5
Medical Factors
There are several medical conditions listed in the U.S. Department of Defense (DoD) Instruction 6130.4 that are disqualifying for military service. Some of these are permanent disqualifiers, whereas others are subject to a waiver of disqualification by one or more of the Services. The top five medical disqualifiers accounted for 53 percent of the total medical disqualifications from May 2003 to April 2005 (data provided by U.S. Military Entrance Processing Command, 2005): excessive body mass index (BMI) and body fat (23.3 percent), use of marijuana (12.6 percent), mental health (6.1 percent), lower extremity injury (5.8 percent), and diseases of the lungs (5.3 percent).
Screening for two of these conditions, excessive BMI and body fat and diseases of the lungs and chest, are discussed in this chapter. (Musculoskeletal injury is discussed in Chapter 4, mental health in Chapter 6, and substance abuse in Chapter 7.) The committee decided not to address orthopedic screening because these conditions are diverse, they lack specificity, and the data are sparse and not linked to outcomes. Most orthopedic screening problems are diagnosed by imaging using an X-ray, CT scan, or MRI. These techniques identify the obvious problems (i.e., a broken pelvis); however, many times, when there is pain, there is no visually identifiable disruption in the system. An example of low sensitivity is in the back; 85 to 90 percent of people with back pain have no identifiable problem via imaging and 10-15 percent of people without back pain have a problem identifiable through imaging. The injury conditions covered in this chapter, such as stress fractures, are easily identifiable by clinical examination or self-report of previous history of problems. Also, as noted
earlier, there is no routine linkage of the medical failure database to administrative data on basic training attrition.
BODY WEIGHT AND COMPOSITION
Prevalence of Overweight in U.S. Population
The percentage of children and adults who are overweight or obese is a growing problem in the United States. Results from the 1999-2002 National Health and Nutrition Examination Survey (NHANES) show that 65 percent of adults are either overweight or obese as defined by BMI.1 This figure represents an increase of 16 percent over the prevalence for these two categories in 1988-1994 (NHANES III) and an increase of 38 percent over the prevalence found in 1978-1980 (NHANES II). Overweight and obesity in adults are defined by the Centers for Disease Control and Prevention (CDC) as a BMI between 25 and 29.9 for overweight and a BMI of 30 or greater for obesity (http://www.cdc.gov). These definitions have been endorsed by more than 50 scientific and medical organizations and are used as indicators of increased health risks (National Heart, Lung, and Blood Institute, 1998).
Overweight and obesity have a strong impact on heath, disability, and quality of life. Most recently, however, Flegal et al. (2005) compared the relative risk of underweight, overweight, and obese categories with normal, healthy weight using data from NHANES I, II, and III with follow-up through 2000. They found that adults in all age groups classified as overweight (BMI = 25.5-29.9) had a slightly lower mortality rate than adults in the average range of 18.5 to 25.5, while individuals above 29.9 and below 18.5 were shown to be at greater risk for mortality than those in the average group.
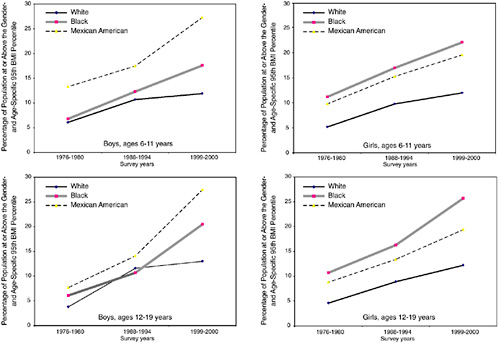
In the youth population, the prevalence of overweight in children ages 6 to 11 and adolescents ages 12 to 19 tripled between 1963 and 1999 (U.S. Department of Health and Human Services, 2001). For these age groups, overweight is determined by sex- and age-specific BMIs that are over the 95th percentile on the CDC growth charts. Trend data provided in the Handbook of Obesity (Bray, Bouchard, and James, 2004) and taken from NHANES III show increases for both boys and girls in these age groups from 1963 to 2000. The prevalence of overweight in 2000 was 15.5 percent for adolescent boys and girls, 16 percent for boys ages 6 to 11, and 14.5 percent for girls ages 6 to 11.
Recently, Hedley et al. (2004) published a study of the prevalence of overweight and obesity among children, adolescents, and adults in the United States between 1999 and 2002. Over the entire period (1999-2002), the percentage of children and adolescents (ages 6 to 19) at risk for overweight was 31 percent. Table 5-1 shows the breakdown of risk for overweight in children and adolescents by gender and ethnicity for those above the 85th percentile (at risk for overweight) and 95th percentile (overweight) based on the CDC growth charts. For boys ages 6 to 19, 31.8 percent (± 1.4 percent) were at risk for overweight and 16.8 percent (± 0.8 percent) were overweight; the results for girls show that 30.3 percent (± 1.3 percent) were at risk for overweight and 15.1 percent (± 1.1 percent) were overweight. The highest prevalence of overweight was among Mexican American boys ages 6 to 11 (26.5 percent: ± 2.2 percent) and non-Hispanic black girls ages 12 to 19 (23.6 percent ± 1.8 percent). The prevalence of risk for overweight for these two groups was 43.9 percent and 41.9 percent, respectively, compared with 27 percent for white youth of both genders. A graphic representation of the trends in childhood and adolescent obesity by gender and ethnicity is shown in Figure 5-1. It can be seen that the prevalence of obesity is increasing faster for Mexican American and black children than for their white counterparts. Among boys, the greatest rate of increase is among Mexican American youth ages 12 to 19; among girls, the greatest rate of increase is among black youth ages 12 to 19. These data suggest that Mexican American and black youth are more likely than white youth to qualify for military service on the basis of current BMI standards.
