5
Coordinating Care for Better Mental, Substance-Use, and General Health
Summary
Mental and substance-use problems and illnesses seldom occur in isolation. They frequently accompany each other, as well as a substantial number of general medical illnesses such as heart disease, cancers, diabetes, and neurological illnesses. Sometimes they masquerade as separate somatic problems. Consequently, mental, substance-use, and general health problems and illnesses are frequently intertwined, and coordination of all these types of health care is essential to improved health outcomes, especially for chronic illnesses. Moreover, mental and/or substance-use (M/SU) problems and illnesses frequently affect and are addressed by education, child welfare, and other human service systems. Improving the quality of M/SU health care—and general health care—depends upon the effective collaboration of all mental, substance-use, general health care, and other human service providers in coordinating the care of their patients.
However, these diverse providers often fail to detect and treat (or refer to other providers to treat) these co-occurring problems and also fail to collaborate in the care of these multiple health conditions—placing their patients’ health and recovery in jeopardy. Collaboration by mental, substance-use, and general health care clinicians is especially difficult because of the multiple separations that characterize mental and substance-use health care: (1) the greater separation of mental and substance-use health care from general health care; (2) the separation of mental and substance-
use health care from each other; (3) society’s reliance on the education, child welfare, and other non–health care sectors to secure M/SU services for many children and adults; and (4) the location of services needed by individuals with more-severe M/SU illnesses in public-sector programs apart from private-sector health care.
This mass of disconnected care delivery arrangements requires numerous patient interactions with different providers, organizations, and government agencies. It also requires multiple provider “handoffs” of patients for different services and transmittal of information to and joint planning by all these providers, organizations, and agencies if coordination is to occur. Overcoming these separations also is made difficult because of legal and organizational prohibitions on clinicians’ sharing information about mental and substance-use diagnoses, medications, and other features of clinical care, as well as a failure to implement effective structures and processes for linking the multiple clinicians and organizations caring for patients. To overcome these obstacles, the committee recommends that individual treatment providers create clinically effective linkages among mental, substance-use, and general health care and other human service agencies caring for these patients. Complementary actions are also needed from government agencies, purchasers, and accrediting bodies to promote the creation of these linkages.
To enable these actions, changes are needed as well to address the less-evolved infrastructure for using information technology, some unique features of the M/SU treatment workforce that also have implication for effective care coordination, and marketplace practices. Because these issues are of such consequence, they are addressed separately in Chapters 6, 7, and 8, respectively.
CARE COORDINATION AND RELATED PRACTICES DEFINED
Crossing the Quality Chasm notes that the multiple clinicians and health care organizations serving patients in the American health care system typically fail to coordinate their care. That report further states that the resulting gaps in care, miscommunication, and redundancy are sources of significant patient suffering (IOM, 2001).1 The Quality Chasm’s health care quality framework addresses the need for better care coordination in
one of its ten rules and in another rule calls attention to the need for provider communication and collaboration to achieve this goal:
Cooperation among clinicians. Clinicians and institutions should actively collaborate and communicate to ensure an appropriate exchange of information and coordination of care.
Shared knowledge and the free flow of information. Patients should have unfettered access to their own medical information and to clinical knowledge. Clinicians and patients should communicate effectively and share information. (IOM, 2001:62)
These two rules highlight two prerequisites to coordination of care: communication and collaboration across providers and within and across institutions. Communication exists when each clinician or treatment provider caring for a patient shares needed treatment information with other clinicians and providers caring for the patient. Information can be shared verbally; manually in writing; or through information technology, such as a shared electronic health record. Collaboration is multidimensional and requires the aggregation of several behaviors, including the following:
-
A shared understanding of goals and roles—Collaboration is enhanced by a shared understanding of an agreed-upon collective goal (Gittell et al., 2000) and clarity regarding each clinician’s role. Role confusion and role conflict are frequent barriers to interdisciplinary collaboration (Rice, 2000).
-
Effective communication—Multiple studies have identified effective communication as a key feature of collaboration (Baggs and Schmitt, 1988; Knaus et al., 1986; Schmitt, 2001; Shortell et al., 1994). “Effective” is defined variously as frequent, timely, understandable, accurate, and satisfying (Gittell et al., 2000; Shortell et al., 1994).
-
Shared decision making—In shared decision making, problems and strategies are openly discussed (Baggs and Schmitt, 1997; Baggs et al., 1999; Rice, 2000; Schmitt, 2001), and consensus is often used to arrive at a decision. Disagreements over treatment approaches and philosophies, roles and responsibilities, and ethical questions are common in health care settings. Positive ways of addressing these inevitable differences are identified as a key component of effective caregiver collaboration (Shortell et al., 1994).
It is important to note that, according to health services researchers, collaboration is not a dichotomous variable, simply present or absent. Rather, it is present to varying degrees (Schmitt, 2001).
Collaboration also is typically characterized by necessary precursors. Clinicians are more likely to collaborate when they perceive each other as having the knowledge necessary for good clinical care (Baggs and Schmitt, 1997). Mutual respect and trust are necessary precursors to collaboration as well (Baggs and Schmitt, 1988; Rice, 2000); personal respect and trust are intertwined with respect for and trust in clinical competence.
Care coordination is the outcome of effective collaboration. Coordinated care prevents drug–drug interactions and redundant care processes. It does not waste the patient’s time or the resources of the health care system. Moreover, it promotes accurate diagnosis and treatment because all providers receive relevant diagnostic and treatment information from all other providers caring for a patient.
Care integration is related to care coordination. As defined by experts in health care organization and management (Shortell et al., 2000), integration of care and services can be of three types:
-
“Clinical integration is the extent to which patient care services are coordinated across people, functions, activities, and sites over time so as to maximize the value of services delivered to patients” (p. 129).
-
Physician (or clinician) integration is the extent to which clinicians are economically linked to an organized delivery system, use its facilities and services, and actively participate in its planning, management and governance.
-
Functional integration is “the extent to which key support functions and activities (such as financial management, strategic planning, human resources management, and information management) are coordinated across operating units so as to add the greatest overall value to the system” (p. 31). The most important of these functions and activities are human resources deployment strategies, information technologies, and continuous improvement processes.
Shortell et al.’s clinical integration corresponds to care coordination as addressed in the Quality Chasm report.
In the context of co-occurring mental and substance-use problems and illnesses, the Substance Abuse and Mental Health Services Administration (SAMHSA) similarly identifies three levels of integration (SAMHSA, undated):
-
Integrated treatment refers to interactions between clinicians to address the individual needs of the client/patient, and consists of “any mechanism by which treatment interventions for co-occurring disorders are combined within the context of a primary treatment relationship or service setting” (p. 61).
-
Integrated program refers to an organizational structure that ensures the provision of staff or linkages with other programs to address all of a client’s needs.
-
Integrated systems refers to an organizational structure that supports an array of programs for individuals with different needs through funding, credentialing/licensing, data collection/reporting, needs assessment, planning, and other system planning and operation functions.
SAMHSA’s integrated treatment corresponds to Shortell et al.’s clinical integration; both appear to equate to coordination of care as used in the Quality Chasm report. In this report, we use the Quality Chasm terminology of care coordination and address the coordination of care at the level of the patient. We do not address issues surrounding the other levels of coordination or integration represented by Shortell et al.’s clinician and functional integration or SAMHSA’s integrated programs and systems.
FAILED COORDINATION OF CARE FOR CO-OCCURRING CONDITIONS
Co-Occurring Mental, Substance-Use, and General Health Problems and Illnesses
Mental or substance-use problems and illnesses seldom occur in isolation. Approximately 15–43 percent of the time they occur together (Kessler et al., 1996; Kessler, 2004; Grant et al., 2004a,b; SAMHSA, 2004). They also accompany a wide variety of general medical conditions (Katon, 2003; Mertens et al., 2003), sometimes masquerade as separate somatic problems (Katon, 2003; Kroenke, 2003), and often go undetected (Kroenke et al., 2000; Saitz et al., 1997). As a result, individuals with M/SU problems and illnesses have a heightened need for coordinated care.
Co-Occurring Mental and Substance-Use Problems and Illnesses
The 1990–1992 National Comorbidity Survey well documented the high rates of co-occurring mental and substance use conditions, finding an estimated 42.7 percent of adults aged 15–54 with an alcohol or drug “disorder” also having a mental disorder, and 14.7 percent of those with a mental disorder also having an alcohol or drug disorder (Kessler et al., 1996; Kessler 2004). These findings are reaffirmed by more recent studies. According to the National Institute on Alcohol Abuse and Alcoholism (NIAAA) 2001–2002 National Epidemiologic Survey on Alcohol and Related Conditions, 19.7 percent of the general adult (18 and older) U.S. population with any substance-use disorder is estimated to have at least one
co-occurring independent (non–substance-induced) mood disorder, and 17.7 percent to have at least one co-occurring independent anxiety disorder. Among respondents with a mood disorder, 20 percent had at least one substance-use disorder, as did 15 percent of those with an anxiety disorder. Rates of co-occurrence are higher among individuals who seek treatment for substance-use disorders; 40.7 percent, 33.4 percent, and 33.1 percent of those who sought treatment for an alcohol-use disorder had at least one independent mood disorder, anxiety disorder, or other drug use disorder, respectively. Among those seeking treatment for a drug-use disorder, 60.3 percent had at least one independent mood disorder, 42.6 percent at least one independent anxiety disorder, and 55.2 percent a comorbid alcohol-use disorder (Grant et al., 2004a).
Similar or higher rates of co-occurrence are found for other types of mental problems and illnesses (Grant et al., 2004b), as well as for serious mental illnesses generally. The 2003 National Survey on Drug Use and Health documented that among adults aged 18 and older not living in an institution or inpatient facility, an estimated 18 percent of those who had used illicit drugs in the past year also had a serious mental illness.2 Over 21 percent of adults with substance “abuse” or dependence were estimated to have a serious mental illness, and 21.3 percent of adults with such an illness had been dependent on or “abused” alcohol or illicit drugs in the past year (SAMHSA, 2004).
One longitudinal study of patients in both mental health and drug treatment settings found that mental illnesses were as prevalent and serious among individuals treated in substance-use treatment facilities as among patients in mental health treatment facilities. Similarly, individuals served in mental health treatment facilities had substance-use illnesses at rates and severity comparable to those among individuals served in substance-use treatment facilities (Havassy et al., 2004).
Co-occurrence with General Health Conditions
M/SU problems and illnesses frequently accompany a substantial number of chronic general medical illnesses, such as diabetes, heart disease, neurologic illnesses, and cancers, sometimes masquerading as separate somatic problems (Katon, 2003). Approximately one in five patients hospitalized for a heart attack, for example, suffers from major depression, and evidence from multiple studies is “strikingly consistent” that post–heart attack depres-
sion significantly increases one’s risk for death: patients with depression are about three times more likely to die from a future attack or other heart problem (Bush et al., 2005:5). Depression and anxiety also are strongly associated with somatic symptoms such as headache, fatigue, dizziness, and pain, which are the leading cause of outpatient medical visits and often medically unexplained (Kroenke, 2003). They also are more often present in individuals with a number of medical conditions as yet not well understood, including chronic fatigue syndrome, fibromyalgia, irritable bowel syndrome, and nonulcer dyspepsia (Henningsen et al., 2003).
The converse also is true. Individuals with M/SU conditions often have increased prevalence of general medical conditions such as cardiovascular disease, high blood pressure, diabetes, arthritis, digestive disorders, and asthma (De Alba et al., 2004; Mertens et al., 2003; Miller et al., 2003; Sokol et al., 2004; Upshur, 2005). Persons with severe mental illnesses have much higher rates of HIV and hepatitis C than those found in the general population (Brunette et al., 2003; Rosenberg et al., 2001; Sullivan et al., 1999). Moreover, specific mental or substance-use diagnoses place individuals at higher risk for certain general medical conditions. For example, those in treatment for schizophrenia, depression, and bipolar illness are more likely than the general population to have asthma, chronic bronchitis, and emphysema (Sokol et al., 2004). Persons with anxiety disorders have higher rates of cardiac problems, hypertension, gastrointestinal problems, genitourinary disorders, and migraine (Harter et al., 2003). Individuals with schizophrenia are at increased risk for obesity, heart disease, diabetes, hyperlipidemia, hepatitis, and osteoporosis (American Diabetes Association et al., 2004; Goff et al., 2005; Green et al., 2003). And chronic heavy alcohol use is associated with liver disease, immune system disorders, cardiovascular diseases, and diabetes (Carlsson et al., 2000; Corrao et al., 2000; NIAAA, 2000).
Substance use, particularly injection drug use, carries a high risk of other serious illnesses. In a large cohort study of middle-class substance-using patients, the prevalence of hepatitis C was 27 percent in all substance users and 76 percent in injection drug users (Abraham et al., 1999). Injection drug use accounts for about 60 percent of new cases of hepatitis C (Alter, 1999) and remains the second most common risk behavior for acquisition of HIV in the United States (CDC, 2001). Evidence of past infection with hepatitis B also is common in injection drug users (Garfein, et al., 1996). Hepatitis C and coinfection with HIV and active hepatitis B are associated with more-severe liver disease (Zarski et al., 1998). Alcohol use is prevalent among HIV-infected patients (Conigliaro et al., 2003), and accelerates cognitive impairment in HIV-associated dementia complex (Fein et al., 1998; Tyor and Middaugh, 1999).
Given that patients with HIV infection are now living longer, the impact of comorbid conditions in these patients, including alcohol and drug-use
problems, has become increasingly important. Hepatitis C–related liver injury progresses more rapidly in both HIV coinfected persons and alcohol users. Laboratory and preliminary clinical evidence indicates that both alcohol use and hepatitis C can negatively affect immunologic and clinical HIV outcomes. Furthermore, both alcohol and drug use may adversely affect the prescription and efficacy of and adherence to HIV medications (Moore et al., 2004; Palepu et al., 2003; Samet et al., 2004).
