2
Current and Future State of Performance Measurement and Reporting
CHAPTER SUMMARY
This chapter provides an overview of the current state of health care performance measurement and reporting. To better align and coordinate existing efforts in this area, the committee calls for a national system for performance measurement and reporting and identifies key attributes of a well-functioning system that can meet this need.
In recent years, improving health care quality has become a top priority for all major stakeholders in the health care system—the federal government, group purchasers, health care professionals, health care providers, state governments, oversight organizations, consumer groups, and others. Hundreds of efforts now under way, including public reporting, pay-for-performance, and ongoing quality improvement programs, are aimed at enhancing quality.
Many public- and private-sector health care programs now engage in public reporting of data that allow comparison of the quality of institutional and provider performance. The Centers for Medicare and Medicaid Services (CMS) produces comparative quality reports on many of its participating providers, including health plans, hospitals, nursing homes, home health agencies, and renal dialysis centers (CMS, 2005c). The National Committee for Quality Assurance (NCQA) makes available comparative quality information on health plans (NCQA, 2005c). State governments, private purchasers, coalitions, and others operate additional public reporting programs (AHRQ, 2003; CMS, 2003; Joint Commission Resources, 2005; NBCH, 2004; New York State Department of Health, 2004). A recent review of hospital reporting initiatives found 45 Web sites in the United
States and two in other countries that provide online comparative hospital performance information (Delmarva Foundation, 2005).
Widespread concerns about quality have stimulated quality improvement efforts at all levels of the health care system. Quality monitoring and improvement are critical responsibilities of all types of health care providers, and quality improvement is now regarded as a core competency that all types of health care professionals should possess. Major accreditation and certification bodies have increased requirements for monitoring and demonstrating improvements in quality and safety (ABIM, 2005; JCAHO, 2004; NCQA, 2000). And Medicare, through its Quality Improvement Organization Program, provides about $350 million per year for surveillance functions and technical assistance (U.S. DHHS, 2004a).
In an effort to reward providers for improvements in quality, many private purchasers and health plans have implemented pay-for-performance programs that characteristically link a modest amount of provider payments to performance across a number of measures (Dudley, 2005; Rosenthal and Booth, 2004; Rosenthal et al., 2005). In addition, the public sector has been active in conducting demonstration projects linking performance on a set of standardized measures to bonuses, calling for “value-based purchasing” (U.S. Congress, 2005a,b; U.S. DHHS, 2002, 2004b).
Reflecting the priority accorded to improving quality, many private organizations, such as health plans, hospitals, provider groups, and professional associations, have made considerable progress in developing measures that capture important areas of clinical care and organizational performance. Measures of patients’ perceptions or experiences of care have emerged through efforts of consumer advocates. CMS has also demonstrated leadership in encouraging the development of these measures through demonstration projects.
The development of multiple quality measures has been driven by stakeholders eager to see certain features of care recognized and rewarded as part of quality improvement initiatives. These efforts rely greatly upon consensual efforts and private support from key membership organizations. Yet while the private sector has made valuable contributions in moving the quality agenda forward through pioneering and innovative efforts, the emerging quality measures resulting from these efforts are unable to address all six aims for the health care system articulated in the Quality Chasm report (IOM, 2001): safety, effectiveness, patient-centeredness, timeliness, efficiency, and equity. The current patchwork of existing measures fluctuates over time and includes many gaps when assessed against the six aims. Few or no measures exist in the areas of efficiency, equity, and patient-centeredness. In addition, the variety of measures that exist in certain areas creates competing demands for data that can be burdensome to providers.
The magnitude of the various quality improvement initiatives has generated high expectations for the use of valid, objective, and reliable performance measures. All of these initiatives—public reporting, quality improvement within providers’ offices, and pay for performance—depend upon the availability of an array of measures whose implementation can contribute to realizing the fundamental aims of the nation’s health care system. The committee concludes that federal leadership is necessary to ensure that performance measures address all six aims, as well as to balance private-sector initiatives with investments in quality measures for neglected areas that may lack strong constituencies. Federal leadership is also essential to provide stability, coordination, and direction when fluctuations and tensions in the health care system create an unpredictable environment for data collection and reporting. The challenge is multifaceted:
-
To identify the national goals that performance measures should serve.
-
To clarify data requirements in areas in which multiple measures have been proposed.
-
To identify areas in which greater effort is needed.
-
To build the capacity to produce, report, and analyze performance data throughout the public and private sectors of the health care system.
PERFORMANCE MEASUREMENT AND REPORTING: WHAT DO WE MEAN?
Quality-related efforts in all of the areas noted above—public reporting, quality improvement initiatives, and pay for performance—rely on some form of performance measurement and reporting. Components of a system that can perform these functions include the following:
-
Standardized performance measures—Performance measures include measures of the health care process (e.g., periodic blood and urine tests for diabetic patients), patient outcomes (e.g., 60-day survival rate for cardiac bypass patients), patient perceptions of care (e.g., experience with patient–provider communication), and organizational structure and systems associated with the ability to provide high-quality care (e.g., medication order entry systems). Standardized performance measures are those with detailed specifications (e.g., definitions for the numerator and denominator, sampling strategy if appropriate) allowing for “apples-to-apples” comparisons, sometimes requiring effective risk adjustment or stratification of results across key subgroups.
-
Access to patient data—Calculation of many performance measures requires access to patient-level data from administrative files and chart
-
reviews. Other measures require asking patients to complete surveys that allow assessment of their perceptions of their care, their quality of life, or their functional status.
-
Data verification and auditing—A key element of a quality measurement and reporting system is ensuring that data for performance measures are reported accurately. For many measures that are submitted by individual providers (i.e., self-reported), an external auditing function is often desirable and, for some regulators, mandatory.
-
Comparative analysis and reporting capability—A performance measurement system that produces information to support the decisions of consumers, purchasers, referring physicians, and other stakeholders in choosing plans, providers, or treatment options requires some form of effective comparative reporting capability. Similarly, improvement efforts that draw on knowledge of best practices benefit from comparative data.
While the current proliferation of measure sets and related reporting activities provides important building blocks for a performance measurement and reporting system, it may have unintended consequences. The above components frequently draw upon different data sets. Excessive attention and energy may be required of providers to comply with externally imposed reporting requirements and quality improvement priorities. These resources may be diverted from patient care and internally generated quality improvement efforts. External reporting requirements that fail to yield readily understandable, pertinent, and reliable information may result in frustrated consumers and angry providers. It is not surprising, then, that numerous expert panels have identified the need for greater standardization of performance measures and reporting requirements (IOM, 2002; President’s Advisory Commission on Consumer Protection and Quality in the Health Care Industry, 1998).
