3
Main Findings
In this chapter we describe and analyze qualitative and quantitative data gleaned from records and reports of and interviews with the four nongovernmental organizations (NGOs). The objective of the qualitative analysis is to find possible reasons for the variations in utilization rates with regard to security and the management approaches by the different agencies. Quantitative data have been used when they were available from the NGOs to address the five specific objectives of this study. Table 3-1 presents a comparison of the financing approaches of the four NGOs. Table 3-2 presents a comparison of their management approaches.
Objective 1: To identify which management and financing approaches, including the setting of fees, are used by four NGOs supporting health care in the eastern Democratic Republic of the Congo.
DIFFERENT APPROACHES CONCERNING INDIGENT CARE
All four organizations employ the term “indigent” to define the poorest of the poor, but they do not distinguish indigent status in similar ways. The main problem is that there is no internationally accepted or clear definition of indigence. As a result, the organizations either do not establish criteria or they formulate variations of the basic definition of and criteria for indigent status.
The dilemma facing organizations in defining who are indigent is finding a balance between the people who truly need support for health care and those who can afford the health care costs. Either way, assessing or setting up a well-functioning system that supports indigent care is time-and labor-intensive in a chronic crisis situation.
In the Democratic Republic of the Congo (DRC), each agency has found a different resolution to the indigent dilemma. The International Rescue Committee (IRC) works with coupons and a maximum quota for the indigent for each health zone. This is a system of enfranchisement in which coupons given to the indigent substitute for pay for services, a bit like a ration card in a refugee camp. Using the criteria, local health committees determine the indigent status of those who ask for coupons. The health nurse also checks their status; in this way, the local health committee and the health nurse can control each other’s work. The IRC reimburses the health centers for the coupons that they receive. While the main disadvantage is that the system takes up considerable time and resources, it has four strong advantages:
-
The integrity of the health system is maintained, because health centers continue to generate revenues from indigent treatment.
-
The more indigent patients the health staff treats, the more money it earns. In other words, there is no disincentive for treating the indigent.
-
There is no pull effect of free health care for the indigent from other zones.
-
It allows the health staff and the IRC to monitor the indigent and their (impact on) health care.1
Except for the IRC, none of the organizations currently employs an indigent care system with coupons. Merlin reimburses the drugs, but not the consultations, for the indigent. The other two organizations do not employ explicit indigence criteria and do not reimburse indigent treatment. While these organizations maintain that the indigent are treated for free,
|
1 |
Some health staff was concerned about the continuation of the coupon system, if IRC would leave. In this sense, the IRC needs to develop and explain a clear exit strategy. Currently, the part of the revenues allocated for buying medicine is put into a savings account. Using these savings can help ensure continuation of local health care for an extended period of time once the international organizations leaves (see Table 3-1). |
TABLE 3-1 Comparison of Financing Approaches
|
Finance |
IRC |
Merlin |
|
Drug supply |
Free/monthly |
Free/monthly (more often with outbreaks) |
|
Savings |
Yes |
No, revenues spent on incentives for zone bureaus, health centers, and health committee |
|
Support to |
Health centers, reference health centers (primary health care) and limited support to hospitals for indigent treatment in Kabare Health Zone. Katana followed with new memorandum of understanding |
Health centers, reference health centers, and hospitals (primary and secondary health care) |
|
Type of fee |
Bundled fee per episode of illness covering consultation, lab test and drugs (tarif forfaitaire) |
Stopped nominal fee in 2001 and adopted variable pricing system for all drugs and services based on 60% of market price. |
|
Exemption (no payment for type of service) |
BDOM also supports chronically ill, such as diabetes and tuberculosis |
|
|
Malteser |
ASRAMES |
Conclusions |
|
Free/monthly (but health centers pay 15% of cost price to zone bureau) |
Free/monthly |
Given the economic situation, free and monthly is the common approach |
|
No (locked BDOM account has been abolished) |
Before Sept. 1999, yes. After Sept. 1999 revenues spent on incentives for zone bureau, health centers and health committee |
No system of savings has functioned well enough to limit or withdraw international support |
|
Health centers, reference health centers, and hospitals (primary and secondary health care) |
Health centers, reference health centers, and hospitals (primary and secondary health care) |
Humanitarian organizations traditionally focus on primary health care, more development-oriented work also focuses on hospitals, which reduces the referral problem of the indigent |
|
Bundled fee (consultation, drugs, lab research) per episode of illness |
Bundled fee per episode of illness. Before September 1999 fee per service for cost recovery of drugs and medical supplies |
Fees are considered important for sustainability, dignity of client, and to prevent unnecessary use of health care. Provincial health inspector/inspection determines the type of fee |
|
No exemptions, but low fees (see fees height and reductions) |
Common attempt to either abolish or diminish fees for children. Regular adjustment necessary for optimization of use due to insecurity and economic decline (e.g., 4 times a year). |
|
Finance |
IRC |
Merlin |
|
Waiver (no payment for population group) |
Coupons for the indigent. Reimbursement to health centers by IRC |