The co-occurrence of mental, substance-use, and general health problems and illnesses has important implications for the recovery of individuals with these illnesses. All of these conditions need to be to be detected and treated; however, this often does not happen, and even when it does, providers dealing with one condition often fail to detect and treat the co-occurring illness and to collaborate in the coordinated care of these patients.
Failure to Detect, Treat, and Collaborate in the Care of Co-Occurring Illnesses
Although detection of some common mental illnesses, such as depression, has increased over the past decade, general medical providers still too often fail to detect alcohol, drug, or mental problems and illnesses (Friedmann et al., 2000b; Miller et al., 2003; Saitz et al., 1997, 2002). In a nationally representative survey of general internal medicine physicians, family medicine physicians, obstetrician/gynecologists, and psychiatrists, for example, 12 percent reported that they did not usually ask their new patients whether they drank alcohol, and fewer than 20 percent used any formal screening tool to detect problems among those who did drink (Friedmann et al., 2000b). Moreover, evidence indicates that general medical providers often assume that the health complaints of patients with a prior psychiatric diagnosis are psychologically rather than medically based (Graber et al., 2000).
Similarly, mental health and substance-use treatment providers frequently do not screen, assess, or address co-occurring mental or substance-use conditions (Friedmann et al., 2000b) or co-occurring general medical health problems. In a survey of patients of one community mental health center, 45 percent of respondents reported that their mental health provider did not ask about general medical issues (Miller et al., 2003).
Evidence presented in Chapter 4 documents some of the failures of providers to treat co-occurring conditions. Other studies have added to the evidence that even when co-occurring M/SU conditions are known, they are not treated (Edlund et al., 2004; Friedmann et al., 2000b, 2001). The above-cited longitudinal study of patients with comorbid conditions at four public residential treatment facilities for seriously mentally ill patients and three residential treatment facilities for individuals with substance-use ill-
nesses found no listings of co-occurring problems or illnesses in patient charts despite the existence of significant comorbidity. “Patient charts in the public mental health system generally include a primary psychiatric disorder; co-occurring psychiatric or substance use disorders are not systematically included. Substance abuse treatment sites only documented substance use disorders” (Havassy et al., 2004:140). In the national survey of primary care providers and psychiatrists described above, 18 percent of physicians reported that they typically offered no intervention (including a referral) to their problem-drinking patients, in part because of misplaced concern about patients’ sensitivity on these issues (Friedmann et al., 2000b). Nearly the same proportion (15 percent) reported that they did not intervene when use of illicit drugs was detected (Friedmann et al., 2001). A 1997–1998 national survey found that among persons with probable co-occurring mental and substance-use disorders who received treatment for either condition, fewer than a third (28.6 percent) received treatment for the other (Watkins et al., 2001).
Additional evidence of the failure to coordinate care is found in the complaints of consumers of M/SU services. The President’s New Freedom Commission reported that consumers often feel overwhelmed and bewildered when they must access and integrate mental health care and related services across multiple, disconnected providers in the public and private sectors (New Freedom Commission on Mental Health, 2003).
These failures to detect and treat co-occurring conditions take place in a health care system that has historically and currently separates care for mental and substance-use problems and illnesses from each other and from general health care, to a greater extent than is the case for other specialty health care. Absent or poor linkages characterize these separate care delivery arrangements. Numerous demonstration projects and strategies have been developed to better link health care for general, mental, and substance-use health conditions and related services. These include The Robert Wood Johnson Foundation’s Depression in Primary Care: Linking Clinical and Systems Strategies Project (Upshur, 2005) and the MacArthur Foundation’s RESPECT—Depression Project (Dietrich et al., 2004).
NUMEROUS, DISCONNECTED CARE DELIVERY ARRANGEMENTS
“Every system is perfectly designed to achieve exactly the results it gets.”
(Berwick, 1998)
Organizations and providers offering treatment and services for mental, substance-use, and general health care conditions typically do so through separate care delivery arrangements:
-
Arrangements for the delivery of health care for mental and substance-use conditions are typically separate from general health care (financially and organizationally more so than other specialty health care services).
-
In spite of the frequent co-occurrence of M/SU problems and illnesses, the delivery of health care for these conditions also typically occurs through separate treatment providers and organizations.
-
Some health care for mental and substance-use conditions and related services are delivered through governmental programs that are separate from private insurance—requiring coordination across public and private sectors of care.
-
Non–health care sectors—education, child welfare, and juvenile and criminal justice systems—also separately arrange for M/SU services.
Traversing these separations is made difficult by a failure to put in place effective strategies for linking general, mental, and substance-use health care and the other human services systems that also deliver much-needed services for M/SU problems and illnesses; by a lack of agreement about which entity or entities should be held accountable for coordinating care; and by state and federal laws (and the policies and practices of some health care organizations) that limit information sharing across providers.3
Separation of M/SU Health Care from General Health Care
Although the proportion has been declining in recent years, two-thirds of Americans (64 percent in 2002) under the age of 65 receive health care through private insurance offered by their or their family member’s employer (Fronstin, 2003). Over the past two decades, employers and other group purchasers of health care (e.g., state Medicaid agencies) have increasingly provided mental and substance-use health care benefits through health insurance plans that are separate administratively and financially from the plans through which individuals receive their general health care. These separate M/SU health plans are informally referred to as “carved out.” In payer carve-outs, an employer or other payer offers prospective enrollees one or more health plans encompassing all of their covered health care except that for mental and substance-use conditions. Covered individuals are then enrolled in another health plan that includes a network of M/SU
|
3 |
In addition, the less-evolved infrastructure for deploying information technology among mental health and substance-use treatment providers inhibits ease of coordination (see Chapter 6). Some of the unique features of the M/SU treatment workforce (e.g., the greater number of provider types, variation in their training and focus, and their greater location in solo or small group practices) that also contribute to this problem are addressed in Chapter 7. |
providers chosen separately by the employer/payer. In health plan carve-outs, employees enroll in just one comprehensive health plan, and the administrators of that plan arrange internally to have M/SU health care provided and managed through a separate vendor. Estimates of the proportion of employees receiving M/SU health services through carve-out arrangements with managed behavioral health organizations (MBHOs) vary from 36 to 66 percent, reflecting differences in targeted survey respondents (e.g., employers, MBHOs, or employees) and what is being measured (e.g., carved-out services can include utilization review or case management only, or the provision of a full array of M/SU services) (Barry et al., 2003).
The MBHOs that provide these carve-out M/SU services arose in part in response to financial concerns. In the 1980s, employers’ costs for behavioral health services were increasing at twice the rate of medical care overall and four times the rate of inflation. Evidence is clear that MBHOs have been successful in reducing these costs and also in achieving greater use of community-based care as opposed to institutionalization. They also have been credited with playing a role in keeping costs down in the face of broadened benefits, which has assisted in securing support for greater parity of mental health benefit coverage. Moreover, MBHOs have helped move clinicians from solo into group practices (Feldman, 2003), which, as discussed in Chapter 7, can facilitate quality improvement. Carve-out arrangements can nurture recognition and support for specialized knowledge of M/SU problems and illnesses and treatment expertise. They also can attenuate problems involving the adverse selection of individuals with M/SU illnesses in insurance plans (see Chapter 8).
In contrast to the clear evidence for the benefits described above, evidence for the effects of carve-out arrangements on quality of care is limited and mixed (Donohue and Frank, 2000; Grazier and Eselius, 1999; Hutchinson and Foster, 2003). However, models of safety and errors in health care suggest that whenever individuals are cared for by separate organizations, functional units, or providers, discontinuities in care can result unless the unavoidable gaps in care are anticipated, and strategies to bridge those gaps are implemented (Cook et al., 2000). A previous Institute of Medicine (IOM) report found that carved-out M/SU services “do not necessarily lead to poor coordination of care…. However the separation of primary care and behavioral health care systems brings risks to coordination and integration…” (IOM, 1997:116). The President’s New Freedom Commission on Mental Health care deemed the separation between systems for mental and general health care so large as to constitute a “chasm” (New Freedom Commission on Mental Health, 2003).
Several factors could help account for problems with coordinating care in the presence of M/SU carve-outs. First, under carve-out arrangements, primary care physicians generally are not expected to treat (and may not
always be able to be reimbursed for treating) M/SU problems and illnesses (Feldman et al., 2005; Upshur, 2005). The employer or other purchaser of health insurance benefits for the individual has, by contract, specified that general health care is to be provided by one network of providers though a health plan covering that care, and M/SU care through a different health plan’s network of specialty M/SU providers. This is different from the situation with other medical problems and illnesses. For example, when a patient seeks care for diabetes, asthma, allergies, heart problems, or other general medical conditions, the patient’s primary care provider is allowed to treat these illnesses and can be reimbursed for those services. When the primary care provider and/or the patient decides that the problem requires the attention of a specialist, the provider makes a referral or the patient self-refers to a specialist. Use of a specialist comes about based generally on the primary care provider’s and/or patient’s judgment. In contrast, under M/SU carve-out arrangements, M/SU health care often is predetermined by the employer or other group purchaser to require the attention of a specialist and must therefore be provided by a second provider. As a result, one method of care coordination—care by the same provider—is not available to the patient. While not all primary care providers have the expertise and/or desire to treat M/SU illnesses (see Chapters 4 and 7), some do, and evidence indicates that many patients typically turn initially to their primary care provider for help with M/SU problems and illnesses (Mickus et al., 2000).
A second obstacle to care coordination is that information about the patient’s health problem or illness, medications, and other treatments must now be shared across and meet the often differing privacy, confidentiality, and additional administrative requirements imposed by the different health plans. Consumers also are required to navigate the administrative requirements of both health plans.
Finally, as described in Chapter 4, the use of carve-outs poses difficulties for quality measurement and improvement—including measurement and improvement of coordination—in two ways. First, because primary care providers cannot always be reimbursed for M/SU health care, they sometimes provide the care but code the visit according to the patient’s somatic complaint (for which the treatment they provide can be reimbursed) (Rost et al., 1994). This situation masks the true prevalence of M/SU illnesses in primary care and impedes quality measurement and improvement efforts. Moreover, the existence of two parallel health plans serving the patient creates some confusion about accountability for quality and coordination. For example, the National Committee for Quality Assurance’s mental and substance-use quality measures (i.e., those contained in its Health Plan Employer Data and Information Set [HEDIS] measurement set) are required to be reported by comprehensive managed
care plans seeking accreditation, but not by MBHOs seeking accreditation.4 Also, as discussed later in this chapter, accreditation standards do not always make clear the responsibilities for care coordination when an individual is served by two health plans, such as a managed care plan providing general health care and an MBHO.
Separation of Health Services for Mental and Substance-Use Conditions from Each Other
The mental health and substance-use treatment systems evolved separately in the United States as a result of the different historical understandings of and responses to these illnesses described in Chapter 2. This separation became increasingly institutionalized with the evolution of three separate institutes of the National Institutes of Health (NIH) (the National Institute of Mental Health [NIMH] in 1949 and National Institute on Alcohol Abuse and Alcoholism [NIAAA] and the National Institute on Drug Abuse [NIDA] in 1974) and separate programming and funding divisions within SAMHSA. This separation at the federal policy level is frequently mirrored at the state level, where separate state mental health and substance-use agencies exist (although they are combined in some states).
The separation of service delivery that mirrors this separation of policy making and funding does not optimally serve individuals with co-occurring mental and substance-use illnesses. A congressionally mandated study of the prevention and treatment of co-occurring substance-use and mental conditions (SAMHSA, undated) found that the difficulties faced by individuals with these co-occurring conditions in receiving successful treatment and achieving recovery are due in part to the existence of these two separate service systems. The study notes: “Too often, when individuals with co-occurring disorders do enter specialty care, they are likely to bounce back and forth between the mental health and substance abuse services systems, receiving treatment for the co-occurring disorder serially, at best” (SAMHSA, undated:i). The study further states that this separation of public-sector substance-use and mental health service systems is accompanied by marked differences in “staffing resources, philosophy of treatment, funding sources, community political factors, regulations, prior training of staff, credentials of staff, treatment approaches, medical staff resources, assertive community outreach capabilities, and routine types of evaluations and testing procedures performed” (SAMHSA, undated:v). Of greatest concern, the study found that individuals with these co-occurring conditions also may be
excluded from mental health programs because of their substance-use condition and from substance-use treatment programs because of their mental condition (SAMHSA, undated).
Frequent Need for Individuals with Severe Mental Illnesses to Receive Care Through a Separate Public-Sector Delivery System
Treatment for M/SU conditions also is unique in that state and local governments manage public-sector health care systems that are separate from the private-sector health care system for individuals with M/SU illnesses. Indeed, “behavioral disorders remain essentially the only set of health problems for which state and local governments finance and manage a specialty treatment system. [Although] public funds pay for a large portion of the costs of care for certain other disorders (such as Medicare financing of dialysis), and public services exist for a few rare disorders such as leprosy, … the public mental health system is the only substantial disorder-specific treatment system in existence today” (Hogan, 1999:106).
Because (as discussed in Chapter 3) individuals with M/SU illnesses face greater limitations in their insurance coverage than is the case with coverage for other illnesses, some individuals with M/SU illnesses who start receiving their care through private insurance must switch to public insurance (Medicaid or the State Children’s Health Insurance Program [SCHIP])5 or other publicly funded programs at the state and local levels when their private insurance is exhausted. Evidence indicates that these benefit limits most often are reached by individuals with some of the most severe mental illness diagnoses, including depression, bipolar disorder, and psychoses. There is also evidence that other serious diagnoses appearing in childhood, such as autism, are excluded from coverage under certain private health benefit plans (Peele et al., 2002). The lesser availability of health insurance for severe mental illnesses and for substance-use treatment also helps explain the involvement of other public sectors (i.e., child welfare and juvenile justice) in the delivery of mental health care (as described below).
