2
Plenary Session
INTRODUCTIONS TO THE SYMPOSIUM AND FOR REPRESENTATIVES OF THE AMERICAN SOCIETY OF CLINICAL ONCOLOGY AND THE INSTITUTE OF MEDICINE
Ellen Stovall, Vice Chair, Committee on Cancer Survivorship: Improving Care and Quality of Life; and President and CEO, National Coalition for Cancer Survivorship
Good morning. My name is Ellen Stovall, and I am a 34-year cancer survivor. I am president of the National Coalition for Cancer Survivorship (NCCS) and one of the editors of this wonderful report that we are here today to celebrate. I want to begin by thanking the American Society of Clinical Oncology (ASCO) for sponsoring this wonderful symposium today.1 We would not be here today without the efforts of many of the people here today. Looking at you all fills me with great joy and a sense of extraordinary accomplishment. So, thank you.
I want to introduce our first two speakers today, Dr. Sandra Horning and Dr. Fitzhugh Mullan. Both of them are cancer survivors. Dr. Sandra Horning is Professor of Medicine, Oncology and Blood and Marrow Transplantation, at Stanford University. She is also the president of the American Society of Clinical Oncology, and a great friend to all of us in the community. Dr. Fitzhugh Mullan is a dear friend, and the architect of our 20-year-
|
1 |
The symposium agenda can be found in Appendix A. |
old survivorship movement and the founder of the NCCS. He is the Murdock Head and Professor of Medicine and Health Policy and Professor of Pediatrics at George Washington University. I am delighted to introduce them both here to you today.
INTRODUCTORY REMARKS
Sandra Horning, President, American Society of Clinical Oncology
Thank you. It is a distinct pleasure for me to be here as ASCO president, and as a cancer survivor, to introduce today’s symposium. As you know, the purpose of the symposium is to convene the stakeholders, you, who are committed to the care and the quality of life of cancer survivors, so that we can discuss the findings of this report, present the challenges that are outlined, and develop action plans to realize the recommendations.
ASCO is clearly committed to cancer survivorship, and we have made a lot of progress in the last year.2 First of all, an expert panel was convened by my predecessor, David Johnson, also a cancer survivor. This ASCO Survivorship Task Force is co-chaired by Patricia Ganz and myself. Members of the task force participated in the planning of today’s symposium. Our charge was to fully integrate survivorship into the activities throughout ASCO and all of its committees. We are also currently discussing partnerships with primary care societies in joint educational activities.
Survivorship is one of three major themes for the 2005-2006 ASCO year. It is very prominent in our member communications and is displayed prominently in our logo. And there will be concentrated sessions on survivorship and visibility of these issues at the 2006 annual meeting.
Some of our accomplishments in the areas of education and science include providing a permanent home for survivorship in our patient and survivor care track. This means that we have, and will continue to recruit, individuals with an interest and expertise in survivorship to populate both of our committees.
Our educational sessions at the 2006 meeting will include among others, Dr. Ganz talking about the development of a survivorship care plan and Dr. Lois Travis (NCI) talking about assessment of the risks of secondary cancers. We feel that having this permanent home in our scientific programs will help us to attract and promote survivorship research on a permanent basis. We have also begun to integrate survivorship into the core curriculum for oncology fellows.
|
2 |
For more information on ASCO’s survivorship activities, see its November 7, 2005, press release in Appendix B. |
ASCO members are working as we speak on guidelines that relate to cancer survivorship. These include the areas of fertility preservation; hormone replacement therapy; bone health; cardiovascular late effects; neurocognitive and psychosocial issues; as well as second cancers.
In the area of communications ASCO sponsored a Meet the Expert media event in December of the past year, and held a press conference in May that was dedicated to cancer survivorship and the research presented at the 2005 annual meeting of the society. The coverage, both press and national broadcast media, on survivorship research presented at our last annual meeting was extensive.
And our award-winning peoplelivingwithcancer.org web site has featured survivorship stories. There will be ongoing chats with survivorship experts. And we have shared content with the Lance Armstrong Foundation.
Cancer survivors, as we all know, number 10 million and are growing strong. My professional interest in lymphoma and Hodgkin’s disease results in my seeing a lot of cancer survivors. My mother is a cancer survivor. I am a cancer survivor. I am clearly in great support of the work that all of you have done over these many years, culminating in this comprehensive report and call to action. Cancer survivors need to be found, and their needs must be met. I know you look forward, as I do, to a very productive day. Thank you for your attention.
INTRODUCTORY REMARKS
Fitzhugh Mullan, Member, Institute of Medicine
Thank you, Sandra, and thank you, Ellen. It is a pleasure to be here. Survivors say that at the opening of meetings with a particular verve. It is really good to be here. I am a 30-year survivor of a primary mediastinal seminoma. I am also an IOM member, and I would like to extend a welcome from the IOM. It is a wonderful place, both intellectually, institutionally, and architecturally. The IOM has served the nation fabulously well in its ability to take issues, mediate them, broker them, raise them to new levels of evidence-based visibility, and put them on the national stage. And that this is being done with survivorship by dint of this committee and this report I think is just fabulous.
My own reading of the report, which I was fortunate to have the opportunity to do before today, From Cancer Patient to Cancer Survivor, is that it is a monumental piece of work, both for the science and the public policy that it brings to the fore, and for the fact that it takes issues that many of us have been grappling with for many years in happily lessening obscurity, but obscurity to begin with, and puts them between two hard
covers and out into the public policy stream in a far more potent way than has ever happened before. So, it is terrific.
My story was that one day in 1975, I took my own chest x-ray, because I had been having some funny feelings, and put the x-ray up on the viewing screen, and I didn’t know what it was, but I knew what I saw didn’t belong there. It was big and it was ugly, and it led to a return to Washington, treatment at the National Naval Medical Center, radiation, chemotherapy, surgery, and a pretty hellacious course of events over the next couple of years.
I was fixated then on the question of would I live, as everyone is, and when would I know that I would live, when would I be cured? And it was that intellectual and spiritual struggle that sort of brought to my attention the fact that while I wasn’t dead, happily yet, I wasn’t alive in the way I had been before, at least not at that point, whether it was in the ICU tubed up, or back at home sort of struggling along 30 pounds down, with radiation burns and an uncertain future.
I was surviving, and although the survivorship concept was with us, it was used in the context of Holocaust survivors and airline crash survivors, but not to refer to this purgatory or this period of time following the diagnosis of cancer. The term “survivorship” was used, but not in the cancer lexicon.
As I cast about for help or guidance or counsel, there was little in that regard. I found many people who were struggling with this both personally as survivors, and professionally as oncologists, oncology nurses, physicians, social workers, and counselors. Although the idea began to percolate in my mind, and certainly others understood it, it was then a fairly amorphous phenomenon. And in the 1985 paper, “The Seasons of Survival,” I wrote about it (Mullan, 1985). I went back and re-read it just this week, and just to quote a couple of things: “Despite the success on the treatment front, we have done very little in a concerted and well-planned fashion to investigate and address the problems of survivors. It is as if we had invented sophisticated techniques to save people from drowning, but once they had been pulled from the water, we leave them on the dock to cough and splutter on their own in the belief that we have done all that we can.” And then later on, “Survivorship should be studied as a phenomenon in itself, rather than as a byproduct or afterthought of basic research on cancer treatment.” And I really am delighted that the work of this committee, and the work in this report, has raised those concerns to a new level and given them a new poignancy. And this isn’t to say that in between 1985 and 2005, there hasn’t been a great deal of accomplishment in this area, but today’s report is really a high-water mark for that.
Now, it is a victory, and it is terrific that it is here. You could argue it has been a long time coming. Certainly, the survivors in the world, or the
survivors in the room might say, yes, but couldn’t we have gotten here quicker? And one could sketch out a phenomenon or scenario where that might have happened.
I do think particularly speaking to the research community, but also to the clinical community, we tend to focus particularly as researchers or clinicians on victories. You want to win. You want cures. One wants cures, and certainly patients do, too. But the world view, the environment, intellectual, clinical view that is thereby created is one of victors. And we celebrate victors. Lance Armstrong has perhaps done a better job than anyone in doing that, and that is good. But there is the reality that many of the victories in cancer are encumbered by ongoing issues: uncertainty as to outcome; compromises as a result of therapies; psychosocial issues; et cetera, that we know well and are well documented in the report. Developing and supporting clinicians, research scientists, and support system personnel who really see as their mission in life a very rigorous set of activities, whether they are clinical or investigative with survivors, is really a change in the paradigm, or it is an addition to the paradigm, and happily that is coming. But I do think the natural proclivity to look for victory is both to be respected, and also to be looked askance at, or to be at least challenged. You’ve got to remember it isn’t just a question of pulling them out of the water. But you get them on the dock. Are they going to stay on the dock? And are they going to have a reasonably civil time on the dock, or is it going to be hellacious while everybody turns their back on them and goes back to pulling somebody else out of the water? Without pushing the metaphor too far, I think that this is really a mission.
I would like to credit the NCCS, and Ellen in particular, for keeping survivorship on the agenda. And if it has taken arguably 20 years from the birth of the NCCS to today’s report, which really puts this, as I say, in the national pantheon of topical issues, both medically and socially, it has been a hard forced march, and Ellen has been at the front of the column for most of that time, leading to this effort. So, I think it is a real salute to her and to all the organizations in cancer care, including ASCO, but the NCCS has been on message week in, week out over those two decades.
A couple of words about Lost in Transition, the report. I think that subtitle is great. I will remember it as Lost in Transition more easily than, From Cancer Patient to Cancer Survivor. Three recommendations I think stand out, and given a couple of moments at the podium, I just want to take the opportunity to hit those home.
The survivorship care plan concept, an individualized roadmap for each survivor, ought to be part of what we do clinically, and what people into survivorship encounter. It is terribly important. Just to pause for a moment, the late Peter Jennings, as we know, had a difficult and rapid downhill course with lung cancer. And you probably noted, that on the day
he announced his cancer, he said, “I am a survivor.” Actually, the quote in The Washington Post was, “I’m told I’m a survivor,” which meant he had to learn that this is a concept. But that that concept had gotten that far I think is a credit again to people in this room, both the clinical and the patient community that have pushed this idea, and gotten it to the newsmakers of America, even though they take a little instructing at that moment. And his survivorship was short, but the concept was there, and I think that is important. And while I don’t know the intimate details of it, I suspect it was useful to him. But the notion that Peter Jennings and every one of us ought to have a survivorship care plan I think is just a terrific idea.
Survivorship research is a “gimme” in IOM reports—they always say there should be more research, and once again, we have said that. I think that is true, underline, exclamation point. The issues of long-term outcomes, of secondary effects of second tumors, which Dr. Horning has been particularly involved in personally herself, really need to be high on the agenda of cancer research. And I say that as a customer of cancer research and cancer care. I have not recently examined the figures, although I did at one point, and the amount we spent on what would be characterized as survivorship research was a pittance compared to what we spent trying to move ahead on more cures and more heroic rescues. It is good work, but we also have to look at the survivorship side.
And finally, what is not a gimme in all reports, although the IOM happily has had a number concerning it, is the issue of universal health insurance coverage. I could not leave this podium without hitting that home. There was a figure in the report stating that 11 percent of adult cancer survivors under age 65 do not have insurance. Nationally, 15 percent of the population does not have health insurance. And if you exclude the Medicare-eligible population, who virtually all have insurance, it is almost 18 percent of the population under 65 that are uninsured. I do not understand why cancer patients have a higher rate of insurance. But whether it is 11 percent or 18 percent, it is a bunch of folks. If it is the 18 percent, it is almost 1 in 5, and this presents a problem beyond being diagnosed with cancer. Being diagnosed with cancer now in an environment rich in interventions, rich in therapies, and even rich in a word I do not always use, cures or at least extended survivorship, and yet lacking the ticket to get into that care, that is a huge problem.
