1
Introduction
Human beings are the heart of health care. It is their labor and their intellect that translate science and technology into healing and hope. Just as oils and brushes without painters cannot create art, drugs and diagnostics without health workers cannot create health care. Nowhere is this more evident today than in the fight against global HIV/AIDS, the greatest health crisis of our time. As of this writing in 2005, close to 40 million people harbor HIV, 95 percent of whom live in resource-poor areas. Even before the pandemic hit, the health systems in these areas were weak and understaffed. Since the disease emerged, the dearth of health workers to treat and care for these HIV-infected individuals has reached crisis proportions.
The few health professionals practicing in many of the countries highly impacted by HIV/AIDS—workers often stressed, ill prepared, and scant in number—must now cope with a staggering new burden of disease while at the same time acquiring the knowledge, skills, and technology to deliver lifelong antiretroviral drug regimens, HIV/AIDS clinical and palliative care, and prevention services. Arguably, their task represents the most profound challenge in the scaling up of health care the world has ever known. They cannot accomplish this task alone.
This report explores potential strategies for mobilizing U.S. health personnel and technical experts to assist in the battle against HIV/AIDS in 15 African, Caribbean, and Southeast Asian countries highly affected by the disease. Commissioned by the U.S. Department of State as part of a historic global health initiative—the $15 billion 5-year President’s Emergency Plan for AIDS Relief (PEPFAR), the report presents the results of a study con-
ducted by the Institute of Medicine’s Committee on the Options for Overseas Placement of U.S. Health Professionals.
STUDY CONTEXT
In his State of the Union address of January 28, 2003, President George W. Bush announced PEPFAR with three extraordinary goals: (1) providing antiretroviral therapy (ART) for 2 million people; (2) preventing 7 million new HIV infections; and (3) providing care to 10 million people infected with or affected by HIV/AIDS, including orphans and vulnerable children. On May 27, 2003, the U.S. Congress passed the United States Leadership against HIV/AIDS, Tuberculosis, and Malaria Act of 2003 (Public Law 108-25) to realize the President’s vision. The act supports a phased expansion of critical programs, improved agency coordination, increased resources for multilateral and bilateral efforts, expansion of private-sector efforts, and intensified efforts to develop relevant HIV/AIDS therapies. Recognizing the contributions that U.S. health professionals can make in fighting HIV/AIDS, malaria, and tuberculosis in heavily affected, often resource-poor areas, the act also calls for a pilot program to demonstrate the feasibility of deploying U.S. personnel to such areas for periods of up to 3 years to provide basic health care services, deliver on-the-job training, and augment the health education of local populations. The legislation calls for a broad recruitment effort nationwide, including incentives such as loan repayment to encourage participation.
Without such reinforcement of human resources for health, PEPFAR’s ambitious targets will be difficult if not impossible to achieve. Few African countries, for example, have more than one doctor per 5,000 persons; the number of physicians currently practicing is already insufficient to meet other needs without the additional burden of providing ART for the millions of medically eligible Africans now and over the next decade. The need for nurses and other health workers for ART scale-up is even more acute. In Uganda in 2005, for example, the projected ratio of diagnostic laboratory staff supporting ART scale-up to the annual output from in-country training institutions is roughly 10 to 1 (Adano et al., 2004). Pharmacists are similarly scarce. And assuming that all Ugandan nursing graduates worked on ART scale-up, there would still be a projected national shortfall of almost 2,000 nurses—roughly the same shortfall projected in South Africa, where major deficits of medical officers, pharmacists, dietitians, social workers, and counselors are also anticipated (South Africa Ministry of Health, 2003). In fact, comparable human resource needs—which do not even begin to address the larger agenda of HIV/AIDS counselling and testing, prevention of maternal-to-child transmission, and social and palliative care
services—exist in virtually all of the 15 countries that are the focus of PEPFAR1 (Adano et al., 2004).
Another factor exacerbating the human resource crisis in addressing global HIV/AIDS is the so-called “brain drain.” Currently, many nurses and other health care workers trained in poor countries receive offers of employment in wealthier countries that are experiencing their own health care staffing shortages. A few examples begin to illustrate the dimensions of the problem. According to a report of the U.S. Agency for International Development (USAID) published in 2003, only 360 of the 1,200 doctors trained in Zimbabwe in the 1990s still practice domestically; in Zambia, only 50 of the 600 doctors trained locally since independence have remained in their country. Overall, many countries in sub-Saharan Africa have as many or fewer health workers today relative to 30 or even 40 years ago (JLI, 2004). The continued exodus of health personnel could seriously jeopardize ART scale-up.
Indigenous health professionals must be trained, supported, and retained if they are to be used to leverage and sustain the U.S. fiscal and human resource investment in services related to HIV/AIDS, including ART scale-up, as well as to other global health issues. The training of these professionals should encompass a wide range of clinical, social service, and administrative skills and values. Launching new, comprehensive health care delivery services that are effective and efficient will also require a mix of senior, midlevel, and junior professionals and suitably managed technical support. For example, laboratory assets must be well utilized and maintained and appropriately resourced with expendable supplies. Reliable drug delivery systems, along with education to maximize adherence, will be critical to prolong the durability of current treatment regimens. The treatment regimens themselves must be introduced at the optimal time in the natural history of the infection and appropriately monitored to reduce toxicity and the emergence of resistance. Experience has already shown that improper use of ART selects drug-resistant viruses. These strains, in turn, complicate the treatment of individuals while accelerating the spread of drug-resistant virus in the population as a whole, thus greatly increasing both the cost and complexity of HIV/AIDS care.
All of these lessons have already been learned over a 20-year history of comprehensive HIV/AIDS care in industrialized countries. A network of U.S. providers drawing on this experience should therefore have a positive
impact in fostering the most effective use of the U.S. dollars invested in PEPFAR and efforts in other developing countries.
Study Goals and Approach
This study was undertaken to provide a rapid, independent review of mechanisms for mobilizing the quantity and quality of relevant U.S. health personnel and technical experts needed in the 15 PEPFAR focus countries. In response to its charge, the committee explored both short- and long-term options for mobilizing, preparing, sending, managing, and compensating U.S. health professionals for service in these countries. Over its 7-month tenure, the committee:
-
Reviewed available data sources to project the optimum size and composition of a U.S. global health professions service program to augment, train, and collaborate with the public health and clinical professionals already present in the host countries
-
Assessed the relative strengths and weaknesses of existing and potential organizational models for such a program that could rapidly be activated or adapted to recruit, train, and place program participants
-
Articulated principles that can be applied in evaluating the advantages and disadvantages of those models
-
Examined other contextual issues bearing on the successful implementation of a U.S. global health professions service program
Committee members and consultants were selected for their international experience in low- and middle-income countries, as well as their individual expertise in the following areas relevant to the committee’s charge: clinical medical practice; nursing; nongovernmental organizations and partnering; social science, health education, and training programs; pharmacy, logistics, and informatics; laboratory services in resource-constrained areas; administration and policy with regard to international health resources; epidemiology and operations research; academic health care; and faith-based organizations. A brief profile of each member and consultant can be found in Appendix H.