The federal Substance Abuse Prevention and Treatment (SAPT) and Community Mental Health Services (CMHS) Block Grant programs provide funds to states help fill these gaps. SAPT and CMHS grants to states support the planning, delivery, and evaluation of M/SU treatment services. SAPT funds can be used for individuals regardless of the severity of their substance-use problem or illness, while CMHS grant funds may be used only for individuals with serious mental illnesses and children with “serious
emotional disturbances” (SAMHSA, undated). Some of these funds also are given to county and other local government units to use in the planning and delivery of care. In a number of states, major responsibility for mental health services rests with local government, and the extent of coordination between state and local governments is variable.
In addition, public mental health hospitals play a key role in the care of forensic patients—those charged with crimes and being evaluated for competence to stand trial or assume criminal responsibility, or for other issues; those found incompetent to stand trial and being treated to restore competence; those found not guilty by reason of insanity and being treated; those referred for presentencing evaluation; and those sent from prison for hospital-based treatment. In some states, these and related categories account for more than half of all inpatient beds in public mental hospitals. A growing number of people in each of these categories are also being treated in the public (or equivalent community mental health clinic–based) outpatient system. To a considerable extent, this is a function that the public sector has always served. But as other functions have shrunk or been transferred to the private sector (e.g., acute care in many states), forensic functions have come to account for a larger percentage of the public system.
Involvement of Non–Health Care Sectors in M/SU Health Care
M/SU problems and illnesses often are detected (sometimes for the first time) by agencies or organizations that are not part of the traditional health care sector, such as schools, employers, or the welfare and justice systems. These organizations often refer, arrange for, support, monitor, and sometimes deliver M/SU health services. School mental health services and the child welfare and juvenile justice systems provide access to mental health services for the majority of children (DHHS, 1999). The criminal justice system also plays a role in securing M/SU services for some adults. In the private sector, employee assistance programs play a key role in the identification, referral, and provision of services to individuals with M/SU problems and illnesses. Moreover, many other publicly funded entities, such as housing programs, programs for individuals who are homeless, income maintenance programs, and employment programs, provide services that are essential to the recovery of many individuals with severe and chronic M/SU illnesses. The involvement of this array of human service providers generally not considered to be part of the health care sector necessitates additional levels of care coordination. This coordination must be effected despite the inevitable difficulties of working with multiple bureaucracies and in systems with differing priorities, knowledge bases, and practices.
Schools
Most children and adolescents who receive health care for mental conditions receive that care through their schools, not from primary medical or specialty mental health care providers (Kessler et al., 2001). The approaches used by schools to deliver M/SU health care services are highly variable, ranging from (1) class-room based, teacher-implemented programs; to (2) multifaceted, schoolwide programs that employ multiple strategies, such as modification of school policies, classroom management strategies, curriculum changes, and facilitation of parent–school communications; to (3) therapy provided to an individual student, group, or family; to (4) other strategies, such as parent training and education, case management, and consultation. Some of these approaches are prevention-oriented, while others are designed to treat individuals with identified psychopathology. Service modality, intensity, and duration also vary according to individual needs (Rones and Hoagwood, 2000). Some programs rely primarily or exclusively on school-supported mental health professionals (e.g., school social workers, guidance counselors, school nurses), while others have varying degrees of linkage with community mental health agencies and providers (e.g., clinical psychologists, social workers, psychiatrists) who either provide the mental health services exclusively in the school or partner with school staff. In some cases, mental health providers from the school and/or community work on-site in school-based health centers in partnership with primary care providers (Weist et al., 2005).
A review of research on such school-based mental health services published between 1985 and 1999 found that although evidence exists for the effectiveness of a subset of strong programs across a range of emotional and behavioral problems, most school-based programs have no evidence to support their impact, and no programs are targeted to specific clinical syndromes such as anxiety, attention deficit hyperactivity disorder (ADHD), and depression. This same study also found that precisely what is provided by schools under the rubric of mental health services is largely unknown, as is whether those services are effective (Rones and Hoagwood, 2000).
To learn more about school-based mental health services, SAMHSA and Abt Associates recently conducted a national survey aimed at providing information on mental health services delivered in U.S. public schools, including:
-
The types of mental health problems/issues encountered most frequently in the school setting.
-
The types of mental health services delivered, and models and arrangements for their delivery in public elementary, middle, and secondary schools.
-
Barriers to the provision and coordination of mental health services in school settings.
-
The numbers, availability, and qualifications of mental health staff in public schools.
The final report is to be released during fall 2005.6
Experts on school-based mental health services note that (1) schools should not be viewed as responsible for meeting all the mental health needs of their students (in some cases they are already overburdened with demands that should be addressed elsewhere); and (2) connections between school-based mental health services and substance-use treatment services are nonexistent or tenuous (Weist et al., 2005). These two factors, plus the need to coordinate M/SU services with general health care, impose responsibilities on school-based M/SU providers to collaborate with other specialty and general health care providers serving the student, and for the other specialty and general health care providers to do the same.
Child Welfare Services
Almost half (47.9 percent) of a nationally representative, random sample of children aged 2–14 who were investigated by child welfare services in 1999–2000 had a clinically significant need for mental health care (Burns et al., 2004). Even higher rates have been observed in children placed in foster care arrangements (Landsverk, 2005). This is not surprising given that the circumstances of children who are the subject of reports of maltreatment and investigated by child welfare services are characterized by the presence of known risk factors for the development of emotional and behavioral problems, including abuse, neglect, poverty, domestic violence, and parental substance abuse (Burns et al., 2004). Moreover, substantial rates of substance use among adolescents in child welfare have been detected (Aarons et al., 2001).
Ensuring the well-being of children is typically considered part of the mandate of child welfare services, and the children served by these agencies also have very high rates of use of mental health services. However, the first nationally representative study examining the well-being of children and families that came to the attention of child welfare services (the National Survey of Child and Adolescent Well-Being [NSCAW]) found that three of four youths in child welfare who met a stringent criterion of need did not receive mental health care within 12 months of a child abuse and neglect investigation (Landsverk, 2005). States have traditionally used Medicaid to provide medical, developmental, and mental health services to children in
foster care;7 however, use of this resource requires that child welfare services first identify children in need of such services. Analysis of the NSCAW data found that although 94 percent of counties participating in the survey assessed all children entering foster care for physical health problems, only 47.8 percent had policies for assessing mental health problems (Leslie et al., 2003). Data from the NSCAW also indicate that underutilization of needed services can be alleviated when there is strong coordination between local child welfare and public mental health agencies (Hurlburt et al., 2004).
Justice Systems
Criminal justice system The proportion of U.S. citizens incarcerated has been increasing annually—from a rate of 601 persons in custody per 100,000 U.S. residents in 1995 to 715 persons in custody per 100,000 residents in 2003. As of mid-2003, the nation’s prisons and jails8 held 2,078,570 persons—one in every 140 U.S. residents (Harrison and Karberg, 2004). Corrections facilities increasingly must attend to M/SU treatment because of this growth in the proportion of the U.S. population that is incarcerated and the requirement that prisons and jails provide treatment to inmates with medical needs (Haney and Specter, 2003).
A rigorous epidemiologic study of the prevalence of mental and substance-use illnesses in correctional settings has not been undertaken.9 According to the U.S. Bureau of Justice, however, approximately 16 percent of all persons in jails and state prisons reported having either a mental “condition” or an overnight stay in a psychiatric facility, as did 7 percent of those in federal prisons (Ditton, 1999). Consistent with the evidence in Chapter 3 indicating that those with mental illnesses are responsible for a small share of violence in society, this rate is not much higher than that among the U.S. population overall (13 percent of those over age 18 reported receiving mental health treatment in an inpatient or outpatient setting in 200310) (SAMHSA, 2004). Also consistent with the evidence in
Chapter 3, substance use plays a larger role in incarceration. Over half of inmates in state prisons and local jails were under the influence of alcohol or other drugs at the time of their offense, as were 33 to 46 percent of federal prison inmates (Ditton, 1999). In an average year, moreover, approximately one-third of new admissions to prisons result from a violation of parole conditions, nearly 16 percent of which are for some type of drug-related violation, such as a positive test for drug use or possession of drugs (Hughes et al., 2001). Although the majority of prisons and jails screen, assess, and provide treatment for mental illnesses, far fewer prisoners receive treatment for their substance-use problems and illnesses. When they do, detoxification and self-help group/peer support counseling are most commonly provided (Wolff, 2004).
The police and courts also interact with systems providing treatment for M/SU illnesses as they exercise their judgment and license to divert individuals with such illnesses from criminal processing (Metzner, 2002). As discussed in Chapter 3, courts increasingly influence the receipt of treatment for M/SU illnesses through the use of specialty drug and mental health courts. Defendants in these courts have the option of treatment or incarceration. If they choose treatment, they may forgo criminal processing altogether, or undergo criminal processing but forgo sentencing. The court supervises compliance with treatment. Police also influence treatment; as the gatekeepers for the criminal justice process, they are charged with determining whether to “socialize, medicalize, or criminalize” the event. And probation and parole officers influence treatment in exercising their oversight over compliance with terms of probation and parole. All of these actors’ decisions are influenced by their personal understanding of these issues, the culture of their agency, and their localities’ enforcement policies and social norms (Wolff, 2004).
Appropriate decision making about diverting or prosecuting, exercising coercion into treatment in a way that preserves patient-centered care (see Chapter 3), and fulfilling the right of incarcerated persons to medical treatment requires policies and practices that reflect an understanding of M/SU problems and illnesses and their effective treatment, as well as knowledge of the availability of treatment in the local community. However, individual agents of the judicial system vary in their training on these issues, and the policies and practices of each locality vary according to local norms and the public’s beliefs about M/SU illnesses11 (Wolff, 2004). As a result, coordination with specialty M/SU providers, organizations, and systems is essential to the development of evidence-based criminal justice policies and
|
11 |
Since the chief prosecutor in each jurisdiction is typically elected, the public’s perception of M/SU illnesses and dangerousness, for example (see Chapter 3), even if erroneous, may shape policies and practices (Wolff, 2004). |
practices and to the delivery of effective care to individuals in the criminal justice system.
However, numerous and sizable obstacles to coordination between M/SU health care and criminal justice systems have been documented. Several actions that are consistent with the Quality Chasm framework for redesigning health care have been recommended to overcome these obstacles. These include using performance measures of the coordination between M/SU health care and criminal justice systems at the system, agency, program, and individual levels; providing combined, interdisciplinary training in collaboration and coordination for personnel from both types of agencies and programs; incentivizing coordination through promotion, salary, and budget decisions; providing education and decision support to prosecutors and judges; and using information systems to facilitate the communication of information essential to responding appropriately to each individual (Wolff, 2004).
Juvenile justice system Primary components of the juvenile justice system include intake, detention centers, probation services, secure residential facilities, and aftercare programs (Cocozza, 2004). Although research on the prevalence and nature of M/SU illnesses in juvenile justice systems is limited (Cocozza, 2004), between 60 and 75 percent of youths in these systems are estimated to have a diagnosable mental health “disorder” (Cocozza 2004; Teplin et al., 2002; Wierson et al., 1992), and 20 percent are conservatively estimated to have a severe mental illness (Cocozza and Skowyra, 2000). Rates of co-occurring substance-use illnesses also are high (Cocozza, 2004; Grisso, 2004).
Moreover, in a 2003 survey of all (698) secure juvenile detention facilities in the United States,12 two-thirds of the facilities reported holding youths (prior to, after, or absent any pending adjudication) because they were awaiting community mental health services. Further, like youths who are not abused or neglected but are placed in child welfare solely to obtain mental health services (discussed in Chapter 1), children who are not guilty of any offence are similarly placed in local juvenile justice systems and incarcerated solely to obtain mental health services not otherwise available. Although no formal counting and tracking of such children takes place, juvenile justice officials in 33 counties in the 17 states with the largest populations of children under age 18 estimated that approximately 9,000 such children entered their juvenile justice systems under these circumstances in 2001. County juvenile justice officials’ estimates ranged from zero to 1,750, with a median of 140. Nationwide the number of children
placed in juvenile justice systems is likely to be higher; 11 states reported to the Government Accountability Office (GAO) that they could not provide estimates even though they were aware that such placements occur (GAO, 2003).
Although the vast majority of juvenile justice facilities report providing some type of mental health service (Goldstrom et al., 2001), “numerous investigations suggest that many youth in the juvenile justice system do not receive needed mental health services and that available services are insufficient and inadequate.” Most existing programs have not been evaluated, and some of the most popular and widely implemented programs have no evidence to support them and may actually be harmful. Juvenile justice systems, however, lack the training, service, and expertise to respond more effectively (Cocozza, 2004). Because many youths are in juvenile justice systems for relatively minor, nonviolent offenses, there also is a growing sentiment that whenever possible, youths with serious mental illnesses should be diverted from those systems. However, the limited amount of research on the efficacy of juvenile diversion programs has yielded mixed results. To achieve appropriate diversion and the provision of evidence-based care to children and youths in juvenile justice, coordination is crucial: “Almost every study and report that has focused on youth with mental health disorders who come in contact with the juvenile justice system has arrived at the same conclusion—that collaboration between mental health and juvenile justice (and other systems such as child welfare and education as well) at every level and at every stage is critical to any progress. The problem cannot be solved by any single agency” (Cocozza, 2004:35).
Employee Assistance Programs
An increasing number of individuals are covered by employee assistance programs (EAPs). An estimated 66.5 million employees were enrolled in such programs in 2000—a 245 percent increase since 1994 and a 13 percent increase over the year before (Fox et al., 2000). EAPs offered by employers13 to their employees (and frequently employees’ family members) vary in structure, types and qualifications of personnel, scope and length of services provided, location, and relationship to health plans providing M/SU and general health care services to the same employees. Although EAPs began as occupational programs to address alcohol-related problems in the workplace, they now typically offer consultation with personnel in identifying and resolving other job performance issues, and pro-
vide further assessment, referral, and follow-up services. Additional services offered include assistance to employees experiencing stressful events, wellness training, assistance with work/life issues, legal assistance, and financial services. EAPs sometimes have a formal relationship with the M/SU services offered by a health plan and/or serve as a required gateway to M/SU services (Masi et al., 2004). Thus, an EAP’s caseload can include individuals with severe M/SU problems and illnesses (Masi, 2004). EAPs are distinct in that their services are typically brief (an average of six counseling sessions) and often are provided via telephone or the Internet by a provider in a different location—perhaps several states away—and with round-the-clock access (Masi, 2004).