Data from NHANES 1999-2000 and NHANES 2001-2002 showing the distribution of BMI for the general population of youth ages 16 to 24 indicate that 40 percent have BMIs of over 25 and more that 15 percent have BMIs of 30 and over. What are the implications of these findings for military recruiting?
Current Military Standards
Standards for BMI and body fat are determined by each Service. In order to develop a picture of the BMI distribution for first-term recruits, the committee plotted the BMI means and standard deviations found in military personnel basic training studies against the BMI distribution in the youth population, ages 16 to 24. Data that characterize the youth population were obtained from NHANES 1999-2000 and NHANES 2001-2002 and included 1,531 men and 1,611 women. The downloaded files consist of demographic and BMI variables. Percentile ranks for each group were calculated using SUDAAN. Separate racial analyses were conducted to assess the association between BMI and race. The participants were
TABLE 5-1 Prevalence of Risk for Overweight and Overweight in Children by Sex, Age, and Racial/Ethnic Group: United States, 1999-2002
|
|
|
Prevalence (percentage) (standard error in parentheses) |
|||
|
|
|
At Risk for Overweight and Overweight (BMI for Age ≥ 85th Percentile) |
|||
|
Sex |
Age |
All |
Non-Hispanic White |
Non-Hispanic Black |
Mexican American |
|
Both |
6-19 |
31.0 (1.1) |
|||
|
|
2-5 |
22.6 (1.5) |
20.8 (2.0) |
23.2 (2.3) |
26.3 (2.7) |
|
|
6-11 |
31.2 (1.8) |
28.6 (2.6)b |
33.7 (1.6) |
38.9 (2.2)c |
|
|
12-19 |
30.9 (1.0) |
36.8 (1.3)c |
40.7 (1.6)c |
|
|
Boys |
6-19 |
31.8 (1.4) |
29.2 (2.4)b |
31.0 (1.3)b |
|
|
|
2-5 |
23.0 (2.3) |
21.7 (3.2) |
20.9 (2.5) |
27.6 (3.1) |
|
|
6-11 |
32.5 (2.3) |
29.3 (3.8)b |
29.7 (2.2)b |
|
|
|
12-19 |
31.2 (1.5) |
29.2 (2.3)b |
32.1 (2.1)b |
|
|
Girls |
6-19 |
30.3 (1.3) |
40.1 (1.4)c |
36.6 (1.8)c |
|
|
|
2-5 |
22.3 (1.8) |
20.0 (2.3) |
25.6 (3.0) |
25.0 (3.8) |
|
|
6-11 |
29.9 (2.1) |
27.7 (2.8) |
37.9 (2.8) |
33.8 (2.6) |
|
|
12-19 |
30.5 (1.3) |
41.9 (1.7)c |
39.3 (2.3)c |
|
|
NOTE: BMI = body mass index, calculated as weight in kilograms divided by square of height in meters. BMI was rounded to the nearest tenth. Pregnant girls were excluded. All racial/ethnic groups included in each category are not shown separately. |
|||||
stratified into three groups: non-Hispanic white, non-Hispanic black, and Mexican American. Due to small numbers in the “other” category, those participants were excluded from the racial analysis (n = 274). Nine studies report BMI measures for male recruits, and eight studies report BMI measures for female recruits.
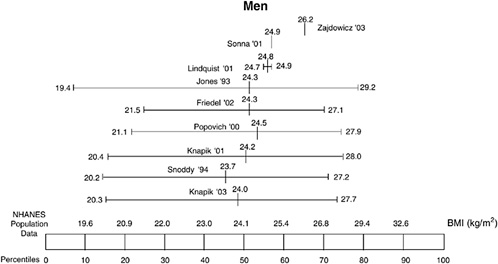
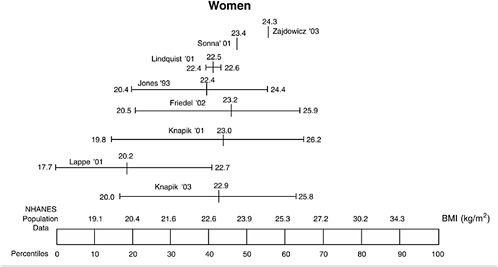
The BMIs of male military recruits relative to the U.S. population of youth ages 16 to 24 are presented in Figure 5-2; the BMIs of female recruits are presented in Figure 5-3. The mean BMI for men ranged from the 45th to 65th percentiles, and the standard deviations ranged from the 10th to 80th percentiles. Thus, the BMI of male military recruits were in the lower 80 percent of the distribution, which corresponds to a BMI of 29.2 kg/m2 or less. For women, the mean BMI ranged from the 20th to 55th percentiles and the standard deviations ranged from the 10th to 65th percentiles. Therefore, female military recruits were in the lower 65 percent of the distribution, which corresponds to a BMI of 26.2 kg/m2 or less. There were no differences in BMI among the three races for men; for
|
Overweight (BMI for Age ≥ 95th Percentile) |
|||
|
All |
Non-Hispanic White |
Non-Hispanic Black |
Mexican American |
|
16.0 (0.8) |
20.5 (0.8)c |
22.2 (1.1)c |
|
|
10.3 (1.2) |
8.6 (1.5) |
8.8 (1.5) |
13.1 (2.0) |
|
15.8 (1.1) |
19.8 (1.4)c |
21.8 (1.7)c |
|
|
16.1 (0.8) |
21.1 (1.2)c |
22.5 (1.3)c |
|
|
16.8 (0.8) |
14.3 (1.1)b |
17.9 (1.0)b |
25.5 (1.3)a |
|
9.9 (1.6) |
8.2 (1.9) |
8.0 (1.8) |
14.1 (2.1) |
|
16.9 (1.3) |
14.0 (1.5)b |
17.0 (1.5)b |
|
|
16.7 (0.9) |
14.6 (1.3)b |
18.7 (1.7) |
24.7 (1.9)c |
|
15.1 (1.1) |
23.2 (1.1)c |
18.5 (1.4)c |
|
|
10.7 (1.5) |
9.1 (2.0) |
9.6 (1.8) |
12.2 (3.4) |
|
14.7 (1.6) |
13.1 (2.3)a |
22.8 (2.5)c |
17.1 (2.0) |
|
15.4 (1.2) |
12.7 (1.8)a |
23.6 (1.8)c |
19.9 (1.9) |
|
aSignificantly different from non-Hispanic blacks at P < .05, with Bonferroni adjustment. bSignificantly different from Mexican Americans at P < .05, with Bonferroni adjustment. cSignificantly different from non-Hispanic whites at P < .05, with Bonferroni adjustment SOURCE: Hedley et al. (2004). |
|||
women, all racial groups differed. Non-Hispanic white women had a lower mean BMI (24.9 kg/m2) compared with non-Hispanic black women (27.7 kg/m2; p = 0.0001) and Mexican American women (26.5 kg/m2; p = 0.004). Non-Hispanic black women had a higher mean BMI than Mexican Americans (p = 0.04).
