5
Technology and Communications
Daniel Conway is a 65-year-old male who has a sudden onset of excruciating back pain. He calls his primary caregiver, Dr. Thompson, who tells him to call an ambulance to bring him to the Eastern Hospital emergency department (ED).
Dr. Thompson clicks on a Web page for the Eastern Hospital Emergency call-in program. He imports his last progress note with Mr. Conway’s history and adds a personal note describing his concerns that the patient’s uncontrolled hypertension could have led to a ruptured abdominal aortic aneurysm.
The ED immediately receives the on-line submission and begins preparations for the patient’s arrival while the ambulance is still en route. Paramedics, using interoperable communications systems that give them equal capability to communicate with fire and police agencies on one hand and hospitals on the other, inform the ED that Mr. Conway’s vital signs are stable but he is in severe pain. The emergency physician advises them to administer a dose of intravenous morphine and carefully monitor his blood pressure, oxygenation, and respiratory rate. Upon arrival, Mr. Conway is rapidly transported to a preassigned room, where the emergency physician, Dr. Hendricks, and his team are waiting. While the nurses take his vital signs and the doctor examines him, a clerk arrives at the bedside with a wireless laptop. After the initial evaluation, she collects the information necessary to register him in the system without delay. The paramedics complete their run report on
a tablet computer and use the wireless network to beam it into the hospital databases.
Mr. Conway is in too much pain to recall all of his medications accurately. Dr. Hendricks queries a clinical data-sharing network, which compiles a list from the computerized records of local pharmacies. The doctor has a question about which would be the best diagnostic test to order given the specifics of Mr. Conway’s history. He consults the hospital’s digital library, and with several mouse clicks he confirms that a computer-assisted tomography (CAT) scan is still the expert-recommended choice. He orders the study via the computerized physician order entry (CPOE) system and also orders some pain-relieving medication. The program alerts him that his choice could have a dangerous interaction with one of the medications Mr. Conway is taking. The computer suggests an alternative, which the doctor selects instead.
A few moments later, Dr. Hendricks sees that the patient is not in his room. He looks at the electronic dashboard, which is tracking the radio frequency identification (RFID) tag on Mr. Conway’s wristband. He learns that the patient was transported to radiology 5 minutes ago and is currently undergoing the scan. Shortly thereafter, an alert on the dashboard warns him that the radiologist has reported an abnormality on the study. Luckily, the pain is being caused by a kidney stone instead of something more serious. With a single click the emergency physician is able to view the digital images and confirm the findings.
Looking for assistance in managing Mr. Conway’s kidney stone, Dr. Hendricks pages a urologist. Instead of wasting time waiting by the phone, he immediately goes to see another patient. He knows that whenever his call is returned, it will be routed to the digital communication device he wears on his lapel.
Dr. Hendricks generates the documentation for the patient’s ED visit through a wireless dictation or wireless tablet system that allows him to note historical and physical findings, order laboratory tests and radiographs, and submit orders via CPOE with integrated decision support. In either case, he does not have to search for a chart or wait for someone else to finish using it.
The dashboard is updated with Mr. Conway’s pending discharge so the housekeeping manager can ensure that the resources required to clean the room will be available when needed. The triage nurse in the ED selects the next patient to use the room when it becomes available.
A short time later, Mr. Conway is feeling better and is ready to be discharged home. He receives a computer-generated instruc-
tion sheet with information about his diagnosis of a kidney stone, including what warning signs to watch for, as well as whom to follow up with and when. Upon discharge, the system sends the patient’s primary care physician, Dr. Thompson, and the consulting urologist a secure e-mail summarizing the ED visit and the patient’s discharge instructions. The e-prescribing module, having screened for potential drug interactions and provided dosage guidance, electronically routes Mr. Conway’s prescriptions to the pharmacy near his home, saving time and reducing the risk of errors associated with legibility problems.
Mr. Conway uses his secure doctor–patient messaging application to communicate with Dr. Thompson 2 days later, letting him know he passed the stone and is feeling much better. He also mentions how pleased he was with his emergency visit. Even though the ED seemed to be incredibly busy, everything went smoothly and efficiently, and he feels he got great care.
Although the story of Mr. Conway’s visit to the ED sounds futuristic, all of the technology described above exists today as both home-built and commercial products. But the diffusion of these technologies to date has been limited. The average community hospital and even some large medical centers lack basic information technology (IT) enhancements that have been shown to improve the efficiency of care and patient flow, inform clinical decision making, and enhance provider-to-provider and provider-to-patient communications. This chapter describes the current state of the art in health care IT and highlights several specific IT tools that have proven ability to improve emergency care in six key areas: management and coordination of patient flow and hospital patient care, linkage of the ED to the wider health care community, clinical decision support, clinical documentation, training and knowledge enhancement, and population health monitoring. The chapter also considers some of the new clinical technologies that are expected to impact emergency care within the coming decade. This is followed by a discussion of challenges and barriers hospitals may face in adopting these technologies. Finally, the chapter addresses the need for and approaches to prioritizing investments in technologies that can improve emergency care now and in the future.
INFORMATION TECHNOLOGY IN THE HEALTH CARE DELIVERY SYSTEM
The early application of health care IT was limited almost exclusively to hospital accounting systems. As early as the 1960s, hospitals began to use
various computer programs for business operations and financial management (Detmer, 2000; Shortliffe, 2005). By the mid-1970s, a small number of hospitals had equipped their programs to process data with medical content (Henley and Wiederhold, 1975; Hospital Financial Management Association, 1976). During the 1980s and 1990s, many hospitals further enhanced their systems to include electronic health records (EHRs), a trend that was also seen among a small percentage of private physician practices (IOM, 1991, 2003).
Despite these early advances, progress toward widespread adoption of health IT has been slow. This is especially true of applications aimed at improving the quality and timeliness of patient care, such as programs that assist with patient flow, clinical decision making, and medical communications. Today, it is estimated that fewer than one-third of hospitals and one-fifth of private physicians use EHRs. Use of CPOE systems is even less common, with only 12 percent of hospitals and 10 percent of private physicians using the technology (Brailer and Teresawa, 2003; Goldsmith et al., 2003; The Lewin Group, 2005; Healthcare Information and Management Systems Society, 2005; Burt and Hing, 2005; Bower, 2005). In comparison, more than one-half of primary care physicians in New Zealand and the United Kingdom have reported using both EHRs and CPOEs in their daily practices (Harris Interactive, 2001). Commonly cited barriers to the adoption of these and other IT tools include prohibitive costs, lack of standardization, and physician resistance to change; additional discussion of these barriers is provided later in this chapter.
While usage rates for specific IT applications remain low, data do suggest that American physicians are increasingly reliant on computer-based resources within their offices. According to a recent American Medical Association survey, 99 percent of private practices and 96 percent of physicians use computers in their offices, 84 percent have a computer network in place, and 75 percent have Internet access. At the same time, however, the interconnectedness of these resources with other points in the health care system, such as the ED, has been found to be lagging, with only 35 percent of physicians reporting a connection with a hospital or laboratory (Chin, 2002). The apparent isolation of this emerging IT usage raises significant concerns about the continuity of care, particularly for ED patients, for whom immediate access to medical records can mean the difference between lifesaving intervention and life-threatening medical errors.
Data also suggest providers’ growing recognition of the potential of IT to significantly improve the quality of health care in the United States. For example, a majority of respondents to a 2005 survey conducted by the Healthcare Information Management and Systems Society (HIMSS) cited “reducing medical errors and improving patient safety” as their top IT priority. Of these respondents, nearly two-thirds indicated their next IT
development would be the adoption of an EHR system. Other applications identified by respondents included CPOE and clinical decision support systems (CDSSs). The HIMSS survey respondents included hospitals, physician offices, mental/behavioral health facilities, long-term care facilities, and home health agencies with annual gross revenues ranging from $50 million or less to $1 billion or more (Healthcare Information and Management Systems Society, 2005).
Given that more providers recognize and are turning to IT as a tool to improve the safety and quality of care, one might expect to find significant IT investments occurring in the health care field. After all, the United States invests approximately $1.7 trillion, or 16 percent of its gross domestic product (GDP), on health care annually. Data reveal, however, that the expected level of investment simply has not occurred. In 2004, just $17–$42 billion, or 10–25 percent of all U.S. health care investments, was applied to health IT. Less than one-third of this amount, or approximately $7 billion, was invested in hospital clinical systems such as EHRs, CPOE, or CDSSs (Goldsmith et al., 2003; Bower, 2005; The Lewin Group, 2005).
The health care field has also failed to keep pace with IT investments as a percentage of industry revenue. While spending on health care IT as a percentage of revenue has increased slightly in recent years, rising from 1–2 percent in 1998 to 2–3 percent today, these figures are far below those for the IT and financial services industries, which invested 10 and 7 percent, respectively (The Lewin Group, 2005). This disparity becomes even more striking when one examines IT investment rates on a per worker basis; while most U.S. industries invested approximately $8,000 per worker for IT in 2004, the health care industry invested only about $1,000 (DHHS and ONCHIT, 2005).
The paucity of investments in health care IT has ramifications far beyond the financial. Without adequate resources for the coordinated development or implementation of proven IT systems, efforts to enhance safety, optimize workflow, and foster communication among and across health care settings have largely stalled. Further, where improvements have been made, they have occurred in relative isolation, resulting in islands of innovation rather than systemic repairs to a failing system.
Progress toward a highly integrated and coordinated emergency care system has been slow even though the value of such integration and coordination has long been recognized (NHTSA, 1996). Instead, multiple systems of varied quality have developed independently of one another. The resulting fragmentation undermines the quality, safety, and timeliness of emergency care; limits the application of proven health care IT; and prevents the aggregation of data for public health surveillance and research purposes (Halamka et al., 2005).
The federal government recently assumed a leadership role through the provision of funding and other support to develop a uniform national health information infrastructure capable of supporting integrated health IT (Taylor, 2004; Cunningham, 2005; Hillestad et al., 2005; Shortliffe, 2005). This initiative can lead to significant improvements in emergency care, as well as in other areas. Federal leadership is needed because of failures in the health IT marketplace, including asymmetrical risks and rewards for technological innovation and the inability to offer aggregated data comparisons (Taylor, 2004; Middleton, 2005). Moreover, such leadership is needed today to ensure that IT advances are made in a coordinated way that facilitates the necessary interoperability and communication.
The federal government has shown the ability to initiate essential industry innovation when market forces have failed to do so. The Hill-Burton Act, for example, is largely responsible for the nation’s hospital infrastructure (Halvorson, 2005). Adopted in 1946, Hill-Burton provided federal grants to states for the construction of hospitals, requiring states to adopt plans ensuring that constructed facilities would meet a variety of minimum requirements. Over the course of the next 30 years, Hill-Burton subsidized the construction of 40 percent of all U.S. hospital beds. Other examples of federal leadership filling a market void include the Rural Electrification Act of 1936 and the Federal Aid Highway Act of 1956 (Halvorson, 2005).
A number of other industrial nations have already embraced the need for national leadership in and funding of health IT innovation. Britain’s National Health Service (NHS), for example, recently embarked on the world’s largest civilian IT project, planning to spend approximately $11 billion on a national system that will replace the existing hodgepodge of local systems and paper medical records (The Lewin Group, 2005). Among the IT tools to be featured in this effort are lifelong EHRs coordinated at the national level, integrated information sharing among all health care settings, and online communications and data access for patients and providers (Detmer, 2000).
Using a Regional Health Information Organization (RHIO) model that provides common elements across the full continuum of health care settings, the U.S. government has the potential to significantly improve the quality, safety, and timeliness of emergency care. While the direct costs associated with this effort are estimated at $276 billion over 10 years, a national health information infrastructure would generate direct savings amounting to $613 billion over the same period and $94 billion annually thereafter—this in addition to the many ancillary savings associated with such benefits as improved management of chronic disease (Kleinke, 2005).
INFORMATION TECHNOLOGY IN THE EMERGENCY DEPARTMENT
The ED is a unique setting in modern medicine—a complex and chaotic environment that presents an increasing number of challenges. ED clinicians are frequently called upon to make crucial decisions under pressure with limited data while maintaining continual readiness for new arrivals, stressing available resources. Because ED providers must often make critical decisions without patient records or histories, it has been said that EDs operate on “information fumes.” EDs are subject to increasing patient volumes and more complex conditions, yet over the last decade they have experienced a diminished capacity caused by decreasing resources. One solution to the serious challenges facing today’s EDs may be found in IT, which can both facilitate analysis of the problems and support solutions.
