5
Improving Awareness, Diagnosis, and Treatment of Sleep Disorders
CHAPTER SUMMARY The public health burden of chronic sleep loss and sleep disorders coupled with the low awareness among the general population, health care professionals, and policy makers requires a well-coordinated strategy to improve sleep-related health care. Increasing the awareness and improving the diagnosis and treatment of sleep disorders necessitates a multipronged effort that includes three key components: public education, training for health professionals, and surveillance and monitoring. First, a public health campaign is required to increase awareness among the general population. Second, specific education and training strategies are needed to increase awareness among health care professionals, including improved curriculum content and certification requirements. There are a number of surveillance and monitoring tools, but very few examine issues pertaining to sleep loss and sleep disorders. Thus, third, improved surveillance and monitoring of the general population is needed. The preeminent goal of this strategy is to create and sustain a broad societal commitment to engaging in proper sleep habits as a primary tenet of health. Such a commitment will involve participation by those individuals and organizations in a position to educate the public at national, state, local, and community levels—including K–12 education, colleges and universities, medical schools and other health profession education programs, hospitals, community clinics, local health departments, private industry (e.g., transportation, manufacturing facilities, nursing homes), and entertainment media. It will also require simultaneous investment in public education cam-
paigns for all age groups as well as a sustained effort to integrate sleep-related content into curricula of undergraduate health science programs all the way through continuing education programs for health professionals.
CHALLENGES FACING INDIVIDUALS WITH SLEEP DISORDERS
Sleep is often viewed by the general public as a “perceptual hole in time”—during which nothing productive occurs (Dement and Vaughn, 1999). One only has to examine common colloquialisms such as “don’t get caught napping,” “if you snooze you loose,” or “time is money” to gain a sense of the prevailing attitude that sleep is either optional, a luxury, or unimportant. In fact, being able to “get by on 4 hours of sleep” (and thus being able to increase productivity) is often considered an enviable trait.
Daily sleeping and waking patterns are no longer driven by the light and dark cycle but, rather, by work schedules, economic interests, and increasing globalization. Unfortunately, the resulting “24/7” schedules are typically not optimal in terms of filling physiological requirements for sleep. Thus, daytime sleepiness and its consequences are becoming increasingly common problems affecting up to 15 percent of the population (Punjabi et al., 2003). For some, sleep disruption and constant sleepiness are often deemed an inevitable part of their social roles as spouses, workers, caregivers, and so on. Although improving diet and exercise as a part of a healthy lifestyle program is acceptable, sleep continues to be considered an expendable luxury (Dzaja et al., 2005). Thus, performance and social responsibilities may often take precedence over sleep, largely because of multiple role demands and expectations.
Stigma is a problem that often complicates chronic illness. Acceptable standards for roles and activities are socially determined, and individuals who deviate from these expectations because of chronic illness are often labeled as “different” and are thus stigmatized (Falvo, 2005). Similarly, individuals with certain sleep disorders, which are often chronic in nature, may also be stigmatized because of the inability to fulfill role expectations. An additional factor that may underlie this stigma is that sleep is typically misperceived as an “asocial” activity. However, sleep is actually a very important type of social interaction—an activity that is negotiated with self, family, friends, employers, lawmakers, fellow drivers on the road, and so on (Meadows, 2005). When, where, and how sleep occurs is an extremely important sociocultural matter (Taylor, 1993; Williams, 2002), and there can be considerable negative sociocultural consequences when the sleep behavior, either intentionally or unintentionally, is unacceptable (Mehlman,
2001; Moore et al., 2002). Obesity also presents another challenge to some individuals with sleep disorders. Obesity engenders negative feelings among caregivers, which may affect an individual’s health care (Banno and Kryger, 2004).
The lack of awareness among the general public that results from the absence of sleep content in public health education programs causes patients to be hesitant about discussing sleep problems with their health care providers. In addition, fear of being labeled as having a psychiatric problem or exhibiting drug-seeking behaviors are also deterrents (Culpepper, 2002). In the case of insomnia, the most common of all sleep-related complaints, patients typically do not seek help because they believe either that nothing can be done or that the health care providers will do nothing to address the problem (Engstrom et al., 1999).
Patients with excessive daytime sleepiness represent the largest group seeking help at sleep laboratories but often only after they have encountered numerous problems that interfere with performance of normal activities of daily living, their ability to hold a job and maintain a marriage, interact socially, or have had an accident. All too often, these individuals have been labeled lazy or unmotivated. For children with narcolepsy, for example, the stigma associated with their increased daytime sleep tendency can affect social acceptance owing to unusual behavior as well as future risk of increased psychiatric disorders, potential obesity, and depressive symptoms (Dahl et al., 1994; Guilleminault and Pelayo, 1998). Thus, individuals may have to overcome a stigma attached to having a sleep disorder, and seeking appropriate treatment is a very serious issue.
Somnology Public Health Education Campaigns
A review of the National Center on Sleep Disorders Research (NCSDR), Centers for Disease Control and Prevention (CDC), and private foundations demonstrate a limited investment in education and awareness campaigns directed toward increasing the general public’s knowledge of the health implications associated with chronic sleep loss and sleep disorders.
National Center on Sleep Disorders Research Public Education Campaigns
The NCSDR was established within the National Heart, Lung, and Blood Institute (NHLBI), partially in response to the previous experience and success the NHLBI had in public education campaigns (see below). As directed by the congressional authorization language, the NCSDR is responsible for coordinating the “disseminat[ion of] public information concerning the impact of sleep disorders and sleep deprivation” (Appendix D)
(U.S. Congress, Senate, 1993). It has also developed a variety of education materials; however, resources have not been devoted to an in-depth evaluation of the effectiveness of these materials. The primary education programs that the NCSDR have initiated include the following:
-
Sleep, Sleep Disorders, and Biological Rhythms is a curriculum supplement developed for grades 9 through 12 (NHLBI, 2003b). Approximately 12,000 copies of the curriculum supplement have been sent to teachers. There have been more than 11,000 visitors to the sleep curriculum website and 10,000 downloads. More than 2,000 students entered sleep diary data on the Internet.
-
The Garfield Star Sleeper Campaign was designed to educate children, parents, educators, and health care providers about the importance of nighttime sleep during childhood (NHLBI, 2005b).
-
Time For Kids is a magazine on sleep that was developed and distributed by the NCSDR to 30,000 third-grade teachers and the 750,000 children in their classes in connection with National Sleep Awareness Week (NHLBI, 2004).
-
The Healthy Sleep Handbook is a booklet that will be available to the general public and provide an overview of sleep disorders with signs and symptoms, consequences, and potential treatments. It will explain why sleep is needed, what happens if you don’t get enough sleep, and tips on how to obtain enough sleep (NHLBI, 2006).
As these examples demonstrate, apart from campaigns directed toward children and adolescents, which have been inadequately evaluated, the NCSDR has not engaged in widespread multimedia public education campaigns directed toward other susceptible populations, including college students, adults (especially shift workers), elderly people, and high-risk minority populations. This is in part owing to the limited resources of the NCSDR for public education (see Chapter 7). A potential strategy to strengthen these activities is to collaborate with other federal agencies including the CDC, as was directed by the congressional authorization; however, there has been limited involvement of the CDC and other federal agencies in these activities.
Private Foundations Education and Awareness Campaigns
Although limited, private foundations and professional societies, and to a lesser extent patient advocacy organizations, have developed a number of public education programs. A highly successful example is the National Sleep Foundation’s (NSF) National Sleep Awareness Week campaign. This campaign coincides annually with the start of daylight savings
time and brings together over 750 sleep centers and 100 government agencies and other nonprofit organizations to plan and implement several public awareness and education projects. Activities have included sleep health fairs, lectures, and a public policy and sleep leadership forum. The NSF also conducts the Sleep in America poll, an annual telephone survey that gauges how and when Americans sleep, and created a multimedia educational tool called Cycles of Sleeping and Waking with the Doze Family that illustrates information about sleep and includes a website, print materials, and CD-ROM.
Although the Sleep Research Society (SRS) and the American Academy of Sleep Medicine (AASM) are primarily professional societies, they also have contributed to increasing the awareness among researchers, health care providers, and the general public. For example the SRS is a cosponsor of the Trainee Day at annual meeting of Associated Professional Sleep Societies, recently published the Basics of Sleep Research guide, and established the Sleep Research Society Foundation, which annually supports up to six $20,000 grants. The AASM professional initiatives and public education efforts include among others, the CPAP (continuous positive airway pressure) Compliance Campaign, establishing accreditation programs for sleep technologists and behavioral sleep medicine training programs, and assisting in the development of new clinical practice guidelines. Other private organizations such as the American Sleep Apnea Association, Restless Legs Syndrome Foundation, and Academy of Dental Sleep Medicine have also created smaller public education tools such as patient education brochures, support groups, and online videos.
Educational Activities of the Centers for Disease Control and Prevention
The public education efforts coordinated by the CDC provide additional models that could be used to increase awareness about the health implications of chronic sleep loss and disorders. The CDC has extensive experience in health education and has developed very effective programs in such diverse areas as obesity, colorectal cancer screening, and adolescent health.
The CDC’s public information campaign to encourage physical activity includes a website that covers the importance of physical fitness including the health benefits, how much exercise is needed, how to overcome barriers to exercise, and specific tips for becoming more active. The website includes references to documents and other organizations that are resources for individuals interested in this topic (CDC, 2006).
The CDC also partners with other related government and private entities to make these public health campaigns even more effective. For example, the Screen for Life campaign is a successful multimedia colorectal
cancer screening education program in which the CDC has partnered with other organizations including state departments of health, the National Colorectal Cancer Research Alliance, and the Entertainment Industry Foundation. This program targets the general public as well as health professionals and encourages colorectal cancer screening for every person after age 50. In addition to the education and awareness campaign, the CDC also developed a nationwide surveillance program to assess the capacity to perform colorectal cancer screening tests and follow-up for the United States population aged 50 years or older.
One advantage of working with an organization such as the CDC is its credibility and connections to individuals and organizations that can increase program effectiveness. For example, Katie Couric, NBC Today Show host, and Academy Award-winning actor Morgan Freeman have served as spokespersons for different campaigns.
Given that chronic sleep loss and sleep disorders are a major public health problem, a public and professional campaign on sleep conditions would fit in well with existing CDC mission and programs.
PUBLIC EDUCATION
Sleep loss and daytime sleepiness affect 30 to 40 percent of the general population (Hossain and Shapiro, 2002); however, millions of individuals suffering from sleep disorders remain undiagnosed and untreated. For example, 80 to 90 percent of obstructive sleep apnea cases remain undiagnosed, which increases the burden of this disorder (Young et al., 1997; Kapur et al., 2002). Most large-scale public health education programs and campaigns to date have focused primarily on diet and exercise and have not included adequate information about sleep. However, the time is right for the development of a sleep campaign. There is a beginning public awareness of the importance of sleep owing to recent articles in the popular press and television programs. Two concurrent strategies are required to increase awareness among the general public: a multimedia public education and awareness campaign, and improved education and training programs to increase awareness among health care professionals.