Body composition screening in the military is a two-stage process. In the first stage, BMI is used. If the recruit is within the acceptable range, than no further screening for body composition is required. If the recruit is above the standard, then a body fat measurement is applied. The current DoD BMI screening standard ranges between 25 and 27.5; a BMI of 25 is the most stringent screen, and a BMI of 27.5 is the least stringent screen recommended for use by the Services. These standards have been justified on the basis of public health data provided by CDC. If a BMI of 25 is used, approximately 40 percent of both men and women ages 16 to 24 could be at risk of disqualification from military service. It is important to note that youth are not significantly affected by the diseases linked to
TABLE 5-2 Maximum Body Mass Index (BMI) for New Recruits and After Entry
|
|
|
Men |
Women |
||
|
Service |
Age |
New Recruit |
After Entry |
New Recruit |
After Entry |
|
Air Force |
All ages |
27.4-27.5 |
27.4-27.5 |
27.5 |
27.4-27.5 |
|
Army |
17-20 |
27.1 |
25.8 |
23.5 |
22.8 |
|
|
21-27 |
27.5 |
26.5 |
24.1 |
23.5 |
|
Marine Corps |
16-20 |
30.7 |
27.5 |
23.6 |
25.0 |
|
|
21-24 |
31.8 |
27.5 |
24.1 |
25.0 |
|
|
25-30 |
31.8 |
27.5 |
|
25.0 |
|
Navy |
All ages |
27.5-27.8 |
27.5 |
26.6 |
26.6 |
|
DoD |
|
27.5 |
|
27.7 |
|
|
SOURCE: http://www.military.com/Recruiting/Content/0,13898,rec_step07_hw,,00.html (accessed June 2005). |
|||||
overweight and obesity in adults. One exception is the incidence of type 2 diabetes in certain Native American Tribes. In general, type 2 diabetes, which appears to be on the rise, is found in less than 1 percent of the youth population. However, there have been no definitive studies to date of the U.S. population (American Diabetes Association, 2000).
Each Service has developed its own height and weight tables. The standards currently in use by each Service for new recruits and for retention after entry are shown in Table 5-2. It can be seen that for men, the Marine Corps has the most liberal screen, whereas the other three Services are at or close to the 27.5 recommended by DoD. Both the Army and the Marine Corps have a more liberal standard for male recruits than for retention after entry. Standards for female recruits are the most stringent in the Army and the Marine Corps. Retention standards for women are more stringent than new recruit standards in the Army, whereas retention standards for female Marines are more liberal than they are for new recruits. There is no rationale given for this variability.
As noted above, if a recruit exceeds the BMI screening standard, body fat measures may be taken. There are DoD-recommended body fat measures for men and women that are calculated by formulas that use height and body circumference (DoD Instruction 1308.3, “DoD Physical Fitness and Body Fat Programs Procedures”). For men, body circumference is determined by subtracting the circumference of the neck from the circumference of the abdomen; for women, the body circumference is deter-
mined by adding the waist and hip circumferences and subtracting the neck circumference. The formulas are as follows:
Men: % body fat = 86.010 × log10 (abdomen II − neck) − 70.041 × log10 (height) + 36.76
Women: % body fat = 163.205 × log10 (waist + hip − neck) − 97.684 × log10 (height) − 78.387
Table 5-3 shows the criteria for maximum body fat percentage of men for each Service. As noted in the table, the Navy and the Marine Corps use the DoD procedure described above; however, the Army uses different formulas and, for women, different measurements. The Air Force is currently using only waist circumference. The DoD-recommended standard for men is 26 percent body fat; the Services range from 18 percent (Marines) to 28 percent (Army, ages 25 to 30). For women, the DoD standard is 36 percent body fat; the Services range from 26 percent (Marines) to 33 percent (Navy).
The DoD formulas are based on those developed for the Navy by James Hodgdon in the early 1980s (Hodgdon and Friedl, 1999). As reported by these authors, these equations have been cross-validated in several research studies. Specifically, they were validated against a four-compartment model that included measures of bone mineral content (DXA) and total body water using bioelectric impedance analysis. The results of the cross-validation for men resulted in a correlation coefficient
TABLE 5-3 Criteria for Maximum Body Fat Percentage
|
|
|
Age |
||
|
Service |
Formula |
17-20 |
21-24 |
25-30 |
|
DoD |
% body fat = 86.010 × log10 (abdomenII circumference − neck circumference) − 70.041 × log10 (height) + 36.76 |
26% |
26% |
26% |
|
Navy |
Same as DoD |
22% |
22% |
22% |
|
Marine Corps |
Same as DoD |
18% |
18% |
18% |
|
Army |
% body fat = 76.46 × log (abdomen circumference − neck circumference) − 68.68 × log(height) + 46.89 |
24% |
26% |
28% |
|
Air Force |
Waist circumference |
— |
— |
— |
of r = .88 and a standard error of measurement of 3.15 percent body fat; for women the correlation coefficient was r = .89 and the standard error of measurement was 3.12 percent body fat. It should be noted that the most important predictors are abdomen circumference in men and waist circumference in women. More recently, Leu and Friedl (2002) examined the relationship between the DoD equations and the Army equations. The correlation between the two equations for men was r = .99, for women r=.86. For women, the DoD equation reduced the percentage of Service members classified as overweight or overfat from 17 percent (using the Army equation) to 12 percent. This result is in line with the prevalence for men of 11 percent.
