6
The Emergency Care Workforce
Emergency care is delivered in an inherently challenging environment, often requiring providers to make quick life-and-death decisions based on minimal information. Many who enter the emergency care profession enjoy the challenging work and the high-pressure environment, and take satisfaction in providing care to patients in urgent need. But providers on the front lines of emergency care increasingly express frustration with the deteriorating state of the emergency care system and the health care safety net. They experience the imbalance between demand and capacity described in earlier chapters on a daily basis, and find themselves spending an increasing proportion of their time on such tasks as getting patients admitted to crowded inpatient units; finding specialists willing to come in during the middle of the night; and finding psychiatric centers, skilled nursing facilities, or specialists who are willing to accept referrals. They also face a rigid regulatory environment that can make it difficult to address patients’ needs in the most efficient, effective, and patient-centered manner.
This chapter describes the professionals working in the emergency department (ED) and addresses the unique challenges hospitals face in staffing EDs. A wide range of professionals deliver care in the ED, including physicians from multiple specialties, nurses, physician assistants, emergency medical technicians (EMTs), social workers, pharmacists, and technicians. The chapter begins with an overview of the roles and responsibilities, training, and demographic characteristics of these workers. The rest of the chapter addresses the committee’s concerns with regard to the size, competency, effectiveness, and safety of the ED workforce.
PHYSICIANS
Several different types of physicians work in the ED extensively. With the exception of many rural hospitals, most hospitals have full-time coverage by emergency physicians, although the training and background of those physicians can vary considerably. Larger hospitals, particularly those designated as trauma centers, also have a host of other types of physicians on staff who can respond in the event a patient needs specialized medical care beyond what emergency physicians are trained to provide.
Emergency Physicians
Emergency physicians evaluate the presenting problems of patients, make diagnoses, and initiate treatment. They must be prepared for a wide variety of medical emergencies, and for this reason must be well versed in the emergency care aspects of such diverse subjects as anesthesia, cardiology, critical care, environmental illness, neurosciences, obstetrics/gynecology, ophthalmology, pediatrics, psychiatry, resuscitation, toxicology, trauma, disaster management, and wound management. In addition, because they often represent the sole source of primary care for patients whose only access to care is through EDs, they must be expert at delivering care for minor illnesses and injuries, providing care for chronic conditions, and delivering primary and preventive care. Emergency physicians also have specialized responsibilities beyond their scheduled clinical duties. A survey by Moorhead and colleagues (2002) found that physicians spend several hours per week performing unscheduled clinical duties; administrative work, such as ED quality improvement; medical direction of emergency medical services (EMS); supervision of midlevel providers, such as physician assistants (PAs) and nurse practitioners (NPs); teaching; and research. Many ED physicians also must serve on call for the ED (Moorhead et al., 2002).
Emergency physician staffing models are quite different from those seen in most other specialties. The Physician Socioeconomic Statistics Survey (AMA, 2003) found that 32 percent of emergency medicine physicians are self-employed, 19.8 percent are independent contractors, and 48.2 percent are employees. Of the employees, 29.6 percent are employed by freestanding centers or group practices and 66.8 percent by hospitals, medical schools, or state and local governments. These figures suggest that approximately 14 percent (29.6 percent of 48.2 percent) of emergency physicians are employed by contract management groups (CMGs), although there are conflicting data on this point. One survey of board-certified emergency physicians estimated only 18 percent to be employed by a multihospital contract company (Plantz et al., 1998). However, this study did not survey physicians who staffed the ED but were not board certified and was limited by its relatively small size (465 responses out of 1,050 surveyed). The
American Academy of Emergency Medicine estimates that approximately half of all EDs are staffed by large, national CMGs with majority ownership by non-physicians (Scaletta, 2003). Many of these are small, rural EDs that are unable to attract board certified emergency physicians. Penetration of CMGs is generally lower among large and urban hospitals.
A specialty in emergency medicine exists for physicians wishing to practice in the ED. Emergency medicine residency training involves 3–4 years of specialized training after medical school (see Box 6-1). Approximately 62 percent of physicians who identify their primary site of practice as a hospital ED are board certified in emergency medicine. Academic medical centers and large private hospitals in urban areas are much more likely than other types of hospitals to have residency-trained and board-certified emergency medicine physicians (Moorhead et al., 2002).
Physicians Not Board Certified in Emergency Medicine
Approximately 38 percent of practicing ED physicians are neither board certified nor residency trained in emergency medicine. EDs in suburban and rural locations are more likely to be staffed by emergency physicians that are not residency trained or board certified in emergency medicine than are academic medical centers and large urban hospitals (Moorhead et al., 2002). The majority (84 percent) of these physicians have completed a residency in another specialty, most commonly family practice or internal medicine (Moorhead et al., 2002).
The supply of board-certified emergency physicians is not sufficient to staff all ED physician positions, and in the absence of a large-scale expansion of training in the field will not be sufficient for several decades (Holliman et al., 1997). Therefore, physicians from other disciplines (e.g., internal medicine, family practice, pediatrics) are currently filling positions in EDs. Although they lack board certification, these physicians represent an essential component of the ED workforce at many hospitals, especially smaller facilities in suburban and rural settings. Many acquire a high level of competency in emergency care through a combination of postresidency education, directed skills training, and on-the-job experience.
Demographics
It is difficult to determine precisely how many ED physicians practice in the United States. A 2002 study of the emergency physician workforce in 1999 estimated that approximately 32,000 physicians were working in EDs in 1999, a figure that includes both board-certified and non-board-certified emergency medicine physicians (Moorhead et al., 2002). In a 2004 American Medical Association (AMA) physician survey, however, 25,500 physi-
|
BOX 6-1 The Specialty of Emergency Medicine The specialty of emergency medicine began to organize in the mid-1960s in response to the growing demand by hospitals for full-time emergency room physicians. The American College of Emergency Physicians (ACEP) was founded in 1968 (Danzl and Munger, 2000). In 1970, leaders in emergency medicine established an educational curriculum for residency training, and the first emergency medicine residency program began at the University of Cincinnati. By 1975 there were 23 approved residency programs in the United States. In 1976, a Section on Emergency Medicine was formed at the American Medical Association, and pressure grew for the American Board of Medical Specialties (ABMS) to recognize the specialty. The American Board on Emergency Medicine (ABEM) was established in 1976, but the ABMS did not formally recognize it. The development of the specialty was initially resisted by physicians who believed that training in another discipline, such as internal medicine or family practice, was sufficient to practice emergency medicine (Rosen, 1995). Moreover, emergency medicine represented competition for “adjacent” specialties, such as trauma surgery, cardiology, and primary care. After 3 years of negotiations, however, the ABEM was accepted as a modified-conjoint board, making emergency medicine the twenty-third medical specialty (Rosen, 1995). The ABMS finally granted primary board status to the ABEM in 1989. In 1980, 600 emergency physicians sat for the first certification exam. Emergency medicine developed a critical mass of specialists by allowing experienced practitioners to sit for the certifying exam until 1988, when the “practice track” to board certification was phased out (Marx, 2005). Approximately 20 percent of emergency physicians are board certified as emergency medicine physicians but not residency trained in emergency medicine (Moorhead et al., 2002). Since this “grandfather” track is no longer open, the number of physicians certified through this pathway will decrease over time and eventually disappear. Board certification has also been granted by the American Osteopathic Board of Emergency Medicine (AOBEM) since 1980, and now includes additional certifications in toxicology and sports medicine. In addition to ACEP, another small but growing emergency medicine specialty practice group is the American Academy of Emergency Medicine (AAEM). The |
cians self-identified themselves as having an emergency medicine specialty (AMA, 2004); this number likely includes some physicians not board certified in emergency medicine but practicing in an ED on a full-time basis.
The AMA survey also provided some basic demographic information on those physicians. The composition of practicing self-identified emergency
|
AAEM was formed in 1993 as an organization limited to those emergency physicians with ABEM/ABOEM certification or eligibility for such certification. It has a particular focus on issues related to fair business practices (e.g., open books, physician practice ownership, contract negotiations) with respect to contract management companies. Residency training requirements for emergency medicine physicians were established by the Accreditation Council for Graduate Medical Education, and since then, accredited emergency medicine residency programs have been growing at a rapid rate—from 1 in 1970 to 43 in 1980, 81 in 1990, and 132 in 2005. A recent report cites 3,909 new emergency medicine physicians being trained in accredited residency programs (ACEP Research Committee, 2005). In 2003, board-certified emergency physicians and pediatric emergency physicians were available at 63.5 percent and 18.1 percent of emergency departments, respectively (McCaig and Burt, 2005). Emergency medicine has demonstrated a regular increase in the percentage of U.S. medical students entering the specialty, growing from 2 percent in 1987 to 4 percent in 2002. There are now several subspecialties within emergency medicine: pediatric emergency medicine, medical toxicology, sports medicine, and undersea and hyperbaric medicine. There are also a number of nonaccredited fellowships not funded by Medicare’s Graduate Medical Education (GME) funding that emergency medicine physicians may pursue. These include disaster medicine, medical direction of emergency medical services, ultrasound, health services research, and international emergency medicine. A small number of emergency physicians hold Board Certification in Emergency Medicine (BCEM) from the American Board of Physician Specialties. This certification, which requires completion of a residency in some field plus 5 years of clinical practice in emergency medicine, is recognized only in Florida (ABPS, 2005). While residency programs have grown at a rapid pace, academic departments in emergency medicine have progressed more gradually. The Society of Academic Emergency Medicine (SAEM) was formed in 1989 through the merger of the University Association for Emergency Medicine (UAEM) and the Society of Teachers of Emergency Medicine (STEM) to foster the development of academic emergency medicine and promote research in the field. Today there are 64 autonomous departments of emergency medicine at U.S. medical schools and 135 emergency medicine residency programs. |
medicine physicians is less diverse than that of the general physician population. Eighty-three percent of self-identified emergency physicians are non-Hispanic white, compared with 75 percent of physicians overall. The primary difference, however, appears to be the lower number of Asians in emergency medicine: in 2002, Asians represented 13 percent of all physicians but only
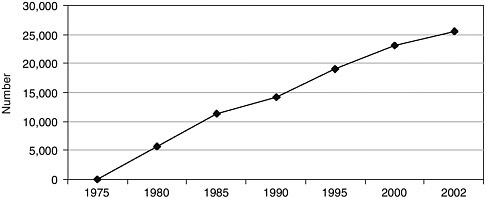
FIGURE 6-1 Number of nonfederal emergency medicine physicians in the United States, 1975 to 2002.
SOURCE: AMA, 2004.
7 percent of emergency medicine physicians. Additionally, only 20 percent of emergency medicine physicians are women, compared with 25 percent of all physicians. Emergency medicine physicians also tend to be younger than other physicians. Nearly one-quarter were under the age of 35 in 2002, and fully half were under the age of 45; among the overall physician population, 59 percent of physicians were aged 45 and older (AMA, 2004).
The number of self-identified emergency physicians in the United States has increased substantially since 1979, when emergency medicine was first recognized as a specialty (see Figure 6-1). Growth in emergency medicine has been much stronger than that in medicine overall. Since 1990, the number of self-identified emergency physicians in the United States has increased from 14,000 to more than 25,500—an increase of 79 percent compared with a 39 percent increase in the number of all physicians. One of the key reasons for the rapid growth in emergency medicine residency programs is that academic medical centers find these programs quite useful for staffing their own EDs. The “fill rate” of emergency medicine residency positions is quite high, reflecting the fact that the field is a popular career choice for U.S. medical students.
Physician Payment
ED physicians often are not hospital employees and are reimbursed separately from the hospital. Medicare physician payment is based on a resource-based relative value scale (RBRVS). The provider reports to the payer the service’s Current Procedural Terminology (CPT) evaluation/management (E/M) code, which describes the intensity of the physician service
given. Over 80 percent of ED care falls under the five emergency care CPT E/M codes (ACEP, 2004). The codes are converted by the Centers for Medicare and Medicaid Services (CMS) into relative value units (RVUs) and modified by area factors. There are three RVU categories: physician work, practice expense, and professional liability. Each of these RVUs is multiplied by a corresponding geographical practice cost index (GPCI). Medicare then pays the physician 80 percent of the charge, and the patient is responsible for the other 20 percent. An anomaly of reimbursement for emergency physicians is that they are sometimes not credited for some of the tasks they perform. In many cases, the emergency physician is the first to read a patient’s electrocardiogram (EKG) or x-ray and use it to make the relevant clinical decisions. Hospital radiologists and cardiologists sometimes read these results and dictate interpretations hours or even days after treatment has been rendered, and then bill for the service. CMS will reimburse only one physician for each interpretation, and payment often goes to whoever rereads the study at a later time rather than to the emergency physician who applies his or her own interpretation to real-time patient care decisions.
Medicaid programs use similar systems that have different rates and details (Kaiser Commission on Medicaid and the Uninsured, 2003). In fact, over 70 percent of all ED physician payments for both public and private care are derived from an RBRVS (ACEP, 2004).
Uncompensated Care
The American College of Emergency Physicians (ACEP) has been active in an effort to increase the practice expense RVU, including a push to count uncompensated care mandated by the 1986 Emergency Medical Treatment and Active Labor Act (EMTALA) toward that RVU. An AMA survey of physicians in 2000 estimated that emergency physicians incurred an annual average of $138,000 in bad debt by providing care mandated by EMTALA (Kane, 2003). Actual foregone income is probably substantially less than this on average, since the $138,000 is based on charges and not actual payments. Nonetheless, a reimbursement rate of 50 percent suggests significant foregone income that has not been remediated through changes in the CMS practice expense RVU. It should be noted that other specialties that provide emergency care also deliver substantial amounts of uncompensated care and face similar economic problems. Reimbursement of on-call physicians is discussed later in this chapter.
Contract Management Groups
CMGs provide hospitals with ED physicians who work on a contract basis, allowing hospitals to staff their EDs around the clock, and they
often provide contract management services, including coding and billing (McNamara, 2006). About 16 percent of emergency physicians are employed by a CMG company. If independent contractors are included, however, this figure rises to close to 40 percent of emergency physicians (AMA, 2004).