List of the local indigent by health committee and health staff. Indigent are treated for free, no reimbursement to health centers by Merlin. Social control by local representatives (e.g., from health committee) |
|
Fee height and reductions |
Before August 1998: Adult $3.00 Child $2.00 After August 1998: Adult $2.00 Child $1.00 December 2000 Adult $1.00 Child $0.50 Sept 2002 Adult $0.80 Child $0.40 Sept 2001, health centers have child rate for under age 15, but no uniformity in child age before this date. Antenatal care $0.40 bundled fee |
No fixed charge, but variable pricing of drugs and services over time and in different zones. Nominal (symbolic) pricing replaced in 2001 by 60% of local pharmacy prices. Plan to adjust prices 4 times a year, but in practice this happens less often |
|
Malteser |
ASRAMES |
Conclusions |
|
Health committees and health centers arrange this on their own initiative. |
The indigent are treated for free. No coupon system. Nurse decides on indigent status together with health committee, but no reimbursement to health centers by ASRAMES |
Regular adjustment necessary for optimization of use due to insecurity and economic decline. Important to provide incentives to health center staff in order to promote treatment of the indigent. Claims of free indigent treatment hard to verify without control and indigent care system |
|
Before January 2001 $2.00 $1.00 After $1.00 $0.50 It is not clear how much patients really pay |
Since September 1999 Urban/rural maximum Adult $1.0/$0.5 Child $1.0/$0.5 May 2000 increase in fees urban/rural: Adult $1.5/1 Child $1.5/1 Oct 2000 decrease in fees: Adult $1.0/$0.5 Child $1.0/$0.5 Antenatal care $1.0/$0.5 (first time) Under age 5 consultation $1.0/$0.5 (first time) Delivery $7.0/$5.0 Observation $1.0/$0.4 Small surgery $2.5/$2.0 August 2002 urban rates discontinued If antenatal care/under age 5 consultation material provided by UNICEF or ASRAMES maximum fee is $0.20 |
Regular adjustment necessary for optimization of use due to insecurity and economic decline. Whether the different zones need different fee structures, exemption and waiver systems should be studied further |
|
In hospital after reference: reduction of $3.00 for adult $2.00 for a child |
|
|
Finance |
IRC |
Merlin |
|
Allocation of revenues |
30% drugs and supplies (to savings account) 40% incentives 30% running cost |
Old 45% incentives 10% running costs 25% zone bureau subsidy 20% community fund Proposed 70% incentives 20% running cost/community fund 10% zone bureau subsidy Adopted 65% incentives 20% running cost/community fund 15% zone bureau subsidy |
|
Debt of health center |
Growing, especially at reference health centers with more complex treatments |
No information |
|
Utilization rates |
Strong growth, especially of indigent attendance |
Strong growth |
|
Malteser |
ASRAMES |
Conclusions |
|
Old system changed in September 2001. |
60% incentives 30% health center running costs 10% zone bureau running costs |
Incentives and high enough revenues are crucial for staff motivation and preventing the sale of drugs to the private market. If revenues are not high enough the 4 organizations attempt to provide direct subsidies, e.g., for preventive services |
|
New Health center pays 15% of the costs of the drugs to the zone bureau. Of the remaining revenues: 40% running costs 60% incentives |
||
|
No information |
Growing debt led to humanitarian cost-sharing policy. Currently, drugs are free, so no debt. No data on new system yet, but may become a problem |
Important topic requires further research in terms of both debts of patients to HC and debts of HCs to zone bureau |
|
Little information, BDOM report inconclusive. Later study showed underreported attendance |
Strong growth after lowering of fees Raising fees led to immediate decline Monitoring new raise |
Lower fees matter, but so do supervision, reclassification of < 15s, and reimbursement of indigent treatments |
TABLE 3-2 Comparison of Management Approaches
|
Management |
IRC |
Merlin |
|
Supervision/monitoring by health supervisors |
At least once a week, 1 health supervisor for 4 health centers, with joint visit for supervision with zone bureau staff member once a month |
1 or more supervisors per health zone, visits twice a month on average |
|
Number of health committees |
One for each health center. Depending on health center, participation varied and could be strengthened further |
One for each health center |
|
Health committee tasks |
Manage administration of health center, including finances, indigent status and guarding drugs and supplies |
Participates in health management. President signs the contracts. |
|
Malteser |
ASRAMES |
Conclusions |
|
Two health supervisors per health zone. Visits once a month for each health center. Security problems may obstruct visits |
6 health supervisors for 19 health zones. 17 health zones (2 inaccessible) = 17 health zone visited every 2 months (in 2002 every month |
Two poles: hands-off “contract” or “strong supervision” models. An adaptable middle ground would be either a decentralized supervision system or a shadowing exercise in which health authorities are required to undertake a certain amount of supervisory visits in order to receive continued support |
|
Does not cooperate closely with health committees yet, but will do so in the future. Louvain Développement takes initiatives for improvement, mainly training |
One for each health center. 100% operational (checked on the basis of health committee minutes, reporting forms on number of meetings, decisions and actual execution, as well as supervisory visits) |
Well-functioning health committee that participates in local health management is a useful condition for free drug supply. Important participatory mechanism that requires continuous care |
|
Limited cooperation with health committee training and the indigent. Health staff and health committee sometimes have tense relations |
Manage administration of health center, including finances, indigent status, and guarding drugs and supplies. Minutes of health committee meetings are a condition for ASRAMES support. |
Functioning health committee that participates in health management is a condition for free drug supply and improving management, prevention and local involvement |
|
Management |
IRC |
Merlin |
|
Criteria for indigence |
