6
Employment, Insurance, and Economic Issues
A history of cancer can have a significant impact on employment opportunities and may also affect the ability to obtain and retain health and life insurance. In addition, financial difficulties may arise because cancer survivors’ health-related work limitations may necessitate a reduced work schedule. The economic burden of cancer can be compounded by high out-of-pocket expenses for prescription drugs, medical devices and supplies, and expenses related to co-insurance and copayments. These employment, insurance, and economic issues are not necessarily limited to the cancer survivor—they may extend to family members, limiting access to insurance and posing a financial burden. The extent of these socioeconomic problems and current legal remedies to address them are described in this chapter, as are potential programmatic, educational, legislative, and advocacy responses.1 Selected federal and state programs are described that are relevant to cancer survivors, including the Medicare prescription drug program that will be implemented in 2006; a state Medicaid option available since 2000 to provide poor and uninsured women with coverage for treatment and follow-up of breast and cervical cancer; recent federal investments in state high-risk insurance pools that provide insurance coverage to people who cannot get insurance because of poor health; and federal income replacement programs through the Social Security Administration for individuals too disabled to work.
EMPLOYMENT
Impact of Cancer on Survivors’ Employment Opportunities
There are an estimated 3.8 million working-age adults (ages 20 to 64) with a history of cancer as of 2002, and consequently more cancer survivors are in the workplace now than ever before, (NCI, 2005). The proportion of individuals with a history of cancer rises with age, from 1 percent among individuals ages 40 to 44 to 8 percent among those age 60 to 64 (see Chapter 2). Consequently, many employers have had to address issues related to the reintegration of workers following their treatment and the alteration of work schedules and environment to accommodate any lingering cancer-related impairments.
Most cancer survivors who worked before their diagnosis return to work following their treatment (Spelten et al., 2002). In fact, with the advent of effective interventions to curb the side effects of cancer therapies and an increased reliance on outpatient care, some individuals are able to work throughout their cancer treatment (Messner and Patterson, 2001). Retaining one’s employment status has obvious financial benefits and is often also necessary for health insurance coverage, self-esteem, and social support (Voelker, 1999; Spelten et al., 2002). On the other hand, cancer may prompt retirement from an undesirable job or launch a search for a new career that is more satisfying personally, but less lucrative. Work after cancer must therefore be assessed in the context of an individual’s priorities and values, rather than exclusively using social or economic metrics (Steiner et al., 2004).
Employers, supervisors, and co-workers may assume that persons with cancer are not able to perform job responsibilities as well as they did before the diagnosis. They may also perceive them as a poor risk for promotion. These misconceptions can lead to subtle or blatant discrimination in the workplace (Messner and Patterson, 2001). Cancer survivors have reported problems in the workplace that include dismissal, failure to hire, demotion, denial of promotion, undesirable transfer, denial of benefits, and hostility (NCCS and Amgen, undated; Fesko, 2001; Hoffman, 2004b). Studies conducted prior to the passage of comprehensive employment discrimination laws suggest that survivors of cancer encountered substantial employment obstacles (Mellette, 1985; Hoffman, 1989, 1991; Bordieri et al., 1990; Brown and Ming, 1992).
Federal and state laws passed in the early 1990s have helped to ease problems related to job discrimination. The most important is the Americans with Disabilities Act (ADA), which protects disabled workers. In addition, the Health Insurance Portability and Accountability Act (HIPAA) and the Consolidated Omnibus Budget Reconciliation Act (COBRA) have
helped workers move from one job to another without loss of health insurance. Since the enactment of these laws (and their enforcement), employment practices have improved and employees have gained some protections (Hoffman, 1999). Common accommodations made for those living with illnesses include reduced and flexible schedules. Such flexibility is increasingly common in the workplace to meet the needs of employees with family responsibilities. However, providing flexibility in production or assembly line scheduling can be more difficult for “blue collar” workers (Voelker, 1999). Even with these new protections and improvements in employer practice, contemporary workers may lose employment because of cancer (Box 6-1).
To fully understand the impact of cancer on work outcomes, one would
|
BOX 6-1 Allison Yowell, a seventh-grade teacher in a Virginia public school, was forced from her job when her Hodgkin’s disease recurred. Although her prognosis was good, school officials notified her that she must resign, or face firing, because she had used all her sick days. As a recent hire, she was ineligible to request leave without pay. It was recommended that she resign before being terminated to avoid marring her teaching record. She submitted her resignation, but was reinstated only after adverse publicity regarding the case. Ms. Yowell, who wanted 4 months of leave without pay, couldn’t take advantage of the federal Family and Medical Leave Act, which grants 12 unpaid weeks per year, because it applies only after an employee has worked a full year. John Magenheimer, who had headed a research laboratory at a major company, was recovering from surgery, chemotherapy, and radiation treatment for cancer when he learned that his company had fired him and that his health, life, and dental insurance had been terminated. He and 180 other employees of the company who had been placed on long-term disability were fired. Most companies used to pay health benefits for the long-term disabled until they were 65, but as health insurance costs and the number of disabled employees have climbed, more companies are firing them. According to a survey of 723 companies in 2002, 27 percent had a policy to dismiss employees as soon as they went onto long-term disability and 24 percent dismissed them at a set time thereafter, usually 6 to 12 months. Only 15 percent of companies had a policy to keep the disabled on as employees with benefits until age 65. Mr. Magenheimer had the option of continuing his health insurance through a federal law known as COBRA, and as a disabled worker he could purchase Medicare coverage after 18 months. Both kinds of coverage cost thousands of dollars a year, which many disabled workers can ill afford. SOURCES: Pereira (2003); Laris (2005a,b). |
ideally have results from studies that had the following six characteristics (Steiner et al., 2004):
-
Inclusion of cancer survivors that represented the entire population of U.S. cancer survivors. Many studies are based on survivors followed at one cancer center, or who are from particular geographic areas. Their employment experience may not reflect that of the nation. Ideally, survivors would be selected for study from population-based cancer registries.
-
Designed to provide a prospective and longitudinal look at work outcomes so that both short-term and long-term work outcomes could be assessed and the dynamic nature of employment could be understood.
-
Include assessments of work, including information on the type, amount, content, physical demands, cognitive demands, and attitudes about work.
-
Include assessments of the impact of cancer on the economic status of the individual and the family.
-
Identify moderators of work return and work function, particularly those that are susceptible to intervention (e.g., availability of health insurance and disability benefits to offset lost income).
-
Include a cohort of survivors that is sufficiently large to allow multivariate statistical analysis and that provides information on important groups (e.g., minority groups, cancer types).
The committee reviewed the literature published in the past 10 years on the employment experience of U.S. cancer survivors who were studied in 1992, the year the ADA took effect, or later.2 Most of the studies reviewed had some, but rarely all, of the ideal attributes just described. There are few prospective studies of cancer’s effects on employment, but those that are available provide important insights into how interventions could be designed to assist cancer survivors.
In one prospective study, women with invasive breast cancer were less likely to work 6 months following diagnosis relative to a control sample of women. Breast cancer survivors who remained working worked fewer hours than women in the control group (Bradley et al., 2005a). At 12 months, however, many women who had stopped working had returned to work (Bradley, 2004). The nonemployment effect of breast cancer diagnosis and treatment at 6 months was twice as large for African-American women. Similar findings were evident among men with prostate cancer. Here, 28
percent of men were not employed 6 months following diagnosis but, at 12 and 18 months, survivors’ employment was statistically not different from controls (Bradley, 2004). At 12 months, 26 percent of men with prostate cancer reported that cancer interfered with their ability to perform tasks that involved physical effort (Bradley et al., 2005b). Up to 16 percent of men said that they noticed changes in their ability to perform cognitive tasks (e.g., concentrate, keep up with others, learn new things). The implication of these findings is that interventions to assist survivors who stop working (e.g., income replacement programs, information about access to health insurance) are needed within 6 months of diagnosis. Workplace reintegration programs may be most needed through the year following diagnosis.
Nearly one out of five cancer survivors reported cancer-related limitations in ability to work when interviewed 1 to 5 years following their diagnosis as part of one of the largest cross-sectional studies to date (Short et al., 2005b). Nine percent were unable to work at all. Labor force participation dropped by 12 percentage points from diagnosis to follow-up and about two-thirds of survivors who quit working attributed the change to cancer. Other studies have found the drop in employment following cancer to be similar in magnitude. For example, a 10 percentage point greater decline in employment was noted among breast cancer survivors as compared to women without breast cancer (Bradley et al., 2002a,b).
The impact of cancer on employment has not been well studied across all types of cancer. However, work-related outcomes have been shown to be significantly worse for cancers of the central nervous system, hematologic cancers (Short et al., 2005b), and cancer of the head and neck. In one study, 52 percent of survivors of head and neck cancer who had worked before their diagnosis were disabled by their cancer treatment and could no longer work when assessed, on average, more than 4 to 5 years following their diagnosis (Taylor et al., 2004). Nearly three-quarters (74 percent) of survivors considered potentially cured of acute myelogenous leukemia (excluding those receiving allogenic marrow transplants) returned to full-time work according to a long-term follow-up study (median of 9.2 years from first or second complete remission) (de Lima et al., 1997). Less than a third of those who were not working cited physical limitation as the reason.
Other studies of cancer survivors have also shown that most cancer survivors continue to work, but that a minority have limitations that interfere with work. Of those working at the time of their initial diagnosis, 67 percent of survivors of lung, colorectal, breast, or prostate cancer were employed 5 to 7 years later when interviewed in 1999 (Bradley and Bednarek, 2002). Survivors in this study who stopped working did so because they retired (54 percent), were in poor health or disabled (24 percent), quit (4 percent), their business closed (9 percent), or for other reasons
TABLE 6-1 Limitations Imposed by Cancer and Its Treatment on Patients Currently Working
|
At least some of the time task requires: |
Cancer Interfered with Work Performance (percentage) |
|
Physical tasks |
18 |
|
Lift heavy loads |
26 |
|
Stoop, kneel, or crouch |
14 |
|
Concentrate for long periods of time |
12 |
|
Analyze data |
11 |
|
Keep pace with others |
22 |
|
Learn new things |
14 |
|
SOURCE: Adapted from Bradley and Bednarek (2002). |
|
(9 percent). Many employed survivors worked in excess of 40 hours per week, although some reported various degrees of disability that interfered with job performance. When work required lifting heavy loads, for example, 26 percent of subjects reported that cancer interfered with their performance (Table 6-1).
Other investigators point to the vulnerability of employees with jobs involving manual labor. In one study, type of occupation was the main determinant of whether individuals were employed after diagnosis. Although 76 percent of respondents indicated that they were working at the time of diagnosis and 82 percent said they wanted to work full- or part-time, only 56 percent were working at the time of the study (Rothstein et al., 1995). Laborers were most likely, and professionals least likely, to have some of their job duties reassigned upon their return to work.
Relatively few studies have examined the effect of cancer on income in the context of the family household. In one study that studied such effects, breast cancer survivors who were working at the time of their diagnosis experienced higher rates of functional impairment and significantly larger reductions in annual earnings over the 5-year study period than did working control subjects. These losses arose mostly from reduced work effort, not changes in pay rates. Changes in total household earnings were lower for survivors, suggesting the presence of family adjustments to the disease. However, no significant differences were detected between the groups in changes in total income or assets over the study period (Chirikos, 2001; Chirikos et al., 2002a,b). This study suggests that cancer can have an economic impact on the entire family, requiring compensatory employment behaviors on the part of family members to maintain earnings.
Analyses of national health surveys have provided some information on
the effects of cancer on employment. According to analyses of the 2000 National Health Interview Survey (NHIS), cancer survivors were found to have poorer outcomes across all employment-related burden measures relative to matched control subjects (Yabroff et al., 2004). Cancer survivors were less likely than control subjects to have had a job in the past month. Furthermore, they were more likely to be unable to work because of health, more limited in the amount or kind of work because of a health problem, and had more days lost from work in the past year. The decrements in productivity were generally consistent across tumor sites. When analyzed by time since diagnosis, a higher percentage of survivors diagnosed in the past year also reported having jobs than survivors in any of the other time-since-diagnosis intervals. However, this group of survivors also had the most reported work loss days. This analysis included information on cancer survivors of all ages.3 In an analysis of three years of NHIS data (1998 to 2000) limited to adults ages 18 to 64, nearly one in six individuals (17 percent) with a history of cancer reported that they were unable to work because of a physical, mental, or emotional problem (Hewitt et al., 2003). An additional 7.4 percent of cancer survivors were limited in the kind or amount of work they could do. This level of work limitation exceeded that of working-age individuals without a history of cancer (Figure 6-1). In an attempt to isolate cancer-related effects, investigators compared individuals reporting a history of cancer but no other chronic disease to individuals without a history of cancer or with no other chronic illness. Using multivariate analyses to control for potentially confounding factors (i.e., age, sex, race/ethnicity, educational attainment, health insurance status, and marital status), individuals with cancer but no other chronic disease were found to be three times more likely to be unable to work than individuals without a history of cancer and reporting no chronic illness. The likelihood of work limitation was much higher among cancer survivors who also reported comorbid chronic diseases (i.e., cardiovascular disease, diabetes, emphysema, ulcer, weak/failing kidneys, liver condition). They were 12 times more likely to be unable to work relative to those without cancer or other chronic illnesses.
The NHIS in 1992 included a supplement funded by the National Cancer Institute (NCI) with a section on issues related to cancer survivorship. Individuals who reported a recent history of cancer (within the past 10 years) were asked about changes in health or life insurance coverage and cancer-related problems with employment. Nearly one in five (18.2 percent) individuals who worked immediately before or after their cancer was
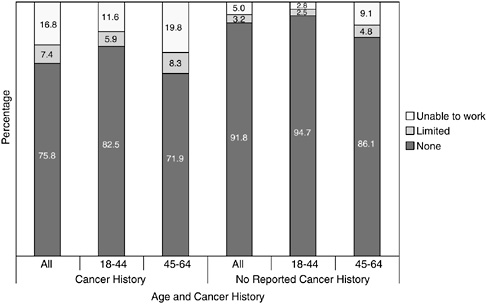
FIGURE 6-1 Work limitations by age and self-reported history of cancer, 1998–2000.
SOURCE: Hewitt et al. (2003).
diagnosed (but who were not self-employed) reported at least one of the following problems (Hewitt et al., 1999):
-
Believed they could not take a new job because of a change in insurance related to cancer (13.2 percent).
-
Believed they could not change jobs because of cancer (7.8 percent).
-
Faced on-the-job problems from an employer or supervisor directly related to their cancer (4.5 percent).
-
Refrained from applying for a new job because they did not want their medical records made public (4.4 percent).
-
Were fired or laid off from their job because of their cancer (3.7 percent).
Kessler and colleagues, in an analysis of the MacArthur Foundation Midlife Development in the United States (MIDUS) survey, found 88 percent of employed people who develop cancer remain at work after receiving their diagnosis and during at least some part of their treatment (2001). Of all of the conditions examined, cancer had the highest reported prevalence of any 30-day work impairment. Two-thirds (66 percent) of those reporting
cancer reported such impairment as compared to 48 percent of those with heart disease and 39 percent of those with arthritis.4 An analysis of symptoms reported on the survey suggested that fatigue may have accounted for much of the impact of cancer on work impairment.
Whether or not cancer survivors disclose their diagnosis once they return to work has not been well researched. In one study of colorectal cancer patients who had been employed before their diagnosis, most (89 percent) returned to work and, of those returning to work, most disclosed their cancer history to employers (81 percent) and co-workers (85 percent) and did so for personal and work-related reasons (Sanchez and Richardson, 2004). Communication with physicians about work return decisions may have facilitated cancer history disclosure. Such high disclosure rates could be accounted for by the fact that anyone who requests a formal leave of absence from work must disclose their cancer diagnosis. Discussions with physicians about work return decisions should take place prior to the initiation of treatment because the acute effects of treatment may affect one’s ability to work full time. Some patient’s treatment decisions may be influenced by employment considerations.
From an employer’s perspective, cancer represents a potential health and productivity burden. In addition to medical costs that may be borne by employers, there are concerns about absenteeism from work, disability program use, workers’ compensation program costs, turnover, family medical leave, and on-the-job productivity losses. Consequently, the cost of cancer to employers greatly exceeds the cost of health insurance alone (Lee, 2004). Cancer accounts for about 10 percent of an employer’s or insurer’s annual medical claim costs, 10 percent of short-term disability claim costs, and 10 percent of long-term disability costs, according to a recent analysis (Pyenson and Zenner, 2002). One study that examined physical and mental health conditions contributing to employer health and productivity cost burden found that cancer ranked relatively low in burden relative to other chronic conditions such as heart conditions, diabetes mellitus, chronic obstructive pulmonary disease, low back disorders, trauma, sinusitis, and renal failure (Goetzel et al., 2003).5 Other investigators found annual health care and disability costs for persons with cancer to be about five times
higher than for their counterparts without cancer (Barnett et al., 2000).6 Medical conditions not directly related to cancer accounted for about half of the total excess expenditures for patients with cancer. For example, infections, asthma, and dental procedures, although not immediately thought of as being associated with cancer, cost considerably more among cancer patients than controls.
In summary, a number of studies have been conducted to gauge the effect of cancer on employment. However, it is difficult to judge overall effects because these studies have:
-
Included individuals with different types of cancer and survival probabilities;
-
Assessed employment patterns at different lengths of time following treatment;
-
Had relatively low participation rates, with healthier individuals enrolling in studies more readily than less healthy individuals;
-
Examined employment at one point in time, possibly obscuring important transitions in and out of work over time;
-
Been conducted in different parts of the country with varying employment patterns; and
-
Had no control group or used control groups that may not have been well matched to subjects. Without adequate control subjects in such studies, it is difficult to distinguish declines in employment following cancer from those that might be expected for other reasons.
Information from the one prospective study that has been conducted indicates that employment is most affected in the period immediately following treatment, suggesting that programs, policies, and financial assistance are critical at this time. The type of occupation appears to be a key determinant of employment difficulties, with workers whose jobs involve physical labor most adversely affected. In terms of cancer site, cancers of the central nervous system, hematologic cancers, and head and neck cancer seem to be associated with poorer work outcomes. The finding from one of the largest cohort studies, that roughly 20 percent of people working at the time of their diagnosis face cancer-related work limitations 2 to 3 years later, is consistent with results of cross-sectional national survey research. This research suggests that cancer is one of several chronic conditions that markedly increase the likelihood of work-related disability.