Contracting with a CMG is an attractive option for some rural hospitals because it guarantees full-time physician coverage of the ED (Williams et al., 2001). The availability of an ED staff also helps attract physicians from other specialties, who are relieved of the need to staff the ED on a rotating basis. CMGs may be an attractive option for physicians as well as they handle many of the business details of practice, such as billing, and provide health and other benefits. These advantages may come at a price, however. In some areas of the country, CMG companies represent such a large share of emergency physician practices that it may be difficult for a physician to practice emergency medicine unless employed by a CMG, which may require physicians to sign noncompete agreements.
Moonlighting
The pressing need for ED physicians frequently leads hospitals to augment their staffs with emergency medicine residents, known as “moonlighters,” often to cover evening and weekend shifts. While typically emergency medicine residents, these moonlighters may also include nonemergency physicians and residents training in other specialties, who usually have no specific training or qualifications in emergency medicine (Kellermann, 1995). More than half of all emergency residents reported moonlighting in one survey, though not all in EDs (Li et al., 2000); they cited a variety of reasons for doing so, including supplementing their income and enhancing their educational experience. The practice is discouraged by the emergency medicine specialty organizations because it may place both the resident and the patient at risk, especially when there is no experienced backup in the ED (Keim and Chisholm, 2000). In addition to moonlighters, some physicians working in EDs are provided by “locum tenens” firms that supply physicians to hospital EDs to fill staffing gaps on an as-needed basis.
Trauma Surgeons
The other specialty of particular relevance to emergency care is the surgical subspecialty of trauma/critical care surgery. Trauma is defined as any bodily injury severe enough to pose a threat to life and limb. It requires an organized emergency response that guarantees immediate intervention, including, if needed, the immediate commencement of surgery. Trauma is a major national health problem and remains the leading cause of death for
all Americans under age 44. In addition, it takes a huge economic toll on society as it accounts for the greatest loss of productive life in the nation. Trauma care requires a systemic approach that mandates coordination of all prehospital and hospital-based services to optimize care and outcomes. Trauma often occurs during off hours, and trauma centers are therefore busier at night and on weekends and holidays. This requires a 24-hour-a-day operational status that is costly in terms of both facility and human resources.
Most severe trauma care is directed by trauma surgeons who are general surgeons with a special commitment to the provision, management, and organization of trauma care within their hospital and region. The term “trauma surgeon” usually refers to a person trained in general surgery who has an additional 1 to 2 years of training in trauma surgery and critical care. These surgeons focus their practice and expertise on trauma surgery and care management, surgical critical care, and recently all emergency general and vascular surgery. They generally complete a minimum of 7 years of residency training—a complete 5-year general surgery residency, followed by 2 years of fellowship training in trauma surgery and surgical critical care. The American College of Surgeons estimates that there are currently about 3,000 trauma surgeons practicing in the United States (Personal communication, C. Williams, February 17, 2006).
Trauma surgeons tend to focus their practice in specially designated units known as trauma centers. Indeed, a key component of the trauma center designation process is documentation of continuous coverage by trauma surgeons. For level I designation, a trauma surgeon must be available 24 hours a day, 7 days a week. Most level I and some level II trauma centers have trauma surgeons in house 24 hours a day, 7 days a week, who are responsible for all aspects of care of the trauma patient. Trauma care is also provided by emergency physicians, especially in some level II, III, and IV trauma centers. Subspecialists in anesthesia, emergency medicine, orthopedics, neurosurgery, radiology, and, in some states, rehabilitation medicine are required for all level I and II trauma center accreditation.
In the last 30 years, the development of trauma centers and trauma systems has been recognized as a key factor in improving outcomes from injuries, especially those involving vehicular crashes. In addition, trauma centers are a critical component of the safety net system and play a vital role in preparations for potential disasters, both natural and man-made, as well as for acts of terrorism. Trauma that is treated at trauma centers and within an established system has the best outcomes, with significantly lower mortality rates than those seen in non–trauma center hospitals (MacKenzie et al., 2006). The development of trauma systems and trauma surgery practice has been largely directed and codified through a series of reports by the
American College of Surgeons and its Committee on Trauma, including, most recently, the so-called “Gold Book,” The Optimal Care of the Injured Patient (Committee on Trauma, ACS, 1998).
Currently, hospitals face a decline in the numbers of trauma surgeons due to large amounts of uncompensated care, high levels of medical malpractice risk, and the burden placed by trauma practice on family life. A key factor is the low number of general surgeon trainees electing to go into trauma surgery. Today the majority of fellowships in trauma and surgical critical care are not filled. A national shortage of these specialists will become critical as trauma surgeons now in their late fifties and sixties retire. Furthermore, the trauma capacity in certain cities and regions has declined as trauma centers have closed because of high costs and high levels of uncompensated care.
Specialists Who Provide On-Call Emergency and Trauma Care Services
Hospitals that offer specialist services for inpatients, such as neurosurgery and vascular surgery, must make the same services available to patients who present at the ED (Glabman, 2005). ED physicians rely on and consult these specialists for a range of services—clinical consultation, surgical follow-up, inpatient care, and postdischarge care (Macasaet and Zun, 2005). The limited availability of certain specialists, however, is a well-documented problem that is concerning for both consumers and emergency care providers. Over the past several years, hospitals have found it increasingly difficult to secure specialists for their ED patients. In a 2004 survey by ACEP, two-thirds of ED medical directors reported shortages of on-call specialists at their hospitals (ACEP, 2004). An update to this survey found that the situation is growing worse. In 2005, 73 percent of EDs reported problems with on-call coverage, in contrast to 67 percent the year before (ACEP, 2006). Numerous other studies and surveys have investigated the shortage of on-call specialists, finding that the problem extends across many different specialties and all regions of the country and that it appears to be worsening (Green et al., 2005; O’Malley et al., 2005).
Consider the experience of a patient in San Antonio in his twenties who came to the ED with a vascular injury to his leg artery, the result of a gunshot wound. The vascular circulation needed to be repaired within 6 hours or the patient would risk losing his leg. When the patient arrived at the hospital, ED staff attempted to contact the specialist on call, but he was in surgery and could not respond. Another on-call surgeon was also unavailable because he was performing surgery. The ED staff ultimately decided to transfer the patient hundreds of miles away to a hospital with the expertise to treat him. By the time the patient arrived, however, too much time had elapsed for his leg to be saved (Glabman, 2005). EMTALA
currently requires hospitals to have contingency plans for such situations, but unfortunately many do not.
The experience of this patient in San Antonio is not uncommon, yet it is remarkable. One would expect the city to have adequate specialty resources to care for a patient with such an injury. Another reason why the shortage of on-call specialists is remarkable is because it affects all patients, regardless of income or insurance status; insured patients are at the same risk as uninsured patients of not having a specialist available when needed.
Surveys of hospital administrators, ED staff, and specialists indicate that there are at least five underlying factors affecting the availability of emergency and trauma care specialists: (1) the supply of specialists, (2) compensation for providing emergency services, (3) quality-of-life issues, (4) liability concerns, and (5) relaxed EMTALA requirements for on-call panels (Yoo et al., 2001; California Healthcare Association, 2003; Taheri and Butz, 2004; Green et al., 2005; Salsberg, 2005). Each of these factors is discussed in turn below.
Supply of Specialists
Hospital by-laws often require physicians to take ED call for a certain period of time (e.g., 15 years) in exchange for admitting privileges. Historically, this arrangement worked well; it allowed hospitals to fill their on-call panel and gave young specialists an opportunity to build up their practices. But with the movement of specialists to large, multispecialty groups, younger physicians no longer need to rely on ED call to supply patients. Hospitals have less leverage to tie admitting privileges to ED call, and many groups discourage their members from taking ED call (Taheri and Butz, 2004).
The availability of on-call specialists is also dependent upon the local supply of specialists. If there are many specialists in the market, they may be more likely to serve on emergency call panels to draw new patients into their practices, assuming that some of these patients are insured. On the other hand, if there are shortages of certain specialists in a market, those specialists will likely be able to fill their practices without taking call. Indeed, in many areas of the country there is a shortage of certain specialists needed to cover the ED (GAO, 2003a). One reason is that medical school enrollment has not kept pace with the growing population. Neurosurgery is a good example of this point. Despite substantial increases in the U.S. population and in the number of trauma visits, there were fewer practicing neurosurgeons in 2002 (3,050) than there were 12 years earlier. There are far fewer neurosurgeons in the United States than the number of EDs (4,900) (Couldwell et al., 2003). The specialty attributes this decline largely to medical liability problems (discussed below).
The shortage of available on-call specialists is a serious and complex
dilemma that appears to defy simple resolution. It reflects long-term trends in professional practice and physician supply that would take years to address even if the solution were clear. There are two approaches, however, that the committee believes warrant special consideration: regionalization of specialty services and development of an emergency surgery subspecialty.
Regionalization of specialty services Much like the regionalization of trauma services, regionalization of certain specialty services would direct patients to those hospitals having access to the needed specialists and having demonstrated superior outcomes. The intent of regionalizing specialists would be to rationalize the limited supply of specialists by facilitating agreements that would ensure coverage at the key tertiary and secondary locations based on actual need. This arrangement would replace the current haphazard approach that is based on many factors other than patient need. Without such a regional arrangement, some hospitals may have an overabundance of certain specialists while others face a constant shortage. These patterns may be based on physician practice preferences, academic affiliations, reimbursement issues, contractual arrangements, or myriad other factors. They may also be due to simple ignorance of communitywide needs. Regionalization would provide a framework for recognizing and addressing these needs and imbalances through the collection of information on specialist demand and supply and the use of that information to reallocate specialist services through various arrangements, including payment incentives.
While there is limited direct evidence regarding regionalization of on-call specialty services, the approach has proven effective in other contexts and is consistent with the committee’s broader vision of a regionalized emergency care system. There are few examples of regionalization with specific reference to emergency and trauma care specialty on-call services. One such effort is Palm Beach County’s nascent attempt to regionalize the services of certain on-call specialists through a communitywide cooperative that will contract collectively for their services (described more fully in Chapter 3). Despite the current lack of direct evidence, however, the committee believes the approach holds promise and should be encouraged and evaluated. Therefore, the committee recommends that hospitals, physician organizations, and public health agencies collaborate to regionalize critical specialty care on-call services (6.1).
Emergency surgery subspecialization To expand the pool of surgeons available to emergency and trauma patients, a new specialty designation of emergency surgeon has been proposed. The emergency surgeon would receive broad training in elective and emergency general surgery, trauma surgery, and surgical critical care. In addition to performing what is con-
ventionally considered general trauma surgery (for neck, thoracic, and abdominal injuries), the emergency surgeon could also perform selected and limited neurosurgical and orthopedic procedures, with support from fellow surgical specialists (The Committee to Develop the Reorganized Specialty of Trauma, Surgical Critical Care and Emergency Surgery, 2005). The intent is not for this new specialist to perform major neurosurgical or orthopedic procedures, but only those procedures that can safely be performed without the direct intervention of those other specialists, thus enabling them to concentrate their efforts on more difficult cases.
In the traditional surgical practice model, surgeons may end up working all night operating or covering the intensive care unit (ICU) and then spend the following day seeing their own admitted patients, a physically stressful approach. Under the proposed new model, emergency surgical services would be shared by the emergency surgery group. Each surgeon would work 8–12 hours at a stretch and then be off until the next shift, with another member of the group assuming responsibility.
There has been some controversy about the inclusion of emergent neurological and orthopedic surgical procedures in this new training curriculum. However, the need for the new emergency surgeon to perform these procedures would come into play only when neurological and orthopedic surgical specialists were not available in emergent situations. This might occur in urban facilities where the latter specialists were on staff but unwilling to provide the coverage or in rural areas where the emergency surgeon might be the only surgeon available to provide this care.
Compensation
Another reason specialists may be unwilling to take emergency call is that they often receive little or no compensation for these services because of the large numbers of uninsured and underinsured patients that present in the ED. Yoo and colleagues (2001) reported the results of a 2000 California Medical Association survey on reimbursement for on-call emergency services. Nearly 80 percent of the respondents reported difficulty in obtaining payment for their services, regardless of insurance type. Fully 54 percent responded that they received no payment for on-call services, though the frequency of nonpayment is unclear. Another 42 percent reported underpayment and payment delay. Forty percent of the physicians who took voluntary call stated that lack of payment had forced them to reduce call, while 20 percent said they would be unable to continue voluntary call under the present circumstances.
Perhaps the most common strategy has been for hospitals to provide a stipend or extra payment for physicians to take call. According to a 2004 American Hospital Association (AHA) survey, approximately 40 percent of
hospitals pay some specialists for ED call, with a median stipend of $1,000 per night (Glabman, 2005). Stipends have helped individual hospitals secure the availability of certain specialists, but the long-term viability of this strategy is questionable as the stipends are quite large for some specialists, and not all hospitals have funding to support such stipends. For example, one hospital in Miami is reportedly spending $13 million annually to compensate physicians for taking call in the ED (Mays et al., 2005). A Phoenix-area hospital reported paying each of its neurosurgical groups $10,000 per week in exchange for taking call (Hurley et al., 2005). These payments are in addition to any patient revenue the specialists may collect. Moreover, the practice of paying physicians to be on call is controversial. With many hospitals operating at a deficit, the AHA claims that hospitals cannot make these stipends a permanent feature of emergency call (Maguire, 2001). Additionally, the question of which specialists should receive payment may incite controversy across specialties.
An alternative model that may have advantages over paying stipends has been implemented successfully at Scripps Health in San Diego. This model uses an exclusive contract to secure neurosurgery coverage for the trauma center. It involves combining all emergency neurosurgery and trauma cases and issuing a request for proposals for exclusive rights to providing care for these patients. Substantial competition for the contract resulted in a qualified and committed group of neurosurgeons providing services for emergent and trauma care. The contract requires prompt response, participation in all process improvement and educational programs, and leadership in neurosurgical quality improvement. This model is likely to be more successful in areas where stipends for on-call staff are used and are rising quickly (Scheck, 2004).
Quality-of-Life Issues
The new generation of specialists appear to be less inclined to take call than their older colleagues because of quality-of-life issues. There is no question that the demands of on-call coverage are substantial. When on call, specialists may be summoned in the middle of the night and required to perform complex surgeries, diagnoses, or other services. It is not unusual for a surgeon on call to work through the night and then see a full day’s worth of patients in the office. Specialists taking daytime call may be interrupted in the middle of a busy day of seeing patients in the office, forcing patients to reschedule. Furthermore, as the availability of specialists taking emergency call declines, the burden on those who continue to take call grows. In 2003, the Accreditation Council for Graduate Medical Education (ACGME), following the earlier lead of the New York State Bell Commission, placed
strict limits on resident work hours, including the number of consecutive hours doctors in training can be required to work on call without a period of intervening sleep. The same limits do not apply to practicing physicians, and are routinely exceeded by surgical specialists and others who take overnight emergency call.
