1
INTRODUCTION
A teenager diving into a shallow lake, a young mother in a car accident on her way to work, a collapse of a workman’s scaffolding, an elderly woman falling down a flight of stairs—spinal cord injuries can happen to anyone at any time. Going from daily routine to a life-changing spinal cord injury can put independent living in jeopardy and totally reconfigure the realities of daily life. The events that cause spinal cord injuries are sudden and unexpected; however, the resulting physical and lifestyle constraints and limitations remain lifelong challenges.
Although advances in medicine and neuroscience have resulted in limited progress in developing therapeutic interventions for spinal cord injuries, many current avenues of research suggest that a concerted research effort on spinal cord injuries could result in important gains in restoring function and improving quality of life. This report highlights the current status of spinal cord injury research, examines the research and infrastructure needs, and provides recommendations for advancing and accelerating progress in the treatment of spinal cord injuries.
The ancient Egyptians declared spinal cord injury as a condition “not to be treated.” Early efforts to treat spinal cord injuries began to be developed by the Greek physician Hippocrates, who constructed several rudimentary forms of traction using a board or ladder to immobilize the patient’s back (Eltorai, 2002). Development of antiseptics and sterilization techniques in the 1800s improved the rates of survival from surgery. However, it has been estimated that during World War I 90 percent of the individuals who sustained a spinal cord injury died within 1 year of the injury and only approximately 1 percent survived more than 20 years (Swain
and Grundy, 2002). “Up until the 1940s, spinal cord injury was essentially a death sentence. If the injury itself didn’t prove fatal, then the complications … became fatal” (Kreutz, 2004). Since then, the development of antibiotics, improvements in general medical care, and advances in rehabilitation medicine and in technologies such as respirators have resulted in gains in patient survival, care, and life expectancy. Although the life expectancy for an individual with a spinal cord injury has improved dramatically, it remains lower than that for the general population (Charlifue and Lammertse, 2002).
EXTENT AND COSTS
It is estimated that 11,000 spinal cord injuries occur each year in the United States and that 247,000 Americans are living with a spinal cord injury (NSCISC, 2004). Most individuals with spinal cord injuries are young adults, primarily males (78.2 percent of cases since 2000) (NSCISC, 2004). The average age at the time of injury has increased in recent years, from an average of 28.6 years in 1979 to the current average of 38 years. Explanations for this trend include greater numbers of injuries in the population over 60 years of age (the percentage of individuals older than 60 years of age at the time of injury increased from 4.7 percent before 1980 to 10.9 percent since 2000) and the general aging of the U.S. population (NSCISC, 2004). Only about 5 percent of spinal cord injuries occur in children, usually as a result of traffic accidents or falls (Swain and Grundy, 2002).
Historical trends in spinal cord injury incidence in the United States showed an increase from 22 per million population in the period from 1935 to 1944 to 71 per million population from 1975 to 1981. That rate has fallen, however, to the current rate of approximately 40 incidents of spinal cord injuries per million population each year, a rate that has remained stable for the past 20 years (Sekhon and Fehlings, 2001; DeVivo, 2002). These statistics indicate that unless new treatments or preventive measures are developed, spinal cord injuries will likely continue to be the source of severe disability and loss of function for thousands of Americans each year.
On the basis of reports to the National Spinal Cord Injury Statistical Center (NSCISC), the major causes of spinal cord injuries in the United States are motor vehicle crashes and traffic accidents (50.4 percent); followed by falls (23.8 percent); violent acts (11.2 percent), primarily gunshot wounds; and recreational sports activities (9.0 percent) (NSCISC, 2004). Recent trends, however, show a decrease in work-related causes of injuries and an increase in sports and recreational causes (Sekhon and Fehlings, 2001). Causes of injuries also vary between regions of the country and between urban and rural locations. Table 1-1 provides NSCISC demo-
TABLE 1-1 Demographics of Persons in the NSCISC Database by Year of Injury
graphic data for individuals with spinal cord injuries occurring in the periods from 1973 to 1977 and 1995 to 1999.
