2
Answers to the Military’s Questions
This chapter presents the committee’s conclusions and recommendations regarding the specific questions posed by the military on the optimal nutrient composition of the assault ration. Chapter 3 provides additional comments and suggestions related to food ration development because the success of the ration is ultimately associated with its acceptability by the soldiers in the field.
The need for specific nutrients is influenced by the health status and specific scenario and environmental conditions in which soldiers are deployed. To provide context for the recommendations, assumptions of the characteristics of the soldiers’ diets and health, the missions, and other issues were formulated. These assumptions were compiled throughout the deliberations of the committee, open sessions with sponsor representatives and other military personnel, information from a field survey conducted in Afghanistan, and available literature. As a result, a worst-case scenario was constructed so that the recommended assault ration would diminish, to the extent possible, significant losses of body fat and protein, which, if allowed to occur, might prevent soldiers completing an assault mission from being redeployed to a subsequent mission in the immediate future.
Finally, where the committee identified gaps in the information available, research needs to establish nutrient requirements and to unravel food technology challenges are provided. This chapter presents the assumptions, along with the committee’s conclusions and recommendations, and research needs specific for each nutrient.
ASSUMPTIONS
The assault ration recommended in this report is designed for healthy male soldiers with an average body weight of 80 kg, approximately 16 percent body fat who are relatively fit and within an age range of 18–45 years (average < 25 years) while on military assault missions. As evident in Table 1-1, the ration recommended does not meet the military recommended nutrient intakes for garrison in AR 40-25 (US Departments of Army, Navy, and Air Force, 2001) nor does it meet the recommended nutrient intakes for civilians (IOM, 1997a, 1998, 2000, 2001b, 2002a, 2004). For very active male soldiers in the field, daily energy intakes rarely are over 3,000 kcal (IOM, 1995) and unpublished data suggest they average 2,400 kcal (see Montain, 2004 in Appendix B), which in the event of energy expenditures of 4,500 kcal are significantly hypocaloric. Prolonged and continuous use of this hypocaloric ration as the sole source of sustenance at such high energy expenditures will lead to substantial weight loss. The committee emphasizes that this ration is meant to be used for repetitive three- to seven-day missions that last for a maximum total period of one month and that include recovery periods of 24 to 72 hours between missions. With the expected energy expenditures of 4,500 kcal/day during the missions, it is possible that some soldiers might lose as much as 10 percent body weight before the end of the month, even with refeeding between missions; this degree of weight loss could result in adverse, but mild performance decrements. However, there is not likely to be any serious consequences for health. Therefore, it is recommended that weight loss be measured after one month of use, and if weight loss is higher than 10 percent for a soldier, he should not be sent on assault missions until weight is regained to within 5 percent of initial weight.
Scenarios Before and After Deployment on Assault Missions
The committee assumes that, before being deployed on a mission, soldiers may be living in one of three general scenarios:
-
A base in the United States or a foreign country in which food is relatively abundant and consumed on an ad libitum, uncontrolled basis. Soldiers have ready access to beverages, often including alcohol, and dietary supplements.
-
A more highly controlled environment in a military theatre of operations. In such an environment, food consumption is ad libitum from either field kitchens or conventional foods in a garrison situation. There is a variable but generally more limited availability of other substances including food and dietary supplements.
-
A recovery site where soldiers are in the process of rehabilitation from a prior assault mission. Food choice is even more limited, with fewer menu
-
items available, and provided ad libitum but in a more controlled environment than in the field kitchen. Nevertheless, the amount of food and calories available are more abundant than while deployed on an assault mission.
The probability of soldiers deploying from any of these scenarios will no doubt vary, depending on the theatre of operations for the assault mission.
Diets Prior to Assault Mission
Food Consumption
It is unclear what foods and beverages soldiers would be likely to consume before an assault mission. Existing literature and soldier interviews indicate that their food usually comes from a field kitchen. The soldiers may be eating Meals, Ready-to-Eat (MREs) or hot meals with bread and dessert served in a portable cafeteria line, but without fresh fruits or vegetables. Food in the pre-deployment setting is generally provided ad libitum. The committee assumes that the soldiers’ diet prior to the assault mission is ad libitum from a field kitchen without fresh fruits or vegetables.
Alcohol Consumption
Although military policy strictly prohibits alcohol consumption in the field operations, some alcoholic beverages are probably available in the local environment in many theatres of military operations. Some soldiers may have consumed alcohol in the days immediately before the mission. The likelihood of this happening depends on whether soldiers are deployed to the mission from a controlled environment or not (see scenarios above). Available information suggests that excessive alcohol consumption is unlikely to be a major problem among those being deployed on assault missions in the field. The committee assumes that soldiers may consume alcohol before the assault mission, but this is unlikely to be a major problem.
Use of Dietary Supplements and Other Substances
Dietary supplements, caffeine, and other substances such as tobacco may be available locally from several sources, as well as from shipments from home. As a result, effects of these on nutrient requirements as well as withdrawal symptoms may be relevant. The committee assumes that a soldier may use supplements and caffeine before the assault mission and withdrawal symptoms may interfere with performance. The general use of tobacco products is also assumed.
Diets Immediately Before Assault Mission
Existing reports suggest that immediately (i.e., a day or hours) before the assault mission, soldiers are well hydrated. Indeed, because soldiers know that fluids are likely to be limited during the mission, with only four to five liters of water available, they may attempt to overhydrate themselves for a few hours before the mission. While a soldier could eat in excess or use protein-rich supplements in the period immediately prior to deployment on an assault mission, in general it has been reported that soldiers pay little attention to nutritional considerations during this time. It has also been reported that approximately 40 percent of the soldiers increase energy intake (primarily as carbohydrate) prior to deployment. Alcohol is strictly prohibited, although some alcohol may be available from the local environment; alcohol use was not reported as a problem. It is estimated that 20–30 percent of the soldiers smoke and as many as 60 percent chew or dip tobacco. The committee assumes that immediately prior to a mission soldiers are well hydrated, often use tobacco products, and do not abuse alcohol.
Scenario During Assault Mission
Duration of Mission
The worst-case scenario is depicted as three- to seven-day missions that will be repeated several times with little rehabilitation in between missions, leading to increased physiological stress. Based on experiences in Afghanistan, in a 30-day period soldiers might be in assault operations as many as 24 days. The committee assumes that a soldier is in an assault mission 24 out of 30 days, with each mission lasting three to seven days.
Physical Activity and Energy Expenditure
The energy expenditure of soldiers while on an assault mission is reported to be approximately 4,500 kcal/day due to intermittent periods of high energy expenditure (> 50 percent VO2max) and periods of low-intensity, sustained movement. According to the experiences in Afghanistan, during a mission many soldiers sleep about five to six hours per day; the average sleep time, however, was four hours. The committee assumes that a soldier is physically active for a total of 20 hours per day, gets four hours per day of sleep, and expends about 4,500 kcal/day.
Consumption of Ration Food Items
Observational data from testing First Strike Rations (FSRs), a lightweight ration prototype being developed for assault missions by the US Department of
Defense Combat Feeding Directorate in Natick, Massachusetts, showed little wastage at approximately 2,400 kcal when used in military training. Some reports, however, suggest that with other higher-calorie rations, soldiers trade and selectively discard items (stripping) according to individual preferences. It appears that there is less stripping of the FSR than was the case in Desert Storm using MREs in the early 1990s (personal communication, S. Montain, US Army Research Institute of Environmental Medicine [USARIEM], August 9, 2004). When stripping of rations does occur, the carbohydrate-rich (e.g., candies) and protein-rich (or those entrees that are perceived as high in protein) meal items are the ones most frequently preserved. Items stripped depend on the environment; some items are favored in hot climates and others in cold climates. Relevant to these discussions is the fact that during Ranger Training in which one MRE per day plus a bread item (1,600 kcal/day) was provided, the rangers did not discard but rather ate 100 percent of the ration; however, their daily energy expenditure averaged 4,000 kcal and the period of training in the field was twice as long (56 days) as the time being considered in this report (Shippee et al., 1994). Other observations indicate that during recent Iraq missions troops discarded food items from MREs to carry more ammunition and then became hungry. It is not known what or how much was thrown away.
The committee assumes that, if palatable, when provided with an assault ration of 2,400 kcal or less per day, soldiers expending 4,500 kcal per day will consume virtually 100 percent of the ration.
Accessibility to Water
It is assumed that soldiers have four to five liters of chlorinated water (i.e., 2-5 ppm chlorine) available during the mission. Water will be resupplied or obtained from other sources during the mission.
Health Issues
Little specific information is available on prevalence of diarrhea during recent assault missions in Afghanistan. Cases of diarrhea were reported as being a problem when soldiers ate local foods. Very few of the cases of diarrhea resulted in dehydration so severe that personnel had to be evacuated from the theatre of operation, although many more cases were probably treated medically in the field. Constipation in the field appears not to be of concern, according to interviews and information available to the committee. There is little information on the prevalence of kidney stones in the field, but it was mentioned as a concern in anecdotal reports. Some cases of kidney stones, though, were thought to be not the result of the rations consumed but of some preexisting condition previous to deployment (personal communication, C. Koenig, USARIEM, November 19, 2004). It is assumed that cases of diarrhea and kidney stones
occur during missions and are an important consideration when making recommendations on nutritional composition of assault rations.
Environmental Conditions
The climatic conditions and geographical sites in which combat can take place vary from hot, dry deserts to cold, high-altitude mountain terrains. Deployment to these varying environments can affect the nutrient requirements of soldiers due to differences in fluid intake as well as in sweat and excretory losses of nutrients. Even more unknown are the effects of these varied environments on food preferences, acceptability, and eating behavior. Although there was no attempt to consider all the possible environmental conditions, two environmental temperatures (20 and 30°C) were assumed in cases in which losses of a particular nutrient through sweat could be significant. In line with the committee’s philosophy of assuming the worst-case scenario, when sweat losses of minerals are significant (i.e., could lead to adverse health effects), an extra amount of the nutrient was included to cover the losses endured by soldiers engaged in significant energy expenditure (4,500 kcal) in warm temperatures.
Physiological Compensation for Changes in Electrolyte Intake
Electrolyte, especially sodium, intake in garrison and on mission may be very different. Adaptation to a lower level of intake is fairly rapid as reequilibrium of serum levels occurs quickly (e.g., within a few days for potassium and sodium; Luft et al., 1979; Ruppert et al., 1994). It is assumed that soldiers have different electrolyte intakes before a mission than during a mission but that the period of biological adjustment to these changes will be relatively short and thus of little consequence.
Assault Ration
Size and Weight Limits
The daily assault ration for sustained operations could be distributed in various components but must fit in 0.12 cubic feet (e.g., a 6-inch cube) and weigh no more than 3 lb (1.36 kg). Packaging material constitutes 0.181 kg of the 1.36 kg. It is assumed that the ration is on average approximately 12–17 percent water, varying greatly from one item to the other; most items are energy dense, intermediate moisture food products with negligible packaging material weight.
Form of Food
In addition to food products of intermediate moisture, gels or powders high in carbohydrate and/or electrolytes that can be added to water and candy are
possible food forms that can be used in an assault ration. The committee assumed that there will be no liquid foods in the rations, and that gels, powders, or candy are alternate forms of food.
Micronutrients
Electrolytes may be supplemented as candy, gels, or powders to be added to fluid. It is assumed that all other required micronutrients, however, are provided within the food items making up the basic ration.
Food Consumption During Recovery After Deployment on Assault Missions
It is difficult to determine whether soldiers consciously attempt to gain weight during recovery or rehabilitation after missions. Anecdotal information indicates that after an assault mission and during recovery, soldiers generally eat to appetite if food is readily available, and most do not attempt to gain or lose weight. A complete reversal of the deficits incurred during the assault mission may not occur during the 1–3-day recovery period of time. For example, a report from recent operations in Afghanistan suggests that personnel are re-deployed on repeated assault missions with little time for recovery between missions. Thus, soldiers would rarely have adequate time to build up bodily stores for the next assault exercise. The committee assumes that food consumption after return from an assault mission will not allow for complete rehabilitation. However, it is also assumed that the food available during recovery will provide at a minimum the nutritional standards for operational rations as delineated in AR 40-25 (US Departments of Army, Navy, and Air Force, 2001).
QUESTION A
Should the energy content of the ration (energy density) be maximized so as to minimize the energy debt, or is there a more optimal mix of macronutrients and micronutrients, not necessarily producing maximal energy density?
RECOMMENDATION: The basic ration’s energy content should be approximately 2,400 kcal/day. While this level does not maximize energy density, this is the average daily energy intake that has frequently been reported for soldiers during training. Choosing this caloric level minimizes the possibility of discarding food items that might result in inadequate intakes of necessary micronutrients; however, in case ration items are discarded, micronutrients should be distributed as evenly as possible throughout the food items in the ration (rather than clustering them in a few items) to prevent significant amounts of individual micronutrients from
being discarded. It should also be emphasized that rations should only be used over intermittent short terms (three to seven days) that, together, may last for a total of no more than a month.
Options for the Energy Content of the Ration
The committee discussed options that provide different macronutrient profiles and caloric content to meet the needs of soldiers on assault missions. Given the weight and size constraints of the ration (0.12 cubic feet, 1.36 kg) and unique circumstances encountered in the assault scenario, three options that represent the spectrum of possibilities were developed, and the most feasible option based on review of expected benefits and drawbacks was identified.
The first option was to design a ration that would provide enough energy (i.e., 4,500 kcal) to meet the expected needs during the mission. The advantage of such a ration, if it were eaten completely, would be that soldiers would maintain energy equilibrium and avoid the adverse consequences of a periodic hypocaloric diet. The major disadvantage of this first option would be that when food items are discarded, as is often the case when higher-calorie rations are provided, nutrients would be discarded as well, potentially resulting in inadequate intakes of essential nutrients. Therfore, a major challenge with this scenario is to design a ration of sufficient palatability so that it is eaten in its entirety. When soldiers in the field do not consume all of their ration items when they are provided with enough MREs to meet their energy needs (personal communication, C. Koenig, USARIEM, November 19, 2004), then the risk of soldiers discarding foods containing rich sources of essential nutrients and increased risk for nutrient deficiency cannot be dismissed. Although it might be possible to design a ration in which nutrients are equally distributed among items, the acceptability of such a ration would be low compared to a ration that included foods that offer variety and familiarity (see Chapter 3, Food Matrix Considerations). Given the routine practice of stripping based on food preferences, providing a ration with a variety of highly acceptable products that ensures 100 percent consumption is more important than providing a ration with a high caloric value that may result in important components being discarded.
A second option was to design a ration that would provide the usual energy needs of soldiers when not on assault operations; such energy needs are assumed to be approximately 3,500 kcal/day. The major advantage of this second option is that it would create a comparatively small energy deficit when energy expenditure is at the level of 4,500 kcal/day. However, this option design presents the same challenges as the one above, namely to design a ration that is fully eaten when the caloric content is higher than what they would normally eat. Given the challenge of designing a highly acceptable ration that is fully eaten by soldiers under stress in an assault operation, and due to concerns about selective discarding of some items in the ration, this is also not a viable design.
The third energy level option would provide as a basic ration 2,400 kcal/day, with a supplemental source of energy. Observations in the field indicate that during training and with 3,600 kcal (3 MREs), a soldier’s voluntary energy intake is approximately 2,400 kcal/day, even when the energy expenditure is high (>7,000 kcal for marines at high altitudes and cold temperatures or ~ 6,000 kcal for Army rangers in warm temperatures) (see Montain, 2004 in Appendix B); therefore, 2,400 kcal/day represents an energy level at which virtually all of the ration should be consumed (personal communication, A. Young, USARIEM, August 9, 2004). The ration would include 100 to 120 g of protein, 350 g of carbohydrate, and the remainder as fat (approximately 22–25 percent) (see questions B and C and Box 2-1) for a total of 2,400 kcal, as well as the micronutrient recommendations which follow (see questions D and E).
|
BOX 2-1 Basic Ration:
Carbohydrate (and Electrolyte) Supplement:
Salt Tablets (Available Through Medical Personnel):
NOTE: This ration is intended for use over three- to seven-day missions for up to a month. Prolonged and continuous use of these rations as a sole source of sustenance may lead to substantial weight loss. Constraints: weight of 3 lb (1.36 kg) and volume of 0.12 cubic feet. |
To provide an energy level closer to the level of energy expended, 400 additional kcal should be supplemented to the basic ration, increasing the total energy content of the ration to 2,800 kcal/day. This can be accomplished with the addition of supplements in individual, small packages with a total amount of up to 100 g (400 kcal) of carbohydrate in four forms: as a powder to be dissolved in a liquid, as a gel, as candy, or as some combination of these depending on the delivery system. Although soldiers would still be in a negative energy balance, little evidence exists to suggest that a periodic hypocaloric diet, if otherwise adequate in protein and other essential nutrients as specified in the following sections, is likely to be harmful when consumed over brief periods of time (repetitive three to seven days, up to a month), even if some weight loss occurs (< 10 percent of body weight). However, with the expected energy expenditures of 4,500 kcal/day during the missions, it is possible that some soldiers might lose as much as 10 percent body weight before the end of the month, even with refeeding between missions; this degree of weight loss could result in adverse, but mild, performance decrements. However, this level of weight loss is not likely to be of any serious consequences for health. Therefore, it is recommended that weight loss be measured after one month of use, and if weight loss is higher than 10 percent for a soldier, he should not be sent on assault missions until weight is regained to within 5 percent of initial weight.
Rationale for Energy Content
Energy expenditures of soldiers during combat assault missions have been reported to be high (about 4,500 kcal/day). The committee based its recommendation for energy level on the premise that, to maintain health and performance, it is critical that soldiers have adequate nutrient intakes and that, based on experience, in this type of military operations voluntary daily energy intakes approximates 2,400 kcal.
While it is possible to construct a ration with up to 4,500 kcal within the constraints of weight and size, given the research reviewed and anecdotal information, soldiers would most likely selectively discard unwanted items (“cherry pick”) and, in this way, would likely consume less of essential nutrients. A strategy to avoid nutrient inadequacies due to stripping would be to design a ration with nutrients equally distributed among items. While this might appear ideal and highly desirable from the nutritional standpoint, it is unlikely that a ration can be designed that, in addition to having nutrients equally distributed, is also palatable and acceptable, two key requirements to enhancing intake. Typically, nutrients in palatable, commercially available products are not equally distributed. To maximize acceptability and encourage consumption, the ration should contain a variety of foods that are similar to those commercially available rather than relying on the “bar” type of product fortified to contain the recommended levels of all nutrients. Moreover, given the fact that water needs increase
with caloric intake, a lower calorie ration may be advantageous. Providing a ration with a variety of highly acceptable products that ensure 100 percent consumption is more important than providing a ration with a high caloric value that may result in important components being discarded.
Given the weight and volume restrictions and considerations described above, a 2,400 kcal basic ration is the most nutritionally appropriate choice among the three options discussed above (i.e., energy content of 4,500, 3,600, and 2,400 kcal). Recent experience with prototype FSRs at approximately similar levels of energy content (approximately 2,400 kcal) indicates that selective discarding of menu items in the rations was not widely practiced (personal communication, A. Young, USARIEM, August 9, 2004). A ration of 2,400 kcal, although hypocaloric, will be above the basal level necessary for covering resting metabolism in all individuals in the military. Since the caloric deficit is not likely to be sustained for more than three to seven days at a time during the assault mission, the concern about the potential inadequate intake of important nutrients when stripping a higher caloric ration outweighs the concern about the effects of multiple hypocaloric periods.
In addition to the enery content of the basic ration of 2,400 kcal, an additional 100 g (400 kcal) of carbohydrate would be a readily available source of carbohydrate. This supplemental energy source could be consumed on a periodic basis in bolus doses to keep energy (and electrolytes) at more satisfactory levels or as a supplement of energy for individuals with even greater caloric expenditure. Also, such energy-dense snacks appear to be particularly popular among the troops (personal communication, C. Koenig, USARIEM, November 19, 2004).
Even with such a low-caloric ration, specific items containing concentrated sources of a particular nutrient may be selectively discarded, leading to an increased risk of nutrient deficits. This is particularly true for items other than high-carbohydrate foods. Therefore, to further ensure the maximum consumption of all essential nutrients in the ration, the micronutrients and macronutrients should be distributed as evenly as possible; this should be accomplished without compromising acceptability across menu items in the ration.
Research Needs Related to Energy Content
-
Test the acceptability of the prototype assault ration under field conditions and determine the actual amounts eaten. The extent of discarding ration items under combat conditions needs to be evaluated in field surveys, and the findings must be taken into account in ration development and refinement.
QUESTIONS B AND C
What would be the optimal macronutrient balance between protein, fat, and carbohydrate for such an assault ration to enhance performance during combat missions?
What are the types and levels of macronutrients (e.g., complex versus simple carbohydrates, proteins with specific amino acid profiles, type of fat, etc.) that would optimize such an assault ration to enhance performance during combat missions?
Protein
RECOMMENDATION: The protein level of the ration should be 100–120 g total protein (based on 1.2–1.5 g/kg of body weight for an 80 kg average male soldier). This level will likely spare muscle protein loss as well as attenuate net nitrogen loss and adequately provide for synthesis of serum proteins while the individual is in a hypocaloric state. In addition, this level of protein will likely maintain the immune and cognitive functions requiring protein or amino acids.
The committee recommends that the protein added to the ration be of high biological value. At this time, there is insufficient evidence to believe that the addition of specific amino acids or specific proteins with rapid rates of absorption would be of any additional benefit; more evidence is necessary before making a recommendation in this respect.
Background
The multiple stressors (e.g., sleep deprivation, increased energy expenditure, hypocaloric diet) during short-term combat missions may result in decrements of mental and physical function that would compromise military success and may even jeopardize lives. Optimizing the ration’s protein and carbohydrate levels may be particularly important for muscle performance and cognitive function. The Recommended Dietary Allowance (RDA) for dietary protein set by the Institute of Medicine (IOM) of 0.8 g/kg of body weight per day (IOM, 2002a) and the safe amount of dietary protein to maintain body weight and nitrogen balance set for healthy persons in international dietary standards of 0.75 g/kg of body weight per day (FAO/WHO/UNU, 1985) do not necessarily apply to individuals under stress. The combination of physical and psychological stressors during combat missions presents a complex and unique situation. Nutritional needs and impact on performance in such situations have yet to be examined. Therefore, until more data become available, the committee concluded, it is prudent to include liberal amounts of protein high in biological value to avoid possible short-falls.
Limited energy intake (approximately, 2,400 kcal/day) combined with high levels of physical activity results in energy deficits of about 50 percent for a three- to seven-day assault mission and can result in muscle loss and impairments in performance. Muscle loss during simulated sustained operations has not been clearly demonstrated (Montain and Young, 2003; Nindl et al., 2002), but this is possibly due to the poor sensitivity of the methodology used to estimate losses. Other evidence, however, suggests that such energy deficits will result in muscle loss.
Many classical studies have demonstrated the importance of energy balance for body nitrogen balance (Butterfield and Calloway, 1984; Todd et al., 1984). Nitrogen balance could clearly not be maintained over the long term when energy intake was 15 percent less than expenditure, and nitrogen balance was shown to be better maintained when energy balance was positive or at least zero (Todd et al., 1984). Presumably, a major source of this nitrogen loss would be from the body’s predominant and readily accessible source of nitrogen, muscle protein. Energy restriction over longer time periods results in loss of lean mass during very low-calorie dieting (Layman et al., 2003); however, the metabolic mechanisms remain to be delineated. Animal studies also showed similar findings (Anthony et al., 2000). These perturbations in muscle metabolism due to energy deficits may occur very rapidly, as evidenced by the immediate signs of muscle catabolism stimulated by a 20 percent energy intake reduction in a study that included males and females (Tipton et al., 2003). Taken together, these findings suggest that soldiers participating in missions during which energy intake is half of the energy output would be losing nitrogen; most nitrogen would be from muscle protein, although some might also come from the gastrointestinal or other internal organs.
In addition to the effects due to a hypocaloric diet, the loss of muscle protein may also be exacerbated by the intensity of the physical activity. Evidence from studies on very strenous physical activity and muscle metabolism in rats (Anthony et al., 1999) suggests that, rather than increasing protein utilization, the physical activity involved in prolonged military missions may be detrimental to muscle protein metabolism. Although sports experts advise athletes to consume approximately 1.5 g protein per kg every day (ACSM/ADA/DA, 2000), which is nearly twice the RDA (IOM, 2002a), insufficient evidence was found to conclude that high-level physical activity alone increases the normal protein requirement. More recent reviews have come to the same conclusion (Fielding and Parkington, 2002; Tipton and Wolfe, 2004).
It thus appears that the energy deficit combined with the stressful situation found in combat alters muscle protein metabolism during missions of this type.
Rationale for the Level of Protein
Although there is a great deal of controversy over the protein requirements for athletes and active individuals, it is a reasonable and conservative hypothesis
that increased protein intake would be advantageous in a situation in which the substantial energy deficit is exacerbated by high levels of physical activity (see Hoffer, 2004 in Appendix B).
Lean Tissue and Nitrogen Balance. Under eucaloric conditions, the RDA for protein (0.8 g/kg/day) (IOM, 2002a) will maintain lean tissue and normal values of its usual physiologic and laboratory markers—lean tissue maintenance and nitrogen balance—but this amount of protein might not be adequate when energy is restricted. As mentioned above, improvements in protein metabolism may be produced by increasing the protein intake. A recent study demonstrated that a greater proportion of weight lost during energy restriction came from fat rather than lean mass when protein intake was increased (Layman et al., 2003). Although this study was conducted on obese individuals, most of whom were female, in weight loss situations and they did not involve exercise, it may be inferred from the data that under mild energy deficits a higher level of protein in a diet is protein sparing.
The level of protein intake that will be necessary to assure nitrogen balance depends on the severity of the energy deficit but it will be somewhat greater than the RDA of 0.8g/kg/day (IOM, 2002a). At severe energy deficits of less than 50 percent of total energy expenditure, an intake of about 1.5 g/kg of body weight will maximize protein sparing effects (Hoffer et al., 1984). This study showed that moderately obese females on a diet to lose weight for periods of up to 4 weeks with caloric intakes of about 600–800 kcal and twice the energy expenditures achieved nitrogen equilibrium at 1.5 g/kg ideal body weight but not at 0.8g/kg protein (under eucaloric conditions). It has also been shown that in severely burned patients there is no further protein sparing when 1.4 g protein/kg versus 2.3 g protein/kg are provided (Patterson et al., 1997). Increases in energy expenditure through physical activity do not markedly alter protein requirements; thus, despite a likely energy deficit of 50 percent under combat mission conditions, protein intakes of somewhat less than 1.5 g/kg body weight/day would probably be sufficient for optimal sparing of lean tissue. Parenthetically, at this level of 1.5 g protein/kg body weight/day, this is also the maximal level of protein sparing found during severe catabolic illness and during repletion of malnourished subjects (Bistrian and Babineau, 1998; Wolfe et al., 1983). Thus, a recommendation of 1.2–1.5 g protein/kg body weight/day (i.e., 100–120 g total protein daily for an average body size of 80 kg) for the assault ration would be the committee’s best estimate to attenuate net nitrogen and lean body mass loss at the recommended energy level. This amount is in fact the intake by the average American (although, in percentage, is greater than the average intake). Although it can be argued that a high protein level will increase energy expenditures due to protein thermogenesis, based on a regression analysis by Westerterp (2004), the difference in thermogenesis for a diet with 0.8 or 1.5 g/kg of protein is estimated to be about 40 kcal, a rather small difference compared to the overall energy expenditures.
Synthesis of Serum Proteins. Over the expected short-term duration of assault missions, achievement of nitrogen balance may not be a sufficient criterion to establish the desirable protein level for the ration. Another criterion to be considered is the proper functioning of antioxidant systems. The stress response, whether due to intense physical activity or systemic inflammatory response leading to oxidative stress, may impair the amino acid and protein component of the antioxidant systems (Jackson et al., 2004). The glutathione redox cycle is one such antioxidant system and one of the most important body defense systems against metabolic stress. Glutathione is a tripeptide composed of the amino acids cysteine, glutamate, and glycine. Cysteine is the rate-limiting amino acid for glutathione synthesis (Lu, 1998). It has been postulated that feeding diets marginal in protein may affect glutathione synthesis given its need for a constant amino acid supply to produce the peptide (Jackson et al., 2004). The existence of an adaptation period to lower protein diets in experimental studies is well known. For example, when switching from a usual protein intake of 1.13 g/kg/day to the lower intake of 0.75 g/kg/day, nitrogen balance was negative for the first few days and reestablished after 10 days (Gibson et al., 2002). Other studies have found similar results (Pacy et al., 1994); nitrogen balance is restored by reducing whole-body protein turnover and net protein catabolism, which maintains the endogenous rate of indispensable amino acid synthesis (Gibson et al., 2002). However, although the plasma levels of albumin, HDL apolipoprotein A1, retinol-binding protein, transthyretin, haptoglobulin, and fibrinogen are maintained, the synthetic rates of nutrient transport proteins are not (Afolabi et al., 2004). In their latest study in which on days 3 and 10 the usual protein intake was decreased, erythrocyte glutathione concentrations and synthetic rates decreased by day 3 and recovered by day 10, but erythrocyte concentrations of the constituent amino acids of glutathione were still elevated at day 10, suggesting that functional changes occurred that were related to this lower level of protein intake (Jackson et al., 2004).
Although not studied in this experimental model, amino acid availability would also be an important factor in optimizing immune function (Moldawer et al., 1978). Prior to going into combat missions, trained soldiers will likely have a protein intake greater than the 1.13 g/kg used in these studies. They then will undergo metabolic or physical stress that will exacerbate the need for essential amino acids to mount an optimal stress response. This greater need constitutes an additional reason to provide a higher protein level than the RDA.
In summary, it is likely that neither nitrogen balance nor synthesis of serum proteins will be maintained with the RDA level of protein intake when consuming a hypocaloric diet under a highly stressful scenario. A high protein intake not only will spare muscle protein but also will contribute to energy needs. Although some of the findings are ambiguous, a higher protein level may also help improve immune function (Booth et al., 2003; Keenan et al., 1982) and cognitive function (Dye et al., 2000; Fischer et al., 2002; Holt et al., 1999; IOM, 1995; Keys et al., 1950).
Food Quality. Maintaining nitrogen balance and serum protein synthesis are, by themselves, valid reasons from a physiological standpoint to recommend a high protein level for this ration. Equally important is the need to enhance the sensory properties of food items to optimize acceptability. Food items with higher amounts of protein may in fact encourage higher consumption since a ration composed of foods that are naturally high in protein, such as meats, poultry, and nuts, introduces a variety of flavors and textures that have been shown to enhance food intake (Sorensen et al., 2003).
In conclusion, both from a physiological and food quality standpoint, a higher-protein ration is superior. There is little reason to believe that a hypocaloric diet, if otherwise adequate in protein as justified above and in other essential nutrients, presents any potential for harm when consumed over multiple brief periods of time (repetitive three- to seven-day periods for up to a month) even if some weight loss occurs. However, with the expected energy expenditures of 4,500 kcal/day during the missions, it is possible that some soldiers might lose as much as 10 percent body weight before the end of the month, even with refeeding between missions; this degree of weight loss could result in adverse, but mild, performance decrements. However, this level of weight loss is not likely to be of any serious consequences for health. Therefore, it is recommended that weight loss be measured after one month of use, and if weight loss is higher than 10 percent for a soldier, he should not be sent on assault missions until weight is regained to within 5 percent of initial weight.
Rationale for the Source of Protein
Evidence from acute metabolic studies in fasting subjects suggests that increased muscle protein synthesis and net muscle protein synthesis result from provision only of indispensable amino acids. That is, dispensable amino acids are unnecessary to stimulate muscle protein accretion (Borsheim et al., 2002; Tipton and Wolfe, 2001; Tipton et al., 1999, 2003). Furthermore, acute metabolic studies of fasting subjects showed that, following resistance exercise, 6 g of indispensable amino acids resulted in amino acid uptake that was more than double that of 20 g of whole proteins (Borsheim et al., 2002; Tipton et al., 2004). Another recent study showed that indispensable amino acids, when combined with exercise, ameliorated the amino acid release from muscle in response to a 20 percent energy deficit (Tipton et al., 2003). Although the addition of amino acids might benefit performance, however, the use of amino acids as a source of protein might not present additional benefits over and above the high-protein ration recommended by the committee.
The committee considered the addition of some specific amino acids, such as branched amino acids, glutamine, or arginine, because their consumption might result in physiological effects of interest. For example, glutamine has been promoted as an immune-enhancing nutrient, particularly when catabolic stress is
present as in trauma or infection; however, most of this benefit has been shown with glutamine delivered by parenteral routes (Novak et al., 2002) so that high serum glutamine levels could be achieved. Since the gastrointestinal tract metabolizes glutamine, it is difficult to achieve sufficient oral intake of glutamine to alter serum levels. Therefore, most clinical trials of oral glutamine have not been effective. Furthermore, glutamine is quite unstable and has a short shelf-life. Arginine has also been promoted for its immune-enhancing properties. It has some ability to improve hospital outcome in postsurgical patients, but only when provided with other putative immune-enhancing nutrients (Beale et al., 1999; Heyland et al., 2001; Heys et al., 1999). When provided alone, arginine has not been beneficial (Luiking et al., 2005) except in incidences of sepsis in critically ill patients. In addition, postsurgical patients are clinically much more susceptible to infection than are soldiers. Thus, inclusion of arginine as an amino acid supplement to the ration is not a high priority at this time.