I had the opportunity in one of my other lives as a journalist to interview Senator Connie Mack when he was still in the Senate. Senator Mack, as you perhaps know, is a survivor himself, and has multiple family members who had cancer, and was a real champion in the Senate for cancer funding, cancer research, cancer support. He also was a fairly outspoken opponent of healthcare reform, expanded coverage in various ways. And I put that question to him. I said, on the one hand you have been terribly
articulate and very effective in generating support for cancer therapies and for new treatments, and for getting people saved. And yet, we have this orifice, this huge, gaping hole in our national tapestry of care called the uninsured, which lots of cancer patients fall into. And yet, you are not seemingly exercised about that. As a survivor and the champion of survivorship, doesn’t that strike you as something that ought to be at the top of the agenda. And he answered in a fulsome way. He said, “Well, I hear what you are saying. But I am concerned that if we go to more governmental interventions in the field of healthcare coverage, it will discourage innovation. That if we get involved, it will mean more regulation, and the very productive research sector and the drug industry and so forth in America will be discouraged and will not continue to be as productive as they have been.” And essentially, you could boil that down to saying that a move towards equity will kill off enterprise. I think he would agree that is essentially his argument. And that is a holdable position. That is an arguable case. I happen to think it is wrong, and I also happen to think that it is a formula for continued unfairness, and continued suffering. And certainly, from the perspective of cancer patients, that is a real issue.
Cancer patients whatever their views are—right, left, or center; Democrat or Republican—when they get diagnosed and do not have health insurance coverage, have a huge problem. And we have a huge problem as spokespeople for them and for that area. So, universal coverage, and you can color it or brand it whichever way you like, has got to be front and center on the agenda of survivorship in cancer, and I am delighted that it is in the report; one more good point in a great report. Thank you.
A SHORT VIDEO PRODUCED TO ACCOMPANY THE IOM REPORT AND ILLUSTRATE ITS FINDINGS AND RECOMMENDATIONS WAS SHOWN (IOM, 2006a)
INTRODUCTION TO THE PLENARY SESSION SPEAKERS
Sheldon Greenfield, Director, Center for Health Policy Research, University of California, Irvine
I am Shelly Greenfield, co-chair with Ellen Stovall of the IOM committee that issued the survivorship report. I am a primary care internist. There were four of us with a primary care focus on the committee amongst the people with various backgrounds, a testimony to the wisdom of the IOM in the recognition that survivorship is a truly integrative process, for which coordination of the various aspects of care is important. Before introducing
the panel, I want to thank the members of this committee and its staff. I have had the privilege and honor of being associated with many IOM committees over the past 10 years, and I will say that I have been on no committee or participated in no committee in which the members have been as diligent and as emotionally engaged as this committee.
I am not going to introduce the speakers this morning. You know them. I might ask them to say for outsiders, a word or two about themselves. Ellen has already introduced herself. So, we will just ask them to come forward. We will ask each of them to try to confine their comments to 15 to 20 minutes. We will have a few questions afterwards, and hopefully there will be a little bit of time after everybody has spoken for more general questions.
MEETING THE NEEDS OF CANCER SURVIVORS—RECOMMENDATIONS FROM THE IOM
Ellen Stovall, President and CEO, National Coalition for Cancer Survivorship
Thank you, Shelly. I would like to begin with a brief history. Almost everyone in this room knows about some of the landmark events that informed this report. But to let you know how this all got started, it began with changing the language of the words “victim” and “patient” to the word “survivor” in 1985, when Fitzhugh Mullan wrote his landmark article in the New England Journal of Medicine (Mullan, 1985). The term “survivorship” existed nowhere in the medical literature in 1986 when the NCCS was founded. It was a term of art only. You couldn’t find any references to it in any journal articles. Today, thankfully, it is a term of science.
In 1989, Natalie Davis Spingarn, one of the early founders of the NCCS, crafted the Cancer Survivor Bill of Rights, which laid forth many of the principles that are embodied in this report, including the survivorship care plan. The NCCS’s Imperatives for Quality Care, published in 1995, we very proudly note led to the establishment of the Office of Cancer Survivorship at the NCI in 1996. We wanted a division, we got an office. And in 2003, the Centers for Disease Control and the Lance Armstrong Foundation brought many of us in the community together to create a national action plan on cancer survivorship, taking cancer survivorship into the public health arena (CDC and LAF, 2004). In 2003-2004, the President’s Cancer Panel did a series of reports on cancer survivorship that have continued to inform us (President’s Cancer Panel, 2004a; President’s Cancer Panel, 2004b).
The IOM’s survivorship report’s origin can be traced to 1999, when the National Cancer Policy Board at the Institute of Medicine issued its report,
Ensuring Quality Cancer Care (IOM, 1999). Among the report’s many findings was that “for many types of cancer, answers to basic questions are not yet available, for example, how frequently patients should be evaluated following their primary cancer therapy, what tests should be included in the follow-up regimen, and who should provide follow-up care.”
The 1999 quality report spawned several other reports: a 2003 report, Childhood Cancer Survivorship: Improving Care and Quality of Life (IOM, 2003), which my friend and colleague Susan Weiner and Maria Hewitt shepherded through the IOM; a 2004 workshop report, Meeting the Psychosocial Needs of Women with Breast Cancer (IOM, 2004), and the report that we are now seeing here today.
The IOM committee that Shelly referred to is an outstanding group of wonderful colleagues and now friends. I am going to ask them just to stand briefly and be acknowledged by all of you. Those that are here today, if you would just stand so people can see you.
The committee started out by identifying who we are calling cancer survivors; about 3 percent of the population in this country and 15 percent of those 65 and older are survivors. Our report concluded that they are often lost to follow-up by oncology and primary care physicians. They are lost to follow-up through our healthcare systems, and they are grossly understudied by the research community. Successes in treating cancer and the aging of the population will bring us more and more cancer survivors as the years go forward.
The charge to the committee was to raise awareness of the consequences of cancer, to define quality care and outline strategies to achieve it, and to recommend policies to improve care and quality of life. The 17-member committee was referred to earlier. It included oncology and primary care physicians, people in urban and rural practice in this country, and people devoted to clinical and health policy research. We met three times over the gestation period, as I call it, to birth this baby, and we heard from lots and lots of outside experts, as the IOM process is exquisitely formulated to do, bringing forth the best and the brightest people in any one specific area of science.
The committee at its outset decided to accept the NCCS and the NCI definitions of a cancer survivor. Accordingly, an individual diagnosed with cancer is a survivor from the moment of diagnosis and for the remainder of his or her life. For purposes of this report we chose to focus on those we felt were most neglected, who fall off the cliff, and who are lost to follow-up, and that is those who have completed their primary treatment and are not being treated for a recurrence of their cancer (or a relapse) and are not receiving end-of-life care.
In its findings, the committee concluded that the negative consequences of cancer and its treatment are substantial and underappreciated. And al-
though the population is heterogeneous with some experiencing few late effects of their cancer, many, many more suffer permanent and disabling symptoms that impair their normal functioning even when their initial primary cancer treatment has been excellent.
Psychological distress, sexual dysfunction, infertility, impaired organ function, cosmetic changes, and limitation in mobility, communication, and cognition are among the many problems faced by cancer survivors. And the survivors’ health, as we all know, is forever altered. And the good news out of this report is there is an awful lot that we can do to ameliorate these conditions.
We also found that survivors may be very unaware of their risk. The public lacks an awareness of cancer’s effects and assumes that survivors have a plan for their follow-up. Shelly was telling us the other night that when he discusses the report’s findings with people, they just can not believe that survivors would not be told what to expect or what to do following their diagnosis, but it is, in fact, the case. And so, opportunities to intervene when these consequences occur may often be missed. We have not tested models of survivorship care that are out there. And we know that the whole system of cancer care, not just this phase, suffers from an absence of coordination.
The committee made ten recommendations. Simply and most importantly, we recommended that awareness of the needs of cancer survivors be raised; that cancer survivorship be established as a distinct phase of cancer care; and that responsible parties act to ensure the delivery of appropriate survivorship care. Awareness needs to be raised for both healthcare providers and for the general public. It is common now for cancer patients to finish their treatment unaware of their risks. They are therefore, ill prepared to manage their future health needs. Oncologists exhibit wide variation in their follow-up practices, and primary care providers often lack up-to-date knowledge on survivorship.
To overcome the problem, the committee recommended that all patients completing primary treatment be provided with a survivorship care plan, and Patti Ganz is going to go into much more detail in the next presentation, so I will not elaborate on that. Survivorship care planning is not a new recommendation. It has been called for by the President’s Cancer Panel (PCP, 2004b), the Centers for Disease Control and Prevention, the Lance Armstrong Foundation’s Action Plan on Survivorship (CDC and LAF, 2004), the NCCS’s Imperatives for Quality Cancer Care (NCCS, 1996), and many, many other groups.
The committee’s third recommendation calls for the development and use of clinical practice guidelines. Some guidelines are available for certain aspects of survivorship care, but most are incomplete and not based on solid evidence. Cancer survivors represent a very large at-risk population, and without evidence-based clinical practice guidelines and quality-of-care
indicators healthcare providers will continue to vary widely in their practices. More than 60 percent of cancer survivors are aged 65 and older, so the Centers for Medicare & Medicaid Services, the administrators of the Medicare Program, have a stake in the development of clinical practice guidelines and quality-of-care measures. Because cancer is a complex disease and its management involves the expertise of many specialists often practicing in different settings, cancer illustrates well the quality chasm that exists within the U.S. healthcare system overall, and the need for health insurance reforms and innovations in healthcare delivery.
Several models that are promising for delivering survivorship care are emerging, including collaborative shared care models that formally link oncology specialists with primary care providers, nurse-led models, and specialized survivorship clinics. Our fifth recommendation calls for demonstration programs to test these potential models for survivorship care.
The report’s sixth recommendation calls for congressional support for the Centers for Disease Control and Prevention and states to develop, implement, and evaluate comprehensive cancer control plans that include consideration of survivorship care.
Recommendation number seven calls for the NCI, professional associations, and voluntary organizations to expand and coordinate their efforts to provide educational opportunities to healthcare providers to equip them to address the health and quality-of-life issues facing cancer survivors. Few oncology and primary care professionals have formal education and training regarding cancer survivorship. With the growing ranks of cancer survivors at 10 million strong today, it is likely that additional health personnel will be needed, particularly nurses with advanced oncology training. To insure access to psychosocial services, continuing education opportunities are needed for social workers and other mental health providers. In addition, efforts are need to maintain social services in cancer programs.
Most cancer patients who worked before their diagnosis continue to work, but they often require some kind of accommodation. As many as 1 in 5 of us who worked at the time of diagnosis have cancer-related limitations in ability to work one to five years later. Half of those with limitations are unable to work at all. All survivors are at risk of experiencing subtle, although not necessarily blatant, employment discrimination. Federal laws enacted in the 1990s have offered cancer survivors some protections from discrimination such as firing or denial of benefits because of cancer. Our eighth recommendation calls for employers, legal advocates, healthcare providers, and others to act to minimize adverse effects of cancer on employment while supporting cancer survivors with short-term and long-term limitations in their ability to work.