The poor without possessions Widows and widowers without other support The severely malnourished Orphans without other support Mentally and physically handicapped without possessions People without work or land Malnourished children and adults with associated pathologies The chronically ill |
Person with mental or physical disabilities Orphan abandoned by other family members Older person living alone Unaccompanied child Widow/widower without income Internally displaced people Undernourished people (temporary coupon system in Kalima) |
|
Zone bureau |
Especially health supervisors work closely together. Questions about parallel structure, in particular in reporting. Direct financial support to zone bureau for supplies, stationery, etc. |
Small supervisory staff, sometimes leads to delay in control. Problem of parallel reporting systems |
|
Support to zone bureaus |
Katana bureau salaries: Of 30% running costs, 44% goes to the zone bureau. And 250 liters of petrol, 5 liters of motor oil a month for supervisory visits and field trips Kabare bureau zone salaries: Of 30% running costs, 60% goes to the zone bureau. And 50 liters of petrol, |
Zone bureau subsidy (see Table 3-1) plus $100 a month as incentive for medical doctors and $150 as incentive for other zone bureau staff |
|
Malteser |
ASRAMES |
Conclusions |
|
No criteria. Health committee and health center staff determine indigent status together. People who cannot pay either receive credit or are not treated. |
No written criteria. 10-20% of patient cannot pay. Nurse at health center decides in cooperation with health committee. As drugs are free, ASRAMES does not reimburse. |
Approaches to the indigent differ from organization to organization, although they all attempt to let the indigent receive free treatment. Insufficient data on nontreatment of indigent, which can be a hidden problem. Organizations should discuss (common?) indigent criteria |
|
Strong delegation to zone bureau, supervision of zone bureau in close cooperation with Malteser |
Very close cooperation, continuous communication. ASRAMES partly fulfills role similar to government control |
Improving management skills of zone bureau crucial for sustainability, but difficult. Organizations take over traditional government control role. Problem of parallel reporting systems. Doubts of capacity and corruption linger |
|
Health center pays 15% of the costs of the drugs to the zone bureau (see Table 3-1) of which $75 a month goes to the provincial health inspection. And an additional $5 for each supervisory visit to a health center |
10% zone bureau running costs (see Table 3-1). The reference health center and hospitals contribute $100 and $150 per month to the zone bureaus. ASRAMES contributes $550 a month to zone bureaus that do not receive support from other NGOs ($200 for |
The four NGOs support the zone bureaus in very different ways. They all support their supervisory visits. At the same time, the NGOs prefer that the zone bureaus do not take to much money from the health facilities |
|
Management |
IRC |
Merlin |
|
|
150 liters of diesel, 10 liters of motor oil Both zone bureaus also receive 2 reams of printer paper a month |
|
|
Training |
No official training program, but health supervisors carry out in-house training with health staff at each facility in collaboration with zone bureau. Health staff receives refresher training in treatment protocols, vaccination techniques, epidemiological surveillance, cholera treatment and other topics as deemed necessary. Occasional finance training for health center |
Regular financial training of health committee members and health staff. |
|
Donor |
OFDA, perhaps USAID in the future |
ECHO |
|
Utilization |
Access has improved, but more work to increase attendance necessary. Uses standard of 3 to 4 visits a year |
Access has improved, but analysis needs to be carried out. More work to increase attendance necessary. Standard of 1 visit a year |
|
Malteser |
ASRAMES |
Conclusions |
|
|
supervision, $150 for fuel, $100 for office supplies, and $100 for equipment maintenance |
|
|
Financial support for training by zone bureau. |
Training of health committee Rational prescription Management of primary health care Financial management and accountancy Training in drugs management Training on the spot of BCZ supervisors Health information systems and management models Training for supervisors and trainers Consulting techniques |
Only information on type of training was collected. Judgment on quality of training is not possible |
|
ECHO |
ECHO for several years, and now PATS |
OFDA and ECHO have different policies for cost sharing and hospital support. This contributes indirectly to fragmentation of health system |
|
Unclear whether access has improved, probably underreported. Insecurity is a problem. Standard of 1 visit a year |
Access has improved, but more work to increase attendance necessary. Standard of 1 visit a year |
Access has improved. The organizations play a useful role, but employ different goals and standards. Health system would fall apart without support |
|
Management |
IRC |
Merlin |
|
Sustainability |
Depends on internal management, donor support, economic and war conditions |
Depends on internal management, donor support, economic and war conditions |
there are no quantitative data to back this claim. More data from regular reporting as well as special research on morbidity and mortality are necessary to convince donors on the merits (or just efficiency) of the different approaches. At the very least, the organizations should compare their approaches and decide on common indigent criteria.
SUPPLY
In early 2000, utilization rates for the IRC were equivalent to those of ASRAMES, but their fee structures differed. One possible cause of this difference in utilization may be the continuous availability of drugs. Lawson (2004) and Burnham, Pariyo, Galiwango, and Wabwire-Mangen (2004) have shown that utilization at health facilities drops when there are stock ruptures for the clinic. Patients, knowing there are no drugs at a clinic, prefer to pay for transport to an area where they are sure to receive treatment rather than one where they will be referred elsewhere, with added transport costs. With heavy supervision and regular stock-ups, the presence of drugs in a health facility boosts patient confidence.
