., Ohta, Y., Radford, M., Yan, H., et al. (1991). Comparative study of affective disorders in three Asian countries: II. Differences in prevalence rates and symptom presentation. Acta Psychiatrica Scandinavica, 84, 313-319.
National Center for Post-Traumatic Stress Disorder and National Center for American Indian and Alaska Native Mental Health Research Center. (1996). Matsunaga Vietnam Veterans Project. White River Junction, VT.
Neighbors, H.W., Jackson, J.S., Bowman, P.J., and Gurin, G. (1983). Stress, coping, and black mental health: Preliminary findings from a national study. Prevention and Human Services, 2, 5.
Nelson, P.B. (1989). Ethnic differences in intrinsic/extrinsic religious orientation and depression in the elderly. Archives of Psychiatric Nursing, 3(4), 199-204.
Newsom, J.T., and Schulz, R. (1996). Social support as a mediator in the relation between functional status and quality of life in older adults. Psychology of Aging, 11(1), 34-44.
Nicassio, P.M. (1985). The psychosocial adjustment of the Southeast Asian refugee: An overview of empirical findings and theoretical models. Journal of Cross-Cultural Psychology, 16(2), 153-173.
Nicholson, B.L. (1997). The influence of pre-emigration and postemigration stressors on mental health: A study of Southeast Asian refugees. Social Work Research, 21(1), 19-31.
Orr, S.T., James, S.A., Miller, C A., Barakt, B., Daikoku, N., Pupkin, M., Engstrom, K., and Huggins, G. (1996). Psychosocial stressors and low birthweight in an urban population. American Journal of Preventive Medicine, 12(6), 457-466.
Padgett, D. (1998). Aging minority women: Issues in research and health policy. Women and Health, 14, 213-225.
Pargament, K.I., Smith, B.W., Koenig, H.G., and Perez, L. (1998). Patterns of positive and negative religious coping with major life stressors. Journal of the Scientific Study of Religion, 37(4), 710-724.
Pruchno, R. (1999). Raising grandchildren: The experiences of black and white grandmothers. The Gerontologist, 39(2), 209-221.
Raskin, A., Crook, T.H., and Herman, K.D. (1975). Psychiatric history and symptom differences in black and white depressed patients. Journal of Consulting and Clinical Psychology, 43, 73-80.
Regier, D.A., Boyd, J.H., Burke, J.D., Rae, D.S., Myers, J.K., Kramer, M., Robins, L.N., George, L.K., Karno, M., and Locke, B.Z. (1988). One-month prevalence of mental disorders in the United States. Based on five epidemiologic area sites. Archives of General Psychiatry, 45, 977-986.
Regier, D.A., Farmer, M.E., Rae, D.S., Myers, J.K., Kramer, M., Robins, L.N., George, L.K., Karno, M., and Locke, B.Z. (1993). One-month prevalence of mental disorders in the United States and sociodemographic characteristics: The Epidemiologic Catchment Area Study. Acta Psychiatrica Scandinavica, 88, 35-47.
Reid, P.T., and Bing, V.M. (2000). Sexual role of girls and women: An ethnocultural lifespan perspective. In C.B. Travis, J.W. White, et al. (Eds.), Sexuality, society, and feminism (pp. 141-166). Washington, DC: American Psychological Association.
Roberts, R.E., Kaplan, G.A., Shema, S.J., and Strawbridge, W.J. (1997a). Does growing old increase the risk for depression? American Journal of Psychiatry, 154(10), 1384-1390.
Roberts, R.E., Roberts, C.R., and Chen, Y.R. (1997b). Ethnocultural differences in prevalence of adolescent depression. American Journal of Community Psychology, 25, 95-109.
Rodgers-Farmer, A.Y. (1999). Parenting stress, depression, and parenting in grandmothers raising their grandchildren. Children and Youth Services Review, 21(5), 377-388.
Rogler, L., Cortes, D.E., and Malgady, R.G. (1991). Acculturation and mental health status among Hispanics: Convergence and new directions of research. American Psychologist, 6, 585-597.
Roysircar-Sodowsky, G., and Maestas, M.V. (2000). Acculturation, ethnic identity, and acculturative stress: Evidence and measurement. In R.H. Dana et al. (Eds.), Handbook of cross-cultural and multicultural personality assessment (pp. 131-172). Hillsdale, NJ: Lawrence Erlbaum Associates.