Linkages with Community and Other Human Services Resources
Individuals with M/SU problems and illnesses sometimes require additional services from a variety of community resources, such as self-help and support programs for individuals with specific diseases, housing services, income maintenance programs, and employment services, that are essential to the recovery of many individuals with severe and chronic M/SU illnesses. Appendix C contains a description of an array of such support services provided by the Veterans Health Administration to veterans with severe M/SU illnesses.
Discharge planning units or similar staff within inpatient facilities, as well as case management staff within outpatient treatment settings or programs, must assess patients for the need for these services, establish referral arrangements, and coordinate the services with the human service agencies providing them. Such coordination of care across inpatient and outpatient providers is essential to ensure timely access to these services. When discharge planning or outpatient care fails to ensure speedy access to these services and continuity of care within the community, patients are at risk for failure to implement their treatment plans, homelessness, incarceration, or other adverse outcomes.
Unclear Accountability for Coordination
Because patients receive care from multiple providers and delivery systems, there often is an unclear point (or points) of accountability for patients’ treatment outcomes. When organizations or providers are reimbursed separately for the services they provide, each may perceive no responsibility for the services delivered by others and, as a result, for any patient outcomes likely to be affected by those services. Unless providers’ accountability for sharing information or collaborating with other providers is explicitly identified in their agreements with purchasers, they may reasonably
believe that those other providers have primary responsibility for initiating and maintaining ongoing communication and collaboration.
Moreover, the concept of collaboration has not been clearly defined (Schmitt, 2001). Thus, when providers do accept responsibility for collaborating with other providers, what constitutes “collaboration” is left to their own interpretation based on historical local practice patterns and limitations imposed by their current workload. This unclear accountability has been acknowledged and addressed in a conceptual model for coordinated care delivery developed by the National Association of State Mental Health Program Directors and the National Association of State Alcohol and Drug Abuse Directors. This model articulates a vision of coordinated care involving primary, mental health, substance-use, and other health and human service providers who share responsibility for delivering care to the full population in need of M/SU health care depending upon the predominance of medical, mental, or substance-use symptoms (SAMHSA, undated).
DIFFICULTIES IN INFORMATION SHARING
The sharing of patient information across providers treating the same patient so that care can be coordinated is widely acknowledged as necessary to effective and appropriate care. This need was acknowledged most recently in regulations governing the privacy of individually identifiable health information under the authority of the Health Insurance Portability and Accountability Act (HIPAA) of 1996. HIPAA’s implementing regulations generally permit health care organizations to release—without requiring patient consent—individually identifiable information (except psychotherapy notes) about the patient to another provider or organization for treatment purposes.14
However, the HIPAA regulations are superseded by other federal and state statutory and regulatory provisions that may make it difficult for different providers or treatment organizations to share information. First, HIPAA itself (Section 264 (c)(2)) requires that regulations promulgated to implement its privacy provisions not supersede any contrary provisions of state law that impose more stringent requirements, standards, or implementation specifications pertaining to patient privacy. Each of the 50 states (and the District of Columbia) has a number of statutes governing the confidentiality of medical records, and specifically governing aspects of mental health records. Many of these statutes are more stringent than the HIPAA requirements, and the variation among them is great (see Appendix B for a detailed discussion of federal and state laws regarding confidential-
ity and the release of health care information pertaining to mental and substance-use conditions).
Second, regulations implementing HIPAA also permit health care organizations to implement their own patient consent policies for the release of patient information to other treating providers.15 As a result, health care organizations may adopt even more stringent privacy protections that require participating providers to adhere to additional procedures before sharing patient information with other treatment providers or organizations.
Moreover, separate federal laws govern the release of information pertaining to an individual’s treatment for drug or alcohol use. These laws do not permit sharing of records related to substance-use treatment or rehabilitation by organizations operated, regulated, or funded by the federal government without the patient’s consent, except within a program or with an entity with administrative control over the program, between a program and organizations that provide support services such as billing and data processing, or in case of a “bona fide medical emergency.” These federal laws are also superseded by any state laws that are more stringent (see Appendix B). The preamble to the HIPAA privacy regulations also recognizes the constraints of the substance-use confidentiality law and states that wherever one is more protective of privacy than the other, the more restrictive should govern (65 Fed. Reg. 82462, 82482–82483).
The bottom line is that clinicians providing treatment to individuals with M/SU illnesses must comply with multiple sets of rules governing the release of information: one prescribed federally and pertaining to information on treatment for alcohol or drug problems, state laws that pertain to information on health care for mental and substance-use conditions (depending upon whether they are more stringent than the federal rules), and other policies prescribed by the organization or multiple organizations under whose auspices patient care is provided.
STRUCTURES AND PROCESSES FOR COLLABORATION THAT CAN PROMOTE COORDINATED CARE
Because of the complexities described above, strategies to improve coordination of care need to be multidimensional (Gilbody et al., 2003; Pincus et al., 2003). A systematic review of studies of organizational and educational interventions to improve the management of depression in primary care settings found that initiatives with the most multidimensional approaches generally achieved positive results in their primary outcomes (Gilbody et al., 2003). Components of multidimensional strategies to im-
prove care coordination that can be used by providers and health care organizations at the locus of care include (1) screening for co-occurring conditions; (2) making a formal determination to either treat, or refer for treatment of, co-occurring conditions; (3) implementing more effective mechanisms for linking providers of different services to enable joint planning and coordinated treatment; and (4) providing organizational supports for collaboration between clinicians on- and off-site. Purchasers and quality oversight organizations can create incentives for providers to employ these strategies through their funding and accountability mechanisms and by exercising leadership within their spheres of influence.
Health Care Provider and Organization Strategies
Screening
Because of the high rates of comorbidity described above—especially among those seeking treatment—screening to detect the presence of comorbid conditions is a necessary first step in care coordination. Screening enables a service provider to determine whether an individual with a substance-use problem or illness shows signs of a mental health problem or illness, and vice versa. If a potential problem is identified, a more detailed assessment is undertaken. Routine screening has been shown to improve rates of accurate mental health and substance-use diagnosis (Pignone et al., 2002; Williams et al., 2002).
The above-mentioned congressionally mandated study of the prevention and treatment of co-occurring substance-use and mental conditions (SAMHSA, undated) identified screening as critical to the successful treatment of comorbid conditions. Similarly, because of the high prevalence of emotional and behavioral problems among children served by child welfare services, screening has been recommended for children in the child welfare system overall (Burns et al., 2004) and especially for those placed in foster care (American Academy of Child & Adolescent Psychiatry and Child Welfare League of America, 2003). The U.S. Preventive Services Task Force also has recommended two types of screening in primary care settings:
-
Screening for alcohol misuse by adults, including pregnant women, along with behavioral counseling interventions.
-
Screening for depression in adults in clinical practices that have systems in place to ensure accurate diagnosis, effective treatment, and follow-up (AHRQ, 2002–2003).
The U.S. Preventive Services Task Force has not addressed the issue of screening for comorbid mental or substance-use conditions among indi-
viduals presenting with either condition. To facilitate the adoption of screening and treatment for comorbid mental and substance-use illnesses, the task force could include among its recommended guidelines screening for a co-occurring mental or substance-use problem at the time of an individual’s initial presentation with either condition.
As discussed earlier, however, when screening is done, it often is not performed effectively (Friedmann et al., 2000b; Saitz et al., 2002). Effectiveness can be increased by use of any of a broad range of available and reliable instruments for screening for mental illnesses and co-occurring substance-use problems and illnesses (NIAAA, 2002; Pignone et al., 2002; Williams et al., 2002). An example is the Patient Health Questionnaire, a self-administered instrument designed to screen for depression, anxiety disorders, alcohol abuse, and somatiform and eating disorders in primary care (Spitzer et al., 1999). Other very brief, single-question screens have been evaluated for use in screening for alcohol-use problems (Canagasaby and Vinson, 2005). NIAAA has developed a single question (one for men and one for women) for screening for alcohol-use problems in primary care and other settings (NIAAA, 2005).
Anticipation of Comorbidity and Formal Determination to Treat or Refer
Again because of the high prevalence of co-occurring conditions, especially among individuals seeking treatment, the congressionally mandated study of the prevention and treatment of co-occurring substance-use and mental conditions (SAMHSA, undated) stated that individuals with co-occurring disorders should be the expectation, not the exception, in the substance-use and mental health treatment systems. SAMHSA and others have concluded that substance-use treatment providers should expect and be prepared to treat patients with mental illnesses, and similarly that mental health care providers should be prepared to treat patients with substantial past and current drug problems (Havassy et al., 2004; SAMHSA, undated). In its report to Congress, SAMHSA stated that one of the principles for effective treatment of co-occurring disorders is that “any door is the right door”; that is, people with co-occurring disorders should be able to receive or be referred to appropriate services whenever they enter any agency for mental health or substance-use treatment.
This same principle is applicable to general health problems and illnesses as well. A review of innovative state practices for treating comorbid M/SU conditions found that agency staff expected their clients to present with co-occurring general health problems. They screened and assessed for related conditions, including HIV/AIDS, physical and sexual abuse, brain disorders, and physical disabilities. Staff were cross-trained in both mental health and substance-use disciplines (although they did not work outside of
their primary discipline) (NASMHPD and NASADAD, 2002). The congressionally mandated study also stated that with training and other supports, primary care settings can undertake diagnosis and treatment of these interrelated disorders (SAMHSA, undated). Alternatively, use of a systematic approach to referral to and consultation with a mental health specialist is often used in model programs for better care (Pincus et al., 2003).
Linking Mechanisms to Foster Collaborative Planning and Treatment
As discussed at the beginning of this chapter, the simple sharing of information, by itself, is insufficient to achieve care coordination. Care coordination is the result of collaboration, which exists when the sharing of information is accompanied by joint determination of treatment plans and goals for recovery, as well as the ongoing communication of changes in patient status and modification of treatment plans. Such collaboration requires structures and processes that enable, support, and promote it (IOM, 2004a).
Not surprisingly, available evidence indicates that referrals alone do not lead to collaboration or coordinated care (Friedmann et al., 2000a). Stronger approaches are needed to establish effective linkages among primary care, specialty mental health and substance-use treatment services, and other care systems that are involved in the delivery of M/SU treatment. These stronger linkage mechanisms vary in form and are theorized to exist along a continuum of efficacy. The extremes range from the ad hoc purchase of services from separate providers to on-site programs (see Figure 5-1) (D’Aunno, 1997; Friedmann et al., 2000a). Linkage mechanisms toward the right of the continuum are theorized to be stronger because they lower barriers or causes of “friction” (e.g., problems in identifying willing providers, clients’ personal disorganization, and lack of transportation16) that prevent patients from receiving services.
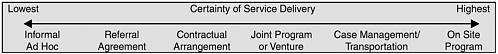
FIGURE 5-1 The continuum of linkage mechanisms.
SOURCE: Friedmann et al., 2000a. Reprinted, with permission, from Health Services Research, June 2000. Copyright 2000 by the Health Research and Educational Trust.
Approaches whose effectiveness in securing collaboration has some conceptual and/or empirical support include collocation and clinical integration of services, use of a shared patient record, case (or care) manage-
|
16 |
These are in addition to the problems in insurance coverage discussed in Chapter 3. |
ment, and formal agreements with external providers. Evidence to date also indicates that some of these approaches are more effective than others. Moreover, their successful implementation requires leadership within an organization, facilitating structures and processes within treatment settings, and often redesigned professional roles and training in these new roles.
Collocation and clinical integration of services Physical proximity of would-be collaborators facilitates collaboration (IOM, 2004a). This point is exemplified by the multiple studies of mental or substance-use health care showing that same-site delivery of both types of care or primary care is more effective in identifying comorbid conditions (Weisner et al., 2001), effectively links clients to the collocated services (Druss et al., 2001; Samet et al., 2001), and can improve treatment outcomes (Unutzer et al., 2001; Weisner et al., 2001). In a 1995 study of a nationally representative sample of all outpatient drug-use treatment units, same-site delivery of services was more effective than formal arrangements with external providers, referral agreements, or case management in ensuring that patients would utilize necessary services (a first step in collaborative care) (Friedmann et al., 2000a). For these reasons, the collocation of multiple services (mental, substance-use, and/or general health) at the same site is a frequently cited feature of many care collaboration programs. The congressionally mandated study of prevention and treatment of co-occurring substance-use and mental conditions (SAMHSA, undated) highlighted “integrated treatment” as an evidence-based approach for co-occurring disorders, defined, in part, as services delivered “in one setting.” The report noted that such integrated treatment programs can take place in either the mental or substance-use treatment setting, but require that treatment and service for both conditions be delivered by appropriately trained staff “within the same setting.”
Others have noted the benefits of integrating behavioral health specialists into primary settings, as well as the reciprocal strategy of including primary care providers at locations that deliver care to individuals with severe mental and substance-use illnesses. This type of collocation facilitates patient follow-through on a referrals, allows for face-to-face verbal communication in addition to or as an alternative to communicating in writing, and allows for informal sharing of the views of different disciplines and easy exchange of expertise (Pincus, 2003).
Such opportunities for face-to-face communication are important because multiple studies identify effective communication as a key feature of collaboration (Baggs and Schmitt, 1988; Knaus et al., 1986; Schmitt, 2001; Shortell et al., 1994). “Effective” communication is described as frequent and timely (Gittell et al., 2000; Shortell et al., 1994),17 and is characterized
by discussion with contributions by all parties, active listening, openness, a willingness to consider other ideas and ask for opinions, questioning (Baggs and Schmitt, 1997; Shortell et al., 1994), and the free flow of information among participants. This type of communication is less easily achieved through electronic, mail, and telephone communications. Nonetheless, when physical integration of services is not feasible, other efforts to promote effective collaboration (i.e., communication between providers by indirect means such as shared patient records or use of a case manager) may yield benefits.