Recommendation nine calls on federal and state policymakers to act to ensure that all cancer survivors have access to adequate and affordable
health insurance. Furthermore, insurers and payers of health care should recognize survivorship care as a distinct part of cancer care, and design benefits, payment policies, and reimbursement mechanisms to facilitate coverage for evidence-based aspects of care. The health insurance issues facing cancer survivors today bring into sharp focus the gaps and limitations of health insurance throughout our country. All Americans are at risk of becoming a cancer survivor and finding themselves without access to adequate and affordable health insurance. Cancer survivors, like other Americans with serious chronic health conditions, face significant barriers to coverage because of their health status. In particular, access to individual health insurance may be denied to residents in many states. Cancer survivors may also face surcharge premiums for coverage, because of their cancer history. The improvements in the care of cancer survivors envisioned by the committee cannot be achieved without health insurance that is accessible, adequate, and affordable.
Our last recommendation concludes that a greater investment in research is needed to learn more about cancer’s late effects and their management. Cancer treatments are constantly evolving and, consequently, what is known about today’s cancer survivors may not be relevant to future patients.
I want to conclude by quoting from an article that was in the Annals of Internal Medicine four years ago (McKinley, 2000):
After my last radiation treatment for cancer, I lay on a cold, steel table, hairless, half-dressed, and astonished by the tears streaming down my face. I thought I would feel happy about finally reaching the end of treatment, but instead I was sobbing. At the time I wasn’t sure what emotions I was feeling. Looking back, I think I cried, because this body had so bravely made it through 18 months of surgery, chemotherapy, and radiation. Ironically, I also cried, because I would not be coming back to that familiar table where I had been comforted and encouraged. Instead of joyous, I felt lonely, abandoned, and terrified. This was the rocky beginning of cancer survivorship for me. I’m done according to the medical profession, but I don’t feel done. I think we survivors are never truly done. We just move from the quantifiable, treatable disease to the immeasurable uncertainty of survivorship. Being in the midst of active treatment means being seen regularly by a nurse or a doctor, being truly cared for. As I got up off that radiation table for the last time and walked away, I found myself alone with a cancer ghost who would not let me forget where I had been, or allow me to freely choose where I might be going. We cancer survivors are a million strong, and our ranks will grow as improved treatments extend our lives, but because the struggle with uncertainty after treatment is completed is usually a silent battle waged outside of the doctor’s office, most physicians don’t think or talk about it. In my life as a primary care doctor before cancer, I certainly did not. Now I believe that we physicians need to talk with our cancer survivors about
the unique struggles of survivorship. Oncologists need to focus on preparing us cancer patients for survivorship. That is, they must address the loss experienced by survivors when active treatment is over, and they are sent away from a very intense environment. They must help survivors understand the impact of fear and uncertainty on their lives, and what might help us to reduce those stresses.”
Dr. Greenfield: Are there questions that we might entertain at this time?
Bob Weiss: I am representing the National Lymphedema Network. In the definition of cancer survivor, do you include the patients who have been diagnosed and treated for ductal carcinoma in situ (DCIS) and lobular carcinoma in situ (LCIS). I know that they are not included in the cancer statistics of cancer diagnoses.
Dr. Ganz: DCIS and LCIS are included in cancer registries. DCIS is stage 0 breast cancer. Women who are treated for DCIS may experience late effects and would be considered a survivor of early stage breast cancer.
IMPLEMENTING THE CANCER SURVIVORSHIP CARE PLAN AND COORDINATING CARE
Patricia Ganz, Director, UCLA Division of Cancer Control, Jonsson Comprehensive Cancer Center
My name is Patti Ganz. I am a medical oncologist. Actually, I am very pleased to be here as well, because I was one of the founding members of the National Coalition for Cancer Survivorship. When Fitz Mullan invited me to go to that small meeting in Albuquerque, I did not know it would lead to this. So, it is really exciting to be here today.
I am going to be talking about the cancer survivorship plan. First, I am going to give you my perspective as an oncologist, reflecting on how things have changed, and why it is important, and why we are where we are now; and some of the complexities and challenges of treatment. I am also going to discuss some of the strategies that we can use, and then specifically how the survivorship care plan can serve as a model of coordinated patient-centered quality of care. Finally, I will review recommendations for implementation. I will be highlighting my experience with breast cancer in my remarks, but most of the themes that emerge are applicable to other cancers.
So, first of all, I am going to talk about breast cancer treatment from a historical perspective. In 1971, I was doing my surgical rotation in medical school and, incredible as it may seem, a woman with a lump in her breast was anesthetized, and had to sign a consent to either a mastectomy or a
biopsy, and would awake with bandages, not knowing whether she had her breast or not. And indeed, she was actually in the setting where I was trained, consenting for the randomized trial, the National Surgical Adjuvant Breast and Bowel Project (NSABP) B-4 trial, so she didn’t even know if she was going to have a modified radical mastectomy or a Halsted radical mastectomy. Again, it is really shocking to think that this is the way we managed breast cancer at that point in time.
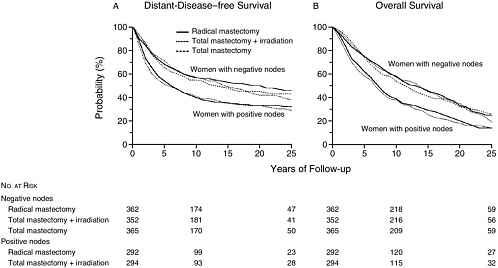
The NSABP B-4 trial was a randomized trial that compared the Halsted radical mastectomy to the less invasive modified radical mastectomy. The Halstead procedure involved removal of all of the pectoral muscles, an axillary dissection that often included the excision of as many as 30 lymph nodes, and left women with substantial morbidity in terms of arm function and edema. The modified radical mastectomy does not remove the pectoral muscles and fewer lymph nodes are excised. Figure 2-1 shows disease-free survival and overall survival rates through 25 years of follow-up from the NSABP B-4 trial for women with node-negative and node-positive disease. For women with breast cancer, the Halsted radical mastectomy proved to be no better than the modified radical mastectomy.
In the 1970s then, there was a growing recognition that breast cancer was a systemic disease, and we recognized then that local treatment of the breast really did not affect mortality, but rather women died because there was distant disease that had escaped before, in fact, the cancer was found. And this was especially critical for women if they had tumor in the lymph nodes. During this period, early trials of adjuvant chemotherapy, which at that time was being given for as long as two years after primary treatment, were initiated, particularly in women with node-positive disease to see if we could do anything to improve the recurrence rate and survival.
In the 1980s there was increasing consumer involvement as in all health care, but particularly in breast cancer. There happily was elimination of the one-step procedure and adoption of a two-step procedure, so that if a woman presented with a lump in her breast, she would first have a biopsy done as an outpatient, and then could go ahead and prepare herself for the fact that she had cancer and needed to have a mastectomy. There was mounting clinical evidence by two large trials, one done in Europe and one done in the United States, that breast-conserving surgery (lumpectomy and radiation therapy) was equivalent to mastectomy, and lo and behold, there began a revolution in the primary treatment of breast cancer. And with this, there was increasing patient involvement in surgical decision-making. That is, if these two treatments are equivalent, would you rather spare your breast, or would you rather have a mastectomy? This was perhaps not a great choice, but clearly one women could opt for. Fortunately, today we don’t present women with that difficult choice. We just tell them they are candidates for breast-conserving surgery.
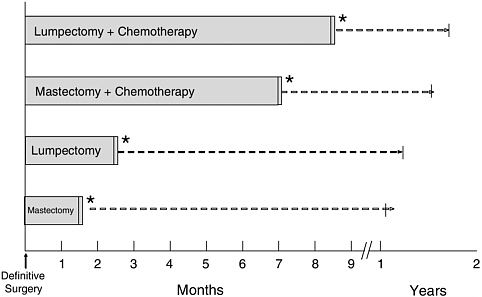
FIGURE 2-2 Current breast cancer primary treatment patterns. Adapted from Ganz et al., 2004, with permission, Oxford University Press.
Three important National Institutes of Health (NIH) consensus conferences have focused on breast cancer. In 1985, there was a consensus conference that concluded that adjuvant therapy with chemotherapy should be given to all pre-menopausal women with node-positive disease. In 1990, a consensus conference focused on the primary treatment of breast cancer, that is, the issue of mastectomy versus breast-conserving surgery. This conference recommended that all women be offered breast-conserving treatment if possible, and that the option of adjuvant therapy be discussed. In 2000, a consensus conference focused on adjuvant chemotherapy and recommended that all women with tumors that were greater than a centimeter in size should receive chemotherapy, and if the tumor contained hormone receptors, women should receive endocrine therapy. This focus on small tumors is notable. The tumors that I first saw when I was a medical student were usually 3, 4, and 5 centimeters in size. Now, with mammographically detected cancers they are often less than a centimeter in size.
Figure 2-2 comes from a study that we recently completed and illustrates how extensive the treatment for breast cancer is. If a woman just has a mastectomy, she may complete her primary treatment in about a month or so in terms of recovering. If she has a lumpectomy with radiation and no chemotherapy, she might be finished with her primary treatment at about
TABLE 2-1 Five-Year Relative Survival (Percent) during Three Time Periods, by Cancer Site
|
Site |
Relative Survival* (%) during Three Time Periods by Cancer Site |
||
|
1974-1976 |
1983-1985 |
1992-1999 |
|
|
All sites |
50 |
52 |
63 |
|
Breast (female) |
75 |
78 |
87 |
|
Colon and rectum |
50 |
57 |
62 |
|
Leukemia |
34 |
41 |
46 |
|
Lung & bronchus |
12 |
14 |
15 |
|
Melanoma |
80 |
85 |
90 |
|
Non-Hodgkin’s lymphoma |
47 |
54 |
56 |
|
Ovary |
37 |
41 |
53 |
|
Pancreas |
3 |
3 |
4 |
|
Prostate |
67 |
75 |
98 |
|
Urinary bladder |
73 |
78 |
82 |
|
*Five-year relative survival rates based on follow-up of patients through 2000. SOURCE: Surveillance, Epidemiology, and End Results Program, 1975-2000, Division of Cancer Control and Population Sciences, National Cancer Institute, 2003. |
|||
three months. With mastectomy and chemotherapy it can go out to eight months. And with lumpectomy and chemotherapy, treatment may extend way beyond nine months because radiation therapy is delayed until after chemotherapy is completed. So, again, this is a very long and complex road that a woman with breast cancer, who has an excellent survival, has to face in terms of the primary treatment of her disease.
Table 2-1 shows statistics that document improvement in survival from the 1970s to the 1990s. Five-year relative survival for all cancer sites has improved from 50 percent when I was doing my training as a medical student and early oncologist to 63 percent by the 1990s. But look at breast cancer, 5-year relative survival has increased from 75 to 87 percent over this period. Improvements have also been made for other cancers including melanoma, prostate cancer, and bladder cancer. These are phenomenal data in terms of survivorship.
Figure 2-3 shows trends in use of screening mammography and adjuvant therapy published in a recent article from the New England Journal of Medicine, again just to show you how things have changed. In 1985, very few women were getting their mammograms, and now we have women getting mammograms regularly which contributes to improvements observed in breast cancer survival rates. Figure 2-3 also shows data on the use
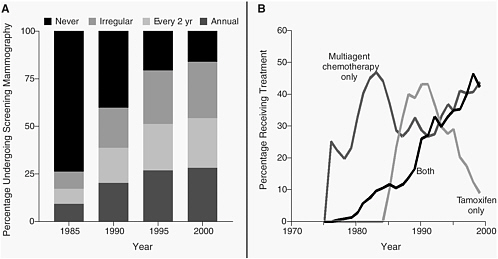
FIGURE 2-3 Changes in the pattern of use of screening mammography among women 40 to 79 years of age (Panel A) and in the use of adjuvant therapy among women 50 to 69 years of age with node-positive stage II or IIIA breast cancer (Panel B).
SOURCE: Berry et al., 2005. Copyright © 2005 Massachusetts Medical Society. All rights reserved.
of adjuvant chemotherapy, and endocrine therapy, indicating the dissemination of both of these modalities, again leading to vast improvements in survival, but adding complexity.