This chapter includes three sections. The first provides an overview of recent efforts to promote standardized quality measurement and reporting. The second lays out a rationale for a national system for performance measurement and reporting. The final section draws on this analysis and the work of other groups to define the key attributes of an effective national system, including 10 design principles the committee believes should guide the system’s development.
RECENT EFFORTS TO PROMOTE STANDARDIZED PERFORMANCE MEASUREMENT
Efforts to standardize quality measurement and reporting in the health care system have been under way for more than 15 years. Of particular significance are the early pioneering efforts of NCQA, the Agency for
Healthcare Research and Quality (AHRQ), the Joint Commission on Accreditation of Healthcare Organizations (JCAHO), and CMS. In recent years, recognition of the need to coordinate and harmonize quality measurement has led to increased collaboration. Widespread participation in standardized measurement and reporting activities has occurred among private purchasers (such as those in the Pacific Business Group on Health, the Leapfrog Group, and Bridges to Excellence), public purchasers (especially CMS, the largest purchaser), private-sector organizations (such as the National Quality Forum [NQF]), and health plans (such as PacifiCare and Aetna).
Pioneering Programs
One of the oldest and perhaps most successful quality measurement efforts is the Health Plan Employer Data and Information Set (HEDIS), first released in 1989 by a coalition of health plans (members of The HMO Group) and large employers. The initial set of measures was subsequently adapted and refined by NCQA (NCQA, 2005b). Health plans seeking accreditation by NCQA are required to report on HEDIS measures, and their performance scores on these measures are factored into the accreditation process.
Originally spearheaded by private purchasers, HEDIS was adapted in the mid-1990s for use by public purchasers (NCQA, 2005b). CMS now requires health plans participating in the Medicare program to submit data on HEDIS-developed measures of health care quality, many of which are incorporated in comparative quality reports available on the CMS Web site (CMS, 2005d). Many state governments also require plans participating in Medicaid to report HEDIS data (New York State Department of Health, 2002; Texas Health and Human Services Commission, 2004; Washington State Department of Health and Human Services, 2005). Additionally, HEDIS measures are frequently used in the nearly 90 pay for performance programs sponsored by private purchasers (Rosenthal et al., 2004).
Most though not all health plans produce HEDIS reports for their privately insured populations. Those plans that choose not to participate in HEDIS reporting are likely to be the very lowest performers (McCormick et al., 2002). NCQA’s Quality COMPASS data repository includes comparative HEDIS reports for more than 300 commercial managed care products (NCQA, 2005c). However, as only health maintenance organizations (HMOs) report on HEDIS measures, recent declines in HMO relative to preferred provider organization enrollment have resulted in a decrease in the total population included in the reporting pool. CMS is attempting to address this problem, at least within the Medicare program, and a few employers are beginning to look at HEDIS measures for the commercial sector.
An important complement to HEDIS has been a 10-year program to develop a family of patient survey instruments under the leadership of AHRQ (AHRQ, 1998). Working with a consortium of private-sector research organizations (including Harvard Medical School, Research Triangle Institute, RAND, and, more recently, the American Institutes for Research), AHRQ released the Consumer Assessment of Health Plans Survey (CAHPS) instrument in 1997 to capture consumer assessments of care received. The original CAHPS survey is now required by NCQA for health plan accreditation, and is used by many public and private purchasers (e.g., CMS’s Medicare program, many state Medicaid programs, the Federal Employees Health Benefit Plan, and many private employers and business coalitions), as well as quality oversight organizations. The CAHPS family has expanded to include a survey of behavioral health services, recently developed with support from AHRQ and the MacArthur Foundation (CAHPS Survey Users Network, 2005; Shaul et al., 2001). The CAHPS program has also evolved to to include various settings of care, and the acronym now stands for the Consumer Assessment of Healthcare Providers and Systems. A version of CAHPS for hospitalized patients has recently been completed (AHRQ, 2004). Other survey instruments are in various stages of development. These include both a health plan survey and a clinician and group survey (developed through the Ambulatory CAHPS process) and two versions of a nursing home survey—one for residents and the other for family members and others who visit residents regularly (CAHPS Survey Users Network, 2005). Also under development is a survey for patients receiving in-center hemodialysis treatment (CAHPS Survey Users Network, 2005).
In the area of hospital care, both the Department of Health and Human Services (DHHS) and JCAHO have played important roles. The development of standardized performance measurement and public reporting programs for hospitals dates back to 1986, when the DHHS Health Care Financing Administration (now known as CMS) released comparative reports on hospital mortality (HCFA, 1987). Also in the mid-1980s, JCAHO developed and field tested six sets of standardized performance measures (perioperative care, obstetrical care, trauma care, oncology care, infection control, and medication use) and announced its intent to require accredited hospitals to collect and submit data on these measures (JCAHO, 2005d). Both of these early efforts were abandoned in the face of strong objections from the hospital sector and others.
In the late 1990s, JCAHO embarked on a second effort to implement performance measures as a condition of accreditation for hospitals, long-term care organizations, networks, home health agencies, and behavioral health care organizations. Health care organizations were allowed great discretion in selecting measures from a large menu, and the measure specifications were not standardized (JCAHO, 2005d). In 2002, JCAHO intro-
duced a set of standardized core measures into its performance requirements for hospitals (JCAHO, 2005c). Hospitals seeking accreditation (approximately 95 percent of acute care hospitals) are currently required to submit data on three of five standardized measure sets (acute myocardial infarction, heart failure, pneumonia, pregnancy and related conditions, and surgical infection prevention) (JCAHO, 2005a). During the next 5 years, JCAHO plans to introduce standardized measures for other types of organizations and clinical conditions (JCAHO, 2005b). In 2004 CMS, working collaboratively with the American Hospital Association and other partners, announced a voluntary hospital reporting initiative linking a hospital’s payment update under Medicare to the submission of data for a set of standardized measures from the JCAHO ORYX system (CMS, 2004). In April 2005, CMS began publicly reporting hospital comparative data based on these measures via its Web-based tool, Hospital Compare (CMS, 2005b).