Finally, the branched-chain amino acids isoleucine, leucine, and valine have been purported to improve skeletal muscle metabolism. The committee, however, concluded that at levels greater than those in 1.2 g/kg/day of high-biological-value protein, which contains 15–20 percent branched-chain amino acids, there is little likelihood that further provision of branched chain amino acids would be effective.
When whole proteins are added to food items, the biological value of the protein is an important consideration. Whole protein of high biological value is recommended for the ration. Examples include soy, casein, whey, and egg. Protein sources need to be relatively low in sulfur amino acids to maintain elevated urinary pH, because this decreases risk of stone formation. Although soy protein would be a good option as a protein source because it is low in sulfur amino acids, its relatively high level of oxalate could also increase the risk of stone formation (Massey et al., 2002). Net protein synthesis might also be influenced by the speed with which protein is absorbed (slow- versus fast-absorption protein) (Dangin et al., 2003). The committee concluded that, at the high level of protein intake recommended and with the high energy deficit, the rate of absorption from the small intestine will not significantly affect protein deposition.
Research Needs
-
Investigate the effects of the higher protein level recommended compared to maintenance protein intakes under high energy expenditure situations resulting in hypocaloric conditions and stress on muscle loss, physical and cognitive performance, and immune function. Muscle loss should be assessed by state-of-the-art techniques such as dual energy X-ray absorptiometry or whole-body nitrogen measurement. Physical performance should be assessed by measurement of maximal oxidative capacity, endurance, and strength. Immune function should be measured by both in vitro and in vivo methods.
-
Continue research efforts on the potential to improve physical and cognitive performance and immune function by supplementing diets with indispensable amino acids compared to supplementing with whole protein.
-
Conduct further research on the potential benefits of adding specific amino acids in addition to protein when subjects are consuming a hypocaloric diet under the environmental conditions and high-stress situations of combat missions. There is suggestive evidence obtained under significantly different conditions that warrants continuing research, specifically with arginine for immune enhancement and wound healing, and glutamine for intestinal function and immune function.
-
Investigate the influence of individual variability on the effect of high-protein diets on performance in hypocaloric states.
-
Study body composition and physical activity as factors that influence protein sparing and prevention of muscle loss.
Carbohydrate
RECOMMENDATION: The carbohydrate in the basic ration should be 350 g to optimize physical performance. An additional 100 g of carbohydrate should be available as a supplement. Therefore, the overall recommendation is for 450 g.
The committee considers palatability to be the major consideration in designing the food products to ensure ration consumption; thus, the food items and the carbohydrate supplement should provide a variety of flavors. The amount of fructose as a monosaccharide should be less than 25 g to avoid the possibility of osmotic diarrhea. Dietary fiber should be 15–17 g and should include both nonviscous, fermentable fiber (e.g., gums, pectin, β-glucans, soy polysaccharides) and viscous, nonfermentable fiber (e.g., cellulose, lignin, hemicellulose).
Background
Carbohydrate as an Energy Source. Carbohydrate is the major energy source for skeletal muscle and the brain. After ingestion, carbohydrate is digested into monosaccharides in the small intestine, absorbed, transported in the blood to the liver by way of the hepatic portal system, and then either removed by the liver or released into the circulation (Williams, 2005). Monosaccharides can be stored as glycogen in the liver or muscle or be used as immediate fuel by muscle and brain cells. Muscle glycogen is metabolized anaerobically through glycolysis in the cytoplasm, where glucose is converted to lactic acid units with the formation of small amounts of adenosine triphosphate (ATP), and aerobically, through glycolysis in the cytoplasm and the tricarboxylic acid cycle-electron transport
system in the mitochondria, resulting in the production of substantially more ATP (Powers and Howley, 1997; Wilmore and Costill, 1999).
In skeletal muscle, anaerobic glycolysis can produce a limited supply of ATP at a rapid rate compared with aerobic glycolysis, which can produce a greater amount of ATP, but at a slower rate (Powers and Howley, 1997; Williams, 2005, p. 91; Wilmore and Costill, 1999). Hence, short-term, high-intensity exercise, in which ATP is needed rapidly, relies predominantly on anaerobic glycolysis, while longer endurance activity relies predominantly on aerobic glycolysis. Glucose (or carbohydrate) ingested during exercise enters directly into these muscle metabolic pathways rather than being stored as muscle glycogen (Williams, 2005). Thus, carbohydrate is a versatile, important energy source in muscle for a wide array of physical activities.
Glucose is also the obligatory energy substrate for the brain (Rosenthal et al., 2001). Because glycogen levels in the brain are low compared to liver and muscle, a constant supply of glucose from the blood is necessary. Blood glucose is tightly regulated by hormonal control (insulin and glucagon) to maintain levels in a narrow range for optimal usage by brain cells. It has been proposed that high cognitive demand may activate specific brain areas and deplete glucose in that area, resulting in cognitive dysfunction (Rosenthal et al., 2001). Functional magnetic resonance imaging has been used to show that the brain oxygenation state is altered by hypoglycemia (Rosenthal et al., 2001). Whether increased cognitive demands during physical activity alter brain glucose needs is unknown.
Carbohydrate for Physical Performance. In the muscle, stored carbohydrate (glycogen) can be used for both anaerobic (short-term, high-intensity) and aerobic (endurance) activity (Powers and Howley, 1997; Williams, 2005; Wilmore and Costill, 1999). During rest, carbohydrate supplies about 15–20 percent of the muscle’s energy need, while during moderate intensity exercise, carbohydrate use increases to over 50 percent and becomes greater as the intensity of exercise is increased (Williams, 2005). Muscle can also draw glucose from the circulation and from the liver to augment energy production. Carbohydrate is more efficient than fat as a fuel, and the rate of supply of ATP for muscle contraction is faster than that of fat. Therefore, maintaining muscle glycogen and blood glucose levels is important for optimal physical performance.
Muscle glycogen levels are directly related to the amount of carbohydrate in the diet. On high-carbohydrate diets (80 percent of total energy), more muscle glycogen is stored compared to a normal carbohydrate diet (55 percent of total energy) (Bergstrom et al., 1967). Early studies found that endurance performance (time to exhaustion) (Ahlborg et al., 1967; Bergstrom et al., 1967) or ability to maintain optimal running pace (Karlsson and Saltin, 1971) was directly related to the initial muscle glycogen level in the exercising muscle.
Athletes ingesting a low-carbohydrate diet (40 percent of total calories) were not able to maintain muscle glycogen levels compared with athletes who ingested a high-carbohydrate diet (70 percent of total calories) (Costill and Miller, 1980).
Diets low in carbohydrate and low muscle glycogen levels were associated with suboptimal performance (Costill and Miller, 1980; Costill et al., 1988). The consumption of either normal or amplified food rations (increased calories and the proportion of carbohydrate) showed no difference in the effect on muscle glycogen level during 4.5 days of field exercises, although in both cases muscle glycogen was severely depleted (Jacobs et al., 1983). These data suggest that extra carbohydrate is used immediately for energy production in muscle, rather than being stored as muscle glycogen. Sufficient carbohydrate is important for maintaining optimal performance during sustained military operations (see Tipton, 2004 in Appendix B).
Carbohydrate Supplementation to Optimize Performance. Because those engaged in strenuous physical activity require an increased amount of carbohydrate to optimize performance, carbohydrate is often supplemented, especially in the form of beverages that also serve to maintain hydration. As reviewed by Coyle (2004 in Appendix B), carbohydrate ingestion has been shown to benefit performance of moderate- to high-intensity continuous or intermittent exercise lasting more than one hour. Convertino et al. (1996) recommended that carbohydrate be ingested at a rate of 30–60 g/hour to maintain carbohydrate oxidation and delay fatigue. Friedl and Hoyt (1997) reviewed the history of military nutrition research in the past century and concluded that one way to deal with the reduced energy intake (≤ 3,000 kcal/day) during field training when energy expenditure could be 4,000 kcal/day or higher was to provide soldiers with a carbohydrate-electrolyte beverage supplement. Typical carbohydrate intake of soldiers in the field is about 300 g/day (Friedl and Hoyt, 1997), which would fall short of the 464–608 g/day or more that may be needed as cited in the next section, Rationale for the Level of Carbohydrate. Therefore, some means to supplement carbohydrate in the diet would appear critical for optimizing performance of soldiers in the field.
Although most research studies examined the effect of supplemental carbohydrate on sport or exercise performance (Coyle, 2004 in Appendix B), research has demonstrated that carbohydrate will also improve performance on military tasks. Tharion and Moore (1993) randomly assigned 15 male soldiers to a 250, 400, or 550 g carbohydrate diet (with total caloric content and protein constant) for a four-day period. These subjects performed a marching exercise on a treadmill for up to 4 hours at the rate of 3.5 mph while carrying a 45 kg backpack. Accuracy and speed for a rifle shooting test were assessed before and after the exercise. A significant deterioration in shooting performance occurred after the exercise when the 250 g carbohydrate diet was followed, but there was no significant decrement in performance for the 400 or 550 g carbohydrate diet.
To evaluate the effect of supplemented carbohydrate on total food intake and activity, the voluntary energy and carbohydrate intake of Marines who were randomly assigned to either a carbohydrate-beverage supplement or a noncaloric placebo beverage during an 11-day field training exercise was estimated, along with energy expenditure (Tharion et al., 2004). Both groups received a similar
total amount of carbohydrate in the food ration. Energy expenditure was assessed by doubly labeled water techniques. Exercises included bouts of repetitive lifting of a 45 kg weight, running, calisthenics, and routine manual work. The total carbohydrate ingested by the carbohydrate-supplemented group averaged 470 g (293 g in the ration, 177 g supplemented), and the corresponding values for the placebo group were 317 g (310 g and 7 g, respectively). Total energy intake of the carbohydrate-supplemented and the placebo groups was 3,120 kcal (13.1 MJ) and 2,670 kcal (11.2 MJ), respectively. Total energy expenditure was 4,380 kcal (18.4 MJ) and 3,840 kcal (16.1 MJ) for the carbohydrate-supplemented and the placebo group, respectively, with no significant difference between groups. The carbohydrate-supplemented group consumed an additional 153 g of carbohydrate and 450 kcal (1.9 MJ)/day of energy. Thus, providing a carbohydrate beverage may reduce energy and carbohydrate deficits that commonly occur during field training (Tharion et al., 2004). It should be noted that this increase in carbohydrate intake was concomitant with a slight decrease in protein intake (105 g protein intake in the placebo group versus 93 g in the experimental group). Although such a slight decrease might not result in adverse effects, the committee cautions that protein intake should remain at the recommended level and should not be compromised when a carbohydrate supplement is provided to increase energy intake.
In another study of military subjects, 27 infantry soldiers were fed diets containing approximately 2,600 kcal/day during three days of field training in hot humid conditions (30°C, 60 percent relative humidity) (Montain et al., 1997). The soldiers were randomly assigned to groups receiving a carbohydrate-electrolyte, placebo, or water beverage. The carbohydrate-electrolyte beverage provided an additional 1,000 kcal/day. The groups ingested on average a total of 462, 175, and 217 g/day of carbohydrate, respectively, while fluid intake was not different among the groups. Soldiers drinking the carbohydrate-electrolyte beverage were more likely to maintain their performance during the uphill run and the marksmanship performance.
Environmental factors also affect the amount of carbohydrate needed. Montain and Young (2003) summarized a study of Askew et al. (1987) who showed that soldiers who ingested carbohydrate-electrolyte drinks compared to a placebo during four days at an altitude of 4,100 m consumed 250 additional grams of carbohydrate and covered more distance during a two-hour run than the placebo group. In hot environments, greater muscle glycogen use during exercise in the heat (41°C) than in cold conditions (9°C) has been demonstrated in a number of studies (Febbraio et al., 1996, Fink et al., 1975). Although two studies have reported that supplemental carbohydrate during exercise in the heat did not improve performance (Febbraio, 2001; Febbraio et al., 1996), the addition of 204 g of carbohydrate in water was found to be more effective in maintaining cycling performance over two hours than water or carbohydrate alone (Fritzsche et al., 2000). These last results suggest that carbohydrate supplementation during
endurance performance in the heat, when dehydration is not a factor, benefits performance by increasing blood glucose uptake and oxidation. Thus, supplemental carbohydrate in a fluid should provide a valuable energy source in field situations that require continuous physical activity.
Carbohydrate for Cognitive Performance. Nutrient influences on psychological and behavioral functions have been reviewed (Dye and Blundell, 2002) and the results of trials exploring nutrient effects on commonly assessed aspects of cognitive performance summarized. Cognitive performance functions include reaction time (simple and complex), vigilance/attention, information processing, memory, reasoning, and psychomotor performance. Nutritional interventions that increase blood glucose appear to improve reaction times in a few studies, while carbohydrate-rich foods may impair reaction times under some circumstances in other studies. Still others find either no effect or improvement (Dye and Blundell, 2002). Similarly, various studies of vigilance and attention found that high-carbohydrate meals, compared to low-carbohydrate meals, led to performances that were better, worse, or no different. Memory is improved when glucose is given, but carbohydrate in other forms has had more variable effects (Dye and Blundell, 2002).
These generally inconclusive results are not surprising given that the studies typically involved very brief (often, one meal) nutritional interventions usually of unstressed adults in sedentary conditions, in addition to varying the methodologies and nutritional manipulations. Importantly, “It is also clear that cognitive performance is normally well protected by a regulatory process that maintains a stable output” (Dye and Blundell, 2002).
Studies of the effects of nutritional interventions on cognitive performance in more challenging settings of high-energy output and physical or psychological stress are therefore more germane to the uses of the assault ration. Such studies offer situations that are more analogous to the demands of assault missions in that they may draw on the participants’ resources to the point at which cognitive decrements might ordinarily be observed.
Other reviews have pointed out that, although performance benefits from supplemental carbohydrate can often be ascribed to effects on metabolism, other factors may also play a role (Coyle, 2004; Kaplan, 2004 in Appendix B). In this regard, several studies have reported the benefits of supplemental carbohydrate feeding when fatigue is not due to a lack of aerobic or anaerobic carbohydrate energy. The exercise tasks used in these studies are general stop-and-go, high-intensity exercise (Coyle, 2004). Performance benefits in this case may be due to preventing a decline in cognitive function. For example, in one study subjects ingested either a carbohydrate-electrolyte beverage or placebo before and during a shuttle-running protocol (Welsh et al., 2002). The carbohydrate-electrolyte beverages (overall ~127.5 g supplemented carbohydrate) enhanced performance, and there was a self-reported reduction of perceived fatigue (assessed by Profile of Mood States [POMS] and improved motor skill performance). In a random-
ized cross-over design, a high-carbohydrate (8.5 g/kg body weight/day) diet was compared to normal carbohydrate diet (5.4 g/kg body weight/day) over the course of 11 days, including seven days of intense physical training (Achten et al., 2004). The high-carbohydrate diet resulted in better maintenance of running performance and global mood state (assessed by the POMS test). Both groups, however, were on fairly high-carbohydrate diets (e.g., for an 80 kg person approximately 432 g and 680 g, respectively).
Using a within-subjects design, changes in reaction times after 100-minute runs were assessed in well-trained athletes, but gender was not specified (Collardeau et al., 2001). The reaction time trials consisted of (1) simple reaction time, where subjects were instructed to lift their thumb off a button in response to a stimulus, and (2) choice reaction time, where subjects were instructed to move a handle in one of four directions as indicated by an arrow on a computer screen. The time to respond to the stimulus was the criterion measured. Subjects received 8 ml/kg body weight of a solution prior to the session followed by a 2 ml/kg body weight every 15 minutes. The solution contained either 5.5 percent carbohydrate (glucose, fructose, maltodextrins) or placebo, with equal electrolyte content. While no effect of supplementation was observed on simple reaction time, the carbohydrate solution (but not the placebo solution) was associated with a significant improvement in complex reaction time immediately after the exercise session, as well as a smaller increase in ratings of perceived exertion over the session.
In another study, 143 young healthy male soldiers were randomly assigned to one of three groups who were given the following supplemented beverage: 6 percent carbohydrate (2.1 g/kg), 12 percent carbohydrate (4.2 g/kg), or placebo beverage. Over the 10-hour study, subjects performed a 19.3 km road march and two 4.8 km runs interspersed with rest and other activities (Lieberman et al., 2002). Vigilance as measured by reaction to an auditory signal improved in a dose-related manner with the percentage of carbohydrate. The negative components of mood (confusion, lack of vigor) as assessed by the standardized POMS test were reduced with the additional carbohydrate. Although carbohydrate supplementation appeared to enhance cognitive performance in individuals engaged in sustained, intense physical activity (Lieberman, 2003), it should be noted that no eucaloric control was used. Thus, increased energy intake may have produced the improvements in vigilance and mood.
It is important to note that the POMS test was designed to measure changes in mood states occurring over a period of a week or more (Lorr et al., 2003) and that it was originally designed to measure mood states among psychiatric patients. Since then, it has been used to measure mood changes in other populations (including sport psychology studies of athletes and studies of medical patients). POMS has not been validated to assess psychologically healthy individuals or to assess changes within shorter time frames (e.g., pre- and postexercise bouts). In addition, the POMS test assesses self-rated emotional states rather than objec-
tively measured neurocognitive performance. While both are psychological domains, they typically are treated separately and there is usually little reason to assume that findings in one domain apply to the other.
Rationale for the Level of Carbohydrate
Carbohydrate Needs for Intense Physical Activity. The new Acceptable Macronutrient Distribution Range (AMDR) of the Dietary Reference Intakes (DRIs) (IOM, 2002a) states that normal, healthy adults should get 45–65 percent of their calories from carbohydrates. The amount of carbohydrate that others have recommended for athletes is 60–70 percent of total energy intake (Anonymous, 1991). It has been suggested, however, that the daily recovery amount of carbohydrate for athletes be expressed in grams per kilogram body weight, and the amount recommended should depend on the level of training (Burke et al., 2004). Using this approach, recommendations for recovery from moderate-duration, low-intensity training are 5–7 g/kg body weight/day, moderate to heavy endurance training 7–12 g/kg body weight/day, and extreme exercise (defined as > 4 hr/day) 10–12 g/kg body weight/day (Burke et al., 2004). For an 80 kg man, the amount of carbohydrate for recovery from moderate to heavy endurance training would be 560 to 960 g. Reviews of diet surveys of nonendurance and endurance male athletes showed daily carbohydrate intakes of 5.8 and 7.6 g/kg body weight/day respectively, which, for an 80 kg male athlete would range from 464 to 608 g (Burke et al., 2004). Given the weight and volume constraints of the ration and needs for other nutrients, the committee recommends including 350 g/day of carbohydrate in the basic ration. This level, however, will not be sufficient to meet the needs of soldiers in high-intensity military operations. In addition to the 350 g in the basic ration, the committee recommends including an extra 100 g of carbohydrate as supplements in the form of gels, candy, or powder to be added to beverage. In this way, the total recommended amount of carbohydrate is 450 g. This amount is the minimal amount of carbohydrate needed to meet the needs of soldiers experiencing intense physical activity.
Carbohydrate Needs for Cognitive Function. Although some studies described above have found that carbohydrate may improve vigilance and reaction time, improvements in other cognitive domains associated with carbohydrate consumption have not been found. Hence, there is a lack of conclusive results on the effect of carbohydrate on cognitive performance. Also, most studies have relied on subjective methodologies that have not been validated for the scenarios of concern. The committee recommends that researchers seeking to determine the effects of carbohydrate on cognitive function develop and use tests that fall within the domain of neurocognitive functioning (e.g., attention, vigilance, short-term memory, reaction time, problem-solving ability) rather than the emotional domain (e.g., depression, anxiety, anger). In summary, although some studies have found that carbohydrate may improve vigilance and reaction time, there is
no conclusive evidence to recommend specific levels of carbohydrate to enhance cognitive function.
Rationale for Type of Carbohydrate
The type of carbohydrate in the food ration menu items should be a mixture of complex and simple carbohydrates so that the food is palatable (not too sweet). Fructose as a monosaccharide should be limited due to the association between dietary fructose and diarrhea (Skoog and Bharucha, 2004). Some studies have found that dietary glucose increases the absorption of fructose, so the recommended use of a mixture of carbohydrates should limit the malabsorption of fructose (Skoog and Bharucha, 2004; Truswell et al., 1988). Because reports that consumption of 25 g of fructose as a monosaccharide for three consecutive days caused malabsorption symptoms in healthy adults (Born et al., 1994), the amount of fructose as a monosaccharide should be less than 25 g.
The supplemental carbohydrate should be available in easily digestible forms, such as powder to mix in with water (to a 4–8 percent solution) (Coyle and Montain, 1992), in carbohydrate gels, or in candy. A study by Murray and colleagues in which gastric emptying of exercising subjects was measured after drinking water or carbohydrate beverages suggests that gastric emptying significantly decreases after the 8 percent carbohydrate beverage; this decrease was not observed with either water or 4 or 6 percent carbohydrate beverages. The authors concluded that such a delay is not optimal for fluid replacement (Murray et al., 1999). Therefore, the concentration (and possibly type of carbohydrate) should be an important consideration when developing a carbohydrate beverage. As mentioned in the section above, supplemental carbohydrate delivered in fluid form should provide the most benefit to performance compared to carbohydrate alone (Fritzsche et al., 2000).
Rationale for Amount and Type of Dietary Fiber
The adequate intake (AI) for dietary fiber is based on 14 g dietary fiber/1,000 kcal, a level that has been shown to decrease risk of cardiovascular disease by virtue of its presence in foodstuffs in the gut (IOM, 2002a). Although the consumption of high amounts of total dietary fiber is desirable to reduce the risks of chronic diseases, in the case of short-term missions, avoiding diarrhea and constipation and decreasing stool weight are of greater concern to the military. Therefore, it is recommended that the range of dietary fiber in the assault ration be based on a minimum amount to avoid constipation to the extent possible and on estimates of the intake of young men in the US population. It is assumed that these amounts should prevent diarrhea and constipation. The estimated median intake and the 95th percentile intake from the Continuing Survey of Food Intake for Individuals in 1994–1996 (CSFII, 1998) in the United States for men 19–30
years old is 17.4 and 32.3 g/day of total dietary fiber, respectively (IOM, 2002a). When adjusted for the lower energy intake of the soldiers (approximately 2,400 kcal) compared to the normal population (median and 95th percentile intake of 2,718 and 4,374 kcal, respectively [IOM, 2002a]), the median intake and the 95th percentile would be approximately 15 and 17 g/day, respectively.
The type of fiber is also important. Both viscous and nonviscous fiber typically found in foods of plant and vegetable origin are important (IOM, 2002a). The available literature suggests that the viscous (liquid-like but thick and resistant to flow), nonfermentable fiber can alter blood glucose and cholesterol concentrations and optimize laxation; nonviscous, fermentable fiber can also impart beneficial effects, such as act as immunomodulators. Beta-glucan might be included as an example of a nonviscous, fermentable fiber. Beta-glucan has been evaluated as an immunostimulant and can be fermented into short-chain fatty acids in the large bowel, which improves intestinal function (i.e., acts as prebiotics) (Brown and Gordon, 2003; Frank et al., 2004). In addition, β-glucan may decrease blood cholesterol levels, and, therefore, the risk of coronary heart disease. The Food and Drug Administration recently recognized these benefits by approving the health claim that β-glucan may reduce the risk of coronary heart disease (Food Labeling. Specific Requirements for Health Claims. 21 C.F.R. §101, 2002).
Based on the median and 95th percentile intake adjusted for energy intake, the committee recommends including total dietary fiber in the range of 15–17 g/day. The committee concluded that a mixture rather than a single source of fiber might be better tolerated physiologically and may help prevent constipation. Therefore, the committee recommends that the amount provided include nonviscous, fermentable fiber (e.g., gums, pectin, β-glucans, soy polysaccharides) as well as viscous, nonfermentable fiber (e.g., cellulose, lignin, hemicellulose).
Research Needs
-
Investigate the type of carbohydrate (disaccharides versus starches) that best enhances physical and cognitive performance.
-
Determine whether specific fiber types will reduce the incidence of diarrhea.
-
Determine the carbohydrate “dosing/delivery” schedule (e.g., continuous versus bolus) that will contribute to best improving physical and cognitive performance.
-
Confirm the effects of carbohydrate on performance and cognition under conditions analogous to the high-stress situations of military operations.
Fat
RECOMMENDATION: After protein and carbohydrate needs are met, the ration should provide 58–67 g fat (22–25 percent of energy intake) to be
distributed across a variety of foods. The ration should provide a balance of dietary fatty acids between monounsaturated, polyunsaturated, and saturated fats, with at least 17 g linoleic acid and 1.6 g α-linolenic acid, recognizing essential fatty acid needs as well as the undesirable pro-oxidant properties of large amounts of unsaturated fatty acids. This balance can be determined by food formulation criteria. There is no recognized benefit to modifying fatty acid type in the ration or to adding structured lipids.
Background
The primary reason for fat in the ration is to provide a readily digestible, palatable, energy-dense source of calories to help soldiers perform physically and cognitively demanding military operations. Since appetite may be depressed under conditions of high-intensity physical activity and stress, maximal consumption of the ration is a primary goal. Fat provides a highly palatable source of calories that can be expected to promote ration intake. Among energy sources, fat has been shown to be less satiating (Gerstein et al., 2004; Mattes, 2004 in Appendix B), which should increase consumption under field conditions. In addition, recent studies indicated that greater satiety results from consumption of foods higher in protein and carbohydrate than fat (see also Chapter 3). While the desire to increase ration consumption as much as possible would support the addition of a higher level of fat, increasing the fat content would result in a decrease in the amount of carbohydrate or protein in the ration. The committee believes that, although increasing consumption is desirable, satiety is only one of the many factors that influence consumption, and the available data do not yet provide an unequivocal answer. A better understanding of the influence of nutrient composition on satiety is needed before considering it as the basis for nutrient level recommendations.
Other roles of fat must be considered as well. The ration must also satisfy essential fatty acid needs. In addition, dietary fat is frequently the vehicle for intake and absorption of fat-soluble vitamins. It can be assumed, however, that healthy young men will have adequate fat-soluble vitamin stores and that, as depot fat is utilized to meet energy needs, such fat will be the main source of fat-soluble vitamins. Thus, this role of dietary fat is not of consequence, although some supplementation with fat-soluble vitamins beyond what is naturally present in the food items may be required.
Rationale for Level of Fat
Fat as a Fuel Source. Several factors were taken into consideration in setting the fat level. First, the levels of macronutrients recommended are meant to optimize protein and carbohydrate intake. The rationale for setting the levels of protein and carbohydrate in the ration are described in detail earlier in this chapter.
Briefly, they are based on the facts that the physical demands of high-intensity military operations require a high contribution of protein to preserve lean mass, and that a high contribution of carbohydrate will maintain vigilance and physical performance. The committee concludes that, after protein and carbohydrate needs are met, fat should be used to maximize palatability and energy density.
Maintaining carbohydrate availability to muscle is critical for sustained, intense, physical activity. Numerous studies show that carbohydrate benefits performance. For example, Coyle and colleagues (1986) demonstrated that feeding carbohydrate during prolonged strenuous exercise results in high enough carbohydrate oxidation to delay fatigue. Hawley and colleagues showed improved performance capacity with high-carbohydrate diets (Hawley et al., 1997). Whether the improvement in performance occurs because the intake of carbohydrate spares muscle glycogen or because blood glucose levels are maintained is still not clear. Conversely, fat feeding induces a higher rate of fat oxidation and a rapid repletion of muscle triacylglycerol stores (Hawley, 2000). Carbohydrate, however, is more efficient than fat as a fuel and carbohydrate’s rate of supply of ATP for muscle contraction is faster than that of fat. Among the macronutrients used as fuel, fat offers the advantage of providing the highest amount of calories per gram; that is fat, provides 9 kcal/g of energy compared with 4 kcal/g for protein and carbohydrate. A recent theory suggests that high-fat feeding (≥ 65 percent energy) provides an alternate fuel source, which might help to preserve muscle glycogen or slow its rate of use (Burke and Hawley, 2002; Helge, 2000). Accordingly, there might be some advantage to manipulating the diet to modify the pattern of fuel utilization to preserve or enhance performance. Currently, however, evidence in support of this theory is not convincing. A recent review of the literature concluded that fat adaptation over one to three days was not sufficient to elicit the purported metabolic shift in favor of fat utilization (Burke and Hawley, 2002). Likewise, fat adaptation over a longer period (more than seven days) did not provide performance benefits, and in some cases led to performance decrements. Switching from fat adaptation to high-carbohydrate intake did result in higher rates of fat oxidation and concomitant muscle glycogen sparing; however, this strategy did not benefit physical performance (Helge, 2000; see Helge, 2004 in Appendix B).
Two studies compared the effects of high-fat versus high-carbohydrate feeding on cognitive outcomes during endurance training. In both studies, subjects were able to complete the training, but those on high-fat feeding experienced higher perceived exertion and reported that they required more mental effort to complete the task than those on high-carbohydrate feeding (Marsh and Murlin, 1928; Stepto et al., 2002).
During military operations, high energy expenditure is likely to occur in the context of an energy deficit. None of the studies cited above considered the dual burdens of intense physical work and energy deficit on physical performance. This situation is somewhat unique to the military, and few research studies have
investigated this interaction; however, one study in men who traversed the Greenland icecap on cross-country skis pulling sleds is instructive (Helge et al., 2003). The men were in energy deficit of approximately 1,000–1,500 kcal/day and consumed 30–40 percent energy as fat and 50–60 percent energy as carbohydrate. This macronutrient mix was sufficient for the men to complete their task.
Another study with distance runners varied the amount of dietary fat (17 percent, 31 percent, or 44 percent energy as fat) to maximize energy and nutrient intakes. Energy intakes were lower than energy expenditure under all feeding conditions, over approximately 30 days. However, energy intakes were higher on the medium- and high-fat diets, and subjects reported being less hungry on them. While on the 31 percent fat diet, male runners consumed 2,900 kcal/day, and intakes of essential fatty acids and vitamins were adequate (Horvath et al., 2000). For the purposes of energy delivery, it seems desirable to provide 30–40 percent of the energy in the ration as fat. Increasing the fat beyond this level does not appear to improve physical or cognitive performance. In addition, a period of 14–21 days is needed to metabolically adapt to a high-fat diet, which is beyond the period of intermittent use for this ration (Phinney et al., 1983). Given the energy recommendation of 2,400 kcal/day as well as protein and carbohydrate needs for health and performance, a ration providing 22–25 percent energy as fat appeared to be a reasonable level of intake. This level of total fat will likely provide acceptable palatability while serving as an important source of energy. In support of this level, the energy density of the average man’s food is 1.91 kcal/g (Ledikwe et al., 2005) which is similar to the recommended ration’s energy density of 2.03 kcal/g (1,360 g [total weight]–181 g [packaging] = 1,179 g; 2,400 kcal/1,179 g = 2.03 kcal/g).
Fat and Palatability. An ongoing concern for the military is that soldiers do not eat enough during field operations (IOM, 1995), particularly during high-intensity combat situations (Popper et al., 1989). Intense physical activity and stress are known to reduce food intake in trained athletes (King et al., 1997); however, the combined effects of highly intense physical activity, acute stress, and energy deficit on appetite mechanisms are poorly understood. Again, this combination of factors is rarely encountered outside the military context and has been seldom studied. Since both hunger and the motivation to eat may be compromised in soldiers during high-intensity field operations, it seems prudent to maximize the palatability of the ration to the extent possible.
It is well known that taste is a primary determinant of food choices (Glanz et al., 1998). Energy-dense foods such as fats are generally preferred over low-energy foods and seem to enhance overall food intake (Drewnowski, 1997). Nevertheless, there is considerable individual variation in the preferred level of fat in specific foods and for the diet as a whole (Cooling and Blundell, 2001; Mela and Sacchetti, 1991). The biological and personal factors that contribute to these differences are not well understood and need further study.
For the purposes of this report, typical intakes could be considered as an index of acceptable levels of fat in the diet. The mean estimated fat intake of young adult men in the general population is 33 percent (IOM, 2002a). Also, evidence from population studies suggests that diets providing less than 30 percent energy as fat can be well tolerated, particularly by highly motivated individuals. In the Women’s Health Initiative, participants in the intervention group adhered to a diet providing approximately 25–27 percent energy as fat for five years (Women’s Health Initiative Study Group, 2004). The FSRs, which are under development by the USARIEM, provide approximately 27 percent energy as fat. The military reports that FSRs are almost completely consumed in limited field tests (personal communication, C. Koenig, USARIEM, November 19, 2004). Whether the FSR provides the preferred level of fat for elite war fighters is unknown and should be ascertained in future studies. Nevertheless, based on previous experience, it is reasonable to assume that a ration providing 22–25 percent energy as fat will be relatively well accepted by soldiers in the field. Every effort should be made to optimize fat content and palatability of the ration design.
