9
Diagnosis and Treatment of Conditions Leading to Spontaneous Preterm Birth
ABSTRACT
The diagnosis and treatment of preterm labor is currently based on an inadequate literature. Not only is there a paucity of welldesigned and adequately powered clinical trials, but there is incomplete understanding of the sequence and timing of events that precede clinical evidence of preterm labor. To date, there is no single test or sequence of assessment measures to accurately predict preterm birth. Prevention of preterm birth has primarily focused on the treatment of the woman with symptomatic preterm labor. Treatment has been directed toward the inhibition of contractions. This approach has not decreased the incidence of preterm birth but can delay delivery long enough to allow administration of antenatal steroids and to transfer the mother and the fetus to an appropriate hospital, two interventions that have consistently been shown to reduce the rates of perinatal mortality and morbidity. Preterm birth has historically not been emphasized in prenatal care, in the belief that the majority of preterm births are due to social rather than medical or obstetric causes or are the appropriate result of pathological processes that would benefit the mother or the infant, or both. Because preterm labor or premature rupture of membranes may occur in response to conditions that threaten fetal or maternal well-being, whether preterm birth is appropriately preventable is a topic that regularly influences clinical decision making. The ultimate goal of treatment for preterm labor is to eliminate or reduce
perinatal morbidity and mortality. Thus, despite several interventions designed to inhibit preterm labor and prolong pregnancy, the frequency of preterm birth continues to pose a major barrier to the health of newborns worldwide. Although current obstetric and neonatal strategies have resulted in improved rates of neonatal survival and an earlier threshold for viability, effective strategies for the prevention of preterm birth are urgently needed. As basic and translational research continues to reveal more of the complex endocrinological and immunological aspects of parturition, investigators must continue to search for biologically plausible new therapies to prevent preterm birth and develop markers or multiple markers to diagnose the disease accurately in its early stages.
Nearly 75 percent of the cases of perinatal mortality and approximately half of the cases of long-term neurologic morbidity occur in infants born preterm. Preterm births have been organized into two broad categories, spontaneous and indicated, based on the presence or absence of factors that place the mother or the fetus at risk (Meis et al., 1987, 1995, 1998). Spontaneous preterm births occur as a result of preterm labor or preterm premature rupture of fetal membranes before 37 weeks of gestation and account for the majority of preterm births in developed countries. Preterm births that are the result of conditions that directly threaten the health of the mother or fetus, such as preeclampsia, placenta previa, and fetal growth restriction, are categorized as indicated preterm births and account for the remaining 25 to 30 percent of preterm deliveries (Meis et al., 1987, 1995, 1998). Although categorization of preterm births as indicated versus spontaneous allows analysis of preterm births according to those that might be prevented versus those that might be beneficial, there is increasing recognition that this distinction may understate the contribution of factors such as vascular compromise or fetal stress to the pathogenesis of preterm labor. This is suggested by reports that infants born after spontaneous preterm labor in the absence of apparent maternal disease have a higher than expected rate of poor intrauterine growth (Bukowski et al., 2001b; Gardosi, 2005). Figure 9-1 shows the negative skew in birth weights for fetuses destined for preterm birth versus the range of fetal weights of fetuses ultimately born at term. Efforts to prevent preterm birth must therefore be applied and evaluated primarily for their effects on perinatal mortality and morbidity.
The care of infants born preterm and their mothers may be described as primary (prevention and reduction of risk in the population), secondary (identification of and treatment for individuals with an increased risk), and tertiary (treatment aimed at reducing morbidity and mortality after the
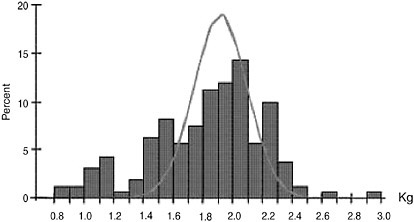
FIGURE 9-1 Ultrasound versus birth weight standard at 32 weeks of gestation.
SOURCE: Gardosi et al. (2005). Reprinted with permission from Early Human Development, Vol. 81, Pg. 45, © 2004 by Elsevier.
preterm parturitional process has begun). In the past 30 years, important strides in obstetric and neonatal tertiary care have been made to reduce the rates of infant morbidity and mortality related to preterm birth. However, the primary and secondary interventions used to date have not reduced the rate of spontaneous preterm birth. This chapter describes and assesses the success of secondary- and tertiary-care practices. As will become evident as these are recounted, there are major impediments to the appropriate application of reasonable interventions for the risk factors for preterm birth. Many risk factors have been identified and removed without affecting the rate or morbidity of preterm birth. Cofactors, both exogenous and innate, that might contribute to or impede the success of an intervention are not well understood. Because clinically overt evidence of preterm labor is often preceded by weeks or months of activation of the parturitional process, the optimal timing for effective interventions is not always clear. Figure 9-2 presents these interactions.
Remarkably, current prenatal care is focused on risks other than preterm birth. Birth defects, adequate fetal growth, preeclampsia, gestational diabetes, selected infections (urinary tract, group B streptococcus, and rubella virus infections), and complications of postdate pregnancy are emphasized in the prenatal record (see Attachment 9-1). Preterm birth has historically not been emphasized in prenatal care in the belief that the majority of preterm births are due to social rather than medical or obstetrical causes (Main et al., 1985; Taylor, 1985) or are the appropriate result of pathological processes that would benefit the mother or the infant, or both. More recently, the failure of repeated efforts to prevent preterm birth (see
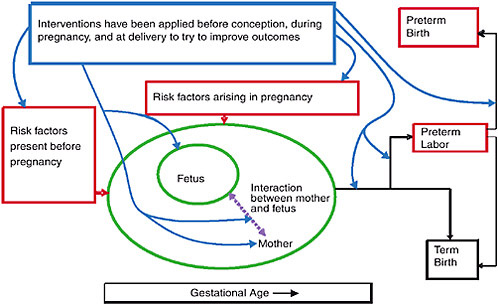
FIGURE 9-2 Interventions for preterm birth.
below) has lent support to the historical view. Because preterm labor or preterm premature rupture of membranes may occur in response to conditions that threaten fetal or maternal well-being, whether preterm birth is appropriately preventable is a topic that regularly influences clinical decision making.
Thus, efforts to prevent preterm birth have increasingly focused on early pregnancy and preconceptional care. Some risks are amenable to intervention, whereas others serve primarily to inform theories of causation or to identify at-risk groups for further study.
Finding 9-1: Prenatal care was designed to address one complication of pregnancy; namely, preeclampsia. The proper timing of visits and the appropriate content of prenatal care for the detection or management of preterm delivery are not known.
PREDICTION AND ASSESSMENT OF RISK OF PRETERM BIRTH
The rationale for prediction of spontaneous preterm birth is threefold. First, by delineating factors predictive of preterm birth, the mechanisms and biological pathways that lead to spontaneous preterm parturition may be better understood. Second, the use of predictors of spontaneous preterm
birth permits identification of a group of women at the highest risk for whom an intervention may be tested and for whom intervention is most needed. The third motivation for prediction of spontaneous preterm birth is a corollary of the second: by identifying women at low risk for preterm birth, unnecessary, costly, and sometime hazardous interventions might be avoided. To date, no single test or sequence of tests has an optimal sensitivity or predictive value. This section reviews clinical, biophysical, and biochemical tests that can be used as predictors for preterm birth.
CLINICAL PREDICTORS
Clinical risk factors alone or in combination most frequently report a sensitivity of about 25 percent for prediction of preterm birth (Goldenberg et al., 1998; Mercer et al., 1996). Low prepregnancy weight (body mass index less than 19.8), genitourinary bacterial colonization or infection, and African American ethnicity have relative risks (RRs) of about twofold but contribute significant attributable risk because of their prevalence in the population. African American women deliver before 37 weeks of gestation twice as often as women of other races and ethnicities and deliver before 32 weeks of gestation three times as often as white women. The strongest risk factors in all racial-ethnic groups are multiple gestation (RR = five- to six-fold), a history of preterm birth (RR = three- to fourfold), and vaginal bleeding (RR = threefold).
The risk of preterm and low-birth-weight delivery rises in direct proportion to the number of fetuses, as can be seen Table 9-1.
Vaginal bleeding in pregnancy is a risk factor for preterm birth because of placenta previa, because of placental abruption, and when the origin is unclear (Ekwo et al., 1992; Meis et al., 1995; Yang et al., 2004b). Unexplained vaginal bleeding is particularly associated with preterm birth if it is persistent and if it occurs in white women (Yang et al., 2004b).
The risk of recurrent preterm birth rises with the number of prior preterm births, with maternal African American ethnicity, and as the gestational age of the prior preterm birth decreases (Adams et al., 2000; Mercer et al., 1999). The effect of a woman’s prior obstetrical history on the risk of preterm birth is shown in Table 9-2.
The data in Table 9-2 describe a homogeneous population from Norway. Data from the United States show the same phenomenon, with markedly increased rates of preterm birth for African Americans, reaching 50 percent or more for an African American woman with two or more prior preterm deliveries (Adams et al., 2000; Mercer et al., 1996). Other reported risk factors include the use of assisted reproductive technology, poor nutrition, periodontal disease, absent or inadequate prenatal care, age less than 18 years or over 35 years, strenuous work, high levels of personal stress,
TABLE 9-1 Risks of Preterm and Low Birth Weight Births by Number of Fetuses
|
Births |
Twin |
Triplet |
Quadruplet |
Quintuplet |
|
<32 wk |
12 percent |
36 percent |
60 percent |
78 percent |
|
<37 wk |
58 percent |
92 percent |
97 percent |
91 percent |
|
Mean GA |
35 wk |
32 wk |
30 wk |
28 wk |
|
<1.5 kg |
10 percent |
34 percent |
61 percent |
84 percent |
|
<2.5 kg |
55 percent |
94 percent |
99 percent |
94 percent |
|
|
Risk of Preterm Birth or Low Birth Weight (%) |
|||
|
No. of Births |
<32 wk of Gestation |
<37 wk of Gestation |
Birth Weight <1.5 kg |
Birth Weight <2.5 kg |
|
Twin |
12 |
58 |
10 (35 wk)a |
55 (35 wk) |
|
Triplet |
36 |
92 |
34 (32 wk) |
94 (32 wk) |
|
Quadruplet |
60 |
97 |
61 (30 wk) |
99 (30 wk) |
|
Quintuplet |
78 |
91 |
84 (28 wk) |
94 (28 wk) |
|
aTimes in parentheses are mean gestational age. SOURCE: CDC (2002c). |
||||
TABLE 9-2 Risk of Preterm Delivery by Obstetrical History
|
Outcome of First Birth |
Outcome of Second Birth |
Number of Women |
Likelihood of Peterm Birth in Next Pregnancy |
|
|
|
|
|
Percent |
RR |
|
Term |
|
25,817 |
4.4 |
1.0 |
|
Preterm |
|
1,860 |
17.2 |
3.9 |
|
Term |
Term |
24,689 |
2.6 |
.6 |
|
Preterm |
Term |
1,540 |
5.7 |
1.3 |
|
Term |
Preterm |
1,128 |
11.1 |
2.5 |
|
Preterm |
Preterm |
320 |
28.4 |
6.5 |
|
SOURCE: Bakketeig and Hoffman (1981). |
||||
anemia, cigarette smoking, cervical injury or abnormality, and uterine anomaly (Meis et al., 1995; Mercer et al., 1996). As discussed in Chapter 5, the increased number of pregnancies conceived after the use of assisted reproductive technologies is associated with a rise in preterm birth not only because of multiple gestations but also because the singleton gestations that
occur after the use of assisted reproductive technologies have a twofold increased risk of preterm birth (Jackson et al., 2004; Schieve et al., 2004; Van Voorhis, 2006).