The committee convened twice between September 2004 and February 2005. The committee also cast a broad net to review relevant experience in mobilizing, preparing, sending, managing, and compensating U.S. health professionals willing to work overseas in developing countries. Testimony and data were presented at the committee’s meetings and further discussed in frequent telephone conferences among subgroups, each consisting of three to six committee members and consultants. In addition, the committee reviewed and considered information from the published literature;
websites for governmental and nongovernmental organizations; and a variety of other sources, including four commissioned papers (see Appendixes B–E). The results of these efforts informed the committee in its preparation of this report.
BACKGROUND
Poverty and Health
Throughout history, poverty has plagued humankind. Today it remains the normal condition of life for at least a third of the world’s population. Around 2.8 billion people worldwide live on less than $2 a day, while well over a billion subsist on less than $1 a day. As a consequence, almost everything that residents of wealthy countries take for granted—good nutrition, access to education, low rates of communicable disease, long life expectancies—is the exception rather than the rule for these global neighbors, whose daily reality often is characterized by unsafe drinking water, lack of sanitation, illiteracy, periodic food shortages, epidemic diseases, and premature death. One well-known economist alluded to the broad, ravaging effects of poverty when—advocating for greatly expanded health aid to the Third World—he observed that “millions of people…are dying from their poverty right now” (Africa Recovery, 2002:22).
The first preconditions for health that distinguish rich and poor nations are clean water and sanitation. In low-income countries today, more than 1.1 billion people lack safe drinking water, and another 2.4 billion lack access to sanitation (WHO and UNICEF, 2000). The resulting death toll, according to recent estimates of the World Health Organization (WHO), is 1.6 million people each year (WHO, 2004a).
A rich–poor gap can also be seen in childhood immunization. Almost 34 million infants each year still do not have access to basic immunization services, with the lowest coverage being found in sub-Saharan Africa. In 2001, of an estimated 745,000 deaths from measles (a disease that can be prevented with a single vaccine costing U.S. $0.26), more than half occurred in sub-Saharan Africa (WHO, 2002a).
In 2005, the three global scourges most interrelated with poverty are HIV/AIDS, malaria, and tuberculosis. Together they accounted for 5–7 million deaths (WHO, 2002b), and these diseases remain a major reason why the poor stay poor (Commission on Macroeconomics and Health, 2001). In other words, not only do HIV/AIDS, malaria, and tuberculosis target the poor, but in each case they also stunt economic growth and development in the communities and regions where they flourish.
How does one begin to battle the triple scourge of HIV/AIDS, malaria, and tuberculosis? Providing effective drugs to affected populations—albeit
essential to any comprehensive strategy—is simply not enough. Each disease has unique and complex features that mandate knowledge and customized approaches to prevention, control, and clinical management. Thus without competent professionals to administer them and infrastructure to support their delivery, drugs alone do not equal life-saving health care.
By offering support and expertise to counterparts overseas and assisting in the training of new generations of desperately needed health workers, American health professionals can bring help and hope to those parts of the world where HIV/AIDS, malaria, and tuberculosis are laying the greatest waste to human life and spirit. In so doing, these “healers abroad” can also fight poverty and help sustain the long-term global health effort by multiplying essential skills and services. As citizens of a small world, we must acknowledge that in the end, such efforts benefit us all.
The Health Care Workforce and Global Health
Human Resources and Health2
Throughout history, human beings have driven health care (Anand and Barnighausen, 2004; World Bank, 1993). Health workers are active—not passive—agents of change. Often commanding two-thirds of today’s health budgets, they link together the many parts of the health system to spearhead the provision of health care (Berman et al., 1999).
Why are health workers so important? A quick look at success stories in disease control—from yellow fever, hookworm, and smallpox eradication; to the child health revolution in the 1980s; to the imminent eradication of polio—reveals that all were built on human resource strategies. The formal, science-based education of physicians in the United States, first codified in the Flexner Report (Flexner, 1910), contributed to the doubling of life expectancy in the United States over the last century.
In a recent analysis of the global health care workforce, the Joint Learning Initiative—a consortium of more than 100 health leaders—argues that mobilizing and strengthening human resources will be central to combating health crises in some of the world’s poorest countries and to building sustainable health systems in all countries (JLI, 2004). Yet nearly all nations today are challenged by worker shortages, skill mix imbalances, misdistribution of resources, negative work environments, and weak knowledge bases. This is particularly true in the poorest countries. In several of the most heavily impacted African countries, for example, the
prevalence of HIV among adults approaching 40 percent. The health sector is doubly affected by the HIV/AIDS epidemic: it must respond to the crippling burden of ill health among the general population while simultaneously dealing with the impact of the epidemic on health professionals. This situation represents the most profound change in the burden of disease ever experienced by any health system—much less those systems already weak and underfinanced before the advent of HIV/AIDS.
Added to this burden are new demands for diagnosis and treatment, including the challenges associated with provision of ART. Proper prescription of and monitoring of compliance with antiretroviral drug regimens are essential if patients are to benefit and if the grave possibility of emerging drug resistance is to be reduced. People living with HIV infection also require access to a wide range of care—from primary, secondary, and tertiary health care; to social services; to community-based support and home care.
Supervision and management skills and capacity are also critical to the effective delivery of all health care, including that focused on HIV/AIDS. In Tanzania and Chad, Kurowski and colleagues (2003) found evidence that improved staff management could result in substantial increases in staff productivity in the provision of HIV/AIDS care (Kurowski et al., 2003). Increased access to ART, voluntary counseling and testing, and prevention of mother-to-child transmission will require management as well as technical skills in relation to systems, administration, procurement, logistics, delivery, and referral; effective links between the formal and informal sectors will also be necessary. This challenge of good management is especially timely and pertinent within the broader contexts of decentralization and health-sector reform.
Despite general recognition of the crucial role of human resources in the provision of health care, the development of the health care workforce in low-income countries has suffered from years of national and international neglect (as discussed further below). Indeed, the dearth of qualified health care professionals in most low-income countries is the single most important constraint faced in responding to health care needs (Narasimhan et al., 2004). The Commission on Macroeconomics and Health, for example, has advocated a greatly increased investment in health, rising in low-income countries to a per capita expenditure of $34 per year. According to the commission, however, the main problem in implementing this recommendation is not the difficulty in raising the additional funds but the capacity of the health sector itself to absorb them (Habte et al., 2004). Likewise, senior officials in Ethiopia, Nigeria, and Uganda have all cited the lack of health care personnel as a main constraint in responding to health challenges (WHO AFRO, 2002). And Botswana, a comparatively rich African country that has committed to providing free ART to all eligible citi-
zens, is hindered in doing so principally by a lack of health personnel (WHO, 2004b).