Despite laws allowing portability of health insurance (see section on health insurance below), individuals with a history of cancer report in recent studies of being afraid to change jobs because of concerns about continuation of health insurance. More than 25 percent of cancer survivors in Short and colleagues’ recent study expressed such fears (Short et al., 2005a). Most individuals returning to work appear to inform their supervisors and colleagues of their cancer for both personal and work-related reasons. Relatively few (5 percent) cancer survivors faced on-the-job problems from an employer or supervisor directly related to their cancer, according to survey research conducted in the early 1990s. However, at this time, 4 percent of cancer survivors employed before their diagnosis said they were fired or laid off from their jobs because of their cancer.
Population-based, prospective cohort studies with adequate control groups are needed to better understand the effects of cancer on employment and in order to observe transitions in and out of the work force over time following diagnosis. Also needed are studies of work-related outcomes other than employment status alone (e.g., full-time versus part-time, job mobility, limitations in ability to work) and systematic assessments of employment differences among cancer survivors, as well as between cancer survivors and noncancer control groups. Efforts to identify remediable risk factors and interventions to ameliorate the deleterious effects of cancer on employment are also needed. Investigators have proposed a conceptual model of work after cancer and have defined important work outcomes that should be monitored to improve our understanding of the relationships among cancer, quality of life, and work outcomes (Steiner et al., 2004).
Cancer Survivors’ Current Employment Rights
Although cancer survivors do not have an unqualified right to obtain and retain employment, they do have the right to freedom from discrimination and to be treated according to their individual abilities. Four federal laws—the ADA, the Family and Medical Leave Act (FMLA), the Employee Retirement and Income Security Act (ERISA), and the Federal Rehabilitation Act—provide cancer survivors with some protection against employment discrimination.
Americans with Disabilities Act
The Americans with Disabilities Act of 1990 prohibits certain employers from discriminating against individuals with disabilities (see Box 6-2). A qualified individual with a disability is protected by the ADA if he or she can perform the essential functions of the job. Under the ADA, a disability is a major health impairment that substantially limits the ability to do
|
BOX 6-2 What is the ADA? Title I of the Americans with Disabilities Act of 1990 prohibits private employers, state and local governments, employment agencies, and labor unions from discriminating against qualified individuals with disabilities in job application procedures, hiring, firing, advancement, compensation, job training, and other terms, conditions, and privileges of employment. Who does the ADA cover? The ADA covers employers with 15 or more employees, including state and local governments. It also applies to employment agencies and to labor organizations. The ADA’s nondiscrimination standards also apply to federal-sector employees. Who is considered disabled under the ADA? An individual with a disability is a person who has a physical or mental impairment that substantially limits one or more major life activities; has a record of such an impairment; or is regarded as having such an impairment. A qualified employee or applicant with a disability is an individual who, with or without reasonable accommodation, can perform the essential functions of the job in question. Reasonable accommodation may include, but is not limited to:
What is an employer required to do under the ADA? An employer is required to make a reasonable accommodation to the known disability of a qualified applicant or employee if it would not impose an “undue hardship” on the operation of the employer’s business. Undue hardship is defined as an action requiring significant difficulty or expense when considered in light of factors such as an employer’s size, financial resources, and the nature and structure of its operation. An employer is not required to lower quality or production standards to make an accommodation, nor is an employer obligated to provide personal-use items such as glasses or hearing aids. SOURCE: EEOC (2004b). |
everyday activities, such as talking, caring for oneself, and getting to work. Some have the misperception that “hidden” disabilities such as cancer, AIDS, arthritis, and mental illness are not bona fide disabilities needing accommodation. The U.S. Department of Labor, however, explicitly states that such hidden disabilities, just like those that are visible, can result in functional limitations that substantially limit one or more of the major life activities (U.S. Department of Labor, 2000).
Cancer survivors, regardless of whether they are in treatment, in remission, or cured, are usually protected as persons with a disability because their cancer represents an impairment that substantially limits a major life activity. Federal courts and the Equal Employment Opportunities Commission (EEOC) usually consider cancer to be a disability under the ADA (Hoffman, 1999). Whether a cancer survivor is covered by the ADA is determined, however, on a case-by-case basis. Because the U.S. Supreme Court has not, to date, squarely addressed whether all cancer survivors are protected by the ADA, cancer survivors’ rights under the law vary depending on the facts of the individual case and the court in which the case is heard.
Some courts have concluded that cancer survivors are “persons with a disability” as defined by the statute. Other courts, however, have placed cancer survivors in a “Catch-22” by concluding that a cancer survivor who is sufficiently healthy to work is not a person with a disability as defined by the ADA (Hoffman, 2000). In one case a woman with breast cancer was acknowledged to have experienced nausea, fatigue, swelling, inflammation, and pain resulting from her treatment, but the U.S. Court of Appeals for the Fifth Circuit found that she could nonetheless perform her essential job duties with accommodations (Ellison v. Software Spectrum Inc.). Although the Court of Appeals found that the woman’s cancer affected her ability to work, it concluded that these limitations were not sufficient to render her a “person with a disability” as defined by the ADA. Other courts have followed the reasoning of the Fifth Circuit and rejected lawsuits by cancer survivors. In another case, a long-term survivor of non-Hodgkin’s lymphoma, fired because his employer feared that future health insurance claims would cause his insurance costs to rise, was determined not to be covered under the ADA after his dismissal (Hirsch v. National Mall and Serv., Inc.). The court concluded that “the ADA was not truly meant to apply to this situation” because the claimant was discriminated against due to the costs of his cancer treatment, and not because of the cancer itself” (Hirsch, 989 F. Supp. 977, 980 [N.D. Ill. 1997]).
The ADA prohibits discrimination in most job-related activities such as hiring, firing, and the provision of benefits. In most cases, a prospective employer may not ask applicants if they have ever had cancer. An employer has the right to know only if an applicant is able to perform the essential
|
BOX 6-3
SOURCE: Job Accommodation Network (Loy and Batiste, 2004). |
functions of the job. A job offer may be contingent on passing a relevant medical exam, provided that all prospective employees are subject to the same exam. An employer may ask detailed questions about health only after making a job offer.
Cancer survivors who need extra time or help to work are entitled to a “reasonable accommodation.” Common accommodations for cancer survivors include changes in work hours or duties to accommodate medical appointments and treatment side effects (Box 6-3). An employer does not have to make changes that would impose an “undue hardship” on the business or other workers. “Undue hardship” refers to any accommodation that would be unduly costly, extensive, substantial, or disruptive, or that would fundamentally alter the nature or operation of the business. For example, an employer may replace a survivor who has to miss an extended period of work (e.g., 6 months or longer) that cannot be performed by a temporary employee.
Some employers express concerns about the costs of accommodations and whether accommodations interfere with typical work schedules and
productivity (Roessler and Sumner, 1997). According to some estimates, the costs of accommodations for workers with disabilities needing special accommodations are typically very low; 71 percent of accommodations cost $500 or less, with 20 percent of those costing nothing (U.S. Department of Labor, 2004b).
Most employment discrimination laws protect only the employee. The ADA offers protection more responsive to survivors’ needs because it also prohibits discrimination against family members. Employers may not discriminate against workers because of their relationship or association with a “disabled” person. Employers may not assume that an employee’s job performance would be affected by the need to care for a family member who has cancer. An important exclusion of the Americans with Disabilities Act is contractual employees. Many people are “self-employed,” but contract their services to large organizations that may terminate a survivor’s contract without regard to the provisions of the ADA. Also excluded from ADA protection are those working for employers with fewer than 15 employees. Among private employees, an estimated 15 percent work for companies with fewer than 10 employees and an additional 11 percent work for companies with 10 to 19 employees (Bureau of Labor Statistics, 2005).7
The EEOC is charged with enforcing the ADA and other civil rights laws. During the 4-year period FY 2000–2003, the EEOC received 1,785 charges of cancer-related disability discrimination under the ADA, representing about 3 percent of all charges during this period (Table 6-2). The EEOC resolved 2,013 cancer-related disability discrimination charges,8 with one-quarter (510/2,013) having outcomes favorable to charging parties or charges with meritorious allegations. The EEOC recovered $11 million in monetary benefits for 352 people (including charging parties and other aggrieved individuals). This amount does not include monetary benefits obtained through litigation.
Another source of information regarding the extent of cancer-related employment problems is the Job Accommodation Network (JAN), a service of the Office of Disability Employment Policy of the U.S. Department of Labor (U.S. Department of Labor, 2004c). JAN provides employers and other interested parties with information on job accommodations and employment opportunities and policies. In 2003, JAN handled 514 cases related to cancer (about 2 percent of their calls and e-mails). These came from
TABLE 6-2 Resolution of Cancer-Related ADA Charges, FY 2000–2003
|
Number of charges for all disabilities/conditions |
63,675 |
|
Cancer-related charges |
1,785 |
|
Cancer-related resolutions |
2,013 |
|
Merit resolutionsa |
510 |
|
People with monetary benefits |
352 |
|
Total monetary benefit |
$10,969,314 |
|
aMerit resolutions are charges with outcomes favorable to charging parties and/or charges with meritorious allegations. These include negotiated settlements, withdrawals with benefits, successful conciliations, and unsuccessful conciliations. SOURCE: U.S. Equal Employment Opportunity Commission (EEOC, 2004a). |
|
both employers and individuals. Most inquiries related to accommodations such as use of leave time and scheduling issues (Personal communication, A. Hirsh, JAN, June 14, 2004).
Family and Medical Leave Act
The Family and Medical Leave Act enacted in 1993 requires employers with at least 50 workers to provide certain benefits for serious medical illness, including cancer, for employees or dependents (U.S. Department of Labor, 2004a). The employee must have worked with his or her employer for at least 1 year. Box 6-4 shows a number of benefits of the statute.
The FMLA attempts to balance the needs of the employer and employee. It:
-
Requires employees to make reasonable efforts to schedule foreseeable medical care so as to not unduly disrupt the workplace;
-
Requires employees to give employers 30 days’ notice of foreseeable medical leave, or as much notice as is practicable;
-
Allows employers to require employees to provide certification of medical needs and allows employers to seek a second opinion, at the employer’s expense, to corroborate medical need; and
-
Permits employers to provide leave provisions more generous than those required by the FMLA.
|
BOX 6-4
SOURCE: U.S. Department of Labor (2004a). |
The Employee Retirement and Income Security Act
The Employee Retirement and Income Security Act (ERISA) prohibits an employer from discriminating against an employee to prevent him or her from collecting benefits under an employee benefit plan. Employee benefit plans are defined broadly, and include any plan providing “medical, surgical, or hospital care benefits, or benefits in the event of sickness, accident, disability, death, or unemployment.” Employers who offer group benefit packages to their employees are subject to ERISA. Some employers fear that the participation of a cancer survivor in a group medical plan will drain benefit funds or increase the employer’s insurance premiums. An employer may violate ERISA if, upon learning of a worker’s cancer history, it dismisses that worker to exclude him or her from a group health plan. An employer also may violate ERISA by encouraging a person with a cancer history to retire as a “disabled” employee. Most benefit plans define disability narrowly to include only the most debilitating conditions. Individuals with a cancer history often do not fit under such a definition and should not be compelled to so label themselves.
ERISA covers both participants (employees) and beneficiaries (spouses and children). Thus, if the employee is fired because his or her spouse has cancer, the employee may be entitled to file a claim. ERISA, however, is
inapplicable to many victims of employment discrimination, including individuals who are denied a new job because of their medical status, employees who are subjected to differential treatment that does not affect their benefits, and employees whose compensation does not include benefits.
Federal Rehabilitation Act
The Federal Rehabilitation Act of 1973 is designed to promote equal employment opportunities for people with disabilities. Unlike the ADA, it is limited to employers of any size that receive money, equipment, or contracts from the federal government. Types of employers subject to the Act include schools, hospitals, defense contractors, and state and local governments. The Act does not apply to the military. The Federal Rehabilitation Act uses the same definition of “individual with a disability” as does the ADA. Also like the ADA, it requires employers to make reasonable accommodations to the physical or mental limitations of qualified individuals.
Executive Order
Unlike many private and state employees, federal employees are protected from genetic-based discrimination. An Executive Order issued in 2000 prohibits federal departments and agencies from making employment decisions about civilian federal employees based on protected genetic information (White House, 2000). The Order also prohibits federal employers from requiring genetic tests as a condition of being hired or receiving benefits.
Genetic nondiscrimination laws have also been enacted in most states. Discrimination in hiring, firing, or terms of employment based on the results of genetic tests is prohibited in 33 states, with many states also restricting the access of employers to genetic information (NCSL, 2005). Some states extend the protections to inherited characteristics, family history, the test results of family members, and information on receipt of genetic services.
State Employment Rights Laws
All states except Alabama and Mississippi have laws that prohibit discrimination against people with disabilities in public and private employment (Hoffman, 2002, 2004b).9 Several states, such as New Jersey, cover
|
BOX 6-5 In Washington state, the “Sick Leave for Sick Families” bill was signed into law in 2002. The bill allows workers, public and private, to use sick leave and other paid leave to care for a child with a medical condition requiring treatment or supervision, or to care for a spouse, parent, parent-in-law, or grandparent who has a serious health condition or an emergency condition. Other states, such as Arizona and Hawaii, have also proposed this type of initiative. In other states, such as California, New Jersey, and New York, lawmakers have introduced plans to extend temporary disability insurance benefits to workers who take family and medical leave. California signed S.B. 1661 into law in 2002, expanding the state’s disability insurance program to provide up to 6 weeks of wage replacement benefits to workers who take time off to care for a seriously ill child, spouse, parent, or domestic partner, or to bond with a new child. Another model under consideration in Illinois creates a cost-sharing fund, with contributions from the employer, employee, and state, and provides employees on leave with partial wage replacement. In Hawaii, Massachusetts, New Hampshire, and Washington, states have proposed establishing temporary disability Family Leave Insurance funds, financed by small payroll contributions by employers and/or employees, which would help working families SOURCE: Center on an Aging Society (2004). |
all employers regardless of the number of employees. The laws in most states, however, cover only employers with a minimum number of employees. A few states, such as California and Vermont, expressly prohibit discrimination against cancer survivors.
Most state laws define “individual with a disability” much as it is defined in the ADA. Therefore, most survivors in those states would be considered “disabled” under those state discrimination laws. The rights of cancer survivors in states whose laws do not mirror the ADA vary depending on how those laws define the protected class.
Many states have leave laws similar to the federal FMLA in that they guarantee employees in the private sector unpaid leave for pregnancy, child-birth, and the adoption of a child (see Box 6-5). Some state laws provide employees with medical leave to address a serious illness, such as cancer. Several states provide coverage more extensive than the federal law.
State medical leave laws vary widely as to:
-
How long an employee can take leave;
-
Which employees may take leave (most states require an employee to have worked for a minimum period of time);
-
Which employers must provide leave (a few states have leave laws that apply to employers of fewer than 50 employees);
-
The definition of “family member” for whose illness an employee may take family medical leave;
-
The type of illness that entitles an employee to medical leave;
-
How much notice an employee must give prior to taking leave;
-
Whether an employee continues to receive benefits while on leave and who pays for them;
-
How the law is enforced (by state agency or through private lawsuit); and
-
Provision and extent of replacement wages.
Programs to Ameliorate Employment Problems
Most employers treat cancer survivors fairly and legally. Some employers, however, erect unnecessary and sometimes illegal barriers to survivors’ job opportunities (Hoffman, 1999, 2004b). Most personnel decisions are driven by economic factors, not by charitable or personal consideration. Employers may be motivated to fire an employee with cancer (or a history of cancer) because of concerns about increased costs due to insurance expenses and lost productivity or because of concerns about the psychological impact of a survivor’s cancer history on other employees. Some employers may fail to revise their personnel policies to comply with new laws and, even among those with updated policies, employers may not train their personnel managers properly to comply with these laws. The interpretation of laws designed to prohibit discriminatory practices is sometimes unclear and is being resolved in the courts. Some employers and co-workers treat cancer survivors differently from other workers, in part because they have misconceptions about survivors’ abilities to work during and after cancer treatment (NCCS and Amgen, undated). In an effort to educate employers regarding their responsibilities to employees with cancer, Business and Health published a special report, “Living, Coping, and Working with Cancer.” A set of recommendations from a panel of health care and business experts convened by Business and Health is shown in Box 6-6.
Information, Support, and Referral
This section reviews sources of employment-related information, support, and referral available through employers, cancer voluntary organizations, consumer advocacy programs, and federal and state government programs. The next section reviews the provision of financial support (including health and disability insurance).
|
BOX 6-6
SOURCE: Business and Health Special Report (Voelker, 1999). |
The role of employers Employers may provide information, support, and referral services of relevance to cancer survivors through onsite health programs or workplace intranets. Several employers offer their employees web-based personal health management tools allowing them to get information and identify resources (Blumklotz and Lansky, 2001). Toll-free medical decision support services are available to employees to help them make better informed health care purchasing decisions. Cancer questions and requests for information lead all other health care inquiries at some of these programs (Lee, 2004). To help employees balance their personal and professional lives, some companies have provided so-called “work-life” programs offering flexible work options, elder care programs, employee assistance programs (EAPs), and health care and wellness programs (Center on an Aging Society, 2004). Such programs are of benefit to individuals undergoing cancer treatment or in need of flexible scheduling upon a return to work. Leave policies may be prescribed by law (see earlier section on the
Family and Medical Leave Act and related state laws), but some employers provide benefits that exceed those mandated.
Many employers in the private and public sectors have formal or informal disability management and return-to-work programs (Bruyere, 2000). EAPs address productivity issues by helping employees identify and resolve personal concerns that may affect job performance, including issues related to health, marriage, family, substance abuse, stress, and legal problems (Employee Assistance Professionals Organization, 2004). EAPs may provide one-on-one assistance, employee training programs, and leadership consultations. An estimated 56 percent of companies with more than 100 employees provide EAPs that address work-life issues (FWI, 1998; Center on an Aging Society, 2004). In an effort to increase the availability of psychosocial support for cancer patients, the Individual Cancer Assistance Network project (funded by the Bristol-Myers Squibb Foundation) has trained master’s-level counselors in EAPs and family service organizations located in Florida (Bristol-Myers Squibb, 2004; Alter, 2005).