Younger physicians are assigning greater importance to the balance among work, marriage, and family time and are therefore demanding greater control over their work schedules, fewer absolute work hours, and more time devoted to their private practice (Salsberg, 2005). Further, many do not view ED call as a professional obligation to the degree that previous generations of specialists did, particularly when market factors enable them to build a successful practice without the addition of emergency patients (Taheri and Butz, 2004).
Liability Concerns
The high risk of being sued and the high costs of professional liability insurance premiums further discourage specialists from providing on-call services. Procedures performed on emergency patients are inherently risky and expose specialists to an increased likelihood of litigation. There are several reasons for this: emergency and trauma patients are often sicker than other patients and may have serious comorbidities, and the on-call physician usually has no preexisting relationship with the patient or his/her family.
Primary care physicians often refer patients with serious or complex medical problems to hospital EDs to shield themselves from liability during diagnostic workups (Berenson et al., 2003). Safety net hospitals are especially affected by the liability problem. As panels diminish at community hospitals, they increasingly transfer patients to the large safety net hospitals, which have no choice but to accept them; the result is even higher concentrations of uninsured, high-risk patients. Several reports have documented closings of trauma centers, at least temporarily, or downgrading of their status because of staffing shortages associated with liability concerns (Whaley, 2002). In the current environment of high liability risk, safety net hospitals are at risk of becoming the dumping ground for the liability crisis.
A 2004 nationwide survey of neurosurgeons conducted by the American Academy of Neurological Surgeons found that 35.8 percent of respondents had been sued by patients seen through the hospital ED (Perception Solutions, Inc., 2004). For this reason, specialists who regularly take ED call pay more for liability coverage than those who do not. An analysis of premiums paid by specialists in Palm Beach County, Florida, revealed that orthopedists who take regular ED call pay 75 percent more for malpractice insurance than orthopedists who do not take call (Taheri and Butz, 2004). One
neurosurgeon reported being told by his insurance company that he must limit coverage of the ED to 10 nights per month or his premiums would be increased to prohibitive levels (Byrne and Bagan, 2004).
Liability premiums for specialists in general have been rising at an increasing rate. Data from the Medical Liability Monitor show that premiums for general surgeons grew approximately 1 percent in 1998 and 1999, but 7 percent in 2000, 12 percent in 2001, and 21 percent in 2002 (Thorpe, 2004). The result is burdensome premiums for specialists in many areas of the country. For example, the largest underwriter of professional liability insurance in Illinois reported that the average premium in 2005 for neurosurgeons in the Chicago area was $235,000 per year for only $1 million in coverage. While $1 million may appear to be adequate coverage, nearly half of settlements in the Chicago area exceeded $1 million in 2003, and more than 10 settlements exceeded $10 million (Byrne and Bagan, 2004). Growth in physician liability premiums has not been offset by growth in revenues. In fact, patient revenues, which are often set to the Medicare payment schedule, have actually been declining, making the burden of increased premium payments even greater (Valadka, 2004).
The specific effects of liability premiums on emergency and trauma care specialists were addressed in a 2003 report by the U.S. Government Accountability Office (GAO, 2003b). The report was based on a study that compared experiences in five states having reported medical malpractice problems (crisis states) with experiences in four states not having such problems. The GAO found that in the crisis states, access to emergency care was reduced, particularly for trauma and obstetrical services; transfers of patients were increased; and the availability of on-call specialists to EDs was reduced, especially for critical specialties such as orthopedic and neurological surgery. The study further documented that reduced on-call coverage resulted in frequent delays in care and transfers of patients to alternative facilities up to 100 miles away to receive specialist care. A section of West Virginia lost all neurosurgical coverage for 2 years, requiring all emergency patients needing neurosurgical consults to be transferred more than 60 miles away. The report noted, however, that confirmed problems in access frequently involved hospitals, often rural, with long-standing problems in maintaining the availability of services.
Trauma services were affected in every state in the study. The effects included temporary trauma center closings due to loss of on-call specialist services for trauma care in West Virginia, Pennsylvania, and Nevada. In each of these cases, the state had to resolve the crisis by either providing liability coverage or making the specialists state employees, thus limiting their exposure.
The effect of placing caps on malpractice awards at the state level to ameliorate access problems has been the subject of numerous research ef-
forts over the past few years. The growing consensus is that state liability reforms have helped reduce physician liability premiums to some extent (Thorpe, 2004) and have led to some small increases in physician supply (Hellinger and Encinosa, 2005), particularly in rural areas (Encinosa and Hellinger, 2005; Matsa, 2005). However, the direct impact of these reforms on the delivery of emergency services has not been adequately examined.
A number of additional approaches could be used to protect emergency care specialists without compromising patient safety. One would be to provide “conditional immunity” for emergency physicians and specialists while seeing patients on call. Another promising approach is a public no-fault system modeled on the National Vaccine Injury Compensation System. In such a system, malpractice in emergency care would be compensated through a fund that would be supported by hospitals and physicians. Such an approach would provide much more rapid and certain compensation than the current tort system while encouraging hospitals and individual providers to address patient safety issues in a transparent and energetic manner. Alternatively, caps on noneconomic damage awards, which have been effective in some states, could be placed on emergency services (Thorpe, 2004).
Whatever liability reform strategies are used to ease the crisis in availability of emergency providers, they must be balanced by protections for patient safety. One proposed mechanism is the establishment of a national emergency care patient safety initiative. This initiative would include reporting systems for sentinel events, with penalties for failure to report incidents; a national database of patient safety events; development of standards of care; monitoring and reporting of performance standards; and corrective measures to be taken in instances of repeated problems. An additional feature that might be considered is tying protections from liability exposure to demonstrated performance on quality-of-care indicators.
Many states have enacted some form of liability reform, though the types of reforms undertaken have varied. These reforms have created a “natural experiment” through which researchers can investigate their impact. Congressional policy makers, with advice from health services researchers, should monitor the impact of these reforms at the state level and consider federal liability reform.
Because of the critical nature of the on-call specialty crisis and the substantial role that liability appears to play in creating and sustaining this crisis, the committee believes it is of crucial importance to the nation to understand more clearly the true impact of liability on specialty services, to identify the range of public policy and private initiatives that can make a significant difference in resolving the problem, and to take urgent actions based on these findings. Therefore, the committee recommends that Congress appoint a commission to examine the impact of medical malpractice lawsuits on the declining availability of providers in high-risk emergency
and trauma care specialties, and to recommend appropriate state and federal actions to mitigate the adverse impact of these lawsuits and ensure quality of care (6.2).
The committee recognizes that medical malpractice is a national issue that affects all areas of medicine, not just emergency care. But it also recognizes that the issue represents a unique and urgent challenge in emergency care that cannot wait for long-term national or state solutions. Special consideration is warranted not only because of the crisis facing emergency care, but also because of emergency care’s unique public-good characteristics. Medical emergencies are unpredictable events, and the emergency care system must maintain a state of readiness to handle them as they arise. Because individuals cannot know when they will need emergency services, they will underconsume the readiness aspect of emergency care. Government intervention is warranted to maintain an efficient level of readiness. Liability protections for emergency providers could be a stop-gap measure until broad, national legislation addressing medical malpractice reform is enacted.
Relaxed Requirements of the Emergency Medical Treatment and Active Labor Act
The responsibility of hospitals to ensure the availability of on-call staff was revisited by CMS in guidance published in September 2003. Prior to the 2003 amendment, there was considerable confusion surrounding hospitals’ on-call list responsibilities. Afraid of violating EMTALA, many hospitals adopted a “rule of three” policy, which states that if a hospital has more than three physicians in a specialty, it must provide continuous ED coverage for that specialty. Struggling to maintain their on-call lists, some hospitals required specialists to be on call 24 hours a day, 7 days a week (Russell, 2004). Complaints by on-call physicians and hospitals led to a clarification of the policy in 2003. CMS stated that EMTALA does not require hospitals to follow the “rule of three” and changed its statutory language as follows: “Each hospital must maintain an on-call list of physicians on its medical staff in a manner that best meets the needs of the hospital’s patients who are receiving services required under this section in accordance with the resources available to the hospital, including the availability of on-call physicians” (42 Code of Federal Regulations §489.24). CMS also clarified that physicians could be on call at more than one hospital simultaneously (hospitals must have procedures in place for when a physician is on call at another hospital and is unable to respond) and that surgeons could perform elective surgery while on call (Russell, 2004).
The impact of the EMTALA amendment on the supply of and access to on-call specialists is not clear. Many believe that access to on-call spe-
cialists has worsened as a result. In the example cited earlier of the patient from San Antonio, the local on-call surgeons would not have been allowed to perform elective surgeries while on call prior to the 2003 EMTALA guidance. Though it is unclear in the above example whether the on-call specialists were performing elective or emergency surgery, it is easy to see how the change to EMTALA potentially makes access to on-call specialists more difficult. But others argue that the amendment has been beneficial. Had CMS not loosened on-call requirements, they argue, more specialists might have refused to take call in the ED altogether.
As an alternative, some have advanced the idea of a more direct approach in which CMS would hold specialists rather than hospitals accountable for providing on-call services. One variation on this approach would be to require specialists to take call as a condition for Medicare participation. While the directness of this approach has some appeal, it fails to address the underlying problems, such as the declining numbers of specialists, and is indeed likely to contribute to that decline.
Hospitalists and Critical Care Specialists
Hospitalists
In 2003 more than 8,000 hospitalists—physicians who focus exclusively on managing hospital inpatients—were practicing in U.S. hospitals according to the Society of Hospital Medicine (Society of Hospital Medicine, 2006). That number is expected to reach 30,000 in the next decade. The use of hospitalists will increase as hospitals seek to reduce costs, streamline patient flow, and improve patient safety (Pham et al., 2005).
Hospitalists have traditionally been used to care for inpatients, and their service has been shown to decrease lengths of stay and reduce morbidity. Adding them to a hospital’s medical staff is an attractive option because they are generally more willing to accept emergency admissions after hours or at night, avoiding the need to involve the patient’s office-based physician. Faster acceptance by the admitting physician can help an ED maintain patient flow and reduce the risks of crowding and ambulance diversion. In some hospitals, hospitalists may provide backup when the ED is particularly busy by assisting with the disposition of patients who clearly need to be admitted. Hospitalists can also staff observation units in EDs (Dresnick, 1997).
On the other hand, hospitalists sometimes utilize ED resources (e.g., space and staff) in conducting workups of patients they are admitting, placing a drain on crowded EDs. This situation is alleviated in some hospitals by admissions units that are separate from the ED. Because hospitalists focus on inpatient care rather than traveling back and forth from their office, they are often more efficient than office-based practitioners. One hospital found
that by using hospitalists to coordinate care immediately following the admission decision, the hospital cut the average length of stay for patients admitted through the ED by 2 days, increasing bed availability (Brewster and Felland, 2004). Many hospitalists are being asked to become more involved in ED triage decisions. The theory is that hospitalists may have more time than emergency physicians to fully evaluate patients, and may also be more familiar with home care or skilled nursing facilities (Wachter, 2004). However, this strategy is not without its drawbacks. Hospitalists may refuse to be the physician of record for unassigned patients in communities with large uninsured populations, and many hospitals do not have the funding to hire hospitalists (Maguire, 2001).
Hospitalists may also help alleviate some problems with the availability of on-call staff. Hospitalists in the ED can assess the status of unassigned patients and make a determination as to whether a specialist is needed. According to a survey for the California Healthcare Foundation, emergency physicians appreciate the availability of hospitalists as timesavers, and specialists value fewer calls and fewer late-night trips to the ED. In fact, more survey respondents favored using hospitalists to address the on-call problem than favored mandating on-call coverage or contracting with a third party for call coverage. However, hospitalists are best used for medical patients and are unlikely to help alleviate problems with on-call subspecialists and surgeons (Green et al., 2005).
Critical Care Specialists/Intensivists
Critical care specialists are an essential component of emergency and trauma care in addressing the needs of severely ill and injured patients. The use of intensivists has been associated with a 30 percent reduction in hospital mortality and a 40 percent reduction in ICU mortality (Pronovost et al., 2002). Greater use of intensivists has also led to significantly reduced hospital and ICU lengths of stay (Pronovost et al., 1999). The Leapfrog Group is promoting the use of a full-time intensivist model to meet its ICU Physician Staffing standard. Currently only 10 percent of ICUs actually meet this standard (The Leapfrog Group, 2004).
As discussed earlier, because inpatient units are becoming increasingly crowded, critically ill patients are boarding in the ED for longer periods of time. This is a challenge for EDs because critically ill patients require an intensive amount of resources, including medical attention, monitoring equipment, and medications (Church, 2003). This situation has led some hospitals to use intensivists in the ED. The committee recognizes the importance of providing critical care services quickly to admitted patients but does not endorse the practice of using intensivists as a way to accommodate the practice of boarding. Instead, the committee encourages hospitals to address
the root causes of boarding so that critically ill patients are moved quickly to intensive care beds.
There is currently a severe national shortage of critical care physicians—so much so that the critical care societies have petitioned Congress to increase the number of foreign medical graduates with critical care training. Emergency physicians with subspecialty certification in critical care medicine could help address this shortage, provide a margin of safety for ED boarders, and provide extra capability in community hospitals that cannot afford to keep both types of providers on staff every night (Osborn and Scalea, 2002). However, the American Board of Medical Specialties (ABMS) currently blocks residency-trained, board-certified emergency physicians and other acute and primary care specialists from obtaining subspecialty certification in critical care. To increase the pool of well-trained intensivists in both adult and pediatric practice, the committee recommends that the American Board of Medical Specialties and its constituent boards extend eligibility for certification in critical care medicine to all acute care and primary care physicians who complete an accredited critical care fellowship program (6.3).