In the area of long-term care, CMS has played a pivotal role in the development of standardized performance measures. Starting in the mid-1980s, CMS supported the development of patient assessment instruments used by organ transplant centers, nursing homes, and home health agencies. The Minimum Data Set (MDS), the assessment instrument for nursing home patients, was first implemented by CMS in 1990 (Manard, 2002). By 1999, a set of 24 quality indicators based on MDS data had become part of a routinely administered nursing home survey; in 2002, CMS also established a Web-based reporting mechanism, Nursing Home Compare, to provide the public and other stakeholders with comparative quality data on nursing homes (CMS, 2005c; Manard, 2002). In 1999, CMS furthered its efforts by requiring home health agencies to submit patient assessment data using the Outcome and Assessment Information Set (AHRQ, 2002); CMS started making comparative quality data for home health agencies available in 2003 on its Home Health Compare Web site (CMS, 2005c).
In summary, these pioneering performance measurement initiatives have provided a foundation for the identification of standardized measures; laid the groundwork for collaboration; and built a broad base of stakeholder support for public reporting, pay for performance, and quality oversight programs.
Widespread Collaborative Efforts
As the twenty-first century approached, the need to coordinate the national bodies involved in the promulgation of standardized performance measures became increasingly apparent. In addition to the efforts of the major national players, dozens of more narrowly focused or local efforts were aimed at establishing new standardized measure sets. Concern arose that the absence of a national infrastructure for performance measurement
would impose an enormous burden on providers, institutions, and health care professionals. More important, the time and resources available to providers to support quality improvement efforts would increasingly be consumed by data collection across a wide range of measures, resulting in less time and fewer resources available for the redesign of care processes.
It also became clear that many stakeholders would use standardized measures and data for a variety of purposes, including public reporting, pay for performance, quality improvement, and professional certification. The existing patchwork of measurement and reporting efforts could not be relied upon to respond to the diverse information needs of consumers, purchasers, providers, and other stakeholders. Publicly available performance information varied greatly in terms of availability by geographic area, participation of various types of providers, comprehensiveness and relevance of quality measures, validity and reliability of data, and usefulness of public reporting formats. Health care leaders recognized the need for a national infrastructure and process for setting goals and priorities for performance measurement and improvement, promulgating standardized measure sets for use by all stakeholders, and streamlining data collection and reporting.
In 1998, the President’s Advisory Commission on Consumer Protection and Quality in the Health Care Industry identified key components of a national quality strategy and infrastructure, including (1) the promulgation of a set of aims for improvement, accompanied by specific, measurable objectives; and (2) a measurement and reporting system consisting of standardized measures and data collection and reporting capabilities. The commission also recommended creating two public–private partnership entities (President’s Advisory Commission on Consumer Protection and Quality in the Health Care Industry, 1998):
-
Advisory Council for Health Care Quality—The expert advisory council would identify national aims and specific objectives for improvement, establish goals and objectives for measurement, and track and report on the nation’s progress. The council would be located in the public sector and publicly financed.
-
Forum for Health Care Quality Measurement and Reporting—The forum would define a plan for implementing quality measurement, data collection, and reporting standards, and identify and update core sets of quality measures and standardized reporting methods. The forum would be a private-sector membership organization, financed by member dues.
In 1999, the private-sector component, NQF, was established by a Forum Planning Committee convened under the auspices of the office of the Vice President of the United States. However, the public-sector component (the Advisory Council for Health Care Quality) was not established by
Congress. At the time, other important initiatives, such as the Patient’s Bill of Rights, were competing for the President’s and Congress’ attention and resources. Furthermore, the importance of establishing a public entity that would be responsible for identifying aims for quality improvement, setting national goals for measurement and reporting, and tracking progress was not fully recognized or supported by political will. In hindsight, this omission can be viewed as a missed opportunity.
Once operational, NQF created a Strategic Framework Board (SFB) to provide advice and counsel as it began to pursue its mission. Operating independently from NQF, the SFB consisted of nine experts with a broad spectrum of research and managerial experience. The board’s purpose was to (1) design a strategy for national performance measurement and reporting, (2) articulate the guiding principles and priorities for a national system, and (3) identify potential barriers to successful implementation and propose possible solutions (McGlynn, 2003). The SFB was also conceived as a means to fulfill one of the intended roles of the proposed Advisory Council for Health Care Quality: to create and sustain a “dynamic tension” designed to bring an aspirational dimension to the forum’s work.
NQF continues today as a not-for-profit membership organization whose governing board includes representatives of consumers, public and private purchasers, employers, health care professionals, provider organizations, health plans, accrediting bodies, labor unions, and other stakeholders. Financial support for the organization comes from two major sources: member dues and project-specific contracts and grants.
The mission of NQF is “to improve American healthcare through endorsement of consensus-based national standards for measurement and public reporting of healthcare performance data that provide meaningful information about whether care is safe, timely, beneficial, patient-centered, equitable and efficient” (NQF, 2005a). The accomplishments of NQF include the following:
-
Establishment of a well-described process for endorsing voluntary consensus standards that satisfies the requirements of the National Technology Transfer and Advancement Act of 1995 (NQF, 2004b).
-
Review and endorsement of measure sets applicable to numerous health care settings and clinical areas and services, for example, hospital care, diabetes care, and nursing sensitive care (NQF, 2002b, 2003b, 2004a).
-
Conduct of educational and convening activities that address key health care challenges, such as patient safety, health care disparities, and the implementation of information technology (NQF, 2002a, 2003a,c).
Despite these noteworthy achievements, the vision for the NQF articulated by the President’s Advisory Commission has not yet been fully real-
ized. Indeed, the forum’s experience offers valuable lessons learned with regard to the essential components of an effective and sustainable national performance measurement and reporting strategy. The absence of a public arm (the Advisory Council for Health Care Quality) has created a national leadership vacuum and led to insufficient funding for quality improvement initiatives. Consequently, NQF—whose structure is based on a private-sector business model—has few alternatives to depending on outside sources to support its work. Thus, its projects tend to reflect the priorities of available funding sources rather than addressing a discrete set of national goals. As a result, a comprehensive strategy for the development and implementation of health care performance measures does not yet exist. While many collaborative efforts are under way, they are not coordinated; they do not include all the key organizations; and they are not taking place in the context of a comprehensive and ongoing plan specifying aims for improvement, measure development, and implementation.