IRC-supported clinics are in a single health zone. The furthest clinic is reachable via road in six hours, and supervisors visiting there can stay overnight and return the next day. In this way, clinics are well stocked most of the time. Looting of clinics occurs, but again, the proximity and accessibility of the IRC to those clinics (and the health teams in Bukavu should the IRC be unable to reach health facilities because of insecurity) allow for restocking to occur regularly. The contrary is true of ASRAMES-supported
|
Malteser |
ASRAMES |
Conclusions |
|
Depends on internal management, donor support, economic and war conditions |
Depends on internal management, donor support, economic and war conditions |
Management setup of organizations differs in terms of supervision, indigent care, and zone bureau support. ECHO and OFDA differences also important. Economy and war are crucial extraneous factors |
areas. Frequent insecurity as well as the movement of the front line through the ASRAMES health zone in 2000 may have meant that drugs stocks were ruptured (or looted) frequently.
The four organizations display great similarities in the processes they have developed to supply drugs and medical supplies. They differ, however, in the actual goods that they supply.
-
All organizations provide essential drugs once a month, either for free or for nominal prices, as Merlin used to do. Merlin is the only organization that allows special orders during the month. It also has special provisions to respond to epidemic outbreaks.
-
Supervisors and zone bureau staff generally examine the orders for medicines for correctness.
-
The IRC, Malteser, Merlin, and ASRAMES all have conditions that the health centers must fulfill in order to ensure delivery. These conditions differ but generally include a functioning health committee, supervisory visits, and respect for the fee system (see Tables 3-1 and 3-2 for more information on the supervision system).
-
Some drugs turn up on the black market, which indicates that either health staff are augmenting their wages through the resale of drugs or patients are selling drugs. The former is more likely; studies have shown that households that receive drugs in health facilities usually use some of the drugs and distribute the rest to household members (see Ferrinho et al., 2004). Such resale may indicate that the revenues from cost sharing are insufficient for ensuring staff motivation.
SUPERVISION: CAPACITY BUILDING, MONITORING, AND EVALUATION
As mentioned earlier, there are two poles along a continuum of management approaches toward supervision: the intense supervision pole and the hands-off contract pole. A higher degree of supervision would in theory lead to less stock depletion at a health facility as frequency of contact between health facilities and people with access to drug stocks is increased. The relatively small area covered by the IRC in comparison with ASRAMES may also have increased the likelihood of drugs supplies getting to health facilities without, or soon after, any interruption of stocks. While Malteser also covered a relatively small area (comparable to the IRC-supported zones), it faced more issues of security regarding accessibility to health facilities in the zones it supported. More rebel factions were present in the Walungu health zone, meaning that health teams frequently had to negotiate with fighting factions to get to health facilities or areas in the zone.2
In practice, a hands-off approach does not suffice for the organizations in this study. Due to the years of neglect, the degraded education system, the wars, the economic crisis, and suspicions of corruption, they all need to focus on capacity building, supervisory support, and control. Merlin’s current approach emphasizes intensive supervision, and Malteser also would like to strengthen its supervision further. In this sense, the organizations take over some roles that the state often fulfils in more stable societies. The promise of a less labor-intensive contract approach cannot be realized in the dilapidated health structure of the war-torn eastern DRC.
Although the labor-intensive approach is less favored by some national and international agencies, its benefits include the ability to aggregate health data more easily and provide on-the-spot training. Also, supervisory influence on the drug supply is direct, in that health facilities stocks are monitored and stocked accordingly. In addition, supervision can help prevent health staff from raising prices, increase respect for opening hours, and contribute to more professional and efficient, even friendlier, care.
The exact effects of supervision in the eastern DRC, however, are difficult to quantify.
Objective 2: To determine how these management and financing approaches affect utilization rates in the health zones supported by the four NGOs.
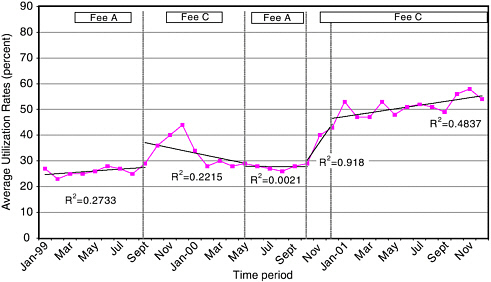
For the purposes of comparison, utilization rates for the four NGOs between the time periods January 1999 and December 2001 are described if a time series of a year or more is available. Detailed data for over a year were available for ASRAMES and the IRC, as such much of the analysis focuses on these two organizations. The health zone with the highest average utilization rates between 1999 and 2001 is Katana (average 42 percent), supported by the IRC. Both ASRAMES and the IRC had rising trends in utilization for the entire period described (Figure 3-1). The Kabare health zone had the highest recorded averages (87 percent) for the time period for which data were available (September 2001 to July 2002).
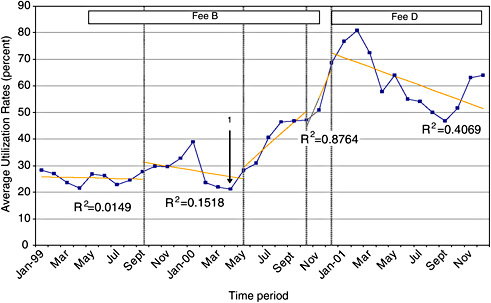
Comparing the data for the IRC and ASRAMES, differences in utilization rates emerged in September 1999 when ASRAMES changed user fee schemes. From September 1999 to May 2000, ASRAMES fees dropped in rural health facilities to $0.5 ($1 in urban areas), while IRC fees remained unchanged. Average utilization rates during this period for ASRAMES and the IRC were 33 and 28 percent, respectively. However, the overall trend for utilization in ASRAMES-supported areas during this period was negatively correlated with time (Figure 3-2). What are the possible reasons for the negative trend in ASRAMES utilization, even with a drop in user fees?