NURSES AND OTHER CRITICAL PROVIDERS
Nurses
There are approximately 90,000 nurses working in EDs (NHT, 2006). According to the Emergency Nurses Association (ENA), emergency registered nurses (RNs) perform the following tasks: assessment, analysis, nursing diagnosis, planning, implementation of interventions, outcome identification, evaluation of responses, triage and prioritization, emergency operations preparedness, stabilization and resuscitation, and crisis intervention for unique patient populations (e.g., sexual assault survivors) (Cole et al., 1999). In a 2000 national survey of nurses commissioned by the Department of Health and Human Services (DHHS), nurses working in EDs overwhelmingly reported that their dominant function was direct patient care (83 percent). Smaller numbers of ED nurses reported working in supervision (3.5 percent) or administration (2.5 percent).
To become a nurse, an individual can either pursue an associate’s degree in nursing (ADN) or a bachelor of science in nursing (BSN). The ADN course is typically a 2-year degree program and is focused on the practical applications of nursing. The BSN is a 4-year course of study that expands into the theoretical realms of patient care. A third course of study is the diploma, which was common prior to the 1970s. The diploma program is a 2- to 3-year course of study that is located in a hospital and prepares students for hospital positions. There are fewer than 100 diploma programs
in existence today (All Nursing Schools, 2005). In recent years, national nursing organizations have pushed to mandate that the BSN be a minimum requirement for being a professional nurse. After graduation from one of these programs, nurses must take the state board examination to become an RN.
Emergency Nurses
The Emergency Department Nurses Association was formed in 1970. The name of the organization was changed to the Emergency Nurses Association in 1975 to reflect that emergency nurses may work in a variety of settings (ENA, 2005a). In the late 1970s, a committee was convened to write a certification examination, and the ENA helped establish a Board of Certification for Emergency Nursing. The first certification examination was administered in 1980, and 902 emergency nurses passed the exam. In the early 1990s, the board also assisted with the development of the certification program for flight nurses (ENA, 2005b).
In 2004, 13,115 RNs nationwide were credentialed as certified emergency nurses (CENs). There are also other advanced degree options for nurses, including master’s and doctoral degree programs with various areas of specialization and practice. Many nursing management positions require advanced degrees. Some ED nurses specialize in caring for children and may work in pediatric EDs, but no certification is available in pediatric emergency nursing, and there is a paucity of data available regarding these nurses. State boards of nursing may require training in pediatric advanced life support for nurses providing conscious sedation. Pediatric EDs are likely to require advanced pediatric courses and may even require advanced training in neonatal resuscitation for nurses.
According to DHHS’s National Center for Health Workforce Analysis, ED nurses are overwhelmingly non-Hispanic white (88.5 percent). All racial/ ethnic groups are severely underrepresented in the ED nursing population relative to the U.S. population. ED nurses are predominantly female (86 percent) and are younger on average than nurses that work in other settings, with a median age of 40 compared with 43 for other nurses. But ED nurses are aging at approximately the same rate as other nurses, with the median age increasing by 3 years (from 37 to 40) between 1988 and 2000. ED nurses generally have less experience than nurses in other settings. Thirty percent reported graduating in the last 5 years, compared with 20.6 percent of other nurses. Only 11.4 percent of ED nurses reported graduating 26 or more years ago, compared with 22.6 percent of all nurses. ED nurses were more likely than other nurses to report an associate’s degree as their highest level of education (45.6 versus 36.6 percent) and were less likely to have attained a master’s degree (5.8 versus 10.6 percent) (DHHS, 2000).
Advanced Practice Nurses
Advanced practice nurses (APNs) are masters-prepared RNs who provide significant medical care to patients, often with supervision by a physician depending upon their role and scope of practice. APNs include nurse practitioners (NPs), clinical nurse specialists (CNSs), certified registered nurse anesthetists (CRNAs), and certified nurse midwives (CNMs). APNs are required to have a defined scope-of-practice statement for their role, approved by the state board of nursing.
There is no national certification for APNs in emergency care, but NPs and other APNs may obtain training in emergency care skills through university-based programs, continuing education, and work experiences (Cole et al., 1999). In a recent survey sponsored by the ENA, APNs in emergency settings were most likely to report specialties in family NP (43 percent), acute care NP (13 percent), adult care NP (12 percent), critical care CNS (9 percent), or pediatric NP (7 percent) (Cole et al., 2002).
National data are not available on the demographic characteristics of APNs in EDs. However, data collected on licensed NPs in New York State in 2000 allow examination of some of these characteristics in this one state. NPs in EDs were somewhat less likely to be female than other NPs. Despite being younger, ED NPs had spent slightly more years on average as an NP than other NPs (5.5 versus 5) and had also been in their current position for a longer period of time (3 years versus 2 for other NPs). NPs in EDs were more likely than other NPs to hold a Drug Enforcement Administration (DEA) certification, which is required to prescribe controlled substances (86.3 versus 66.3 percent), although they were less likely than other NPs to have hospital admission privileges (4.5 versus 7.3 percent) (Center for Health Workforce Studies, 2000).
Nursing Supply Issues
The nursing shortage in both hospital and nonhospital settings has been the subject of press reports and research articles for years (DHHS, 2002). Although shortages of nurses persist, and the average age of practicing nurses continues to grow, the pipeline of new nursing graduates has been very favorable for the last several years. Enrollments in undergraduate nursing programs increased by 20.8 percent in 2005 and the number of graduates by 26.1 percent (National League for Nursing, 2005). In fact, 147,000 qualified nursing school candidates were turned away in 2005, an 18 percent increase over the previous year. It appears that the limiting factor in the growth of the nursing workforce is the number of nursing programs and faculty.
Nevertheless, the shortages facing many hospitals today are acute and extremely difficult to address on a day-to-day basis. These continuing short-
ages disrupt hospital operations, complicate attempts to deal with ED crowding, and are detrimental to patient safety and quality of care. Until the nursing school pipeline generates significant increases in the nursing workforce, the nursing shortage will continue to be a problem for hospitals and medical centers in all units. Indeed, the problem is expected to worsen before it gets better; as a result of the aging of the population, the demand for nursing services is expected to outpace the number of new nurses for some time. And robust research studies have shown a direct link between nurse staffing levels and patient outcomes (Aiken et al., 2002; Needleman et al., 2002).
EDs are particularly vulnerable to the nursing shortage. Because of the intensity of emergency care, EDs often have more vacant nursing positions than the hospital’s average. Nationwide, it is estimated that 12 percent of RN positions for which hospitals are actively recruiting are in EDs. This makes the ED the third most common source of nursing position openings in hospitals (following general medical/surgical and critical care units). Among hospitals surveyed in New York City, 83 percent reported actively recruiting for nurses in their ED (Greater New York Hospital Association, 2004). A majority of nurses responding to a 2002 survey in New York State said there was “definitely” no shortage of jobs for nurses with their experience, training, and skills; however, there was “definitely” a shortage of qualified nurses with their experience, training, and skills. This trend was more pronounced among ED nurses than those working in other settings (New York State Education Department, 2003).
The impact of the nursing shortage on ED patient care has not been effectively evaluated; however, many speculate that the shortage has a negative impact on patient care for two reasons. First, as with other areas of the hospital, if the ED lacks appropriate nursing levels, patients will not receive the care or attention they need. For example, a triage nurse may be overwhelmed by the number of patients he or she has to evaluate and may miss an important sign of a severe illness or injury. Likewise, if a nurse in the ED must care for too many acutely ill and injured patients simultaneously while assessing newly arriving patients and monitoring admissions who are boarding in the ED, the potential for delayed care or medication errors is dramatically increased. Also, the nursing shortage adds to the problem of ED crowding by limiting the number of staffed inpatient beds available for emergency admissions.
Traditionally, hospitals have determined levels of nurse staffing in the ED using a productivity measure called hours per patient visit (HPPV). Under this system, the total number of paid nursing staff hours is divided by the total number of ED visits to generate a number of hours per patient visit. Obviously, the shortcoming of this method is that patients with varying levels of severity of illness receive the same consideration with regard to nursing staff time (Robinson et al., 2004). More recently, labor unions,
some nursing organizations, and the public have been advocating the use of mandatory nurse staffing ratios in an effort to promote patient safety and quality care (Hackenschmidt, 2004). In the ED, nurse staffing ratios tend to range from 1:4 for general ED patients to 1:1 for trauma patients (Robinson et al., 2004).
Hospitals have opposed mandatory nurse staffing ratios because of the nursing shortage, which makes meeting the ratios difficult; the potential increase in costs; and the increased risk of litigation if a hospital fails to comply with the ratios (Hackenschmidt, 2004). There are particular difficulties associated with maintaining nurse staffing ratios in the ED. The patient census may change rapidly, and the care requirements of patients change significantly during the course of their ED stay.
In 1999, California was the first state to introduce specific nurse-to-patient ratios in EDs, though the ratios were not instituted until 2004 (Hackenschmidt, 2004). The minimum staffing ratios used by the California Department of Health are one nurse to four general ED patients, one nurse to two critical care ED patients, and one nurse to one ED trauma patient. Triage nurses are not included in the ratios. The reaction to the staffing ratios in California among ED nurses is mixed. Some report feeling relieved about the improved staffing; others believe the law is too strict and does not allow for flexibility based on the unit and patient severity of illness. While individual patient care may improve as a result of mandatory ratios, wait times in the ED may increase if ED nurses may care for only a limited number of patients at a time (Hackenschmidt, 2004).
The ENA has spoken out against the use of HPPV and legislated nurse-to-patient staffing ratios, claiming that they are limited in scope and fail to consider the factors that affect the consumption of nursing resources. Indeed, there is a lack of scientific evidence to support the ratio numbers (Hackenschmidt, 2004). The ENA has in turn developed its own staffing guidelines based on six factors: patient census, patient severity of illness, patient length of stay, nursing time for nursing interventions and activities by severity of illness, skill mix for providing patient care based on nursing interventions that can be delegated to a non-RN, and an adjustment factor for the non–patient care time included in each full-time equivalent (FTE) position (Ray et al., 2003).
Despite the controversy over appropriate staffing levels, hospitals still struggle to fill vacant ED nursing positions. They have tried several strategies to compensate for the shortage of ED nurses, including recruiting nurses from foreign countries and using “float” or borrowed nurses from other units of the hospital when the ED is particularly busy. While recruitment from other countries, particularly Canada, has helped relieve the shortages, the use of float nurses is more problematic because those individuals are not familiar with the complexity of the ED or emergency nursing practice
(Schriver et al., 2003). Additionally, in many areas of the country, hospitals use mandatory overtime as a management tool to meet staffing requirements (Jacobsen et al., 2002). Mandatory overtime is a controversial practice, opposed by all of the major nursing organizations. While almost 20 states have considered banning mandatory overtime for nurses, only a handful have done so (Rogers et al., 2004).
Even offering voluntary overtime to nurses is not without controversy, however. Nurses often work longer than their scheduled time, and many shifts extend longer than 12 hours. Research has shown that the risk of medical errors increases significantly when nurses’ shifts exceed 12 hours, when they work overtime, and when they work more than 40 hours per week (Rogers et al., 2004). In Keeping Patients Safe: Transforming the Work Environment of Nurses, the Institute of Medicine (IOM) recommended that voluntary overtime for nurses be limited (IOM, 2004a).
Physician Assistants
According to the American Association of Physician Assistants (AAPA), 4,508 physician assistants (PAs) (9.8 percent of all PAs) worked in EDs in 2003. PAs provide medical care to patients under the supervision of a licensed physician. They perform a number of functions, including conducting physical exams, diagnosing and treating illnesses, ordering and interpreting tests, counseling on preventive health care, and in most states, writing prescriptions (Allied Health Schools, 2005). PAs must be granted clinical privileges at the hospital in which they work.
Most PA programs can be completed through 2 years of training after college. The first year of training consists of coursework in the basic sciences, while the second gives students clinical experience in such areas as internal medicine, rural primary care, emergency medicine, surgery, pediatrics, neonatology, and occupational medicine. Some PAs pursue additional education in a specialty area, such as emergency medicine (Allied Health Schools, 2005). There are three PA educational programs in the United States offering specializations in emergency medicine, although PAs do not need to graduate from such a program to practice in EDs.
Racial and ethnic diversity is low among PAs practicing in EDs; 88 percent are non-Hispanic white. The majority are men. PAs in EDs generally tend to be older than other PAs, in direct contrast to the patterns found among other emergency care personnel (AAPA, 2005).
Pharmacists
The ED is a high-risk area that is prone to medical errors, including medication errors (Goldberg et al., 1996; Selbst et al., 1999; Schenkel, 2000;
Croskerry et al., 2004). In the 1970s, hospitals began integrating pharmacists into ED staff. Their roles generally involved improving medication billing and inventory control. Since that time, the role of pharmacists in the ED has grown to include clinical consultation, education of ED staff, and research (Thomasset and Faris, 2003). Clinical pharmacy specialists (CPSs) that work in EDs typically have a doctor of pharmacy degree and have completed a 1-year residency.
Substantial evidence indicates that including pharmacists on the care team can improve the quality and safety of patient care in both inpatient and outpatient settings (Bates et al., 1995; Leape et al., 1999; Kaushal et al., 2001; Kaushal and Bates, 2001). There are several reasons for including a CPS on the ED care team. The first is to ensure that patients’ medication needs are met. With the growing number of drugs available and the increased complexity of drug selection, administration, and monitoring, there is some justification for having a doctorally trained pharmacist participate on the care team. Participation of a pharmacist on the care team is in line with guidelines of the Joint Commission on Accreditation of Healthcare Organizations (JCAHO) for promoting a multidisciplinary approach to patient care. Second, as noted, medication errors are a serious problem in EDs, and pharmacists may be able to lead system changes that can reduce or eliminate these errors. Finally, medication costs are rising, and pharmacists are in a good position to evaluate which medications are most cost-effective for patients and the hospital.
Still, the prevalence of pharmacists, particularly full-time pharmacists, in EDs remains limited. A 2001 survey of directors of pharmacy in hospitals with at least one accredited pharmacy residency program was conducted to ascertain the prevalence and characteristics of pharmaceutical services in EDs nationwide (Thomasset and Faris, 2003). Only 3 percent of respondents reported having a dedicated pharmacist in an ED satellite pharmacy; 14 percent reported having a dedicated pharmacist who provided services to ED patients. But the demand for pharmacists or pharmacy assistance may grow over the next few years as a result of JCAHO’s 2005 National Patient Safety Goals and Requirements, which call for complete and accurate medication reconciliation across the continuum of care (JCAHO, 2005).