Although a complete national infrastructure for standardized performance measurement and reporting has not emerged, major national standards-setting bodies, in concert with key public and private purchasers, have taken important actions to focus and harmonize measurement efforts. Much of this collaborative work has focused on performance measurement for physician practices—a particularly challenging problem for several reasons. First, public and private purchaser data must be pooled to obtain meaningful information on small practice settings. Individual insurers do not account for a large enough share of a provider’s practice to yield meaningful measures of performance. Second, some aspects of performance are difficult or impossible to assess. At the disease-specific level, for example, individual doctors may simply not see enough patients, and therefore their individual practices cannot yield enough data to support reliable or valid characterizations of their performance (Hofer et al., 1999). Third, growing awareness of the systemic nature of both excellence and defects in quality has increased support for the concept that all providers involved in a patient’s care share responsibility for the quality of the care process and for patient outcomes. Designing and implementing shared incentives and reward processes that fairly reflect the degree of influence and responsibility of each individual provider is a new challenge.
In 1998, the American Medical Association (AMA), JCAHO, and NCQA established a Performance Measurement Coordinating Council to integrate the development of performance measures and to “speak with a common private-sector voice on critical public policy issues related to quality and performance measurement” (AMA et al., 2001a). In 2001, the council released pain management assessment and management standards and a standardized measure set for diabetes (AMA et al., 2001a,b; American Pain Society, 2000).
In 2002, the AMA established the Physician Consortium for Performance Improvement, building on prior efforts including the AMA Physician Office Assessment program (AMA, 2002). The consortium, which includes representatives from more than 50 national medical specialty societies, AHRQ, and CMS, has developed measure sets in the following areas: asthma, coronary artery disease, diabetes, heart failure, hypertension, depression, osteoarthritis of the knee, prenatal testing, and preventive care and screening (AMA, 2005). Working collaboratively with JCAHO and NCQA, the consortium recently released a set of Principles for Performance Measurement in Health Care (Physician Consortium for Performance Improvement, 2004).
In 2004, the Physician Consortium for Performance Improvement, CMS, and NCQA released a set of ambulatory care clinical performance measures relevant mainly to primary care (AMA, 2005). This ambulatory measure set includes measures from HEDIS, the various measure sets of the Physician Consortium for Performance Improvement, and measures developed by the federal government (i.e., CMS and the Veterans Health Administration). Most of the measures require use of the costly chart review abstraction method and are therefore expensive to administer.
To build more consensus around a set of standardized measures for physician practices for use in public reporting and pay for performance, the Ambulatory care Quality Alliance1 (AQA) was launched in the fall of 2004. The alliance has endorsed a standardized set of 26 measures for physician practices that draws heavily on the 2004 ambulatory care clinical performance measure set released by the Physician Consortium for Performance Improvement, CMS, and NCQA, thereby eliminating duplication (ACP, 2005). Concurrently with the work of AQA, NQF conducted an expedited review of ambulatory care clinical performance measures; a set of these measures was endorsed in August 2005 (NQF, 2005b). The administrator of CMS has hailed this initial ambulatory measure set as a “milestone” and pledged CMS’s support for the alliance’s continued efforts (McClellan, 2005). All of the ambulatory measures endorsed by NQF2 and the subset of those measures adopted by AQA are “owned” by the Physician Consortium for Performance Improvement or NCQA. The NCQA measures in that set are adaptations of HEDIS measures (used at the health plan level) that have been respecified for use at the physician office level in situations where there is no enrolled population.
In addition to public reporting and pay for performance programs, performance measurement systems are now used to support several provider recognition and certification programs. Working in partnership with the American Diabetes Association and the American Heart Association/American Stroke Association, NCQA has established the Diabetes Physician Recognition Program and the Heart/Stroke Physician Recognition Program to identify physicians who demonstrate high-quality care in these clinical areas (NCQA, 2005d). A third physician recognition program, Physician Practice Connections, was developed by NCQA and then adapted to a pay-for-performance application in collaboration with several physician bonus programs, such as Bridges to Excellence and the pay-for-performance program of California’s Integrated Healthcare Association. Physician Practice Connections recognizes physician practices that use up-to-date information systems, as well as achievements in such areas as delivery system design, patient self-management support, and decision support that enhance patient care. In February 2005, NCQA and the American Board of Internal Medicine (ABIM) announced an agreement to harmonize their measure systems and activities pertaining to physicians so that internists can submit performance data to NCQA, which in turn will share results with ABIM (NCQA, 2005a). NCQA will use the performance data in its physician recognition programs, while ABIM will use the data in its maintenance-of-certification processes.
In yet another collaborative effort, CMS has furthered its commitment to advancing measure development by awarding a contract for specialty and subspecialty measure development to Mathematica Policy, in collaboration with the Physician Consortium for Performance Improvement and NCQA, starting October 1, 2005. This represents what could be a new level of collaboration around measure development between private-sector entities and CMS (CMS, 2005a).
In summary, the pioneering efforts of a number of organizations have altered the performance measurement landscape (see Appendix B for a synopsis of the contributions of these organizations). Although current national measure sets constitute the major accomplishments, dozens of “niche” measurement sets have emerged as well. The committee reviewed this array of measures (discussed further in Chapter 4) and identified many areas of duplication, inconsistency in specifications, and serious gaps in the assessment of important components of quality care. To overcome these limitations, some key players are collaborating on the development of measure sets that standardize specifications for multiple uses. Beyond harmonization, however, more leadership is necessary to shift the mounting array of efforts from one that is driven principally by individual stakeholder interests to one that is focused on a set of national goals developed through a deliberative process that reflects both public and private concerns.
PERFORMANCE MEASUREMENT EFFORTS IN OTHER COUNTRIES
The United States is not alone in its efforts to improve performance measurement in health care. Many other nations, for similar reasons, have developed research agendas and public policy initiatives in reporting, assessment, regulation, and improvement of care that depend upon standardized performance measures. Although performance measurement and reporting systems are tailored to each country’s political, social, and economic context, much can be learned from those experiences. For one thing, performance measurement in other countries demonstrates the potential value of centralized leadership and a streamlined, coordinated approach. The United States would therefore benefit from a careful assessment of the efforts of the United Kingdom, Australia, and other nations.
Perhaps the strongest such example in the past decade has been the Modernisation Program of the English National Health Service (NHS Modernisation Agency, 2003). In 1998, the Labor government in the United Kingdom, under Prime Minister Tony Blair, launched a massive effort to increase investment in health services from the then-current level of about 6.5 percent of gross domestic product to the European average of about 8.5 percent over 5 years (New Statesman, 2000). A series of carefully developed National Service Frameworks was created to guide this massive new investment and to ensure the value of the Modernisation Program. The frameworks specified hundreds of goals, benchmarks, and associated measures for targeted clinical areas, such as heart disease, cancer care, orthopedics, and primary care. Various agencies and departments within the government were charged to measure, track, and report on progress. That effort continues today. (Note that although the National Health Service has counterparts in Scotland, Wales, and Northern Ireland, the Modernisation Program described here is that in England, rather than throughout the United Kingdom.)