All of the common medical tasks performed by doctors involve information processing: taking a history, examining a patient, ordering and interpreting test results, considering diagnoses, devising a treatment plan, and communicating with other providers about the appropriateness of admission or discharge. All of these are data management tasks. Information is generated when procedures are performed, and simply by the presence and flow of patients. Emergency providers are eager consumers of available past clinical data and are creators of information to be used during followup. The quality of information management determines how well providers manage the care of their patients.
Today, there is an especially urgent need to apply IT to the delivery of emergency care. Among other factors, this urgency stems from the life-and-death nature of emergency care, the myriad threats to such care posed by ED crowding, and the increasingly common role of the ED as the public’s portal of choice for medical services.
Six key areas of emergency care could immediately benefit from an infusion of IT:
-
Management and coordination of patient flow and hospital patient care—Technologies such as electronic dashboards, radio frequency tracking, and wireless communications systems can help ED staff manage patients and maintain control over department workflow.
-
Linkage of the ED to the wider health care community—Enhanced communications among providers within a community can greatly improve the availability of useful clinical information for emergency care, coordination of care, and allocation of community health care resources. Computerized messaging between patients and doctors can ensure that all providers fully coordinate their care. And telemedicine enables advanced medical knowledge to improve the care of patients in remote areas.
-
Clinical decision support—As stand-alone units or part of a broader system, CDSSs can help guide clinicians in choosing the optimal and most economical therapy and can enhance the safety and efficiency of triage. Clinical alerts and reminders can warn providers if a proposed treatment plan poses unrecognized risks.
-
Clinical documentation—Electronic documentation of emergency services can facilitate the timely, accurate collection and storage of information regarding the course of patient care, serving as proof of services rendered for reimbursement purposes and supporting public health and research functions, among other benefits.
-
Training and knowledge enhancement—Computerized education and training resources can make the most up-to-date medical knowledge rapidly available to clinicians so they can deliver quality care.
-
Population health monitoring—Emerging IT applications can provide real-time population health monitoring, including syndromic surveillance and outbreak detection, necessary for many public health and homeland security priorities.
In each of these areas, IT has the potential to significantly enhance the timeliness, safety, and quality of emergency care, improving patient flow and reducing health costs in the process. The challenge for the future is to integrate these technologies effectively so that hospitals can invest in applications that address goals and objectives in all of the above six areas. For example, systems should be able to support clinical decisions as well as operations management. It should also be emphasized that the future development and advancement of IT applications must accommodate the special needs of pediatric patients.
Management and Coordination of Patient Flow and Hospital Patient Care
The case of Mr. Conway presented above illustrates the need for seamless communications among prehospital IT systems; hospital departmental systems, such as laboratory and radiology; and hospital patient-tracking systems. To meet the complex data needs of an ED clinician, data must be shared easily and securely between clinical and financial systems using widely accepted standards and protocols. Among the IT tools currently available to assist with the management and coordination of emergency care are those described below.
Electronic Dashboards
The pre-IT solution for managing ED flow was for staff to track patients on a centrally visible whiteboard. Commonly arranged in the form of a grid, this whiteboard contained a list of patients and their locations, current providers, the status of the visit, and orders to be completed. The information was updated manually when the staff noticed a change and had the time to update the board. Such a system provides a useful central source of individual data points. However, many management decisions are based on aggregate information that needs to be assembled in real time. Since information on whiteboards is updated only when someone notices a change and has time to enter the update, this manual process breaks down during the ED’s busiest times, when the accuracy and timeliness of information are most critical. This problem tends to self-propagate: outdated data cause inefficiencies, further taxing a harried staff that then does not have time to update the whiteboard with further changes.
Computer technology transforms the manual whiteboard into an electronic “dashboard” that continuously displays updated information and integrates multiple data sources, such as laboratory, radiology, and admitting databases. Using a combination of colors or symbols to represent ongoing tasks and processes, many dashboards can present information in a tabular, grid-like format (similar to the manual whiteboard), while others arrange the screen as a graphical representation of the ED. Sometimes, the dashboard tracking function is used as a central point of an ED information system, providing links to other systems discussed in this chapter. At other times, the system is a stand-alone tool that can be modified to interface with other components of the hospital information system.
However they are configured, electronic dashboards allow providers to see the most recent information without the need for manual input. Computerized systems provide an excellent overview of the ED and patient flow for both clinicians in the ED and administrators in their offices. Bottlenecks become readily apparent, staff members are able to see developing problems, and action can be taken before operations are affected.
Long-term storage of the data tracked by a dashboard system, as with several other systems discussed in this chapter, is another useful tool that can aid in resource planning and error identification, analysis, and prevention. Given accurate models of patient flow and information on past bottlenecks, it becomes possible to anticipate future demands on staff and maximize the efficient deployment of resources (Cone et al., 2002). The complexity of the ED makes error identification a difficult process, and sole reliance on clinician reporting will likely be inadequate to effect change (Handler et al., 2000). Readily accessible data on all ED visits facilitates analysis of standard quality assurance measures, such as unplanned revisits, as well as the formu-
lation of new metrics for quality care. In the case of an adverse event, analysis of stored dashboard parameters can allow reconstruction of the event, similar to the capability provided by an airplane’s “black box” after a crash.
Further, allowing clinicians (especially trainees) to access stored tracking data to follow up on their patients encourages self-monitoring for errors and helps mitigate a key deficiency of the feedback system of the ED: that an unknown result of treatment has the same reinforcing effect as a positive outcome (Croskerry, 2000). Often, errors and near misses are caught during follow-up care but not reported back to the original treating clinician. Storage of visit data makes it easy for ED providers to review a list of patients they have seen in the past. That list could integrate data from the ED course with other information from the hospital system, allowing providers to follow up on whether their diagnoses were correct and their treatments appropriate.
While there have been only a few effectiveness studies concerning comprehensive ED dashboard systems, preliminary findings appear to support the benefits of their use. Among these benefits, hospitals with ED dashboards have reported reductions in lengths of stay, fewer patients leaving prior to treatment, and less time spent on diversion (Jensen, 2004). Providing emergency physicians with an updated display of the status of laboratory tests has been shown to improve their perceptions of efficiency and communication with patients (Marinakis and Zwemer, 2003). And the ability to better communicate estimated wait times to patients using dashboard technology has been found to improve patient satisfaction with emergency care (Thompson et al., 1996).
Radio Frequency Identification Tracking
Effective workflow in the ED requires knowledge of the locations of patients, caregivers, and equipment. New tracking technologies, such as radio frequency identification (RFID), can show the exact locations of people and resources, enabling caregivers to optimize workflow and empowering administrators to understand how people move through the department.
Such tracking systems are available in two basic forms: (1) passive systems that require the use of RFID scanners to read unpowered RFID tags and (2) active systems that use existing hospital wireless networks to track battery-operated RFID transmitters. Using hardware and software, active RFID systems then track the position of these transmitters with enough accuracy to identify the room in which they are located.
Several pilot studies of RFID tracking in the ED offer insight regarding the potential of this technology to improve the quality, timeliness, and efficiency of emergency care. At Beth Israel Deaconess Medical Center in Boston, for example, RFID is being used to track equipment and key staff
members. At Summa Health System in Akron, Ohio, RFID is being used to optimize patient flow and track patient location. Finally, an ED in Memphis is using RFID as a means to reduce patient waiting times by providing realtime notification of bed availability.
Digital Voice Communications
While the ED dashboard provides complete integration of all hospital data in a single location, there is still a need for real-time discussion of patient care issues among caregivers. Cellular technologies appear to be an obvious answer to this real-time need given the ubiquity of such devices, but pose a number of challenges for hospitals, including electronic interference, varied reception, and germ transfer (Tri et al., 2001; Shaw et al., 2004). One means of addressing these issues is hands-free Voice over Internet Protocol (VoIP) devices for voice communications over existing hospital wireless data networks. Newer VoIP devices provide dual capability—automatic use of the hospital network when indoors and automatic use of the standard cellular network when outdoors. Of note, users of such technology must remain cognizant of their surroundings to ensure that patient confidentiality is protected and that ambient noise does not degrade voice recognition.
Wireless Registration
In a typical ED, several components of emergency care occur simultaneously. A patient having a heart attack, for example, may require a physician performing an exam, a nurse inserting an intravenous tube, and a medical technician performing an electrocardiogram (EKG). At the same time, the laboratory will be processing blood tests, while radiology is developing an x-ray and the catheterization laboratory is being instructed to prepare for a new arrival. In most EDs, however, there is a critical point of failure in the simultaneous nature of this response: the ED registration clerk.
Currently at most facilities, ED registration represents a significant bottleneck in what should be a serial process. For patients who have been triaged with a high severity of illness, one strategy for improvement is to move the formal registration process to the bedside via a wireless network. Such an approach would make the registration process more flexible as it would remove the need to tie the registration process to a single physical space (Smith and Feied, 1998).
Mobile Computing
Mobile computing (MC) technology, such as specialized wireless laptop carts equipped with 24-hour batteries or specialized tablet PCs, are being
increasingly well received by ED physicians and their patients (Bullard et al., 2004). Among their other applications, MC technology can provide ED staff with bedside access to patient EHRs and CDSSs. Tablets can also enable physicians and nurses to document their findings and care in real time rather than dictating later, and provide the clinician with feedback to ensure proper documentation for coding and billing purposes. These devices also help clinicians remember the relevant questions to ask, findings to check, and checklists to review before administering hazardous treatments, such as thrombolytic therapy. In addition, MC technology can enhance the capability of the ED to deploy a fully functional system to any location at a moment’s notice, as might be required during severe crowding or a mass casualty event.
Handheld Wireless Devices
Handheld computers and multifunction wireless devices, such as Blackberries, are increasingly popular with physicians who use them in their clinical practice (ACP and ASIM, 2005). Numerous published reports describe their utility for medical education (Bertling et al., 2003), dissemination of new medical practice guidelines (Strok et al., 2003), and documentation of patient care and procedures in the ED (Bird et al., 2001). When integrated with wireless communications devices, handheld computers can be used to view patient data (Duncan and Shabot, 2000), record and transmit real-time patient vital signs during intrahospital transport (Lin et al., 2004), and serve as triage and screening tools for large public events (Chang et al., 2004). These devices also can be used to enhance patient safety by alerting physicians to abnormal test results (Bates and Gawande, 2003).
Digital Radiography and Picture Archiving and Communications Systems
In recent years, many hospitals have migrated from film to digital capture and display of x-ray, magnetic resonance imaging (MRI), computed tomography (CT), angiography, and ultrasound images. These images are then stored in a picture archiving and communications systems (PACS). Both digital radiography and PACS have been shown to provide interpretations that are as reliable as traditional film-based methods (Kundel et al., 2001). With respect to emergency care in particular, a number of benefits are associated with these technologies, such as reduction of the time required to capture images (Redfern et al., 2002). PACS offer instantaneous sharing of images with multiple clinicians, reduce the risk of films being irrevocably lost or misplaced, and eliminate all delays associated with retrieving films from archives and record rooms. And both technologies facilitate remote interpretation of films, a service especially important in rural or community ED settings, which may not have access to 24-hour radiologist coverage. In
addition, PACS enable on-call specialists to view films from home, office, or another hospital, thereby expediting care.
Electronic Health Records
Whether implemented as stand-alone systems or part of a more comprehensive IT array, each of the coordination and management tools discussed here has the potential to significantly improve patient flow and enhance the quality, timeliness, and safety of care in the ED. This is particularly true when these tools are complemented by an integrated system of EHRs.
The ED operates in a relative data vacuum with respect to information on patients and their conditions. Typically, there is no medical record for ED patients, who may be uncommunicative or unconscious upon arrival. Moreover, extreme urgency of treatment is paramount as life-threatening illnesses or injuries have occurred. Under such circumstances, accurate diagnosis is made more difficult, drug allergies can be missed, and important comorbidities can go undetected. Fortunately, EHRs offer a solution to this information void.