EMS Professionals
Increasingly, EMS professionals are supplementing their prehospital EMS practice by working in hospital EDs. Because of their relevant training and experience, they can serve as effective adjuncts to regular ED staff. According to a 2004 survey of EMS personnel conducted by the National Registry of EMTs, a considerable number of EMTs spend time working
professionally in EDs—32.9 percent of EMT-Bs,1 34.9 percent of EMT-Is, and 29.8 percent of paramedics (NREMT, 2005). These figures represent a substantial increase over previous years. Anecdotal evidence suggests that this is a nationwide phenomenon that is prevalent in both rural and urban environments. There is substantial variation across states in how EMTs can be used in the ED, and some states (e.g., Kansas) have bridge courses that facilitate migration between EMT and RN credentials. This phenomenon may be explained in part by the substantial differences in pay and amenities between the two environments.
Psychologists, Social Workers, and Patient Advocates
A variety of patient care professionals play a critical and generally undervalued role in assisting patients with issues related to family, living arrangements, food and shelter, public and private insurance programs, mental health, and human dignity. The number of such practitioners in the ED is not well known. As the diversity of patients seen in the ED has increased, so, too, has the variety of their social and psychological needs. The importance of these providers has risen, by all accounts, at a much faster pace than their supply.
ENHANCING THE SUPPLY OF EMERGENCY CARE PROVIDERS
The ED workforce includes a broad cross section of the larger health care system—physicians in fields ranging from family medicine to neurosurgery, residents, nurses, pharmacists, and PAs—as well as those who specialize in emergency care, including emergency medicine physicians, emergency nurses, trauma surgeons, and certain medical and surgical specialists. There are substantial concerns about the long-term supply of emergency professionals in several of these categories.
Ensuring an adequate supply of highly trained professionals in every category is the goal. However, there are a number of challenges associated with enumerating the current ED workforce (e.g., how to count part-time workers, individuals who work in multiple EDs, different scopes of practice across states), and estimating the size of the ED workforce needed for the
future is an even more challenging task. Bioterrorism preparedness, the aging of the population, changing morbidity patterns, potential reforms to the health care system, and technological advances are just some of the factors that will impact the size of the ED workforce needed in the future.
While the national supply of physicians and other medical specialists is critical, so is the distribution of the workforce. The most highly trained and specialized clinicians tend to cluster in metropolitan areas, while rural and frontier areas lack even basic medical coverage. This is not, of course, a problem that is restricted to emergency care. But the lack of qualified emergency care personnel in rural areas has a disproportionate impact on health because of the urgency involved: people can schedule elective visits and procedures at distant locations, but in an emergency, that may not be an option. Addressing the rural distribution of the emergency care workforce will require concerted efforts along many fronts, including training, incentives, and enhancement of the rural provider pipeline. For example, the frequently high debt burden of many emergency medicine residents and the limited opportunity to earn sufficient revenue to pay off educational debt in rural settings pose a significant barrier to rural practice, even for those who may prefer it. Enhanced rural training options combined with loan forgiveness programs is a possible approach for enhancing the rural emergency care workforce.
Developing effective strategies to ensure an adequate supply of trained ED professionals in the future requires an understanding of the needs of the nation 10 and 20 years into the future. The committee therefore recommends that the Department of Health and Human Services, the Department of Transportation, and the Department of Homeland Security jointly undertake a detailed assessment of emergency and trauma workforce capacity, trends, and future needs, and develop strategies to meet these needs in the future (6.4). This assessment should be conducted in the context of regionalized systems, which will require a different mix of skills than might otherwise be anticipated. Further, the assessment should consider optimal combinations of professional skills—including emergency and family physicians, NPs, PAs, pharmacists, hospitalists, trauma surgeons, on-call specialists, pediatric and geriatric specialists, social workers, psychologists, and EMS providers. Based on the findings of this assessment, targeted strategies should be considered to address long-term projected shortages, including subsidizing graduate and continuing education programs to increase the number of providers trained in those fields.
This assessment should also address such issues as the impact of graduate medical education allocations at medical centers. These allocations are usually capped, making it difficult for a newer specialty to increase the number of positions, which would require reducing positions in other, established departments. Also, even though emergency physicians are broadly
trained (they are more “generalist” in their practice than any specialty other than family medicine), they are excluded from the definition of “primary care” because they do not generally provide continuity of care. Emergency physicians are thereby excluded from certain federal and state programs designed to promote the training of primary care physicians, although in some rural counties, primary care is provided predominantly through the ED.
The above discussion focuses only on emergency physicians, but concerns about the numbers of funded residency positions apply to virtually all specialties that provide emergency care. These concerns are especially important now that the physician workforce is projected to be inadequate for the nation’s future needs.
BUILDING CORE COMPETENCIES
Core competencies are the critical skills, knowledge, abilities, and behaviors that a field or industry has agreed must be achieved if a person is to be accepted as competent at a particular level. The specialty of emergency medicine pioneered the concept of a core curriculum for training emergency medicine residents, and now has a detailed roadmap of the training and competencies required for the practice of emergency medicine. The core content eventually developed into a model of the clinical practice of emergency medicine that has served as the foundation for medical school training and residency curricula, certification exam specifications, continuing education objectives, and residency program review requirements (Hockberger et al., 2001). The model was revised in 2004 to incorporate the six core competencies promoted by ACGME: patient care, medical knowledge, practice-based learning and improvement, interpersonal skills, professionalism, and system-based practice (Chapman et al., 2004). The major professional organizations focused on emergency medicine, which include ACEP, SAEM, the Council of Emergency Medicine Residency Directors (CORD), ABEM, the Emergency Medicine Residents Association (EMRA), and the Residency Review Committee for Emergency Medicine (RRC-EM), ensure that the core content specific to the specialty is frequently updated.
As discussed earlier, however, a significant number of physicians practicing in EDs are not residency trained or board certified in emergency medicine (Moorhead et al., 2002). Their level of competency in emergency medicine is not well known. Only a small number of very limited studies have been conducted to compare the competencies of board-certified or residency-trained emergency physicians and those of other emergency physicians. Results of these studies suggest benefits of emergency medicine residency training in the performance of airway management and care of patients with acute myocardial infarction (Friedman et al., 1999; Jones et al., 2002; Weaver et al., 2004). Results of one study also indicate
significantly fewer closed malpractice claims against emergency medicine residency–trained physicians relative to ED physicians without such training (Branney et al., 2000); however, there is a need for more robust research in this area.
Competencies in nursing are established and assessed in a similar manner. The ENA developed the Emergency Nursing Core Curriculum for nurses wishing to take the CEN exam. Those nurses with the CEN credential possess the basic competencies deemed appropriate by the ENA. However, most nurses working in EDs are not CENs, and their level of competency and training relevant to emergency care is not well known.
Furthermore, while specialties have established core competencies within their respective fields, there is no uniform standard of care for the multiple disciplines practicing within the ED. Although most EDs treat cardiac patients, not all hospitals require physicians and nurses to take the Advanced Cardiac Life Support course. Similarly, not all hospitals require ED nurses to take the Emergency Nursing Pediatric Course and the Trauma Nursing Core Course, and not all require ED physicians to take the Advanced Trauma Life Support Course. Yet while exposure to these courses may help improve the level of competency for some providers, particularly those with little formal training in emergency care, it does not ensure competency.
As a result of the variability in initial and continuing education received by ED providers, there is also variability in the emergency care received by the public. The committee believes the uncertainty about the quality and consistency of emergency care across the nation is unacceptable and that it is important to define clearly what qualifies as competent care and what does not. Therefore, the committee recommends that the Department of Health and Human Services, in partnership with professional organizations, develop national standards for core competencies applicable to physicians, nurses, and other key emergency and trauma professionals, using a national, evidence-based, multidisciplinary process (6.5). The core competencies developed should not simply represent one minimum level of competency that all ED providers must attain. If that were the case, the competencies would be a challenge for only the most resource-strapped hospitals. Instead, the core competencies should be tiered and reflect the categorization of the ED. EDs categorized at the highest levels should be subject to the most stringent competency requirements, while providers working in EDs with a lower categorization should be subject to less rigorous requirements. The competency standards should be developed to challenge hospitals, yet must be attainable. State regulatory agencies should monitor adherence to these standards.
These national standards should ensure that core competencies for all providers working in the ED are assessed in accordance with the level of ED in which they practice, regardless of board certification or CEN status. Research should be conducted to track patient outcomes as a means of
monitoring the benefits of having such universal core competencies. Additionally, the efficacy of the core competencies should be periodically assessed and adjusted as necessary.
ADDRESSING THE ISSUE OF PROVIDER SAFETY
Working in an ED has the potential to be highly rewarding but is often very stressful, and at times dangerous. The work is complicated by limited access to patients’ past medical history, the episodic nature of the care being provided, and the uncontrolled or unpredictable environments in which care must be provided (Cole et al., 1999). Physical threats to safety abound in the ED, ranging from a chance needle stick to the risk of assault, either physical or verbal, from patients who may be under psychological stress or the influence of intoxicants. Additionally, the psychological toll of working in a high-pressure environment, coupled with exposure to the pain and suffering of illness and injury, can result in tremendous stress on ED providers. This section reviews the day-to-day dangers that affect ED workers. The next chapter addresses provider safety in the context of disasters, including chemical and biological exposure.
Mental Stress
Numerous studies both in the United States and abroad have identified stress as a major concern for emergency care providers. Emergency physicians in 2002 spent an average of 55.7 hours per week on professional activities. This figure is slightly lower than the average number of hours spent on professional activities by all physicians (57.6); however, emergency physicians on average report more total patient visit hours (45.8 versus 43) and have more patient visits per week (118.4 versus 107.2) than other physicians (AMA, 2004). Furthermore, in contrast to most physicians, who follow an established panel of patients, most if not all ED physicians work with new patient encounters, which are often more demanding, time-consuming, and complex. Moreover, ED patients generally present with more acute conditions than are seen in a typical office practice. ED physicians also are prone to stress related to disruption of circadian rhythms because of the frequency and irregularity of night shifts, as well as stress related to the intensity and high levels of severity of illness among the patients they see, the unscheduled nature of emergency visits, the high medico-legal risk of missed diagnoses and complications of care, and the psychological drain of being second-guessed by consultants and admitting physicians. Emergency physicians must handle multiple patients at once and deal with a wide variety of social situations with little backup. As a result, emergency physicians who attempt
to work a total number of hours similar to those of office-based practitioners are prone to burnout.
Nurses working in the ED also experience significant stress. Lambert and Lambert (2001) found a lack of job control, work overload, exposure to death and dying, and poor work relationships to be major sources of stress for nurses. A 2002 survey of registered nurses in New York State revealed that RNs working in EDs feel they are under great stress significantly more often relative to RNs working in other settings. Thirty-seven percent of ED RNs reported feeling under great stress “almost every day” (compared with 30 percent of other RNs), while only 10 percent said they felt great stress less than once a week (compared with 19 percent of other RNs), and none said that they “never” felt great stress (compared with 3 percent of other RNs) (New York State Education Department, 2003).
Violence
According to data from the Bureau of Labor Statistics for 1993, workers in the health care field experienced the highest incidence of assault injuries. One study found that 82 percent of nurses surveyed had been assaulted on the job, that 56 percent had been assaulted in the year prior to the survey, and that many assaults went unreported (Erickson and Williams-Evans, 2000). Several characteristics of the ED, the community it serves, and specific patients make the ED and its employees especially prone to such violence. Few steps have been taken to explore this issue and provide ED workers and patients the security they require. With the support of hospital administrators and in cooperation with local officials, security measures and specialized training can be instituted in EDs to enhance provider safety.
Workplace violence encompasses physical assaults and threats of assaults directed toward persons at work or on duty, and can encompass witnessing or being a victim of physical assaults, sexual assaults, nonverbal intimidation, and verbal threats (Flannery et al., 2000). Researchers have attempted to identify key risk factors associated with violence in the ED and the broader health care field in an effort to increase provider awareness and encourage the development of strong violence prevention programs. Those specific risk factors include staff shortages and long wait times, which can aggravate an already distraught patient or family member.
ED patients in poor mental health or those with substance-abuse problems may instigate violence in the ED. This threat has grown with the shift toward privatization and deinstitutionalization; the ED has seen an increase in visits from psychiatric patients (Flannery et al., 2000). High crime rates in larger urban communities can also translate into violent incidents in the ED; gang-related incidents are becoming more common, and weapons are
increasingly being confiscated from patients and visitors upon entry into the ED (Ordog et al., 1995).
Safety measures to protect ED providers vary in cost and utilization. Many busy EDs are staffed with armed security personnel specially trained to handle disruptive or violent patients. Some EDs have metal detectors and controlled access to limit patients’ ability to interfere with or threaten the care of others. Designated security phones or push buttons can provide direct links to local police departments. Additionally, assigning multiple staff members to violence-prone patients and ensuring two points of entry into an exam room can help protect providers.
Bloodborne and Airborne Pathogens
Health care delivery by nature poses unique threats to both patients and providers. Movement from one sick patient to another with the constant uncertainty of medical history or the presence of infectious disease makes the ED susceptible to a host of biological hazards, including bloodborne pathogens. Up to 800,000 injuries through the skin may occur annually in the United States, and these injuries account for approximately 82 percent of exposures to blood or other body fluids among health care workers (National Institute for Occupational Safety and Health, 2004). Although exposure to these occupational hazards and the prevalence of occupational injuries have increased for health care workers, the steady decline in rates of provider infection speaks to the value of nationwide protective measures. Over a 17-year period, the adoption of recommended universal precautions and the Occupational Safety and Health Administration’s (OSHA) Bloodborne Pathogens Standard helped decrease the number of hepatitis B viral infections among health care workers from nearly 11,000 in 1983 to fewer than 400 in 1999 (CDC National Center for Infectious Disease, 2002). Yet while there is growing concern about the risk of exposure to airborne pathogens, including multidrug-resistant tuberculosis, severe acute respiratory syndrome (SARS), and emerging strains of influenza, most EDs have few negative pressure rooms to isolate staff and other patients from respiratory pathogens (Augustine et al., 2004).
The SARS outbreak in Toronto was triggered in part by a patient who sought care in a Toronto ED for fever and a cough. He stayed overnight in a crowded ED awaiting admission for what was thought at the time to be community-acquired pneumonia. Over the course of the night, he infected 2 nearby patients and several hospital staff members with SARS. Both this index case and the 2 patients he infected subsequently died from the disease, and a total of 31 patients and staff fell ill. Ironically, the same
hospital where this incident occurred continues to board admitted patients in its ED (Cass, 2005).