Rationale for Type of Fat
The polyunsaturated fatty acids (PUFA) omega-6 (n-6) and omega-3 (n-3) are essential in the human diet. The ration should contain, at a minimum, the recommended amounts of linoleic and α-linolenic acid to satisfy essential fatty acid needs. The effects of fatty acid type, including n-3 and n-6 fatty acids, on physical and cognitive performance, immune function, and gene expression. There is some evidence that feeding n-3 fatty acids improves endurance performance in rats (Ayre and Hulbert, 1996) and increases aerobic capacity and intracellular fatty acid transport in skeletal muscle (Clavel et al., 2002); however, the evidence for these effects in humans is extremely limited (Lukaski et al., 2001). Other evidence suggests that n-3 fatty acids, especially in combination with protein supplements, increase muscle mass and protect against muscle wasting in cancer patients (Barber et al., 1999; Fearon et al., 2003). Although these findings are provocative, they have little application to the military context at this time.
Recommended intakes of PUFA for the assault ration are thus set at the AI for men ages 19–30 years and should be at least 17 g/day of n-6 PUFA (as linoleic acid) and 1.6 g/day of n-3 PUFA (as α-linolenic acid) (IOM, 2002a). In addition, the committee believes the ration should provide for the potential health benefits of PUFA related to cardiovascular disease without unduly increasing potential pro-oxidant activity (IOM, 2002a). To that end, the committee recommends that the AMDR for these fatty acids (5–10 percent of energy from linoleic acid and 0.6–1.2 percent of energy from n-3 fatty acids [as α-linolenic acid; IOM, 2002a]) be taken into consideration in formulating food products for the ration.
The effects of structured lipids (including medium-chain triglycerides and conjugated linoleic acid) on exercise performance were also considered. Studies reviewed by Jandacek (IOM, 1994) and more recent data (Vistisen et al., 2003) found no improvement in performance with structured lipids. The committee concluded that there is insufficient evidence at this time supporting a benefit of these lipids on performance. The committee recommends that the ration contain a balance mix of saturated, polyunsaturated, and monounsaturated fatty acids, with palatability and stability the prime determinants of the specific mixture.
Research Needs
-
Study the combined effects of intense physical activity, acute stress, and energy deficit on hunger and appetite.
-
Explore the potential role of n-3 and n-6 fatty acids in immune and brain function.
-
Investigate the biological and personal factors that influence food preferences and diet palatability.
-
Develop a systematic approach to optimizing ration palatability, which would incorporate the wants and needs of end-users, early in the design process.
QUESTION D
What are the types and levels of micronutrients such as direct antioxidants (e.g., vitamin C and E, carotenoids), cofactors in antioxidant and other biochemical reactions with high metabolic flux (e.g., B vitamins, zinc, manganese, copper), or other bioactives (e.g., caffeine) that could be added to such rations to enhance performance during combat missions?
Vitamin A
RECOMMENDATION: The assault ration should contain at least 300 µg retinol activity equivalents (RAE)/day and no more than 900 µg RAE/day based on prevention of night blindness and the current RDA.
Background
Vitamin A is essential for vision, growth, cellular differentiation, integrity of epithelial cells, and the reproductive and immune systems. The RDA is set at 900 µg RAE/day for men (IOM, 2001b) based on the amount required to maintain a body pool in well-nourished subjects with liver reserves of 20 µg RAE/g (estimated four months of body storage) (Haskell et al., 1997; IOM, 2001b). The
Tolerable Upper Level (UL) for men was established at 3,000 µg of preformed vitamin A per day based on risk of liver abnormalities (IOM, 2001b).
In National Health and Nutrition Examination Survey (NHANES) III, the median and the 95th percentile dietary intake of vitamin A for 19- to 30-year-old men in the United States was 744 and 1,487 µg RAE/day, respectively (IOM, 2001b). There is no evidence of vitamin A inadequacy among the adult US population. An early symptom of actual deficiency is night blindness; that is, the inability to adapt to night vision due to impaired regeneration of rhodopsin. Although vitamin A deficiency is not a public health problem in the United States, it is a continuous concern in developing countries, and when diets are inadequate, supplementation reduces the risk of mortality of children and infants.
Rationale for Levels of Vitamin A
As much as 90 percent of vitamin A total body stores is in the liver (Olson, 1987), and liver stores of vitamin A are high in the US population. Using radioisotopic methods, researchers have estimated the retention of consumed vitamin A to be 50 percent (Bausch and Rietz, 1977; Sauberlich et al., 1974). There is little or no evidence of vitamin A inadequacy among the adult US population (IOM, 2001b).
An adequate level of vitamin A is critical for successful performance of certain tasks in the military. For example, optimal night vision is a consideration that may determine vitamin A requirements for the combat ration. Although there is a clear association between vitamin A deficiency and night blindness, the high liver stores exhibited by the US population would ensure an adequate supply of vitamin A to peripheral tissues. Moreover, there are no known reports of night blindness among the troops. Nevertheless, to err on the conservative side, the committee recommends a level of vitamin A that would prevent night blindness. Studies on adaptation to darkness in developing countries or clinical research studies (Batchelder and Ebbs, 1943; Blanchard and Harper, 1940; Hume and Krebs, 1949; Sauberlich et al., 1974) indicate that 300 µg RAE is the median intake in adults to prevent night blindness (i.e., the Estimated Average Requirement [EAR] because an RDA for night blindness prevention could not be calculated due to the high variability in the data) (IOM, 2001b). This level, 300 µg RAE, should be considered the minimum amount in the short-term assault rations. The committee recommends an upper limit of 900 µg RAE/day. This level represents the RDA for men, which is estimated to provide four months of liver stores of vitamin A for 97–98 percent of the population (IOM, 2001b). There are no toxicity concerns at these levels.
Food Form
The sources of vitamin A could be included as preformed vitamin A or provitamin A carotenoids. All of these forms could be found naturally in foods
(e.g., animal-derived foods, fruits, vegetables, and cereals); food could also be fortified to achieve a level of vitamin A within the recommended range.
Vitamin C
RECOMMENDATION: The assault rations should include a vitamin C level of 180–400 mg. This level considers the current RDA for US males 19–30 years old, 90 mg/day, plus 35 mg/day to account for the higher vitamin C requirements of smokers; to establish the lower limit of the range (180 mg), another 50 percent was added due to the potential degradation of vitamin C over the shelf-life of the ration. The upper level is the 95th percentile dietary intake of vitamin C. To minimize its interaction with pro-oxidants in the ration and further degradation, encapsulation of vitamin C should be considered. If shelf-life of the ration is such that degradation would not occur, then a lower amount (< 400 mg) should be considered as the upper end of the range.
Background
The biological function of vitamin C comes from its ability to donate reducing equivalents to reactions, including reduction of reactive oxygen that damages cells. Vitamin C is the electron donor for eight enzymes involved in collagen hydroxylation, carnitine biosynthesis, and hormone and amino acid biosynthesis. Vitamin C deficiency is characterized by impairments in connective tissue, specifically impairment of collagen synthesis. Vitamin C has also been shown to affect components of the immune response (IOM, 2000). The RDA for vitamin C was based on maintaining near-maximal neutrophil concentrations with minimal urinary loss at 90 mg for men. The median intake and the 95th percentile intake of US males ages 19–30 is 127 mg and 400 mg, respectively. The UL is set at 2 g/day based on a criterion of gastrointestinal disturbance (IOM, 2000).
Rationale for Levels of Vitamin C
Vitamin C as Antioxidant. Although the properties of vitamin C as an antioxidant suggest that a high level of vitamin C intake might prevent oxidative damage and muscle injury associated with high-intensity exercise, recent studies have indicated that supplementing the diet with vitamin C at doses of 200 and 1,000 mg does not affect markers of muscle damage, soreness, or interleukin (IL)-6 after eccentric exercise (Thompson et al., 2001, 2004). In addition, contrary to the antioxidant theory, other studies suggest that high-dose vitamin C supplementation could result in pro-oxidant adverse effects (Childs et al., 2001).
Vitamin C could exert an antioxidant effect by serving as an electron donor
to oxidized vitamin E that is created (in reaction to oxidative stress) during exercise (Evans, 2000). The combination of vitamin C (500 mg) and vitamin E (up to 1,200 international units [IU]), however, shows mixed effects on signs and symptoms of muscle damage (e.g., muscle soreness and swelling were not affected, whereas maximal voluntary isometric contraction force and eccentric contractile torque and work were affected by the supplementation) (Shafat et al., 2004). The potential benefits of antioxidant supplementation were investigated in a study that provided ultramarathon runners with vitamins E (300 mg) and C (1,000 mg) for six weeks. The supplemented group was protected from lipid oxidation as evidenced by the lower level of F2-isoprostanes; however, there was no marked effect on inflammatory markers, muscle damage markers. or DNA damage markers (Mastaloudis et al., 2004a, b). For a more detailed explanation of these studies, the reader is referred to Traber and Mastaloudis (2004) in Appendix B. Similar findings were reported by Dawson et al. (2002). Animal studies show that intake of vitamin E alone after stress was more effective in lowering lipid peroxidation than other treatments, including vitamin C supplementation. In addition, an IOM committee (IOM, 1999) concluded in a letter report that there is little evidence to support the idea that supplementation with vitamin C beyond the military nutrient reference value (90 mg/day) would protect against short-term acute oxidative stress. The committee concurs with this conclusion and finds that, although future studies may prove that under certain circumstances supplementation with vitamin C or vitamin E or both might prove beneficial, at this time there is no consistent evidence that either of the vitamins alone or in combination enhances performance or health. Since the time of publication of that letter report, there has been no evidence to the contrary.
Vitamin C and Immune Function. The effectiveness of vitamin C against the common cold is also a matter of controversy. To date, supplementation with vitamin C has not been unequivocally shown to reduce the incidence or severity of the common cold (Hemila, 1994, 1997; Hemila et al., 2002; Takkouche et al., 2002)—except perhaps in those with low vitamin C intakes (e.g., males in the United Kingdom) (Hemila, 1997). Furthermore, significant effects on other aspects of the immune function have not been proven (IOM, 2000).
Vitamin C and Tobacco Consumption. One factor that the committee considered to be important in determining the level of vitamin C in the ration was the fact that most soldiers are, or become, tobacco users while being deployed. According to two studies using radiolabeled tracer ascorbic acid in healthy male smokers and nonsmokers, the metabolic turnover of the vitamin C was about 35 mg/day greater in smokers than in nonsmokers (Kallner et al., 1979, 1981). Considering the high percentage of smokers among US soldiers, the committee decided to factor in an additional 35 mg/day for the recommended level of vitamin C.
Food Form
Due to issues involving the lack of stability of vitamin C, an additional 50 percent over the desired intake level would need to be added to the food (IOM, 1997b), resulting in approximately 180 mg/day (125 + 60) in the ration. The 95th percentile intake for adult men in the United States is 400 mg/day. The committee believes that this amount will not increase the risk of stone formation since a review of the evidence for an RDA concluded that levels below 1,000 mg/day are considered safe based on risk stone formation (Levine et al., 1996). The committee recommends that food developers aim at including 180 mg but no more than 400 mg of vitamin C in the ration. If shelf-life of the ration is such that degradation would not occur, then a lower amount (< 400 mg) should be considered as the upper end of the range to avoid potential for increased stone formation.
Dried fruits that naturally contain vitamin C could be included in the ration; ration foods can also be fortified with vitamin C. If fortification is considered, vitamin C may be coated with various substances, such as ethyl cellulose, cyclodextrins, or lipids, to prevent contact with iron, copper, or nickel. As explained in Chapter 3, encapsulation of vitamin C slows its degradation under high heat and moisture conditions and protects it from oxidation by metals.
Research Needs
-
Investigate the potential synergistic effects of a mixture of antioxidants on physical performance and immune function in a randomized trial.
-
Conduct studies on the effects of vitamin C supplementation with high dietary levels of the vitamin, rather than pharmacological levels. Before conducting such studies, valid markers of antioxidant activity that will permit comparison of studies across laboratories are needed.
-
Explore the use of vitamin C supplementation to prevent colds in young people.
-
Determine the stability of vitamin C in the food under extreme environmental conditions during shelf-life of rations.
-
Investigate the effects of smokeless tobacco use on vitamin C.
Vitamin D
RECOMMENDATION: The assault ration should contain 12.5–15 µg of vitamin D based on the amount of vitamin D needed to maintain a serum level of 70 nmol /L of 25(OH)D and on the amount shown to maintain serum 25(OH)D levels in military personnel assigned to submarine duty over a three-month period.
Background
Vitamin D is essential in that it maintains normal serum levels of calcium and phosphorus. Other roles of vitamin D, such as in immune disorders and cancer, are still not clear, although there is enough evidence from studies with animal models to suggest important functions (Deluca and Cantorna, 2001; Griffin et al., 2003; van Etten et al., 2002). The endogenous synthesis of pre-vitamin D from 7-dehydrocholesterol by the action of ultraviolet B (UVB) light on skin is a major contributor to the pool of vitamin D in the human body. People with dark skin, however, have high melanin levels that block UVB light; thus, they tend to be at risk of vitamin D deficiency due to a decrease in the amount of UVB light that is available for cutaneous vitamin D synthesis. In addition, the number of sunlight hours also affects the amount of endogenous synthesis. Therefore, latitude and season are factors that should be considered when determining the amount needed in the assault ration.
Unlike most other nutrients, estimates of dietary intake are not available from NHANES or the CSFII. Estimates of average vitamin D intakes for men 19–30 years old based on modeling of food and supplement intake from two nutrition surveys (NHANES III from food and supplements; CFSII from food only) have been made, and are 8 and 4.8 µg/day, respectively (Moore et al., 2004). Due to the numerous factors that affect vitamin D status, in 1997 the AI for adults was derived by increasing the amount shown to maintain adequate levels of serum 25(OH)D (> 30 nmol/L) in women during winter in Nebraska, 3.3 to 3.4 µg/day, to a total of 5 µg to cover the needs of adults 19–50 years regardless of exposure to sunlight. The UL of 50 µg/day was based on vitamin D intakes resulting in hypercalcemia (IOM, 1997a).
Rationale for Levels of Vitamin D
Using assumptions required to estimate vitamin D intakes (Moore et al., 2004), intakes of men 19–30 years old appear to approach the AI level of 5 µg/day. It is possible, however, that some soldiers may enter missions with low levels of serum 25(OH)D. Although liver storage could be expected to ensure sufficient amounts of vitamin D during short-term assault missions, recent epidemiological studies showed prominent vitamin D deficiency (defined as serum 25 (OH)D levels less than 37.5 nmol/L) in US adolescents, especially among African Americans (37 percent compared to 6 percent and 22 percent for white and Hispanic adolescents, respectively) (Gordon et al., 2004). Higher frequencies of insufficiency in the African-American population (Calvo and Whiting, 2003) and lower serum concentrations of 25(OH)D in the Mexican-American population (Reasner et al., 1990) as compared with the white population, are of concern. Because the level of sunlight will vary with the particular environment of military missions (e.g., desert versus mountainous environments), it is appropriate to
assume the conservative scenario that most vitamin D will be derived from the diet.
In addition to concerns about vitamin D status for some subpopulations within the military, based on new studies experts are now questioning whether the cutoff for the accepted criterion of adequacy, serum concentration of 25(OH)D, should be higher (e.g., > 80 nmol/L) (Holick, 2004) than that used in 1997 (> 30 nmol/L) when the current AI was established (IOM, 1997a). This criterion of adequacy was based on estimates of intake and the related 25(OH)D serum levels of women in Nebraska (> 30 nmol/L), where sunlight is more limited. The question, however, remains whether this level indicates optimal health. A recent intervention study reported that during winter an oral intake level of 12.4 µg/day was required to sustain serum 25(OH)D levels at or above an average of 70 nmol/L (Heaney et al., 2003). Others have recommended that indicators of chronic disease, rather than levels 25(OH)D, might provide a better basis to establish the AI (Specker, 2005). The possible need for amounts in excess of the AI, along with reports of apparent vitamin D deficiency in adolescents and young men, suggests that the level of vitamin D for the assault ration be set at 12.5 µg/day, a level that should maintain serum vitamin D levels at 70 nmol/L without depending on sunlight exposure or body liver stores to contribute to available vitamin D. In support of this, a study with submariners showed that a dietary intake of 15 µg of vitamin D could generally maintain serum concentrations of 25(OH)D for three months. Using the conservative assumption that sunlight exposure during missions may be lacking, to prevent depletion of body stores and to remediate possible previous inadequate intakes, particularly in African-American soldiers, the committee recommends that the ration contain from 12.5 to 15 µg of vitamin D. The lower level of the range is based on possible benefits to optimal health and is based on the amount of vitamin D needed to maintain a level of 70 nmol/L of 25(OH)D in serum over time, while the upper end of the range is based on an amount shown to maintain serum 25(OH)D levels in military personnel assigned to submarine duty over a three-month period (15 µg). The committee recommends that, as the new data indicating the need for reviewing the AI and the UL are further evaluated, the military consider revising the range in light of such deliberations.
Food Form
Very few foods are good sources of vitamin D. Most vitamin D in the diet comes from fortified foods, with the exception of small amounts in animal products. Cereals and milk products are typically fortified with vitamin D in the United States, whereas in other countries, margarine and other staples are fortified. It is envisioned that food items in the ration will need to be fortified with vitamin D.
Research Needs
-
Evaluate the effect of clothing on vitamin D status parameters in soldiers while in field operations.
-
Evaluate vitamin D status of soldiers in the field in different environments, particularly after deployments in cold weather, at high latitudes, and at high altitudes where sunlight will be limited.
-
Examine ethnic differences in vitamin D status in these military environments.
Vitamin E
RECOMMENDATION: The ration should contain a level in the range of 15–20 mg of α-tocopherol, based on the RDA to prevent erythrocyte lysis and on dietary intake levels. If necessary, this form can be added into the food products because natural foods are limited in this form of tocopherol.
Background
The main role of vitamin E (by definition, α-tocopherol; IOM, 2000) is as an antioxidant that prevents the propagation of free radical formation, a process that may be related to many of the chronic diseases of aging, such as cardiovascular disease, cancer, and diabetes. Overt signs of vitamin E deficiency occur very rarely in humans and have not been reported as a result of low dietary intakes, except when combined with moderate to severe malnutrition. Individuals who have overt signs of deficiency of vitamin E, due to a genetic abnormality in vitamin E transport or to fat malabsorption, develop scaly skin and eventually neurological symptoms. The RDA for vitamin E is set at 15 mg for men 19–50 years of age. This requirement was based on maintaining plasma tocopherol concentration at a level that limited hemolysis in red blood cells due to peroxide exposure to less than 12 percent. According to NHANES III serum data, this amount would ensure that at least 95 percent of the population is protected against vitamin E deficiency. The median and the 95th percentile dietary intake of α-tocopherol are 9 and 19 mg/day, respectively, for men 19–30 years of age (NHANES III; IOM, 2000). The UL of vitamin E was established at 1,000 mg based on hemorrhagic effects.
Rationale for Levels of Vitamin E
Vitamin E as Antioxidant. High levels of physical activity create oxidative damage, and, as with vitamin C, vitamin E requirements might differ for individuals under physical stress. Although dietary vitamin E appears to have a protective role against oxidative stress, the studies conducted until now have not
clearly shown a benefit either in reducing muscle injury due to exercise or in improving performance (Sacheck and Blumberg, 2001). The effect of vitamin E on exercise-induced changes in creatine kinase (CK), oxidative damage to lipids, and markers for DNA damage is uncertain. One study showed that supplementing 800 IU/day of vitamin E for 60 days actually promoted lipid peroxidation and inflammatory markers after a triathlon, as evidenced by an increase in plasma F2-isoprostanes and IL-6; however, there was no effect on performance (Nieman et al., 2004).
The existing data on the effects of vitamin E as an antioxidant and enhancer of performance often come from studies that used pharmacologic doses of the vitamin. An added difficulty comes from appropriately choosing antioxidant indicators of oxidative stress and muscle damage. For example, Cannon et al. (1990) questioned whether an increase of CK after exercise reflects undesirable muscle damage. Their research comparing young and old subjects (Cannon et al., 1990) suggests that the increase in CK might be due to the need to clear damaged proteins with an increase in muscle protein turnover (Cannon et al., 1991). There are studies that show that supplementation with vitamin C and E together (compared to vitamin C or E alone) is more effective in protecting from oxidative stress due to regeneration of vitamin E by vitamin C. For more details, the reader is referred to the section on vitamin C above.
Vitamin E and Immune Function. Vitamin E has been investigated as a potentiator of immune function. At levels from 60–800 mg/day for 4–8 months, vitamin E was shown to increase immune status markers in the elderly; no adverse effects were reported (Meydani et al., 1997, 1998). Studies have also specifically looked at the effect of vitamin E on the incidence of common colds. A recent study found that supplementing the diet with 220 mg/day during one year lowered the incidence of common colds in elderly nursing home residents (Meydani et al., 2004). Another study, however, reported no beneficial effect of supplementing the diet of noninstitutionalized elderly individuals with the same amount (Graat et al., 2002). Unfortunately, most studies have been conducted with the elder population, and data on effects of vitamin E supplementation on the immune system of young adults are scarce.
The committee concludes that there is no clear evidence that providing high, pharmacologic levels (> 60 mg) of vitamin E in the ration is efficacious whether to improve performance or to enhance the immune function. Therefore, the level recommended is based on the RDA for this age group and dietary intake validated by chemical analysis of duplicate samples. The committee does not consider using the UL for the general population (1,000 mg/day) (IOM, 2000) as reasonable due to reports on the risk of hemorrhage, increased prothrombin time, and interruption of blood coagulation (Booth et al., 2004). A recent meta-analysis (Miller et al., 2005) suggests that such high amounts of vitamin E may be associated with other adverse events, including increased death rate. Therefore, rather than using the UL, the committee based the upper limit of the recommendation
on chemically measured dietary intakes. It is recognized that, although the RDA was set at 15 mg/day, dietary intakes are likely underestimated. For example, in Holland, chemical testing showed that conventional menus contained 20.9 mg of α-tocopherol (van het Hof et al., 1999). The committee concluded that these data justify setting a range of 15–20 mg/day of vitamin E for combat rations. There are concerns also with the use of aspirin, or other drugs with anticoagulant properties, in combination with vitamin E due to the potential additive, adverse effects on coagulation.
A recent study showed that plasma α-tocopherol disappearance was faster in smokers compared to nonsmokers and that these rates correlated with plasma ascorbic acid concentration in smokers but not in nonsmokers. The authors concluded that smokers have an increased requirement for α-tocopherol (Bruno et al., 2005). At this time, however, it is premature to recommend the addition of a specific amount of α-tocopherol due to smoking.
Food Form
Since many common food sources are generally low in α-tocopherol, it is expected that the committee recommendation will not be met by the foods in the ration. Because only the α-tocopherol form of vitamin E can be transported by transfer proteins in the liver, and other forms (β-, γ-, and δ-tocopherols and the tocotrienols) will be excreted, foods should be fortified with vitamin E as α-tocopherol. Other forms (β-, γ-, and, δ-tocopherols and the tocotrienols) will be present as natural components of food in the ration.
Research Needs
-
Investigate the potential synergistic effects of a mixture of antioxidants in a randomized trial on physical performance and immune function. Before conducting such studies, valid markers of antioxidant activity that will permit comparison of studies across laboratories are needed.
-
Conduct studies on the effects of vitamin E supplementation on physical performance and immune function using more physiologic levels of the vitamin (15–60 mg), rather than pharmacologic levels.
-
Explore the use of supplementation of vitamin E to prevent colds in young people.
-
Determine if smokers need supplemental levels of vitamin E.
-
Study the use of aspirin by individuals consuming a diet high in vitamin E, since the action of both may affect coagulation.
-
Further study adverse events associated with vitamin E.
Vitamin K
RECOMMENDATION: The committee assumes that enough vitamin K would occur naturally in the ration foods; therefore, additional vitamin K is not necessary.
Background
Vitamin K acts as a cofactor during the synthesis of blood coagulation enzymes. The median and 95th percentile dietary intake for men 19–30 years old are 101.1 and 181.3 µg/day, respectively (NHANES III; IOM, 2001b). The AI is based on dietary intake data for healthy individuals and was established at 120 µg/day for adult men. There have been no adverse events reported, so no UL was established (IOM, 2001b).
Rationale for Levels of Vitamin K
Turnover from lipid fraction is rapid and hepatic reserves deplete rapidly if the intake of vitamin K is restricted (Usui et al., 1990). The committee believes that for the short terms of the combat mission, however, it is not essential to add vitamin K to the ration because it is stored in the liver and is naturally present in foods. In addition, vitamin K deficiency is rare.
Thiamin
RECOMMENDATION: Assuming an energy content of 2,400 kcal in the assault ration and an average energy expenditure of 4,500 kcal/day, the assault ration should contain a level of 1.6–3.4 mg of thiamin.
Background
Thiamin is essential in the metabolism of carbohydrate and branched-chain amino acids. Thiamin is a coenzyme that affects the cardiovascular, muscular, nervous, and gastrointestinal system (Tanphaichitr, 1999). The RDA for men ages 19–30 years is set at 1.2 mg/day thiamin (IOM, 1998). The 95th percentile intake of thiamin is 3.4 mg/day for men between the ages of 19–30 years (IOM, 1998). Thiamin deficiency signs and symptoms include anorexia, weight loss, mental dysfunction, muscle weakness, and cardiovascular effects. A UL was not set because there have been no sufficient data on adverse effects associated with thiamin consumption.
Rationale for the Levels of Thiamin
Thiamin is required for the metabolism of carbohydrate (conversion of pyruvate to acetyl CoA), branched-chain amino acids, and fat (tricarboxylic acid [TCA] cycle enzymes). There are no metabolic feeding studies examining the amount of thiamin required to maintain good status in active individuals. The EAR for thiamin is based on the need for 0.3 mg thiamin/1,000 kcal (IOM, 1998), assuming individuals were in energy balance. Rather than basing the amount in the assault ration on its caloric level, given the restriction in energy intake of soldiers, a recommendation for thiamin based on energy expenditure is a reasonable approach. Assuming a 4,500 kcal/day energy expenditure, a minimum recommended daily intake of 1.6 mg of thiamin/day would be calculated, based on increasing the EAR of 0.3 mg/day/1,000 kcal by 20 percent for twice the assumed CV of requirements for thiamin of 10 percent (0.3 mg/day/1,000 kcal × 4.5 × 120 percent = 1.6 mg/day needed) (IOM, 1998). In addition, based on NHANES III data, the 95th percentile intake of thiamin is 3.4 mg/day for men between the ages of 19 and 30 (IOM, 1998). Using these numbers, the committee concluded that 1.6–3.4 mg/day of thiamin, which is above the current RDA for men (1.3 mg/day), would cover the thiamin needs of the soldiers. There are no reports available of adverse effects from consumption of excess thiamin by ingestion of food or supplements (IOM, 1998). Thiamin can be either naturally occurring in food or added to the food.
Riboflavin
RECOMMENDATION: Assuming an energy content of 2,400 kcal in the assault ration and an average energy expenditure of 4,500 kcal/day, the assault ration should contain a level of 2.8–6.5 mg of riboflavin.
Background
Riboflavin is an essential nutrient due to its function as a coenzyme in numerous redox reactions. Riboflavin is involved in numerous metabolic pathways and in energy production. Signs and symptoms of deficiency include sore throat, hyperemia and edema of the pharyngeal and oral mucosal membranes, cheilosis, angular stomatitis, among others (McCormick, 1999). The RDA in healthy males of ages 19–30 years is 1.3 mg/day riboflavin (IOM, 1998). The 95th percentile intake of riboflavin is 6.5 mg/day for men between the ages of 19 and 30 (IOM, 1998). A UL has not been set because there is insufficient data on adverse effects associated with riboflavin consumption.
Rationale for Levels of Riboflavin
Riboflavin is important for physical activity because it is involved in carbohydrate, protein, and fat metabolism, and in the conversion of vitamin B6 and folate to their active forms (IOM, 1998; Manore, 2000). Data from Belko et al. (1985) provided information about riboflavin needs under conditions of low energy intake and exercise. This study used the same level of energy restriction experienced by the soldiers (approximately 50 percent of energy needs). Thus, their estimate based on energy intake was used for the calculation of riboflavin needs. This differs from the approach used in developing the EAR (and thus, the RDA) (IOM, 2000) in which estimates were based on requirements at normal activity levels where a relationship to energy intake was not demonstrated. Using the recommendations in Belko et al. (1985) and an energy intake of 2,400 kcal/day, soldiers on assault missions would need approximately 2.78 mg of riboflavin to maintain good nutritional status (1.16 mg riboflavin × 2.4 = 2.78 mg). In addition, according to NHANES III data, the 95th percentile intake of riboflavin is 6.5 mg/day for men between the ages of 19 and 30 (IOM, 1998). Using these numbers, the committee agreed that 2.8–6.5 mg/day of riboflavin would cover the need of the soldiers. This range is above the current RDA for riboflavin (1.3 mg) for men 19–30 years old. There are no adverse effects associated with riboflavin consumption from food or supplements (IOM, 1998). Riboflavin can be either naturally occurring in food or added to the food.
Niacin
RECOMMENDATION: Assuming an energy content of 2,400 kcal in the daily ration and an average energy expenditure of 4,500 kcal/day, the assault ration should contain a level of 28–35 mg of niacin equivalents (NE).
Background
Niacin is an essential precursor of nucleotides that are key components of redox reactions, ATP synthetic pathways, and adenosine diphosphate ribose transfer reactions. The RDA for men ages 19–30 years is set at 16 mg/day of NE (IOM, 1998). The 95th percentile intake of niacin for men between the ages of 19 and 30 years is 45 mg/day (NHANES III; IOM, 1998). Deficiency manifests itself as pellagra with signs and symptoms like rash, diarrhea, or constipation associated with changes in digestive tract as well as neurological symptoms such as fatigue and loss of memory. Due to flushing that has been seen in studies of subjects given an excess of the vitamin, the UL is set at 35 mg/day of NE from forms added to foods or as supplements only.
Rationale for Levels of Niacin
Niacin (NAD and NADP) is required for the metabolism of carbohydrate (glycolysis and electron transport) and fat (β-oxidation of fats) and for protein synthesis. No metabolic feeding studies examined the amount of niacin required to maintain good status in active individuals. In addition, no studies have examined the impact of dieting and exercise on niacin status. The EAR for niacin was determined to be 4.8 NE/1,000 kcal, assuming that individuals were in energy balance (IOM, 1998). Because the energy intake of soldiers is low during missions, basing the recommendation for niacin on energy expenditure instead of intake would be a reasonable approach. Assuming a 4,500 kcal/day energy expenditure, a minimum recommended daily intake of 28 mg of niacin/day would result, based on increasing the EAR of 4.8 mg/day/1,000 kcal by 30 percent for twice the assumed CV of requirements for thiamin of 15 percent (4.8 mg/day/1,000 kcal × 4.5 × 130 percent = 28.1 mg/day needed) (IOM, 1998). Since the UL of niacin (35 mg/day) is below the NHANES III 95th percentile intake of niacin for men 19–30 years old (45 mg/day) (IOM, 1998), the committee recommends a range of 28–35 mg/day of niacin. This recommended range is above the RDA (16 mg/day) and below the UL for this age range (35 mg/day). Thus, it should ensure adequate amounts and minimal risk of adverse effects. If adequate amounts of niacin are provided, endogenous synthesis of niacin from tryptophan will be minimized. The niacin can be either naturally occurring or added to the food. A minimum of 28 mg should be present in the ration, and not more than 35 mg be added to foods.
Vitamin B6
RECOMMENDATION: Based on an estimated body protein loss of approximately 52 g/day due to the soldiers’ negative energy balance and a minimum protein intake of 100 g/day, the assault ration should contain a level of 2.7–3.9 mg/day of vitamin B6; if a higher protein level is provided, this amount should be increased proportionally.
Background
Vitamin B6 is an essential coenzyme for metabolism of amino acids, glycogen, and sphingoid bases. It is essential for immune and nervous system function and affects gluconeogenesis, niacin formation, red cell metabolism, and steroid function. Classical signs and symptoms of deficiency of vitamin B6 include stomatitis, cheilosis, glossitis, irritability, depression, and confusion (Leklem, 1999). The RDA set for healthy normal men 19–30 years is 1.3 mg/day of vitamin B6 (IOM, 1998). The 95th percentile intake of vitamin B6 is 3.91 mg/day for men between
the ages of 19 and 30 (NHANES III; IOM, 1998). The UL, based on the risk of developing sensory neuropathy, is 100 mg/day of vitamin B6 (IOM, 1998).
Rationale for Levels of Vitamin B6
Vitamin B6 is required for the metabolism of carbohydrate (gluconeogenesis and glycogen breakdown) and protein (transamination reactions). Thus, vitamin B6 is important in helping to provide energy to exercising muscles (Manore, 2000). Based on the recent metabolic feeding data by Huang et al. (1998) and Hansen et al. (2001), in order to maintain adequate vitamin B6 status, 0.019–0.020 mg B6/g protein was required in sedentary young women who were weight stable and consuming 70–85 g protein/day. The committee assumes that the soldiers will be consuming 2,400 kcal/day while expending 4,500 kcal/day. Under these conditions, the soldier is exercising vigorously and losing weight. Using data collected on male soldiers consuming 1,600 kcal/day and expending 4,500 kcal/day, Nindl et al. (2002) found a loss of 1.5 kg fat-free mass (FFM) in three days. In order to calculate the amount of body protein lost in the Nindl et al. study (2002), the committee assumed that 50 percent of this FFM weight was water loss. Assuming a nitrogen-to-lean tissue ratio of 30:1 and a 6.25 factor to convert nitrogen to protein, there would be a protein loss of 156 g in 3 days or 52 g/day in this study. In applying these data to the combat assault situation posed here, the committee assumed about 33 percent less protein was lost (100 g or 33 g/day), since intake of energy (2,400 kcal/day) and protein (100 g/day) would be higher. Thus, protein metabolism would include components of both dietary protein (100 g) and protein lost from the body (33 g) for a total of 133 g protein. Using a requirement of 0.020 mg B6/g protein (Hansen et al., 2001), 2.7 mg/day of B6 of would be needed to metabolize 133 g of protein. In NHANES III data, the 95th percentile intake of vitamin B6 is 3.91 mg/day for men between the ages of 19 and 30 (IOM, 1998). Using the calculations above and the 95th percentile intake of vitamin B6, providing 2.7–3.9 mg/day B6 would cover the needs of the soldiers. This range falls above the current RDA for vitamin B6 (1.3 mg/day) and below the UL for vitamin B6 (100 mg/day). Vitamin B6 can be either naturally occurring in food or added to the food.