Body Composition, Injury, and Attrition
It is reasonable to consider that body composition may influence military performance. Studies by Pate and colleagues have examined the relationship between fitness and body composition. In one study, correlations were found between cardiorespiratory fitness and body composition (measured by skinfold) on the order of .32 in boys ages 15 and 16 and .26 in girls in the same age group (Pate and Shepard, 1989); in a second large-scale study, an inverse relationship was demonstrated between running speed and body composition in children ages 6 to 18 ranging from −.179 to −.253 for boys and .156 to −.273 for girls (Pate, Slentz, and Katz, 1989).
Higher weight (and fatness) negatively impact endurance performance in two ways: (1) weight appears in the denominator of the VO2 expression—greater weight is associated with lower weight-relative VO2max; and (2) greater weight increases the energy cost (and required VO2) associated with any level of activity. Therefore, the percentage of VO2max required by any level of activity is higher in heavier (and fatter) individuals because energy cost is increased and weight-relative VO2max is reduced. Since a measure of endurance fitness is reflective of both physiological fitness and weight status, BMI adds little to a model for predicting injury that includes fitness.
According to studies conducted at Fort Jackson and Fort Leonard Wood in the 1980s and 1990s (Jones et al., 1993b; Jones, 1992), there are no systematic relationships between injury and BMI or injury and body fat in military recruits. In one study, the highest percentage of injuries was found in the low and high BMI quartiles; in another study there was only slight variability across quartiles; and in a third study the injury rates in the top three quartiles were not significantly different from one another (38 to 42 percent). These patterns were similar for men and women, although the injury rates for women were double the rates for men.
To model the effect of changes in the distribution of body mass index on injury and attrition, the committee obtained data on medically attended injuries and first-time attrition from the U.S. Army Center for Health Promotion and Preventive Medicine (USACHPPM). These data were used to make projections about potential future changes in injury and attrition, assuming a variety of hypothetical scenarios for the BMI distribution of the recruit class in years ahead, either as a result of a continuation of the current shift toward higher BMI in the youth population, or as a result of possible changes in the recruitment standards for height and weight.
Injury data came from a prospective cohort study of six battalions of male (n = 2,945) and female (n = 2,080) Army trainees during nine weeks of the basic combat training at Fort Jackson, South Carolina, between 1998 and 2000 (Knapik et al., 2001a; Jones, Darkajy, and Knapik, 2004). These data are described in Chapter 4. Demographic characteristics of the recruits used in the BMI/injury analyses are shown in Table 4-5.
To examine injury and attrition risk, USACHPPM initially stratified by quartiles of BMI and run-time performance. Following examination of the data, they combined the middle two quartiles to improve the precision of the estimates of injury attrition risk. Tables 4-6 and 4-7 show the associations of successive levels of BMI and run time with injury and attrition, respectively.
Within categories of fitness, lower BMI recruits tended to have a higher risk of injury for both men and women. However, for the fastest quartile of men, this trend reversed and the higher BMI recruits had a higher risk. Among men, attrition followed a similar pattern to injury. The pattern of female attrition was very different from the pattern of female injury, with the higher BMI women having a higher risk of attrition (within fitness categories). The reasons for these variations need to be better understood, but it is clear that BMI and fitness jointly influence the risk of injury and attrition.
From these data, we projected changes in injury and attrition risk of the recruit population, based on the assumption that the distribution of BMI could shift toward leaner or fatter recruits, either as a result of changes in the U.S. youth population or through future modifications to the current height and weight screening criteria. Figures 5-4 and 5-5 show the results of these projections, which are adjusted for differences in physical fitness (as measured by performance on the entry run test) among BMI groups. However, it is still possible that there are variations in fitness within BMI categories, and these are not accounted for in this analysis.
The results indicate that fluctuations in the BMI distribution have a very limited effect on the overall injury risk (Figure 5-4) provided the current upper bounds for BMI and the current waiver procedures remain largely unaltered. This is also true for attrition among men, however, attrition among women rises as a greater percentage of higher BMI women
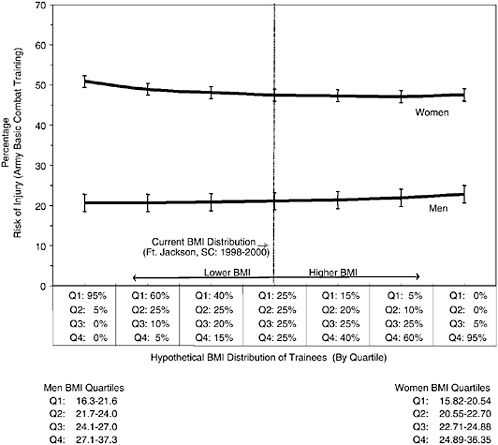
FIGURE 5-4 Relationship between risk of injury and body mass index (BMI).