Physical Stress
Nurses have the highest prevalence of back pain among health care workers and the highest incidence of workers’ compensation claims for back injuries (Edlich et al., 2001). Estimates show that 12 percent of nurses leave the profession annually because of back injuries, and more than 52 percent report chronic back pain (Robinson et al., 2004). General back pain is often considered an inevitable consequence of nursing practice. Nurses spend much of their time standing. Additionally, they often work in physically awkward positions since they must maneuver around patient equipment; work in space that is often limited; and handle patients with unique sizes, shapes, or deformities. ED nurses also must lift heavy patients or equipment. National Institute for Occupational Safety and Health (NIOSH) guidelines state that the average provider must not lift more than 45 pounds; this translates to a need for more than three providers to be present when lifting the average patient (Edlich et al., 2001). However, time pressures and lack of sufficient resources may force a provider to administer care without adequate support. Specialized patient lifting techniques and machines can help prevent the common back injuries that many nurses experience. Several EDs have acquired lifting machinery to protect providers from injury and/or instituted guidelines for providers to assist each other in executing physically demanding or straining tasks.
It is imperative that EDs be as safe an environment as possible for emergency providers to deliver the highest level of care to patients. In fact, patient safety is positively impacted when a comfortable, supportive, and safe work setting is fostered.
INCREASING INTERPROFESSIONAL COLLABORATION
The concept of interprofessional collaboration gained strength in the late 1990s as attention to medical errors grew. Health services researchers and others interested in improving patient safety were energized by successes in the aviation industry, where teamwork training for the private and government aviation workforce led to reductions in errors and improved performance (Sprague, 1999). Research in the aviation industry indicated that effective teamwork does not arise spontaneously, but must be developed and practiced (Risser et al., 1999). The similarities between pilots and doctors—highly trained technically, accustomed to viewing themselves as
bearers of ultimate authority and responsibility, independent yet increasingly dependent on others of varying skill levels—suggest that teamwork training may be influential in reducing errors in the medical field (Sprague, 1999).
Several organizations, including the IOM and the Institute for Healthcare Improvement (IHI), have embraced the concept of teamwork training for health professionals. In 2000, the IOM report To Err Is Human: Building a Safer Health System recommended that health care organizations establish team training programs for personnel in critical areas, including the ED (IOM, 2000). These recommendations are beginning to take hold. A November 2004 survey of members of ECRI’s (formerly the Emergency Care Research Institute) Healthcare Risk Control System indicated that one-third of respondents provided teamwork training to employees, and nearly half that did not said they planned to do so in the next year (ECRI, 2005).
Teamwork training has considerable potential for improving the quality of care in EDs for several reasons. First, the ED parallels the environment in the aviation industry in many ways; high-stress, time pressure, and uncertainty abound in both (Small et al., 1999). Second, ED staff tend to have little or no formal training in teamwork skills, yet the delivery of emergency care requires rapid decision making and effective coordination of groups of caregivers, often from multiple disciplines, with vastly different training, professional missions, cultural identities, and feelings of empowerment. This unique environment joins together in real-time interaction such diverse providers as nurses, pharmacists, social workers, neurosurgeons, psychologists, and patients’ attending physicians from the community. Patient outcomes can be undermined if caregivers do not work well together and coordinate their services appropriately (Risser et al., 1999). Third, teamwork failures in the ED are not uncommon. A review of closed malpractice claims from several EDs found that 43 percent of errors were due to problems with team coordination, and 79 percent of those errors could have been mitigated or prevented if there had been an effective team structure in the ED and ED personnel had received team behavior training. The researchers also concluded that better teamwork would have saved $3.50 per ED patient visit in legal costs (Risser et al., 1999; Shapiro et al., 2004). White and colleagues (2004) noted that communication issues were associated with 30 percent of the ED risk management files they studied and appeared to contribute directly to adverse medical outcomes in 20 percent of those cases.
Research on the impact of teamwork training in the ED is thin but promising. MedTeams, a Department of Defense project that introduced teamwork training to health care, developed an Emergency Team Coordination course—an 8-hour didactic course for physicians, nurses, technicians, and support personnel. An evaluation of the course revealed considerable success. EDs using it experienced a 67 percent increase in error-averting behavior and a 58 percent reduction in observable errors (Risser et al., 1999;
Shapiro et al., 2004). The research team also identified behaviors associated with teamwork failures, including failure to identify an established protocol for patient care and failure to cross-monitor the actions of other team members. They found as well that in most of the adverse events studied, some team member had a piece of information, observed an action, possessed a skill, or had a doubt or suspicion that, if acted upon, could have prevented or mitigated the error (Wears and Simon, 2000).
Key to teamwork training for ED providers is the use of simulations and promotion of interprofessional collaboration. Simulation training involves giving ED providers practice in performing tasks in lifelike circumstances using models or virtual reality, and includes feedback from observers, other team members, and video cameras to assist in the improvement of skills. Human simulators can give clinicians experience in dealing with high-risk, low-frequency events. For example, a pregnant human patient simulator can be used to train clinicians for emergency cesarean-section procedures. These simulators allow providers to learn from mistakes without harming an actual patient (ECRI, 2005). Moreover, the stress experienced by trainees when using a high-fidelity patient simulation model reproduces realistic patient encounters and reflects the difficulty associated with performing under stress (Vozenilek et al., 2004). The IOM report To Err Is Human: Building a Safer Health System recommended use of simulation training as a strategy to prevent medical errors (IOM, 2000).
Again, evidence of the effectiveness of simulation-based training is thin, but initial research indicates it has benefits. In one study, ED staff including nurses, physicians, emergency medicine residents, and technicians were randomly assigned to receive 8 hours of intensive training with a simulator in which three scenarios of increasing difficulty were presented following a didactic training session. Unlike a control group that received only the didactic training, the group that experienced the simulation training displayed an improvement in the quality of team behavior. Those who underwent the simulation training believed it was a useful educational method (Shapiro et al., 2004).
The use of simulation training is becoming more common. An example is the Advanced Cardiac Life Support course for third-year medical students at Brown University, which involves assigning students to multidisciplinary teams with nurses and technicians. The teams receive teamwork training while learning advanced cardiac life support using a high-fidelity simulation mannequin (Morchi, 2002). At Regions Hospital, emergency medicine residents spend 30 to 40 hours per year at a simulation center where, among other things, residents learn teamwork skills and develop their ED team leadership skills in realistically complex, challenging, and stressful emergency situations. The sessions are taped, and faculty and residents review and discuss the residents’ performance (Patow, 2005).
Interprofessional collaboration is also a critical consideration in teamwork training, particularly in EDs where individuals from various medical disciplines must work together effectively (see Box 6-2). Differences in views often exist among health care professionals that can act as barriers to team performance (IOM, 2004a). Interprofessional collaboration in the ED may not develop naturally because of the high-pressure, high-stress environment, coupled with the strong personalities and egos of providers.
Interprofessional collaboration refers to an aggregation of attributes that include a shared understanding of goals and roles, effective communication, shared decision making, and conflict management. Evidence supports the effectiveness of interprofessional collaboration as a means of improving patient outcomes. There are several ways in which hospital leadership can nurture interprofessional collaboration through changes in organizational structure and processes. These strategies were endorsed by the IOM in the report Keeping Patients Safe: Transforming the Work Environment of Nurses (IOM, 2004a).
Most important in the present context is the need to enhance partnerships among the diverse professionals that function within the ED to solve the problems of crowding, diversion, communication, and coordination so as to provide better patient care. This collaboration goes beyond transforming the patient care work environment, but must take place in parallel with such changes. For example, the operations management solutions to crowding discussed in Chapter 4 cannot work without buy-in and collabo-
|
BOX 6-2 Example of Effective Collaboration in the ED During an extremely busy shift in an ED whose entire staff had recently been trained in teamwork and collaboration, an emergency physician had just come from a resuscitation and was seeing a patient with an acute but non-life-threatening condition. During the history and physical exam, the patient told the physician twice about his severe allergy to a particular medication. The physician noted the allergy, and as he left the patient’s room was pulled into another resuscitation. During a momentary break, the physician wrote orders on the patient’s chart prescribing the medication to which he was allergic. An experienced nurse caught the mistake and showed no hesitation in bringing it to the physician’s attention in a professional manner. Somewhat angry at himself for making the error, the physician was nonetheless very appreciative that the error had been caught and that the nurse had felt empowered to bring it to his attention. |
ration among emergency physicians, admitting surgeons, and other critical specialists that make it possible to attempt changes in the status quo—in this case, changing long-established admitting and operating room (OR) blocking patterns. Likewise, unless emergency and trauma surgeons collaborate with on-call specialties, it will be difficult to fashion solutions to the on-call problems that plague hospitals and contribute substantially to crowding and boarding of patients.
Hospital leadership should model collaborative behaviors as a way to persuade other ED staff to adopt the same behaviors. Moreover, hospital leadership should support the ongoing acquisition and maintenance of staff members’ clinical knowledge and skills. Research indicates that individual clinical competence is an essential precursor to collaborative practice. ED work and workspaces should be designed to facilitate collaboration. Workspaces should encourage physical proximity among ED personnel who work together, and staffing patterns should ensure that personnel have the time to participate in collaborative activities. Hospital leadership should encourage mechanisms for interprofessional practice. Structured interprofessional forums, such as patient rounds or regularly scheduled interprofessional meetings, are effective in improving patient care. Sharing of patient records and documents also promotes interprofessional collaboration.
Finally, human resource policies should be designed to support collaboration. Hostile behaviors, such as verbal abuse, should be identified and addressed. Managers should set practice expectations for staff, endorsing cooperation and communication with others while displaying regard for their dignity; shouting, foul language, and rudeness must be restricted. Performance evaluations might include measures of the extent to which staff are viewed as collaborators by staff from other disciplines.
ADDRESSING THE SHORTAGE OF RURAL EMERGENCY CARE PROVIDERS
The workforce in rural EDs has mirrored many of the challenges of overall recruitment and retention of health care providers in rural areas. A recent IOM study, Quality Through Collaboration: The Future of Rural Health, described the special problems of rural health care and the unique challenges of providing high-quality medical services in rural areas, particularly core health services such as emergency care. The report highlighted the urgent shortages of medical personnel in rural areas, the critical need to address these shortages, and the complex challenges associated with strengthening the rural workforce (IOM, 2004b). Although 21 percent of Americans live in rural areas, only slightly more than 12 percent of emergency physicians, regardless of training or certification status, practice in these settings (Moorhead et al., 2002). Thus a pattern of population-based
maldistribution exists, and in fact has worsened since 1997, when 15 percent of emergency physicians practiced in rural areas (Moorhead et al., 1998; Williams et al., 2001). This change may reflect the rapid growth in urban areas with rising numbers of emergency medicine residency training programs rather than a sharp decline in rural communities. Nevertheless, this maldistribution is a problem that must be addressed.
The specialty of emergency medicine has focused on strategies for increasing the number of emergency medicine specialists in rural areas, but workforce issues in rural EDs may never be resolved by such efforts alone. The difficulties of recruitment and retention in rural EDs are due to a variety of causes, but are generally assignable to either work-related factors or personal and community characteristics (Pan et al., 1996). There exists a strong correlation between where a physician is raised and the community in which he or she later chooses to practice (Williams et al., 2001). Additionally, the location of residency training is a major factor in the choice of practice location for emergency medicine residency graduates regardless of previous geographic ties (Steele et al., 1998). Rural hospitals that have residency training programs are more successful in recruiting and retaining physicians when they complete their residency (Connor et al., 1994; Cutchin, 1997). The fact that the majority of emergency medicine residency programs are located in urban areas suggests that residency graduates will likely continue to choose to practice in those areas. Graduates also are faced with lower levels of compensation in rural than in urban areas (Bullock et al., 1999). The high debt burden of many emergency medicine residents, coupled with the limited opportunity to earn sufficient income to pay off educational debt in rural settings, is a significant barrier to rural practice. Increased workload in rural areas is another barrier: rural emergency medicine physicians spend 35 percent more time in on-call backup relative to the average for all emergency physicians (Moorhead et al., 2002). Given the fewer resources and consultants typical of rural settings (Sklar et al., 2002), the lack of physicians trained in emergency medicine in these settings is not surprising.
One strategy for increasing the emergency care workforce in rural areas would be to increase the number of emergency medicine residency programs in these areas. However, ACGME program requirements enforced by the Residency Review Committee (RRC) make it virtually impossible to gain certification for a “rural” residency program unless it is situated in a large referral hospital. The RRC is equally reluctant to recognize satellite sites at rural hospitals if they are geographically remote from the program’s base hospital, regardless of distance. Changes in such ACGME requirements might increase rural emergency medicine training during residency and ultimately benefit the rural emergency medicine workforce and the quality of care provided in rural settings. Another approach would be to develop programs that would cover the costs of medical education in return for
future assignment to a rural area, based on the National Health Service Corps or Public Health Service Commissioned Corps model but specifically targeting emergency medicine.
To compensate for manpower shortages, rural EDs have resorted to alternative methods and providers in an effort to maintain minimum levels of staffing. This strategy is evident if one examines the physician characteristics in rural EDs. In one survey of random hospitals across the United States, rural EDs, comprising 25 percent of all EDs, reported an average of 4.74 physicians per institution, 40 percent fewer than the average for all locales (Moorhead et al., 2002). Numbers of FTEs, defined as those working 40 clinical hours per week, were also significantly lower in rural EDs; there were 3.42 FTEs per rural ED—35 percent fewer than average. Rural EDs were noted to have the highest percentage of osteopathic physicians (14 percent) and non-U.S.-trained physicians (14 percent). It is significant that 67 percent of rural emergency medicine physicians are neither residency trained nor board certified in emergency medicine. Of the 33 percent of physicians with emergency medicine credentials, fewer than half are both emergency medicine residency trained and board certified. Only 12 percent of rural respondents in the survey reported requiring any emergency medicine credentials for ED hiring. In summary, rural EDs have lower levels of staffing, and when they are staffed by physicians, these physicians are much less likely to be emergency medicine specialists and more likely to be trained in family practice or other primary care specialties.