Between May and October 2000, ASRAMES fees rose to their previous rates, and IRC fees remained unchanged (Figure 3-1). Average utilization rates for ASRAMES and the IRC were 28 and 40 percent, respectively, yet both organizations’ fees were the same as the first period in 1999 (January to September) when average consultations were equivalent. In the case of ASRAMES, rates had stabilized at those seen during the first period before fees were changed. However, for IRC, while fees remained unchanged, utilization rates rose steeply (Figure 3-3). What is the difference between the periods January to September 1999 and May to October 2000 when each organization’s fee schemes remained the same for both periods, yet utilization rates differed for the IRC?
In addition to supervision and ruptures in stock, we first have to look at seasonal trends in the DRC. From both ASRAMES and the IRC data of
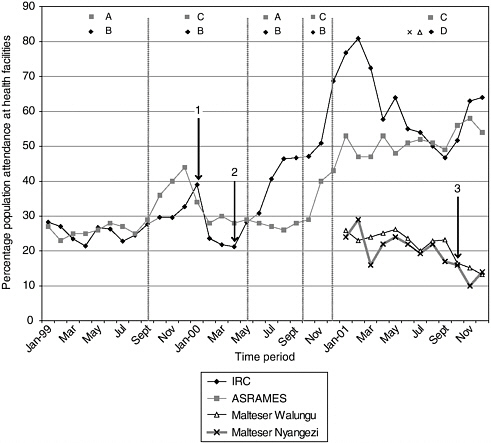
FIGURE 3-1 Utilization of health facilities supported by NGOs in eastern DRC.
NOTE:
Fee A: $1.5 urban; $1 rural
Fee B: $2 Adults; $1 children
Fee C: $1 urban; 0.5 rural
Fee D: $1 adults; $0.5 children
Arrow 1: Start of IRC indigent coupon scheme
Arrow 2: Reported influx of IDPs into Katana Health zone
Arrow 3: Closure of several health facilities in Walungu and Nyangezi due to insecurity
1999, a peak in utilization is evident late in each year. This coincides with the rainy season in the South Kivu province, when malaria transmission increases. Thus a seasonal rise of some sort should be expected around October of each year. This peak is smaller in North Kivu, where the rainy seasons are less pronounced.
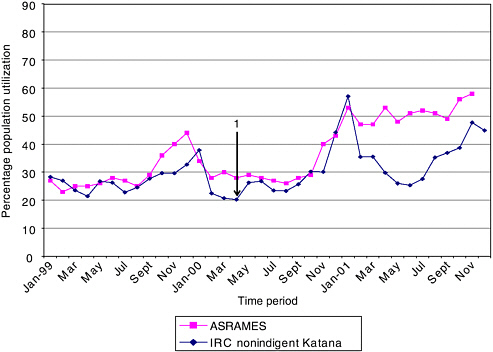
FIGURE 3-4 Utilization rates in ASRAMES clinics compared with rates of nonindigent utilization in IRC clinics.
NOTE: Arrow 1: Start of IDP coupon system in Katana health zone.
Second, utilization rates for ASRAMES and the IRC in late 2000 were 10 percent and 40 percent above those of the previous year, respectively. Thus seasonal variation in utilization does not explain the steep increase in IRC utilization from March 2000 onward. Looking back on reports from that period, IDP influxes were occurring from March, into and around the Katana area. The increase in utilization during the period from March-August 2000 could thus be a result of these influxes into the health zone. No simultaneous rise or security reports are recorded from the ASRAMES health zones. We can suggest that the first steep rise in utilization rates was a result of internally displaced persons moving into the Katana health zone.
This conclusion is supported by results, described in Figure 3-4, in which the nonindigent use of IRC-supported facilities is described in comparison with ASRAMES utilization rates for the same period. The figure shows comparable rates for both ASRAMES and the IRC when only the nonindigents in IRC health zones are taken into account. The IRC classification of indigent would include internally displaced people, and thus their
influx into the health zone and use of health facilities at no cost could result in the numbers graphed in Figure 3-1 from March 2000 to October 2000.3
The second and larger peak in rates for both the IRC and ASRAMES from October to December 2000 is more difficult to interpret. Both organizations report large rises compared with the previous year’s figures for the same period. Yet for the IRC there is a decline in indigent utilization from August 2000 onward, indicating that many internally displaced persons were leaving the area and nonindigent groups were using health facilities. The trend in ASRAMES utilization rates around this time is similar to those of the IRC, with a peak in November and December 2000 in the utilization of health facilities. In fact, once indigent use of health facilities is factored out of the IRC figures, the IRC utilization rates are closely associated with ASRAMES rates (Figure 3-4).
Again, we have to remember that the IRC and the zonal health bureau had still not dropped fees at health facilities in Katana to the levels found in ASRAMES health facilities. What are the possible explanations for the large rises in both the IRC and ASRAMES utilization rates?