SOURCE: Jones, Knapik, and Darakjy (2004). U.S. Army Center for Health Promotion and Preventive Medicine. Previously unpublished data from samples of male and female trainees at Fort Jackson, South Carolina.
are enlisted (Figure 5-5). Thus, these projections suggest that a shift toward a higher BMI Army would be unlikely to adversely impact injury in men and women, and attrition risk in men, but potentially could increase the attrition risk in women. It should be noted that this conclusion is based on data from those who qualified under the current standard. There are currently no data on the injury and attrition experience of those who are disqualified under current height and weight body fat standards; however, the currently ongoing Assessment of Recruit Motivation and Strength (ARMS) study by the Accessions Medical Standards Analysis and Research Activity (AMSARA) is expected to yield information about the effect of screening in applicants who pass a fitness test but are disqualified on other grounds (Krauss, 2004).
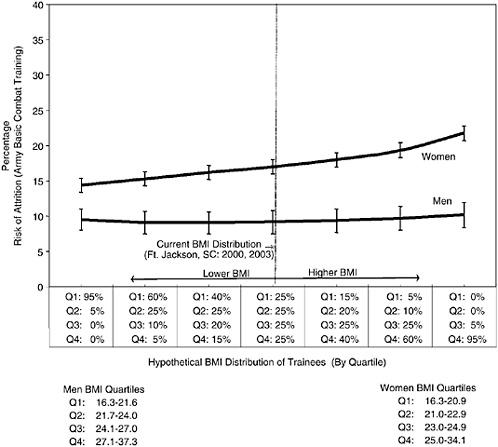
FIGURE 5-5 Relationship between risk of attrition and body mass index (BMI).
SOURCE: Jones, Darakjy, and Knapik (2004). U.S. Army Center for Health Promotion and Preventive Medicine. Previously unpublished data from samples of male and female trainees at Fort Jackson, South Carolina.
Body Composition and Military Job Performance
The relationship between body size and composition and the performance of physically demanding military jobs has been discussed by researchers from the U.S Army Research Institute of Environmental Medicine (Harman and Frykman-Scott, 1992; Friedl, 2004). Harman and Frykman-Scott (1992:105) suggest that lifting and carrying are the most common military tasks:
Typical military lifting tasks include loading artillery shells, lifting supplies onto and removing them from trucks, moving construction equipment, and assembling or disassembling heavy equipment. Most lifts involve raising an object from the ground to between waist and shoulder
height. Carrying is usually associated with lifting. A soldier is generally expected to lift objects weighing as much as 50 kg single-handedly, with heavier objects lifted by more than one individual. In heavy lifting jobs, 85 to 200 pound objects may be lifted and carried up to 200 yards by a single individual. Packs in excess of 100 pounds and other heavy loads may be lifted and carried for several miles.
A case is made by Harman and Frykman-Scott that loaded performance tests are the best measures of military task performance and that larger individuals with more lean body mass and more fat mass perform better on these tasks. They found a higher correlation between load carriage performance and lean body mass than between load carriage and percentage of body fat. Based on their results, they conclude that it is more important to screen for lean body mass than for body fat. According to Friedl (2004), today’s soldiers are heavier than before, “reflecting both increased muscle and fat components.” They are also healthier and more fit than ever before.
Weight Reduction and Maintenance
Each Service provides general guidance on weight management programs, which differ from one installation to another. According to a report on weight management by the Institute of Medicine (2003), the Services have done little with regard to medical and physiological research on weight loss and maintenance, and there is essentially no long-term follow-up beyond six months to evaluate the effectiveness of these programs. Enlisted personnel who exceed weight guidelines are required to participate in weight loss and maintenance programs. Some of the programs have weight loss requirements, and some have behavioral and nutrition counseling.
The Army offers weight control counseling through physical fitness trainers and operates several hospital-based weight loss and weight maintenance programs overseen by physicians (Army Regulation AR 600-9). The Marine Corps program is similar to the Army program and includes diet counseling. The Navy provides a six-month program that is managed by a command-trained physical fitness coordinator and includes mandatory physical exercise. It provides a self-study guide for nutrition and weight control. The Air Force program is centrally controlled and includes behavioral and dietary counseling by medical personnel as well as an exercise program. After the first three months, if weight loss goals are met, the personnel enter a six-month weight management program.
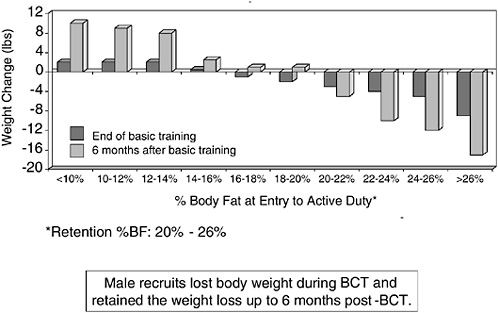
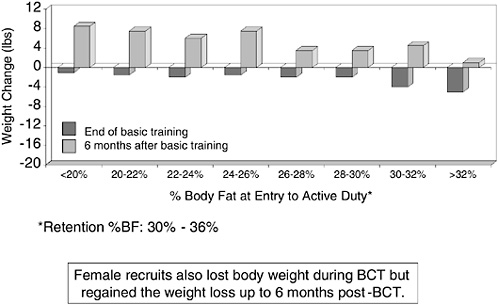
Friedl (2004) measured changes in body weight during basic training and the first six months following basic training for 1,048 male and 816 female recruits according to initial adiposity. Figure 5-6 shows that male
recruits whose body fat measured less than 16 percent gained weight in basic training and continued to gain weight through the first six months while male recruits whose body fat measured 16 to over 26 percent lost weight in basic training and continued to lose weight through the first six months. Figure 5-7 shows the results for female recruits: all lost weight during basic training, regained, and added weight by the end of six months. The weight loss achieved during basic training may be attributed to diet control and vigorous exercise. As noted above, interventions capable of producing systematic weight loss across broad populations over the long term have not been demonstrated to date.