Research Needs
-
Determine the requirements of niacin, riboflavin, thiamine, and vitamin B6 when individuals are consuming a hypocaloric diet under the environmental conditions and high-stress situations of combat missions (e.g., intense physical activity, high energy expenditure, reduced caloric intake, and hot and humid conditions).
Folate
RECOMMENDATION: The assault ration should contain 400–560 µg of folate (either as food folate or folate added to foods), based on the current RDA for folate and the 95th percentile intake for folate.
Background
Folate is essential in single-carbon transfers in the metabolism of nucleic and amino acids. The RDA for healthy men 19–30 years of age is 400 µg/day of dietary folate equivalents (DFEs) (IOM, 1998). The 95th percentile intake of folate is 564 µg/day for men between the ages of 19 and 30 (NHANES; IOM, 1998). The UL for folate is 1,000 µg/day from fortified food or supplements (IOM,1998).
Rationale for Levels of Folate
Folate is involved in a number of metabolic processes associated with physical activity. Folate is important for red blood cell (RBC) formation and, thus, for the transport of oxygen to the working muscle. Folate is also involved in the synthesis of pyrimidine and purine nucleotides, protein synthesis, and normal cell growth.
As reviewed by the IOM (1998), naturally existing folate from food is only 50 percent bioavailable. Folate added to foods fortified with folic acid has much higher bioavailability, about 85 percent (i.e., a bioavailability ratio of 1.7). When a mixture of folic acid plus food folate is consumed, as in the assault ration, dietary folate equivalents are estimated as follows:
µg of DFEs provided = µg of food folate + (1.7 × µg of folic acid)
This formula can also be used to calculate the EAR. No metabolic feeding studies have examined the amount of folate required to maintain good status in active individuals. In general, studies examining dietary intakes of active males report that mean intakes of folate are adequate (Manore and Thompson, 2000). These adequate intakes can be attributed to the relatively high-energy intakes of these individuals. Poor folate status has been associated with depression in healthy subjects between the ages of 15 and 39 (Morris et al., 2003) and poor cognitive function (Calvaresi and Bryan, 2001) but data are mixed (Malouf et al., 2003). NHANES III data, which were collected before folate fortification, indicate that the median and 95th percentile intake of folate from foods is 277 and 564 µg/day for men between the ages of 19 and 30, respectively (IOM, 1998). Based on the RDA and the 95th percentile intake, providing 400–564 µg/day of folate to soldiers would cover their folate needs.
Food Form
Folate occurs naturally in food or can be added to the food. The formula described above should be used to derive the dietary folate equivalents from food, which takes into consideration the availability of both the food folate and the added folic acid.
Vitamin B12
RECOMMENDATION: The committee assumes that enough vitamin B12 would occur naturally in the ration, if some of the protein is of animal source and, therefore, that additional vitamin B12 is not necessary.
Background and Rationale
Vitamin B12 is necessary for RBC formation, normal cell growth, and proper folate metabolism. The RDA for men between the ages of 19 and 30 is 2.4 µg/day vitamin B12 (IOM, 1998). There is no UL for vitamin B12 (IOM, 1998). In normal, healthy men vitamin B12 stores have been estimated as sufficient for 2 years (IOM, 1998); the risk of depletion over a few days is low. Thus, there is no compelling reason to add B12 to the ration to supplement what would occur naturally in food.
Biotin
RECOMMENDATION: The committee assumes that enough biotin would occur naturally in the ration foods; therefore, additional biotin is not necessary.
Background and Rationale
Biotin is required for a number of metabolic functions related to physical activity. It is required for the metabolism of carbohydrate (gluconeogenesis), amino acid (leucine degradation), and fat (TCA cycle), and for fat synthesis. No metabolic feeding studies have examined the amount of biotin required to maintain good status in active individuals. In addition, no studies have examined the impact of dieting and exercise on biotin status. There is no UL for biotin. Currently, the AI for biotin is 30 µg/day for men (IOM, 1998).
Pantothenic Acid (CoA)
RECOMMENDATION: The committee assumes that enough pantothenic acid would occur naturally in the ration foods; therefore, additional pantothenic acid is not necessary.
Background and Rationale
Pantothenic acid (CoA) is required for the metabolism of carbohydrate (gluconeogenesis and glycolysis), fat (β-oxidation, TCA cycle), and protein. No metabolic feeding studies have examined the amount of pantothenic acid required to maintain good status in active individuals. In addition, no studies have examined the impact of dieting and exercise on pantothenic acid status. There is no UL for pantothenic acid. Currently, the AI for pantothenic acid is 5 mg/day for men (IOM, 1998).
Choline
RECOMMENDATION: The committee assumes that enough choline would occur naturally in the ration foods; therefore, additional choline is not necessary.
Background and Rationale
Choline accelerates the synthesis and release of acetylcholine, an important neurotransmitter involved in memory storage, muscle storage and muscle control; its deficiency is marked by changes in liver enzymes. The AI for choline is 550 mg/day for men between the ages of 19 and 30. The UL for choline is 3.5 g/day for adults 19 years of age or older, based on fishy body odor and hypotension (IOM, 1998).
Calcium
RECOMMENDATION: The assault ration should contain 750–850 mg of calcium. This range is based on a factorial approach to estimating calcium requirements and potential sweat losses during prolonged exercise, also taking into account concerns about renal stone formation.
Background
The AI for men 19–30 years of age is 1,000 mg/day based on balance studies to determine intakes at which there are gains in bone mineral content. The UL for adults was established at 2,500 mg/day based on the risk of nephrolithiasis (formation of renal stones) (IOM, 1997a).
Intestinal absorption of calcium is enhanced at low levels of calcium intake (approximately 300 mg) due to an active transport process in the proximal small intestine, resulting in an increased fractional absorption of calcium (Ireland and Fordtran, 1973). Absorption of additional calcium from higher intakes occurs via passive cell-mediated diffusion not requiring the action of 1,25-dihydroxyvitamin D3 (calcitriol).
Calcium requirements in the field are based on a number of factors that affect its absorption as well as its excretion via urine and sweat. Sweat losses may be appreciable given the expected level of energy expenditure and possible environmental heat. In addition, renal stone formation has been reported in troops deployed to the Middle East (personal communication, C. Koenig, USARIEM, November 19, 2004). Therefore, the major concerns considered in deriving the recommended range for calcium in the assault ration are sweat losses and the prevention of renal stone formation.
Rationale for Levels of Calcium
Effect of Energy Expenditure on Calcium Absorption and Excretion. Some evidence is available that indicates the fractional rates of calcium absorption are slightly higher in response to aerobic exercise in endurance trained athletes than in the untrained (Zittermann et al., 2002). In spite of this increase, however, markers of bone collagen formation were decreased in that study. Other studies have shown a slight but significant increase in 24-hour renal calcium excretion in trained young men compared to matched untrained control subjects (Zittermann et al., 2000) who also had higher calcium absorption rates as well as plasma calcitriol levels. Thus, it appears that endurance exercise at levels less than that expected in the soldier during active assault periods may result in both increased calcium absorption and increased urinary calcium excretion and decreased bone formation. These studies did not evaluate the extent of increased losses of calcium via sweat due to the high energy level expended.
Effect of Calcium Lost via Sweat. Calcium concentration of sweat in soldiers has been measured (Armstrong et al., 1992). Sweat calcium concentration declines as the volume of sweat increases. Intermittent exercise over 6 hours at 30°C resulted in a lower concentration of calcium in sweat with higher volumes of sweat, decreasing from 250 mg/L at a sweat rate of 0.37 L/hour to 70 mg/L at a rate of 0.62 L/hour (Armstrong et al., 1992).
Methodological problems may, in part, be responsible for differences in estimated calcium losses via sweat in the few available studies (Consolazio et al., 1966; Shirreffs and Maughan, 1997). Additionally, urinary calcium excretion in response to changes in sweat volume declines (Armstrong et al., 1992; Bullen et al., 1999). Unfortunately, compensatory changes in calcium absorption have not been estimated. For soldiers who are assumed to be sweating due to heavy prolonged exercise in hot, humid climates, it is important to ensure adequate calcium intakes to replace these potential calcium losses.
Effect of Sodium Intake. High sodium chloride intake has been shown to result in increased urinary excretion of calcium in hypertensive individuals (Kurtz et al., 1987). Quantitatively, 100 mmol (2,300 mg) of sodium as sodium chloride increased urinary calcium excretion by 1 mmol (40 mg) in postmenopausal women (Nordin and Polley, 1987). While this appears to occur at moderate and
high calcium intakes, it is not evident at lower calcium intakes (less than 300 mg/day), possibly due to modulation by parathyroid hormone (Dawson-Hughes et al., 1996).
Based on the results of Nordin and Polley (1987), the potential increased loss (i.e., 80–240 mg/day) due to the high sodium content of the diet (4–12 g) will not be considered in setting the minimum amount of calcium for the assault ration for the following reasons:
-
increased urinary losses will be balanced to some extent by increased fractional absorption of calcium due to the higher level of physical activity expected (see above); and
-
there is concern about the increased risk of hypercalciuria and renal stones when fluid restriction is combined with a comparatively high amount of dietary calcium, such as the daily median dietary intake for calcium for young men in the United States (954 mg; IOM, 1997a). Although it might appear to be sensible and without adverse consequences to provide this level when the recommended daily level of sodium (AI = 1,000 mg; IOM, 1997a) is also close to the median intake of sodium, under conditions of fluid restriction the potential for adverse effects cannot be overlooked.
Effect of Dietary Protein Level. Although increased dietary protein intake increases calcium excretion (Linkswiler et al., 1981; Margen et al., 1974; Walker and Linkswiler, 1972), this effect of protein is due in part to the content of sulfur amino acids and it was demonstrated at protein intake levels higher than the range recommended for the assault ration (100–120 g/day). Also, more recent research suggests that the calciuretic effect of protein is partly explained by increased calcium absorption, and that calciuretic effects are considerably modified by long-term adaptation (Dawson-Hughes et al., 2004; Kerstetter et al., 2005). Thus, this potential effect will not be considered further in establishing a range for the assault ration.
Effect of Calcium Intake on Fat Oxidation. Recent studies evaluating the effect of consumption of dairy products and weight loss have implicated calcium in enhancing whole-body fat oxidation (Davies et al., 2000, Melanson et al., 2003; Zemel et al., 2000) while other studies have not (Jacobsen et al., 2005) except only for fecal fat excretion. This is an area of recent interest and little has been well established; however, given the concern with maintaining body weight to the extent possible while in combat missions, the potential adverse effects of higher calcium intakes on body weight should continue to be investigated. At the same time there is also evidence that losses in bone mass are attenuated on hypocaloric diets when calcium intakes are relatively high (Ricci et al., 1998); these effects should also be evaluated.
Effect of Lower Levels of Calcium Intake on Calcium Balance. A recommended daily dietary intake level of approximately 800 mg/day should result in
both passive as well as active absorption, assuming that vitamin D included in the food packet of the ration is provided in the same food items and is at or above 5 µg per day (IOM, 1997a).
Effect of Calcium Intake on Stone Formation. High intakes of calcium along with possibly lower than normal urinary volumes due to water scarcity may result in hypercalciuria and consequently renal stone formation. Based on observations in military field hospitals in Iraq and Afghanistan (personal communication, C. Koenig, USARIEM, November 19, 2004), a comparatively high incidence of renal stone formation (urolithiasis) has been noted in soldiers in these theaters of operation, possibly due to lower fluid consumption concomitant with significant losses of sweat due to high environmental temperatures and a high level of physical activity.
Renal stone formation is due to crystallization of calcium oxalate, calcium phosphate, or both (Tiselius, 1997). Urine supersaturated with these components enhances crystal formation and growth. The most important determinants of supersaturation in forming calcium oxalate crystals are the presence of high amounts of oxalate, calcium, citrate, and magnesium, and for calcium phosphate crystals, urinary pH, high amounts of calcium, phosphate, and citrate. Citrate inhibits growth of both types of renal stones, while magnesium inhibits growth of calcium phosphate stones (Tiselius, 1997). Increasing urine volume to greater than 2 L has been shown to halve stone recurrence following first idiopathic calcium stone episodes (Borghi et al., 1996).
Renal oxalate stone formation is also enhanced with higher intakes of oxalate, particularly in individuals who are intestinal hyperabsorbers of oxalate (Siener et al., 2003). Endogenous synthesis of oxalate, while a factor, is not the significant component contributing to calcium oxalate stone formation. There is controversy regarding the contribution of both dietary oxalate and dietary ascorbic acid to urinary oxalate (Holmes, 2000; Williams and Wandzilak, 1989). A study by Baker and colleagues (1966) which showed about 40 percent of the urinary oxalate is from ascorbate breakdown has been criticized because there is question about the pH to which urine samples were exposed prior to analysis for oxalate when estimates of breakdown rates from ascorbate to oxalate were made (Holmes, 2000). Hepatic synthesis is estimated to be 10–20 mg/day, with estimates of urinary oxalate derived from the diet via intestinal absorption varying from 10–20 percent (de O G Mendonca et al., 2003) to 67 percent (Holmes et al., 1995). Recent studies have shown that lower calcium diets (400 mg compared to 1,000 or 1,200 mg per day) lead to increased oxalate absorption, probably due to the decreased amount of unabsorbable calcium-oxalate complexes formed, thus allowing more free oxalate to be absorbed and subsequently excreted, thereby contributing to oxalate stone formation (Borghi et al., 2002; Holmes et al., 2001).
Determination of Estimated Needs. The committee’s concern about stone formation stems from the soldiers’ high volumes of sweat and possibly curtailed fluid intake. Therefore, risk of stone formation is a major factor in determining
the recommended range for calcium. The expected loss of calcium due to significant sweat production is also a major factor. While the AI of 1,000 mg for this age group (IOM, 1997a) is at a level which, in normal situations, does not lead to hypercalciuria, given the environmental temperatures in the field and the energy expenditure expected, a lower level of calcium intake than the AI is recommended. Although exercise involving weight-bearing activity itself will result in less bone loss, the level of calcium should be as high as possible to prevent bone resorption, given that the ration may be consumed for a total of up to 24 days in a 30-day period. The level should be above 400 mg/day to minimize oxalate absorption and below 1,200 mg/day to minimize the risk of stone formation. Intake between these two levels (e.g., 800 mg/day) should provide for oxalate binding in the gut as well as diminishing bone loss resulting from hypercalciuria brought on by the potential level of dehydration expected in this environment. A range of 750–850 mg of calcium is thus recommended. This level assumes a sweat loss of 6.5 L/day in acclimatized individuals expending approximately 4,500 kcal/day under temperatures of approximately 20°C (IOM, 2004). In hotter environments (e.g., 30°C), sweat loss is assumed to be 10.5 L/day on average (IOM, 2004).
While additional sweat losses of calcium with higher ambient temperatures may result, no further increase in the calcium content of the ration is recommended. In all likelihood, the total fluid intake may not increase equivalently, resulting in increased urinary concentration and enhancing the risk of stone formation. Under these conditions, the additional sweat will have lower concentrations of calcium, and less additional calcium will be lost. It is also assumed that, due to the increased level of physical activity and any additional body demand for calcium, fractional absorption of calcium will increase to cover some of the additional sweat losses.
In summary, the level of 750–850 mg/day of calcium is recommended. This level will minimize hypercalciuria while allowing for both active and passive absorption. It also will enhance gut formation of unabsorbable calcium-oxalate complexes in asymptomatic individuals considered oxalate hyperabsorbers.
Food Form
Most of the calcium in foods comes from dairy products. The ration will likely have cheese spreads but not in quantities enough to meet the level of calcium recommended. In addition, cereals and fruits have some calcium. In order to achieve the amount of calcium recommended in the ration (750–850 mg), ration items, such as cereals will have to be fortified with calcium; such fortified products are already commercially available and therefore acceptability is not anticipated to be an issue.
Research Needs
-
While enhancements to encourage fluid intake need to be sought, additional research is needed on the relationships between calcium, magnesium, and phosphorus on the maintenance of bone mineral density in hot environments resulting in significant sweating. This should include determining the appropriate levels of intake to maintain bone mineral density while diminishing hypercalciuria to the extent possible.
Chromium
RECOMMENDATION: The committee assumes that enough chromium would occur naturally in the ration foods; therefore, additional chromium is not necessary.
Background
Chromium is essential because it promotes the action of insulin so that the body can utilize fats, carbohydrates, and protein. Chromium is a potentiator of insulin activity (Mertz, 1969, 1993; Mertz et al., 1961). It is hypothesized to function by complexing with a low-molecular-weight chromium-binding substance that binds and activates the insulin receptor of insulin-dependant cells.
The AI for chromium is based on estimated mean intakes and is 35 µg/day (IOM, 2001b). No UL was established due to few known serious adverse effects. Also, evidence of deficiency in humans is limited to individuals on prolonged total parenteral nutrition therapy. In these cases, individuals affected developed weight loss and peripheral neuropathy that was reversed upon chromium administration.
Rationale for Levels of Chromium
The committee does not consider it necessary to provide supplemental chromium in the ration in spite of its possible role in potentiating the effects of insulin. It is assumed that, because of the wide distribution of chromium in foods (Anderson et al., 1992), food items in the ration will have enough chromium to meet the needs of soldiers. Given the lack of reports indicating deficiencies in individuals in the population, concerns about inadequate intake while consuming food based diets are minimal, especially for the short terms of combat missions. Additionally, there is no conclusive evidence that chromium supplementation enhances performance (Clarkson, 1997; Lukaski, 2001).
Research Needs
-
Determine whether supplementation with chromium affects physical performance for individuals on a hypocaloric diet under the environmental conditions of combat missions.
Copper
RECOMMENDATION: The assault ration should contain copper at a level in the range of 900–1,600 µg/day based on the RDA and potential sweat losses.
Background
Copper is a component of many metalloenzymes that act as oxidases, such as amine oxidases, ferroxidases, and superoxidase dismutase. Due to the ubiquity of copper, its deficiency affects many physiological functions: outcomes of deficiency include connective tissue defects, anemia, and immune and cardiac dysfunction. Copper deficiency in humans is rare but has been seen in premature infants and in patients receiving parenteral nutrition (IOM, 2001b). Even in the absence of signs and symptoms of deficiency, various immune system parameters may be altered (Percival, 1998) if copper status is deficient. Copper toxicity, which can also occur, results in increased lipid peroxidation and DNA damage.
The RDA is based on a factorial method and is set at 900 µg/day for men. The factorial method takes into account the amount needed in the diet to replace obligatory losses (i.e., losses from sweat, hair, nails). The UL level for men is 10 mg/day and is based on a level that presents no toxicity to the liver (IOM, 2001b). Susceptibility to copper toxicity depends on numerous factors, including the efficiency of absorption and expression of copper transport and storage proteins (Bremner, 1998). The median intake and the 95th percentile of intake of men 19–30 years old in the US is estimated to be 1,630 and 2,650 µg/day, respectively (NHANES III; IOM, 2001b).
Rationale for Levels of Copper
There is no consistent evidence of deficient copper status in the US population. Also, there is no strong evidence that inadequate copper intake leads to in any chronic disease (Jacob et al., 1981). Although copper status could affect energy metabolism based on its presence in key enzymes involved, there is no scientific literature supporting a benefit from supplementing copper on either cognition or physical performance.
Some evidence indicates that excess copper may have a pro-oxidant effect through catalyzing the formation of hydroxyl groups (Bremner, 1998). A recent
study explored the effects of a high copper diet, in which supplements of 7.0 mg/day (compared to 1.6 mg/day) were given. After almost five months of a high-copper diet, subjects had a lower concentrations of neutrophils (as a percentage of total white blood cells) and a lower concentration of IL-2 receptor; in addition, their antibody titer after influenza immunization decreased (Turnlund et al., 2004).
A study by the military reported that under hot conditions, sweat, skin and hair copper losses may increase several fold from the average basal amount of 250 µg/day to up to 1,600 µg/7 hour at 37.8°C (Consolazio et al., 1964). It is not known, however, whether such high increased losses are sustained.
Given the concern about possible pro-oxidant effects of large amounts of added copper, it is not recommended to raise the level of copper in the assault ration above the level to replace the high obligatory losses. As mentioned above, there are reports of higher copper losses in the heat (up to 1,600 µg/7 hr at 37.8°C). The committee concludes that these losses need to be considered and recommends an upper limit of 1,600 µg/day in the ration. Levels above this might result in interferences with the bioavailability of other nutrients (see Food Form section below).
Food Form
The committee assumes that copper will occur naturally in food items of the assault ration. Copper is a pro-oxidant and catalyzes unsaturated fat and oil oxidation, as well as ascorbic acid oxidation; it could also interfere with bioavailability of other minerals, such as zinc, although this has not been proven in humans at the levels recommended here (Lonnerdal, 2000). Furthermore, this would occur most likely only if fortification is needed, an unlikely event since copper would be naturally present in food in sufficient amounts.
Research Needs
-
Measure copper sweat losses in studies which simulate the environment encountered by soldiers in similar types of operations (e.g., intense physical activity, high energy expenditure, reduced caloric intake, in hot and humid conditions) in order to evaluate the additional requirements for copper.
Iodine
RECOMMENDATION: The assault ration should contain 150–770 µg of iodine. This range is based on the RDA and the 95th percentile intake from food sources.
Background
Iodine is essential for the diet because it is a component of thyroid hormones and therefore involved in many key biochemical reactions critical to life. Most iodine deficiency disorders affect growth and development due to insufficient thyroid hormones. The most severe disorders affect the developing brain. The RDA is set at 150 µg/day for men 19–50 years of age. It was estimated from thyroidal radio-iodine accumulation in turnover studies. The UL was established at 1,100 µg/day based on elevated concentrations of thyroid stimulating hormone. The median dietary intake and the 95th percentile dietary intake are 240–300 and 920 µg/day (from food sources [770 µg] and supplements [150 µg]), respectively, for men 19–30 years old (US Food and Drug Administration, Total Diet Study; IOM, 2001b).
Rationale for Levels of Iodine
The committee considers that it is important to ensure an adequate intake of iodine to minimize the risk of goiter and other impairments of the thyroid function, particularly if the ration is used repeatedly. Excess intake iodine would not create concerns because of the mechanisms that permit the thyroid to adapt to increases in iodine (Aurengo et al., 2002). A range of 150–770 mg iodine/day is recommended based on the RDA and 95th percentile of iodine intake of US adult men.
Food Form
The most feasible way to introduce iodine in the ration will be in the form of iodized salt. It is recommended that iodized salt contains 20–40 mg of iodine per kg of salt (IOM, 2002b). When all the salt in the ration is iodized, about 250 µg of iodine will be provided per 1,000 kilocalories, which is within the range recommended here.
Iron
RECOMMENDATION: The assault ration should contain iron in the range of 8–18 mg per day. The lower level of the range is based on the RDA; the higher level of the range is based on increasing the RDA to account for the potential losses of iron in sweat during high energy expenditures and for a potential lower bioavailability from the ration foods. Since iron deficiency is rare in men, if there are palatability or stability problems, the level could be closer to the 8 mg level, the RDA for men.
Background
Iron functions in oxygen transport and energy utilization as a cofactor for a number of enzymes involved in energy metabolism. The RDA for men, 8 mg/day, is based on estimated basal requirements of body losses (i.e., an average of 0.9–1.0 mg/day, based on studies using radiolabeled iron [Green et al., 1968]) and an estimated bioavailability from foods of 18 percent. Basal losses include fecal losses, urinary losses, and losses due to normal skin and miscellaneous losses. The UL for adults is 45 mg/day based on the risk of gastrointestinal distress. The median dietary intake is 17.9 mg and the 95th percentile is 31.1 mg/day for men 19–30 years old (NHANES III; IOM, 2001b). Clinical effects of deficiency include impaired physical and cognitive performance.
The estimate of bioavailability (18 percent) is based on an assumption that 10 percent of the iron in the daily diet will come from heme iron, 25 percent of which is absorbed (Hallberg and Rossander-Hulten, 1991), and 90 percent will come from non-heme iron sources, of which approximately 17 percent is absorbed (Cook et al., 1991). In the absence of heme iron, estimates of bioavailability drop to 10 percent (IOM, 2001b). As iron stores rise, there is a decrease in the percent of dietary iron that is absorbed, thus decreasing the availability of dietary iron.
Rationale for Levels of Iron
Iron Status and Physical Performance. The impact of adequate iron and iron supplements on maintenance and possibly enhancement of physical performance was evaluated during sports training and in endurance athletes (Newhouse and Clement, 1988). Most studies of iron were with female athletes, many of whom had evidence of iron depletion or anemia or both (see Lukaski and Penland, 2004 in Appendix B). Hematological parameters such as hematocrit, hemoglobin, and serum iron were decreased in response to intense exercise maintained over time. This phenomenon is known as “sports anemia” (Aguilo et al., 2004).
Based on review of over 20 years of research on iron and athletic performance and health, Beard and Tobin (2000) concluded that reductions in hemoglobin concentration and tissue iron content can be detrimental to exercise performance, and that iron status is negatively altered in many populations of chronically exercising individuals. Decreased hematocrit and hemoglobin impair the delivery of oxygen to the tissues and lead to a reduced VO2max. Supplementation of individuals with iron to a normal hematocrit improves VO2max (Beard and Tobin, 2000) and, hence, exercise capacity and performance (Woodson, 1984).
Deficits of the nonheme iron that is associated with enzyme systems (e.g., electron transport) can also result in significant detrimental effects on athletic performance (Beard and Tobin, 2000), while constituting only 1 percent of total
body iron. Iron-depleted, nonanemic women engaged in aerobic training were studied for six weeks with or without iron supplementation (Brownlie et al., 2002, 2004; Hinton et al., 2000). Improvements in measures of endurance capacity with training were lower in those with tissue iron deficiency and provision of supplementary iron reversed this decrease. A subsequent placebo-controlled study from the same laboratory in similar iron-depleted, nonanemic women found that iron supplementation improved indices of progressive muscle fatigue resistance (Brutsaert et al., 2003). Note that these were untrained women, which may not be analogous to what might be expected among men in assault operations.
A study of Australian soldiers consuming combat rations during operations in Australia (Booth et al., 2003) found serum ferritin levels declining by 13 percent over 12 days in a field exercise in tropical conditions while consuming an estimated 2,850 kcal/day (Booth et al., 2003). Ferritin levels in those soldiers receiving only one-half the combat ration pack (estimated to consume about 1,600 kcal) dropped by 17 percent over the 12-day operation. However, in this paper, no conclusion was made about the consequences of the alteration in ferritin status on health or performance. It is unknown whether soldiers involved in assault operations who expend significant energy (approximately 4,500 kcal/day) may present altered iron status.
Iron Status and Mental Performance. The association of iron deficiency anemia with impaired mental performance has been noted for many years, particularly in infants and young children (IOM, 2001b). Of interest to developing the assault ration are data on the use of iron supplementation to improve attention and short-term memory in adolescent girls who were iron deficient but not anemic (Bruner et al., 1996). Accuracy and attention-, memory-, and learning-reaction times were directly related to higher ferritin and transferrin saturation in young women while, in other studies, markers of cortical activation were directly related to serum iron and ferritin levels (see Lukaski and Penland, 2004 in Appendix B). Given the reported increased feelings of fatigue, loss of vigor, and confusion as well as decreased serum ferritin levels and dehydration when consuming restricted rations (Booth et al., 2003), maintaining adequate iron status is probably an important component of preserving brain function and mental performance.
Iron Status and Immune Function. Exercise affects iron requirements and metabolism (Gleeson et al., 2004). Reallocation of available circulating and body iron stores occurs due to significant physical activity and resulting high energy expenditure and iron sweat losses may result in impaired immune function.
Maintaining optimal resistance to infection is a complex process that involves many nutrients, including iron. Some studies have shown that infection by specific pathogenic organisms (e.g., Plasmodium falciparum, which causes malaria) that require iron to replicate may be less frequent in individuals who appear to be iron deficient (Nyakeriga et al., 2004). In addition, other studies suggest that continued use of oral or parenteral iron or the presence of excess
stored iron as a result of hemochromatosis may be associated with enhanced susceptibility to infections (Gleeson et al., 2004; Keusch, 1999), perhaps due to release of free iron radicals that facilitate bacterial growth or an increase in the formation of destructive hydroxyl radicals (Shephard and Shek, 1998).
In individuals who are mildly iron deficient and are treated with oral iron, such as may be the case in those engaged in assault operations, data to demonstrate an adverse effect on infection rate or severity is scarce (Keusch, 1999).
Iron Losses Through Sweat. Studies have been conducted to estimate the amount of potential losses of iron due to sweating in hot environments and as a result of exercise. Sweat loss of whole-body iron has been estimated to be 0.09 mg/m2/hour in men during 60 minutes of exercise on a cycle ergometer at 50 percent VO2max in a hot environment (35°C). The concentration decreased with time during the exercise (within the first 30 minutes of exercise) and was less than that seen with sweat during heat without exercise, which also produced less sweat (Waller and Haymes, 1996).
In a subsequent study, the iron content of sweat in recreational cyclists who exercised for 120 minutes at 50 percent VO2max in a temperate environment (23°C) was estimated (DeRuisseau et al., 2002). Sweating rates (volume/time) increased during the first hour, and then remained constant during the second hour. Sweat iron concentration was significantly lower during the second hour. Sweat iron concentrations during the second hour were approximately 0.10 mg/L at a rate of about 0.43 L/m2/hour while sweat concentrations during the first hour were approximately 0.17 mg/L at the same rate as the second; the average iron lost for the two-hour study period in the male subjects was about 0.23 mg.
These studies alone show that during combat missions sweat losses may be appreciable due to high rates of energy expenditure (generating internal body heat) and high humidity and climatic temperatures in which the activity is conducted. Losses are difficult to estimate, as they vary considerably due to the following factors: (1) environmental conditions; (2) method of sweat collection; (3) whether sweat losses include dermal losses; (4) the level of acclimation to a given environmental condition, and (5) the body size of the individual. While estimates vary significantly, loss of iron in sweat does not appear related to dietary intake (Vellar, 1968). The sweating rate (volume/time) is greater at higher temperatures, but sweat iron concentration (mg/volume) has been shown to be lower when higher volumes are produced (Waller and Haymes, 1996). The available data are too varied to adequately determine the differences between estimates in temperate versus hot environments. Therefore, taking into account only the estimated values from studies conducted in hot climates or with exercise, where the final measurement (cell-free, if available) was taken after a period of sweating, and using the lowest value if using two methods or doing a series of measurements, the estimate of the average iron content in sweat is 0.156 mg/L (Brune et al., 1986; Cohn and Emmett, 1978; Consolazio et al., 1964; DeRuisseau et al., 2002; Jacob et al., 1981; Vellar, 1968; Waller and Haymes, 1996).
Iron Losses Through Urine. In athletes, especially runners, hemoglobin and myoglobin often appear in urine (Jones and Newhouse, 1997; Weaver and Rajaram, 1992). This is thought to result from repeated foot contact with the ground where RBCs are crushed, a process termed foot-strike hemolysis. Other studies have found an increase in the loss of hemoglobin in urine or feces of endurance runners, perhaps indicating irritation and bleeding in the gastrointestinal tract (Horn and Feller, 2003).
Bioavailability. The absorption rate of iron from a typical US diet with a mix of animal and vegetable protein was estimated to be 18 percent when establishing the RDA (IOM, 2001b). If the assault ration is formulated primarily with cereal based food ingredients, it may contain more inhibitors of iron absorption, such as polyphenols in tea and coffee (Disler et al., 1975), calcium (Hallberg et al., 1991), and phytate in legumes, rice, and grains (Brune et al., 1992; Cook et al., 1997). Therefore, 10 to 18 percent bioavailability should be used when calculating the levels of iron in the assault ration depending on the source of foods in the ration. This range is in line with the 1988 Food and Agriculture Organization (FAO)/World Health Organization (WHO) recommendation that “constrained vegetarian diets” were judged to be 10 percent bioavailable (FAO/WHO, 1988) and with the value estimated for bioavailability (18 percent) if more animal foods (containing heme iron) are included in the ration (IOM, 2001b).
Determination of Estimated Needs. The RDA for men at the 97.5 percentile of estimated requirements is 8.49 mg /day (IOM, 2001b), assuming an absorption rate of 18 percent. When adjusted for a bioavailability of 10 percent, minimum daily dietary iron needed in the assault ration increases to approximately 15 mg/day.