National Sleep Public Education and Awareness Campaign
Considering the burden that chronic sleep loss and sleep disorders have on all age groups, a multifocal campaign is required to improve awareness among children, adolescents, adults, elderly people, and high-risk populations. The primary role of a campaign would be to improve recognition of the health and economic benefits of proper sleep, as well as educating parents and adults of the consequences associated with not receiving adequate
sleep. In this regard it will be important to inform the public and policy makers of the negative consequences of chronic sleep loss and sleep disorders. The campaign could argue that by taking specific personal actions to improve sleep hygiene, by recommending specific behaviors for all age groups, the adverse health and economic consequences could be reduced.
The need for such a campaign rests on the following assumptions:
-
The general public does not recognize the prevalence of, or the consequence associated with chronic sleep loss and/or sleep disorders.
-
Most health care providers neither recognize the prevalence of, nor the many risks associated with, chronic sleep loss and/or sleep disorders.
-
Many of the technological advances made in the previous century (e.g., television, Internet) serve to deprive people, especially children and adolescents, of needed sleep.
-
Sleep loss and sleep disorders are associated with numerous other health complications
-
Increased understanding will lead to better sleep behaviors and thus improved health and function.
Treatment of sleep problems, even if only behavioral and educational in nature, has the potential to increase an individual’s well-being and productivity. Such a campaign would offer new information to both the general population and health care providers. In addition, the activities of a broad sleep awareness campaign could be linked to all stakeholders— government agencies, private industry, foundations, professional societies, patient advocacy organizations, educators, colleges and universities, and community organizations.
The committee envisions that wherever possible, a national campaign would coordinate activities with local needs and provide for the tailoring of its messages for different communities, including specific age groups, minority groups, and shift workers. In addition, the committee envisions that the campaign should be developed in coordination with the NCSDR, CDC, the proposed National Somnology and Sleep Medicine Research and Clinical Network (see Chapter 8), the Department of Transportation, the Department of Labor, the Department of Education, other relevant federal departments and agencies, with input from private organizations such as the NSF and the AASM. Rigorous evaluation is a critical component. Further, this campaign could be integrated and coordinated with other public health campaigns, including those on obesity and heart disease, with the purpose of increasing the awareness among all Americans of the importance of sleep and the adverse health and social consequences of poor sleep. Further, reinforcing messages should be provided in diverse media and effectively coordinated with other events and dissemination activities.
In proposing the National Sleep Public Education and Awareness Campaign, this committee considered and recognized the associated costs and challenges. These include the following:
-
Educating and convincing leaders in the public health field that the health and economic burden associated with chronic sleep loss and sleep disorders requires a national campaign.
-
The expenses associated with developing and operating a large nationwide public education and awareness program.
-
Coordinating federal, state, and local government agencies that would be involved in a campaign.
-
Coordinating the activities of foundations, professional societies, and private companies.
-
The large number of individuals experiencing sleep loss or sleep disorders span all age groups, each of which will require a specific strategy.
In summary, although evidence is limited, previously coordinated health education campaigns demonstrate the potential value of efforts designed to increase the awareness of both the prevalence and consequences of chronic sleep loss and sleep disorders. For example, broad coordinated national campaigns such as the NHLBI’s National High Blood Pressure Campaign (Roccella, 2002), the National Institute of Child Health and Human Development’s (NICHD) Back to Sleep Campaign, the CDC’s Screen for Life colorectal cancer campaign, the antitobacco efforts of the late 1960s and early 1970s and the late 1990s and early 2000s (Warner, 1981; Siegel, 2002), and the antidrug campaigns of the middle 1980s (IOM, 2002) have had corresponding reductions in risky behavior.
Back to Sleep Campaign
The Back to Sleep program offers an example of a very successful public education awareness campaign that arose from a strong associative discovery between infant sleeping position and the risk of sudden infant death syndrome (SIDS) (Willinger, 1995; Kemp et al., 1998). In 1993, the American Academy of Pediatrics released its first policy statement on reducing the risk of SIDS that recommended that infants be placed on their backs while sleeping. The following year, the NICHD spearheaded the Back to Sleep campaign. Cosponsors included the Maternal and Child Health Bureau, the American Academy of Pediatrics, the SIDS Alliance, and the Association of SIDS and Infant Mortality Programs. The NCSDR was involved in planning and developing communication materials for the campaign.
Before it was instituted, the death rate for SIDS was approximately 1.3 per 1,000 live births (CDC, 1996). Postsurveillance analysis showed a 50 percent reduction in SIDS rates since the Back to Sleep campaign began (NICHD, 2003). The campaign increased public awareness of SIDS risks and safety through a series of radio and television public service announcements and distribution of more than 20 million pieces of literature to health care professionals and the public.
National High Blood Pressure Education Campaign
Another successful public education program is the National High Blood Pressure Education Program. It was established by the NHLBI in 1972 “to reduce death and disability related to high blood pressure through programs of professional, patient, and public education” (NHLBI, 2005a). The NHLBI coordinates a group of federal agencies, voluntary and professional organizations, state health departments, and numerous community-based programs. At the core of the education activities is the program’s coordinating committee, which follows a consensus-building process to identify major issues of concern and to develop program activities. Each representative from the coordinating committee member organizations work together to provide program guidance and to develop and promote educational activities through their own constituencies. The National High Blood Pressure Education Program is responsible for the five following areas: information collection and dissemination; public, patient, and professional education; community program development; evaluation and data analysis; and technology transfer and electronic distribution of materials.
The education campaign does not depend greatly on advertising, but rather relies heavily on actions by other institutions: campaign organizers working with physicians’ organizations to encourage physicians to provide advice about high blood pressure consistent with national guidelines; proposing stories to newspapers and television and radio that convey the priority messages; and developing affiliations with, and providing materials to, grassroots organizations interested in hypertension (Roccella, 2002). When the program began there was very little awareness and treatment for hypertension. Less than one-fourth of the American population understood the relationship between hypertension and stroke and hypertension and heart disease and only 31 percent sought treatment. Today, more than three-fourths of the population recognizes that relationship and over 53 percent seek treatment (NHLBI, 2005a).
Recommendation 5.1: The National Center on Sleep Disorders Research and the Centers for Disease Control and Prevention should establish a multimedia public education campaign.
The National Center on Sleep Disorders Research—working with the Centers for Disease Control and Prevention, the proposed National Somnology and Sleep Medicine Research Network, private organizations and foundations, entertainment and news media, and private industry—should develop, implement, and evaluate a long-term national multimedia and public awareness campaign directed to targeted segments of the population (e.g., children, their parents, and teachers in preschool and elementary school; adolescents; college students and young adults; middle-aged adults; and elderly people) and specific high-risk populations (e.g., minorities).
To implement this recommendation, the following should be done:
-
This campaign should be developed in coordination with appropriate federal departments and agencies and with input from independent experts to focus on building support for policy changes.
-
This campaign should be built upon and integrated within existing public health campaigns, including those focused on diet and exercise (e.g., obesity and heart disease).
-
Reinforcing messages disseminated through multiple media should be effectively coordinated with events targeting providers of health information such as physicians, nurses, and teachers.
PROFESSIONAL TRAINING AND AWARENESS IS REQUIRED
Societal misperceptions also stem from a lack of professional knowledge about the benefits and impact of sleep. Therefore, the success of the proposed National Sleep Public Education Awareness Campaign particularly relies on increased awareness and more sleep-oriented curricula for the health care providers. Further, underutilization of sleep centers in the United States to assist in diagnosing and treating sleep disorders partly stems from both the lack of public and professional awareness and insufficient training of primary caregivers (Wyatt, 2004). Without widespread recognition of the importance of sleep on the part of both the public and health care providers, society is at significant risk for sleep-related health problems. If health care providers are unaware of the symptoms and problems that occur as a result of compromised sleep, they simply will not pursue the topic with patients. Thus, patient contacts with the health care system are often major sources of “missed opportunities” to diagnose sleep problems and share important information about sleep. In addition, increasing the aware-
ness of health care providers also offers an opportunity to attract health care professionals into the field (see Chapter 7 for detailed discussion). Those who receive sleep-related education are more likely to ask individuals about past or current sleep problems (Haponik and Camp, 1994).
Some progress is being made in developing strategies to improve education and awareness among health care professionals. For example, competency-based goals and teaching strategies for sleep and chronobiology in undergraduate medical education have recently been proposed (Harding and Berner, 2002; Federman, 2003). Similar curricula content has also been developed for undergraduate and graduate nursing programs (Lee et al., 2004). A survey conducted in 1992 revealed that minimal, if any, didactic content on sleep was included in medical and nursing programs (Buysse et al., 2003; Rosen et al., 1998; NHLBI, 2003a). Although curricula in medical and nursing school have been updated since 1992, and there are no recent surveys, anecdotal evidence suggests that sleep-related content is still not adequately addressed. Considerable progress remains to be made.
Treatment of Sleep Disorders Requires Interdisciplinary Training
Sleep disorders vary widely in their complexity, their comorbidities, the risks they represent, and the scope of their manifestations (Chapter 3). They may be a symptom of a behavioral or social change, a secondary manifestation associated with a primary disease, or may be the primary problem. Examination of the disorders associated with each of these categories demonstrates the requirement for educated multidisciplinary health care specialists who have the capacity to recognize, diagnose, and treat chronic sleep loss and sleep disorders. At minimum, there are 13 different health care specialties and subspecialties that are involved in diagnosis and treatment—anesthesiology, cardiology, dentistry, endocrinology, immunology, neurology, nursing, nutrition, otolaryngology, pediatrics, psychiatry, psychology, and pulmonology. For example, individuals with obstructive sleep apnea (OSA) typically require recognition by a primary care physician, and diagnosis and treatment from a sleep specialist who is a pulmonologist, neurologist, psychiatrist, or otolaryngologist. Following, or concurrent with, diagnosis and treatment, the chronic nature of a sleep disorder also may require being seen by a specialist (e.g., endocrinologist for diabetes and obesity, cardiologist for hypertension). Patient and family education, primary care, follow-up and support are often provided by nurses with expertise in the field. Therefore, proper treatment of chronic sleep loss and sleep disorders requires multidisciplinary care. However, as discussed below, there has been very little education of health care professionals about the pathology, etiology, or treatment of chronic sleep loss and sleep disorders.
Undergraduate Sleep-Related Education
Education at the undergraduate level provides a unique opportunity to share important health information when readiness to learn has transcended adolescent levels. It also provides an important opportunity to expose students to the topics and potentially increase the number of individuals interested in this area of medicine. In fact, curricula that include sleep-related material at the undergraduate level may be particularly appropriate and effective for a number of reasons.
First, leaving home to attend college is often the first time that young adults are totally responsible for self-care. Numerous studies have demonstrated that one of the most common difficulties undergrads experience is sleep disturbance. For example, in a survey of 191 college students, most reported that they had developed some form of sleep disturbance (Buboltz et al., 2001). Further, a recent study of 964 undergraduate residence hall students found that sleep problems were among the list of significant predictors of stress (Dusselier et al., 2005). A study of 1,300 students in the United States Military Academy found that incoming cadets were significantly sleep deprived, receiving only about 4 hours and 50 minutes of sleep per night during the week in their first fall semester (Miller and Shattuck, 2005). The reasons for the high prevalence of these sleep problems in undergraduate students are likely related to a variety of factors including poor sleep hygiene, stress associated with changes in lifestyle, study demands, socializing, use of stimulants, and in some cases a feeling of the need to demonstrate mental and physical toughness.