Although ideally all EDs would be staffed by residency-trained, board-certified emergency physicians, this is highly unlikely to occur in the near to mid term, if ever. Therefore, alternative staffing models must be developed. Clinicians other than physicians—such as PAs, NPs, CNMs, and CNSs—are often used in the staffing of rural EDs (Moorhead et al., 2002). With national efforts to lower costs and the demonstrated success of using nonphysician clinicians in certain prescribed roles, their use in the staffing of rural EDs may increase (Blunt, 1998). At the same time, it should be noted that rural EDs experience problems with recruitment and retention of all clinicians, not just physicians, and for similar reasons (Bullock et al., 1999).
Rural ED providers exhibit wide variability in their skill levels and the competence with which they provide emergency care. Care often falls short of established guidelines. In a study of acute stroke care in nonurban EDs, patients were found to have been treated in ways discordant with AHA recommendations. Hypertension was often treated too aggressively, and inappropriate medications were sometimes used. Additionally, it was suggested that nonmotor symptoms of stroke were less likely to be recognized or were treated with less urgency than motor symptoms of stroke (Burgin et al., 2001). Although these data are far from conclusive, results of such studies may explain in part the stigma of decreased competence attributed
to rural emergency physicians (Leap, 2000). Yet the reality is that rural emergency physicians are often called upon to care single-handedly for critically ill and injured patients in a challenging setting typically lacking in manpower, equipment, and access to consultants. The deficit of rural health care providers has complicated the roles these providers must fill. It is typical for rural primary care physicians’ practices to entail management of patients in EDs, outpatient clinics, inpatient wards, and ICUs, as well as additional duties related to health care administration. Additionally, the low patient census in a rural ED may contribute to the difficulty experienced by physicians and midlevel providers in maintaining a high level of proficiency in emergency medicine.
Furthermore, certain specialists who provide on-call emergency and trauma services are even scarcer in rural areas. Substantial near-term increases in the capacity to provide advanced emergency and trauma care in rural settings are unlikely. This situation makes effective regional solutions to the transport of patients to definitive emergency and trauma care essential. But effective transport requires effective stabilization, critical care management, and in some cases surgical intervention. The proposed subspecialty in emergency surgery described earlier in this chapter has particular applicability to rural settings, where there are unlikely to be other specialists with the skills to adequately address certain serious emergencies.
All patients, regardless of setting, deserve prompt access to high-quality emergency care. Initiatives to improve the quality of emergency care in rural areas have recognized the need to develop strategies for enhancing the knowledge and training and expanding the size of the rural emergency care workforce. Given current workforce shortages in emergency care and economic conditions in the health system, rural EDs are unlikely to have residency-trained, board-certified emergency physicians on a round-the-clock basis. Approaches recommended to address this situation include increased collaboration between emergency medicine and primary care specialties (such as family practice physicians who provide emergency medical care in rural areas) and increased links between academic medical centers and rural hospitals (Williams et al., 2001). Emergency physicians and family practitioners in Minnesota, for example, have developed a course for training teams of health care providers in comprehensive advanced life support that can serve as a model for collaborative training in rural emergency medicine (Carter et al., 2001).
The committee supports these efforts, and recommends that states link rural hospitals with academic health centers to enhance opportunities for professional consultation, telemedicine, patient referral and transport, and continuing professional education (6.6).
SUMMARY OF RECOMMENDATIONS
6.1: Hospitals, physician organizations, and public health agencies should collaborate to regionalize critical specialty care on-call services.
6.2: Congress should appoint a commission to examine the impact of medical malpractice lawsuits on the declining availability of providers in high-risk emergency and trauma care specialties, and to recommend appropriate state and federal actions to mitigate the adverse impact of these lawsuits and ensure quality of care.
6.3: The American Board of Medical Specialties and its constituent boards should extend eligibility for certification in critical care medicine to all acute care and primary care physicians who complete an accredited critical care fellowship program.
6.4: The Department of Health and Human Services, the Department of Transportation, and the Department of Homeland Security should jointly undertake a detailed assessment of emergency and trauma workforce capacity, trends, and future needs, and develop strategies to meet these needs in the future.
6.5: The Department of Health and Human Services, in partnership with professional organizations, should develop national standards for core competencies applicable to physicians, nurses, and other key emergency and trauma professionals, using a national, evidence-based, multidisciplinary process.
6.6: States should link rural hospitals with academic health centers to enhance opportunities for professional consultation, telemedicine, patient referral and transport, and continuing professional education.
REFERENCES
AAPA (American Association of Physician Assistants). 2005. 2005 AAPA Physician Assistant Census Report. [Online]. Available: http://www.aapa.org/research/05census-intro.html [accessed June 16, 2006].
ABPS (American Board of Physician Specialties). 2005. Eligibility Requirements. [Online]. Available: http://www.abpsga.org/certification/emergency/eligibility.html [accessed August 10, 2005].
ACEP (American College of Emergency Physicians). 2004. Two-Thirds of Emergency Department Directors Report On-Call Specialty Coverage Problems. [Online]. Available: http://www.acep.org/1,34081,0.html [accessed September 28, 2004].
ACEP. 2006. The National Report Card on the State of Emergency Medicine: Evaluating the Environment of Emergency Care Systems State by State. Dallas, TX: ACEP.
ACEP Research Committee. 2005. Report on Emergency Medicine Research. Washington, DC: ACEP.
Aiken LH, Clarke SP, Sloane DM. 2002. Hospital staffing, organization, and quality of care: Cross-national findings. International Journal for Quality in Health Care 14(1):5–13.
All Nursing Schools. 2005. Entry Level Nursing Programs. [Online]. Available: http://www.allnursingschools.com/faqs/programs.php [accessed February 15, 2005].
Allied Health Schools. 2005. Become a Physician Assistant (PA): Physician Assistant Training and Careers. [Online]. Available: http://www.allalliedhealthschools.com/faqs/physician_assistant.php [accessed August 9, 2005].
AMA (American Medical Association). 2003. Physician Socioeconomic Statistics. Chicago, IL: AMA.
AMA. 2004. Physician Characteristics and Distribution in the U.S.: 2004 Edition. Chicago, IL: AMA.
Augustine J, Kellermann A, Koplan J. 2004. America’s emergency care system and severe acute respiratory syndrome: Are we ready? Annals of Emergency Medicine 43(1):23–26.
Bates DW, Boyle DL, Vander Vliet MB, Schneider J, Leape L. 1995. Relationship between medication errors and adverse drug events. Journal of General Internal Medicine 10(4): 199–205.
Berenson RA, Kuo S, May JH. 2003. Medical malpractice liability crisis meets markets: Stress in unexpected places. Issue Brief (Center for Studying Health System Change) (68):1–7.
Blunt E. 1998. Role and productivity of nurse practitioners in one urban emergency department. Journal of Emergency Nursing 24(3):234–239.
Branney SW, Pons PT, Markovchick VJ, Thomasson GO. 2000. Malpractice occurrence in emergency medicine: Does residency training make a difference? The Journal of Emergency Medicine 19(2):99–105.
Brewster LR, Felland LE. 2004. Emergency department diversions: Hospital and community strategies alleviate the crisis. Issue Brief (Center for Studying Health System Change) (78):1–4.
Bullock K, Rodney WM, Gerard T, Hahn R. 1999. Advanced practice family physicians as the foundation for rural emergency medicine services (part I). Texas Journal of Rural Health 17(1):19–29.
Burgin WS, Staub L, Chan W, Wein TH, Felberg RA, Grotta JC, Demchuk AM, Hickenbottom SL, Morgenstern LB. 2001. Acute stroke care in non-urban emergency departments. Neurology 57(11):2006–2012.
Byrne RW, Bagan B. 2004. Academic center ERs bear brunt of Chicago-area transfers. American Association of Neurological Surgeons Bulletin 13(4):14–15.
California Healthcare Association. 2003. On-Call Physician ED Backup Survey. Sacramento, CA: California Healthcare Association.
Carter DL, Ruiz E, Lappe K. 2001. Comprehensive advanced life support. A course for rural emergency care teams. Minnesota Medicine 84(11):38–41.
Cass D. 2005. Once upon a time in the emergency department: A cautionary tale. Annals of Emergency Medicine 46(6):541–543.
CDC (Centers for Disease Control and Prevention) National Center for Infectious Disease. 2002. National Notifiable Diseases Surveillance System (NNDSS). Unpublished.
Center for Health Workforce Studies. 2000. 2000 Survey of Nurse Practitioners Licensed in New York State. Rensselaer, NY: Center for Health Workforce Studies, School of Public Health, SUNY Albany.
Chapman D, Hayden S, Sanders A, Binder L, Chinnis A, Corrigan K, LaDuca T, Dyne P, Perina D, Smith-Coggins R, Sulton L, Swing S. 2004. Integrating the accreditation council for graduate medical education core competencies into the model of the clinical practice of emergency medicine. Annals of Emergency Medicine 43(6):756–769.
Church A. 2003. Critical care and emergency medicine. Critical Care Clinician 19(2): 271–278.
Cole FL, Ramirez E, Luna-Gonzales H. 1999. Scope of Practice for the Nurse Practitioner in the Emergency Setting. Des Plaines, IL: Emergency Nurses Association.
Cole FL, Kuensting LL, Maclean S, Abel C, Mickanin J, Bruske P, Wilson ME, Rehwaldt M. 2002. Advance practice nurses in emergency care settings: A demographic profile. Journal of Emergency Nursing 28(5):414–419.
Committee on Trauma, ACS (American College of Surgeons). 1998. Resources for Optimal Care of the Injured Patient: 1999. Chicago, IL: ACS.
The Committee to Develop the Reorganized Specialty of Trauma, Surgical Critical Care and Emergency Surgery. 2005. Acute care surgery: Trauma, critical care, and emergency surgery. The Journal of Trauma 58(3):614–616.
Connor RA, Hillson SD, Kralewski JE. 1994. Association between rural hospitals’ residencies and recruitment and retention of physicians. Academic Medicine 69(6):483–488.
Couldwell WT, Gottfried ON, Weiss MH, Popp AJ. 2003. Too many? Too few. New study reveals current trends in U.S. neurosurgical workforce. AANS Bulletin 7–9.
Croskerry P, Shapiro M, Campbell S, LeBlanc C, Sinclair D, Wren P, Marcoux M. 2004. Profiles in patient safety: Medication errors in the emergency department. Academic Emergency Medicine 11(3):289–299.
Cutchin MP. 1997. Community and self: Concepts for rural physician integration and retention. Social Science & Medicine 44(11):1661–1674.
Danzl D, Munger B. 2000. History of Academic Emergency Medicine. Emergency Medicine: An Academic Career Guide (2nd edition). Lansing, MI: Society for Academic Emergency Medicine and Emergency Medicine Residents Association.
DHHS (U.S. Department of Health and Human Services). 2000. National Sample Survey of Registered Nurses. Rockville, MD: Health Resources and Services Administration, Bureau of Health Professions, National Center for Health Workforce Analysis.
DHHS. 2002. Projected Supply, Demand, and Shortages of Registered Nurses, 2000–2020. Rockville, MD: Health Resources and Services Administration, Bureau of Health Professions, National Center for Health Workforce Analysis.
Dresnick S. 1997. The future of the private practice of emergency medicine. Annals of Emergency Medicine 30(6):754–756.
ECRI. 2005, March 25. Teamwork takes hold to improve patient safety. The Risk Management Reporter.
Edlich RF, Woodard CR, Haines MJ. 2001. Disabling back injuries in nursing personnel. Journal of Emergency Nursing 27(2):150–155.
ENA (Emergency Nurses Association). 2005a. ENA History. [Online]. Available: http://www. ena.org/about/history/ [accessed February 9, 2005].
ENA. 2005b. History of the Certification Examination for Emergency Nurses. [Online]. Available: http://www.ena.org/bcen/about/History.asp [accessed February 9, 2005].
Encinosa WE, Hellinger FJ. 2005. Have state caps on malpractice awards increased the supply of physicians? Health Affairs (Millwood, VA) Suppl. Web Exclusives W5-250–W5-258.
Erickson L, Williams-Evans SA. 2000. Attitudes of emergency nurses regarding patient assaults. Journal of Emergency Nursing 26(3):210–215.
Flannery RB Jr, Fisher W, Walker A, Kolodziej K, Spillane MJ. 2000. Assaults on staff by psychiatric patients in community residences. Psychiatric Services 51(1):111–113.
Friedman L, Vilke GM, Chan TC, Hayden SR, Guss DA, Krishel SJ, Rosen P. 1999. Emergency department airway management before and after an emergency medicine residency. Journal of Emergency Medicine 17(3):427–431.
GAO (U.S. Government Accountability Office). 2003a. Hospital Emergency Departments: Crowded Conditions Vary among Hospitals and Communities (GAO-03-460). Washington, DC: GAO.
GAO. 2003b. Medical Malpractice: Implications of Rising Premiums on Access to Health Care (GAO-03-836). Washington, DC: GAO.
Glabman M. 2005. Specialist shortage shakes emergency rooms; more hospitals forced to pay for specialist care. The Physician Executive 6–11.
Goldberg RM, Mabee J, Chan L, Wong S. 1996. Drug-drug and drug-disease interactions in the ED: Analysis of a high-risk population. American Journal of Emergency Medicine 14(5):447–450.
Greater New York Hospital Association. 2004. Survey of Nurse Staffing in GNYHA Member Hospitals, 2003. New York: Greater New York Hospital Association.
Green L, Melnick GA, Nawathe A. 2005. On-Call Physicians at California Emergency Departments: Problems and Potential Solutions. Oakland, CA: California Healthcare Foundation.
Hackenschmidt A. 2004. Living with nurse staffing ratios: Early experiences. Journal of Emergency Nursing 30(4):377–379.
Hellinger FJ, Encinosa WE. 2005. Impact of State Laws Limiting Malpractice Awards on Geographic Distribution of Physicians. Rockville, MD: Department of Health and Human Services, Agency for Healthcare Research and Quality.
Hockberger RS, Binder LS, Graber MA, Hoffman GL, Perina DG, Schneider SM, Sklar DP, Strauss RW, Viravec DR, Koenig WJ, Augustine JJ, Burdick WP, Henderson WV, Lawrence LL, Levy DB, McCall J, Parnell MA, Shoji KT, American College of Emergency Physicians Core Content Task Force II. 2001. The model of the clinical practice of emergency medicine. Annals of Emergency Medicine 37(6):745–770.
Holliman CJ, Wuerz RC, Chapman DM, Hirshberg AJ. 1997. Workforce projections for emergency medicine: How many emergency physicians does the United States need? Academic Emergency Medicine 4(7):725–730.