It has been recommended that, in order to conservatively cover the increased iron losses associated with exercise and endurance training among athletes, the estimated EAR should be increased by 30 percent (IOM, 2001b). This would increase the amount required from 15 mg/day to a level at or above 20 mg /day. With significant sweating due to heavy work, high relative humidity, and high environmental temperature, iron losses of the soldier will substantially increase in field operations. If calculated by considering a loss of 6.5 L (IOM, 2004, see Figure 2-1) in temperate climates (20°C) at energy expenditures of 4,500 kcal/day, an additional 1.0 mg/day would be lost (6.5 L × 0.156 mg/L). With a rate of absorption of approximately 10 percent, this would mean that an additional 10 mg/day of dietary iron would be needed, for a total of 25 mg /day, more than two-thirds the estimated amount of 15 mg needed to meet basal losses when consuming foods with lower bioavailable iron.
Following the same approach, at 30°C the estimated volume of water lost is approximately 10.5 L/day (IOM, 2004, and Figure 2-1), which at 0.156 mg/L and a 10 percent rate of absorption, would require an additional 16.4 mg of iron each day above the 15 mg/day for basal losses (i.e., 31 g/day).
Other factors such as increased iron needs (Cook et al., 1974), the presence of ascorbic acid (see vitamin C recommendation), which has been shown to
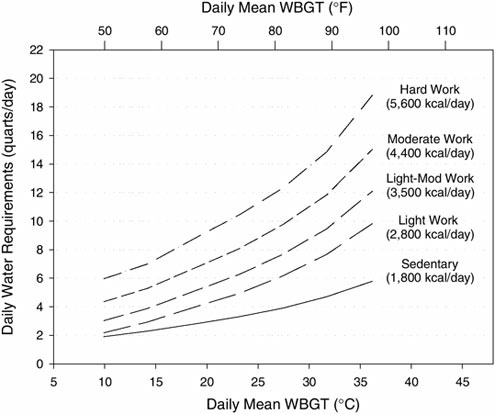
FIGURE 2-1 Approximate daily water requirements as a function of climatic temperature (wet bulb globe temperature, WBGT) and total energy expenditure (kcal).
SOURCE: Sawka and Montain (2001), International Life Sciences Institute, used with permission.
increase absorption of nonheme iron (Allen and Ahluwalia, 1997), and the reduction of phytate and tannins to the extent possible should improve the amount absorbed. Calcium has been shown to decrease absorption as well (Hallberg et al., 1991), so it would be advantageous to limit the amount of calcium contained in individual ration components that have higher iron content.
Recommending that the assault ration should contain such a high level of iron (25 or 31 g/day) might put some individuals in the military at risk of iron accumulation; namely those who carry the genetic disorder for hemochromatosis. Of special concern are those who have not been diagnosed as being homozygous at risk of iron accumulation (occult hemochromatosis). Other factors in support of a lower level of iron are that bioavailability might be closer to 18 percent, depending on the protein sources used in the ration, and that iron deficiency is rare in men. Thus, the recommendation for the assault ration is kept to 8–18 mg
iron /day. The lower level of 8 mg is based on the RDA with the expectation that the rate of absorption will increase as the body’s demand increases and that bioavailability from foods may be more than 10 percent. In situations of strenuous exercise, the higher amount of 18 mg will provide an additional 3 mg to cover the additional needs due to sweat and energy expenditure above that estimated to meet basal losses in 97.5 percent of young men, assuming a rate of absorption of 10 percent. This level of 18 mg is also the estimated median intake of men in the 19–30 age group from NHANES III (IOM, 2001b). A higher level, such as the 95th percentile of intake (31 mg/day), was not chosen due to the concerns of occult hemochromatosis and potential for interactions with other nutrients if iron fortification is needed.
In summary, since iron deficiency in men is rare, the recommended range chosen is based on current RDA, potential losses in sweat, and potential lower bioavailability from foods.
Food Form
There are possible shelf stability issues inherent in providing 18 mg iron (the majority of which is derived from supplemental sources) in the assault ration (Hurrell, 2002a, b; see also Chapter 3). Depending on which food items in the ration contain iron, it is possible that flavor may also be adversely affected (see Chapter 3). Since the primary concern in formulating this ration is to provide highly palatable food to increase energy intake to the extent possible, the level of iron could be reduced as needed to the minimum of 8 mg/day. As noted above, the committee concludes that US men have generally enough iron storages and iron deficiency would be rare and, therefore, low levels of iron intake for brief periods will have no appreciable effect on iron stores and no adverse physiologic effects.
Research Needs
-
Measure iron fecal, sweat, and urine losses in studies which simulate the environment encountered by soldiers in similar types of operations (e.g., intense physical activity, high energy expenditure, reduced caloric intake, in hot and humid conditions) in order to evaluate the additional requirements for iron.
Magnesium
RECOMMENDATION: The assault ration should contain magnesium in the range of 400–550 mg/day. This range covers the current RDA based on magnesium balance and the 95th percentile of intake of adult men.
Background
Magnesium is the second most abundant intracellular cation and functions in muscle metabolism and bone (50–60 percent of the magnesium in the body is found in bone). Magnesium is a required cofactor for hundreds of enzyme systems (Wacker and Parisi, 1968), including energy generation via the Mg-ATP complex or directly as an enzyme activator (Garfinkel and Garfinkel, 1985). In magnesium depletion, intracellular calcium increases, affecting skeletal and smooth muscle contraction.
The 95th percentile of intake is 553 mg for men 19–30 years old. The RDA for men 19–30 years old is 400 mg. The UL was established at 350 mg for magnesium from supplements, because supplements are the only known sources of adverse effects; no adverse effect is known from ingesting magnesium from food (IOM, 1997a).
Rationale for Levels of Magnesium
Magnesium and Physical Performance. Reviews of magnesium nutrition and performance have suggested that magnesium supplementation may not enhance performance although more research may be warranted (Clarkson and Haymes, 1995; McDonald and Keen, 1988). During chronic endurance exercise, however, plasma or serum magnesium concentrations fall, as does urinary magnesium (Buchman et al., 1998). This might suggest a need for additional magnesium in the diet of those who exercise regularly and strenuously. In contrast, provision of magnesium supplements were shown neither to enhance performance in a study of marathon runners (Terblanche et al., 1992), nor to increase serum or muscle magnesium levels or improve endurance performance in athletes who received 500 mg of magnesium for three weeks (Weller et al., 1998).
Other studies have found various effects on physical performance. During submaximal exercise, decreased oxygen uptake was noted when physically active men were supplemented with magnesium (270 mg/day for 4 weeks), but there was no increase in run-time to exhaustion (Brilla and Gunter, 1995). During a progressive rowing test, men receiving 360 mg of magnesium daily for 4 weeks had reduced serum lactate concentrations and oxygen uptake (Golf et al., 1993). In another study in which physically active men were evaluated, magnesium supplementation at a level of 250 mg/day for 7 weeks [total intake of 500mg/day (diet + supplementation)] increased muscle strength and power in a strength-training regimen; however, the placebo group had an average lower magnesium intake than the recommended level (Brilla and Haley, 1992). Thus, the weight of the data suggests that magnesium supplementation over recommended levels of intake has little to no effect on exercise performance.
Magnesium and Mental Performance. One study evaluated the effect of decreased magnesium levels (not necessarily due to magnesium depletion) on
mental performance. Electroencephalograms of male and female athletes with low serum magnesium levels showed decreased alpha activity compared to those with normal serum magnesium levels (Delorme et al., 1992). Other studies have not been described in the literature.
Magnesium and Immune Function. A few recent studies have evaluated the role of magnesium status on immune function in athletes (Konig et al., 1998; Mooren et al., 2003; Shephard and Shek, 1998). Magnesium in vitro mediates cell immune function (Mooren et al., 2003) via its effect on granulocyte function; however, supplementing students for two months with 365 mg/day of magnesium in a placebo-controlled study did not change blood, intracellular, or extracellular free, ionized, or total magnesium concentrations, nor did it register the alterations in immune cell function typically seen with exhaustive exercise, perhaps because the students were not considered deficient in magnesium (Mooren et al., 2003). While potentially applicable to the soldier in special operations, given the information currently available, providing additional magnesium above predicted requirements would not be of benefit.
Effect of High Levels of Dietary Magnesium. Increasing dietary magnesium intake has been shown to decrease calcium phosphate renal stone growth in individuals with previous calcium phosphate stones (Tiselius, 1997). A high-protein, low-carbohydrate diet also resulted in decreased magnesium intake, and consequently lower magnesium excretion (Reddy et al., 2002). Provision of 252 mg of magnesium as a potassium-magnesium citrate supplement (which provided 1,640 mg of potassium and 4 g of citrate total per day as well) to patients who had at least two previous episodes of calcium oxalate stones markedly reduced the risk of recurrent stone formation (Ettinger et al., 1997). No data were provided on their intake of dietary magnesium from food, nor on the extent to which the potassium and citrate provided could have contributed to the decreased rate.
Bolus doses have been demonstrated to produce diarrhea (Bashir et al., 1993) when given as a magnesium salt. Because diarrhea was reported in the study to a greater extent in patients receiving the potassium-magnesium-citrate supplement compared to the placebo (Ettinger et al., 1997), caution is warranted in using magnesium salts to enhance the magnesium content of the ration.
In summary, providing magnesium at a level equivalent to or greater than the RDA (400 mg for 19- to 30-year-old men; IOM, 1997a) should provide higher levels of intake than generally consumed (median intake 328 mg/day for 19 to 30 year-old men; 1994 CSFII; IOM, 1997a). This level of intake should have a positive influence on decreasing formation of calcium phosphate stones. Possible benefits to increasing intake above this level are not well established.
Due to adverse reactions (e.g., diarrhea) to magnesium in mineral supplements, and given the concerns about the potential for taste disturbances, it is recommended that the higher end of the range in the ration be no greater than the 95th percentile of intake of 553 mg, if it must be supplemented to ration foods as
a salt (IOM, 1997a). A ration containing magnesium at levels above 553 mg would not be of concern if no magnesium fortificant was required in the product formulation. Magnesium fortification should only be used if the lower level of 400 mg cannot be met with food sources. In this case, the supplemented amount would be at levels substantially below 350 mg, the UL for magnesium supplements.
Food Form
It is assumed that most of the magnesium in the assault ration would occur naturally in foods and food ingredients. Significant experience in the use of magnesium salts resulting in a bitter and sour taste (Lawless et al., 2003) and the potential for gastrointestinal distress at higher levels limits the advisability of adding magnesium salts to the assault ration in substantial quantities. Although it is possible, however, for magnesium salts to partially replace sodium salts in breads without deterioration in the sensory properties of the food product (Salovaara, 1982), if the added magnesium salts to achieve the recommended lower level of the range (400 mg) result in taste problems, encapsulation could be considered.
Research Needs
-
Study the effect of higher levels of magnesium on enhancing both physical and cognitive performance in studies which simulate the environment encountered by soldiers in similar types of operations (e.g., intense physical activity, high energy expenditure, reduced caloric intake, in hot and humid conditions).
-
Study the role of magnesium in maintaining and enhancing immune function and response under the same conditions as above.
Manganese
RECOMMENDATION: The committee assumes that enough manganese would occur naturally in the ration foods; therefore, additional manganese is not necessary.
Background and Rationale
Manganese is a component with various proteins, including metalloenzymes (e.g., arginase, glutamine synthetase, and manganese superoxide dismutase) and other manganese-activated enzymes; it participates in formation of bone and in amino acid, cholesterol, and carbohydrate metabolism. An AI was set at 2.3 mg/day for men 19 years and older based on median intakes (US Food and Drug Administration Total Diet Study; IOM, 2001b). The UL was established at 11 mg/day based on the risk of neurotoxicity (IOM 2001b).
The committee believes that, under the assumed conditions of short-term intake, additional manganese is not necessary and that food items in the ration will have enough manganese to avoid deficiencies. In addition, clinical signs and symptoms of deficiency have not been clearly associated with poor dietary intakes (IOM, 2001b).
Molybdenum
RECOMMENDATION: The committee assumes that enough molybdenum would occur naturally in the ration foods; therefore, additional molybdenum is not necessary.
Background and Rationale
Molybdenum is a cofactor for various enzymes mostly involved with catabolism of sulfur amino acids and heterocyclic compounds such as purines and pyridines. Its essentiality derives from the discovery of a genetic disease in which sulfite oxidase is not synthesized; that is, molybdenum is only essential when this genetic disease is present. The RDA is 45 µg/day based on balance studies. A UL was set at 2,000 µg/day (IOM, 2001b).
The committee believes that, under the assumed conditions of short-term intake, additional molybdenum is not necessary and that food items in the ration will have enough molybdenum for deficiencies not to occur. In addition, no deficiencies have been observed in healthy people and no symptoms of deficiency have been achieved in animals even when the activity of molybdoenzymes was greatly suppressed.
Phosphorus
RECOMMENDATION: The assault ration should contain 700–2,500 mg/day of phosphorus. This range is based on the RDA and 95th percentile of intake for adult men to maintain serum inorganic phosphate levels while taking into account concerns about renal stone formation observed at high levels of intake. Ration formulation at levels above 700 mg should be from food ingredients, not from the addition of phosphate salts, due to concern about diarrhea.
Background
Phosphorus, most commonly as phosphate, is found broadly in all animal and plant tissues. Most of it (85 percent) in adults is in bone. Dietary and bone phosphorus is initially found in blood and extracellular fluid. Inorganic phosphorus is then either excreted in urine or made into structural or high-energy phosphate.
Phosphorus stores and transfers energy, activates proteins, and maintains pH through its buffering capacity. The 95th percentile of intake for 19- to 30-year-old individuals in the United States is nearly 2,500 mg (CSFII; IOM, 1997a). The RDA is 700 mg for men 19–50 years of age, using serum inorganic phosphorus as the functional indicator. Hypophosphatemia occurs as a result of inadequate intake and is expressed as anorexia, muscle weakness, increased susceptibility to infection, bone pain, and mental impairment. The UL of 4.0 g was established based on normal inorganic phosphorus in the serum because dietary hyperphosphatemia has not been reported.
Adults fed mixed diets absorb about 60–65 percent of the phosphorus in foods (Heaney and Recker, 1982; Wilkinson, 1976). Phytate phosphorus in unleavened bread and cereal is poorly absorbed (IOM, 1997a).
Rationale for Levels of Phosphorus
The effects of inadequate dietary phosphorus have been studied in individuals who experience periods of significant energy expenditure. Oral or parenteral refeeding of individuals following significant energy depletion due to heavy endurance exercise, without adequate attention to supplying phosphorus, can precipitate extreme, even fatal, hypophosphatemia (Bushe, 1986; Dale et al., 1986). Thus, it is important to ensure that phosphorus is present in most of the individual items making up the ration. While phosphorus is found both in bone and soft tissue, little evidence is available to suggest that additional requirements due to high rates of energy expenditure or high levels of physical activity demand higher intakes. Estimates of phosphorus content of sweat indicate negligible amounts (less than 2.6 mg/L) of phosphorus (Consolazio et al., 1963; Nishimuta et al., 2004).
Calcium phosphate and calcium oxalate stone formation can be a concern when fluid intake is suboptimal (Borghi et al., 1996). It appears that the recommended intake for soldiers engaging in multiple assault operations should be the same as that for other individuals; thus, a level at or above the RDA should be sufficient. It is expected that the phosphorus level of the ration may well be above the RDA due to its presence in most foods and food ingredients.
While intakes above the 95th percentile of intake (2,500 mg, IOM, 1997a) in individuals consuming high-energy diets (more than 6,000 kcal/day) have not caused harmful effects, high levels of dietary phosphorus (above 3,500 mg) can result in serum inorganic phosphate levels above normal (> 1.4 mmol/L) (IOM, 1997a). Such high levels act to reduce urinary calcium loss, renal synthesis of 1,25 dihydroxyvitamin D, and serum-ionized calcium, all of which can increase serum parathyroid hormone levels (Portale et al., 1989), which increases calcium released from bone and phosphorus urine loss. If prolonged, elevated phosphorus levels can result in ectopic calcification of kidney and soft tissue (Janigan et
al., 1997; Wood et al., 1988). The inorganic phosphate levels, however, must be high enough to prevent increased bone resorption, but not so high as to increase the formation of calcium phosphate renal stones. Therefore, the range proposed, 700–2,500 mg/day, will be adequate to meet needs but not so high as to increase renal stone formation.
Food Form
Inorganic phosphates are used as cathartics and result in diarrhea in amounts above 1 g of phosphorus/dose (Grimm et al., 2001; Whybro et al., 1998). Based on this concern, it is recommended that phosphate salts be used in the assault ration only to attain the level of 700 mg, but not to increase the daily intake above 2,500 mg. Intakes from 700 mg to 2,500 mg should come from foods and food ingredients only.
Research Needs
-
Given the role of phosphorus as both a nutrient required for normal intracellular function and as well as a structural component of bone formation, studies are needed to evaluate changes (if any) in the ability of soldiers to perform physical and mental function tests under varying levels of phosphorus intake.
Potassium
RECOMMENDATION: Food developers should aim for a level of potassium in the ration of 3.3–4.7 g based on 50th percentile dietary intake and the AI for adult men.
Background
Potassium is the major intracellular cation in the body and is needed for cellular function. Potassium deficiency results in cardiac arrhythmias, muscle weakness, and glucose intolerance. The AI of 4.7 g/day for adult men was established based on effects on reduction of blood pressure and renal stone formation. The reduction of both blood pressure and renal stone formation seen with high potassium intakes appears to be related to a decrease in the sodium-to-potassium ratio. However, although there is a clear relationship between sodium and potassium, there is not enough evidence to establish requirements on the basis of this dependency. The median intake and 95th percentile for US men 19–30 years old is 3.3 and 4.3 g/day, respectively (NHANES III; IOM, 2004).
Rationale for Levels of Potassium
Potassium Losses Through Sweat. Mild potassium depletion can occur under military operations if potassium intake is not adequate. Malhotra et al. (1981) showed that male soldiers working in winter-cold conditions developed negative potassium balance at intakes of 1.76–2.15 g/day. Balance was achieved at 3.32 g/day. A review by Knochel (1993) predicted negative potassium balance in soldiers engaged in prolonged training in hot weather. They reported sweat levels around 0.3 to 0.4 g/L. Assuming that these extreme conditions and work loads produce 10.5 L of sweat (Figure 2-1), the potassium sweat losses potentially could be 3–4 g/day. In addition, aldosterone secretion increases with exercise to promote sodium retention; the sodium retention could enhance potassium losses (Sacks et al., 2001), although most studies show no difference in total body potassium under these conditions (Knochel, 1993). Finally, soldiers may experience some muscle loss due to extensive exercise and hypocaloric diets (see Friedl, 1997; Hoffer, 2004 in Appendix B). This muscle loss will release muscle potassium that may be available for metabolic functions or may be lost in the urine.
Potassium and Renal Stones. The role of potassium in preventing renal stones formation is relevant when establishing levels of potassium due to the high protein level recommended in the assault ration (100–120 g/day), even though the primary protein source may not be of animal origin. Metabolic acidosis due to protein metabolism produces increased bone resorption leading to hypercalciuria. The combination of metabolic acidosis (Arnett, 2003; Frassetto et al., 1998) and dehydration increases the risk of renal stone formation. The addition of dietary potassium, however, may ameliorate this risk. Intake of dietary potassium at the AI of 4.7 g/day (IOM, 2004) in relation to the recommended intake of 100–120 g/day of protein may decrease endogenous noncarbonic acid production (Frassetto et al., 1998; Zwart et al., 2004) and reduce the risk of renal stone formation.
Potassium-to-Sodium Ratios. Although the relationship is not clear, there is an association between sodium-to-potassium ratio and urinary excretions of both cations, salt sensitivity, and blood pressure responses to dietary electrolyte intake. The IOM report (2004) does not make a specific recommendation on the potassium-to-sodium ratio, although using the AI for potassium and sodium, the ratio is calculated to be over 3 (4.7/1.5). Based on the committee’s recommendations, the ration’s ratio of potassium to sodium (see sodium section) is calculated to be about 1.5 (4.7/3). This ratio is above what the US population consumes, which is less than 1; for many individuals it is less than 0.5. The committee concluded that, given the importance of palatability, the risk on stone formation, the loss of sodium through sweat, and the need to maintain body levels of sodium and potassium, a potassium-to-sodium ratio of 1.5 is reasonable.
In summary, recognizing that this might be a challenge for the development of the assault ration, the committee recommends aiming for 3.3–4.7 g/day of potassium in the ration; this range is based on the median intake for the US population (3.3 g/day), an attainable level, and the AI (4.7 g/day). The AI of 4.7g/day is based on long-term health consequences, including protection from hypertension and bone loss. There is no rationale for increasing potassium intake above the AI value because potassium sweat losses are as low as 0.090–0.626 g/L (IOM, 2004). The importance of adequate potassium intake for cardiac and muscle function (IOM, 2004) and to reduce the risk of renal stone formation (Curhan et al., 1993) supports the recommended AI level. Hypokalemia (serum potassium level below 136 mmol/L) may cause cardiac arrhythmias, muscle weakness, hypercalciuria, and glucose intolerance (IOM, 2004), all of which are dangerous in combat conditions. Potassium balance is affected by level of dietary potassium and sodium as well as other dietary factors such as fiber. In addition to the benefits of maintaining an adequate potassium status, the committee finds that, with the high dietary sodium levels recommended, potassium levels must be equally high.
Food Form
The difficulty in recommending high levels of potassium relates to maintaining palatability. The US diet can provide the AI level from foods depending on consumption of green leafy vegetables, fruits, root vegetables and legumes—all foods not normally part of a combat ration. Furthermore, according to NHANES III data, the US diet intake ranges from 2.9 to 3.3 g/day (IOM, 2004). It appears that providing 4.7 g/2,400 kcal in the assault ration may be difficult. The committee’s recommendation is to include foods with naturally high potassium levels in the ingredients (e.g., banana chips or spinach products that have 150 mg/oz, or nuts such as almonds), or to fortifiy foods with forms of potassium such as citrate, rather than chloride, to maintain palatability.
Another strategy to provide more potassium would be to include it as part of supplements in the form of powder to add to fluids, gels, or candy. Whether potassium is added to the basic ration foods or to supplements, however, the flavor of potassium chloride is difficult to mask; therefore, the committee believes it would be advantageous to develop palatable products that increase potassium intakes.
Research Needs
-
Identify new ways to increase potassium levels in the food and still maintain palatability.
Selenium
RECOMMENDATION: The ration should include at least 55 µg selenium but not more than 230 µg. This is based on the current RDA and 95th percentile of dietary intake for adult men.
Background
Selenium functions through its association with selenoproteins. Glutathione peroxidases and iodothyronine deiodinases are selenium-dependent enzymes whose action might affect physical performance; in addition, the stressful situations under consideration might affect their level of activity. Numerous studies have demonstrated the increase in reactive oxygen species and oxidative stress developed in muscle after intense exercise; this increase might result in muscle damage and fatigue and can be attenuated by a properly developed antioxidant defense system. Glutathione peroxidases are critical enzymes in that they participate in one of the most essential antioxidant systems in the body by catalyzing the decomposition of oxygen-reactive species that form during exercise. In this regard, the supplementation of diets with selenium has been considered as a way to ensure the proper functioning of glutathione peroxidases. Selenium also forms complexes with iodothyronine deiodinases, which regulate thyroid hormone metabolism.
The EAR was based on two intervention studies and was established at 45 µg/day for men 19–30 years old, with the RDA established at 55 µg/day for this same group. The median intake was 154 µg/day for males 19–30 years old and the 95th percentile of dietary intake is 230 µg/day (NHANES III, IOM, 2000). The UL for adults was based on the appearance of signs of seleniosis and was established at 400 µg/day (IOM, 2000). When selenium deficiency occurs in association with other deficiencies or stresses, it can lead to biochemical changes that predispose soldiers to illness. On its own, however, selenium deficiency does not appear to be a real concern.
Rationale for Levels of Selenium
As with other micronutrients, the need to recommend a different selenium level from the established RDA for assault rations depends upon possible increased selenium needs for the soldiers due to stress, immune function, and level of physical activity. There are data that show the effect of selenium on immune function (Broome et al., 2004; Ravaglia et al., 2000), activity of antioxidant glutathione peroxidase during exercise (Clarkson and Thompson, 2000; Sen and Packer, 2000), and energy needs related to thyroid function (Arthur et al., 1993; Bianco et al., 2002; Vanderpas et al., 1993). Selenium is involved in both antioxidant metabolism through glutathione peroxidases and thyroid func-
tion; thus, any change in oxidation status that includes exercise and stress and energy metabolism with includes thyroid function would be impacted by deficiency in selenium. For healthy individuals under combat conditions, however, there is no clear evidence to support raising the requirement of selenium.
Research Needs
-
Investigate the effects on performance of supplementation with selenium for periods of high-energy expenditure and physical and mental stress comparable to those encountered by soldiers in assault missions.
Sodium
RECOMMENDATION: The assault ration should contain 3 or more grams of sodium, the specific amount depending on palatability and acceptability of the ration. In addition, to ensure that the needs of individuals who lose salt in excess or who are in extremely hot or strenuous situations are met, additional sodium up to 12 g should be available as a supplement and in salt tablets. Food developers should aim at including sodium and other electrolytes as a supplement in the form of candy, gels, or powder to be mixed with fluid; however, because palatability will limit the amount of additional sodium that can be added to these products, sodium should also be available in the form of tablets to be provided by medical personnel or under medical guidance when needed.
Background
Sodium is the main cation in the extracellular fluid and is required to maintain plasma volume. Sodium also maintains the potential of the membrane, playing an important role in active transportation of molecules through the membrane. A low level of sodium or hyponatremia affects blood lipids, insulin resistance, and cardiovascular disease. It often is not associated with low dietary intake but rather with excessive losses (e.g., during exercise) or consumption of hypotonic fluids. The AI value of 1.5 g/day (65 mmoles/day) for men 19–50 years old (IOM, 2004) is based on the replacement of daily obligatory losses of sodium of up to 0.18 g/day calculated by adding urinary losses (0.005–0.035 g/day), stool losses (0.01–0.125 g/day), and nominal sweat (0.025 g/day) (see Shirreffs, 2004 in Appendix B). Other considerations in setting the AI were the evidence supporting that 1.5 g/day would minimize potential adverse effects on blood lipid concentrations and insulin resistance and the fact that this intake would also be met with a typical Western diet. In addition, that level would cover sodium losses by unacclimatized individuals. The UL is 2.3 g/day and considers the risk of high blood pressure (IOM, 2004).
Rationale for Levels of Sodium
Sodium Losses Through Sweat. As part of the electrolyte regulatory system, urinary sodium losses increase with increases in dietary sodium intakes. In addition, urinary sodium and sweat sodium concentrations decrease when individuals become dehydrated, causing a decrease in plasma volume. Conn (1949) showed sodium balance in healthy persons sweating 5–9 L/day with an intake of sodium 0.76 g/day (33.2 mmoles/day) to 1.28 g/day (55 mmoles/day). As mentioned above, the AI value for sodium (1.5 g/day) accounts for sweat losses for unacclimatized individuals in addition to achieving balance in relatively sedentary individuals.
There also is a large variability in sodium losses between individuals due in part to variations in adaptation to heat and exercise capabilities. Thus, the committee’s recommendation is based on the assumption that soldiers doing moderate work (4,400 kcal/day) could lose up to 10.5 L water in sweat each day (see Figure 2-1), with ranges of sweat sodium concentrations between 0.12 and 4.2 g/L depending on the sodium intakes, subject characteristics, ambient conditions, and length and type of activities (Armstrong et al., 1985; Consolazio et al., 1963; Costill et al., 1976b; Dill et al., 1976). Calculations that included the maximum potential sodium losses from sweat could lead to high sodium losses, such as 10–12 g/day. Costill et al. (1976a) reported increases in aldosterone secretion and decreases in urinary sodium losses with 60 min of 60 percent VO2max and 30°C; thus, the body compensates for the elevated sweat sodium losses.
The recommended value of 3 or more grams per day was increased from the AI (1.5 g/day) to allow for the increased sodium losses that occur with elevated energy expenditure and ambient temperatures. Allsopp et al. (1998) showed that acclimated individuals at ambient temperature of 40°C and dietary sodium intakes of 4 g/day for 8 days had sweat losses of 1.8 g/day. Taking this approach and assuming that the AI level includes 0.1 g sweat losses, then the value for sodium need would be 3.2 g/day (1.8 + 1.4 = 3.2). A second approach is to assume heavy exercise, approximately 4,400 kcal/day under two different ambient temperatures. If the temperature is high (30°C), then the total sweat losses will increase to about 10.5 L water/day (IOM, 2004, or Figure 2-1). With the sweat sodium concentrations varying from 0.23 g/L (Allan and Wilson, 1971, no dietary information, 40°C, 60 min of exercise) to 1.4 g/L (Inoue et al., 1999, no dietary information, at 43°C, 90 min of exercise), sweat sodium losses can be 2.3 g to 14 g/day. Using the lower level of 0.23 g/L, assuming 10.5 L of sweat, the calculated value for sodium needs is 3.7 g/day ([0.23 * 10] + 1.4 [AI − 0.1]) = 3.7). If the temperature is low (20°C), then the sweat losses will be less—about 6.5 L/water per day (IOM, 2004 or Figure 2-1)—but the concentration of sodium in the sweat will likely be more. For example, if 1.4 g/L were used, then as much as 9.1 g/day could be lost. Consolazio and co-workers (1963) showed a range of sodium sweat losses from 1.6–11.0 g/day when working at 37.7°C for 7.5 hr.
Given the large variations in energy level, ambient conditions, and individual acclimatization to ambient conditions (Conn, 1949), the recommendation is to provide ≥3 g/day of sodium, with additional sodium up to a total of 12 g provided through supplementation. Palatability will be a factor that limits the amount in the ration. Based on intake data for the US healthy population, it is not envisioned that an amount significantly higher than 3 g would be acceptable (see Food Form below).
When sodium intake does not meet losses, aldosterone secretion increases to conserve sodium by reducing urinary sodium levels (Costill et al., 1976a). Given the body’s natural conservation, combined with decreases in sweat sodium concentration in acclimatized subjects in most work and heat conditions, a level of approximately 3 g/day of sodium is adequate.
Other Sodium Losses. For nonacclimatized soldiers or for those who lose excessive salt, extra salt may be needed. In addition, when average daily temperatures increase above 30°C/day and work load exceeds 2,800 kcal/day, sweat losses may exceed dietary intakes (Figure 2-1). Therefore, for these cases, extra sodium should be available (up to 12 g). The committee recommends that this be provided through a supplement, either to be added to their water supply or in candy or gel preparations. Palatability will limit the amount of sodium that can be added to these products and, therefore, sodium should also be available in the form of tablets to be provided by medical personnel or under medical guidance when needed.
In addition to fluid loss through sweat, more fluid may be lost due to diarrhea. For these cases, dry powder preparations that could be mixed with water should be available during combat or upon return to the base.
Sodium and Renal Stones. The committee had concerns about renal stones because soldiers could easily become dehydrated, and renal stones have occurred among troops (personal communication, C. Koenig, USARIEM, November 19, 2004). It is generally assumed that urinary calcium excretion reflects urinary sodium especially at urinary sodium levels above 2 g/day (Devine et al., 1995; Goulding and Lim, 1983; Massey and Whiting, 1996). Dawson-Hughes et al. (1996) showed that healthy men and women over age 65 had positive correlations of sodium and calcium excretion when calcium intake was over 1,000 mg/day with a normal sodium intake. Space flight data demonstrate a similar relationship (Whitson et al., 1997). The calcium recommendation for this ration is 750–850 mg/day, a level that should not promote renal stones with the sodium intakes of 4 g/day.
Food Form. The committee evaluated the feasibility of providing 3 or more grams of sodium per 2,400 kcal without compromising palatability. Intake data from NHANES III for 1988–1998 estimate that males 19–50 years of age consume 1.9–8.2 g/day of sodium (IOM, 2004) at energy intakes of 1,223–4,703 kcal (IOM, 2002a). These data suggest that males in this group would find 3 g/2,400 kcal acceptable. Acceptability of sodium levels in foods has been well
studied; studies on salt levels with highest acceptability in specific foods have been conducted (Norton and Noble, 1991). Some people prefer high-salt diets when exercising (Leshem et al., 1999). The available data support the recommendation that ≥3 g/day of sodium would not only be acceptable but necessary for palatability for individuals who may have some decreases in appetite due to stress and exercise (Beauchamp et al., 1991).
Due to the impact of dehydration on performance after heavy activity, individuals should be encouraged to take extra sodium (see Shirreffs, 2004 in Appendix B). To ensure that the needs of individuals who lose salt in excess or who are in extremely hot or strenuous situations are met, additional sodium up to 12 g should be available as a supplement and in salt tablets. For the supplemental sodium, carbohydrate gels—some of them already commercially available—are easy to consume and carry and provide a feasible form to add sodium. Due to palatability issues, however, the amount of sodium in these products is only about 1 percent. Commercially available beverage supplements contain between 2.8 and 4.5 g of sodium per liter of water. With good rehydration procedures, this concentration of sodium in water would easily replace sodium sweat losses (Maughan and Shirreffs, 1997). To the extent possible, this supplemental amount (up to 12 g) should be included in the form of candy, gels, or powder to be mixed with fluid. However, because palatability will limit addition of sodium to these products, salt tablets should also be available and provided by medical personnel or under medical guidance when needed.