Ruiz, D.S. (1995). A demographic and epidemiologic profile of the ethnic elderly. In D. Padget (Ed.), Handbook on ethnicity, aging, and mental health (pp. 3-21). Westport, CT: Greenwood Press.
Sabogal, F., Marin, G., and Otero-Sabogal, R. (1987). Hispanic familism and acculturation: What changes and what doesn’t? Hispanic Journal of Behavioral Sciences, 9, 397-412.
Sands, R.G., and Goldberg-Glen, R.S. (2000). Factors associated with stress among grandparents raising their grandchildren. Family Relations, 49, 97-105.
Schoevers, R.A., Beekman, A.T.F., Deeg, D.J.H., Geerlings, M.I., Jonker, C., and Van Tilburg, W. (2000). Risk factors for depression in later life: Results of a prospective community based study (AMSTEL). Journal of Affective Disorders, 59(2), 127-137.
Seeman, T.E., Bruce, M.L., and McAvay, G.J. (1996). Social network characteristics and onset of ADL disability: MacArthur studies of successful aging. Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 51(4), S191-S200.
Seeman, T.E., Singer, B.H., Rowe, J.W., Horwitz, R.I., and McEwen, B.S. (1997). Price of adaptation—allostatic load and its health consequences: MacArthur studies of successful aging. Archives of Internal Medicine, 157, 2259-2268.
Seeman, T.E, Unger, J.B, McAvay, G., and Mendes de Leon, C.F. (1999). Self-efficacy beliefs and perceived declines in functional ability: MacArthur studies of successful aging . Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 54(4), P214-222.
Seeman, T.E., Lusignolo, T.M., Albert, M., and Berkman, L. (2001). Social relationships, social support, and patterns of cognitive aging in healthy, high functioning older adults: MacArthur studies of successful aging. Health Psychology, 20(4), 243-255.
Shaw, B.A., and Krause, N. (2001). Exploring race variations in aging and personal control. Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 6(2), S119-S124.
Shiono, P.H., Rauh, V.A., Park, M., Lederman, S.A., and Suskar, D. (1997). Ethnic differences in birthweight: Lifestyle and other factors. American Journal of Public Health, 87(5), 787-793.
Siegel, J.M., Aneshensel, C.S., Taub, B., Cantwell, D.P., and Driscoll, A.K. (1998). Adolescent depressed mood in a multiethnic sample. Journal of Youth and Adolescence, 27(4), 413-427.
Singer, B., and Ryff, C.D. (1999). Hierarchies of life histories and associated health risks. In N.E. Adler, M. Marmot, B.S. McEwen, and J. Stewart (Eds.), Socioeconomic status and health in industrial nations: Social, psychological, and biological pathways (pp. 96-115). New York: New York Academy of Sciences.
Smedley, B.D., Stith, A.Y., and Nelson, A.R. (Eds.). (2002). Unequal treatment: Confronting racial and ethnic disparities in health care. Washington, DC: National Academy Press.
Snowden, L.R. (1998). Racial differences in informal help-seeking for mental health problems. Journal of Community Psychology, 26(5), 429-438.
Snowden, L.R., and Cheung, F.K. (1990). Use of inpatient mental health services by members of ethnic minority groups. American Psychologist, 45, 347-355.
Somervell, P.D., Leaf, P.J., Weissman, M.M., Blazer, D.G., and Bruce, M.L. (1989). The prevalence of major depression in black and white adults in five United States communities. American Journal of Epidemiology, 130(4), 725-735.
Sorenson, S.B., Rutter, C.M., and Aneshensel, C.S. (1991). Depression in the community: An investigation into age of onset. Journal of Consulting and Clinical Psychology, 59, 541-546.
Strawbridge, W.J., Wallhagen, M.I., Shema, S.J., and Kaplan, G.A. (1997). New burdens or more of the same? Comparing grandparent, spouse, and adult child caregivers. The Gerontologist, 37(4), 505-510.
Strawbridge, W.J., Shema, S.J., Cohen, R.D., Roberts, R.E., and Kaplan, G.A. (1998). Religiosity buffers effects of some stressors on depression but exacerbates others. Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 53(3), S118-S126.