As new resources are being mobilized to fight HIV/AIDS, tuberculosis, malaria, and other global diseases, the health workforce crisis—especially in Africa—is daily becoming more apparent and dire. External grants and funding to address global HIV/AIDS, estimated at $5 billion in 2003, could reach $20 billion by 2007 (UNAIDS, 2004). At present, however, there is simply insufficient human capacity in many developing countries to absorb, apply, and make efficient use of these new funds and critical health initiatives.
The Current Global Health Care Workforce
After a century of the most spectacular health advances in human history, we confront unprecedented and interlocking health crises. Some of the world’s poorest countries face rising death rate and plummeting life expectancy, even as global pandemics threaten us all. Human survival gains are being lost because of feeble national health systems. On the front line of human survival, we see overburdened and overstressed health workers, too few in number, without the support they so badly need—losing the fight. Many are collapsing under strain; many are dying, especially from AIDS; and many are seeking a better life and more reward work by departing for richer countries (Chen et al., 2004).
According to statistics compiled by WHO, the world had 9 million doctors and 15 million nurses in 2000 (WHO, 2004c), representing an average density of 1.6 doctors and 2.5 nurses per 1,000 population. When compared with the results of the last published global survey in 1971 (which estimated a pool of 2.3 million doctors worldwide), the 2000 data suggest that the global supply of doctors is growing, on average, about 5 percent per year (Mejia and Pizurki, 1976). The total global health workforce is currently estimated at more than 100 million—a figure that includes 24 million recorded doctors, nurses, and midwives, plus another pool of uncounted informal, traditional, community, and allied workers (Chen et al., 2004).
These numbers do not tell the whole story, however. There is an extreme imbalance in the distribution of credentialed professionals among regions and countries. The supply of nurses and doctors relative to the population of sub-Saharan Africa, for instance, is one-tenth of that in Europe. To take an even more extreme case, Ethiopia has one-fiftieth of Italy’s supply of health professionals (Chen et al., 2004).
Many factors contribute to this global imbalance in individual settings, but Chen and colleagues (2004) point to three major macro faced by assail-
ing health workers: (1) the triple impact of HIV/AIDS, which, as noted above, increases the workloads of health care workers and exposes them to infection, while also stressing their morale (see Box 1-1) (Tawfik and Kinoti, 2003); (2) increased worker labor migration, depleting nurses and doctors from countries that can least afford the loss (as discussed in detail below) (Alkire and Chen, 2004); and (3) chronic underinvestment in human resources stemming from two decades of economic and sectoral reform that capped expenditures, froze recruitment and salaries, and restricted public budgets, thereby depleting working environments of basic supplies, drugs, and facilities (Narasimhan et al., 2004).
Educational systems of developing countries are another major impediment to the ongoing production of health workers. Europe produces 173,800 doctors a year, and Africa only 5,100 (JLI, 2004) (see Figure 1-1). One doctor is produced for every 5,000 people in Central and Eastern Europe and the Baltic States, compared with one doctor for every 115,000 people in sub-Saharan Africa. Moreover, in many health professions schools in developing countries, curricula are misaligned with prevailing patterns of disease, and teaching methods do not emphasize the practical problem-solving skills needed to address local health issues (Ndumbe, 2004). Instead of working competencies, production of health professionals is based on certification or Western medical standards. The result is a greater proportion of graduates focused on professional status and income generation, which further increases potential out-migration to wealthier countries.
The production of public health specialists is also insufficient in areas where these workers are most needed, leading to another critical disparity between rich and poor countries. A recent survey, for example, found that more than half of countries in Africa had no graduate training program in public health (Ijsselmuiden, 2003).
In many countries, including those with high HIV prevalence, the inability to recruit and retain an effective, well-motivated, appropriately skilled workforce stems from a range of additional problems that include low pay, poor work conditions, and weak management. Some workers experience a triple bind: their workplaces are understaffed and their compensation packages woefully inadequate, but civil service or public expenditure reforms prevent recruitment of new staff or substitutes for missing colleagues (sometimes called “ghost workers”). In recent years, these factors have fueled the trends for some health professionals to move from the public to the private sector or to leave their professions altogether, as well as the above-noted trend to migrate internationally in pursuit of more favorable opportunities.
The most common grievance of health workers is poor pay. Wages are often insufficient to cover personal and family needs. In addition, salaries may not be adjusted for rising inflation and may not be paid on time. In
|
BOX 1-1 Increased Workload Longitudinal hospital-based surveys in HIV-endemic areas confirm the rising inpatient burden of HIV/AIDS since the early days of the epidemic. Arthur and colleagues (2000, 2001) describe a steady rise in HIV-infected patients admitted to Kenyatta National Hospital, Nairobi, from 4.3 per day in 1988 to 13.9 in 1997. The rise in bed occupancy over the same period was 190 percent, plateauing at 40 percent HIV-positive census. A recent report of the U.K. Department for International Development (DFID, 2003) estimates the current bed occupancy at Kenyatta National Hospital even higher, at 300 percent, 70 percent HIV-related. The report also states that 50 percent of bed occupancy in Eldoret, Kenya, is HIV-related, and 75 percent of Eldoret’s tuberculosis (TB) patients are coinfected with HIV. In KwaZulu Natal, South Africa, hospital admissions rose by 81 percent over 10 years, while adult TB admissions (an indirect reflection of the HIV/AIDS burden) rose by 360 percent, accounting for 47 percent of male and 30 percent of female medical ward admissions and 11 percent of total hospital admissions (Floyd et al., 1999). According to the 2001 Swaziland Human Development Report, people with HIV occupied 50 percent of the beds in some health care centers (DFID, 2003). In Zimbabwe, HIV prevalence among hospitalized patients also rose to 50 percent, making HIV the leading cause of hospitalization. A study in Tanzania found that patients with HIV had three times the average length of stay of non-HIV patients (18 versus 6 days); two Tanzanian district hospitals had to construct new wards to cope with the increasing demand for HIV-related care (Malecela-Lazaro et al., 2001). Against this backdrop of growing HIV/AIDS-related inpatient burdens, Tawfik and Kinoti (2003) note that only scanty, mainly anecdotal information exists regarding the impact of the epidemic on individual health professionals (Tawfik and Kinoti, 2003). It is clear, however, that HIV/AIDS brings increasing and changing workloads, often demanding higher skills (especially with the introduction of ART). Recent modeling of human resources for health in Tanzania and Chad suggests that many tasks and activities are carried out by staff not formally qualified to perform them, and that surpluses of staff with lower skills must compensate for deficits of staff with higher skills (Kurowski et al., 2003). China, a country where more than 1 million people in rural areas have contracted HIV through unsafe blood collection procedures, is experiencing difficulties in providing ART because of the shortage of doctors with the necessary training and skills (Sui, 2003). Along with increased workload, health workers in areas highly impacted by HIV/AIDS must cope with new roles for which they are neither trained nor equipped—in particular, the psychosocial support of patients and families facing the emotional trauma of the disease. Finally, HIV has a negative effect on staff productivity through absenteeism related to caring for ill relatives and attending funerals. |