For the IRC, a possible explanation is the reclassification of everyone under age 15 as children and eligible for lower rates at health facilities (at this stage, $1). This reclassification occurred in September 2001, prior to the massive peak in rates.
For ASRAMES, the trend in consultation rates was positive between October 2000 and November 2001. The user fee decrease in October 2000 seems to have influenced the trend in consultations.
What is the difference between the time periods September 1999 to April 2000 and October 2000 to November 2001? An epidemic (possibly malaria, as seen in Burundi during the same period) may have resulted in high usage for both agencies, perhaps more so for the IRC facilities as they are based in more highland areas. However, ASRAMES utilization rates were sustained at high levels throughout 2001, whereas the IRC rates decreased dramati-
cally, to an approximate equivalent with ASRAMES—further suggesting an epidemic of some sort, which was more pronounced in the Katana health zone.
The conclusions that we can draw from the data are
-
Providing free treatment support to indigent patients increases attendance only if health facilities have a defined set of criteria for indigence and, more critically, that health facilities are reimbursed for indigent fees.
-
Factors other than the cost of care and reimbursement for indigent groups contribute to higher utilizations rates, as seen when comparing figures between ASRAMES and the IRC in the early part of 2000.
-
There are crucial differences in the management of the organizations that could be contributing to the higher utilization rates at IRC-supported health facilities. Notably, these differences relate to the IRC’s intensive system of supervision to improve health care quality and local capacities, including the classification of indigent, the reclassification of those under age 15 as children, and the accessibility of the agency to the health zones it supports.
From the data under Objective 1, it seems that indigent support as well as intensive supervision and regular drug supplies lead to higher utilization rates. However, are those utilization rates high enough to create revenues that will allow health facilities some independence from external funding? When, in a chronic crisis, is external funding most needed?
Objective 3: To assess how these utilization rates compare with donor and humanitarian standards.
Utilization rates in an area of conflict such as the DRC are expected to be as much as three or four times per year per person as recommended in the Sphere guidelines (Sphere Project, 2004). The highest utilization rates of 1.15 per person per year were in Kabare health zone, where more than 80 percent of the population were classified as indigent (data not shown).
The organizations use different standards for measuring normal attendance. The IRC refers to the Sphere standard of four visits a year per person. Merlin, Malteser, and ASRAMES refer to the World Health Organization norm for situations comparable to the eastern DRC of one visit a year. This difference in baseline data is important for evaluation judgments as
well as goal-orientated action. The prospect of increasing attendance to an expected three or four times per year in a conflict area may drive an agency to push to reduce fees in order to increase utilization to this expected goal.
Objective 4: To determine at what level fees must be to allow for adequate cost-recovery/sharing in health facilities.
Cost sharing is defined as a system in which users pay a proportion of the costs relating to health care service delivery. The World Bank had predicted that user fees would generate 15-20 percent of health expenditures before administrative costs were included (Creese and Kutzin, 1995).
None of the local health system staff were in favor of providing health care for free, however, for reasons other than those given by the World Bank. They argued that it could lead to abuse of the health system, take away patients’ dignity and would not be sustainable in the long run (especially not when the international organizations leave). In fact, most health staff strongly prefer to charge clients. Professional considerations for either improving or discontinuing the fee system, such as price elasticity and transaction costs, do not figure prominently in the decisions to adopt cost sharing. The immediate need for cash of the health staff and facilities routinely overrides other concerns. In addition, some donor organizations, such as the Programme d’Appui Transitoire au Secteur de la Santé, want to show that others, in particular the local population, also provide financial inputs.
The provincial health inspector officially determines the fee system, but in practice the NGOs influence the inspector’s decisions. Different provincial health inspections, and moreover, different agencies, work with different fee systems, causing fragmentation of the overall health system in the eastern DRC. The IRC, Malteser, and ASRAMES work with a bundled fee per illness episode that includes the consultation, drugs, and laboratory costs. Merlin works with variable rates that can differ by health zone based on (60 percent of) local private pharmacy prices. The patient pays for all services and drugs separately.
Setting up a well-functioning fee system is difficult for all the organizations involved. Choices that determine the type and size of the fees are
-
Bundled fee or fee per service?
-
Nominal (symbolic) fee or fee based on costs?
-
Adult or child?
TABLE 3-3 Potential Revenues When Populations Attend Facilities 0.5, 1, and 3 Times Per Year
|
Agency and Zone/Province |
Estimated Population |
Consultation Fees ($) as of December 2000 |
Under Age 5 Attendance |
Adult Attendance |
|
IRC—Katana |
347,000 |
Under 15 = 1 Adults = 2 |
(under 15) 173,500 |
173,500 |
|
IRC—Kabare |
142,000 |
Under 15 = 0.5 Over 15 = 1 |
(under 15) 71,000 |
71,000 |
|
Merlin—Kindu |
180,000 |
Unknown but estimated at 0.98a |
36,000 |
144,000 |
|
Malteser—Walungu |
504,000 |
Under 5 = 1 Over 5 = 2 |
100,800 |
403,200 |
|
ASRAMES—N. Kivu |
3,859,381 |
Under 5 = 0.5 Over 5 = 1 |
771,876.2 |
3,087,505 |
|
aUser fees for Kindu assumed to be the same as those for Maniema as cited in Poletti (2004). |
||||
-
Urban and rural areas?