The new government contract with general practitioners constituted a second major advance in measurement and public reporting in the National Health Service (Roland, 2004; Smith and York, 2004; Stevens, 2004). That contract included a bold and innovative measurement system, in which general practitioners are assessed on a 1,050-point system with respect to several dozen performance measures encompassing both structural and process variables in their practices. Substantial financial incentives are linked to point scores at the practice level. The effects of this new contract on care are now under active assessment through several government-sponsored research projects.
Australia established a Council for Safety and Quality in Health Care in January 2000, led by Australian health ministers, to guide national efforts to improve safety and quality throughout the country’s health care system. The council reports annually to all health ministers, is supported by
all state and territorial jurisdictions, and works closely with other national bodies to complement the efforts of others working to improve care (Australian Council for Safety and Quality in Healthcare, 2004). In January 2005, the council awarded $1 million in grants for 50 innovative projects across Australia to address specific patient safety and quality issues (Australian Council for Quality and Safety in Healthcare, 2005). These efforts have also led to a groundswell of companies implementing multiple ways of measuring and reporting on performance, thus becoming truly transparent and accountable (Australian Government, 2002).
LIMITATIONS OF CURRENT PERFORMANCE MEASUREMENT EFFORTS
The above discussion highlights the scope of performance measurement activities currently under way and the high expectations for these efforts. It also underscores the deep commitment of many key stakeholders to performance measurement and the remarkable progress that has been achieved through their collective efforts. At the same time, the committee believes the current approach to quality measurement in the United States falls short of constituting an effective national system for performance measurement and reporting for the following reasons:
-
The current approach fails to set goals and aims consistent with the vision of the Quality Chasm report. The focus of the measures presently available is too narrow and does not move the health care system toward that bold vision.
-
The current approach produces measures that are inconsistent, complex, and unstable, imposing on providers of care uncertainty and the burden of conflicting measures.
-
The current approach faces a continually uncertain future because of inadequate and unstable funding and persistent conflicts among stakeholders, relying on fragile consensus-driven procedures.
-
The current approach learns too little and too late from successes and failures. The evidence base for quality improvement, public reporting, and pay for performance is thin, and will remain so without cogent and well-supported evaluation.
Creating a coherent national system that can help stakeholder groups work more effectively, respond to their various needs, and address gaps in leading measure sets is a major challenge. To create such a system, strong, independent leadership is needed to coordinate current efforts. Sustained, adequate funding will be essential to support a structure capable of encouraging multiple initiatives while also withstanding the pressures of narrow
stakeholder interests, as well as keeping patients’ interests in the foreground. An investment in learning how measurement can best accelerate improvement is imperative as well.
In light of the long history of multiple, sometimes competing efforts to promulgate and report on performance measures, it appears unlikely that the current activities of key stakeholders will lead to the national system that the IOM committee believes to be crucial to quality improvement. To overcome the limitations delineated above and to ensure the emergence of a viable national system for performance measurement and reporting, performance measurement will need to be embraced as a public good requiring leadership—though not a takeover—from the federal government. In the next section, the committee sets forth the attributes of such a national system and proposes a conceptual framework to guide its development.
ATTRIBUTES OF A WELL-FUNCTIONING SYSTEM FOR PERFORMANCE MEASUREMENT AND REPORTING
The major limitations of current performance measurement and reporting capabilities are briefly summarized in Table 2-1. The table also suggests how each of these limitations can be reframed as key attributes of a well-coordinated national system for performance measurement and reporting.
In developing the concept of a national system, the committee drew heavily on the earlier work of the Strategic Framework Board.3 The committee also conducted a systematic examination of several physician practices that illuminated potential success factors and barriers to the implementation of performance measurement (see Appendix C for details). The committee’s analysis led to the conclusion that a national system should possess the following attributes (see Figure 2-1):
-
Specify a purpose and aims for the health care system.
-
Set national goals.
-
Establish and implement a plan for the development and promulgation of performance measures.
-
Ensure data collection, data validation, and aggregation processes.
-
Develop and promulgate public performance reports to support the decisions of many stakeholders.
-
Establish and fund necessary research.
-
Continually evaluate, through an impact assessment, the effectiveness of performance measurement, payment reform, and quality improvement initiatives.
TABLE 2-1 Major Limitations of Efforts to Measure the Performance of the U.S. Health Care System and Corresponding Attributes of a National System for Performance Measurement and Reporting
|
Limitations of Current System |
Corresponding Attributes of a National System for Performance Measurement and Reporting |
|
Purpose/aims—No coherent approach to specifying purposes and aims of measurement. |
Specify a clear national purpose for the health care system and explicit aims for improvement. |
|
Measures—Limited scope of measurement (failure to measure in many domains) and a multiplicity of competing measures in some domains. Lack of clarity and uniformity prevents information technology vendors from planning to include measures. |
Establish a national system of standardized performance measures that are linked to aims, comprehensive in scope, and aligned with current and expected capabilities for reporting. |
|
Data aggregation/reporting—Lack of standardization, multiple conflicting stakeholders collecting data independently, unjustifiable reporting burden on providers, and reporting that often confuses consumers. |
Ensure well-developed data collection and aggregation processes to minimize the burden on providers while ensuring efficient measurement across payers and providers. Develop public reports that are valid, understandable, and actionable. |
|
Funding—Inadequate and unstable funding for performance measurement activities and research. |
Sustain adequate funding for a structure able to withstand pressures of stakeholder interests and keep patients’ needs in the foreground. |
|
Capacity to learn—Efforts to improve quality constrained by a lack of evidence on the effectiveness of alternative improvement strategies, potential adverse effects of measurement, best ways to communicate quality information to providers and consumers, and effectiveness of pay-for-performance initiatives. |
Evaluate the effectiveness of performance measurement, public reporting, and payment systems and quality improvement initiatives to minimize potential adverse effects, detect unintended consequences, and maximize the eventual benefits of performance measurement. |
Additionally, the committee concluded that a national system should support the needs of stakeholders within the public and private health care sectors along three dimensions:
-
Accountability—Many stakeholders make important decisions that motivate or influence care delivery. Purchasers and consumers make decisions about the selection of health plans, providers, and treatment options;
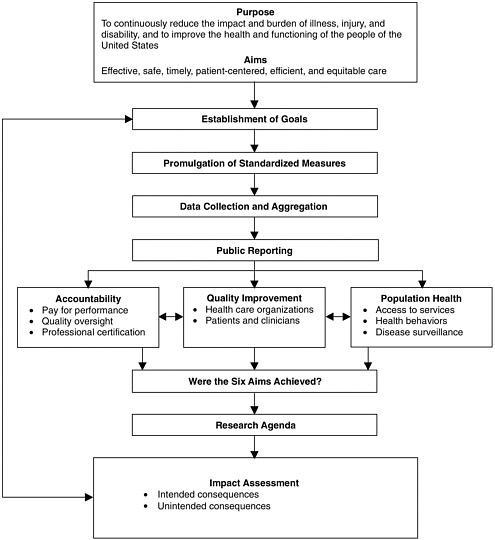
FIGURE 2-1 A national system for performance measurement and reporting.