Now, what is happening in the 21st century? After the 2000 NIH consensus conference, there was a very short period of time where we agreed on what to do. But here we are, and now women are getting endocrine therapy for at least 10 years and maybe more. There will be clinical trials testing this. Adjuvant trastuzumab (Herceptin®) was recently shown to have a phenomenal benefit in terms of the adjuvant therapy for women whose tumors over-express human epidermal growth factor receptor 2 (HER2), and treatment with this particular agent is intravenously given for a year, and there are some studies looking at two years of therapy. Again, I want to tell you that the story of breast cancer and the success in terms of survivorship is really replicated for many other cancers. This is just one tumor history and story.
So, what are the challenges that this particular anecdote brings to mind? Well, cancer treatment is, if nothing else, very complex. It is multi-modal. There are many individuals involved in the care, and it is usually a surgeon, a radiotherapist, and a medical oncologist. There may be multiple consultations prior to going on to an experimental protocol. It is very, very complicated. It is toxic, and there is no doubt about that. That is why we have to look at the safety, as well as the benefit issues in terms of our treatment. And it is very expensive. And this is again, high out on the radar screen for the Centers for Medicare & Medicaid Services (CMS) and other funders of insurance. And finally, it is often poorly coordinated. Even though I have shown you that there have been tremendous advances in dissemination of what we know, often individuals are even lost during this primary treatment; it is not just lost in transition.
Cancer treatment usually occurs in isolation from primary healthcare delivery. If you can imagine yourself as a patient going through one of these scenarios in terms of treatment, it is pretty hard to get up the energy to go visit your primary care doctor to have a chat. And unless you have a lot of other co-morbid conditions that have to be managed simultaneously along with your cancer, you are probably not going to check in with your primary doctor, who may have diagnosed your cancer, until many months or even a year or more later. So, there is a natural isolation, because of the complexity of treatment.
There are other challenges in survivorship care. There has been limited systematic study of the late effects of cancer therapy, and this is documented very well in our report. Follow-up care plans have been ad hoc, with a limited focus on surveillance for recurrence. And that is really what the oncologist’s primary interest is. “Now that I have gotten you through this treatment, I want to make sure that you do not have a recurrence,” and
that is again all of what we learn in our training in terms of how we follow patients on clinical trials, the emphasis being on detecting a recurrence. There is little emphasis placed on health promotion and disease prevention. And again, this is really the issue. When can we make that transition? When is the person considered out of the woods in terms of recovering from the toxicity of therapy, so that we can say, “Well, you need to lose weight and you need to go out and exercise” and put this high on the radar screen? Another important survivorship issue with quality-of-life implications is infertility. Women have commonly been told, “Dear, you should just be happy to be alive.” I don’t think that is acceptable today. If we expect somebody to live a normal life span after their primary treatment, we need to address the issue of infertility, and this goes for both men and women.
So, why does cancer care present such a challenge? And again, just to summarize, an average of three specialists are involved per patient. Consequently, if you want to do chart reviews, you have to get all these charts to thoroughly evaluate quality. Treatments may occur across time and space and not be confined to the same institution. In a place like Los Angeles, where I work, very few patients get radiotherapy at my facility. They go to a place closer to their home. There is limited communication among the treating physicians, and there are multiple medical records.
Proposed strategies to address these challenges, even in the primary treatment of cancer, include an integrated electronic medical record. People are using patient navigators. Many savvy cancer centers have facilitators for the patients to help them get through this maze. And people like Laura Esserman have looked at a consultation planning session. Shelly Greenfield and his wife Sherry Kaplan did this a long time ago, where they prompted patients about what to do in terms of going into their visits with their doctors. But none of these strategies is actually widely available, even for patients receiving active treatment. And so, it is not surprising that they fall through the cracks when treatment ends.
So, why do we need this survivorship care plan now? I think it is critical that we summarize and communicate what transpired during the cancer experience. Certainly, the patient who may be stressed by that process and going through it may understand in the beginning about what they are going to be getting, but they have no idea often what exact drugs they got, what their side effects are, what the doses were, and so forth. We need to somehow summarize this information for them, and for the physicians who are going to be caring for them in the future, and for the medical record, so that there is one place in the record we can find it. The survivorship care plan is also needed to describe any known and potential late effects of cancer treatments, with the expected time course. There is a paucity of information on some late effects, but we do have information on some, and what we do know needs to be adequately communicated. We also need to
|
BOX 2-1
SOURCE: (IOM, 2001). |
communicate to the survivor and other healthcare providers what has been done, and again importantly, what needs to be done in the future, again, to the best of our abilities at that point in time. The survivorship care plan is also needed to promote a healthy lifestyle to prevent recurrence and reduce the risk of other co-morbid conditions. Wendy Demark-Wahnefried, Julia Rowland, and others just wrote a wonderful article in the Journal of Clinical Oncology talking about the missed opportunities for prevention and healthy lifestyle promotion in survivors (Demark-Wahnefried et al., 2005). Cancer survivors are at risk not only because of their exposures, but because they get other co-morbid conditions due to aging. There is never a time to miss the opportunity to provide consultation.
The optimal delivery of survivorship care, as Ellen has already alluded to, flows from recommendations from other IOM reports focused on quality of care, in particular, Crossing the Quality Chasm (IOM, 2001). The attributes of a system delivering quality care are listed in Box 2-1. I think the issues of shared knowledge and free flow of information, the need for transparency, and the anticipation of needs are really important. Vital also is cooperation among clinicians, again, because of the fragmentation of our system.
Committee member Rodger Winn eloquently pointed out in our discussions that most oncologists do not realize that there is a distinct group of people within the cancer care trajectory that are in need of survivorship care. This survivorship care phase of the cancer care trajectory is repre-
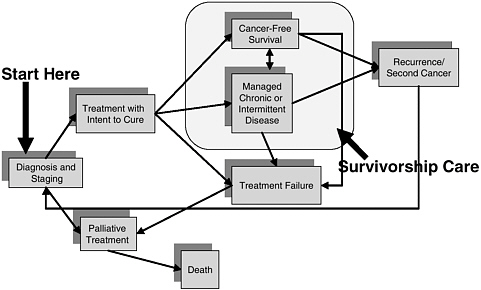
FIGURE 2-4 Survivorship care as a part of the cancer care trajectory.
SOURCE: IOM, 2006b.
sented in Figure 2-4 as the large shaded box. In the figure, everybody comes into the treatment system upon diagnosis. Some patients may be candidates only for palliative treatment at the beginning, but the majority of patients we see are treated, often with an attempt to cure. And the very large number of individuals wind up in this shaded space where, again, we have little information about how care should be managed, and no communication about the transition into this phase. So, this is what we are acknowledging in this report, this phase of the cancer care trajectory, which patients may, in fact, inhabit for a very long time, completely disease-free, or go back and forth, or be maintained very well with long-term therapy.
The other point that I would like to make is that the survivorship care plan is really a place to start in ensuring quality cancer care. We have paid a lot of lip service to this, and again, if we want to start somewhere, it may be somewhat simpler to address the quality of survivorship care than to address the quality of primary treatment for each of the different cancers. We can focus on quality during this transitional phase by establishing a care plan and it will be applicable for the vast majority of individuals treated for cancer.
The key elements of the survivorship care plan are outlined in Box 2-2. The care plan should communicate to the patient clearly: their diagnosis; the stage of the disease; the initial treatment plan; whether they actually got what had been planned for them, or whether excessive toxicity limited the
|
BOX 2-2
SOURCE: (IOM, 2006b). |
ability to deliver what was planned; and toxicities experienced during treatment. Patients, for example, sometimes receive blood transfusions during treatment which can pose risks for hepatitis and other infections that can have long-term health consequences. Other key elements of the survivorship care plan include the expected short- and long-term toxicities or late effects expected from the treatments and the kind of surveillance and monitoring needed both for these late effects, as well as for recurrence or second cancers.
Critical to this plan is designating who will take responsibility for what aspects of follow-up care. In sitting down with the patient and presenting the plan, the oncologist can say, “Well, I’ll take care of your follow-up mammograms, but your primary care doctor needs to take care of your hypertension, your diabetes, checking your cholesterol, and making sure that you get your bone density studies done. And we’ll talk frequently about the results and how they may be related to the treatment that you received.” Also important is attending to psychosocial and vocational needs, as highlighted in our video. Interventions are also needed to prevent additional sequela that may occur, and the common problems that people have in our society because of obesity and lifestyle risk factors.
So, how should we use this in practice? I am thinking about this written care plan as a document that would facilitate communication at the end of treatment visits. It would enable me to sit down with the patient and go over the key elements in a systematic way, very much the way I do initially with patients when I have their initial pathology report, and I discuss the randomized trials that are available to discern what type of treatment is
best for them. It is kind of a bookend to that initial consultation. The survivorship care plan is a formalized way to coordinate follow-up care, and to really define who will take charge, and what follow-up care is needed. Critically, it is a form of communication for all involved with the patient’s care, those who have been involved in the past, and those who need to be involved in the future. The care plan also tells a story about what went on. And again, as I have told you by my anecdote about breast cancer, it is pretty complicated. Often the primary care physician is not along for the ride, and has to pick up the pieces afterwards.
What do we need to do to implement this survivorship care plan? First, I think we need to have widespread acceptance of cancer as a chronic disease. And unlike other chronic diseases, which may actually accelerate and get worse over time, we have this up-front intensive therapy and then diminished treatment activity. So, again, cancer care doesn’t strictly follow the usual chronic model, say of a disease like diabetes or asthma. Secondly, we need to provide adequate reimbursement for this evaluation and management time that will be required both to prepare the plan for that consultation, and to effectively communicate it to patients and those providers who are involved in their care. Thirdly, we need to expand the evidence base of knowledge regarding late effects. And of course this needs to be through systematic research. And more importantly, we need to find the health professionals out there who are willing to focus on this topic. Lastly, we need to train physicians starting at the medical school level, but going through post-graduate education and also for practitioners in practice about how they can in fact work together to ensure high-quality care for cancer survivors.
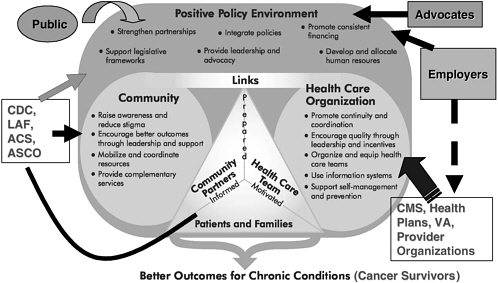
Figure 2-5 illustrates where a cancer survivorship care plan might fit in a chronic care model, where we have a proactive, prepared practice team, and we have an informed, activated patient. And again, I can think of nothing better than the survivorship care plan to be interdigitated in this interaction. We have the rest of the healthcare system in the external part, but we are talking about patient-centered care, survivorship-centered care, and again, this type of document can greatly facilitate this activity.
Some of the facts you have already heard. Importantly, there are now more than 10 million cancer survivors, representing about 3.5 percent of the U.S. population. That is really what the imperative is for us. Who are the stakeholders? And how can they be influenced to promote the survivorship care plan? Figure 2-6 is a busy diagram, and I hope I haven’t missed identifying stakeholders. To ensure better outcomes for chronic conditions including cancer, we have to influence the policy environment through the public, advocates, and employers, and through important community links through organizations such as the Centers for Disease Control and Prevention (CDC), the Lance Armstrong Foundation (LAF), the American Cancer
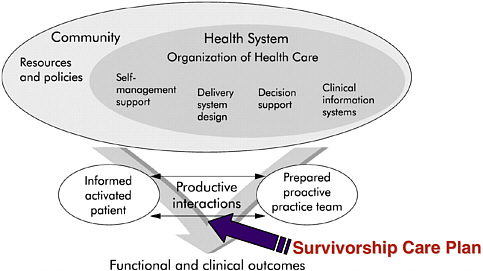
FIGURE 2-5 Where does the survivorship care plan fit into the chronic care model?