In summary, the AI for adult men (1.5 g/day) accounted for sodium sweat losses for unacclimatized individuals, but this level is not appropriate for individuals who are highly active, are exposed to prolonged heat, or who lose sodium in excess. The committee’s sodium recommendation is based on estimates of sodium losses due to heavy exercise in potentially extreme temperatures, the interaction of high sodium and protein intakes with calcium losses in an environment prone to dehydration (Giannini et al., 1999; Whitson et al., 1997), and the importance of palatable food. Although this recommendation (≥3 g/day) is higher than the UL (2.3 g/day), the committee does not anticipate any adverse health effects on high blood pressure because the UL was established considering chronic intakes and not for short periods envisioned for the consumption of the assault ration; in any case, palatability issues will limit the amount of sodium in the ration and the tablet supplements should only be provided under medical guidance to individuals that lose excess salt or in extremely hot or strenuous situations.
Research Needs
-
Evaluate the additional requirements for sodium and measure fecal, sweat, and urine losses in studies which simulate the environment encountered by soldiers in similar types of operations (e.g., exercise, high energy expenditure and reduced caloric intake, in high humidity and temperature).
Zinc
RECOMMENDATION: The assault ration should contain a level in the range of 11–25 mg of zinc. This range is based on the RDA for adult men, established with a factorial approach, and potential sweat losses during intense physical activity.
Background
Zinc participates in many physiological functions with catalytic, structural, immunologic, and regulatory roles that are essential for life. More than 100 enzymes depend on it for activity, and it is due to its properties as an electron acceptor that zinc becomes an essential element for enzymatic activity. Zinc-containing enzymes participate in macronutrient metabolism. Its importance in the proper functioning of the immune system derives in part from its structural role in the binding of tyrosine kinase to T-cell receptors. Because zinc has multiple roles, deficiency presents multiple signs and symptoms. Some of the clinical effects seen in zinc deficiencies are depressed growth, immune dysfunction, diarrhea, altered cognition, and altered appetite.
The RDA is set at 11 mg/day for adult men and was based on a factorial approach in which the principal indicator was the minimal quantity of absorbed zinc adequate to replace endogenous losses. The UL was set at 40 mg/day based on evidence of no adverse effects noted at this level (i.e., no suppression of immune response, no decrease in high-density lipoprotein cholesterol, and no reduced copper status). The median intake and 95th percentile intake in healthy US men age 19–30 years is 14.8 and 23.9 mg/day, respectively (IOM, 2001b).
Rationale for Levels of Zinc
Zinc Losses Through Sweat. Intense exercise is considered to affect zinc status. One of the factors affecting plasma levels is zinc loss either through urine or sweat. Urinary losses of zinc have been documented to rise from 0.4–0.7 mg/day during a 34-day training exercise in military field conditions (Miyamura et al., 1987). When sweat losses were studied over 16 days in the heat and after submaximal exercise, zinc losses ranged from 13.7 mg/day (first 4 days) to 2.2 mg/day (day 5 to day 12) with declining losses during acclimatization (Consolazio et al., 1964). Whereas one might have expected a rise in plasma zinc due to muscle damage or turnover, these losses were accompanied by small declines in serum zinc. Tipton et al. (1993) found that when sweat rates were included in the calculations, the rate of zinc loss was the same under hot (35°C) and neutral (25°C) conditions. Zinc losses in sweat might reach significant amounts and should be considered when recommending a level for the ration. The committee recommends a range of 11–25 mg in the ration. The lower limit of the range is
based on the RDA for adult men; the upper limit is based on the addition of potential sweat losses during intense physical activity (14 mg) for a total of 25 mg.
Zinc and the Immune System. The beneficial effect of zinc as a modulator of the immune system and, particularly, in the prevention of upper respiratory infections is promising (Bhaskaram, 2002), but research findings have not reached clear, definite conclusions. Studies with the elderly population have shown either no effect of supplementation with zinc (Bogden et al., 1988), a mix of beneficial and adverse effects (Bogden et al., 1990), or beneficial effects only when mixed with other micronutrients (Bogden, 2004). There is conflicting evidence on whether zinc supplements shorten duration of colds; however, there is no evidence that supports the idea that zinc supplements prevent upper respiratory infections (Eby et al., 1984; Farr et al., 1987; Jackson et al., 2000; Prasad et al., 2000; Turner and Cetnarowski, 2000). Several immune function parameters decline with zinc deficiency, but zinc supplements at either 15 or 100 mg/day suppressed delayed-type skin hypersensitivity (an indicator of immune system function) in subjects > 60 years (Bogden et al., 1990). Similar findings on the impairment of the immune function were observed by Chandra (1984) when healthy adults were given 300 mg of zinc for 6 weeks. Unfortunately, there are no data on the effects of 15 mg/day on immunity in young healthy adults.
Zinc is one of the essential minerals that, due to its involvement as a cofactor with up to 100 enzymes, has been considered a dietary supplement for athletes. A review of the published literature, however, reveals that there is no strong evidence that zinc supplements in normally nourished individuals have an effect on immunity or physical and cognitive performance (Lukaski, 2004). A balance study conducted with obese men for over 40 days found that restricted-calorie diets (400 kcal) resulted in an increase in serum zinc, and also an increase in urine and fecal zinc; but zinc balance was not negative until 30–40 days (Lowy et al., 1986). The relevance of this study for the highly fit individuals who consume combat rations is not known.
Other Considerations. The committee is concerned that accurately assessing zinc status in stress conditions might not be feasible due to shifts between compartments (via cytokines) and the high variability in sweat and urine losses. Zinc intakes can be quite low even under normal dietary conditions and deficits resulting in health and performance effects could possibly develop. Meetings with the USARIEM representatives revealed that soldiers probably consume insufficient amounts of zinc during military operations, and that they could become mildly zinc deficient under stress. Due to these uncertainties (i.e., variable sweat losses, difficulties in assessing zinc status, marginal zinc status of many soldiers), the committee is taking a conservative approach, recommending zinc in the range of 11–25 mg. The higher end is meant to account for potential sweat losses of about 14 mg/day. It is unlikely that this amount (25 mg) will have any adverse effects on the immune system of young healthy adults. Although several studies reported gastrointestinal adverse effects at higher doses
of zinc (> 100 mg/day) when ingested as zinc lozenges (Al-Gurairi et al., 2002; Garland and Hagmeyer, 1998), side effects at the level recommended here (25 mg/day) are not anticipated. The committee has concerns, however, that a higher limit of 40 mg/day, which is the UL for adults, might result in interactions with other minerals and undesirable anorexic effects or some gastrointestinal tract intolerance. Although supplementing with high amounts of iron (in the range of 34–400 mg) might interfere with zinc absorption (Kordas and Stoltzfus, 2004; Solomons and Jacob, 1981; Troost et al., 2003), with the amounts of iron recommended here (8–18 mg/day) there should be no such interference.
Questions regarding the bioavailability of zinc from the ration foods remained unanswered (see Food Form below).
Food Form
Zinc will be naturally present in ration foods such as cereals and red meats but may also need to be added to foods. Due to palatability issues, fortification with zinc should be done in foods, in which off-flavors can be masked, rather than in gels, candy, or powder forms. In addition to palatability issues, food developers should consider that the range of zinc recommended might affect appetite, a concern for soldiers in combat operations who already undereat.
As mentioned above, the bioavailability of zinc from the ration foods, whether zinc is naturally occurring or added, is not known. Estimates of absorption of zinc from foods differ depending on the data used (total diet data compared to single meal data) and on the nature of the diet considered. For example, the estimated absorption of zinc used in establishing the EAR (and, thus, the RDA) was 41 percent (IOM, 2001b) when data from studies conducted with male subjects were considered in a single diet category; in comparison, the International Zinc Nutrition Consultative Group (IZiNCG, 2004) estimated 26 and 18 percent absorption when calculated as a function of the diet type (i.e., mixed or cereal-based diet, respectively) and with data from studies conducted with both male and female subjects. When zinc doses up to 12 mg were given as a supplement to male and female subjects, average intestinal absorption was 55 percent (Payton et al., 1982). Another study in which subjects were given a total level of zinc of approximately 15 mg/day reported an average absorption of 64 percent (August et al., 1989). Thus, while there is substantial variability in estimates of zinc bioavailability and the bioavailability of recommended 14 mg added to the RDA is not known, it is likely to be in the same range of 45 to 65 percent.
Research Needs
-
Determine the effects of supplemental levels of zinc on suppressing appetite for those in a stressful situation and under the hypocaloric rations in the field.
-
Determine the effects of zinc on flavor and palatability of rations and identify ways to mask objectionable flavors.
-
Measure fecal, sweat, and urine losses in studies which simulate the environment encountered by soldiers in similar types of operations (e.g., exercise, high energy expenditure and reduced caloric intake, in high humidity and temperature) in order to evaluate the additional requirements for zinc.
Other Bioactives and Dietary Supplements
General Background
In recent years there has been increased interest among athletes in augmenting traditional diets to optimize physical and mental performance. Earlier approaches of adding more protein or “carbo-loading” are still practiced by athletes. In addition, there has been increased use of herbals and bioactive components of foods; these include a variety of substances ranging from essential and nonessential amino acids, metabolites, energy enhancers, “muscle builders,” and stimulants such as caffeine. Frontline soldiers wishing to gain a performance edge may well seek out and use such nontraditional food components, stimulants, and herbals. The key question is whether any of these compounds enhance performance with relatively few adverse effects at levels of use. Of importance to developing a ration for short-term, high-energy assault operations is whether any of these compounds should be provided in the ration to enhance performance.
A number of classes of compounds might be considered performance enhancers that could fall into the broad category of “other bioactive food components.” Supradietary levels of traditional nutrients such as tyrosine, tryptophan, or carotenoids can be considered to function as bioactives. Megadose levels of vitamin E or C would be in this category because these levels are consumed for pharmacological effects. These nutrients are discussed in earlier sections of this chapter. Supplements of biological metabolites like creatine, L-carnitine, or coenzyme Q10 are also part of this category. In addition, thousands of plant polyphenols such as the flavonoids make up a huge category of compounds that in some situations have antioxidant and perhaps other properties. Stimulants such as caffeine have been shown to maintain cognitive performance. Finally, herbals such as ginkgo, ginseng, and tea and berry extracts contain potentially bioactive compounds and are reported in some studies to maintain or enhance performance.
Costello and Chrousos (2004 in Appendix B) evaluated the potential performance-enhancing effects of a number of bioactive food and dietary supplements. Among the materials reviewed were the neurotransmitter precursors tyrosine and L-tryptophan, the potential energy enhancers L-carnitine and coenzyme Q10, and several herbals reported to increase energy or cognitive function. They did not find compelling evidence that any of these compounds enhanced performance. Except for creatine, few studies have been carried out in a randomized
and blinded manner. Enough evidence warrants continued investigation of some of the components reviewed. As Costello and Chrousos suggest, a number of issues need to be considered in the design of future studies, including overtly controlling for coping status of subjects because those coping poorly under stress may respond better to the supplemented bioactive component than those who are coping well. The researchers also suggest future studies to identify food matrixes that can serve as delivery vehicles for bioactive substances. The committee discussed a variety of bioactive compounds or extracts (e.g., carnitine, creatine, Ginkgo biloba extract, glutamine) and concluded that, with the exception of caffeine, inclusion in the assault ration is not appropriate at this time. The following paragraphs highlight the committee’s conclusions and recommendations on selected bioactive compounds that enhance performance (e.g., caffeine) and others that show promise but need further study as performance enhancers (e.g., creatine) or promising antioxidants (e.g., flavonoids).
Caffeine: Recommendation and Rationale
RECOMMENDATION: The committee supports the recommendations of past IOM committees regarding caffeine use for the military. Rations for combat missions should be supplemented with caffeine at levels of 100–600 mg, with no more than 600 mg in a single dose.
The effect of caffeine as a restorative compound when subjects are sleep deprived and as a performance enhancer for athletes or soldiers in sustained military operations is well documented (IOM, 2001a; Kalmar and Cafarelli, 2004; Magkos and Kavouras, 2004; Penetar et al., 1994). The Committee on Military Nutrition Research (CMNR) has been asked to evaluate the use of nutrients for performance enhancement in previous requests from the US Army Medical Research and Material Command. In 1994, the report Food Components to Enhance Performance (IOM, 1994) recommended that the military conduct research on the mechanisms of caffeine’s effects on cognitive performance, on the feasibility of including caffeine in a different food vehicle in the ration, and on the optimized levels of caffeine that could help develop maximum performance for both caffeine-habituated individuals and casual caffeine users. That committee concluded that caffeine is a safe ingredient at levels necessary to maintain alertness and to overcome the cognitive function detriment resulting from sleep deprivation. For those used to caffeine, levels of 300–600 mg/70 kg person were recommended for alertness.
In 1998, as a result of new research on caffeine completed by the military and the need to make management decisions about its use, the military asked the CMNR to confirm its previous recommendations on caffeine use, and to provide recommendations on health risks of readily available caffeine. The committee was also charged with recommending safe levels for efficacy, better alternatives
to caffeine, feasible vehicles to deliver caffeine, as well as recommendations on whether including it with other compounds would increase its effectiveness.
That committee concluded in the report Caffeine for the Sustainment of Mental Task Performance that caffeine in doses of 100–600 mg may be used to maintain cognitive performance, especially when an individual is sleep deprived or when fast reactions and acute vigilance may be needed (IOM, 2001a). A level of 200–600 mg was found to enhance physical endurance. Those amounts might be best provided in increments of 100 mg every 3–4 hours, and a single dose should not exceed 600 mg regardless of the habituation level. A recent review indicated that at those moderate doses the diuretic effect of caffeine is minimal (Maughan and Griffin, 2003). Another literature review to assess potential effects of caffeine during exercise suggested that athletes will not incur detrimental fluid-electrolyte imbalances or dehydration if they consume caffeine beverages in moderation (Armstrong, 2002). The committee also concluded that there were no current alternatives to caffeine for enhancing physical and cognitive performance when soldiers are sleep deprived, but that research should be conducted on the synergistic effects of using a combination of carbohydrate and caffeine. Chewing gums and food bars were suggested as the best delivery methods for caffeine (IOM, 2001a).
Caffeine is currently consumed by many Americans on a daily basis to maintain cognitive function. Soldiers also consume this stimulant regularly and would suffer withdrawal symptoms if caffeine were not available during the assault phases of operations. Provision of caffeine supplements in rations with the appropriate user advice is recommended, especially for those soldiers who will have minimal opportunities for sleep.
More recent published literature supports the recommendations of the IOM committee. The effects of caffeine ingestion on target detection and rifle marksmanship following a military exercise were investigated. When two doses were provided at 5 and 2.5 mg/kg of body weight prior to and following the exercise, respectively, target detection and engagement speed was improved. More complex tasks, such as friend-foe discrimination and shooting performance, were unaffected by this caffeine supplementation regime (Gillingham et al., 2004). Similar findings were reported by Tikuisis et al. (2004) when supplementing caffeine to sleep-deprived subjects. At the end of a 22-hour period without sleep, subjects who consumed a single dose of 400, 100, and 100 mg of caffeine at different times prior to the task showed improvement in target detection (a measure of cognitive function) versus decrements reported by the subjects who did not use caffeine. Caffeine, however, was not effective in restoring decrements in shooting accuracy and precision (a measure of psychomotor function) that occur with sleep deprivation.
Caffeine has also been studied in connection with improving physical performance. One study showed that physical performance as measured by rating of perceived exertion, time to complete a task, and time to exhaustion was also
improved with a single dose of 400 mg and with two 100 mg doses of caffeine at intervals of a few hours during 24 hours of wakefulness (McLellan et al., 2004). Improvements in physical performance with caffeine were also reported with high-intensity cycling studies (Doherty et al., 2004).
Research Needs
-
Determine the optimal levels of caffeine supplementation in hot and cold climates and at high altitude.
-
Conduct further research on the optimal delivery methods of caffeine in rations.
Muscle Mass Enhancement Bioactives—Creatine and Other Bioactives
Dietary supplements are frequently used by athletes in an attempt to increase muscle mass or lean body mass (Clarkson and Rawson, 1999). Among the supplements used for this purpose have been the hormone dehydroepiandrosterone, β-methyl-hydroxy-β-methybutryrate), amino acid and protein supplements, elements (e.g., chromium and boron) as well as creatine. Reviews of such practices have concluded that “overall, it appears that there is little scientific documentation that most nutritional supplements will increase muscle mass as purported…” (Clarkson and Rawson, 1999, p. 324). The authors called for further research to document efficacy of supplements, possible mechanisms of action, and long-term safety. They did note that there was some evidence for the effectiveness of creatine in increasing muscle mass from a review of more than 15 studies.
Reports from observers in field operations (personal communication, C. Koenig, USARIEM, November 19, 2004) indicate widespread use of dietary supplements by soldiers. Given the lack of demonstration of efficacy and the potential for abuse of such substances, concern is warranted.
RECOMMENDATION: The committee notes the reports of substantial current use of the supplement creatine by troops. The potential efficacy of creatine on muscle performance during combat situations appears to be very limited. The committee is concerned about the metabolic effects of long-term use of this supplement, as well as the potential impact of withdrawal effects due to a sudden consumption decrease of creatine as troops begin assault operations. Both of these issues require attention.
Creatine continues to be a popular oral supplement among soldiers who are interested in enhancing muscle mass and athletic performance. The committee was informed by a team of military medical officers (personal communication, F. Christopher, S. Lewis, T. Phelps, US Army, October 22, 2004) that many
combat troops currently consume creatine supplements. Thus, the efficacy and safety of this supplement is of special interest to the committee.
In 2000, the American College of Sports Medicine (Terjung et al., 2000) issued a consensus statement on the physiological and health effects of oral creatine supplementation. That panel noted that creatine supplementation can increase muscle phosphocreatine content in some individuals, leads to weight gain within a few days of supplementation, likely due to water retention, and is associated with an enhanced accrual of strength in strength-training programs. Performance enhancements, however, are small and are found only under specific exercise conditions. The group concluded that “the apparent high expectations for performance enhancement, evident by the extensive use of creatine supplementation, are inordinate” (Terjung et al., 2000, p. 706). A recent review of the creatine literature identified roughly 300 studies that have been carried out to evaluate the effects of creatine on exercise performance and concluded that it appears that creatine allows some athletes, perhaps due to their genetic makeup, to train with higher work loads; thus, it promotes strength gain in a resistance training program (Rawson and Clarkson, 2003). Creatine appears to improve performance in repeated, high-intensity exercises each lasting less than 30 seconds (e.g., sprinting activities) (Rawson and Clarkson, 2003).
Research Need
-
Pursue randomized, well-controlled trials to elucidate the risks (e.g., withdrawal effects) and potential benefits (e.g., cognitive performance) of taking selected bioactives that are often consumed in the field, such as creatine; these trials should be conducted under conditions that mimic combat situations.
Food-Based, Mixed Antioxidants: Recommendation and Rationale
RECOMMENDATION: Food items should be designed to contain whole pieces or purees of fruit and other foods high in flavonoids and other polyphenols in order to enhance acceptability of rations and increase the quantity of naturally occurring antioxidants.
Antioxidant defense systems protect the human organism from tissue injury that occurs during chronic or acute exercise. Antioxidant nutrients such as vitamins C and E, the carotenoids, and selenium have received a great deal of scientific interest regarding their abilities to enhance a body’s ability to cope with excess oxidative stress brought on by exercise. These nutrients and food components are also under study for their abilities to enhance or maintain cognitive functions. The committee’s conclusions regarding those nutrients are found earlier in this chapter under each nutrient discussion.
Many foods of plant origin, especially foods derived from fruits, whole grains, and vegetables, contain a host of other less well characterized compounds that may function as cellular antioxidants and have the potential to aid in enhancing performance or decreasing the time of recovery after acute energy expenditure. Moreover, some of these other food components may act in synergy with other antioxidant defense systems to enhance performance. Antioxidant defense mechanisms in the body include a variety of enzymes such as catalase, superoxide dismutase, and glutathione peroxidase as well as nonenzymatic counterparts including vitamins C and E, carotenoids, and glutathione (Nijveldt et al., 2001).
One class of antioxidant compounds from plant-based foods is the polyphenols. Several hundred polyphenols have been isolated from edible plants. While they are primarily secondary metabolites of plants and serve in defense mechanisms in those plants, they have structural elements that suggest that they may play a role in prevention of oxidative stress in mammals (Manach et al., 2004).
Flavonoids, a subclass of the polyphenols with about 4,000 compounds, have received extensive research attention. Flavonoids occur naturally in fruits, vegetables, and beverages such as tea and wine (Nijveldt et al., 2001). There are a number of favorable in vitro investigations on the impact of various flavonoids on biomarkers of disease or symptoms such as cardiovascular events, inflammation, antitumor activity, and thrombosis. While outcomes of these studies need to be verified in vivo and in clinical trials and thus are less relevant to the combat soldier during assault missions, the general antioxidant effect of these compounds may be important to overall performance.
More relevant to the combat soldier during assault missions is the maintenance of an antioxidant defense system that optimizes the body’s ability to cope with oxidative stress during periods of high physical and mental activity. The antioxidant defense systems should protect the body systems from excess production of reactive oxygen and nitrogen species. While it is not known whether the plant polyphenol substances specifically can enhance performance or decrease recovery time, it has been hypothesized that flavonoids may have additive effects with the endogenous reactive species’ scavenging mechanisms (Liu, 2004). Various flavonoids, at least in vitro, have been shown to directly scavenge free radicals and to interact in antioxidant enzyme systems (Nijveldt et al., 2001). Much more work is needed in the context of assault operations to determine the synergy of these compounds with endogenous enzyme protection systems and with known dietary antioxidants.
Flavonoids are found in high concentrations in foods like fruits, vegetables, tea, and chocolate. It is important for the components of rations to have both good taste and optimal nutritional value. Both goals can be achieved by using food matrixes that contain some of these food sources. For example, dried fruit or fruit pastes (e.g., blueberry, grape, and cranberry) can be used in food items such as fruit roll-ups, cookies, purees, or gels. These fruit items contain significant levels of flavonoids as well as carotenoids and potentially vitamin C if
processing conditions are mild. Concentrated fruit can also be fortified with vitamins C and E. Chocolate items have always been widely accepted by soldiers and have concentrated sources of flavonoids and other polyphenols. Coffee, and to a lesser extent tea, are also consumed by soldiers and, thus, provide flavonoids as well. There is no compelling reason to provide supplements or pills of concentrated flavonoids at this time. There are ample opportunities to include foods and beverages high in polyphenols for both acceptability and possibly for health reasons.
Research Needs
-
Determine whether the addition of foods, food extracts, and beverages that are all high in antioxidant polyphenols enhances the acceptability of the rations.
-
Determine whether the addition of foods, food extracts, and beverages that are high in antioxidant polyphenols would reduce the effects of oxidative stress under similar combat conditions, either along or through synergy with endogenous enzyme protection systems and known dietary antioxidants.
WATER REQUIREMENTS
Although the committee was not charged with making recommendations regarding water needs, the close links between diet, hydration status, and physiological function cannot be overlooked. Proper hydration is a major factor in maintaining sustained mental and physical performance. Information provided to the committee indicates that 4–5 L of water per day is made available during a combat mission. Part of these water needs is used to replace fluid losses due to the intense exercise. For example, assuming 4,400 kcal of energy expenditure, it can be estimated that sweat volumes could be as high as 6.5 and 10.5 L at 20 and 30°C, respectively.
In addition to sweat losses and metabolic rate, water needs are governed by nutrient intake, primarily protein and salt intake. Protein and sodium provide most of the excreted osmoles as urea and sodium and accompanying anions. The recommendation of 100–120 g of protein per day, while reasonable from a nutritional standpoint, will induce a higher water excretion via the kidneys to handle the increased solute load due to the production of approximately 16–19 g of urea nitrogen, 2–5 g more than with a 80 g protein intake. This additional increment of urea would require about 0.2 L more of urine, assuming a urinary concentration of 800 mOsm or as much as 0.4 L assuming a more conservative urine concentration of 400 mOsm. Maximal urinary concentration is approximately 1,200 mOsm. When such estimates are experimentally determined, subjects are usually in nitrogen balance, that is, urinary excretion of nitrogen equals nitrogen
intake. Gamble (1947) found that 50–100 g of carbohydrate per day was more beneficial than protein to reduce renal water excretion and enhance hydration in fasting individuals. Other studies have shown that 100 g of carbohydrate reduce the deficit of body water by preventing ketosis (thus, decreasing ketones contribution to the osmolar excretion requirements) as well as reducing required urine volume due to the antinatriuretic effect of insulin stimulated by the dietary glucose. In the present situation, the provision of some energy and ample carbohydrate improves protein utilization over that in a fasting and severely hypocaloric state, resulting in a decreased production of urea from accelerated tissue protein breakdown. While the protein recommended by the committee (100–120 g) will add to the need for water, the high level of carbohydrate in the ration (450 g) should compensate for some of this need through improved protein utilization and limitation of renal excretion of sodium and its anions. Thus, the recommended carbohydrate in the ration constitutes an advantage in this regard.
While the committee did not provide specific recommendations for water, adequate amounts of water must be consumed with this ration to maintain and optimize physiological function and performance. Considering the expected level of stress and sweat volumes and the nature of the ration, water in excess of the 4–5 L/day must be available to ensure optimal performance in combat missions in which energy expenditure is high or carried out in hot and humid environments.
REFERENCES
Achten J, Halson SL, Moseley L, Rayson MP, Casey A, Jeukendrup AE. 2004. Higher dietary carbohydrate content during intensified running training results in better maintenance of performance and mood state. J Appl Physiol 96(4):1331–1340.
ACSM/ADA/DA (American College of Sports Medicine/American Dietetic Association/Dietitians of Canada). 2000. Joint postition statement. Nutrition and athletic performance. Med Sci Sports Exerc 32(12):2130–2145.
Afolabi PR, Jahoor F, Gibson NR, Jackson AA. 2004. Response of hepatic proteins to the lowering of habitual dietary protein to the recommended safe level of intake. Am J Physiol Endocrinol Metab 287(2):E327–E330.
Aguilo A, Tauler P, Fuentespina E, Villa G, Cordova A, Tur JA, Pons A. 2004. Antioxidant diet supplementation influences blood iron status in endurance athletes. Int J Sport Nutr Exerc Metab 14(2):147–160.
Ahlborg B, Bergstrom J, Ekelund LG, Hultman E. 1967. Muscle glycogen and muscle electrolytes during prolonged physical exercise. Acta Physiol Scand 70(2):129–142.
Al-Gurairi FT, Al-Waiz M, Sharquie KE. 2002. Oral zinc sulphate in the treatment of recalcitrant viral warts: Randomized placebo-controlled clinical trial. Br J Dermatol 146(3):423–431.
Allan JR, Wilson CG. 1971. Influence of acclimatization on sweat sodium concentration. J Appl Physiol 30(5):708–712.
Allen LH, Ahluwalia N. 1997. Improving Iron Status through Diet. The Application of Knowledge Concerning Dietary Iron Bioavailability in Human Populations. OMNI Technical Papers, No. 8. Arlington, VA: John Snow International.
Allsopp AJ, Sutherland R, Wood P, Wootton SA. 1998. The effect of sodium balance on sweat sodium secretion and plasma aldosterone concentration. Eur J Appl Physiol 78(6):516–521.
Anderson RA, Bryden NA, Polansky MM. 1992. Dietary chromium intake. Freely chosen diets, institutional diet, and individual foods. Biol Trace Elem Res 32:117–121.
Anonymous. 1991. Foods, nutrition, and sports performance. Final consensus statement. J Sports Sci 9:iii.
Anthony JC, Anthony TG, Layman DK. 1999. Leucine supplementation enhances skeletal muscle recovery in rats following exercise. J Nutr 129(6):1102–1106.
Anthony JC, Anthony TG, Kimball SR, Vary TC, Jefferson LS. 2000. Orally administered leucine stimulates protein synthesis in skeletal muscle of postabsorptive rats in association with increased eIF4F formation. J Nutr 130(2):139–145.
Armstrong LE. 2002. Caffeine, body fluid-electrolyte balance, and exercise performance. Int J Sport Nutr Exerc Metab 12(2):189–206.
Armstrong LE, Hubbard RW, Szlyk PC, Matthew WT, Sils IV. 1985. Voluntary dehydration and electrolyte losses during prolonged exercise in the heat. Aviat Space Environ Med 56(8):765–770.
Armstrong LE, Szlyk PC, De Luca JP, Sils IV, Hubbard RW. 1992. Fluid-electrolyte losses in uniforms during prolonged exercise at 30 degrees C. Aviat Space Environ Med 63(5):351–355.
Arnett T. 2003. Regulation of bone cell function by acid-base balance. Proc Nutr Soc 62(2):511–520.
Arthur JR, Nicol F, Beckett GJ. 1993. Selenium deficiency, thyroid hormone metabolism, and thyroid hormone deiodinases. Am J Clin Nutr 57(2 Suppl):236S–239S.
Askew EW, Claybaugh GM, Hashiro GM, Stokes WS, Sato A, Cucinell SA. 1987. Mauna Kea III: Metabolic Effects of Dietary Carbohydrate Supplementation During Exercise at 4,100 m Altitude. Technical Report No. T12-87. Fort Detrick, MD: US Army Medical Research and Development Command.
August D, Janghorbani M, Young VR. 1989. Determination of zinc and copper absorption at three dietary Zn-Cu ratios by using stable isotope methods in young adult and elderly subjects. Am J Clin Nutr 50(6):1457–1463.
Aurengo A, Leenhardt L, Aurengo H. 2002. Adaptation of thyroid function to excess iodine. Presse Med 31(35):1658–1663.
Ayre KJ, Hulbert AJ. 1996. Effects of changes in dietary fatty acids on isolated skeletal muscle functions in rats. J Appl Physiol 80(2):464–471.
Baker EM, Saari JC, Tolbert BM. 1966. Ascorbic acid metabolism in man. Am J Clin Nutr 19(6):371–378.
Barber MD, Ross JA, Preston T, Shenkin A, Fearon KC. 1999. Fish oil-enriched nutritional supplement attenuates progression of the acute-phase response in weight-losing patients with advanced pancreatic cancer. J Nutr 129(6):1120–1125.
Bashir Y, Sneddon JF, Staunton HA, Haywood GA, Simpson IA, McKenna WJ, Camm AJ. 1993. Effects of long-term oral magnesium chloride replacement in congestive heart failure secondary to coronary artery disease. Am J Cardiol 72(15):1156–1162.
Batchelder EL, Ebbs JC. 1943. Some observations of dark adaptation in mand and their bearing on the problem of human requirement for vitamin A. Rhode Island Agricultural Experiment Station Bulletin. No. 645:295–302.
Bausch J, Rietz P. 1977. Method for the assessment of vitamin A liver stores. Acta Vitaminol Enzymol 31(1–5):99–112.
Beale RJ, Bryg DJ, Bihari DJ. 1999. Immunonutrition in the critically ill: A systematic review of clinical outcome. Crit Care Med 27(12):2799–2805.
Beard J, Tobin B. 2000. Iron status and exercise. Am J Clin Nutr 72(2 Suppl):594S–597S.
Beauchamp GK, Bertino M, Engelman K. 1991. Human salt appetite. In: Friedman ME, Tordoff MG, Kare MR, eds. Chemical Senses. Vol. 4. New York: Marcel Dekker. Pp. 85–107.
Belko AZ, Meredith MP, Kalkwarf HJ, Obarzanek E, Weinberg S, Roach R, McKeon G, Roe DA. 1985. Effects of exercise on riboflavin requirements: Biological validation in weight reducing women. Am J Clin Nutr 41(2):270–277.
Bergstrom J, Hermansen L, Hultman E, Saltin B. 1967. Diet, muscle glycogen and physical performance. Acta Physiol Scand 71(2):140–150.
Bhaskaram P. 2002. Micronutrient malnutrition, infection, and immunity: An overview. Nutr Rev 60(5 Pt 2):S40–S45.
Bianco AC, Salvatore D, Gereben B, Berry MJ, Larsen PR. 2002. Biochemistry, cellular and molecular biology, and physiological roles of the iodothyronine selenodeiodinases. Endocr Rev 23(1):38–89.
Bistrian BR, Babineau T. 1998. Optimal protein intake in critical illness? Crit Care Med 26(9):1476–1477.
Blanchard EL, Harper HA. 1940. Measurement of vitamin A status of young adults by the dark adaptation technic. Arch Int Med 66:661–669.
Bogden JD. 2004. Influence of zinc on immunity in the elderly. J Nutr Health Aging 8(1):48–54.
Bogden JD, Oleske JM, Lavenhar MA, Munves EM, Kemp FW, Bruening KS, Holding KJ, Denny TN, Guarino MA, Holland BK. 1990. Effects of one year of supplementation with zinc and other micronutrients on cellular immunity in the elderly. J Am Coll Nutr 9(3):214–225.
Bogden JD, Oleske JM, Lavenhar MA, Munves EM, Kemp FW, Bruening KS, Holding KJ, Denny TN, Guarino MA, Krieger LM. 1988. Zinc and immunocompetence in elderly people: Effects of zinc supplementation for 3 months. Am J Clin Nutr 48(3):655–663.
Booth CK, Coad RA, Forbes-Ewan CH, Thomson GF, Niro PJ. 2003. The physiological and psychological effects of combat ration feeding during a 12-day training exercise in the tropics. Mil Med 168(1):63–70.