Undergraduates also experience the consequences of poor sleep habits and require the necessary health information to make appropriate lifestyle changes. Earlier studies demonstrated that students’ poor sleep quality was associated with increased tension, irritability, depression, confusion, and lower life satisfaction as well as increases use of marijuana and alcohol (Pilcher et al., 1997). In addition, poor sleep has been associated with impaired academic performance and deficits in learning and memory (Lack, 1986; Gais et al., 2000; Stickgold et al., 2000; Walker et al., 2003; Fenn et al., 2003). Unfortunately, many students who experience academic problems do not realize that poor sleep may be a crucial contributing factor (Buboltz et al., 2001).
Chronic Sleep Loss and Sleep Disorders Awareness Programs for Undergraduates
Although some sleep-related public health educational activities have been developed (see previous section), their impact appears to be minimal. Thus, new ways to incorporate sleep education into undergraduate student
life are needed. First and foremost, university administrators need to recognize and acknowledge that students’ sleep habits and problems are an important component of campus life. Including content regarding sleep in orientation programs, even in the form of a simple informational flier, may provide a forum for further discussions in other types of programs and activities. Advisors might ask basic questions regarding overall sleep patterns and make recommendations regarding class times that are more compatible with a student’s normal sleep patterns. Further, university and college administrators should examine how campus and community environments, such as activities, schedules, sports, and work routines, contribute to sleep disruption (Buboltz et al., 2001) and encourage academic departments to educate their faculty regarding the sleep-related problems of students (Miller and Shattuck, 2005). In addition, awareness campaigns should be developed to target undergraduate students in dormitories and academic health centers. Similar effective programs have been developed for public health campaigns concerning sexually transmitted disease, alcohol abuse, nutrition, and suicide. For example, the American College Athletic Association and the National Association of Student Personnel Administrators have helped design and integrate a number of public health campaigns for college students, such as the Health Education and Leadership Program.
Undergraduate Somnology and Sleep Medicine Curriculum Development
Colleges and universities can both educate students and stimulate interest in the field by making simple cost-effective changes in curriculum. For example, at the United States Military Academy, the general psychology course that is taken by all freshmen now includes information on acute and chronic sleep loss (Miller and Shattuck, 2005). Numerous other types of freshman courses, such as general health, biology, and sports education, might include similar content and easily incorporate it with other health-related information such as nutrition, alcohol and drug abuse, and suicide prevention (Miller and Shattuck, 2005). Offering an elective course, perhaps in collaboration with an academic sleep center, might also help recruit future clinicians and scientists to the field. Curriculum recommendations for both nursing and undergraduate medical students have recently been proposed (Strohl et al., 2003; Lee et al., 2004). Other types of novel activities might include the following:
-
Develop undergraduate research experiences in sleep to increase the interactions of these students with graduate students in this area (Box 5-1).
-
Develop sleep consortiums among two or more universities and educational programs that could be shared using advanced technology, as the
|
BOX 5-1 Summer Sleep and Chronobiology Research Apprenticeship The Summer Sleep and Chronobiology Research Apprenticeship is a unique undergraduate training program in the behavioral sciences at Brown University, which fosters behavioral science research education primarily for undergraduate students, but also for young pre- and post-doctoral scientists. The program provides undergraduate students an intensive research and academic experience in a human sleep and chronobiology research laboratory. It spans 13 weeks, including 2.5 weeks of intensive laboratory skills training, a week attending the annual meeting of the sleep professional societies (APSS), and a 10-week research apprenticeship in an ongoing study of sleep and circadian rhythms in adolescents. The program also supports one or two graduate student teaching assistants, providing role models to the apprentices, additional teaching experience, time for research projects, and full summer stipend. Each year the program concludes with a 2-day “retreat” colloquium. At this retreat, every apprentice is responsible for preparing and presenting a brief talk at the APSS meeting on a research theme they began to examine and researched through the summer. The National Institute of Mental Health (NIMH) should be commended for funding the training program for 8 years. This brought an unprecedented level of fiscal stability, focus, and opportunity for young trainees. Unfortunately, the NIMH no longer supports undergraduate training programs. The Trans-NIH Sleep Research Coordinating Committee should be encouraged to continue to support similar undergraduate mentorship programs. Because the program is largely designed for undergraduate students, its success is somewhat difficult to measure. Not every student has gone on to behavioral science research; some are in medicine, others in such disparate fields as law or business. Others, however, have followed the route to graduate study. One former student is working with a noted sleep and chronobiology scientist. Another student is performing research on sleep in birds. A third is a graduate student in neurobiology using electroencephalograms (EEG) and magnetic resource imaging (MRI) as methods to investigate the relationship between thalamic activation and cortical activation during sleep spindles. Another individual recently received a young investigator award from the European Sleep Research Society (2004, Prague ESRS meeting) for research on adolescent sleep patterns. |
-
numbers of faculty qualified to teach information about sleep may be limited in particular settings.
Students in the clinical health science majors, such as those in nursing and premedicine, should have didactic and associated clinical work in sleep medicine that include specific content in the following:
-
Interactions between sleep and health.
-
The neurobiology and functions of sleep.
-
Effects of restricted or reduced sleep on pathophysiology of diseases.
-
Mechanisms that lead to sleep disorders across the life span and across genders.
-
Normal sleep processes across ages, genders, and socioeconomic groups.
-
Effective sleep interventions for sleep disorders (Strohl et al., 2003).
GRADUATE RESEARCH TRAINING IN SOMNOLOGY AND SLEEP DISORDERS
Graduate school is traditionally a time of focused concentration on a specific area of investigation, and the curricular requirements for graduate degrees in biological sciences are typically highly variable among disciplines, programs, and universities. Exposure to research on sleep-related topics is probably most applicable to interdisciplinary programs in neuroscience, as well as to single-discipline programs (e.g., pharmacology, physiology, biochemistry, anatomy, and cell biology). Although the content of these curricula typically depend on the research interests of the local faculty, it is in the interest of the students to have a broad exposure to neuroscience that is usually accomplished via a graduate level survey course in the field, and for that course, or other relevant courses, to include some exposure to sleep-related research. Although there are limited data, it appears that this exposure does not occur. For example, one of the top neuroscience and sleep programs, the neuroscience graduate course in the health sciences and technology program at Harvard University and Massachusetts Institute of Technology, includes only a single lecture on the molecular biology of circadian rhythms and no exposure to sleep-related research (personal communication, C.B. Saper, Harvard University, December 1, 2005).
OVERVIEW OF MEDICAL SCHOOL SOMNOLOGY EDUCATION
The inadequacy of somnology education in medical curricula has been a long-standing issue. As far back as 1978, a survey by the American Sleep Disorders Association (now the AASM) revealed that 46 percent of medical
schools provided no sleep-related education and 38 percent sponsored minimal instruction (Orr et al., 1980). Although the percentage of medical schools that include sleep disorders in their curricula has risen modestly from 54 percent in 1978 (Orr et al., 1980) to 63 percent in 1993, the time devoted averages only 2.11 hours (Rosen et al., 1998). Eighty-nine percent of medical students never performed a clinical evaluation of an individual with a sleep disorder (Rosen et al., 1993).
The situation has slowly improved. A survey performed by a special subcommittee of the AASM, called Taskforce 2000, in 1995 indicated a growth in time devoted to somnology content to 4 hours in the preclinical basic sciences and 2 hours in the clinical clerkships (Rosen et al., 1998). However, structured learning experience in the sleep laboratory and clinical evaluation of individuals with sleep disorder remain limited. Major barriers continue to be lack of time in the medical curriculum, the need for better resources and teaching facilities, and the need for leadership and effective advocacy.
Barriers to Implementation of Sleep-Related Medical Curriculum
Efforts to enhance the training and education in somnology and sleep medicine at all levels of medical education continue to face important challenges. These include the following:
-
Somnology and sleep medicine is still a relatively new field, cutting across many traditional disciplinary boundaries. Therefore, there is a need to implement a cohesive, interdisciplinary, and centrally organized sleep medicine curriculum.
-
The importance of sleep to good health is often poorly appreciated; hence, it is underrepresented in the medical curriculum.
-
Somnology and sleep medicine is a budding interdisciplinary field; sleep and circadian rhythms interact and influence nearly every organ system. A coordinated curriculum that includes content related to somnology and sleep disorders is needed in every related teaching block.
-
Limited availability of faculty and mentors with appropriate scientific and clinical expertise creates a need for “content champions” to push the educational agenda in a centrally organized way.
-
A paucity of local educational resources, including clinical infrastructure, exists (Orr et al., 1980; Rosen et al., 1993, 1998; Owens, 2005). As described below, the NIH and AASM have contributed significant resources to the development and establishment of somnology medicine curricula in the past. However, there has been limited evaluation of these efforts.
Sleep Academic Award
From 1996 to 2003 the NCSDR and the NHLBI cosponsored the Sleep Academic Award program. Its primary objective was to develop and evaluate model curricula in somnology and sleep medicine for adaptation into academic institutions. In tandem with curricular development, the Sleep Academic Award program also sought to promote interdisciplinary learning environments and faculty development in somnology and sleep medicine. The model curriculum for medical schools encompassed these four basic core competencies:
-
Explain the nature and causation of sleep.
-
Discuss the impact of sleep and circadian disorders.
-
Perform a sleep history.
-
Initiate measures to improve sleep and to reduce sleepiness.
Other Sleep Academic Award professional education initiatives included the addition of sleep questions to board examinations in psychiatry, pediatrics, otolaryngology, and pulmonary medicine; the creation of a sleep clinical case vignette bank for use in objective structured clinical examinations and problem-based learning seminars; the development of continuing medical education lectures and courses; and the implementation of faculty development workshops.
The Sleep Academic Award program also undertook initiatives in graduate medical training related to the effects of sleep loss and fatigue. These initiatives included collaboration with the American Medical Association and the Accreditation Council for Graduate Medical Education (ACGME) on work hours for residents. The MedSleep dissemination initiative distributes educational resources and products for free, including web-based materials, slide sets, videotaped case histories, and curriculum outlines (AASM, 2005). In addition, the AASM Medical Education Committee has established a network of sleep-related education advocates in over 100 of the nation’s medical schools to continue the development and implementation of educational materials and to provide evaluation.
Effectiveness of the Sleep Academic Award Program
Although the overall impact and durability of Sleep Academic Award program initiatives have not been measured, they have provided time and money for academic career development in somnology (research and scholarship), training in educational methodology, opportunity for mentorship, and access to leadership positions in professional organizations. Similarly, the durability of institutional impact, while difficult to predict precisely, has
included: provision of teaching, educational support, and materials; increases in the knowledge base of graduates; research opportunities; and engagement of multiple disciplines in somnology and sleep medicine education.
Several empirical studies regarding somnology medical education supported by the Sleep Academic Award program have been published in a special section of the January 2005 edition of Sleep Medicine. These studies have shown the following:
-
The efficacy of a pediatric screening tool (the BEARS) to increase the amount of sleep information recorded in primary health care settings (Owens and Dalzell, 2005).