Biophysical Predictors
Uterine Contractions
The detection of uterine contractions through maternal self-perception (Mercer et al., 1996) and electronic monitoring (Iams et al., 2002; Main et al., 1993; Nageotte et al., 1988) has been studied to predict preterm delivery. The threshold number of contractions most often studied is four per hour. An increased frequency of self-reported contractions is associated with preterm delivery before 35 weeks of gestation in both nulliparous women (RR 2.41; 95% interval [CI] 1.47–3.94; p < 0.001) and parous women (RR 1.62; 95% CI 1.20–2.18; p = 0.002) women (Mercer et al., 1996). In a study of 306 women in whom uterine contraction frequency was electronically recorded for 2 or more hours a day at least twice weekly between 22 and 37 weeks of gestation, contraction frequency was significantly greater in women who delivered before 35 weeks of gestation than in women who delivered after 35 weeks of gestation (Table 9-3) (Iams et al., 2002). Con-
TABLE 9-3 Prediction of Spontaneous Preterm Birth before 35 Weeks of Gestation (22 to 24 and 27 to 28 Weeks of Gestation) in 306 Women at Risk of Preterm Birth
|
Gestational Length and Test |
Sensitivity (%) |
Specificity (%) |
Predictive Value (%) |
|
|
Positive |
Negative |
|||
|
22 to 24 wk |
||||
|
UC ≥4/h |
6.7 |
92.3 |
25.0 |
84.7 |
|
Bishop score ≥4 |
32.0 |
91.4 |
42.1 |
87.4 |
|
CL ≤25 mm |
40.8 |
89.5 |
42.6 |
88.8 |
|
Fibronectin level ≥50 ng/ml |
18.0 |
95.3 |
42.9 |
85.6 |
|
27 to 28 wk |
||||
|
UC ≥4/h |
28.1 |
88.7 |
23.1 |
91.1 |
|
Bishop score ≥4 |
46.4 |
77.9 |
18.8 |
92.9 |
|
CL ≤25 mm |
53.6 |
82.2 |
25.0 |
94.1 |
|
Fibronectin level ≥50 ng/ml |
21.4 |
94.5 |
30.0 |
91.6 |
|
NOTE: UC = uterine contractions; CL = cervical length. SOURCE: Iams et al. (2002). |
||||
tractions increased significantly as gestational age advanced and were more frequent between 4 p.m. and 4 a.m. Although the difference in contraction frequency was statistically significant, contraction frequency was not a clinically efficient predictor of preterm birth at 24 or 28 weeks of gestation. The threshold of four or more contractions per hour at 24 and 28 weeks of gestation for prediction of the risk of preterm birth had sensitivities of 8.6 and 28 percent, respectively, and positive predictive values of 25 and 23 percent, respectively (Iams et al., 2002).
Clinical studies of the symptoms of preterm birth (Hueston, 1998; Macones et al., 1999b) confirm the poor performance of contraction frequency as a test for acute preterm labor as well.
Cervical Examination
Manual examination Cervical dilatation, effacement, consistency, position, and station of the presenting part as determined by manual examination have been related to an increased risk of preterm birth (Copper et al., 1990; Iams et al., 1996; Mercer et al., 1996; Newman et al., 1997). However, even when these features are combined in composite scores (e.g., Bishop scores [Bishop, 1964] or cervical scores [Newman, 1997]) of cervical readiness for labor, the sensitivity is low. The RRs for birth before 35 weeks of gestation were increased at 24 weeks of gestation: 5.3 (95% CI 3.4–8.5) for the cervical score (defined as cervical length in centimeters minus the cervical dilatation in centimeters) and 3.5 (95% CI 2.4–5.0) for the Bishop score. The sensitivities of both scores for prediction of the risk of preterm birth in a general obstetrical population were low, however: 13.4 and 27.6 percent, respectively (Iams et al., 1996; Newman et al., 1997).
Sonographic evaluation A decreased cervical length as measured by endovaginal ultrasound examination has also been related to an increased risk of preterm birth. The RR of preterm birth before 35 weeks of gestation was about sixfold higher (95% CI 3.84–9.97) among women whose cervical length was less than the 10th percentile (25 millimeters [mm]) than that among women with a cervical length above the 75th percentile (40 mm), but the absolute risk of birth before 35 weeks of gestation and the sensitivity were both only 40 percent in two studies performed in the United States (Iams et al., 1996, 2002). A study of cervical length in low-risk women found an eightfold increased risk of preterm birth when the cervix was less than 29 mm at 18 to 22 weeks of gestation, but the sensitivity and positive predictive value were low: 19 and 6 percent, respectively (Taipale and Hiilesmaa, 1998). Finally, the likelihood ratio for prediction of birth before 34 weeks of gestation for a cervical length of 25 mm or less when the length was measured before 20 weeks of gestation was estimated to be +6.3 (95%
CI 3.3–12.0), indicating that the risk of preterm birth is 6.3 times greater for women whose cervical length is < 25 mm than for those whose cervical length is >25 mm (Honest et al., 2003).
Biological Predictors
Biological markers may be collected from maternal blood or urine, cervicovaginal fluid secretions, or amniotic fluid. Maternal blood and vaginal fluids have been the most studied. Table 9-4 summarizes the myriad efforts used to identify the risk of preterm birth based on biomarkers from asymptomatic women (Vogel et al., 2005).
Serum Biomarkers
Maternal serum is routinely drawn several times during prenatal care. Screening of serum biomarkers for various conditions, such as open neural tube defects and aneuploidy, is already part of routine prenatal care (Canick et al., 2003; Cheschier, 2003). The use of serum biomarkers of spontaneous preterm birth to identify several pathways to preterm birth have been investigated, as described by Romero and colleagues (1994) and Lockwood and Kuczynski (2001) and described in Chapter 6, including (1) activation of maternal or fetal hypothalamic-pituitary-adrenal axis (e.g., corticotropinreleasing hormone) and (2) inflammation due to upper genital tract infection (e.g., defensins and tumor necrosis factor alpha) or decidual hemorrhage or ischemia (e.g., thrombin-antithrombin III complex). No serum biomarkers of pathologic uterine overdistension have been described.
Lower Genital Tract Markers
Bacterial vaginosis (BV) is an alteration of the maternal vaginal flora in which normally predominant lactobacilli are largely replaced by gram-negative anaerobic bacteria, such as Gardnerella vaginalis and Bacteroides, Prevotella, Mobiluncus, and Mycoplasma species. BV in pregnancy is consistently associated with a twofold increased risk of spontaneous preterm birth (Hillier et al., 1995; Meis et al., 1995). The association of BV with preterm birth has been reported to be stronger when the condition is present in the first half of pregnancy (Hay et al., 1994), but a recent analysis of the relationship between gestational age at the time of detection of BV and pregnancy outcome in 12,937 women found “the odds ratio of preterm birth among BV-positive versus -negative women raged from 1.1 to 1.6 and did not vary significantly according to the gestational age at which BV was screened” (Klebanoff et al., 2005, p 470). Despite the consistency of the reports relating BV to preterm birth, the clinical utility of tests for BV to
TABLE 9-4 Ability of Selected Biomarkers to Predict Preterm Delivery in Asymptomatic Women
|
Biomarker |
No. of Subjects |
Compartment |
GA (wk) at Sampling |
End Point (GA [wk]) |
LR+ |
SENS (%) |
FP (%) |
Referencea |
|
Multiple gestations (≥2 of 5) |
177 |
S/P, C, V+C |
24 |
<32 |
24 |
59 |
2 |
58 |
|
Ureaplasma urealyticum |
254 |
Amniotic fluid |
<17 |
<37 |
10 |
88 |
9 |
9 |
|
Relaxin |
176 |
S/P |
<24 |
<34 |
6.8 |
27 |
4 |
64 |
|
Cervical length |
Meta-analysis |
Cervix |
<24 |
<34 |
6.3 |
|
|
29 |
|
Alkaline phosphatase |
1,868 |
S/P |
<20 |
<37 |
4.6 |
14 |
3 |
69 |
|
CRH |
860 |
S/P |
<30 |
<37 |
3.0 |
39 |
13 |
40 |
|
G-CSF |
388 |
S/P |
24 |
<32 |
3.3 |
49 |
15 |
16 |
|
Interleukin-6 |
250 |
V+C |
24 |
<32 |
3.3 |
20 |
6 |
15 |
|
Interleukin-6 |
580 |
Amniotic fluid |
<20 |
<34 |
2.8 |
14 |
5 |
14 |
|
Fetal fibronectin |
Meta-analysis |
V+C |
>20 |
<37 |
2.9 |
|
|
22 |
|
α-Fetoprotein |
254 |
S/P |
24 |
<35 |
2.6 |
35 |
13 |
58 |
|
Chlamydia |
380 |
U |
24 |
<37 |
2.5 |
16 |
6 |
10 |
|
Ferritin |
100 |
S/P |
34 |
<37 |
2.2 |
75 |
33 |
70 |
|
C-reactive protein |
484 |
S/P |
<21 |
<37 |
1.8 |
26 |
15 |
75 |
|
Bacterial vaginosis |
Meta-analysis |
V+C |
<24 |
<37 |
1.6 |
|
|
8 |
|
Ferritin |
364 |
V+C |
<25 |
<37 |
1.4 |
35 |
25 |
71 |
|
NOTE: LR+ = likelihood ratio; SENS = sensitivity; FP = false-positive rate; CRH = corticotropin-releasing hormone; G-CSF = granulocyte colony-stimulating factor; U = uterine; V = vaginal secretions; C = cervical secretions; S/P = serum or plasma; GA = gestational age. aCitations in the paper by Vogel et al. (2005). SOURCE: Vogel et al. (2005). |
||||||||
identify women at risk is low, owing to the modest strength of the association, the high prevalence of BV in some populations, and the high degrees of variation in the accuracies of the tests used to detect BV (Honest et al., 2004).