|
Exposure to HIV Infection While individual health workers are generally subject to the same risks of acquiring HIV/AIDS as the general population, they may also risk infection in the course of caring for HIV-infected and other patients. This occupational risk of infection varies between developed and resource-poor countries and across health worker categories. A study in a South African hospital investigating the potential for HIV transmission from needle sticks and other sharp-instrument injuries found that 41 percent of such injuries occurred among nurses and 38 percent among cleaners, although the latter comprised only 16 percent of total hospital personnel (de Villiers, 2000). Nurses are probably at high risk overall. In just a few years, the HIV prevalence rate among nurses in Lusaka, Zambia, rose from 34 to 44 percent (Ndongko and Oladepo, 2003). Health workers are also at risk of acquiring other infections in their workplaces, such as tuberculosis transmitted through respiratory secretions and additional blood-borne pathogens, such as hepatitis B and C, acquired through exposure to the blood and body fluids of carriers. In one study, the incidence of tuberculosis was found to have increased several-fold among health workers in areas with high HIV prevalence (Whiteside, 2002). Husain and Badcock-Walters (2002) have estimated that a country with a stable 15 percent prevalence rate can expect between 1.6 percent and 3.3 percent of its health care providers to die from HIV/AIDS each year. As of 1999, it was estimated that in Botswana, 17 to 32 percent of health workers were HIV-infected, and between 28 and 41 percent would be infected by 2005. Malawi and Zambia have experienced five- to sixfold increase in illness and death rates among health workers. A recent report of the Joint United Nations Programme on HIV/AIDS (UNAIDS) suggests that training of doctors and nurses in southern Africa needs to increase by 25 to 40 percent by 2010 simply to compensate for these expected losses (UNAIDS, 2002). Psychosocial Effects HIV/AIDS has profound psychosocial impacts on health workers. In some cases, the epidemic raises workers’ awareness of previously excluded social groups, while other health professionals either withdraw from or reject patients who are sex workers or intravenous drug users. Emotional reactions may also include exaggerated fears of exposure to HIV, homophobia, and other negative attitudes towards specific social groups, as well as cultural, social, or moral resistance to promoting certain HIV/AIDS preventive practices, such as the use of condoms. Tawfik and Kinoti (2003) and Malecela-Lazaro and colleagues (2001) underscore that feelings of professional inadequacy and hopelessness may partly explain poor work performance in some areas of high HIV/AIDS burden. For example, workers may believe that providing health care to dying HIV/AIDS victims is a waste of time and resources that could be used to treat and cure other patients. |
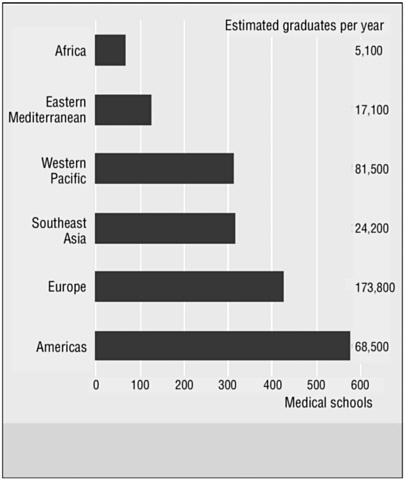
FIGURE 1-1 Regional disparities in medical schools and graduates.
NOTE: Region refers to WHO regions.
SOURCE: Adapted from JLI (2004) and Eckhert (2002).
many countries, civil service wages have actually fallen in recent years. In Tanzania, a civil servant’s wage in 1998 was only 70 percent of that in 1969 (JLI, 2004). Wages of registered nursed in Malawi when adjusted for the cost of living amount to about $489 a month (Vujicic et al., 2004). In Ghana and Zambia, the average monthly salary for a doctor is just over $400 (HLF, 2004).
Low wages in the public sector can also drive workers into “dual practices,” whereby public servants provide private services (Ferrinho et al., 2004; Vujicic et al., 2004). Such practices are breeding grounds for professional and financial conflicts of interest as workers juggle their public obligations while attempting to maximize income from more lucrative assign-
ments and services (often based in urban centers). In the worst case, inadequate compensation of health workers can lead to overtly predatory behavior—for example, marketing and selling of drugs, or demands for illegal payments for services.
Poor work environments also negatively impact retention and performance by workers in the health sector. Heavy workloads, burnout, excessive administrative duties, isolation from colleagues, lack of teamwork, and occupational hazards are additional reasons for low worker morale. Finally, a lack of recognition, a lack of career opportunities, and atmospheres that generally discourage creativity all serve to demotivate health workers who are already underpaid.
On the other hand, nonfinancial incentives—career advancement and continuing education, flexible work hours, good employment conditions, adequate vacation time, and access to child care—can increase worker motivation. Upgrading competencies, facilitating access to specialized training in the future, and accelerating promotion and career development can also be helpful in at least temporarily redressing geographic imbalances in the health care workforce. Indonesia and Thailand, for example, set aside specialist training slots for workers who have completed rural service in order to improve rural access to workers (Chomitz et al., 1998; Wibulpolprasert, 1999; Wibulpolprasert and Pengpaibon, 2003). South Africa and Malawi have used bonding or compulsory service regulations to shift their geographic distribution of health workers, although these methods have proven difficult to monitor and enforce (Chomitz et al., 1998; Hammer and Jack, 2002).
Goals for Achieving Global Health
At the Millennium Summit of the United Nations General Assembly in September 2000, delegates adopted an ambitious set of goals aimed at reducing global poverty, ignorance, and ill health over the next 15 years. Some goals had been proposed at earlier summits devoted to specific social problems, such as health and education, but never before had the United Nations backed such a comprehensive antipoverty agenda. The following seven goals were adopted:
-
Halving the proportion of people who live in extreme poverty and the proportion of people in hunger over the period 1990–2015
-
Achieving universal primary education for both boys and girls by 2015
-
Promoting gender equality and the empowerment of women
-
Reducing child (under age 5) mortality by two-thirds between 1990 and 2015
-
Reducing maternal mortality by three-quarters between 1990 and 2015
-
Halting and beginning to reverse the spread of HIV/AIDS, malaria, and other major diseases by 2015
-
Integrating principles of environmental sustainability into national development goals
The density of health workers in a given country will make an enormous difference to the likelihood that its population will meet specific indicators for the health-related goals listed above. For example, the prospects for achieving 80 percent coverage of measles immunization and skilled attendants at birth are much higher in countries where worker density exceeds 2.5 per 1,000 population. Seventy-five countries with 2.5 billion people currently fall below this minimum threshold (JLI, 2004).