Stern, S.L., Dhanda, R., and Hazuda, H.P. (2001). Hopelessness predicts mortality in older Mexican and European Americans. Psychosomatic Medicine, 63(3), 344-351.
Sue, D., and Sue, S. (1987). Cultural factors in the clinical assessment of Asian Americans. Journal of Consulting and Clinical Psychology, 55(4), 479-487.
Sue, S., Fujino, D., Hu, L., Takeuchi, D., and Zane, N. (1991). Community mental services for ethnic minority groups: A test of the cultural responsiveness hypothesis. Journal of Consulting and Clinical Psychology, 59, 533-540.
Swenson, C.J., Baxter, J., Shetterly, S.M., Scarbro, S.L., and Hamman, R.F. (2000). Depressive symptoms in Hispanic and non-Hispanic white rural elderly: The San Luis Valley Health and Aging Study. American Journal of Epidemiology, 152(11), 1048-1055.
Szinovacz, M.E. (1998). Grandparents today: A demographic profile. The Gerontologist, 38, 37-52.
Takeuchi, D.T., Leaf, P.J., and Kuo, H.S. (1988). Ethnic differences in the perception of barriers to help-seeking. Social Psychiatry and Psychiatric Epidemiology, 23(4), 273-280.
Takeuchi, D.T., Chung, R.C., Lin, K.M., Shen, H., Kurasaki, K., Chun, C., and Sue, S. (1998). Lifetime and twelve-month prevalence rates of major depressive episodes and dysthymia among Chinese Americans in Los Angeles. American Journal of Psychiatry, 155, 1407-1414.
Taylor, R.J. (1993). Religion and religious observances. In J.S. Jackson, L.M. Chatters, and R.J. Taylor (Eds.), Aging in black America (pp. 101-123). Thousand Oaks, CA: Sage.
Taylor, S.E., Repetti, R.L., and Seeman, T.E. (1997). Health psychology: What is an unhealthy environment and how does it get under the skin? Annual Review of Psychology, 48, 411-447.
Turnbull, J.E., and Mui, A.C. (1995). Mental health status and needs of black and white elderly: Differences in depression. In D.K. Padgett (Ed.), Handbook on ethnicity, aging, and mental health (pp. 73-98). Westport, CT: Greenwood Press.
Turvey, C.L., Conwell, Y., Jones, M.P., Phillips, C., Simonsick, E., Pearson, J.L., and Wallace, R. (2002). Risk factors for late-life suicide: A prospective community-based study. American Journal of Geriatric Psychiatry, 10(4), 398-406.
Unger, J.G., McAvay, G., Bruce, M.L., Berkman, L., and Seeman, T. (1999). Variation in the impact of social network characteristics on physical functioning in elderly persons: MacArthur studies of successful aging. Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 54(5), S245-S251.
U.S. Census Bureau. (2001). United States Census 2000. Available: http://www.census.gov [accessed March 2003].
Van den Berg, M.D., Oldehinkel, A.J., Bouhuys, A.L., Brilman, E.I., Beekman, A.T.F., and Ormel, J. (2001). Depression in later life: Three etiologically different subgroups. Journal of Affective Disorders, 65, 19-26.
Vega, W.A., Kolody, B., Aguilar-Gaxiola, S., Alderete, E., Catalano, R., and Caraveo-Anduaga, J. (1998). Lifetime prevalence of DSM-III-R psychiatric disorders among urban and rural Mexican Americans in California. Archives of General Psychiatry, 55, 771-782.
Villarosa, L. (Ed.). (1994). Body and soul: The black women’s guide to physical health and emotional well-being. A National Black Women’s Health Project Book. New York: HarperCollins.
Wade-Gayles, G. (Ed.). (1995). My soul is a witness: African-American women’s spirituality. Boston: Beacon Press.
Walen, H.R., and Lachman, M.E. (2000). Social support and strain from partner, family, and friends: Costs and benefits for men and women in adulthood. Journal of Social and Personal Relationships, 17(1), 5-30.
Weissman, M.M., Bruce, M.L., Leaf, P.J., Florio, L.P., and Holzer, C., III. (1991). Affective disorders. In L.N. Robins and D.A. Regier (Eds.), Psychiatric disorders in America: The epidemiologic catchment area study (pp. 53-80). New York: The Free Press.