The potential of EHRs to improve patient care in all health care settings has been well recognized for more than a decade, with the Institute of Medicine (IOM) having called for the complete elimination of paper-based medical records as early as 1991 (IOM, 1991). As currently defined by the IOM, an EHR system consists of four key elements: (1) longitudinal collection of electronic health information for and about patients, defined as including information pertaining to the health of an individual or health care provided to an individual; (2) immediate electronic access to patient-and population-based information for those with designated authority; (3) provision of knowledge and decision support to enhance the quality, safety, and efficiency of patient care; and (4) support for efficient processes of health care delivery (IOM, 2003).
Over the last 15 years, numerous studies have documented the advantages of EHR systems over traditional paper-based medical records. Among these advantages, EHRs improve the reliability of chart access, allow multiple individuals to access the record simultaneously, and facilitate electronic communication between health care providers. They enhance the quality and completeness of medical data and facilitate the integration of clinical decision support for providers. They also provide efficient access to medical references and assist with the collection of population health measures (Holbrook et al., 2003). Studies examining the use of EHR systems in EDs have yielded similar findings, concluding that the systems can improve documentation, patient care, and patient satisfaction without detracting from direct patient care or resident education or supervision (Buller-Close et al., 2003).
Linkage of the ED to the Wider Health Care Community
A number of IT tools are available to improve provider-to-provider and provider-to-patient communications during the course of ED care and beyond.
Prehospital Communications
The potential for IT to improve patient flow and enhance the quality, timeliness, and safety of emergency care begins even before the patient reaches the hospital. Prehospital EMS units often are the first caregivers to acquire medical information about patients en route to the ED. The ability of these units to accurately capture and transmit vital signs, patient history, and early treatment information to receiving hospitals can be enhanced by several IT applications. For example, prehospital 12-lead electrocardiography has been shown to be safe, to improve times to reperfusion therapy, and to decrease patient morbidity and mortality (Urban et al., 2002). Also, the rapid diffusion of messaging and data transmission through commercial cellular telephones suggests a significant potential for the development of cell-based prehospital–hospital communications. It is critically important that the design and implementation of these systems support full interoperability, that is, allow EMS personnel to “talk” to each other, the police, emergency management personnel, fire departments, and EDs.
Emergency Management
A number of cities have begun to eliminate communication barriers by purchasing equipment that enables officials from public safety and public health to communicate in real time (GAO, 2004). Some cities have also begun to address disaster preparedness communication issues with the help of the Health Alert Network, a nationwide communication network designed to facilitate communications through high-speed Internet connectivity, broadcast capabilities, and training.
In addition, the real-time capture and transmission of EMS dispatch data can improve the coordination of prehospital and emergency care for critically ill patients (Teich et al., 2002). Such data exchange allows EMS teams to quickly determine the best location to which they should deliver patients. This capability not only minimizes delays caused by routine ambulance diversions, but also significantly strengthens a community’s ability to respond to mass casualty events. Retrospective analysis of EMS dispatch data also suggests that the monitoring of EMS data is a viable approach to public health monitoring and surveillance (Mostashari et al., 2003).
Regional Health Information Organizations
The development of RHIOs holds significant promise for connecting emergency medical services (EMS), EDs, and other providers within regions (Koval, 2005). Regional health systems can link providers who serve the safety net so they can coordinate emergency and other community care. Many communities already have primary care networks that integrate hospital EDs into their planning and coordination efforts. A rapidly growing number of communities, such as San Francisco and Boston, have developed RHIOs that coordinate the development of information systems to facilitate patient referrals and tracking and the sharing of medical information between providers to optimize the patient’s care across settings. The San Francisco Community Clinic Consortium, for example, brings together primary care, specialty care, and EDs in a planning and communications network that closely coordinates the care of safety net patients throughout the city.
The development of these networks is a centerpiece of the federal government’s strategic plan for health care IT (Thompson and Brailer, 2004). The Agency for Healthcare Research and Quality (AHRQ) has provided seed money through grants to a number of RHIO startups.
Telemedicine
Telemedicine has a number of important applications for improving the delivery of emergency and trauma services in remote locations, including emergency patient care, education, research, and patient follow-up. A recent IOM study, Quality Through Collaboration: The Future of Rural Health, highlighted the growing application of telemedicine to emergency and trauma care (IOM, 2004b). The use of two-way videoconferencing, available since the 1960s, has begun to increase as a result of the accelerated development of telecommunications infrastructure in the last decade, the introduction of digital communications, and the improved capabilities and cost value of computer hardware and applications. Videoconferencing has facilitated specialty consultation in a number of critical areas, including trauma, radiology, cardiology, and orthopedics.
Cost and outcome studies on the role of telemedicine in rural areas are limited and warrant further attention. Studies have shown telemedicine to be effective in the delivery of acute care to victims of trauma in remote locations (Marcin et al., 2004). Teleradiology has been found to have a significant impact on diagnosis and treatment decisions (Lee et al., 1998). Studies have also indicated high levels of patient and provider satisfaction with these technologies (Boulanger et al., 2001).
Automated Discharge Systems
For many patients who enter the health care system through the ED, treatment concludes with discharge instructions on self-care and on when to return for follow-up care. Unfortunately, patient recall of these instructions is often quite poor, a problem exacerbated by the frequent use of medical jargon and difficult-to-read handwriting (Vukmir et al., 1993). Further, patients’ noncompliance with instructions for follow-up services often hampers recovery, thereby contributing to return ED visits. These problems are compounded for non-English-speaking patients. Good communication between patient and clinician is essential to quality care and good outcomes. The IOM report Health Literacy: A Prescription to End Confusion documented the poor state of health literacy, even among English-speaking patients, and the serious consequences this can have for health outcomes (IOM, 2004a). For non-English-speaking patients, the problem is clearly more critical. As the number of non-English-proficient U.S. residents increases, the need for IT solutions will grow.
A number of IT tools available today can assist with the discharge process. These include automated discharge programs that produce clear, concise, legibly written instructions proven to enhance patients’ understanding of their condition and their adherence to treatment plans (Vukmir et al., 1993; Jolly et al., 1995). In addition, discharge communication programs allow ED physicians to establish a primary care appointment for follow-up care, a service that has been shown to markedly improve patient show rates at follow-up appointments, providing an additional opportunity to offer important preventive services (O’Brien et al., 1999).
Automated Referral Systems
A common frustration facing ED staff today is how best to receive information on patients who are referred to the ED by their primary care physician. In an effort to streamline care, referring physicians often wish to share insights and suggestions about the patient they are referring. In large EDs, however, it is often impractical and interruptive to have a busy ED physician stop patient care to take a call from a referring physician. To solve this problem, some EDs make fax or phone transcription options available to callers. Yet at the busiest times, a large number of patient referrals can pile up by the triage desk, and matching them up accurately as patients arrive becomes a challenging and time-consuming task.
To address this challenge, many hospitals are adopting automated referral systems to facilitate information transfer. Beth Israel Deaconess Medical Center in Boston, for example, developed a system that allows physicians to access a secure Web page and input or import the patient’s information.
Once the information has been submitted, the system prints out a summary report and attaches an electronic copy of the report to the patient’s EHR. Thus even if the triage staff is unable to match the paper referral to the appropriate patient chart, clinical staff can still see and act on the information via the dashboard display. Prior to the system’s implementation, ED administration at Beth Israel Deaconess Medical Center received several complaints per week related to this problem; now such complaints are almost nonexistent.
Electronic Prescribing
Electronic prescribing, or the electronic transfer of prescription data from clinicians to pharmacies, is an increasingly common method of ensuring that providers, pharmacists, and patients have timely access to accurate prescription and medication information. ED clinicians can use electronic prescribing technology to send discharge medication prescriptions automatically to a pharmacy that is convenient for their patients. This capability improves the timeliness and accuracy of prescriptions and eliminates risks due to poor handwriting or inaccurate transcription (Bizovi et al., 2002). It also improves enforcement of formularies and enhances communication among providers. Electronic prescribing technology can be implemented alone or integrated with other discharge programs, such as those as described above.
Electronic Communications
The complexity of modern medicine has made the sharing of information a critical function in health care. Failures of communication between health care providers are among the most common factors contributing to adverse events (Bates and Gawande, 2003). Health care IT can facilitate communication between physicians, as well as between patients and providers. It can also help make the dissemination of information more efficient by ensuring that the information is received and handled with appropriate priority.
There are currently two common approaches to secure electronic communications. The first is Secure/Multipurpose Internet Mail Extensions (S/MIME) gateways. With this approach, organizations obtain digital certificates that are used to encrypt e-mail as it travels over the Internet. Thus, the organization-to-organization transmission of e-mail is protected. Once the electronic message has arrived at the destination organization, it is treated as secure internal e-mail. The second approach involves storing all messages in a secure database accessible only via a password-protected encrypted website. Doctors and patients communicate via this website, but reminders are sent to their regular e-mail accounts informing them that
they have new messages pending. In this way, no patient-identified information is sent via regular, unsecured e-mail technologies. This secure website approach enables discharge summaries, admission notification, and other clinical correspondence to be transmitted electronically between doctors. Additionally, patients and doctors can use the system to exchange clinical results and clinical messages.
With both of these approaches, efforts must be made to facilitate use of the system in ways that make both providers and patients more comfortable with the technology. A recent study found that while 45 percent of on-line consumers wished to communicate with their physicians using e-mail, only 6 percent had done so (Manhattan Research, 2002). The adoption of privacy standards and other protections is needed to encourage use of electronic communications at both ends of the care spectrum. An example of a system linking patients and providers is described in Box 5-1.
Clinical Decision Support
Adverse events can often be prevented if additional information is known at the time critical decisions are made. Sometimes the pivotal facts are available, but because of information overload, they are not readily apparent among a large volume of less important data. Computers can be programmed to use guidelines to alert physicians of unexpected results or remind them of important information at the time decisions are being made. Numerous studies have shown that alerts and reminders are an effective means of changing physician behavior and improving the quality of care (McDonald, 1976; Kuperman et al., 1999; Kilpatrick and Holding, 2001). Specific examples of clinical decision-support tools currently available to improve emergency care are described below.
Automated Triage Systems
Automated triage systems are commonly used to refer patients to the appropriate levels of medical care. For example, nurse call centers routinely use protocols and guidelines to triage patients to self-care, primary care, or emergency care. Initial attempts at the development and implementation of such systems for use in the ED have achieved variable levels of success (Brillman et al., 1996; Haukoos et al., 2002; Dale et al., 2003). While additional research on the potential of triage systems to enhance ED patient flow and improve the quality of emergency care is needed, there is at least one tool available to assist with ED triage efforts—the Emergency Severity Index (ESI).
Consisting of a five-level triage system, the ESI has been shown to correlate reliably with resource utilization, the need for hospitalization, and
|
BOX 5-1 The PatientSite Project CareGroup HealthCare Systems is an integrated health care delivery system based in Boston consisting of five hospitals, including its flagship facility, the Beth Israel Deaconess Medical Center. The system employs approximately 1,700 medical staff who provide care to more than 1 million patients at CareGroup centers and through numerous affiliated practices. CareGroup implemented the world’s first clinical computer system and on-line medical record program. In 1999, CareGroup and Beth Israel staff began discussing how best to involve patients in their care and meet the demands of on-line patients. Using a variety of information servers and databases, including some developed by project authors, the team established an independent clinical platform that could display patient information on a secure website accessible through a number of web browsers. Known as PatientSite, this system features secure messaging among patients, providers, and staff; it allows patients to perform routine tasks, such as requesting appointments, obtaining prescription refills, or requesting primary care referrals, on-line; and it supports patient homepages that can be customized with a range of health education links, as well as messages from identified providers. Patients registered with PatientSite have access to a comprehensive medical file, including medical records, established at the time of their registration. They also can maintain personal medical records, recording such information as medication problems, allergies, and other pertinent notes. Numerous security measures are in place to ensure that patients have access only to their own files. Physicians registered with PatientSite, by contrast, have access to information on all of their patients. In early 2003, PatientSite claimed more than 120 participating providers representing 40 CareGroup centers and practices. It had more than 11,000 active patients, defined as those who had logged on at least once following their registration. Participation rates for both providers and patients have steadily increased since the program’s inception in 2000. Additional information about PatientSite, including a demonstration page, is available at http://www.patientsite.org. SOURCE: Sands and Halamka, 2004. |
length of stay (Wuerz et al., 2000). It has excellent interrater reliability and a high correlation with the need for intensive care unit (ICU) admission (Tanabe et al., 2004). The ESI also has been validated in pediatric populations (Baumann and Strout, 2005). Integrating the ESI into automated triage systems in the ED could assist in the accurate and rapid assignment
of severity scores, and immediate capture of the results could help expedite care and provide real-time data on departmental workload. Further, when combined with metrics of throughput and capacity, ESI data could be used to plan staffing and bed requirements, helping to avoid the need for ambulance diversion and minimizing the impact of ED overcrowding.