Testing of the cervicovaginal secretions of asymptomatic women have been screened for markers of preterm birth, including fetal fibronectin (Goldenberg et al., 1996b,c, 1998), interleukins 6 and 8 (Goepfert et al., 2001; Kurkinen-Raty et al., 2001), and tumor necrosis factor alpha and matrix metalloproteinases (Vogel et al., 2005). The biochemical test for fetal fibronectin is the one about which the most data are available and is the only one marketed in the United States for that purpose.
Fetal Fibronectin
Fetal fibronectin is a glycoprotein of fetal origin that normally resides at the decidual-chorionic interface within the uterus but is present in cervicovaginal secretions in 3 to 4 percent of pregnant women at between 21 and 37 weeks of gestation (Goldenberg et al., 1996c; Lockwood et al., 1991). Evaluation of fibronection levels in asymptomatic women at 24 weeks of gestation has a sensitivity of 20 to 30 percent for the prediction of spontaneous preterm birth at before 35 weeks of gestation (Goldenberg et al., 1996c; Iams et al., 2002). The sensitivity of determination of fibronectin levels for prediction of early preterm births before 28 weeks of gestation was found to be 63 percent (Goldenberg et al., 1996c). Determination of fibronectin levels is a better test for screening for the risk of delivery within 2 weeks of sampling than for delivery before a specific gestational week of pregnancy (Goldenberg et al., 1997).
Combination of Markers
Given the pathophysiological heterogeneity of the causes of spontaneous preterm birth, the clinical utility of any individual biomarker for predicting preterm birth is limited. Combinations of markers can increase the sensitivity of the prediction by combining risk predictors that address diverse causes of spontaneous and indicated preterm birth (Goldenberg et al., 2001). The positive predictive value can also be increased (at the sacrifice of sensitivity) by combining selected markers such as the woman’s obstetric history and cervical length; for example, a sonographic cervical length less than 25 mm predicted recurrent preterm birth in 100 percent of African American women with a prior preterm birth (Yost et al., 2004).
Goldenberg and colleagues (1998) sought to develop a multiple-marker test for preterm birth with data collected in the Preterm Prediction Study of
the Maternal-Fetal Medicine Units (MFMU) Network of the National Institute of Child Health and Human Development (NICHD). They performed a nested case-control study with a cohort of 2,929 women with singleton gestations recruited from the general obstetric populations of the 10 participating centers (Goldenberg et al., 2001). The women in that study underwent serial assessment of serum, cervical, vaginal, ultrasound, and historical markers or risk factors. The serum markers associated with spontaneous preterm birth at less than 32 weeks of gestation were α-fetoprotein, alkaline phosphatase, granulocyte-macrophage colony-stimulating factor, and defensins. The only serum markers related to spontaneous preterm birth at less than 35 weeks of gestation were α-fetoprotein and alkaline phosphatase. Importantly, the overlap between the biomarkers was small, supporting the concept that there are several heterogeneous pathways to spontaneous preterm birth. Use of the markers in concert improved the predictive ability. No individual serum biomarker of spontaneous preterm birth was useful when used alone; but when the woman was positive for any one of markers alkaline phosphatase, maternal serum α-fetoprotein, and granulocyte colony-stimulating factor, these three tests had a collective sensitivity of 81 percent and a specificity of 78 percent for prediction of spontaneous preterm birth at less than 32 weeks of gestation and 60 percent sensitivity and 73 percent specificity for prediction of spontaneous preterm birth at less than 35 weeks of gestation. Because this was a nested case-control study, the true-positive and negative predictive values are uncertain.
Despite the enhanced sensitivity of a multiple-marker approach, no prediction model to date provides adequate utility for justification of its routine clinical use, especially in the absence of an effective intervention for women with a positive screening test result. Development of an effective prediction model may permit the evaluation of targeted therapies, such as the provision of supplemental progesterone (described below). Interventions directed at women with a single marker, for example, a positive test for BV (Carey et al., 2000), fetal fibronectin (Andrews et al., 2003), or a short cervix (Rust et al., 2001; To et al., 2004), have been unsuccessful. Future directions for research in this area will involve the development and validation of multiple markers with diverse prospective cohorts. Research to develop novel markers for premature labor is crucial and may be facilitated by the use of high-throughput proteomic and metabolomic technologies and the use of more complex modeling techniques, such as those involving neural networks and artificial intelligence.
Finding 9-2: Current methods for the identification of women at risk for preterm birth by the use of demographic, behavioral, and biological risk factors have low sensitivities. Although the sensitivities increase as pathways and clinical syndromes are identified, the
efficacies of interventions decline as the parturitional process progresses.
PREVENTION STRATEGIES
The prevention of preterm birth has been attempted by the use of interventions aimed at each of the risk factors described in the previous chapters, largely without success (Table 9-5).
Most interventions are based on the traditional medical model of identifying and correcting each potential cause or risk factor for preterm birth, with the expectation that the rate of preterm births would decline in accordance with the contribution of that factor to the prematurity rate. Intervention trials have thus addressed the early identification of preterm labor through patient education, pharmacologic suppression of uterine contractions, antimicrobial therapy of vaginal microorganisms, the use of cerclage sutures to bolster the cervix, reduction of maternal stress, improved nutrition and improved access to prenatal care, and reduced physical activity. Some trials enrolled women with the risk factor in question without regard to obstetric history (e.g., antibiotics for women with a positive culture for a genital microorganism), whereas others were limited to women with a prior preterm delivery (e.g., the European cerclage trials or the recent progesterone supplementation studies [Da Fonseca et al., 2003; Meis et al., 2003]). Although successful elimination of single risk factors has been accomplished, for example, by antibiotic treatment of a targeted vaginal organism or suppression of contractions with tocolytic compounds (laborinhibiting agents), successful removal of a risk factor has not produced a decrease in preterm birth rates. In fact, the overall rate of preterm birth has continued to increase.
Future studies of the etiology and means of prevention of preterm birth should recognize the implications of these findings to develop a more sophisticated understanding of preterm birth as a syndrome in which multiple physiological pathways operate simultaneously to initiate preterm parturition. The common complex disorder model currently used in cardiovascular disease and neoplasia may be an appropriate replacement for the more unifactorial approach that has dominated the last two decades of research. The findings of studies of prevention strategies described below reinforce this recommendation.
Medical Interventions
Early Detection of Preterm Labor
Early diagnosis of preterm labor has been pursued with the expectation that the use of tocolytic drugs to stop labor would be more effective if they
TABLE 9-5 Summary of Studies of Medical Interventions to Prevent Preterm Birth
|
Risk Factor or Population Studied |
Interventions Tested in RCT |
Outcome |
Reference(s) |
|
Nutritional deficiencies |
Nutritional supplements Vitamins C and E |
No benefit, vitamin C-CPEP Trial, inadequate data |
Rumbold and Crowther, 2005 |
|
Prior preterm birth and bacterial vaginosis |
Antibiotics during pregnancy |
Mixed results |
McDonald et al., 1994; Carey et al., 2000; Hauth et al., 1995; Carey, 2000; Lamont et al., 2003; Guise et al., 2001; Okun et al., 2005 |
|
Prior preterm birth |
Cervical cerclage |
Mixed but mostly negative |
Berghella et al., 2005; see also Odibo et al., 2003; Harger, 2002; Owen et al., 2003; Bachmann et al., 2003; Belej-Rak et al., 2003; Drakeley et al., 2003 |
|
Positive risk score |
Education and self-detection of contractions |
No benefit |
Collaborative Group on Preterm Birth Prevention, 1993; Mueller-Heubach and Guzick, 1989 |
|
Prior preterm birth (singletons) |
Progesterone suppository and intramuscular 17α-hydroxyprogesterone caproate |
33 percent reduction in preterm birth rates |
Da Fonseca et al., 2003; Meis et al., 2003; see also metaanalyses by Dodd et al., 2005; Sanchez-Ramos et al., 1999 |
|
Prior preterm birth and increased contractions (singletons) |
Nurse contact and/or contraction monitor |
No benefit meta-analyses |
CHUMS, 1995; Dyson et al., 1998 |
|
Positive vaginal swab cultures for various organisms |
Antibiotics during pregnancy |
No benefit; mixed if also positive cultures VIP |
Brocklehurst et al., 2000; Gibbs et al., 1992; Carey and Klebanoff, 2003; Riggs and Klebanoff, 2004; Klebanoff et al., 2005 |
are given early, before significant cervical changes occur. The results of an initial experience that used a program of preterm labor risk assessment and education of at-risk women about preterm labor were favorable (Herron et al., 1982), but larger trials of similar interventions with diverse populations found no benefit (Collaborative Group on Preterm Birth Prevention, 1993; Mueller-Heubach and Guzick, 1989). This approach was expanded by using sensitive electronic monitoring of uterine contractions at home accom-
panied by daily nursing contact, but the intervention had no effect on eligibility for tocolysis, the rate of preterm birth, or neonatal outcomes in large randomized controlled trials conducted with women at risk (CHUMS, 1995a,b; Dyson et al., 1998; Hueston et al., 1995). The largest such trial (Dyson et al., 1998) enrolled 2,422 women with an increased risk of preterm birth, including 844 women with twins, in a three-armed trial in which the participants were assigned to receive (1) education plus weekly nursing contact, (2) daily nursing contact, or (3) daily nursing contact and daily electronic uterine contraction monitoring. The women in the last two groups were seen and treated more frequently, but the group assignment had no effect on the preterm birth rate or eligibility for tocolysis.
Antibiotics to Prevent Preterm Birth
The serendipitous observation (Elder et al., 1971) of a reduced frequency of preterm birth in women who received tetracycline as prophylaxis for urinary tract infection has been followed by a mixed literature describing the successes and failures of this intervention, as shown in Table 9-6.