In the civilian sector, the National Heart, Lung, and Blood Institute of the National Institutes of Health has issued Clinical Guidelines on Identifying, Evaluating, and Treating Overweight and Obesity in Adults (National Heart, Lung, and Blood Institute, 1998). Evidence concerning the various treatment interventions was identified and evaluated on the strength of the particular treatment to provide efficacy. The evidence supporting various treatments was categorized according to the following (type A providing the strongest evidence): (1) type A—randomized controlled trials in which a large number of studies were performed, (2) type B—randomized controlled trials in which a limited number of studies were performed, (3) type C—nonrandomized trials and observational studies, and (4) type D—panel consensus judgments. The recommendations from this report covered the areas of dietary therapy, physical activity, behavioral therapy, pharmacotherapy, and weight loss surgery.
Reduction in calorie intake was identified as the sine qua non for weight loss. Diet composition under this reduced calorie regimen was not determined to be an important factor, although it was noted that some people perceive certain diet compositions to facilitate “sticking to” an overall reduced calorie diet. Data were not sufficient to define or recommend any particular diet, only to recommend a reduction in total calories. Concerning physical activity, the data showed only a very modest (~ −2 kg) average effect on weight loss. While the guidelines recommend 30 to 45 minutes per day, 3 to 4 days per week of moderate physical activity, the consensus was that physical activity may be adjunctive to a calorie-restricted diet, but alone has little or no effect on obesity.
Some evidence has been found to suggest that some behavioral support can be helpful in encouraging adherence to a calorie restricted diet. Weight loss drugs approved by the Food and Drug Administration were also seen as adjunctive in support of a calorie-restricted diet. And weight loss surgery was endorsed by the National Heart, Lung, and Blood Institute for those with severe intractable obesity.
An Institute of Medicine committee on weight management concluded (2003:111):
Apart from the obvious need to increase energy expenditure relative to intake, none of the strategies that have been proposed to promote weight loss or maintenance of weight loss are universally recognized as having any utility in weight management. The efficacy of individual interventions is poor, and evidence regarding the efficacy of combinations of strategies is sparse, with results varying from one study to another and with the individual. Recent studies that have focused on identifying and studying individuals who have been successful at weight management have identified some common techniques. These include self-monitoring, contact with and support from others, regular physical activity, development of problem-solving skills (to deal with difficult environments and situations), and relapse-prevention/limitation skills. However, an additional factor identified among successful weight managers, and one not generally included in discussing weight-management techniques, is individual readiness that is strong personal motivation to succeed in weight management.
Conclusions and Recommendations
Committee projections based on data provided by the Army suggest that a shift toward a higher BMI force would be unlikely to adversely impact injury and attrition risk in men, but might slightly increase the attrition risk in women. It is important to note that this conclusion is based on data from individuals who qualified under the current standard.
Recommendation 5-1: As BMI is less predictive of injury and attrition than aerobic fitness, we recommend that it not be used as a proxy measure for fitness in the military population.
Recommendation 5-2: As a BMI standard is not justified on the basis of links to injury or attrition, we recommend that such links not be used as the basis for any use of BMI.
Standards for appearance and bearing are issues of military values and thus are outside the committee’s charge.
Although a relatively small number of individuals with high motivation and high self-control can lose weight and retain that weight loss through diet and high levels of physical activity, such results are not the norm, and research has not identified programs that have a high likelihood of success for achieving long-term substantial, sustainable weight loss. Given the evidence regarding the difficulties of maintaining weight loss, the committee thinks that it is unrealistic for retention standards to be more stringent than accession standards.
Recommendation 5-3: Any BMI standard used for retention should not be more stringent than a standard used for accession.
ASTHMA
Asthma Trends in the General Population
Asthma is one of the most common chronic illnesses in the United States (Centers for Disease Control and Prevention, 2002). Table 5-4 illustrates that the rate of those who have ever experienced an asthma episode varies between 38 and 43 per 1,000 people in the population. Table 5-5 shows this rate according to age group and gender. The rate is the same in individuals ages 15 to 34 but higher in those under age 15. The rate for non-Hispanic blacks over age 15 is similar but slightly higher when compared with non-Hispanic whites and Hispanics. When reporting episodes experienced in the previous year, blacks report greater frequency (5 percent) than Hispanics (4 percent) (Centers for Disease Control and Prevention, 2004). In the group ages 15 to 34, 4 percent report current asthma symptoms with slightly higher rates during the winter months (7 percent). Women report a higher level of current symptoms (8 percent) than men (6 percent). CDC data from 1980 to the mid-1990s indicate that women were over twice as likely than men to be hospitalized for asthma (Centers for Disease Control and Prevention, 2004).