It is important to note that employers cannot search records and then initiate contact with employees based on their health status, no matter how commendable their intentions (Lee, 2004). Such contact is prohibited by HIPAA.
Cancer voluntary organizations and consumer advocacy programs Several nonprofit cancer organizations provide education, counseling, and legal advice regarding employment to cancer survivors. The American Cancer Society (ACS) (2004a), the Lance Armstrong Foundation (LAF, 2004), the National Coalition for Cancer Survivorship (NCCS) (Hoffman, 2004a), and CancerCare (CancerCare, 2005), for example, provide information about employment concerns following a diagnosis of cancer.
A number of programs provide legal assistance to cancer survivors concerned about their employment and insurance rights (Box 6-7). For example, legal counseling and education and training for professionals and individuals with cancer are available through the Cancer Legal Resource Center, Western Law Center for Disability Rights. Supported in part by the California Division of ACS, callers to the ACS information line with legal questions are referred to the Center. In 2004 the Center served more than 3,000 callers and reached about 6,000 people through training and outreach. Approximately 13 percent of calls relate to employment, concerns about telling a new employer about cancer, expectations when going back to work, disclosure of cancer history when returning to work, and loss of a job (Schwerin, 2005). The Center serves individuals nationwide, and about half the people calling for assistance are from outside California.
CancerCare is a national nonprofit organization that provides free counseling (individual and group), education, information and referral, and
|
BOX 6-7 The Cancer and ALS Legal Initiative of the Atlanta Legal Aid Society provides free legal assistance to low-income persons living with cancer in the metro Atlanta area. Cancer Legal Resource Center provides information and educational outreach on cancer-related legal issues. Cancer Legal Services Project of the Bar Association of San Francisco provides free services directly to low-income people with cancer. Legal Advocacy for Cancer Patients at the Temple Legal Aid Office provides free attorney and advocate services to individuals in Philadelphia. Legal Information Network for Cancer provides legal assistance to individuals with cancer in central Virginia and referrals to attorneys who provide services on a sliding-scale basis. LegalHealth offers a comprehensive legal clinic onsite in New York area hospitals and at community-based organizations addressing the needs of chronically and seriously ill low-income New Yorkers. Training of doctors, social workers, and other medical professionals is also provided. SOURCES: Legal Information Network for Cancer (2004); Bar Association of San Francisco (2004); New York Legal Assistance Group (2004); ABA (2004). |
direct financial assistance to more than 90,000 people with cancer each year (Personal communication, C. Messner, CancerCare, September 22, 2004) (CancerCare, 2005).10 Staff oncology social workers and case managers address issues related to employment through a program called “Cancer in the Workplace,” where issues related to legal rights and reentering the workplace are discussed. CancerCare sponsors teleconferences regularly, including a series called “Strength for Caring: Living, Working, and Coping with Cancer” (Box 6-8). Some teleconferences are specifically for employers and are promoted through direct contact to companies and partnerships with other organizations. Human resources personnel are able to discuss employer responsibilities, accommodations, helping co-workers deal with colleagues with cancer, and how to interpret laws such as the FMLA and ADA. Teleconferences for patients and caregivers facilitate discussions on disclosure of cancer status to employers, physical examinations, and dealing with physical limitations at work. Caregiver rights under FMLA and ADA are also addressed.
|
BOX 6-8
SOURCE: CancerCare (2004). |
“Good Health for Life” is a program dedicated to getting cancer survivors back to work. Associated with Stanford University Medical Center, the program provides entrepreneurship resources for cancer survivors and educational programs for business and governments (Good Health for Life, 2004).
Federal and state government programs A number of education and referral programs offered by NCI address employment issues. For example, Life After Cancer Treatment, part of NCI’s “Facing Forward Series” of publications, describes federal sources of information regarding employment rights, disability, and discrimination (NCI, 2002). Survivors concerned about employment issues are referred to fact sheets and other information provided by the EEOC, the federal agency that coordinates the investigation of employment discrimination. Other federal sources of information and referral include the U.S. Department of Justice, which provides information to assist persons with disabilities with legal issues, questions about the ADA, mediation services, and other employment issues. The U.S. Department of Labor’s Office of Disability Employment Policy also provides information regarding discrimination, workplace accommodation, and legal rights. The Job Accommodation Network, a service of the U.S. Department of Labor, provides information on workplace accommodation to both employers and employees.
In addition to education and referral programs, 80 federally funded state vocational rehabilitation agencies employing more than 11,000 voca-
tional counselors throughout the United States provide direct services to facilitate a return to work (Personal communication, J. Pepin, U.S. Department of Education, Office of Special Education and Rehabilitation, September 24, 2004). As of 2003, 2,191 individuals with cancer had completed rehabilitation at one of these agencies. Nearly 60 percent of these cancer survivors, upon completion of the rehabilitation program, were placed in a job and worked for at least 90 days (Personal communication, P. Nash, U.S. Department of Education, Office of Special Education and Rehabilitation, September 22, 2004). Individuals with a history of cancer represent less than 1 percent of those served by the federal/state rehabilitation system. It is unclear why so few persons with cancer complete rehabilitation programs—it may be that cancer survivors do not need, desire, or qualify for the services or, alternatively, that they are not referred to, or accepted by, such programs (Conti, 1990; Mundy et al., 1992). The programs are required to prioritize service delivery to those with severe disabilities, and cancer survivors may not always meet eligibility requirements.
In summary, a number of employer, consumer advocacy organizations, and governmental programs are available to provide information, counseling, and rehabilitation services to address employment-related concerns of cancer survivors. There is little information regarding the extent to which cancer survivors or their providers are aware of these services, or use them. There appears to be a patchwork of services, and it is unclear how accessible they are across the country, how comprehensive the services are, and whether they are meeting the needs of cancer survivors.
Financial Assistance
Private short- and long-term disability insurance and disability programs of the Social Security Administration can be important sources of income replacement for cancer survivors who have had extended times away from work or who are disabled and can no longer work. This section briefly reviews these programs. Sources of financial assistance for individuals’ health-related expenditures are described in the next section of the chapter following a review of health insurance issues.
Short- and long-term disability insurance Private short- and long-term disability insurance can provide invaluable financial assistance to individuals who have exhausted their sick and annual leave at work. However, relatively few workers have employment-based disability benefits. In 2004, 39 percent of all workers in private industry had access to short-term disability benefits, other than paid sick leave, while 30 percent had access to long-term disability benefits. Access to these disability benefits is greater among higher wage earners and those working for large employers (Table 6-3).
TABLE 6-3 Percentage of Workers with Access to Disability Insurance Benefits, by Selected Characteristics, Private Industry, 2004
|
Characteristic |
Short-Term Disability Benefits |
Long-Term Disability Benefits |
|
All workers |
39 |
30 |
|
Worker characteristics |
||
|
White-collar occupations |
43 |
41 |
|
Blue-collar occupations |
45 |
22 |
|
Service occupations |
23 |
12 |
|
Full time |
47 |
38 |
|
Part time |
14 |
5 |
|
Union |
67 |
30 |
|
Nonunion |
36 |
30 |
|
Average wage <$15 per hour |
29 |
17 |
|
Average wage ≥$15 per hour |
55 |
48 |
|
Establishment characteristics |
||
|
Goods-producing |
54 |
31 |
|
Service-producing |
35 |
30 |
|
1-99 workers |
28 |
19 |
|
100 workers or more |
53 |
44 |
|
SOURCE: Bureau of Labor Statistics (2004). |
||
Short-term disability programs are required by law in some states (e.g., New Jersey, New York).
Federal Social Security Administration programs Since 1974, the Supplemental Security Income (SSI) program has guaranteed a minimum level of income for needy aged, blind, or disabled individuals (SSA, 2004b). To be considered disabled, an individual must have a medically determinable physical or mental impairment that is expected to last (or has lasted) at least 12 continuous months or to result in death. For those aged 18 and older, the impairment must prevent him or her from doing any substantial gainful activity. The SSI program was designed to provide “assistance of last resort.” It is means-tested and takes into account all income and resources that an individual has or can obtain. Generally, SSI recipients are immediately eligible for Medicaid. The program includes work incentives that
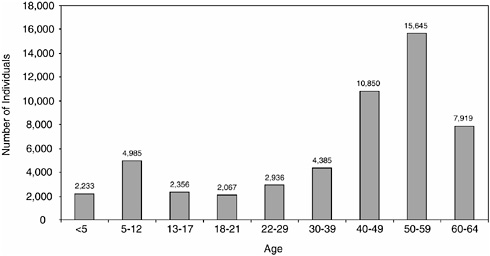
FIGURE 6-2 Number of SSI recipients eligible because of a cancer diagnosis, by age, December 2003. SOURCE: SSI Annual Statistical Report, 2003, Table 25 (SSA, 2004b).
enable recipients who are disabled to work and retain benefits and, in certain circumstances, extended Medicaid eligibility.
In December 2003, an estimated 53,376 individuals under age 65 were receiving SSI benefits because of a diagnosis of cancer. Cancer survivors represent only 1.1 percent of the total number of SSI recipients under age 65 (4.9 million) (Figure 6-2). Most SSI recipients under age 65 (58 percent) become eligible because of a mental disorder (SSA, 2004b). In December 2003, the average monthly federal SSI payment to beneficiaries with cancer was $404 (payment depends on income, and 45 states provide supplemental payments) (SSA, 2004b).
Social Security Disability Insurance (SSDI) is an insurance program that provides payments to persons with disabilities based on their history of Social Security-covered earnings. In contrast, the SSI program is a means-tested program that does not require prior participation in the labor force. The definition of disability and the process of determining disability are the same for both programs (IOM, 2002b). To be eligible, an individual must be unable to work at all, in any job, for at least 12 months or be in the terminal stages of illness. As of 2003, 160,986 disabled workers under age 65 were receiving SSDI payments because of cancer, representing 2.7 percent of all disabled workers receiving SSDI benefits (SSA, 2004a).
Summary: Employment Issues
It is difficult to gauge the extent of cancer-related employment problems, but recent evidence suggests that as many as 20 percent of survivors face work limitations 2 to 3 years after their diagnosis. Survivors appear to be most vulnerable in the immediate post-treatment period. A number of federal and state laws enacted in the 1990s provide some level of protection from employer discriminatory practices. However, these laws are not comprehensive and the courts continue to interpret the extent of protections provided to cancer survivors. A patchwork of educational, counseling, and referral sources is available. Unknown is whether cancer survivors are aware of their legal protections or of the services that are available to them. Limited financial assistance in the form of income replacement is available through the Social Security Administration to those who are poor and too disabled by cancer to work. Some individuals have some financial protection through short- and long-term disability programs, but these benefits tend to be offered by relatively few employers.
HEALTH INSURANCE
The Impact of Cancer on Health Insurance
Cancer care is very costly and represents one of the three most expensive conditions in the United States (Cohen and Krauss, 2003). Cancer-related medical expenditures in the United States totaled an estimated $48 billion in 2002 (AHRQ, 2004).11 Although most cancer-related expenditures are for initial treatment, expenditures for continuing care are not insubstantial, especially for those cancers with good prognoses (Figure 6-3).
Most Americans have health insurance that provides coverage for most cancer-related care. However, the lack of health insurance for 42 million Americans has serious negative consequences and economic costs not only for the uninsured themselves, but also for their families, the communities they live in, and the nation as a whole (Cohen and Martinez, 2005; IOM, 2004a). The uninsured do not receive the care they need; they suffer from poorer health, and are more likely to die early than are those with coverage. Aside from the health consequences, even one uninsured person in a family can put the financial stability and health of the whole family at risk. Furthermore, a community’s high uninsured rate can adversely affect the over-
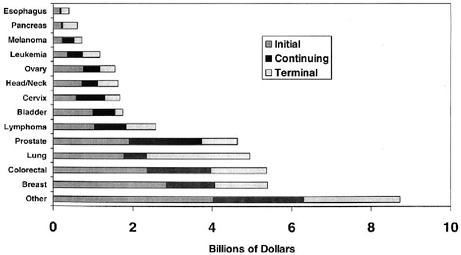
FIGURE 6-3 National U.S. Medicare expenditures in 1996 by cancer type and phase of care.
DATA SOURCE: SEER-Medicare database (Brown et al., 2002). Reprinted with permission from Lippincott, Williams & Wilkins. Brown ML, Riley GF, Schussler N, Etzioni R. 2002. Estimating health care costs related to cancer treatment from SEER-Medicare data. Med Care 40(8 Suppl):IV-104–IV-117.
all health status of the community and its health care institutions and providers, and the access of its residents to certain services. These are among the conclusions reached by the Institute of Medicine’s (IOM’s) Committee on the Consequences of Uninsurance in their 2004 report, Insuring America’s Health: Principles and Recommendations (IOM, 2004a).
Many studies link lack of health insurance with poor cancer outcomes (Ayanian et al., 1993; Lee-Feldstein et al., 2000; Ferrante et al., 2000; Roetzheim et al., 2000a,b; Penson et al., 2001; IOM, 2001, 2002a). Access to health insurance has been found to influence the amount and quality of health care received, which in turn is likely related to survival. Three-year relative cancer survival was markedly poorer for those without health insurance as compared to the insured, according to one state’s population-based study (Grann and Jacobson, 2003; McDavid et al., 2003). The link between insurance status and health outcomes is complex and confounded by socioeconomic status, race and ethnicity, and other factors. In one study, non-elderly cancer patients without insurance were found to be at risk for receiving inadequate cancer care, especially if they were Hispanic (Thorpe and Howard, 2003). Here, expenditures for uninsured patients under age 65 were nearly half (57 percent) that of privately insured patients over a 6-month period. Spending differences were believed to be due, in part or
completely, to differences in use, suggesting that raising coverage rates would improve cancer treatment. These findings are consistent with other studies of the chronically ill that have compared those with and without health insurance and found the uninsured lack needed physician care and prescription medicines (Families USA, 2001).
To overcome such health disparities, the IOM Committee on the Consequences of Uninsurance envisioned an approach to health insurance that would promote better overall health for individuals, families, communities, and the nation by providing financial access for everyone to necessary, appropriate, and effective health services. The committee articulated five principles to guide the extension of coverage (Box 6-9) and recommended that the President and Congress develop a strategy to achieve universal insurance coverage and to establish a firm and explicit schedule to reach this goal by 2010. Many plans to reform the nations’ health care insurance system have been proposed, and these principles are useful in assessing the relative merits of current proposals and in designing future strategies for extending coverage to everyone.
The IOM Committee on Cancer Survivorship agrees with the vision and implementation plan that has been put forth. Only through such an effort will cancer survivors, their families, and health care providers be able to fully focus on care and well-being without being burdened by financial worries. Although addressing national health care proposals to extend health insurance coverage to more Americans was not within the scope of the Committee on Cancer Survivorship’s work, the committee wishes to highlight in this report the serious consequences of lack of insurance coverage to cancer survivors, their families, and their caregivers. The actions recommended in the IOM’s insurance-focused work are endorsed by the Cancer Survivorship Committee.
|
BOX 6-9
SOURCE: IOM (2004a). |
TABLE 6-4 People Without Health Insurance Coverage by Age, United States, 2004
This section of the report begins with a description of the extent of the problem of lack of insurance coverage among cancer survivors and the limited remedies available to the uninsured who wish to gain health insurance coverage. Next, problems of cancer survivors with insurance are reviewed, including difficulties in maintaining health insurance coverage, gaining access to needed treatments and specialists, and paying health care out-of-pocket costs that stem from underinsurance (either due to insurance exclusions or benefit limits). In particular, the problem of paying for costly prescription medications is discussed. The limited number of programs to ameliorate financial hardships that result from uninsurance and underinsurance are described. Lastly, issues related to access to life insurance are briefly discussed.
As many as 15 percent of Americans lack health insurance (Table 6-4) and, for these individuals, cancer can be financially devastating. Among adults aged 45 to 64, an age when many develop cancer, 13 percent are uninsured. Adults aged 35 to 44 have even higher rates of being uninsured (18 percent). Vulnerability increases when measured over a longer timeframe. While 44 million Americans were uninsured in 2003, nearly twice that number, an estimated 84 million, were uninsured for at least 1 month over a 3-year period (Short et al., 2003). This, in part, reflects the dynamic nature of the population of the uninsured: About 2 million people become uninsured every month, while about the same number gain insurance (Short et al., 2003). Vulnerability also increases as health status declines. Research shows people in poor health are twice as likely to encounter a lengthy spell without health insurance compared to people in good health (Haley and Zuckerman, 2003).
The increase in the number of uninsured Americans in the past several years has been confined to adults, as public programs have expanded to offset the general decline in employer insurance for children. Among adults, loss of insurance can be traced to declines in employer-based insurance (DeNavas-Walt et al., 2004; Kaiser Family Foundation, 2004a). Employer-sponsored health insurance for retirees is also becoming less available, making it more difficult for survivors with significant health problems to retire early (American Benefits Council, 2004). Retirees are increasingly responsible for a larger share of the cost of their health care. Most uninsured adults had employer-based coverage prior to becoming uninsured. Several safety net laws and programs have been created to help people navigate coverage transitions and offer coverage to the uninsured. Although the protections offered by these laws and programs are important, they are incomplete. People with cancer can, and sometimes do, lose health insurance just when they need it most.
Much of the research that has documented insurance problems among cancer survivors was conducted prior to the enactment of laws to improve access to insurance coverage and protect consumers from some forms of discrimination. This literature documents instances of insurers refusing new applications, canceling or reducing policies, charging higher premiums, waiving or excluding preexisting conditions, or extending waiting periods for coverage (Kornblith, 1998; Guidry et al., 1998; Hoffman, 1999). Not much is known of the impact on contemporary cancer survivors of the relatively new federal and state laws that should facilitate obtaining and maintaining insurance coverage (Pollitz et al., 2000). What has been well documented are the very high costs associated with cancer and how such costs can serve as barriers to cancer care for both those with and those without health insurance (Guidry et al., 1998).
Cancer Survivors Who Are Uninsured
Virtually all (99 percent) cancer survivors aged 65 and older have health insurance coverage through the nation’s Medicare program.12 The problems the elderly have in coverage are discussed in the next section. With 39 percent of cancer survivors under age 65 and the potentially devastating impact of a cancer diagnosis on personal finances, the committee analyzed data from the National Health Interview Survey (NHIS) (2000 to 2003) to answer several questions about health insurance coverage among nonelderly cancer survivors (see Appendix 6A for details on the NHIS and the methods used to derive these estimates).
|
12 |
This estimate is based on staff analyses of the National Health Interview Survey described in Table 6-5. |
-
How many nonelderly cancer survivors lack health insurance? Among cancer survivors ages 25 to 64, 11 percent are uninsured (approximately 572,000 individuals) (Table 6-5).