The University of Alberta’s eTRIAGE system, developed in conjunction with the Alberta provincial government, uses the five-level Canadian Triage Acuity Scale (CTAS). It has been prospectively validated and found to have a high level of interrater reliability (Dong et al., 2005). Existing computer triage systems can also be modified to support syndromic surveillance. Even more promising is the notion of modifying eTRIAGE and similar systems to alert the triage nurse automatically whenever a patient presents with a history, symptoms, or clinical signs that suggest exposure to a bioterrorism agent or other public health threat.
Electronic and even manual triage systems can be designed to facilitate advance ordering of diagnostic tests (e.g., urinalysis, pregnancy test, ankle x-rays) in accordance with evidence-based clinical algorithms. This enables testing to begin before the patient is even seen by the physician.
Computerized Physician Order Entry
Recent efforts to decrease the incidence of adverse drug events have focused on providing clinical alerts at the time of ordering. CPOE systems force the entry of key information and provide suggestions for changes or additional orders as appropriate. Many CPOE systems prevent errors by checking that safe and effective doses have been prescribed, while others add checks for allergies or interactions with other prescribed medications. Adverse reactions to medications occur even when prescribers follow dosing recommendations and safety checks are performed; a detailed audit from CPOE systems and automated dispensing machines (discussed below) can assist with the identification of these rare events.
Over the last decade, CPOE systems have been shown to save time (Tierney et al., 1993), improve resource utilization (Tierney et al., 1988; Bates et al., 1999), improve adherence to clinical guidelines (Overhage et al., 1997; Teich et al., 2000), and decrease medication errors (Bates et al., 1998, 1999). They also have been found to enhance patient safety by providing extra safeguards for high-risk situations (Kuperman et al., 2001). These advantages have been shown only for custom-written CPOE software, however, and may not be replicable with commercial systems (Kaushal and Bates, 2001). It should also be noted that although efforts to implement CPOE in the ED are just beginning—as of 2003, only 18 percent of emergency medicine residency–affiliated EDs reported having medication order entry systems, and only 7 percent reported having systems that could check
for errors (Pallin et al., 2003)—results of preliminary studies suggest that these systems have the potential to introduce inefficiencies (Shu et al., 2001; Field, 2004). A process change in a busy ED that slows care not only would be frustrating, but also could cause more harm than a CPOE system would prevent. As a result, it is especially important that CPOE systems for the ED be specifically designed for use in that setting and that their impacts on the quality, timeliness, and safety of emergency care be carefully monitored (Handler et al., 2004).
Automated Dispensing Machines
Automated dispensing machines (ADMs) are another patient-safety technology that has been gaining acceptance among health care providers. These devices are cabinets that contain multiple drawers filled with medications. They process medication orders and restrict the user’s access to those medicines that have been prescribed, helping to ensure that the correct drug is chosen. The ADM maintains an audit trail that records which provider had access to each medication, facilitating investigation of adverse events. The machines are usually networked with a central pharmacy that keeps track of inventory and proactively replenishes stocks when they are running low.
While ADMs appear to have the potential to promote safety and improve patient flow, further study is needed to determine whether their benefits outweigh their negative aspects (Murray, 2001; Oren et al., 2003). For example, if the number of machines installed is inadequate, efficiency may be compromised as staff wait in line instead of caring for patients. Further, certain classes of medications (e.g., those used in case of cardiac arrest) need to be accessed immediately, and therefore are not appropriate for storage in ADMs in the ED.
Clinical Decision Support Systems
CDSSs integrate information on the characteristics of individual patients with a computerized knowledge base for the purpose of generating patient-specific assessments or recommendations designed to aid clinicians and/or patients in making clinical decisions in three areas: prevention and monitoring tasks, prescribing of drugs, and diagnosis and management (IOM, 2001). Use of CDSSs has been found to improve clinician compliance with a number of prevention and monitoring guidelines, including vaccinations, breast cancer screening, colorectal cancer screening, and cardiovascular risk reduction (Shea et al., 1996; Balas et al., 2000). Studies examining CDSS usage for drug selection, screening for interactions, and monitoring and documenting of adverse side effects similarly suggest some
positive effect (Classen et al., 1992; Evans et al., 1998; Hunt et al., 1998). However, serious questions have emerged regarding the systems’ ability to have a meaningful role in diagnosis or to improve patient outcomes (Wexler et al., 1975; Chase et al., 1983; Pozen et al., 1984; Wellwood et al., 1992; Hunt et al., 1998; Gallagher, 2002). If the time needed to consult a CDSS inadvertently slowed the delivery of emergency care, for example, the system’s implementation would result in far more negative consequences than the benefits its use could offer. Additional research concerning the effectiveness and safety of CDSSs for diagnosis and management, particularly in the ED, is therefore warranted.
Clinical Documentation
All emergency encounters require documentation of the salient details of the visit. This information is maintained to fulfill a number of important goals: it serves as a record to assist in the care of the patient, it serves as proof of services rendered for reimbursement purposes, it records the provider’s thoughts for use in defense against a potential negligence claim, and it supports public health and research functions. Creating documentation that is legible and meets these goals is a time-consuming task. Physicians overwhelmingly prefer to spend their time caring for patients rather than documenting the visit. The result has been a number of programs aimed at making the documentation process as efficient as possible.
Among the clinical documentation programs available, some require entering information in a structured manner, forcing the user to choose from provided options by selecting findings from rows of checkboxes, traversing a nested hierarchical tree of options, or clicking on symbols on a diagram of a human body. Others permit unstructured input, allowing users to type free text or dictate with minimal or no restrictions on what they can enter. A third technology is computer-assisted dictation, whereby a computer voice-recognition program makes a first pass at understanding the words, and a human “correctionist” then verifies the accuracy of the results.
Free-text and unstructured entry options permit rapid input. Because of limitations in computer understanding of human language, however, they do not provide much more capability than computer-assisted storage and transmission. Structured systems usually involve a more cumbersome and time-consuming data entry process, but they store information in a way that programs can easily understand, allowing them to serve as the basis for many other computer-assisted functions. Often, the increased time spent entering the data is compensated by increases in efficiency elsewhere. Human factors play a key role in the choice among these technologies, and the ways clinicians actually use and interact with different systems will
ultimately determine the best approach. A well-designed tablet may turn out to be more efficient than dictation.
For example, fully computerized ED charts can support automated error surveillance (Schenkel, 2000) and help monitor the quality of ED care. Computer algorithms that search for the presence or absence of certain physical examination findings can lead to increases in the sensitivity of biosurveillance algorithms (Teich et al., 2002). CDSSs use programmed rules to promote safer health care; with a structured computerized chart, these rules can be written to handle a much wider range of less common clinical scenarios without the inefficiency or annoyance of asking the user too many questions.
The user-interface and data-entry modules of clinical documentation systems should be rigorously crafted to promote high-quality data entry and efficiency. Although there are many potential benefits to electronic clinical documentation, carelessly designed interfaces will slow the charting task and leave clinicians with two bad choices: allow the system to delay care in the ED, or batch the charting for completion at a later time (Davidson et al., 2004). These systems often necessitate a trade-off between obtaining more accurate and detailed information on patients and increasing the amount of time required to input the information.
Training and Knowledge Enhancement
IT can provide ED and associated staff with a number of informational and educational tools. Examples of these technologies are described below.
Integrated Information Resources
With the increasing complexity of medical care, emergency providers may care for patients who have conditions that were unheard of during their training or who are being treated with medications just recently approved. It is impossible for anyone with patient care responsibilities to memorize current information on every possible pathology, medication, or therapy that he or she could potentially encounter. Given the rapidly expanding volume of medical information and the wide variety of conditions that present to an ED, easy access to electronic references is key to improving patient safety (Bates et al., 1999).
Through new IT tools, the medical reference industry is now able to bring medical knowledge to the point of care in the ED and beyond. For example, textbook websites offer on-line versions of key medical texts and publications, a format that facilitates remote viewing, subject searches, and
routine errata and addendums. Likewise, medication websites provide ED physicians and other staff with quick access to monographs on all prescription, nonprescription, and herbal preparations, as well as information on drug interactions and prescription costs. Many of these services are evolving to provide an increased level of integration into the clinical information system so that, for example, a provider who encountered an unfamiliar diagnosis in a patient record could read a summary simply by clicking on its name.
In addition, IT translation and visual communication tools can help providers deal with the dozens of languages that are heard in the ED. Important applications include the gathering of information for triage and diagnosis, communication regarding treatment decisions and care in the hospital, and provision of written information to patients for subsequent compliance and follow-up.
Training and Simulation
The nature of emergency medicine requires clinicians to rapidly assess a situation and execute an intervention plan, often with incomplete information. Extensive training can help prepare future emergency medicine staff for these types of challenging situations. Just as with the training of commercial airline pilots, computer-driven simulators can provide valuable educational experiences for both the development and evaluation of emergency practitioners’ knowledge (Gordon et al., 2004). Simulation also can be especially useful for training emergency medicine residents in invasive procedures (Vozenilek et al., 2004). The potential of IT-based training and simulation recently led the Society of Academic Emergency Medicine to issue the following recommendation:
EM residency programs should consider the use of high-fidelity patient simulators to enhance the teaching and evaluation of core competencies among trainees…. The impact of patient simulation on emergency medicine resident training is believed to be so significant that, were it not mindful of administrative and cost burdens for individual programs, the consensus panel would have advised that all emergency residency programs obtain access to a simulator. (Vozenilek et al., 2004, P. 1153)
Population Health Monitoring
Real-time population health monitoring is an emerging technology in emergency and public health informatics. Initial efforts have focused largely on regional monitoring of disease among ED patients. Interest and funding in this area were propelled in 2000 and 2001 by concerns about bioterrorism.
Public health agencies have long used surveillance—the systematic monitoring of health conditions of importance within populations—to measure the incidence of disease, identify outbreaks, and evaluate the impact of prevention programs (Buehler et al., 2004). Active surveillance using traditional methods such as postcards, telephone lines, faxed forms, and even e-mail is erratic because clinicians may forget to report a case when they see one or assume someone else is doing so. This can be true whether the condition involves an infectious disease such as tuberculosis or a high-impact injury, such as a gunshot wound (Kellermann et al., 2001). Electronic monitoring of key triage complaints and/or discharge diagnoses would greatly facilitate ED compliance with this traditional public health obligation.
A relatively recent development in population health monitoring is the notion of syndromic surveillance (Mandl et al., 2004)—methods relying on the detection of individual and population health indicators that are discernible before confirmed diagnoses are made. Before there is laboratory confirmation of an infectious disease, ill persons may behave according to identifiable patterns or have symptoms, signs, or laboratory findings that can be tracked through mining of data sources, including ED chief complaints (Fleischauer et al., 2004), International Classification of Diseases (ICD)-9 codes (Espino and Wagner, 2001), laboratory data, and pharmaceutical data (Tsui et al., 2003).
The goal of outbreak detection is to generate an alert whenever observed data depart sufficiently from an expected baseline. To this end, the system must be able to detect a signal (i.e., disease outbreak) against background noise (i.e., normally varying baseline disease in the region). A number of syndromic surveillance systems are currently being developed regionally as well as nationally. These include the Automated Epidemiologic Geotemporal Integrated Surveillance System (AEGIS) in Massachusetts (Mandl et al., 2004; Children’s Hospital Informatics Program, 2005), the Real Time Outbreak Disease Surveillance System (RODS) in Pittsburgh (Tsui et al., 2003), the Electronic Surveillance System for the Early Notification of Community-based Epidemics (ESSENCE) system in the National Capital Area (Lombardo et al., 2003), and the national BioSense system being developed by the Centers for Disease Control and Prevention (Loonsk and CDC, 2004).
As such systems become more advanced, the need for standard protocols for alerting appropriate personnel of abnormal conditions becomes more pressing. One model may be AEGIS, which fully automates population health monitoring from end to end and interfaces with a statewide health alert network. This network, a comprehensive communication and alert messaging switch that provides message content and routing, is an example of a communications technology that helps unite clinical and public health entities.