SOURCE: Adapted from Epping-Jordan et al., 2004.
Society (ACS), ASCO, and associations representing primary care providers. Coordinated efforts are needed to raise community awareness, encourage better outcomes, and mobilize and integrate resources. In terms of healthcare organizations, we have the employers playing a big role as a major source of health insurance. But clearly CMS, the Department of Veterans Affairs (VA), even the provider organizations that deliver the care need to encourage and provide the environment in which the chronic care management for cancer survivors can become a reality.
So, some final thoughts. I think we are really at a critical juncture in time here. Again, many of us bemoan the fact that we have a huge federal deficit, that there are very few resources now for research in the way we have had them over the past decade. But sometimes we can work more creatively and efficiently under these kinds of constraints. There may be opportunities for us to find and save money, decrease waste, and increase coordination of care by doing something as simple as implementing the cancer survivorship plan. Cancer care is high on the agenda because it is a major component of the healthcare budget and our drugs are very beneficial, but it is also very expensive. The majority of cancer patients are Medicare beneficiaries, and with rapid expansion of this group over the next several decades because of the aging of the baby boom population, cancer survivorship should become a high priority on the policy agenda for
CMS. I believe it is time to use cancer survivorship as a model for quality chronic disease management, and the survivorship care plan is a place to start.
Dr. Greenfield: Are there any questions?
Susan Leigh: I am one of the very proud founding members of NCCS. Patti, thank you so much for your overview of the survivorship care plan. I would like to add that there is one area that we really need to start focusing on, and that is how we prepare people for the potential risks and for the different decisions that have to be made once something happens. In following up on your example for breast cancer, I am a long-term Hodgkin’s survivor who then developed breast cancer. My decision-making was very, very different from someone who was initially diagnosed with breast cancer. I know that you want to start taking a look at that particular population, because we are all having to make very different decisions, because we have got different kinds of cancers, and we have different histories with the therapies that we had in the past.
Dr. Ganz: Thank you.
Dr. Greenfield: I am sure to most people in this room, this is like water flows down hill. I don’t want to blindside you, but could you give your sense of the resistance against this notion of a survivorship care plan?
Dr. Ganz: I am a sensitive, caring, cancer survivorship doctor. Do I use a survivorship care plan? No. Why? Because nobody has told me that I should do it. I do sit down with patients at the end of treatment, and I do have a systematic discussion about how often I am going to see them, and what kind of problems to expect. I am certainly attending to their menopausal symptoms that they have gotten as a result of my treatments, and I am doing all of those things verbally in my consultations. I am going to follow those patients, and I am not going to abandon them. And I usually have pretty good relationships with the physicians whose patients I see. But I do not send a consult note to their primary care physician at the end of treatment, which is what I do at the beginning. I do not have a structured, written set of materials, which I do when I see a new patient with breast cancer. I have kind of an education sheet that I actually go through. So, while I hate to say we need regulation and external reasons to do this, I think things that would facilitate survivorship care planning include the development of templates, a call to action that this is the expectation, and training medical oncology fellows, surgeons, and others who take care of cancer patients to consider this as an aspect of quality care. So, we have to
start at all these levels. I think it can become a reality, but right now it is just not a routinized part of practice.
DEVELOPING GUIDELINES, INSTITUTING QUALITY IMPROVEMENT, AND STRENGTHENING PROFESSIONAL EDUCATION PROGRAMS
Rodger Winn, Clinical Consultant, National Quality Forum
Good morning. I am a medical oncologist who has worked in both private practice and academic settings and have been an observer of the healthcare system in cancer. I have been involved with the development of clinical practice guidelines and quality measures, so I bring that sort of expertise to this symposium. I am going to address the issues of education, guidelines, and quality measures as we discuss moving ahead and implementing the IOM’s recommendations. As Patti Ganz has already mentioned, I advocated to the IOM committee that we view cancer survivorship as a distinct phase of the cancer trajectory with a unique constellation of needs and problems requiring specific interventions. This conceptualization was, in part, inspired by the experience with end-of-life care. Until fairly recently, there was a perception that individuals with a cancer recurrence went from recurrence to death, and that there was nothing in between. And then a group of very bright people said there is something called end-of-life care, which is a distinct phase of care, and which requires its own set of interventions and assessments. It is only when this distinct phase of care became recognized, that the whole field moved forward, and end-of-life care became integrated into practice. I think we have recognized that following primary treatment, there is another “box” called survivorship care. Having said that, the question then is “Once you recognize it, is that all that there is to it?” I would like to suggest that it is not a given that our healthcare professionals will, in fact, be able to deal with this “box.” They may not possess the appropriate knowledge and skills to assess and address the unique needs and problems of cancer survivors.
This is probably not a perfect analogy, but one could consider mantle cell lymphoma, which is a lymphoma variant that was widely recognized several years ago once special tests became available. Individuals with mantle cell lymphoma now require colonscopy and aggressive therapy. For the lymphoma doctors, the recognition of this variant did not represent a departure from their practices. There was no change in the paradigm. Once you recognized it, it took some different kinds of interventions, but they moved right into it. The other example that might be more applicable to survivorship is your primary care doctor in the early eighties who suddenly has a pneumonia patient with AIDS. This is no longer a pneumonia patient.
|
BOX 2-3
|
This is a totally different “box,” if you will. This takes a whole different set of skills and learning to deal with. The question for us here today is where are we with survivorship?
Survivorship care is incredibly comprehensive as reflected in its many domains (Box 2-3). Many of these areas are really outside of the purview of what is called active treatment. How do we gear up to provide this range of services? Can we do it?
Just to illustrate this issue, we can take the management of depression as an example. Table 2-2 provides data from the work of Steve Passik on oncologists’ recognition of depression among their patients (Passik et al., 1998). He assessed over 1,000 patients in 12 oncologists’ practices for depression using the Zung Self-Rating Depression Scale. He compared these results to oncologists’ ratings of their patients’ level of depressive symptoms. About 60 percent of the patients had stable or no evidence of disease, so they were in the survivorship phase. While physician ratings of depression were concordant with patient reports of no significant depressive symptoms 79 percent of the time, they were only concordant 33 and 13 percent of the time in the mild-to-moderate and severe ranges, respectively. Nurses assessments really were not very much better. It is not sufficient just to say that depression is part of survivorship care. We really need to increase providers’ skills in this area.
The IOM committee identified three areas where recommendations could advance the field—professional education, clinical practice guidelines, and healthcare quality measures. My presentation on these topics may sound like a litany of despair, but I would like to show you where we are now, because that at least shows us where we need to start, and how we can move forward.
TABLE 2-2 Oncologists’ Recognition of Depression
|
|
Percent Concordance |
|
|
Oncologists |
||
|
• |
No depression |
79 |
|
• |
Mild-to-moderate depression |
33 |
|
• |
Severe depression |
13 |
|
Nurses |
||
|
• |
Mild to moderate |
29 |
|
• |
Severe |
14 |
|
SOURCE: Passik et al., 1998. |
||
In the area of education, the IOM committee’s seventh recommendation calls for the NCI, professional associations, and voluntary organizations to expand and coordinate their efforts to provide educational opportunities to healthcare providers to equip them to address the healthcare and quality-of-life issues facing cancer survivors. I reviewed professional education and training opportunities for physicians including residency and fellowship programs, medical textbooks and journals, and continuing medical education (CME) programs. Committee member Betty Ferrell completed a comparable review for nursing.
So, what about physician training programs? When you look at the curricula developed by the American Academy of Family Physicians (AAFP) and the American Board of Internal Medicine (ABIM), there is really virtually nothing on cancer survivorship. When I looked at the curriculum for clinical oncologists, survivorship content was lacking, but Dr. Horning mentioned this morning that survivorship is being put into the curricula for fellows. Very often, the curricula I reviewed would address certain relevant domains, but survivorship was not covered comprehensively.
How about medical texts? If you are in practice, where do you go to learn about a new subject? One resource is medical textbooks. I reviewed seven family practice and internal medicine textbooks available at the library, and my first observation was that survivorship was not indexed in any of the texts. And I am not sure why this is. There is a lot of emphasis on Hodgkin’s disease follow-up and on issues related to genetics, both of which are important. However, half of cancer survivors have a history of breast, prostate, or colorectal cancer and there is virtually nothing on issues directly pertaining to them. I do not know why a focus on these more common cancers is lacking. But even more important, very often the information pertaining to survivorship is purely descriptive. For example, a text might say, “If you have a patient with this, make sure that there are no
sexuality problems.” But the text does not then tell you how to assess sexuality problems, nor does it tell you what to do about them. So the text just says it might be there, so it is not really a lot of help.
If you look up survivorship in the index of the latest edition of the oncology text authored by Vincent DeVita and colleagues (DeVita et al., 2004), you find that there are two whole pages listed. When you turn to them, however, it is really only half a column on one page, and half a column on the other page. Having said that, in reality there are two 100-page chapters looking at late effects and follow-up, et cetera. So, at least for medical oncologists, there actually is a pretty good resource.
When you go to the specialty oncology texts, the only one that I could find that really gets into survivorship is the Harris text, Diseases of the Breast (Harris et al., 2004). This text has six chapters looking at all phases of rehabilitation and convalescence from breast cancer. It is very, very good. We are fortunate to have Frank Johnson here in the audience and represented on our committee. He has written a book, Cancer Patient Follow-Up, that includes a very good review and discussion of follow-up strategies, mostly concentrating on surveillance (Johnson and Virgo, 1997). Berger’s textbook, Principles and Practice of Palliative Care and Supportive Oncology, has a chapter on survivorship authored by Noreen Aziz who works in the NCI’s Office of Cancer Survivorship (Aziz, 2002). The remaining texts that I reviewed included very fragmentary sections related to survivorship. The classic example of difficulties in coverage of survivorship in specialty oncology textbooks comes from urology. I pulled out a couple of urology texts to see what they cover. Given that urologists specializing in oncology see so many prostate cancer survivors, I looked up impotence, thinking that it would definitely be covered. Well, it was buried under social work. Penile implants are discussed under social work! I guess it is a social disease, but I am not quite sure how someone interested in this area would ever find the relevant text.
I also reviewed coverage of survivorship in primary care and oncology journals. In the primary care journals, there was a focus on breast and colon cancer with a heavy emphasis on genetics and menopause. There was not much coverage of long-term effects, and really no articles that told providers how to monitor individuals with a history of cancer. It became clear from this review, that primary care providers need a cancer survivorship care plan because there are few readily available resources for them. The survivorship-related content I found in internal medicine journals was very narrowly focused original research with limited generalizability. There was very little on how to monitor patients following their primary treatment.
In terms of the oncology journals I reviewed, the Journal of Clinical Oncology covers a broad range of survivor-related studies. Most articles reflect focused primary research, but the findings and discussions are most
often generalizable to the broad survivor population. Probably the best single journal source for information on cancer patient follow-up, if I had to identify one right now, would be two Seminars in Oncology issues published in 2003, Post-treatment Surveillance for Potentially Curable Malignancies and Late Effects of Treatment and Survivorship Issues in Early-Stage Breast Carcinoma. Both issues include comprehensive reviews of the literature.
It seems to me that one of the first steps, and a very easy one to take, would be to develop a comprehensive bibliography to include the broad range of review articles related to specific survivorship domains. A list of these could be published and distributed, or an online virtual text could be created which could be kept updated.
