ESTIMATING THE CONTRIBUTIONS OF LIFESTYLE-RELATED FACTORS TO PREVENTABLE DEATH—A WORKSHOP SUMMARY
The Institute of Medicine (IOM) of the National Academy of Science held a workshop, December 13–14, 2004, to estimate the contributions of lifestyle-related factors to preventable death. The workshop’s statement of task included these specific questions:
-
What are the best available methods for estimating the number of preventable deaths among the leading causes of death in the United States?
-
Can scientists estimate the relative contribution of lifestyle-related factors as causes of preventable deaths with an acceptable level of accuracy?
-
What are the best measures of the public health burden of these preventable deaths: the number of preventable deaths, years of life lost, reduction in quality of years lived, disabilities caused by lifestyle factors, or the economic costs of death and disability?
-
What types of estimates provide the most scientifically sound basis for public policies that aim to reduce preventable deaths from lifestyle-related factors?
The workshop was sponsored by the Centers for Disease Control and Prevention.
Dr. Harvey Fineberg, President of the Institute of Medicine moderated the workshop, which included presentations from experts in statistical design, epidemiology, quality-of-life measures, communication, and public policy and discussions among the participants. Panels of experts addressed the following topics: methodological issues when estimating the public health burden of lifestyle factors; estimating “attributable risk” in practice; alternative ways of measuring the health burden; public policy issues. Dr. Michael Stoto, workshop rapporteur was charged with summarizing the highlights of the presentations and discussions from the two days and presenting them to the audience. At the end of the second day, Dr. Fineberg asked each participant to provide observations on lesson learned from the workshop and ideas for possible next steps.
This report summarizes the workshop presentations and discussions. Neither the workshop nor the summary is designed to draw conclusions or offer collective recommendations. In particular, the section on lessons learned and next steps should be understood as observations made by participants. Appendix A provided the workshop agenda, Appendix B contains speaker biosketches, and Appendix C provides a list of the individuals who attended the workshop.
Please note that in the summary of a number of discussions the report uses the term “obesity” or “poor diet and physical inactivity”. The concepts are different, as several presenters explain, and the terms used reflect the choice of the speakers.
INTRODUCTION
Moderator: Dr. Harvey Fineberg
This workshop is designed to enrich understanding of the contribution of lifestyle-related factors to preventable death and guide public policy designed to combat such death and related disease. While most of the presentations will address measurement and interpretation, the workshop’s broader purpose is to raise questions about the role of preventable death as a driving force in public health.
The term “preventable death” is somewhat of a misnomer, for no death is truly preventable. The real questions concern death’s timing and cause. The answers tell us whether death occurs prematurely—and, if so, what can be done to prolong life through behavior change or public policy.
The topic of preventable death poses questions that are partly philosophical, partly logical, partly methodological, and partly epistemological. Experts assembled here need to bear in mind the topic’s complexity when considering how to measure the impacts on public health of such factors and interpret research findings. The implications of efforts to extend life and improve its quality are far-reaching: they shape the actions of individuals, communities, and decision makers at local, national, and international levels.
Measuring the Health Impact of Lifestyles: Scientific Challenges
Presenter: Dr. Julie Gerberding
The IOM offers a unique setting for scientists to discuss dispassionately efforts by the Centers for Disease Control and Prevention (CDC) to quantify and interpret lifestyle contributions to preventable death. CDC can benefit by listening to, and learning from, experts who have come together to explore the topic, discuss controversial and emerging scientific issues, and move the field forward.
The workshop aims to address the methodology of a recent CDC study of the causes of preventable death, as well as the broader issues it raises (Mokdad et al. 2004). Appearing in the Journal of the American Medical Association (JAMA), the CDC study updated another study published a decade ago (McGinnis and Foege 1993). That earlier study broke new ground by estimating the contribution of several modifiable lifestyle factors—including tobacco use, alcohol use, and poor diet and physical inactivity—to death. The study set the stage for years of research, analysis, and public health policy. Yet while attempting to refine the earlier study’s estimates, the 2004 study created controversy over its methodology. CDC also discovered, after publication, a computer-related computational error that slightly overestimated the contribution of diet and physical activity as causes of preventable death. CDC submitted an erratum to the same journal correcting the computation, and launched a review of its internal mechanisms of peer review. The corrected figure is 365,000 deaths, instead of 400,000, from poor diet and physical inactivity (Mokdad et al. 2005).
CDC’s main objective for this workshop is to improve the study’s methodology. The process of developing and publishing the study has brought to the fore several broad scientific challenges.
Developing a Health Protection Research Agenda
The biggest challenge is simple: there is not enough research to estimate with the precision that we would like ultimately to achieve the contributions of lifestyle factors to mortality, and to reduce their impact. Though much is known that can serve as the basis for public health action, gaps remain concerning how optimally to protect the public’s health by measuring the burden of disease, determinants of risky behavior, interventions to change lifestyle, assessing the preventable fraction of deaths from these factors, the cost-effectiveness of interventions, and communications to maximize diffusion of effective interventions. Recognizing that CDC previously gave insufficient priority to research on preventable death, the agency is planning—through its health protection research agenda—to focus on two major research gaps: measuring the preventable fraction, and evaluating the cost-effectiveness of interventions to reduce morbidity and mortality.
Closing the Knowledge Gap
CDC and the public health field have been working for four decades to weigh tobacco’s impact on mortality and morbidity. Despite this longstanding focus, the science is not perfect, particularly regarding multiple risk factors interacting in various populations and at various stages of life. Perfection is obviously unattainable, but we have ample, unequivocal evidence for public health action. Greater uncertainty surrounds the impact of diet and physical fitness on mortality and morbidity. Research has focused on these factors for less than a decade, and views diverge on methods for estimating the impact of diet and physical fitness, the effects of co-factors and interacting risk factors. Scientists need to think through what is being measured and the utility of the measures for the public and policymakers. One lesson CDC has learned is humility: there is no room for scientific arrogance and overconfidence in an emerging area of knowledge with no right answer. We also will often need to act (as we do in other areas of public policy) based on the preponderance of evidence together with other considerations (such as the costs of not acting) rather than wait for absolute scientific certainty.
Bringing Together Diverse Disciplinary Threads
The need for collaboration across disciplines, life stages, advocacy groups, and funding lines is great. The public health community must work together to transcend these divides to focus on the real people whose health needs protection. People are more than a collection of body parts and risk behaviors, such as tobacco use and lack of physical fitness. They and their families often face more than one health issue, and live in communities confronting more than one health threat. Scientific collaboration helps ensure a more holistic approach to protecting health. This recognition has propelled CDC to restructure itself to create new processes for scientific collaboration from the outset of research rather than at the tail end.
Balancing Scientific Diversity and Scientific Consensus
Science is a quest for new knowledge that thrives on healthy expression of differences, competing hypotheses, peer review, and self-correction. However, the public often misinterprets these processes, which work so well within the field, as lack of knowledge, uncertainty, or incompetence. Given scientific debate surrounding lifestyle risks, researchers must press for the best possible science and avoid “group think” and premature consensus, while also striving to communicate uncertainty to the public without appearing inept.
Communicating to Policy Makers and the Public
Scientists are often so cautious about the caveats and limitations of their findings that the public cannot make sense of what they are saying. The public health community needs to achieve the right balance between scientific language and information that non-scientists can interpret. This is not a new problem, but the issues surrounding diet and physical exercise illustrate very well why communication with the public is so challenging.
CDC wishes to improve its methods and approaches—and, especially, to advance its research agenda—to provide the most accurate estimates of the health burden of various behavioral factors. CDC also would like to do a much better job of communicating science both internally and externally. Its overt goal is to overcome these challenges while creating an environment where efforts to advance one health issue do not detract from the importance of others.
Attributing Risks in Preventable Deaths: What Metrics Best Inform Health Policy?
Presenter: Dr. George A. Mensah
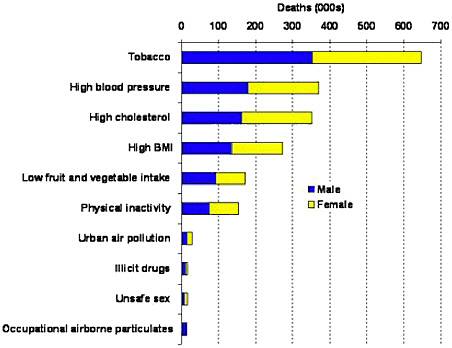
The challenges facing public health in the twenty-first century are remarkably different from past challenges. Whereas infectious diseases were once the leading causes of mortality in the United States, today chronic diseases have taken their place. More than 1.7 million Americans die annually of chronic diseases. Four of those diseases—heart disease, cancer, stroke, and diabetes—cause almost two-thirds of all deaths (see Figure 1).
One key question for health policymakers is whether death is the best measure of the societal burden of chronic disease. What other outcome measures might give policymakers a sensitive and reliable gauge of the public health impact of chronic diseases? Options include life expectancy, mortality from all lifestyle-related causes or specific causes, preventable deaths (premature mortality), disability, healthy days (quality of life), direct or indirect costs, cost-benefits, and return on investment. Policymakers could focus their attention on health programs and interventions that yield the most beneficial impact on the selected outcome measure. Health impact could be measured in a variety of ways, including lower mortality, better access to quality health services, healthier environments, expanded wellness programs, or reduced health disparities.
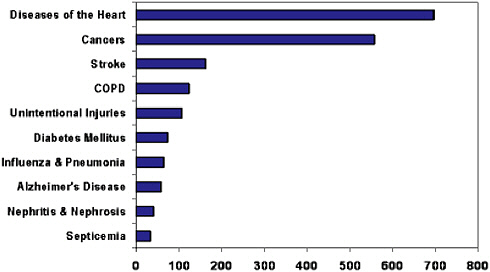
FIGURE 1. The 10 Leading Causes of Death in the United States, 2002
SOURCE: Anderson et al. 2002.
For example, decision makers might choose preventable death as the key measure to inform policy, considering that some 33 percent of all U.S. deaths can be attributed to three behaviors: tobacco use, physical inactivity, and poor eating habits. Or policymakers could select cost as their key measure and target resources to preventing the costliest conditions, which include heart disease, cancer, trauma, and mental disorders. As another alternative, policymakers or their counterparts in the business or insurance industry could focus on programs that generate the biggest return on investment, such as worksite programs to promote health. One study found that every dollar spent on Citibank’s worksite health promotion program saved nearly $5 in medical expenditures (Ozminkowski et al. 1999). Several other studies have found similarly high returns on investment for worksite health programs (Ozminkowski et al. 2002), including one study that reviewed 13 health promotion programs (Aldana 2001).
Other useful indices for informing policy include objective measures of morbidity such as hospitalizations. Policymakers interested in reducing the burden of heart attacks, for example, might adopt smoke-free ordinances for public places and worksites. The impact of this intervention can can be assessed using changes in hospital admissions. for myocardial infarction. After Helena, Montana, passed an ordinance in 2002 banning smoking in public places, hospital admissions for acute myocardial infarction decreased significantly (from an average of 40 admissions during the same months in the years before the law was in effect, to a total of 24 admissions during the six months the law was enforced). After a court order suspended the law several months later, the hospital admissions increased to the previous years’ average. (see Figure 2) (Sargent et al. 2004).
The purpose of this workshop is to promote discussion on which metrics or combination of metrics will best inform policymakers. The agency is also seeking the best ways to communicate to the public and policymakers the nature of the scientific evidence, especially in complex issues such as obesity and health. Informing policymakers requires not only the best scientific measure(s) but also clear, concise, and consistent messages about the practical health implications of observed changes in these metrics.
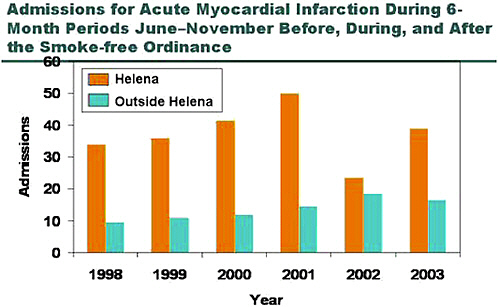
FIGURE 2 Admissions for Acute Myocardial Infarction During 6-Month Periods June–November Before (1998-2001), During (2002), and After (2003) the Smoke-Free Ordinance
SOURCE: Sargent et al. 2004.
SETTING THE STAGE FOR DISCUSSION
Causality
Presenter: Dr. Richard Scheines
The essential philosophical problem underlying this workshop is estimating the effects of an intervention regarding lifestyle factors and mortality from statistical associations among passively observed variables. For instance, scientists may know the “unmanipulated” probability [natural state] that a person will survive to age 80, given one hour of exercise a day and many other factors. However, we also want to know the “manipulated” probability [probability after imposing an intervention on an otherwise unmodified natural state]—the probability that a person will survive to age 80 given he or she is forced to do exactly one hour of exercise a day. In other words, the challenge is to use non-experimental data to estimate the effects of intervention.
In a typical clinical trial, a randomization procedure determines which subjects receive a placebo and which receive treatment. The randomization procedure determines the distribution of who takes the drug and who does not, and replaces the factors that naturally might influence taking a drug. We can model this with causal graphs, and given the pre-manipulation joint distribution of all the variables and a random assignment of treatment, we can calculate the post-manipulation joint distribution. We cannot do this as easily when, instead of randomizing treatment, we observe things passively. Why? Because unless we know important features of the causal structure, we cannot use non-experimental associations to estimate the associations following an intervention.
Analysts have developed a number of approaches to calculate, estimate, or search for the causal structure from non-experimental data. Most of this work hinges on the connection between causal structure and probability in terms of independent relationships called the causal Markov condition. The Markov condition is the assumption that every variable is independent of its non-effects and is conditional on its direct causes. With this assumption, we can start with a causal graph and compute what independence relations are predicted to be true in a distribution generated by that graph. We then use regression, logistic regression, contingency tables, and other analyses to determine what independence relations actually hold in the data to see if the predictions made by the causal graph holds in the data.
The difficulty in proceeding from data to graph is that many causal explanations are consistent with the same set of associations or independencies. To sort these out, scientists rely on discovery algorithms to use any available background knowledge and statistical work to determine which models are causally consistent with—or explain—those data.
While this work typically occurs informally, quite a few algorithms have been developed for moving from statistical data to causal equivalence classes. For instance, Spirtes, Glymour and Scheines (2000) have developed algorithms that are provably correct for computing the set of equivalent models given a set of observed associations.
One problem with the causal graph approach is that the interventions that policymakers are interested in are rarely ideal, so modeling them from data is very difficult. An ideal intervention on X would target X directly, be exogenous to the system and completely determine P(X). Another problem is that when scientists estimate the effect of manipulating something, we often assume that the marginal difference we predict from the population we observe will be the same in another target population, no matter how different.
Moreover, even though the idea of intervening and setting the value of a variable is the foundation on which this approach rests, what actually happens given an intervention is sometimes ambiguous. Serum cholesterol can be modified, for instance, by changing either its high-density or low-density components, or both. Depending on which of these components change, the risk of heart disease can rise or fall. So understanding how aggregate variables such as total serum cholesterol supervene on more finely grained variables that combine to form cholesterol is crucial in estimating the effect of interventions on preventable death.
In summary, what has been presented here are some of the challenges faced when trying to calculate or estimate causal structure from data that is in non-experimental contexts, and some techniques that have been used to improve inferring causal claims from data.