NEW CLINICAL TECHNOLOGIES
New clinical technologies can be expected to alter the way care is delivered in the ED, but in ways that are difficult to predict. In general, however, a wide range of technologies that provide faster and more mobile diagnostic capabilities can be anticipated. Such technologies can be expected to diffuse gradually from the hospital to the prehospital environment. For example, strategically locating advanced imaging equipment in the ED would shorten patient wait times and improve throughput by accelerating diagnosis. Among the technologies positioned to do just that are 16-slice or higher CT scanners and high-field magnetic resonance (MR) systems, cardiac CT angiography (CTA), portable ultrasound systems, rapid diagnostics, and laboratory automation. As with all medical technologies, well-designed, controlled studies should be used to assess their efficacy and cost-effectiveness in general and for ED applications in particular.
Multislice Computed Tomography Scanners and High-Field Magnetic Resonance Systems
The improved temporal resolution and ever-increasing thin-slice imaging ability of these systems will have a significant impact on ED imaging. The performance of 16-slice CT is the proven standard for general whole-body clinical utility in the ED. However, 64-slice scanners offer a full complement of applications for both radiology and cardiology. In between, there are 32- and 40-slice systems that are less costly than 64-slice systems and are upgradable.
Manufacturers are redefining “open” MR by improving the performance of these systems with stronger magnets or redefining the term to include wider-bore, short-cylinder systems with traditional high-field image quality. With some of these systems, such as the Siemens Magnetom Espree, the patient’s head frequently remains outside the gantry. The combination of a patient table with lateral movements and wide offset capability makes these systems well suited to orthopedic studies.
Although 1.5-tesla MR imaging systems continue to offer the broadest range of applications and clinical utility, the newer very-high-field (3.0-tesla) MR systems offer improved performance, particularly for neurologic, orthopedic, and spinal studies. Body imaging techniques continue to improve with new surface coils and software designed to reduce motion artifacts. The 3.0-tesla MR imaging systems show promise for cardiac imaging with cardiac sequences that are near-real-time and do not require patients to hold their breath. Adoption of very-high-field MR is currently limited but will expand as more sequence development work using these systems is done.
A promising new imaging system developed in South Africa is currently
being evaluated at a handful of medical centers around the country. It allows the trauma team to obtain a quick, low-dose “total body x-ray” to evaluate the entire patient in under 30 seconds.
Cardiac Computed Tomography Angiography
Over the next decade, CTA will become part of routine clinical practice in the ED, where its high negative predictive value for coronary artery disease will provide efficient triage of patients with chest pain. In cases where the diagnosis for chest pain is not clear after more basic tests have been completed, CTA offers a rapid evaluation of three possible causes of the pain—abdominal aortic aneurysm, pulmonary embolism, and coronary artery obstruction. Although a 16-slice scanner is the minimum performance level for cardiac imaging, the newer 64-slice scanners have better image quality, particularly for very small vessels. Scanners with dedicated cardiac application packages provide CTA for the heart, great vessels, and peripherals, as well as calcium scoring and other functional cardiology tools.
Portable Ultrasound Systems
Ultrasound systems have become increasingly compact and mobile. The size of a laptop computer, these portable units come equipped with linear probes for vascular and small-parts imaging for use in echocardiography. These ultrasound systems will become a mainstay in the ED as they allow the emergency physician to perform focused echocardiography and vascular studies, resulting in earlier diagnosis and treatment. Several manufacturers offer portable systems that can be used at the bedside. An example is Zonare’s US system, which features the ability to remove the handheld data processing unit and probe from the cart, complete an exam, then return the system to the cart to review the results. ED ultrasound is for focused identification of time-critical events, such as focused abdominal sonography for trauma (FAST) scans or right upper quadrant ultrasounds to look for gallstones, or a scan to identify the internal jugular vein for placement of a central line. The technology is not intended to replace the precision of comprehensive ultrasound exams by radiologists at a later time—a qualifier radiologists would insist on emphasizing.
Rapid Diagnostics
Current methods for rapid diagnosis of disease in the ED are limited. As an example, 90 percent of aseptic meningitis cases are caused by entero-viruses that result in benign disease. Only 10 percent of patients need to
be admitted and given intravenous antibiotics, but many are unnecessarily hospitalized because of the difficulty of distinguishing aseptic meningitis from more severe bacterial meningitis. Currently, when a patient suspected of having meningitis presents to the ED, he or she is admitted and prescribed prophylactic antibiotics while awaiting results from the laboratory culture, a process that takes 3 to 10 days. Given that infections of various types and fevers of unknown origin are among the top 20 diagnoses sending patients to the ED, technologies that can speed diagnosis will have an important benefit in improving ED workflow.
For example, real-time polymerase chain reaction (PCR) tests designed to identify enterovirus (EV) infection can diagnose EV-positive patients within 5 hours. The patient remains in the ED and is admitted only after the results have identified the cause as bacterial or of unknown origin. Rapid diagnostic tests are available for an increasing number of conditions seen in the emergency setting, including Streptococcus pneumoniae infection, meningitis, bloody diarrhea, and septicemia. Emerging real-time PCR tests will replace laboratory evaluations for occult bacteremia and with their rapid, accurate test results may sharply decrease the use of antibiotics. Early targeted disease detection not only expedites diagnosis and improves the accuracy of clinical decision making, but also speeds recovery by identifying causative organisms and allowing for optimal antibiotic selection.
At least initially, most molecular tests that will impact the ED will be offered through centralized molecular diagnostics laboratories. As the technology advances over the next 2 to 5 years, however, real-time PCR will allow decentralization to rapid-response laboratories with even faster test turnaround times. Recent advances in real-time PCR improve its speed. The traditional PCR requires three steps, real-time PCR requires two steps, and the next generation of real-time PCR will require one step. This translates into samples that can be extracted, amplified, and detected in less than 25 minutes, significantly reducing patient wait times and expediting diagnosis.
An added benefit is that rapid diagnostics can be used to determine whether a patient is a carrier of a disease that could potentially harm other patients and health care workers. For example, rapid bedside testing could help EDs identify difficult-to-reach patients who are at risk of HIV infection and refer them for treatment. A substantial subgroup of patients come to the ED for care but are unlikely ever to seek HIV testing at a health department. Provision of rapid bedside screening with an oral swab rather than a blood draw might allow ED personnel to detect HIV-infected patients, advise them to modify high-risk activity, and refer them for treatment, although evaluations are needed to validate the social and clinical feasibility of this strategy.
Laboratory Automation
The automation of laboratory services will have a significant impact on care provided in the ED. As laboratory testing devices become smaller and easier to use, it will become possible to perform laboratory tests more frequently at the point of care. Laboratory information systems allow for the rapid transfer of test results to the ED and in some circumstances can even provide real-time information, as in the case of PCR-based tests.
In the ED, point-of-care testing will improve patient throughput. To reduce lengthy ED stays, Massachusetts General Hospital established a point-of-care satellite testing laboratory in the ED to perform urinalysis, glucose tests, rapid strep tests, pregnancy tests, tests for cardiac markers, and influenza tests. As a result, test turnaround times were reduced by 87 percent, ED lengths of stay declined by 41 minutes per patient, and ED diversions decreased. Also, emergency physicians’ satisfaction with the laboratory’s turnaround time increased by 50 percent (Lee-Lewandrowski et al., 2003).
Laboratory automation can also eliminate ED bottlenecks by providing test results in a timely manner. Northwestern Memorial Hospital in Chicago improved its ED performance through the use of an automated centralized laboratory. Northwestern found that 18 percent of the average 4.5-hour ED visit was attributed to waiting for laboratory results (Personal communication, K. Clarke, 2004). The hospital developed a system to better connect its laboratory services to the ED, using an early draw process to reduce wait times. Now when a patient presents to the ED, the nurse screens the patient and, whenever possible, orders laboratory tests based on standing physician orders. After the nurse draws the patient’s blood, an ED laboratory technician orders the tests on the laboratory information system and labels tubes with bar codes. The tubes are transported pneumatically to the automated laboratory. The results are available by the time the physician performs the initial patient examination. If additional tests are necessary, their results are available within 5 to 20 minutes. As a result of the use of automation in the centralized laboratory, patient throughput and room utilization increased by 20 percent, patient wait times were reduced by 40 percent, and Press-Ganey patient satisfaction survey scores rose to the 80th percentile.
A number of hospital IT tools have been demonstrated to be effective in improving patient flow and efficiency, and to have a direct and substantial impact on ED crowding and the quality of emergency care. Given the sporadic adoption of these IT tools to date, the committee believes hospitals should increase their efforts to enhance their IT capabilities that impact emergency and trauma care. The committee therefore recommends that hospitals adopt robust information and communications systems to improve the safety and quality of emergency care and enhance hospital efficiency (5.1).
BARRIERS TO THE ADOPTION OF INFORMATION TECHNOLOGY
Given the array of IT tools available to improve patient flow and enhance the quality, safety, and timeliness of emergency care, the argument for the widespread adoption of such tools appears clear. From prehospital care to ED and ancillary services to recovery and rehabilitation, IT has the potential to address many of the challenges currently facing the U.S. emergency care system. Nonetheless, health care IT has not been widely implemented in the ED or other health care settings, and significant barriers to its implementation remain. It would be difficult to exaggerate the daunting challenges hospital face in implementing state-of-the-art IT systems. Limited resources—financial, physical, and intellectual—often stand in the way of even modest goals. The need to win the acceptance of older physicians and to deal with the existence of (often inadequate) hardware and software already in place compounds the problems involved. The investment required to achieve the goals described in this chapter is substantial, and must be addressed through public policy if the adoption of health care IT is to move forward rapidly. Five specific barriers to the adoption of health care IT in the ED are described below.
Financial Requirements
For most health care facilities, the lack of financial support continues to be the most significant barrier to IT implementation (Healthcare Information and Management Systems Society, 2005). Not only is capital needed to purchase and install new technology, a process that is often associated with sizable short-term transition costs, but specialized training and education costs also must be incurred to help physicians and other staff adapt to the new high-tech environment. Adding to these challenges is the fact that access to capital may be particularly limited for certain types of health care organizations, including the nonprofit hospitals that provide much of the nation’s safety net emergency care. Further, while large for-profit hospitals and health plans may have ready capital to invest, they may lack the leverage and incentives needed to implement various IT tools (IOM, 2001).
While there are few published estimates of the costs of widespread implementation of health care IT, there are a number of estimates regarding specific IT applications. For example, the RAND Corporation recently projected that the cumulative cost for 90 percent of hospitals to adopt EHR systems would be $98 billion, assuming that 20 percent of these hospitals currently have such systems in place. Average yearly costs for hospitals across a 15-year adoption period would be $6.5 billion. For physicians, the cumulative costs for 90 percent adoption would be $172 billion, with average yearly costs of approximately $1.1 billion (Hillestad et al., 2005).
Efforts to quantify the return on investment of these costs suggest that short- and long-term returns would far exceed initial outlays. At 90 percent adoption of EHRs, for example, the RAND study projected average annual savings of more than $77 billion, with $42 billion saved each year on average during the 15-year adoption period. Related improvements in prevention and chronic disease management could result in an additional $147 billion in savings annually, while transaction improvements could yield up to $10 billion in savings annually (Hillestad et al., 2005). Estimated net potential savings associated with EHRs are shown in Figure 5-1.
Beyond EHRs, Kaiser Permanente of northern California estimates that it will break even on its systemwide $1.2 billion IT investment in 6.5 years, with a 200 percent return on investment to be achieved in 10 years (Detmer, 2000). Similarly, with IT-related improvements in quality and efficiency and reductions in medical errors, it is estimated that Medicare could save up to 30 percent of its annual spending (The Lewin Group, 2005). Altogether, at the national level, the federal government estimates that the nation would save $140 billion annually, or 20 percent of health care costs, through improved use of health care IT (DHHS and ONCHIT,
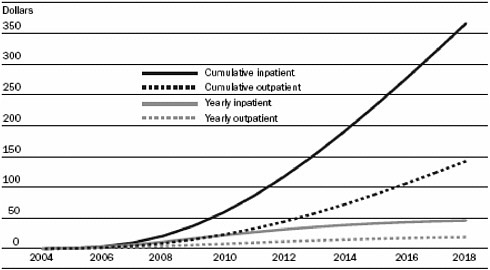
FIGURE 5-1 Net potential savings (efficiency benefits over adoption costs) for hospitals and physicians adopting electronic health record systems during a 15-year adoption period (2004–2018).