Anand and Barnighausen (2004) conducted a quantitative cross-national analysis of human resource density and health status in 118 countries for which data were available. Not surprisingly, lower maternal, infant, and under-5 mortality rates were associated with higher income, higher female adult literacy, and lower poverty. After controlling for these expected findings, however, the analysis also showed that human resource density (physicians, nurses, and midwives per 1,000 population) mattered significantly in determining health outcome measures. Specifically, the authors found that as the density of health workers increased, maternal, infant, and under-5 mortality fell (see Figure 1-2). Maternal mortality was most sensitive to health worker density: a 10 percent increase in the density of the health workforce was correlated with a 4 percent decline in maternal mortality. A 10 percent increase in health worker density was correlated with a 2 percent decline in under-5 mortality.3
Achieving the above goals for health will therefore require concerted efforts to increase the total health workforce in developing countries. The Joint Learning Initiative estimates that sub-Saharan African countries must nearly triple their current health workforce by adding the equivalent of 1 million workers through retention, recruitment, and training if they are to come close to meeting these goals (Chen et al., 2004).
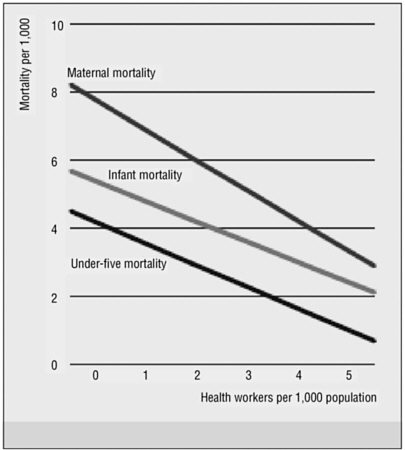
FIGURE 1-2 More health workers, fewer deaths.
SOURCE: Adapted from JLI (2004) and Anand and Barnighausen (2004). Reprinted, with permission, from Elsevier (The Lancet 2004:1606).
The Health Workforce Crisis in Africa4
The problem of insufficient human resources for health care is most acute in sub-Saharan Africa, which bears 25 percent of the world’s burden of disease but houses only 1.3 percent of the world’s health workforce. Currently, an estimated 750,000 health workers serve the 682 million people of sub-Saharan Africa. The ratio of health care workers to population is 10 to 15 times higher in countries of the Organization for Economic Cooperation and Development (OECD) (HLF, 2004).
The High-Level Forum on the Health Millennium Development Goals (2004) identifies four major factors contributing to the low density of health workers in Africa compared with other regions of the world:
-
Insufficient training opportunities—Two-thirds of sub-Saharan African countries have only one medical school, and 11 sub-Saharan African countries have no medical school (Hagopian et al., 2004).
-
Deteriorating health of the workforce—The International Labor Organization has suggested that 18 to 41 percent of the workforce in many countries of sub-Saharan Africa is infected with HIV-1 (Cohen, 2002).
-
Rural/urban imbalance—In Tanzania, the city of Dar-es-Salaam alone has nearly 30 times as many medical officers and medical specialists as other rural districts (Wyss, 2004). Only about 5 of Uganda’s roughly 100 surgeons work outside of urban areas (Wasike, 2003). A 2003 USAID report notes that only one-fourth of rural doctors in South Africa are South African nationals, with most of the remainder coming from other African countries, such as Zambia, Zimbabwe, and Congo (Kober and Van Damme, 2004).
-
The transnational flow of health professionals, or the “brain drain”—The international migration of health workers is discussed in greater detail in the following section. However, the High Level Forum anticipates that still-rising investments in health by OECD countries (projected to increase 10-fold over the next 50 years) (Chen, 2004) will continue to fuel the exodus of African health workers to wealthy countries if countermeasures are not taken.
A quick comparison of selected categories of health care providers in the 15 countries currently targeted by PEPFAR reveals a wide range of available providers in 2004 (see Table 1-1). By comparison, the current U.S. ranges as of October 2004 are shown in Table 1-2. The estimated gap in the total number of nurses, doctors, and midwives for the 15 PEPFAR focus countries, based on a minimum density of 2.5 doctors, nurses, and midwives per 1,000 population, is presented in Table 1-3.
International Migration of Health Care Workers
Of the 175 million people (2.9 percent of the world’s population) living outside the country of birth in 2000, 65 million were economically active. The rise in the number of people migrating is significant for many developing countries because they are losing their better-educated nationals to richer countries. Medical practitioners and nurses represent a small proportion of the highly skilled workers who migrate, but the loss for devel-
TABLE 1-1 Health Care Providers (per 100,000 Population) in Selected PEPFAR Countries
|
Providers |
Low |
High |
|
Physicians |
1.9 (Rwanda) |
69.0 (South Africa) |
|
Nurses and Midwives |
8.8 (Uganda) |
388.0 (South Africa) |
|
Dentists |
0.05 (Rwanda) |
10.5 (South Africa) |
|
Pharmacists |
0.1 (Rwanda) |
24.2 (South Africa) |
|
SOURCE: WHO (2004c). |
||
TABLE 1-2 Health Care Providers (per 100,000 Population) in the United States
|
Providers |
Number |
|
Physicians |
293 |
|
Nurses and Midwives |
773 |
|
Dentists |
59 |
|
Pharmacists |
69 |
|
SOURCE: WHO (2004c). |
|
oping countries of human resources in the health sector may mean that the capacity of the health system to deliver health care equitably is significantly compromised. It is unlikely that migration will stop given the advances in global communications and the development of global labor markets in some fields, which now include nursing (Stilwell et al., 2004).
The migration of health personnel across international borders is having major negative impacts on health systems in developing countries. Migration is currently possible for all health professionals who have marketable skills. Despite temporary declines in demand from recipient countries, overall demand for health professionals has increased since the 1970s, facilitated by globalized markets and free-trade agreements that have reduced barriers to trade and to the mobility of services, products, and people (Martineau et al., 2004). Although the migration of doctors receives the most attention, it is the movement of nurses and other health professionals that can cripple a health system. Nurses are in particularly high demand for aging populations in wealthy countries, and are proactively recruited by professional firms through enticements of 10-fold or greater salary differentials (Narasimhan et al., 2004). This migration, a consequence of globaliza-
TABLE 1-3 Deficit or Surplus of Doctors, Nurses, and Midwives
|
PEPFAR Countries |
Population (in thousands) |
Doctors, Nurses, and Midwives per 1,000 Population |
Surplus/Deficita |
|
Guyana |
759 |
2.77 |
+200 |
|
Haiti |
7,797 |
0.36 |
−16,700 |
|
Vietnam |
79,197 |
1.28 |
−96,600 |
|
Ethiopia |
68,961 |
0.23 |
−156,500 |
|
Botswana |
1,697 |
2.70 |
+300 |
|
Cote d’Ivoire |
14,685 |
0.55 |
−28,600 |
|
Kenya |
27,390 |
1.03 |
−40,300 |
|
Mozambique |
17,861 |
0.31 |
−39,100 |
|
Namibia |
1,750 |
3.14 |
+1100 |
|
Nigeria |
114,746 |
1.45 |
−120,500 |
|
Rwanda |
8,273 |
0.23 |
−18,800 |
|
South Africa |
44,416 |
4.57 |
+91,900 |
|
Tanzania |
36,276 |
0.39 |
−76,500 |
|
Uganda |
25,004 |
0.14 |
−59,000 |
|
Zambia |
9,371 |
1.20 |
−12,200 |
|
TOTAL |
|
|
−571,300 |
|
aActual number rounded to nearest hundred. NOTE: Human Resources in Health (HRH) density of 2.5 doctors, nurses, and midwives per 1,000 population. SOURCE: JLI (2004). |
|||
tion, is one of the priority issues being addressed by mode 4 of the General Agreement on Trade in Services.