Attributable Risk in Epidemiology: Interpreting and Calculating Population Attributable Fractions
Presenter: Dr. Steven Goodman
The epidemiological concept of “attributable risk” is central to this workshop’s focus on lifestyle and preventable deaths. However, textbooks and courses for public health professionals rarely cover attributable risk and related epidemiological concepts in depth. Major issues concern
definition, terminology, properties, and interpretation, raising questions about the usefulness of the concept for evaluating the impact of an intervention on a population
Terminology
Attributable risk for a given factor in an individual is defined as the excess risk incurred by exposure to that risk factor, i.e. the component of overall risk “attributable” to exposure. It is measured by calculating the difference in risk between exposed individuals and unexposed individuals. The implication is that removing the exposure would reduce an exposed individual’s risk to that of an unexposed individual.
For public policy purposes, a more important epidemiological concept is the “population attributable fraction” (PAF). Unlike attributable risk, population attributable fraction applies to a population rather than to an individual, and it is not a measure of “risk”. PAF is the fraction of disease cases in a population associated with an exposure. “Attributable” is somewhat misleading because it implies causality, i.e. that removal of that exposure would in fact eliminate that fraction of cases. We will see that is typically not true, one reason being that complex causal connections, such as that between obesity and mortality, are not fully understood. Still, this term is preferable to its synonyms (which include population attributable risk and population attributable risk percent) because it avoids the term “risk.” Population attributable fraction should not be confused with similar concepts (such as etiologic fraction,1 incidence density fraction, and preventable fraction). Perhaps the best term would be population associated fraction (which would maintain the same acronym), but for the purposes of consistency with current terminology, I will retain the term “attributable”.
Population attributable fraction is the probability of the disease in the overall population (the average risk in both unexposed and exposed people) minus the probability of disease in the unexposed population.
Re-expressing the probability of disease as conditional upon exposure:
This general formula is very important to keep in mind because it makes clear that PAF is based on contrast of risks on an additive scale. In the 1950s, Levin (Levin, 1953) developed a simple way of calculating this ratio based on a multiplicative measure, the relative risk:
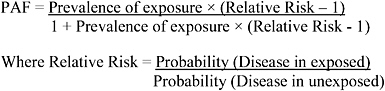
We will see later that this use of a multiplicative measure to calculate an additive contrast only applies in certain very simple situations, situations that rarely occur in modern epidemiologic analyses, and is the source of much confusion today.
Use and Interpretation
Proper use and interpretation of PAF requires a nuanced understanding of Levin’s formula, how each component is derived, and what types of outcome measures the formula requires. This formula and conception requires that the outcome be all-or-none, i.e. that if not for the exposure, the outcome would never have occurred within a defined period (e.g., birth defects, rare cancers, infections, injuries). PAF is not a good measure of population impact if the timing of the outcome is relevant. Time-related outcomes are those that would have occurred eventually (e.g. all-cause mortality) or almost certainly (e.g. highly prevalent age-related outcomes), and the exposure serves mainly to hasten occurrence. For these outcomes, other measures such as adjusted life years lost, may be more desirable than PAF for measuring the population impact of an intervention. Calculating PAFs with Levin’s formula requires actual measures of relative risk. Odds ratios, generated by logistic regressions, do not accurately estimate the relative risk except when the risk is rare (<10 percent). In addition, Levin’s formula uses the ratio of cumulative risks, not the incidence rate ratio, the latter being measured by two other popular regression approaches – proportional hazards and Poisson models. So most standard multivariate approaches to epidemiologic analyses do not produce the quantity that is used in the Levin formula, although they sometimes come close.
PAFs are commonly misinterpreted as being additive, i.e. summing to 100 percent. In fact, PAFs are not additive when multiplicative (e.g. logistic) models of data analysis are used to generate the relative risk inputs, models which are standard in epidemiologic analyses. PAFs are also non-additive when causes are multifactorial, when individual lifestyle factors require each other to exert their effect, or when one factor is in the causal pathway of the other (cholesterol elevation and obesity, for example). The major implication of non-additivity is that it is incorrect to say that if 30 percent of deaths are attributable to one lifestyle factor (e.g., poor diet), then 70 percent are due to the other factors (e.g., tobacco, alcohol, firearms, sexual behavior). As with PKU disease, it can be completely correct to say that a case of disease is 100 percent attributable to an environmental factor (phenylalanine exposure) and is also 100 percent genetic (the phenylketonuria [PKU] gene).
Another caveat is that interpreting PAFs depends on properly adjusting for the impact of confounders (other factors that affect the risk of the outcome being studied). This adjustment is quite different than the adjustment that occurs in a standard multiplicative regression model, since even if the relative risk of an exposure is constant at different ages, the PAF associated with that same exposure could be quite different in populations with different age structures. This occurs for the same reason that a constant relative risk produces very different absolute risk differences as the underlying risk changes. So one cannot take a RR “adjusted for age” and then ignore the age structure of the population for whom the PAF is being calculated. The proper equations for calculating population-attributable fraction (PAF) take this into account, but it is important that we recognize that our intuition about multiplicative “adjustment” doesn’t apply. Interpreting PAFs also depends on understanding whether interactions occur between lifestyle factors and confounders
(obesity could interact with age to influence the risk of death, for example). Thus PAFs are not easily predictable from standard multiplicative measures and models.
In addition to requiring an all-or-none outcome, PAFs (using the Levin formula) also require an all-or-none exposure. In the case of an exposure measured on a continuum, e.g. weight, physical activity, etc., we must be very careful about how we define the baseline state, i.e. the state that corresponds to an “elimination” of the exposure. While we can eliminate smoking, we cannot eliminate BMI. It is more meaningful to measure the impact of a shift in the exposure distribution, e.g. everyone losing 10 lbs, rather than everyone attaining an “ideal” BMI of less than 25. PAFs can be calculated for situations when exposures shift, but not with simple formulae.
PAFs do not measure the proportion of cases for which a given factor plays a causal role. That measure is the etiologic fraction. Nor do PAFs, by themselves, indicate the impact of any given intervention on modifying risk, for many reasons. An intervention might not eliminate a given exposure, it could have adverse effects that offset its benefits, it may have effects on other factors that augment its benefits, and it may affect the size of the population at risk by modifying competing risks. Finally, and perhaps most important, we often don’t actually know what the causal risk effect is of changing a person’s exposure. That is, we may know the mortality risk of persons with a BMI of 25, and those with a BMI of 30, but this does not necessarily tell us what the risk change will be for a person with a BMI of 30 who drops to a BMI of 25. That person will almost certainly not attain the same risk of someone who is naturally at the lower level, and it may depend on how exactly that BMI alteration occurred, e.g. by severe calorie restriction, by diet and exercise, or by surgical means. This again underscores the importance of specifying the intervention designed to change a risk factor.
Thus, a significant and serious problem of calculating and interpreting PAFs is that they confuse numbers associated with risk factors with the effects of interventions. For both policy and scientific purposes, it is the impact of an intervention that we are interested in, not the impact of changing a single risk factor in an equation; those numbers can be profoundly different. If we change our language and conceptualization from mathematical manipulations of isolated variables to assessing the effects of achievable interventions then many of the problems discussed previously disappear. Predicting the effects of interventions in the absence of randomized trials still remains a challenge, but the intervention perspective keeps us focused on the proper concepts, measures and actions.
In Levin’s era, the exposure that motivated him (smoking) and the intervention (smoking cessation) were closely related, and the causal effect of a successful intervention was virtually identical to the effect predicted by the variable in equations, so these distinctions were not critical. But as we apply the concept he developed in much more complex settings, we must appreciate the nuances of its interpretation and calculation, and be careful to distinguish between the mathematical effects of variable changes with the health effects of interventions.
METHODOLOGICAL ISSUES WHEN ESTIMATING LIFESTYLE FACTORS
Partial Adjustment
Presenter: Dr. Katherine Flegal
Estimating the impact of lifestyle factors on mortality can be accomplished by calculating the population attributable fraction (PAF). Levin’s formula for PAF uses only two parameters: the prevalence of exposure to a lifestyle factor (such as obesity), and the unadjusted relative risk of mortality associated with that factor. However, Levin’s formula can be biased when there is confounding of the exposure-outcome relationship. Those circumstances require a different approach.
The “weighted sum” method is one way to calculate PAF without bias when there is confounding. In a simple example, consider a population in which there are two subgroups and subgroup member is a confounding factor, because the prevalence of the exposure and the probability of deaths both differ by subgroup, but the relative risks are the same in the two subgroups. The weighted sum method calculates the number of excess deaths in each subgroup using Levin’s formula and then sums them to get an estimate for the entire population. To use the method, analysts have to know the number of deaths within each subgroup (such as the number of deaths among smokers and the number of deaths among never-smokers)—information usually not available for the U.S. population.
The “partially adjusted” method (Mokdad et al.2004)does not require knowing the number of deaths in each subgroup. Instead, the method calculates the relative risk adjusted for subgroup membership and then applies that adjusted relative risk to the prevalence of exposure in the entire population, using Levin’s formula for unadjusted relative risks. This method may be referred to as “partially adjusted” because the relative risk is adjusted but the attributable fraction formula itself is not adjusted. However, this use of the formula is biased, and the magnitude of bias depends on the degree of confounding. In a 1998 review article, Beverly Rockhill maintained that the use of adjusted relative risk in a formula only appropriate for unadjusted relative risks is probably the most common error in PAF calculations (Rockhill 1998).
To characterize the magnitude of the bias in the partially adjusted method applied to the obesity-mortality association, Flegal and colleagues (2004) constructed hypothetical examples that are plausible approximations of reality based on U.S. data. These scientists looked at confounding by age and sex, because those are strong confounders of the obesity-mortality relationship; older people have higher mortality rates and a lower prevalence of obesity. In this case, because this is a hypothetical example, the “correct” number of deaths attributable to obesity is fixed at 195,000. However, the partially adjusted method yields an estimate of 230,000—a 17 percent overestimate.
Another issue in the relationship between obesity and mortality is “effect modification”: the relative risk of mortality associated with obesity declines with age. Typically, the relative risks for a PAF calculation come from a derivation cohort such as the Framingham Heart Study, and are applied to a target population such as the entire United States. The prevalence of exposures can be
derived from a population-based survey such as the National Health and Nutrition Examination Survey (NHANES). With effect modification, the degree of bias in the partially adjusted measure depends on the similarity of the derivation cohort and the target population.
The derivation cohort may differ from the target population for a variety of reasons, including the prevalence of obesity and the age structure. Flegal and colleagues investigated a number of differences. In one example, 3.4 percent of the target population was over 80 years of age, and the “true” number of deaths attributable to obesity was 230,000. If the elderly accounted for only 0.4 percent of the derivation cohort, the estimated number of deaths attributable to obesity would be 283,000—a 42 percent overestimate.
In sum, the partially adjusted method attempts to solve the problem of combining adjusted relative risk from one cohort with exposure data from a different source by using a formula appropriate only for unadjusted relative risks. This approach is intuitively appealing and commonly used, but is not correct. The literature acknowledges that it can lead to bias, and suggests that, in the case of obesity and mortality, the bias from only partially adjusting for confounding is probably at least a 20–25 percent overestimation. The next speaker will discuss a different approach that addresses this problem.
Calculating the Number of Deaths Attributable to a Risk Factor Using National Survey Data
Presenter: Dr. Barry Graubard
(Delivered by Dr. Mitchell Gail)
A variety of studies, including nationally representative survey data, are often used to calculate the number of deaths attributable to a lifestyle factor such as obesity. These calculations rely on three essential elements: (1) a joint relative risk model for mortality for each combination (i) of risk factors and confounders; (2) p(ai) is the proportion of the population at age “a” with risk combination i estimated from a population-based survey such as NHANES; and (3) the number of deaths (D) obtained from vital statistics.
The first element can be expressed in terms of adjusted relative risks (rai) for each age “a” and combination i of risk factor (e.g., body mass index group) and confounders (e.g., smoking, race). These adjusted relative risks can be estimated from a proportional hazard regression analysis of a cohort. These rai can then be combined with prevalence estimates, pai, for each combination of risk factors, the second element, at each age with the following formula:
(where ao is the baseline incidence at age “a”)
With this as a starting point, we can calculate what would happen if everyone with a particular risk factor and confounder combination i were transformed into a group that had the lowest level of the lifestyle exposure, but all the other components of the risk factor combination were unchanged, rai* with the following formula:
The PAF for each age group (ARa) is then calculated as:
Once we have this fraction, we can multiply it by the number of deaths in a particular age group, the third element, to get the number of deaths attributable to modifying the lifestyle exposure.
The prevalence estimates (pai) of each of the combinations of risk factors are from a nationally representative, population-based survey such as the NHANES survey, but the information on relative risk comes from a separate study with a population that is not necessarily representative of the national population. Sampling weights from the nationally representative survey can be applied to the ri to get unbiased estimates of ARa.
To conclude, I have presented a method for estimating an adjusted number of attributable deaths from a particular lifestyle risk factor. What distinguishes this calculation from other approaches is that it uses the information on prevalence from the general population as a basis for calculating attributable risk, rather than using a representative sample of cases to determine the prevalence of combinations of joint risk factors. National survey data can provide representative data not only for relative risks but also for the prevalence of the joint risk factors. Further, survey methods developed over the last 20 years allow for calculating confidence intervals, taking into account complex sampling design.
Caveats in Using Estimates of Deaths Attributable to Lifestyle Factors
Presenter: Dr. Mitchell Gail
Several challenges may arise in trying to estimate the number of deaths attributable to lifestyle exposure. One is that various investigators will approach similar sorts of data with very different goals. A modest goal might be to try to describe the attributable mortality in a target population, such as the U.S. population in the year 2000. (This goal is modest only if people have agreed on the important confounders and all the other technical issues.) A different goal is to establish that the lifestyle factor has a causal connection to mortality by controlling for confounders or investigating special subgroups. Trying to infer how many deaths could be prevented by a hypothetical intervention in the lifestyle factor is still another goal.
Another challenge is difficulty in measuring the lifestyle factor. Obesity, for instance, can be measured in terms of body mass index (BMI), weight, or the distribution of adipose tissue. The lifestyle factor could be evaluated through a single measurement or repeated measurements over time. Determining the measure that best captures the lifestyle factor should be linked to a scientific understanding of what is occurring, and obtaining consensus on the measure is important.
To illustrate the problem, let us say that BMI is the agreed-on measure. BMI can be categorized in a number of ways to represent the risk-factor levels of underweight, normal weight, overweight, mildly obese, and obese. Suppose there is a distribution over these risk-factor levels. Researchers could ask what would happen if someone in the mildly obese category underreported weight, thus putting that person in the overweight category. Unlike the kind of error epidemiologists confront, in which the error distribution is thought to be independent of what they are trying to estimate, this error relates directly to what scientists are trying to estimate, because mildly obese people may try to make themselves look better. This type of measurement error can induce important bias.
Researchers must also ask whether the study population is representative of the target population. This might not be true if there are period effects (for example, changes in treatment over time), if the researchers are extrapolating an earlier study to the current population, or if they are applying a current study to future populations. A mismatch between the study population and the target population could also result from self-selected cohorts, cohorts from special populations (e.g., nurses), or subgroups selected at the time of analysis (e.g., excluding smokers or events that occurred in the first five years of follow-up). Subpopulations can provide many insights about the role of confounding, but if a simple estimate in a particular population is the goal (e.g. U.S. population in 2000), some caution is needed in using data from special subgroups.
Difficulties also arise when controlling for confounding. Some potential confounders, such as health status, are difficult to measure unambiguously. Measuring and controlling for time-varying covariates is also difficult. In some cases there is ambiguity about what to control for. Researchers must ask whether the covariate is on a causal pathway, and the answer is not always clear. In addition, the covariates adjusted for in determining attributable risk must also correspond to those adjustments made for the component relative risks.