NOTE: Dollar figures are billions.
SOURCE: Reprinted from Hillestad et al., 2005, with permission from PROJECT HOPE via Copyright Clearance Center.
2005). Improved interoperability and shared diffusion would likely result in even more substantial savings.
Clinical technologies are somewhat different in that their adoption is linked more directly to reimbursement than to cost savings as in the case of other information technologies. There is a robust market for the development of new medical technologies. These and other changes will occur whether or not there is an active policy to promote their development and utilization or government support for their diffusion.
Lack of Interoperability Standards
A key factor inhibiting the rate of adoption of new health care technologies is the lack of development of common health care IT standards (Goldsmith et al., 2003). Data communication standards are sets of rules that allow disparate computer systems to exchange information without requiring custom programming for each new connection. Without such standards in place, a number of factors discourage the effective integration of multiple data sources into one useful whole. For example, data may be stored in isolated locations; they may be collected and stored using different internal systems, structures, or coding; and they may be generated in ways that do not match the expectations of clinical providers, researchers, or health care managers (McDonald et al., 2001). Widespread adoption of shared standards is necessary to overcome these barriers and permit the creation of clinical data-sharing networks that can build bridges between the various islands of information.
|
We have people showing up at emergency rooms all the time and their data is not there. We’ve never stopped to ask, What are the standards that we need to get someone’s data to the emergency room? —David Brailer, National Health Information Technology Coordinator (Cunningham, 2005) |
The health care industry is just starting to realize the improvements in efficiency, safety, and quality that shared data systems can offer. Providers participating in the Massachusetts Healthcare Data Consortium, for example, have access to pharmacy prescription databases for treatment purposes. Such information is critical in emergency care as many patients arriving in the ED are unable to tell staff exactly which medicines they take, whether because of alterations to their mental status, forgetfulness, or the sheer number of different pills involved. Data communication standards also facilitate
the sharing of clinical information, such as past medical histories, allergies, and EKG results. With standards in place, data sharing has already been proven effective within and among various health care systems (Halamka et al., 1997; Overhage et al., 2002).
In an article in the New England Journal of Medicine, Senate Majority Leader William H. Frist (R-Tennessee) recently described his vision for how interoperability standards allowing the sharing of clinical data could be used to save the life of a patient having a heart attack (Frist, 2005). Senator Frist, along with Senator Hillary Rodham Clinton (D-New York) and Representatives Nancy L. Johnson (R-Connecticut) and Patrick J. Kennedy (D-Rhode Island), is currently leading congressional efforts to promote the development and implementation of interoperability standards for health care IT. At the same time, President George W. Bush has called for federal action, establishing the Office of the National Coordinator for Health Information Technology (ONC) to provide “leadership for the development and nationwide implementation of an interoperable health information technology infrastructure to improve the quality and efficiency of health care and the ability of consumers to manage their care and safety” (DHHS and Office of the Secretary, 2005). ONC recently established the Healthcare Information Technology Standards Panel to harmonize health care data standards for the nation.
Limited IT Knowledge
With new technology comes the need for new expertise. Just as the purchase of health care IT tools requires significant investments of financial capital, human capital (e.g., professional time and knowledge) is needed if the tools are to be implemented and maintained successfully. Whereas many larger hospitals and health care systems may have dedicated IT staff able to oversee the adoption of new technologies, smaller organizations often lack such resources. Moreover, while IT staff is an essential part of the equation, failed attempts to launch new IT tools suggest that clinical staff must also be comfortable and conversant with the technology if its potential is to be realized.
Resource sharing, such as that offered by Beth Israel Deaconess Medical Center and the Veterans Health Administration (VHA), is one way to help ensure that all health care settings have access to the knowledge and expertise needed to adopt proven IT solutions. The VHA’s Veterans Health Information Systems and Technology Architecture (VistA) program is described in Box 5-2. Comprehensive IT training modules, such as those supported by AHRQ, are another approach.
|
BOX 5-2 Veterans Health Information Systems and Technology Architecture (VistA) The Veterans Health Administration (VHA) is the nation’s largest integrated health care system. With a staff of nearly 200,000, VHA provides care to more than 5.1 million veterans and other enrollees annually. It operates over 1,300 facilities nationwide, including 157 medical centers, with one in every state, Puerto Rico, and Washington, DC. It also oversees the nation’s largest medical education and health professions training program, turning out approximately 83,000 health professionals each year. A critical component of VHA operations is the Veterans Health Information Systems and Technology Architecture (VistA). Key aspects of VistA include the Computerized Patient Record System (CPRS), which offers providers a single interface through which they can review and update patients’ medical records, as well as place orders for medications, laboratory tests, and other services. In its next-generation system, HealtheVet, VistA also implements standard functions for health data repository systems, registration systems, provider systems, management and financial systems, and information and educational systems. VHA has shared both its health information and health IT resources—including software and staff expertise—with other federal agencies through the Health Information Technology Sharing (HITS) program since the late 1990s. The HITS program was expanded to include some non-governmental and international organizations in 2001. Through the recent HealthyPeople Initiative, VistA software and expertise are now available as well at minimal or no cost to public- and private-sector organizations that serve the poor and near-poor. SOURCE: Department of Veterans Affairs, 2005. |
Human Factors
Some of the most challenging barriers to the adoption of IT in health care involve human factors. Currently there are more than 780,000 physicians and 2.2 million nurses, as well as many other health care providers, involved in the delivery of patient care in the United States (HRSA, 2003). These individuals possess highly varied levels of IT-related knowledge and experience. Further, clinicians tend to be conservative and reluctant to adopt new automated approaches, especially if previous attempts at IT solutions failed to prove useful in solving diagnostic, therapeutic, or workflow problems (Kassirer, 2000; IOM, 2001).
An important potential hurdle for institutions planning major IT enhancements is the 6- to 12-month learning curve for physicians. Implementation of such systems must be carefully executed and supported, and products must be tailored to each institution through use and modification over time. No system is fully applicable directly off the shelf. Unless the system brings demonstrable value to its users, the potential for physician dissatisfaction and indirect patient dissatisfaction is substantial.
Human factors research deals with human–computer interaction and has developed methods for testing and improving the usability of software. Used by the aviation industry for more than a decade, human factors research is largely credited with minimizing pilot error and improving the safety of air travel (Vincente, 2004). Many of the actual and perceived problems with health care IT in the ED could be overcome by employing human factors techniques (Helmreich, 2000; Wears and Perry, 2002).
For example, the “usability” of software is based on its perceived usefulness as well as its perceived ease of use. A useful program enhances the performance of its users; it makes them more efficient or improves the quality of their work. A program’s ease of use is judged by the amount of effort required to accomplish tasks. Studied barriers to program use include accessibility (whether there are enough computers for all users), availability (whether the system crashes when people wish to use it), start–stop times (whether it takes too long to begin/resume a task or save work to be continued later), system dynamics (whether the response time is too slow), training barriers (whether it takes too many hours to learn to use the program effectively), and lack of consistency (whether various components of a system work together in the same way).
Several examples can be found to demonstrate the inefficiencies and reductions in patient safety that accompany poor implementation of health care IT (Ash et al., 2004). As noted earlier, for example, Cedars-Sinai Medical Center removed its CPOE system after less than 6 months as a result of significant resistance by doctors and nurses who claimed the system was difficult to use. Such resistance may be less pronounced among emergency clinicians as IT adoption typically occurs more rapidly in ED than other settings (Healthcare Information and Management Systems Society, 2005).
While the barriers to IT adoption are significant, research demonstrates that they are hardly insurmountable. In fact, as was so clearly stated in Crossing the Quality Chasm: A New Health System for the 21st Century, “solutions to these barriers can and must be found given the critical importance of the judicious application of IT to addressing the nation’s health care quality concerns” (IOM, 2001, p. 166). An essential step in realizing the potential of health care IT to improve patient flow and enhance the quality, safety, and timeliness of patient care is the creation of a national health information infrastructure, discussed earlier.
Confidentiality
One of the biggest challenges to the development of electronic systems for tracking patients, documenting care, and communicating among clinicians is protecting the confidentiality of patient information. As quickly as systems are developed, protections against security breaches and new methods of attack are devised. While technical solutions exist, there must also be trade-offs between the capabilities of systems and the requirements for confidentiality.
PRIORITIZING INVESTMENTS IN EMERGENCY CARE INFORMATION TECHNOLOGY
The specific costs and benefits of many of the technologies described above to individual hospitals are largely unknown, and can be expected to vary according to the individual circumstances and the technology infra-
|
BOX 5-3 Roadmap for the Implementation of Health Information Technologies In an ideal world, where all hospitals and health care systems were equally flush with capital and similarly motivated to invest in new health care information technologies, the IT tools known to improve the quality, safety, and timeliness of emergency care would be immediately adopted and embraced by staff and patients alike. In the real world, however, financial and other limitations temper the pace at which IT improvements can be implemented. This is particularly true among the nation’s small, rural, and safety net hospitals, which typically have less revenue and more limited IT systems at their disposal. Given these real-world constraints, it is important that IT investments in the ED be made strategically, with close attention paid to such issues as total costs, staff education and training requirements, and the time needed to complete workplace transitions. For example, automated discharge systems represent a relatively inexpensive, easy-to-use technology that many hospitals could turn to as a first step in modernizing their care delivery. While significantly more expensive than automated discharge systems, electronic dashboards are also a priority because they have the potential to improve so many aspects of patient care management. Dashboards also can serve as a launching pad for future IT investments, such as clinical decision support systems (CDSSs) and computerized physician order entry (CPOE). |
|
Clinical documentation programs are the next logical choice for many hospitals and health care systems seeking to improve patient flow and enhance quality and safety. Wireless registration, radio frequency identification (RFID) tracking, and digital hands-free Voice over Internet Protocol (VoIP) communications can facilitate more seamless care with fewer interruptions and more time for direct patient care. These programs also can capitalize on existing hospital wireless networks or dashboard programs, further reducing costs and encouraging coordination. Finally, hospitals may look to CPOE systems to reduce errors, improve safety, and save time in the ED. Efforts should be made to ensure that applied CPOE systems are customized for use in the ED, a task that will require additional expenditures. Further, the impact of such systems on the quality, timeliness, and safety of emergency care should be carefully monitored. Several organizations are moving to make their IT tools more widely available through resource sharing and discounted pricing. For example, the Veterans Health Administration routinely shares its health information and health IT resources—including software and staff expertise—through the Health Information Technology Sharing Program at no or minimal cost. Further, through its Center for Healthcare Information Technology, the American Academy of Family Physicians is making low-cost, standards-based IT more available to family physicians nationwide. In many rural hospitals, it is family physicians who represent the bulk of ED staff. |
structure and readiness of each institution. For example, adopting advanced systems in a hospital that has a limited existing IT platform would probably not be cost-effective; on the other hand, in a hospital with a sophisticated platform, adoption of such systems could be highly cost-effective as the marginal costs associated with their addition would be very small. Given these inherent variations, it would be difficult to prioritize the many technologies in a way that could be generalized to all hospitals. However, the committee identified categories of technologies that would have a substantial impact on emergency care and that could feasibly be adopted by many institutions within 3–5 years:
-
Technologies that facilitate patient flow management, such as electronic dashboards and tracking systems
-
Technologies that improve the continuity of care across the continuum of care, particularly EMS–hospital system linkages and RHIOs that enhance the information available to clinicians across settings
-
Decision-support tools, such as automated triage, that facilitate optimal use of resources
-
Systems that reduce the likelihood of errors in the ED, such as CPOE
-
Systems that facilitate public health surveillance
Some specific strategies for the cost-effective adoption of these technologies are described in Box 5-3. The committee also believes the ED should be a priority site for the early development of enterprisewide IT systems. For example, the development of EHRs is important throughout the hospital and across the health care delivery system. The ED has a particular need for this technology, especially since 43 percent of inpatients are admitted to the hospital through the ED (Merrill and Elixhauser, 2005).
SUMMARY OF RECOMMENDATIONS
5.1: Hospitals should adopt robust information and communications systems to improve the safety and quality of emergency care and enhance hospital efficiency.
REFERENCES
ACP, ASIM (American College of Physicians, American Society of Internal Medicine). ACP-ASIM Survey Finds Nearly Half of U.S. Members Use Handheld Computers. [Online]. Available: http://www.acponline.org/college/pressroom/handheld_survey.htm [accessed July 1, 2005].