TABLE 9-6 Randomized Trials of Antibiotics to Prevent Preterm Birth
|
Reference |
Entry Criteria |
Antibiotics |
Outcome |
|
Elder et al., 1971 |
Bacteriuria |
Oral tetracycline |
↓ LBW |
|
Romero et al., 1989 |
Bacteriuria |
Meta-analysis |
↓ LBW |
|
Smaill, 2001 |
Bacteriuria |
Meta-analysis |
↓ LBW |
|
Eschenbach et al., 1991 |
U. urealyticum infection |
Oral erythromycin |
No effect |
|
Klebanoff et al., 1995 |
Group B streptococcus infection |
Oral erythromycin |
No effect |
|
Hauth et al., 1995 |
Prior PTD or maternal weight <50 kg |
Oral metronidazole and erythromycin |
No effect if BV negative, ↓ PTD if BV positive |
|
Joesoef et al., 1995 |
BV |
Vaginal clindamycin |
No effect |
|
McDonald et al., 1997 |
BV |
Oral metronidazole |
None if no Hx PTD, benefit if Hx PTD |
|
Gichangi et al., 1997 |
Poor obstetric Hxa |
Cefetamet-pivoxil |
↓ LBW |
Metronidazole and erythromycin treatment (Hauth et al., 1995) and metronidazole treatment (McDonald et al., 1997) were reported to reduce the risk of recurrent preterm delivery in women with BV who also had had a prior preterm birth, but metronidazole treatment had no effect on the rate of preterm birth in a placebo-controlled trial with 1,900 women with asymptomatic BV (Carey et al., 2000). Analysis by obstetric history of preterm birth, race-ethnicity, gestational age at the initiation of treatment, eradication of BV, and prepregnancy weight in that study did not reveal any subgroup in which treatment improved the perinatal outcome. Trials of clindamycin administered orally (n = 485) (Ugwumadu et al., 2003) or vaginally (n= 409) (Lamont et al., 2003) to women with BV reported reductions in the rates of preterm birth, especially if treatment was administered early in pregnancy, but two other studies of vaginal clindamycin found no benefit. One found no difference in preterm birth rates, despite the successful elimination of BV in treated women (n = 601) (Joesoef et al., 1995), and the other found an increased rate of preterm birth before 34 weeks of gestation in women who were fully compliant with clindamycin treatment compared with the rate in the placebo group (9 versus 1.4 percent) (Vermeulen and Bruinse, 1999).
A review of seven randomized clinical trials of screening and antibiotic treatment of BV in pregnancy to reduce preterm birth found no benefit in low-risk women or in women with an unspecified “increased risk” of preterm birth (Guise et al., 2001; Okun et al., 2005). The most recent American College of Obstetricians and Gynecologists (ACOG) Practice Bulletin (ACOG, 2001) specifically noted “There are no current data to support the use of … BV screening as a strategy to identify or prevent preterm birth.” McDonald and colleagues (2005) concluded in a recent Cochrane Review, “Antibiotic treatment can eradicate bacterial vaginosis in pregnancy … [but there is] little evidence that screening and treating all pregnant women with asymptomatic bacterial vaginosis will prevent preterm birth and its consequences. For women with a previous preterm birth, there is some suggestion that treatment of bacterial vaginosis may reduce the risk of preterm prelabour rupture of membranes and low birthweight.” The failure of antibiotics to reduce the rates of preterm birth, despite successful eradication of the genital tract organisms linked to preterm birth, is an urgent research issue that will require sophisticated studies of the host response to infection and inflammation and environmental influences on infection and inflammation.
The disappointing results of studies of the use of antibiotic treatment to reduce the risk of preterm birth have prompted investigation of the preconceptional use of antibiotics for women with a history of preterm birth, under the theory that relatively benign microorganisms colonizing the up-
per genital tract might produce intrauterine inflammation after conception (Andrews and Goldenberg, 2003). In a study of women with a prior preterm birth who were treated with metronidazole and azithromycin or placebo at 3-month intervals between pregnancies, Andrews et al. (in press) found no reduction in the rates of preterm birth in those who received antibiotic treatment. Of concern, that report included data that suggested that antibiotic use might actually increase the likelihood of preterm birth, a finding similar to the NICHD Network trial of metronidazole treatment for women infected with Trichomonas vaginalis (Klebanoff et al., 2001). Although the data from these two studies are preliminary, they argue against the clinical use of antibiotics solely to prevent preterm birth until future research explains these findings. Therefore, investigation of strategies that can be used to prevent infection-related preterm birth is justified and, indeed, urgent.
Although genital tract colonization and infection are frequent in women who deliver preterm, most women with BV do not deliver preterm, and most preterm births are not accompanied by evidence of infection. Thus, studies of the use of antibiotics in women with infection or prior preterm birth, or both, are likely to include many women for whom antibiotics have no potential benefit (Romero et al., 2003). Future research should therefore emphasize the identification of the particular subset of women with BV for whom antimicrobial or anti-inflammatory therapies might prove beneficial. The pathways by which genital tract infection is related to early delivery merits renewed research efforts so that more sophisticated interventions might be developed.
Infections outside the genital tract are also related to preterm birth, most commonly to urinary tract and intra-abdominal infections, for example, pyelonephritis and appendicitis (Romero et al., 1989). The presumed mechanism is inflammation of the nearby reproductive organs; but infections at remote sites, especially if the infection is chronic, have also been associated with an increased risk of spontaneous preterm birth. The recent literature provides information that links maternal periodontal disease to preterm birth (Goepfert et al., 2004; Jeffcoat et al., 2001a,b; Offenbacher et al., 2001) and to “late miscarriage” (loss of a pregnancy at between 12 and 24 weeks of gestation) and stillbirth (Moore et al., 2004). This association remains after confounding covariables are controlled for and suggests that the effect may be mediated by the systemic induction of cytokines in response to chronic inflammation (Boggess et al., 2005b).
Interestingly, periodontitis is characterized by an altered host flora and is thus similar to BV. A study of periodontal screening and treatment in pregnant women to reduce the rate of preterm birth (Jeffcoat et al., 2003) enrolled 366 women who were randomized at 21 to 25 weeks of gestation to one of three treatment groups: routine dental care plus placebo medica-
tion, scaling and root planing (intensive physical treatment of periodontal plaque) plus metronidazole (250 milligrams [mg] three times a day for 1 week), or scaling and root planing plus placebo medication. The rates of preterm birth (before 35 weeks of gestation) in the three groups were 4.9, 3.3, and 0.8 percent, respectively. Although good dental care is important for all pregnant women, there is insufficient evidence to conclude that dental care will reduce the occurrence of preterm birth (Khader and Ta’ani, 2005). Periodontal disease and other causes of systemic inflammation and their relationship to preterm birth are thus promising areas of research that merit funding for interdisciplinary investigations.
Other Prophylactic Medications
Tocolytic Prophylaxis
Studies of the use of tocolytic agents as prophylaxis for preterm birth have shown no evident benefit (Berkman et al., 2003; King et al., 1988; Sanchez-Ramos et al., 1999). Evidence that the parturitional process begins well in advance of coordinated uterine activity (Challis et al., 2000) may explain the inability of contraction suppression to prevent preterm birth in randomized trials.
Progesterone
Investigations summarized and reanalyzed by Keirse (1990) suggested that supplemental administration of progesterone might reduce the rate of preterm birth in women at increased risk. Two randomized placebo-controlled trials whose findings were published in 2003 found that progesterone, administered as either weekly intramuscular injections of 250 mg of 17α-hydroxprogesterone caproate (Meis et al., 2003) or daily progesterone vaginal suppositories (Da Fonseca et al., 2003), reduced the rate of recurrent preterm delivery by about a third. When these data were combined with data from earlier trials of supplemental progesterone in meta-analyses (Dodd et al., 2005; Sanchez-Ramos et al., 2005), the risk of recurrent preterm birth was reduced by 40 to 55 percent (in the study of Dodd et al. [2005] the RR was 0.58 and the 95 percent CI was 0.48 to 0.70; in the study of Sanchez-Ramos et al. [2005] the RR was 0.45 and the 95 percent CI was 0.25 to 0.80). Unlike strategies targeted at a specific risk factor such as infection, supplemental progesterone treatment was effective at reducing the rates of preterm birth in women chosen only because of a prior preterm birth. This suggests three possibilities: (1) that progesterone is effective in inhibiting a pathway shared by diverse causes of preterm birth, (2) that progesterone has diverse effects that act on several different pathways, or
(3) that progesterone is very effective against one highly prevalent pathway or cause.
Although progesterone supplementation is promising, several questions about its use remain incompletely answered:
-
How does progesterone work? The original rationale for progester-one prophylaxis was that it is a uterine relaxant, but some studies (Elovitz and Mrinalini, 2005; Kelly, 1994; Ragusa et al., 2004; Szekeres-Bartho, 2002) suggest it may act through an effect on the inflammatory response. The optimal dose, interval, and duration of treatment have also not been determined. Pharmacokinetic, pharmacodynamic, and pharmacogenetic studies of progesterone are urgently needed.
-
Is supplemental progesterone safe? There is little evidence from studies with humans that progesterone presents a teratogenic risk (Meis, 2005), but theoretical concern remains that it may blunt a fetal signal for labor generated by an in utero risk.
-
Who should receive supplemental progesterone? Data showing that progesterone provides a benefit are available only for women with a prior preterm birth at between 18 and 36 weeks of gestation. There is evidence that progesterone offers the greatest benefit for women with a prior preterm birth before 34 weeks of gestation (Spong et al., 2005).
Petrini et al. (2005) projected that use of 17P in women with a prior pretem birth would have a small but significant effect on the rate of preterm birth in the US (12.1% to 11.8% [p < .001]).
No studies of 17α-hydroxyprogesterone have been conducted with women with other risk factors, such as a multiple gestation, short cervix, positive fibronectin, a history of cervical insufficiency or cerclage, or preterm labor in the current pregnancy.
Surgical Interventions
Prophylactic Cerclage for Women with a Risk of Preterm Birth
Recognition that some early preterm births may be due to variant clinical presentations of cervical insufficiency led to consideration of cervical cerclage treatment for women with such a history. A randomized trial of cerclage for women with a prior preterm birth (MacNaughton et al., 1993) found that cerclage resulted in fewer preterm births before 33 weeks of gestation in women with multiple prior early births but that it had no effect on the overall rate of preterm birth in women treated with cerclage.