The nature and extent of spinal cord injuries vary widely, depending on the site of the injury and its severity. Table 1-2 highlights the heterogeneous nature of the functional outcomes resulting from spinal cord injuries. Each individual’s experience is unique in terms of the degree of paralysis and pain, the extent of spasticity, and the therapies involved in stabilizing autonomic system dysfunction. Therefore, how a spinal cord injury impacts a person’s life is highly individualized. Injuries to the upper sections of the spine nearest the head can result in quadriplegia (also termed tetraplegia), with the individual losing motor and sensory functions in the arms and legs, as well as bowel, bladder, chest, abdominal, and diaphragm function. Injuries occurring in the lower areas of the spine may
TABLE 1-2 Activities of Daily Living, by Level of Spinal Cord Injury
|
Activities of Daily Living |
Level of Injury |
|||
|
Cervical 1-3 |
Cervical 4 |
Cervical 5 |
Cervical 6 |
|
|
Respiratory control |
|
May be able to breathe without ventilator |
|
|
|
Bowel control |
Total assist |
Total assist |
Total assist |
Independent to total assist |
|
Bladder control |
Total assist |
Total assist |
Total assist |
Some to total assist |
|
Bed mobility |
Total assist |
Total assist |
Some assist |
Independent to total assist |
|
Bed and wheelchair transfers |
Total assist |
Total assist |
Total assist |
Independent to total assist |
|
Pressure relief and positioning |
Total assist; may be independent with equipment |
Total assist; may be independent with equipment |
Independent with equipment |
Independent with equipment |
|
Eating |
Total assist |
Total assist |
Total assist for setup, then independent eating with equipment |
Independent |
|
Dressing |
Total assist |
Total assist |
|
|
|
Grooming |
Total assist |
Total assist |
Some to total assist |
Some assist to independent |
|
Bathing |
Total assist |
Total assist |
Total assist |
|
|
Wheelchair propulsion |
|
|
|
|
|
Standing and ambulation |
Total assist |
Total assist |
Total assist |
Total assist |
|
Communication |
Total assist to independent |
Total assist to independent |
Independent to some assist |
Independent |
|
Transportation |
Total assist |
Total assist |
Total assist to independent |
Independent |
|
Amount of assistance required |
24-hour care |
24-hour care |
Home care: 6 hours/day Personal care: 10 hours/day |
Home care: 4 hours/day Personal care: 6 hours/day |
|
Activities of Daily Living |
Level of Injury |
|||
|
Cervical 7-8 |
Thoracic 1-9 |
Thoracic 10-Lumbar 1 |
Lumbar 2-Sacral 5 |
|
|
Respiratory control |
|
Low endurance |
Intact function |
Intact function |
|
Bowel control |
Some to total assist |
Independent |
Independent |
Independent |
|
Bladder control |
Independent to some assist |
Independent |
Independent |
Independent |
|
Bed mobility |
Independent to some assist |
Independent |
Independent |
Independent |
|
Bed and wheelchair transfers |
Independent to some assist |
Independent |
Independent |
Independent |
|
Pressure relief and positioning |
Independent |
Independent |
Independent |
Independent |
|
Eating |
Independent |
Independent |
Independent |
Independent |
|
Dressing |
|
Independent |
Independent |
Independent |
|
Grooming |
Independent |
Independent |
Independent |
Independent |
|
Bathing |
|
Independent |
Independent |
Independent |
|
Wheelchair propulsion |
Independent to some assist |
Independent |
Independent |
Independent |
|
Standing |
Independent to some assist |
Independent |
Independent |
Independent |
|
Communication |
Independent |
Independent |
Independent |
Independent |
|
Transportation |
Independent |
Independent |
Independent |
Independent |
|
Amount of assistance required |
Home care: 2 hours/day Personal care: 6 hours/day |
Homemaking: 3 hours/day |
Homemaking: 2 hours/day |
Homemaking: 0-1 hour/day |
|
SOURCE: Reprinted with permission, from Sie and Waters, 2002. Copyright 2002 by Demos Medical Publishing. |
||||
result in paraplegia (loss of movement and sensation in the lower body) or the loss of specific functions.