-
Which groups of cancer survivors are less likely to be insured? Lacking health insurance is more common among younger survivors (ages 25 to 44) (19 percent) and Hispanic/Latino survivors (26 percent) (Table 6-5).
-
To what extent do nonelderly cancer survivors rely on public health insurance programs? An estimated 14 percent of non-elderly cancer survivors depend on Medicare or Medicaid for coverage. Lack of insurance and reliance on public insurance coverage increase with years since diagnosis. Rates of private insurance coverage are higher for survivors with breast and prostate cancer. This could reflect differences in age distribution (older individuals are more likely to have health insurance) or perhaps indicate that those with insurance are more likely to be screened and then survive their cancer (Table 6-5).
-
How does the health insurance status of cancer survivors compare to that of the general population and to individuals with other chronic illnesses? The uninsured rate among nonelderly cancer survivors is no higher than those seen in the general population (it is lower, 11.3 percent versus 16.3 percent). This may, in part, be explained by the older age distribution of cancer survivors and the general trend of increasing rates of insurance coverage with age (Table 6-4). It could also reflect greater efforts to maintain coverage by those with a chronic illness as compared to healthy individuals. Alternatively, it may be the case that individuals without health insurance and access to primary health care are not represented among cancer survivors (see Chapter 2). Lacking insurance is a problem of similar magnitude for cancer survivors (11.3 percent) and those with cardiovascular disease (12.1 percent) and diabetes (12.6 percent). People with other chronic conditions that are more prevalent in younger populations (e.g., diabetes) also exhibit higher coverage rates, however. This suggests people with chronic conditions may take on greater burdens and make more sacrifices, such as job lock, to get and keep coverage, compared to healthy individuals who can navigate insurance transitions with less difficulty and expense.
-
To what extent does a lack of insurance coverage impede cancer survivors’ access to care? Among cancer survivors ages 25 to 64 and without health insurance, many report access problems due to concerns about cost—51 percent (291,000 individuals) report delays in obtaining medical care; 44 percent (250,000 individuals) report not getting needed care; and 31 percent (178,000 individuals) report not getting needed prescription medicine. Similar consequences of a lack of coverage have been documented among those with other chronic illnesses (Tu, 2004).
TABLE 6-5 Health Insurance Status of Cancer Survivors Ages 25 to 64, by Selected Characteristics, 2000–2003
|
Characteristic |
Estimated Population |
|
|
In Millions |
% |
|
|
Total |
5.0 |
100.0 |
|
Age |
||
|
25–44 |
1.5 |
30.6 |
|
45–64 |
3.5 |
69.4 |
|
Sex |
||
|
Male |
1.5 |
29.8 |
|
Female |
3.5 |
70.2 |
|
Race/ethnicity |
||
|
White, non-Hispanic |
4.3 |
85.3 |
|
Hispanic |
0.3 |
5.2 |
|
Black, non-Hispanic |
0.4 |
7.1 |
|
Other |
0.1 |
2.3 |
|
Years since diagnosis |
||
|
<2 |
0.8 |
16.6 |
|
2–4 |
1.2 |
23.7 |
|
5–9 |
1.1 |
21.3 |
|
10–19 |
1.2 |
24.0 |
|
20+ |
0.7 |
14.5 |
|
Age at interview, age at diagnosis |
||
|
25–44, <45 |
1.5 |
30.7 |
|
45–64, <45 |
1.5 |
29.0 |
|
45–64, 45–64 |
2.0 |
40.3 |
|
Cancer type |
||
|
Female breast |
1.0 |
19.4 |
|
Female reproductivea |
1.5 |
29.7 |
|
Prostate |
0.2 |
4.7 |
|
Colorectal |
0.3 |
5.9 |
|
Other |
2.0 |
40.3 |
|
Has other chronic disease |
||
|
Yes |
1.8 |
35.1 |
|
No |
3.3 |
64.9 |
|
Self-reported health status |
||
|
Excellent/very good |
2.1 |
41.5 |
|
Good |
1.5 |
30.5 |
|
Fair/poor |
1.4 |
28.0 |
|
NOTE:—indicates too few cases for reliable estimate. The NHIS estimate of the number of cancer survivors ages 25 to 64 (5 million) is somewhat higher than that estimated from surveillance data (4 million). This could be explained if there is overreporting of a cancer history among those ages 25 to 64 and interviewed for the NHIS. |
||
|
Health Insurance Status (percentage distribution) |
||||
|
Medicare |
Medicaid |
Private |
Other Coverage |
Uninsured |
|
7.4 |
6.8 |
70.6 |
3.9 |
11.3 |
|
3.5 |
9.2 |
65.3 |
3.6 |
18.5 |
|
9.1 |
5.8 |
72.9 |
4.1 |
8.2 |
|
10.5 |
5.1 |
70.9 |
5.2 |
8.3 |
|
6.0 |
7.6 |
70.5 |
3.4 |
12.6 |
|
7.1 |
5.8 |
73.2 |
4.0 |
10.0 |
|
— |
10.2 |
56.4 |
— |
25.8 |
|
10.0 |
14.1 |
56.0 |
— |
15.0 |
|
— |
— |
52.5 |
— |
— |
|
— |
6.4 |
76.0 |
— |
7.9 |
|
6.3 |
6.5 |
75.2 |
— |
9.5 |
|
8.3 |
7.1 |
68.7 |
4.3 |
11.5 |
|
8.8 |
7.2 |
67.1 |
— |
13.1 |
|
7.6 |
7.1 |
66.3 |
— |
14.7 |
|
3.3 |
9.3 |
65.3 |
3.5 |
18.6 |
|
7.9 |
6.3 |
71.4 |
3.4 |
11.0 |
|
9.9 |
5.5 |
74.3 |
4.4 |
5.9 |
|
6.3 |
5.1 |
80.2 |
— |
5.4 |
|
4.9 |
10.6 |
61.8 |
4.0 |
18.7 |
|
— |
— |
80.0 |
— |
— |
|
— |
— |
72.0 |
— |
— |
|
9.4 |
5.5 |
71.1 |
3.8 |
10.2 |
|
15.2 |
11.2 |
56.2 |
5.3 |
12.1 |
|
3.1 |
4.5 |
78.3 |
3.2 |
10.9 |
|
— |
— |
84.2 |
2.6 |
10.2 |
|
4.0 |
5.6 |
74.6 |
3.7 |
12.1 |
|
20.1 |
15.9 |
45.6 |
6.2 |
12.1 |
|
aFemale reproductive cancer includes cancer of the cervix, uterus, and ovary. SOURCE: NHIS tabulations, committee staff. See Appendix 6A for a description of the NHIS and the methods used to derive these estimates. |
||||
These estimates of health insurance coverage among cancer survivors are based on a national survey and have limitations. First, the results pertain only to the adult civilian noninstitutionalized household population and not to cancer survivors who reside in institutions (e.g., hospices or nursing homes). The NHIS interviews rely on self-reports of cancer, and such reports tend to underestimate cancer prevalence (Hewitt et al., 1999; Desai et al., 2001). Furthermore, the survey is cross-sectional and does not capture the dynamic nature of insurance coverage status.
What are the options for the estimated 572,000 cancer survivors under age 65 who lack health insurance, but wish to obtain coverage? A safety net of sorts exists, but there are many barriers to coverage that is simultaneously available, affordable, and adequate.
Limited access to public insurance coverage Medicaid, the leading safety net program for health insurance coverage, is not available to millions of uninsured poor Americans. Only certain categories of people are eligible for Medicaid: children, parents of dependent children, pregnant women, the elderly, and the disabled. In many states, adults who fit one of these eligibility categories also must have income far below the federal poverty level in order to qualify for Medicaid coverage. If individuals are uninsured and have income above Medicaid eligibility levels, medical expenses related to cancer may force them to “spend down” to become eligible for Medicaid—that is, to deplete their assets until they meet income eligibility criteria. This option is not available in all states, however, and in states where there is a “spend-down” option, individuals still need to meet other eligibility categories (i.e., be a child, parent of a dependent child, disabled, or elderly). The Medicaid spend-down option, therefore, is far from a comprehensive safety net for the uninsured who are seriously ill. Those too disabled to work and under age 65 may qualify for Medicaid (if very poor and eligible for SSI disability benefits) or Medicare (if eligible for SSDI benefits, and disabled for a period of 2 years) (Kaiser Family Foundation, 2001, 2004e). For those who do qualify for Medicaid, coverage may be transient (i.e., change from month-to-month) so that once an individual’s condition improves, he or she may no longer qualify for Medicaid coverage. Furthermore, those who “spend down” their assets may only qualify for Medicaid in months with high medical expenses.
Some women who are uninsured and poor may become eligible for Medicaid if they are diagnosed with breast or cervical cancer through the Centers for Disease Control and Prevention (CDC) National Breast and Cervical Cancer Early Detection Program. Breast and cervical cancer screening is available to low-income, uninsured, and underserved women through this program. All states have also accepted the option, available since 2000, to provide Medicaid coverage for women diagnosed with cancer through
this program so that they have access to treatment (CDC, 2004; CMS, 2004b). Medicaid coverage is not limited to treatment of breast and cervical cancer. However, the coverage ends when a woman’s course of treatment is completed (CMS, 2004d). The scope and duration of Medicaid coverage under this program needs to be clarified because evidence suggests there is confusion about what services are covered and for how long (e.g., coverage of Tamoxifen therapy, which is typically prescribed for 5 years) (Kenny et al., 2004). In terms of access to this gateway for coverage for treatment, CDC’s early detection program is severely limited—the program reaches fewer than 15 percent of women who are eligible for screening by virtue of their income, age, and insurance status (CDC, 2005). In addition, once enrolled in Medicaid, women in some states may encounter other limits on covered benefits. In Texas, for example, Medicaid covers only three prescription drugs per month.
Limited access to private insurance Individuals who are uninsured, without access to group coverage, and not eligible for public programs may try to purchase private health insurance on an individual basis, but for those with a history of cancer, such coverage may be unavailable, very costly, or restrictive. Common circumstances that lead people to seek individually purchased health insurance include self-employment, early retirement, working part-time, divorce or widowhood, or “aging off” a parent’s policy (Pollitz et al., 2001). An estimated 17 million individuals had individually purchased health insurance coverage in 2002 (Williams and Fuchs, 2004). One in four adults have a need for individual health insurance at some point over a 3-year period (Duchon et al., 2001). The barriers to obtaining private individual coverage can be categorized as those of availability, affordability, and adequacy (referred to as “the three A’s”) (Box 6-10).
The three “A’s” barriers facing cancer survivors in the individual health insurance market are well illustrated by a study commissioned by the Kaiser Family Foundation. As part of this study, 19 insurance companies and health maintenance organizations (HMOs) in eight markets around the country were asked to consider for coverage (using rates in effect in 2000) hypothetical applicants with different health histories (Pollitz et al., 2001). One of the scenarios was for a 48-year-old, 7-year breast cancer survivor. Insurers reviewing the “applicants” determined whether or not they would be offered coverage and on what terms. The application made on behalf of the breast cancer survivor was rejected 43 percent of the time (i.e., in 26 of 60 applications filed for this case). Of the 34 offers of coverage received, 18 had limits on benefits covered. Most often the policies had riders excluding coverage for her treated breast, her implant, or cancer of any type. Eighteen offers imposed a premium surcharge, ranging from 40 to 100 percent (including 13 that were accompanied by some other benefit restriction). A
|
BOX 6-10 Availability barriers
Affordability barriers
Adequacy barriers
SOURCE: Pollitz (2004). |
unmodified offer for coverage was made only 18 percent of the time (11 of 60 applications). The average annual premium for this hypothetical applicant was $3,912, with a range from $1,464 to $16,344 per year.
In the 1990s, states enacted individual market reforms to make coverage more available and affordable, especially for higher risk people (Williams and Fuchs, 2004). New York, for example, requires all individual-market health insurance to be sold on a guaranteed-issue, community-rated basis—which means no resident can be turned down or charged more due to their health status, age, or gender (Pollitz et al., 2001; Georgetown University Health Policy Institute, 2004). Some states have also restricted the extent to which premium rates can vary based on health status and/or age. Florida law prohibits insurers from denying coverage or imposing exclusion riders based on breast cancer if treatment ended more than 2 years prior to application. Florida does not prohibit premium rate-ups for breast cancer survivors.
More than half of the states operate high-risk insurance pools to help provide coverage to individuals with serious medical conditions who have been denied private health insurance in the individual market (Achman and Chollet, 2001; Abbe, 2005). These risk pools, however, typically do not provide coverage that is available, affordable, and adequate (Box 6-11). Relatively few people are covered by state high-risk pools; 172,000 people as of 2003 (U.S. DHHS, 2003c), representing a very small share (2 percent) of individual market participants in those states. To improve access to such coverage, the federal government for the first time provided assistance to
|
BOX 6-11 Availability barriers
Affordability barriers
Adequacy barriers
SOURCE: Pollitz (2004). |
states in support of high-risk pools under the Trade Act of 2002. In 2002, $20 million was appropriated to help states create high-risk pools and $80 million was appropriated over 2 years to offset a portion of losses incurred by states from operating high-risk pools (U.S. DHHS, 2002, 2003a,b,c). These grant programs expired at the end of 2004. In the 109th Congress, legislation has been introduced to reauthorize $15 million in seed grants for fiscal years 2005 and 2006 for states launching high-risk insurance pools and to provide $75 million in grants for fiscal years 2005 through 2009 for states that currently operate high-risk pools (State High Risk, 2004, 2005; Kaiser Family Foundation, 2004c).
Comprehensive state reforms of the individual market that were made in the 1990s increased the availability of coverage for higher risk people, according to a recent assessment of their impact (Williams and Fuchs, 2004). However, while premiums for higher risk people decreased, coverage became less affordable, on average. States with comprehensive reforms experienced a decrease in coverage rates overall because people with lower risks left the market due to the higher price they faced for individual insurance, although coverage increased for people who were older and in poorer health. This problem might be alleviated if tax credits or other assistance to
individual buyers reduce the effective premium to the point where insurance remains attractive to low-risk people (Merlis, 2005).
Relatively little is known directly of the experience of individuals with a history of cancer who lack health insurance. A recent study in California of the uninsured population’s access to specialty care found the safety net to be inadequate (Felt-Lisk et al., 2004). Nearly one-third (32 percent) of medical directors of the state’s federally qualified health centers (FQHCs) in 2002–2003 indicated that uninsured patients have difficulty obtaining oncology care “often” or “always.” Obtaining neurology, endocrinology, and allergy/immunology care were much more problematic. One-half of the FQHC medical directors reported that access to specialty care in general had gotten worse in the past 2 years. Hospitals were found to be the major source of specialty care for the uninsured. That chronic symptoms or conditions were not well managed or treated on a timely basis were among the findings from focus groups held among uninsured individuals with a range of chronic conditions requiring specialty care services. In other research, community health centers were found to be able to provide primary care and other services to most of their uninsured patients, but were limited in their ability to provide diagnostic, specialty, and behavioral health services. Uninsured patients often failed to receive additional services for which they were referred (Gusmano et al., 2002).
Cancer Survivors with Health Insurance
Cancer survivors with health insurance coverage may have problems maintaining their coverage following a cancer diagnosis. In addition, those with coverage may find it is inadequate to pay for all of the care and services they need. Sometimes, it is unclear whether an insurance policy covers recommended treatments. For example, insurers may challenge claims for interventions designed to prevent or ameliorate late effects of cancer because of interpretations of what constitutes accepted and appropriate care. In some cases, states have mandated that insurers cover survivorship-related services such as breast prostheses and lymphedema therapy. Federal law mandates coverage for reconstructive surgery and these survivorship-related services in health plans that cover mastectomy.
Maintaining health insurance coverage For cancer survivors who lose their jobs, the federal law known as COBRA mandates that they can keep the health insurance they had through their employer for 18 months.13 Some
states have enacted “mini” COBRA laws similar to the federal law to provide individuals with extended coverage. Although the survivor, and not the former employer, must pay for the continued coverage, the rate may not exceed by more than 2 percent the rate set for the survivor’s former co-workers. Not all employees are aware of COBRA benefits and roughly one in five persons who are eligible for coverage claim it, although some studies suggest take-up is higher among individuals who are older and have health problems (Gruber and Madrian, 1993).
Many cancer survivors (and family members who hold the family’s health insurance policy) avoid changing jobs because they fear losing health insurance and other employment-related benefits. In one study, more than one-quarter (27 percent) of cancer survivors reported this sense of “job lock” (Short et al., 2005a). Congress tried to remedy this problem in 1996, enacting the Health Insurance Portability and Accountability Act (HIPAA)14 to improve the portability and continuity of health insurance coverage in private insurance markets and among employer-sponsored group health plans.
For people changing jobs, HIPAA added important protections. It prohibited employers and insurers from conditioning eligibility for health benefits on health status. In addition, it limited the imposition of preexisting condition exclusion periods and required credit to be given for continuous prior coverage. However, federal law does not require employers to offer health benefits nor, for the most part, does it require minimum standards for what must be covered under job-based health plans. As a result, cancer survivors who change jobs may still find the next job does not offer coverage, or offers a plan that does not cover all the health services and providers a cancer survivor may need.
HIPAA also limits the ability of insurers in the individual market to deny or limit coverage because of preexisting conditions such as cancer. This protection applies to people who are “HIPAA eligible,” that is, who have left job-based coverage, exhausted COBRA, and meet other requirements. However, the increased cost of premiums for portable insurance products and difficulties in implementing and enforcing the law have limited the value of these protections for consumers (GAO, 1997, 2000, 2001). Some of the limitations of HIPAA’s protections are outlined in Box 6-12.
|
|
more than 20 employees are required to make continued insurance coverage available to employees (and their covered spouses and dependents) who quit, are terminated, or work reduced hours. Coverage must extend to spouses and dependent children who would otherwise lose coverage due to the death, divorce, legal separation, or Medicare eligibility of a covered worker, and to children who attain the age of majority and lose dependent status. |
|
BOX 6-12 Availability barriers
Affordability barriers
Adequacy barriers
SOURCE: Pollitz (2004). |
Foremost among these is the HIPAA eligibility requirement that individuals have elected and exhausted COBRA benefits and the high costs associated with premiums.15
Inadequate health insurance coverage Consumer cost sharing has increased greatly in recent years, placing a larger financial burden on those with insurance. Employers are asking employees to pay more for health care through higher contributions and deductibles, lower subsidies for dependent coverage, and numerous benefit changes that increase spending at the point of care (Goff, 2004). Out-of-pocket spending for medical services increases with the number of chronic conditions a person has, and large out-of-pocket expenditures can limit access to care, affect health status and quality of life, and leave insufficient income for other necessities (Hwang et al., 2001).