Shared patient records Coordination of care provided by different providers can also be facilitated by shared patient records and documentation practices that promote interdisciplinary information exchange. Electronic health records (EHRs) are supported as an important mechanism for sharing such information and have been highlighted as one of the essential components of the developing National Health Information Infrastructure (NHII). EHRs allow (1) the longitudinal collection of electronic information pertaining to an individual’s health and health care; (2) immediate electronic access—by authorized users only—to person- and population-level information; (3) provision of knowledge and decision support to enhance the quality, safety, and efficiency of patient care; and (4) support for efficient processes of health care delivery (IOM, 2003b). Although still in a minority, hospitals and ambulatory practices are increasingly investing in EHRs; these investments typically are being made by larger facilities, creating what is referred to as the “adoption gap” between large and small organizations (Brailer and Terasawa, 2003). Although sharing of patient information maintained in paper-based records can still take place, the capture and storage of patient information electronically is endorsed as a more thorough and efficient mechanism for timely access to needed information by the many providers serving a patient.
Case (care) management Case (or care) management refers to varying combinations of actions performed by a designated individual18 (i.e., case manager) to arrange for, coordinate, and monitor health, psychological, and social services important to an individual’s recovery from illness and the effects of these services on the patient’s health. Although the services encompassed by case management often vary by the severity of the illness, the needs of the individual, and the specific model of case management
employed (Gilbody et al., 2003; Marshall et al., 2004), typical activities include assessment of the patient’s need for supportive services; individual care planning, referral, and connection of the patient with other necessary services and supports; ongoing monitoring of the patients’ care plan; advocacy; and monitoring of the patient’s symptoms.
Although systematic reviews of the effectiveness of case management for individuals with serious mental illnesses have been conducted with different review strategies and produced conflicting findings (Marshall et al., 2004; Ziguras and Stuart, 2000) (perhaps in part because of the large number of different models of case management [Zwarenstein et al., 2000]), the approach continues to be a common component of many mental health treatment services for individuals with other than mild mental illnesses. A systematic review of studies of organizational and educational interventions to improve the management of depression in primary care settings found that although most initiatives used multiples strategies, case management was one of two approaches used most often in projects achieving positive outcomes and health-related quality of life19 (Gilbody et al., 2003). More recently, within The Robert Wood Johnson Foundation’s national program for depression treatment in primary care, all eight demonstration sites independently designed their interventions to incorporate case management, often with expanded roles for case managers that include ensuring that treatment guidelines and protocols are followed and that a depression registry is used by clinicians. Case managers also serve as intermediaries between patients’ primary care providers and mental health specialists (Anonymous, 2004; Rollman et al., 2003). Case management is an essential element as well of the MacArthur Foundation’s RESPECT—Depression Project for improving the treatment of depression in primary care, and of disease management programs such The John A. Hartford Foundation and California Health Care Foundation’s Project IMPACT program for treating late-life depression (Unutzer et al., 2001).
Formal agreements with external providers Formal agreements with external providers also can influence patients’ appropriate utilization of needed services (Friedmann et al., 2000a). Such agreements can include, for example, a substance-use treatment or mental health organization that contracts with a medical group practice to provide physical examinations and routine medical care for its patients. The advantages of this approach are
that it requires fewer organizational and physical plant resources than do collocated services, and it makes use of existing community resources (Samet et al., 2001). Specialty consultation with primary care providers is another frequently identified service that can be secured through a formal agreement with an external provider (Pincus et al., 2003). At a minimum, formal agreements with external providers should include not just the agreement to provide the referred service, but also provisions addressing information sharing, joint treatment planning, and monitoring of patient outcomes.
Organizational Support for Collaboration
Successfully implementing the above strategies for care coordination requires facilitating structures and processes within treatment settings. Collaboration also often requires changes in the design of work processes at treatment sites, in particular, flexibility in professional roles. Effective leadership is an overarching need to help health care providers successfully adopt, adapt to, and sustain these changes.
Facilitating structures and processes at treatment sites Structures and processes that encourage multidisciplinary providers to come together for joint treatment planning foster collaboration. For example, in acute, general inpatient care, there is evidence that using interdisciplinary rounds can be effective in improving patient care (Curley et al., 1998). Improvement in care can also be achieved by involving primary and mental health care providers in interdisciplinary team meetings (Druss et al., 2001; Unutzer et al., 2001) at which joint care planning takes place, or by providing case managers (see above) to facilitate patient education, monitoring, and communication between primary care providers and M/SU specialists (Feldman et al., 2005). In addition, a number of more general quality improvement strategies, such as medication algorithms, hold the potential to improve coordination of care by standardizing care processes and creating channels of communication. For instance, the Texas Medication Algorithm Project includes a clinical coordinator to help ensure appropriate coordination among clinicians, patients, and family members in promoting adherence to medication guidelines (Miller et al., 2004; Rush et al., 2003).
In a randomized controlled trial of the integration of medical care with mental health services, it was found that same-site location, common charting, enhanced channels of communication (including joint meetings and e-mail), and in-person contact facilitated the development of common goals and sharing of information between medical and mental health providers. Interdisciplinary team meetings involving primary and behavioral health care providers can do the same (Druss et al., 2001).
Heavy workloads can interfere with the formation of collaborative relationships. Collaboration requires that staff have the time to participate in such activities as interdisciplinary team meetings (Baggs and Schmitt, 1997). Illustrating this point, additional staff resources and reduced caseload were identified as two of several components of success in a randomized controlled trial of collocating and integrating medical care with mental health care (Druss et al., 2001). When staff are overwhelmed with caregiving responsibilities, they may not take the time to collaborate. Yet while unilateral decision making is easier in the short run, collaborative relationships are viewed as saving time in the long run (Baggs and Schmitt, 1997).
The committee also calls attention to the Chronic Care Model, used to improve the health care of individuals with chronic illnesses in primary care settings. This model has six components: (1) providing chronic illness self-management support to patients and their families (see Chapter 3); (2) redesigning care delivery structures and operations; (3) linking patients and their care with community resources to support their management of their illness (described above); (4) providing decision support to clinicians (see Chapter 4); (5) using computerized clinical information systems to support compliance with treatment protocols and monitor patient health indicators (see Chapter 6); and (6) aligning the health care organization’s (or provider’s) structures, goals, and values to support chronic care (discussed below) (Bodenheimer et al., 2002). The Chronic Care Model has been applied successfully to the treatment of a wide variety of general chronic illnesses, such as diabetes, asthma, and heart failure (The National Coalition on Health Care and The Institute for Healthcare Improvement, 2002), as well as to common mental illnesses such as depression (Badamgarev et al., 2003), and has been theorized to have the potential for improving the quality of care for persons with other M/SU illnesses (Watkins et al., 2003).
The Chronic Care Model also emphasizes the use of certain organizational structures and processes, including interdisciplinary practices in which a clear division of the roles and responsibilities of the various team members fosters their collaboration. Instituting such arrangements may necessitate new roles and divisions of labor among clinicians with differing training and expertise. In the Chronic Care Model, for example, physician team members are often responsible for the treatment of patients with acute conditions, intervene in stubbornly difficult chronic care problems, and train other team members. Nonphysician personnel support patients in the self-management of their illnesses and arrange for routine periodic health monitoring and follow-up. Providing chronic care consistent with this model requires support from health care organizations, health plans, purchasers, insurers, and other providers. Elements of the Chronic Care Model have been implemented in a variety of care settings, including private general medical practices, integrated delivery systems, and a community health
center for general health care (Bodenheimer et al., 2002). The committee believes this model should be developed for use in the care of individuals with chronic M/SU illnesses as a mechanism for improving coordination of care, as well as other dimensions of quality.
Flexibility in professional roles As seen in the Chronic Care Model, collaboration sometimes requires revision in professional roles, including the shifting of roles among health care professionals and the expansion of roles to include new tasks (Gilbody et al., 2003; Katon et al., 2001). It also often requires participating as part of an interdisciplinary team with certain prescribed roles (Unutzer et al., 2001). Research findings and other empirical evidence show that health care workers of all types are capable of performing new tasks necessitated by advances in therapeutics, shortages in the health care workforce, and the pressures of cost containment. For example, the development of safer and more effective medications for mental and substance-use illnesses (e.g., selective serotonin reuptake inhibitors) has enabled the treatment of depression by primary care clinicians. Other medications, such as buprenorphine, may do the same. Other developments that are likely to require redefinition of professional roles include the use of peer support personnel (described in Chapter 3) and the delivery of more M/SU health care in primary care settings and by primary care providers (Strosahl, 2005).
However, new communication patterns and changes in roles, especially functioning as part of an interdisciplinary team, can at times be uncomfortable for health professionals. Role confusion and conflict are a frequent barrier to interdisciplinary collaboration (Rice, 2000). As a result, it may be necessary to provide training and development in collaborative practice behaviors, such as effective communication and conflict resolution (Disch et al., 2001; Strosahl, 2005). Collaboration is enhanced by a shared understanding of agreed-upon collective goals and new individual roles (Gittell et al., 2000).
Leadership Leadership is well known to be a critical factor in the success of any major change initiative or quality improvement effort (Baldridge National Quality Program, 2003; Davenport et al., 1998) and an essential feature of successful programs in care coordination (NASMHPD, NASADAD, 2002). Effective leadership in part models the behaviors that are expected at the clinical care level. For example, in The Robert Wood Johnson Foundation’s Initiative on Depression in Primary Care, leadership was one of six component interventions to overcome barriers to the delivery of effective care for depression in primary care settings. Teams of primary care, mental health, and senior administrative personnel were responsible for securing needed resources, representing stakeholder interests, promot-
ing adherence to practice standards, setting goals for key process measures and outcomes, and encouraging sustained efforts at continuous quality improvement (Pincus et al., 2003). Such activities ensure that the structures and processes that enable and nurture collaboration are in place at the locus of care.
Practices of Purchasers, Quality Oversight Organizations, and Public Policy Leaders
Clinicians and health care organizations will not be able to achieve full coordination of patient care without complementary and supporting activities on the part of federal and state governments, health care purchasers, quality oversight organizations, and other organizations that shape the environment in which clinical care is delivered. As noted earlier, care coordination has been identified by the IOM as one of 20 priority areas deserving immediate attention by all participants in the American health care system. Health care purchasers, quality oversight organizations, and public policy leaders can help give care coordination this immediate attention by (1) clarifying their expectations for information sharing, collaboration, and coordination in their purchasing agreements; (2) including the care coordination practices recommended above in their quality oversight standards and purchasing criteria; and (3) modeling collaborative practices across health care for general, mental, and substance-use health conditions in their policy-making and operational activities.
Purchaser Practices
Purchasers can stimulate and incentivize better coordination of care among general, mental, and substance-use health care by including care coordination as one of the quality-of-care parameters used to evaluate proposals and award contracts for the delivery of general, specialty M/SU, and comprehensive (general and M/SU) health care (see Chapter 8). In soliciting health plans and providers to deliver these health care services, purchasers can ask bidders to specify what care coordination practices they require of their clinicians, and how the organization supports clinicians and measures care coordination. When awarding contracts, purchasers can clarify in contracts with health care plans their expectations for information sharing, collaboration, and coordination. In addition, purchasers should allow primary care providers to bill for the M/SU treatment services they provide, a practice now under way in some MBHO settings (Feldman et al., 2005). Doing so will allow consumers and their primary care providers to determine jointly, as they do for other medical conditions, when specialty consultation and care are appropriate; enable coordination of care
through the use of a single provider to treat general and M/SU conditions; and eliminate the adverse consequences that arise when primary care providers code visits related to M/SU problems and illnesses as being due to somatic complaints.
Quality Oversight Practices
Many purchasers delegate their attention to care coordination and other quality-related issues by accepting the quality-of-care determinations made by expert quality oversight organizations, such as accrediting bodies. Four main organizations accredit M/SU health care organizations (and sometimes individual providers). The National Committee for Quality Assurance (NCQA) accredits managed care organizations, MBHOs, and disease management programs and recognizes physician practices through other oversight programs. The Joint Commission on Accreditation of Healthcare Organizations (JCAHO) accredits hospitals and specialty behavioral health care organizations. The Commission on Accreditation of Rehabilitation Facilities accredits a wide variety of behavioral health programs and services. Finally, the Council on Accreditation for Children and Family Services, Inc. accredits a wide variety of counseling and other M/SU programs and services, as well as EAPs. These accrediting bodies generally perform their quality oversight activities either through review of an organization’s structures and operational practices or through measurement of an organization’s or provider’s clinical care processes and outcomes. Clinical care processes and outcomes are generally evaluated through performance measures (discussed in Chapter 4). Organizational structures and processes such as the linking strategies recommended above are typically reviewed through evaluation of compliance with the established structural and procedural standards that make up an organization’s accreditation standards.
Although the accreditation standards of each of the above four organizations address care coordination and collaboration to some extent (CARF, 2005; COA, 2001; JCAHO, 2004; NCQA, 2004), accreditation standards for care coordination could be improved. For example, NCQA’s MBHO accreditation standards address care coordination between M/SU and general health care in Standard QI 10, “Continuity and Coordination between Behavioral Health and Medical Care,” which states (NCQA, 2004:91):
The organization collaborates with relevant medical delivery systems or primary care physicians to monitor and improve coordination between behavioral health and medical care.