An injury is categorized as complete if the patient has no sensory or motor function below the level of injury and as incomplete if the patient has such function (see Chapter 2). Data from the Model Spinal Cord Injury System since 2000 show that the most frequent neurological category at discharge is incomplete quadriplegia (34.3 percent), followed by complete paraplegia (25.1 percent), complete quadriplegia (22.1 percent), and incomplete paraplegia (17.5 percent) (NSCISC, 2004). Depending on the extent of the injury, the individual can recover some function and sensation (Levi, 2004). Many patients with complete paraplegia at 72 hours postinjury do not regain any function (Maynard et al., 1979). Individuals with incomplete paraplegia or tetraplegia have higher rates of improvements in motor function (Ditunno et al., 2000). An important prognostic factor is the preservation of sensation, particularly in the anal area. In one study, 47 percent of patients with incomplete sensory function at 72 hours postinjury and 87 percent of patients with incomplete motor function at 72 hours postinjury recovered the ability to walk within a year (Maynard et al., 1979).
The economic costs of spinal cord injuries largely depend on the severity of the injury and the nature of the resulting disability. The costs are highest in the first year after injury, primarily because of emergency, hospital, and rehabilitation care costs. Data on hospital admissions show that the average length of hospital stay in the acute care unit for patients with spinal cord injuries declined from 25 days in 1974 to 15 days in 2002; over that same period similar decreases were seen for stays in rehabilitation facilities (a decrease from 115 days to 40 days) (NSCISC, 2004). An analysis of the potential impacts of these reductions was not provided.
In 1996, the total annual cost of spinal cord injuries in the United States was estimated to be $9.73 billion, including an estimated $2.6 billion in lost productivity (Table 1-3) (Berkowitz et al., 1998). Of the total cost, first year costs were estimated to be $2.58 billion. Individuals with spinal cord injuries also incur significant costs for home and vehicle modifications, equipment purchase, medications, and personal assistance services (Table 1-4), with an estimate of $244,000 for each individual’s first-year medical and home modification costs (Berkowitz et al., 1998). Costs are higher for those with more disabling injuries (Table 1-4).
In discussing the health outcomes from spinal cord injuries and their associated costs, it is helpful to put these types of injuries into perspective with other diseases and health conditions (Table 1-5). Spinal cord injuries, although relatively infrequent health outcomes, impose heavy economic costs on society, particularly as they often affect young people and severely limit their productivity and quality of life. The economic costs to an indi-
TABLE 1-3 Costs of Spinal Cord Injuries to Society (1996)
|
Service |
Costs ($ millions) |
|
First-Year Costs |
|
|
First-year medical and related costs |
2,366.57 |
|
Initial home modifications |
221.58 |
|
Total first-year costs |
2,588.15 |
|
Annual Costs |
|
|
Medical care (recurring) |
1,624.86 |
|
Medications and supplies |
449.02 |
|
Vehicle modifications |
103.01 |
|
Home modifications (recurring) |
67.83 |
|
Wheelchairs |
235.60 |
|
Personal assistance |
2,068.10 |
|
Total annual costs |
4,548.42 |
|
Indirect Costs |
2,591.11 |
|
Total Costs |
9,727.68 |
|
SOURCE: Reprinted with permission, from Berkowitz et al., 1998. Copyright 1998 by Demos Medical Publishing. |
|
TABLE 1-4 Average Yearly Individual Expenses (2004 dollars)
|
Severity of Injury |
First-Year Expenses |
Expenses for Each Subsequent Year |
|
High tetraplegia (C1 to C4) |
$682,957 |
$122,334 |
|
Low tetraplegia (C5 to C8) |
$441,025 |
$50,110 |
|
Paraplegia |
$249,549 |
$25,394 |
|
Incomplete motor function |
$201,273 |
$14,106 |
|
NOTE: C1 to C8 refer to the site of the injury on the cervical section of the spinal column (see Chapter 2). SOURCE: Reprinted with permission, from NSCISC, 2004. Copyright 2004 by NSCISC. |
||
vidual over his or her lifetime can be as high as $2.7 million for someone with high tetraplegia who is injured at 25 years of age (NSCISC, 2004). On the other hand, the average age at diagnosis of many of the diseases that affect the nervous system is older, resulting in lower lifetime costs. For example, only 15 percent of those diagnosed with Parkinson’s disease are younger than age 50. Of the individuals with Alzheimer’s disease, 3 percent are between the ages of 65 to 74 at the time of diagnosis, whereas nearly