The problems raised above relate to bias (the tendency of an estimate to be systematically too high or too low). Statistical precision is also an issue. This arises in part because different sources of data are used to estimate relative risk and prevalence. The required data often involve complex sampling, so special methods are needed to calculate confidence intervals. Also, confidence intervals are often wide because a small variation in relative risk can induce a large variation in attributable risk (Flegal et al. 2004).
Finally, researchers must consider differences between hypothetical and achieved intervention effects. They must choose an appropriate exposure level or exposure distribution—the baseline. An intervention may fail to achieve the desired alteration in the distribution of lifestyle exposure. Another fundamental problem is that an observed association of exposure with mortality may not reflect a causal relationship between the exposure and the outcome. Finally, the intervention can have various effects on mortality apart from its effects on the lifestyle exposure (exercise recommended to reduce weight also has other effects on health, for example). Thus, the impact of the intervention may be hard to anticipate.
In summary, the challenges entailed in estimating deaths attributable to lifestyle factors include the difficulty of defining and measuring lifestyle exposures, and the problems posed by self-reported exposures. The latter may be subject to certain kinds of bias that are not removed by standard measurement error models. Other challenges include difficulties in controlling confounding and lack of statistical precision. Techniques are available, given the sampling plan, for
obtaining good estimates of precision, but there is an inherent lack of precision because of the nonlinearity of attributable risk, unless a study has extremely large cohorts. There are also many reasons why an intervention may not achieve the hypothetical estimate of its impact on mortality.
Estimating Population Attributable Risks: A Simulation Model Based on the NHANES I Followup Study and NHANES III
Presenter: Dr. Louise B. Russell
The National Health and Nutrition Examination Surveys (NHANES) offer ideal datasets for estimating the net effects of risk factors on health outcomes. Using the NHANES I Followup Study (a longitudinal survey begun in 1971–1975) and the NHANES III, our research team developed a simulation model to estimate the attributable fractions due to major risk factors for three outcomes: all-cause mortality, hospital admissions, and nursing home admissions. The simulation model enables us to manipulate these risk factors, especially in the absence of clinical trials, and then determine their impact on health by calculating the PAF.
The simulation model is used to predict and compare the impact of various types of public heath goals (such as targeted reductions of blood pressure), and to study relationships among risk factors. It allows simulation of interventions to change smoking, blood pressure, total cholesterol, physical activity, body mass index, and chronic conditions such as diabetes. The projection methodology controls for age and sex. Combined with other analyses, such as cost-effectiveness analysis (see the later presentation by L. Russell), the simulation model can be used to generate a comprehensive picture of prevention and health.
The NHANES are large and representative datasets of the adult U.S. population. Through interviews and physician examinations, they measure major known risk factors. NHANES I was fielded from 1971 to 1975, with follow-ups to 1992 to collect data on mortality, hospitalizations, and nursing home admissions. Our research team developed a series of regression equations based on the NHANES I Followup Study to arrive at the net effects of each risk factor on health outcomes. The model was not a test of the risk factors; rather, the risk factors were a test of the model.
The equations were first validated to show that the major risk factors did indeed have a statistically significant impact on health outcomes: they also generated risk ratios that were reasonable in light of the published literature. Moreover, equations based on followup data through 1987 projected well to the 1992 NHANES findings. The equations were then updated with the 1992 data.
The equations can be applied to any cohort of adults for which data on the same risk factors are available. In the current version of the simulation model, they are applied to NHANES III adults. NHANES III was fielded from 1988 to 1994 and is more representative of today’s adults, who smoke less and are more overweight.
As an example of how the model can be used, we recently applied it to estimate the effects of prehypertension, the new category of risk identified in 2003 by the Joint National Committee on Prevention,Detection, Evaluation, and Treatment of High Blood Pressure. The model was used to
calculate the PAF for two scenarios: 1) eliminating residual hypertension by reducing systolic blood pressure (SBP) to 139 mm Hg for all NHANES III adults with SBPs of 140 mm Hg or higher, and 2) eliminating both residual hypertension and prehypertension by reducing SBP to 119 mm Hg for NHANES III adults with SBPs of 120 mm Hg or higher. The simulation found that prehypertension and residual hypertension accounted for nearly 14 percent of deaths, 4.7 percent of hospital admissions, and nearly 10 percent of nursing home admissions (Russell et al. 2004; see Figure 3). Prehypertension alone accounted for more than half of those percentages.
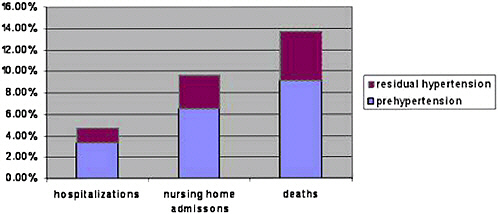
FIGURE 3 Simulation: Hospitalizations, Nursing Home Admissions, and Deaths Attributable to Prehypertension and Residual Hypertension in adults aged 25-74
SOURCE: Russell et al. 2004.
This simulation model provides a framework for consistently estimating attributable risk for different lifestyle factors. It enables valid comparisons of alternative interventions and programs. The same methods could be used with other large longitudinal datasets such as the Framingham Heart Study.
Discussion of Methodological Issues When Estimating Lifestyle Factors
Discussants voiced the following points:
-
The analysis of PAF from large, nationally representative surveys (e.g., NHANES) is limited by the nature of the data. Most surveys collect data on individual risk factors, yet neglect to obtain data on the social and regulatory context in which individual risk factors occur. The social and regulatory context can also be manipulated.
-
Empirical evidence that regulatory manipulations affect a health outcome can implicate the regulatory environment as part of the causal pathway.
-
PAF analyses tend to ascribe death to a single cause or risk factor when, in fact, multiple causes of mortality often interact. Explaining interactive causes to the public may be easier than trying to parse out, by analyzing data, a single cause of death.
-
Phenylketonuria (PKU) illustrates that when two risk factors interact (e.g., genes and phenylalanine exposure), it is important to focus on the PAF of the manipulable factor (phenylalanine exposure) rather than the genetic cause, which cannot be manipulated.
-
Sample re-weights in the analysis bring the calculations of PAF closer to the true PAF than do the empirical data.
-
Quasi-experimental studies showing pre-post changes in population disease patterns (such as the study of Helena, Montana, by Sargent et al. 2004) are very useful because they help validate the PAF models discussed at this workshop. But their value is greatest when there is a close temporal relationship between the risk factor (e.g., smoking) and certain outcomes (e.g., cardiac admissions), as opposed to situations with a long lag time (e.g., lung cancer).
-
If PAFs for obesity and mortality are not calculated with proper stratification by age, the effect will likely be overestimated, but the magnitude of the overestimation is not fully known. One ballpark estimate was that the overestimation was about 100,000 deaths. Regarding other interactions, generalizing about whether the result could be an overestimation or an underestimation is difficult.
The greatest impact on public health will occur if analysts examine their hidden assumptions about where it is feasible to intervene or manipulate a risk factor’s effect.
ATTRIBUTABLE RISK IN PRACTICE: EXAMPLES FROM THE FIELD
Overview of Actual Causes of Death, 1993
Presenter: Dr. J. Michael McGinnis
The predecessor study to CDC’s analysis of attributable risk examined actual causes of death in 1990 (McGinnis and Foege 1993). My co-author and I had three goals in completing the 1990 analysis. They included raising awareness of preventable deaths and enhancing a prevention perspective; quantifying the impact of lifestyle factors on number of deaths, allowing policymakers and the public to compare those factors; and allowing analysts to track progress on reducing the impact of lifestyle factors.
Drawing on published reports between 1987 and 1993, we assigned point estimates to each preventable factor, or manipulable cause of premature death. We chose our point estimates from ranges and then rounded them for reporting purposes. To avoid the appearance of precision and underscore our findings as estimates, we used the following rounding rules: we rounded point estimates over 100,000 to the nearest 100,000, point estimates over 50,000 to the nearest 10,000, and point estimates below 50,000 to the nearest 5,000. We corrected for rudimentary double-counting (e.g., overlaps of alcohol with motor-vehicle fatalities, or alcohol with firearm fatalities), but not for double-counting embedded in a given study's report of attributable fractions. We found that the nine factors we analyzed accounted for about half of all deaths in 1990, with tobacco and diet/physical activity playing leading roles (see Table 1).
TABLE 1 Findings on Actual Causes of Death, 1990
|
Cause |
1990 no. (est.) |
|
Tobacco |
400,000 |
|
Diet/activity patterns |
300,000 |
|
Alcohol |
100,000 |
|
Microbial agents |
90,000 |
|
Cause |
1990 no. (est.) |
|
Toxic agents |
60,000 |
|
Firearms |
35,000 |
|
Sexual behavior |
30,000 |
|
Motor vehicles |
25,000 |
|
Illicit use of drugs |
20,000 |
|
Total |
1,060,000 |
|
All causes |
2,150,000 |
Our initial intention was to separate the impact of diet on mortality from that of physical activity. We decided to link the two after realizing that obesity was an important common denominator, and that the epidemiological literature did not adequately differentiate the contributions of the two. Because the evidentiary base was fragile, we used the lower bound of the estimates for diet/activity.
We recognized several methodological shortfalls and areas in need of attention. Those were large then and remain large today. The need for better understanding of the absolute impact of etiologic factors on disease and disability is great. The focus should include deaths occurring before age 80 or 85 instead of age 75, which was the focus of our calculations. The impact should be expanded to cover morbidity and quality of life in addition to death. More attention should be given to the impact of socioeconomic factors and access to healthcare. The resource implications of addressing premature death and disability also need to be addressed.
In our editorial accompanying the CDC study (McGinnis and Foege 2004), we noted that the non-obesity component of the impact of poor diets and sedentary lifestyles was likely greater than the 15,000 deaths reported by CDC. This is a salient research topic for the coming months and years. But the main point of our editorial was to appreciate the similarities across the two papers: despite different approaches and separation by a decade, the estimates were of similar overall magnitude. Both then and now, tobacco, diet/activity, and alcohol were the three leading causes of death. We also pointed out that the impact of tobacco is declining (after accounting for population growth), while the impact of diet/activity is growing.
Rationale for Actual Causes of Death, 2000
Presenter: Dr. Donna Stroup
This presentation addresses CDC’s rationale for updating the 1990 study of actual causes of death by McGinnis and Foege (1993) and outlines our most recent efforts.
Over the past decade the country has seen a substantial shift in lifestyle patterns. Because of the widespread use of the 1993 study, we embarked on an updated study to determine if a measurable shift in lifestyle-related causes of death had occurred during the 1990s. The new study, published in JAMA (Mokdad et al. 2004), was a classic replication study: its methodology was largely similar to that of the earlier study, in order to allow for comparisons of the 1990 and 2000 estimates. We used published causes of death reported for 2000, relative risk and prevalence estimates from the published literature, and readily available government reports.
One additional objective was to provide a methodology that states could replicate. National estimates—while useful for asking questions and fostering training—were of limited value to states,
which need to customize analyses for decision makers. We hoped that our methodology would be readily available to state and local agencies.
We found that mortality rates from heart disease, stroke, and cancer declined between 1990 and 2000, while behavioral changes led to greater prevalence of physical inactivity, poor diet, and diabetes. We showed that a large proportion of the more than 2 million deaths each year in the United States are preventable through lifestyle changes, such as tobacco cessation, better nutrition, and increased physical activity (Mokdad et al. 2004).
The 2004 article attracted considerable media coverage. Part of that coverage focused on competing risk factors, which this workshop can address. The article also spurred letters from some scientists about our methods and assumptions. During the past decade, other investigators have used different approaches to analyze the health burden associated with conditions and risks. Some groups of scientists contend that the methodology we used actually underestimated obesity-related deaths.
We undertook a post-publication review of the 2004 paper and, in so doing, discovered an error in our computations caused by a computational mistake. This error produced an overestimate of the number of deaths caused by poor nutrition and physical activity. We published an erratum in JAMA (Mokdad et al. 2005). However, our overall finding still shows a substantial increase in diet/activity-related mortality compared with McGinnis’s figure for 1990.
Neither the Department of Health and Human Services nor any other part of the government tried to influence the design or outcome of our study or the presentation of findings. The error in the 2004 publication was simply a computational mistake. Our overall conclusions remain unchanged: tobacco use, poor nutrition, and physical activity are lifestyle choices that contribute to the largest number of deaths. The number of deaths from the constellation of risks and conditions related to poor nutrition and physical activity is also growing.
After the article was published, several independent scientists, including statisticians, reviewed our approaches and discovered no other computational errors. A post-publication review—which included scientists from the National Institutes of Health and the Agency for Health Care Research and Quality—made it clear, however, that significant scientific questions remain regarding the best methods for assessing the number of deaths and the overall burden of disease from specific modifiable risks and causes. Different investigators examining the same set of issues have used different approaches. The letters that followed our study's publication discussed the lack of standard approaches.
To address the clear need for greater consensus, CDC initiated this workshop. We believe that more information on the health burden represented by years of life lost, healthcare costs, quality of life, and morbidity would be of great value to both researchers and policymakers.
We cannot afford to ignore these leading causes of death, and we must maintain a strong public health commitment to fighting tobacco use, poor nutrition, and physical inactivity. This workshop is important in airing some of the assumptions and attributes of these methodologies.
The Numbers Are the Easy Part: Interpreting and Using Population Attributable Fractions
Presenter: Dr. Beverly Rockhill
Beyond the statistical calculations discussed at this workshop, researchers must address a number of conceptual and philosophical issues to properly interpret and use population attributable fraction (PAF). The key question is whether the calculation of PAF suggests realistic and effective prevention strategies.
PAF will rise with an increasingly broad definition of exposure (e.g., an increasingly broad definition of “overweight/obese”), as long as every group added to the exposed group has a relative risk greater than 1.0, compared to the remaining unexposed. This means that if the definition of exposure is broadened, the proportion exposed goes up, and even though the overall relative risk (comparing all exposed to unexposed) may go down, the PAF will rise. Thus, the PAF can usually be made high simply by defining exposure so that nearly everyone—or at least a large proportion of the population—is labeled as exposed. This illustrates, in a subtle way, the tremendous difficulty of communicating this kind of information to individuals.
The question of how to interpret PAF when nearly everyone in the population is exposed is thus raised. One implication of a PAF calculation which has employed a broad definition of exposure is that nearly the entire population will have to shift in terms of their exposure distribution to achieve the calculated reduction in risk in the population. Further, from a statistical standpoint, it means that the PAF estimate will be highly unstable.
The core definition of PAF depends on the notion of a causal association between the exposure(s) underlying the estimation and the outcome being considered. PAF calculations do not help us understand the occurrence of disease; their value lies in what they can tell us about potential prevention strategies. However, the tendency to equate the concepts of “attribute,” “explain,” and “cause” leads to problems in interpreting PAF calculations. Those words can be both misleading and alarming. They are misleading because they seem to imply that we suddenly know something about disease that we did not know before. They are alarming to the many people who have the risk factors but who are not going to wind up with the disease.
Furthermore, the natural result of conflating explanation with cause is that PAFs are commonly misinterpreted as the proportion of cases who actually have the risk factors. But a PAF has no meaning for individuals. The fact that the attributable fraction for obesity and inactivity has risen over the past 10 years should not make it any more or less urgent for an individual to think about changing his or her behavior.
In conclusion, researchers need to keep several points in mind:
-
The population attributable fraction depends on the exposure cutoff point. Estimates can be made high—and they will become very imprecise—if analysts consider a high proportion of the population exposed to the risk factor.
-
The choice of exposures, or “causes,” is often arbitrary and sometimes even meaningless. Some estimates of attributable fraction include exposures simply because data are available.
-
A population-level interpretation of attributable fraction is necessary. To avert a relatively small number of cases, many people have to change their exposure. Communicating this to individuals is difficult.