The introduction of cervical sonography in the early 1990s produced strong evidence that a short cervix in midpregnancy is associated with an
increased risk of early delivery (see above), but the basis for this association remains inadequately understood. There is evidence that a cervical length below the 10th percentile in the second trimester may represent at the short end of a biological continuum of inherent cervical function (Goldenberg et al., 1998; Iams et al., 1995) or result as well from biochemical (inflammatory) or biophysical (stretch or contraction) processes. It is likely that all of these factors are operative to various degrees in an individual, but to date there is no satisfactory method to determine the contributions of physical and biochemical influences on the cervix and, thus, no way to select an appropriate therapy.
The literature on the use of cerclage includes the findings of trials with women with a prior preterm birth and current ultrasound evidence of cervical effacement (Althuisius et al., 2001; Berghella et al., 2004) and of trials with women with ultrasound findings alone (To et al., 2004; Rust et al., 2001). The evidence of a benefit of cerclage is the strongest from studies of women who have a history of preterm birth and who have a short cervix in the current pregnancy. Data from these four trials were reanalyzed by the original authors (Berghella et al., 2005). When data for women with singleton pregnancies enrolled in four trials were combined, the risk of birth before 35 weeks of gestation was significantly reduced with cerclage treatment for women with a prior preterm birth and a short cervix (defined as <2.0 centimeters [cm]) in the current pregnancy (RR 0.63; 95% CI 0.48– 0.85), but there was no advantage of cerclage for women with a short cervix who did not have a prior preterm birth (RR 0.84; 95% CI 0.60–1.17).
Evidence indicates that the efficacy of cerclage may vary according to the cause of the short cervix. In the meta-analysis by Berghella and colleagues (2005), cerclage was not effective at reducing the rates of preterm birth in women with twin gestations, in which uterine stretch is an important factor. In this group, cerclage for a short cervix was associated with increased rates of preterm birth (RR 2.15; 95% CI 1.15–4.01). A recent study found evidence that intracervical inflammation was related to the success or failure of cerclage in women with a short cervix. Sakai et al. (2006) studied women treated with cerclage for a short cervix and found reduced rates of preterm birth in women with low levels of the inflammation-related marker interleukin-8 in their cervical fluid and increased rates of preterm birth when the level of interleukin-8 was high. Further research to identify appropriate candidates for cerclage is thus needed.
Nonmedical Interventions
Nonmedical interventions, such as social support, reduction of stress, improved access to prenatal care, and reduced physical activity, can be used to reduce the rates of preterm birth and were reviewed in Chapter 3. A
recent study examined the rates of low birth weight among participants in a Medicaid-funded prenatal program for high-risk women (Ricketts et al., 2005). The results indicated that the infants of women who stopped smoking had a rate of low birth weight of 8.5 percent, whereas the rate was 13.7 percent among the infants of women in the program who did not stop smoking. The infants of women with adequate weight gain had a rate of low birth weight rate of 6.7 percent, whereas the rate was 17.2 percent among the infants of women with inadequate weight gain. Finally, the infants of women who eliminated all risks had a low birth weight rate of 7.0 percent, whereas the rate was 13.2 percent among the infants of women who eliminated none of their risks. Those who attended at least 10 program visits were more likely to eliminate their risks than women who attended fewer visits.
Although many nonmedical efforts have had limited success to date, considerable opportunity for further research on nonmedical efforts at reducing the rates of preterm birth exists. Activity modification is widely practiced, but the evidence of a benefit does not exist. Most studies of nonmedical interventions have been conducted with women identified as being at risk, as defined by their ethnicity, socioeconomic condition, or medical and obstetric history (e.g., prior preterm birth and multiple gestations). Future studies of nonmedical interventions to reduce the rates of preterm birth with women who are defined by specific criteria for risk are needed. These could include, for example, studies of social interventions in women with measurable evidence of stress and studies of activity restriction in women with short cervical lengths.
Finding 9-3: Studies of intervention strategies for the prevention of preterm birth have had preterm birth as their only outcome variable. The study samples have not been large enough for sufficient investigations of morbidity, mortality, and neurological morbidity.
DIAGNOSIS AND TREATMENT OF PRETERM LABOR
The methods for the diagnosis and treatment of preterm labor are based on an inadequate literature that is compromised not only by the oft-cited paucity of well-designed and adequately powered clinical trials but also, even more, by an incomplete understanding of the sequence and timing of events that precede clinical evidence of preterm labor, such as progressive cervical dilatation and ruptured membranes. Because the progression from subclinical preterm parturition to overt preterm labor is often gradual, standard criteria for the diagnosis of preterm labor (uterine contractions accompanied by cervical change) lack precision. Consequently, preterm labor is often overdiagnosed so that women with frequent contractions who are
not in labor are enrolled in studies of tocolytic drugs (King et al., 1988). Women treated to prevent or arrest preterm labor may therefore have been treated successfully or may not have required treatment at all. The true result of treatment is known with confidence only for those whose treatment was unsuccessful.
Useful studies of methods for the prevention or arrest of preterm labor therefore depend on the development of more accurate methods for the diagnosis of preterm labor. The current uncertainty is reflected by the division of clinicians into two camps: those who believe that nothing works and others who claim great success with various interventions. The truth likely falls somewhere in between but will emerge only if additional resources are devoted to improving the means of diagnosis of preterm labor.
Diagnosis of Preterm Labor
Preterm labor must be considered whenever abdominal or pelvic symptoms occur after 18 to 20 weeks of gestation. Symptoms like pelvic pressure, increased vaginal discharge, backache, and menstrual-like cramps are common with advancing pregnancy and suggest preterm labor more by their persistence than by their severity. Contractions may be painful or painless, depending on the resistance offered by the cervix. Contractions against a closed, uneffaced cervix are likely to be painful, but recurrent pressure or tightening may be the only symptoms, as often occurs when cervical effacement precedes the onset of contractions (Olah and Gee, 1992). The traditional criteria for labor, persistent uterine contractions accompanied by dilatation or effacement of the cervix, or both, are reasonably accurate when the frequency is six or more contractions per hour, cervical dilatation is 3 cm or more, effacement is 80 percent or greater, and membranes rupture or bleeding occurs (Hueston, 1998; Macones et al., 1999a). When lower thresholds for contraction frequency and cervical change are used, a false-positive diagnosis of labor is common (in up to 40 percent of cases) (King et al., 1988) but the sensitivity of the diagnosis does not necessarily increase (Peaceman et al., 1997).
The accurate diagnosis of early preterm labor is difficult because the symptoms (Iams et al., 1994) and signs (Moore et al., 1994) of preterm labor commonly occur in healthy women who do not deliver preterm and because digital examination of the cervix in early labor (less than 3 cm of dilatation and less than 80 percent effacement) is not highly reproducible (Berghella et al., 1997; Jackson et al., 1992). Women whose symptoms are cervical dilatation of less than 2 cm or effacement of less than 80 percent, or both, present a diagnostic challenge. In a clinical trial to identify women with true preterm labor, Guinn et al. (1997) randomly assigned 179 women with preterm contractions and minimal cervical dilatation to receive intra-
venous hydration, observation without intervention, or a single dose of 0.25 mg of subcutaneous terbutaline (a tocolytic agent). Intravenous hydration did not decrease preterm contractions. Women whose contractions recurred despite transient cessation after terbutaline treatment were more often found to be in preterm labor; those whose contractions stopped and did not recur were sent home. The authors concluded that a single dose of subcutaneous terbutaline was an efficient method of identifying those with actual preterm labor.
Other means of enhancing diagnostic accuracy in preterm labor include transvaginal sonographic measurement of cervical length and testing for fetal fibronectin in cervicovaginal fluid (ACOG, 2003; Leitich et al., 1999a,b). Both of these tests improve the diagnostic accuracy by reducing the possibility of a false-positive diagnosis of labor. Transabdominal sonography, however, has a poor reproducibility for cervical length measurement (Mason and Maresh, 1990) and the findings should not be used clinically without confirmation of the findings by transvaginal ultrasound. A cervical length of 30 mm or more by endovaginal sonography, however, suggests that preterm labor is unlikely in symptomatic women if the examination is properly performed (Iams, 2003). Similarly, a negative fibronectin test in women with symptoms before 34 weeks of gestation with cervical dilatation of less than 3 cm can also reduce the rate of a false-positive diagnosis of labor if the result is returned promptly and the clinician is willing to act on a negative test result by not initiating treatment (Chien et al., 1997; Leitich et al., 1999b). The combined use of tests for cervical length and fibronectin identifies a group of patients with a very high risk of preterm birth when the fibronectin test is positive and the sonographic cervical length is less than 30 mm (Table 9-7).
Despite evidence that the overdiagnosis of preterm labor in women with frequent contractions is common and results in unnecessary treatment, the clinical use of the fibronectin test and cervical sonography is not widespread.
Barriers to improved accurate diagnosis before treatment is initiated include a lack of professional and public education about the parturitional process and the risks of preterm birth for the infant (Massett et al., 2003), inadequate training of medical professionals other than physicians to perform the appropriate examinations (speculum examination of the cervix, endovaginal cervical sonography), and medicolegal fears that failure to treat a pregnant woman who may be in labor may invite lawsuits. Research and educational programs should aim to address these problems and to identify the most appropriate point(s) at which parturition should be arrested once it has begun.
TABLE 9-7 Frequency of Spontaneous Preterm Delivery According to Cervical Length (cutoff 30 mm) and Vaginal Fibronectin Results
|
Cervical Length <30 mm |
Fetal Fibronectin + |
Delivery Within 48 Hours |
Delivery Within 7 Days |
Delivery Within 14 Days |
Delivery ≤32 Weeks |
Delivery ≤35 Weeks |
|
No |
No |
2.2% |
2.2% |
3.2% |
0% |
1.1% |
|
|
|
(2/93) |
(2/93) |
(3/93) |
(0/47) |
(1.93) |
|
No |
Yes |
0% |
7.1% |
14.3% |
0% |
21.4% |
|
|
|
(0/14) |
(1/14) |
(2/14) |
(0/5) |
(3/14) |
|
Yes |
No |
7.1% |
11.4% |
12.9% |
6.5% |
17.1% |
|
|
|
(5/70) |
(8/70) |
(9/70) |
(2/31) |
(12/70) |
|
Yes |
Yes |
26.3% |
44.7% |
52.6% |
38.9% |
47.4% |
|
|
|
(10/38) |
(17/38) |
(20/38) |
(7/18) |
(18/38) |
|
Prevalence of the outcome |
7.9% |
13.0% |
15.8% |
8.9% |
15.8% |
|
|
|
|
(17/215) |
(28/215) |
(34/215) |
(9/101) |
(34/215) |
|
SOURCE: Gomez et al. (2005). Reprinted from American Journal of Obstetrics and Gynecology, Vol. 192, Pg. 354, © 2005, with permission from Elsevier. |
||||||
Finding 9-4: Current methods for the diagnosis and treatment of women at risk of an imminent preterm birth are not sufficiently evidence based.