SOURCE: Adapted from Strategic Framework Board (McGlynn, 2003).
-
clinicians about the referral of patients to specialists, hospitals, and other providers; public- and private-sector oversight organizations about licensure, accreditation, board certification, and recognition awards; and health plans about which providers to include in their networks.
-
Quality improvement—Stakeholders engaged in the delivery of health care services need information they can act upon to improve the quality of those services. Clinicians need performance data to support on-
-
going quality improvement. Health care administrators and managers and the members of their governing boards need performance data to support efforts directed at the redesign of care processes and the operation of systems to support care delivery. Health care providers need both performance data and evidence on those interventions provided by physicians, nurses, and other clinicians that are most likely to yield desired outcomes.
-
Population health—The health care delivery system is one of many factors that can influence the health of a population. A well-functioning performance measurement and reporting system should provide information to support the broad range of public policy decisions that influence population health and ultimately the need for health care services. The system should be designed to complement and support traditional public health reporting systems. It might include, for example, measures of access to health care services by various populations, including the uninsured and racial/ethnic minorities, the use of preventive services and health behaviors, and disease surveillance. Such a system would be an important asset in such areas as emergency preparedness, disease surveillance, and health protection.
Through its deliberations and its examination of existing measure sets (described more fully in Chapter 4), the committee formulated 10 design principles for a progressively improving national performance measurement and reporting system. Table 2-2 summarizes these design principles (see Appendix D for a complete description). These same principles can guide the future development of measures, as discussed in subsequent chapters.
NEXT STEPS
This committee recognizes that it will take a number of years to fully implement a national system for performanace measurement and reporting. There is a great variation in the degree of knowledge and experience pertaining to the various components of the system. As discussed above, there has been nearly two decades of experience with standardized measurement, but much less experience with public reporting. While data repositories for some measures already exist at the state or national level, no clear consensus has emerged on the proper structure of such registries, and many issues of data ownership and privacy protection must be resolved. It is clear, therefore, that some components of the system can be established immediately; for others, additional work will be needed to identify the best approach. The next chapter analyzes alternatives for achieving a national system that embodies the design principles described in Table 2-2 and presents the committee’s recommended strategy.
TABLE 2-2 Design Principles for a National System for Peformance Measurement and Reporting
|
Principle |
Description |
|
Principle 1: Comprehensive Measurement |
A performance measurement system should advance the core purpose of the health care system and foster improvements in all six quality aims identified in the Quality Chasm report (IOM, 2001): safety, effectiveness, patient-centeredness, timeliness, efficiency, and equity. |
|
Principle 2: Evidence-Based Goals and Measures |
A performance measurement system should be guided by a comprehensive set of evidence-based goals for improvement. |
|
Principle 3: Longitudinal Measurement |
Standardized performance measures should characterize health and health care both within and across settings and over time. |
|
Principle 4: Supportive of Multiple Uses and Stakeholders |
A performance measurement system should provide information for multiple uses, including provider-led improvement efforts, public reporting, payment and benefit design, and population health initiatives. |
|
Principle 5: Measurement Intrinsic to Care |
Performance measurement should be intrinsic to the care process. |
|
Principle 6: A Central Role for the Patient’s Voice |
A performance measurement system should include direct reports and ratings from patients and family caregivers. |
|
Principle 7: Patient-Level, Population-Based, and Systems-Level Measurement |
Measurement and measures should assess the health and health care of both individuals and populations and the many systems within which care is provided. |
|
Principle 8: Shared Accountability |
Measurement should not be constrained by the absence of a current, identifiable, single responsible agent. |
|
Principle 9: A Learning System |
A performance measurement system should be a learning system, continually evaluating its own performance and advancing knowledge regarding performance measurement. |
|
Principle 10: Independent and Sustainable |
A performance measurement system should be continually enhanced and financed in a way that ensures its independence and sustainability. |
REFERENCES
ABIM (American Board of Internal Medicine). 2005. About Maintenance of Certification. [Online]. Available: http://www.abim.org/moc/index.shtm [accessed March 30, 2005].
ACP (American College of Physicians). 2005. ACP Online—The Revitalization of Internal Medicine Initiative. Ambulatory Care Quality Alliance Approves Uniform Starter Set of Performance Measures. [Online]. Available: http://www.acponline.org/revitalization/am_care.htm?hp [accessed May 3, 2005].
AHRQ (Agency for Healthcare Research and Quality). 1998. Consumer Assessment of Health Plans (CAHPS[R]): Overview. [Online]. Available: http://www.ahcpr.gov/qual/cahps/dept1.htm [accessed February 25, 2005].
AHRQ. 2002. AHRQ Report on Home Health Quality Measures for CMS Public Reporting: Results of Technical Expert Panel Meeting and AHRQ Recommendations. Rockville, MD: AHRQ.
AHRQ. 2003. National Healthcare Quality Report. [Online]. Available: http://www.qualitytools.ahrq.gov/qualityreport/archive/2003/browse/browse.aspx [accessed November 16, 2005].
AHRQ. 2004. Fact Sheet: Hospital CAHPS(R) (HCAHPS[R]). [Online]. Available: http://www.ahcpr.gov/qual/cahps/hcahpfact.htm [accessed February 25, 2005].
AMA (American Medical Association). 2002. Physician Consortium for Performance Improvement: Taking the Lead Together. Chicago, IL: AMA.