Ash JS, Berg M, Coiera E. 2004. Some unintended consequences of information technology in health care: The nature of patient care information system-related errors. Journal of the American Medical Informatics Association 11(2):104–112.
Balas EA, Weingarten S, Garb CT, Blumenthal D, Boren SA, Brown GD. 2000. Improving preventive care by prompting physicians. Archives of Internal Medicine 160(3):301–308.
Bates DW, Gawande AA. 2003. Improving safety with information technology. New England Journal of Medicine 348(25):2526–2534.
Bates DW, Leape LL, Cullen DJ, Laird N, Petersen LA, Teich JM, Burdick E, Hickey M, Kleefield S, Shea B, Vander Vliet M, Seger DL. 1998. Effect of computerized physician order entry and a team intervention on prevention of serious medication errors. Journal of the American Medical Association 280(15):1311–1316.
Bates DW, Teich JM, Lee J, Seger D, Kuperman GJ, Ma’Luf N, Boyle D, Leape L. 1999. The impact of computerized physician order entry on medication error prevention. Journal of the American Medical Informatics Association 6(4):313–321.
Baumann MR, Strout TD. 2005. Evaluation of the emergency severity index (version 3) triage algorithm in pediatric patients. Academic Emergency Medicine 12(3):219–224.
Bertling CJ, Simpson DE, Hayes AM, Torre D, Brown DL, Schubot DB. 2003. Personal digital assistants herald new approaches to teaching and evaluation in medical education. WMJ: Official Publication of the State Medical Society of Wisconsin 102(2):46–50.
Bird SB, Zarum RS, Renzi FP. 2001. Emergency medicine resident patient care documentation using a hand-held computerized device. Academic Emergency Medicine 8(12):1200–1203.
Bizovi KE, Beckley BE, McDade MC, Adams AL, Lowe RA, Zechnich AD, Hedges JR. 2002. The effect of computer-assisted prescription writing on emergency department prescription errors. Academic Emergency Medicine 9(11):1168–1175.
Boulanger B, Kearney P, Ochoa J, Tsuei B, Sands F. 2001. Telemedicine: A solution to the followup of rural trauma patients? Journal of the American College of Surgeons 192(4):447–452.
Bower AG. 2005. The Diffusion and Value of Healthcare Information Technology. Santa Monica, CA: Rand Corporation.
Brailer DJ, Teresawa EL. 2003. Use and Adoption of Computer-Based Patient Records. Oakland, CA: California HealthCare Foundation.
Brillman JC, Doezema D, Tandberg D, Sklar DP, Davis KD, Simms S, Skipper BJ. 1996. Triage: Limitations in predicting need for emergent care and hospital admission. Annals of Emergency Medicine 27(4):493–500.
Buehler JW, Hopkins RS, Overhage JM, Sosin DM, Tong V. 2004. Framework for evaluating public health surveillance systems for early detection of outbreaks: Recommendations from the CDC Working Group. Morbidity and Mortality Weekly Report 53(RR05):1–11.
Bullard MJ, Meurer DP, Colman I, Holroyd BR, Rowe BH. 2004. Supporting clinical practice at the bedside using wireless technology. Academic Emergency Medicine 11(11):1186–1192.
Buller-Close K, Schriger DL, Baraff LJ. 2003. Heterogeneous effect of an emergency department expert charting system. Annals of Emergency Medicine 41(5):644–652.
Burt CW, Hing E. 2005. Use of computerized clinical support systems in medical settings: United States, 2001–03. Advance Data (353):1–8.
Chang P, Hsu YS, Tzeng YM, Sang YY, Hou IC, Kao WF. 2004. The development of intelligent, triage-based, mass-gathering emergency medical service PDA support systems. Journal of Nursing Research: JNR 12(3):227–236.
Chase CR, Vacek PM, Shinozaki T, Giard AM, Ashikaga T. 1983. Medical information management: Improving the transfer of research results to presurgical evaluation. Medical Care 21(4):410–424.
Children’s Hospital Informatics Program. 2005. Research. [Online]. Available: http://www. chip.org/research.cgi [accessed December 1, 2005].
Chin T. 2002, December 2. Have physician offices become more wired? American Medical News.
Classen DC, Evans RS, Pestotnik SL, Horn SD, Menlove RL, Burke JP. 1992. The timing of prophylactic administration of antibiotics and the risk of surgical-wound infection. New England Journal of Medicine 326(5):281–286.
Cone DC, Nedza SM, Augustine JJ, Davidson SJ. 2002. Quality in clinical practice. Academic Emergency Medicine 9(11):1085–1090.
Croskerry P. 2000. The feedback sanction. Academic Emergency Medicine 7(11):1232–1238.
Cunningham R. 2005. Action through collaboration: A conversation with David Brailer. Health Affairs 24(5).
Dale J, Higgins J, Williams S, Foster T, Snooks H, Crouch R, Hartley-Sharpe C, Glucksman E, Hooper R, George S. 2003. Computer assisted assessment and advice for “non-serious” 999 ambulance service callers: The potential impact on ambulance dispatch. Emergency Medicine Journal 20(2):178–183.
Davidson SJ, Zwemer FL Jr, Nathanson LA, Sable KN, Khan AN. 2004. Where’s the beef? The promise and the reality of clinical documentation. Academic Emergency Medicine 11(11):1127–1134.
Department of Veterans Affairs. 2005. Facts about the Department of Veterans Affairs. [Online]. Available: http://www1.va.gov/opa/fact/vafacts.html [accessed September 1, 2005].
Detmer DE. 2000. Information technology for quality health care: A summary of United Kingdom and United States experiences. Quality in Health Care 9(3):181–189.
DHHS, Office of the Secretary (Department of Health and Human Services, Office of the Secretary). 2005. Office of the National Coordinator for Health Information Technology; Statement of Organization, Functions, and Delegations of Authority. [Online]. Available: http://a257.g.akamaitech.net/7/257/2422/01jan20051800/edocket.access.gpo.gov/2005/05-16446.htm [accessed May 20, 2006].
DHHS, ONCHIT (Department of Health and Human Services, Office of the National Coordinator for Health Information Technology). 2005. Value of HIT. [Online]. Available: http://www.hhs.gov/healthit/valueHIT.html [accessed July 1, 2005].
Dong SL, Bullard MJ, Meurer DP, Colman I, Blitz S, Holroyd BR, Rowe BH. 2005. Emergency triage: Comparing a novel computer triage program with standard triage. Academic Emergency Medicine 12(6):502–507.
Duncan RG, Shabot MM. 2000. Secure remote access to a clinical data repository using a wireless personal digital assistant (PDA). American Medical Informatics Association Annual Symposium Proceedings 210–214.
Espino JU, Wagner MM. 2001. Accuracy of ICD-9-coded chief complaints and diagnoses for the detection of acute respiratory illness. American Medical Informatics Association Annual Symposium Proceedings 164–168.
Evans RS, Pestotnik SL, Classen DC, Clemmer TP, Weaver LK, Orme JF Jr, Lloyd JF, Burke JP. 1998. A computer-assisted management program for antibiotics and other antiinfective agents. New England Journal of Medicine 338(4):232–238.
Field MH. 2004. The perils of CPOE. Lancet 363(9402):86.
Fleischauer AT, Silk BJ, Schumacher M, Komatsu K, Santana S, Vaz V, Wolfe M, Hutwagner L, Cono J, Berkelman R, Treadwell T. 2004. The validity of chief complaint and discharge diagnosis in emergency department-based syndromic surveillance. Academic Emergency Medicine 11(12):1262–1267.
Frist WH. 2005. Shattuck lecture: Health care in the 21st century. New England Journal of Medicine 352(3):267–272.
Gallagher EJ. 2002. How well do clinical practice guidelines guide clinical practice? Annals of Emergency Medicine 40(4):394–398.
GAO (U.S. Government Accountability Office). 2004. Homeland Security: Effective Regional Coordination Can Enhance Emergency Preparedness. Washington, DC: Government Printing Office.
Goldsmith J, Blumenthal D, Rishel W. 2003. Federal health information policy: A case of arrested development. Health Affairs 22(4):44–55.
Gordon JA, McLaughlin S, Shapiro M, Spillane L, Bond W. 2004. Simulation in Emergency Medicine. Loyd GE, Lake CL, Greenberg R, eds. Philadelphia, PA: Hanley and Belfus.
Halamka J, Overhage JM, Ricciardi L, Rishel W, Shirky C, Diamond C. 2005. Exchanging health information: Local distribution, national coordination. As more communities develop information-sharing networks, a coordinated approach is essential for linking these networks. Health Affairs 24(5):1170–1179.
Halamka JD, Szolovits P, Rind D, Safran C. 1997. A WWW implementation of national recommendations for protecting electronic health information. Journal of the American Medical Informatics Association 4(6):458–464.
Halvorson GC. 2005. Wiring health care. Healthcare cannot be reengineered without data. Health Affairs 24(5):1266–1268.
Handler JA, Gillam M, Sanders AB, Klasco R. 2000. Defining, identifying, and measuring error in emergency medicine. Academic Emergency Medicine 7(11):1183–1188.
Handler JA, Feied CF, Coonan K, Vozenilek J, Gillam M, Peacock PR Jr, Sinert R, Smith MS. 2004. Computerized physician order entry and online decision support. Academic Emergency Medicine 11(11):1135–1141.
Harris Interactive. 2001. U.S. Trails Other English Speaking Countries in Use of Electronic Medical Records and Electronic Prescribing. [Online]. Available: http://www.harrisinteractive.com/news/allnewsbydate.asp?NewsID=367 [accessed July 1, 2005].
Haukoos JS, Witt MD, Zeumer CM, Lee TJ, Halamka JD, Lewis RJ. 2002. Emergency department triage of patients infected with HIV. Academic Emergency Medicine 9(9): 880–888.
HRSA (Health Resources and Services Administration). 2003. United States Health Workforce Personnel Factbook. Washington, DC: Bureau of Health Professions.
Healthcare Information and Management Systems Society. 2005. 16th Annual HIMMS Leadership Survey, February 2005. [Online]. Available: http://www.himms.org/2005survey/ [accessed July 1, 2005].
Helmreich RL. 2000. On error management: Lessons from aviation. British Medical Journal 320(7237):781–785.
Henley RR, Wiederhold G. 1975. An Analysis of Automated Ambulatory Medical Record Systems. San Francisco, CA: AARMS Study Group, University of California-San Francisco.
Hillestad R, Bigelow J, Bower A, Girosi F, Meili R, Scoville R, Taylor R. 2005. Can electronic medical record systems transform health care? Potential health benefits, savings, and costs. The adoption of interoperable EMR systems could produce efficiency and safety savings of $142–$371 billion. Health Affairs 24(5):1103–1117.
Holbrook A, Keshavjee K, Troyan S, Pray M, Ford PT, COMPETE Investigators. 2003. Applying methodology to electronic medical record selection. International Journal of Medical Informatics 71(1):43–50.
Hospital Financial Management Association. 1976. State of Information Processing in the Health Care Industry. Chicago, IL: Hospital Financial Management Association.
Hunt DL, Haynes RB, Hanna SE, Smith K. 1998. Effects of computer-based clinical decision support systems on physician performance and patient outcomes: A systematic review. Journal of the American Medical Association 280(15):1339–1346.
IOM (Institute of Medicine). 1991. The Computer-Based Patient Record: An Essential Technology for Health Care. Washington, DC: National Academy Press.
IOM. 2001. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academy Press.
IOM. 2003. Patient Safety: Achieving a New Standard for Care. Washington, DC: The National Academies Press.
IOM. 2004a. Health Literacy: A Prescription to End Confusion. Washington, DC: The National Academies Press.
IOM. 2004b. Quality Through Collaboration: The Future of Rural Health. Washington, DC: The National Academies Press.
Jensen J. 2004. United hospital increases capacity usage, efficiency with patient-flow management system. Journal of Healthcare Information Management 18(3):26–31.
Jolly BT, Scott JL, Sanford SM. 1995. Simplification of emergency department discharge instructions improves patient comprehension. Annals of Emergency Medicine 26(4): 443–446.
Kassirer JP. 2000. Patients, physicians, and the internet. Health Affairs 19(6):115–123.