However, the following note is appended to this standard:
Note: If the organization does not have any formal relationship with the medical delivery system through contracts, delegation, or otherwise, NCQA considers this standard NA. (NCQA, 2004:91). NCQA’s customer support line clarifies that “NA” means “Not Applicable.”20
Collaboration and Coordination in Policy Making and Programming
Throughout this report, the committee emphasizes the need for collaboration and coordination in mental, substance-use, and general health care policy making and programming that parallels desired collaboration and coordination at the care delivery level—for example, in the dissemination of information on innovations in new treatments (see Chapter 4), in the measurement of the quality of M/SU care (see Chapter 4), and in the development of information technology for M/SU care (see Chapter 6). Such attention to coordination and collaboration at the policy and programming represents an opportunity for federal, state, and local officials to model and promote the coordination and collaboration needed at the clinical level—across M/SU health care and across providers of these specialty health care services and general health care. The importance of seizing this opportunity is emphasized in the IOM report Leadership by Example: Coordinating Government Roles in Improving Health Care Quality. That report, commissioned by Congress to examine and recommend quality improvement activities in six major federal programs,21 concluded that the federal government must assume a strong leadership role in quality improvement:
By exercising its roles as purchaser, regulator, provider of health services, and sponsor of applied health services research, the federal government has the necessary influence to direct the attention and resources of the health care sector in pursuit of quality. There is no other stakeholder with such a combination of roles and influence. (IOM, 2002:x)
Because coordination of care is one dimension of quality, the federal government needs to exercise leadership and model coordination and collaboration in general, mental, and substance-use health care. This coordination and collaboration should be practiced across the separate Centers
for Substance Abuse Prevention and Treatment and Center for Mental Health Services within SAMHSA, across SAMHSA and other operating divisions of the Department of Health and Human Services (DHHS), across DHHS and other departments, and across the public and private sectors.
A strong example of such leadership in coordination and collaboration is found in the federal action agenda, Transforming Mental Health Care in America, formulated to implement the recommendations of the President’s New Freedom Commission on Mental Health. This action agenda is the collaborative product of 12 DHHS agencies (the Administration on Aging, Administration for Children and Families, Agency for Healthcare Research and Quality, Centers for Disease Control and Prevention, Centers for Medicare and Medicaid Services, Health Resources and Services Administration, Indian Health Service, National Institutes of Health, Office for Disability, Office for Civil Rights, Office of Public Health and Science, and SAMHSA), five other departments (Education, Housing and Urban Development, Justice, Labor, and Veterans Affairs), and the Social Security Administration. To guide the implementation of this agenda, DHHS is leading an intra- and interagency Federal Executive Steering Committee composed of high-level representatives from DHHS agencies and other federal departments that serve individuals with mental illnesses (SAMHSA, 2005). This strong model of collaboration and coordination could be strengthened by including on the action agenda items addressing the substance-use problems and illnesses that so frequently accompany mental illnesses, and by including more explicitly in implementation activities the SAMHSA centers and state agencies responsible for planning and arranging for care for co-occurring substance-use illnesses. Similarly engaging key private-sector entities, especially those in the general health sector who deliver much care for mental illnesses, would strengthen this collaborative approach and help break down the separations discussed earlier in this chapter between mental and substance-use illnesses, between specialty M/SU and general health care, and between the public and private sectors.
New Mexico provides one example of processes now under way to achieve such coordination and collaboration at the state level (see Box 5-1). While the fruits of this initiative are not yet known, these efforts are testimony to the critical need for such coordination and collaboration at the policy level and the importance of high-level leadership in meeting this need.
|
BOX 5-1 In 2003 the Governor of New Mexico identified as a major policy issue the fact that New Mexico’s behavioral health system (like others across the United States) reflected the problems cited in the report of the President’s New Freedom Commission: insufficient and inappropriate services, uneven access and quality, failure to maximize resources across funding streams, duplication of effort, higher administrative costs for providers, and overall fragmentation that makes service systems difficult to access and manage effectively. After consultation with key cabinet secretaries, the governor announced a new approach to address these problems through the creation of a high-level policy collaborative. This executive-level body was charged specifically with achieving better access, better services, and better value for taxpayer dollars in mental and substance-use health care. This group, consisting of 17 members including the heads of 15 agencies, was established in law by the New Mexico legislature effective May 2004 and charged with creating a single behavioral health (mental and substance-use treatment) delivery system across multiple state agencies and funding sources. The vision that guided this effort, based on months of public participation, was that this single system must support recovery and resiliency so that consumers can participate fully in the life of their communities. The agencies forming the collaborative reflected these broad goals and included those responsible for such areas as housing, corrections, labor, and education, as well as primary health and human services agencies. To ensure that this broad perspective would be reflected in the collaborative’s actions, the group decided that decisions would be made whenever feasible by consensus, but that if votes were required, each agency would have a single vote regardless of its budget or size. The group is cochaired by the secretary of Human Services and (in alternating years) the secretary of Children, Youth, and Families or the secretary of Health. Such a broad policy vision clearly also required that the collaborative develop coordinated structures for the efficient management of a broad range of funds and services. Therefore, a request for proposals was issued, and a contractor was selected as the single statewide entity to manage approximately $350,000,000 in cross-agency funds for the first phase of the change process. In addition, the collaborative has formed senior-level coordination teams, including one focused specifically on cross-cutting policy issues. A single Behavioral Health Planning Council has also been established to form an ongoing partnership with consumers, families, providers, and state agencies in keeping the system on track. In addition, local collaboratives are being formed with cross-agency state assistance across all of the state’s 13 judicial districts, as well as in its Native American communities, to ensure strong feedback and coordination involving stakeholders at the local level as a guide for collaborative state policies and actions. The overall transformation also is being carefully evaluated by multiple groups to help guide future work of this broad policy nature. SOURCE: Personal communication, Leslie Tremaine, Behavioral Health Coordinator, New Mexico BH Collaborative, on July 28, 2005. |
Recommendations
To address the complex obstacles to care coordination and collaboration described above, the committee recommends a set of related actions to be undertaken by individual clinicians, health care organizations, health plans, health care purchasers, accrediting organizations, and policy officials.
Recommendation 5-1. To make collaboration and coordination of patients’ M/SU health care services the norm, providers of the services should establish clinically effective linkages within their own organizations and between providers of mental health and substance-use treatment. The necessary communications and interactions should take place with the patient’s knowledge and consent and be fostered by:
-
Routine sharing of information on patients’ problems and pharmacologic and nonpharmacologic treatments among providers of M/SU treatment.
-
Valid, age-appropriate screening of patients for comorbid mental, substance-use, and general medical problems in these clinical settings and reliable monitoring of their progress.
Recommendation 5-2. To facilitate the delivery of coordinated care by primary care, mental health, and substance-use treatment providers, government agencies, purchasers, health plans, and accreditation organizations should implement policies and incentives to continually increase collaboration among these providers to achieve evidence-based screening and care of their patients with general, mental, and/or substance-use health conditions. The following specific measures should be undertaken to carry out this recommendation:
-
Primary care and specialty M/SU health care providers should transition along a continuum of evidence-based coordination models from (1) formal agreements among mental, substance-use, and primary health care providers; to (2) case management of mental, substance-use, and primary health care; to (3) collocation of mental, substance-use, and primary health care services; and then to (4) delivery of mental, substance-use, and primary health care through clinically integrated practices of primary and M/SU care providers. Organizations should adopt models to which they can most easily transition from their current structure, that best meet the needs of their patient populations, and that ensure accountability.
-
DHHS should fund demonstration programs to offer incentives for the transition of multiple primary care and M/SU practices along this continuum of coordination models.
-
Purchasers should modify policies and practices that preclude paying for evidence-based screening, treatment, and coordination of M/SU care and require (with patients’ knowledge and consent) all health care organizations with which they contract to ensure appropriate sharing of clinical information essential for coordination of care with other providers treating their patients.
-
Organizations that accredit mental, substance-use, or primary health care organizations should use accrediting practices that assess, for all providers, the use of evidence-based approaches to coordinating mental, substance-use, and primary health care.
-
Federal and state governments should revise laws, regulations, and administrative practices that create inappropriate barriers to the communication of information between providers of health care for mental and substance-use conditions and between those providers and providers of general care.
With respect to the need for purchasers to modify practices that preclude paying for evidence-based screening, treatment, and coordination of health care for mental and substance-use conditions, the committee calls particular attention to practices that prevent primary care providers from receiving payment for delivery of the M/SU health services they provide and the failure of some benefit plans to cover certain evidence-based treatments.
Recommendation 5-3. To ensure the health of persons for whom they are responsible, M/SU providers should:
-
Coordinate their services with those of other human services and education agencies, such as schools, housing and vocational rehabilitation agencies, and providers of services for older adults.
-
Establish referral arrangements for needed services.
Providers of services to high-risk populations—such as child welfare agencies, criminal and juvenile justice agencies, and long-term care facilities for older adults—should use valid, age-appropriate, and culturally appropriate techniques to screen all entrants into their systems to detect M/SU problems and illnesses.
Recommendation 5-4. To provide leadership in coordination, DHHS should create a high-level, continuing entity reporting directly to the secretary to improve collaboration and coordination across its mental,
substance-use, and general health care agencies, including the Substance Abuse and Mental Health Services Administration; the Agency for Healthcare Research and Quality; the Centers for Disease Control and Prevention; and the Administration for Children, Youth, and Families. DHHS also should implement performance measures to monitor its progress toward achieving internal interagency collaboration and publicly report its performance on these measures annually. State governments should create analogous linkages across state agencies.
With respect to recommendation 5-4, the committee notes that this recommendation echoes the call made in the report Leadership by Example: Coordinating Government Roles in Improving Health Care Quality for Congress to consider directing the Secretary of DHHS to produce an annual progress report “detailing the collaborative and individual efforts of the various government programs to redesign their quality enhancement processes” (IOM, 2002:11).
REFERENCES
Aarons GA, Brown SA, Hough RL, Garland AF, Wood PA. 2001. Prevalence of adolescent substance use disorders across five sectors of care. Journal of the American Academy of Child & Adolescent Psychiatry 40(4):419–426.
Abraham HD, Degli-Esposti S, Marino L. 1999. Seroprevalence of hepatitis C in a sample of middle class substance abusers. Journal of Addictive Diseases 18(4):77–87.
AHRQ (Agency for Healthcare Research and Quality). 2002–2003. U.S. Preventive Services Task Force Ratings: Strength of Recommendations and Quality of Evidence. Guide to Clinical Preventive Services. Periodic updates, 2002–2003. Rockville, MD: AHRQ. [Online]. Available: http:www.ahrq.gov/clinic/3rduspstf/ratings.htm [accessed February 28, 2005].
Alter MJ. 1999. Hepatitis C virus infection in the United States. Journal of Hepatology 31 (Supplement 1):88–91.
American Academy of Child & Adolescent Psychiatry and Child Welfare League of America. 2003. Policy Statement: AACAP/CWLA Policy Statement on Mental Health and Use of Alcohol and Other Drugs, Screening and Assessment of Children in Foster Care. [Online]. Available: http://www.aacap.org/publications/policy/collab02.htm [accessed December 2, 2005].
American Diabetes Association, American Psychiatric Association, American Association of Clinical Endocrinologists, North American Association for the Study of Obesity. 2004. Consensus development conference on antipsychotic drugs and obesity and diabetes. Journal of Clinical Psychiatry 65(2):267–272.
Anonymous. 2004. Depression in Primary Care—Linking Clinical & System Strategies. [Online]. Available: http://www.wpic.pitt.edu/dppc [accessed December 23, 2004].
Badamgarev E, Weingarten S, Henning J, Knight K, Hasselblad V, Gano A Jr, Ofman J. 2003. American Journal of Psychiatry 160(12):2080–2090.
Baggs J, Schmitt M. 1988. Collaboration between nurses and physicians. IMAGE: Journal of Nursing Scholarship 20(3):145–149.
Baggs J, Schmitt M. 1997. Nurses’ and resident physicians’ perception of the process of collaboration in an MICU. Research in Nursing & Health 20(1):71–80.
Baggs J, Schmitt M, Mushlin A, Mitchell PH, Eldredge DH, Oakes D, Hutson AD. 1999. Association between nurse-physician collaboration and patient outcomes in three intensive care units. Critical Care Medicine 27(9):1991–1998.
Baldridge National Quality Program. 2003. Criteria for Performance Excellence. National Institute of Standards and Technology, U.S. Department of Commerce. [Online]. Available: http://www.quality.nist.gov/PDF_files/2003_Business_Criteria.pdf [accessed April 24, 2003].
Barry CL, Gabel JR, Frank RG, Hawkins S, Whitmore HH, Pickreign JD. 2003. Design of mental health benefits: Still unequal after all these years. Health Affairs 22(5):127–137.
Berwick DM. 1998. Keynote Address: Taking action to improve safety: How to increase the odds of success. 1998 Conference: Enhancing Patient Safety and Reducing Errors in Health Care. National Patient Safety Foundation. Rancho Mirage, CA, on November 8–10, 1998. [Online]. Available: http://www.npsf.org/congress_archive/1998/html/keynote.html [accessed December 16, 2004].
Bodenheimer T, Wagner EH, Grumbach K. 2002. Improving primary care for patients with chronic illness. Journal of the American Medical Association 288(14):1775–1779.
Brailer DJ, Terasawa E. 2003. Use and Adoption of Computer-Based Patient Records in the United States. Presentation to IOM Committee on Data Standards for Patient Safety on January 23, 2003. [Online]. Available: http://www.iom.edu/file.asp?id=10988 [accessed October 17, 2004].
Brunette MF, Drake RE, Marsh BJ, Torrey WC, Rosenberg SD. 2003. Five-Site Health and Risk Study Research Committee. Responding to blood-borne infections among persons with severe mental illness. Psychiatric Services 54(6):860–865.
Burns BJ, Phillips SD, Wagner R, Barth RP, Kolko DJ, Campbel Y, Landsverk J. 2004. Mental health need and access to mental health services by youths involved with child welfare: A national survey. Journal of the American Academy of Child and Adolescent Psychiatry 43(8):960–970.