Information Informing Decisions Surrounding Perinatal Interventions
Obstetricians are taught that their first obligation and priority is the mother’s health but that women and families are willing to accept some degree of increased risk to the mother if it will benefit her fetus (see Appendix C for a discussion of ethical issues). A decision to arrest preterm labor may increase the risk to both the mother and the fetus if the pregnancy is complicated by bleeding, hypertension, or infection. A lesser risk usually attends uncomplicated preterm labor; but intrauterine fetal stress or compromise may contribute to the onset of preterm labor, and tests of fetal well-being are imperfect. Tocolytic drugs, which are used to arrest labor, can have serious maternal and fetal side effects, especially if they are used in increasing doses, for prolonged periods, or in combination with one another. The decision about whether to arrest preterm labor, to transfer the mother and the fetus in utero to another hospital, or to administer antenatal glucocorticoids is made against this background in an environment of spoken and unspoken assumptions about their wisdom, according to current information and beliefs. The quality of this information necessarily varies with the dissemination and local application of advancements in perinatal and neonatal care. Beliefs about the anticipated rates of morbidity and mortality for preterm infants according to gestational age are the foundation for decisions regarding obstetric and perinatal care.
Reports of improved perinatal outcomes for preterm infants could be expected to and do apparently result in an increased willingness to choose delivery and neonatal care over the uncertainties of continuing the pregnancy. The mortality and morbidity of prematurely born infants are discussed in Chapter 10. Recent data from one center are shown in Figure 9-3 to illustrate how improved outcomes for infants born after 32 weeks of gestation might lead to a decision to allow preterm delivery rather than initiate treatment with drugs that may prolong the pregnancy for only a few days (Mercer, 2003).
Finding 9-5: The goal of prevention of preterm birth is subordinate to the goal of improved perinatal morbidity and mortality outcomes. This goal is important, because the continuation of pregnancy in women with preterm parturition in some instances may increase the health risk for the mother or the fetus, or both.
FIGURE 9-3 Perinatal mortality and gestational age.
SOURCE: Mercer (2003). Reprinted with permission from Obstetrics & Gynecology, Vol. 101, Pg. 180, © 2003 by the American College of Obstetricians and Gynecologists.
Although the expectations of obstetric and neonatal doctors and nurses about neonatal and infant outcomes are known to influence decision making in perinatal care (Bottoms et al., 1997), these same practitioners’ assessments are not necessarily accurate. Morse et al. (2000) found that both obstetric and neonatal care providers’ predictions of neonatal survival and survival without handicap were substantially below the actual rates, indicating a need for improved information before and after delivery (Figures 9-4 and 9-5). Finally, the medical-legal environment may also be a consideration; however, the extent of its influence on this decision-making process is unknown.
Finding 9-6: The knowledge and beliefs of health care providers influence their attitudes toward and their management of mothers with threatened preterm delivery and their infants.
Treatment Strategies and Effectiveness
The prevention of preterm birth has primarily been focused on the treatment of the woman with symptomatic preterm labor. This strategy is based
FIGURE 9-4 Estimated versus actual survival rates.
SOURCE: Morse et al. (2000). Reproduced with permission from Pediatrics, Vol. 105, Pg. 1047, © 2000 by the American Academy of Pediatrics.
on the assumption that clinically apparent labor is commensurate with the initiation of the parturitional process and that successful inhibition of labor should prevent delivery. Thus, treatment has been directed toward the inhibition of myometrial contractions. This approach has not decreased the incidence of preterm birth but can delay delivery long enough to allow administration of antenatal steroids and to transfer the mother and fetus to an appropriate hospital, two interventions that have consistently been shown to reduce the rates of perinatal mortality and morbidity.
Labor inhibition has not prevented preterm birth because arresting myometrial contractions does not address the specific initiators of preterm labor. In addition, few medications can inhibit uterine contractions safely and effectively for more than a few days. Research to find tocolytic drugs is hampered by the inaccurate diagnosis of preterm labor, such that many women with preterm labor are not detected early enough to expect success, whereas others are treated for preterm contractions that do not result in
FIGURE 9-5 Estimated versus rates of freedom from handicap.
SOURCE: Morse et al. (2000). Reproduced with permission from Pediatrics, Vol. 105, Pg. 1047, © 2000 by the American Academy of Pediatrics.
labor. The treatment strategies used to treat women diagnosed with preterm labor are reviewed below.
Tocolytics
Labor-inhibiting agents are commonly referred to as tocolytic drugs, after the Greek tokos, meaning childbirth, and lysis, meaning to release. The purpose of tocolytic agents is to inhibit myometrial contractions. The labor-inhibiting agents used today abrogate myometrial contractility by one of two major pathways. These drugs affect either the contractile proteins (usually the phosphorylation of myosin) by generation or alteration of an intracellular messenger or inhibit the synthesis or block the action of a known myometrial stimulant. The first group includes the β-adrenergic re-
ceptor agonists, nitric oxide donors, and magnesium sulfate and the calcium channel blockers. The second group includes prostaglandin synthesis inhibitors and oxytocin antagonists.
Randomized, controlled trials of tocolytics have shown that they successfully inhibit contractions for 2 to 7 days. They have not been useful for long-term maintenance of contraction inhibition and in most studies have not improved perinatal outcomes, although their use does allow time for the administration of corticosteroids and maternal transfer to an appropriate hospital.
Magnesium sulfate The precise mechanism by which magnesium affects uterine contractions has not been completely elucidated. Magnesium likely competes with calcium at the level of plasma membrane voltage-gated channels. It hyperpolarizes the plasma membrane and inhibits myosin light-chain kinase activity by competing with intracellular calcium at this site. Interference with the activity of myosin light-chain kinase reduces myometrial contractility (Cunze et al., 1995; Lemancewicz et al., 2000; Mizuki et al., 1993). In two randomized, placebo-controlled trials of magnesium sulfate, magnesium sulfate did not lead to improved birth outcomes, although the cessation of contractions for a short interval was demonstrated (Cox et al., 1990; Fox et al., 1993). Three of four randomized clinical trials that compared magnesium sulfate with terbutaline found no difference in perinatal outcomes (Berkman et al., 2003). Meta-analysis also indicates that magnesium sulfate is ineffective for the treatment of preterm labor (Crowther et al., 2002). Potential adverse effects of magnesium sulfate include respiratory depression, flushing, nausea, and pulmonary edema.
Beta-mimetic drugs The β-adrenergic receptor agonists cause myometrial relaxation by binding with β2-adrenergic receptors and increasing intracellular adenyl cyclase. An increase in intracellular cyclic adenosine monophosphate levels activates protein kinase, which results in the phosphorylation of intracellular proteins. The resultant drop in intracellular free calcium levels interferes with the activity of myosin light-chain kinase, which inhibits the interaction between actin and myosin, and thus, myometrial contractility is diminished (Caritis et al., 1979, 1987, 1991).
Beta-sympathomimetic drugs, including terbutaline and ritodrine, have been widely used as tocolytics for many years. The most commonly used beta-mimetic in the United States is terbutaline (marketed in the United States as a drug for the treatment of asthma); but others, including albuterol, fenoterol, hexoprenaline, metaproterenol, nylidrin, orciprenaline, and salbutamol, are used in other countries. Ritodrine hydrochloride, the only drug ever approved for use as a parenteral tocolytic by the Food and Drug Administration (FDA), never achieved widespread use because of frequent
maternal side effects. It is no longer marketed in the United States. Terbutaline is more commonly used because clinicians are familiar with it and it has a rapid onset of action (3 to 5 minutes) when it is given subcutaneously. Published protocols often use subcutaneous administration, with a usual dose of 0.25 mg (250 micrograms) every 3 to 6 hours.
Once frequently prescribed for acute and maintenance therapy of women with suspected preterm labor, beta-mimetic drugs are less commonly used because of reports of their limited efficacy for this syndrome and because of concern about their cardiovascular and metabolic side effects. The Cochrane database includes data for 1,332 women enrolled in 11 randomized, placebo-controlled trials of beta-mimetic drugs. Those data indicate that treated subjects were less likely to deliver within 48 hours (RR 0.63; 95% CI 0.53–0.75) but not within 7 days (Anotayanonth et al., 2004). Although a 48-hour delay in delivery allows sufficient time for in utero transfer to an appropriate hospital and treatment with steroids, the rates of perinatal and neonatal death and perinatal morbidity were not reduced in that analysis. Side effects requiring a change or a cessation of treatment were frequent. Previous reviews have found similar results (Berkman et al., 2003, Gyetvai et al., 1999).
Long-term or maintenance use of beta-mimetic drugs has been advocated to suppress contractions to prevent preterm labor, but tachyphylaxis or desensitization of the adrenergic receptor occurs after prolonged exposure to beta-agonists, so that increasing dosages are required to sustain a response. After animal studies suggested that the myometrium remains quiescent longer with pulsatile administration of lower doses of beta-mimetics (Casper and Lye, 1986), a protocol that used a continuous subcutaneous infusion of terbutaline at lower doses was reported to result in fewer side effects than the numbers of side effects encountered with oral administration (Lam et al., 2001; Perry et al., 1995). Although these protocols suppress contractions, they had no effect on the rates of preterm birth or perinatal morbidity in randomized, placebo-controlled trials (Guinn et al., 1998; Wenstrom et al., 1997), and the use of beta-mimetic compounds is not recommended by ACOG (ACOG, 2001). A 2002 Cochrane Review also concluded that current evidence does not support terbutaline infusion to prolong pregnancy (Nanda et al., 2002).