TABLE 1-5 Comparison of the Extent and Costs of Selected Neurological Conditions
|
Injury or Disease |
Estimated Current Prevalence in the U.S. (number of cases) |
Estimated Annual Incidence in the U.S. (number of new cases per year) |
Estimated Annual Cost to Society, $ billions (year used as base estimate)a |
|
Spinal cord injury |
247,000 |
11,000 |
9.7 (1996) |
|
Multiple sclerosis |
400,000 |
10,400b |
20.0 |
|
Epilepsy |
2,300,000 |
181,000 |
12.5 (1995) |
|
Parkinson’s disease |
500,000 |
50,000 |
5.6 |
|
Alzheimer’s disease |
4,500,000 |
377,000 |
100.0 (1991) |
|
Stroke |
5,400,000 |
700,000c |
56.8 |
|
aThe cost estimates were calculated by a variety of methods and with various years as their basis. Most of the estimates include direct and indirect costs. Where available the year used as the basis for the estimate is included in parentheses. bThis number is based on the National Multiple Sclerosis Society estimate that 200 individuals are diagnosed each week with multiple sclerosis. cIn any given year, 500,000 are first attacks and 200,000 are recurrent attacks. SOURCES: Ernst and Hay, 1994; Berkowitz et al., 1998; Begley et al., 2000; Hebert et al., 2001, 2003; National Multiple Sclerosis Society, 2004; NINDS, 2004; NSCISC, 2004; American Heart Association, 2005. |
|||
half of those age 85 and older may have the disease (Alzheimer’s Disease Education & Referral Center, 2004). The average age for those who suffer spinal cord injuries (28.6 years) is similar to that of individuals who are diagnosed with multiple sclerosis or who suffer a brain trauma.
These economic costs are only a hint of the enormously devastating physical, social, and emotional burdens that individuals and their families face after a spinal cord injury. To have limited or no ability to walk, pick up a coffee cup, or write with a pencil or pen and to face daily routines that take many times longer than before the injury are a fraction of the hardships and challenges that individuals living with spinal cord injuries continually encounter. With tenacity, creativity, and compassion, these challenges have been and continue to be overcome by individuals living with spinal cord injuries and their families. Furthermore, a number of
nonprofit organizations work tirelessly to support individuals with spinal cord injuries and their families and caregivers.
SPECTRUM OF PREVENTION TO TREATMENT
In delineating the scope of this report, it is useful to consider the framework that has been developed in the field of injury prevention and control to represent the injury process. Injury events are attributable to the uncontrolled release of physical energy (kinetic, chemical, thermal, electrical, or radiation energy) (Haddon, 1968). In considering the events that result in an injury, there are three temporal phases of injury causation: pre-event, event, and postevent (Haddon, 1980). Each phase requires different types of interventions to prevent or treat the resulting injury. In the pre-event phase, efforts are focused on how to prevent the injury from occurring. Examples of pre-event interventions include highway design improvements and the construction of pedestrian crosswalks and overpasses. Research on interventions in the second phase, when the injury is occurring, is focused on the transfer of energy to the individual and the negation or minimization of the injury. Second-phase interventions include the installation of airbags in vehicles, the use of bicycle and motorcycle helmets, appropriate emergency medical services at the time of injury, and rapid transfer and evacuation to definitive care. These are active areas of research that have resulted in innovations that have saved lives and reduced the severities of injuries, including spinal cord injuries.
The third phase—the postevent phase of the injury—is the focus of this report. After the injury has occurred, the goal is to minimize the damage and restore the lost function and former quality of life. As described in greater detail in Chapter 2, the acute-care phase of the injury—the short period of time just after the injury has occurred—is a window of opportunity to minimize the injury and prevent further damage or loss of function from occurring. Once the patient is stabilized, there are opportunities for a range of therapeutic interventions to improve or restore the lost function. Developing acute and chronic care interventions is the challenge facing the spinal cord injury research community.