According to analyses of the 2001–2002 Medical Expenditure Panel Survey (MEPS), health-related out-of-pocket expenditures made by those reporting health effects of cancer are high, averaging $1,267 annually for those ages 25 to 64 (13.5 percent of total expenditures) and $1,456 annually (12.5 percent of total expenditures) for those aged 65 and older (Figures 6-4 and 6-5) (see Appendix 6A for a description of MEPS and the
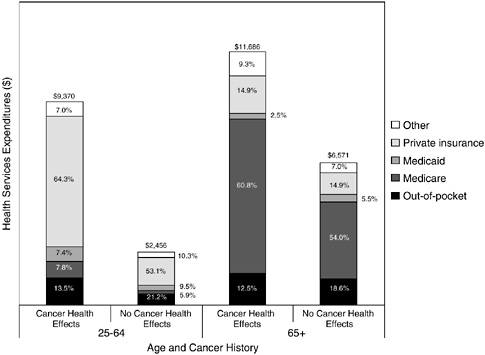
FIGURE 6-4 Sources of payment for health services expenditures among people reporting cancer-related health effects, by age, 2001–2002. The “cancer health effects” group does not necessarily include all cancer survivors; cancer survivors who do not experience adverse cancer-related health effects would not be included. Expenditures include both spending for care directly related to cancer and spending for other medical care unrelated to cancer (see Appendix 6A for a description of the Medical Expenditure Panel Survey and the methods used to derive these estimates).
SOURCE: Special tabulations of MEPS (Friedland, 2005).
methods used to derive these estimates). These expenditures are significantly higher than those made by individuals who do not report health effects of cancer ($520 among those ages 25 to 64 and $1,221 for those aged 65 and older) (Figure 6-5).
These expenditures represent a considerable burden, especially for those with low incomes. In 1998, health-related out-of-pocket spending among those with a cancer history represented 9 percent of income for those with an annual family income under $20,000 and about 1 percent for those with an annual family income of $55,000 or more (Center on an Aging Society, 2002).
The experiences of cancer survivors who are poor and privately insured are likely similar to individuals with other chronic illnesses. Between 2001
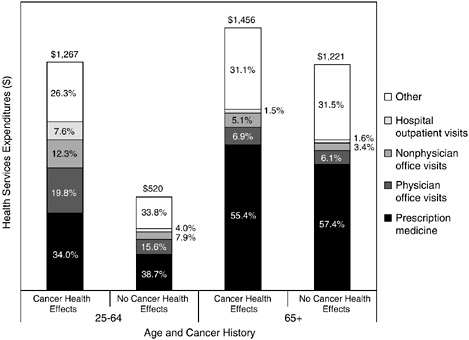
FIGURE 6-5 Average annual out-of-pocket expenditures among people reporting cancer-related health effects, by age, 2001–2002. The “cancer health effects” group does not necessarily include all cancer survivors; cancer survivors who do not experience adverse cancer-related health effects would not be included. Expenditures include both spending for care directly related to cancer and spending for other medical care unrelated to cancer (see Appendix 6A for a description of the Medical Expenditure Panel Survey and the methods used to derive these estimates).
SOURCE: Special tabulations of the Medical Expenditure Panel Survey (MEPS), Friedland (2005).
and 2003, the proportion of low-income, chronically ill people with private insurance who spent more than 5 percent of their income on out-of-pocket health care costs grew from 28 percent to 42 percent (Tu, 2004). In 2003, 12.3 million people aged 18–64 with chronic conditions,16 lived in families with problems paying medical bills (Tu, 2004). Among families with medical bill problems, nearly two-thirds report having difficulty paying for other basic necessities—rent, mortgage payments, transportation, or food—as a
result of medical debt (May and Cunningham, 2004). About half of the 1.5 million American families that filed for bankruptcy in 2001 did so because of medical costs and, among these, about 10 percent reported that the cost of cancer care bankrupted them (i.e., an estimated 75,000 individuals) (Himmelstein et al., 2005). A new bankruptcy law will make it more difficult for such individuals to regain their financial footing. Under the old law, people who filed for bankruptcy under Chapter 7 were allowed to erase their debt and start fresh. The new measure makes is less likely that debtors—particularly those who earn more than their state’s median income level—will qualify for Chapter 7. Instead, they will have to file under Chapter 13, which requires paying off some or all debt over a designated period of time (Fleck, 2005).
Some cancer survivors with health insurance lack coverage for needed care. In one study of the insurance experience of cancer survivors, 20 of 60 subjects reported that their insurer refused to pay for some aspect of care, including wigs, referrals, out-of-state consultations, antidepressant drugs, and basic supplies (Calhoun and Bennett, 2003). Cancer survivors may have coverage for a needed service (e.g., psychological counseling), but find that the specialists needed to deliver it, for example, a psychologist or social worker trained in oncology, may not be available within their plan’s network of providers (IOM, 2004b). Others may face financial hardship paying for services that are explicitly not covered by their policies. Of particular concern for cancer survivors are the costs of expensive drugs used as adjuvant therapies. In a study of men who had transferred from non-Veterans Affairs (VA) hospitals to the VA system for prostate care, the most common reason (reported by 35 percent of men) for transferring care was the high out-of-pocket costs associated with hormonal therapies, primarily oral nonsteroidal antiandrogens (Calhoun and Bennett, 2003).
Some types of coverage for services needed by cancer survivors are mandated by the federal government. The Women’s Health and Cancer Rights Act of 1998, for example, is a federal law that requires group health plans or health insurance issuers that cover mastectomies to pay for related services, including reconstruction and surgery to achieve symmetry between the breasts, prostheses, and management of complications resulting from a mastectomy (including lymphedema). This federal law covers those plans not currently covered by state law and sets a minimum standard for women in all states (ACS, 2001; CMS, 2004e).
Every state regulates policies sold by insurance companies in the state. These laws vary significantly. Some states require insurance policies to cover off-label chemotherapy, minimum hospital stays for cancer surgery, and benefits for certain types of cancer treatment and screening. Information on private insurers’ policies regarding coverage of post-treatment interventions of potential benefit to cancer survivors is scant. For services re-
lated to breast cancer care, 29 states had mandates for coverage of post-mastectomy prosthetic devices for women with breast cancer and 19 states had mandated coverage for post-mastectomy lymphedema therapy as of 2004 (NCI, 2004b). These state mandates, however, do not affect most individuals (54 percent) with employer-based private insurance because of their enrollment in self-insured plans.17 Such plans are not subject to state health insurance regulation, including regulation relating to mandated benefits and consumer protection (Claxton et al., 2004).
Health insurers have not yet made policies relating to certain cancer-related services of potential benefit to cancer survivors. For example, health insurance coverage of prophylactic mastectomy and oophorectomy varied in one study, with only 44 percent of private plans surveyed having specific policies for coverage of prophylactic mastectomy for patients with a strong family history of breast cancer and 20 percent having a policy for coverage of prophylactic oophorectomy under any clinical circumstance (Kuerer et al., 2000).
Medicare coverage issues The majority of cancer survivors are protected from some elements of insurance discrimination and financial burden because they have Medicare coverage by virtue of being aged 65 and older (61 percent of cancer survivors are aged 65 and older). Because of gaps in Medicare’s coverage, however, the elderly spent an estimated 22 percent of their income, on average, for health care services and premiums in 2003 (Caplan and Brangan, 2004). Most individuals covered by Medicare have supplemental insurance through employer-sponsored benefits, Medigap policies, or Medicaid (Kaiser Family Foundation, 2004e).18 Even with this extent of coverage, however, out-of-pocket expenditures are high. Elderly cancer survivors who report cancer-related health effects had out-of-pocket expenditures that were on average $1,456 as compared to $1,221 among the elderly not reporting cancer-related health effects in 2001–2002 (Figure 6-5). Much of the out-of-pocket expenditures were accounted for by prescription medications which, at the time, Medicare did not cover. Nonelderly cancer survivors face substantially greater incremental out-of-
pocket expenditures (either because many lack insurance or are underinsured, or because fewer people without cancer have other significant conditions).
In an assessment of 1995 expenditures among cancer survivors aged 70 and older, out-of-pocket spending represented roughly one-quarter of yearly income for those in the bottom income quartile (Langa et al., 2004). Insurance programs that fill Medicare’s gaps are important, but even those with supplemental coverage through Medigap policies and retiree health benefits can lack coverage for some out-of-pocket costs. Nearly one-quarter (23 percent) of Medicare beneficiaries, for example, own a Medigap policy, but only 7 percent of all beneficiaries had drug coverage from Medigap (Kaiser Family Foundation, 2004e).
Because so many cancer survivors have health insurance coverage through the federal Medicare program by virtue of their age, its coverage policies are of particular interest. Coverage may vary by the type of Medicare plan in which a survivor may be enrolled. Most Medicare beneficiaries’ care is provided through the traditional fee-for-service program. Only 11 percent of beneficiaries are covered by so-called “Senior Advantage Programs” that are managed care plans, primarily HMOs (Kaiser Family Foundation, 2004d). Medicare covers more than 41 million Americans: 35 million seniors and 6 million nonelderly people with disabilities. Medicare consists of four parts (Kaiser Family Foundation, 2004e):
-
Part A, the Hospital Insurance program, covers inpatient hospital, skilled nursing facility, hospice, and home health care.
-
Part B, Supplementary Medical Insurance, covers physician and outpatient hospital care, laboratory tests, medical supplies, and home health (the monthly Part B premium is $78.20 in 2005).
-
Part C refers to managed care plans, referred to as Medicare Advantage (formerly called Medicare+Choice).
-
Part D refers to the outpatient prescription drug benefit that will be fully implemented in 2006, enacted under the Medicare Prescription Drug, Improvement, and Modernization Act of 2003. The Congressional Budget Office estimates the average monthly Part D premium will be $35 in 2006, although premiums are expected to vary across plans.
The new prescription drug benefit provided by Medicare is of particular interest to cancer survivors because some of the recommended adjuvant and other therapies are extremely costly and currently not covered by Medicare (Marcus, 2004). For example, Tamoxifen, which is prescribed for many women with breast cancer for a period of 5 years following primary treatment, costs an estimated $1,642 annually. Gleevec, a recently approved drug that must be taken indefinitely to treat individuals with chronic myel-
TABLE 6-6 Annual Costs for Cancer Drugs Commonly Administered to Cancer Survivors
|
Disease |
Compound Name (Brand Name) Description of Drug |
Annual Estimated Retail Costa |
|
Breast cancer (Stages II to IV) |
Letrozole (Femara®) belongs to the family of drugs called nonsteroidal aromatase inhibitors. Letrozole is used to decrease estrogen production and suppress the growth of estrogen-dependent tumors. |
$2,843 |
|
|
Exemestane (Aromasin®) is used to decrease estrogen production and suppress the growth of estrogen-dependent tumors. |
$2,827 |
|
Anastrozole (Arimidex®) is a nonsteroidal aromatase inhibitor used to decrease estrogen production and suppress the growth of estrogen-dependent tumors. |
$2,700 |
|
|
Tamoxifen (Nolvadex®) belongs to the family of drugs called antiestrogens and blocks the effects of the hormone estrogen in the breast. It is used to treat breast cancer, and to prevent it in women who are at a high risk of developing breast cancer. |
$1,642 |
|
|
Toremifene (Fareston®) is an antiestrogen that may help control some cancers from growing, and it may delay or reduce the risk of cancer recurrence. |
$1,411 |
|
|
Cutaneous T cell lymphoma |
Bexarotene (Targretin®) is used to decrease the growth of some types of cancer cells. It belongs to the family of drugs called retinoids. Also called LGD1069. |
$61,320 |
|
Chronic myelogenous leukemia |
Imatinib Mesylate (Gleevec®) inhibits the growth of certain cancers by interfering with an enzyme controlling cell proliferation. Also called STI571. |
$45,952 |
|
Disease |
Compound Name (Brand Name) Description of Drug |
Annual Estimated Retail Costa |
|
Multiple myeloma |
Thalidomide (Thalomid®) belongs to the family of drugs called angiogenesis inhibitors. It prevents the growth of new blood vessels into a solid tumor. |
$24,098 |
|
Gastrointestinal stromal tumor |
Imatinib Mesylate (Gleevec®) inhibits the growth of certain cancers by interfering with a portion of the protein produced by the bcr/abl oncogene. Also called STI571. |
$45,952 |
|
NOTE: Descriptions of drugs adapted from NCI Cancer Dictionary (NCI, 2004a). aThe estimated annual retail cost is based on 100 percent of Average Wholesale Price (AWP) from the March 2004 Redbook for a typical dosage; actual retail price for an individual may be more or less. SOURCES: CMS (2004a). |
||
ogenous leukemia and gastrointestinal stromal tumors, costs $45,952 per year (Table 6-6). These estimates represent annual retail costs, and the extent to which individuals bear the cost depends largely on their insurance policy drug coverage. How Medicare pays for cancer drugs administered in physicians’ offices is a subject of great controversy. However, this report focuses on payment issues related primarily to commonly used oral drugs that are now excluded under Medicare’s traditional benefit (Part B). Oral and self-administered drugs have not been covered under Medicare and so the cost of many cancer survivors’ adjuvant therapy drugs has to be paid for through other means.
Until the Part D prescription drug benefit goes into effect in 2006, beneficiaries can sign up for a federally approved drug discount card, with some low-income beneficiaries receiving a $600 subsidy to help pay drug costs, although relatively few have done so. As of January 2006, beneficiaries will be able to opt for private Part D insurance coverage. Under the standard benefits of such plans, beneficiaries would pay (Kaiser Family Foundation, 2004e):
-
The first $250 in drug costs (annual deductible);
-
25 percent of total drug costs between $250 and $2,250;
-
100 percent of drug costs between $2,250 and $5,100 in total drug costs (the $2,850 gap or “hole in the doughnut”), equivalent to a $3,600 out-of-pocket limit; and
-
The greater of $2 for generics, $5 for brand drugs, or 5 percent co-insurance after reaching the $3,600 out-of-pocket limit ($5,100 catastrophic threshold).
More generous coverage will be available to those who are poor. About 14 million beneficiaries with limited assets and annual incomes would have 85 to 95 percent of their prescription drug costs covered under Medicare (Kaiser Family Foundation, 2004b,f). Part D premiums and deductibles are to be waived for beneficiaries who are eligible for both Medicare and Medicaid and would require copayments of $1 to $3 per prescription.
A pilot program announced in June 2004 provides prescription drug coverage to 500,000 Medicare beneficiaries with certain serious illnesses, including cancer, until 2006, when the Part D Medicare drug benefit will go into effect (CMS, 2004c). The program provides generous coverage for many of the oral drugs used by cancer survivors (the nine drugs described in Table 6-6 and altretamine [Hexalen] and gefitinib [Iressa]). As of mid-September 2004, fewer than 7,000 individuals had applied to participate in the program. The low levels of participation may be attributed to a lack of awareness of the program on the part of physicians and patients or difficulties in applying to the program (Kaiser Family Foundation, 2004a).
Managed care issues Many people receive care through a managed care plan offered either by a private insurer, Medicaid, or other provider (e.g., military services). Improved access to primary care and coordination of care are potential benefits of managed care plans. There are, however, potential disadvantages within managed care plans for adults with chronic illnesses who need specialized complex care. Under fee-for-service arrangements, individuals with chronic or disabling conditions generally are able to receive specialty care through tertiary care centers and specialty clinics, and from specialty providers. Fully capitated managed care plans may control the use of specialists, especially those outside of their plans’ networks. For example, there are anecdotal reports of insurers denying coverage for treatment of lymphedema because the plan does not include a certified lymphedema specialist (Parker-Pope, 2004).
Increasingly, mental health services are being provided by managed behavioral health organizations under separate contracts between the payor and a behavioral health provider. These so-called “carve-out” managed behavioral health care arrangements allow payors to isolate mental health services from overall insurance risk and have mental health care services managed separately from general health care. Some efforts have been made to reintegrate these carve-outs back into health plans in an effort to better coordinate medical and psychosocial care, but there are still hundreds of large corporations that have a behavioral health manager independent of
their health insurer (Lee, 2004). This separation is generally acceptable for physically healthy individuals. However, it is highly disadvantageous to patients with a life-threatening or chronic illness who require psychiatric/psychological consultation for related mental disorders. The separation of care delivery can lead to fragmentation of services across medical and behavioral health providers (IOM, 2004b).
Programs Providing Financial Assistance to Help Pay for Care and Other Services
Limited financial assistance is available through government, charitable, and other programs to those who cannot pay for their cancer-related care. These programs and services cannot substitute for adequate insurance coverage for cancer care, but they can ease the financial burden somewhat for small numbers of individuals in need.
A federal program called the Hill-Burton Free Care Program provides limited free or reduced-cost medical services through obligated facilities (mostly hospitals). In exchange for federal funds for construction and modernization, facilities agree to provide a reasonable volume of services to persons unable to pay. Applicants for assistance must meet income eligibility requirements, and assistance may be denied once a facility has given out its required amount of free care (HRSA, 2004).
Many charitable organizations provide free services, financial assistance, or information on getting financial aid to individuals with cancer who lack the means to pay for their care and related expenses:
-
The American Cancer Society offers services that can offset some patient costs. The volunteer-based Road to Recovery program, for example, provides transportation for breast cancer patients to and from medical appointments and treatments (ACS, 2004b). The ACS is building “Hope Lodges” near cancer centers where housing and transportation during treatment are available. The extent of ACS services varies from state to state. Not all units offer the same services.
-
CancerCare, a nonprofit, voluntary agency, provides, on a limited basis, financial assistance for treatment-related expenses (e.g., transportation, child care, home care, pain medication) (CancerCare, 2003).
-
The Leukemia and Lymphoma Society offers financial aid to patients who have leukemia, non-Hodgkin’s lymphoma, Hodgkin’s disease, or multiple myeloma.