-
The population attributable fraction does not have meaning at the individual level because it says nothing about the causes of individual cases, or about which cases are or will be attributable to the exposure. The fact that we know that a certain number of deaths in the United States will be due to inactivity, obesity, or breast cancer risk factors tells us nothing about which individuals will die as a result of those exposures. To an individual, the attributable fraction has no meaning, but it does have meaning for those working on prevention policy.
Thus, plugging in relative risk and the prevalence of exposure is comparatively easy. The harder part is deciding what cutpoints are meaningful, in terms of separating “exposed” from “unexposed.” Harder still is the key question underlying all PAF analyses: what is the implication of the analysis for a realistic and effective prevention strategy that will shift exposure in a high proportion of the population?
Estimating the Health Impacts Attributable to Alcohol
Presenter: Dr. Robert Brewer
Excessive drinking is the third leading lifestyle-related cause of death in the U.S. and results in approximately $180 billion in economic costs per year. However, most excessive drinkers are not alcohol dependent.
More than a decade ago, CDC released a software program, ARDI2, to help states assess the public health impact of alcohol consumption. Prepared as a Lotus spreadsheet program, the software was designed to estimate alcohol-related impacts, including deaths, years of potential life lost (YPLL), and economic costs. In the last few years, CDC has sought to update the software, both scientifically and technically, and release it as a Web-based application. The project, funded by the Robert Wood Johnson Foundation, highlights methodological issues involved in determining public health impacts due to excessive drinking.
CDC began its update of ARDI software by convening a work group of experts in alcohol and public health. The work group was charged with choosing a conceptual approach, updating the list of alcohol-attributable conditions, selecting risk estimates or alcohol-attributable fractions, and choosing prevalence cutoff points.
Consistent with the goals of the U.S. Public Health Service’s Healthy People 2010 and the recommendations of the World Health Organization, the work group decided to primarily focus on the health impacts of excessive drinking. However, the work group felt that the software should also be designed to accommodate the assessment of health impacts from any alcohol consumption. In addition, they decided to separate chronic from acute conditions, and to rely on data sources that are readily available to state health departments, such as the Behavioral Risk Factor Surveillance System (BRFSS).
One of the key activities of the work group was to determine the methods that would be used to estimate Alcohol-Attributable Fractions (AAFs) for the 54 alcohol-related conditions that they selected for ARDI. Some conditions (e.g., alcoholic cirrhosis of the liver) are 100 percent alcohol-attributable (AAF=1.0); thus, all deaths from these conditions are included in ARDI estimates of alcohol-attributable deaths. However, most conditions are only partially attributable to alcohol (AAF <1.0). The methods used to estimate the AAFs for these conditions vary, depending on whether they are chronic (e.g., chronic hepatitis) or acute (e.g., drowning). For most chronic conditions (e.g., liver cancer), AAFs are calculated using Levin’s formula. The relative risk estimates for calculating these AAFs are obtained from meta-analyses, and prevalence data on alcohol use are obtained from the BRFSS. For most acute conditions (e.g., injuries), AAFs are based on studies or surveillance systems (e.g., the Fatality Analysis Reporting System) that collected direct measurements of the blood alcohol concentration of decedents.
Once the AAF is known, alcohol-attributable deaths can be easily calculated using the following equation:
Alcohol-Attributable Deaths = AAF × Cause-specific Mortality
To calculate YPLLs, the work group stratified alcohol-attributable deaths by gender and age using standard five-year age groupings. These age- and sex- specific death estimates are then multiplied by the corresponding estimate of life expectancy.
National estimates of deaths and YPLL due to excessive alcohol consumption for 2001 were published in CDC’s “Morbidity and Mortality Weekly Report” in September 2004, at which time the new ARDI software was also released. In 2001, there were over 75,000 alcohol-attributable deaths and 2.3 million YPLLs. Some 46 percent of these deaths were due to chronic conditions, and 72 percent of them involved men.
One of the largest limitations in estimating the public health impact of excessive drinking relates to prevalence: the Behavioral Risk Factor Surveillance System and other surveys substantially underreport alcohol use. Another problem is that the risk estimates used in ARDI were calculated by using average daily alcohol consumption levels that begin at levels greater than those typically used to define excessive drinking in the United States. Finally, age-specific estimates of AAFs were available only for motor-vehicle traffic deaths, despite the fact that alcohol involvement varies by age, especially for acute conditions. For these and other reasons, the estimates of deaths and YPLLs likely understate the true public health impact of excessive drinking in the United States.
Estimating Deaths Attributable to Alcohol Consumption
Presenter: Dr. Michael Thun
Efforts to quantify the number of deaths attributable to alcohol consumption have confronted many of the same methodological difficulties that complicate estimation of deaths attributable to diet/inactivity. The CDC has developed a standardized method for calculating population-atttibutable burden that minimizes variation in the estimates. Consequently, four U.S. epidemiological studies showed relatively small variation, estimating that 2.7–4.5 percent of deaths
result from alcohol abuse. Particularly important in CDC’s efforts to standardize the methodology has been to establish a consistent definition of alcohol abuse, and to confine the estimates to deaths caused by excessive drinking, and not to consider the net effect across all levels of alcohol consumption.
International studies, on the other hand, have revealed a threefold-to-fourfold (rather than twofold) variation in deaths from alcohol. Sources of variation include the use of different criteria for excessive drinking, different diagnostic categories, and varying relative risk estimates to calculate the attributable fraction. Sources of uncertainty or error include underreports by individuals of their alcohol consumption (a problem also found with reports of weight), underrepresentation of severe alcoholism in epidemiological studies, and the use of same relative risk estimate for all ages.
Some 41 percent of U.S. deaths from excessive alcohol consumption are from external causes, including motor-vehicle accidents, homicide, and suicide. Cirrhosis of the liver and liver cancer account for 15 percent and 3 percent of alcohol-attributable deaths, respectively.
Demographic factors such as age, gender, and socioeconomic status influence the prevalence of alcohol-related conditions in the population. Age, for example, modifies the balance between cardiovascular and external causes of death in men. Among people aged 15 to 29, the vast majority of alcohol-attributable deaths are from external causes, whereas after age 60 nearly 45 percent of such deaths stem from cardiovascular causes and only 3 percent from external causes. The relative risk of all-cause mortality varies by alcohol consumption, age, and cardiovascular risk, with the findings resembling a J-shaped curve (see Figure 4, drawn from the American Cancer Society cohort).3
Thus age, consumption, and cardiovascular risk influence the relative risk estimates used to estimate the population-attributable fraction. When possible, researchers should stratify their analyses to apply the appropriate relative risk to the population denominator.
In communicating cause-of-death findings to the public, analysts need to point out that estimates of PAF are not an exact science. Scientists also need to discourage the media from treating the findings as a horserace between the leading causes of death (tobacco and diet/activity) rather than focusing on the fact that both are huge causes of death.
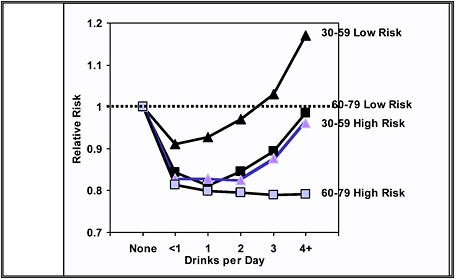
FIGURE 4 Relative Risk of All-Cause Mortality by Alcohol Consumption, Age, and Cardiovascular Risk, CPS-II Men and Women Combined
Estimating Adverse Health Impacts Attributable to Tobacco Use
Presenter: Dr. Corinne Husten
This presentation summarizes the method of estimating smoking-attributable mortality by CDC’s Office on Smoking and Health. Since 1987, CDC has used the smoking attributable mortality, morbidity and economic cost application, or what we call SAMMEC,4 to estimate the disease impacts of smoking for the nation, for states, and for large populations.
The method of estimating smoking-attributable deaths relies on Levin’s attributable risk approach. We restrict calculation of prevalence of deaths to the population aged 35 years and older. Because the relative risks of coronary heart disease and cerebrovascular disease decline with age, we stratify those risks into two groups: 35 to 64 years of age, and age 65 and above. We do not stratify by age for cancers and chronic obstructive pulmonary disease because age does not markedly affect relative risk. We have found little residual confounding (once age was taken into account) for education, occupation, race, alcohol use, hypertension, diabetes, and diet. We do stratify by sex because of the large gender differences in smoking histories and relative risk. We estimate prevalence and relative risk for both current smokers and former smokers because both are at higher risk of disease compared with people who have never smoked. Then, to avoid including causes of death that do not meet the Surgeon General's criteria for causality, our methodology uses cause-specific deaths.
We estimate that 440,000 deaths in 2000 were attributable to tobacco. That estimate has four components: 1) 18 tobacco-related adult diseases, 2) 4 infant conditions causally related to maternal smoking during pregnancy, 3) deaths among nonsmokers attributed to secondhand smoke, and 4) deaths from residential fires caused by smoking.
Our greatest concern is that simple all-cause methodology can overestimate the number of deaths attributed to tobacco use. Death rates for smokers are higher than for non-smokers for many conditions, but excess deaths for some of these are unlikely to be causally related to tobacco use. One example would be the inclusion in mortality figures of excess deaths among smokers in motor-vehicle accidents. While those accidental deaths could have occurred because drivers were distracted while lighting a cigarette, hot ash fell in their lap, or a cigarette butt flew into the back seat (instead of being pitched out the window) and lit a fire, the deaths are more likely due to the fact that smokers engage in other high-risk behaviors such as drinking and driving, and not to smoking per se.
Some causes of deaths have complicated confounders, which makes it difficult to parse out the number of deaths attributed to smoking from those attributable to other risk factors (e.g., alcohol use, tobacco use, and liver cancer). We do not include conditions for which the evidence of causality is suggestive but still evolving (e.g., smoking and colorectal cancer). If we computed deaths based on all causes of death with age stratification, the estimate would be 550,000 deaths per year. Without age stratification, a simple all cause methodology would result in an estimate of over 640,000 deaths per year.
Our overall estimates are likely conservative because we include only diseases meeting the Surgeon General's criteria for causality; we do not include all forms of tobacco use; we do not include all adverse effects of parental smoking; and we could be underestimating the risk for current smokers by relying on a major epidemiology study by the American Cancer Society (ACS) (citation 7 in Mokdad et al. 2004) which only assessed smoking status at the start of the study. Because some smokers quit during the 6 years of follow-up (and were therefore at decrease risk of disease) their classification as current smokers would bias the relative risk for current smoking downward. In addition, smoking histories of today’s smokers may be different than for smokers in the ACS study (done in the 1980s).
The tobacco industry and others have challenged the validity of our estimates, often asserting that our methodology incorrectly classifies too many diseases as smoking-related. A review by the General Accounting Office concluded that our methodology was reasonable in all respects, including our methodological assumptions, choice of datasets, and assessment of the pros and cons of alternative methods and data sources (GAO 2003). We do recognize, however, that we need to continue to improve and refine our methodology, such as by considering using more recent cohort studies. However, having a single source of data for all relative risks (ACS’s large prospective Cancer Prevention Study), is a strength of the current methodology. We also need to include mortality for all forms of tobacco use, update the SHS estimates, expand the diseases caused by parental smoking, and to consider more stratification (by age, duration of smoking, duration of quitting, etc.) However, we need to balance any potential increase in precision with the potential loss of accuracy and increased complexity, particularly in using SAMMEC to derive state-specific mortality estimates. We believe that the published estimate of 440,000 smoking attributable deaths is a sound one; we will be updating the estimate soon, based on new diseases deemed causal in the 2004 Surgeon General’s Report and updated prevalence estimates
Tobacco Use and Preventable Mortality
Presenter: Dr. Graham Colditz
Future PAF calculations of tobacco-related deaths face two key methodological challenges. First is the quality of the data on how relative risk varies with age. CDC’s Office of Smoking and Health has so far used only two age strata in estimates of the relative risks of ischemic heart disease and cerebrovascular disease (35 to 64 years, and 65-plus years). The second issue is whether CDC should rely on one source of relative risk estimates to calculate PAF,. For tobacco-related mortality this is the approach, but this is not the caase for alcohol-related mortality. The latter relies on multiple data sources of relative risks.
Data on variation in relative risk by age are sparse. The American Cancer Society's prospective cohort study, the Cancer Prevention Study (CPS-II)—the sole source of data for tobacco deaths—used only two age stratifications. The results diverge with those of the British Doctors Study, for which 50-year follow-up data have recently been published (Doll et al. 2004). The British study found that the overall relative risk for lung cancer was 15.9—lower than that found in CPS-II. Importantly, what appears to be driving the lower relative risk in the British study are 218 lung cancer deaths in men under age 64. Could this finding be a cohort effect, or something else, rather than a true age effect? We do not know, as we are short on statistical power when relying solely on CPS-II. With the launch of CPS-III, estimates will become more reliable.
There also is evidence that as life expectancy rises, the proportion of tobacco deaths increases among the oldest study subjects (after age 80). However, hardly any epidemiological baseline data on this age group are available. Is it premature to generate relative risk estimates for this age group, especially considering that, as the age of death rises, the accuracy of death certificates likely declines? This age group has multiple chronic conditions, yet no data have been published on the accuracy of death classifications.
Is it appropriate to rely on CPS-II as a single data source? This dataset has been extrapolated to many countries besides the United States (Peto, Lopez et al 1994). However, it may underestimate variability in underlying relative risk. The Canadian Center on Substance Abuse—using meta-analysis to identify relative risks from tobacco and illicit drug use—obtained lower relative risk estimates for lung cancer, chronic obstructive pulmonary disease, and ischemic heart disease. The overall number of smoking-related deaths in the Canadian study was 15 percent lower than that estimated by CPS-II. For lung cancer alone, the Canadian meta-analysis combined 11 studies, including CPS-II. That analysis found an overall relative risk of 30 for current smoking, compared with 23 from CPS-II. The relative risk for women was also different, with the Canadian study reporting a relative risk of 11.4, compared with 12.7 from CPS-II.
What is not yet clear is whether these differences are cohort effects. Did the Canadians mix cohorts of different ages with different levels of maturity in the smoking epidemic? If the latter, the estimates would not apply to the current U.S. generation. Nevertheless, the Canadian study found tobacco the leading cause of preventable mortality. That is the message that we should emphasize to the public, rather than differences in study methodology.
Another key public message is the uncertainty in our estimates. Michael J. McGinnis illustrated that concept nicely when he discussed the rounding rules that he and his co-author devised for their 1993 study. Rounding is one way to deal with uncertainty, which we cannot avoid when estimating preventable deaths. But all in all, methodological issues—while important for refining estimates—are not likely to affect the fundamental public health message that smoking and obesity are major causes of preventable morbidity and mortality.
Obesity, Weight Loss, and Mortality
Presenter: Dr. David Allison
This presentation covers the relationship between body mass index (BMI) and mortality, the relationship between body composition and BMI, the effects of weight loss, and methodological issues.
The relationship between BMI and mortality depends on population, age, gender, ethnicity, and other factors. But, overall, the relationship appears to resemble a J-shaped curve, as analyzed in a meta-analysis by Troiano and colleagues (1996; see also Figure 5). The probability of death is elevated at both ends of the BMI spectrum, yet more so at the high end (BMI >29). The mortality association at low BMI is controversial, for it could be true causation or an artifact. Because illness makes people lose weight and also makes people die earlier, the confounding effects of illness could explain the apparent relationship between low BMI and mortality to some extent. But there is also some biological plausibility for thinness as a risk factor.