DEFINING A CURE
Defining what constitutes a “cure” is an integral part of discussions on future directions for spinal cord injury research. In large part, the general public’s perception of a cure for spinal cord injury has been the restoration of motor function—to walk. However, a spinal cord injury affects many systems and functions of the body that are vital to the health and well-being of the injured person. Neural control of motor, sensory, autonomic, bowel,
and bladder functions are compromised, often leading to pain, pressure sores, infection, and diminished physiological well-being.
After carefully considering input from individuals with spinal cord injuries, researchers, and clinicians, the committee decided to take a broad approach to “defining a cure” and to frame its definition around alleviating the multiple disabilities that result from spinal cord injury.
Spinal cord injury research should focus on preventing the loss of function and on restoring lost functions—including sensory, motor, bowel, bladder, autonomic, and sexual functions—with the elimination of complications, particularly pain, spasticity, pressure sores (decubitus ulcers), and depression, with the ultimate goal of fully restoring the activity and function of an individual to his or her preinjury levels.
By setting forth a set of goals for spinal cord injury research, the committee wishes to emphasize the different stages of the injury during which interventions are needed and the multiple health impairments that affect an individual’s daily quality of life and that require the development of effective therapeutic interventions (Figure 1-1).
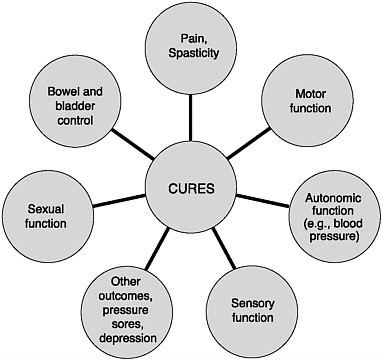
FIGURE 1-1 Outcomes of spinal cord injuries.
Walking again is not my “gold standard.” If I could take a pill and be cured of paralysis and be able to walk, that is just fine. But I guarantee you that in this chair I could keep up with any one of you going down the street outside. My problem everyday is the little things. It is the pressure sore. It is the dexterity. It is that kind of thing that I wish that we could make progress as far as restoration of function is concerned.
—John Bollinger
Paralyzed Veterans of America
FROM CHALLENGES TO OPPORTUNITIES
Although breakthroughs in the biomedical sciences in the past 50 years have resulted in medications and interventions for the treatment of many health disorders and diseases, progress in treating spinal cord injuries has been slow and uneven. However, a confluence of factors (described below) now points to more rapid progress. Some of the hurdles that have stymied progress in the past are now being overcome and other opportunities are being realized. A few of these opportunities are highlighted below, and these and others are further discussed throughout the report.
-
Understanding the biology of the nervous system. For years it was thought that neurons in mammals do not regenerate and that it was not possible to initiate axonal growth. However, beginning in the 1980s, the discovery that neurons in rat spinal cords could regenerate and make functional connections and that regeneration could be enhanced with changes in the environment of the damaged nerve cells opened possibilities to an array of research approaches to the treatment of spinal cord injuries. Other recent advances—including the ongoing elucidation of the biological blockers and promoters of nerve regeneration—have continued to accelerate research progress and move research closer toward clinical therapies
-
Emergency medical treatment. Emergency care for individuals with spinal cord injuries has only recently reached a point at which rapid response, standardized protocols for the immobilization and treatment of neck injuries, and the training of emergency medical technicians have led to increased survival rates and decreases in the number of complete spinal cord injuries. More patients thus present to the emergency department with residual function. Furthermore, the challenges of conducting clinical trials of emergency care interventions may be beginning to be overcome with the development of networks of trauma centers and the development of protocols and standards for addressing informed-consent issues in emergency situations.
-
Research tools and imaging techniques. Improved laboratory tech-
-
niques and refined statistical methodologies are opening up opportunities for more closely monitoring the effects of potential therapeutic interventions. Furthermore, significant advances have made it possible to more closely visualize neuronal growth and alterations in vivo and to identify regions of damage to the spinal cord.
-
Leveraging progress in treating other conditions. Progress in other fields of research may well be critical in advancing therapies for spinal cord injuries. Insights into neuronal injury and repair are being gained through research on neurodegenerative disorders, and research in other areas (such as understanding the role of stem cell biology in cancer) may prove important.