-
The development and validation of a tool (the Dartmouth Sleep Knowledge and Attitude Survey) in assessing outcomes of educational interventions in sleep medicine (Sateia et al., 2005).
-
The impact of education in improving the recognition of sleep disorders in a community-based setting (Zozula et al., 2005).
-
The positive impact of lecture and case-based discussion on the performance of medical students in an objective structured clinical examination (Papp and Strohl, 2005).
-
The use of the objective structured clinical examination for sleep medicine to gain access to the medical school curriculum by providing objective structured clinical examinations on sleep problems such as obstructive sleep apnea and chronic insomnia (Rosen et al., 2005).
One important outcome of the Sleep Academic Award has been an improvement in the number of somnology and sleep disorders questions on board exams; however, the representation is still low, given the public health burden. For example, the content outline of the board exam for internal medicine indicates zero to two sleep-related questions. The American Board of Otolaryngology lists corrective sleep surgery as 1 of 22 surgical concepts that is covered in the exam, where surgical concepts represents 15 percent of the exam content (American Board of Otolaryngology, 2006). The American Board of Psychiatry and Neurology mentions somnology and sleep disorders as 1 of 20 areas covered in the exam’s physiology section—physiology also constitutes 15 percent of the exam (American Board of Psychiatry and Neurology, 2006). The content specifications for the American Board of Pediatrics mentions somnology and sleep disorders 19 times (American Board of Pediatrics, 2006).
Nurses as Care Managers
Another key group of health care providers that could play an especially significant role in advocating healthy sleep and promoting the diag-
nosis and management of sleep problems are nurses—the largest number of health care providers in the United States. Nurses are in a unique position to contribute to new knowledge about sleep and health promotion, provide primary care, as well as monitor sleep habits and disseminate information to patients, and enhance patient compliance with treatment (Lee et al., 2004). Unfortunately, nursing education faces many of the same challenges as other health care provider educational programs regarding the incorporation of sufficient sleep content in its programs. Recently, curriculum recommendations for somnology and chronobiology education for nursing at the undergraduate and graduate level programs have been developed (Lee et al., 2004). These guidelines have been integrated into a limited number of nursing programs; however, greater integration of sleep-related material is required in nursing education programs.
OVERVIEW OF SOMNOLOGY IN MEDICAL RESIDENCY TRAINING CURRICULA
To ensure a high degree of recognition and the most effective clinical care, it is important that more training programs educate residents about the need for early detection and, whenever possible, the prevention of chronic sleep loss and sleep disorders. Primary care providers are largely responsible for this surveillance in the medical system. Therefore, it is imperative that internists, family medicine doctors, and pediatricians are sufficiently trained to assume the surveillance role. As many individuals are referred to pulmonologists, neurologists, psychiatrists, and otolaryngologists for disorders that are related to sleep problems, extensive training in sleep medicine also should be integrated into those program curricula.
The current ACGME program requirements for residency training in internal medicine, family medicine, pediatrics, and psychiatry do not mention chronic sleep loss or sleep disorders. Program requirements for residency in neurology list sleep disorders as one of 22 subjects to be addressed in seminars and conferences. However, except for residency programs in otolaryngology, none of the other four residency program requirements address clinical experiences in sleep medicine (ACGME, 2005a).
Curricula should be designed to ensure that knowledge and skills required to detect the broad range of sleep disorders and to manage those that are not complex should be a component of general competency in each of the five relevant specialty areas of medicine. General competency in somnology and sleep medicine should be certified and recertified by the respective boards of the American Board of Medical Specialties (ABMS). With guidance from the residency review committee of the ACGME, each training program in these five specialty areas must develop curriculum content for somnology and sleep medicine. Departments sponsoring these train-
ing programs have a responsibility to have in place, or alternatively, to identify faculty-level expertise in somnology and sleep medicine, and ensure availability of these individuals for learners in the residency training program. As a result of the multidisciplinary nature of sleep medicine, interdepartmental sharing of expertise for training should be required in many settings. Clinical experience with diagnosis and management of patients with sleep disorders is preferred to didactic experiences. For this reason, the presence of an institutional sleep disorders clinic, laboratory, or center should be a key component of the educational infrastructure. Exposure of residents to the multidisciplinary nature of sleep evaluation and treatment will best prepare them for roles as primary caregivers, particularly for identification, treatment of simple sleep problems, and triage of more complicated patients to appropriate subspecialists.
Residents should become aware of the general health consequences of sleep disorders, such as the relationship between sleep deprivation and obesity, cardiovascular disease, and behavioral disorders. In addition, subspecialists in internal medicine and pediatric prevention, diagnosis, and treatment should be fully familiar with the sleep-related consequences of chronic disease and incorporate this awareness into their practices and subspecialty fellow training. Providing generalists with sleep-related education would enable them to be competent to care for a substantial number of sleep problems and refer individuals to sleep specialists as needed.
In view of the workforce shortage in the field (see Chapter 7) and the small number of both training programs and individuals enrolled in somnology and or sleep medicine training programs (see below), exposure of residents to this area of medicine will enhance awareness of career opportunities in this discipline and improve clinical care. Thus, the goal of embedding somnology and sleep medicine exposure and experiences in core residency training is to prepare a wide range of individuals to participate as frontline caregivers, and also to ensure that somnology and sleep medicine is visible to learners early in their training process and possibly foster their consideration of somnology or sleep medicine as a career focus. Exposure of residents to discovery and translational research related to sleep medicine might also enhance the attractiveness of the field. Therefore, somnology and sleep medicine investigators should participate, wherever possible, in the residency training process.
OVERVIEW OF SLEEP MEDICINE FELLOWSHIP TRAINING
AASM-Accredited Fellowship Training Programs
Until recently fellowship training programs in sleep medicine were rare, with a small number of academic institutions, hospitals, and other facilities
hosting programs that were not standardized. To address this, a formal accreditation program for fellowship training programs in sleep medicine was established by the AASM. The number of fellowships has grown progressively, particularly over the last decade. There are now 53 fellowship training programs (Table 5-1). Reflecting the multidisciplinary roots of sleep medicine, these training programs are housed in various departments within these institutions.
TABLE 5-1 Accredited Programs for Fellowship Training in Somnology and Sleep Medicine
|
Date Accredited |
Name of Institution |
Department Affiliation |
|
1980 |
Stanford University |
Psychiatry and Behavioral Sciences |
|
1989 |
Center for the Study of Sleep and Waking |
Psychiatry and Behavioral Sciences |
|
1991 |
Detroit Veterans Affairs Medicinal Center |
Neurology |
|
1991 |
Henry Ford Hospital |
Pulmonary Division |
|
1992 |
Mount Sinai Sleep Disorders Center |
Pulmonary Division |
|
1993 |
Michael S. Aldrich Sleep Disorders Laboratory |
Neurology and Psychiatry |
|
1993 |
Newark Beth Israel Sleep Disorders Center |
Department of Pulmonary Medicine |
|
1993 |
University of Pittsburgh School of Medicine |
Psychiatry and Medicine, Pulmonary Division |
|
1994 |
Cleveland Clinic Foundation |
Neurology |
|
1995 |
Mayo Sleep Disorders Center |
Pulmonary and Critical Care |
|
1996 |
Rush University Medical Center |
Departments of Psychology and Medicine |
|
1997 |
Wayne State University |
Pulmonary Division |
|
1998 |
University of Kentucky |
Internal Medicine |
|
1998 |
University of Mississippi Medical Center |
Psychiatry |
|
1998 |
Intermountain Sleep Disorders Center |
Pulmonary Division |
|
1999 |
Children’s Memorial Hospital |
Pediatrics |
|
2000 |
Brigham and Women’s Hospital |
Medicine |
|
2000 |
Duke University Medical Center |
Pulmonary, Clinical Neurology, and Clinical Neuropatholgy |
|
Date Accredited |
Name of Institution |
Department Affiliation |
|
2001 |
Sleep Medicine and Circadian Biology Program/ Indiana University School of Medicine |
Pulmonary, Allergy, Critical Care, and Occupational Medicine |
|
2001 |
State University of New York at Buffalo School of Medicine |
Medicine |
|
2001 |
University of Nebraska Medical Center |
Pulmonary Critical Care Section of the Department of Internal Medicine |
|
2001 |
Rush University Medical Center |
Department of Psychology |
|
2001 |
Northwestern University Medical School |
Department of Neurology |
|
2001 |
Worcester Medical Center Campus at St. Vincent Hospital |
Department of Neurology |
|
2001 |
Scott and White Memorial Hospital and Clinic |
Department of Pulmonary/Critical Care |
|
2001 |
Lahey Clinic |
Pulmonology |
|
2001 |
University of Pennsylvania |
Pulmonary, Critical Care, and Sleep Section |
|
2001 |
Case Western Reserve University |
Departments of Medicine, Pediatrics, and Neurology |
|
2002 |
Southwestern Medical Center |
Department of Psychiatry |
|
2002 |
Seton Hall University School of Graduate Medical Education |
|
|
2002 |
St. Elizabeth’s Medical Center |
Pulmonary Division, Department of Medicine |
|
2002 |
Long Island Jewish Medical Center |
Department of Medicine |
|
2002 |
New Mexico Center for Sleep Medicine |
|
|
2002 |
University of Iowa Hospitals and Clinics Sleep Disorder Center |
Neurology |
|
2002 |
Hackensack University Medical Center Institute of Sleep-Wake Disorders |
|
|
2002 |
Dartmouth Hitchcock Medical Center |
Department of Psychiatry |
|
2003 |
Mayo Clinic/Mayo Graduate School of Medicine, Jacksonville |
Division of Education Services |
|
2003 |
Johns Hopkins University Sleep Disorders Center |
Pulmonary/Critical Care |
|
Date Accredited |
Name of Institution |
Department Affiliation |
|
2003 |
Tulane University Health Science Center |
Comprehensive Sleep Medicine Center |
|
2003 |
Wake Forest University Health Sciences |
Department of Psychiatry |
|
2003 |
Beth Israel Deaconess Medical Center |
Department of Neurology |
|
2003 |
Beth Israel Deaconess Medical Center |
Division of Pulmonary, Critical Care, Sleep Medicine |
|
2003 |
University of Texas Health Science Center, Houston |
Division of Pulmonary, Critical Care, Sleep Medicine |
|
2003 |
Center for Sleep Disorders at Johnson City Medical Center |
Pulmonary/Critical Care/Internal Medicine |
|
2003 |
University of Wisconsin-Madison |
Department of Medicine |
|
2003 |
Clinilabs, Inc. (Sleep Disorders Institute) |
|
|
2003 |
State University of New York at Buffalo |
Department of Neurology |
|
2004 |
St. Mary’s Medical Center/Ultimate Health Services |
Regional Sleep Center |
|
2004 |
University of Washington |
Medicine and Neurology |
|
2004 |
Norwalk Hospital Sleep Disorders Center |
Department of Medicine |
|
2004 |
Temple University Health System Sleep Disorders Center |
Department of Internal Medicine, Division of Pulmonary and Critical Care |
|
2004 |
Washington University School of Medicine |
Department of Neurology |
|
2004 |
University of Louisville/Kosair Children’s Hospital |
Department of Pediatrics |
|
SOURCE: Personal communication, J. Barrett, AASM, December 12, 2005. |
||
With the complex nature of sleep medicine in mind, the guidelines for accreditation allowed programs to design fellowship training in two ways. The first design allowed for the sleep medicine fellowship to be a minimum of 12 months of training in comprehensive sleep medicine that could be done during or after specialty fellowship training. The second design allowed for the sleep medicine fellowship to be of a combined nature, in
which a substantial portion of the sleep medicine training is embedded within the primary specialty training.