AMA. 2005. AMA (CQI) Measurement Sets: Clinical Performance Measurement Tools to Support Physicians in Their Efforts to Enhance the Quality of Patient Care. [Online]. Available: http://www.ama-assn.org/ama/pub/category/4837.html [accessed February 23, 2005].
AMA, JCAHO, NCQA (American Medical Association, Joint Commission on Accreditation of Healthcare Organizations, National Committee for Quality Assurance). 2001a. AMA, JCAHO and NCQA Release Common Measures for Diabetes Care. Press release. April 25, 2001 . Chicago, IL.
AMA, JCAHO, NCQA. 2001b. AMA, JCAHO and NCQA to Focus on Measuring Effectiveness of Appropriate Pain Management. Press Release. December 17, 2001. Chicago, IL.
American Pain Society. 2000. New JCAHO Standards for Pain Management. [Online]. Available: http://www.ampainsoc.org/pub/bulletin/jul00/pres1.htm [accessed March 30, 2005].
Australian Council for Quality and Safety in Healthcare. 2005. One Million Dollars to Improve Patient Safety. [Online]. Available: http://www.safetyandquality.org/index.cfm [accessed March 31, 2005].
Australian Council for Safety and Quality in Healthcare. 2004. Safety and Quality Council. [Online]. Available: http://www.safetyandquality.org/index.cfm [accessed March 31, 2005].
Australian Government. 2002. Triple Bottom Line Measurement and Reporting in Australia: Making it Tangible. [Online]. Available: http://www.deh.gov.au/industry/finance/publications/triple-bottom/executive-summary.html [accessed March 31, 2005].
CAHPS Survey Users Network. 2005. CAHPS Survey Products. [Online]. Available: http://www.cahps-sun.org/Products/ProductIntro.asp [accessed February 22, 2005].
CMS (Centers for Medicare and Medicaid Services). 2003. Nursing Home Compare. [Online]. Available: http://www.medicare.gov/NHCompare/Home.asp [accessed March 29, 2005].
CMS. 2004. Hospital Quality Alliance (HQA): Improving Care Through Information. [Online]. Available: http://www.cms.hhs.gov/quality/hospital/HQAFactSheet.pdf [accessed March 30, 2005].
CMS. 2005a. Centers for Medicare and Medicaid Services. [Online]. Available: http://www.cms.hhs.gov/ [accessed October 19, 2005].
CMS. 2005b. Hospital Quality Initiative. [Online]. Available: http://www.cms.hhs.gov/quality/hospital/ [accessed February 21, 2005].
CMS. 2005c. Medicare Compare for Medicare Advantage Plans, Hospitals, Home Health, Nursing Homes, and End-Stage Renal Dialysis Centers. [Online]. Available: http://www.Medicare.gov [accessed March 1, 2005].
CMS. 2005d. Medicare Personal Plan Finder. [Online]. Available: http://www.medicare.gov/default.asp [accessed March 30, 2005].
Delmarva Foundation. 2005. The State of the Art of Online Hospital Public Reporting: A Review of Forty-Seven Websites. [Online]. Available: http://www.delmarvafoundation.org/html/public_reporting_summit_052604/WebSummariesFinal9.2.04.pdf [accessed May 13, 2005].
Dudley RA. 2005. Pay-for-performance research: How to learn what clinicians and policy makers need to know. Journal of the American Medical Association 294(14):1821–1823.
HCFA (Health Care Financing Administration). 1987. Medicare Hospital Mortality Information, 1986. Washington, DC: U.S. Government Printing Office.
Hofer TP, Hayward RA, Greenfield S, Wagner EH, Kaplan SH, Manning WG. 1999. The unreliability of individual physician “report cards” for assessing the costs and quality of care of a chronic disease. Journal of the American Medical Association 281(22):2098–2105.
IOM (Institute of Medicine). 2001. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academy Press.
IOM. 2002. Leadership by Example: Coordinating Government Roles in Improving Health Care Quality . Corrigan JM, Eden J, Smith BM, eds. Washington, DC: The National Academies Press.
JCAHO (Joint Commission on Accreditation of Healthcare Organizations). 2004. Our Commitment to Patient Safety. [Online]. Available: http://www.jcaho.org/general+public/patient+safety/index.htm [accessed March 30, 2005].
JCAHO. 2005a. Core Measure Information, Specification Manual for National Hospital Quality Measures [Online]. Available: http://www.jcaho.org/pms/core+measures/aligned_manual.htm [accessed February 17, 2005].
JCAHO. 2005b. Performance Measurement: Future Goals and Objectives. [Online]. Available: http://www.jcaho.org/pms/reference+materials/future+goals+and+objectives.htm [accessed February 17, 2005].
JCAHO. 2005c. Performance Measurement in Health Care. [Online]. Available: http://www.jcaho.org/pms/index.htm [accessed February 17, 2005].
JCAHO. 2005d. Performance Measurement: Key Historical Milestones. [Online]. Available: http://www.jcaho.org/pms/reference+materials/key+historical+milestones.htm [accessed February 17, 2005].
Joint Commission Resources. 2005. Public Information Policy: The Quality Report. [Online]. Available: http://www.jcrinc.com/subscribers/perspectives.asp?durki=7712&site=10&return=6062 [accessed March 29, 2005].
Manard B. 2002. Nursing Home Quality Indicators: Their Uses and Limitations. Washington, DC: AARP Public Policy Group.
McClellan MB. 2005. Statement of Mark B. McClellan, M.D., Ph.D. Administrator, CMS on Ambulatory Care Quality Measures. [Online]. Available: http://www.cms.hhs.gov/media/press/release.asp?Counter=1443 [accessed May 12, 2005].
McCormick D, Himmelstein DU, Woolhandler S, Wolfe SM, Bor DH. 2002. Relationship between low quality-of-care scores and HMOs’ subsequent public disclosure of quality-of-care scores. Journal of the American Medical Association 288(12):1484–1490.
McGlynn EAP. 2003. Introduction and overview of the conceptual framework for a national quality measurement and reporting system. Medical Care 41(Suppl. 1):I-1–I-7.
NBCH (National Business Coalition on Health). 2004. Coalition Report Card Weblink Project. [Online]. Available: http://www.nbch.org/members/reportcards.cfm [accessed March 29, 2005].
NCQA (National Committee for Quality Assurance). 2000. NCQA to Define Accreditation Program to Focus Attention on Patient Safety. [Online]. Available: http://www.ncqa.org/communications/news/patsafrel.htm [accessed March 22, 2004].