-
AVONCares Program provides limited financial assistance for women with breast cancer for transportation, child care, and home care services (CancerCare, 2003).
-
Some states support care for the poor and uninsured. Maryland, for example, has a state-funded program (not Medicaid) that provides free treatment for low-income, uninsured women with breast cancer (Pollitz et al., 2004).
-
Sharing Hope, a program started by the advocacy organization Fertile Hope, offers cancer patients significant price reductions for sperm banking and egg or embryo freezing through participating reproductive service providers (Fertile Hope, 2005). The Lance Armstrong Foundation is providing funding for the administration of the Sharing Hope program.
Many pharmaceutical companies have patient assistance programs to help individuals with expensive prescription drugs. These programs have stringent eligibility requirements and do not provide comprehensive coverage. In addition, applications for assistance and renewals may be considered on a case-by-case basis and can be time consuming for physicians and their patients. Such programs are vital to cancer survivors; however, they are often limited because of the costly nature of the drugs prescribed for cancer survivors (Table 6-6). The ACS call center links people to pharmaceutical companies that provide financial assistance and helps them with the paperwork.
The National Coalition for Cancer Survivorship, in collaboration with the Oncology Nursing Society, Association of Oncology Social Work, and National Association of Social Workers, has developed a Cancer Survival Toolbox that addresses health insurance and financial resources (NCCS, 2004). The NCCS also publishes What Cancer Survivors Need to Know About Health Insurance, which describes types of health insurance, legal issues, and information sources (Calder and Pollitz, 2002). A number of other organizations provide comprehensive consumer information related to health insurance (CancerCare, 2003; ACS, 2004a).
The Patient Advocate Foundation is a national nonprofit organization that serves as a liaison between patients and their insurer, employer, and/or creditors to resolve insurance, job retention, and/or debt crisis matters relative to their diagnosis through case managers, doctors, and attorneys. Mediation is provided to assure access to care, maintenance of employment, and preservation of financial stability. The Foundation also provides financial assistance to patients who meet certain qualifications to help them pay for prescriptions and/or treatments. A search by state and type of service needed is available at its website (PAF, 2005).
In summary, very limited financial assistance is available to cancer survivors who are uninsured or underinsured. Evidence suggests such cancer survivors may be financially strained paying for needed care out of pocket, and may delay or forego needed care when they cannot pay. Some of the care provided to such individuals may be uncompensated care borne
by physicians and hospitals. The goal of anyone with a history of cancer is to use available means to gain access to health insurance. For the estimated 75,000 individuals facing bankruptcy as a result of cancer-related medical bills, a newly enacted bankruptcy law will make it more difficult for them to get out of debt.
LIFE INSURANCE
Obtaining life insurance coverage may be difficult for survivors of cancer. Because life insurance plans are based on an actuarial risk of death (or survival), the cancer history is often taken into account because it increases the potential risk of death at an earlier age (Lemaire et al., 2000). Some life insurance companies will not insure cancer survivors, and others will charge very high premiums. After 5 years without treatment, some survivors may qualify for standard rates (Lankford, 2002).
Group life insurance (through employment) is a possible solution because a health history is not usually required for such plans. Table 6-7 shows that in 2003, only half of workers in private industry have access to life insurance through their employer (Bureau of Labor Statistics, 2004). Those who have full-time employment are higher wage earners, and those working in large establishments were more likely to have access to life insurance at work.
FINDINGS AND RECOMMENDATIONS
Most working cancer patients require some kind of accommodation to work throughout treatment, and some experience difficulties at work after treatment. Estimates of the impact of cancer on employment vary, but one large recent study showed that one of five individuals who had worked at the time of diagnosis had cancer-related limitations in ability to work 1 to 5 years later. Half of those with limitations were unable to work at all. Cancer-related work limitations appear to be most pronounced in the first 6 months following diagnosis. Many individuals who leave work during treatment are able to return to work a year or two later. Cancer survivors whose jobs involve physical labor are especially likely to have difficulty returning to work following treatment for cancer.
All survivors are at risk of experiencing subtle, although not necessarily blatant, employment discrimination. Federal laws enacted in the 1990s have offered cancer survivors some protections from discriminatory practices such as firing or denial of benefits because of cancer. Such laws have clarified the responsibilities of employers to accommodate workers returning to work with health-related limitations. The most important of these laws, the ADA, continues to be interpreted by the courts and, while protec-
TABLE 6-7 Percentage of Workers with Access to Life Insurance Benefits, by Selected Characteristics, Private Industry, 2003
|
Characteristic |
Life Insurance |
|
All workers |
50 |
|
Worker characteristics |
|
|
White-collar occupations |
56 |
|
Blue-collar occupations |
53 |
|
Service occupations |
29 |
|
Full time |
62 |
|
Part time |
11 |
|
Union |
63 |
|
Nonunion |
49 |
|
Average wage <$15 per hour |
40 |
|
Average wage ≥$15 per hour |
65 |
|
Establishment characteristics |
|
|
Goods-producing |
61 |
|
Service-producing |
47 |
|
1-99 workers |
36 |
|
100 workers or more |
66 |
|
SOURCE: Bureau of Labor Statistics (2004). |
|
tions cover disabled cancer survivors, some survivors have not been fully protected from job loss and access to accommodations for cancer-related work limitations. Successful resolutions on the part of cancer survivors who have filed formal complaints against employers suggest that not all employers have yet fully complied with the law.
Opportunities exist for employers to assist cancer survivors through disability management and return-to-work programs. In addition, information and support can be provided to employees facing cancer through employer-sponsored health programs, workplace intranets, work-life programs, and employee assistance programs. Many employment-related services are available to cancer survivors through public and private voluntary and advocacy organizations, including education, counseling, support, legal advice, vocational rehabilitation, and referral. Limited financial assistance is available as income replacement for cancer survivors who have extended times away from work or who are disabled and can no longer
work. Resources available include private short- and long-term disability insurance, available to a minority of employees as a benefit of employment, and income support through the Social Security Administration to those who are disabled.
Recommendation 8: Employers, legal advocates, health care providers, sponsors of support services, and government agencies should act to eliminate discrimination and minimize adverse effects of cancer on employment, while supporting cancer survivors with short-term and long-term limitations in ability to work.
-
Cancer professionals, advocacy organizations, and the National Cancer Institute and other government agencies should continue to educate employers and the public about the successes achieved in cancer treatment, the improved prospects for survival, and the continuing productivity of most patients who are treated for cancer.
-
Public and private sponsors of services to support cancer survivors and their families should finance programs offering education, counseling, support, legal advice, vocational rehabilitation, and referral for survivors who want to work.
-
Providers who care for cancer survivors should become familiar with the employment rights that apply to survivors who want to work and make available information about employment rights and programs that provide counseling, legal services, and referral.
-
Providers should routinely ask patients who are cancer survivors if they have physical or mental health problems that are affecting their work, with the goal of improving symptoms and referring patients for rehabilitative and other services.
-
Employers should implement programs to assist cancer survivors. Examples include short- and long-term disability insurance, return-to-work programs, wellness programs, accommodation of special needs, and employee assistance programs.
-
Cancer survivors should tell their physicians when health problems are affecting them at work. Survivors should educate themselves about their employment rights and contact support organizations for assistance and referrals when needed.
The health insurance issues facing cancer survivors bring into sharp focus the gaps and limitations of health insurance in the United States. All Americans are at risk of becoming a cancer survivor and finding themselves without access to adequate and affordable health insurance. Cancer survivors, like other Americans with serious, chronic health conditions, face significant barriers to coverage because of their health status. In particular, access to individual health insurance may be denied to residents in many
states if they have a history of cancer. Cancer survivors may also face surcharged premiums for coverage because of their cancer history, depending on where they live and what type of coverage they seek. The improvements in the care of cancer survivors envisioned by the committee can not be achieved without health insurance that is accessible, adequate, and affordable.
Health insurance provides protection from the very high costs of cancer care. Most cancer survivors have health insurance through the federal Medicare program because they are aged 65 and older. Nevertheless, more than 4 million cancer survivors are under the age of 65. Eleven percent of cancer survivors ages 25 to 64 (approximately 572,000 individuals) are uninsured, and for these individuals, the costs of cancer care can be financially devastating. These younger uninsured cancer survivors report problems in access to care due to concerns about cost—51 percent report delays in obtaining medical care; 44 percent report not getting needed care; and 31 percent report not getting needed prescription medicine. The financial problems posed by cancer loom larger, because even those with health insurance can have trouble paying for prescription drugs and other types of care.
Some evidence indicates that individuals without health insurance have worse cancer outcomes because they receive less appropriate care. Even for those with health insurance, however, out-of-pocket expenditures for cancer care can be high. According to the committee’s analyses of the 2001–2002 Medical Expenditure Panel Survey, health-related out-of-pocket expenditures made by those reporting health effects of cancer are high, averaging $1,267 annually for those ages 25 to 64 (13.5 percent of total expenditures) and $1,456 annually (12.5 percent of total expenditures) for those aged 65 and older. These expenditures are significantly higher than those of individuals without a history of cancer.
Since 2000, most states have provided Medicaid coverage to poor and uninsured women who are diagnosed with breast or cervical cancer through the Centers for Disease Control and Prevention’s (CDC’s) state-based screening programs. Such coverage affords women treatment and follow-up services. The screening program currently serves only 15 percent of the low-income, uninsured women it is intended to serve, so this is not an avenue for many women to ultimately get coverage for their breast or cervical cancer.
State reforms of the individual health insurance market have improved access to coverage among those with chronic health conditions; however, there is evidence that the increased premiums have led some who had individual coverage to forego insurance. High-risk pools are available in most states as insurers of last resort for those ineligible for public or private insurance programs. However, costs of coverage are high and many have limited benefits. The federal government for the first time in 2002 has
provided support to assist states with the losses incurred by high-risk pool programs.
HIPAA and COBRA provide some assurance of continuation of insurance coverage if individuals move from one job to another. Cancer survivors, however, continue to have fears regarding maintenance of health insurance—more than one-quarter of survivors expressed concerns about job lock, according to a recent study of cancer survivors’ employment-related experiences.
Some benefits needed by cancer survivors have been mandated by the federal government or by states. Women who have had mastectomies, for example, are entitled to reconstruction, prostheses, and care for complications, including lymphedema. Many cancer survivors, however, lack coverage for oral adjuvant therapies that can be very expensive. Medicare’s prescription drug plan will go into effect in 2006 and provide some coverage for drugs currently not covered by the program (orally administered cancer drugs). Until then, a pilot program has provided generous prescription drug coverage to cancer survivors in need of these drugs. Relatively few cancer survivors, however, have signed up for this program.
Very limited direct financial assistance is available through the government or voluntary organizations to offset the high costs of cancer care for those who are uninsured or underinsured. The Hill-Burton Free Care Program provides some care, and voluntary organizations sometimes provide assistance for transportation, medicine, and medical supplies. Pharmaceutical companies have patient assistance programs to help individuals with prescription drug costs, but they provide limited assistance and the application process can be onerous. The goal for those without insurance is to gain access to it through available means, for example, through a high-risk insurance pool.
The IOM Committee on the Consequences of Uninsurance, in its 2004 report, Insuring America’s Health, recommended that the President and Congress develop a strategy to achieve universal insurance coverage and to establish a firm and explicit schedule to reach this goal by 2010 (IOM, 2004a). Only through such efforts will cancer survivors, their families, and health care providers be able to fully focus on care and well-being without being burdened by financial worries. Consistent with this goal, the IOM Committee on Cancer Survivorship recommends the following steps that can be taken between now and 2010 to strengthen health security for cancer survivors.
Recommendation 9: Federal and state policy makers should act to ensure that all cancer survivors have access to adequate and affordable health insurance. Insurers and payors of health care should recognize survivorship care as an essential part of cancer care and design benefits,
payment policies, and reimbursement mechanisms to facilitate coverage for evidence-based aspects of care.
Cancer survivors, like all Americans, may encounter spells when no health insurance is available to them. Most uninsured Americans are not eligible for job-based health benefits (even though the vast majority are in working families) or for Medicaid (even though the vast majority have low incomes). In addition, cancer survivors, like other Americans with serious, chronic health conditions, face other barriers to coverage because of their health status. In particular, access to individual health insurance may be denied to residents in many states if they have a history of cancer. Policy makers should act to ensure that cancer survivors and others with serious chronic health conditions can obtain health insurance that is adequate and affordable. For example, federal funding could support improvements in state high-risk pools—such as premium subsidies, lower cost-sharing options, expanded coverage for prescription drugs, and elimination of preexisting condition exclusion periods. This could help such programs better serve the needs of cancer survivors (as well as people with other serious and chronic health conditions). COBRA, HIPAA, and other programs that guarantee availability of coverage could also be expanded to include premium subsidies.
Because federal legislation generally covers only federal programs such as Medicare and Medicaid, many insurance reforms must be addressed at the state level. Health insurance reforms to expand access to individuals with chronic health conditions must be considered. Whether states pursue reforms through private markets, public programs, or some other means, the goal must be to ensure that all people have access to affordable, adequate health coverage, and furthermore, that the ability to obtain and maintain such coverage is not dependent on health status.
Policy makers can also improve other existing programs aimed at improving health insurance coverage of cancer survivors. In 2000, Congress established a new eligibility category option in Medicaid for uninsured women with breast and cervical cancer. However, only women screened through CDC-funded programs are eligible for this Medicaid coverage and CDC-funded programs today reach less than 15 percent of the program-eligible population. Policy makers could strengthen and build on this program first by ensuring that more eligible women with breast and cervical cancer are reached by it, and second by expanding screening services and Medicaid eligibility to include other cancer patients and survivors who have no other coverage options.
All health insurance in the United States—including Medicare, Medicaid, employer-sponsored group health plans, and individually purchased policies—should cover effective cancer survivorship care. National cover-
age standards should be promulgated for effective cancer survivorship care, and must include interventions for which there is good evidence of effectiveness (e.g., certain post-treatment surveillance strategies, treatments for late effects, management of symptoms, rehabilitative services). Importantly, coverage standards should include the development of a post-treatment survivorship care plan (see Chapter 3, Recommendation 2). National coverage standards should evolve with the development of clinical guidelines and evidence-based research into quality and effectiveness, and provide adequate reimbursement for quality care provided by cancer centers as well as specialists and primary care providers in communities. The application of cost-sharing requirements to cancer survivorship care must be limited so that financial barriers do not deter access to covered services. Congress has already taken preliminary steps to assure adequacy of some cancer survivorship care. The Women’s Health and Cancer Rights Act requires health insurance to cover reconstructive surgery, prostheses, and care for complications following mastectomy, including lymphedema. This model could be expanded to assure minimum federal standards for all cancer survivorship care under all health insurance.
APPENDIX 6A
DESCRIPTION OF THE NATIONAL HEALTH INTERVIEW SURVEY AND THE MEDICAL EXPENDITURE PANEL SURVEY AND THE METHODS USED TO DERIVE ESTIMATES OF INSURANCE COVERAGE AND MEDICAL EXPENDITURES PRESENTED IN THE CHAPTER
NATIONAL HEALTH INTERVIEW SURVEY (NHIS)
Information on the health insurance status of cancer survivors ages 25 to 64 is based on analyses of 4 years of NHIS data (2000 through 2003) (NCHS, 2002, 2003a,b, 2004). The NHIS is a multipurpose health survey conducted by the National Center for Health Statistics, Centers for Disease Control and Prevention. The NHIS is the principal source of information on the health of the civilian, noninstitutionalized, household population of the United States. Analyses were limited to the adult sample component of the survey. Sample sizes and response rates for the sample adult component are shown by year in Table 6A-1.
Computer-assisted personal interviews are conducted in the homes of respondents. The data collected in the NHIS are obtained through a complex sample design involving stratification, clustering, and multistage sampling. African Americans and Hispanics/Latinos are oversampled. All pro-
TABLE 6A-1 NHIS Sample Size and Response Rates, 2000–2003
|
Year |
Sample Size |
Response Rate (%) |
|
2000 |
32,374 |
72.1 |
|
2001 |
33,326 |
73.8 |
|
2002 |
31,044 |
74.3 |
|
2003 |
30,852 |
74.2 |
|
SOURCES: NCHS (2002, 2003a,b, 2004). |
||
portions and population counts (average annual) presented are weighted to provide national estimates.
History of cancer Respondents were asked “Have you ever been told by a doctor or other health professional that you had cancer or a malignancy of any kind?” If the respondent reports a history of cancer, he/she is asked the site of the cancer (the interviewer asked about 30 possible cancer sites) and the age when he/she was first diagnosed with that type of cancer (up to three cancer sites/types could be reported). In these analyses, cancer survivors include respondents who reported ever having a diagnosis of cancer, regardless of whether they had symptoms of cancer at the time of the survey. The current cancer status (i.e., active disease or remission) was not ascertained in the interview. A total of 3,150 sample adults ages 25 to 64 reported a history of cancer (excluding nonmelanoma skin cancers).
Insurance status Individuals with more than one type of insurance were coded as having coverage by Medicare, Medicaid, private, or other type of health insurance, in that order. Other coverage includes state-sponsored health plans, other government programs, and military coverage (includes VA, TRICARE, and CHAMP-VA). The uninsured are persons who did not report having health care coverage at the time of the interview under private health insurance (from employer or workplace, purchased directly, or through a state, local government, or community program), Medicare, Medicaid, Children’s Health Insurance Program, a state-sponsored health plan, other government programs, or military health plan.
Number of years since diagnosis Years since diagnosis was calculated from the reported age at interview and age at first diagnosis. When more than one cancer was reported, years since the first diagnosis (excluding superficial skin cancer) were used to calculate years since diagnosis. In a few instances, a correction was made for respondents who provided years since diagnosis instead of age at diagnosis.
MEDICAL EXPENDITURE PANEL SURVEY (MEPS)
Information on cancer-related medical expenditures is based on analyses of 2 years of data from MEPS, 2001–2002. MEPS is co-sponsored by the Agency for Healthcare Research and Quality (AHRQ) and the National Center for Health Statistics (AHRQ, 2005). The household component of MEPS is a nationally representative survey of the U.S. civilian noninstitutionalized population that collects medical expenditure data at both the person and household levels.