To get a better understanding of CME opportunities in primary care, I surveyed offerings at meetings convened by the AAFP and the American College of Physicians (ACP). Survivorship was rarely covered, and when it was there was a narrow focus on such topics as genetics and the use of hormone replacement therapy among breast cancer survivors. I gave one lecture at the AAFP on cancer survivorship and, based on the poor attendance, learned that this issue is not yet on their agenda. We have got to get it there. There is an excellent AAFP resource that I would like to call to your attention. The AAFP published a comprehensive, 60-page monograph on cancer survivorship which covers all the major areas including risk of recurrence, follow-up, late effects of treatment, psychosocial issues, sexuality, health behaviors, alternative medicine, disability, and discrimination. It was published as part of a home-study self-assessment program in 2001, and it is only available through a subscription at a cost of about $375 (Hamblin and Schifeling, 2001). They got 6,000 subscribers, and it has subsequently been sitting on their shelf. There are no plans to distribute it or update it so it represents a huge lost opportunity. The ACP CME activities related to survivorship were very sporadic, usually in the form of case studies.
When I surveyed ASCO on their survivorship CME about three years ago, I found that there were some fragmentary efforts. But by this year, there were quite a few opportunities, in large part, through the efforts of Patti Ganz. Patti is our Erin Brokovich. I can hardly wait until Julia Roberts plays you in the movie.
Committee member Betty Farrell helped us review the status of the oncology nurse workforce and nursing education. We recognized that nurses with advanced training can assume important roles in survivorship management, but found there are only about 19,000 oncology-certified nurses, and about 1,500 nurses with advanced oncology certification out of a total of 2.2 million licensed registered nurses nationally. Of great concern is that nursing programs are actually decreasing their oncology emphasis. In a review of 17 programs with an oncology focus, 11 of the 17 programs had
curricula that covered survivorship issues, but only 3 programs covered rehabilitation. So, nursing programs also have to be ramped up to ensure an adequate survivorship workforce.
In conclusion, survivorship as an educational focus is infrequently addressed in primary care training programs, but is getting increased attention in oncology training. When survivorship is addressed, it tends to be presented in a fragmented manner. A shortcoming of available survivorship education is that problems are often delineated without offering information about evaluation or treatment. To overcome these challenges and provide comprehensive training, we really need our professional organizations to step up and accept the survivorship paradigm.
Let me move on to guidelines. Recommendation three in the IOM report states that “health care providers should use systematically developed, evidence-based clinical practice guidelines, assessment tools, and screening instruments to help identify and manage late effects of cancer and its treatment. Existing guidelines should be refined and new evidence-based guidelines should be developed through public- and private-sector efforts” (IOM, 2006b). According to the IOM, clinical practice guidelines are “systematically developed statements to assist practitioner and patient decisions about appropriate health care for specific clinical circumstances” (IOM, 1990).
There are a couple of models to consider in developing survivorship guidelines. The guidelines could be specific to a particular cancer as is the case for treatment guidelines. Here, each type of cancer has its own work-up and treatment guideline, and also a type-specific survivorship guideline. Another model has generic guidelines that are applicable to several types or possibly all cancers. Accordingly, each type of cancer may have unique treatment guidelines, but could have the same survivorship guideline. This is the palliative care model. It does not matter what tumor you have, if you have pain at the end of life, it really generates a single guideline.
What is survivorship? Does it follow the multiple or the generic model? If you compared Hodgkin’s disease and breast cancer, most of the survivorship syndromes—I call them syndromes—are primarily tumor-specific. There are some components, such as anthracycline cardiomyopathy, which are generic, and for others, we do not know. Are the psychosocial problems of a survivor of Hodgkin’s disease different from those experienced by a woman with breast cancer? A lot more research has to be done to determine which model applies, but at this point, I think we are going to have hybrid guidelines. A bigger share of them will be tumor-specific, but they will also include generic components.
How should survivorship guidelines be structured? Supportive care guidelines developed by the National Comprehensive Cancer Network (NCCN) include the following steps: screen to see if something is going on; if something is going on, perform a risk assessment; triage according to the
TABLE 2-3 Content Analysis of 24 Breast Cancer Survivorship Guidelines
|
Topic |
Number |
|
|
• |
Follow-up schedule and testing |
12 |
|
• |
Monitoring for second primary tumors; Chemoprevention for second primary tumors |
11 |
|
• |
Menopause; Hormone replacement |
8 |
|
• |
Locus of care |
5 |
|
• |
Reconstruction |
4 |
|
• |
Lymphedema |
4 |
|
• |
Sexuality/fertility |
4 |
|
• |
Psychosocial |
4 |
|
• |
Genetics |
2 |
risk assessment providing specialized evaluation and specific interventions when indicated; re-evaluate; and follow-up. This type of model would seem to work well in the development of survivorship guidelines. The IOM recommendation calls for the development of screening and risk assessment tools which are consistent with this paradigm for guideline development.
The IOM committee attempted to assess the status of survivorship guidelines and reviewed 24 guidelines for breast cancer, 15 for colorectal cancer, 4 for prostate cancer, and 2 for Hodgkin’s disease. Breast cancer is at the forefront on survivorship, and there are many available guidelines. In contrast, there are relatively few survivorship guidelines for prostate cancer and almost no survivorship guidelines for Hodgkin’s disease. What characterizes these guidelines is their tremendous variation. Among the 24 breast cancer guidelines, for example, content varies widely (Table 2-3).
When you look at the areas that are discussed in the guideline, half address the appropriate follow-up schedule and testing, 11 cover issues related to second primary tumors, and then there is a marked drop-off. Lymphedema is only addressed in four of the guidelines. It is interesting that locus of care, that is, who should take care of the patient following primary treatment, is an element in the European guidelines, and very rarely appears in the American guidelines. We are not used to telling physicians where care should be delivered, but we may have to consider it.
In our review of survivorship, we found that the overall consistency of guidelines is good when the evidence underlying them is of high quality. If the evidence is soft, there tends to be variation in emphasis or in the strength of the recommendations. In the case of equivocal evidence, guideline recommendations may be contradictory. A recent example of guideline variation can be found in a comparison of various organization’s recommenda-
TABLE 2-4 Guideline Recommendations on Liver Imaging for Post-Treatment Surveillance Among Colorectal Cancer Survivors
|
Organization |
Cancer site |
Test and recommendation |
|
ASCO |
Colon, rectum |
Annual chest and abdomen CT scan for three years for patients who are at higher risk of recurrence and who could be candidates for curative-intent surgery |
|
ASCO |
Rectum |
Pelvic CT scan, especially for patients with several poor prognostic factors, including those who have not been treated with radiation |
|
ESMO |
Colon |
Abdominal CT scan, restricted to patients with suspicious symptoms; abdominal ultrasound every six months for three years then yearly for two years |
|
ESMO |
Rectum |
No imaging studies recommended |
|
CCO |
Colon, rectum |
Liver ultrasound or CT scan every six months for three years and then annually for three years |
|
NCCN |
Colon, rectum |
Abdominal CT scan for patients at high risk defined as poorly differentiated cancers or those with perineural or venous involvement (no frequency) |
|
ASCRS |
Colon, rectum |
No imaging studies recommended |
|
ACRONYMS: ASCO, American Society of Clinical Oncology; ESMO, European Society of Medical Oncology; CCO, Cancer Care Ontario; NCCN, National Comprehensive Cancer Network; ASCRS, American Society of Colorectal Surgeons; CT, computed tomography. SOURCE: Desch et al., 2005. |
||
tions for liver imaging following treatment for colorectal cancer (Table 2-4) (Desch et al., 2005). ASCO has just updated their guidelines and recommends annual computed tomography (CT) scans of the chest and abdomen for three years for colorectal cancer survivors. ASCO recommends that rectal cancer survivors also get a pelvic CT scan. The European Society of Medical Oncology (ESMO) recommends that abdominal CT scans be restricted to colon cancer survivors with suspicious symptoms, but it recommends ultrasound examinations every six months for three years. The ESMO recommends no imaging studies for rectal cancer survivors. Cancer Care Ontario (CCO) recommends an ultrasound or a CT scan every six
months for three years. The NCCN says that abdominal CT scans should be considered for patients at high risk. The American Society of Colorectal Surgeons (ASCRS) recommends no imaging studies.
Given the conflicting recommendations, there needs to be an amalgamation of the forces that develop guidelines. This example is provided, not to disparage the work of these groups, but rather to point out how variation is encouraged when evidence is deficient. How to deal with this is very challenging.
To summarize where we are with survivorship guidelines, the IOM committee concluded that there is no comprehensive set of survivor guidelines for any type of cancer; the guidelines that exist are fragmented and variable in their content; survivorship guidelines will likely have to be tumor-specific with some generic and modular elements; guideline development will optimally be multidisciplinary and interdisciplinary; and lastly, guideline development is instrumental in pointing out areas of deficient evidence and areas for further research.
The IOM committee also recommended that a set of survivorship care measures be developed. Quality measures fit well into a mechanism for trying to improve care. The mechanisms by which this works were elucidated well in the 1920s and 1930s by Elton Mayo, a Harvard Business School professor. He studied productivity at the Western Electric Company’s Hawthorne Plant in Cicero, Illinois, and found that when you pay attention to workers, that is, you measure their performance, you can actually get them to be more productive. Individuals altered their work behavior because they knew they were being studied. This, so-called Hawthorne effect is now widely recognized, but first identified by Elton Mayo.
Quality measures can be used as part of accountability and public reporting programs, internal quality improvement programs, and surveillance for policy setting and resource allocation. Using quality measures to direct our own internal quality improvement programs is the application that most professional associations are most comfortable with and that may be the way to start. What you try to do is drive performance by reporting who is good and who is bad. We will discuss this a little bit more in the breakout group.
One of the difficulties applying quality measures in these contexts for survivorship is that we are going to have to decide how to attribute performance on aspects of care. If a woman does not get her mammogram following breast cancer surgery, whose fault is it: the surgeon, the medical oncologist, the family practice physician, the hospital, or the health plan?
In our review, the committee found very, very few survivorship-related measures out there. And some that have been looked at like follow-up mammography or follow-up colonoscopy have shown that there is varia-
tion in care, so that in fact there is room for measuring something. We really need efficiency measures, and one of the easiest ways to look at that is overutilization of tests—patients who are getting follow-up tests that they do not need. And most importantly of course, we need measures of patient-centered care, which may involve health surveys. The whole performance measurement movement needs to move forward and consider issues related to survivorship.
In conclusion, the committee found the training and management programs required to prepare healthcare professionals to appropriately manage the full range of survivorship needs to be rudimentary. A necessary next step is the development of formal and well-designed educational programs, guidelines, and quality measures through public-private partnerships.
Dr. Greenfield: Do we have a couple of questions?
Bob Weiss, National Lymphedema Network (NLN): I would add to your CME resources a session for physicians on the diagnosis and treatment of lymphedema held at the NLN’s biennial seminar (next conference will be in Nashville, Tennessee, in early November). There is also usually a half-day session on wound care for individuals with lymphedema. Such training is needed because doctors must know how to treat the 20-30 percent of cancer survivors who will develop lymphedema. These CME opportunities are a wonderful source. NLN also has available videos for self-care.
Dr. Winn: Thank you. Actually, I have given you a little bit of short shrift in terms of the available opportunities. There is a whole chapter on professional educational opportunities in the IOM report, and I urge you all to read that chapter, because there is a much greater universe of potential teaching resources than I have described.
Dr. Greenfield: Let us now turn to John Ayanian to hear about research issues.
ADDRESSING GAPS AND NEW PRIORITIES IN CANCER SURVIVORSHIP RESEARCH
John Z. Ayanian, Associate Professor of Medicine and Health Care Policy, Department of Health Care Policy, Harvard Medical School and Brigham and Women’s Hospital
Thank you, Shelly and Ellen. It is great to be here. What I find particularly exciting about the process that our committee embarked on, and that we are bringing to the next stage of development today, is really moving
from thought and reflection to priority setting and action. A very important part of that process is the role of research.