Booth SL, Golly I, Sacheck JM, Roubenoff R, Dallal GE, Hamada K, Blumberg JB. 2004. Effect of vitamin E supplementation on vitamin K status in adults with normal coagulation status. Am J Clin Nutr 80(1):143–148.
Borghi L, Meschi T, Amato F, Briganti A, Novarini A, Giannini A. 1996. Urinary volume, water and recurrences in idiopathic calcium nephrolithiasis: A 5-year randomized prospective study. J Urol 155(3):839–843.
Borghi L, Schianchi T, Meschi T, Guerra A, Allegri F, Maggiore U, Novarini A. 2002. Comparison of two diets for the prevention of recurrent stones in idiopathic hypercalciuria. N Engl J Med 346(2):77–84.
Born P, Zech J, Stark M, Classen M, Lorenz R. 1994. Carbohydrate substitutes: Comparative study of intestinal absorption of fructose, sorbitol and xylitol. Med Klin (Munich) 89(11):575–578.
Borsheim E, Tipton KD, Wolf SE, Wolfe RR. 2002. Essential amino acids and muscle protein recovery from resistance exercise. Am J Physiol Endocrinol Metabol 283(4):E648–E657.
Bremner I. 1998. Manifestations of copper excess. Am J Clin Nutr 67(5 Suppl):1069S–1073S.
Brilla LR, Gunter KB. 1995. Effect of magnesium supplementation on exercise time to exhaustion. Med Exerc Nutr Health 4:230–233.
Brilla LR, Haley TF. 1992. Effect of magnesium supplementation on strength training in humans. J Am Coll Nutr 11(3):326–329.
Broome CS, McArdle F, Kyle JAM, Andrews F, Lowe NM, Hart CA, Arthur JR, Jackson MJ. 2004. An increase in selenium intake improves immune function and poliovirus handling in adults with marginal selenium status. Am J Clin Nutr 80(1):154–162.
Brown GD, Gordon S. 2003. Fungal beta-glucans and mammalian immunity. Immunity 19(3):311–315.
Brownlie T 4th, Utermohlen V, Hinton PS, Giordano C, Haas JD. 2002. Marginal iron deficiency without anemia impairs aerobic adaptation among previously untrained women. Am J Clin Nutr 75(4):734–742.
Brownlie T 4th, Utermohlen V, Hinton PS, Haas JD. 2004. Tissue iron deficiency without anemia impairs adaptation in endurance capacity after aerobic training in previously untrained women. Am J Clin Nutr 79(3):437–443.
Brune M, Magnusson B, Persson H, Hallberg L. 1986. Iron losses in sweat. Am J Clin Nutr 43(3):438–443.
Brune M, Rossander-Hulten L, Hallberg L, Gleerup A, Sandberg AS. 1992. Iron absorption from bread in humans: Inhibiting effects of cereal fiber, phytate and inositol phosphates with different numbers of phosphate groups. J Nutr 122(3):442–449.
Bruner AB, Joffe A, Duggan AK, Casella JF, Brandt J. 1996. Randomised study of cognitive effects of iron supplementation in non-anaemic iron-deficient adolescent girls. Lancet 348(9033):992–996.
Bruno RS, Ramakrishnan R, Montine TJ, Bray TM, Traber MG. 2005. α-Tocopherol disappearance is faster in cigarette smokers and is inversely related to their ascorbic acid status. Am J Clin Nutr 81(1):95–103.
Brutsaert TD, Hernandez-Cordero S, Rivera J, Viola T, Hughes G, Haas JD. 2003. Iron supplementation improves progressive fatigue resistance during dynamic knee extensor exercise in iron-depleted, nonanemic women. Am J Clin Nutr 77(2):441–448.
Buchman AL, Keen C, Commisso J, Killip D, Ou CN, Rognerud CL, Dennis K, Dunn JK. 1998. The effect of a marathon run on plasma and urine mineral and metal concentrations. J Am Coll Nutr 17(2):124–127.
Bullen DB, O’Toole ML, Johnson KC. 1999. Calcium losses resulting from an acute bout of moderate-intensity exercise. Int J Sport Nutr 9(3):275–284.
Burke LM, Hawley JA. 2002. Effects of short-term fat adaptation on metabolism and performance of prolonged exercise. Med Sci Sports Exerc 34(9):1492–1498.
Burke LM, Kiens B, Ivy JL. 2004. Carbohydrates and fat for training and recovery. J Sports Sci 22(1):15–30.
Bushe CJ. 1986. Profound hypophosphataemia in patients collapsing after a “fun run”. Br Med J 292(6524):898–899.
Butterfield GE, Calloway DH. 1984. Physical activity improves protein utilization in young men. Br J Nutr 51(2):171–184.
Calvaresi E, Bryan J. 2001. B vitamins, cognition, and aging: A review. J Gerontol B Psychol Sci Soc Sci 56(6):P327–P339.
Calvo MS, Whiting SJ. 2003. Prevalence of vitamin D insufficiency in Canada and the United States: Importance to health status and efficacy of current food fortification and dietary supplement use. Nutr Rev 61(3):107–113.
Cannon JG, Meydani SN, Fielding RA, Fiatarone MA, Meydani M, Farhangmehr M, Orencole SF, Blumberg JB, Evans WJ. 1991. Acute phase response in exercise. II. Associations between vitamin E, cytokines, and muscle proteolysis. Am J Physiol 260(6 Pt 2):R1235–R1240.
Cannon JG, Orencole SF, Fielding RA, Meydani M, Meydani SN, Fiatarone MA, Blumberg JB, Evans WJ. 1990. Acute phase response in exercise: Interaction of age and vitamin E on neutrophils and muscle enzyme release. Am J Physiol 259(6 Pt 2):R1214–R1219.
Chandra RK. 1984. Excessive intake of zinc impairs immune responses. J Am Med Assoc 252(11):1443–1446.
Childs A, Jacobs C, Kaminski T, Halliwell B, Leeuwenburgh C. 2001. Supplementation with vitamin C and N-acetyl-cysteine increases oxidative stress in humans after an acute muscle injury induced by eccentric exercise. Free Radic Biol Med 31(6):745–753.
Clarkson PM. 1997. Effects of exercise on chromium levels. Is supplementation required? Sports Med 23(6):341–349.
Clarkson PM, Haymes EM. 1995. Exercise and mineral status of athletes: Calcium, magnesium, phosphorus, and iron. Med Sci Sports Exerc 27(6):831–843.
Clarkson PM, Rawson ES. 1999. Nutritional supplements to increase muscle mass. Crit Rev Food Sci Nutr 39(4):317–328.
Clarkson PM, Thompson HS. 2000. Antioxidants: What role do they play in physical activity and health? Am J Clin Nutr 72(2 Suppl):637S–646S.
Clavel S, Farout L, Briand M, Briand Y, Jouanel P. 2002. Effect of endurance training and/or fish oil supplemented diet on cytoplasmic fatty acid binding protein in rat skeletal muscles and heart. Eur J Appl Physiol 87(3):193–201.
Cohn JR, Emmett EA. 1978. The excretion of trace metals in human sweat. Ann Clin Lab Sci 8(4):270–275.
Collardeau M, Brisswalter J, Vercruyssen F, Audiffren M, Goubault C. 2001. Single and choice reaction time during prolonged exercise in trained subjects: Influence of carbohydrate availability. Eur J Appl Physiol 86(2):150–156.
Conn JW. 1949. The mechanism of acclimatization to heat. Adv Int Med 3:373–393.
Consolazio CF, Matoush LO, Nelson RA, Harding RS, Canham JE. 1963. Excretion of sodium, potassium, magnesium and iron in human sweat and the relation of each to balance and requirements. J Nutr 79:407–415.
Consolazio CF, Matoush LO, Nelson RA, Isaac GJ, Canham JE. 1966. Comparisons of nitrogen, calcium and iodine excretion in arm and total body sweat. Am J Clin Nutr 18(6):443–448.
Consolazio CF, Nelson RA, Matoush LO, Hughes RC, Urone P. 1964. The Trace Mineral Losses in Sweat. Report No. 284. Denver, CO: US Army Medical Research and Nutrition Laboratory.
Convertino VA, Armstrong LE, Coyle EF, Mack GW, Sawka MN, Senay LC, Sherman WM. 1996. American College of Sports Medicine Position Stand on exercise and fluid replacement. Med Sci Sports Exerc 28(1):i–vii.
Cook JD, Dassenko SA, Lynch SR. 1991. Assessment of the role of nonheme-iron availability in iron balance. Am J Clin Nutr 54(4):717–722.
Cook JD, Lipschitz DA, Miles LE, Finch CA. 1974. Serum ferritin as a measure of iron stores in normal subjects. Am J Clin Nutr 27(7):681–687.
Cook JD, Reddy MB, Burri J, Juillerat MA, Hurrell RF. 1997. The influence of different cereal grains on iron absorption from infant cereal foods. Am J Clin Nutr 65(4):964–969.
Cooling J, Blundell JE. 2001. High-fat and low-fat phenotypes: Habitual eating of high- and low-fat foods not related to taste preference for fat. Eur J Clin Nutr 55(11):1016–1021.
Costello RB, Chrousos GP. 2004 (August 10). Other Bioactive Food Components and Dietary Supplements. Paper presented at the Institute of Medicine Workshop on Optimization of Nutrient Composition of Military Rations for Short-Term, High-Stress Situations, Natick, MA. Institute of Medicine Committee on Optimization of Nutrient Composition of Military Rations for Short-Term, High-Stress Situations.
Costill DL, Miller JM. 1980. Nutrition for endurance sport: Carbohydrate and fluid balance. Int J Sports Med 1(1):2–14.
Costill DL, Branam G, Fink W, Nelson R. 1976a. Exercise induced sodium conservation: Changes in plasma renin and aldosterone. Med Sci Sports 8(4):209–213.
Costill DL, Cote R, Fink W. 1976b. Muscle water and electrolytes following varied levels of dehydration in man. J Appl Physiol 40(1):6–11.
Costill DL, Flynn MG, Kirwan JP, Houmard JA, Mitchell JB, Thomas R, Park SH. 1988. Effects of repeated days of intensified training on muscle glycogen and swimming performance. Med Sci Sports Exerc 20(3):249–254.
Coyle EF. 2004 (August 9). Carbohydrate Ingestion Prior To and During Intense Activity. Paper presented at the Institute of Medicine Workshop on Optimization of Nutrient Composition of Military Rations for Short-Term, High-Stress Situations, Natick, MA. Institute of Medicine Committee on Optimization of Nutrient Composition of Military Rations for Short-Term, High-Stress Situations.
Coyle EF, Montain SJ. 1992. Benefits of fluid replacement with carbohydrate during exercise. Med Sci Sports Exerc 24(9 Suppl):S324–S330.
Coyle EF, Coggan AR, Hemmert MK, Ivy JL. 1986. Muscle glycogen utilization during prolonged strenuous exercise when fed carbohydrate. J Appl Physiol 61(1):165–172.
Curhan GC, Willett WC, Rimm EB, Stampfer MJ. 1993. A prospective study of dietary calcium and other nutrients and the risk of symptomatic kidney stones. N Engl J Med 328(12):833–838.
Dale G, Fleetwood JA, Inkster JS, Sainsbury JR. 1986. Profound hypophosphataemia in patients collapsing after a “fun run”. Br Med J (Clin Res Ed) 292(6518):447–448.
Dangin M, Guillet C, Garcia-Rodenas C, Gachon P, Bouteloup-Demange C, Reiffers-Magnani K, Fauquant J, Ballevre O, Beaufrere B. 2003. The rate of protein digestion affects protein gain differently during aging in humans. J Physiol 549(Pt 2):635–644.
Davies KM, Heaney RP, Recker RR, Lappe JM, Barger-Lux MJ, Rafferty K, Hinders S. 2000. Calcium intake and body weight. J Clin Endocrinol Metab 85(12):4635–4638.
Dawson B, Henry GJ, Goodman C, Gillam I, Beilby JR, Ching S, Fabian V, Dasig D, Morling P, Kakulus BA. 2002. Effect of Vitamin C and E supplementation on biochemical and ultra-structural indices of muscle damage after a 21 km run. Int J Sports Med 23(1):10–15.
Dawson-Hughes B, Fowler SE, Dalsky G, Gallagher C. 1996. Sodium excretion influences calcium homeostasis in elderly men and women. J Nutr 126(9):2107–2112.
Dawson-Hughes B, Harris SS, Rasmussen H, Song L, Dallal GE. 2004. Effect of dietary protein supplements on calcium excretion in healthy older men and women. J Clin Endocrinol Metab 89(3):1169–1173.
de O G Mendonca C, Martini LA, Baxmann AC, Nishiura JL, Cuppari L, Sigulem DM, Heilberg IP. 2003. Effects of an oxalate load on urinary oxalate excretion in calcium stone formers. J Ren Nutr 13(1):39–46.
Delorme O, Bourdin H, Viel JF, Rigaud ML, Kantelip JP. 1992. Spectral analysis of electroencephalography data in athletes with low erythrocyte magnesium. Magnes Res 5(4):261–264.
Deluca HF, Cantorna MT. 2001. Vitamin D: Its role and uses in immunology. FASEB J 15(14):2579–2585.
DeRuisseau KC, Cheuvront SN, Haymes EM, Sharp RG. 2002. Sweat iron and zinc losses during prolonged exercise. Int J Sport Nutr Exerc Metab 12(4):428–437.
Devine A, Criddle RA, Dick IM, Kerr DA, Prince RL. 1995. A longitudinal study of the effect of sodium and calcium intakes on regional bone density in postmenopausal women. Am J Clin Nutr 62(4):740–745.
Dill DB, Soholt LF, Oddershede IB. 1976. Physiological adjustments of young mean to five-hour desert walks. J Appl Physiol 40(2):236–242.
Disler PB, Lynch SR, Charlton RW, Torrance JD, Bothwell TH, Walker RB, Mayet F. 1975. The effect of tea on iron absorption. Gut 16(3):193–200.
Doherty M, Smith P, Hughes M, Davison R. 2004. Caffeine lowers perceptual response and increases power output during high-intensity cycling. J Sports Sci 22(7):637–643.
Drewnowski A. 1997. Taste preferences and food intake. Annu Rev Nutr 17:237–253.
Dye L, Blundell J. 2002. Functional foods: Psychological and behavioral functions. Br J Nutr 88(Suppl 2):S187–S211.
Dye L, Lluch A, Blundell JE. 2000. Macronutrients and mental performance. Nutrition 16(10):1021–1034.
Eby GA, Davis DR, Halcomb WW. 1984. Reduction in duration of common colds by zinc gluconate lozenges in a double-blind study. Antimicrob Agents Chemother 25(1):20–24.
Ettinger B, Pak CY, Citron JT, Thomas C, Adams-Huet B, Vangessel A. 1997. Potassium-magnesium citrate is an effective prophylaxis against recurrent calcium oxalate nephrolithiasis. J Urol 158(6):2069–2073.
Evans WJ. 2000. Vitamin E, vitamin C, and exercise. Am J Clin Nutr 72(2 Suppl):647S-652S.
FAO/WHO (Food and Agriculture Organization/World Health Organization). 1988. Requirements of Vitamin A, Iron, Folate, and Vitamin B12. FAO Food Nutrition Series No. 23. Rome: FAO. Pp. 33–50.
FAO/WHO/UNU (Food and Agriculture Organization/World Health Organization/United Nations University). 1985. Energy and Protein Requirements. Technical Report Series 724. Geneva: World Health Organization.
Farr BM, Conner EM, Betts RF, Oleske J, Minnefor A, Gwaltney JM Jr. 1987. Two randomized controlled trials of zinc gluconate lozenge therapy of experimentally induced rhinovirus colds. Antimicrob Agents Chemother 31(8):1183–1187.
Fearon KC, Von Meyenfeldt MF, Moses AG, Van Geenen R, Roy A, Gouma DJ, Giacosa A, Van Gossum A, Bauer J, Barber MD, Aaronson NK, Voss AC, Tisdale MJ. 2003. Effect of a protein and energy dense N-3 fatty acid enriched oral supplement on loss of weight and lean tissue in cancer cachexia: A randomised double blind trial. Gut 52(10):1479–1486.
Febbraio MA. 2001. Alterations in energy metabolism during exercise and heat stress. Sports Med 31(1):47–59.
Febbraio MA, Murton P, Selig SE, Clark SA, Lambert DL, Angus DJ, Carey MF. 1996. Effect of CHO ingestion on exercise metabolism and performance in different ambient temperatures. Med Sci Sports Exerc 28(11):1380–1387.
Fielding RA, Parkington J. 2002. What are the dietary protein requirements of physically active individuals? New evidence on the effects of exercise on protein utilization during post-exercise recovery. Nutr Clin Care 5(4):191–196.
Fink WJ, Costill DL, Van Handel PJ. 1975. Leg muscle metabolism during exercise in the heat and cold. Eur J Appl Physiol Occup Physiol 34(3):183–190.
Fischer K, Colombani PC, Langhans W, Wenk C. 2002. Carbohydrate to protein ratio in food and cognitive performance in the morning. Physiol Behav 75(3):411–423.
Frank J, Sundberg B, Kamal-Eldin A, Vessby B, Aman P. 2004. Yeast-leavened oat breads with high or low molecular weight beta-glucan do not differ in their effects on blood concentrations of lipids, insulin, or glucose in humans. J Nutr 134(6):1384–1388.
Frassetto LA, Todd KM, Morris RC Jr, Sebastian A. 1998. Estimation of net endogenous noncarbonic acid production in humans from diet potassium and protein contents. Am J Clin Nutr 68(3):576–583.
Friedl KE. 1997. Variability of fat and lean tissue loss during physical exertion with energy deficit. In: Kinney JM, Tucker HN, eds. Physiology, Stress, and Malnutrition: Functional Correlates, Nutritional Intervention. Philadelphia: Lippincott-Raven. Pp. 431–450.
Friedl KE, Hoyt RW. 1997. Development and biomedical testing of military operational rations. Annu Rev Nutr 17:51–75.
Fritzsche RG, Switzer TW, Hodgkinson BJ, Lee SH, Martin JC, Coyle EF. 2000. Water and carbohydrate ingestion during prolonged exercise increase maximal neuromuscular power. J Appl Physiol 88(2):730–737.
Gamble JL. 1947. Physiological information gained from studies on the life raft ration. In: The Harvey Society of New York, eds. The Harvey Lectures. Lancaster, PA: The Sciences Press Printing Co. Pp. 247–273.
Garfinkel L, Garfinkel D. 1985. Magnesium regulation of the glycolytic pathway and the enzymes involved. Magnesium 4(2–3):60–72.
Garland ML, Hagmeyer KO. 1998. The role of zinc lozenges in treatment of the common cold. Ann Pharmacother 32(1):63–69.
Gerstein DE, Woodward-Lopez G, Evans AE, Kelsey K, Drewnowski A. 2004. Clarifying concepts about macronutrients’ effects on satiation and satiety. J Am Diet Assoc 104(7):1151–1153.
Giannini S, Nobile M, Sartori L, Dalle Carbonare L, Ciuffreda M, Corro P, D’Angelo A, Calo L, Crepaldi G. 1999. Acute effects of moderate dietary protein restriction in patients with idiopathic hypercalciuria and calcium nephrolithiasis. Am J Clin Nutr 69(2):267–271.
Gibson NR, Jahoor F, Ware L, Jackson AA. 2002. Endogenous glycine and tyrosine production is maintained in adults consuming a marginal-protein diet. Am J Clin Nutr 75(3):511–518.
Gillingham RL, Keefe AA, Tikuisis P. 2004. Acute caffeine intake before and after fatiguing exercise improves target shooting engagement time. Aviat Space Environ Med 75(10):865–871.
Glanz K, Basil M, Maibach E, Goldberg J, Snyder D. 1998. Why Americans eat what they do: Taste, nutrition, cost, convenience, and weight control concerns as influences on food consumption. J Am Diet Assoc 98(10):1118–1126.
Gleeson M, Nieman DC, Pedersen BK. 2004. Exercise, nutrition and immune function. J Sports Sci 22(1):115–125.
Golf SW, Bohmer D, Nowacki PE. 1993. Is magnesium a limiting factor in competitive exercise? A summary of relevant scientific data. In: Golf S, Dralle D, Vecchiet L, eds. Magnesium 1993. London: John Libbey & Co. Pp. 209–219.
Gordon CM, DePeter KC, Feldman HA, Grace E, Emans SJ. 2004. Prevalence of vitamin D deficiency among healthy adolescents. Arch Pediatr Adolesc Med 158(6):531–537.
Goulding A, Lim PE. 1983. Effects of varying dietary salt intake on the fasting urinary excretion of sodium, calcium and hydroxyproline in young women. N Z Med J 96:853–854.
Graat JM, Schouten EG, Kok FJ. 2002. Effect of daily vitamin E and multivitamin-mineral supplementation on acute respiratory tract infections in elderly persons: A randomized controlled trial. J Am Med Assoc 288(6):715–721.
Green R, Charlton R, Seftel H, Bothwell T, Mayet F, Adams B, Finch C, Layrisse M. 1968. Body iron excretion in man. A collaborative study. Am J Med 45:336–353.
Griffin MD, Xing N, Kumar R. 2003. Vitamin D and its analogs as regulators of immune activation and antigen presentation. Annu Rev Nutr 23:117–145.
Grimm M, Muller A, Hein G, Funfstuck R, Jahreis G. 2001. High phosphorus intake only slightly affects serum minerals, urinary pyridinium crosslinks and renal function in young women. Eur J Clin Nutr 55(3):153–161.
Hallberg L, Rossander-Hulten L. 1991. Iron requirements in menstruating women. Am J Clin Nutr 54(6):1047–1058.
Hallberg L, Brune M, Erlandsson M, Sandberg AS, Rossander-Hulten L. 1991. Calcium: Effect of different amounts on nonheme- and heme-iron absorption in humans. Am J Clin Nutr 53(1):112–119.
Hansen CM, Shultz TD, Kwak HK, Memon HS, Leklem JE. 2001. Assessment of vitamin B-6 status in young women consuming a controlled diet containing four levels of vitamin B-6 provides an estimated average requirement and recommended dietary allowance. J Nutr 131(6):1777–1786.
Haskell MJ, Handelman GJ, Peerson JM, Jones AD, Rabbi MA, Awal MA, Wahed MA, Mahalanabis D, Brown KH. 1997. Assessment of vitamin A status by the deuterated-retinol-dilution technique and comparison with hepatic vitamin A concentration in Bangladeshi surgical patients. Am J Clin Nutr 66(1):67–74.
Hawley J. 2000. Nutritional strategies to enhance fat oxidation during aerobic exercise. In: Burke L, Deakin V, eds. Clinical Sports Nutrition. 2nd ed. Roseville, Australia: McGraw Hill Australia. Pp. 428–454.
Hawley JA, Schabort EJ, Noakes TD, Dennis SC. 1997. Carbohydrate-loading and exercise performance. An update. Sports Med 24(2):73–81.
Heaney RP, Recker RR. 1982. Effects of nitrogen, phosphorus, and caffeine on calcium balance in women. J Lab Clin Med 99(1):46–55.
Heaney RP, Davies KM, Chen TC, Holick MF, Barger-Lux MJ. 2003. Human serum 25-hydroxycholecalciferol response to extended oral dosing with cholecalciferol. Am J Clin Nutr 77(1):204–210.
Helge JW. 2000. Adaptation to a fat-rich diet. Effects on endurance performance in humans. Sports Med 30(5):347–357.
Helge JW. 2004 (August 9). Optimization of Macronutrient Composition for Carbohydrate and Fat Intake: What is the Optimal Balance. Paper presented at the Institute of Medicine Workshop on Optimization of Nutrient Composition of Military Rations for Short-Term, High-Stress Situations, Natick, MA. Institute of Medicine Committee on Optimization of Nutrient Composition of Military Rations for Short-Term, High-Stress Situations.
Helge JW, Lundby C, Christensen DL, Langfort J, Messonnier L, Zacho M, Andersen JL, Saltin B. 2003. Skiing across Greenland icecap: Divergent effects on limb muscle adaptations and substrate oxidation. J Exp Biol 206(Pt 6):1075–1083.
Hemila H. 1994. Does vitamin C alleviate the symptoms of the common cold? A review of current evidence. Scand J Infect Dis 26(1):1–6.
Hemila H. 1997. Vitamin C intake and susceptibility to the common cold. Br J Nutr 77(1):59–72.
Hemila H, Kaprio J, Albanes D, Heinonen OP, Virtamo J. 2002. Vitamin C, vitamin E, and beta-carotene in relation to common cold incidence in male smokers. Epidemiology 13(1):32–37.
Heyland DK, Novak F, Drover JW, Jain M, Su X, Suchner U. 2001. Should immunonutrition become routine in critically ill patients? A systematic review of the evidence. J Am Med Assoc 286(8):944–953.
Heys SD, Walker LG, Smith I, Eremin O. 1999. Enteral nutritional supplementation with key nutrients in patients with critical illness and cancer: A meta-analysis of randomized controlled clinical trials. Ann Surg 229(4):467–477.
Hinton PS, Giordano C, Brownlie T, Haas JD. 2000. Iron supplementation improves endurance after training in iron-depleted, nonanemic women. J Appl Physiol 88(3):1103–1111.
Hoffer LJ. 2004 (August 9). Optimum Protein Intake in Hypocaloric States. Paper presented at the Institute of Medicine Workshop on Optimization of Nutrient Composition of Military Rations for Short-Term, High-Stress Situations, Natick, MA. Institute of Medicine Committee on Optimization of Nutrient Composition of Military Rations for Short-Term, High-Stress Situations.
Hoffer LJ, Bistrian BR, Young VR, Blackburn GL, Matthews DE. 1984. Metabolic effects of very low calorie weight reduction diets. J Clin Invest 73(3):750–758.
Holick MF. 2004. Vitamin D: Importance in the prevention of cancers, type 1 diabetes, heart disease, and osteoporosis. Am J Clin Nutr 79(3):362–371.
Holmes RP. 2000. Oxalate synthesis in humans: Assumptions, problems, and unresolved issues. Mol Urol 4(4):329–332.
Holmes RP, Goodman HO, Assimos DG. 1995. Dietary oxalate and its intestinal absorption. Scanning Microsc 9(4):1109–1120.
Holmes RP, Goodman HO, Assimos DG. 2001. Contribution of dietary oxalate to urinary oxalate excretion. Kidney Int 59(1):270–276.
Holt SH, Delargy HJ, Lawton CL, Blundell JE. 1999. The effects of high-carbohydrate vs high-fat breakfasts on feelings of fullness and alertness, and subsequent food intake. Int J Food Sci Nutr 50(1):13–28.
Horn S, Feller ER. 2003. Gastrointestinal (GI) bleeding in endurance runners. AMAA J 16(1):5–6, 11.
Horvath PJ, Eagen CK, Ryer-Calvin SD, Pendergast DR. 2000. The effects of varying dietary fat on the nutrient intake in male and female runners. J Am Coll Nutr 19(1):42–51.
Huang YC, Chen W, Evans MA, Mitchell ME, Shultz TD. 1998. Vitamin B-6 requirement and status assessment of young women fed a high-protein diet with various levels of vitamin B-6. Am J Clin Nutr 67(2):208–220.
Hume EM, Krebs HA. 1949. Vitamin A Requirement of Human Adults. An Experimental Study of Vitamin A Deprivation in Man. Medical Research Council Special Report Series No. 264. London: His Majesty’s Stationaery Office.
Hurrell RF. 2002a. Fortification: Overcoming technical and practical barriers. J Nutr 132(4 Suppl):806S–812S.
Hurrell R. 2002b. How to ensure adequate iron absorption from iron-fortified food. Nutr Rev 60(7 Pt 2):S7–S15.
Inoue Y, Havenith G, Kenney WL, Loomis JL, Buskirk ER. 1999. Exercise- and methylcholine-induced sweating responses in older and younger men: Effect of heat acclimation and aerobic fitness. Int J Biometeorol 42(4):210–216.
IOM (Institute of Medicine). 1994. Food Components to Enhance Performance. Washington, DC: National Academy Press.
IOM. 1995. Not Eating Enough. Washington, DC: National Academy Press. Pp. 285–302.
IOM. 1997a. Dietary Reference Intakes. Calcium, Phosphorus, Magnesium, Vitamin D, and Fluoride. Washington, DC: National Academy Press.
IOM. 1997b. Vitamin C Fortification of Food Aid Commodities. Washington, DC: National Academy Press.
IOM. 1998. Dietary Reference Intakes. Thiamin, Riboflavin, Niacin, Vitamin B6, Folate, Vitamin B12, Pantothenic Acid, Biotin, and Choline. Washington, DC: National Academy Press.
IOM. 1999. Letter Report to the Office of the Surgeon General United States Army on Antioxidants and Oxidative Stress in Military Personnel. Washington, DC: Institute of Medicine.
IOM. 2000. Dietary Reference Intakes for Vitamin C, Vitamin E, Selenium, and Carotenoids. Washington, DC: National Academy Press.
IOM. 2001a. Caffeine for the Sustainment of Mental Task Performance. Formulations for Military Operations. Washington, DC: National Academy Press.
IOM. 2001b. Dietary Reference Intakes. Vitamin A, Vitamin K, Arsenic, Boron, Chromium, Copper, Iodine, Iron, Manganese, Molybdenum, Nickel, Silicon, Vanadium, and Zinc. Washington, DC: National Academy Press.
IOM. 2002a. Dietary Reference Intakes. Energy, Carbohydrate, Fiber, Fat, Fatty Acids, Cholesterol, Protein, and Amino Acids. Washington, DC: The National Academies Press.
IOM. 2002b. High-Energy, Nutrient-Dense Emergency Relief Food Product. Washington, DC: National Academy Press.
IOM. 2004. Dietary Reference Intakes. Water, Potassium, Sodium, Chloride, and Sulfate. Washington, DC: The National Academies Press.
Ireland P, Fordtran JS. 1973. Effect of dietary calcium and age on jejunal calcium absorption in humans studied by intestinal perfusion. J Clin Invest 52(11):2672–2681.
IZiNCG (International Zinc Nutritional Consulative Group). 2004. Assessment of the risk of zinc deficiency in populations and options for its control. Hotz C, Brown KH, eds. Food Nutr Bull 25(1 Suppl 1):S91–S204.
Jackson AA, Gibson NR, Lu Y, Jahoor F. 2004. Synthesis of erythrocyte glutathione in healthy adults consuming the safe amount of dietary protein. Am J Clin Nutr 80(1):101–107.
Jackson JL, Lesho E, Peterson C. 2000. Zinc and the common cold: A meta-analysis revisited. J Nutr 130(5S Suppl):1512S–1515S.
Jacob RA, Sandstead HH, Munoz JM, Klevay LM, Milne DB. 1981. Whole body surface loss of trace metals in normal males. Am J Clin Nutr 34(7):1379–1383.
Jacobs I, Anderberg A, Schele R, Lithell H. 1983. Muscle glycogen in soldiers on different diets during military field maneuvers. Aviat Space Environ Med 54(10):898–900.
Jacobsen R, Lorenzen JK, Toubro S, Krog-Mikkelsen I, Astrup A. 2005. Effect of short-term high dietary calcium intake on 24-h energy expenditure, fat oxidation, and fecal fat excretion. Int J Obes Relat Metab Disord 29(3):292–301.
Janigan DT, Perey B, Marrie TJ, Chiasson PM, Hirsch D. 1997. Skin necrosis: An unusual complication of hyperphosphatemia during total parenteral nutrition therapy. J Parenter Enteral Nutr 21(1):50–52.
Jones GR, Newhouse I. 1997. Sport-related hematuria: A review. Clin J Sport Med 7(2):119–125.
Kallner A, Hartmann D, Hornig D. 1979. Steady-state turnover and body pool of ascorbic acid in man. Am J Clin Nutr 32(3):530–539.
Kallner AB, Hartmann D, Hornig DH. 1981. On the requirements of ascorbic acid in man: Steady-state turnover and body pool in smokers. Am J Clin Nutr 34(7):1347–1355.
Kalmar JM, Cafarelli E. 2004. Caffeine: A valuable tool to study central fatigue in humans? Exerc Sport Sci Rev 32(4):143–147.
Kaplan RJ. 2004 (August 9). Macronutrient Composition of Military Rations for Cognitive Performance in Short-Term, High-Stress Situations. Paper presented at the Institute of Medicine Workshop on Optimization of Nutrient Composition of Military Rations for Short-Term, High-Stress Situations, Natick, MA. Institute of Medicine Committee on Optimization of Nutrient Composition of Military Rations for Short-Term, High-Stress Situations.
Karlsson J, Saltin B. 1971. Diet, muscle glycogen, and endurance performance. J Appl Physiol 31(2):203–206.
Keenan RA, Moldawer LL, Yang RD, Kawamura I, Blackburn GL, Bistrian BR. 1982. An altered response by peripheral leukocytes to synthesize or release leukocyte endogenous mediator in critically ill, protein-malnourished patients. J Lab Clin Med 100(6):844–857.
Kerstetter JE, O’Brien KO, Caseria DM, Wall DE, Insogna KL. 2005. The impact of dietary protein on calcium absorption and kinetic measures of bone turnover in women. J Clin Endocrinol Metab 90(1):26–31.
Keusch GT. 1999. Iron metabolism, microbial virulence, and host defenses. In: Institute of Medicine. Military Strategies for Sustainment of Nutrition and Immune Function in the Field. Washington, DC: The National Academy Press. Pp. 317–336.