In acknowledging the opportunities ahead for spinal cord injury research, care must also be taken not to minimize the challenges. Treating spinal cord injury, particularly in the near term, will involve improving functional deficits and quality of life. The complexity of the nervous system, the varied nature of spinal cord injuries, and the severity of the loss of function present real and significant hurdles to be overcome to reach the ultimate goals of restoring total function. The urgent need to cure this devastating condition should not tempt overly optimistic predictions of recovery or time frames that cannot be met.
SCOPE AND ORGANIZATION OF THIS REPORT
In 1998 the state of New York established the New York State Spinal Cord Injury Research Trust to focus on funding and coordinating research on therapeutic interventions for spinal cord injuries (see Chapter 8). Monies for this fund are obtained from surcharges on fines for certain traffic violations, as well as from gifts and donations. In 2002, the New York State Spinal Cord Injury Research Board requested that the Institute of Medicine (IOM) examine the current state of research on spinal cord injuries and make recommendations on priorities for research efforts, particularly with a focus on translational research and strategies to accelerate progress in this field (Box 1-1).
The IOM appointed a 13-member committee with expertise in neuroscience, clinical research, trauma surgery, health care, physiology, and biomedical engineering. The committee met four times during the course of its work and held three workshops (Appendix A) to receive input on future directions for spinal cord injury research. Additionally, the committee received input from individuals with spinal cord injuries and from relevant nonprofit organizations.
This report provides the committee’s recommendations for furthering spinal cord injury research. Written for a broad audience that includes
|
BOX 1-1 Spinal cord injuries are a leading cause of major disability, and there is currently no cure for such injuries. However, over the last several decades there has been a steady flow of new scientific findings suggesting that spinal connections damaged by injury can be functionally restored. An Institute of Medicine committee will identify approaches and strategies that offer the promise of accelerating the development of cures for spinal cord injuries. Particular attention will be paid to strategies for translating the advances in neuroscience and cell biology to clinical research and treatment. In addition, the study will provide recommendations to its sponsor, the Health Department of the State of New York and its Spinal Cord Injury Research Board, about how to best utilize its resources to facilitate progress in translational spinal cord injury research. The committee will:
|
individuals with spinal cord injuries, advocates, policy makers, researchers, and clinicians, the report provides both broad overviews of the issues as well as specific details on the science of spinal cord injury. Chapter 2 introduces the biology of spinal cord injury and the state of the science. Chapter 3 focuses on advances in research technologies and tools. Chapter 4
describes the current status of therapeutic interventions for spinal cord injuries, and Chapter 5 provides an overview of the progress that is being made in neural repair and regeneration. Chapter 6 discusses the issues involved in moving research from the laboratory to the bedside and particularly addresses the challenges and opportunities for clinical trials on therapeutic interventions for spinal cord injuries. In Chapter 7, the committee examines the research infrastructure and proposes recommendations for accelerating progress in spinal cord injury research. Chapter 8 highlights the state programs in spinal cord injury research and provides recommendations to the New York State Spinal Cord Injury Research Board, the sponsor of this study.
REFERENCES
Alzheimer’s Disease Education & Referral Center. 2004. General Information. [Online]. Available: http://www.alzheimers.org/generalinfo.htm#howmany [accessed November 11, 2004].
American Heart Association. 2005. Heart Disease and Stroke Statistics—2005 Update. Dallas: American Heart Association.
Begley CE, Famulari M, Annegers JF, Lairson DR, Reynolds TF, Coan S, Dubinsky S, Newmark ME, Leibson C, So EL, Rocca WA. 2000. The cost of epilepsy in the United States: An estimate from population-based clinical and survey data. Epilepsia 41(3): 342-351.
Berkowitz M, Harvey C, Greene CG, Wilson SE. 1998. Spinal Cord Injury: An Analysis of Medical and Social Costs. New York: Demos Medical Publishing.
Charlifue S, Lammertse D. 2002. Spinal cord injury and aging. In: Lin V, Cardenas DD, Cutter NC, Frost FS, Hammond MC, Lindblom LB, Perkash I, Waters R, eds. Spinal Cord Medicine: Principles and Practice. New York: Demos Medical Publishing. Pp. 829-838.