The guidelines for accreditation of fellowship training required that programs provide graduates with clinical, technical, and research experience that promotes sound clinical judgment and a high level of knowledge about the diagnosis, treatment, and prevention of sleep disorders. The guidelines emphasized education in specific content areas, including basic neurological sleep mechanisms; chronobiological mechanisms; cardiovascular, pulmonary, endocrine, and gastrointestinal sleep physiology; specific disorders of sleep; and the psychopharmacology of sleep, as well as the operation of polysomnographic equipment, polysomnographic interpretation, and troubleshooting.
Eligibility requirements for an accredited program include at least one year of training preceded by the completion of an accredited residency program, and sponsorship by an institution that meets fellowship training requirements set forth by the ACGME. The director of the program must be a physician who is a diplomate of the American Board of Sleep Medicine (ABSM), and the program has to be associated with a sleep disorders center accredited by the AASM.
Completion of training in an accredited program satisfies requirements for eligibility to sit for the sleep medicine certification examination administered by the ABSM.
ACGME Sleep Medicine Fellowship Training Programs
In 2002, the AASM submitted an application to ACGME for accreditation of fellowship training programs in sleep medicine. ACGME approved the program requirements for sleep medicine fellowship training programs in June 2004. Accreditation of fellowship training programs by the ACGME now provides a framework for the continued expansion of specialized clinical training in sleep medicine and draws greater attention to the necessity of training programs.
The ACGME fellowship requires 1 year of clinical sleep medicine. Trainees can enter the sleep medicine fellowship if they have been trained in one of the following: general internal medicine (3 years of postgraduate training); neurology (4 years of postgraduate training); psychiatry (4 years of postgraduate training); general pediatrics (3 years of postgraduate training); otolaryngology (5 years of postgraduate training).
In June 2004, ACGME convened a Sleep Medicine Working Group to develop requirements for fellowship training in sleep medicine and formalize the accreditation process. The working group created a comprehensive program guideline that included requirements to ensure competence in core areas, including facility and resources for training, faculty, assignment of
rotation and duty, curriculum, program content, and clinical experience (ACGME, 2005b). The first round of program accreditation was effective July 1, 2005, and 25 programs have received accreditation from ACGME for fellowship training.
DEMONSTRATION OF KNOWLEDGE: BOARD CERTIFICATION
ABSM Certification
In response to increasing recognition and awareness of the importance of sleep and sleep disorders, professional certification in sleep medicine has been administered for physicians and practitioners to demonstrate skill and competence.
The American Sleep Disorders Association (now the AASM) in 1978 established an examination committee. That same year, the committee held the inaugural clinical polysomnography examination; 21 candidates passed the exam. Each year the examination committee received an increasing number of applications, which led to discussions regarding the future of certification. In 1989, the AASM voted to create an independent entity, and in 1991 the ABSM was incorporated and assumed all the activities and responsibilities of the former examination committee.
The ABSM is an independent nonprofit organization and has a board of directors that oversees all aspects of exam administration and governance. The ABSM was self-designated and was not recognized by the ABMS.
Until 2005, the ABSM certification examination consisted of two parts. The part I examination consisted of multiple choice questions covering the basic sciences of sleep, clinical sleep medicine, and interpretation of polysomnogram fragments and other material. Part II was computer-based and consisted of a series of clinical cases with partial polysomnograms, Multiple Sleep Latency Tests, and other relevant data, with candidates typing short answers to questions. The ABSM decided to fuse the two parts of the examination in 2005 and offer a single-day, one-part examination that incorporates the format of both former parts.
Eligibility for the examination is dependent on a candidate fulfilling five requirements as well as possessing acceptable experience in the evaluation of sleep disorders patients. These eligibility requirements ensure adequate and proper education and training—either through an accredited fellowship program or through a combination of training and experience—and competency evaluation through certification of a primary board. Professionals from other clinical disciplines, such as doctoral psychologists and nurses who met all criteria, were also eligible to sit for the examination.
Over the past 14 years, the ABSM certification examination has developed a strong reputation in the medical community and experienced tre-
mendous growth in terms of applicants. The number of candidates applying for the certification examination as well as the number of diplomates (Figure 5-1) has increased dramatically each year; however, as will be discussed in detail in Chapter 6, the capacity is still not sufficient to diagnose and treat all individuals with sleep disorders.
Establishment of the ABMS in Sleep Medicine
Despite its growth in reputation and numbers of diplomates, it became evident by the late 1990s that the ABSM as a freestanding board would not be recognized as fully legitimate by organized medicine. Because sleep medicine requires only 1 year of postresidency fellowship training, the ABSM was ineligible to join the ABMS as an independent board.
In 2002, the ABSM met with several specialty societies and professional organizations to discuss the necessity for certification examination in sleep medicine and the best design for such an examination. A consensus plan was developed for the establishment of a new subspecialty examination in sleep medicine to be jointly offered by the American Board of Internal Medicine, the American Board of Psychiatry and Neurology, and the American Board of Pediatrics; the American Board of Otolaryngology joined later as a sponsoring board. Following further successful negotiations, a plan for this examination was submitted to the ABMS in early 2004. In March 2005, the ABMS announced approval of the certification examination in sleep medicine. A specific time frame for the new examination has not been set; it is expected, however, that the first examination cycle will begin in 2007.
There are three pathways that qualify physicians to sit for the new examination: (1) certification by one of the primary sponsoring boards and
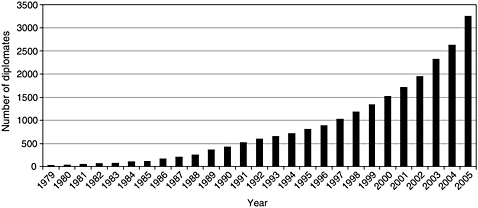
FIGURE 5-1 Total number of diplomates of the ABSM (1979–2005).
SOURCE: Personal communication, J. Barrett, AASM, December 15, 2005.
the current ABSM; (2) certification by one of the primary sponsoring boards and completion of training in a 1-year sleep medicine fellowship program, not overlapping with any other residency or fellowship; and (3) clinical practice experience. This clinical practice experience pathway may consist of a 5-year “grandfathering” period open to physicians who are board certified in one of the sponsoring specialty boards and who can attest that he or she has the equivalent of 1 year of clinical practice experience in sleep medicine during the prior 5 years. This experience could, for example, be gained by an individual practitioner who has devoted one-third of his or her practice to sleep medicine over 3 years. Physicians in the clinical practice pathway will also have to attest to a specified minimum number of patients seen and polysomnograms and Multiple Sleep Latency Tests read. At the end of this initial 5-year period, the only route to board eligibility will be through an ACGME accredited fellowship training program. This creates a one-time, unprecedented opportunity for pulmonologists, neurologists, otolaryngologists, psychiatrists, and other physicians already working in the field to sit for the board examination. However, not all sleep clinicians will be eligible for this accreditation. The ACGME only permits accreditation of doctors, thus nurses, dentists, and doctorally prepared sleep specialists (e.g. psychologists and behavioral health specialists) in other fields are no longer eligible to sit for the examination. As a consequence, there is the potential that in the future particular bodies of knowledge will not be represented in sleep medicine.
Representatives from all four boards are developing and setting standards for the new examination. The American Board of Internal Medicine has administrative responsibility for examination development, and the participating/sponsoring boards have responsibility for setting admission criteria for their own diplomates. These standards and criteria are expected to be announced in 2006.
Although this new structure is based on sleep medicine becoming recognized as an independent specialty, it is too early to tell how well this new approach will work in developing the needed workforce of practitioners for sleep medicine and the next generation of physician-scientists. The fellowship is somewhat unusual in that there is only the requirement for 1 year of training beyond completion of residency. It is unclear whether pulmonologists, who have until now formed the majority of the clinical workforce in sleep medicine (60 percent of diplomates in 2005), will continue to be attracted to the field (Figure 5-2). Clinical requirements for pulmonary medicine involve 18 months of training beyond residency. It appears that this will not count to training in sleep medicine even though there is now a defined curriculum for sleep medicine in pulmonary medicine (American Thoracic Society, 2005) and 10 to 15 percent of the board examination for pulmonary medicine is about sleep disorders. An additional clinical year of train-
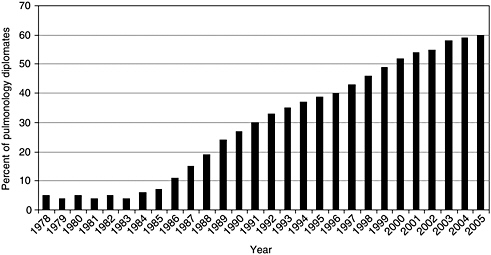
FIGURE 5-2 Percent of pulmonology diplomates of ABSM.
SOURCE: Personal communication, J. Barrett, AASM, December 15, 2006.
ing above and beyond that for pulmonary medicine may represent a barrier to pulmonologists entering this discipline. It is hoped that this issue is addressed, as pulmonologists encompass a significant percentage of the clinical workforce of practitioners in sleep medicine.
Another area of uncertainty is funding for these new sleep fellowships. Previously, when the fellowship was not ACGME-approved, fellows could obtain reimbursements for their clinical activities, including sleep study interpretation. In some other programs, sleep medicine training was incorporated into multiyear research training supported by training grants from the National Institutes of Health (NIH). Neither of these options is available in the new format.
Unfortunately, the rules introduced by the ACGME are not flexible and require 1 complete year of clinical training even in programs that are multi-year and committed to research training. This may have a negative impact on the already fragile pipeline of physician-scientists in this new discipline as outlined elsewhere in this report (see Chapter 7). As described in detail in Chapter 8, the committee encourages the proposed Type II comprehensive academic sleep centers to incorporate research training into their sleep medicine fellowships, while for Type III centers this is considered an essential component.
A final potential limitation of this new examination structure is that it is open exclusively to physicians. Other clinician scientists in fields such as psychology, neuroscience, and nursing will not be eligible to sit for the examination as was the case in prior years. Currently, there are 154 ABSM
PhDs board-certified by the AASM (personal communication, J. Barrett, AASM, January 13, 2006). Excluding these individuals may have an important negative effect on patient access, interdisciplinary nature of sleep programs, and the decision of talented potential scientists and clinicians to pursue the study of somnology.