Hurley RE, Pham HH, Claxton G. 2005. A widening rift in access and quality: Growing evidence of economic disparities. Health Affairs Web Exclusive.
IOM (Institute of Medicine). 2000. To Err Is Human: Building a Safer Health System. Washington, DC: National Academy Press.
IOM. 2004a. Keeping Patients Safe: Transforming the Work Environment of Nurses. Washington, DC: The National Academies Press.
IOM. 2004b. Quality Through Collaboration: The Future of Rural Health. Washington, DC: The National Academies Press.
Jacobsen C, Holson D, Farley J, Charles J, Suel P. 2002. Surviving the perfect storm: Staff perceptions of mandatory overtime. JONA’s Healthcare Law, Ethics and Regulation 4(3):57–66.
JCAHO (Joint Commission for the Accreditation of Healthcare Organizations). 2005. 2005 Hospitals’ National Patient Safety Goals. [Online]. Available: http://www.jcaho.org/accredited+organizations/patient+safety/05+npsg/05_npsg_hap.htm [accessed August 9, 2005].
Jones JH, Weaver CS, Rusyniak DE, Brizendine EJ, McGrath RB. 2002. Impact of emergency medicine faculty and an airway protocol on airway management. Academic Emergency Medicine 9(12):1452–1456.
Kaiser Commission on Medicaid and the Uninsured. 2003. Medicaid Benefits. [Online]. Available: http://www.kff.org/medicaid/benefits/index.cfm [accessed August 20, 2004].
Kane CK. 2003. Physician Marketplace Report: The Impact of EMTALA on Physician Practices. Chicago, IL: American Medical Association, Center for Health Policy Research.
Kaushal R, Bates DW, Landrigan C, McKenna KJ, Clapp MD, Federico F, Goldmann DA. 2001. Medication errors and adverse drug events in pediatric inpatients. Journal of the American Medical Association 285(16):2114–2120.
Kaushal R, Bates D. 2001. The clinical pharmacist’s role in preventing adverse drug events. In: Making Health Care Safer: A Critical Analysis of Patient Safety Practices (Evidence Report/Technology Assessment, No. 43). Rockville, MD: Agency for Healthcare Research and Quality.
Keim S, Chisholm C. 2000. Moonlighting and emergency medicine: Raising the standard. Academic Emergency Medicine 7(8):927–928.
Kellermann AL. 1995. Moonlighting. Annals of Emergency Medicine 26(1):83–84.
Lambert VA, Lambert CE. 2001. Literature review of role stress/strain on nurses: An international perspective. Nursing & Health Sciences 3(3):161–172.
Leap E. 2000. The stigma of being a rural EP. EM News. P. 12.
Leape L, Cullen D, Dempsey Clapp M, Burdick E, Demonaco H, Ives Errickson J, Bates D. 1999. Pharmacist participation on physician rounds and adverse drug events in the intensive care unit. Journal of the American Medical Association 281(3):267–270.
The Leapfrog Group. 2004. ICU Physician Staffing Factsheet. Washington, DC: The Leapfrog Group.
Li J, Tabor R, Martinez M. 2000. Survey of moonlighting practices and work requirements of emergency medicine residents. American Journal of Emergency Medicine 18(2):147–151.
Macasaet A, Zun A. 2005. The On-Call Physician. [Online]. Available: http://www.Emedicine. com [accessed February 10, 2006].
MacKenzie EJ, Rivara FP, Jurkovich GJ, Nathens AB, Frey KP, Egleston BL, Salkever DS, Scharfstein DO. 2006. A national evaluation of the effect of trauma-center care on mortality. New England Journal of Medicine 354(4):366–378.
Maguire P. 2001, November. Wanted: Doctors willing to take ER call. ACP-ASIM Observer.
Marx J. 2005. Education. [Online]. Available: http://www.carolinas.org/education/meded/ emergency/emergency_chairman.cfm [accessed February 8, 2005].
Matsa D. 2005. Does Malpractice Liability Keep the Doctor Away? Evidence from Tort Reform Damage Caps. Boston, MA: MIT.
Mays GP, Bodenheimer T, Felland LE, McKenzie KL, Regopoulos LE. 2005. Uninsured Patients, Malpractice Insurance Woes Stress Miami Health Care Market. Washington, DC: Center for Studying Health System Change.
McCaig LF, Burt CW. 2005. National Hospital Ambulatory Medical Care Survey: 2003 Emergency Department Summary. Hyattsville, MD: National Center for Health Statistics.
McNamara R. 2006. Emergency Medicine and the Physician Practice Management Industry: History, Overview, and Current Problems. [Online]. Available: http://www.aaem.org/ corporatepractice/history.shtml [accessed March 1, 2006].
Moorhead JC, Gallery ME, Mannle T, Chaney WC, Conrad LC, Dalsey WC, Herman S, Hockberger RS, McDonald SC, Packard DC, Rapp MT, Rorrie CC Jr, Schafermeyer RW, Schulman R, Whitehead DC, Hirschkorn C, Hogan P. 1998. A study of the workforce in emergency medicine. Annals of Emergency Medicine 31(5):595–607.
Moorhead JC, Gallery ME, Hirshkorn C, Barnaby DP, Barsan WG, Conrad LC, Dalsey WC, Fried M, Herman SH, Hogan P, Mannle TE, Packard DC, Perina DG, Pollack CV Jr, Rapp MT, Rorrie CC Jr, Schafermeyer RW. 2002. A study of the workforce in emergency medicine: 1999. Annals of Emergency Medicine 40(1):3–15.
Morchi R. 2002. High-fidelity medical simulation and teamwork training to enhance medical student performance in cardiac resuscitation [Abstract]. Academic Emergency Medicine 9(10):1055.
National Institute for Occupational Safety and Health. 2004. Worker Health Chartbook, 2004. Cincinnati, OH: Department of Health and Human Services.
National League for Nursing. 2005. Despite Encouraging Trends Suggested by the NLN’s Comprehensive Survey of All Nursing Programs, Large Number of Qualified Applications Continue to be Turned Down. [Online]. Available: http://www.nln.org/newsreleases/nedsdec05.pdf [accessed February 17, 2006].
Needleman J, Buerhaus P, Mattke S, Stewart M, Zelevinsky K. 2002. Nurse-staffing levels and the quality of care in hospitals. New England Journal of Nursing 346(22):1715–1722.
New York State Education Department. 2003. Registered Nurses in New York State, 2002, Survey Data. Albany, NY: NY State Education Department.
NHT (Nurses for a Healthier Tomorrow). 2006. Emergency Nurse. [Online]. Available: http://www.nursesource.org/emergency.html [accessed February 1, 2006].
NREMT (National Registry of EMTs). 2005. National EMS Practice Analysis. Columbus, OH: NREMT.
O’Malley AS, Gerland AM, Pham HH, Berenson RA. 2005. Rising Pressure: Hospital Emergency Departments: Barometers of the Health Care System. Washington, DC: The Center for Studying Health System Change.
Ordog GJ, Wasserberger J, Ordog C, Ackroyd G, Atluri S. 1995. Weapon carriage among major trauma victims in the emergency department. Academic Emergency Medicine 2(2):109–113; discussion 114.
Osborn TM, Scalea TM. 2002. A call for critical care training of emergency physicians. Annals of Emergency Medicine 39(5):562–563.
Pan S, Geller JM, Muus KJ, Hart LG. 1996. Predicting the degree of rurality of physician assistant practice location. Hospital & Health Services Administration 41(1):105–119.
Patow CA. 2005, March/April. Advancing medical education and patient safety through simulation learning. Patient Safety & Quality Healthcare.
Perception Solutions, Inc. 2004. AANS-CNS Neurological Survey—Emergency and Trauma Services: Analysis & Result Reporting. Aurora, IL: Perception Solutions, Inc.
Pham HH, Devers KJ, Kuo S, Berenson R. 2005. Health care market trends and the evolution of hospitalist use and roles. Journal of General Internal Medicine 20(2):101–107.
Plantz SH, Kreplick LW, Panacek EA, Mehta T, Adler J, McNamara RM. 1998. A national survey of board-certified emergency physicians: Quality of care and practice structure issues. American Journal of Emergency Nursing 16(1):1–4.
Pronovost P, Wu AW, Dorman T, Morlock L. 2002. Building safety into ICU care. Journal of Critical Care 17(2):78–85.
Pronovost PJ, Jenckes MW, Dorman T, Garrett E, Breslow MJ, Rosenfeld BA, Lipsett PA, Bass E. 1999. Organizational characteristics of intensive care units related to outcomes of abdominal aortic surgery. Journal of the American Medical Association 281(14):1310–1317.
Ray C, Jagim M, Agnew J, McKay J, Sheehy S. 2003. ENA’s new guidelines for determining emergency department nurse staffing. Journal of Emergency Nursing 29(3):245–253.
Risser DT, Rice MM, Salisbury ML, Simon R, Jay GD, Berns SD. 1999. The potential for improved teamwork to reduce medical errors in the emergency department. The MedTeams Research Consortium. Annals of Emergency Medicine 34(3):373–383.
Robinson KS, Jagim MM, Ray CE. 2004. Nursing Workforce Issues and Trends Affecting U.S. Emergency Departments. Falls Church, VA: KAR Associates.
Rogers AE, Hwang W-T, Scott LD, Aiken LH, Dinges DF. 2004. The working hours of hospital staff nurses and patient safety. Health Affairs 23(4):202–212.
Rosen P. 1995. History of Emergency Medicine. New York: Josiah Macy, Jr. Foundation. Pp. 59–79.
Russell T. 2004. Understanding the latest changes in EMTALA: Our country’s emergency care safety net. ACS Cross Country (February). [Online]. Available: www.facs.org/ahp/feb04crosscountry.html 89 [accessed June 22, 2006].
Salsberg E. 2005. Physician Workforce Issues and Trends: Implications for Surgical Specialties. Presentation at the meeting of the ACS Meeting on Workforce Issues, Chicago, IL.
Scaletta T. 2003. Performing without a Net. [Online]. Available: http://www.aaem.org/ commonsense/rules5.shtml [accessed January 26, 2005].
Scheck A. 2004. Payments to specialists are rescuing on-call panels. Emergency Medicine News 26(10):1, 28–29.
Schenkel S. 2000. Promoting patient safety and preventing medical error in emergency departments. Academic Emergency Medicine 7(11):1204–1222.
Schriver J, Talmadge R, Chuong R, Hedges J. 2003. Emergency nursing: Historical, current, and future roles. Academic Emergency Medicine 10(7):798–804.
Selbst SM, Fein JA, Osterhoudt K, Ho W. 1999. Medication errors in a pediatric emergency department. Pediatric Emergency Care 15(1):1–4.
Shapiro MJ, Morey JC, Small SD, Langford V, Kaylor CJ, Jagminas L, Suner S, Salisbury ML, Simon R, Jay GD. 2004. Simulation based teamwork training for emergency department staff: Does it improve clinical team performance when added to an existing didactic teamwork curriculum? Quality and Safety in Healthcare 13(6):417–421.
Sklar D, Spencer D, Alcock J, Cameron S, Saiz M. 2002. Demographic analysis and needs assessment of rural emergency departments in New Mexico (DANARED–NM). Annals of Emergency Medicine 39(4):456–457; author reply 457.
Small SD, Wuerz RC, Simon R, Shapiro N, Conn A, Setnik G. 1999. Demonstration of high-fidelity simulation team training for emergency medicine. Academic Emergency Medicine 6(4):312–323.
Society of Hospital Medicine. 2006. FAQ’s. [Online]. Available: http://www.hospitalmedicine.org/AM/Template.cfm?Section=FAQs&Template=/FAQ/FAQListAll.cfm [accessed February 1, 2006].
Sprague L. 1999. Reducing Medical Error: Can You Be As Safe in a Hospital As You Are in a Jet? Washington, DC: National Health Policy Forum.
Steele MT, Schwab RA, McNamara RM, Watson WA. 1998. Emergency medicine resident choice of practice location. Annals of Emergency Medicine 31(3):351–357.
Taheri PA, Butz DA. 2004. Specialist On-Call Coverage of Palm Beach County Emergency Departments. Palm Beach County, FL: Palm Beach County Medical Society Services.
Thomasset KB, Faris R. 2003. Survey of pharmacy services provision in the emergency department. American Journal of Health-System Pharmacy 60(15):1561–1564.
Thorpe K. 2004. The medical malpractice “crisis”: Recent trends and the impact of state tort reforms. Health Affairs Web Exclusive W4–20.
Valadka A. 2004. RE: The ER, who is answering call? American Association of Neurological Surgeons 13(4):6–12.
Vozenilek J, Huff JS, Reznek M, Gordon JA. 2004. See one, do one, teach one: Advanced technology in medical education. Academic Emergency Medicine 11(11):1149–1154.
Wachter R. 2004. The hospitalist movement: Ten issues to consider. Hospital Practice 2.
Wears RL, Simon R. 2000. Testimony of Robert L. Wears and Robert Simon. Panel 2: Broad-based Systems Approaches. Written Statement: Creating Complementary Roles for Behavioral Solutions and Technology Applications to Patient Safety. National Summit on Medical Errors and Patient Safety Research.
Weaver CS, Avery SJ, Brizendine EJ, McGrath RB. 2004. Impact of emergency medicine faculty on door to thrombolytic time. The Journal of Emergency Medicine 26(3):279–283.
Whaley S. 2002, July 10. Opinion offers hope for trauma center. The Las Vegas Review Journal. P. 18.
White AA, Wright SW, Blanco R, Lemonds B, Sisco J, Bledsoe S, Irwin C, Isenhour J, Pichert JW. 2004. Cause-and-effect analysis of risk management files to assess patient care in the emergency department. Academic Emergency Medicine 11(10):1035–1041.
Williams J, Ehrlich P, Prescott J. 2001. Emergency medical care in rural America. Annals of Emergency Medicine 38(3):323–327.
Yoo GJ, Dawson-Rose C, Chang YJ, Aquino J. 2001. Factors Impacting the Availability of Emergency On-Call Coverage in California: Report to the California State University Faculty Fellows Program. [Online]. Available: http://www.csus.edu/calst/Government_Affairs/reports/Emergency_Room_On-Call_Coverage.pdf [accessed June 23, 2005].


















