-
Specific service exemptions: antenatal care, under 5 consultation, delivery, observation, surgery, etc.?
-
Waivers, for example for specific age groups, displaced people, or the indigent?
-
Reduction because of funding by other donors, for example, UNICEF? Some of the waivers include free drugs; for example, Merlin provides folic acid for pregnant women.
Table 3-3 shows revenues that would be gained as a result of utilization rates of half, 1.0, and 3.0 times per year and the percentage of all operational costs of the health facility that these revenues would make up.
|
Total Revenue 0.5 Times a Year |
Total Annual Revenue 1 Time a Year |
Total Revenue 3 Times a Year |
% Running Costs Only |
|
$260,250 average 32% indigent = 176,970 |
$520,500 average 32% Indigent = 353,940 |
$1,561,500 average 32% indigent = 1,061,820 |
(0.5/yr) 62% (1/yr) 124% (3/yr) 372% |
|
53,275a average 87% indigent = 5,860 |
106,550a average 87% indigent = 11,721 |
319,650a average 87% indigent = 35,162 |
(0.5/yr) 3.8% (1/yr) 7.6% (3/yr) 22.8% |
|
88,200 |
176,400 |
529,200 |
(0.5/yr) 24.2% (1/yr) 48.4% (3/yr) 145% |
|
453,600 |
907,200 |
2,721,600 |
Not calculable; no data on operational costs |
|
1,563,049 |
3,126,099 |
9,378,296 |
(0.5/yr) 25% (1/yr) 50.6% (3/yr) 150% |
REVENUES
IRC-Supported Health Facilities
According to the IRC, health facilities cost, on average, $850 per month. Applying this figure to Katana data means that health facility running costs would total $326,400 per year for all health facilities. Based on the ideal minimum standard goal of three visits per person per year, IRC revenues would result in revenues amounting to $1,061,820, taking into account free health care for indigent populations. Subtracting operational costs from total revenues would leave $735,420 for costs outside health facilities. This seems an enormous amount; however, we cannot estimate how much of the total cost of support, including IRC internal costs, of the
TABLE 3-4 Estimated Revenues from Nonindigent Use of Health Facilities and Reimbursements for Indigent Utilization June 2000-2001
|
Time Period |
Revenues Raised from Nonindigent Utilization of Health Facilities ($) |
Reimbursement Due for Indigent Use of Health Facilities ($) |
|
June-September 2000 |
$51,397.20 |
$33,994.80 |
|
October-December 2000 |
43,105.00 |
28,545.00 |
|
January-June 2001 |
53,966.00 |
35,232.00 |
|
TOTAL REVENUE 2000-2001 |
148,468.20 |
97,771.80 |
health system is covered on the basis of available information. Beyond this, the utilization at health facilities is not currently three times a year or even twice a year. Utilization, at its highest in Kabare health zone, is 1.15 per year, and in Katana, at its highest point, 0.8 per year—leading to the revenues described in Table 3-4.
The revenues gained through the IRC system would make up 46 percent of those needed to run health facilities alone on a month to month basis. However, this figure drops to 16 percent when the reimbursement for indigent populations is taken into account.
According to the allocation of resources at the IRC health facilities, spending on staff incentives would be 40 percent of revenues—that is, $59,387 ($20,278 without reimbursement) would be allocated to health staff. Estimating that an average health facility maintains at least 5 staff members, this would leave incentives of approximately $371 per year ($127 without reimbursement) per staff member per year. Written another way, one staff member’s incentive for one month’s work would be $31 (or $11 without reimbursement).
ASRAMES-Supported Health Facilities
Using the ASRAMES estimate, facilities require on average $1,400/month to function. Calculating for the ASRAMES clinics, this would require $4,569,600. Thus the actual estimated revenues raised comprise 46 percent of those required to run health facilities alone without any other operational costs included (Table 3-5).
TABLE 3-5 Estimated Revenues from Health Facilities in June 2000-2001
|
Time Period |
Estimated Attendance |
Revenue ($) Raised from June 2000-2001a |
|
June-September 2000 |
1,053,611 |
$790,208 |
|
October 2000-June 2001 |
1,752,159 |
1,314,119 |
|
TOTAL |
|
2,104,327 |
|
aFigures were taken as an average between rural and urban fees ($0.75). |
||
Staff incentives would be made up of 60 percent of revenues, in this case $1,262,596. Again estimating an average of 5 staff members per clinic, $956.50 per year would be available for each staff member. In reality, there are probably more staff being supported by incentives, and $956.50 is an overestimation.
Merlin-Supported Health Facilities
We were unable to calculate per capita expenditure in one year on the basis of available data.
Malteser-Supported Health Facilities
Based on IRC calculations for a similar area, the cost of health facility support per month is estimated at $850. Yearly costs for support to 25 health facilities would therefore require a total of $255,000. Based on the calculations for 2001, Malteser would raise 38.8 percent of required funds for health facility support alone from patient revenues. Staff incentives (again using an average of 5 staff per center) would be approximately $528 per person per year (Table 3-6).
TABLE 3-6 Estimated Revenues from Health Facilities in January-December 2001
|
Under Age 5 Attendance |
Over Age 5 Attendance |
Total Estimated Revenues Raised ($) from Jan 2001-December 2001 |
|
$21,731 |
$86,923 |
$97,789 |
Objective 5: To identify the managerial problems that confront the four NGOs.