NEXT STEPS
Medical, nursing, and pharmacy students along with individuals in graduate training, residency, and fellowship training programs require greater exposure to the public health burden of sleep loss and disorders; they also must understand the relationship between sleep problems and the proper diagnosis and treatment of a wide range of medical problems throughout an individual’s life span. Although the data are limited, they suggest that focused training about sleep can positively influence the performance of medical students (Haponik and Camp, 1994), residents (Owens and Dalzell, 2005), physicians (Haponik et al., 1996; Rosen et al., 2005; Papp and Strohl, 2005), and primary care clinical staff (Zozula et al., 2005). For example, interns who had previous instruction about sleep-related material often asked patients about past or current sleep problems (82 percent of the time), while sleep histories were rarely obtained by interns who did not have any previous instruction (13 percent of the time) (Haponik et al., 1996).
The challenges that lie ahead, outlined below, are many:
-
Sustaining educational initiatives begun by the Sleep Academic Award program.
-
Monitoring progress and developing new and updated educational materials, such as sleep objective structured clinical examinations.
-
Coordinating efforts across institutions.
-
Identifying remaining gaps by assessing the impact of sleep education on physician knowledge, skills, and attitudes; clinical practice; and public health.
-
Assessing the relative value and effectiveness of sleep curricula that are integrated across other areas versus those that are stand-alone units.
-
Developing means of credentialing nurses, psychologists, and other clinicians who will not qualify for American Board of Medical Specialties certification.
-
Integrating sleep-related content into continuing education requirements.
To these ends, educational outcomes research grants and partnerships with appropriate medical subspecialty groups for development and dissemi-
nation of educational programs is essential. Further, many health care-related programs are actively embracing new technologies for teaching (e.g., computer simulations of office practices) that provide an opportunity to ensure that sleep-related materials are incorporated into evolving curricula.
Most important, however, somnology health care providers need to be engaged in curriculum development and implementation. This will enable more effective curricular time and resources necessary for addressing basic educational goals in sleep disorders medicine and for integrating sleep materials into other academic areas. A coordinated curriculum—one that is not departmentally based—offers many advantages to encouraging more rational allocation of time and resources to critical areas of public health, including sleep and its disorders (Reynolds et al., 1995). This could be critical to a new integrative approach to teaching and learning about somnology and sleep disorders for the rest of the medical curriculum.
Recommendation 5.2: Academic health centers should integrate the teaching of somnology and sleep medicine into baccalaureate and doctoral health sciences programs, as well as residency and fellowship training and continuing professional development programs.
The subjects of sleep loss and sleep disorders should be included in the curricula of relevant baccalaureate and graduate educational and research programs of all the health sciences. Similarly, postgraduate, residency, and fellowship training programs, as well as continuing professional development programs, must include this content. The curriculum should expose students in the fields of medicine and allied health fields to the etiology, pathophysiology, diagnosis, treatment, prevention, and public health burden of sleep loss and sleep disorders. Relevant accrediting bodies and licensing boards ought to define sleep-related curriculum requirements and expectations for knowledge and competency (e.g., Liaison Committee on Medical Education, Accreditation Council for Graduate Medical Education, American Board of Medical Specialties, the National League for Nursing, the Commission on Collegiate Nursing Education, and the Council on Education for Public Health). Further, a means for credentialing nonphysicians should be maintained by the American Board of Sleep Medicine, or new mechanisms should be developed by relevant organizations.
DATA SYSTEMS FOR SURVEYING SLEEP AND SLEEP DISORDERS
Adequate public health education not only requires informing public and health care practitioners, but also adequate monitoring of the public health burden. The development of adequate surveillance and monitoring systems is important for informing policy makers, health care providers, researchers, and the public about the effectiveness of health care services, programs, and policies. However, there is currently very little ongoing nationwide surveillance. A number of existing national and statewide databases that can be used for surveillance and monitoring of disease burden in the United States population are available. The CDC manages and coordinates many of the large national surveys. Two of these databases, the National Health and Nutrition Examination Survey (NHANES) and the National Health Interview Survey (NHIS), have readily available information relevant to chronic sleep patterns and sleep disorders. Other data systems would need to add new components that incorporate sleep-related measures to be of use to researchers in the field. However, not only is it important for new criteria to be added to surveillance and monitoring systems, but researchers must also be encouraged to make use of these datasets.
National Center for Health Statistics
The National Center for Health Statistics (NCHS) is one of the centers of the CDC, and its primary goal is to monitor health trends throughout the nation and to guide actions and policies to improve the health of Americans. The NCHS has permanent surveillance systems of health and disease outcomes (e.g., vital statistics); it also conducts permanently ongoing nationwide studies and surveys. In addition, it conducts special studies as need arises (e.g., supplemental components to national surveys on a limited time basis). As described below, data relevant to sleep research are currently available from some of these systems, but the possibility of additional data collection to fill current knowledge gaps should be carefully considered.
There are a number of major health statistics sources in the United States, stratified according to the local, state, and national nature of their frame. Some sources are purely national (e.g., NHANES, the National Health Care Survey, and the Medical Expenditure Panel Survey); others are state (e.g., Behavioral Risk Factor Surveillance System, the State and Local Area Integrated Telephone Survey) or local (e.g., the National Immunization Survey); yet, the frame for other sources span across all levels of government (e.g., vital statistics, Medicare, and Medicaid).
National Health and Nutrition Examination Survey (NHANES)
Since 1959, a series of health examination surveys of the United States population have been conducted by the CDC and the NCHS. NHANES protocol is designed to monitor the health and nutritional status of Americans. In 1999 NHANES was changed from a periodic survey to an annual survey with public data files released in 2-year periods to protect confidentiality and increase statistical reliability. As in previous national health examination surveys, participants are interviewed in their homes followed by a complete health examination, part of which includes biological specimen collection. The examinations are conducted in a mobile examination center. Each mobile examination center consists of four interconnected specially designed trailers, which house biomedical equipment and laboratory capabilities. An examination team composed of 16 specially trained health professionals and support staff, including a licensed dentist, physician, interviewers, health technicians, and an x-ray technician, operates each mobile examination center.
NHANES monitors the prevalence of diseases and risk factors, nutritional habits and anthropometry status, growth and development, and environmental exposures. Because of its cyclical nature, in addition to its core components, NHANES temporarily adds components (either additional questionnaires or exam procedures). Starting in 2005, and scheduled to end in 2008, a sleep section was added to the household questionnaire. This was done with cosponsorship from the NHLBI and targeted participants in the survey older than 16 years. The NHANES sleep questionnaire is based on instruments previously used in epidemiological studies and includes questions on sleep habits as well as questions on functional outcomes of sleep disorders (Table 5-2).
National Health Interview Survey
The NHIS is the core survey of the Department of Health and Human Services, and since its establishment in 1957 it has been the principal source of information on the health of the civilian noninstitutionalized population of the United States (excluding patients in long-term care facilities, Armed Forces personnel on active duty, and U.S. nationals living abroad). Its main objective is to monitor the health of the U.S. population through the collection and analysis of data on a broad range of health topics. It is designed as a cross-sectional household interview continuously running throughout each year. The current sampling plan was redesigned in 1995, and it is based on a multistage area probability sample that permits the selection of a nationwide representative sample of households on a weekly basis. Approximately 43,000 households (including about 106,000 persons) are successfully re-
TABLE 5-2 NHANES Sleep Questionnaire, 2005–2008
|
How often do you experience: |
|
Trouble falling asleep |
|
Wake up during night/difficulty getting back to sleep |
|
Wake up too early/difficulty getting back to sleep |
|
Feel unrested during the day |
|
Feel excessively sleepy during the day |
|
Do not get enough sleep |
|
Take sleeping pills |
|
Nasal stuffiness, etc., at night |
|
Leg cramps and leg jerks |
|
Have you ever been told you have a sleep disorder? |
|
What sleep disorder? |
|
Sleep apnea? |
|
Insomnia? |
|
Restless legs syndrome? |
|
Have you ever snored? |
|
How long does it take for you to fall asleep? |
|
Do you have difficulty carrying out following activities because you are too tired or sleepy: |
|
Concentrating |
|
Remembering |
|
Working on a hobby |
|
Performing employed or volunteer work |
|
Operating a motor vehicle |
cruited each year. Since 1995, both African American and Hispanic persons are oversampled, and samples are drawn for each state.
The core content of the survey questionnaire (the “basic module”) remains largely unchanged from year to year, thus allowing for trend analyses and for data from more than 1 year to be pooled to increase sample size for analytical purposes. However, survey content is updated every 10 to 15 years. The latest significant revision was put in place in 1997. It includes the Family Core, the Sample Adult Core, and the Sample Child Core. The Family Core includes information on household composition, sociodemographic characteristics, information for matches to administrative databases, and basic indicators of health status and utilization of health care services; it is the sampling frame for additional integrated surveys such as the Medical Expenditure Panel Survey (see below). From each family, one sample adult and one sample child (if any) are randomly selected and given the corresponding core interviews that cover the individual’s health status, disability, health behaviors, use of health care services, and immunizations. In addition to the Basic Module, the NHIS includes a Periodic Module and a Topical Module that contain supplemental sections to respond to new public health data needs as they arise.
The NHIS has only one question related to sleep: “On average how many hours of sleep do you get a night (24-hour period)?”. This question was included in the supplemental surveys administered in 1977, 1985, and 1990, and was added to the core survey in 2004. Based on these data, the percentage of adults who reported sleeping 6 hours or less jumped from approximately 20 percent of the population in 1985 (Schoenborn, 1986) to 25 percent in 2004 (National Center for Health Statistics, National Health Interview Survey, 2004) across all age groups.
One important feature of the NHIS is its use as a sampling frame for other national surveys such as the National Survey of Family Growth and the Medical Expenditure Panel Survey. Because of its relevance for this report, the latter is described in more detail below.
Vital Statistics and the National Death Index
Vital statistics include data on all births and deaths. The latter are based on information contained in the death certificate and include identifying information (name and social security number), demographic data, and data on underlying and contributing causes of death. NCHS’s National Death Index is a resource available to investigators seeking information surrounding the death of individual participants in prospective cohort studies. This is useful for investigators exploring the association between sleep disorders identified in study participants and risk of mortality from certain causes (e.g., cardiovascular, disease, hypertension, depressive disorders, and injuries). It also provides the opportunity to conduct aggregate analyses of distribution and trends of mortality directly attributable to sleep problems.
National Health Care Survey
The National Health Care Survey is a collection of health care provider surveys that obtains information about the facilities that supply health care, the services rendered, and the characteristics of the patients served (Table 5-3). Each survey is based on a multistage sampling design that includes health care facilities or providers and patient records. Data are collected directly from the establishments and/or their records, rather than from the patients. The participating surveys identify health care events—such as hospitalizations, surgeries, and long-term stays—and offer the most accurate and detailed data on diagnosis and treatment, as well as on the characteristics of the institutions. These data are used by policy makers, planners, researchers, and others in the health community to monitor changes in the use of health care resources, to monitor specific diseases, and to examine the impact of new medical technologies, to mention a few.
TABLE 5-3 Surveys Included in the National Health Care Survey’s System
|
National Ambulatory Medical Care Survey |
|
National Employer Health Insurance Survey |
|
National Health Provider Inventory |
|
National Home and Hospice Care Survey |
|
National Hospital Ambulatory Medical Care Survey |
|
National Hospital Discharge Survey |
|
National Nursing Home Survey |
|
National Survey of Ambulatory Surgery |
Two of the participating surveys are of particular relevance for the study of health care resources utilization in relation to sleep disorders: the National Ambulatory Medical Care Survey and the National Hospital Discharge Survey.