The sample for the household component of MEPS was selected from respondents to the NHIS. MEPS is a panel survey, and data are collected through a precontact interview that is followed by a series of five rounds of interviews over 2 years. Two calendar years of medical expenditure and utilization data are collected from each household and captured using computer-assisted personal interviewing.
A history of cancer is not directly asked about as part of MEPS. Instead, the respondent is asked, “We’re interested in learning about health problems that may have bothered you since [date].” A history of cancer would be identified if the respondent identified cancer as a condition that had bothered him or her during the reference period. A cancer history would also be identified if a person sought care for cancer, had a bed day or disability day attributable to cancer, or took a prescription medicine for cancer (Personal communication, K. Beauregard, AHRQ, March 2, 2005). Medical conditions reported during the interview were coded using International Classification of Disease, 9th Revision, Clinical Modification (ICD-9-CM) codes. For analyses presented in this chapter, individuals reporting superficial skin cancer were excluded. MEPS may not identify individuals with a history of cancer if they do not have symptoms, are not seeking care for cancer, or are not taking cancer-related prescription medicines.
Expenditures in MEPS refer to payments for health care services. These expenditures are defined as the sum of direct payments for care provided during the year, including out-of-pocket payments and payments by private insurance, Medicaid, Medicare, and other sources. Payments for over-the-counter drugs, alternative care services, and phone contacts with medical providers are not included in MEPS total expenditure estimates. Expenditure data are from a sample of medical and pharmaceutical providers that provided care and medicines to individuals interviewed for the survey. These data from providers are used to improve the overall quality of expenditure data.
In addition to expenditures for total health services, expenses are classified into eight broad types of services and equipment: hospital inpatient, emergency room, outpatient services, medical provider visits, prescribed medicines, dental services, home health services, and other medical equipment and services. These categories are described below:
Hospital inpatient services—This category includes room and board and all hospital diagnostic and laboratory expenses associated with the basic facility charge and payments for separately billed physician inpatient services.
Emergency room (ER) services—This category includes hospital diagnostic and laboratory expenses associated with the ER facility charge and payments for separately billed inpatient services.
Outpatient services—This category includes outpatient diagnostic and laboratory expenses associated with the basic facility charge and payments for separately billed inpatient services.
Medical provider visits—This category covers expenses for visits to a medical provider seen in an office-based setting.
Prescribed medicines—This category includes expenses for all prescribed medications that were initially purchased or otherwise obtained during the calendar year as well as any refills.
Dental services—This category covers expenses for any type of dental care provider, including general dentists, dental hygienists, dental technicians, dental surgeons, orthodontists, endodontists, and periodontists.
Home health services—This category includes expenses for care provided by home health agencies and independent home health providers. Agency providers accounted for most of the expenses in this category.
Other medical equipment and services—This category includes expenses for eyeglasses, contact lenses, ambulance services, orthopedic items, hearing devices, prostheses, bathroom aids, medical equipment, disposable supplies, and other miscellaneous items or services that were obtained, purchased, or rented during the year.
Source-of-Payment Categories
Estimates of sources of payment are classified as follows:
-
Out of pocket by user or family.
-
Private insurance—Includes payments made by insurance plans covering hospital and medical care (excluding payments from Medicare, Medicaid, and other public sources). Payments from Medigap plans or CHAMPUS and CHAMPVA (Armed Forces-related coverage) are included. Payments from plans that provide coverage for a single service only, such as dental or vision coverage, are not included.
-
Medicare—A federally financed health insurance plan for the elderly, persons receiving Social Security disability payments, and most persons with end-stage renal disease. Medicare Part A, which provides hospital insurance, is automatically given to those who are eligible for Social Secu-
-
rity. Medicare Part B provides supplementary medical insurance that pays for medical expenses and can be purchased for a monthly premium.
-
Medicaid—A means-tested government program jointly financed by federal and state funds that provides health care to those who are eligible. Program eligibility criteria vary significantly by state, but the program is designed to provide health coverage to families and individuals who are unable to afford necessary medical care.
-
Other public programs—Includes payments from the Department of Veterans Affairs (excluding CHAMPVA); other federal sources (Indian Health Service, military treatment facilities, and other care provided by the federal government); various state and local sources (community and neighborhood clinics, state and local health departments, and state programs other than Medicaid); and Medicaid payments reported for people who were not enrolled in the Medicaid program at any time during the year.
-
Other sources—Includes payments from Workers Compensation; other unclassified sources (automobile, homeowner’s, or liability insurance, and other miscellaneous or unknown sources); and other private insurance (any type of private insurance payments reported for people without private health insurance coverage during the year as defined in MEPS).
REFERENCES
ABA (American Bar Association). 2004. Breast Cancer Pro Bono Legal Referral Services. [Online]. Available: http://www.abanet.org/women/probono.html [accessed September 24, 2004].
Abbe B (CA, Inc.). 2005. Overview—State High Risk Health Insurance Pools Today. [Online]. Available: http://www.selfemployedcountry.org/riskpools/overview.html [accessed April 27, 2005].
Achman L, Chollet D (Mathematica Policy Research, Inc.). 2001. Insuring the Uninsurable: An Overview of State High-Risk Health Insurance Pools. New York, NY: Commonwealth Fund.
ACS (American Cancer Society). 2001. Women’s Health and Cancer Rights Act. [Online]. Available: http://www.cancer.org/docroot/MIT/content/MIT_3_2X.asp [accessed September 22, 2004].
ACS. 2004a. Financial Guidance for Cancer Survivors and Their Families: Off Treatment. Atlanta, GA: ACS.
ACS. 2004b. Reach to Recovery. [Online]. Available: http://www.cancer.org/docroot/ESN/content/ESN_3_1x_Reach_to_Recovery_5.asp?sitearea=SHR [accessed September 27, 2004].
AHRQ (Agency for Healthcare Research and Quality). 2004. Total Number of People Accounting for Expenditures (deduplicated) by Site of Service: United States, 2002. Medical Expenditure Panel Survey Household Component Data. [Online]. Available: http://www.meps.ahrq.gov/MEPSNet/TC/TC15.asp?File=HCFY2002&Table=HCFY2002_CNDXP [accessed March 1, 2005].
AHRQ. 2005. Overview of the MEPS Website. [Online]. Available: http://www.ahrq.gov/data/mepsweb.htm [accessed April 15, 2005].
Alter C. 2005 (January 27–29). ICAN: The Individual Cancer Assistance Network. Presentation at the Second Annual Meeting of the American Psychosocial Oncology Society, Phoenix, AZ.
American Benefits Council. 2004. Safe and Sound: A Ten-Year Plan for Promoting Personal Financial Security, An Employer Perspective. Washington, DC: American Benefits Council.
Ayanian JZ, Kohler BA, Abe T, Epstein AM. 1993. The relation between health insurance coverage and clinical outcomes among women with breast cancer. N Engl J Med 329(5):326–331.
Bar Association of San Francisco. 2004. Bar Association of San Francisco homepage. [Online]. Available: http://www.sfbar.org/ [accessed September 24, 2004].
Barnett A, Birnbaum H, Cremieux PY, Fendrick AM, Slavin M. 2000. The costs of cancer to a major employer in the United States: A case-control analysis. Am J Manag Care 6(11):1243–1251.
Blumklotz A, Lansky DJ. 2001. Health Care Communications for Employees With Chronic Conditions. Washington, DC: National Health Care Purchasing Institute.
Bordieri JE, Drehmer DE, Taricone PF. 1990. Personnel selection bias for job applicants with cancer. Journal of Applied Social Psychology 20(3):244–253.
Bradley C. 2004 (June 16–18). Labor Market Outcomes of Cancer Survivors. Presentation at the National Cancer Institute and American Cancer Society Meeting, Cancer Survivorship: Pathways to Health After Treatment, Washington, DC.
Bradley CJ, Bednarek HL. 2002. Employment patterns of long-term cancer survivors. Psychooncology 11(3):188–198.
Bradley CJ, Bednarek HL, Neumark D. 2002a. Breast cancer survival, work, and earnings. J Health Econ 21(5):757–779.
Bradley CJ, Bednarek HL, Neumark D. 2002b. Breast cancer and women’s labor supply. Health Serv Res 37(5):1309–1328.
Bradley CJ, Neumark D, Bednarek HL, Schenk M. 2005a. Short-term effects of breast cancer on labor market attachment: Results from a longitudinal study. J Health Econ 24(1):137–160.
Bradley CJ, Neumark D, Luo Z, Bednarek HL, Schenk M. 2005b. Employment outcomes of men treated for prostate cancer. J Natl Cancer Inst 97(13):958–965.
Bristol-Myers Squibb. 2004. Creating a Legacy of Hope: Corporate Social Responsibility at Bristol-Myers Squibb. New York, NY: Bristol-Myers Squibb.
Brown HG, Ming TS. 1992. Vocational rehabilitation of cancer patients. Semin Oncol Nurs 8(3):202–211.
Brown ML, Riley GF, Schussler N, Etzioni R. 2002. Estimating health care costs related to cancer treatment from SEER-Medicare data. Med Care 40(8 Suppl): IV-104–IV-117.
Bruyere SM. 2000. Disability Employment Policies and Practices in Private and Federal Sector Organizations. Ithaca, NY: Cornell University.
Bureau of Labor Statistics. 2004. National Compensation Survey: Employee Benefits in Private Industry in the United States, March 2004. Washington, DC: U.S. Department of Labor.
Bureau of Labor Statistics. 2005. Private industry by supersector and size of establishment: Establishments and employment, first quarter 2003, by State. [Online]. Available: http://www.bls.gov/cew/ew03table4.pdf [accessed July 18, 2005].
Calder KJ, Pollitz K. 2002. What Cancer Survivors Need to Know About Health Insurance. Silver Spring, MD: National Coalition for Cancer Survivorship.
Calhoun EA, Bennett CL. 2003. Evaluating the total costs of cancer. The Northwestern University Costs of Cancer Program. Oncology (Huntingt) 17(1):109–114; discussion 119–121.
CancerCare. 2003. Financial Needs: CancerCare’s Financial Assistance Programs. [Online]. Available: http://www.cancercare.org/FinancialNeeds/FinancialNeedsList.cfm?c=387 [accessed September 19, 2004].
CancerCare. 2004. Cancer in the Workplace. [Online]. Available: http://www.cancercare.org/TelephoneEducationWorkshopArchive/TelephoneEducationWorkshopArchiveList.cfm?c=408 [accessed September 23, 2004].
CancerCare. 2005. CancerCare homepage. [Online]. Available: http://www.cancercare.org [accessed May 11, 2005].
Caplan C, Brangan N. 2004. Out-of-Pocket Spending on Health Care by Medicare Beneficiaries Age 65 and Older in 2003. Public Policy Institute Data Digest. Washington, DC: AARP Public Policy Institute.
CDC (Centers for Disease Control and Prevention). 2004. Breast and Cervical Cancer Prevention and Treatment Act of 2000. [Online]. Available: http://www.cdc.gov/cancer/nbccedp/law106-354.htm [accessed September 22, 2004].
CDC. 2005. NBCCEDP Screening Program Summaries. [Online]. Available: http://www.cdc.gov/cancer/nbccedp/sps/index.htm#2 [accessed April 26, 2005].
Center on an Aging Society. 2002. Cancer: A major national concern. Challenges for the 21st Century: Chronic and Disabling Conditions Series. No. 4. Washington, DC: Georgetown University.
Center on an Aging Society. 2004. Workers affected by chronic conditions: How can workplace policies and programs help? Challenges for the 21st Century: Chronic and Disabling Conditions Series. No. 7. Washington, DC: Georgetown University.
Chirikos TN. 2001. Economic impact of the growing population of breast cancer survivors. Cancer Control 8(2):177–183.
Chirikos TN, Russell-Jacobs A, Cantor AB. 2002a. Indirect economic effects of long-term breast cancer survival. Cancer Pract 10(5):248–255.
Chirikos TN, Russell-Jacobs A, Jacobsen PB. 2002b. Functional impairment and the economic consequences of female breast cancer. Women Health 36(1):1–20.
Claxton G, Gil I, Finder B, Holve E, Gabel J, Pickreign J, Whitmore H, Hawkins S, Fahlman C. 2004. Employer Health Benefits 2004 Annual Survey. Menlo Park, CA and Chicago, IL: Henry J. Kaiser Family Foundation and Health Research and Educational Trust.
CMS (Centers for Medicare and Medicaid Services). 2004a. Beneficiary Fact Sheet (External Use). [Online]. Available: http://www.cms.hhs.gov/researchers/demos/FctSht_Benefic_REVISED_COSTS_070104.pdf [accessed May 10, 2005].
CMS. 2004b. Breast and Cervical Cancer Prevention and Treatment Activity Map. [Online]. Available: http://www.cms.hhs.gov/bccpt/bccptmap.asp [accessed February 17, 2005].
CMS. 2004c. The Medicare Replacement Drug Demonstration. [Online]. Available: http://www.cms.hhs.gov/researchers/demos/drugcoveragedemo.asp [accessed September 24, 2004].
CMS. 2004d. SHO Letter. [Online]. Available: http://www.cms.hhs.gov/states/letters/sho01041.asp [accessed February 17, 2005].
CMS. 2004e. The Women’s Health and Cancer Rights Act. [Online]. Available: http://www.cms.hhs.gov/hipaa/hipaa1/content/whcra.asp [accessed September 22, 2004].
Cohen JW, Krauss NA. 2003. Spending and service use among people with the fifteen most costly medical conditions, 1997. Health Aff (Millwood) 22(2):129–138.
Cohen RA, Martinez ME. 2005. Health Insurance Coverage: Estimates from the National Health Interview Survey, 2004. [Online]. Available: http://www.cdc.gov/nchs/nhis.htm [accessed July 19, 2005].
Conti JV. 1990. Cancer rehabilitation: Why can’t we get out of first gear? Journal of Rehabilitation 56(4):19–22.
de Lima M, Strom SS, Keating M, Kantarjian H, Pierce S, O’Brien S, Freireich E, Estey E. 1997. Implications of potential cure in acute myelogenous leukemia: Development of subsequent cancer and return to work. Blood 90(12):4719–4724.
DeNavas-Walt C, Proctor BD, Mills RJ (U.S. Census Bureau). 2004. Income, Poverty, and Health Insurance Coverage in the United States: 2003. Current Population Reports, Pp. 60–226. Washington, DC: U.S. Census Bureau.
Desai MM, Bruce ML, Desai RA, Druss BG. 2001. Validity of self-reported cancer history: A comparison of health interview data and cancer registry records. Am J Epidemiol 153(3):299–306.
Duchon L, Schoen C, Doty MM, Davis K, Strumpf E, Bruegman S. 2001. Security Matters: How Instability in Health Insurance Puts U.S. Workers at Risk . Washington, DC: The Commonwealth Fund.
EEOC (U.S. Equal Employment Opportunity Commission). 2004a. Americans with Disabilities Act of 1990 (ADA) Charges FY 1992–FY 2003. [Online]. Available: http://www.eeoc.gov/stats/ada-charges.html [accessed June 1, 2004].
EEOC. 2004b. Disability Discrimination. [Online]. Available: http://www.eeoc.gov/types/ada.html [accessed June 1, 2004].
Employee Assistance Professionals Organization. 2004. Employee Assistance Professionals Organization. [Online]. Available: http://www.eapassn.org [accessed September 20, 2004].
Families USA. 2001. Getting Less Care: The Uninsured With Chronic Health Conditions. Washington, DC: Families USA.
Felt-Lisk S, McHugh M, Thomas M. 2004. Examining Access to Specialty Care for California’s Uninsured: Full Report. Oakland, CA: California HealthCare Foundation.
Ferrante JM, Gonzalez EC, Roetzheim RG, Pal N, Woodard L. 2000. Clinical and demographic predictors of late-stage cervical cancer. Arch Fam Med 9(5):439–445.
Fertile Hope. 2005. Financial Assistance. [Online]. Available: http://www.fertilehope.org/resources/assistance.cfm [accessed February 20, 2005].
Fesko SL. 2001. Workplace experiences of individuals who are HIV+ and individuals with cancer. Rehabil Couns Bull 45(1):2–11.
Fleck C. 2005. Throw me a lifeline: The new bankruptcy law could sink families with big medical bills. AARP Bulletin (May):28.
Friedland R (Georgetown Center on an Aging Society). 2005. Special analysis of the Medical Expenditure Panel Survey (MEPS). Commissioned by the IOM Committee on Cancer Survivorship. Unpublished.
FWI (Families and Work Institute). 1998. Business Work-Life Study. [Online]. Available: http://www.familiesandwork.org/summary/worklife.pdf [accessed April 27, 2005].
GAO (General Accounting Office). 1997. The Health Insurance Portability and Accountability Act of 1996: Early Implementation Concerns. Washington, DC: GAO.
GAO. 2000. Implementation of HIPAA: Progress Slow in Enforcing Federal Standards in Nonconforming States. Washington, DC: GAO.
GAO. 2001. Private Health Insurance: Federal Role in Enforcing New Standards Continues to Evolve. Washington, DC: GAO.
Georgetown University Health Policy Institute. 2004. Summary of Key Consumer Protections in Individual Health Insurance Markets. Washington, DC: Georgetown University.
Goetzel RZ, Hawkins K, Ozminkowski RJ, Wang S. 2003. The health and productivity cost burden of the “top 10” physical and mental health conditions affecting six large U.S. employers in 1999. J Occup Environ Med 45(1):5–14.
Goff V. 2004. Consumer Cost Sharing in Private Health Insurance: On the Threshold of Change. NHPF Issue Brief No. 798. Washington, DC: National Health Policy Forum.
Good Health for Life. 2004. Good Health for Life homepage. [Online]. Available: http://www.ghfl.org/ [accessed September 20, 2004].
Grann VR, Jacobson JS. 2003. Health insurance and cancer survival. Arch Intern Med 163(18):2123–2124.
Gruber J, Madrian BC. 1993. Health Insurance and Early Retirement: Evidence From the Availability of Continuation Coverage. NBER Working Paper Series, Working Paper No. 4594. Cambridge, MA: National Bureau of Economic Research.
Guidry JJ, Aday LA, Zhang D, Winn RJ. 1998. Cost considerations as potential barriers to cancer treatment. Cancer Pract 6(3):182–187.
Gusmano MK, Fairbrother G, Park H. 2002. Exploring the limits of the safety net: Community health centers and care for the uninsured. Health Aff (Millwood) 21(6):188–194.