My presentation this morning will focus on our tenth recommendation, which addresses the research needs related to cancer survivors, and really, the opportunity to move beyond addressing gaps. So, I have modified the title of my talk from what is in the program. In addition to addressing research gaps, I will be focusing on new priorities in cancer survivorship research. Looking at research gaps is really an observational experience. What has been exciting about our committee’s work has been moving forward from the identification of those research gaps to identifying important priorities for policy and for practice. I would like to focus in my talk on a discussion of research that would really move this field forward and make care and quality of life better for cancer survivors.
As background, I am a primary care physician, a general internist at Brigham and Women’s Hospital, and also a researcher in the Department of Health Care Policy at Harvard Medical School, focusing on issues of access to care and quality of care. And in my primary care practice I very much enjoy and am challenged by the opportunities to care for cancer survivors in collaboration with my colleagues in medical oncology, surgical oncology, radiation oncology, and other fields involved in the care of cancer survivors. And so, my talk today is a reflection on what our committee identified as priorities, combined with my own experience caring for cancer survivors and working with colleagues, and really coming to the recognition in my own practice and research that well-coordinated care is one of the most important goals that we should be striving for here; care that is well coordinated between primary physicians and specialists. It is often difficult, and it is a challenge going forward, to define what we mean by well-coordinated care. But when patients experience it, when their families experience it, when doctors participate in it, they know what it is. And people know it when they see it, when they experience it. So, that is one of the research priorities that I want to highlight going forward.
The committee’s tenth recommendation states that the National Cancer Institute, the Centers for Disease Control and Prevention, the Agency for Healthcare Research and Quality, the Centers for Medicare & Medicaid Services, the Department of Veterans Affairs, and private organizations, particularly the American Cancer Society, and others involved in cancer care should increase support for survivorship research and expand mechanisms to conduct this research. As Dr. Mullan suggested earlier this morning, a concluding recommendation for more research is in some sense a “gimme” for an IOM report. But it is important to emphasize that we are not just saying more research, we are really emphasizing who should be setting the agenda and investing in further research. I would like to focus on the goals of a research portfolio that we believe would
actually help us to move forward to improve quality of life and the quality of care for cancer survivors.
The first priority for new research is assessment of late effects of cancer and its therapies. Here, there is a need for some basic, clinical, and epidemiologic research, looking at the prevalence and risk factors of cancer late effects and cancer treatment late effects, as well as their mechanisms, because understanding those factors will help us to move forward in terms of improved and more targeted care. That then needs to be translated into improved guidelines and assessment tools, and understanding which interventions are best applied to reduce symptoms and improve functioning for cancer patients. And I think what is important about the research recommendation here, as you will see as I move through my slides, is that it is really a cross-cutting recommendation that draws on and advances many of the other nine recommendations in our report.
A second major priority for new research is improving quality of care. And this draws on three other recommendations in our report addressing the survivorship care plans that Dr. Ganz has discussed, the quality indicators that Dr. Winn has discussed, and the coordination of specialty care and primary care. At the same time, we can address the issue of resources and trying to do things more efficiently and effectively. We need to understand from a research perspective, which care models and surveillance strategies are the most effective and which are the most cost effective, so that we can use resources and help the maximum number of people with the resources that we have available, while at the same time pushing for a greater investment of resources in these areas.
Improving quality of life, as a third area of priority, moves forward in several dimensions in terms of our seventh recommendation regarding educating healthcare professionals. We not only need to develop programs to educate professionals, but to also involve our colleagues who are experienced educational researchers in studying which of those educational programs are most effective. From my perspective, one-time continuing education courses will only set the stage. We really need to build some mechanism for ongoing education and continuous learning into our training programs of health professionals, as well as for health professionals in practice. We need to understand what works in terms of making them effective providers for cancer survivors.
We need to understand the factors that facilitate return to employment following cancer treatment, drawing attention to our eighth recommendation. What types of programs, from a research perspective, help people to return to work, and work effectively? We also need to understand the financial burdens that cancer patients face. I had the opportunity to serve not just on this committee, but on the Institute of Medicine committee addressing the consequences of uninsurance that concluded its work last
year after issuing six reports on the topic. And what was very interesting to see in our own committee’s discussion about cancer survivors is this intersection of priorities from previous IOM reports such as the consequences of uninsurance, with the special needs of cancer survivors. Cancer survivors are a high-risk, high-need group who are vulnerable in terms of the financial burdens of treatment costs and their potential limited ability to work. We need research to assess what we can do to ensure that people have good quality insurance and access to appropriate services.
Enhancing support for family caregivers is a hidden topic that is just beginning to get more attention and research. We need to think of cancer survivors not just as individuals, but as members of families and households and communities. We need to support the cancer survivor and, in addition, address the physical and psychological needs of people providing care to loved ones.
And finally, there is that whole domain of research that could pursue the role of legal protections such as the Americans with Disabilities Act, the Family and Medical Leave Act, and the Health Insurance Portability and Accountability Act (HIPAA). All of these legislative actions create both opportunities as well as potential risks for cancer survivors in terms of how they navigate the healthcare system, the insurance system, and the employment system. And we need to understand how those legal protections are working for cancer survivors.
What are some mechanisms to expand survivorship research? As a committee, we came to the conclusion that one of the most important mechanisms is more attention to long-term follow-up of enrollees in clinical trials. What I would suggest is thinking of cancer survivors with forethought, instead of afterthought in our research agenda. Here we have a group of people who have already committed themselves as willing participants in research to help us understand more about the acute treatments for cancer. They are an underutilized or untapped resource for understanding the long-term effects and the ways that we can improve their care and quality of life. And I would venture that many participants in clinical trials would be very willing to participate in survivorship studies going forward if we made those opportunities available to them.
Another important resource is special studies in our various national registry programs including the Surveillance, Epidemiology, and End Results Program supported by the National Cancer Institute, the National Program of Cancer Registries, supported by the CDC, and the National Cancer Database, supported by the American College of Surgeons’ Commission on Cancer. All of these registries have been designed to count people who are diagnosed with cancer, in some cases to understand their acute treatment (initial treatment within four months of diagnosis), and then potentially to track whether they survive. With targeted investment, each of these re-
sources could do a much better job of following people after their acute treatment, and really provide a foundation of opportunity for studying cancer survivors’ quality of care and quality of life experienced after the initial treatment period. Within the cancer registries, a special focus needs to be on cancer recurrences. Right now, many cancer registries track whether people survive or die, but do not have the resources needed to track whether they develop a recurrence of their initial cancer, or develop a second cancer. There are opportunities through links to Medicare data and electronic data from health plans and other organizations to understand the whole domain of cancer recurrence in much greater detail.
We also have large cohort studies and research networks in place that could be used to further survivorship research. One that I am actively involved with is the Cancer Care Outcomes Research and Surveillance Consortium (CanCORS). We have enrolled nearly 10,000 patients with colorectal cancer and lung cancer. We are supported by the National Cancer Institute and the Veterans Administration to study this group’s health care and outcomes in the first year after diagnosis. With further investment, it represents a great opportunity to study what happens to people after that first year of living with cancer. The Cancer Research Network is another resource funded by the National Cancer Institute. It is a consortium of health maintenance organizations around the country that have large enrolled populations, and the ability to track with electronic data systems who is developing cancer, and what happens to them over time. We also have practice-based research networks supported by the Agency for Healthcare Research and Quality that typically involve networks of primary care practices around the country that are willing participants in research. These networks are advantageous because they have a connection to the community and could move cancer survivorship, which is now largely in the domain of comprehensive cancer centers, out to a broader array of delivery settings, all of which have a very important role to play. Most cancer survivors are treated in community-based practices, not in comprehensive cancer centers.
Finally, our committee felt that national surveys have an important role to play in furthering the survivorship research agenda. Our federal government has made a strong investment in collecting health-related data on a representative cross-section of Americans through surveys such as the National Health Interview Survey, the Medical Expenditure Panel Survey, and the Behavioral Risk Factor Surveillance System. In some cases, there is great opportunity to focus on cancer survivors, identifying who they are in these national samples, and then developing modules to learn more about their quality of life and quality of care. We could get a much more representative understanding of how people are living with cancer through such surveys.
The committee also identified challenges in survivorship research. First, we need to recognize that long-term follow-up is labor intensive and expen-
sive. It will require investment of resources, but we believe that the dividends paid by those investments could be substantial. It is also challenging because many studies are multi-institutional in nature, and thus require multiple institutional review boards (IRBs) to approve them and monitor them, often with widely varying standards. Consequently, there is a role for the federal government to help the research community to develop more common standards for IRBs. One particular IRB could potentially be designated as a coordinating IRB for multi-institutional studies. There may be models for this in the world of clinical trials, and we also need to develop them in the domain of survivorship research. Finally, we have continued to grapple with HIPAA standards over the past two years. There is a lot of uncertainty among patients, family members, and healthcare providers about the privacy of medical information, and how privacy can be assured in the context of research. In some cases, there has been an overreaction by community practitioners, leading them to defend their medical records and to be very cautious about releasing them for research. We need to educate both patients and providers about the value of research. With appropriate confidentiality and privacy protections we need to partner with hospitals and community-based practitioners to gain access to medical records in a way that is compliant with HIPAA, but not stymied by HIPAA.
To conclude, cancer survivors’ needs must become a research priority. This is a clarion call from our report today. Research is essential to improve quality of care and quality of life for cancer survivors. It is not something that can be done on the side. Instead, it is really a central springboard to addressing many of the issues that we have been talking about today, and will continue to discuss. We need to better understand how quality of care and quality of life should be measured, and how they can be improved in practice. The research agenda that we are addressing today would advance multiple recommendations in the IOM report. Finally, there are opportunities to build on the existing infrastructure that we have with new federal support focused on an expanded role for clinical trials, cancer registries, large cohort studies, and national surveys. We have the building blocks in place. Now we have to make them work for cancer survivors so we can improve their care and quality of life.
Dr. Greenfield: We have some time for questions for John, and then for the rest of the speakers as well.
Dr. Anna Meadows: I want to thank you for putting research in such an incredible perspective in terms of the rest of the report. I only wish the research chapter had come at the beginning of the report, because I think everything follows from that. I have been doing research in cancer survivorship for 30 years, and I was a part of the Childhood Cancer Survivor Study
in the beginning. This large cohort study requires an enormous amount of resources to follow. I was also recently part of the development of guidelines for the Children’s Oncology Group, so I know it is important to have consensus for guidelines.
One of the problems that I see in both the Childhood Cancer Survivor Study and the development of guidelines and the way to provide clinical care is that unless we really have guidelines that we know are not just based on the consensus of opinion of people who take care of patients, but are truly developed from research that we can conduct, then the care plans that we give to patients are almost touchy-feely. How often do you do cardiac studies in patients who have had anthracycline? And what is the dose of anthracycline that requires that you do such studies twice a year, rather than once a year? These are questions that need to be addressed with research. And unfortunately, not putting the research first, really misses the point.
The other problem is that when we do the research, or will do in the future, if we do not follow all the patients, we will not get the right results. We have been missing at least half of our childhood cancer survivors in our research studies, and we do not know about the other half of this cohort. We started with 20,000 eligible patients in the Childhood Cancer Survivor Study, and we are down to 10,000 now. Admittedly, these were patients who were treated a long time ago, but we do not have information on their outcomes. So, I really think that the thrust for research is so important, again, I am surprised it was not the topic for the first chapter.
Dr. Ayanian: The chapter on research is the final chapter of this report, but we should also think of it as the first chapter of our work going forward. That is what our committee has tried to lay out in the agenda today.