The National Ambulatory Medical Care Survey
The National Ambulatory Medical Care Survey, which has been conducted annually since 1989, is a national survey designed to meet the need for objective, reliable information about the provision and use of ambulatory medical care services in the United States. Findings are based on a sample of visits to non-federally employed office-based physicians who are primarily engaged in direct patient care. Specially trained interviewers visit the physicians prior to their participation in the survey in order to provide them with survey materials and instruct them on how to complete the forms. Data collection from the physician, rather than from the patient, provides an analytic base that expands information on ambulatory care collected through other NCHS surveys. Each physician is randomly assigned to a 1-week reporting period. During this period, data for a systematic random sample of visits are recorded by the physician or office staff on an encounter form provided for that purpose. Data are obtained on patients’ symptoms, physicians’ diagnoses, and medications ordered or provided. The survey also provides statistics on the demographic characteristics of patients and services provided, including information on diagnostic procedures, patient management, and planned future treatment.
The National Hospital Discharge Survey
The National Hospital Discharge Survey (NHDS), which has been conducted annually since 1965, is a national probability survey designed to provide information on characteristics of inpatients discharged from non-
federal short-stay hospitals in the United States. The NHDS collects data from a sample of approximately 270,000 inpatient records acquired from a national sample of about 500 hospitals. Only hospitals with an average length of stay of fewer than 30 days for all patients, general hospitals, or children’s general hospitals are included in the survey. However, the NHDS excludes data from a number of hospitals, including federal, military, and Veterans Affairs (VA) hospitals; hospital units of institutions (such as prison hospitals); and hospitals with fewer than six beds staffed for patient use. The data includes information related to the personal characteristics of the patient—age, sex, race, ethnicity, marital status, expected sources of payment, and diagnoses and procedures coded to the International Classification of Diseases, 9th Revision, Clinical Modification. It also includes administrative items such as admission and discharge dates (which allow calculation of length of stay). Annually, data from the NHDS are made available to the public. As an example of the amount of data available in this survey, the estimated number of all listed sleep disorders diagnoses in NHDS in 2003 was 322,000. Although the NHDS excludes information obtained through VA hospitals, there is a similar database provided by the VA that has been used to examine the association of psychiatric disorders and sleep apnea (Sharafkhaneh et al., 2005).
Data from these surveys could be used to monitor prevalence of complaints related to sleep disorders; trends in sleep-related diagnosis and services; characteristics of patients, characteristics of health care providers; use of medical technology and how use differs according to region or patients’ access to care; emergence of alternative care sites; and medication use in ambulatory care settings.
Behavioral Risk Factor Surveillance System
Funded by CDC, the Behavioral Risk Factor Surveillance System complements the NCHS national surveys by providing state-specific data on prevalence of the major behavioral risks among adults associated with premature morbidity and mortality. The main objective is to collect data on actual behaviors, rather than on attitudes or knowledge, that would be especially useful for planning, initiating, supporting, and evaluating health promotion and disease prevention programs at the state and local levels.
The Behavioral Risk Factor Surveillance System is an annual telephone survey (based on random digit dialing) in each participating state. The telephone surveys methodology was chosen not only because of cost advantages but also because telephone surveys were considered especially desirable at the state and local level, where the necessary expertise and resources for conducting area probability sampling for in-person household interviews were not likely to be available.
The survey started in 1984 with 15 participating states. By 1994, all states, the District of Columbia, and three territories were participating. Although the survey was designed to collect state-level data, a number of states from the outset stratified their samples to allow them to estimate prevalence for regions within their respective states. The CDC developed a standard core questionnaire for states to use to provide data that could be compared across states.
The emergence of telemarketing and increasing use of mobile phones and automatic answering systems resulted in dwindling response rates over the last few years. However it remains as the only state-specific source of health-related data nationwide. There are currently no sleep-related questions in Behavioral Risk Factor Surveillance System.
Medical Expenditure Panel Survey
Funded by the Agency for Healthcare Research and Quality, the Medical Expenditure Panel Survey is a national probability survey designed to continually provide policy makers, health care administrators, businesses, and others with timely, comprehensive information about health care use and costs in the United States, and to improve the accuracy of their economic projections. The survey began in 1977 and comprises three component surveys: the Household Component, the Medical Provider Component, and the Insurance Component. The Household Component provides a variety of measures of health status, health insurance coverage, health care use and expenditures, and sources of payment for health services. The Medical Provider Component covers hospitals, physicians, and home health care providers and is meant to estimate the expenses of people enrolled in health maintenance organizations and other types of managed care plans. Finally the Insurance Component is used to analyze the behavior and choices made with respect to health care use and spending, as well as the amount, types, and costs of health insurance available to Americans through their workplace.
Medicare Current Beneficiary Survey
Funded by Centers for Medicare and Medicaid Services, the Medicare Current Beneficiary Survey is a continuous, multipurpose survey of a nationally representative sample of aged, disabled, and institutionalized Medicare beneficiaries. The Medicare Current Beneficiary Survey is the only comprehensive source of information on the health status, health care use and expenditures, health insurance coverage, and socioeconomic and demographic characteristics of the entire spectrum of Medicare beneficiaries. The purpose of the survey is to determine expenditures and sources of payment
for all services used by Medicare beneficiaries; to establish all types of health insurance coverage and relate coverage to sources of payment; and to trace changes over time, such as health status, and the impacts of programmatic changes. It includes survey data on measures of health status and access to care that are linked to the physicians and hospital claims data. The survey was initiated in 1991 and is designed to support both cross-sectional and longitudinal analysis. Data are collected through interviews that take place over 4-month intervals. Each interview includes questions regarding the household composition; an accounting of the individual’s health insurance coverage; a review of an individual’s health care utilization in the period since the last interview; details about each type of service, provider characteristics, and medicines prescribed; and a detailed account of charges and payments associated with these health care events. The interview data are linked to Medicare claims.
Youth Risk and Behavior Survey
The Youth Risk Behavior Surveillance System includes national, state, and local school-based surveys of representative samples of 9th- through 12th-grade students (National Center for Chronic Disease Prevention and Health Promotion, 2005). These surveys are conducted every 2 years, usually during the spring semester. The national survey, conducted by CDC, provides data representative of high school students in public and private schools in the United States. The state and local surveys, conducted by departments of health and education, provide data representative of the state or local school district. The Risk Behavior Surveillance System was developed in 1990 to monitor priority health risk behaviors that contribute markedly to the leading causes of death, disability, and social problems among youth and adults in the United States. These behaviors, often established during childhood and early adolescence, include: tobacco use, dietary behaviors, physical activity, alcohol and other drug use, sexual behaviors, and behaviors that contribute to unintentional injuries and violence. Despite the importance of sleep deprivation and other sleep disorders in young adolescents (see Chapter 3), no questions on sleep and sleep behaviors have ever been included in the survey.
Process for Inclusion of New Components in Surveys
One impediment for the addition of greater sleep-related content in surveillance and monitoring instruments is the process required to have new components added. In addition to a high standard of scientific merit, inclusion of new components also often requires specific sponsorship. The
following is a description of the criteria for adding components or questions to NHANES. Other surveys and monitoring instruments have similar requirements.
Criteria for Adding Components to NHANES
Criteria for adding components or questions to NHANES and the NHIS are based on scientific merit, public health importance, costs, sponsorship, lead time, feasibility and logistics in the context of the rest of the survey components, priority ranking in relation to competing components, and survey burden.
NHANES runs in 2-year cycles and is governed by an internal committee formed by NCHS leadership, epidemiologists, statisticians, and physicians. Every 2 years, this committee requests proposals for adding components to the upcoming 2-year cycle, including both questionnaire components and mobile examination center exams. Proposals are received through a competitive bidding process and are expected to include detailed rationale for the public health relevance of the proposal, eligibility criteria (e.g., age, gender eligibility), detailed estimates of costs, personnel needs, amount of time required to do the exam, needs for laboratory or other type of equipment, statistical power estimates, quality assurance/quality control procedures, and the availability of external funds to subsidize the additional component. The committee then makes a preliminary determination as to its suitability before it reviews the proposal. Proposals under consideration are then examined by a team of NCHS personnel and proponents to carefully study and work out all the details and logistics of the implementation of the new exam.
New components to the exam are typically introduced for a single 2-year cycle, sometimes for multiple cycles (e.g., the sleep questionnaire is introduced for two cycles from 2005 to 2008). Eventually components are rotated off when sufficient data and sample size are acquired; some exams may be rescheduled at a later date in order to monitor changes and trends overtime. Other NCHS surveys follow similar procedures for review of added components with a few differences.
Both public and private organizations are eligible to propose new components to add to the NHANES and other NCHS surveys. Federal, state, or local government agencies can provide funds to the NCHS to cofinance the costs of the proposed additions. For example, the sleep questions on NHANES are sponsored by the NHLBI. Nonprofit organizations and private companies can also make proposals but cannot provide funds to the NCHS; cosponsorship from private industry, however, can occur through money deposited in the CDC foundation.
Recommendation 5.3: The Centers for Disease Control and Prevention and National Center on Sleep Disorders Research should support additional surveillance and monitoring of sleep patterns and sleep disorders.
The Centers for Disease Control and Prevention, working with the National Center on Sleep Disorders Research, should support the development and expansion of adequate surveillance and monitoring instruments designed to examine the American population’s sleep patterns and the prevalence and health outcomes associated with sleep disorders.
REFERENCES
AASM (American Academy of Sleep Medicine). 2005. MedSleep. [Online]. Available: http://www.aasmnet.org/MedSleep_Home.aspx [accessed December 17, 2005].
ACGME (Accreditation Council of Graduate Medical Education). 2005a. Program Requirements for Residency Education in Neurology. [Online]. Available: http://www.acgme.org/acWebsite/downloads/RRC_progReq/180pr105.pdf [accessed March 22, 2006].
ACGME. 2005b. Residency Review Committees for Sleep Medicine. [Online]. Available: http://www.acgme.org/acWebsite/downloads/RRC_PIF/520pif2_0405.doc [accessed December 16, 2005].
American Board of Otolaryngology. 2006. Otolaryngology Training Exam. [Online]. Available: http://www.aboto.org/blueprint.pdf [accessed January 10, 2006].
American Board of Pediatrics. 2006. General Pediatrics Examination. [Online]. Available: http://www.abp.org/ [accessed January 10, 2006].
American Board of Psychiatry and Neurology. 2006. Psychiatry and Neurology Examination. [Online]. Available: http://www.abpn.com/certification/neuro-neuro_items.html [accessed January 10, 2006].
American Thoracic Society. 2005. Curriculum and competency assessment tools for sleep disorders in pulmonary fellowship training programs. American Journal of Respiratory and Critical Care Medicine 172(3):391–397.
Banno K, Kryger MH. 2004. Factors limiting access to services for sleep apnea patients. Sleep Medicine Reviews 8(4):253–255.
Buboltz WC, Brown F, Soper B. 2001. Sleep habits and patterns of college students: A preliminary study. Journal of the American College of Health 50(3):131–135.