REVENUES AND THEIR CONTRIBUTION TO THE HEALTH SYSTEM
No organization has made progress with cost sharing to the extent that local health centers can gradually assume responsibility for purchasing essential drugs and equipment. In other words, due to the war, the health system cannot go back to full cost recovery.
-
High enough revenues are important to ensure staff motivation. Cost sharing generally does not generate sufficient resources to do so. If the Sphere standard were reached, however, such a level of revenues could be achieved. But paradoxically, the fee would need to be lowered to increase utilization, which means lower revenues per patient.
-
Deciding where to allocate revenues (see Table 3-1 for actual revenue allocation):
-
Incentives take between 40 and 70 percent. It is safe to assume that incentives should be at least 40 percent.
-
Running costs vary from 10 to 30 percent for health centers and from 10 to 25 percent for zone bureaus.
-
Savings should contribute to running costs or buying medicine once the NGO terminates its support.
-
The direct subsidies, especially to zone bureaus, require more attention, in particular such issues as transparency and interplay with cost sharing.
-
ECONOMIC AND SECURITY SITUATION
Organizations can provide free health care after a natural disaster, such as after the Nyiragongo eruption that destroyed large parts of Goma. Free health care during an acute stage can be available for a small period of time and, hence, uses a limited amount of resources. With chronic emergencies, free health care becomes more difficult. In these situations, health care is often caught in a vicious cycle of the local population’s inability to pay, worsening access, lower quality, and destruction of capacity. Can partial cost recovery—in other words, cost sharing—help to break this cycle? And together with international support can it put a more progressive cycle into motion?
The contribution of cost recovery/cost sharing is limited to covering only a part of the total operational costs, mainly drugs and supplies. International support thus remains necessary. Yet the organizations cannot create peace or a well-functioning state that is able to stop warlord politics in order to support health and other social services. Nor can they ensure a resumption of economic growth. As the World Health Organization/UNICEF Joint Mission (18-29 June 2001:2) argued, without opportunities for the households to increase income and reduce barriers to essential social services, “the [health] situation will continue to spiral down rapidly.” In this sense, the organizations face a sustainability dilemma (see MacRae, 2001). It also shows the limits of cost recovery/cost sharing: if a large part of the population becomes indigent, as in the Kabare health zone, does it make sense to continue cost recovery? The international organizations are divided on this, but most local health staff do not want to lose these resources. They will promote cost recovery as long as there is no functioning state.
ROLE OF THE DONORS
Current cost-sharing revenues are not high enough to ensure autofinancing of the health system. As a result, donors need to find better ways to fund continuing programs in chronic crises, because neither a traditional relief nor a developmental approach sufficiently addresses these long-lasting emergencies.
The different approaches of donors, for example with funding for hospital care, do have a strong impact. Nowadays, the Office of U.S. Foreign Disaster Assistance helps the IRC with funding for indigent referral to the hospitals. The Humanitarian Aid Office of the European Union more strongly incorporates hospital support. The Department for International Development, advocating free health care, did not want to fund IRC’s cost-sharing program in Kabare, which led to a 16-month interruption of program activities until OFDA took over funding. Nor will UNICEF, which also prefers free care, appreciate the 10 percent fee raise of ASRAMES.
Funding in chronic emergencies is normally given for 6-month periods. Rarely are projects funded for more than one year. Thus, the issue of long-term planning and strategy formulation becomes difficult for agencies when funding is so short term. In addition, writing proposals and reports for the donors is labor-intensive. The organizations spend considerable time and resources to get the proposals accepted.
LOCAL MANAGEMENT
The main direct impact of the provincial health inspection is its determination of the fee structure, which differs from province to province. For the local health staff, varying from health center to provincial health inspection, the lack of revenues is a continuous concern that negatively impacts motivation. Local staff strongly feels the dilemma between lowering fees to raise access and increasing fees in the hope of a higher degree of financial sustainability. They tend to prefer to raise fees in order to make a decent living or at least to survive. In the DRC, the bad economic situation and insecurity create an incentive for short-term economic gain; the health system is no different in this respect.
The provincial health inspection and health zone management officials often worry that the international organizations and donors do not work sufficiently with them and bypass them when making important decisions or getting information out to the public, locally as well as internationally. At the same time, local health staff and management acknowledge that they do lack capacity. This brings up the question whether international support should focus on control and supervision, or whether these resources could be used directly to ensure motivation. Except for Malteser, the organizations in this study made the trade-off by emphasizing supervision, control, and capacity building.
Finding a balance between the hands-off contract approach and the intensive supervision approach ultimately depends on the managerial and professional skills of the zone bureau, provincial health inspection, and other health service staff. It is clear that the zone bureaus and local health staff require technical and management support. The control mechanisms for the contract approach should be established clearly in advance (goals, reporting procedures, supervision, evaluation, and so on). For the organizations in this study, the crucial question will be whether the zone bureau and other health staff have the capacity to operate well with minimal supervision. A related question concerns whether they can be trusted to operate well with minimal supervision. Currently, the organizations prefer capacity building and control. In this sense, they have moved away from traditional relief and rehabilitation, to a long-term presence that stresses intensive support and control. A hands-off contract approach is not feasible; the intensive contract approach with a relatively high degree of supervision is more likely. Still, the zone bureaus and provincial health inspection would prefer a stronger reliance on their own structures.