Weissman, M.M., Bland, R.C., Canino, G.J., Faravelli, C., Greenwald, S., Hwu, H., Joyce, P.R., Karam, E.G., Lee, C., Lellouch, J., Lepine, J., Newman, S.C., Rubio-Stipec, M., Wells, J.E., Wickramaratne, P.J., Wittchen, H., and Yeh, E. (1996). Cross-national epidemiology of major depression and bipolar disorder. Journal of the American Medical Association, 276(4), 293-299.
Wickrama, K.A.S., Conger, R.D., Wallace, L.E., and Elder, G.J., Jr. (1999). The intergenerational transmission of health-risk behaviors: Adolescent lifestyles and gender moderating effects. Journal of Health and Social Behavior, 40(3), 258-272.
Williams, D.R. (1999). Race, socioeconomic status, and health: The added effects of racism and discrimination. In N.E. Adler, M. Marmot, B.S. McEwen, and J. Stewart (Eds.), Socioeconomic status and health in industrial nations: Social, psychological, and biological pathways (pp. 173-188). New York: New York Academy of Sciences.
Williams, D.R., Takeuchi, D.T., and Adair, R. (1992). Socioeconomic status and psychiatric disorder among blacks and whites . Social Forum, 71, 179-194.
Williams, D.R., Yu, Y., Jackson, J.S., and Anderson, N.B. (1997). Racial differences in physical and mental health: Socio-economic status, stress and discrimination. Journal of Health Psychology, 2(3), 335-351.
Wilson, C., Civic, D., and Glass, D. (1995). Prevalence and correlates of depressive syndromes among adults visiting an Indian Health Service primary care clinic. American Indian Alaska Native Mental Health Research, 6(2), 1-12.
Wong, P.T., and Reker, G.T. (1985). Stress, coping and well-being in Anglo and Chinese elderly. Canadian Journal on Aging, 4(1), 29-37.
Wong, P.T.P., and Ujimoto, V K. (1998). The elderly: The stress, coping, and mental health. In L.C. Lee and N.W.S. Zane (Eds.), Handbook of Asian American psychology (pp. 165-209). Thousand Oaks, CA: Sage.
Woo, J., Ho, S.C., Lau, J., and Yuen, Y.K. (1994). The prevalence of depressive symptoms and predisposing factors in an elderly Chinese population. Acta Psychiatrica Scandinavica, 89(1), 8-13.
Woods, T.E., Antoni, M.H., Ironson, G.H., and Kling, D.W. (1999). Religiosity is associated with affective status in symptomatic HIV-infected African-American women. Journal of Health Psychology, 4(3), 317-326.
Yamamoto, J., Rhee, S., and Chang, D. (1994). Psychiatric disorders among elderly Koreans in the United States. Community Mental Health Journal, 30(1), 17-27.
Yamamoto, J., Chung, C., Nukariya, K., Ushijima, S., Kim, J., Dai, Y., Zhang, S., Ao, M., Cheung, F., Chang, D., and Winn, T. (1997). Depression prevention, suicide prevention in elderly Asian Americans. American Journal of Forensic Psychiatry, 18, 75-83.
Yu, E.S. (1986). Health of the Chinese elderly in America. Research on Aging, 8, 84-109.
Zambrana, R.E., Dunkle-Schetter, C., Collins, N.L., and Scrimshaw, S.C. (1999). Mediators of ethnic-associated differences in infant birth weight. Journal of Urban Health, 76(1), 102-116.
Zane, N., Enomoto, K., and Chun, C.-A. (1994). Treatment outcomes of Asian and white American clients in outpatient therapy. Journal of Community Psychology, 22, 177-191.
Zhang, A.Y., and Snowden, L.R. (1999). Ethnic characteristics of mental disorders in five U.S. communities. Cultural Diversity and Ethnic Minority Psychology, 5(2), 134-146.
Zhang, A.Y., Snowden, L.R., and Sue, S. (1998). Differences between Asian and white Americans’ help seeking and utilization patterns in the Los Angeles area. Journal of Community Psychology, 26(4), 317-326.
Zheng, Y.P., Lin, K.M., Takeuchi, D.T., Kurasaki, K.S., and Cheung, F. (1997). An epidemiological study of neurasthenia in Chinese-Americans in Los Angeles. Comprehensive Psychiatry, 38(5), 249-259.