Keys A, Brozek J, Henschel A, Mickelsen O, Taylor HL. 1950. The Biology of Human Starvation. Minneapolis, MN: The University of Minnesota Press. Vol. II.
King NA, Tremblay A, Blundell JE. 1997. Effects of exercise on appetite control: Implications for energy balance. Med Sci Sports Exerc 29(8):1076–1089.
Knochel JP. 1993. Potassium deficiency as the result of training in hot weather. In: Institute of Medicine. Fluid Replacement and Heat Stress. Washington, DC: National Academy Press. Pp. 117–126.
Konig D, Weinstock C, Keul J, Northoff H, Berg A. 1998. Zinc, iron, and magnesium status in athletes—influence on the regulation of exercise-induced stress and immune function. Exerc Immunol Rev 4:2–21.
Kordas K, Stoltzfus RJ. 2004. New evidence of iron and zinc interplay at the enterocyte and neural tissues. J Nutr 134(6):1295–1298.
Kurtz TW, Al-Bander HA, Morris RC Jr. 1987. “Salt-sensitive” essential hypertension in men. Is the sodium ion alone important? N Engl J Med 317(17):1043–1048.
Lawless HT, Rapacki F, Horne J, Hayes A. 2003. The taste of calcium and magnesium salts and anionic modifications. Food Qual Pref 14(4):319–325.
Layman DK, Boileau RA, Erickson DJ, Painter JE, Shiue H, Sather C, Christou DD. 2003. A reduced ratio of dietary carbohydrate to protein improves body composition and blood lipid profiles during weight loss in adult women. J Nutr 133(2):411–417.
Ledikwe JH, Blanck HM, Khan LK, Serdula MK, Seymour JD, Tohill BC, Rolls BJ. 2005. Dietary energy density determined by eight calculation methods in a nationally representative United States population. J Nutr 135(2):273–278.
Leklem JE. 1999. Vitamin B6. In: Shils ME, Olson JA, Shike M, Ross AC, eds. Modern Nutrition in Health and Disease. 9th ed. Baltimore, MD: Williams and Wilkins. Pp. 413–421.
Leshem M, Abutbul A, Eilon R. 1999. Exercise increases the preference for salt in humans. Appetite 32(2):251–260.
Levine M, Conry-Cantilena C, Wang Y, Welch RW, Washko PW, Dhariwal KR, Park JB, Lazarev A, Graumlich JF, King J, Cantilena LR. 1996. Vitamin C pharmacokinetics in healthy volunteers: Evidence for a recommended dietary allowance. Proc Natl Acad Sci USA 93(8):3704–3709.
Lieberman HR. 2003. Nutrition, brain function and cognitive performance. Appetite 40(3):245–254.
Lieberman HR, Falco CM, Slade SS. 2002. Carbohydrate administration during a day of sustained aerobic activity improves vigilance, as assessed by a novel ambulatory monitoring device, and mood. Am J Clin Nutr 76(1):120–127.
Linkswiler HM, Zemel MB, Hegsted M, Schuette S. 1981. Protein-induced hypercalciuria. Fed Proc 40(9):2429–2433.
Liu RH. 2004. Potential synergy of phytochemicals in cancer prevention: Mechanism of action. J Nutr 134(12 Suppl):3479S–3485S.
Lonnerdal B. 2000. Dietary factors influencing zinc absorption. J Nutr 130(5S Suppl):1378S–1383S.
Lorr M, McNair DM, Heuchert JW. 2003. Profile of Mood States (POMS). [Online]. Multi-Health Systems, Inc. Available: https://www.mhs.com/ecom/product.asp?Cou=USA&AppGrpID=BEM&RptGrpID=POM&SubAppGrpID=BHE&node= [accessed December 13, 2004].
Lowy SL, Fisler JS, Drenick EJ, Hunt IF, Swendseid ME. 1986. Zinc and copper nutriture in obese men receiving very low calorie diets of soy or collagen protein. Am J Clin Nutr 43(2):272–287.
Lu SC. 1998. Regulation of hepatic glutathione synthesis. Semin Liver Dis 18(4):331–343.
Luft FC, Rankin LI, Bloch R, Weyman AE, Willis LR, Murray RH, Grim CE, Weinberger MH. 1979. Cardiovascular and humoral responses to extremes of sodium intake in normal black and white men. Circulation 60(3):697–706.
Luiking YC, Poeze M, Ramsay G, Deutz NE. 2005. The role of arginine in infection and sepsis. J Parenter Enteral Nutr 29(1 Suppl):S70–S74.
Lukaski HC. 2001. Magnesium, zinc, and chromium nutrition and athletic performance. Can J Appl Physiol 26 (Suppl):S13–S22.
Lukaski HC. 2004. Vitamin and mineral status: Effects on physical performance. Nutrition 20(7–8):632–644.
Lukaski HC, Penland JG. 2004 (August 9). Zinc, Magnesium, Copper, Iron, Selenium, and Calcium in Assault Rations: Roles in Promotion of Physical and Mental Performance. Paper presented at the Institute of Medicine Workshop on Optimization of Nutrient Composition of Military Rations for Short-Term, High-Stress Situations, Natick, MA. Institute of Medicine Committee on Optimization of Nutrient Composition of Military Rations for Short-Term, High-Stress Situations.
Lukaski HC, Bolonchuk WW, Klevay LM, Milne DB, Sandstead HH. 2001. Interactions among dietary fat, mineral status, and performance of endurance athletes: A case study. Int J Sport Nutr Exerc Metab 11(2):186–198.
Magkos F, Kavouras SA. 2004. Caffeine and ephedrine: Physiological, metabolic and performance-enhancing effects. Sports Med 34(13):871–889.
Malhotra MS, Sridharan K, Venkataswamy Y, Rai RM, Pichan G, Radhakrishnan U, Grover SK. 1981. Effect of restricted potassium intake on its excretion and on physiological responses during heat stress. Eur J Appl Physiol 47(2):169–179.
Malouf M, Grimley EJ, Areosa SA. 2003. Folic acid with or without vitamin B12 for cognition and dementia. Cochrane Database Syst Rev (4):CD004514.
Manach C, Scalbert A, Morand C, Remesy C, Jimenez L. 2004. Polyphenols: Food sources and bioavailability. Am J Clin Nutr 79(5):727–747.
Manore MM. 2000. Effect of physical activity on thiamine, riboflavin, and vitamin B-6 Requirements. Am J Clin Nutr 72(2 Suppl):598S–606S.
Manore M, Thompson J. 2000. Sport Nutrition for Health and Performance. Champaign, IL: Human Kinetics.
Margen S, Chu JY, Kaufmann NA, Calloway DH. 1974. Studies in calcium metabolism. I. The calciuretic effect of dietary protein. Am J Clin Nutr 27(6):584–589.
Marsh E, Murlin JR. 1928. Muscular efficiency on high carbohydrate and high fat diets. J Nutr 1:105–137.
Massey LK, Whiting SJ. 1996. Dietary salt, urinary calcium, and bone loss. J Bone Miner Res 11(6):731–736.
Massey LK, Grentz LM, Horner HT, Palmer RG. 2002. Soybean and soyfood consumption increase oxalate excretion. Top Clin Nutr 17:49–59.
Mastaloudis A, Morrow JD, Hopkins DW, Devaraj S, Traber MG. 2004a. Antioxidant supplementation prevents exercise-induced lipid peroxidation, but not inflammation, in ultramarathon runners. Free Rad Biol Med 36(10):1329-1341.
Mastaloudis A, Yu TW, O’Donnell RP, Frei B, Dashwood RH, Traber MG. 2004b. Endurance exercise results in DNA damage as detected by the comet assay. Free Rad Biol Med 36(8):966–975.
Mattes RD. 2004 (August 11). Food Intake Regulation: Liquid versus Solid. Paper presented at the Institute of Medicine Workshop on Optimization of Nutrient Composition of Military Rations for Short-Term, High-Stress Situations, Natick, MA. Institute of Medicine Committee on Optimization of Nutrient Composition of Military Rations for Short-Term, High-Stress Situations.
Maughan RJ, Griffin J. 2003. Caffeine ingestion and fluid balance: A review. J Hum Nutr Dietetics 16(6):411–420.
Maughan RJ, Shirreffs SM. 1997. Recovery from prolonged exercise: Restoration of water and electrolyte balance. J Sports Sci 15(3):297–303.
McCormick DB. 1999. Riboflavin. In: Shils ME, Olson JA, Shike M, Ross AC, eds. Modern Nutrition in Health and Disease. 9th ed. Baltimore, MD: Williams and Wilkins. Pp. 391–399.
McDonald R, Keen CL. 1988. Iron, zinc and magnesium nutrition and athletic performance. Sports Med 5(3):171–184.
McLellan TM, Bell DG, Kamimori GH. 2004. Caffeine improves physical performance during 24 h of active wakefulness. Aviat Space Environ Med 75(8):666–672.
Mela DJ, Sacchetti DA. 1991. Sensory preferences for fats: Relationships with diet and body composition. Am J Clin Nutr 53(4):908–915.
Melanson EL, Sharp TA, Schneider J, Donahoo WT, Grunwald GK, Hill JO. 2003. Relation between calcium intake and fat oxidation in adult humans. Int J Obes Relat Metab Disord 27(2):196–203.
Mertz W. 1969. Chromium occurrence and function in biological systems. Physiol Rev 49(2):163–239.
Mertz W. 1993. Chromium in human nutrition: A review. J Nutr 123(4):626–633.
Mertz W, Roginski EE, Schwarz K. 1961. Effect of trivalent chromium complexes on glucose uptake by epididymal fat tissue of rats. J Biol Chem 236(2):318–322.
Meydani SN, Leka LS, Fine BC, Dallal GE, Keusch GT, Singh MF, Hamer DH. 2004. Vitamin E and respiratory tract infections in elderly nursing home residents: A randomized controlled trial. J Am Med Assoc 292(7):828–836.
Meydani SN, Meydani M, Blumberg JB, Leka LS, Pedrosa M, Diamond R, Schaefer EJ. 1998. Assessment of the safety of supplementation with different amounts of vitamin E in healthy older adults. Am J Clin Nutr 68(2):311–318.
Meydani SN, Meydani M, Blumberg JB, Leka LS, Siber G, Loszewski R, Thompson C, Pedrosa MC, Diamond RD, Stollar BD. 1997. Vitamin E supplementation and in vivo immune response in healthy elderly subjects. A randomized controlled trial. J Am Med Assoc 277(17):1380–1386.
Miller ER 3rd, Pastor-Barriuso R, Dalal D, Riemersma RA, Appel LJ, Guallar E. 2005. Metaanalysis: High-dosage vitamin E supplementation may increase all-cause mortality. Ann Intern Med 142(1):37–46.
Miyamura JB, McNutt SW, Lichton IJ, Wenkam NS. 1987. Altered zinc status of soldiers under field conditions. J Am Diet Assoc 87(5):595–597.
Moldawer LL, Trerice MS, Flatt JP, Bistrian BR, Blackburn GL. 1978. A protein sparing model in the rat during hypocaloric feeding: Factors determining preservation of visceral protein function. J Surg Res 25(5):424–432.
Montain SJ. 2004 (August 9). Physiological Demands of Combat Operations. Paper presented at the Institute of Medicine Workshop on Optimization of Nutrient Composition of Military Rations for Short-Term, High-Stress Situations, Natick, MA. Institute of Medicine Committee on Optimization of Nutrient Composition of Military Rations for Short-Term, High-Stress Situations.
Montain SJ, Young AJ. 2003. Diet and physical performance. Appetite 40(3):255–267.
Montain SJ, Shippee RL, Tharion WJ. 1997. Carbohydrate-electrolyte solution effects on physical performance of military tasks. Aviat Space Environ Med 68(5):384–391.
Moore C, Murphy MM, Keast DR, Holick MF. 2004. Vitamin D intake in the United States. J Am Diet Assoc 104(6):980–983.
Mooren FC, Golf SW, Volker K. 2003. Effect of magnesium on granulocyte function and on the exercise induced inflammatory response. Magnes Res 16(1):49–58.
Morris MS, Fava M, Jacques PF, Selhub J, Rosenberg IH. 2003. Depression and folate status in the US Population. Psychother Psychosom 72(2):80–87.
Murray R, Bartoli W, Stofan J, Horn M, Eddy D. 1999. A comparison of the gastric emptying characteristics of selected sports drinks. Int J Sport Nutr 9(3):263–274.
Newhouse IJ, Clement DB. 1988. Iron status in athletes. An update. Sports Med 5(6):337–352.
Nieman DC, Henson DA, McAnulty SR, McAnulty LS, Morrow JD, Ahmed A, Heward CB. 2004. Vitamin E and immunity after the Kona Triathlon World Championship. Med Sci Sports Exerc 36(8):1328–1335.
Nijveldt RJ, van Nood E, van Hoorn DE, Boelens PG, van Norren K, van Leeuwen PA. 2001. Flavonoids: A review of probable mechanisms of action and potential applications. Am J Clin Nutr 74(4):418–425.
Nindl BC, Leone CD, Tharion WJ, Johnson RF, Castellani JW, Patton JF, Montain SJ. 2002. Physical performance responses during 72 h of military operational stress. Med Sci Sports Exerc 34(11):1814–1822.
Nishimuta M, Kodama N, Morikuni E, Yoshioka YH, Takeyama H, Yamada H, Kitajima H, Suzuki K. 2004. Balances of calcium, magnesium and phosphorus in Japanese young adults. J Nutr Sci Vitaminol (Tokyo) 50(1):19–25.
Nordin BE, Polley KJ. 1987. Metabolic consequences of the menopause. A cross-sectional, longitudinal, and intervention study on 557 normal postmenopausal women. Calcif Tissue Int 41 (Suppl 1):S1–S59.
Norton VP, Noble JM. 1991. Acceptance of quantity recipes with zero added salt by a military population. J Am Diet Assoc 91(3):312–315.
Novak F, Heyland DK, Avenell A, Drover JW, Su X. 2002. Glutamine supplementation in serious illness: A systematic review of the evidence. Crit Care Med 30(9):2022–2029.
Nyakeriga AM, Troye-Blomberg M, Dorfman JR, Alexander ND, Back R, Kortok M, Chemtai AK, Marsh K, Williams TN. 2004. Iron deficiency and malaria among children living on the coast of Kenya. J Infect Dis 190(3):439–447.
Olson JA. 1987. Recommended dietary intakes (RDI) of vitamin A in humans. Am J Clin Nutr 45(4):704–716.
Pacy PJ, Price GM, Halliday D, Quevedo MR, Millward DJ. 1994. Nitrogen homeostasis in man: The diurnal responses of protein synthesis and degradation and amino acid oxidation to diets with increasing protein intakes. Clin Sci 86(1):103–118.
Patterson BW, Nguyen T, Pierre E, Herndon DN, Wolfe RR. 1997. Urea and protein metabolism in burned children: Effect of dietary protein intake. Metabolism 46(5):573–578.
Payton KB, Flanagan PR, Stinson EA, Chodirker DP, Chamberlain MJ, Valberg LS. 1982. Technique for determination of human zinc absorption from measurement of radioactivity in a fecal sample or the body. Gastroenterology 83(6):1264–1270.
Penetar DM, McCann U, Thorne D, Schelling A, Galinski C, Sing H, Thomas M, Belenky G. 1994. Effects of caffeine on cognitive performance, mood, and alertness in sleep-deprived humans. In: Food Components to Enhance Performance. Washington, DC: National Academy Press.
Percival SS. 1998. Copper and immunity. Am J Clin Nutr 67(5 Suppl):1064S–1068S.
Phinney SD, Bistrian BR, Wolfe RR, Blackburn GL. 1983. The human metabolic response to chronic ketosis without caloric restriction: Physical and biochemical adaptation. Metabolism 32(8):757–768.
Popper R, Smits G, Meiselman HL, Hirsch E. 1989. Eating in combat: A survey of US Marines. Mil Med 154(12):619–623.
Portale AA, Halloran BP, Morris RC Jr. 1989. Physiologic regulation of the serum concentration of 1,25-dihydroxyvitamin D by phosphorus in normal men. J Clin Invest 83(5):1494–1499.
Powers SK, Howley ET. 1997. Exercise Physiology. Theory and Application to Fitness and Performance. 3rd ed. Boston, MA: McGraw-Hill.
Prasad AS, Fitzgerald JT, Bao B, Beck FW, Chandrasekar PH. 2000. Duration of symptoms and plasma cytokine levels in patients with the common cold treated with zinc acetate. A randomized, double-blind, placebo-controlled trial. Ann Intern Med 133(4):245–252.
Ravaglia G, Forti P, Maioli F, Bastagli L, Facchini A, Mariani E, Savarino L, Sassi S, Cucinotta D, Lenaz G. 2000. Effect of micronutrient status on natural killer cell immune function in healthy free-living subjects aged >/=90 y. Am J Clin Nutr 71(2):590–598.
Rawson ES, Clarkson PM. 2003. Scientifically debatable: Is creatine worth its weight? Gatorade Sports Science Institute: Sports Science Exchange #91 16(4):1–6.
Reasner CA 2nd, Dunn JF, Fetchick DA, Liel Y, Hollis BW, Epstein S, Shary J, Mundy GR, Bell NH. 1990. Alteration of vitamin D metabolism in Mexican-Americans. J Bone Miner Res 5(1):13–17.
Reddy ST, Wang CY, Sakhaee K, Brinkley L, Pak CY. 2002. Effect of low-carbohydrate high-protein diets on acid-base balance, stone-forming propensity, and calcium metabolism. Am J Kidney Dis 40(2):265–274.
Ricci TA, Chowdhury HA, Heymsfield SB, Stahl T, Pierson RN Jr, Shapses SA. 1998. Calcium supplementation suppresses bone turnover during weight reduction in postmenopausal women. J Bone Miner Res 13(6):1045–1050.
Rosenthal JM, Amiel SA, Yaguez L, Bullmore E, Hopkins D, Evans M, Pernet A, Reid H, Giampietro V, Andrew CM, Suckling J, Simmons A, Williams SC. 2001. The effect of acute hypoglycemia on brain function and activation: A functional magnetic resonance imaging study. Diabetes 50(7):1618–1626.
Ruppert M, Overlack A, Kolloch R, Kraft K, Lennarz M, Stumpe KO. 1994. Effects of severe and moderate salt restriction on serum lipids in nonobese normotensive adults. Am J Med Sci 307(Suppl 1):S87–S90.
Sacheck JM, Blumberg JB. 2001. Role of vitamin E and oxidative stress in exercise. Nutrition 17(10):809–814.
Sacks FM, Svetkey LP, Vollmer WM, Appel LJ, Bray GA, Harsha D, Obarzanek E, Conlin PR, Miller ER 3rd, Simons-Morton DG, Karanja N, Lin PH. 2001. Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. DASH-Sodium Collaborative Research Group. N Engl J Med 344(1):3–10.
Salovaara H. 1982. Sensory limitations to replacement of sodium with potassium and magnesium in bread. Cereal Chem 59(5):427–430.
Sauberlich HE, Hodges RE, Wallace DL, Kolder H, Canham JE, Hood J, Raica N Jr, Lowry LK. 1974. Vitamin A metabolism and requirements in the human studied with the use of labeled retinol. Vitam Horm 32:251–275.
Sawka MN, Montain SJ. 2001. Fluid and electrolyte balance: Effects on thermoregulation and exercise in the heat. In: Bowman BA, Russell RM, eds. Present Knowledge in Nutrition. 8th ed. Washington, DC: ILSI Press. Pp. 115–124.
Sen CK, Packer L. 2000. Thiol homeostasis and supplements in physical exercise. Am J Clin Nutr 72(2 Suppl):653S–669S.
Shafat A, Butler P, Jensen RL, Donnelly AE. 2004. Effects of dietary supplementation with vitamins C and E on muscle function during and after eccentric contractions in humans. Eur J Appl Physiol 93(1–2):196–202.
Shephard RJ, Shek PN. 1998. Immunological hazards from nutritional imbalance in athletes. Exerc Immunol Rev 4:22–48.
Shippee R, Friedl K, Kramer T, Mays M, Popp K, Askew E, Fairbrother B, Hoyt R, Vogel J, Marchitelli L, Frykman P, Martinez-Lopez L, Bernton E, Kramer M, Tulley R, Rood J, Delany J, Jezior D, Arsenault J. 1994. Nutritional and Immunological Assessment of Ranger Students with Increased Caloric Intake. Technical Report No. T95-5. Fort Detrick, MD: US Army Medical Research and Materiel Command.
Shirreffs S. 2004 (August 10) Optimization of Nutrient Composition of Military Rations for Short-Term, High-Stress Situations: Sodium, Potassium and Other Electrolytes. Paper presented at the Institute of Medicine Workshop on Optimization of Nutrient Composition of Military Rations for Short-Term, High-Stress Situations, Natick, MA. Institute of Medicine Committee on Optimization of Nutrient Composition of Military Rations for Short-Term, High-Stress Situations.
Shirreffs SM, Maughan RJ. 1997. Whole body sweat collection in humans: An improved method with preliminary data on electrolyte content. J Appl Physiol 82(1):336–341.
Siener R, Ebert D, Nicolay C, Hesse A. 2003. Dietary risk factors for hyperoxaluria in calcium oxalate stone formers. Kidney Int 63(3):1037–1043.
Skoog SM, Bharucha AE. 2004. Dietary fructose and gastrointestinal symptoms: A review. Am J Gastroenterol 99(10):2046–2050.
Solomons NW, Jacob RA. 1981. Studies on the bioavailability of zinc in humans: Effects of heme and nonheme iron on the absorption of zinc. Am J Clin Nutr 34(4):475–482.
Sorensen LB, Moller P, Flint A, Martens M, Raben A. 2003. Effect of sensory perception of foods on appetite and food intake: A review of studies on humans. Int J Obes Relat Metab Disord 27(10):1152–1166.
Specker B. 2005 (December 8). Vitamin D Requirements. Presented at the Institute of Medicine Symposium on Dietary Reference Intakes: Framing the Next Generation, Washington, DC: Food and Nutrition Board.
Stepto NK, Carey AL, Staudacher HM, Cummings NK, Burke LM, Hawley JA. 2002. Effect of short-term fat adaptation on high-intensity training. Med Sci Sports Exerc 34(3):449–455.
Takkouche B, Regueira-Mendez C, Garcia-Closas R, Figueiras A, Gestal-Otero JJ. 2002. Intake of vitamin C and zinc and risk of common cold: A cohort study. Epidemiology 13(1):38–44.
Tanphaichitr V. 1999. Thiamin. In: Shils ME, Olson JA, Shike M, Ross AC, eds. Modern Nutrition in Health and Disease. 9th ed. Baltimore, MD: Williams and Wilkins. Pp. 381–389.
Terblanche S, Noakes TD, Dennis SC, Marais D, Eckert M. 1992. Failure of magnesium supplementation to influence marathon running performance or recovery in magnesium-replete subjects. Int J Sport Nutr 2(2):154–164.
Terjung RL, Clarkson P, Eichner ER, Greenhaff PL, Hespel PJ, Israel RG, Kraemer WJ, Meyer RA, Spriet LL, Tarnopolsky MA, Wagenmakers AJ, Williams MH. 2000. American College of Sports Medicine roundtable. The physiological and health effects of oral creatine supplementation. Med Sci Sports Exerc 32(3):706–717.
Tharion WJ, Moore RJ. 1993. Effects of Carbohydrate Intake and Load Bearing Exercise on Rifle Marksmanship Performance. Technical Report No. T5-93. Natick, MA: US Army Medical Research and Development Command.
Tharion WJ, Hoyt RW, Cline AD, DeLany JP, Lieberman HR. 2004. Energy expenditure and water turnover assessed by doubly labeled water during manual work in a dry and warm environment. J Human-Environ Syst 7(1):11–17.
Thompson D, Bailey DM, Hill J, Hurst T, Powell JR, Williams C. 2004. Prolonged vitamin C supplementation and recovery from eccentric exercise. Eur J Appl Physiol 92(1–2):133–138.
Thompson D, Williams C, Kingsley M, Nicholas CW, Lakomy HK, McArdle F, Jackson MJ. 2001. Muscle soreness and damage parameters after prolonged intermittent shuttle-running following acute vitamin C supplementation. Int J Sports Med 22(1):68–75.
Tikuisis P, Keefe AA, McLellan TM, Kamimori G. 2004. Caffeine restores engagement speed but not shooting precision following 22 h of active wakefulness. Aviat Space Environ Med 75(9):771–776.
Tipton KD. 2004 (August 9). Carbohydrate/Protein Balance for Muscle Performance. Paper presented at the Institute of Medicine Workshop on Optimization of Nutrient Composition of Military Rations for Short-Term, High-Stress Situations, Natick, MA. Institute of Medicine Committee on Optimization of Nutrient Composition of Military Rations for Short-Term, High-Stress Situations.
Tipton KD, Wolfe RR. 2001. Exercise, protein metabolism, and muscle growth. Int J Sport Nutr Exerc Metab 11(1):109-132.
Tipton KD, Wolfe RR. 2004. Protein and amino acids for athletes. J Sports Sci 22(1):65–79.
Tipton KD, Borsheim E, Wolf SE, Sanford AP, Wolfe RR. 2003. Acute response of net muscle protein balance reflects 24-h balance after exercise and amino acid ingestion. Am J Physiol Endocrinol Metabol 284(1):E76–E89.
Tipton KD, Elliott TA, Cree MG, Wolf SE, Sanford AP, Wolfe RR. 2004. Ingestion of casein and whey proteins result in muscle anabolism after resistance exercise. Med Sci Sports Exerc 36(12):2073–2081.
Tipton KD, Ferrando AA, Phillips SM, Doyle D Jr, Wolfe RR. 1999. Postexercise net protein synthesis in human muscle from orally administered amino acids. Am J Physiol 276(4 Pt 1):E628–E634.
Tipton K, Green NR, Haymes EM, Waller M. 1993. Zinc loss in sweat of athletes exercising in hot and neutral temperatures. Int J Sport Nutr 3(3):261–271.
Tiselius HG. 1997. Risk formulas in calcium oxalate urolithiasis. World J Urol 15(3):176–185.
Todd KS, Butterfield GE, Calloway DH. 1984. Nitrogen balance in men with adequate and deficient energy intake at three levels of work. J Nutr 114(11):2107–2118.
Traber MG, Mastaloudis A. 2004 (August 9). Vitamin C and E in the Prevention of Oxidative Stress, Inflammatory and Fatigue from Exhaust Exercise. Paper presented at the Institute of Medicine Workshop on Optimization of Nutrient Composition of Military Rations for Short-Term, High-Stress Situations, Natick, MA. Institute of Medicine Committee on Optimization of Nutrient Composition of Military Rations for Short-Term, High-Stress Situations.
Troost FJ, Brummer RJ, Dainty JR, Hoogewerff JA, Bull VJ, Saris WH. 2003. Iron supplements inhibit zinc but not copper absorption in vivo in ileostomy subjects. Am J Clin Nutr 78(5):1018–1023.
Truswell AS, Seach JM, Thorburn AW. 1988. Incomplete absorption of pure fructose in healthy subjects and the facilitating effect of glucose. Am J Clin Nutr 48(6):1424–1430.
Turner RB, Cetnarowski WE. 2000. Effect of treatment with zinc gluconate or zinc acetate on experimental and natural colds. Clin Infect Dis 31(5):1202–1208.
Turnlund JR, Jacob RA, Keen CL, Strain JJ, Kelley DS, Domek JM, Keyes WR, Ensunsa JL, Lykkesfeldt J, Coulter J. 2004. Long-term high copper intake: Effects on indexes of copper status, antioxidant status, and immune function in young men. Am J Clin Nutr 79(6):1037–1044.
US Departments of Army, Navy, and Air Force. 2001. Nutrition Standards and Education. AR 40-25/BUMEDINST 10110.6/AFI 44-141. Washington, DC: US Department of Defense Headquarters.
Usui Y, Tanimura H, Nishimura N, Kobayashi N, Okanoue T, Ozawa K. 1990. Vitamin K concentrations in the plasma and liver of surgical patients. Am J Clin Nutr 51(5):846–852.
van Etten E, Decallonne B, Mathieu C. 2002. 1,25-dihydroxycholecalciferol: Endocrinology meets the immune system. Proc Nutr Soc 61(3):375–380.
van het Hof KH, Brouwer IA, West CE, Haddeman E, Steegers-Theunissen RP, van Dusseldorp M, Weststrate JA, Eskes TK, Hautvast JG. 1999. Bioavailability of lutein from vegetables is 5 times higher than that of beta-carotene. Am J Clin Nutr 70(2):261–268.
Vanderpas JB, Contempre B, Duale NL, Deckx H, Bebe N, Longombe AO, Thilly CH, Diplock AT, Dumont JE. 1993. Selenium deficiency mitigates hypothyroxinemia in iodine-deficient subjects. Am J Clin Nutr 57(2 Suppl):271S–275S.
Vellar OD. 1968. Studies on sweat losses of nutrients. II. The influence of an oral iron load on the iron content of whole body cell-free sweat. Scand J Clin Lab Invest 21(4):344–346.
Vistisen B, Nybo L, Xu X, Hoy CE, Kiens B. 2003. Minor amounts of plasma medium-chain fatty acids and no improved time trial performance after consuming lipids. J Appl Physiol 95(6):2434–2443.
Wacker WE, Parisi AF. 1968. Magnesium metabolism. N Engl J Med 278(12):658–663.
Walker RM, Linkswiler HM. 1972. Calcium retention in the adult human male as affected by protein intake. J Nutr 102(10):1297–1302.
Waller MF, Haymes EM. 1996. The effects of heat and exercise on sweat iron loss. Med Sci Sports Exerc 28(2):197–203.
Weaver CM, Rajaram S. 1992. Exercise and iron status. J Nutr 122(3 Suppl):782–787.
Weller E, Bachert P, Meinck HM, Friedmann B, Bartsch P, Mairbaurl H. 1998. Lack of effect of oral Mg-supplementation on Mg in serum, blood cells, and calf muscle. Med Sci Sports Exerc 30(11):1584–1591.
Welsh RS, Davis JM, Burke JR, Williams HG. 2002. Carbohydrates and physical/mental performance during intermittent exercise to fatigue. Med Sci Sports Exerc 34(4):723–731.
Westerterp KR. 2004. Diet induced thermogenesis. Nutr Metab (Lond) 1(1):5–9.
Whitson PA, Pietrzyk RA, Pak CY. 1997. Renal stone risk assessment during Space Shuttle flights. J Urol 158(6):2305–2310.
Whybro A, Jagger H, Barker M, Eastell R. 1998. Phosphate supplementation in young men: Lack of effect on calcium homeostasis and bone turnover. Eur J Clin Nutr 52(1):29–33.
Wilkinson R. 1976. Absorption of calcium, phosphorus, and magnesium. In: Nordin BEC, ed. Calcium, Phosphate, and Magnesium Metabolism. Clinical Physiology and Diagnostic Procedures. New York: Churchill Livingstone. Pp. 36–112.
Williams HE, Wandzilak TR. 1989. Oxalate synthesis, transport and the hyperoxaluric syndromes. J Urol 141(3 Pt 2):742–749.
Williams MH. 2005. Nutrition for Health, Fitness, and Sport. 7th ed. Boston, MA: McGraw-Hill.
Wilmore JH, Costill DL. 1999. Physiology of Sport and Exercise. 2nd ed. Champaign, IL: Human Kinetics. Pp. 115–154.
Wolfe RR, Goodenough RD, Burke JF, Wolfe MH. 1983. Response of protein and urea kinetics in burn patients to different levels of protein intake. Ann Surg 197(2):163–171.
Women’s Health Initiative Study Group. 2004. Dietary adherence in the Women’s Health Initiative Dietary Modification Trial. J Am Diet Assoc 104(4):654–658.
Wood RJ, Sitrin MD, Rosenberg IH. 1988. Effect of phosphorus on endogenous calcium losses during total parenteral nutrition. Am J Clin Nutr 48(3):632–636.
Woodson RD. 1984. Hemoglobin concentration and exercise capacity. Am Rev Respir Dis 129(2 Pt 2):S72–S75.
Zemel MB, Shi H, Greer B, Dirienzo D, Zemel PC. 2000. Regulation of adiposity by dietary calcium. FASEB J 14(9):1132–1138.
Zittermann A, Sabatschus O, Jantzen S, Platen P, Danz A, Dimitriou T, Scheld K, Klein K, Stehle P. 2000. Exercise-trained young men have higher calcium absorption rates and plasma calcitriol levels compared with age-matched sedentary controls. Calcif Tissue Int 67(3):215–219.
Zittermann A, Sabatschus O, Jantzen S, Platen P, Danz A, Stehle P. 2002. Evidence for an acute rise of intestinal calcium absorption in response to aerobic exercise. Eur J Nutr 41(5):189–196.
Zwart SR, Hargens AR, Smith SM. 2004. The ratio of animal protein intake to potassium intake is a predictor of bone resorption in space flight analogues and in ambulatory subjects. Am J Clin Nutr 80(4):1058–1065.







































































