TABLE 5-4 Rates of Experiencing an Asthma Episode in the Past 12 Months Among Persons of All Ages: United States, 1997-2003
|
|
Rate per 1,000 Population (95% Confidence Interval) |
|
|
Year |
Crude Estimate |
Age-Adjusteda |
|
1997 |
41.8 (39.7-43.8) |
41.5 (39.4-43.5) |
|
1998 |
39.5 (37.4-41.7) |
39.3 (37.2-41.5) |
|
1999 |
38.6 (36.4-40.9) |
38.5 (36.2-40.7) |
|
2000 |
40.0 (37.7-42.2) |
39.9 (37.6-42.1) |
|
2001 |
43.2 (40.8-45.5) |
43.1 (40.8-45.4) |
|
2002 |
42.6 (40.2-44.9) |
42.5 (40.2-44.9) |
|
2003 |
38.7 (36.5-40.9) |
38.7 (36.5-41.0) |
|
aEstimates are age-adjusted to the 2000 projected U.S. standard population using three age groups: 0-14 years, 15-34 years, and 35 years and over. SOURCE: Centers for Disease Control and Prevention (2004). Early release of selected estimates based on data from the January-March 2004 National Health Interview Survey (NHIS), Figure 15.1. |
||
TABLE 5-5 Rates of Experiencing an Asthma Episode in the Past 12 Months Among Persons of All Ages, by Age Group and Gender: United States, 2003
|
Age and Sex |
Rate per 1,000 Population |
95% Confidence Interval |
|
0-14 years |
||
|
Total |
54.4 |
49.2-59.7 |
|
Male |
63.3 |
55.2-71.3 |
|
Female |
45.2 |
38.0-52.4 |
|
15-34 years |
||
|
Total |
38.6 |
34.7-42.6 |
|
Male |
30.4 |
25.0-35.9 |
|
Female |
46.9 |
40.8-52.9 |
|
35 years and over |
||
|
Total |
32.2 |
29.5-34.9 |
|
Male |
18.5 |
15.3-21.7 |
|
Female |
44.4 |
40.3-48.5 |
|
SOURCE: Centers for Disease Control and Prevention (2004). Early release of selected estimates based on data from the January-March 2004 National Health Interview Survey (NHIS), Figure 15.2. |
||
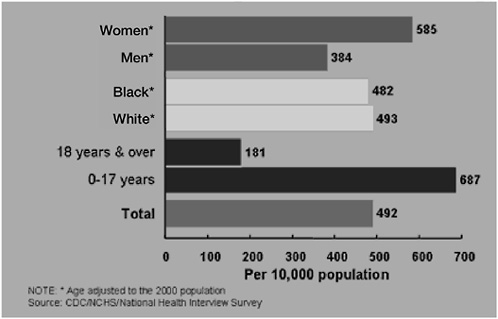
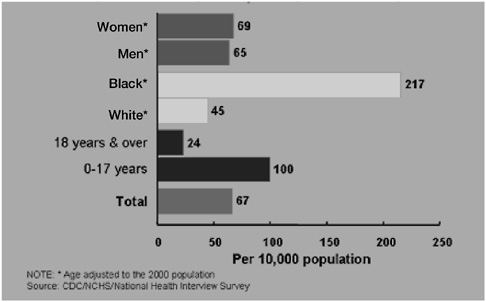
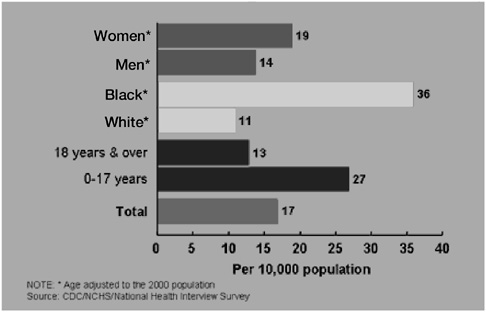
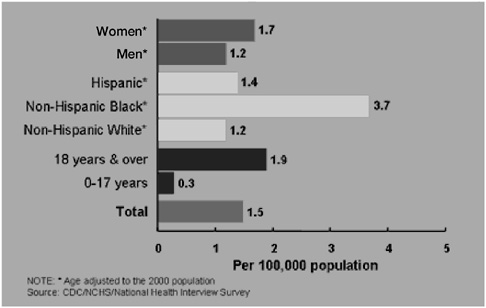
Figure 5-8 illustrates that 181 out of 10,000 adults made outpatient visits for asthma in 2002. Figures 5-9 and 5-10 show that 24 of 10,000 made asthma emergency department visits and 13 were hospitalized. Figure 5-11 shows that 1.9 adults per 10,000 died from asthma in 2002. In 1996 death rates (rate per 20 million) for asthma in the group ages 15 to 24 are dramatically higher for blacks (20) than whites (.5) (Centers for Disease Control and Prevention, 1996).
Asthma in Military Populations
Complete asthma prevalence data for the military population are not available; however, recruitment data and a few small studies suggest that it is commonly observed among recruits and military personnel. Asthma has been among the top 10 conditions for which waivers are requested. Between May 2003 and April 2004, 3,700 applicants were rejected at one military entrance processing station for medical disqualifiers in the lungs and chest; approximately 38 percent of these sought and received a waiver. An analysis by gender, race, and Service branch shows that a smaller percentage of female enlistees received waivers (29 percent) compared with male enlistees (39 percent); a slightly higher percentage of white enlistees received waivers (40 percent) compared with black enlistees (34 percent); and a slightly lower percentage of Air Force enlistees (30 per-
cent) received waivers compared with the other three Services (see tables in Appendix B). A further breakdown of the lung and chest disqualifiers by International Classification of Diseases (ICD-9) coding shows that over 70 percent of those in the chest and lung area were coded as having some form of asthma. These results were obtained through the committee’s analysis of data provided from the U.S. Military Entrance Processing Command Integrated Resource System database.
DoD Instruction 6130.4 on accession health standards states:
Asthma (493), including reactive airway disease, exercise-induced bronchospasm or asthmatic bronchitis, reliably diagnosed and symptomatic after the 13th birthday is disqualifying. Reliable diagnostic criteria may include any of the following elements: Substantiated history of cough, wheeze, chest tightness and/or dyspnea which persists or recurs over a long period of time, generally more than 12 months.
Recruits can request an asthma waiver and, if granted, can move forward to basic training. Some personnel develop asthma during military service and unless disqualified can continue their duties.
A number of investigations conducted with military personnel contribute to understanding how asthma is evident in this population. For example, Young et al. (2001) sampled active and retired military service personnel (1997-1998) enrolled in TRICARE (a military health care system) and residing in region 11 (includes Washington, Oregon, and northern Idaho) of the United States. They found that being a woman, being younger, engaging in less exercise, and having a higher BMI were all associated with the presence of asthma.