Dr. Beth Kosiak: I am from the Agency for Healthcare Research and Quality, but this comment that I would like to make is coming more as a stage 3 melanoma survivor. And what I would like to say is that one of the issues that came up for me in looking at the excellent research agenda laid out on cancer survivorship is how critical that research agenda is for informing newly diagnosed patients. Because as a newly diagnosed patient, you want to know what happened to people who chose different courses of treatment, because often times, as in my case, there is not an obvious course of treatment that is clearly recommended by the clinical community. And because they are divided, then you have to look at your own choices, and look for resources to make a choice. Having the information that you would get from the cancer survivorship research focus would really help newly diagnosed patients make that choice, because there would be that longitudinal information to help them look at what happens if I do nothing,
which was one of the choices that was offered to me. So, again, there are a lot of other comments that we will be able to make later in the day, but I just wanted to note that it really closed the loop for me, and I think it is an important aspect of the research.
Dr. Jerome Yates: I am from the American Cancer Society, and from my perspective one of the real difficulties in looking at the research agenda is the intersection of the physical factors such as the disease stage and the treatment selected, and the social factors such as age, where people live, and access to health care. These are so complex, that they are going to require many, many analytic compartments. And this means that we have to use information systems to better advantage to sort out the information, and also to develop accessible educational materials that may be available.
Just to follow-up on what Anna has said about the loss of the children to follow-up, in my former life at a cancer institute we provided free follow-up for the children for as long as they came back to the institution. The further out they get from their initial cancer, the more unlikely they are to come back, even if you provide them with transportation when it is needed, and the other things to encourage follow-up.
The last comment I would make is that we have to do something about litigation because there are opportunities for lawyers to sue for things that we know were not known at the time of treatment. This raises real difficulties for the physicians. The classic case of this is the retinal changes with oxygen in the young children, and the recent Vioxx (rofecoxib) story are just two examples of how we cannot afford to not do something about the litigation issues.
Dr. Greenfield: If I might just respond to the legal issues that Dr. Yates brought up. These legal issues are why Rodger Winn’s slide about the different organizations agreeing and not agreeing about guidelines is so very important. If there is an overwhelming consensus, if you will, about doing or not doing something as we have seen in diabetes and some aspects of heart disease, it blunts a lot of the potential for litigation. Let’s have general questions for any member of the panel now.
Dr. Archie Bleyer of Cure Search, the LIVESTRONG™ Young Adult Alliance, and the Children’s Oncology Group: The survivorship care plan is a place to start. Dr. Greenfield asked earlier about resistance to implementing the care plan. The video was superb, the presentations were outstanding, and the report speaks for itself, but I wonder about a potential downside. Dr. Winn has described the cancer care trajectory, and Dr. Ganz has shown in Figure 2-4 the shaded box representing survivorship care. We now recognize the box. This conceptualization takes the patients or survivors out of
the trajectory from the oncologist, puts them into a different sphere, and then probably takes the survivor back to the oncologist with a recurrence or later in life. Although I support the survivorship care plan, are we turning this care back to the generalist, to the primary care providers, including two of our panelists, a little too quickly? Is the “hand off,” the term used in the video, too abrupt, too definite? Will we use the survivorship care plan as oncologists to close the book, as Patti put it, write the final chapter, and turn the patient over to that shaded box? As a pediatrician, that is not what we have done. So, I am worried about that potential downside.
Dr. Ganz: I would like to comment on a few things. Number one, ASCO’s Cancer Prevention Committee did a survey, and we actually asked medical and radiation oncologists and surgeons who care for adult cancer patients about whether they cared for cancer survivors. The vast majority, 60 to 70 percent, of these providers said that survivors were a major part of their practice and that they provided many aspects of routine care for them. So, in fact most oncologists, at least in this survey, said that they were providing survivorship care. Isolating and defining that shaded box in the care trajectory, does not specify how care is to be delivered. It just says that it is a phase in the care trajectory. And as you will hear later from other discussions, one of the models applicable to survivorship is a shared model of care. Many practice according to this model. For example, I continue to follow all of my breast cancer survivors. I have patients that I have taken care of for 15 to 20 years. I see them once a year, so I am not attending to all their interim health care needs. These patients have primary care physicians that feel very comfortable approaching me if something comes up in relation to their cancer history. There was no intent in discussing the survivorship plan to convey a cessation of treatment by the oncologist. When I mentioned “closing the book,” I was referring to getting closure on the acute phase of treatment. There is a beginning and there is an end of acute treatment. And we need to summarize what went on in between, and that is what the retrospective part of the plan includes. But the perspective of the rest of the plan is really looking forward. And as I discussed in quite a bit of detail, it is defining who is going to do what in that follow-up plan. What is the oncologist going to do? What is the primary care physician going to do? What is the nurse practitioner going to do? What is the social worker going to do? So, I think you may have seen it in that way, but I do not think that was our intent.
Dr. Winn: Let me just chime in. Archie, I think the model you describe is a failed model that pervades in medicine. It is a linear model of hand offs and no feedbacks, et cetera. I think what we really are talking about here is a parallel model with interconnections between the parallel streams, and that
is the only way it can work. I think one of the most exciting things from the IOM’s point of view may be in cancer taking the lead in trying to show other chronic disease models how, in fact, you should be coordinating this care moving forward.
Ms. Stovall: At the end of the process of completing the committee’s work I had some conversations with IOM staff and fellow committee members about what was next. And the NCCS made a decision to sponsor a workshop next spring to show what it would take to bring people together to implement this care plan and answer a lot of the questions that have been raised. There are a lot of recommendations that are intended to take ideas and flesh them out. They can not be done right away. But this recommendation has been sitting around a long time because the need is so great. I think that one of the frustrating things in the advocacy community and the patient community over many years is that people always say, bring us the evidence, bring us the evidence. And when does a body of anecdote become enough evidence? We now have studies that quantify the problems and we have people’s stories that illustrate in excruciating detail the gaps in the care system. And if it is not ready for public health now, when will it be? So, we have to arrive at a place where reasonableness is a justification that we are willing to accept in order to implement some of these things that just make sense. I am excited about the recommendation, if only for the fact that it gives us an opportunity to flesh it out even further. And I know the Lance Armstrong Foundation has indicated a willingness to work with the NCCS, ASCO, and NCI to further this work. So, we will be back to you with more on that in the future.
Dr. Greenfield: We will take a couple more questions and then take a break.
Dr. Runowicz: I am from the University of Connecticut as a representative of ASCO’s Survivorship Committee, and I am also president-elect of the American Cancer Society, so I wear multiple hats. In response to Ellen Stovall and also to Anna Meadows, in terms of evidence for decision-making, I think it is not an either/or situation. It is important to keep in mind that expert opinion is a level of evidence. It may not be the best that we have, but if it is all that we have, then that is what we go with while we are trying to get the answer to how many scans we do of the heart in patients who have had adriamycin, or do we need any? I think we have interim guidelines, and then we replace them with evidence-based guidelines when data are available.
Ms. Stovall: Thank you for that comment. I just also want to say that maybe being in Washington as long as I have breeds discontent on a lot of
levels. One of those levels is that as an advocate and an activist to go to the Hill with either a universal healthcare message or another message. The reaction is often “show me the evidence.” Sometimes, this response is a way to keep things from happening. It is used as a reason to deny the things we need, rather than to promote the things that we know would help us.
Dr. Antonio Wolff: I am a breast cancer medical oncologist at Johns Hopkins, and also chair-elect of ASCO’s Health Services Committee. One of the things that strikes me the most, and I always like to say that, ultimately, the enemy is us, because I think somehow every time that I see my ear, nose, and throat (ENT) physician, and he spends five minutes doing a nasal endoscopy and charges me $600 and then I see how much money my department charges for my medical oncology consultation when I spend an hour with a patient, I think the incentives are wrong. And when you see the way we created Medicare and other systems to provide acute care, you realize that as a society, we focus on acute care that is perceived to be sexy and fancy. But we do not focus on things like survivorship care. I think all of us are very well intentioned, and we want to do the right thing. It is the same as with the clinical practice guidelines. As clinicians, we want to do the right thing. Between all the pressures and all the incentives, and for many providers the need to make a living, pay your expenses, make a profit, et cetera, I think until the system changes, all the beautiful products that we are putting out, and educating individuals, it is going to be difficult to get the message out.
Dr. Greenfield: Rodger Winn, do you want to respond to Dr. Wolff’s comment from the viewpoint of efficiency and resource use?
Dr. Winn: Use of time and resources is a very important consideration. I did a little back-of-the-envelope study on cancer patient follow-up for a breast cancer doctor who treats half his patients with adjuvant chemotherapy, and where they do beautifully and they live. Five years down the road, 26 percent of your practice is going to be those survivors, and 10 years down the road 40 percent of your practice is going to be delivering survivorship care. You are going to have people with acute concerns with cancer treatment waiting to get through the door. And this forecast for resource use is an example of why shared models, nurse-led models, or survivorship clinics have to be explored going forward so that the incentives are right to give these patients the care they need.
Dr. Greenfield: A lot of big employers are pushing very hard for efficiency measures, now more euphemistically termed “resource use.” And most of it comes from big companies. That is the stimulus. These mechanisms involve
consideration of cost and may be useful, but as physicians, we do not like to hear about them. Pressures to reduce cost may limit the overuse of unnecessary services and free up resources to counter underuse of necessary services.
Dr. Susan Weiner: I am from the Children’s Cause for Cancer Advocacy. I was involved in the first survivorship report on childhood cancer. I would like to first congratulate everybody who worked on this report. It is an absolutely fabulous companion piece to the childhood cancer survivors report that the IOM produced about a year and a half ago. My question has to do with issues related to hand offs and transitions. Survivors of childhood cancer have problems that are more dramatic perhaps than those of adults. They develop and change, they grow, and they become adults, and they end up in clinicians’ practices. My question is for Dr. Ayanian, but also for the panel generally. I would like to know whether you would be willing to address the question of transition to adult care for childhood cancer survivors either in one of the breakout sessions or in whatever follow-up activities there are?
Dr. Ayanian: It is a great point that you raise, and something that I face in my clinical practice at Brigham Women’s Hospital across the street from Children’s Hospital of Boston. It is not infrequent that we care for survivors of childhood chronic disease, including cancer or other conditions such as sickle cell anemia or severe asthma, who then need to transition to adult care sometime in their late teens or early twenties. Because of their chronic condition, sometimes these adolescents and young adults end up with their pediatric providers into their late twenties and early thirties. It is certainly a topic that we need to pay more attention to. In areas of the country where pediatricians and internists are accustomed to working closely together, often in major academic centers, where children’s hospitals and adult hospitals are side by side, these centers should be leading the way in studying and developing new care models to ensure there is continuity of care. These young adults are a special group of patients who are particularly at risk of getting lost in transition and we need to pay more attention to them. From a professional standpoint, we have a growing number of people who are jointly trained in pediatrics and medicine, and many of them are starting to address questions just like the one you raised about how care should be transitioned for patients with childhood cancers who survive into adulthood.
Dr. Greenfield: Let’s have one more response, and then we’re going to have to close.
Dr. Winn: This issue came up during our committee’s deliberation. Who, for example, should follow childhood Hodgkin’s disease? Steve Woolf is
sitting there with the family practice hat on saying, give us a good guideline, and we will do it. Sara Donaldson is there from Stanford saying, “Over my dead body.” And the answer is we do not have all the answers. But certainly, the issue was addressed, and what it really did is bring the two participants to the table, because that is the only way that this is all going to move forward.
Dr. Greenfield: We are going to have to close this session. I think your question and many others that came up earlier will be discussed and answered during the breakout sessions.