Calcium channel blockers Calcium channel blockers directly block the influx of calcium ions through the cell membrane. They also inhibit the release of intracellular calcium from the sarcoplasmic reticulum and increase the level of calcium efflux from the cell. The ensuing decrease in intracellular free calcium levels leads to inhibition of calcium-dependent myosin light-chain kinase phosphorylation and results in myometrial relaxation. One study compared nifedipine, the most commonly studied calcium channel
blocker, with magnesium but showed no difference between nifedipine and magnesium in prolonging pregnancy or improving the perinatal outcome (Floyd et al., 1995). Use of the combination of magnesium and calcium channel blockers could, in theory, cause respiratory depression and extreme hypotension; so use of this combination is best avoided.
Eight randomized clinical trials and one nonrandomized trial have compared calcium channel blockers with beta-mimetics. In two trials, women treated with nifedipine had a longer interval between treatment and delivery and their infants had a greater mean estimated gestational age at delivery (Jannet et al., 1997; Papatsonis et al., 1997), but five other trials showed no significant differences in perinatal outcomes (Berkman et al., 2003). Side effects of nifedipine include dizziness, headache, flushing, and edema.
Cyclooxygenase inhibitors Cyclooxygenase (COX; prostaglandin synthase) is the enzyme responsible for the conversion of arachidonic acid to prostaglandins, which are critical in parturition. Prostaglandins enhance the formation of myometrial gap junctions and increase the amount of intracellular calcium available by raising transmembrane influx and the sarcolemmal release of calcium (Challis et al., 2002). COX exists in two isoforms, COX-1 and COX-2. COX-1 is constitutively expressed in gestational tissues, whereas COX-2 is the inducible form. COX-2 is the isoform whose levels dramatically increase in the decidua and the myometrium during term and preterm labor. COX inhibitors decrease prostaglandin production by either general inhibition of COX or specific inhibition of COX-2, depending on the agent. These inhibitors include indomethacin, sulindac, and ibuprofen.
The first randomized placebo control trial of indomethacin involved 30 patients with preterm labor. One of 15 patients who received indomethacin but 9 of 15 patients in the placebo group began labor after 24 hours (Niebyl et al., 1980). Although the maternal adverse effects of COX inhibitors are largely limited to mild gastrointestinal upset, fetal effects of concern include oligohydramnios and premature closure of the ductus arteriosus. Limiting indomethacin therapy to 24 to 48 hours of treatment before 32 weeks of gestation avoids these concerns (Moise et al., 1988).
Oxytocin receptor antagonists In normal parturition, oxytocin stimulates contractions by inducing the conversion of phosphatidylinositol to inositol triphosphate, which binds to a protein in the sarcoplasmic reticulum that causes the release of calcium into the cytoplasm. Oxytocin receptor antagonists compete with oxytocin for binding to receptors in the myometrium and decidua, thus preventing the increase in intracellular free calcium levels that occurs with receptor binding (Goodwin et al., 1996; Phaneuf et al., 1994). Atosiban is a selective oxytocin-vasopressin receptor antagonist that inhibits spontaneous and oxytocin-induced contractions
but not prostaglandin-induced contractions. Because oxytocin receptors are mostly confined to the uterus and myoepithelial cells of the breast, maternal side effects are minimal (Romero et al., 2000). Oxytocin antagonists cross the placenta, but fetal cardiovascular status and acid-base status are not affected.
In a placebo-controlled trial, the duration of pregnancy after the initiation of therapy with atosiban was not different (26 days for treated women and 21 days for women in the placebo group; p = 0.6) when the entire group of women was evaluated (gestational age, 20 to 33 weeks 6 days; n = 531), but atosiban treatment prolonged pregnancy significantly more often than placebo for up to 48 hours and for up to 7 days in women treated at 28 weeks of gestation or later (n = 424) (Romero et al., 2000). In a randomized trial (n = 733) in which atosiban was compared with intravenous betamimetic drug (Moutquin et al., 2001), the rates of delivery within 48 hours and 7 days after the initiation of therapy were not different, but women treated with atosiban had fewer and less severe side effects.
Despite these results, FDA did not approve atosiban for use because adverse outcomes were noted in fetuses of less than 28 weeks of gestation. It is not clear whether these outcomes were related to the drug or to greater numbers of pregnancies treated before 28 weeks of gestation in the atosiban arm. Atosiban is available for clinical use in Europe, where it is the most commonly used tocolytic drug in many countries (personal communication, H.P. van Geijn and D. Papatsonis, Free University Hospital, Amsterdam, the Netherlands, December 16, 2005).
Nitric oxide donors Nitric oxide (NO) is produced in a variety of cells and is essential for maintenance of normal smooth muscle tone. NO is synthesized during the oxidation of L-arginine (an essential amino acid) to L-citrulline, which then diffuses from the source cell. This reaction is catalyzed by the enzyme nitric oxide synthase. The interaction between NO and soluble guanylyl cyclase, which is present in nearby effector cells, represents a widespread signal transduction mechanism that couples the diverse extracellular stimuli of NO formation to the synthesis of cyclic guanosine 3′,5′-mono-phosphate (cGMP) in target cells. The increase in cGMP content in smooth muscle cells activates myosin light-chain kinases, leading to smooth muscle relaxation (Yallampalli et al., 1998). NO donors such as nitroglycerin inhibit spontaneous and oxytocin- and prostaglandin-induced activity in vitro and effectively inhibit postsurgical uterine contractility in pregnant monkeys and humans. A randomized study comparing intravenous nitroglycerin and magnesium sulfate found that magnesium therapy was more likely to successfully delay delivery for at least 12 hours (El-Sayed et al., 1999). Two other randomized trials comparing transdermal nitroglycerin with placebo or ritodrine found no difference in their abilities to prolong pregnancy
for 48 hours (Lees et al., 1999; Smith et al., 1999). There is thus insufficient evidence at this time to recommend the use of NO donors for the inhibition of preterm labor.
Summary of tocolytic drug treatment The ultimate goal of treatment for preterm labor is to eliminate or reduce perinatal morbidity and mortality. No trials of the efficacies of tocolytics of sufficient sample size are available to assess these outcomes. The surrogate or secondary outcomes used instead of neonatal morbidity are pregnancy prolongation, frequency of preterm birth, and gestational age at birth. Few placebo-controlled trials of tocolytic drugs have been conducted. β-Adrenergic receptor agonists, indomethacin, and atosiban have demonstrated superiority over placebo in achieving limited pregnancy prolongation. The findings of other of the efficacies of tocolytics have been less persuasive and have included those that have compared two active agents, that enroll women at a very low risk of preterm delivery, and that have had an inadequate power to demonstrate any statistically significant difference between agents. Meta-analyses address the issue of sample size but do not overcome problems with poor study design, selection criteria, and the use of intermediate outcomes. Delaying the time to delivery to allow maternal transfer to the most appropriate hospital and the administration of corticosteroids antenatally is clearly supported by the available evidence and is the strongest argument for the short-term use of tocolytic drugs.
Antibiotics and Preterm Labor
Abundant evidence supports an association between subclinical infection and preterm labor. The mechanism of this association has not been elucidated. Among 14 randomized controlled trials performed between 1986 and 2001 to evaluate the benefit of antibiotic treatment of women with preterm labor and intact membranes, only 2 showed a prolongation of pregnancy and a decreased rate of preterm delivery by the use of antibiotic therapy. In a meta-analysis of seven trials that enrolled 795 patients treated with broad-spectrum antibiotics or placebo, the length of pregnancy was unchanged by antibiotic administration (Egarter et al., 1996). Although the rates of occurrence of some neonatal outcomes such as pneumonia and necrotizing enterocolitis were reduced, the risk of neonatal mortality was increased (odds ratio = 3.25; 95% CI 0.93–1.38). Antibiotic administration had no effect on neonatal sepsis or intraventricular hemorrhage.
The largest study to date randomized 6,295 women in spontaneous preterm labor to receive (1) erythromycin, (2) co-amoxicillin–clavulanic acid (co-amoxiclav), (3) erythromycin and co-amoxiclav, or (4) placebo (Kenyon et al., 2001a). None of the antibiotic treatments was associated with a pro-
longation of pregnancy or improvements in perinatal outcomes. Maternal infections were reduced in women exposed to antibiotics.
Despite the association of various infections with preterm labor, the use of broad-spectrum antibiotics for women in preterm labor has not improved any outcome. Most authors have explained this by noting that the timing of antibiotic treatment after preterm labor is clinically manifest is too late to influence any outcomes other than acute neonatal or maternal infection.
Antibiotics for Preterm Premature Rupture of Fetal Membranes
Although antibiotics have been unsuccessful for the treatment of women with intact membranes, adjunctive antibiotic therapy is recommended for women who are managed expectantly after preterm premature rupture of membranes (PPROM). (PROM refers to premature rupture of membranes, meaning before the onset of labor at any gestational age; hence, although “preterm PROM” is apparently redundant, it is not, given the definition of PROM, and is abbreviated here PPROM.) Evidence from appropriately conducted placebo-controlled trials has shown that antibiotic treatment can reduce morbidity for infants born after PPROM and prolong the interval from rupture to delivery. A study that compared ampicillin plus erythromycin and placebo (Mercer et al., 1997) demonstrated improved neonatal outcomes (risk of death, respiratory distress syndrome, sepsis, severe intraventricular hemorrhage, and severe necrotizing enterocolitis) in the infants of women receiving antibiotics compared with the neonatal outcomes in women receiving placebo. Another study of 4,826 women with PPROM showed that erythromycin was associated with a prolongation of pregnancy and improved neonatal outcomes (Kenyon et al., 2001b). That trial showed a significant increase in the occurrence of necrotizing enterocolitis in those infants exposed to co-amoxiclav.
A meta-analysis of 14 randomized clinical trials that included more than 6,000 women found that treatment with broad-spectrum antibiotics prolonged latency and led to significant decreases in neonatal infections, positive neonatal blood cultures, the need for surfactant treatment and oxygen therapy, and abnormal ultrasounds before hospital discharge. Although the rate of neonatal mortality was reduced, it was not statistically significant. Antibiotic treatment was also found to be associated with a statistically significant reduction in maternal infection and chorioamnionitis (Kenyon et al., 2004).