Other studies have looked at participation in military life and activities for people with asthma. The AMSARA active-duty enlistee study followed 313 “existing prior to service” discharges at Fort Jackson. Findings must be considered with caution as the self-administered survey had a low return rate. Data show that 14 percent of total discharges were for asthma. Many more asthmatics (26 to 1) believed that they could not have completed basic training because of their condition. Discharges were eight times more likely to have a history of asthma. Of those with asthma, two-thirds experienced daily or continuous symptoms, and two-thirds had symptoms one night a week or more.
Clark and colleagues (2000) reviewed records of 587 disqualified recruits and found that there was no difference in their attrition compared with the general military population (Clark et al., 2000). Sims and colleagues reviewed 119 Navy disqualification packages for individuals with asthma and found that enlisted personnel and submarine recruits were significantly more likely to be discharged than other types of personnel (Sims, Tibbles, and Jackman, 1999). More blacks were disqualified, and
most disqualifications for mild asthma followed a diagnostic work-up. Krauss (2004) conducted a 5-year study following a cohort of 3,398 active-duty recruits. In a one-year period (2002), just over 5 percent of disqualifications of first-time applicants were for asthma. Those with asthma waivers were more likely to remain on active duty than those without asthma. Of those identified with asthma (17 percent), 70 percent had preenlistment symptoms.
AMSARA data on a cohort followed for five years explored asthma outcomes among Navy recruits and active-duty enlistees who were identified with asthma after enlistment. As part of this effort, Project REMAIN looked at data on the experience of 162 Navy recruits during 9 months (2001) and observed that 66 had asthma. They found that mild asthmatics were more likely to leave active duty soon after diagnosis. Recruits without asthma were more likely than asthmatics to remain in training. However, after training there was no difference in retention rates. Recruits with asthma were 1.4 times more likely to make medical visits. Mild asthmatics were at no additional risk of hospitalization than the general military population.
A REMAIN case control three-year follow-up study was conducted at the Great Lakes Naval Training Center of personnel identified with asthma after enlistment. Findings indicated that 40 percent of mild asthmatics were retained on active duty with no adverse consequences. The greatest frequency of health care use and recruitment loss occurred in basic training. Following training there were no attrition differences between those recruits with or without asthma, although health care costs were higher (relative risk: RR 1.7 for those with asthma). Figure 5-12, using AMSARA accession data (Krauss, 2004), shows that the probability of enlistees in all Services granted a waiver for asthma remaining on active duty was greater over a four-year period than enlistees with no asthma waiver.
Asthma Interventions
Diagnosis and treatment guidelines for asthma have been provided by the National Asthma Education and Prevention Program (National Institutes of Health, 1997). The guidelines discuss interventions that enable individuals with asthma to function more fully and exert optimal control over the disease. Daily use of anti-inflammatory medicine in people with persistent asthma has been associated with reduced symptoms and emergency department use.
Meta-analyses of nonpharmacological interventions for asthma have been conducted. Gibson and colleagues (2002) reviewed self-management
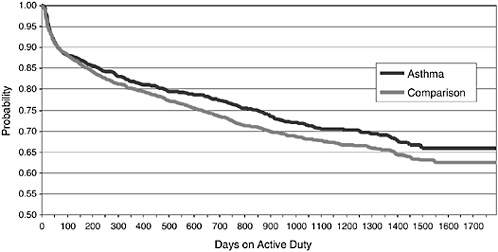
FIGURE 5-12 Probability of remaining on active duty among enlistees granted a waiver for asthma versus matched comparison subjects, all Services.
SOURCE: Krauss (2004).
education studies of adults and found that such interventions improve asthma outcomes. Janson and Roberts (2003) observed that mild asthmatics as well as those with more severe disease can benefit from educational interventions. Both group and individualized self-management programs can produce positive results (Wilson et al., 1993). Use of asthma action plans as part of these programs has been shown to be important to positive results (Gibson et al., 2002). Clark et al. (2000) showed that clinicians can be trained to enhance self-management by patients, and this results in fewer symptoms and less health care use with no more physician time expended. No evaluations of interventions for military personnel are available, however.
Issues for the Military
Asthma is ubiquitous in the general population, affecting about 8 percent of the population, with higher prevalence noted among blacks compared with others and women compared with men. An appreciable number of potential military recruits can therefore be expected to have asthma.
Available data indicate that military personnel with asthma waivers, in fact, have lower attrition rates than those without the condition, although studies show that their health care costs are higher. Some evi-
dence suggests those with asthma discovered after enlistment are more likely to drop out during basic training. A reasonable question is whether or not having asthma should make an individual ineligible for military service. Currently, asthma at any level of severity precludes participation in the military. It is likely that individuals without symptoms for a prolonged period of time or even those with mild and infrequent symptoms could carry out their service requirements, especially if they received optimal medical therapy and self-management education. However, there are costs associated with ensuring timely access of personnel to needed medical therapies and making self-management education available. Furthermore, existing data are not informative regarding whether the conduct of certain military operations is more conducive to problems for those with asthma than others, for example, whether environmental conditions or specific tasks may trigger exacerbations. Nonetheless, in general, available data do not suggest a negative service trajectory after initial training for individuals with asthma compared with those without. Using asthma as an exclusionary factor for military service is likely to work against minorities and women, as these groups exhibit the highest prevalence of asthma.
It may be that the goal-oriented climate of military recruitment discourages disclosure by some individuals who have asthma. Data suggest that those who have the condition but do not initially disclose it may drop out more frequently from basic training, while those who disclose a history of the illness at the time of enlistment and receive a waiver have lower attrition rates. Encouraging disclosure in a benign environment is a desired goal.
CONCLUSION
In light of current data, the existing standard and waiver process regarding asthma is appropriate. Research on the cost-benefit consequences of enlisting individuals with more severe asthma would be needed prior to recommending any change in enlistment policy regarding asthma.