Kaushal R, Bates DW. 2001. Computerized physician order entry (CPOE) with clinical decision support systems (CDSSs). In: Shojania KG, Bradford DW, McDonald KM, Wachter RM, eds. Evidence Report/Technology Assessment. Vol. 43 (AHRQ Publication No. 01-E058). Rockville, MD: Agency for Healthcare Research and Quality.
Kellermann AL, Bartolomeos K, Fuqua-Whitley D, Sampson TR, Parramore CS. 2001. Community-level firearm injury surveillance: Local data for local action. Annals of Emergency Medicine 38(4):423–429.
Kilpatrick ES, Holding S. 2001. Use of computer terminals on wards to access emergency test results: A retrospective audit. British Medical Journal 322(7294):1101–1103.
Kleinke JD. 2005. Dot-Gov: Market failure and the creation of a national health information technology system. The market has failed to produce a viable health information technology system; we need government intervention instead. Health Affairs 24(5):1246–1262.
Koval D. 2005. Real-world RHIO. A regional health information organization blazes a trail in upstate New York. Journal of American Health Information Management Association 76(3):44–48.
Kundel HL, Polansky M, Dalinka MK, Choplin RH, Gefter WB, Kneelend JB, Miller WT Sr, Miller WT Jr. 2001. Reliability of soft-copy versus hard-copy interpretation of emergency department radiographs: A prototype study. American Journal of Roentgenology 177(3):525–528.
Kuperman GJ, Teich JM, Tanasijevic MJ, Ma’Luf N, Rittenberg E, Jha A, Fiskio J, Winkelman J, Bates DW. 1999. Improving response to critical laboratory results with automation: Results of a randomized controlled trial. Journal of the American Medical Informatics Association 6(6):512–522.
Kuperman GJ, Teich JM, Gandhi TK, Bates DW. 2001. Patient safety and computerized medication ordering at Brigham and Women’s Hospital. Joint Commission Journal on Quality Improvement 27(10):509–521.
Lee JK, Renner JB, Saunders BF, Stamford PP, Bickford TR, Johnston RE, Hsaio HS, Phillips ML. 1998. Effect of real-time teleradiology on the practice of the emergency department physician in a rural setting: Initial experience. Academic Radiology 5(8):533–538.
Lee-Lewandrowski E, Corboy D, Lewandrowski K, Sinclair J, McDermot S, Benzer TI. 2003. Implementation of a point-of-care satellite laboratory in the emergency department of an academic medical center. Impact on test turnaround time and patient emergency department length of stay. Archives of Pathology & Laboratory Medicine 127(4):456–460.
The Lewin Group. 2005. Health Information Technology Leadership Panel, Final Report. Falls Church, VA: The Lewin Group.
Lin YH, Jan IC, Ko PC, Chen YY, Wong JM, Jan GJ. 2004. A wireless PDA-based physiological monitoring system for patient transport. IEEE Transactions on Information Technology in Biomedicine 8(4):439–447.
Lombardo J, Burkom H, Elbert E, Magruder S, Lewis SH, Loschen W, Sari J, Sniegoski C, Wojcik R, Pavlin J. 2003. A systems overview of the electronic surveillance system for the early notification of community-based epidemics (Essence II). Journal of Urban Health 80(2 Suppl. 1):i32–i42.
Loonsk JW, CDC (Centers for Disease Control and Prevention). 2004. Biosense: A national initiative for early detection and quantification of public health emergencies. Morbidity & Mortality Weekly Report 53(Suppl.):53–55.
Mandl KD, Overhage JM, Wagner MM, Lober WB, Sebastiani P, Mostashari F, Pavlin JA, Gesteland PH, Treadwell T, Koski E, Hutwagner L, Buckeridge DL, Aller RD, Grannis S. 2004. Implementing syndromic surveillance: A practical guide informed by the early experience. Journal of the American Medical Informatics Association 11(2):141–150.
Manhattan Research. 2002. CyberCitizen Health V2.0. New York: Manhattan Research.
Marcin JP, Schepps DE, Page KA, Struve SN, Nagrampa E, Dimand RJ. 2004. The use of telemedicine to provide pediatric critical care consultations to pediatric trauma patients admitted to a remote trauma intensive care unit: A preliminary report. Pediatric Critical Care Medicine 5(3):251–256.
Marinakis HA, Zwemer FL Jr. 2003. An inexpensive modification of the laboratory computer display changes emergency physicians’ work habits and perceptions. Annals of Emergency Medicine 41(2):186–190.
McDonald CJ. 1976. Protocol-based computer reminders, the quality of care and the non-perfectability of man. New England Journal of Medicine 295(24):1351–1355.
McDonald CJ, Schadow G, Suico J, Overhage JM. 2001. Data standards in health care. Annals of Emergency Medicine 38(3):303–311.
Merrill CT, Elixhauser A. 2005. Hospitalization in the United States, 2002 (HCUP Fact Book No. 6, AHRQ Publication No. 05-0056). Rockville, MD: Agency for Healthcare Research and Quality.
Middleton B. 2005. Achieving U.S. health information technology adoption: The need for a third hand government intervention, judiciously and gently applied, can give the extra assistance needed to boost hit adoption nationwide. Health Affairs 24(5):1269–1272.
Mostashari F, Fine A, Das D, Adams J, Layton M. 2003. Use of ambulance dispatch data as an early warning system for communitywide influenzalike illness, New York City. Journal of Urban Health 80(2 Suppl. 1):i43–i49.
Murray MD. 2001. Automated medication dispensing devices. In: Shojania KG, Bradford DW, McDonald KM, Wachter RM, eds. Evidence Report/Technology Assessment. Vol. 43 (AHRQ Publication No. 01-E058). Rockville, MD: Agency for Healthcare Research and Quality.
NHTSA (National Highway and Traffic Safety Administration). 1996. Emergency Medical Services Agenda for the Future. Washington, DC: Government Printing Office.
O’Brien GM, Stein MD, Fagan MJ, Shapiro MJ, Nasta A. 1999. Enhanced emergency department referral improves primary care access. American Journal of Managed Care 5(10):1265–1269.
Oren E, Shaffer ER, Guglielmo BJ. 2003. Impact of emerging technologies on medication errors and adverse drug events. American Journal of Health-System Pharmacy 60(14):1447–1458.
Overhage JM, Tierney WM, Zhou XH, McDonald CJ. 1997. A randomized trial of “corollary orders” to prevent errors of omission. Journal of the American Medical Informatics Association 4(5):364–375.
Overhage JM, Dexter PR, Perkins SM, Cordell WH, McGoff J, McGrath R, McDonald CJ. 2002. A randomized, controlled trial of clinical information shared from another institution. Annals of Emergency Medicine 39(1):14–23.
Pallin D, Lahman M, Baumlin K. 2003. Information technology in emergency medicine residency-affiliated emergency departments. Academic Emergency Medicine 10(8): 848–852.
Pozen MW, D’Agostino RB, Selker HP, Sytkowski PA, Hood WB Jr. 1984. A predictive instrument to improve coronary-care-unit admission practices in acute ischemic heart disease. A prospective multicenter clinical trial. New England Journal of Medicine 310(20):1273–1278.
Redfern RO, Langlotz CP, Abbuhl SB, Polansky M, Horii SC, Kundel HL. 2002. The effect of PACS on the time required for technologists to produce radiographic images in the emergency department radiology suite. Journal of Digital Imaging 15(3):153–160.
Sands DZ, Halamka JD. 2004. PatientSite: Patient-centered communication, services, and access to information. In: Nelson R, Ball MJ, eds. Consumer Informatics: Applications and Strategies in Cyber Health Care. New York: Springer-Verlag. Pp. 20–32.
Schenkel S. 2000. Promoting patient safety and preventing medical error in emergency departments. Academic Emergency Medicine 7(11):1204–1222.
Shaw CI, Kacmarek RM, Hampton RL, Riggi V, Masry AE, Cooper JB, Hurford WE. 2004. Cellular phone interference with the operation of mechanical ventilators. Critical Care Medicine 32(4):928–931.
Shea S, DuMouchel W, Bahamonde L. 1996. A meta-analysis of 16 randomized controlled trials to evaluate computer-based clinical reminder systems for preventive care in the ambulatory setting. Journal of the American Medical Informatics Association 3(6):399–409.
Shortliffe EH. 2005. CPOE and the facilitation of medication errors. Journal of Biomedical Informatics 38(4):257–258.
Shu K, Boyle D, Spurr C, Horsky J, Heiman H, O’Connor P, Lepore J, Bates DW. 2001. Comparison of time spent writing orders on paper with computerized physician order entry. Medical Informatics 10(Pt. 2):1207–1211.
Smith MS, Feied CF. 1998. The next-generation emergency department. Annals of Emergency Medicine 32(1):65–74.
Strok B, Speedie SM, Ratner ER. 2003. A novel way of distributing medical practice guidelines using personal digital assistants (PDA). American Medical Informatics Association Annual Symposium Proceedings 1021.
Tanabe P, Gimbel R, Yarnold PR, Kyriacou DN, Adams JG. 2004. Reliability and validity of scores on the emergency severity index version 3. Academic Emergency Medicine 11(1):59–65.
Taylor TB. 2004. Information management in the emergency department. Emergency Medicine Clinics of North America 22(1):241–257.
Teich JM, Merchia PR, Schmiz JL, Kuperman GJ, Spurr CD, Bates DW. 2000. Effects of computerized physician order entry on prescribing practices. Archives of Internal Medicine 160(18):2741–2747.
Teich JM, Wagner MM, Mackenzie CF, Schafer KO. 2002. The informatics response in disaster, terrorism, and war. Journal of the American Medical Informatics Association 9(2):97–104.
Thompson DA, Yarnold PR, Williams DR, Adams SL. 1996. Effects of actual waiting time, perceived waiting time, information delivery, and expressive quality on patient satisfaction in the emergency department. Annals of Emergency Medicine 28(6):657–665.
Thompson TG, Brailer DJ. 2004. The Decade of Health Information Technology: Delivering Consumer-Centric and Information-Rich Health Care, Framework for Strategic Action. Washington, DC: U.S. DHHS.
Tierney WM, Miller ME, Overhage JM, McDonald CJ. 1993. Physician inpatient order writing on microcomputer workstations. Effects on resource utilization. Journal of the American Medical Association 269(3):379–383.
Tierney WM, McDonald CJ, Hui SL, Martin DK. 1988. Computer predictions of abnormal test results. Effects on outpatient testing. Journal of the American Medical Association 259(8):1194–1198.
Tri JL, Hayes DL, Smith TT, Severson RP. 2001. Cellular phone interference with external cardiopulmonary monitoring devices. Mayo Clinic Proceedings 76(1):11–15.
Tsui FC, Espino JU, Dato VM, Gesteland PH, Hutman J, Wagner MM. 2003. Technical description of rods: A real-time public health surveillance system. Journal of the American Medical Informatics Association 10(5):399–408.
Urban MJ, Edmondson DA, Aufderheide TP. 2002. Prehospital 12-lead ECG diagnostic programs. Emergency Medicine Clinics of North America 20(4):825–841.
Vincente K. 2004. The Human Factor: Revolutionizing the Way People Live with Technology. New York: Taylor and Francis.
Vozenilek J, Huff JS, Reznek M, Gordon JA. 2004. See one, do one, teach one: Advanced technology in medical education. Academic Emergency Medicine 11(11):1149–1154.
Vukmir RB, Kremen R, Ellis GL, DeHart DA, Plewa MC, Menegazzi J. 1993. Compliance with emergency department referral: The effect of computerized discharge instructions. Annals of Emergency Medicine 22(5):819–823.
Wears RL, Perry SJ. 2002. Human factors and ergonomics in the emergency department. Annals of Emergency Medicine 40(2):206–212.
Wellwood J, Johannessen S, Spiegelhalter DJ. 1992. How does computer-aided diagnosis improve the management of acute abdominal pain? Annals of the Royal College of Surgeons of England 74(1):40–46.
Wexler JR, Swender PT, Tunnessen WW Jr, Oski FA. 1975. Impact of a system of computer-assisted diagnosis. Initial evaluation of the hospitalized patient. American Journal of Diseases of Children 129(2):203–205.
Wuerz RC, Milne LW, Eitel DR, Travers D, Gilboy N. 2000. Reliability and validity of a new five-level triage instrument. Academic Emergency Medicine 7(3):236–242.












