Antenatal Corticosteroids
The one intervention that reduces perinatal morbidity and mortality and that is firmly supported by the findings of research is the antenatal
administration of glucocorticoids to women at risk of preterm birth. A 1994 National Institutes of Health Consensus Conference recommended the administration of corticosteroids to women with preterm labor before 34 weeks of gestation and women with PPROM before 32 weeks of gestation by the use of a single course of either betamethasone (two doses of 12 mg intramuscularly administered 24 hours apart) or dexamethasone (four doses of 6 mg intramuscularly administered 12 hours apart). Studies have shown conclusively that the antepartum administration of the glucocorticoids betamethasone or dexamethasone to the mother reduces the risk of death, respiratory distress syndrome, intraventricular hemorrhage, necrotizing entercolitis, and patent ductus arteriosus in the preterm neonate (Crowley, 1999). Other morbidities of preterm birth reduced by antenatal glucocorticoid administration include necrotizing enterocolitis, patent ductus arteriosus, and bronchopulomary dysplasia.
Betamethasone and dexamethasone are apparently equally effective in reducing perinatal morbidity, but there may be some advantage to the use of betamethasone. In a study of infants born between 24 and 31 weeks of gestation, the rate of periventricular leukomalacia was 4.4 percent among 361 infants who were treated antenatally with betamethasone, 11.0 percent among 165 infants who received dexamethasone, and 8.4 percent among 357 infants who were not treated with antenatal corticosteroids (Baud et al., 1999).
Other fetal effects of glucocorticoids have been reported. Transient reductions in fetal breathing and body movements sufficient to affect the interpretation of the biophysical profile have been described after the administration of both drugs but are more common after administration of betamethasone and typically last for 48 to 72 hours after administration of the second dose (Mulder et al., 1997; Rotmensch et al., 1999; Senat et al., 1998). Transient suppression of neonatal cortisol levels has been reported, but the neonatal response to adrenocorticotropin stimulation was unimpaired (Teramo et al., 1980; Terrone et al., 1997, 1999). Neonatal leukocyte counts are not affected by antenatal steroid administration (Zachman et al., 1988). Although maternal adrenal suppression has been described with repeated courses of antenatal steroids, the adrenal suppression had no clinical consequences (Wapner et al., 2005).
Concern about whether corticosteroids given to women with ruptured membranes might increase the risk of neonatal infection has been addressed by reports that found no such association (Harding et al., 2001; Lewis et al., 1996). Harding and colleagues (2001) found no evidence of increased maternal infections (RR 0.86; 95% CI 0.61–1.2) or neonatal infections (RR 1.05; 95% CI 0.66–1.68) in a meta-analysis of steroid treatment of women with PPROM.
The duration of the beneficial effects on the fetus after the administra-
tion of a single course of glucocorticoids is not clear. The issue is difficult to study because the interval between treatment and delivery in clinical trials varies and because some effects may be transient, whereas others are permanent. The benefit to the neonate has been most easily observed when the interval between the first dose and delivery exceeds 48 hours, but some benefit is evident after an incomplete course. One large multicenter trial (Gamsu et al., 1989) found evidence of a benefit for as long as 18 days after the initial course of treatment.
The increasing use of repeated courses of antenatal steroid treatment prompted animal and human studies that have raised concerns about the effects of prolonged exposure to steroids on fetal growth and neurological function. The animal studies showed reduced fetal growth and adverse brain and neurological development and a pattern of decreased fetal growth in several species (Aghajafari et al., 2002; Cotterrell et al., 1972; Huang et al., 1999; Jobe et al., 1998; Quinlivan et al., 2000; Stewart et al., 1997).
Human studies also found reduced growth in fetuses exposed to multiple courses of antenatal steroids. An Australian study found a twofold increase in the numbers of infants with birth weights below the 10th percentile and a significantly reduced head circumference in infants exposed to more than three antenatal courses of steroids (French et al., 1999). A reduced head circumference was also reported in other studies (Abbasi et al., 2000). These reports led NICHD to reconvene the Consensus Conference Panel in August 2000 to review the available information about repeated courses of steroids. That panel reemphasized the benefit and safety of a single course of antenatal corticosteroids (given either as two intramuscular doses of 12 mg 24 hours apart or four doses of dexamethasone every 12 hours) for women between 24 and 34 weeks of gestation who are deemed to be at risk of preterm delivery within 7 days. The panel noted data suggesting a benefit for repeat courses of steroids, but in the absence of appropriate clinical studies, the panel recommended that “repeat courses of corticosteroids … should not be used routinely … [but] should be reserved for patients enrolled in randomized controlled trials” (NIH, 2001, p. 146).
Five prospective, randomized, clinical trials of repeat antenatal corticosteroids in humans have been performed. Three (Guinn et al., 2001; Mercer et al., 2001a,b; Wapner, 2003) have been reported in articles or abstracts, and two (Australian and Canadian trials) are ongoing or have not yet been described. Guinn and colleagues (2001) enrolled 502 women who had received one course of steroids to receive betamethasone once weekly or no further treatment. There was no difference in the composite rates of morbidity (defined as severe respiratory distress syndrome, bronchopulmonary dysplasia, severe intraventricular hemorrhage, periventricular leukomalacia, sepsis, necrotizing enterocolitis, or death) in the two groups (22.5 and 28.0 percent, respectively; p = 0.16). There was a reduction in the
rate of severe respiratory distress syndrome (15.3 and 24.1 percent, respectively; p = 0.01) and composite morbidity (96.4 and 77.4 percent, respectively; p = 0.03) in infants treated repeatedly if they were delivered at between 24 and 27 weeks of gestation.
Another trial (Mercer et al., 2001a,b) compared weekly betamethasone to rescue treatment from enrollment through 34 weeks of gestation. Notably, only 37 percent of women assigned to receive rescue steroids were so treated, indicating the difficulty in predicting imminent preterm delivery. More than 75 percent of the women in the weekly treatment group received corticosteroids within a week of preterm birth (p = 0.001) (Mercer et al., 2001a). The NICHD MFMU Network Study (Wapner, 2003) randomized 495 women, of whom 492 (591 infants) were available for analysis and 252 received repetitive steroids. The trial was stopped by the independent data and safety monitoring board before the planned sample size was reached because of slow enrollment. The investigators found no difference in the primary (composite) outcome for infants who were exposed to multiple courses compared with that for infants who received placebo (7.7 and 9.2 percent, respectively; p = 0.67). Trends toward improvement were seen in the group receiving multiple courses of steroids for each component of the primary outcome and for secondary outcomes related to lung function: use of surfactant (12.5 and 18.4 percent, respectively; p = 0.02), mechanical ventilation (15.5 and 23.5 percent, respectively; p = 0.005), and treatment for hypotension (5.7 and 11.2 percent, respectively; p = 0.02). Among infants delivered before 32 weeks of gestation, the composite morbidities1 included in the primary outcome were less common in the group receiving multiple courses of steroids (21.3 and 38.5 percent, respectively; p = 0.083). Multiple courses of steroid treatment were associated with insignificant trends toward reduced infant weight (2,194 and 2,289 grams for the treatment and placebo groups, respectively; p = 0.09) and length (44.2 and 44.7 cm for the treatment and placebo groups, respectively; p = .09). Infants exposed to four or more courses of steroids had a significant decrease in birth weight (2,396 and 2,561 grams for the treatment and placebo groups, respectively; p = 0.01) (Wapner, 2003).
Other Antenatal Treatments to Reduce Fetal Morbidity
Respiratory distress Several alternative approaches to reducing the rate of occurrence of neonatal respiratory distress syndrome that are used before
and after birth have been studied. Neonatal treatment with surfactant is an effective adjunctive therapy that adds independently and synergistically to the benefit offered by corticosteroids in reducing respiratory distress syndrome-related morbidity (St. John and Carlo, 2003). The use of antenatal thyrotropin-releasing hormone (TRH) to reduce neonatal lung disease has been studied in trials that enrolled more than 4,600 women. TRH did not improve any neonatal outcome when TRH treatment was compared with corticosteroid treatment alone and actually increased the risk of poor outcomes for the infants in some trials (Crowther et al., 2004).
Neurological morbidity Antenatal maternal treatment with phenobarbital, vitamin K, and magnesium sulfate has been studied as a means of reducing or preventing neonatal neurological morbidity. Phenobarbital did not decrease intraventricular hemorrhage when it was given alone (Shankaran et al., 1997) or in combination with vitamin K (Thorp et al., 1995). Antenatal maternal treatment with magnesium has also been studied after observational reports found reduced rates of intraventricular hemorrhage, cerebral palsy, and perinatal mortality in premature infants exposed to antenatal magnesium (Grether et al., 1998, 2000; Mittendorf et al., 1997; Nelson and Grether, 1995; Paneth et al., 1997; Schendel et al., 1996). A randomized placebo-controlled trial of antenatal magnesium conducted with 1,062 women who delivered before 30 weeks of gestation found that magnesiumtreated infants had significantly improved gross motor dysfunction and a trend suggesting a lower rate of cerebral palsy at 2 years of age (Crowther et al., 2003). No significant adverse effects were noted in infants exposed to antenatal magnesium sulfate in this study. The NICHD- and National Institute of Neurological Disorders and Stroke-Sponsored MFMU Network’s BEAM Trial (Randomized Clinical Trial of the Beneficial Effects of Antenatal Magnesium Sulfate) has concluded enrollment and will report on the outcomes for the infants in 2007, when the infants will be 2 years old.
Maternal Transfer
Many states have adopted systems of regionalized perinatal care, in recognition of the advantages of concentrating care for preterm infants, especially those born before 32 weeks of gestation. Hospitals and birth centers caring for healthy mothers and infants are typically designated Level I. Larger hospitals that care for the majority of maternal and infant complications are designated Level II centers; these hospitals have neonatal intensive care units staffed and equipped to care for most infants with birth weights between 1,250 and 1,500 grams. Level III centers typically provide care for the sickest and the smallest infants and for maternal complications requiring intensive care. The use of this approach has been associated with
improved outcomes for preterm infants (Towers et al., 2000; Yeast et al., 1998) (see Chapters 10 and 14 for further discussion).
FUTURE DIRECTIONS
Despite several interventions designed to inhibit preterm labor and prolong pregnancy, the frequency of preterm birth continues to pose a major barrier to the health of newborns worldwide. Although current obstetric and neonatal strategies have resulted in improved rates of neonatal survival and an earlier threshold for viability, effective strategies for prevention of preterm birth are urgently needed. As basic and translational research continues to reveal more of the complex endocrinological and immunological aspects of parturition, investigators must continue to search for biologically plausible new therapies to prevent preterm birth and develop markers or multiple markers to diagnose the syndrome accurately in its early stages.

















