Buysse DJ, Barzansky B, Dinges D, Hogan E, Hunt CE, Owens J, Rosekind M, Rosen R, Simon F, Veasey S, Wiest F. 2003. Sleep, fatigue, and medical training: Setting an agenda for optimal learning and patient care. Sleep 26(2):218–225.
CDC (Centers for Disease Control and Prevention). 1996. Sudden Infant Death Syndrome— United States, 1983-1994. [Online]. Available: http://www.cdc.gov/mmwr/preview/mmwrhtml/00043987.htm [accessed November 29, 2005].
CDC. 2006. Physical Activity for Everyone. [Online]. Available: http://www.cdc.gov/nccdphp/dnpa/physical/index.htm [accessed January 6, 2006].
Culpepper L. 2002. Generalized anxiety disorder in primary care: Emerging issues in management and treatment. Journal of Clinical Psychiatry 63(suppl 8):35–42.
Dahl RE, Holttum J, Trubnick L. 1994. A clinical picture of child and adolescent narcolepsy. Journal of the American Academy of Child and Adolescent Psychiatry 33(6):834–841.
Dement WC, Vaughn C. 1999. The Promise of Sleep: The Scientific Connection Between Health, Happiness, and a Good Nights Sleep. London: Macmillian.
Dusselier L, Dunn B, Wang Y, Shelley MC II, Whalen DF. 2005. Personal, health, academic, and environmental predictors of stress for residence hall students. Journal of the American College of Health 54(1):15–24.
Dzaja A, Arber S, Hislop J, Kerkhofs M, Kopp C, Pollmacher T, Polo-Kantola P, Skene DJ, Stenuit P, Tobler I, Porkka-Heiskanen T. 2005. Women’s sleep in health and disease. Journal of Psychiatric Research 39(1):55–76.
Engstrom CA, Strohl RA, Rose L, Lewandowski L, Stefanek ME. 1999. Sleep alterations in cancer patients. Cancer Nursing 22(2):143–148.
Falvo D. 2005. Medical and Psychosocial Aspects of Chronic Illness and Disability. 3rd ed. Sudbury, MA: Jones and Bartlett.
Federman DD. 2003. Competency-based goals for sleep and chronobiology in undergraduate medical education. Sleep 26(3):251.
Fenn KM, Nusbaum HC, Margoliash D. 2003. Consolidation during sleep of perceptual learning of spoken language. Nature 425(6958):614–616.
Gais S, Plihal W, Wagner U, Born J. 2000. Early sleep triggers memory for early visual discrimination skills. Nature Neuroscience 3(12):1335–1339.
Guilleminault C, Pelayo R. 1998. Narcolepsy in prepubertal children. Annals of Neurology 43(1):135–142.
Haponik E, Camp G. 1994. I snored: A simple sleep history for clinicians. American Journal of Respiratory and Critical Care Medicine 149(A53).
Haponik EF, Frye AW, Richards B, Wymer A, Hinds A, Pearce K, McCall V, Konen J. 1996. Sleep history is neglected diagnostic information. Challenges for primary care physicians. Journal of General Internal Medicine 11(12):759–761.
Harding SM, Berner ES. 2002. Developing an action plan for integrating sleep topics into the medical school curriculum. Sleep and Breathing 6(4):155–160.
Hossain JL, Shapiro CM. 2002. The prevalence, cost implications, and management of sleep disorders: An overview. Sleep and Breathing 6(2):85–102.
IOM (Institute of Medicine). 2002. Speaking of Health: Assessing Health Communication Strategies for Diverse Populations. Washington, DC: The National Academies Press.
Kapur V, Strohl KP, Redline S, Iber C, O’Connor G, Nieto J. 2002. Underdiagnosis of sleep apnea syndrome in U.S. communities. Sleep and Breathing 6(2):49–54.
Kemp JS, Livne M, White DK, Arfken CL. 1998. Softness and potential to cause rebreathing: Differences in bedding used by infants at high and low risk for sudden infant death syndrome. Journal of Pediatrics 132(2):234–239.
Lack LC. 1986. Delayed sleep and sleep loss in university students. Journal of the American College of Health 35(3):105–110.
Lee KA, Landis C, Chasens ER, Dowling G, Merritt S, Parker KP, Redeker N, Richards KC, Rogers AE, Shaver JF, Umlauf MG, Weaver TE. 2004. Sleep and chronobiology: Recommendations for nursing education. Nursing Outlook 52(3):126–133.
Meadows R. 2005. The “Negotiated Night:” An Embodied Conceptual Framework for the Sociological Study of Sleep. Oxford: Blackwell.
Mehlman M. 2001. Employee/employer interactions and responsibilities with special reference to genetically related sleep disorders. Sleep and Breathing 5(3):153–161.
Miller NL, Shattuck LG. 2005. Sleep patterns of young men and women enrolled at the United States Military Academy: Results from year 1 of a 4-year longitudinal study. Sleep 28(7):837–841.
Moore PJ, Adler NE, Williams DR, Jackson JS. 2002. Socioeconomic status and health: The role of sleep. Psychosomatic Medicine 64(2):337–344.
National Center for Chronic Disease Prevention and Health Promotion. 2005. YRBSS: Youth Risk Behavior Surveillance System. [Online]. Available: http://www.cdc.gov/HealthyYouth/yrbs/index.htm [accessed December 18, 2005].
National Center for Health Statistics, National Health Interview Survey. 2004. Percentage of Adults Who Reported an Average of <6 Hours of Sleep per 24-Hour Period, by Sex and Age Group. [Online]. Available: http://www.cdc.gov/mmwr/preview/mmwrhtml/mm5437a7.htm [accessed November 14, 2005].
NHLBI (National Heart, Lung, and Blood Institute). 2003a. National Sleep Disorders Research Plan, 2003. Bethesda, MD: National Institutes of Health.
NHLBI. 2003b. Sleep, Sleep Disorders, and Biological Rhythms: NIH Curriculum Supplement Series, Grades 9-12. Colorado Springs, CO: Biological Sciences Curriculum Study.
NHLBI. 2004. Be a Star Sleep (Student and Teacher Guide Supplement). New York: Time, Inc.
NHLBI. 2005a. National High Blood Pressure Education Program. [Online]. Available: http://www.nhlbi.nih.gov/about/nhbpep/nhbp_pd.htm [accessed November 22, 2005].
NHLBI. 2005b. Garfield Star Sleeper. [Online]. Available: http://www.nhlbi.nih.gov/health/public/sleep/starslp/ [accessed December, 2005].
NHLBI. 2006. Your Guide to Healthy Sleep. [Online]. Available: http://www.nhlbi.nih.gov/health/public/sleep/healthy_sleep.htm [accessed May 27, 2006].
NICHD (National Institute of Child Health and Human Development). 2003. SIDS rate and sleep position 1998-2003. [Online]. Available: http://www.nichd.nih.gov/sids/SIDS_rate_backsleep_03.pdf [accessed November 18, 2005].
Orr WC, Stahl ML, Dement WC, Reddington D. 1980. Physician education in sleep disorders. Journal of Medical Education 55(4):367–369.
Owens J. 2005. Introduction to special section: NIH Sleep Academic Award program. Sleep Medicine 6(1):45–46.
Owens JA, Dalzell V. 2005. Use of the “BEARS” sleep screening tool in a pediatric residents’ continuity clinic: A pilot study. Sleep Medicine 6(1):63–69.
Papp KK, Strohl KP. 2005. The effects of an intervention to teach medical students about obstructive sleep apnea. Sleep Medicine 6(1):71–73.
Pilcher JJ, Ginter DR, Sadowsky B. 1997. Sleep quality versus sleep quantity: Relationships between sleep and measures of health, well-being and sleepiness in college students. Journal of Psychosomatic Research 42(6):583–596.
Punjabi NM, Bandeen-Roche K, Young T. 2003. Predictors of objective sleep tendency in the general population. Sleep 26(6):678–683.
Reynolds CF III, Adler S, Kanter SL, Horn JP, Harvey J, Bernier GM Jr. 1995. The undergraduate medical curriculum: Centralized versus departmentalized. Academy of Medicine 70(8):671–675.
Roccella E. 2002. The contributions of public health education toward reduction of cardiovascular disease mortality: Experiences from the National High Blood Pressure Education Program. In: Hornik R, ed. Public Health Communication: Evidence for Behavior Change. Mahwah, NJ: Lawrence Erlbaum. Pp. 73–84.
Rosen GM, Harris I, Mahowald MW. 2005. Objective structured clinical examinations (OSCE) for sleep. Sleep Medicine 6(1):75–80.
Rosen RC, Rosekind M, Rosevear C, Cole WE, Dement WC. 1993. Physician education in sleep and sleep disorders: A national survey of U.S. medical schools. Sleep 16(3):249–254.
Rosen R, Mahowald M, Chesson A, Doghramji K, Goldberg R, Moline M, Millman R, Zammit G, Mark B, Dement W. 1998. The Taskforce 2000 Survey on Medical Education in Sleep and Sleep Disorders. Sleep 21(3):235–238.
Sateia MJ, Reed VA, Christian JG. 2005. The Dartmouth Sleep Knowledge and Attitude Survey: Development and validation. Sleep Medicine 6(1):47–54.
Schoenborn CA. 1986. Health habits of U.S. adults, 1985: the “Alameda 7” revisited. Public Health Report 101(6):571–580.
Sharafkhaneh A, Giray N, Richardson P, Young T, Hirshkowitz M. 2005. Association of psychiatric disorders and sleep apnea in a large cohort. Sleep 28(11):1405–1411.
Siegel M. 2002. The effectiveness of state-level tobacco control interventions: A review of program implementation and behavioral outcomes. Annual Review of Public Health 23:45–71.
Stickgold R, James L, Hobson JA. 2000. Visual discrimination learning requires sleep after training. Nature Neuroscience 3(12):1237–1238.
Strohl KP, Veasey S, Harding S, Skatrud J, Berger HA, Papp KK, Dunagan D, Guilleminault C. 2003. Competency-based goals for sleep and chronobiology in undergraduate medical education. Sleep 26(3):333–336.
Taylor B. 1993. Unconsciousness and society: The sociology of sleep. International Journal of Politics, Culture, and Society 6(3):463–474.
U.S. Congress, Senate. 1993. National Institutes of Health Revitalization Act of 1993. 103rd Cong., S.104:285b-7.
Walker MP, Brakefield T, Hobson JA, Stickgold R. 2003. Dissociable stages of human memory consolidation and reconsolidation. Nature 425(6958):616–620.
Warner KE. 1981. Cigarette smoking in the 1970s: The impact of the antismoking campaign on consumption. Science 211(4483):729–731.
Williams SJ. 2002. Sleep and health: Sociological reflections on the dormant society. Health (N Y) 6(2):173–200.
Willinger M. 1995. SIDS prevention. Pediatric Annals 24(7):358–364.
Wyatt JK. 2004. Delayed sleep phase syndrome: Pathophysiology and treatment options. Sleep 27(6):1195–1203.
Zozula R, Rosen RC, Jahn EG. 2005. Recognition of sleep disorders in a community-based setting following an educational intervention. Sleep Medicine 6(1):55–61.












