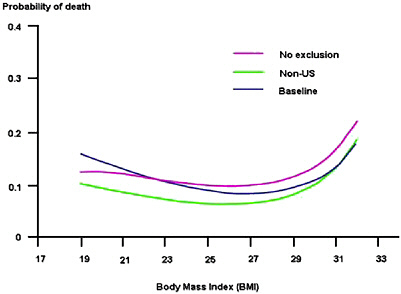
FIGURE 5 Body Mass Index and Probability of Death
SOURCE: Troiano et al. 1996.
Osteoporosis and hip fractures in the elderly can lead to mortality. Being thin is a very plausible biological risk factor that predisposes an individual with osteoporosis to hip fractures and death. Smoking is an unlikely explanation for the low-BMI–mortality association, based on a meta-
analysis published in the American Journal of Epidemiology (BMI in Diverse Populations Collaborative Group 1999—see citation at end). It is unclear whether confounding by preexisting occult disease accounts for the relationship between low BMI and mortality (Allison et al. 1999). As discussed later, I believe the BMI-mortality association is likely to be, in part, an artifact of the fact the BMI is composed of the sum of fat mass divided by the square of height and fat-free mass divided by the square of height (Allison et al., 19975), and direct measures of adiposity should be used in future research.
There clearly is a ‘moderating’ association between age and the association of BMI on mortality (see Figure 6, adapted from Andres et al. 1985). How does BMI interact with age to influence the risk of death? The extent to which age is an effect modifier, a confounder, or both is still an open question.
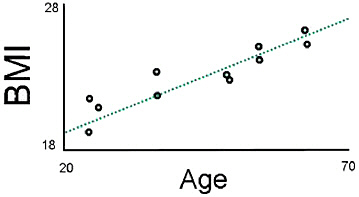
FIGURE 6 The association of Age with the BMI Associated with Lowest Mortality Rate
SOURCE: Andres et al. 1985.
The impact of BMI also can be studied in relation to other endpoints related to mortality. Our findings in white males show a linear relationship between BMI and expected years of life lost (YLLs), such that as BMI increases, so do YLLs (Fontaine et al. 2003). The effect in white males appear more pronounced than in other demographic groups. Obesity-associated YLLs are greatest among younger people with obesity. Several recent studies have also examined the direct healthcare costs of obesity (Allison et al. 1999; Wolfe and Colditz et al. 1998; Wee et al. 2005), quality of life, socioeconomic effects, and morbidity – all of which need to be considered when assessing the total burden of obesity.
Researchers have studied body composition to determine whether they could parse the association between BMI and mortality into opposing effects of body fat and fat-free mass. Studying a large Danish cohort, Bigaard and colleagues (2004) found the familiar J-shaped curve when focusing solely on BMI in relation to mortality. When they looked at body composition (via body fat or fat-free mass), they found the same shape of curve, but it was not as pronounced with the nadir coming at earlier ages (see Figure 7). Analysts need to start retreating from relying solely on BMI, if possible, as is unfolding in NHANES IV.
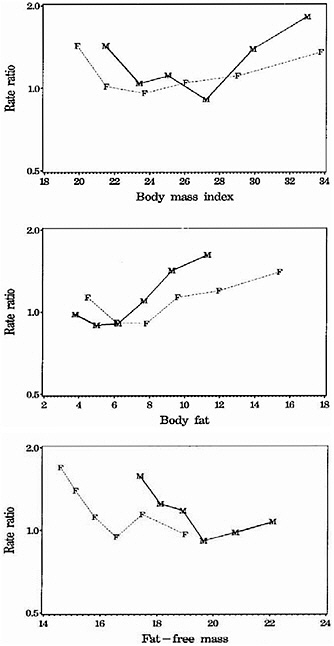
FIGURE 7 The Association between BMI and Mortality, BFMI and Mortality, and FFMI and Mortality, Adjusted for smoking (BFMI and FFMI Mutually Adjusted).
SOURCE: The Danish Diet, Cancer, and Health Study, 1993–2001 (Bigaard et. al. 2004).
NOTE: The vertical axis is logarithmic, and data are illustrated from the 5th to the 95th percentiles (F, females; M, males). BFMI = body fat mass index; FFMI = fat-free mass index.
Despite the enormous social significance, the effects of weight loss on mortality have not been well studied. We have just published findings from obese rats randomized to lose weight or not to lose weight (Vasselli et al., 20056). Regardless of diet type, animals lived substantially longer if they lost weight. Some non-randomized clinical trials in humans also have found that gastric bypass surgery lowers mortality (Christou et al. 2004; Flum and Dellinger 2004). We have found that fat loss conditional on weight loss among non-severely obese people is associated with reduced mortality rate, whereas weight loss conditional on fat loss is associated with greater mortality rate (Allison et al. 1999).
The field faces several key methodological and conceptual issues. How do we best model hazard ratios as a function of BMI? How do we quantify uncertainty due to sampling? How do we account for model uncertainty? On what samples should we be deriving hazard ratios? How do we best incorporate adiposity values throughout the lifetime as opposed to at a single point in time? How and when can we start using body composition in calculating attributable mortality?
Physical Activity
Presenter: Dr. Steven Blair
Calculations of attributable risk fractions have often ignored physical activity. Analysts have used obesity as a surrogate marker for physical activity or diet, largely for ease of data collection by states, but without an understanding of its empirical relationship to physical activity and diet. The assumption is that obesity accounts for the mortality impact of poor diet and physical activity, but that assumption has not been adequately tested and is unlikely to be true. Physical activity and diet should be measured directly to calculate attributable risk fractions. Using obesity as a surrogate for the behaviors of physical activity and diet confuses the issue.
Obesity is the result of a persistent positive balance where energy intake exceeds energy expenditure. The obesity epidemic is driven, in my view, more by decreases in average daily energy expenditure than by increases in average daily energy intake. Unfortunately we do not have data on average daily energy expenditure or on changes in this variable, and the data we have on average daily energy intake are questionable. Therefore the fundamental cause of the increases in obesity prevalence observed over the past several years cannot be determined.
Physical activity is a complex and repetitive behavior that is difficult to assess validly. When self-report measures assess physical activity with reasonable precision, or when objective measures of cardiorespiratory fitness are used (such as a maximal exercise test), the attributable fraction of deaths is substantial. A study of Harvard alumni found that inactivity accounted for 16.1 percent of all-cause mortality (Sesso et al. 2000). Similarly, a study of Finnish men found the attributable fraction 15 percent (Haapanen et al. 1997). Many large observational studies show an association between low fitness levels and mortality. What is lacking are randomized, controlled trials in humans showing greater longevity as a result of exercise, but of course such data also are not available for obesity.
My group has collected data on cardiorespiratory fitness, physical inactivity, and BMI as part of a large prospective observational study of patients examined at the Cooper Clinic in Dallas. The Aerobics Center Longitudinal Study (ACLS) has enrolled more than 80,000 patients since 1970. Mortality surveillance, which is current through 1998, revealed 4,100 deaths, mostly in men. One limitation of the ACLS dataset is that participants are not representative of the U.S. population; most are well-educated, non-Hispanic whites.
Our recent unpublished data reveal that a greater fraction of deaths are attributable to low cardiorespiratory fitness than to inactivity. In men, 9.1 percent of deaths are attributable to inactivity, while 17.6 percent are attributable to low cardiorespiratory fitness (using the maximal exercise test). The attributable fractions in women are somewhat lower, although their relatively few deaths limit the utility of the findings. The fraction of deaths in women attributable to inactivity
is 2.6 percent, while the fraction attributable to low cardiorespiratory fitness is 12.1 percent. There appears to be a gender difference that is particularly strong for inactivity. However, the apparent gender difference may be due to few female deaths or limitations in the physical activity measures. Questionnaires tend not to measure housework and child care activities, for example.
Our unpublished calculation of hazard ratios for overweight or obesity dropped substantially after we adjusted for cardiorespiratory fitness. But the hazard ratios for low cardiorespiratory fitness changed little after we adjusted for overweight or obesity. Cardiorespiratory fitness provides an objective measure that is preferable to overweight/obesity for calculating attributable mortality.
Assessing the Effects of Multiple Public Health Interventions
Presenter: Dr. James Robins
Estimating the effect of interventions is the essence of causal analysis. Philosophically the goal is to compare events as they actually unfold to what would have happened in a counterfactual world where we had intervened. The overall goal is to predict what would happen if we were to intervene in the future. A step on the way to this goal would be to calculate the difference in the observed event rates to the rates that would have existed in a counterfactual world where we had intervened. In principle, we can make calculations of this sort by randomly assigning interventions (including when the interventions occur), and then comparing two population samples: those with and those without the interventions. This ideal experiment does not require assumptions, but it does require an impossibly large sample size to consider a reasonable number of risk factors and possible interventions.
Even if a trial could precisely estimate the impact of an intervention on U.S. mortality from 1983 to 2003, it would provide no direct evidence concerning the exact same intervention beginning in 2003 or 2013. Nor would that trial provide accurate estimates of the effect of a similar intervention on a population that differs from the U.S. population on both measured and unmeasured determinants of mortality, including smoking, cholesterol, high blood pressure, lifestyle patterns, and access to healthcare.
Another problem is that calculations of attributable risk often do not carefully define the intervention under consideration. For example, a simple assertion about the effect of changing the concentration of low-density lipoprotein in the blood implicitly, but perhaps incorrectly, assumes that the way it is changed (such as through drugs or diet) does not matter.
Age is an even more complicated factor, and not just as a confounder as attributable fraction calculations typically assume. If an intervention saves someone’s life today, that person will be a day older and at risk of dying tomorrow. Another way to put it is that because we all eventually die, the attributable fraction for any given exposure over 120 years must be zero.
Statistical models that extrapolate beyond the observed data are needed to actually make estimates, and this introduces the possibility of bias stemming from model misspecification and other problems. Many analysts assume, for instance, that studies can adjust for confounders. However, even in the unlikely event that a study measured all possible confounders, there would not
be enough data to discriminate among multivariate models that fit the data equally well but that produce different estimates of the intervention’s effect.
Our calculations based on the Framingham offspring cohort study provide an application of these ideas. That study examined 5,124 subjects at 4 year intervals over 20 years. Coronary heart disease (CHD) was the primary outcome variable, and the study measured and examined the effect of a variety of common risk factors, although information on dietary fat intake was not available. A Monte Carlo simulation estimated the proportion of people who would develop CHD under each intervention—wherein the joint distribution of CHD and the risk factors roughly equals the joint distribution implied by the parametric g-formula.7 The results obtained are only valid under the assumptions of correct model specification and of no unmeasured confounding factors. A typical result is that the 20-year risk of CHD would drop 8.46–7.65 percent if 50 percent of smokers quit smoking at baseline. These results are limited, however, by the unavailability of data on relevant confounders and the small number of CHD events, especially for women. The possibility of model misspecification is also a concern because of sensitivity of the parametric g-formula results to the choice of specification.
Discussion of Attributable Risk in Practice: Examples from the Field
Discussants voiced the following points:
-
Researchers have devoted inadequate attention to measuring high-fat diets and high sulfide levels. These two are the fundamental causes of cardiovascular disease.
-
When reporting PAF, studies should provide intervals instead of rounded point estimates, and should not rank lifestyle factors. Authors should not report their best guess if they think it is very imprecise.
-
CDC needs to stratify on age when calculating PAFs for obesity. Without this stratification, obesity estimates have about a 30 percent error. According to Dr. Husten's presentation, using all-cause mortality—rather than age stratified by causes of mortality—inflates smoking estimates by 50 percent.
-
Age stratification is possible given access to raw data such as from NHANES, but not if analysts are relying on relative risks from the peer-reviewed literature. CDC stratified where it could, and used age-adjusted estimates where available.
-
Deaths related to alcohol should not be characterized as from alcohol abuse. CDC’s choice of excessive drinking instead of alcohol abuse—which is a diagnosis from the Diagnostic and Statistical Manual of Mental Disorders IV (DSM-IV)—was deliberate: the agency was trying to capture deaths that result from too much drinking. The most common pattern of excessive drinking is episodic intoxication. Individuals who drink heavily and regularly may or may not meet the criteria for a DSM-IV–diagnosable condition related to alcohol. In fact, work in some states shows that people with alcohol diagnoses are a relatively small proportion of excessive drinkers.
-
What is the future of using observational data to understand the impact of interventions? Dr Robbins’s presentation seemed bleak in suggesting that scientists should devote all their resources to experimental data instead of observational data.
-
Ultimately, the answer is empirical. We need many observational analyses done well, as well as many randomized trials. Comparing results of the two types of studies will allow us to understand the value of observational data.
-
We need a theory about why the relative risk relationship changes with age, to determine the best methodology to apply to age stratification. One example concerns cholesterol and age: the importance of cholesterol as a risk factor declines with age. This finding led the field to question whether cholesterol-reducing interventions would be less effective in the elderly. Intervention trials showed that was not the case, suggesting instead that confounding was responsible for the declining importance of cholesterol with age. So before we change the relative risk of obesity with age, we need to better understand what is occurring.
ALTERNATIVE METRICS OF BURDEN
Analysts in the fields of economics, public health, medicine, and health policy commonly use several metrics of disease burden in addition to mortality. These include quality-adjusted life years, years of healthy life, and disability-adjusted life years. In different ways, these metrics merge estimates of life expectancy with morbidity measures of quality of life for a given disease or disease groupings. This portion of the workshop addresses these metrics: their applications, benefits, and limitations for measuring disease burden from lifestyle-related factors.
Quality-Adjusted Life Years (QALYs)
Presenter: Dr. Allison B. Rosen
Quality-adjusted life years, or QALYs, are commonly used for economic assessments of medical interventions, but they can also provide comparative information on which of many interventions produce the greatest public health gains for the resources expended. Unlike earlier metrics—such as events averted—QALYs allow for comparisons across different interventions and different diseases by capturing morbidity and mortality in a single common metric. While the U.S. Public Health Service’s Panel on Cost-Effectiveness recommends QALYs for use in the denominator, or benefit, of cost-effectiveness analyses, QALYs also have inherent appeal for measuring and tracking disease burden, particularly when diseases have a marked impact on quality of life, as with obesity and other lifestyle-related health conditions.
QALYs represent the benefit of a health intervention in terms of time spent in a series of quality-weighted health states, in which the quality weights reflect the desirability of living in that health state. These states range from perfect health (weighted at 1.0) to death (weighted at 0) (see Figure 8). Once the quality weights—or utilities—for each health state are obtained, they are multiplied by the time spent in each state, and the products are then summed to obtain the total number of QALYs.
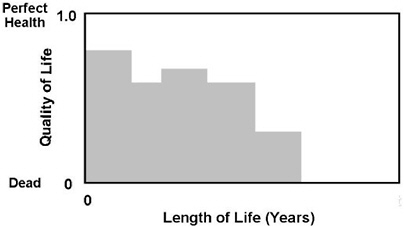
FIGURE 8 QALY Calculation
QALYs require knowledge about life expectancy and health-related quality of life (HRQOL), yet, there is a lack of consensus on the best methods to assess the latter. HRQOL has two components: a description of the health state or its associated health status, and an assessment of preference for that health state. HRQOL can be assessed using preference-based methods (in which preferences for health states are elicited directly) or non-preference-based methods (in which health status is directly assessed but pre-existing preference weights are applied to the measured health status).
Preference-based assessments commonly employ standard gamble, time tradeoff, or rating scale methods. The first two involve explicit choices, while rating scales do not. In the standard gamble, the respondent is asked to compare life in a suboptimal health state with a gamble between two alternate outcomes: perfect health or death. The probabilities are varied until the respondent is indifferent between the suboptimal health state and the gamble. In the time tradeoff, the respondent is asked to choose between life in a suboptimal health state for a fixed amount of time, and life in perfect health for a shorter period of time. The life expectancy in perfect health is varied until the respondent is indifferent. These indifference points are then used to calculate utilities for the suboptimal health state. While different methods may yield different utilities, compared to standard gamble, the time tradeoff has been found relatively valid, whereas rating scales, while easy to use, have been found more subject to measurement bias.