The following examples illustrate the problem:
-
There are reportedly more Malawian doctors in Manchester, England, than in Malawi (JLI, 2004).
-
Only 50 of 600 Zambian doctors trained since independence continue to practice in that country (WHO, 2004d).
-
Doctors in the Philippines are retraining themselves as nurses to pursue lucrative overseas opportunities (Chan, 2003).
-
In 2001, 382 nurses migrated from Zimbabwe to the United Kingdom, increasing the latter country’s nursing stock by only 0.1 percent but depleting Zimbabwe’s available pool by 4 percent (Buchan and Dovlo, 2004).
-
In South Africa, the national HIV/AIDS treatment plan aims to create 12,000 new posts, yet 29,000 positions in the public health sector are currently unfilled. More than 82,000 health workers left South Africa between 1989 and 1997 (Cohen, 2002).
Migration can also affect key services or regions. Wholesale recruitment of the nursing staff of an intensive care unit (ICU) at a hospital in the Philippines essentially cut off access to ICU care for the local population (BBC News, 2003). And the migration of service workers from Malawi to the United Kingdom is leading to the near collapse of maternity service in Malawi’s central hospital (Dugger, 2004).
Currently, foreign doctors can make up as much as a third of the total number of doctors in developed countries (see Figure 1-3). Migration patterns are generated by “push” and “pull” factors facilitated by labor markets, language compatibility, sociocultural affinities, professional equivalency, and visa policies. Six principal factors driving these movements are job satisfaction, career opportunity, governance and management, safety and risks, and social and family reasons (Dovlo and Martineau, 2004).
One way to address this problem is to promote “reverse flows” (JLI, 2004). Box 1-2 describes one such attempt. Innovative strategies include volunteer cadres, expansion of nongovernmental activities, and north–south institutional twinning or partnerships. Exporting countries—for example, Cuba, Egypt, India, and the Philippines—could also accelerate their flows to countries with severe health workforce shortages. Cuba already provides significant human resources to many African and Caribbean nations, while at present, the other three countries target primarily richer, OECD countries (JLI, 2004).
From the broadest perspective, what is needed today is global responsibility and collaboration to slow the pace of doctors and nurses following multiple entry and exit paths from low- to high-income countries. As the Joint Learning Initiative report states, “no country is an island in workforce development.” The report further indicates that migratory flows produce benefits as well as harm, and blocking the movement of people violates human rights and is generally unenforceable. “[Therefore], the global management of medical migration should seek to protect both health and human rights—dampening ‘push’ forces by retaining talent in sending countries and reducing ‘pull’ forces by aiming for educational and workforce self-sufficiency in destination countries” (JLI, 2004:6).
ORGANIZATION OF THE REPORT
In this report, the committee proposes a set of interconnected workforce enhancement programs that would meet the need to augment the health professionals currently waging the fight against HIV/AIDS and other global diseases. The committee believes that, given adequate resources, talent, and political will, these programs would make an enormous contribution to the eventual control of these terrible afflictions.
The report is organized into two parts (see Box 1-3). The first part
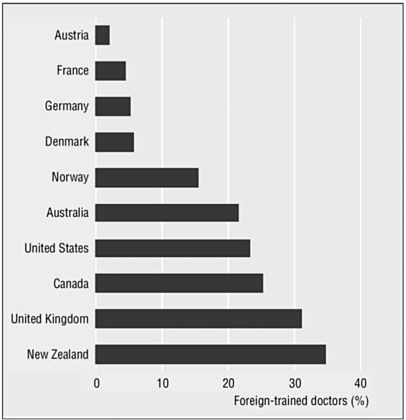
FIGURE 1-3 Percentage of foreign-trained doctors in selected developed countries.
NOTE: Data are for 1998 for Australia and Canada; 2000 for France, Germany, and New Zealand; 2001 for Austria, the United Kingdom, and the United States; 2002 for Norway. Figures shown for Austria represent physicians that have obtained recognition of their qualifications in Austria; for France, as a percentage of the medical workforce in France; Germany as a percentage of the active medical workforce in Germany; for Australia as a percentage of the employed medical workforce in Australia; for New Zealand, as a percentage of the active medical practitioners in New Zealand.
SOURCE: Adapted from JLI (2004) and OECD (2002).
Data adapted from www.oecd.org/dac/stats/crs, © OECD, All rights reserved.
reviews and provides evidence for the current human resource crisis in global health, outlines the challenges of confronting HIV/AIDS (and other global diseases) on the ground, and describes a range of national and international initiatives currently focused on global HIV/AIDS. The second part begins by presenting the philosophy and guiding principles of the master government program—the Global Health Service—envisioned by the com-
|
BOX 1-2 The Transfer of Knowledge through Expatriate Nationals (TOKTEN) program was launched by the United Nations Development Program (UNDP) in 1977 as an attempt to reverse patterns of brain drain by encouraging expatriate nationals to volunteer their expertise in the service of their homelands for short periods of time. The program is currently instituted in more than 25 countries, including Vietnam. Through this program, highly skilled expatriate professionals provide technical expertise, policy advice, and research to governments, private- and public-sector enterprises, universities, and research centers in various fields. TOKTEN consultants are considered volunteers, although UNDP covers travel expenses to and from the participant’s country of residence and provides a generous stipend for living costs. Under the program, qualified expatriate professionals from developing nations return to their countries of origin for typically 1 to 6 months to share the skills they have gained during their residence in developed countries. TOKTEN consultants carry out tasks that might otherwise be performed by international consultants, their volunteering often being motivated by the desire to play a role in the development of their country of origin. Transfer of knowledge occurs at a much lower cost than is the case with foreign consultants (often with savings of 50–70 percent) and more rapidly as well, since TOKTEN consultants need no period of adjustment to become acquainted with the language or the social and cultural context. In virtually all cases, networks are created, and follow-up takes place. TOKTEN was first initiated in Vietnam in 1989, and in the decade since, two projects that include TOKTEN recruitment have been completed. The first TOKTEN project developed a roster of 194 potential expatriate consultants and established relationships between Vietnamese organizations and the organization of each fielded consultant. Between 1990 and 1992, 60 requests for consultants were received, and 20 TOKTEN consultants were placed. The first TOKTEN project was focused mainly in the area of science and technology. The receiving organizations included the Institute for Scientific and Technological Strategic Studies, Institute for Medical Equipment, Ben Tre Committee for Sciences, Institute for Computer Science, and Hanoi Polytechnic. TOKTEN volunteers in Vietnam receive a monthly living allowance with additional amounts given for up to two dependents. SOURCE: Adapted from http://www.papp.undp.org/governance/projects/ and http://www.undp.org.vn/mlist/develvn/042001/post76.htm. |
mittee as the primary vehicle for a new suite of programs designed to address the global HIV/AIDS workforce crisis and help achieve the PEPFAR goals. It then provides detailed descriptions of six proposed programs of the Global Health Service, along with short- and long-term mechanisms for mobilizing, preparing, sending, managing, and compensating U.S. health professionals serving in the PEPFAR focus countries. The last chapter of the
|
BOX 1-3
|
||||||||||||||||
report revisits the big picture of national health capacity development in resource-poor and other countries; value-added investments in achieving the PEPFAR goals; ethical issues in foreign workforce assistance; creative public–private partnerships and alliances under PEPFAR; and processes for monitoring, evaluation, and adjustment.