Bush DE, Ziegeldtein RC, Patel UV, Thombs BD, Ford DE, Fauerbach JA, McCann UD, Stewart KJ, Tsilidis KK, Patel AL, Feuerstein CJ, Bass EB. 2005. Post-Myocardial Infarction Depression. Summary. AHRQ Publication Number 05-E018-1. Evidence Report/Technology Assessment Number 123. Rockville, MD: Agency for Healthcare Research and Quality.
Canagasaby A, Vinson DC. 2005. Screening for hazardous or harmful drinking using one or two quantity-frequency questions. Alcohol and Alcoholism 40(3):208–213.
CARF (Commission on Accreditation of Rehabilitation Facilities). 2005. Standards Manual with Survey Preparation Questions, July 2005–June 2006. Washington, DC: CARF.
Carlsson S, Hammar N, Efendic S, Persson PG, Ostenson CG, Grill V. 2000. Alcohol consumption, Type 2 diabetes mellitus and impaired glucose tolerance in middle-aged Swedish men. Diabetes Medicine 17(11):776–781.
CDC (Centers for Disease Control and Prevention). 2001. HIV Prevention Strategic Plan through 2005. [Online]. Available: www.cdc.gov/nchstp/od/hiv_plan [accessed October 13, 2005].
COA (Council on Accreditation for Children and Family Services, Inc). 2001. Standards and Self-Study Manual, 7th ed., version1.1. New York: COA.
Cocozza JJ. 2004. Juvenile Justice Systems: Improving Mental Health Treatment Services for Children and Adolescents. Paper commissioned by the Institute of Medicine Committee on Crossing the Quality Chasm: Adaptation to Mental Health and Addictive Disorders. Available from the Institute of Medicine.
Cocozza JJ, Skowyra K. 2000. Youth with mental disorders: Issues and emerging responses. Juvenile Justice 7(1):3–13.
Conigliaro J, Gordon AJ, McGinnis KA, Rabeneck L, Justice AC. 2003. How harmful is hazardous alcohol use and abuse in HIV infection: Do health care providers know who is at risk? JAIDS: Journal of Acquired Immune Deficiency Syndromes 33(4):521–525.
Cook RI, Render M, Woods DD. 2000. Gaps in the continuity of care and progress on patient safety. British Medical Journal 320(7237):791–794.
Corrao G, Rubbiati L, Bagnardi V, Zanbon A, Poikolainen K. 2000. Alcohol and coronary heart disease: A meta-analysis. Addiction 95(10):1505–1523.
Curley C, McEachern JE, Speroff T. 1998. A firm trial of interdisciplinary rounds on the inpatient medical wards: An intervention designed using continuous quality improvement. Medical Care 36(8 Supplement):AS4–AS12.
D’Aunno TA. 1997. Linking substance abuse treatment and primary health care. In: Egertson JA, Fox DM, Leshman AI, eds. Treating Drug Users Effectively. Malden, MA: Blackwell. Pp. 311–351.
Davenport T, DeLong D, Beers M. 1998. Successful knowledge management projects. Sloan Management Review Winter(1):43–57.
De Alba I, Samet J, Saitz R. 2004. Burden of medical illness in drug- and alcohol-dependent persons without primary care. The American Journal on Addiction 13(1):33–45.
DHHS (U.S. Department of Health and Human Services). 1999. Mental Health: A Report of the Surgeon General. Rockville, MD: DHHS.
Dietrich AJ, Oxman TE, Williams JW Jr, Kroenke K, Schulberg HC, Bruce M, Barry SL. 2004. Going to scale: Re-engineering systems for primary care treatment of depression. Annals of Family Medicine 2(4):301–304.
Disch J, Beilmann G, Ingbar D. 2001. Medical directors as partners in creating healthy work environments. AACN Clinical Issues 12(3):366–377.
Ditton P. 1999. Mental Health and Treatment of Inmates and Probationers. Bureau of Justice Statistics, NCJ 174463. Washington, DC: Department of Justice.
Donohue J, Frank RG. 2000. Medicaid behavioral health carve-outs: A new generation of privatization decisions. Harvard Review of Psychiatry 8(5):231–241.
Druss B, Rohrbaugh R, Levinson C, Rosenheck R. 2001. Integrated medical care for patients with serious psychiatric illness: A randomized trial. Archives of General Psychiatry 58(9):861–868.
Edlund MJ, Unutzer J, Wells KB. 2004. Clinician screening and treatment of alcohol, drug, and mental problems in primary care: Results from Healthcare for Communities. Medical Care 42(12):1158–1166.
Fein G, Fletcher DJ, Di Sclafani V. 1998. Effect of chronic alcohol abuse on the CNS morbidity of HIV disease. Alcoholism: Clinical and Experimental Research 22(5 Supplement): 196S–200S.
Feldman MD, Ong MK, Lee DL, Perez-Stable EJ. 2005. Realigning economic incentives for depression care at UCSF. Administration and Policy in Mental Health and Mental Health Services Research 33(1):35–39.
Feldman S. 2003. Choices and challenges. In: Feldman S, ed. Managed Behavioral Health Services: Perspectives and Practice. Springfield, IL: Charles C. Thomas Publisher, Pp. 3–23.
Fox A, Oss M, Jardine E. 2000. OPEN MINDS Yearbook of Managed Behavioral Health Market Share in the United States 2000-2001. Gettysburg, PA: OPEN MINDS.
Friedmann PD, D’Aunno TA, Jin L, Alexander J. 2000a. Medical and psychosocial services in drug abuse treatment: Do stronger linkages promote client utilization? HSR: Health Services Research 35(2):443–465.
Friedmann PD, McCulloch D, Chin MH, Saitz R. 2000b. Screening and intervention for alcohol problems: A national survey of primary care physicians and psychiatrists. Journal of General Internal Medicine 15(2):84–91.
Friedmann PD, McCullough D, Saitz R. 2001. Screening and intervention for illicit drug abuse: A national survey of primary care physicians and psychiatrists. Archives of Internal Medicine. 161(2):248–251.
Fronstin P. 2003. Sources of Health Insurance and Characteristics of the Uninsured: Analysis of the March 2003 Current Population Survey. Washington, DC: Employee Benefit Research Institute.
GAO (U.S. General Accounting Office). 2003. Child Welfare and Juvenile Justice: Federal Agencies Could Play a Stronger Role in Helping States Reduce the Number of Children Placed Solely to Obtain Mental Health Services. GAO-03-397. [Online]. Available: http://www.gao.gov/new.items/d03397.pdf [accessed October 25, 2004].
Garfein RS, Vlahov D, Galai N, Doherty MC, Nelson KE. 1996. Viral infections in short-term injection drug users and the prevalence of the hepatitis C, hepatitis B, human immunodeficiency, and human T-lymphotropic viruses. American Journal of Public Health 86(5):655–661.
Gilbody S, Whitty P, Grimshaw J, Thomas R. 2003. Educational and organizational interventions to improve the management of depression in primary care: A systematic review. JAMA 289(23):3145–3151.
Gittell J, Fairfield K, Bierbaum B, Head W, Jackson R, Kelly M, Laskin R, Lipson S, Siliski J, Thornhill T, Zuckerman J. 2000. Impact of relational coordination on quality of care, postoperative pain and functioning, and length of stay. Medical Care 38(8):807–819.
Goff DC, Cather C, Evins AE, Henderson DC, Freudenreich O, Copeland PM, Bierer M, Duckworth K, Sacks FM. 2005. Medical morbidity and mortality in schizophrenia: Guidelines for psychiatrists. Journal of Clinical Psychiatry 66(2):183–194.
Goldstrom I, Jaiquan F, Henderson M, Male A, Mandersheid R. 2001. The Availability of Mental Health Services to Young People in Juvenile Justice Facilities: A National Survey. In: Manderscheid RW, Henderson MJ, eds. Mental Health, United States 2000. (SMA) 01-3537. Washington, DC: U.S. Government Printing Office.
Graber M, Bergus G, Dawson J, Wood G, Levy B, Levin I. 2000. Effect of a patient’s psychiatric history on physicians’ estimation of probability of disease. Journal of General Internal Medicine 15(3):204–206.
Grant BF, Stinson FS, Dawson DA, Chou P, Dufour MC, Compton W, Pickering RP, Kaplan K. 2004a. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Archives of General Psychiatry 61(8):807–816.
Grant BF, Stinson FS, Dawson DA, Chou SP, Ruan WJ, Pickering RP. 2004b. Co-occurrence of 12-month alcohol and drug use disorders and personality disorders in the United States: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Archives of General Psychiatry 61(4):361–368.
Grazier KL, Eselius LL. 1999. Mental health carve-outs: Effects and implications. Medical Care Research and Review 56 (Supplement 2):37–59.
Green AI, Canuso CM, Brenner MJ, Wojcik JD. 2003. Detection and management of comorbidity in patients with schizophrenia. Psychiatric Clinics of North America 26(1):115–138.
Grisso T. 2004. Double Jeopardy: Adolescent Offenders with Mental Disorders. Chicago, IL: University of Chicago Press.
Haney C, Specter D. 2003. Treatment rights in uncertain legal times. In: Ashford JB, Sales BD, Reid WH, eds. Treating Adult and Juvenile Offenders with Special Needs. Washington, DC: American Psychological Association. Pp. 51–80.
Harrison PM, Karberg JC. 2004. Prison and Jail Inmates at Midyear 2003. Bureau of Justice Statistics Bulletin, Office of Justice Programs, NCJ 203947. Washington, DC: U.S. Department of Justice. [Online]. Available: http://www.ojp.usdoj.gov/bjs/pub/pdf/pjim03.pdf [accessed August 4, 2004].
Harter MC, Conway KP, Merikangas KR. 2003. Associations between anxiety disorders and physical illness. European Archives of Psychiatry and Clinical Neurosciences 253(6): 313–320.
Havassy BE, Alvidrez J, Own KK. 2004. Comparisons of patients with comorbid psychiatric and substance use disorders. Implications for treatment and service delivery. American Journal of Psychiatry 161(1):139–145.
Henningsen P, Zimmerman T, Sattel H. 2003. Medically unexplained physical symptoms, anxiety, and depression: A meta-analytic review. Psychosomatic Medicine 65(4):528–533.
Hogan MF. 1999. Public-sector mental health care: New challenges. Health Affairs 18(5): 106–111.
Hughes TA, Wilson DJ, Beck AJ. 2001. Trends in State Parole, 1990–2000. Bureau of Justice Statistics, NCJ 184735. Washington, DC: Department of Justice. [Online]. Available: http://www.Ojp.Usdoj.Gov/Bjs/Pub/Pdf/Tsp00.Pdf [accessed July 31, 2005].
Hurlburt MS, Leslie LK, Landsverk J, Barth RP, Burns BJ, Gibbons RD, Slymen DJ, Zhang J. 2004. Contextual predictors of mental health service use among children open to child welfare. Archives of General Psychiatry 61(12):1217–1224.
Hutchinson AB, Foster EM. 2003. The effect of Medicaid managed care on mental health care for children: A review of the literature. Mental Health Services Research 5(1): 39–54.
IOM (Institute of Medicine). 1997. Edmunds M, Frank, R, Hogan M, McCarty D, Robinson-Beale R, Weisner C, eds. Managing Managed Care—Quality Improvement in Behavioral Health. Washington, DC: National Academy Press.
IOM. 2001. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academy Press.
IOM. 2002. Eden J, Smith BM, eds. Leadership by Example: Coordinating Government Roles in Improving Health Care Quality. Washington, DC: The National Academies Press.
IOM. 2003a. Corrigan JM, Adams K, eds. Priority Areas for National Attention: Transforming Health Care Quality. Washington, DC: The National Academies Press.
IOM. 2003b. Key Capabilities of an Electronic Health Record System. Washington, DC: The National Academies Press.
IOM. 2004a. Fostering interdisciplinary collaboration. Keeping Patients Safe: Transforming the Work Environment of Nurses. Washington, DC: The National Academies Press. Pp. 212–217.
IOM. 2004b. Page A, ed. Keeping Patients Safe: Transforming the Work Environment of Nurses. Washington, DC: The National Academies Press.
Jaycox LH, Morral AR, Juvonen J. 2003. Mental health and medical problems and service use among adolescent substance users. Journal of the American Academy of Child & Adolescent Psychiatry 42(6):701–719.
JCAHO (Joint Commission for the Accreditation of Healthcare Organizations). 2004. Comprehensive Accreditation Manual for Behavioral Health Care 2004–2005. Oakbrook Terrace, IL: Joint Commission Resources.
Katon W. 2003. Clinical and health services relationships between major depression, depressive symptoms, and general medical illness. Biological Psychiatry 54(3):216–226.
Katon W, Von Korff M, Lin E, Simon G. 2001. Rethinking practitioner roles in chronic illness: The specialist, primary care physician, and the practice nurse. General Hospital Psychiatry 23(3):138–144.
Kessler RC. 2004. The epidemiology of dual diagnosis. Biological Psychiatry 56(10): 730–737.
Kessler RC, Nelson CB, McGonagle KA, Edlund MJ, Frank, RG, Leaf PJ. 1996. The epidemiology of co-occurring addictive and mental disorders: Implications for prevention and service utilization. American Journal of Orthopsychiatry 66(1):17–31.
Kessler RC, Costello EJ, Merikangas KR, Ustun TB. 2001. Psychiatric epidemiology: Recent advances and future directions. In: Manderscheid RW, Henderson MJ, eds. Mental Health, United States, 2000. DHHS Publication Number: (SMA) 01-3537. Washington, DC: U.S. Government Printing Office. Pp. 29–42.
Knaus W, Draper E, Wagner D, Zimmerman J. 1986. An evaluation of outcome from intensive care in major medical centers. Annals of Internal Medicine 104(3):410–418.
Kroenke K. 2003. Patients presenting with somatic complaints: Epidemiology, psychiatric comorbidity and management. International Journal of Methods in Psychiatric Research 12(1):34–43.