Non-preference-based instruments, which directly measure respondents’ health status and then apply pre-existing preference weights, include the Health Utilities Index (HUI), Quality of Well-Being Scale (QWB), EuroQOL (EQ-5D), Health and Activities Limitation Index (HALex) and others. These instruments differ in how they define the relevant domains of health, as well as the techniques and the source population (often non-U.S.) used to obtain preference weights. Additionally, sizable differences have been reported in the preferences obtained from different non-preference based instruments, and in the preferences obtained using non-preference-based compared to preference-based assessments.
Regardless of the assessment method, preferences may differ depending on the source population they are elicited from. The U.S. Public Health Service's Panel on Cost-Effectiveness recommends that community members designate preferences, while others advocate for patient preferences. For burden of disease studies, community preferences collected by means of our national surveys are appealing because they provide both community preferences and, when subset into respondents with the condition of interest, patient preferences as well.
Two alternatives to QALYs merit mention: disability-adjusted life years (DALYs), and years of healthy life (YHLs). The former incorporates years of life lost and years lived with disability into a common metric, with the disability weights determined by an expert panel. The latter integrates life years with quality weights obtained by maximizing the correlation between the two health domains (activity limitations and self-perceived health) measured by the HALex. While the HALex is attractive because of its ease of collection (e.g., through CDC’s National Health Interview Survey), its sensitivity to changes in health across a broad spectrum of diseases and population subgroups has yet to be explored.
QALYs are an appealing measure of disease burden for national efforts to measure the impact of lifestyle-related factors on morbidity and mortality. They are the recommended health metric for reporting the cost-effectiveness of interventions. They incorporate patient preferences, which are critical in moving toward patient-centered valuations of health and healthcare. Community preferences, however, are likely the most appropriate for calculating QALYs used to track population health. While many national surveys are starting to collect data for preference-weighted measures of health status, most efforts have focused on measuring changes in health status and then applying preexisting preferences. Because there is no clear reason to believe that preferences for health states are static, it may be time for national surveys to also include a direct preference-based measure, such as the time-tradeoff. This may allow for comparison of the performance of various measures over time for different diseases and different population subgroups.
Comparative Risk Assessment (DALYS)
Presenter: Dr. Christopher Murray*
In 1999, the World Health Organization (WHO) launched a comparative risk assessment of 25 leading risk factors worldwide. In a series of analyses, the Comparative Risk Assessment Collaborating Group measured disease burden and mortality attributable to the 25 risk factors. Those factors included high body mass index (BMI), cholesterol level, physical inactivity, and related indicators of diet or inactivity (Ezzati et al. 2002).8 We focused on 14 epidemiological subregions of the world.
To measure disease burden, we used the common metric disability-adjusted life years, or DALYs. DALYs refer to years of healthy life lost to premature death or disability, and allow analysts to compare burden across diseases. Efforts to calculate DALYs for any given condition rely
on severity weights preassigned by experts.9 The ultimate goal of the WHO undertaking was to help nations target their resources to addressing the foremost modifiable risks to public health.
Our group based its selection of risk factors on several criteria: they had to be among the leading causes of disease burden, not too specific or too broad, causally related to disability or death, and potentially modifiable, with reasonably complete data. To obtain data on the prevalence of exposure to the risk factor, we systematically assessed all available sources, including household surveys, consumption data, community studies, and others. Our sources for prevalence of high BMI and related measures were many of the same large cohort studies used in CDC’s analysis. However, there were methodological differences in how we adjusted for interrelated risk factors and bias in self-reporting BMI, and in how we corrected relative risks for errors in variables or regression dilution bias. We did not see much difference in our results when we used different population-based preference measures. What actually did make a difference was analyzing the impact of death versus years of life lost, and incorporating nonfatal health outcomes.
The attributable disease burden of 20 risk factors—measured as percent of global DALYs—shows that the leading risk factor in the developing world is underweight (see Figure 9). The findings for most of the United States and Canada show that high BMI is the fourth leading risk factor for death, and that it moves up to third when we analyze for disability (see Figures 10 and 11). We are now working on the analysis of NHANES IV. In all likelihood, the use of DALYs will lead to greater societal impact for BMI.
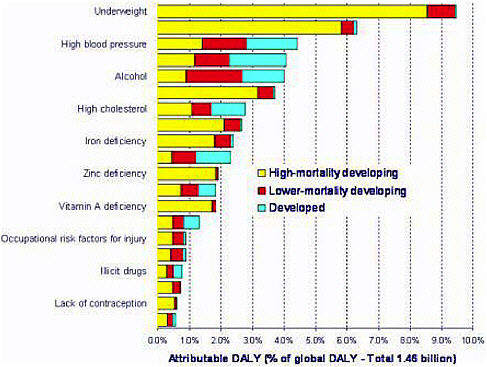
FIGURE 9 Attributable Disease Burden of 20 Risk Factors
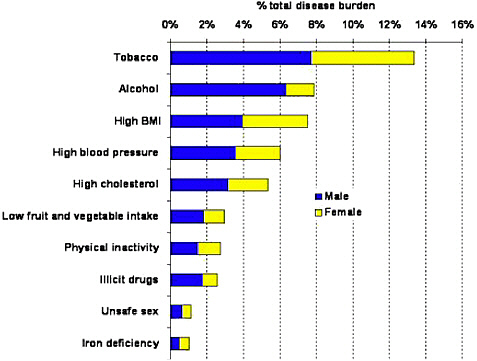
FIGURE 11 Disease Burden in AMR-A Region. The region includes Canada, United States, and Cuba; the US population represents 85% of the region.
HALYs: Measuring Lifestyle-Related Factors that contribute to Premature Death and Disabililty.
Presenter: Dr. Marthe Gold
This presentation explores the benefits of using health-adjusted life years (HALYs) to promote understanding of disease burden for public health policymaking. It also discusses the differences between two specific types of HALYs: QALYs and DALYs.
Because they combine mortality and morbidity into one measure, HALYs provide a more comprehensive picture of disease burden. A 1998 IOM report concluded, “Mortality measures, although important, provide incomplete and insensitive information for decision making” (IOM 1998). Focusing solely on mortality is neither humane—because it neglects the large morbidity burden on individuals and their caretakers—nor pragmatic, because a growing segment of healthcare expenditures are devoted to morbid rather than mortal conditions. Growing reliance on HALYs recognizes that morbidity represents a large component of disease burden. Obesity, for example, exacts a high morbidity toll from chronic, disabling conditions such as diabetes mellitus, hypertension, osteoarthritis, and depression.
Summary measures of population health—HALYs—are increasingly relevant to public health and medical decision making. These summary measures are used to capture trends in population health, make informed decisions about alternative uses of healthcare dollars, and assess the cost-effectiveness of alternative health services and technologies.
Although both QALYs and DALYs can be used in a number of similar decision making contexts, they come from different traditions and one measure may be preferable to the other in
particular settings. QALYs were developed in the late 1960s by economists to measure the benefits of a medical or clinical intervention. QALYs are often seen as a good to be maximized. DALYs, on the other hand, can be seen as capturing gaps in healthcare and the ensuing disability. For example, WHO uses DALYs to measure the global burden of disease, whereas the U.S. Public Health Service’s Healthy People 2010 uses QALYs to measure success in meeting prevention goals.
QALYs are composed of descriptive health states, not diseases, and thus can capture co-morbidity—such as diabetes, angina, and obesity occurring together—and its impact on health quality. DALYs, in contrast, are tied to the individual diseases listed by WHO in its International Classification of Diseases. QALYs and DALYs diverge in other ways, including whether individuals or communities are stating their preferences, and what types of weighting systems apply.
Different weighting systems generate different results. For example, the standard gamble technique used for QALYs generally gives the highest figure, because people are less likely to gamble away to death. The time tradeoff technique yields a somewhat lower figure, while the rating scale tends yield an even lower figure. There is no consensus about which method is best. However, large-scale efforts are under way by Dennis Fryback and collaborators—with funding from the National Institute of Aging—to determine how separate HALY measures relate (e.g., interrelationships between the Health Utilities Index, the EuroQol instrument, and the Quality of Well-Being Scale). Peter Franks has found that the measures are highly correlated (Franks et al. 2004), while a recent meta-analysis of quality-of-life measures for stroke (severe, moderate, and mild) also found significantly high correlations. The latter study concluded that differences between measures relate mostly to scaling, rather than what is being measured (Tengs and Lin 2004).
Researchers are now pursuing several recommendations from IOM's 19 98 report, including gathering information on multiple summary measures in population datasets, conducting crosswalks between measures, and comparing differences in weights across populations. The most important recommendations remaining include examining how well particular measures serve different local, national, and international purposes; linking information on population health to risk factors to generate epidemiological insights; and testing measures to develop an empirical base on the distributive implications of different measures for reducing health disparities.
A measurement system that integrates the outputs of public health efforts and medical care would be ideal, as would linking health measures to specific risks and interventions, as has been done by Michael Wolfson and colleagues at Statistics Canada. Statistics Canada has incorporated the Health Utilities Index in its datasets. CDC leadership is needed to encourage similar integrative functions in the United States, and to ensure that measures capture both morbidity and mortality.
Estimating National and State Medical Costs from Select Risk Factors
Presenter: Dr. Erik Finkelstein
Cost estimates add to our understanding of the societal burden of lifestyle-related risk factors. Going a step beyond mortality and morbidity, such estimates not only quantify total costs but also show how they are apportioned and who pays for them—whether individuals, families,
private health insurers, governments, or society. Cost estimates provide information that policymakers can use to decide how to spend scarce healthcare resources.
Cost estimates also have other benefits: they spur public awareness of a particular public health problem, help set research priorities, and are a crucial first step in valuing interventions.
Costs can be apportioned into short- and long-term medical costs and total lifetime costs—the value of lost wages from absenteeism and early mortality. The financial impact of gunshot injuries illustrates the distinction between medical costs and total lifetime costs. Our analysis for CDC revealed that these injuries represented only 2 percent of the total medical cost of injuries. However, that fraction jumped to 9 percent when we looked at lifetime costs, because these injuries strike young people before they reach their prime earning potential.
The advantage of apportioning payers becomes apparent in considering obesity. My work on the cost of obesity found that the government was paying about half the costs (Finkelstein et al. 2003). That awareness can help spur policymakers to find ways to reduce the costs.
Two approaches to estimating medical and other costs attributable to select risk factors are common: the epidemiologic approach, and the econometric approach. This presentation compares their advantages and disadvantages.
The epidemiological approach is straightforward: it apportions a fraction of the cost of disease to the risk factor by multiplying the PAF by the corresponding disease cost. For obesity, this involves summing the costs from several diseases. The results are subject to the same caveats that apply to estimations of PAF. An additional caveat is that the epidemiological approach to cost valuation assumes that if X percent of the disease is attributable to a risk factor, then X of the disease costs are also attributable to the risk factor. That would not hold if treatment decisions and efficacy vary based on the presence of the risk factor. For example, treatment outcomes for diabetes are likely to differ between obese and non-obese individuals, with the average cost for obese people being substantially greater. Another caveat is that accurate estimates of the cost of disease may be unavailable, or may not be available at the right stratifications (e.g., national versus state level).
The econometric approach begins with this logic: if the only difference between two groups of people is the presence or absence of the risk factor, then the difference in costs is due to the risk factor. It uses regression analysis to quantify cost (direct or indirect) while controlling, to the extent possible, for other observable characteristics that are likely to affect costs and be correlated with the risk factor. A simplified version of the regression equation used to estimate attributable cost based on person-level data is as follows:
Costsi = β0 + β1*rf1 + β2*rf2 + … +βi *rfi *γ'Xi + ei
Where β1 represents the increase in costs associated with risk factor i (rfi) (e.g., obesity, smoking)
The dependent variable is equal to each individual’s costs over a given time period, typically a year. This is the approach we used to estimate annual medical costs of obesity at the state and national level (Finkelstein et al. 2003). It relied on the Medical Expenditure Panel Survey/National Health Interview Survey 5 for modeling national medical costs, and modeled state costs using a
combination of the Medical Expenditure Panel Survey/National Health Interview Survey and the Behavioral Risk Factor Surveillance System.
The econometric approach differs from the epidemiologic approach in a number of ways. It does not require identifying diseases influenced by the risk factor, and it allows for modeling multiple risk factors in a single equation while controlling for covariates (e.g., age, gender, education). The econometric approach also allows for flexibility in the modeling and for computing cost by payer, and it avoids double-counting costs across risk factors (if the model includes them). The econometric approach further avoids double-counting costs across risk factors.
Which approach is better—the econometric approach or the epidemiological approach? The choice likely depends on the risk factor and question being addressed. For obesity, both approaches produce similar estimates (with obesity accounting for about 6 percent of national medical expenditures). The econometric approach easily quantifies external costs. It may be more accurate once obesity treatment becomes more common (costs in the absence of disease). The epidemiologic approach likely produces more accurate estimates for physical activity. For poor diet, the current data may too limited. A potential strategy for improving the estimates is to add questions on risk factor history to the Medical Expenditure Panel Survey/National Health Interview Survey.
Using Population Attributable Risk Estimates to Allocate Resources
Presenter: Dr. Louise Russell
Public policy entails making tradeoffs between numerous health problems and many potential interventions. An enduring problem facing policymakers is how to allocate available resources to achieve the greatest health benefits. Cost- effectiveness analysis strives to provide information that can help policymakers weigh alternative interventions (Russell et al. 1996).
PAF factors in as a key ingredient of cost-effectiveness analysis. PAF indicates the magnitude of the problem, who suffers from the problem, and a sense of proportionality—how the problem compares with other health problems. PAF is essential to calculating the health benefits of a given intervention once it is combined with data on the effectiveness of the intervention, according to a simple formula. This formula answers the question: how much of the problem can the intervention actually prevent or cure?:
Health Effects of an Intervention = Magnitude of the Problem (PAF) x Effectiveness of the Intervention
To determine the cost of an intervention, it is essential to quantify how many people are affected and the resources needed per person (including costs outside the health system). Efforts to change lifestyles not only cost money in the medical sector but also cost individuals in terms of food purchases, exercise centers and programs, and their time. Focusing on the medical sector and savings to health insurers from an intervention often obscures a shift in costs to the consumer. Any cost-effectiveness analysis needs to factor in cost shifts and hidden costs.
Measurements of the cost-effectiveness of an intervention usually rely on a ratio, such as dollars per life-year, or dollars per quality-adjusted life-year. The analysis typically entails
comparing the cost-effectiveness of two different interventions, or two variants of a given intervention (such as screening every three years versus screening every year).
One way to report cost-effectiveness is by examining the number of life-years gained with $1 million expended on an intervention (see Table 2). Influenza vaccine for people 65 and older is easily the most effective use of resources among interventions listed in the table, yielding almost 8,000 life-years per $1 million spent. Smoking cessation programs are the next most effective use of health resources. Tetanus boosters every 10 years are a relatively ineffective use of resources, yielding 4 life-years per $1 million.