NCQA. 2005a. NCQA, ABIM to Align Requirements, Share Data; Agreement Will Allow Joint Application for Maintaining Board Certification, Recognition. [Online]. Available: http://www.ncqa.org/Communications/News/ABIM2-2.htm [accessed February 23, 2005].
NCQA. 2005b. NCQA Timeline. [Online]. Available: http://www.ncqa.org/about/timeline.htm [accessed February 21, 2005].
NCQA. 2005c. Quality Compass 2005: The Most Comprehensive Database of Health Plan Performance Data Anywhere. [Online]. Available: http://www.ncqa.org/Info/QualityCompass/index.htm [accessed February 21, 2005].
NCQA. 2005d. Recognized Physician Directory. [Online]. Available: http://www.ncqa.org/PhysicianQualityReports.htm [accessed February 21, 2005].
New Statesman. 2000. Blair has Made a Historic Pledge: Prime Minister Tony Blair Plans to Increase Health Care Spending in the United Kingdom to the European Union Average by the Year 2006. [Online]. Available: http://www.findarticles.com/p/articles/mi_m0FQP/is_4470_129/ai_59810465 [accessed March 31, 2005].
New York State Department of Health. 2002. NYS Managed Care Plan Performance Report. [Online]. Available: http://www.health.state.ny.us/nysdoh/mancare/qarrfull/qarr01/qarintro1.htm [accessed March 30, 2005].
New York State Department of Health. 2004. Cardiovascular Disease in New York State. [Online]. Available: http://www.health.state.ny.us/nysdoh/heart/heart_disease.htm [accessed March 29, 2004].
NHS Modernisation Agency. 2003. Real Measurement for Real Improvement Using Statistical Process Control. [Online]. Available: http://www.modern.nhs.uk/search/ [accessed March 31, 2005].
NQF (National Quality Forum). 2002a. Improving Healthcare Quality for Minority Patients: Workshop Summary. Washington, DC: NQF.
NQF. 2002b. National Voluntary Consensus Standards for Adult Diabetes Care. Washington, DC: NQF.
NQF. 2003a. Information Technology and Healthcare: Proceedings of a Summit. Washington, DC: NQF.
NQF. 2003b. National Voluntary Consensus Standards for Hospital Care: An Initial Performance Measure Set. Washington, DC: NQF.
NQF. 2003c. Safe Practices for Better Healthcare. Washington, DC: NQF.
NQF. 2004a. National Voluntary Consensus Standards for Nursing-Sensitive Care: An Initial Performance Measure Set. Washington, DC: NQF.
NQF. 2004b. The National Quality Forum’s Consensus Development Process. Version 1.7. Washington, DC: NQF.
NQF. 2005a. NQF: Mission Statement. [Online]. Available: http://www.qualityforum.org/mission/home.htm [accessed February 25, 2005].
NQF. 2005b. NQF-Endorsed National Voluntary Consensus Standards for Ambulatory Care. [Online]. Available: http://www.qualityforum.org/docs/ambulatory_care/tbambphase2diabTABLE09-13-05hww.pdf [accessed October 17, 2005].
Physician Consortium for Performance Improvement. 2004. Clinical Performance Measurement Tools to Support Physicians in Their Efforts to Enhance the Quality of Patient Care: A Consensus Statement from The American Medical Association and The Joint Commission on Accreditation of Healthcare Organizations and The National Committee for Quality Assurance. [Online]. Available: http://www.ama-assn.org/ama1/pub/upload/mm/370/principlesperfmeas.pdf [accessed May 18, 2005].
President’s Advisory Commission on Consumer Protection and Quality in the Health Care Industry. 1998. Quality First: Better Health Care for All Americans—Final Report to the President of the United States. Washington, DC: U.S. Government Printing Office.
Roland M. 2004. Linking Physicians’ Pay to the Quality of Care: A Major Experiment in the United Kingdom. New England Journal of Medicine 351(14):1448–1454.
Rosenthal J, Booth M. 2004. State Patient Safety Centers: A New Approach to Promote Patient Safety. [Online]. Available: http://www.nashp.edu [accessed November 16, 2004].
Rosenthal MB, Fernandopulle R, Song HR, Landon B. 2004. Paying for quality: Providers’ incentives for quality improvement. Health Affairs 23(2):127–141.
Rosenthal MB, Frank RG, Li Z, Epstein AM. 2005. Early experience with pay-for-performance: From concept to practice. Journal of the American Medical Association 294(14):1788–1793.
Shaul JA, Eisen SV, Stringfellow VL, Clarridge BR, Hermann RC, Nelson D, Anderson E, Kubrin AI, Leff HS, Cleary PD. 2001. Use of consumer ratings for quality improvement in behavioral health insurance plans. Joint Commission Journal on Quality Improvement 27(4):216–229.
Smith PC, York N. 2004. Quality incentives: The case of U.K. general practitioners. Health Affairs 23(3):112–118.
Stevens S. 2004. Reform strategies for the English NHS. Health Affairs 23(3):37–44.
Texas Health and Human Services Commission. 2004. Behavioral Health Measures across Medicaid Managed Care Plans and Models. [Online]. Available: http://www.hhsc.state.tx.us/medicaid/reports/082004_BHDR.html [accessed March 30, 2005].
U.S. Congress. 2005a. Medicare Value Purchasing Act of 2005. S. 1356.
U.S. Congress. 2005b. Medicare Value-Based Purchasing for Physicians’ Services Act of 2005. H.R. 3617.
U.S. DHHS (U.S. Department of Health and Human Services). 2002. Physician Group Practice Demonstration. [Online]. Available: http://www.cms.hhs.gov/researchers/demos/PGP.asp [accessed March 1, 2005].
U.S. DHHS. 2004a. FY 2005 Budget in Brief. [Online]. Available: http://www.hhs.gov/budget/05budget/centersformed.html [accessed March 30, 2005].
U.S. DHHS. 2004b. Rewarding Superior Quality Care: The Premier Hospital Quality Incentive Demonstration Fact Sheet. [Online]. Available: http://www.cms.hhs.gov/quality/hospital/PremierFactSheet.pdf [accessed March 1, 2005].
Washington State Department of Health and Human Services. 2005. Washington Medicaid Program Compiles New HEDIS Performance Ratings. [Online]. Available: http://www1.dshs.wa.gov/mediareleases/2005/pr05021.shtml [accessed March 30, 2005].