REFERENCES
Adano U, O’Neil M, Decima E, Kiarie W. 2004. Rapid Assessment of the Human Resource Implications of Scaling Up HIV/AIDS Services in Uganda. Management and Leadership Development Project/USAID. Boston, MA: Management Sciences for Health.
Africa Recovery, United Nations. 2002. To cure poverty, heal the poor. Africa Recovery 16(1):22.
Alkire S, Chen L. 2004. “Medical Exceptionalism” in International Migration: Should Doctors and Nurses Be Treated Differently? Joint Learning Initiative Working Paper 7-3. [Online]. Available: http://www.globalhealthtrust.org/doc/abstracts/WG7/Alkirepaper.pdf [accessed February 8, 2005].
Anand S, Barnighausen T. 2004. Human resources and health outcomes: Cross-country econometric study. Lancet 364(9445):1603–1609.
Arthur G, Bhatt SM, Muhindi D, Achiya GA, Kariuki SM, Gilks CF. 2000. The changing impact of HIV/AIDS on Kenyatta National Hospital, Nairobi from 1988/89 through 1992 to 1997. AIDS 14(11):1625–1631.
Arthur G, Nduba VN, Kariuki SM, Kimari J, Bhatt SM, Gilks CF. 2001. Trends in bloodstream infections among human immunodeficiency virus-infected adults admitted to a hospital in Nairobi, Kenya, during the last decade. Clinical Infectious Diseases 33(2):248–256.
BBC News. 2003, August 27. Nurses Exodus. [Online]. Available: http://news.bbc.co.uk/2/hi/programmes/newsnight/3184479.stm [accessed March 4, 2005].
Berman P, Arellanes L, Henderson P, Magnoli A. 1999. Health Care Financing in Eight Latin American and Caribbean Nations: The First Regional National Health Accounts Network. Partners for Health Reform-LAC-HSR Paper N. 16.
Buchan J, Dovlo D. 2004. International Recruitment of Health Workers to the UK: A Report to DFID. London, England: DFID Health Systems Resource Centre.
Chan D. 2003. Philippine Doctors Study Nursing to Land US Jobs. [Online]. Available: http://www.sikhspectrum.com/032003/p_doctors.htm [accessed March 23, 2005].
Chen L. 2004. Harnessing the Power of Human Resources for Achieving the MDGs. Presentation at the January 9, 2004, Meeting of the High Level Forum on the Health Millennium Development Goals. Geneva, Switzerland.
Chen L, Evans T, Anand S, Boufford JI, Brown H, Chowdhury M, Cueto M, Dare L, Dussault G, Elzinga G, Fee E, Habte D, Hanvoravongchai P, Jacobs M, Kurowski C, Michael S, Pablos-Mendez A, Sewankambo N, Solimano G, Stilwell B, de Waal A, Wibulpolprasert S. 2004. Human resources for health: Overcoming the crisis. Lancet 364(9449):1984–1990.
Chomitz KM, Setiardi G, Azwar A, Ismail N. 1998. What Do Doctors Want? Developing Incentives for Doctors to Serve in Indonesia’s Rural and Remote Areas, Working Paper. Washington, DC: World Bank.
Cohen D. 2002. Human Capital and the HIV Epidemic in sub-Saharan Africa, Working Paper 2. Geneva, Switzerland: International Labour Organization.
Commission on Macroeconomics and Health. 2001. Macroeconomics and Health: Investing in Health for Economic Development. Geneva, Switzerland: WHO.
de Villiers A. 2000 (July 7–12). Abstract TuPeD3637: Retrospective Analysis of Injury on Duty Cases with Specific Emphasis on HIV Transmission as Reported in a Secondary Hospital in Bleomfontein, South Africa. Presented at the XIII International AIDS Conference, Durban, South Africa.
DFID (U.K. Department for International Development) Health Systems Resource Centre. 2003. Scoping Study on the Impact of HIV/AIDS on Health Systems. London, England: DFID and John Snow International. [Online]. Available: http://www.jsiuk.com/docs/hiv_impact_study.pdf [accessed March 1, 2005].
Dovlo D, Martineau T. 2004. Review of Evidence for Push and Pull Factors and Impact on Health Worker Mobility in Africa. Joint Learning Initiative Working Paper. Ghana and Liverpool School of Tropical Medicine, United Kingdom.
Dugger C. 2004, July 12. An exodus of African nurses puts infants and the ill in peril. The New York Times. P. A1.
Eckhert N. 2002. The global pipeline: Too narrow, too wide, or just right? Medical Education 36(7):606–613.
Ferrinho P, Lerberghe WV, Fronteira I, Hipolito F, Biscaia A. 2004. Dual Practice in the Health Sector: A Review of Evidence. Joint Learning Initiative Working Paper. [Online]. Available: http://globalhealthtrust.org/doc/abstracts/WG3/Ferrinhoabstract.pdf [accessed March 1, 2005].
Flexner A.. 1910. Medical Education in the United States and Canada: A Report to the Carnegie Foundation for the Advancement of Teaching. New York, NY: Carnegie Foundation for the Advancement of Teaching.
Floyd K, Reid RA, Wilkinson D, Gilks CF. 1999. Admission trends in a rural South African hospital during the early years of the HIV epidemic. Journal of the American Medical Association 282(11):1087–1091.
Habte D, Dussault G, Dovlo D. 2004. Challenges confronting the health workforce in sub-Saharan Africa. World Hospitals & Health Services 40(2):23–26, 40–41.
Hagopian A, Thompson M, Fordycel M, Johnson K, Hart LG. 2004. The migration of physicians from sub-Saharan Africa to the United States of America: Measures of the African brain drain. Human Resources for Health 2(17).
Hammer J, Jack W. 2002. Designing incentives for rural health care providers in developing countries. Journal of Development Economics 69(1):297–303.
HLF (High Level Forum on the Health Millennium Development Goals). 2004. Addressing Africa’s Health Workforce Crisis: An Avenue for Action. Abuja, Nigeria: World Bank and WHO.