TABLE 2 Life-Years per $1 Million (1997 dollars)
|
Antihypertensive medication, US population |
|
|
Propranolol |
51 |
|
Captopril |
8 |
|
Influenza vaccine, persons 65+ |
7,750 |
|
Tetanus booster every 10 years |
4 |
|
Lovastatin 20mg/d, primary prevention in men, cholesterol 300+ |
|
|
55-64, smoker, DBP 105+, 30%+ overweight |
42 |
|
35-44, nonsmoker, DBP <95, <10% overweight |
2 |
|
Smoking cessation programs |
217 |
|
SOURCE: L. Russell, paper prepared for the Committee on Health and Behavior: Research, Practice, and Policy, Institute of Medicine, October 1999. |
|
The main point of cost-effectiveness analysis is that good use of resources depends not only on the size of the problem but also on the interventions available, how effective those interventions are, and the cost of those interventions (including in terms of people's time and attention). Cost-effectiveness analysis allows policymakers to ask about opportunity costs—namely, whether society can do better by spending resources another way. An opportunity cost refers to the fact that when policymakers make one choice, they must forego another. To make the best choice, policymakers should give up as little as possible. They need to choose the interventions that will exert the greatest impact. And if they must leave something out, choose an intervention that does the least.
Discussion of Alternative Metrics of Burden
Discussants voiced the following points:
-
Calculating costs is often difficult because they vary so much. For example, the price of a drug may range from the average wholesale price, to the price for the Veterans Administration, to the retail price. Tracking costs not paid for with a check is even more difficult.
-
Analysts need to avoid creating a false dichotomy between the size of a public health problem (e.g., as represented by PAF) and the costs and consequences of different interventions, because both are important.
-
PAF is a good place to start because it conveys the size of a problem, but it does not tell policymakers what to do and how many resources they need to modify the risk. Even if scientists and policymakers don’t perform a cost-effectiveness analysis for a given intervention, they must make some kind of comparison.
-
The traditional economics approach to cost-effectiveness analysis—which values people's health according to how much they work—overlooks people’s other contributions, such as in education, childcare, and elder care. A “health effect” measure implicitly covers all of these.
-
Society devotes too little attention to the cost-effectiveness of policy interventions as opposed to the cost-effectiveness of clinical interventions.
-
The figure given for the cost to U.S. society of obesity is estimated at $90 billion per year—which implies that interventions could save $90 billion. However, policy analysts do not seem to have examined the cost-effectiveness of interventions for obesity, and people do not think about costs very soberly.
-
PAFs are better than other measures of disease burden, such as years of life lost and QALYs, because analysts have produced them with much rigor and attention to confounding for many years. Why are we spending all our resources to compute PAFs, and then discard them when we calculate the cost-effectiveness of interventions?
-
Efforts to calculate the benefits of interventions do not discard PAFs—they rely on the same underlying value systems to answer different questions.
-
This workshop aims to address two issues: how best to estimate PAF, and the effectiveness or cost-effectiveness of an intervention. Some may argue that there is no point in calculating PAF if there is no intervention. However, calculating PAF draws attention to a problem and spurs interest in developing interventions.
-
Decisions to adopt policies are not limited to economic costs and social benefits. Rather, such decisions are also based on the business case—an area that is often overlooked.
-
Legislatures seem to care more about short-term rather than long-term costs and benefits. Thus while comprehensive analyses are important, legislators also need narrow estimates. One group at UCSF found, through cost-effectiveness analysis, that policies promoting clean indoor air and smoke-free environments were an order of magnitude cheaper than providing direct clinical services for smoking cessation. This work is in press.
PUBLIC POLICY ISSUES
General Public Policy Issues
Presenter: Dr. Nicole Lurie
The primary focus of this meeting—the measurement and methodology of PAF related to obesity—is important. However, methodological issues have become a smokescreen for several other concerns.
The first is that we should not be pitting obesity against tobacco in terms of prevention. The broader point is that this country invests too little in preventing both these major public health problems. We also hold the false notion that better precision in estimating PAF will erase cynicism about the value of public health interventions. No matter how perfect our methods of measuring the
burden of disease, social criticism is sure to ensue. The focus on methodological problems has also obscured fundamental questions about the roles, rights, and responsibilities of individuals versus governments.
We also need to consider how to extend the precautionary principle to lifestyle interventions. This principle generally holds that scientific uncertainty should not be an excuse to postpone preventive measures for serious or irreversible public health threats. Failure to apply the precautionary principle has come back to haunt us with clearly identifiable diseases such as HIV and Creutzfeldt-Jakob disease. Applying the precautionary principle to lifestyle interventions to combat problems such as smoking and obesity is much more difficult. The harm is indirect—it's harder to see, name, and count individuals, and the social redress for dealing with those failures is very different from that for failing to screen blood, for example. Legal remedies are also very different.
We also need to invest in data and data systems. We can't answer the kinds of questions we wish to answer without continuously better data, more research and development, and better methods of analysis. Better data systems will also enable states to tackle public health problems within their borders.
Efforts to translate and communicate scientific findings are also challenging. The meaning and public health implications of concepts related to populations as opposed to individuals, such as QALYs, DALYs, are hard to grasp.
We also need to clarify the business case for interventions—the return on investment. Return on investment can accrue to individuals, the healthcare system, or the broader society. Failure to take action also manifests itself in many ways, particularly in terms of Medicare and Medicaid expenditures.
The timeframe in which return on investment accrues is also important. We need to be thinking 30 years ahead, when Medicare costs will be so high that we will be unable to pay for our children’s education, even though such a timeframe poses a tremendous problem of accountability. Yet generating short-term improvements through lifestyle interventions that are cost-effective today is also essential.
State Policy Perspective
Presenter: Dr. George Benjamin
This presentation will offer the perspective of a former state health official regarding lifestyle and cause of death, address the value of data, and provide a real-life example.
Policymakers and the public do not fully understand the concept of lifestyle factors and mortality. The preventable components of disease are very complex. The public health establishment has failed to make the case for lifestyle causes of death in terms of measurable public health burden. We have also failed to give the public a sense of scale, comparing the national response to the handful of deaths caused by the anthrax attacks with the poor response to the
thousands killed each year by influenza virus. Attaching understandable numbers to a public health problem is essential to give the public a sense of its size and scope.
We have also failed to convey consistent messages. By emphasizing subtle differences in data and analysis (such as how obesity is measured), we confuse the public and make ourselves look less credible. We also make coherent discussions of the science and its implications for policy far more difficult.
Death is the ultimate discriminator: people understand what it means. Using mortality as the endpoint in PAF analyses is therefore valuable. The public does not understand complex measures such as years of productive life lost. We should generally choose a measure that is more explainable to the public. My experience with Maryland’s Department of Public Health illustrates the benefits of using PAFs to quantify lifestyle factors. A state or local health department is where the rubber meets the road. When I served in government, Maryland ranked second among states in cancer mortality, and the governor decided to take on tobacco and cancer. The state had received $4.5 billion from the tobacco settlement fund, and the governor decided to allocate $100 million annually to the health department over a 10-year period. We had to prioritize which cancers to target with this new funding, to ensure that our anti-cancer and anti-tobacco programs would address the top three or four major causes of death. CDC’s analysis of PAFs provided the rationale for targeting certain tobacco-related cancers rather than other cancers. We also used the CDC study to support our anti-tobacco media campaigns, which the legislature would not otherwise have supported through state funding.
Discussion of Public Policy and State Policy
Discussants voiced the following points:
-
Targeting our analysis to policymakers, particularly at the state level, is essential. Focusing on that intended audience will suggest what methodological tradeoffs epidemiologists need to make in calculating PAFs. For example, we need to supply state-specific prevalence estimates even if they are less precise than national estimates. We should also emphasize that different risk factors—such as obesity, alcohol, and tobacco—vary according to life stages, suggesting the need for age-specific interventions.
-
Promulgating the message that health policymaking should seek to reduce costs may be ill-advised because most efforts to improve health, in fact, increase costs. The critical message is to spend resources in ways that obtain maximal value. That is why cost-effectiveness modeling is so useful: it considers all interventions—treatment and prevention alike—within a similar metric.
Ethical Issues
Presenter: Dr. Daniel Wikler
Efforts to estimate the impact of lifestyle on morbidity and mortality raise several ethical issues. If we employ health measures that seek to incorporate social or ethical values, the extent of
lifestyle’s impact on health may be measured differently according to which values affect the weighting. Responsibility for health might be an example of these values.
Weighting outcomes: As an aid to health resource allocation, the QALY measure includes more information than life years, since quality of life is factored in. This, in turn, could be further adjusted in an attempt to reflect ethical values. For example, the World Health Organization not long ago counted health benefits or burdens befalling young adults as greater than those affecting the very young or old. The basis for this age weighting was a survey in which members of the public assigned greater importance to the health of young adults than to others (probably because they tend to have young dependents). The most natural interpretation of this practice is that the resulting measure (the DALY—disability-adjusted life year) represented both the burden that the symptom or disability placed on the individual and also the ethical or social importance of that person’s burden. It was a “moralized” summary measure of health. Similarly, Alan Williams, the health economist, believes that quality-adjusted life-years for those who have yet to live a normal lifespan should count more (the “fair innings” argument, which he attributes to the philosopher John Harris). In addition, the goal of narrowing disparities in healthy life expectancy might be served by increasing the weight given to health outcomes for those at the low end of the social health gradient. Any estimate of the impact of lifestyle on morbidity that is denominated in moralized QALYs is likely to reflect the weights that have been assigned to incorporate these and other values—as in a society in which the prevalence obesity is greater among the poor.
Responsibility for health: A question in “moralizing QALYs” is whether to adjust for personal responsibility. Should we count QALYs the same regardless of the role of the individual’s personal choices in bringing about their health deficit? Consider, for example, cosmetic surgery: A recent survey from Britain found that most people were willing to pay for removing birthmarks but not tattoos, even when they were equally disfiguring. Another study found that some Americans believe that alcoholics should be given lower priority for liver transplants.
Lifestyle decisions resulting in excess morbidity involve some combination of choice (responsibility) and circumstance (fate), and there is in most cases no objective way to estimate the ratio. John Roemer, an economist, suggests that the population be partitioned according to the sources of health behavior that are reckoned within that society to be beyond the individual’s control. Then, within each resulting group, those whose unhealthy behavior exceeds the median for the group should be held responsible for their choices to that extent. If steelworkers smoke more than mathematicians, for example, and if this reflects circumstances beyond the steelworkers’ control, it will still be true that some steelworkers smoke much more than others and thus, in Roemer’s view, can be held accountable for the excess.
Attributions of personal responsibility, however, are subject to highly tendentious arguments on behalf of special interests. Roger Scruton, a highly-regarded conservative British economist, published an essay (WHO, What, and Why?, 2000) that maintained that the World Health Organization had strayed from its mandate when it sought to curb the promotion of tobacco. For Scruton, an individual’s decision that the pleasures of tobacco use outweigh its threat to health is no business of WHO, which ought instead to focus its attention on communicable diseases that currently overwhelm the world’s poor. This argument, in effect, discounts health deficits stemming from tobacco use, on the grounds that the putative role of voluntary individual choice removes any resulting burden from the public agenda. Scruton’s credibility was shattered when it emerged that he was secretly on retainer to a tobacco company when he wrote this and other essays that pressed
this kind of argument. But the fact remains that his argument was calculated to minimize the significance attached to a category of “lifestyle”-connected health problems—evidence that this kind of claim has resonance among the public. Those concerned with the health impact of “lifestyle choices” cannot avoid the need to contend with its appeal and with the consequent possibility that some of our most pressing health problems will be drained of any sense of urgency. An adequate response requires both evidence on the mechanisms of unhealthy choices and a measure of moral argument that contests their significance for priorities in health policy.
Communication Challenges
Presenter: Dr. Katherine E. Rowan
Numerous communication challenges are inherent in media coverage of the debate over preventable causes of death. This presentation describes a few of these challenges and offers evidence-based steps for addressing them.
Major challenges associated with sharing science news through mass media include explaining scientific uncertainty to lay audiences; dealing with headlines written to emphasize controversy; earning trust from top science and medical reporters, and developing effective ways of explaining commonly misunderstood concepts such as risk factors, uncertainty, and obesity.
There are no magic words to address these challenges, but there is research-based guidance. The “CAUSE” model summarizes some of this research and gives practical tips on earning Confidence, creating Awareness, deepening Understanding, gaining Satisfaction, and motivating Enactment or behavior change when communicating about science and risk (e.g., Rowan et al., 2003).
The model’s analysis suggests that to increase the likelihood of careful news coverage concerning new scientific findings, scientists should identify journalists whose work they respect and invite coverage from these individuals. Communication officers at scientific institutions can facilitate this process. Additionally, in media interviews scientists should state their own values, emphasizing their concern for the public’s health and their respect for journalists’ abilities to increase attention to important topics. It is useful in such contexts to understand that scientific uncertainty may be read as incompetence by a lay audience.
To deepen lay understanding of complexities, scientists should be alert for key terms being used in media coverage of an issue that may not be understood as scientists intend them. For example, in the debate over preventable causes of death, the public should understand that experts in this debate are wrestling with the meaning of the term “obesity” and whether or not “obesity” or “poor dietary practices” are the root cause of preventable death. Another way to have a forum for explaining complexities is to volunteer to write “Sunday pieces” in major circulation newspapers. Sunday pieces are lengthy letters or columns written by experts on timely and important topics such as recent research on causes of preventable death. If coverage of important issues seems consistently poor, scientists can turn for assistance to groups that check the accuracy of reporting such as the Center for Media and Public Affairs. The Center for Media and Public Affairs conducts rapid quantitative assessments or content analyses of mass media news coverage on controversial topics.
In summary, there are no magic words to make communicating science through the mass media a simple process, but there are better and worse ways to proceed. Research on science and risk communication offers additional information on this topic. I am providing some additional references that may be helpful to you.
References and Additional Sources for Further Information
Bibliography on health risk communication available at http://www.nih.gov/pubs/cbm/health_risk_communication.html
Babrow, A. (2001). Uncertainty, value, communication, and problematic integration. Journal of Communication, 51, 553-573.
Booth-Butterfield, M. (2003). Embedded health behaviors from adolescence to adulthood: The impact of tobacco. Health Communication, 15, 171-184.
Brashers, D. E. (2001). Communication and uncertainty management. Journal of Communication, 51, 477-497.
Friedman, S. M., Dunwoody, S., & Rogers, C. L. (1986). Scientists and journalists: Reporting science as news. New York: The Free Press.
Friedman, S. M., Dunwoody, S., & Rogers, C. L. (1999). Communicating new and uncertain science. Mahwah, NJ: Erlbaum.
Rimal, R. N. (2000). Closing the knowledge-behavior gap in health promotion: The mediating role of self-efficacy. Health Communication, 12, 219-237.
Rowan, K. E. (1999). Effective explanation of uncertain and complex science. In S. M. Friedman, S. Dunwoody, & C. L. Rogers (eds.). Communicating new and uncertain science (pp. 201-233). Mahwah, NJ: Erlbaum.
Rowan, K. E., Bethea, L. S., Pecchioni, L., & Villagran, M. (2003). A research-based-guide for physicians communicating cancer risk. Health Communication, 15, 239-252.
Witte, K., Meyer, G., & Martell, D. (2001). Effective health risk messages: A step-by-step guide. Thousand Oaks, CA: Sage.
Rapporteur’s Report
Rapporteur: Dr. Michael Stoto
In thinking about the highlights of the presentations and discussion we need to keep in mind the goals of this workshop and the motivations behind CDC’s analysis of causes of death. Dr. McGinnis reminded us that the analysis of “actual causes of death” in 1990 (McGinnis and Foege 1993) aimed to raise awareness of the importance of prevention, quantify the impact of distinct lifestyle factors so policymakers and the public could compare them, and enable scientists to track progress in reducing the impact of lifestyle factors. Drs. Gerberding and Stroup suggested that the 2000 analysis (Mokdad et al. 2004) aimed to update the earlier analysis, develop methods that would enable individual states to replicate the calculations, and quantify the impact of modifiable behavioral risk factors on mortality.