Haley J, Zuckerman S. 2003. Is Lack of Coverage a Short- or Long-Term Condition? Report to the Kaiser Family Foundation Commission on Medicaid and the Uninsured. Washington, DC: Kaiser Family Foundation.
Hewitt M, Breen N, Devesa S. 1999. Cancer prevalence and survivorship issues: Analyses of the 1992 National Health Interview Survey. J Natl Cancer Inst 91(17):1480–1486.
Hewitt M, Rowland JH, Yancik R. 2003. Cancer survivors in the United States: Age, health, and disability. J Gerontol A Biol Sci Med Sci 58(1):82–91.
Himmelstein DU, Warren E, Thorne D, Woolhandler S. 2005. MarketWatch: Illness and injury as contributors to bankruptcy. Health Aff (Millwood) [Online]. Available: http://content.healthaffairs.org/cgi/reprint/hlthaff.w5.63v1?maxtoshow=&HITS=10&hits=10&RESULTFORMAT=&author1=himmelstein&fulltext=bankruptcy&andorexactfulltext=and&searchid=1121117324126_3699&stored_search=&FIRSTINDEX=0&resourcetype=1&journalcode=healtha [accessed July 11, 2005].
Hoffman B. 1989. Cancer survivors at work: Job problems and illegal discrimination. Oncol Nurs Forum 16(1):39–43.
Hoffman B. 1991. Employment discrimination: Another hurdle for cancer survivors. Cancer Invest 9(5):589–595.
Hoffman B. 1999. Cancer survivors’ employment and insurance rights: A primer for oncologists. Oncology (Huntingt) 13(6):841–846; discussion 846, 849, 852.
Hoffman B. 2000. Between a disability and a hard place: The cancer survivors’ Catch-22 of proving disability status under the Americans with Disabilities Act. Maryland Law Review 59(2):352–439.
Hoffman B. 2002. Policy Recommendations to Address the Employment and Insurance Concerns of Cancer Survivors. Background paper commissioned by the IOM. Unpublished.
Hoffman B. 2004a. A Cancer Survivor’s Almanac: Charting Your Journey. 3rd ed. Hoboken, NJ: John Wiley & Sons.
Hoffman B. 2004b. Working it out: Your employment rights. In: Hoffman B, ed. A Cancer Survivor’s Almanac: Charting Your Journey. 3rd ed. Hoboken, NJ: John Wiley & Sons. Pp. 242–269.
HRSA (Health Resources and Services Administration). 2004. Health Resources and Services Administration homepage. [Online]. Available: http://www.hrsa.gov [accessed September 22, 2004].
Hwang W, Weller W, Ireys H, Anderson G. 2001. Out-of-pocket medical spending for care of chronic conditions. Health Aff (Millwood) 20(6):267–278.
IOM (Institute of Medicine). 2001. Coverage Matters: Insurance and Health Care. Washington, DC: National Academy Press.
IOM. 2002a. Care Without Coverage: Too Little, Too Late. Washington, DC: The National Academies Press.
IOM. 2002b. The Dynamics of Disability: Measuring and Monitoring Disability for Social Security Programs. Wunderlich GS, Rice DP, Amado NL, eds. Washington, DC: The National Academies Press.
IOM. 2004a. Insuring America’s Health: Principles and Recommendations. Washington, DC: The National Academies Press.
IOM. 2004b. Meeting Psychosocial Needs of Women with Breast Cancer. Hewitt M, Herdman R, Holland J, eds. Washington, DC: The National Academies Press.
Kaiser Family Foundation. 2001. Medicaid’s Role for the Disabled Population Under Age 65. Washington, DC: Kaiser Family Foundation.
Kaiser Family Foundation. 2004a. The Economic Downturn and Changes in Health Insurance Coverage, 2000–2003 [Online]. Available at: http://www.kff.org/uninsured/7174.cfm (accessed July 11, 2005).
Kaiser Family Foundation. 2004b. Kaiser Daily Health Policy Report: Bush Administration Releases Proposed Rules for Medicare Prescription Drug Benefit. [Online]. Available: http://www.kaisernetwork.org/daily_reports/rep_index.cfm?DR_ID=24978 [accessed July 27, 2004].
Kaiser Family Foundation. 2004c. Kaiser Daily Health Policy Report: Senate Committee Approves Bill to Help States Create High-Risk Health Insurance Pools. [Online]. Available: http://www.kaisernetwork.org/daily_reports/print_report.cfm?DR_ID=25896&dr_cat+3 [accessed September 23, 2004].
Kaiser Family Foundation. 2004d. Medicare Advantage Fact Sheet. Menlo Park, CA: Kaiser Family Foundation.
Kaiser Family Foundation. 2004e. Medicare at a Glance Fact Sheet. Menlo Park, CA: Kaiser Family Foundation.
Kaiser Family Foundation. 2004f. The Medicare Prescription Drug Law Fact Sheet. Menlo Park, CA: Kaiser Family Foundation.
Kenny KA, Blake SC, Maloy K, Ranji UR, Salganicoff A (George Washington University School of Public Health and Health Services and the Henry J. Kaiser Family Foundation). 2004. Hearing Their Voices: Lessons From the Breast and Cervical Cancer Prevention and Treatment Act. Menlo Park, CA: Kaiser Family Foundation.
Kessler RC, Greenberg PE, Mickelson KD, Meneades LM, Wang PS. 2001. The effects of chronic medical conditions on work loss and work cutback. J Occup Environ Med 43(3):218–225.
Kornblith AB. 1998. Psychosocial adaptation of cancer survivors. In: Holland JC, ed. Psycho-Oncology. New York, NY: Oxford University Press.
Kuerer HM, Hwang ES, Anthony JP, Dudley RA, Crawford B, Aubry WM, Esserman LJ. 2000. Current national health insurance coverage policies for breast and ovarian cancer prophylactic surgery. Ann Surg Oncol 7(5):325–332.
LAF (Lance Armstrong Foundation). 2004. LiveStrong. [Online]. Available: http://www.livestrong.org [accessed September 20, 2004].
Langa KM, Fendrick AM, Chernew ME, Kabeto MU, Paisley KL, Hayman JA. 2004. Out-of-pocket health-care expenditures among older Americans with cancer. Value Health 7(2):186–194.
Lankford K. 2002. Covering a Survivor. Kiplinger’s Personal Finance 56(3):108.
Laris M. 2005a (January 10). Loudoun teacher with cancer forced out. The Washington Post. P. B3.
Laris M. 2005b (January 13). Teacher with cancer is offered her job back. The Washington Post. P. B1.
Lee FC. 2004. Employer-based disease management programs in cancer. Dis Manage Health Outcomes 12(1):9–17.
Lee-Feldstein A, Feldstein PJ, Buchmueller T, Katterhagen G. 2000. The relationship of HMOs, health insurance, and delivery systems to breast cancer outcomes. Med Care 38(7):705–718.
Legal Information Network for Cancer. 2004. LINC homepage. [Online]. Available: http://www.cancerlinc.org/ [accessed September 24, 2004].
Lemaire J, Subramanian K, Armstrong K, Asch DA. 2000. Pricing term insurance in the presence of a family history of breast or ovarian cancer. North American Actuarial Journal 4(2):75–87.
Loy B, Batiste LC. 2004. Accommodating People with Cancer. [Online]. Available: http://www.jan.wvu.edu/media/Cancer.html [accessed June 1, 2004].
Marcus AD. 2004 (September 7). Price becomes factor in cancer treatment. The Wall Street Journal. P. D1.
May JH, Cunningham PJ. 2004. Tough Trade-Offs: Medical Bills, Family Finances, and Access to Care. Issue Brief No. 85. Washington, DC: Center for Studying Health System Change.
McDavid K, Tucker TC, Sloggett A, Coleman MP. 2003. Cancer survival in Kentucky and health insurance coverage. Arch Intern Med 163(18):2135–2144.
Mellette SJ. 1985. The cancer patient at work. CA Cancer J Clin 35(6):360–373.
Merlis M. 2005. Fundamentals of Underwriting in the Nongroup Health Insurance Market: Access to Coverage and Options for Reform. NHPF Background Paper. Washington, DC: National Health Policy Forum.
Messner C, Patterson D. 2001. The challenge of cancer in the workplace. Cancer Pract 9(1):50–51.
Mundy RR, Moore SC, Mundy GD. 1992. A missing link: Rehabilitation counseling for persons with cancer. Journal of Rehabilitation 58(2):47–49.
NCCS (National Coalition for Cancer Survivorship). 2004. Cancer Survival Toolbox. Silver Spring, MD: NCCS.
NCCS and Amgen. Undated. Cancer in the Workplace Survey Highlights. Silver Spring, MD: NCCS.
NCHS (National Center for Health Statistics). 2002. 2000 National Health Interview Survey (NHIS) Public Use Data Release. Hyattsville, MD: NCHS.
NCHS. 2003a. 2001 National Health Interview Survey (NHIS) Public Use Data Release. Hyattsville, MD: NCHS.
NCHS. 2003b. 2002 National Health Interview Survey (NHIS) Public Use Data Release. Hyattsville, MD: NCHS.
NCHS. 2004. 2003 National Health Interview Survey (NHIS) Public Use Data Release. Hyattsville, MD: NCHS.
NCI. 2002. Facing Forward: Life After Cancer Treatment. Bethesda, MD. NCI.
NCI (National Cancer Institute). 2004a. Dictionary of Cancer Terms. [Online]. Available: http://www.nci.nih.gov/templates/db_alpha.aspx?expand=A [accessed September 24, 2004].
NCI. 2004b. Fact Sheet: Breast Cancer. Bethesda, MD. NCI.
NCI. 2005. Estimated U.S. Cancer Prevalence. [Online]. Available: http://cancercontrol.cancer.gov/ocs/prevalence/prevalence.html [accessed July 29, 2005].
NCSL (National Conference of State Legislatures). 2005. State Genetics Employment Laws. [Online]. Available: http://www.ncsl.org/programs/health/genetics/ndiscrim.htm [accessed June 15, 2005].
New York Legal Assistance Group. 2004. NYLAG homepage. [Online]. Available: http://nylag.org/ [accessed September 24, 2004].
PAF (Patient Advocate Foundation). 2005. Report Search. [Online]. Available: http://www.patientadvocate.org/report.php [accessed February 20, 2005].
Parker-Pope T. 2004 (June 1). Efforts mount to combat lymphedema, a devastating side effect of cancer care. The Wall Street Journal. P. D1.
Penson DF, Stoddard ML, Pasta DJ, Lubeck DP, Flanders SC, Litwin MS. 2001. The association between socioeconomic status, health insurance coverage, and quality of life in men with prostate cancer. J Clin Epidemiol 54(4):350–358.
Pereira J. 2003 (July 14). To save on healthcare costs, firms fire disabled workers. The Wall Street Journal. P. A1.
Pollitz K. 2004 (October 27–28). Health Insurance Problems for People with Serious and Chronic Illnesses. Presentation at the meeting of the IOM Committee on Cancer Survivorship, Irvine, CA.
Pollitz K, Lewis S, Kofman M, Bangit E, Lucia K, Libster J. 2004. A Consumer’s Guide to Getting and Keeping Health Insurance in Maryland. Washington, DC: Georgetown University Health Policy Institute.
Pollitz K, Sorian R, Thomas K (Georgetown University Institute for Health Care Research and Policy and K.A. Thomas and Associates). 2001. How Accessible Is Individual Health Insurance for Consumers in Less-Than-Perfect Health? Menlo Park, CA: Kaiser Family Foundation.
Pollitz K, Tapay N, Hadley E, Specht J. 2000. Early experience with ‘new federalism’ in health insurance regulation. Health Aff (Millwood) 19(4):7–22.
Pyenson B, Zenner PA. 2002. The Cost of Cancer to the Worksite. New York, NY: Milliman USA, Inc.
Roessler R, Sumner G. 1997. Employer opinions about accommodating employees with chronic illnesses. Journal of Applied Rehabilitation Counseling 28(3):29–34.
Roetzheim RG, Gonzalez EC, Ferrante JM, Pal N, Van Durme DJ, Krischer JP. 2000a. Effects of health insurance and race on breast carcinoma treatments and outcomes. Cancer 89(11):2202–2213.
Roetzheim RG, Pal N, Gonzalez EC, Ferrante JM, Van Durme DJ, Krischer JP. 2000b. Effects of health insurance and race on colorectal cancer treatments and outcomes. Am J Public Health 90(11):1746–1754.
Rothstein MA, Kennedy K, Ritchie KJ, Pyle K. 1995. Are cancer patients subject to employment discrimination? Oncology (Huntingt) 9(12):1303–1306; discussion 1311–1312, 1315.
Sanchez KM, Richardson JL. 2004 (June 16–18). Cancer History Disclosure in the Workplace. Presentation at the NCI and ACS Cancer Survivorship: Pathways to Health After Treatment meeting, Washington, DC.
Schwerin B. 2005 (January 27–28). The Cancer Legal Resource Center—Assistance for Cancer-Related Legal Issues. Presentation at the Annual Conference of the American Psychosocial Oncology Society, Phoenix, AZ.
Short PF, Graefe DR, Schoen C. 2003. Churn, Churn, Churn: How Instability of Health Insurance Shapes America’s Uninsured Problem. Washington, DC: The Commonwealth Fund Issue Brief.
Short PF, Vasey J, Markowski M, Zabora J, Harper G, Rybka W. 2005a. Quality of Life in a Large Cohort of Adult Cancer Survivors. Penn State Population Research Institute Working Paper 2005–01. [Online]. Available: http://www.pop.psu.edu/general/pubs/working_papers/psu-pri/wp0501.pdf [accessed April 13, 2005].
Short PF, Vasey JJ, Tunceli K. 2005b. Employment pathways in a large cohort of adult cancer survivors. Cancer 103(6):1292–1301.
Spelten ER, Sprangers MA, Verbeek JH. 2002. Factors reported to influence the return to work of cancer survivors: A literature review. Psychooncology 11(2):124–131.
SSA (Social Security Administration). 2004a. Annual Statistical Report on the Social Security Disability Insurance Program. Washington, DC: SSA.
SSA. 2004b. SSI Annual Statistical Report, 2003. Washington DC: SSA.
State High Risk. 2004. State High Risk Pool Funding Extension Act of 2004 (Introduced in Senate). [Online]. Available: http://thomas.loc.gov/cgi-bin/query/z?c108:S.2283: [accessed October 5, 2004].
State High Risk. 2005. State High Risk Pool Funding Extension Act of 2005 (Reported in Senate). [Online]. Available: http://thomas.loc.gov/cgi-bin/query/D?c109:1:./temp/~c109zOUpsl: [accessed April 14, 2005].
Steiner JF, Cavender TA, Main DS, Bradley CJ. 2004. Assessing the impact of cancer on work outcomes: What are the research needs? Cancer 101(8):1703–1711.
Taylor JC, Terrell JE, Ronis DL, Fowler KE, Bishop C, Lambert MT, Myers LL, Duffy SA, Bradford CR, Chepeha DB, Hogikyan ND, Prince ME, Teknos TN, Wolf GT. 2004. Disability in patients with head and neck cancer. Arch Otolaryngol Head Neck Surg 130(6):764–769.
Thorpe KE, Howard D. 2003. Health insurance and spending among cancer patients. Health Aff (Millwood) (Suppl): W3-189–198 [Online]. Available: http://content.healthaffairs.org/cgi/reprint/hlthaff.w3.189v1 (accessed July 11, 2005).
Tu HT. 2004. Rising Health Costs, Medical Debt and Chronic Conditions. Issue Brief No. 88. Washington, DC: Center for Studying Health System Change.
U.S. Department of Labor. 2000. Accommodating Employees with Hidden Disabilities. [Online]. Available: http://www.dol.gov/odep/pubs/ek00/hiddenemp.htm [accessed June 7, 2004].
U.S. Department of Labor. 2004a. Fact Sheet #28: The Family and Medical Leave Act of 1993. [Online]. Available: http://www.dol.gov/esa/regs/compliance/whd/printpage.asp?REF=whdfs28.htm [accessed September 16, 2004].
U.S. Department of Labor. 2004b. Low Cost Accommodation Solutions. [Online]. Available: http://www.jan.wvu.edu/media/LowCostSolutions.html [accessed September 15, 2004].
U.S. Department of Labor. 2004c. What is JAN? [Online]. Available: http://www.jan.wvu.edu/english/whatis.htm [accessed June 4, 2004].
U.S. DHHS (U.S. Department of Health and Human Services). 2002. HHS to Help States Create High-Risk Pools to Increase Access to Health Coverage. [Online]. Available: http://www.hhs.gov/news/press/2002pres/20021126a.html [accessed January 31, 2003].
U.S. DHHS. 2003a. HHS Awards $690,000 to Maryland to Promote High-Risk Pools to Cover Uninsured Residents. [Online]. Available: http://www.hhs.gov/news/press/2003pres/20030430b.html [accessed September 2004].
U.S. DHHS. 2003b. HHS to Award $80 Million to States to Offset Costs of Insurance for Residents Too Sick for Conventional Coverage. [Online]. Available: http://www.hhs.gov/news/press/2003pres/20030428.html [accessed September 2004].
U.S. DHHS. 2003c. HHS Awards Nearly $30 Million to States to Offset Costs of Insurance for Residents Too Sick for Conventional Coverage. [Online]. Available: http://www.hhs.gov/news/press/2003pres/20031217a.html [accessed September 2004].
Voelker R, ed. 1999. Living, Coping, and Working with Cancer. Business and Health. Vol. 3. Montvale, NJ: Medical Economics Company.
White House. 2000. Executive Order to Prohibit Discrimination in Federal Employment Based on Genetic Testing. [Online]. Available: http://www.opm.gov/pressrel/2000/genetic_eo.htm [accessed September 16, 2004].
Williams CH, Fuchs BC (Robert Wood Johnson Foundation). 2004. Expanding the Individual Health Insurance Market: Lessons From the State Reforms of the 1990s. The Synthesis Project, Policy Brief No. 4. Princeton, NJ: Robert Wood Johnson Foundation.
Yabroff KR, Lawrence WF, Clauser S, Davis WW, Brown ML. 2004. Burden of illness in cancer survivors: Findings from a population-based national sample. J Natl Cancer Inst 96(17):1322–1330.







































