Husain I, Badcock-Walters P. 2002. HIV/AIDS, health and education. In: Forsythe S, ed. State of the Art: AIDS and Economics. Washington, DC: Policy Project and Merck and Co. Inc. Pp. 84–95.
Ijsselmuiden C. 2003 (September 29–October 3). Training of Health Care Workers. Graduate Education in Public Health: Afri-Health Survey: Provisional Results and Conclusions. Prepared for the Joint Learning Initiative, Accra Ghana.
JLI (Joint Learning Initiative). 2004. Human Resources for Health: Overcoming the Crisis. Cambridge, MA: Harvard University Press.
Kober K, Van Damme W. 2004. Scaling up access to antiretroviral treatment in southern Africa: Who will do the job? Lancet 364(9428):103–107.
Kurowski C, Wyss K, Abdulla S, Yemadji N, Mills A. 2003. Human Resources for Health: Requirements and Availability in the Context of Scaling-Up Priority Interventions in Low-Income Countries: Case Studies from Tanzania and Chad. London, England: London School of Hygiene and Tropical Medicine.
Malecela-Lazaro M, Mwisongo A, Makundi E, Mubyazi G, Kisinza W, Senkoro K, Magesa S, Malebo H, Mcharo J, Hiza P, Pallangyo, Ipuge Y, Kitua A. 2001. HIV/AIDS Impact on Health Services in Tanzania. Dar-es-Salaam, Tanzania: National Institute for Medical Research Health Systems and Policy Research Department.
Martineau T, Decker K, Bundred P. 2004. “Brain drain” of health professionals: From rhetoric to responsible action. Health Policy 70(1):1–10.
Mejia A, Pizurki H. 1976. World migration of health manpower. WHO Chronicle 30(11): 455–460.
Narasimhan V, Brown H, Pablos-Mendez A, Adams O, Dussault G, Elzinga G, Nordstrom A, Habte D, Jacobs M, Solimano G, Sewankambo N, Wibulpolprasert S, Evans T, Chen L. 2004. Responding to the global human resources crisis. Lancet 363(9419):1469–1472.
Ndongko W, Oladepo O. 2003. Impact of HIB/AIDS on Public Sector Capacity in sub-Saharan Africa: Towards a Framework for the Protection of Public Sector Capacity and Effective Response to the Most Affected Countries. Africa Capacity Building Foundation, Board of Governors. 13th Annual Meeting, June 29, 2004, The Hague.
Ndumbe P. 2004. The Training of Human Resources for Health in Africa. Joint Learning Initiative Working Paper 4-1. [Online]. Available: http://www.globalhealthtrust.org/doc/abstracts/WG4/NdumbeHRHFINAL.pdf [accessed March 1, 2005].
OECD (Organization for Economic Cooperation and Development). 2002. International Migration of Physicians and Nurses: Causes, Consequences, and Health Policy Implications. Draft. Paris, France: OECD.
South Africa Ministry of Health. 2003. Operational Plan for Comprehensive HIV and AIDS Care, Management and Treatment for South Africa. Pretoria, South Africa: South Africa Department of Health.
Stilwell B, Diallo K, Zurn P, Vujicic M, Adams O, Dal Poz M. 2004. Migration of health-care workers from developing countries: Strategic approaches to its management. Bulletin of the World Health Organization 8:596–600.
Sui C. 2003, July 15. China–AIDS: China Starts Offering Free AIDS Drugs but Lacks Doctors to Administer Them. Paris, France: Agence France-Presse. [Online]. Available: http://www.aegis.com/news/afp/2003/AF030781.html [accessed March 4, 2005].
Tawfik L, Kinoti S. 2003. The Impact of HIV/AIDS on the Health Workforce in sub-Saharan Africa: The Issue of Human Resources: Support for Analysis and Research in Africa Project (SARA). Washington, DC: USAID.
UNAIDS (Joint United Nations Programme on HIV/AIDS). 2002. 2002 Report on the Global AIDS Epidemic. Geneva, Switzerland: UNAIDS.
UNAIDS. 2004. 2004 Report on the Global AIDS Epidemic: 4th Global Report. Geneva, Switzerland: UNAIDS.
USAID (United States Agency for International Development). 2003. The Health Sector Human Resource Crisis in Africa: An Issues Paper. Washington, DC: USAID.
Vujicic M, Zurn P, Diallo K, Adams O, Dal Poz MR. 2004. The role of wages in the migration of health care professionals from developing countries. Human Resources for Health 2(1):3.
Wasike A. 2003, December 4. Go to the rural areas, PM tells medics. New Vision, Uganda.
Whiteside A. 2002. HIV/AIDS, health and education. In: Forsythe S, ed. State of the Art: AIDS and Economics. Washington, DC: Policy Project and Merck and Co. Inc. Pp. 24–29.
WHO (World Health Organization). 2002a. World Health Report 2002: Reducing Risks, Promoting Healthy Life. Geneva, Switzerland: WHO.
WHO. 2002b. Report on Infectious Diseases: Scaling-Up the Response to Infectious Diseases. Geneva, Switzerland: WHO.
WHO. 2004a. Investment in Water and Sanitation Yields Health and Economic Benefits. [Online]. Available: http://www.who.int/mediacentre/news/releases/2004/pr28/en/ [accessed March 1, 2005].
WHO. 2004b. Summary Country Profile for HIV/AIDS Treatment Scale-Up: Botswana. [Online]. Available: http://www.who.int/3by5/en/cp_bwa.pdf [accessed March 1, 2005].
WHO. 2004c. Global Atlas of the Health Workforce. [Online]. Available: http://www.who.int/GlobalAtlas/DataQuery/home.asp [accessed March 1, 2005].
WHO. 2004d. Human Resources for Health Country Synthesis. Geneva, Switzerland: WHO.
WHO AFRO (Regional Office for Africa). 2002. Report on Consultative Meeting on Improving Collaboration Between Health Professionals, Governments, and Other Stakeholders in Human Resources for Health Development. Addis Ababa, Ethiopia: WHO. [Online]. Available: http://www.afro.who.int/hrd/consultative_meeting_report.pdf [accessed March 1, 2005].
WHO and UNICEF (World Health Organization and United Nations Children’s Fund). 2000. Global Water Supply and Sanitation Assessment 2000 Report. Geneva, Switzerland: Joint Monitoring Programme for Water Supply and Sanitation.
Wibulpolprasert S. 1999. Inequitable distribution of doctors: Can it be solved? Human Resources for Health Development Journal 3(1):2–39.
Wibulpolprasert S, Pengpaibon P. 2003. Integrated strategies to tackle inequitable distribution of doctors in Thailand: Four decades of experience. Human Resources for Health 1(1):12.
World Bank. 1993. World Development Report 1993: Investing in Health. New York, NY: Oxford University Press.
Wyss K. 2004. Scaling Up Antiretroviral Treatment and Human Resources for Health: What Are the Challenges in sub-Saharan Africa? Berne, Switzerland: Swiss Agency for Development and Cooperation.

