These two analyses seem to have served well their main purposes of raising the profile of prevention and enabling both state and national governments to track progress in addressing
behavioral risk factors. But controversy arises when scientists try to quantify the impact of individual factors, presumably because the results can or should be used to set priorities for social investment. Quantification highlights the mismatch between PAF and related calculations, and between those measures and the questions policymakers and the public want answered or think the calculations answer. In simple terms, the problem arises because “attributable to X” in PAF morphs to “due to X,” “caused by X,” “would not have occurred if X were eliminated,” and eventually “will not occur if X is eliminated.” The fundamental issue is what “cause” and related words mean.
Panelists have identified three possible solutions to that problem: to develop better data and methods to answer the question that policymakers and the public think PAF is addressing; to better explain what PAF calculations mean; and to reformulate the problem to be more policy relevant and answerable.
The first alternative—developing better data and methods—has much potential but is very difficult, as these discussions illustrate. To understand why, consider the examples in Table 3.
Scientists can calculate the impact of a well-defined acute disease such as influenza simply by counting the number of cases in a certain period. Whether the cases have been verified by laboratory analysis—and whether the patients have underlying conditions that might predispose them to die if infected—present only slight complications. The fundamental point is that during an outbreak, determining whether any particular death is “due to” influenza is relatively easy.
In the case of a chronic disease such as coronary heart disease, co-morbidity and multiple causes make assigning a single “cause” to any death difficult. Compositional and substitution effects lead to further complications—basically, people who do not die of coronary heart disease will die of something else—so efforts to calculate the impact of such diseases require demographic and statistical methods.
TABLE 3 Examples of “Attributable” Deaths
|
|
Case counting |
Statistical estimation |
|
Disease |
Influenza Lab verification Predisposing conditions |
Coronary heart disease Definition of coronary heart disease Co-morbidity and multiple causes Compositional and substitution effects |
|
Modifiable risk factor |
Drunken driving Blood alcohol cutoff Road conditions, other drivers, etc. |
Obesity—all of the above, plus PAF methods (partial adjustment, stratify by age and sex, regression simulations, etc.) Continuous vs. dichotomous scale Bias in RR estimates, especially due to extrapolation outside observed distribution Cross-sectional Δ Observed Δ Causal paths Δ in other risk factors and outcomes |
Estimating the impact of a modifiable risk factor such as drunken driving takes us back to case counting, but also entails the problem of assigning a single cause. How high does someone’s blood alcohol concentration have to be before a death is attributed to drunken driving, for example? How do analysts factor in road conditions, the actions of other drivers, and so on?
Efforts to estimate the impact of risk factors such as obesity present all those problems plus additional ones. As speakers have noted, the various statistical methods for calculating attributable deaths make different assumptions. There are also issues such as the use of a continuous versus a dichotomous scale for the risk factor, and bias in estimates of relative risk, especially when extrapolating outside the observed distribution. Other issues include cross-sectional differences interpreted as differences over time, differences in risk factors seen in observational studies versus those intentionally manipulated, complex causal paths, and changes in risk factors and outcomes other than the subject of the calculations.
Faced with such difficulties, we can reasonably ask whether we should focus on better explaining what PAF calculations mean rather than simply trying to improve the calculation of PAF. As speakers have indicated, this entails more than just being careful about what we say and saying it clearly. In particular, speakers noted that we need to find ways to represent uncertainty (including but not limited to confidence intervals), and to present the results of sensitivity analyses.
DISCUSSION OF LESSONS LEARNED AND NEXT STEPS
Edited by Miriam Davis
In closing the workshop, Dr. Harvey Fineberg asked attendees to cite the most important take-home lessons and possible action steps. Comments fell into the following categories: reframing the dialogue, improving methodology, developing an action plan, and guiding public policy and creating messages for the public. These comments are not to be interpreted as consensus comments or recommendations.
Discussants Voiced the Following Take Home Lessons and Next Steps
Reframing the Debate
-
Focus on lifestyle-related risks as a collective problem, as government intervenes on collective risks over which individuals have little or no control.
-
Reframe the debate to focus on the impact of proposed interventions rather than risk factors. Understanding risk factors merely tells us where and how we might pursue interventions. Such a shift would provide estimates most relevant to policymakers, who invest in programs, not risk factors. Conceptual and practical problems remain in assessing the impact of interventions, as observational data are weak or absent. That deficit points to the need for more research and better methodology.
-
Avoid a list of individual attributes and misleading terms like obesity, and do not rush to judgment about the growing prevalence of obesity.
Improving Methodology
-
Bring measures and analyses of the impact of diet, physical activity, and obesity to the same level of sophistication as tobacco-related analyses. IOM and NIH could take the lead in identifying critical gaps in data, methods, and estimates.
-
Develop an annual summary of progress in reducing diet- and activity-related risks, as occurs for tobacco, to drive both research and public health.
-
Ensure that scientific methods are rigorous and defensible. Use several different techniques for measuring lifestyle-related risks and disease burden to analyze identical data, and systematically compare results to determine the best approach.
-
In gathering and analyzing data, remember that the perfect should not be the enemy of the good. There is no perfect method for estimating PAFs. In the face of uncertainty, be conservative.
-
Measure inactivity and nutrition and separate them conceptually from obesity. Yet recognize that while important, inactivity and nutrition will be difficult for states to track.
-
Focus on identifying measures that are easy to communicate to policymakers and the public
-
Use causal models to broaden the range of sensitivity analyses applied to PAF calculations.
-
Stratify by age in computing population attributable deaths from lifestyle-related risks. Failing to do so inflates the estimated number of deaths by 30–50 percent or more.
-
Raise the profile of policy-relevant methods of measuring risk and disease burden as legitimate scientific pursuits for epidemiologists, and ensure that they take them as seriously as more traditional research methods.
Developing an Action Plan
-
Create a coordinated action plan to improve research methods, communicate findings, and develop interventions that would exert an impact on public health. We cannot afford to wait another 10 years to address the role of lifestyle factors in preventable death.
-
Develop a research agenda that offers the strong justification needed to persuade policymakers of the public health importance of reducing the impact of preventable lifestyle-related risks. Ensure that estimates of risk and disease burden are credible and specific enough to suggest cost-effective interventions.
-
Through IOM or the National Institutes of Health (NIH) or other venue, periodically convene a multidisciplinary group of epidemiologists, other scientists, and public health professionals to clarify the questions that need analyzing, determine the appropriate measures to answer each question, and interpret results. Include real-world decision makers in the group…
-
Develop training strategies and improve teaching of PAFs and related concepts.
Guiding Public Policy and Creating Messages for the Public
-
Make public health messages simpler and clearer yet also more explicit regarding the uncertainty underlying estimates of the impact of lifestyle-related risks. Motivate the public to demand policy intervention around preventable illness.
-
Avoid creating a horse race among risk factors such as diet, physical activity, tobacco, and alcohol. We know the importance of a basic nonsmoking, active lifestyle in which alcohol consumption is moderate.
-
Portray lifestyle-related risks as a public health concern rather than an individual problem.
-
Highlight the social costs of under funding the public health surveillance systems that could answer questions about lifestyle-related risks and enable society to use trillions of healthcare dollars more effectively.
-
Demonstrate the economic payoff of interventions on lifestyle-related risks to the business community. That effort is important because that community wields enormous political influence, and because companies can improve their own productivity by focusing on lifestyle interventions.
REFERENCES
Aldana SG. McGinnis JM, Foege WH. 2001. Actual causes of death in the United States. JAMA. 270(18):2207-12.
Aldana SG. 1998.Financial impact of health promotion programs: a comprehensive review of the literature. Am J Health Promot. 15(5):296-320.
Allison DB, Zannolli R, Narayan KM. 1999.The direct health care costs of obesity in the United States. Am J Public Health. 89(8):1194-9.
Allison DB, Zannolli R, Faith MS, Heo M, Pietrobelli A, VanItallie TB, Pi-Sunyer FX, Heymsfield SB. 1999. Weight loss increases and fat loss decreases all-cause mortality rate: results from two independent cohort studies. Int J Obes Relat Metab Disord. 23(6):603-11.
Allison DB, Faith MS, Heo M, Townsend-Butterworth D, Williamson DF. 1999. Meta-analysis of the effect of excluding early deaths on the estimated relationship between body mass index and mortality. Obes Res. 7(4):342-54.
Allison DB, Heo M, Flanders DW, Faith MS, Williamson DF. 1997. Examination of "early mortality exclusion" as an approach to control for confounding by occult disease in Epidemiologic studies of mortality risk factors. Am J Epidemiol. 146(8):672-80.
[No authors listed] 1999. Effect of smoking on the body mass index-mortality relation: empirical evidence from 15 studies. BMI in Diverse Populations Collaborative Group. Am J Epidemiol. 150(12):1297-308.
Andres R. 1985. Mortality and obesity: The rationale for age-specific height-weight tables. In: Andres R, Bierman EL, & Hazzard WR, eds. Principles of Geriatric Medicine. New York: McGraw-Hill Book Co. pp: 311-318.
Anderson RN. 2002. Death: Leading causes for 2000. National Vital Statistics Reports. Hyattsville, Maryland: National Center for Health Statistics 50:16
Bigaard J, Frederiksen K, Tjonneland A, Thomsen BL, Overvad K, Heitmann BL, Sorensen TI. 2004. Body fat and fat-free mass and all-cause mortality. Obes Res. 12(7):1042-9.
Christou NV, Sampalis JS, Liberman M, Look D, Auger S, McLean AP, MacLean LD. 2004. Ann Surg. 240(3):416-23.
Doll R, Peto R, Boreham J, Sutherland I. 2004. Mortality in relation to smoking: 50 years' observations on male British doctors. BMJ. 328(7455):1519. Epub 2004 Jun 22.
Ezzati M, Lopez AD, Rodgers A, Vander Hoorn S, Murray CJ; Comparative Risk Assessment Collaborating Group. 2002. Selected major risk factors and global and regional burden of disease. Lancet. 360(9343):1347-60.
Finkelstein EA, Fiebelkorn IC, Wang G. 2003. National medical spending attributable to overweight and obesity: how much, and who's paying? Health Aff. Jan-Jun; Suppl Web Exclusives:W3-219-26.
Flegal KM, Williamson DF, Pamuk ER, Rosenberg HM. 2004. Estimating deaths attributable to obesity in the United States. Am J Public Health. 94(9):1486-9.
Flum DR, Dellinger EP. 2004. Impact of gastric bypass operation on survival: a population-based analysis. J Am Coll Surg. 199(4):543-51.
Fontaine KR, Redden DT, Wang C, Westfall AO, Allison DB. 2003. Years of life lost due to obesity. JAMA. 289(2):187-93.
Franks P, Lubetkin EI, Gold MR, Tancredi DJ, Jia H. 2004. Mapping the SF-12 to the EuroQol EQ-5D Index in a national US sample. Med Decis Making. 24(3):247-54.
General Accounting Office (GAO). 2003. CDC’s 2002 Report on Health Consequences of Smoking. GAO/03-942R. Washington, DC. Http://www.gao.gov/new.items/d03942r.pdf
Haapanen N, Miilunpalo S, Vuori I, Oja P, Pasanen M. 1997. Association of leisure time physical activity with the risk of coronary heart disease, hypertension and diabetes in middle-aged men and women. Int J Epidemiol. 6(4):739-47.
Institute of Medicine (IOM), 1998. Summarizing Population Health: Directions for the Development and Application of Population Metrics. Washington, D.C.: National Academies Press.
Kmietowicz Z, Ferriman A. 2002. A Pro-tobacco writer admits he should have declared an interest. BMJ. 324(7332):257.
Levin ML. 1953. The occurrence of lung cancer in man. Acta Unio Int Contra Cancrum. 19: 531-541.
McGinnis JM, Foege WH. 2004. The immediate vs the important. JAMA. 291(10):1263-4.
McGinnis JM, Foege WH. 1993. Actual causes of death in the United States. JAMA. 270(18):2207-12.
Mokdad AH, Marks JS, Stroup DF, Gerberding JL. 2004. Actual causes of death in the United States, 2000. JAMA. 291(10):1238-45.
Mokdad AH, Marks JS, Stroup DF, Gerberding JL. 2005. Correction: Actual causes of death in the United States, 2000. JAMA. 293(3):293.
MMWR (Morbidity and Mortality Weekly Report), 2004. Alcohol-attributable deaths and years of potential life lost—United States, 2001. September 24, 2004 53(37); 866-870.
Ozminkowski RJ, Ling D, Goetzel RZ, Bruno JA, Rutter KR, Isaac F, Wang S. 2002. Long-term impact of Johnson & Johnson's Health & Wellness Program on health care utilization and expenditures. J Occup Environ Med.44(1):21-9.
Ozminkowski RJ, Dunn RL, Goetzel RZ, Cantor RI, Murane J, Harrison M. 1999. A return on investment evaluation of the Citibank, N.A., Health Management Program. Am J Health Promot 14(1):31-43.
Pearl J. 2000. Causality: Models, Reasoning and Inference. New York: Cambridge University Press.
Peeters A, Barendregt JJ, Willekens F, Mackenbach JP, Al Mamun A, Bonneux L; NEDCOM, the Netherlands Epidemiology and Demography Compression of Morbidity Research Group. 2003. Obesity in adulthood and its consequences for life expectancy: a life-table analysis. Ann Intern Med. 138(1):24-32.
Robins JM. 1986. A new approach to causal inference in mortality studies with a sustained exposure period: applications to control of the healthy workers survivor effect. Mathematical Modeling. 7: 393-512.
Rockhill B, Weinberg CR, Newman B. 1998. Population attributable fraction estimation for established breast cancer risk factors: considering the issues of high prevalence and unmodifiability. Am J Epidemiol. 147:826-33.
Rommer J. 1993. A pragmatic theory of responsibility for the egalitarian planner. Philosophy and Public Affairs. 22: 146-66.
Russell LB, Valiyeva E, Carson JL. 2004. Effects of prehypertension on admissions and deaths: a simulation. Arch Intern Med. 64(19):2119-24.
Russell LB, Gold MR, Siegel JE, Daniels N, Weinstein MC. 1996. The role of cost-effectiveness analysis in health and medicine. Panel on Cost-Effectiveness in Health and Medicine. JAMA. 276(14):1172-7.
Sargent RP, Shepard RM, Glantz SA. 2004. Reduced incidence of admissions for myocardial infarction associated with public smoking ban: before and after study. BMJ. 328(7446):977-80. Epub 2004 Apr 05.
Scruton, R. (2000) WHO, what and why?: trans-national government, legitimacy and the World Health Organisation. Occasional paper 113. London: Institute of Economic Affairs.
Sesso HD, Paffenbarger RS Jr, Lee IM. 2000. Physical activity and coronary heart disease in men: The Harvard Alumni Health Study. Circulation. 102(9):975-80.
Tengs TO, Lin TH. 2003. A meta-analysis of quality-of-life estimates for stroke. Pharmacoeconomics. 21(3):191-200.
Troiano RP, Frongillo EA Jr, Sobal J, Levitsky DA. 1996. The relationship between body weight and mortality: a quantitative analysis of combined information from existing studies. Int J Obes Relat Metab Disord. 20(1):63-75.
Wee CC, Phillips RS, Legedza AT, Davis RB, Soukup JR, Colditz GA, Hamel MB. 2005. Health Care Expenditures Associated With Overweight and Obesity Among US Adults: Importance of Age and Race. Am J Public Health. 95(1):159-65.
Williams A. 1997. Intergenerational equity: An exploration of the “fair innings” argument. Health Econ. 6:117-132.
Wolf AM, Colditz GA. 1998. Current estimates of the economic cost of obesity in the United States. Obes Res. 6(2):97-106.