DeVivo MJ. 2002. Epidemiology of spinal cord injury. In: Lin V, Cardenas DD, Cutter NC, Frost FS, Hammond MC, Lindblom LB, Perkash I, Waters R, eds. Spinal Cord Medicine: Principles and Practice. New York: Demos Medical Publishing. Pp. 79-85.
Ditunno JF Jr, Cohen ME, Hauck WW, Jackson AB, Sipski ML. 2000. Recovery of upper-extremity strength in complete and incomplete tetraplegia: A multicenter study. Archives of Physical Medicine and Rehabilitation 81(4): 389-393.
Eltorai IB. 2002. History of spinal cord medicine. In: Lin V, Cardenas DD, Cutter NC, Frost FS, Hammond MC, Lindblom LB, Perkash I, Waters R, eds. Spinal Cord Medicine: Principles and Practice. New York: Demos Medical Publishing. Pp. 3-14.
Ernst RL, Hay JW. 1994. The US economic and social costs of Alzheimer’s disease revisited. American Journal of Public Health 84(8): 1261-1264.
Haddon W Jr. 1968. The changing approach to the epidemiology, prevention, and amelioration of trauma: The transition to approaches etiologically rather than descriptively based. American Journal of Public Health & the Nation’s Health 58(8): 1431-1438.
Haddon W Jr. 1980. Advances in the epidemiology of injuries as a basis for public policy. Public Health Reports 95(5): 411-421.
Hebert LE, Beckett LA, Scherr PA, Evans DA. 2001. Annual incidence of Alzheimer disease in the United States projected to the years 2000 through 2050. Alzheimer Disease & Associated Disorders 15(4): 169-173.
Hebert LE, Scherr PA, Bienias JL, Bennett DA, Evans DA. 2003. Alzheimer disease in the US population: Prevalence estimates using the 2000 census. Archives of Neurology 60(8): 1119-1122.
Kreutz D. 2004, October 17. Tucson quadriplegics live Reeve’s battle. Arizona Daily Star. Pp. 2-4.
Levi ADO. 2004. Approach to the patient and diagnostic evaluation. In: Winn HR, Youmans JR, eds. Neurological Surgery: A Comprehensive Reference Guide to the Diagnosis and Management of Neurological Problems. Vol. 4. 5th ed. Philadelphia: W. B. Saunders. Pp. 4869-4884.
Maynard FM, Reynolds GG, Fountain S, Wilmot C, Hamilton R. 1979. Neurological prognosis after traumatic quadriplegia. Three-year experience of California regional spinal cord injury care system. Journal of Neurosurgery 50(5): 611-616.
National Multiple Sclerosis Society. 2004. National Multiple Sclerosis Society. [Online]. Available: http://www.nationalmssociety.org [accessed October 28, 2004].
NINDS (National Institute of Neurological Disorders and Stroke). 2004. Parkinson’s Disease: Hope Through Research. [Online]. Available: http://www.ninds.nih.gov/disorders/parkinsons_disease/detail_parkinsons_disease.htm [accessed November 11, 2004].
NSCISC (National Spinal Cord Injury Statistical Center). 2004. Facts and Figures at a Glance—August 2004. [Online]. Available: http://www.spinalcord.uab.edu/show.asp?durki=21446 [accessed November 11, 2004].
Sekhon LH, Fehlings MG. 2001. Epidemiology, demographics, and pathophysiology of acute spinal cord injury. Spine 26(24 Suppl): S2-12.
Sie I, Waters RL. 2002. Outcomes following spinal cord injury. In: Lin V, Cardenas DD, Cutter NC, Frost FS, Hammond MC, Lindblom LB, Perkash I, Waters R, eds. Spinal Cord Medicine: Principles and Practice. New York: Demos Medical Publishing. Pp. 87-103.
Swain A, Grundy D. 2002. At the accident. In: Grundy D, Swain A, eds. ABC of Spinal Cord Injury. 4th ed. London: British Journal of Medicine. Pp. 1-4.

