Kroenke K, Taylor-Vaisey A, Dietrich AJ, Oxman TE. 2000. Interventions to improve provider diagnosis and treatment of mental disorders in primary care: A critical review of the literature. Psychosomatics 41(1):39–52.
Landsverk J. 2005. Improving the Quality of Mental Health and Substance Use Treatment Services for Children Involved in Child Welfare. Paper commissioned by the Institute of Medicine Committee on Crossing the Quality Chasm: Adaptation to Mental Health and Addictive Disorders.
Leslie LK, Hurlburt MS, Landsverk J, Rolls JA, Wood PA, Kelleher KJ. 2003. Comprehensive assessments for children entering foster care: A national perspective. Pediatrics 112(1): 134–142.
Marshall M, Gray A, Lockwood A, Green R. 2004. Case Management for People with Severe Mental Disorders (Cochrane Review). Chichester, UK: John Wiley & Sons. Issue 4.
Masi D. 2004. Issues in Delivering Mental Health and Substance Abuse Services through Employee Assistance Programs (EAPs). Testimony to the Institute of Medicine Committee on Crossing the Quality Chasm: Adaptation to Mental Health and Addictive Disorders on November 15, 2004. Irvine, California.
Masi D, Altman L, Benayon C, Healy H, Jorgensen DG, Kennish R, Keary D, Thompson C, Marsden B, McCann B, Watkins G, Williams C. 2004. Employee assistance programs in the year 2002. In: Manderscheid RW, Henderson MJ, eds. Mental Health, United States, 2002. DHHS Publication Number: SMA 3938. Rockville, MD: Substance Abuse and Mental Health Services Administration.
Mertens JR, Lu YW, Parthasarathy S, Moore C, Weisner CM. 2003. Medical and psychiatric conditions of alcohol and drug treatment patients in an HMO: Comparison with matched controls. Archives of Internal Medicine 163(20):2511–2517.
Metzner JL. 2002. Class action litigation in correctional psychiatry. Journal of the American Academy of Psychiatry and the Law 30(1):19–29.
Mickus M, Colenda CC, Hogan AJ. 2000. Knowledge of mental health benefits and preferences for type of mental health providers among the general public. Psychiatric Services 51(2):199–202.
Miller AL, Crismon ML, Rush AJ, Chiles J, Kashner TM, Toprac M, Carmody T, Biggs M, Shores-Wilson K, Chiles J, Witte B, Bow-Thomas C, Velligan DI, Trivedi M, Suppes T, Shon S. 2004. The Texas medication algorithm project: Clinical results for schizophrenia. Schizophrenia Bulletin 30(3):627–647.
Miller CL, Druss BG, Dombrowski EA, Rosenheck RA. 2003. Barriers to primary medical care at a community mental health center. Psychiatric Services 54(8):1158–1160.
Moore RD, Keruly JC, Chaisson RE. 2004. Differences in HIV disease progression by injecting drug use in HIV-infected persons in care. JAIDS Journal of Acquired Immune Deficiency Syndromes 35(1):46–51.
NASMHPD, NASADAD (National Association of State Mental Health Program Directors and National Association of State Alcohol and Drug Abuse Directors). 2002. Final report of the NASMHPD-NASADAD Task Force on Co-Occurring Mental Health and Substance Use Disorders. Exemplary Methods of Financing Integrated Service Programs for Persons with Co-Occurring Mental Health and Substance Use Disorders. Alexandria, VA and Washington, DC: NASMHPD, NASADAD. [Online]. Available: http://www.nasmhpd.org/general_files/publications/NASADAD%20NASMHPD%20PUBS/Exemplary%20methods_3.pdf [accessed August 14, 2005].
NCQA (National Committee for Quality Assurance). 2004. Standards and Guidelines for the Accreditation of MBOs. Washington, DC: NCQA.
New Freedom Commission on Mental Health. 2003. Achieving the Promise: Transforming Mental Health Care in America. Final Report. DHHS Publication Number SMA-03-3832. Rockville, MD: U.S. Department of Health and Human Services.
NIAAA (National Institute on Alcohol Abuse and Alcoholism). 2000. 10th Special Report to the U.S. Congress on Alcohol and Health. [Online]. Available: http://www.niaaa.nih.gov/publications/10report [accessed May 6, 2005].
NIAAA. 2002. Screening for Alcohol Problems: An Update. Alcohol Alert. 56. [Online]. Available: http://pubs.niaaa.nih.gov/publications/aa56.htm [accessed October 13, 2005].
NIAAA. 2005. Helping Patients Who Drink Too Much: A Clinician’s Guide. [Online]. Available: http://pubs.niaaa.nih.gov/publications/Practitioner/CliniciansGuide2005/guide.pdf [accessed October 12, 2005].
Palepu A, Tyndall M, Yip B, Shaughnessy MV, Hogg RS, Montaner JSG. 2003. Impaired virologic response to highly active antiretroviral therapy associated with ongoing injection drug use. JAIDS Journal of Acquired Immune Deficiency Syndromes 32(5): 522–526.
Peele PB, Lave JR, Kelleher KJ. 2002. Exclusions and limitations in children’s behavioral health care coverage. Psychiatric Services 53(5):591–594.
Pignone MP, Gaynes BN, Rushton JL, Burchell CM, Orleans TC, Mulrow CD, Lohr KN. 2002. Screening for depression in adults: A summary of the evidence for the U.S. Preventive Services Task Force. Annals of Internal Medicine 136(10):765–776.
Pincus HA. 2003. The future of behavioral health and primary care: Drowning in the mainstream or left on the bank? Psychosomatics 44(1):1–11.
Pincus HA, Hough L, Houtsinger JK, Rollman BL, Frank R. 2003. Emerging models of depression care: Multi-level (‘6P’) strategies. International Journal of Methods in Psychiatric Research 12(1):54–63.
Rice A. 2000. Interdisciplinary collaboration in health care: Education, practice, and research. National Academies of Practice Forum: Issues in Interdisciplinary Care 2(1): 59–73.
Rollman BL, Belnap BH, Reynolds CF, Schulberg HC, Shear MK. 2003. A contemporary protocol to assist primary care physicians in the treatment of panic and generalized anxiety disorders. General Hospital Psychiatry 25(2):74–82.
Rones M, Hoagwood K. 2000. School-based mental health services: A research review. Clinical Child and Family Psychology Review 3(4):223–241.
Rosenberg SD, Goodman LA, Osher FC, Swartz MS, Essock SM, Butterfield MI, Constantine NT, Wolford GL, Salyers MP. 2001. Prevalence of HIV, hepatitis B, and hepatitis C in people with severe mental illness. American Journal of Public Health 91(1):31–37.
Rost K, Smith R, Matthews DB, Guise B. 1994. The deliberate misdiagnosis of major depression in primary care. Archives of Family Medicine 3(4):333–337.
Rush AJ, Crismon ML, Kashner TM, Toprac MG, Carmody TJ, Trivedi MH, Suppes T, Miller AL, Biggs MM, Shores-Wilson K, Witte BP, Shon SP, Rago WV, Altshuler KZ, TMAP Research Group. 2003. Texas Medication Algorithm Project, phase 3 (TMAP-3): Rationale and study design. Journal of Clinical Psychiatry 64(4):357–369.
Saitz R, Mulvey KP, Plough A, Samet JH. 1997. Physician unawareness of serious substance abuse. American Journal of Drug and Alcohol Abuse 23(3):343–354.
Saitz R, Friedman PD, Sullivan LM, Winter MR, Lloyd-Travaglini C, Moskowitz MA, Samet J. 2002. Professional satisfaction experienced when caring for substance-abusing patients: Faculty and resident physician perspectives. Journal of General Internal Medicine 17(5):373–376.
Samet JH, Friedmann P, Saitz R. 2001. Benefits of linking primary medical care and substance abuse services: Patient, provider, and societal perspectives. Archives of Internal Medicine 161(1):85–91.
Samet JH, Horton NJ, Meli S, Freedberg KA, Palepu A. 2004. Alcohol consumption and antiretroviral adherence among HIV-infected persons with alcohol problems. Alcoholism: Clinical and Experimental Research 28(4):572–577.
SAMHSA (Substance Abuse and Mental Health Services Administration). 2004. Results from the 2003 National Survey on Drug Use and Health: National Findings. DHHS Publication Number SMA 04-3964. NSDUH Series H-25. Rockville, MD: SAMHSA.
SAMHSA. 2005. Transforming Mental Health Care in America. The Federal Action Agenda: First Steps. [Online]. Available: http://www.samhsa.gov/Federalactionagenda/NFC_TOC.aspx [accessed July 23, 2005].
SAMHSA. undated. Report to Congress on the Prevention and Treatment of Co-Occurring Substance Abuse Disorders and Mental Disorders. [Online]. Available: http://www.samhsa.gov/reports/congress2002/CoOccurringRpt.pdf [accessed April 25, 2004].
Schmitt M. 2001. Collaboration improves the quality of care: Methodological challenges and evidence from U.S. health care research. Journal of Interprofessional Care 15(1): 47–66.
Shortell S, Zimmerman J, Rousseau D, Gillies RR, Wagner DP, Draper EA, Knaus WA, Duffy J. 1994. The performance of intensive care units: Does good management make a difference? Medical Care 32(5):508–525.
Shortell SM, Gillies RR, Anderson DA, Erickson KM, Mitchell JB. 2000. Remaking Health Care in America: The Evolution of Organized Delivery Systems 2nd ed. San Francisco, CA: Jossey-Bass.
Sokol J, Messias E, Dickerson FB, Kreyenbuhl J, Brown CH, Goldberg RW, Dixon LB. 2004. Comorbidity of medical illnesses among adults with serious mental illness who are receiving community psychiatric services. Journal of Nervous and Mental Diseases 192(6): 421–427.
Spitzer RL, Kroenke K, Williams JBW. 1999. Validation and utility of a self-report version of PRIME-MD: The PHQ Primary Care Study. Journal of the American Medical Association 282(18):1737–1744.
Strosahl KD. 2005. Training behavioral health and primary care providers for integrated care: A core competencies approach. In: O’Donohue WT, Byrd M, Cummings N, Henderson D, eds. Behavioral Integrative Care: Treatments That Work in the Primary Care Setting. New York: Brunner-Routledge.
Sullivan G, Koegel P, Kanouse DE, Cournos F, McKinnon K, Young AS, Bean D. 1999. HIV and people with serious mental illness: The public sector’s role in reducing HIV risk and improving care. Psychiatric Services 50(5):648–652.
Teplin L, Abram K, McClelland G, Dulcan M, Mericle A. 2002. Psychiatric disorders in youth in juvenile detention. Archives of General Psychiatry 59(12):1133–1143.
The National Coalition on Health Care, The Institute for Healthcare Improvement. 2002. Curing the System: Stories of Change in Chronic Illness Care. [Online]. Available: http://www.improvingchroniccare.org/ACT_Report_May_2002_Curing_The_System_.pdf [accessed July 24, 2005].
Tyor WR, Middaugh LD. 1999. Do alcohol and cocaine abuse alter the course of HIV-associated dementia complex? Journal of Leukocyte Biology 65(4):475–481.
Unutzer J, Katon W, Williams JW Jr, Callahan CM, Harpole L, Hunkeler EM, Hoffing M, Arean P, Hegel MT, Schoenbaum M, Oishi SM, Langston CA. 2001. Improving primary care for depression in late life. Medical Care 39(8):785–799.
Upshur CC. 2005. Crossing the divide: Primary care and mental health integration. Administration and Policy in Mental Health 32(4):341–355.
Watkins KE, Burnam A, Kung F-Y, Paddock S. 2001. A national survey of care for persons with co-occurring mental and substance use disorders. Psychiatric Services 52(8):1062–1068.
Watkins K, Pincus HA, Tanielian TL, Lloyd J. 2003. Using the chronic care model to improve treatment of alcohol use disorders in primary care settings. Journal of Studies on Alcohol 64(2):209–218.
Weisner C, Mertens J, Parthasarathy S, Moore C, Lu Y. 2001. Integrating primary medical care with addiction treatment: A randomized controlled trial. Journal of the American Medical Association 286(14):1715–1723.
Weist MD, Paternite CE, Adelsheim S. 2005. School-Based Mental Health Services. Paper commissioned by the Institute of Medicine Committee on Crossing the Quality Chasm: Adaptation to Mental Health and Addictive Disorders. Available from Institute of Medicine.
Wierson M, Forehand R, Frame C. 1992. Epidemiology and treatment of mental health problems in juvenile delinquents. Advances in Behavior Research and Therapy 14: 93–120.
Williams JW, Pignone M, Ramirez G, Perez SC. 2002. Identifying depression in primary care: A literature synthesis of case-finding instruments. General Hospital Psychiatry 24(4): 225–237.
Wolff NP. 2004. Law and Disorder: The Case Against Diminished Responsibility. Paper commissioned by the Institute of Medicine Committee on Crossing the Quality Chasm: Adaptation to Mental Health and Addictive Disorders. Center for Mental Health Services & Criminal Justice Research and Edward J. Bloustein School of Planning and Public Policy, Rutgers, the State University of New Jersey. Available from the author.
Zarski JP, Bohn B, Bastie A, Pawlotsky JM, Baud M, Bost-Bezeaux F, Tran van Nhieu J, Seigneurin JM, Buffet C, Dhumeaux D. 1998. Characteristics of patients with dual infection by hepatitis B and C viruses. Journal of Hepatology 28(1):27–33.
Ziguras SJ, Stuart GW. 2000. A meta-analysis of the effectiveness of mental health case management over 20 years. Psychiatric Services 51(11):1410–1421.
Zwarenstein M, Stephenson B, Johnston L. 2000. Case management: Effects on professional practice and health care outcomes. (Protocol) The Cochrane Database of Systematic Reviews 2000, Issue 4. Art. No.: CD002797. DOI: 10.1002/14651858.CD002797.

















































